Contents
- What is a pituitary tumor
- The pituitary gland
- Pituitary tumors complications
- Pituitary tumor causes
- Pituitary tumors prevention
- Pituitary tumor signs and symptoms
- Large pituitary tumors (macroadenomas) and pituitary carcinomas
- Growth hormone-secreting adenomas (somatotroph adenomas)
- Corticotropin (ACTH)-secreting adenomas (corticotroph adenomas)
- Prolactin-secreting adenomas (prolactinomas or lactrotroph adenomas)
- Thyrotropin (TSH)-secreting adenomas (thyrotroph adenomas)
- Gonadotropin-secreting adenomas (gonadotroph adenomas)
- Can pituitary tumors be found early?
- Pituitary tumor diagnosis
- Medical history and physical exam
- Blood and urine tests of hormone levels
- Somatotroph adenoma (growth hormone-secreting pituitary tumor)
- Corticotroph adenoma (corticotropin or ACTH-secreting pituitary tumor)
- Lactotroph adenoma (prolactin-secreting pituitary tumor) (also called a prolactinoma)
- Gonadotroph adenoma (gonadotropin-secreting pituitary tumor)
- Thyrotroph adenoma (thyrotropin-secreting pituitary tumor)
- Null cell adenoma (non-functional pituitary tumor)
- Testing for diabetes insipidus
- Venous blood sampling
- Imaging tests
- Tests of pituitary tissue samples
- Pituitary tumor staging
- Pituitary tumor treatment
What is a pituitary tumor
A pituitary tumor (also called pituitary adenoma) is a mass of cells that grow on the pituitary gland. Almost all pituitary tumors are benign (not cancer) glandular tumors called pituitary adenomas. These pituitary tumors are called benign because they don’t spread to other parts of the body, like cancers can. Still, even benign pituitary tumors can cause major health problems because they are close to the brain, may invade nearby tissues (like the skull or the sinuses), and because many of them make excess hormones. Some pituitary tumors release hormones, although most do not.
One of the key issues with pituitary tumors is that there’s currently no way to know if a benign pituitary adenoma will become pituitary cancer and grow and spread to other parts of the body. Pituitary cancers (called pituitary carcinomas) are very rare.
About 10,000 pituitary tumors are diagnosed each year in the United States. Almost all of these tumors are benign pituitary adenomas. Very few pituitary tumors are cancers (carcinomas).
The actual number of pituitary tumors may be much higher than the number of tumors that are found each year. When examining people who have died or who have had imaging tests (like MRI scans) of their brain for other health problems, doctors have found that as many as 1 out of 4 people may have a pituitary adenoma without knowing it. These tumors are often small and never cause any symptoms or health problems, so very few of them would normally be diagnosed at all.
Pituitary tumors can occur at any age (including in children), but they are most often found in older adults.
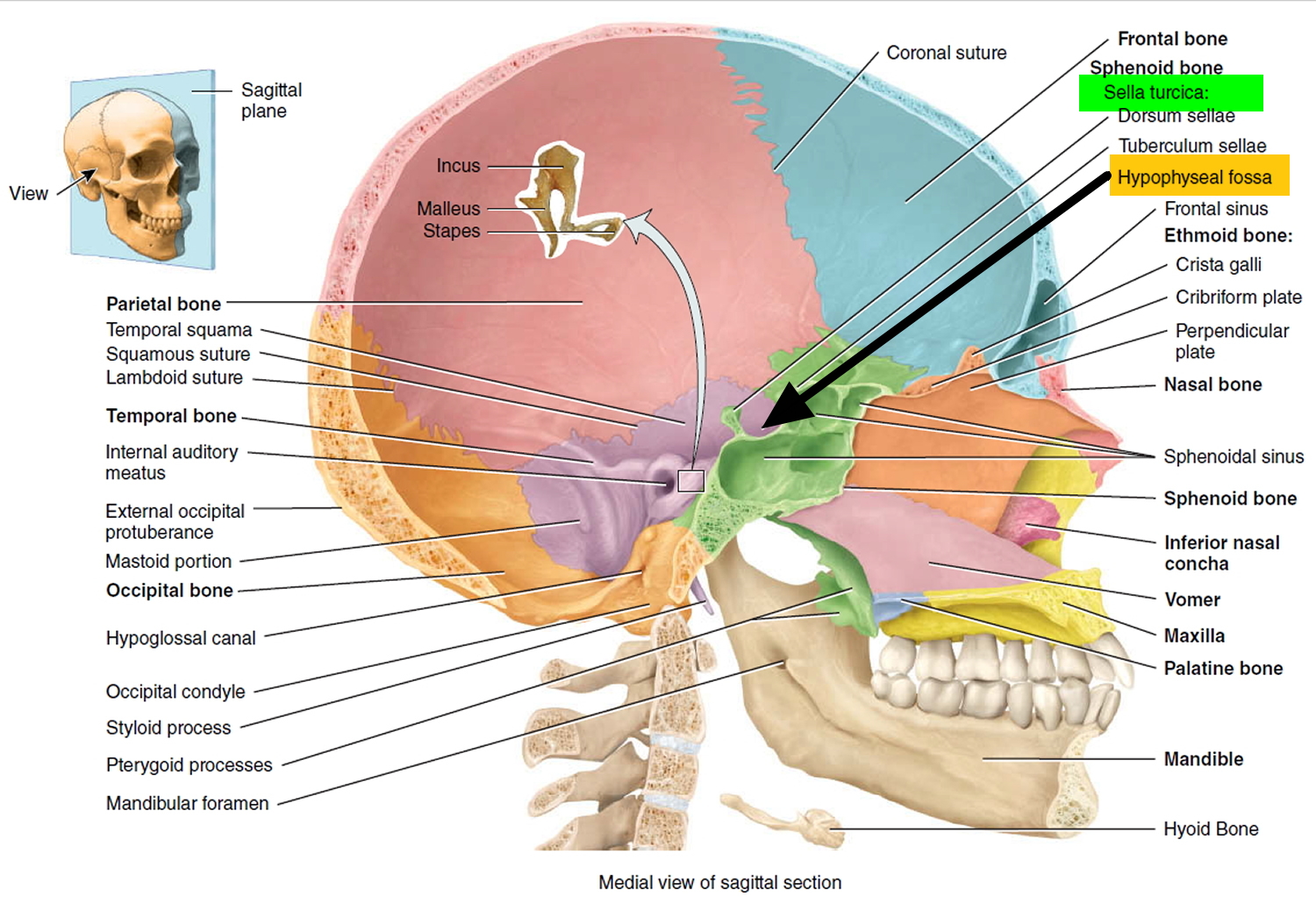
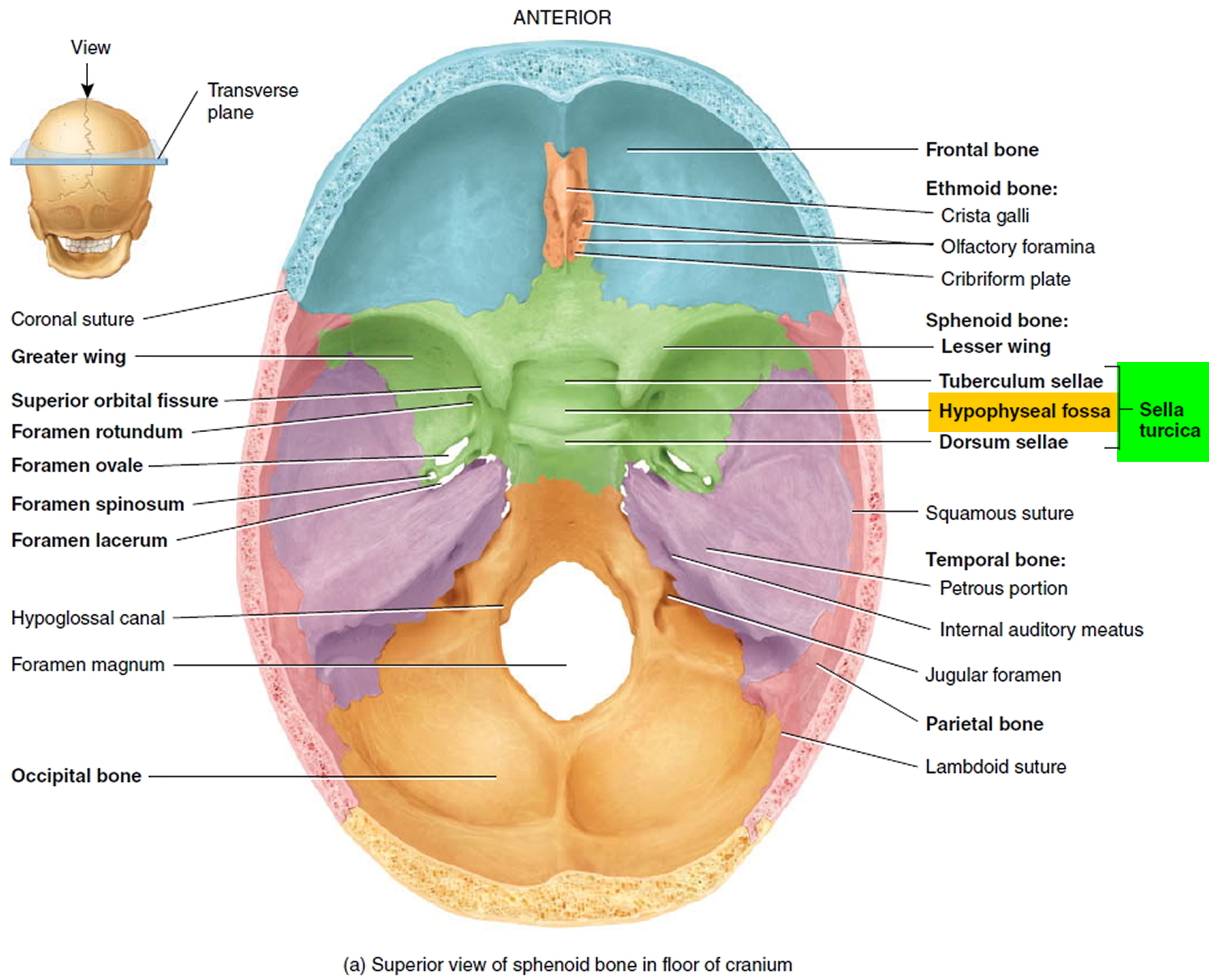
These benign pituitary tumor do not spread outside the skull, so there is no chance of secondary tumors developing. They usually stay in the sella turcica (the tiny space in the skull that the pituitary gland sits in). Sometimes they grow into the boney walls of the sella turcica and nearby tissues, like blood vessels, nerves, and sinuses. They don’t grow very large, but they can have a big impact on a person’s health.
There is very little room for tumors to grow in this part of the skull. So, if the tumor gets larger than about a centimeter (about half an inch) across, it may grow upward, where it can press on and damage nearby parts of the brain and the nerves that arise from it. This can lead to problems like vision changes or headaches.
Not all pituitary tumors cause symptoms. Pituitary tumors that make hormones (functioning) can cause a variety of signs and symptoms depending on the hormone they produce. The signs and symptoms of pituitary tumors that don’t make hormones (nonfunctioning) are related to their growth and the pressure they put on other structures.
Signs and symptoms of pressure from a pituitary tumor may include:
- Headache
- Vision loss, particularly loss of peripheral vision
Pituitary adenomas can be divided into 2 categories based on size:
- Microadenomas are pituitary tumors that are smaller than 1 centimeter (cm) across. Because these tumors are small, they rarely damage the rest of the pituitary or nearby tissues. But they can cause symptoms if they make too much of a certain hormone. Many people actually have small adenomas that are never found because they don’t grow large enough or make enough hormones to cause a problem.
- Macroadenomas are pituitary tumors 1 cm across or larger. Macroadenomas can affect a person’s health in 2 ways. First, they can cause symptoms if they make too much of a certain hormone. Second, they can cause symptoms by pressing on normal parts of the pituitary or on nearby nerves, such as the optic nerves.
Large pituitary tumors — those measuring about 1 centimeter (slightly less than a half-inch) or larger — are known as macroadenomas. Smaller tumors are called microadenomas. Because of the size of macroadenomas, they can put pressure on the normal pituitary gland and nearby structures.
Pituitary adenomas are also classified by whether they make too much of a hormone and, if they do, which type they make. If a pituitary adenoma makes too much of a hormone it’s called functional. If it doesn’t make enough hormones to cause problems it’s called non-functional.
Functional adenomas: Most of the pituitary adenomas that are found make excess hormones. The hormones can be detected by blood tests or by tests of the tumor when it is removed with surgery. Based on these results, pituitary adenomas are classified as:
- Lactotroph adenomas make prolactin and account for about 4 out of 10 pituitary tumors.
- Somatotroph adenomas make growth hormones and make up about 2 in 10 pituitary tumors.
- Corticotroph adenomas make ACTH and account for about 1 in 10 pituitary tumors.
- Gonadotroph adenomas make LH and FSH and are very rare.
- Thyrotroph adenomas make TSH and are very rare.
- Plurihormonal adenomas make more than one hormone.
- Null cell adenomas do not make hormones. (These are non-functional adenomas.)
The kind of hormone an adenoma makes strongly affects what signs and symptoms it causes. It also affects which tests are used for diagnosis, the choice of treatment, and the patient’s outlook.
Non-functional adenomas: Pituitary adenomas that don’t make excess hormones are called non-functional adenomas or null cell adenomas. They account for about 3 in 10 of all pituitary tumors that are found. They are usually found as macroadenomas, causing symptoms because of their size as they press on nearby structures.
Pituitary carcinomas
Cancers of the pituitary gland are rare. Only a few hundred have ever been described in medical journals. They can occur at any age, but most are found in older people. These cancers usually make hormones, just like many benign pituitary adenomas do.
Pituitary carcinomas look like pituitary adenomas (benign pituitary tumors) under a microscope, so doctors have trouble telling them apart. In fact, the only way to tell if a pituitary tumor is a carcinoma and not an adenoma is when the tumor spreads to another part of the body not near the pituitary gland. Most often pituitary carcinoma spreads to the brain, spinal cord, meninges (the covering of the brain and spinal cord), or bone around the pituitary. Rarely, these cancers spread to other organs such as the liver, heart, or lungs.
Other tumors of the pituitary region
There are several other types of benign tumors that grow in the region of the pituitary, as well as some malignant (cancerous) ones. All are much less common than pituitary adenomas.
Teratomas, germinomas, and choriocarcinomas are all rare tumors that usually occur in children or young adults. They don’t develop from the hormone-making cells of the pituitary gland itself, but they can grow into the pituitary and damage it.
Rathke cleft cysts and gangliocytomas of the pituitary are rare tumors that are usually found in adults.
Craniopharyngiomas are slow-growing tumors that start above the pituitary gland but below the brain itself. They sometimes press on the pituitary and the hypothalamus, causing hormone problems. They’re more common in children, but they can be seen in older adults.
Cancers that start in some other parts of the body (like the breast) can sometimes spread to the pituitary. These cancers are classified and treated based on where they started (their primary site) and are not thought of as pituitary tumors.
Pituitary tumors treatment may include surgery, radiation therapy and controlling pituitary tumor growth and managing your hormone levels with medications.
