Contents
- Pneumococcal disease
- Pneumococcal vaccine
- Pneumococcal vaccine schedule for children
- Pneumococcal vaccine schedule for adults 65 years or older
- Pneumococcal vaccine administration
- Side effects of pneumonia vaccine
- Pneumonia vaccine contraindications
- Which underlying medical conditions indicate that a child age 6 through 18 years should receive additional doses of pneumococcal vaccine beyond the routine schedule?
- What are the different serotypes of Streptococcus pneumoniae targeted by different pneumococcal vaccines?
- How effective are pneumococcal conjugate vaccines at preventing pneumococcal carriage or disease?
- How effective is pneumococcal polysaccharide vaccine at preventing pneumococcal carriage or disease?
- Pneumococcal disease cause
- Pneumococcal disease risk factors
- Pneumococcal disease symptoms
- Pneumococcal disease complications
- Pneumococcal disease diagnosis
- Pneumococcal disease treatment
- Pneumococcal disease prognosis
Pneumococcal disease
Pneumococcal disease is a name for any infection caused by Streptococcus pneumoniae or pneumococcus bacteria 1. Streptococcus pneumoniae (pneumococcus) is a Gram-positive bacterium with more than 100 distinct serotypes that differ in their propensity to cause disease overall, as well as their association with case fatality, and antimicrobial resistance 2, 3.
Streptococcus pneumoniae or pneumococcus bacteria can cause many types of infections, including:
- Pneumonia (lung infection)
- Meningitis (infection of the lining of the brain and spinal cord)
- Bacteremia (bloodstream infection)
- Otitis media (middle ear infection)
- Sinusitis (sinus infection)
Streptococcus pneumoniae is the most common cause of fatal community-acquired pneumonia in the elderly and is also one of the most common causes of middle ear infections (otitis media) and bacterial meningitis in children, as well as an important cause of sinusitis, bacteremia, septic arthritis, osteomyelitis, peritonitis, and endocarditis and is the leading cause of infectious death in both children and older adults 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15. In the United States, prior to the widespread use of 7-valent pneumococcal conjugate vaccine (PCV7), the seven most common serotypes isolated from blood or cerebrospinal fluid (CSF) of children younger than age 5 years accounted for 80% of infections; these seven serotypes accounted for about 50% of isolates from older children and adults 16.
The pneumococci bacteria are spread from person to person by droplets in the air. People spread pneumococcal bacteria to others through direct contact with respiratory secretions, like saliva or mucus. The pneumococci bacteria are common inhabitants of the human respiratory tract. They may be isolated from the nasopharynx of 5%–90% of healthy people. Many people, especially children, have the bacteria in their nose or throat at one time or another without being ill. Experts call this “carriage,” and it only rarely leads to sickness 8. The prominence of Streptococcus pneumoniae as a cause of disease is due to the combination of high carriage rates, its genetic adaptability and its ability to shift from a commensal to a pathogenic interaction with its host 17. Scientists do not clearly understand the immunologic mechanism that allows pneumococcal disease to occur in a Streptococcus pneumoniae carrier.
Pneumococcal disease can be invasive, meaning a normally sterile part of the body is infected, or non-invasive.
Invasive pneumococcal disease includes bacteremia (blood stream infection), and meningitis (infection of the meninges that surround the brain). They are both caused by infection with the same bacteria but produce different signs and symptoms.
Pneumococcal pneumonia is a common disease caused by Streptococcus pneumoniae infection. Symptoms include abrupt onset of fever, shaking chills or rigors, chest pain, cough, shortness of breath, rapid breathing and heart rate, and weakness. The case-fatality rate is 5%–7% and is higher in adults 65 years and older and people with certain underlying medical conditions 18. Pneumococcal pneumonia can occur in combination with bacteremia and/or meningitis (invasive pneumococcal pneumonia), or it can occur alone (non-invasive pneumococcal pneumonia). At least 100,000 people were hospitalized each year for pneumococcal pneumonia and at least 30,000 people were hospitalized each year for invasive pneumococcal disease, and about 3,000 people died 18.
About 4,000 cases of pneumococcal bacteremia without pneumonia occur each year in the United States 18. Bacteremia is the most common clinical presentation among children less than 2 years of age, accounting for up to 70% of invasive disease in this age group. The overall case-fatality rate of pneumococcal bacteremia is about 20% and may be as high as 60% among older adults 18.
Anyone can get pneumococcal disease, but some people are at increased risk of pneumococcal disease 19, 20, 21, 22, 23:
- Children younger than 5 years old and adults 65 years or older are at increased risk for pneumococcal disease.
- Race and ethnicity. Experts don’t know why, but people of certain racial and ethnic groups have increased rates of pneumococcal disease:
- Alaska Native people
- African American people
- Certain American Indian people
- Childcare attendance. Young children attending childcare are also at increased risk for severe pneumococcal disease and ear infections.
- Medical conditions. Chronic conditions and other factors that increase someone’s risk for pneumococcal disease include:
- Alcoholism
- Cerebrospinal fluid (CSF) leak
- Chronic heart, kidney, liver, or lung disease
- Cigarette smoking
- Cochlear implant (surgically implanted hearing device to help people with severe hearing loss)
- Diabetes
- Immunocompromising condition (having a weakened immune system)
- Chronic lung disease includes chronic obstructive pulmonary disorder (COPD), emphysema, and asthma.
- Immunocompromising conditions that increase someone’s risk for pneumococcal disease include:
- Damaged spleen or having no spleen
- Disease or condition that weakens the immune system
- Disease or condition treated with medicine that weakens the immune system. This includes cancer and solid organ transplant.
- HIV infection
- Kidney failure requiring maintenance dialysis or nephrotic syndrome (a kidney disorder)
- Sickle cell disease or other inherited blood disorders
Most pneumococcal infections are mild. However, some can result in long-term problems, such as brain damage or hearing loss. Meningitis, bacteremia, and pneumonia caused by pneumococcal disease can be fatal. The World Health Organization (WHO) estimates that about a million children succumb to pneumococcal infections annually, with more than 300,000 being under 5 years of age 1, 24. In the Eastern Mediterranean region, the incidence of pneumococcal disease in 2015 was estimated to be 1261 per 100,000 children (<5 years), of which 1214 per 100,000 were caused by pneumococcal pneumonia 25. In this region, the overall mortality due to pneumococcal disease among children (<5 years) was reported to be around 47/100,000, with a major burden (39/100,000) due to pneumococcal pneumonia 25.
Vaccines can prevent pneumococcal infections. There are two pneumococcal vaccines: pneumococcal conjugate vaccine (e.g., PCV15 [Vaxneuvance], PCV20 [Prevnar 20] or PCV21 [Capvaxive]) and pneumococcal polysaccharide vaccine (e.g., Pneumovax23 [PPSV23]). The Centers for Disease Control and Prevention (CDC) recommends PCV15 (Vaxneuvance) or PCV20 (Prevnar 20) for infants and young children younger than 5 years old. The CDC recommends PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) for all adults 65 years or older, have chronic illnesses or weak immune systems, smoke, have asthma, or live in long-term care facilities 26.
Most pneumococcal infections are treated is with antibiotics 27. Early administration of antibiotics is associated with a better prognosis and the failure to use antibiotics has been associated with an increased risk of in-hospital mortality and more than a five-fold increase in 30-day mortality 28, 29, 30, 31, 32, 33, 34, 35, 36, 37. However, some pneumococcal bacteria have become resistant to certain antibiotics used to treat these infections. People with pneumococcal infections who recently used antibiotics are more likely to have a resistant infection than those who haven’t. People who attend or work at childcare centers are at increased risk for infection with antibiotic-resistant Streptococcus pneumoniae. Other risk factors for having a resistant Streptococcus pneumoniae infection include hospitalization and immunosuppression.
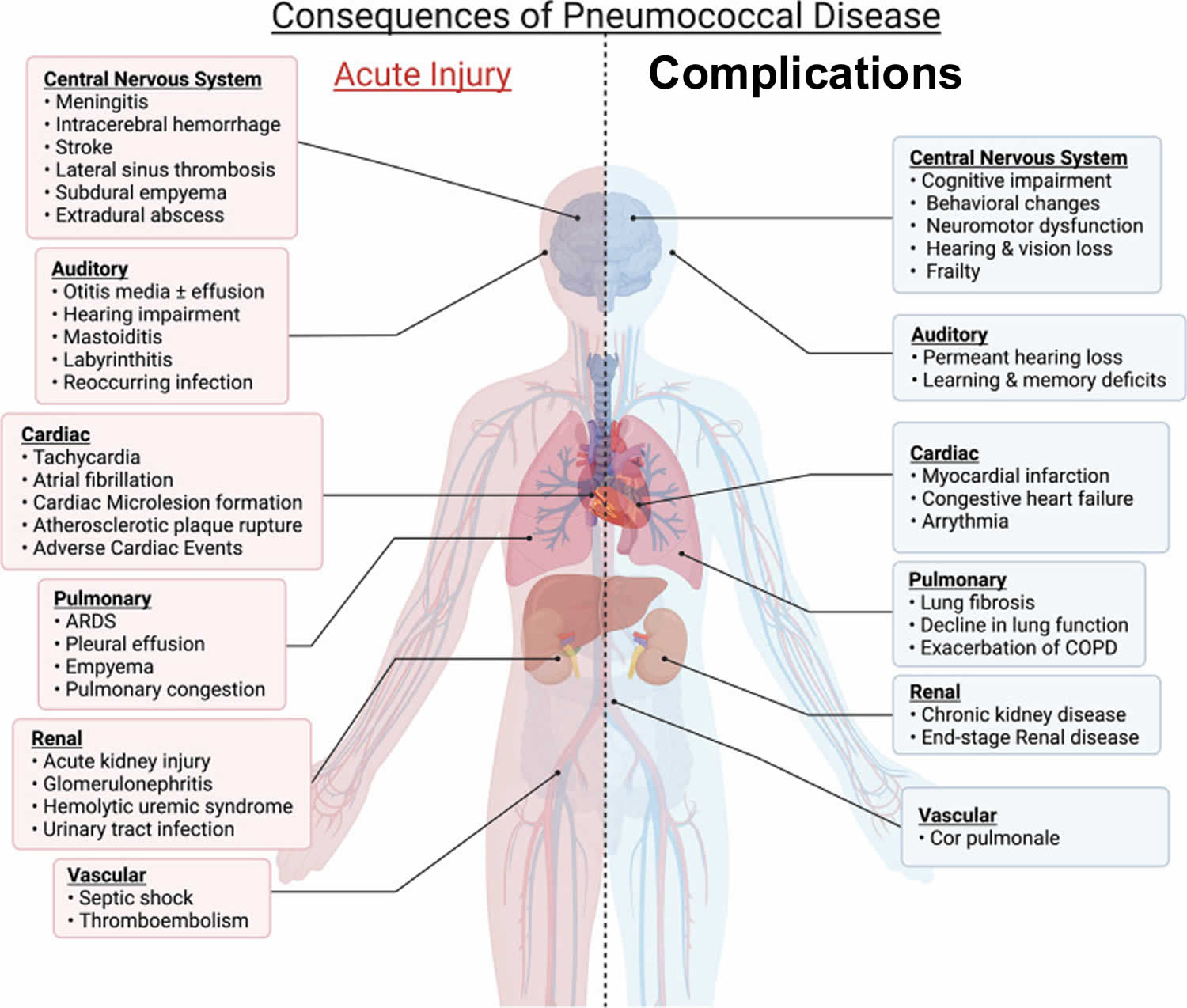
Figure 1. Pneumococcal disease complications
Footnotes: Pneumococcal disease complications during acute infection occur system-wide. Acute pneumococcal pneumonia and invasive disease can be life-threatening. It can also result in organ damage that results in debilitating long-term sequelae. These sequelae, in turn, contribute to loss of physiological resilience and early mortality
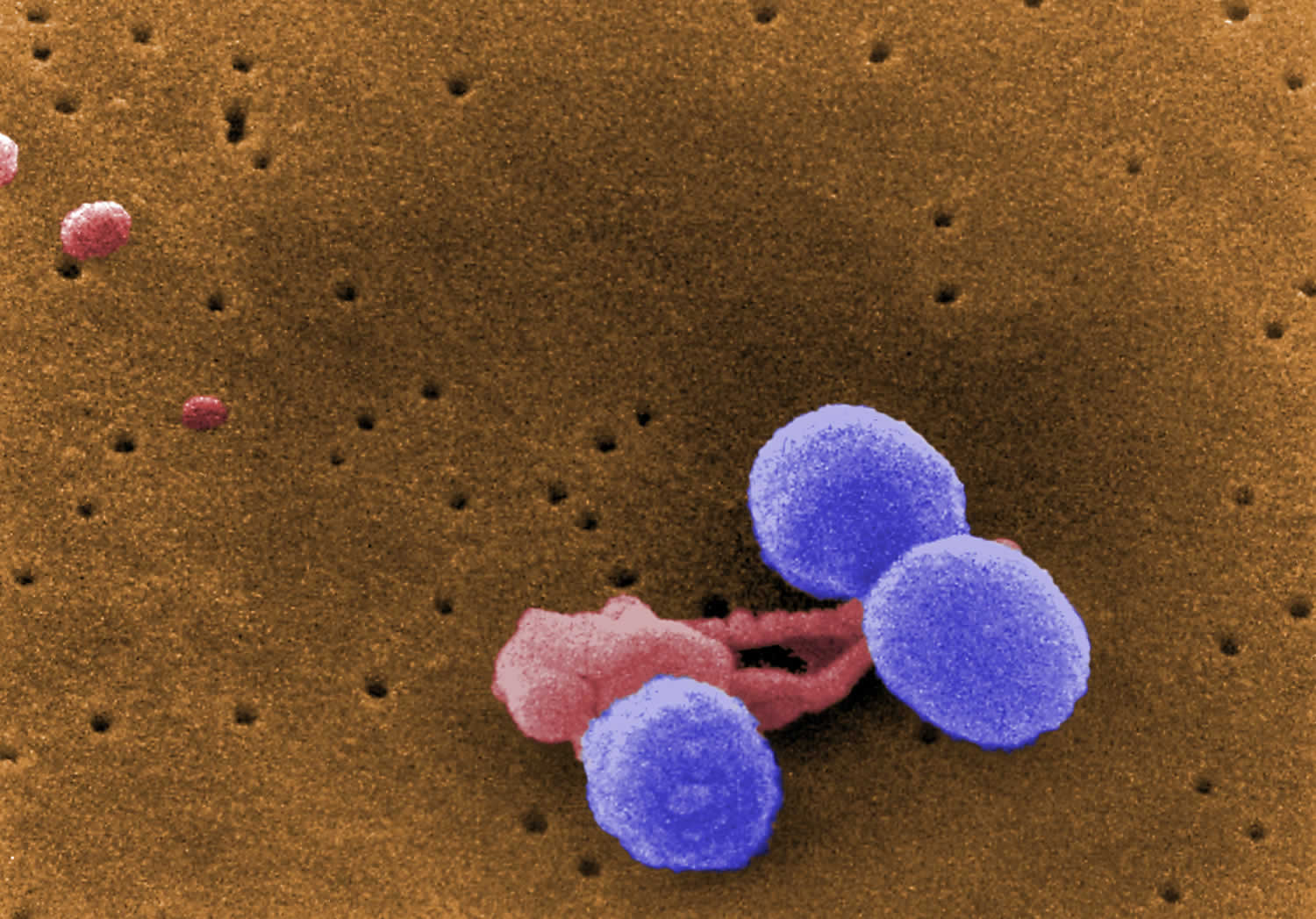
[Source 38 ]Figure 2. Streptococcus pneumoniae bacteria
Footnote: This digitally-colorized, scanning electron microscopic (SEM) image depicts what were three, round-shaped, Gram-positive, Streptococcus pneumoniae bacteria (lavender), as they were being attacked by an irregularly-shaped white blood cell (WBC) (pink). Note what appeared to be unidentified organisms in the upper left corner.