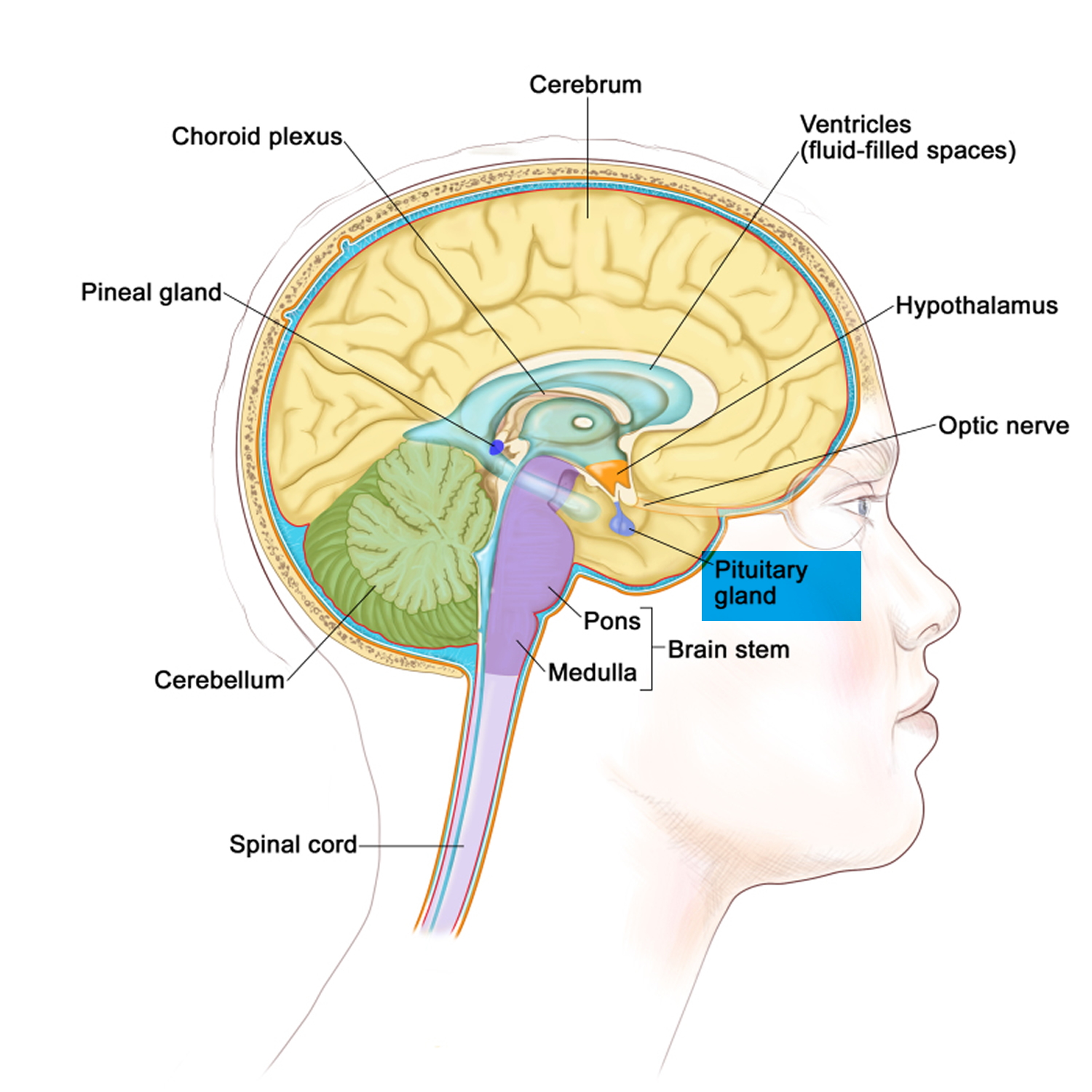
The pituitary gland
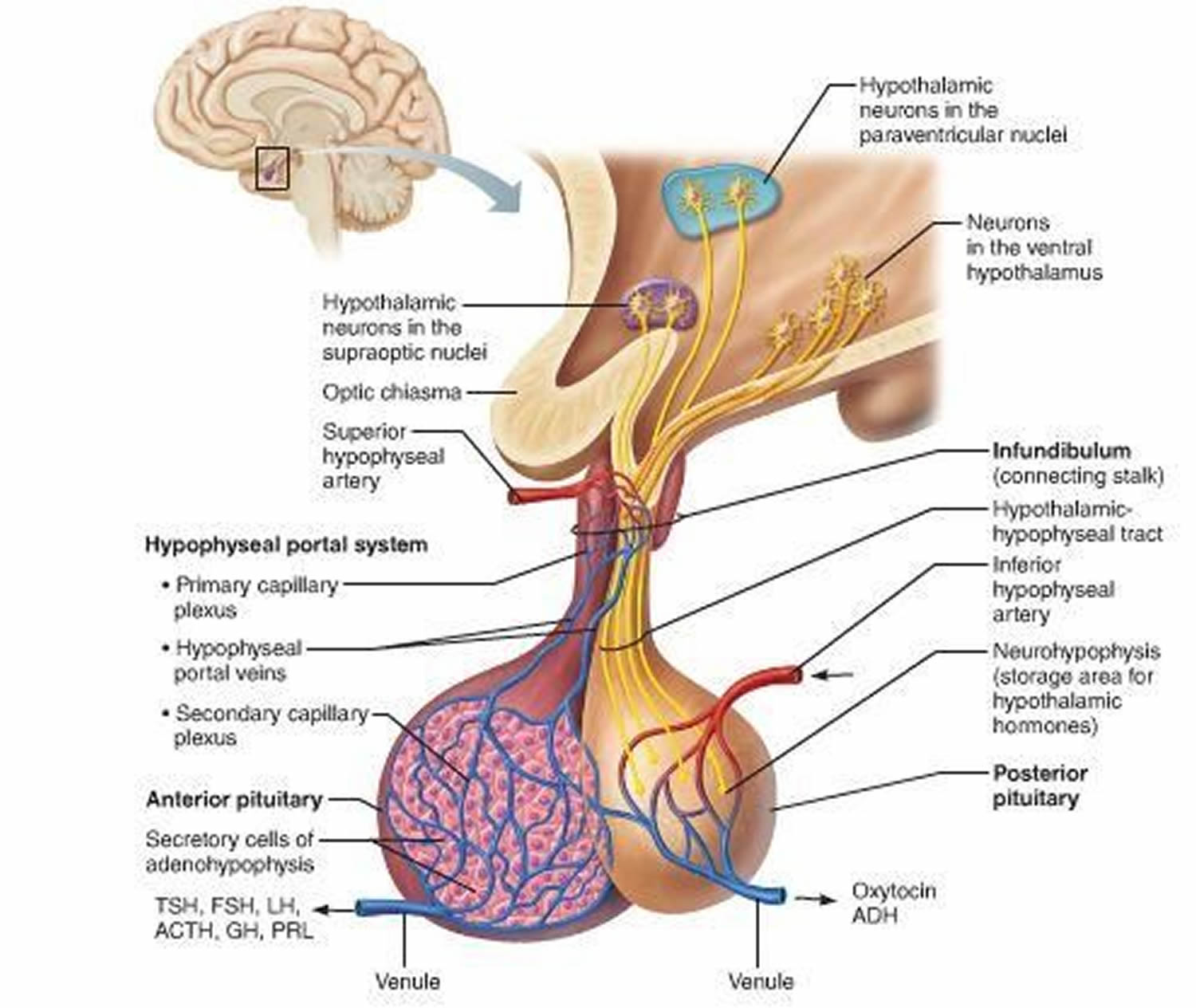
The pituitary gland (hypophysis) is located at the base of the brain and above the nasal passages, which are above the fleshy back part of the roof of the mouth (known as the soft palate), where a pituitary stalk (infundibulum) attaches it to the hypothalamus. The pituitary gland sits in a tiny bony space called the sella turcica. The nerves that connect the eyes to the brain, called the optic nerves, pass close by it.
The pituitary gland is about 1 centimeter in diameter and consists of an anterior pituitary or anterior lobe, and a posterior pituitary, or posterior lobe. The pituitary stalk (infundibulum) contains both blood vessels and nerves. The hypothalamus releases hormones into tiny blood vessels connected to the pituitary gland (see Figure 2). These then cause the pituitary gland to make its own hormones. The pituitary is considered the “master control gland” because it makes the hormones that control the levels of hormones made by most of the other endocrine glands in the body. The pituitary gland controls a system of hormones in the body that regulate growth, metabolism, the stress response, and functions of the sex organs via the thyroid gland, adrenal gland, ovaries, and testes.
The pituitary gland has 2 parts, the anterior pituitary and the posterior pituitary. Each has distinct functions.
Anterior pituitary
Most pituitary tumors start in the larger, front part of the pituitary gland known as the anterior pituitary. This part of the gland makes these hormones that control other endocrine glands:
- Growth hormone (GH, also known as somatotropin) promotes body growth during childhood. If too much is made in a child they will grow very tall. Normally, adults make only small amounts of growth hormone. If an adult makes too much growth hormone, the bones of the hands, feet, and face continue to grow and become quite large, causing their normal features to become distorted. (This condition is called acromegaly.)