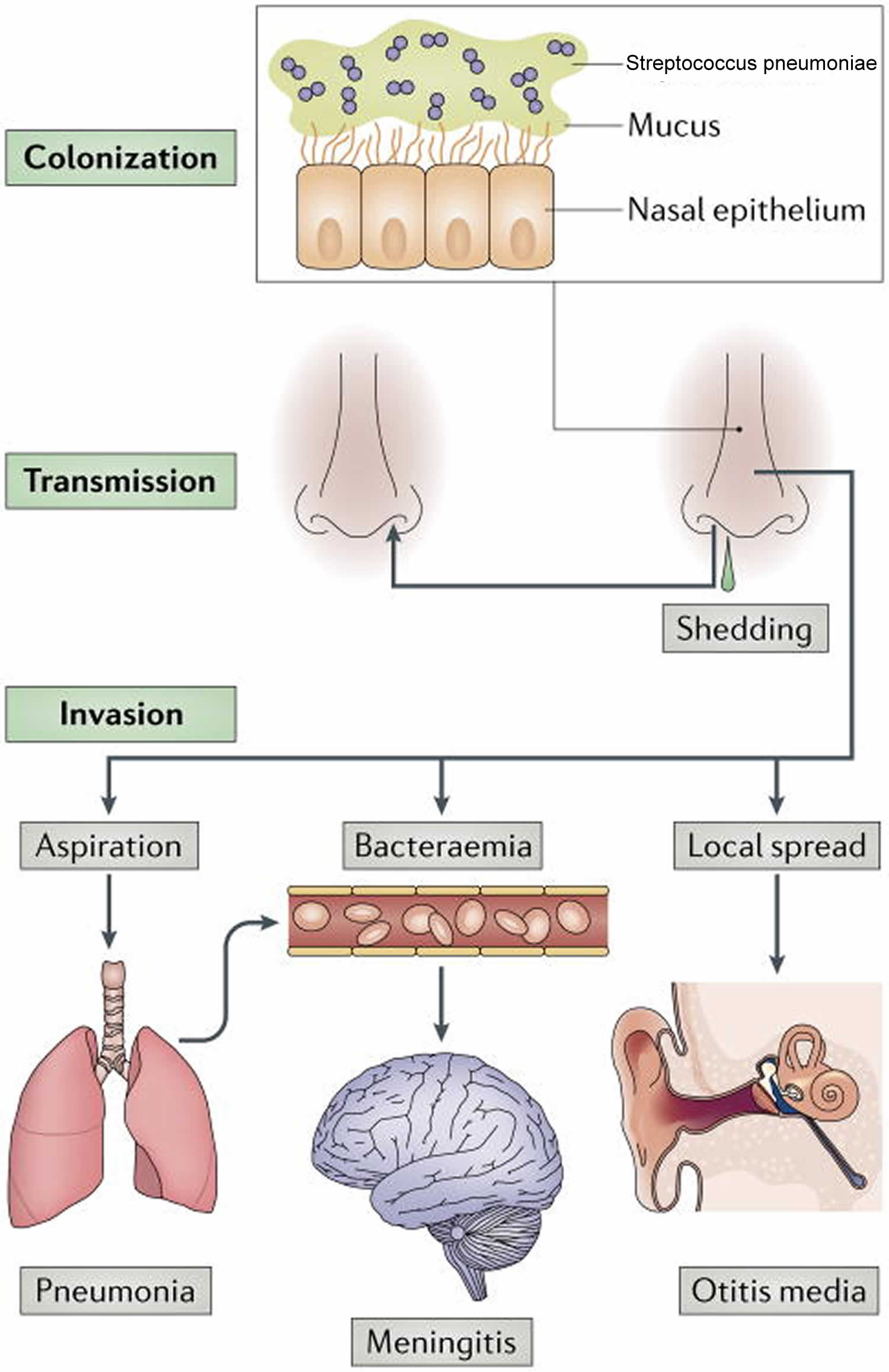
[Source 39 ]Figure 3. Streptococcus pneumoniae life cycle
Footnote: Streptococcus pneumoniae colonizes the mucosa of the upper respiratory tract (URT). This carriage is the prerequisite for both transmission to other individuals and invasive disease in the carrier. Carriers can shed Streptococcus pneumoniae in nasal secretions and thereby transmit the bacterium. Dissemination beyond its niche along the nasal epithelium, either by aspiration, bacteraemia or local spread, can lead to invasive diseases, such as otitis media, community-acquired pneumonia, sepsis and meningitis. As all of these diseases are ‘dead ends’ in the life cycle of the organism, the bacterial factors that cause invasive diseases must also be adaptive for colonization and/or transmission.
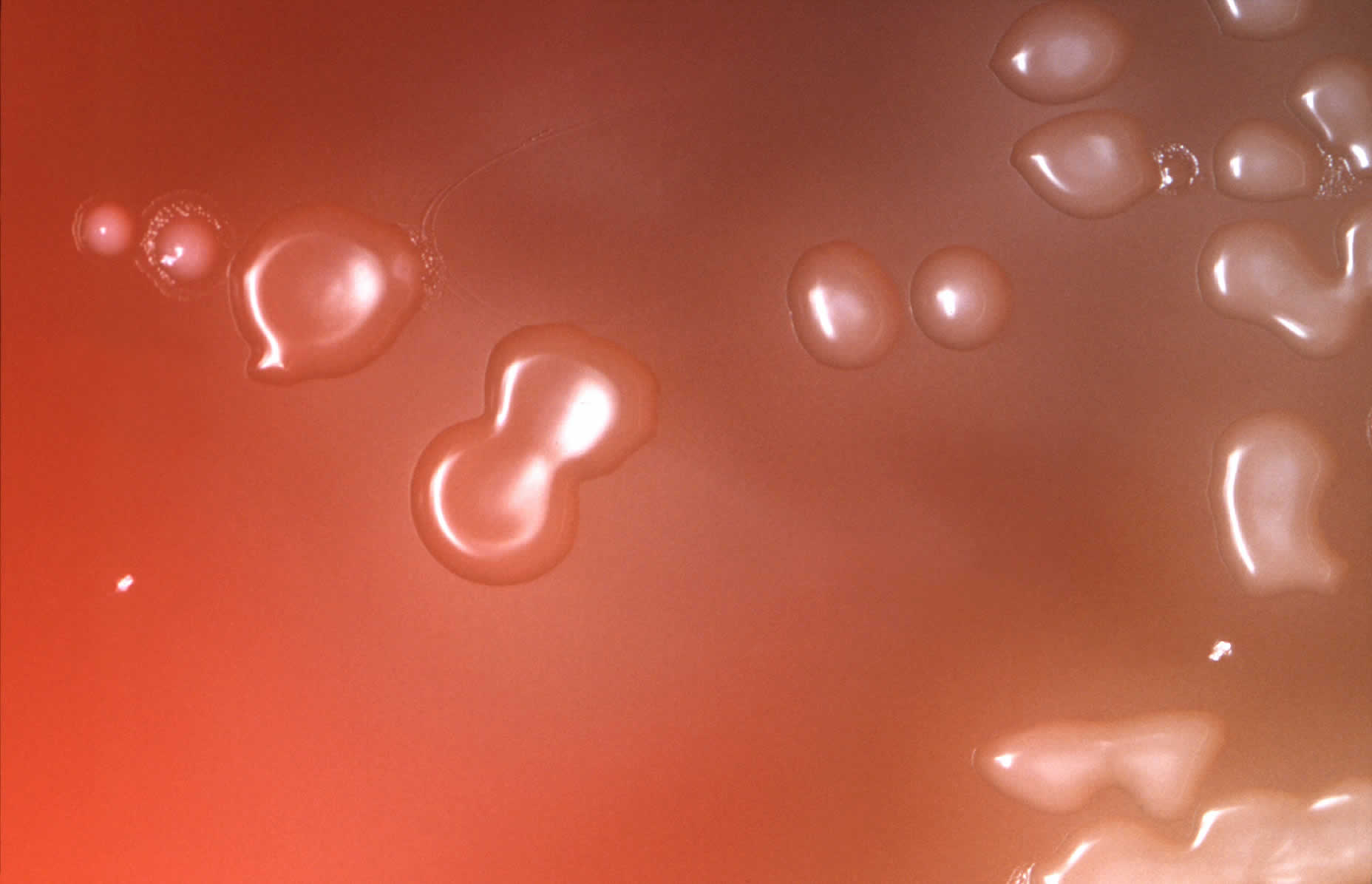
[Source 17 ]Figure 4. Streptococcus pneumoniae in blood agar
Footnote: Under an approximate 10X magnification, this image depicts the colonial characteristics displayed by Streptococcus pneumoniae bacterial colonies that were grown on primary isolation medium, consisting of trypticase-soy-agar, containing 5% sheep’s blood, as well as 5mg of gentamicin/ml. Note that the so called doughnut-shaped colonies are those of Streptococcus pneumoniae. Those that do not have depressed centers are not Streptococcus pneumoniae.