- Thyroid-stimulating hormone (TSH, also called thyrotropin) stimulates growth of the thyroid gland and the release of thyroid hormone. Thyroid hormone regulates metabolism. Too much makes you hyperactive and shaky, and too little makes you sluggish. If a pituitary tumor makes too much TSH, it can cause hyperthyroidism (an overactive thyroid gland).
- Adrenocorticotropic hormone (ACTH, also known as corticotropin) causes the adrenal glands to grow and to make steroid hormones (such as cortisol). Too much ACTH from the pituitary causes Cushing’s disease, the symptoms of which can include rapid weight gain and the build-up of fat in certain parts of the body.
- Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) are also called gonadotropins. In women their main effects are on the ovaries, where they control ovulation (the release of eggs) and the production of the hormones estrogen and progesterone. In men, LH and FSH control testosterone and sperm production in the testicles.
- Prolactin causes milk production in the female breast. Its function in men is not known.
Posterior pituitary
The smaller, back part of the pituitary gland, called the posterior pituitary, is really an extension of brain tissue from the hypothalamus. The posterior pituitary is where hormones made by the hypothalamus (vasopressin and oxytocin) are stored and released into the bloodstream.
- Vasopressin (also called antidiuretic hormone, or ADH) causes the kidneys to keep water in the body and not lose it all in the urine. Without vasopressin, a person urinates too much and becomes dehydrated. This condition is called diabetes insipidus. Vasopressin also can raise blood pressure by causing blood vessels to constrict. It might have other functions as well.
- Oxytocin causes the uterus to contract in women during childbirth and the breasts to release milk when a woman nurses her baby. It might have other functions in both men and women.
Tumors rarely start in the posterior pituitary.
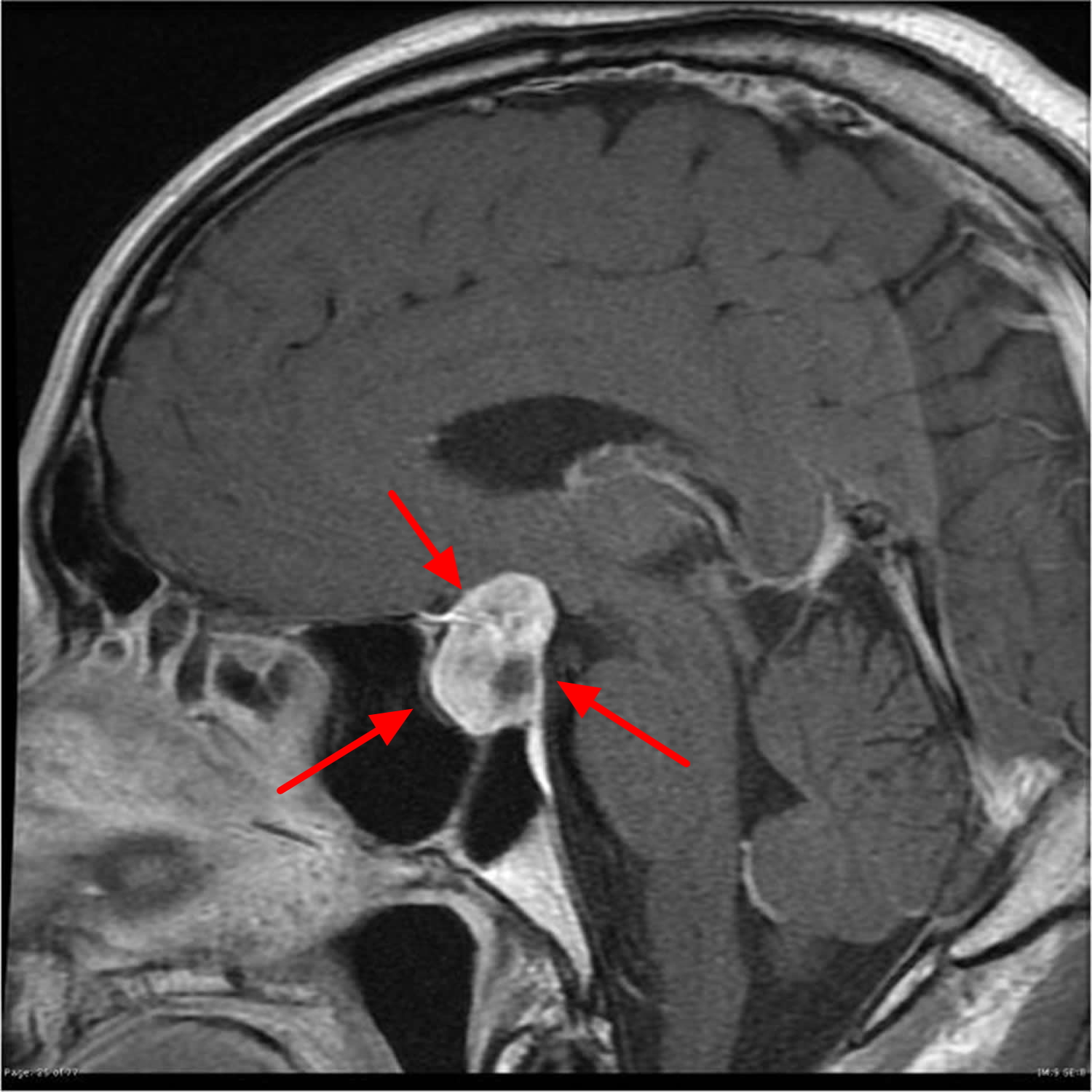
Figure 1. The pituitary gland location
Figure 2. Pituitary gland
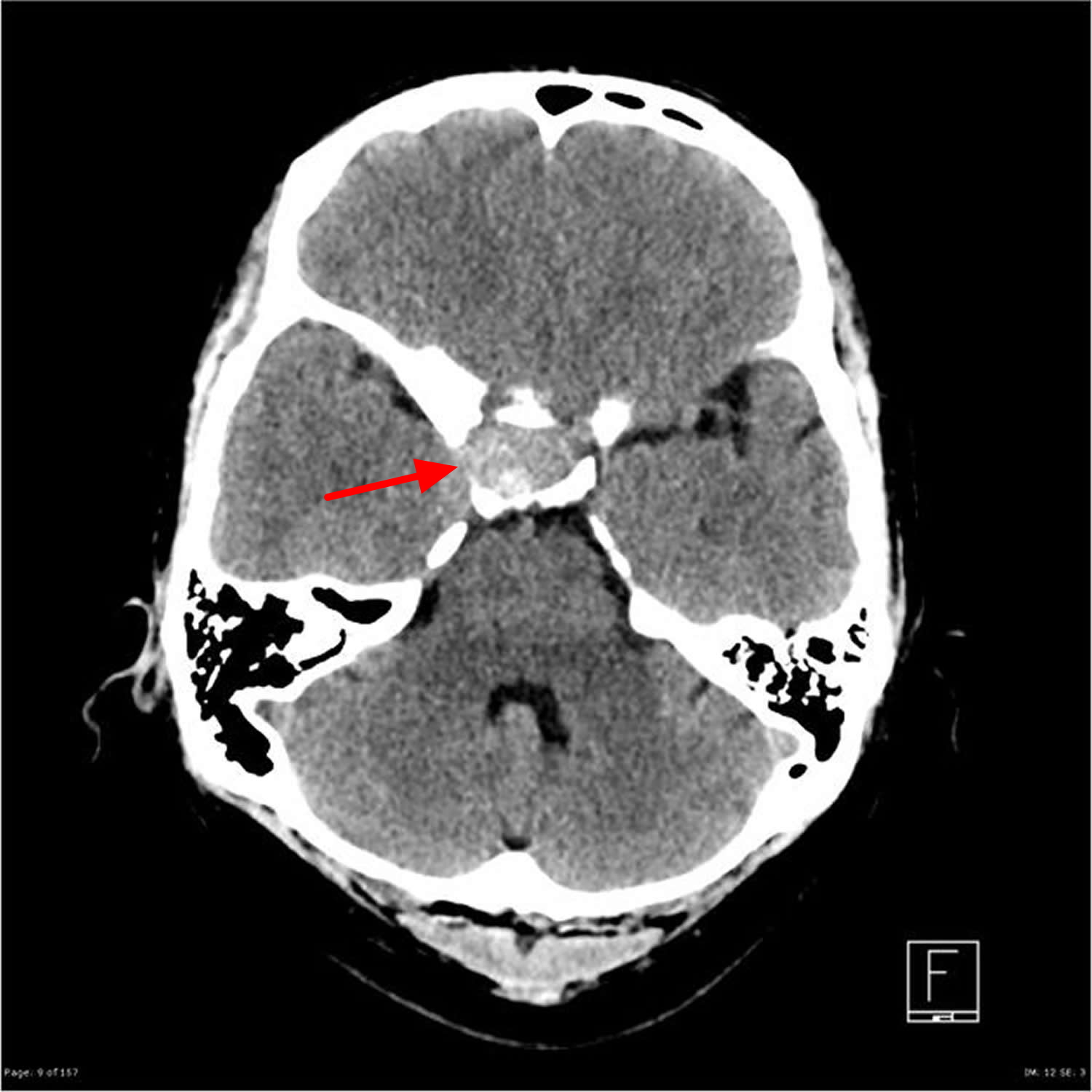
Figure 3. Pituitary tumor MRI
Pituitary tumors complications
Pituitary tumors usually don’t grow or spread extensively. However, they can affect your health, possibly causing:
- Vision loss. A pituitary tumor can put pressure on the optic nerves.