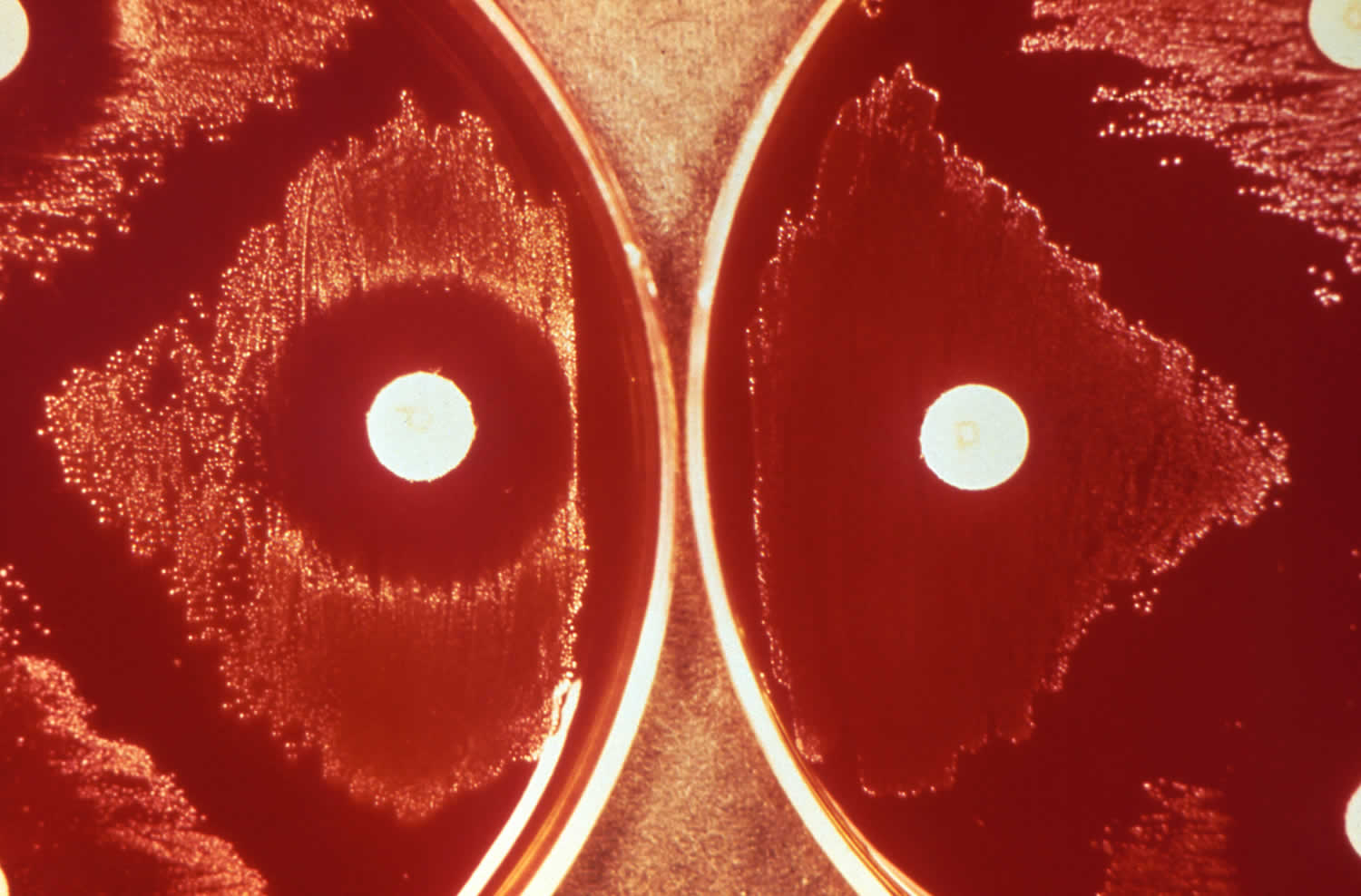
[Source 40 ]Figure 5. Streptococcus pneumoniae optochin test
Footnote: Depicted here, were the results of what is referred to as an optochin (ethylhydrocupreine) test, used to confirm the presence of Streptococcus pneumoniae bacteria, which are optochin-sensitive. In so doing, Streptococcus pneumoniae can then be differentiated from other alpha-hemolytic streptococcal organisms, such as Streptococcus viridans, which are optochin-resistant. The results, revealed that optochin-sensitive, S. pneumoniae, were present on the left, given the zone of inhibition around the optochin imbibed disc, while the optochin-resistant bacteria on the right grew uninhibitedly up to the disc’s edge.
[Source 41 ]How serious is pneumococcal disease?
Pneumococcal disease is a serious disease that causes much sickness and death. An estimated 30,000 cases and 3,000 deaths from invasive pneumococcal diseases (bacteremia and meningitis) occurred in the United States 18. Children younger than 2 years of age and adults age 50 years and older have the highest incidence of serious disease 18. Case-fatality rates are highest for pneumococcal meningitis and bacteremia, and the highest mortality occurs among older adults and patients who have underlying medical conditions.
Pneumococcal vaccine
Pneumococcal vaccines are the best way to protect against serious pneumococcal infections 42. Pneumococcal vaccines help protect against some of the more than 100 serotypes of pneumococcal bacteria 43. The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for children younger than 5 years and adults 65 years or older 26.
There are 2 types of pneumococcal vaccines used in the United States 44, 45:
- Pneumococcal conjugate vaccines (PCVs). A conjugate vaccine is a type of vaccine that joins a protein to an antigen (in the case of pneumococcal vaccines, the protein is connected to unique polysaccharides [long chains of sugar molecules] from the surface of each of the pneumococcal serotypes). The conjugate vaccines have the polysaccharides for different serotypes attached (or conjugated) to a carrier protein. The protein helps improve the quality of the immune system response to the vaccine compared to the response to an unconjugated polysaccharide (PPV). Immune response to pneumococcal conjugate vaccine (PCV) is a T-cell dependent response that produces memory B-cells and reduces carriage of the bacteria in the respiratory track. Pneumococcal conjugate vaccines (PCVs) are given to children younger than 5 years old and to older children who need it. Vaccine providers also give pneumococcal conjugate vaccines (PCVs) to adults 65 years or older and other adults who need it.
- Pneumococcal polysaccharide vaccine (PPV). A polysaccharide vaccine is a type of vaccine that is composed of long chains of sugar molecules called polysaccharides, that resemble the surface of certain serotypes of pneumococcal bacteria in order to help the immune system mount a response. The immune response to the Pneumovax23 (PPSV23) vaccine is a T-cell independent immune response but does not reduce bacterial carriage. Vaccine providers may give Pneumovax23 (PPSV23) to children 2 through 18 years old with certain medical conditions. Vaccine providers give it to adults who receive PCV15 (Vaxneuvance). They also may give it to adults who have received an earlier vaccine called PCV13 (Prevnar 13). PCV13 (Prevnar 13) is FDA-licensed and may still be available in some clinics. PCV13 (Prevnar 13) is no longer routinely recommended; however, CDC guidance allows for its use as previously recommended in situations where PCV15, PCV20, or PCV21 is indicated but unavailable and the alternative is that the patient would not be vaccinated 49.
- PPSV23 (Pneumovax23) helps protect against 23 types of Streptococcus pneumoniae bacteria 50. Following the 2022 changes to the pneumococcal vaccination schedule for adults, PPSV23 (Pneumovax23) is no longer recommended alone, however PPSV23 (Pneumovax23) is recommended for adults following PCV13 (Prevnar 13) or PCV15 (Vaxneuvance) vaccination. PPSV23 (Pneumovax23) is not recommended for people who have previously received a PCV20 (Prevnar 20) or PCV21 (Capvaxive) vaccination.
Each of these vaccines helps protect against specific serotypes, or strains of Streptococcus pneumoniae bacteria. The number at the end of the vaccine name tells how many serotypes the pneumococcal vaccine includes.
The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for 51:
- Children
- All children younger than 5 years old
- Children 5 through 18 years old with certain risk conditions
- Adults
- All adults 65 years or older
- 19 through 64 years old with certain risk conditions
Pneumococcal vaccine schedule for children
The Centers for Disease Control and Prevention (CDC) recommends routine pneumococcal vaccination for all children younger than 5 years old 26.
Administer a 4-dose pneumococcal conjugate vaccine series (PCV15 [Vaxneuvance] or PCV20 [Prevnar 20]), 1 dose at each of the following ages 26:
- 2 months
- 4 months
- 6 months
- with a booster at age 12 through 15 months
Catch-up guidance
Vaccinate children younger than 5 years of age who miss their shots or start the pneumococcal conjugate vaccine series later than recommended. The number of doses recommended and the intervals between doses will depend on the child’s age when vaccination begins. Otherwise healthy children who fall behind should be given catch-up vaccination through age 59 months; if they have certain underlying medical conditions they should be given catch-up vaccination through age 71 months.
Children may be at increased risk for febrile seizures if a pneumococcal conjugate vaccine is administered with inactivated influenza vaccine. However, clinicians may give either pneumococcal conjugate vaccine at the same time as an influenza vaccine.
Currently, no data from clinical trials are available for co-administration of Pneumovax23 (PPSV23) with other childhood vaccines during the same visit.
Pneumococcal vaccine schedule for adults 65 years or older
The Centers for Disease Control and Prevention (CDC) recommends PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) for all adults 65 years or older 26:
- Who have never received any pneumococcal conjugate vaccine (PCV)
- Whose previous vaccination history is unknown
If PCV15 (Vaxneuvance) is used, administer a dose of Pneumovax23 (PPSV23) one year later, if needed. Only one dose of Pneumovax23 (PPSV23) is indicated. If previously administered, another dose isn’t needed. If Pneumovax23 (PPSV23) is not available, one dose of PCV20 (Prevnar 20) or PCV21 (Capvaxive) may be given. Their pneumococcal vaccinations are complete 26.
The minimum interval is 8 weeks and can be considered in adults with 26:
- An immunocompromising condition
- A cochlear implant
- A cerebrospinal fluid leak
If PCV20 (Prevnar 20) or PCV21 (Capvaxive) is used, a dose of Pneumovax23 (PPSV23) isn’t indicated. Regardless of which vaccine is used (PCV20 or PCV21), their pneumococcal vaccinations are complete 26.
Based on shared clinical decision-making, adults 65 years or older have the option to get no additional pneumococcal vaccines, PCV20 (Prevnar 20) or PCV21 (Capvaxive). They can get PCV20 (Prevnar 20) or PCV21 (Capvaxive) if they have received both 26:
- PCV13 (Prevnar 13) (but not PCV15, PCV20, or PCV21) at any age and
- Pneumovax23 (PPSV23) at or after the age of 65 years old
Pneumococcal vaccine administration
Use a needle length appropriate for the age and size (22–25 Gauge) of the person receiving the pneumococcal vaccine. NEVER administer a pneumococcal conjugate vaccine (PCV15, PCV20, or PCV21) and Pneumovax23 (PPSV23) during the same visit 52. If someone is indicated to receive PCV15 (Vaxneuvance) and Pneumovax23 (PPSV23), administer PCV15 (Vaxneuvance) first followed by Pneumovax23 (PPSV23).
- Administer pneumococcal polysaccharide vaccine Pneumovax23 (PPSV23) intramuscularly or subcutaneously 52.
- Administer pneumococcal conjugate vaccines (PCV15 [Vaxneuvance] or PCV20 [Prevnar 20]) intramuscularly 52.
- For infants and young children, use the vastus lateralis muscle in the anterolateral thigh.
- For older children and adults, use the deltoid muscle.
- Administer pneumococcal conjugate vaccine (PCV21 [Capvaxive]) to adults intramuscularly using the deltoid muscle.
The primary series of PCV15 (Vaxneuvance) or PCV20 (Prevnar 20) consists of 3 doses routinely given at 2, 4, and 6 months of age. You can administer the first dose as early as 6 weeks of age. CDC recommends a fourth (booster) dose at 12 through 15 months of age. For children vaccinated when they are younger than 12 months of age, the minimum interval between doses is 4 weeks. Separate doses given at 12 months of age and older by at least 8 weeks.
The number and timing of doses for older children and adults depends on the medical indication, prior pneumococcal vaccination, and age.
For children (2 through 18 years old), the interval between PCV15 (Vaxneuvance) and Pneumovax23 (PPSV23) should be at least 8 weeks. If Pneumovax23 (PPSV23) is inadvertently administered first, wait at least 8 weeks to administer PCV15 (Vaxneuvance).
For adults, the recommended interval is at least 1 year. An 8-week minimum interval can be considered for adults with an immunocompromising condition, cochlear implant, or cerebrospinal fluid leak. If Pneumovax23 (PPSV23) is inadvertently administered first, wait at least 1 year to administer PCV15 (Vaxneuvance).
In adults, you can administer a pneumococcal vaccine (PCV15, PCV20, PCV21, or PPSV23) during the same visit with influenza vaccination or other recommended vaccines. Administer each vaccine with a separate syringe and, if feasible, at a different injection site. Annual influenza vaccination is important to help prevent the flu. Additionally, since having the flu increases the risk of getting pneumococcal disease, receiving a flu vaccine is important for preventing pneumococcal disease.