- Permanent hormone deficiency. The presence of a pituitary tumor or the removal of one may permanently alter your hormone supply, which may need to be replaced with hormone medications.
A rare but potentially serious complication of a pituitary tumor is pituitary apoplexy, when sudden bleeding into the tumor occurs. It feels like the most severe headache you’ve ever had. Pituitary apoplexy requires emergency treatment, usually with corticosteroids and possibly surgery.
Pituitary tumor causes
Scientists don’t know exactly what causes most pituitary tumors. During the past few years, they have made great progress in understanding how certain changes in a person’s DNA can cause cells in the pituitary to produce a tumor. DNA is the chemical in each of our cells that makes up our genes – the instructions for how our cells function. We usually look like our parents because they are the source of our DNA. But DNA affects more than how we look.
Some genes control when cells grow, divide into new cells, and die. Genes that help cells grow, divide, and stay alive are called oncogenes. Genes that slow down cell division or cause cells to die at the right time are called tumor suppressor genes. Tumors can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes.
Some people inherit gene mutations (changes) from their parents that greatly increase their risk for developing pituitary tumors.
But often, gene mutations occur during life rather than having been inherited. In some types of cancer, these acquired mutations can be caused by outside exposures, such as radiation or cancer-causing chemicals. Most pituitary tumors are not cancers, and there are no known environmental causes for these tumors. The gene changes in these tumors might just be random events that sometimes happen when a cell divides, without having an outside cause.
Some non-hereditary (sporadic) pituitary tumors – those that don’t run in families – have acquired mutations in a gene called AIP. Many growth hormone-secreting adenomas have an acquired mutation in a gene called GNAS1. These mutations are much less common in other types of pituitary adenomas.
Changes in other genes have been found in other types of pituitary adenomas, but it’s not clear if abnormal genes are always needed for pituitary tumors to form. What is known is that there is a loss of the regulatory mechanism that normally keeps the pituitary cells from growing and making too much hormone.
Because there are no known lifestyle-related or environmental causes of pituitary tumors, it’s important to remember that there is nothing people with these tumors could have done to prevent them.
Risk Factors for pituitary tumors
A risk factor is anything that changes a person’s chance of getting a disease. For example, smoking is a risk factor for cancer of the lung and many other cancers.
But having a risk factor, or even many risk factors, does not mean that you will get the disease. And many people who get the disease may have few or no known risk factors.
Pituitary tumors have very few known risk factors, and these are related to genetics. There are no known environmental or lifestyle-related risk factors for pituitary tumors. Though science has suggested that people who are overweight or obese might be at increased risk.
Family history
Most people who develop pituitary tumors don’t have a family history of the disease. But rarely, pituitary tumors can run in families.
Sometimes when pituitary tumors run in families, they are found along with other types of tumors as part of an inherited genetic syndrome (see the next section).
Sometimes, though, only pituitary tumors occur. Researchers have found that some of these are due to certain changes in a person’s genes that are inherited from a parent.
Most often, though, the cause of pituitary tumors that run in families is not known.
Genetic syndromes
Pituitary tumors can be a part of a syndrome that includes an increased risk of other types of tumors. These syndromes are caused by abnormal changes (mutations) in a person’s genes. They include:
- Multiple endocrine neoplasia, type I (MEN1): This is a hereditary condition in which people have a very high risk of developing tumors of 3 glands: the pituitary, parathyroid, and pancreas. It is caused by changes in the gene MEN1, and is passed on to about half of the children of an affected parent. If the MEN1 syndrome affects your family, you should discuss testing for this condition with your doctor.
- Multiple endocrine neoplasia, type IV (MEN4): This rare syndrome includes increased risks of pituitary tumors and certain other tumors. MEN4 is caused by inherited changes in a gene called CDKN1B.
- McCune-Albright syndrome: This syndrome is caused by changes in a gene called GNAS1 that aren’t inherited but occur before birth. People with this syndrome have brown patches on their skin (called café-au-lait spots) and develop many bone problems. They can also have hormone problems and pituitary tumors.
- Carney complex: This is a rare syndrome in which people can have heart, skin, and adrenal problems. They also have a high risk of a number of different types of tumors, including pituitary tumors. Many cases are caused by inherited changes in the gene PRKAR1A, but some are caused by changes in other genes that have not yet been identified.
Pituitary tumors prevention
The risk of many types of cancer can be reduced with certain lifestyle changes (such as staying at a healthy weight or quitting smoking). But pituitary tumors have not been linked with any known outside risk factors. As a result, there is no known way to prevent these tumors at this time.
Still, for people at high risk of pituitary tumors (because of certain inherited syndromes), there may be ways to find and treat them early, before they cause problems.
Pituitary tumor signs and symptoms
Not all pituitary tumors (pituitary adenomas) cause symptoms. But when they do, pituitary tumors can cause many different types of symptoms. The first signs of a pituitary tumor often depend on whether the tumor is functional (making excess hormones) or non-functional (not making excess hormones).
Functional pituitary tumors can cause problems because of the hormones they release. Most of the time, a functional pituitary tumor makes too much of a single pituitary hormone. These pituitary tumors are often found while they are still fairly small (microadenomas). Symptoms from functional pituitary tumors are described below, based on which hormone they make.
Pituitary tumors that aren’t making excess hormones (non-functional pituitary adenomas) often become large (macroadenomas) before they are noticed. These pituitary tumors don’t cause symptoms until they press on nearby nerves, parts of the brain, or other parts of the pituitary.
Non-functioning pituitary tumor
This is the most common pituitary tumor and doesn’t release any hormones. Symptoms are caused by a deficiency in the normal pituitary hormones (because the tumor restricts the function of the normal gland), or by pressure on surrounding structures near the pituitary.
Some of the symptoms of a non-functioning pituitary tumor include:
- general fatigue and feeling unwell
- persistent headaches
- menstrual cycle irregularities
- loss of peripheral vision
- loss of libido.
Non-functional pituitary tumors that cause no symptoms are sometimes found because of an MRI or CT scan done for other reasons. These pituitary tumors are now being found more often as more MRI and CT scans of the brain are done. These might be the most common pituitary tumors. As long as they aren’t causing problems, they’e often just watched closely without needing treatment.
Large pituitary tumors (macroadenomas) and pituitary carcinomas
Pituitary macroadenomas (benign pituitary tumors larger than 1 cm) and carcinomas (pituitary cancers), whether functional or not, can be large enough to press on nearby nerves or parts of the brain. This can lead to symptoms such as:
- Eye muscle weakness so the eyes don’t move in the same direction at the same time
- Blurred or double vision
- Loss of peripheral vision (giving you ‘tunnel vision’) or (rarely) double vision
- Sudden blindness
- Headaches
- Facial numbness or pain
- Dizziness
- Loss of consciousness (passing out)
Vision problems occur when the pituitary tumor “pinches” the nerves that run between the eyes and the brain. Sudden loss of vision, loss of consciousness, and even death can result from sudden bleeding into the tumor.