Side effects of pneumonia vaccine
Redness, swelling, pain, or tenderness where the pneumonia vaccine is given, and fever, loss of appetite, fussiness (irritability), feeling tired, headache, muscle aches, joint pain, and chills can happen after pneumococcal conjugate vaccination (PCV) 53.
PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) side effects:
- Redness, swelling, pain, or tenderness where the vaccine provider gave the shot
- Fever or chills
- Loss of appetite
- Fussiness (irritability) in young children
- Feeling tired
- Headache
- Muscle aches or joint pain
Pneumovax23 (PPSV23) side effects:
- Redness or pain where the vaccine provider gave the shot
- Feeling tired
- Fever
- Muscle aches
Young children may be at increased risk for seizures caused by fever after a pneumococcal conjugate vaccine (PCV) if it is administered at the same time as inactivated influenza vaccine. Ask your doctor for more information.
People sometimes faint after medical procedures, including vaccination. Tell your doctor if you feel dizzy or have vision changes or ringing in the ears. As with any medicine, there is a very remote chance of a vaccine causing a severe allergic reaction, other serious injury, or death 53.
An allergic reaction could occur after the vaccinated person leaves the clinic. If you see signs of a severe allergic reaction (hives, swelling of the face and throat, difficulty breathing, a fast heartbeat,
dizziness, or weakness), call your local emergency services number and get the person to the nearest hospital. For other signs that concern you, see your doctor.
Pneumonia vaccine contraindications
You shouldn’t get PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) if you’ve:
- Had a life-threatening allergic reaction after any type of pneumococcal conjugate vaccination (PCV)
- Had a life-threatening allergic reaction to any vaccine containing diphtheria toxoid (DTaP)
- Have a severe allergy to any part of these vaccines
You shouldn’t get Pneumovax23 (PPSV23) if you:
- Are younger than 2 years old
- Had a life-threatening allergic reaction after getting Pneumovax23 (PPSV23)
- Have a severe allergy to any part of Pneumovax23 (PPSV23)
Which underlying medical conditions indicate that a child age 6 through 18 years should receive additional doses of pneumococcal vaccine beyond the routine schedule?
Medical conditions that increase the risk of pneumococcal disease and are indications for additional pneumococcal vaccine doses beyond the routine schedule are broken down into two categories: non-immunocompromising (non-IC) and immunocompromising (IC) 18. Recommendations differ slightly under certain circumstances by non-immunocompromising (non-IC) or immunocompromising (IC) category.
Non-immunocompromising (non-IC) conditions include 18:
- Cerebrospinal fluid (CSF) leak
- Chronic heart disease (especially cyanotic congenital heart disease and heart failure)
- Chronic kidney disease (except as specified in the immunocompromising (IC) list below)
- Chronic liver disease
- Chronic lung disease (including moderate persistent or severe persistent asthma)
- Diabetes mellitus
- Cochlear implant
Immunocompromising (IC) conditions include 18:
- Kidney disease and on maintenance dialysis
- Kidney disease with nephrotic syndrome
- Asplenia or splenic dysfunction
- Congenital or acquired immunodeficiency, including B-(humoral) or T-lymphocyte deficiency; complement deficiencies, particularly C1, C2, C3, and C4 deficiency; and phagocytic disorders (excluding chronic granulomatous disease)
- Treatment with immunosuppressive drugs or radiation therapy (including treatment for Hodgkin disease, leukemias, lymphomas, malignant neoplasm, and solid organ transplant)
- HIV infection
- Sickle cell disease or other hemoglobinopathies
An older child through age 18 years with any high-risk condition who completed a pneumococcal conjugate vaccine (PCV) series before age 6 years that included any dose of PCV20 (Prevnar 20), is not recommended to receive any additional pneumococcal conjugate vaccine (PCV) doses.
Children with non-immunocompromising (non-IC) or immunocompromising (IC) conditions who completed a pneumococcal conjugate vaccine (PCV) series before age 6 years with PCV13 (Prevnar 13) or PCV15 (Vaxneuvance) but who have not received PCV20 (Prevnar 20) or pneumococcal polysaccharide vaccine Pneumovax23 (PPSV23) should receive additional pneumococcal vaccination with a single dose of PCV20 at least 8 weeks after the most recent pneumococcal conjugate vaccine (PCV) dose. If PCV20 (Prevnar 20) is not available, a non-IC or IC child in this circumstance may, alternatively, receive a single dose of Pneumovax23 (PPSV23) at least 8 weeks after the most recent pneumococcal conjugate vaccine (PCV) dose. An immunocompromised (IC) child given Pneumovax23 (PPSV23) in this circumstance would also be due for a dose of either PCV20 (Prevnar 20) or a second dose of Pneumovax23 (PPSV23) at least 5 years after the first Pneumovax23 (PPSV23).
Doses of the PCV7 (Prevnar 7) do not count toward pneumococcal conjugate vaccine (PCV) vaccination when determining the current pneumococcal vaccination needs of a child or teen with a qualifying non-IC or IC condition.
When feasible, administer any needed pneumococcal vaccination at least two weeks before initiating planned interventions that place a child at high risk (such as a cochlear implant or spleen removal).
What are the different serotypes of Streptococcus pneumoniae targeted by different pneumococcal vaccines?
Streptococcus pneumoniae bacteria are serotyped based on the polysaccharides in the outer capsule of the bacteria. Serotypes vary in how common they are and in what percentage of pneumococcal disease they cause.
Among the pneumococcal conjugate vaccines (PCVs), PCV13 (Prevnar 13) includes serotypes: 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F. PCV15 (Vaxneuvance) includes all PCV13 serotypes plus 22F and 33F. PCV20 (Prevnar 20) includes all PCV15 serotypes plus 8, 10A, 11A, 12F, and 15B.
Pneumovax23 (PPSV23) vaccine does not contain serotype 6A, but contains 19 other serotypes present in PCV20, plus serotypes 2, 9N, 17F, and 20.
PCV21 (Capvaxive) is designed to target additional Streptococcus pneumoniae serotypes causing a significant proportion of disease in adults that are not prevented by the vaccines approved for children. PCV21 (Capvaxive)does not contain 10 serotypes found in other pneumococcal vaccines approved for children (1, 4, 5, 6B, 9V, 14, 18C, 19F, 23F, 15B, or 2). Instead, it contains an additional 11 serotypes not found in PCV20 (Prevnar 20): 9N, 17F, 20, 15A, 15C, 16F, 23A, 23B, 24F, 31, and 35B. Because of these differences, CDC estimates that PCV20 (Prevnar 20) targets serotypes that cause between 54% and 65% of invasive pneumococcal disease in adults, and PCV21 (Capvaxive) targets serotypes that cause between 77% and 85% of invasive pneumococcal disease in adults 18.
How effective are pneumococcal conjugate vaccines at preventing pneumococcal carriage or disease?
The United States Food and Drug Administration (FDA) licensed the first pneumococcal conjugate vaccine (PCV) against seven pneumococcus bacteria serotypes (PCV7, Prevnar 7) in 2000. A large clinical trial showed PCV7 (Prevnar7) reduced invasive disease caused by vaccine serotypes by 97%. Compared to unvaccinated children, children who received PCV7 (Prevnar 7) 18:
- Had 20% fewer episodes of chest X-ray confirmed pneumonia
- Had 7% fewer episodes of acute otitis media
- Underwent 20% fewer tympanostomy tube placements
FDA licensed PCV13 (Prevnar 13) based on studies comparing the serologic response of children who received PCV13 (Prevnar 13) to those who received PCV7 (Prevnar 7). Substantial evidence demonstrates that routine infant PCV7 and PCV13 vaccination reduces the carriage and transmission of vaccine serotypes.
Researchers conducted a randomized placebo-controlled trial (CAPiTA trial) in the Netherlands among approximately 85,000 adults 65 years or older from 2008 through 2013 54. The Community-Acquired Pneumonia Immunization Trial in Adults (CAPiTA trial) evaluated the clinical benefit of PCV13 (Prevnar 13) in the prevention of pneumococcal pneumonia. The results of the CAPiTA trial demonstrated 54:
- 46% efficacy against vaccine-type pneumococcal pneumonia
- 45% efficacy against vaccine-type non-bacteremic pneumococcal pneumonia
- 75% efficacy against vaccine-type invasive pneumococcal disease (IPD, i.e., bacteremia or meningitis)
FDA licensed PCV15 (Vaxneuvance) and PCV20 (Prevnar 20) in 2021 based on studies comparing the serologic response of adults who received either PCV15 or PCV20 to those who received PCV13 (Prevnar 13). These studies showed PCV15 (Vaxneuvance) and PCV20 (Prevnar 20) induced antibody levels comparable to those induced by PCV13 (Prevnar 13) and shown to be protective against invasive disease. FDA subsequently expanded the indication for use of PCV15 and PCV20 to include children starting at age 6 weeks in 2022 and 2023, respectively, based on serologic studies. PCV21 (Capvaxive) was licensed in 2024 based on a similar evaluation of serologic response to vaccination.
How effective is pneumococcal polysaccharide vaccine at preventing pneumococcal carriage or disease?
According to CDC, more than 80% of healthy adults who receive Pneumovax23 (PPSV23) develop antibodies against the serotypes contained in the vaccine that persist for at least 5 years 18. Older adults and people with some chronic illnesses or immunodeficiency may not respond as well and their antibody levels may decline more quickly.
Overall, the Pneumovax23 (PPSV23) vaccine is 60% to 70% effective in preventing invasive pneumococcal disease caused by serotypes in the vaccine 18. Pneumovax23 (PPSV23) shows less effectiveness among immunocompromised people; however, because of their increased risk of invasive pneumococcal disease, CDC recommends Pneumovax23 (PPSV23) for people in these groups who receive PCV15 (Vaxneuvance). There has not been consensus regarding the ability of Pneumovax23 (PPSV23) to prevent non-bacteremic pneumococcal pneumonia; however, recent observational studies reported 21%–46% effectiveness against Pneumovax23 (PPSV23)-type pneumococcal pneumonia when PPSV23 was given less than 5 years before illness onset.
Unlike pneumococcal conjugate vaccines (PCVs), Pneumovax23 (PPSV23) vaccination has not been shown to decrease nasal carriage of pneumococcal bacteria among those vaccinated 18.
Pneumococcal disease cause
Pneumococcal disease is caused by Streptococcus pneumoniae or pneumococcus bacteria infection. Streptococcus pneumoniae (pneumococcus) is a Gram-positive bacterium with more than 100 distinct serotypes that differ in their propensity to cause disease overall, as well as their association with case fatality, and antimicrobial resistance 2, 3. Streptococcus pneumoniae or pneumococcus bacteria are encapsulated within a polysaccharide capsule, which is an important virulence factor 55. These Streptococcus pneumoniae (pneumococcus) serotypes have been defined based on differences in their capsular polysaccharide composition 56. The main way people spread Streptococcus pneumoniae bacteria to others is through direct contact with respiratory droplets in the air. People spread pneumococcal bacteria to others through direct contact with respiratory secretions, like saliva or mucus. Streptococcus pneumoniae bacteria often spread within households and in crowded conditions.
The pneumococci bacteria are common inhabitants of the human respiratory tract. They may be isolated from the nasopharynx of 5%–90% of healthy people. Many people, especially children, have the bacteria in their nose or throat at one time or another without being ill. Experts call this “carriage,” and it only rarely leads to sickness. The prominence of Streptococcus pneumoniae as a cause of disease is due to the combination of high carriage rates, its genetic adaptability and its ability to shift from a commensal to a pathogenic interaction with its host 17. Scientists do not clearly understand the immunologic mechanism that allows pneumococcal disease to occur in a Streptococcus pneumoniae carrier.
Transmission of Streptococcus pneumoniae occurs through 57:
- Direct person-to-person contact via respiratory droplets
- Autoinoculation in persons carrying the bacteria in their upper respiratory tract
The pneumococcal serotypes most often responsible for causing infection are those most frequently found in carriers. Although carriage does not necessarily lead to disease, it is an important precursor for pneumococcal disease.
The following factors influence the spread of the organism within a family or household:
- Crowding
- Season. Pneumococcal infections are more common during the winter and in early spring when respiratory diseases are more prevalent.
- Presence of upper respiratory infections or pneumococcal disease, such as pneumonia or otitis media.
The period of communicability for pneumococcal disease is unknown. Presumably, transmission can occur as long as the organism appears in respiratory secretions.