Benign pituitary tumors and pituitary carcinomas (pituitary cancers) can also press on and destroy the normal parts of the pituitary gland. This causes a shortage of one or more pituitary hormones. Low levels of some body hormones such as cortisol, thyroid hormone, and sex hormones cause symptoms. Depending on which hormones are affected, symptoms might include:
- Nausea
- Weakness
- Unexplained weight loss or weight gain
- Loss of body hair
- Feeling cold
- Feeling tired or weak
- Menstrual changes or loss of menstrual periods in women
- Erectile dysfunction (trouble with erections) in men
- Growth of breast tissue in men
- Decreased interest in sex, mainly in men
Diabetes insipidus
Large pituitary tumors can sometimes press on the posterior (back) part of the pituitary, causing a shortage of the hormone vasopressin (also called anti-diuretic hormone or ADH). This can lead to diabetes insipidus. In this condition, too much water is lost in the urine, so the person urinates often and becomes very thirsty as the body tries to keep up with the loss of water. If left untreated, this can cause dehydration and altered blood mineral levels, which can lead to coma and even death. Diabetes insipidus is easily treated with a drug called desmopressin, which replaces the vasopressin. Diabetes insipidus is not related to diabetes mellitus, in which people have high blood sugar levels.
Growth hormone-secreting adenomas (somatotroph adenomas)
The major symptoms from these pituitary tumors are caused by having too much growth hormone (GH). These effects are quite different in children and adults.
In children, high growth hormone (GH) levels can stimulate the growth of nearly all bones in the body. The medical term for this condition is gigantism. Signs include:
- Being very tall
- Very rapid growth
- Joint pain
- Increased sweating
In adults, the long bones (especially in the arms and legs) can’t grow any more, even when growth hormone (GH) levels are very high. So they don’t grow taller and develop gigantism. But bones of an adult’s hands, feet, and skull/face can grow throughout life. This causes a condition called acromegaly. Signs and symptoms are:
- Growth of the skull, hands, and feet, leading to increase in hat, shoe, glove, and ring size
- Deepening of the voice
- Change in how the face looks (due to growth of facial bones)
- Wider spacing of the teeth and protruding jaw (due to jawbone growth)
- Joint pain
- Increased sweating
- High blood sugar or even diabetes mellitus
- Kidney stones
- Heart disease
- Headaches
- Vision changes
- Numbness or tingling in the hands or feet
- Thickening of tongue and roof of mouth, leading to sleep disturbances such as snoring and sleep apnea (pauses in breathing)
- Thickened skin
- Increased growth of body hair
Many of these changes can occur very slowly, and people might not notice them until they look at an old picture of themselves or try to put on a hat or ring they haven’t worn in many years.
Corticotropin (ACTH)-secreting adenomas (corticotroph adenomas)
High ACTH levels cause the adrenal glands to make steroid hormones such as cortisol. Having too much of these hormones causes symptoms that doctors group together as Cushing’s syndrome. When the cause is too much ACTH production from the pituitary it’s called Cushing’s disease. In adults, the symptoms can include:
- Unexplained weight gain (mostly in the face, chest, and belly)
- Purple stretch marks on the chest or belly
- New or increased hair growth (on the face, chest, and/or belly)
- Swelling and redness of the face
- Acne
- Extra fat on the back of the neck
- Moodiness or depression
- Headache
- Vision changes
- Easy bruising
- High blood sugar levels or even diabetes mellitus
- High blood pressure
- Decreased interest in sex
- Changes in menstrual periods in women
- Weakening of the bones, which can lead to osteoporosis or even fractures
Most of these symptoms can also occur in children. Children with Cushing’s disease may also stop growing and have problems with school performance.
Prolactin-secreting adenomas (prolactinomas or lactrotroph adenomas)
Prolactinomas are most common in young women and older men.
- In women before menopause, high prolactin levels cause menstrual periods to become less frequent or to stop. High prolactin levels can also cause abnormal breast milk production, called galactorrhea.
- In men, high prolactin levels can cause breast growth and erectile dysfunction (trouble with erections)
- Both men and women can have:
- Loss of interest in sex
- Infertility
- Weakening of the bones called osteoporosis
If the tumor continues to grow, it can press on nearby nerves and parts of the brain, which can cause headaches and vision problems.
In females who don’t have periods such as girls before puberty and women after menopause, prolactinomas might not be noticed until they cause these symptoms.
Thyrotropin (TSH)-secreting adenomas (thyrotroph adenomas)
These rare tumors make too much thyroid-stimulating hormone (TSH), which then causes the thyroid gland to make too much thyroid hormone. This can cause symptoms of hyperthyroidism (overactive thyroid), such as:
- Rapid or irregular heartbeat
- Tremors (shaking)
- Weight loss
- Increased appetite
- Feeling warm or hot
- Sweating
- Trouble falling asleep
- Anxiety
- Frequent bowel movements
- A lump in the front of the neck (enlarged thyroid)
Gonadotropin-secreting adenomas (gonadotroph adenomas)
These rare tumors make luteinizing hormone (LH) and/or follicle-stimulating hormone (FSH). This can cause irregular menstrual periods in women or low testosterone levels and decreased interest in sex in men.
Many gonadotropin-secreting adenomas actually don’t make enough hormones to cause symptoms, so they are basically non-functional adenomas. These tumors may grow large enough to cause symptoms such as headaches and vision problems before they are found.
Can pituitary tumors be found early?
No imaging tests or blood tests are recommended to screen for pituitary tumors in people who are not at increased risk. Screening is testing for tumors in people without any symptoms.
For members of families known to be at increased risk because of a genetic syndrome such as multiple endocrine neoplasia, type I (MEN1), doctors often recommend regular blood testing of pituitary hormone levels. These tests increase the odds of finding a tumor early so that it can be removed completely, increasing the chance for a cure.
Rarely, a pituitary tumor is found early because a person has a CT or MRI scan of the brain for an unrelated problem. These tumors are sometimes referred to as incidentalomas, meaning they are found incidentally (by accident).
Functional pituitary adenomas (tumors that make excess hormones like prolactin or ACTH) are often found when they are still small because the excess hormones cause symptoms.
Non-functional pituitary tumors are less likely to be found early because they don’t cause symptoms until they’ve grown large enough to press on normal pituitary cells, nerves, or parts of the brain near the pituitary.
Pituitary tumor diagnosis
Pituitary tumors are usually found when a person goes to the doctor because of symptoms they’re having. But sometimes these tumors don’t cause symptoms, and they’re found when doing medical tests done for other health problems.
If there’s a reason to suspect you might have a pituitary tumor, your doctor will use one or more tests to find out. Signs and symptoms might suggest that you could have a pituitary tumor, but tests are needed to be sure of the diagnosis and find out what kind of pituitary tumor it is.
Medical history and physical exam
If your symptoms lead your doctor to believe that you might have a pituitary tumor, the first step is take a complete medical history to check for risk factors and to learn more about your symptoms. Your doctor may ask about your family history of tumors or other problems to see if you might have an inherited genetic syndrome, such as multiple endocrine neoplasia, type I (MEN1).
Your doctor will also examine you to look for possible signs of a pituitary tumor or other health problems. This may include exams to look for vision or nervous system problems that could be caused by a tumor.
If a pituitary tumor is strongly suspected, your doctor may refer you to an eye doctor to check your vision, as pituitary tumors can damage nerves leading to the eyes. The most common test is to measure how well you can see. The doctor may also test your field of vision (or visual fields). At first, pituitary tumors only press on part of the optic nerves. This often leads to the loss of peripheral vision, meaning that you can’t see things off to the side without actually looking right at them. Eye doctors have special instruments that can test for this.
You might also be referred to other doctors, such as an endocrinologist (a doctor who treats diseases in glands that secrete hormones) or a neurosurgeon (a doctor who uses surgery to treat brain and pituitary tumors), who might order other tests.