Streptococcus pneumoniae bacterium most often resides asymptomatically in the nasopharynx but can be aspirated into the lungs to cause pneumonia 8. From the airway, the pneumococcus can gain access to the bloodstream and spread to other sites, where it can cause disseminated organ damage 58, 59, 60. Young children with underdeveloped immune systems, those with immunodeficiencies, adults over the age of 65 with multiple medical conditions, and individuals experiencing or who have recently experienced a respiratory viral infection have increased susceptibility to both becoming infected with and dying from pneumococcal disease 5, 60, 61, 62.
Pneumococcal disease risk factors
Many health conditions and other factors can increase someone’s risk for pneumococcal disease, including severe infections.
Conditions and other factors that increase the risk for invasive pneumococcal disease include 63:
- Alcoholism
- Cerebrospinal fluid leak
- Chronic heart, lung, liver, or renal disease
- Cigarette smoking
- Cochlear implant
- Decreased immune function from disease or drugs
- Diabetes
- Functional or anatomic asplenia, including sickle cell disease
Conditions associated with decreased pulmonary clearance, such as asthma, chronic bronchitis, chronic obstructive pulmonary disease (COPD), viral infections, and active/passive cigarette smoke exposure, also predispose to Streptococcus pneumoniae infection.
Chronic lung conditions that increase someone’s risk include chronic obstructive pulmonary disease (COPD), emphysema, and asthma (in adults) or asthma treated with high-dose steroids (in children).
Persons with a cochlear implant appear to be at increased risk of pneumococcal meningitis.
Conditions that cause immune deficits, including HIV infection, malignancy, diabetes mellitus, functional or anatomic asplenia, humoral immunity defects, complement deficiencies, and neutrophil dysfunction, are associated with an increased risk of disease.
Children with HIV infection or functional or anatomic asplenia, particularly sickle cell disease, are at high risk for invasive pneumococcal disease. Some studies report rates more than 50 times higher than those among children of the same age without these conditions.
Experts do not know why, but children of certain racial and ethnic groups also have increased rates of disease:
- Alaska Native people
- African American people
- Certain American Indian people
Research shows that young children attending childcare are at increased risk for invasive pneumococcal disease and acute otitis media.
Children younger than 5 years, particularly aged 2 years or younger, are at an increased risk of pneumococcal disease 64. In addition, absence of breastfeeding, exposure to cigarette smoke, daycare attendance, and lack of immunization with the pneumococcal conjugate vaccine further increase the risk of disease. Adults older than 55-65 years are also at an increased risk of pneumococcal disease 64.
Children at risk for pneumococcal disease
Children at increased risk for pneumococcal disease include those younger than 2 years old and those with:
- Chronic heart, lung, or kidney disease
- Cerebrospinal fluid (CSF) leak (a health problem where fluid surrounding and protecting the brain and spinal cord leaks)
- Cochlear implant (a small electronic device that is surgically implanted to help people with severe hearing loss be able to hear)
- Diabetes
- HIV infection, cancer, solid organ transplant, or another condition or taking medicine that weakens the immune system
- Nephrotic syndrome (a kidney disorder)
- Sickle cell disease, a damaged spleen, or no spleen
Children with functional or anatomic asplenia, particularly those with sickle cell disease, and children with immunocompromising conditions are at very high risk for invasive disease, with rates in some studies more than 50 times higher than those among children of the same age without these conditions (i.e., incidence rates of 5,000 to 9,000 per 100,000 population). Other conditions that increase the risk of invasive pneumococcal disease in children include chronic heart disease, lung disease (including asthma if treated with high-dose oral corticosteroid therapy), liver disease, CSF leak, and having a cochlear implant. Rates are also increased among children of certain racial and ethnic groups, including Alaska Natives, African Americans, and certain American Indian groups (Navajo and White Mountain Apache). The reason for this increased risk by race and ethnicity is not known with certainty but has also been noted for invasive Haemophilus influenzae infection (also an encapsulated bacterium). Attendance at a childcare center has also been shown to increase the risk of invasive pneumococcal disease and acute otitis media 2- or 3-fold among children younger than age 5 years. Children with a cochlear implant are at increased risk for pneumococcal meningitis.
Adults at risk for pneumococcal disease
Adults 65 years or older are at increased risk for pneumococcal disease.
Adults of all ages are also at increased risk for pneumococcal disease if they have:
- Alcoholism
- Chronic heart, lung, kidney, or liver disease
- Cochlear implant
- CSF leak
- Diabetes
- HIV infection, cancer, solid organ transplant, or another condition or taking medicine that weakens the immune system
- Nephrotic syndrome
- Sickle cell disease, a damaged spleen, or no spleen
Adults with certain medical conditions are at highest risk for invasive pneumococcal disease. Adults who smoke cigarettes are also at increased risk for pneumococcal disease.
For adults age 18 through 64 years with hematologic cancer, the rate of invasive pneumococcal disease in 2013–2014 was 129 per 100,000 population. Other conditions that place adults at highest risk for invasive pneumococcal disease include other immunosuppressive conditions from disease or drugs, functional or anatomic asplenia, and renal disease. Other conditions that increase the risk of invasive pneumococcal disease in adults include chronic heart disease, chronic lung diseases (including chronic obstructive lung disease, emphysema, and asthma), liver disease, smoking cigarettes, alcoholism, CSF leak, and having a cochlear implant.
Pneumococcal disease symptoms
Pneumococcal disease symptoms depend on the part of the body that’s infected. It usually takes 1 to 3 days for pneumonia symptoms to appear after Streptococcus pneumoniae bacteria enter someone’s body. Experts don’t know how long it takes for symptoms to appear for other types of pneumococcal disease. Generally, the symptoms are similar to other bacterial infections in that part of the body.
Pneumonia
Symptoms of pneumococcal pneumonia, a lung infection, include:
- Chest pain
- Cough
- Fever and chills
- Rapid breathing or difficulty breathing
Older adults may experience confusion or low alertness, rather than the more common symptoms listed above.
Meningitis
Symptoms of pneumococcal meningitis, an infection of the lining of the brain and spinal cord, include:
- Confusion
- Fever
- Headache
- Photophobia (eyes being more sensitive to light)
- Stiff neck
In babies, meningitis may cause poor eating and drinking, low alertness, and vomiting.
Bacteremia (bloodstream infection)
Symptoms of pneumococcal bacteremia, a bloodstream infection, include:
- Chills
- Fever
- Low alertness
Ear infection
Symptoms of ear infections include:
- A red, swollen ear drum
- Ear pain
- Fever
- Sleepiness
Streptococcus pneumoniae are a common cause of middle ear infection (acute otitis media). Clinical manifestations may depend on the age of the patient. In young children, ear pain may be shown as irritability, change in sleeping or eating habits, or holding or tugging at the ear. Fever, ear drainage, and hearing loss may be present. Complications of pneumococcal otitis media may include mastoiditis and meningitis. Streptococcus pneumoniae infection is the most common cause of mastoiditis, a complication of middle ear infection (acute otitis media) that was more common in the pre-antibiotic era; this complication is now more commonly associated with untreated or improperly treated cases.
Several early studies demonstrated that middle ear infection (acute otitis media) due to Streptococcus pneumoniae is usually accompanied by fever and pain; the fever associated with pneumococcal otitis media tends to be higher than that caused by other common bacterial pathogens 65. Pneumococcal disease is less likely to resolve spontaneously.
Pneumococcal acute otitis media U.S. statistics:
- Causes up to 20% of all acute otitis media infections, which are the most frequent reasons for pediatric medical visits and pediatric antibiotic prescriptions
Sinus infection
Symptoms of sinus infections include:
- Bad breath
- Cough
- Facial pain or pressure
- Headache
- Post-nasal drip (mucus dripping down the throat)
- Runny or stuffy nose
- Sore throat
Conjunctivitis
Conjunctivitis also called “pink eye”, is an inflammation or infection of the transparent membrane (conjunctiva) that lines your eyelid and covers the white part of your eyeball. When small blood vessels in the conjunctiva become inflamed, they’re more visible. This is what causes the whites of your eyes to appear reddish or pink. Conjunctivitis is commonly caused by a bacterial or viral infection, an allergic reaction, or — in babies — an incompletely opened tear duct.
Bacterial conjunctivitis is more likely to be bilateral and purulent than viral conjunctivitis.
Streptococcus pneumoniae is found in up to one third of patients with bacterial conjunctivitis; the rate of isolates that are not susceptible to penicillin is increasing.
Osteomyelitis and septic arthritis
Streptococcus pneumoniae infection is an uncommon cause of osteomyelitis (bone infection) and septic arthritis (joint infection), causing approximately 4% and 20% of cases in children, respectively.
- Septic arthritis: Pneumococcal septic arthritis usually manifests as painful, swollen, and hot joints. The ankles and knees are most commonly involved, and one or more joints may be affected. Blood or synovial cultures usually grow S pneumoniae. Up to half of patients with pneumococcal septic arthritis have concomitant osteomyelitis.
- Osteomyelitis: The femur and humerus are most often involved in cases of pneumococcal osteomyelitis in children; the vertebral bones are often involved in adult patients. Up to 20% of patients with pneumococcal osteomyelitis develop long-term sequelae, a figure similar to that of rates of osteomyelitis of other causes. One clinical study performed by the Pediatric Multicenter Pneumococcal Surveillance Study Group 66 showed that more than 40% of patients with joint and bone pneumococcal infections had associated bacteremia. Patients with joint prostheses or rheumatic fever are at increased risk for joint disease.
Soft tissue infections
Although uncommon, Streptococcus pneumoniae infection can be a cause of mild-to-serious soft tissue infections, including cellulitis, myositis, periorbital cellulitis, and abscess, particularly in some immunocompromised hosts (eg, those with SLE). Most patients have white blood cell counts greater than 15,000 cells/μL and elevated temperatures. Physical findings are related to the site of infection and usually include redness, warmth, and tenderness of the involved area. Movement may be limited by pain and/or swelling. The incidence of soft tissue infections is increased in persons with HIV infection or underlying connective tissue disease; however, most affected individuals are otherwise healthy and respond well to antibiotic therapy 65.
Peritonitis
Peritonitis is an inflammation (irritation) of the peritoneum. This is the thin tissue that lines the inner wall of the abdomen and covers most of the abdominal organs. Overall, primary peritonitis (peritonitis caused by the spread of organisms via blood or lymph to the peritoneal cavity) is rare, accounting for less than 20% of peritonitis cases.
Streptococcus pneumoniae is the most commonly isolated organism in patients with primary peritonitis. Primary peritonitis in children is usually associated with underlying conditions such as nephrotic syndrome or other immunocompromising diseases. In adults, primary peritonitis is usually associated with cirrhosis.
Females with severe pelvic inflammatory disease due to Streptococcus pneumoniae infection may develop peritonitis. In such cases, organisms may gain access to the peritoneum via the fallopian tubes from the female genital tract. This is the only invasive disease caused by Streptococcus pneumoniae infection that is more common in females. Other persons at risk for peritonitis include persons with gastrointestinal injury, ulcers, or malignancy.
Presenting symptoms of peritonitis include abdominal pain, anorexia, emesis, diarrhea, and fever. Children may present atypically with right lower quadrant abdominal pain that may be mistaken for appendicitis.
Heart infections
In the antibiotic era, pneumococcal cardiac infections are rare.
- Endocarditis: Involvement of native aortic and mitral valves are most common; infection can lead to valve destruction, heart failure, and embolization. Presenting signs and symptoms are typical of those seen in other causes of endocarditis and include fever, new or changing murmurs, muscle and/or joint pains, sweating, fatigue, anorexia, and skin findings. In alcoholics, may be part of the triad of endocarditis, pneumonia, and meningitis.
- Pericarditis: Prior to the widespread use of antibiotics, S pneumoniae infection was the most common cause of purulent pericarditis in children; now, infection in childhood is extremely rare, and nearly all cases of pneumococcal pericarditis occur in adults. Symptoms, signs, and examination findings may include chest and/or pleuritic pain; radiating pain to the neck, abdomen, shoulder, or back; orthopnea; dry cough; extremity swelling; anxiety; fatigue; fever; pericardial rub; and muffled heart sounds.
Acute exacerbations of chronic bronchitis
Acute exacerbations of chronic bronchitis manifest as a change from baseline chronic symptoms. Symptoms include shortness of breath, increased production and/or purulence of sputum, increased sputum tenacity, and cough.
An estimated 80% of cases of acute exacerbations of chronic bronchitis are caused by infection, with about one half of those caused by aerobic bacteria, of which Streptococcus pneumoniae is the most commonly isolated organism.
Symptoms such as sore throat, rhinorrhea, nasal congestion, and dyspnea (shortness of breath) may indicate a viral cause 67.
Pneumococcal disease complications
Serious pneumococcal infections can result in sepsis, long-term problems, or death. Sepsis is a life-threatening emergency resulting from the body’s extreme response to infection.
Pneumonia
Pneumonia can cause:
- Airway blockage, collapsed lungs, and lung abscesses (pus)
- Empyema (infection around the lungs and in the chest cavity)
- Pericarditis (inflammation of the outer lining of the heart)
Pneumococcal pneumonia kills about 1 in 20 people who get it.
Meningitis
Meningitis can cause developmental delay or hearing loss. About 1 in 12 children and 1 in 6 older adults who get pneumococcal meningitis dies of the infection.
Bacteremia
Bacteremia can result in loss of limbs. About 1 in 30 children with pneumococcal bacteremia die of it. Pneumococcal bacteremia kills about 1 in 8 adults who get it.
Minor infections
Complications are rare and not usually severe for mild infections like ear and sinus infections.
Pneumococcal disease diagnosis
How the pneumococcal disease diagnosis is made depends upon where the infection is. Your doctor will do a physical exam and ask about your medical history. If Streptococcus pneumoniae infection is suspected or considered, Gram stain and culture of appropriate specimens should be obtained, when possible. Potential specimens may include 1 or more of the following 15:
- Blood
- Cerebrospinal fluid (CSF)
- Sputum
- Pleural fluid or lung aspirate
- Joint fluid
- Bone
- Other abscess or tissue specimens
Specimens should be obtained prior to the initiation of antibiotic therapy and inoculated directly into blood-culture bottles, when possible.
Antibiotic susceptibilities should be obtained routinely on all cultures with growth of Streptococcus pneumoniae. Note that minimum inhibitory concentration (MIC) breakpoints are different depending on the specimen type.
Other laboratory values that may be helpful in diagnosis and treatment include a complete blood cell (CBC) count and differential, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).
In children who do not produce sputum and in adults with a nonproductive cough, the diagnosis may be made based on urine antigen testing for Streptococcus pneumoniae. As with urinary antigen testing for Legionella, antigenuria may not be present in early infection or in patients without bacteremia, but, if present, may persist after clinical resolution of infection. Evaluation of sputum via a combination of culture, Gram stain, and pneumococcal antigen was found to be the most useful way of achieving an etiologic diagnosis of community acquired pneumonia. Pneumococcal antigen detection in sputum has been shown to have high sensitivity (90%), even compared with urinary antigen detection essays, in early and mild community acquired pneumonia in pretreatment patients whose sputum specimens can be obtained 68. The pneumococcal urinary antigen assay may augment the standard diagnostic methods of blood culture and sputum culture, as it provides rapid results 69.
A commercially available urinary antigen test can detect the C-polysaccharide antigen of Streptococcus pneumoniae as a cause of community-acquired pneumonia. The urinary antigen test:
- Is rapid and simple to use
- Has a reasonable specificity in adults
- Can detect pneumococcal pneumonia after initiation of antibiotic therapy
In the diagnosis of Streptococcus pneumoniae community acquired pneumonia, the urinary antigen test has a sensitivity of 77%-88% and a specificity of 67%-100% 70. However, the clinical usefulness of this pneumococcal urinary antigen test is not well defined. The urinary antigen test is unable to provide antimicrobial susceptibility data, so it does not supplant traditional culture methods. The 2019 Infectious Diseases Society of America community acquired pneumonia guidelines do not recommend routine urinary testing for pneumococcal antigen in adults with community acquired pneumonia, except in adults with severe pneumonia 71.
The role of fiberoptic bronchoscopy is best done in the absence of adequate sputum for culture or when the patient is not responding to current therapy 72.
Culture and sensitivity
Antimicrobial susceptibility testing should be performed on all isolates of Streptococcus pneumoniae, regardless of the isolation site, because of the increasing prevalence of antibiotic resistant isolates. All isolates should be tested for susceptibility to penicillin and either cefotaxime or ceftriaxone. In addition, cerebrospinal fluid (CSF) isolates should be tested for susceptibility to vancomycin and meropenem. Cerebrospinal fluid (CSF) isolates that are found to be nonsusceptible to penicillin should also be tested for susceptibility to rifampin.
Microbiology laboratories should follow established guidelines regarding inoculum size and media (Mueller-Hinton agar with sheep, horse, or lysed horse red blood cells). Isolates from patients with invasive disease should undergo testing with quantitative minimal inhibitory concentration (MIC) techniques (eg, broth microdilution, antibiotic gradient strips).
The Clinical and Laboratory Institute (CLSI) (2010) has defined Streptococcus pneumoniae susceptibility as follows 73, 74:
- Pneumonia: For penicillin-sensitive Streptococcus pneumoniae (MIC < 2 μg/mL), penicillin G or amoxicillin is considered first-line therapy. For penicillin-resistant Streptococcus pneumoniae (MIC ≥2 μg/mL), the choice of antimicrobial agent should be directed by susceptibility testing.
- Cefotaxime or ceftriaxone considerations are as follows:
- Susceptible (non-CNS/CNS): MIC is ≤1/0.5 µg/mL, respectively.
- Intermediate (non-CNS/CNS): MIC is 2/1 µg/mL, respectively.
- Resistant (non-CNS/CNS): MIC is ≥4/2 µg/mL, respectively.
Strains with intermediate or resistant susceptibility patterns should be considered nonsusceptible and alternate therapy used.
Imaging studies
- Chest radiography: Chest radiography should be performed in most patients with evidence of invasive pneumococcal infection and in those with pneumococcal pneumonia. The typical chest radiography finding in adolescents and adults with pneumococcal pneumonia is lobar consolidation. Infants and young children with pneumococcal pneumonia more often have a pattern of scattered parenchymal consolidation and bronchopneumonia. Other chest radiography findings may include air bronchograms, pleural effusions/empyema, pneumatoceles, and, rarely, abscesses. Cavitation is not a feature of Streptococcus pneumoniae pneumonia and, if present, should prompt investigation for other pathogens.
- Ultrasonography/CT scanning:
- Chest ultrasonography or chest CT scanning may be obtained to provide information on the presence and/or extent of pleural effusion/empyema and parenchymal disease. Studies investigating the diagnostic utility of lung ultrasonography to diagnose pneumonia have also been promising 75.
- Echocardiography should be performed in patients in whom endocarditis is suspected.
- Sinus CT scanning may provide information about the presence and extent of sinus disease. Positive findings include opacification or air-fluid levels.
- Facial CT scanning should be obtained in patients with periorbital or orbital cellulitis to look for evidence of soft tissue swelling, bony involvement, cranial nerve impingement, or proptosis.
- MRI/CT scanning:
- MRI or CT scanning of affected bones or joints should be obtained to evaluate for evidence of joint destruction, periosteal elevation, or a mass.
- An MRI of the brain may be obtained in patients with meningitis to determine the location and extent of involvement but is not required by Infectious Disease Society of America (IDSA) guidelines.
Procedures
- Middle ear fluid aspiration
- Pleural fluid aspiration
- Chest tube thoracostomy or catheter placement
- Video-assisted thoracoscopy (VATS) or pleural decortication
- Lumbar puncture
- Joint fluid aspiration and/or wash-out of joint space
- Bone biopsy
- Soft tissue/muscle biopsy
Pneumococcal disease treatment
Antibiotics are the mainstay of treatment in Streptococcus pneumoniae infections 76, 77, 78, 79, 80, 81, 82, 83, 84. The first dose of antibiotics should be given as quickly as possible after the definitive diagnosis. Early administration of antibiotics is associated with a better prognosis and the failure to use antibiotics has been associated with an increased risk of in-hospital mortality and more than a five-fold increase in 30-day mortality 28, 29, 30, 31, 32, 33, 34, 35, 36, 37.
Antibiotic treatment for serious pneumococcal infections typically includes ‘broad-spectrum’ antibiotics until results of antibiotic sensitivity testing are available. Antibiotic sensitivity testing shows which antibiotics will be most successful at treating a bacterial infection. Broad-spectrum antibiotics work against a wide range of bacteria. Once the sensitivity of the bacteria is known, doctors may choose a more targeted (or ‘narrow-spectrum’) antibiotic.
Streptococcus pneumoniae bacteria are resistant to one or more antibiotics in more than 30% of cases 85. The CDC, as well as many state health departments, maintain a population-based surveillance system (the Active Bacterial Core surveillance system) that investigates the epidemiology and susceptibility patterns of invasive pneumococcal infections in the United States. In 2019, Active Bacterial Core surveillance estimated there were about 30,300 cases of invasive pneumococcal disease 86. 3.8% and 2.4% of the isolates obtained showed intermediate or resistant susceptibility patterns to penicillin and cefotaxime, respectively 86. One hundred percent of the isolated were susceptible to vancomycin 86. The prevalence of resistance varies greatly among countries, states, counties, and within populations in particular cities and may be as high as 30%-40% in some locations 87. Resistance rates are generally higher in most European countries, as well as in Hong Kong and Thailand 88.
Penicillin-resistant pneumococci are often resistant to multiple additional classes of antibiotics, including other penicillin derivatives, cephalosporins, sulfonamides, trimethoprim-sulfamethoxazole (through amino acid changes), macrolides (through methylation or via an efflux pump), quinolones (through decreased permeability, efflux pumps, and alteration of enzymes), and chloramphenicol (through inactivating enzymes).
Resistance rates of pneumococcal isolates in the United States to trimethoprim-sulfamethoxazole, tetracycline, and the macrolides are relatively high. Some isolates (< 10% in the United States) that are resistant to macrolides are also resistant to clindamycin.
State and local health departments have reported outbreaks of drug-resistant Streptococcus pneumoniae in 89:
- Long-term care settings
- Institutions for people living with HIV
- Childcare centers
Streptococcus pneumoniae antibiotics
Penicillin and its derivatives are inexpensive effective antibiotics for treating pneumococcal infections when they are used against susceptible isolates. Penicillins can be administered orally or parenterally and work by inhibiting cell wall synthesis. Penicillin G is the parenteral drug of choice for susceptible Streptococcus pneumoniae infections, and other parenteral beta-lactams do not provide additional or improved coverage (nor do beta-lactamase inhibitor combinations).
Cephalosporins’ mechanism of action and modes of resistance are the same as for all other beta-lactams. First-generation cephalosporins provide similar coverage in the treatment of penicillin-susceptible strains, although many of them have higher MICs. Penicillin- and cefotaxime-susceptible strains of Streptococcus pneumoniae were estimated at 96.2% and 97.6%, respectively 86.
In most cases, macrolides have activity against penicillin-susceptible strains of Streptococcus pneumoniae. However, between 1998 and 2011, resistance rates have increased to an estimated 25%-45% in the United States 90. In 2019, the CDC’s active bacterial core surveillance report found the erythromycin resistance rate to be 29.3% 86.
Macrolides have poor CSF penetration and should not be used to treatment meningitis 91.
Most pneumococcal isolates in the United States remain susceptible to respiratory fluoroquinolones. In the United States, less than 1% of Streptococcus pneumoniae isolates are resistant to levofloxacin, moxifloxacin, or gemifloxacin 92. Ciprofloxacin and ofloxacin have limited activity against pneumococcal infections. Fluoroquinolones achieve excellent serum drug levels and tissue penetration. Specific populations in whom the use of fluoroquinolones is traditionally increased (eg, nursing home residents) have shown increased rates of pneumococcal resistance to fluoroquinolones, serving as a reminder that consideration of their empiric use in uncomplicated respiratory infections should be tempered by concern for the promotion of further antimicrobial resistance.
Vancomycin, dalbavancin, and telavancin are glycopeptide antibiotics that have demonstrated efficacy against pneumococcal infections 93. To date, no clinical or in vitro evidence of pneumococcal resistance to vancomycin has been reported in the United States, and it is the drug of choice (with a third-generation cephalosporin) in the treatment of penicillin-resistant pneumococcal meningitis.
The increasing number of pneumococcal isolates resistant to trimethoprim-sulfamethoxazole precludes its use unless susceptibilities are known and beta-lactam use is contraindicated.
Clindamycin may also be used to treat nonmeningeal Streptococcus pneumoniae infections. Approximately 5%-10% of Streptococcus pneumoniae strains in the United States are resistant to clindamycin 94. As such, clindamycin should be used only after susceptibility testing has confirmed activity on clinical isolates. Penicillin or macrolide resistance may also be associated with clindamycin resistance in individual isolates.
Carbapenems are also effective against Streptococcus pneumoniae but should be reserved for specific cases given their broad coverage and the potential for development of resistance by multiple organisms.