Blood and urine tests of hormone levels
If your doctor suspects you might have a hormone-producing pituitary tumor, hormone levels in your blood and/or urine will be measured.
Somatotroph adenoma (growth hormone-secreting pituitary tumor)
A physical exam may alert the doctor to look for this pituitary tumor because the signs and symptoms are often very distinctive.
The next step is to check the levels of growth hormone and insulin-like growth factor-1 (IGF-1) in your blood samples, which are taken in the morning after an overnight fast. When growth hormone levels are high, they cause the liver to make more IGF-1. Testing the IGF-1 level can be more helpful than checking the level of growth hormone. IGF-1 level doesn’t change much during the day, while the level of growth hormone can go up and down.
If both levels are very high, the diagnosis is clearly a pituitary tumor. If the levels are slightly increased, another test called a glucose suppression test is often done to be sure. You’ll be asked to drink a sugary liquid, then the levels of growth hormone and blood sugar will be measured at certain times. The normal response to suddenly taking in so much sugar is a drop in growth hormone levels. If the growth hormone levels stay high, a pituitary adenoma is likely the cause.
Corticotroph adenoma (corticotropin or ACTH-secreting pituitary tumor)
Most of the signs and symptoms of ACTH-secreting pituitary tumors come from having too much cortisol (an adrenal steroid hormone). But quite a few diseases can cause the body makes too much cortisol, which is called Cushing’s syndrome. If you have symptoms suggesting Cushing syndrome, you’ll need tests to see if it’s caused by a pituitary tumor or something else.
One of the tests used measures the levels of cortisol in your saliva late at night to see if they stay elevated. Cortisol level normally drops at night. Another may include measuring levels of cortisol and ACTH in blood samples taken at different times of the day. You also may be asked to collect all of your urine over a 24-hour period, which is then tested to measure your daily production of cortisol and other steroid hormones. One test involves taking a dose of a powerful, cortisone-like drug called dexamethasone, then checking blood or urine cortisol levels. Often more than 1 of these tests is needed to help distinguish ACTH-secreting pituitary tumors from other diseases, such as adrenal gland tumors, that can cause similar symptoms.
Lactotroph adenoma (prolactin-secreting pituitary tumor) (also called a prolactinoma)
Blood prolactin levels can be measured to check for a prolactinoma.
Gonadotroph adenoma (gonadotropin-secreting pituitary tumor)
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) blood levels can be checked to see if you have a gonadotropin-secreting tumor. Levels of related hormones, such as estrogen, progesterone, and testosterone, are often checked as well.
Thyrotroph adenoma (thyrotropin-secreting pituitary tumor)
Tests to measure blood levels of thyrotropin (TSH) and thyroid hormones can usually identify people with a thyrotropin-secreting adenoma.
Null cell adenoma (non-functional pituitary tumor)
A pituitary adenoma is considered non-functional if it doesn’t make too much of any pituitary hormone. Pituitary hormone levels are not high in people with non-functional tumors. Sometimes, though, blood levels of pituitary hormones may actually be low because the adenoma crowds out the cells that normally make these hormones.
Testing for diabetes insipidus
Diabetes insipidus can occur if the part of the pituitary that stores the hormone vasopressin (ADH) is damaged, which leads to too much water being lost in the urine. This condition can be caused by pituitary macroadenomas (or carcinomas in rare cases), or by tumors starting in parts of the brain or nerves next to the pituitary gland. It can also be a side effect of surgery to treat pituitary tumors or tumors near the pituitary gland.
In many cases, this diagnosis is made with tests that measure the amount of urine made over a 24-hour period, sodium and glucose levels in the blood, and osmolality (total salt concentration) of the blood and urine. If these test results are not clear, then a water deprivation study may be done. In this test, you are not allowed to drink fluids for several hours. The test is often done overnight. If your body is not making enough vasopressin, you’ll continue to make urine even though you are not taking in any fluid. You may also be given an injection of vasopressin to see if this corrects the problem.
Venous blood sampling
Corticotroph (ACTH-secreting) adenomas may be too small to be seen on imaging tests such as MRI scans. When the ACTH level is high, but a person’s MRI is normal, a special blood test may be useful to find the tumor.
For this test , catheters (long, soft, small tubes) are put into veins on each inner thigh through tiny cuts in the skin and are guided all the way up into the petrosal sinuses near the base of the brain. The sinuses hold 2 small veins that drain the blood from each side of the pituitary gland. Blood is taken from these 2 veins and your arm. Then an injection of corticotropin-releasing hormone (CRH, a hormone from the hypothalamus that normally causes the pituitary to make ACTH) is given. Blood samples are taken again to see if the ACTH level goes up a lot, or is higher on one side than the other. If it is, the source of the high ACTH level is a pituitary tumor.
Imaging tests
Imaging tests use x-rays, magnetic fields, or other means to create pictures of the inside of your body. They may be done to look for pituitary tumors or to see if they have grown into nearby structures. In some cases, an imaging test of the head done for another reason may show a pituitary tumor.
Magnetic resonance imaging (MRI) scan
MRI scans use radio waves and strong magnets to create detailed pictures of the inside of the body.
They are very helpful in looking at the brain and spinal cord and are considered to be the best way to find pituitary tumors of all types. MRI images are usually more detailed than those from CT scans (see below). They can show macroadenomas of the pituitary gland, as well as most microadenomas. But MRI might not detect microadenomas that are smaller than 3 mm (about 1/8 inch) across. Sometimes the MRI scan will show a small change in the pituitary that has nothing to do with the patient’s symptoms. Between 5% and 25% of healthy people have some minor abnormality of the pituitary gland that shows up on an MRI scan.
Computed tomography (CT) scan
A CT scan uses x-rays to create detailed cross-sectional images of part of your body. CT scans can find a pituitary adenoma if it’s large enough, but MRI scans are used much more often to look at the brain and pituitary gland.
Tests of pituitary tissue samples
In diagnosing tumors of most parts of the body, imaging tests and blood tests may strongly suggest a certain type of tumor, but a biopsy (removing a sample of the tumor to examine under a microscope) is usually the only way to be certain of the diagnosis. In many cases, doctors won’t treat a tumor until a biopsy has been done.
But a biopsy isn’t usually needed before treating a pituitary tumor. One reason is that the hormone tests for some types of adenomas are very accurate, so a biopsy isn’t likely to provide much more information. Biopsies in this part of the body can also pose a very small risk of serious side effects. On top of this, some types of adenomas can be treated without surgery, using medicines or radiation therapy.
When pituitary tumors are removed by surgery, they’re examined under a microscope to determine their exact type. Special stains may be used on the tumor to color the areas making hormones and other tests may be done, too. This helps classify the tumor.
Pituitary tumor staging
Staging is the process of determining how far a cancer has spread. This is done to guide treatment and to help determine the most likely outcome for the patient. But pituitary tumors are nearly always benign (not cancer), so there is no staging system for them. Pituitary carcinoma (cancer) is too rare for a staging system to have been developed.
The most useful information for guiding the treatment of a pituitary tumor (pituitary adenoma) is:
- Whether it is a microadenoma (smaller than 1 centimeter across) or macroadenoma (1 centimeter across or larger)
- Whether it has grown into nearby structures (such as bones of the skull)
- Whether it is causing symptoms such as vision changes
- Whether it is functional (making excess hormones) or non-functional
- Which hormone it releases
Pituitary tumor treatment
Many pituitary tumors don’t require treatment. Treatment for those that do depends on the type of tumor, its size and how far it has grown into your brain. Your age and overall health also are factors.
Treatment involves a team of medical experts, possibly including a brain surgeon (neurosurgeon), endocrine system specialist (endocrinologist) and a radiation oncologist. Doctors generally use surgery, radiation therapy and medications, either alone or in combination, to treat a pituitary tumor and return hormone production to normal levels.
Watchful waiting
In watchful waiting — also known as observation, expectant therapy or deferred therapy — you might need regular follow-up tests to determine if your tumor grows. This might be an option if your tumor isn’t causing signs or symptoms.
Many people with pituitary tumors function normally without treatment if the tumor isn’t causing other problems. If you’re younger, watchful waiting can be an option as long as you accept the possibility of your tumor changing or growing during the observation period, possibly requiring treatment. You and your doctor can weigh the risk of symptoms developing versus treatment.