Pneumococcal pneumonia
Pneumococcal pneumonia treatment is antibiotic therapy and supportive care including mechanical ventilation if necessary. Treatment of community-acquired pneumonia varies based on the area of practice and severity of the disease. In 2019, the Infectious Disease Society of America (IDSA) guidelines for diagnosis and treatment of community-acquired pneumonia were published 71. In healthy outpatient adults without comorbidities (eg, chronic heart, lung, liver or renal disease; diabetes mellitus, alcoholism, malignancy and asplenia), monotherapy with amoxicillin, doxycycline, or a macrolide (clarithromycin or azithromycin) is recommended; however, the use of macrolides should be limited to areas with less than 25% pneumococcal resistance to macrolides. Outpatients with the comorbidities listed above should receive either (1) combination therapy with amoxicillin/clavulanate or a cephalosporin (cefpodoxime or cefuroxime) plus a macrolide or doxycycline or (2) monotherapy with a respiratory fluoroquinolone (moxifloxacin, levofloxacin, or gemifloxacin). Regarding the treatment of hospitalized patients with CAP, the recommended regimens consist of (1) combination therapy with a beta-lactam and a macrolide or (2) monotherapy with a respiratory fluoroquinolone. There was not enough evidence to support beta-lactam monotherapy over fluoroquinolone therapy or combination beta-lactam/macrolide in hospitalized patients.
A recent Cochrane review shows the non-superiority of any outpatient antibiotic regimen for community-acquired pneumonia concerning the other drug classes 95, 96.
The first dose of antibiotics should be given as quickly as possible after the definitive diagnosis. The American College of Emergency Physicians policy statement gives a level B recommendation that there is not enough evidence to establish a benefit in mortality or morbidity from starting the antibiotics in less than 4, 6, or 8 hours 97. The American College of Emergency Physicians clinical policy also notes that there is not enough evidence to determine if there is a benefit in morbidity or mortality from antibiotics being administered within any specific time course but recommends to begin antibiotics as soon as the diagnosis is made.
Patients with pneumococcal pneumonia who do not respond or respond slower than usual to initial treatment should undergo follow-up chest radiography. Worsening disease and/or the presence of a pleural effusion may indicate the need for consultation with a pulmonologist, an infectious disease specialist, and/or a surgeon for further intervention. Oral therapy can be initiated when patients have clinically improved and become afebrile. Repeat chest radiography should be performed 4-8 weeks after therapy is completed to ensure resolution of disease. Chest radiography findings may remain abnormal for weeks to months, particularly following severe disease or complicated pneumonias.
Patients with complicated pneumonia having parapneumonic effusion may need a tube thoracostomy and if it further progresses to empyema and is resistant to drainage by tube thoracostomy then decortication is required with video-assisted thoracoscopic surgery (VATS).
Pneumococcal meningitis
Patients with pneumococcal meningitis should be admitted to the hospital and treated with parenteral antibiotics. Per Infectious Disease Society of America guidelines, the initial treatment for pneumonococcal meningitis should be vancomycin and a third-generation cephalosporin 98.
For the treatment of pneumococcal meningitis in children who are allergic to beta-lactams, a combination of vancomycin and rifampin should be considered. Monotherapy with vancomycin should not be attempted, as it is difficult to achieve sustained adequate bactericidal concentrations of vancomycin in the CSF. Monotherapy with rifampin should also not be attempted owing to the high potential for rapid development of resistance in this setting.
In patients infected with rifampin-sensitive pneumococcal isolates, the addition of rifampin should be considered after 48 hours if (1) the clinical condition has worsened despite treatment with vancomycin and cefotaxime/ceftriaxone, (2) repeat lumbar puncture repeatedly yields positive culture results, and/or (3) the isolate displays an minimum inhibitory concentration (MIC) to cefotaxime/ceftriaxone of ≥4 µg/mL.
The recommendations for treatment of bacterial meningitis in adults are similar to those in children.
The use of systemic steroids within 15 minutes of initiating infusion of antibiotics in adult patients with bacterial meningitis is usually recommended with caution, as they may decrease cerebrospinal fluid (CSF) antibiotic concentration; patients with meningitis treated with steroids should be monitored closely 99.
Steroids can be considered prior to antibiotic therapy in children aged 6 weeks and older with possible pneumococcal meningitis. If used, they should be given before or at the time of the first dose of antibiotics.
A repeat lumbar puncture should be considered after 48 hours of therapy in the following circumstances:
- Patients whose isolates are not susceptible to penicillin based on oxacillin disc diffusion testing or minimum inhibitory concentration (MIC) testing without pending results of cefotaxime and/or ceftriaxone susceptibilities
- Patients whose condition has worsened or has not improved
- Patients who received steroid therapy (which could alter the ability to observe clinical improvement/worsening)
Intravenous fluids, parenteral/enteral nutrition, and other medications should be used as indicated in appropriate clinical instances.
Pneumococcal bacteremia and sepsis
Patients with pneumococcal bacteremia should be treated with appropriate antibiotics and supportive care.
Repeat blood cultures should always be obtained in patients with Streptococcus pneumoniae bacteremia until culture results are negative.
Patients with signs or symptoms of sepsis should be admitted to the hospital and treated aggressively with antibiotics and other medical therapies, as indicated.
Pneumococcal conjunctivitis, otitis media, sinusitis, bronchitis, and tracheobronchitis
Most patients with conjunctivitis, otitis media, sinusitis, bronchitis, and tracheobronchitis due to Streptococcus pneumoniae infection can be treated on an outpatient basis with appropriate antibiotics. Compliance and follow-up should be ensured.
Infants and elderly patients, as well as those with immunodeficiencies, underlying disease, or signs of severe disease, should be treated more aggressively and hospitalized when indicated.
Otitis media
The guideline produced by the American Academies of Pediatrics and Family Practitioners for the treatment of pneumococcal otitis media recommends first-line treatment of most patients with amoxicillin 80-90 mg/kg/day or amoxicillin-clavulanate (amoxicillin 90 mg/kg/day with clavulanate 6.4 mg/kg/day). Alternatives include cefdinir, cefuroxime, cefpodoxime, or ceftriaxone. These alternative antibiotics vary in their efficacy against the different pathogens known to cause otitis media. US data on in vitro susceptibility of Streptococcus pneumoniae to cefdinir and cefuroxime are 70% to 80%, respectively, compared with 84% to 92% to amoxicillin 100.
Patients who do not improve within 48-72 hours should be re-evaluated and their antibiotics switched to amoxicillin-clavulanate or a second- or third-generation oral cephalosporin, although highly resistant pneumococci may require treatment with parenteral ceftriaxone in order to achieve adequate serum levels of antibiotics.
Sinusitis
The typical pathogens that cause sinusitis mimic those of otitis media; therefore, initial therapeutic recommendations are similar. In adult allergic patients and in adults who do not respond to initial therapy, fluoroquinolones provide appropriate coverage. In this clinical situation, this class of antibiotics is not approved for children.
Other invasive pneumococcal infections
Purulent pneumococcal pericarditis and endocarditis are serious diseases and should be treated aggressively with appropriate courses of parenteral antibiotics.
Blood cultures should be obtained until multiple negative sets are documented. Repeat chest radiography, echocardiography, and other imaging tests may be repeated as recommended to monitor disease resolution.
Patients with osteomyelitis and joint infections caused by S pneumoniae infection should be monitored closely for a decrease in pain and inflammatory markers and improved use of the affected limb or joint. Failure to improve should prompt re-evaluation of the area via aspiration, washout, biopsy, or repeat imaging.
Surgical care
Patients with complicated pneumonia may require a chest tube for drainage of pleural fluid; video-assisted thoracoscopic surgery (VATS) or decortication may be required in more severe cases or in those with empyema.
In patients with suspected septic arthritis or osteomyelitis, synovial fluid or bone tissue should be obtained for Gram stain, cell count, histology, and culture.
Patients with recurrent or chronic otitis media, periorbital or orbital cellulitis, or facial cellulitis may require surgical intervention.
Pneumococcal disease prognosis
Pneumococcal conjunctivitis, otitis media, and sinusitis in developed countries where appropriate antibiotics are available usually carry an excellent prognosis 101.
The prognosis of pneumococcal pneumonia depends largely on underlying factors, including age, immunosuppression, availability of antibiotics, and extent of lung involvement. It appears that most adults (mean age, 64.6 years) who survive invasive pneumococcal pneumonia lose a mean 9.9 years of longevity 102.
The prognosis of pneumococcal meningitis is also related in part to host factors. Most studies have shown that morbidity rates in otherwise healthy US children with meningitis are usually less than 10%; however, neurological complications are common 101.
- Al-Jumaili A, Dawood HN, Ikram D, Al-Jabban A. Pneumococcal Disease: Global Disease Prevention Strategies with a Focus on the Challenges in Iraq. Int J Gen Med. 2023 May 29;16:2095-2110. doi: 10.2147/IJGM.S409476[↩][↩]
- Ganaie F., Saad J.S., McGee L., van Tonder A.J., Bentley S.D., Lo S.W., Gladstone R.A., Turner P., Keenan J.D., Breiman R.F., et al. A New Pneumococcal Capsule Type, 10D, is the 100th Serotype and Has a Large cps Fragment from an Oral Streptococcus. mBio. 2020;11:e00937-20. doi: 10.1128/mBio.00937-20[↩][↩]
- Geno K.A., Gilbert G.L., Song J.Y., Skovsted I.C., Klugman K.P., Jones C., Konradsen H.B., Nahm M.H. Pneumococcal Capsules and Their Types: Past, Present, and Future. Clin. Microbiol. Rev. 2015;28:871–899. doi: 10.1128/CMR.00024-15[↩][↩]
- Garcia-Vidal C, et al. Early mortality in patients with community-acquired pneumonia: causes and risk factors. Eur Respir J. 2008;32(3):733–739. doi: 10.1183/09031936.00128107[↩]
- Koivula I, Sten M, Makela PH. Risk factors for pneumonia in the elderly. Am J Med. 1994;96(4):313–320. doi: 10.1016/0002-9343(94)90060-4[↩][↩]
- Metlay JP, et al. Influence of age on symptoms at presentation in patients with community-acquired pneumonia. Arch Intern Med. 1997;157(13):1453–1459. doi: 10.1001/archinte.1997.00440340089009[↩]
- Black RE, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375(9730):1969–1987. doi: 10.1016/S0140-6736(10)60549-1[↩]
- Bogaert D, De Groot R, Hermans PW. Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis. 2004;4(3):144–154. doi: 10.1016/S1473-3099(04)00938-7[↩][↩][↩]
- Berger G. Nature of spontaneous tympanic membrane perforation in acute otitis media in children. J Laryngol Otol. 1989;103(12):1150–1153. doi: 10.1017/S0022215100111247[↩]
- Casselbrant ML, et al. Otitis media with effusion in preschool children. Laryngoscope. 1985;95(4):428–436. doi: 10.1288/00005537-198504000-00011[↩]
- Fria TJ, Cantekin EI, Eichler JA. Hearing acuity of children with otitis media with effusion. Arch Otolaryngol. 1985;111(1):10–16. doi: 10.1001/archotol.1985.00800030044003[↩]
- Williams CJ, Jacobs AM. The impact of otitis media on cognitive and educational outcomes. Med J Aust. 2009;191(S9):S69–72. doi: 10.5694/j.1326-5377.2009.tb02931.x[↩]