Pituitary tumor surgery
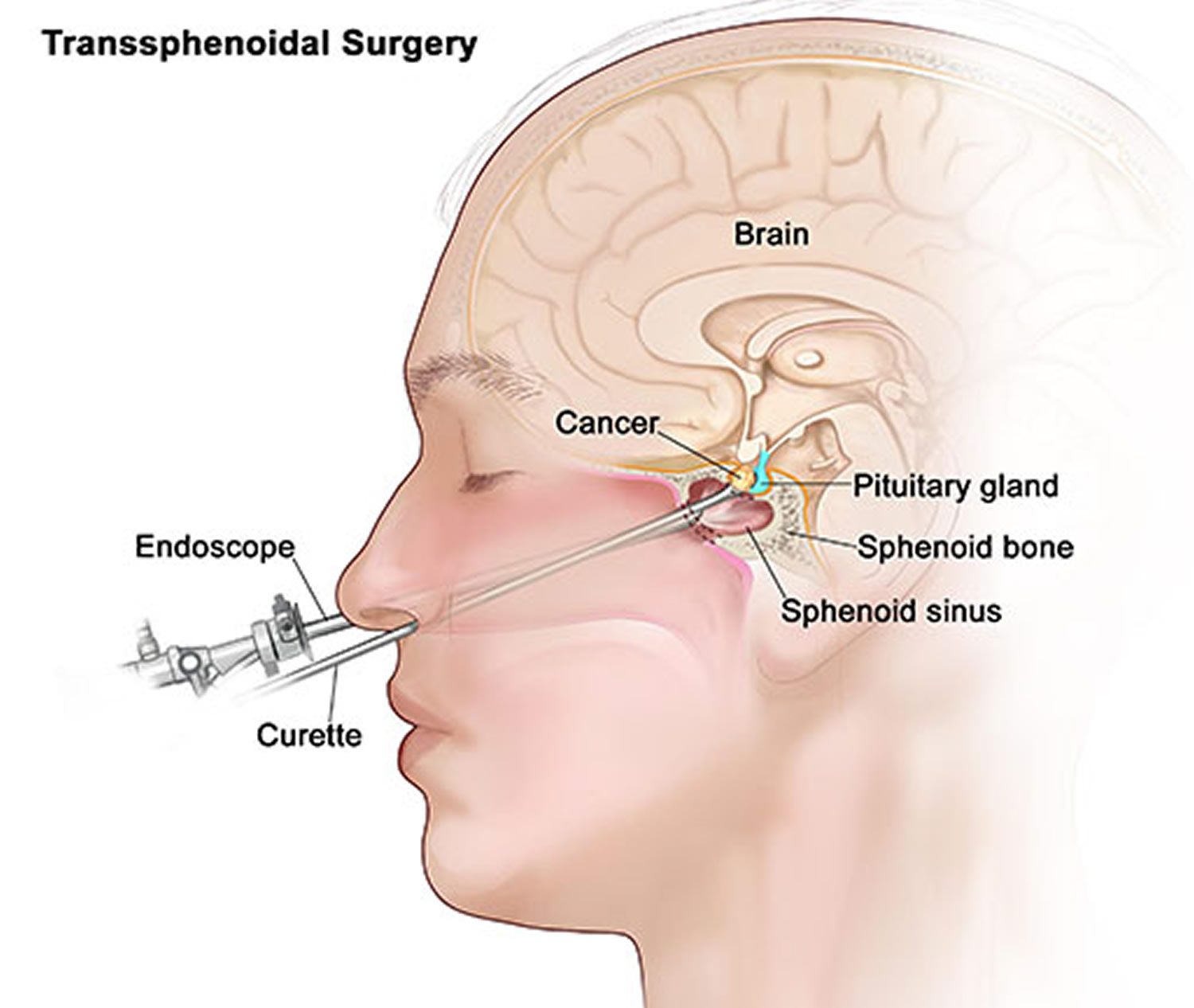
Surgical removal of a pituitary tumor usually is necessary if the tumor is pressing on the optic nerves or if the tumor is overproducing certain hormones. The success of surgery depends on the tumor type, its location, its size and whether the tumor has invaded surrounding tissues. The two main surgical techniques for treating pituitary tumors are:
- Endoscopic transnasal transsphenoidal approach. In transnasal transsphenoidal endoscopic surgery, a surgical instrument is placed through the nostril and alongside the nasal septum to access a pituitary tumor. This usually enables your doctor to remove the tumor through your nose and sinuses without an external incision. No other part of your brain is affected, and there’s no visible scar. Large tumors may be difficult to remove this way, especially if a tumor has invaded nearby nerves or brain tissue.
- Transcranial approach (craniotomy). The tumor is removed through the upper part of your skull via an incision in your scalp. It’s easier to reach large or more complicated tumors using this procedure.
Figure 4. Pituitary tumor surgery – endoscopic transnasal transsphenoidal approach
Radiation therapy
Radiation therapy uses high-energy X-rays to destroy tumors. It can be used after surgery or alone if surgery isn’t an option. Radiation therapy can be beneficial if a tumor persists or returns after surgery and causes signs and symptoms that medications don’t relieve. Methods of radiation therapy include:
- Gamma Knife stereotactic radiosurgery. Often delivered as a single high dose, this focuses radiation beams on the tumor without an incision. It delivers radiation beams the size and shape of the tumor into the tumor with the aid of special brain-imaging techniques. Minimal radiation comes in contact with healthy tissue surrounding the tumor, decreasing the risk of damage to normal tissue.
- External beam radiation. This delivers radiation in small increments over time. A series of treatments, usually five times a week over a four- to six-week period, is performed on an outpatient basis. While this therapy is often effective, it may take years to fully control the tumor growth and hormone production. Radiation therapy may also damage remaining normal pituitary cells and normal brain tissue, particularly near the pituitary gland.
- Proton beam therapy. Another radiation option, this type uses positively charged ions (protons) rather than X-rays. Unlike X-rays, proton beams stop after releasing their energy within their target. The beams can be finely controlled and can be used on tumors with less risk to healthy tissues. This type of therapy requires special equipment and isn’t widely available. The benefits of these forms of radiation therapy often aren’t immediate and may take months or years to be fully effective. A radiation oncologist will evaluate your condition and discuss the pros and cons of each option with you.
Medications
Treatment with medications may help to block excess hormone secretion and sometimes shrink certain types of pituitary tumors:
- Prolactin-secreting tumors (prolactinomas). The drugs cabergoline and bromocriptine (Parlodel) decrease prolactin secretion and often reduce tumor size. Possible side effects include drowsiness, dizziness, nausea, vomiting, diarrhea or constipation, confusion, and depression. Some people develop compulsive behaviors, such as gambling, while taking these medications.
- Growth hormone-secreting tumors. Two types of drugs are available for these types of pituitary tumors and are especially useful if surgery has been unsuccessful in normalizing growth hormone production. One type of drugs known as somatostatin analogs (Sandostatin, Somatuline Depot, others) causes a decrease in growth hormone production and may shrink the tumor. These are given by injections, usually every 4 weeks. These drugs can cause side effects such as nausea, vomiting, diarrhea, stomach pain, dizziness, headache and pain at the site of injection. Many of these side effects improve or even go away with time. They can also cause gallstones and may worsen diabetes mellitus. The second type of drugs, pegvisomant (Somavert), blocks the effect of excess growth hormone on the body. This drug, given by daily injections, may cause liver damage in some people.
Replacement of pituitary hormones
If a pituitary tumor or surgery to remove it decreases hormone production, you’ll likely need to take replacement hormones to maintain normal hormone levels. Some people who have radiation treatment also need pituitary hormone replacement.
Coping and support
It’s natural for you and your family to have questions throughout the diagnosis and treatment of a pituitary tumor. The process can be overwhelming — and frightening. That’s why it’s important to learn as much as you can about your condition. The more you and your family know and understand about each aspect of your care, the better.
You might also find it helpful to share your feelings with others in similar situations. Check to see if support groups for people with pituitary tumors and their families are available in your area. Hospitals often sponsor these groups. Your medical team also may be able to help you find the emotional support you might need.