- Berman S. Otitis media in developing countries. Pediatrics. 1995 Jul;96(1 Pt 1):126-31.[↩]
- Jedrzejas M. J. (2001). Pneumococcal virulence factors: structure and function. Microbiology and molecular biology reviews : MMBR, 65(2), 187–207. https://doi.org/10.1128/MMBR.65.2.187-207.2001[↩]
- Pneumococcal Infections (Streptococcus pneumoniae). https://emedicine.medscape.com/article/225811-overview[↩][↩]
- Pneumococcal Disease. https://www.cdc.gov/vaccines/pubs/pinkbook/pneumo.html[↩]
- Weiser, J. N., Ferreira, D. M., & Paton, J. C. (2018). Streptococcus pneumoniae: transmission, colonization and invasion. Nature reviews. Microbiology, 16(6), 355–367. https://doi.org/10.1038/s41579-018-0001-8[↩][↩][↩]
- Ask the Experts: Pneumococcal. https://www.immunize.org/ask-experts/topic/pneumococcal[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Grabenstein J.D., Musher D.M. 47—Pneumococcal Polysaccharide Vaccines. In: Plotkin S.A., Orenstein W.A., Offit P.A., Edwards K.M., editors. Plotkin’s Vaccines. 7th ed. Elsevier; Amsterdam, The Netherlands: 2018. pp. 816–840.e813.[↩]
- Klugman K.P., Dagan R., Malley R., Whitney C.G. 46—Pneumococcal Conjugate Vaccine and Pneumococcal Common Protein Vaccines. In: Plotkin S.A., Orenstein W.A., Offit P.A., Edwards K.M., editors. Plotkin’s Vaccines. 7th ed. Elsevier; Amsterdam, The Netherlands: 2018. pp. 773–815.e718.[↩]
- Shea K.M., Edelsberg J., Weycker D., Farkouh R.A., Strutton D.R., Pelton S. Rates of Pneumococcal Disease in Adults with Chronic Medical Conditions. Open Forum Infect. Dis. 2014;1:ofu024. doi: 10.1093/ofid/ofu024[↩]
- van Hoek A.J., Andrews N., Waight P.A., Stowe J., Gates P., George R., Miller E. The effect of underlying clinical conditions on the risk of developing invasive pneumococcal disease in England. J. Infect. 2012;65:17–24. doi: 10.1016/j.jinf.2012.02.017[↩]
- Grant L.R., Slack M.P.E., Yan Q., Trzciński K., Barratt J., Sobczyk E., Appleby J., Cané A., Jodar L., Isturiz R.E., et al. The epidemiologic and biologic basis for classifying older age as a high-risk, immunocompromising condition for pneumococcal vaccine policy. Expert Rev. Vaccines. 2021;20:691–705. doi: 10.1080/14760584.2021.1921579[↩]
- Pneumococcal Disease. https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/norms-and-standards/vaccine-standardization/pneumococcal-disease[↩]
- Wahl B, O’Brien KL, Greenbaum A, et al. Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15. Lancet Glob Health. 2018;6(7):e744–e757. doi: 10.1016/S2214-109X(18)30247-X[↩][↩]
- Pneumococcal Vaccine Recommendations. https://www.cdc.gov/pneumococcal/hcp/vaccine-recommendations/index.html[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Ludwig E, et al. The remaining challenges of pneumococcal disease in adults. Eur Respir Rev. 2012;21(123):57–65. doi: 10.1183/09059180.00008911[↩]
- Garnacho-Montero J, et al. Determinants of outcome in patients with bacteraemic pneumococcal pneumonia: Importance of early adequate treatment. Scand J Infect Dis. 2010;42(3):185–192. doi: 10.3109/00365540903418522[↩][↩]
- Garnacho-Montero J, et al. Timing of adequate antibiotic therapy is a greater determinant of outcome than are TNF and IL-10 polymorphisms in patients with sepsis. Crit Care. 2006;10(4):R111. doi: 10.1186/cc4995[↩][↩]
- Zasowski EJ, et al. A Systematic Review of the Effect of Delayed Appropriate Antibiotic Treatment on the Outcomes of Patients With Severe Bacterial Infections. Chest. 2020;158(3):929–938. doi: 10.1016/j.chest.2020.03.087[↩][↩]
- Nauclér P, et al. Impact of time to antibiotic therapy on clinical outcome in patients with bacterial infections in the emergency department: implications for antimicrobial stewardship. Clin Microbiol Infect. 2021;27(2):175–181. doi: 10.1016/j.cmi.2020.02.032[↩][↩]
- Mortensen EM, et al. Effects of guideline-concordant antimicrobial therapy on mortality among patients with community-acquired pneumonia. Am J Med. 2004;117(10):726–731. doi: 10.1016/j.amjmed.2004.06.028[↩][↩]
- Bodi M, et al. Antibiotic prescription for community-acquired pneumonia in the intensive care unit: impact of adherence to Infectious Diseases Society of America guidelines on survival. Clin Infect Dis. 2005;41(12):1709–1716. doi: 10.1086/498119[↩][↩]
- Malone DC, Shaban HM. Adherence to ATS guidelines for hospitalized patients with community-acquired pneumonia. Ann Pharmacother. 2001;35(10):1180–1185. doi: 10.1345/aph.10283[↩][↩]
- Menendez R, et al. Influence of deviation from guidelines on the outcome of community-acquired pneumonia. Chest. 2002;122(2):612–617. doi: 10.1378/chest.122.2.612[↩][↩]
- Lee C-C, et al. Timing of appropriate empirical antimicrobial administration and outcome of adults with community-onset bacteremia. Crit Care. 2017;21(1):119. doi: 10.1186/s13054-017-1696-z[↩][↩]
- Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, Artigas A, Schorr C, Levy MM. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014 Aug;42(8):1749-55. doi: 10.1097/CCM.0000000000000330[↩][↩]
- Kruckow KL, Zhao K, Bowdish DME, Orihuela CJ. Acute organ injury and long-term sequelae of severe pneumococcal infections. Pneumonia (Nathan). 2023 Mar 5;15(1):5. doi: 10.1186/s41479-023-00110-y[↩]
- https://phil.cdc.gov/Details.aspx?pid=9996[↩]
- https://phil.cdc.gov/Details.aspx?pid=10864[↩]
- https://phil.cdc.gov/Details.aspx?pid=19332[↩]
- Pilishvili T., Bennett N.M. Pneumococcal disease prevention among adults: Strategies for the use of pneumococcal vaccines. Vaccine. 2015;33:D60–D65. doi: 10.1016/j.vaccine.2015.05.102[↩]
- Pneumococcal Vaccination: Information for Healthcare Professionals. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/index.html[↩]
- About Pneumococcal Vaccines. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/about-vaccine.html[↩]
- Types of Pneumococcal Vaccines. https://www.cdc.gov/pneumococcal/vaccines/types.html[↩]
- VAXNEUVANCE. https://www.fda.gov/vaccines-blood-biologics/vaccines/vaxneuvance[↩]
- PREVNAR 20. https://www.fda.gov/vaccines-blood-biologics/vaccines/prevnar-20[↩]
- CAPVAXIVE. https://www.fda.gov/vaccines-blood-biologics/capvaxive[↩]
- Centers for Disease Control and Prevention (CDC). Licensure of 13-valent pneumococcal conjugate vaccine for adults aged 50 years and older. MMWR Morb Mortal Wkly Rep. 2012 Jun 1;61(21):394-5. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6121a3.htm[↩]
- PNEUMOVAX 23 – Pneumococcal Vaccine, Polyvalent. https://www.fda.gov/vaccines-blood-biologics/vaccines/pneumovax-23-pneumococcal-vaccine-polyvalent[↩]
- Pneumococcal Vaccination. https://www.cdc.gov/pneumococcal/vaccines/index.html[↩]
- Administering Pneumococcal Vaccines. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/administering-vaccine.html[↩][↩][↩]
- Pneumococcal Conjugate Vaccine: What You Need to Know. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/pcv.pdf[↩][↩]
- Theilacker C, Fletcher MA, Jodar L, Gessner BD. PCV13 Vaccination of Adults against Pneumococcal Disease: What We Have Learned from the Community-Acquired Pneumonia Immunization Trial in Adults (CAPiTA). Microorganisms. 2022 Jan 8;10(1):127. doi: 10.3390/microorganisms10010127. Erratum in: Microorganisms. 2022 May 12;10(5):1018. doi: 10.3390/microorganisms10051018[↩][↩]
- Geno KA, Gilbert GL, Song JY, et al. Pneumococcal capsules and their types: past, present, and future. Clin Microbiol Rev. 2015;28(3):871–899. doi: 10.1128/CMR.00024-15[↩]
- Bentley SD, Aanensen DM, Mavroidi A, et al. Genetic analysis of the capsular biosynthetic locus from all 90 pneumococcal serotypes. PLoS Genet. 2006;2(3):e31. doi: 10.1371/journal.pgen.0020031[↩]
- Pneumococcal Disease Transmission. https://www.cdc.gov/pneumococcal/clinicians/transmission.html[↩]
- Musher DM, et al. Bacteremic and nonbacteremic pneumococcal pneumonia. A prospective study Medicine (Baltimore) 2000;79(4):210–221. doi: 10.1097/00005792-200007000-00002[↩]
- Jover F, et al. A comparative study of bacteremic and non-bacteremic pneumococcal pneumonia. Eur J Intern Med. 2008;19(1):15–21. doi: 10.1016/j.ejim.2007.03.015[↩]
- Klemets P, et al. Invasive pneumococcal infections among persons with and without underlying medical conditions: implications for prevention strategies. BMC Infect Dis. 2008;8:96. doi: 10.1186/1471-2334-8-96[↩][↩]
- Ben-Shimol S, et al. Seasonality of Both Bacteremic and Nonbacteremic Pneumonia Coincides With Viral Lower Respiratory Tract Infections in Early Childhood, in Contrast to Nonpneumonia Invasive Pneumococcal Disease, in the Pre-Pneumococcal Conjugate Vaccine Era. Clin Infect Dis. 2015;60(9):1384–1387. doi: 10.1093/cid/civ023[↩]
- van Mens SP, et al. Bacteraemic and non-bacteraemic/urinary antigen-positive pneumococcal community-acquired pneumonia compared. Eur J Clin Microbiol Infect Dis. 2015;34(1):115–122. doi: 10.1007/s10096-014-2209-5[↩]
- Pneumococcal Disease Risk Factors. https://www.cdc.gov/pneumococcal/clinicians/risk-factors.html[↩]
- Pneumococcal Infections (Streptococcus pneumoniae) Clinical Presentation. https://emedicine.medscape.com/article/225811-clinical[↩][↩]
- Dagan R, Greenberg D, Jacobs MR. Pneumococcal Infections. Feigin RD, Cherry JD, Demmler GJ, Kaplan SL. Textbook of Pediatric Infectious Diseases. 5th. Philadelphia, Pennsylvania: Saunders (Elsevier Science); 2004. 1: 1204-1258/90.[↩][↩]
- Bradley JS, Kaplan SL, Tan TQ, Barson WJ, Arditi M, Schutze GE, Wald ER, Givner LB, Mason EO. Pediatric pneumococcal bone and joint infections. The Pediatric Multicenter Pneumococcal Surveillance Study Group (PMPSSG). Pediatrics. 1998 Dec;102(6):1376-82. doi: 10.1542/peds.102.6.1376[↩]
- Brunton S, Carmichael BP, Colgan R, Feeney AS, Fendrick AM, Quintiliani R, Scott G. Acute exacerbation of chronic bronchitis: a primary care consensus guideline. Am J Manag Care. 2004 Oct;10(10):689-96.[↩]
- Fukushima K, Nakamura S, Inoue Y, Higashiyama Y, Ohmichi M, Ishida T, Yoshimura K, Sawai T, Takayanagi N, Nakahama C, Kakugawa T, Izumikawa K, Aoki N, Nishioka Y, Kosaka O, Kohno S. Utility of a Sputum Antigen Detection Test in Pneumococcal Pneumonia and Lower Respiratory Infectious Disease in Adults. Intern Med. 2015;54(22):2843-50. doi: 10.2169/internalmedicine.54.4082[↩]
- Mandell, L. A., Wunderink, R. G., Anzueto, A., Bartlett, J. G., Campbell, G. D., Dean, N. C., Dowell, S. F., File, T. M., Jr, Musher, D. M., Niederman, M. S., Torres, A., Whitney, C. G., Infectious Diseases Society of America, & American Thoracic Society (2007). Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 44 Suppl 2(Suppl 2), S27–S72. https://doi.org/10.1086/511159[↩]
- Blaschke A. J. (2011). Interpreting assays for the detection of Streptococcus pneumoniae. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 52 Suppl 4(Suppl 4), S331–S337. https://doi.org/10.1093/cid/cir048[↩]
- Metlay, J. P., Waterer, G. W., Long, A. C., Anzueto, A., Brozek, J., Crothers, K., Cooley, L. A., Dean, N. C., Fine, M. J., Flanders, S. A., Griffin, M. R., Metersky, M. L., Musher, D. M., Restrepo, M. I., & Whitney, C. G. (2019). Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American journal of respiratory and critical care medicine, 200(7), e45–e67. https://doi.org/10.1164/rccm.201908-1581ST[↩][↩]
- van der Eerden MM, Vlaspolder F, de Graaff CS, Groot T, Jansen HM, Boersma WG. Value of intensive diagnostic microbiological investigation in low- and high-risk patients with community-acquired pneumonia. Eur J Clin Microbiol Infect Dis. 2005 Apr;24(4):241-9. doi: 10.1007/s10096-005-1316-8[↩]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: 18th Informational Supplement. 2008.[↩]
- Effects of New Penicillin Susceptibility Breakpoints for Streptococcus pneumoniae — United States, 2006–2007. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5750a2.htm[↩]
- Chavez, M. A., Shams, N., Ellington, L. E., Naithani, N., Gilman, R. H., Steinhoff, M. C., Santosham, M., Black, R. E., Price, C., Gross, M., & Checkley, W. (2014). Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respiratory research, 15(1), 50. https://doi.org/10.1186/1465-9921-15-50[↩]
- Waterer GW, Somes GW, Wunderink RG. Monotherapy may be suboptimal for severe bacteremic pneumococcal pneumonia. Arch Intern Med. 2001;161(15):1837–1842. doi: 10.1001/archinte.161.15.1837[↩]
- Houck PM, et al. Empiric antibiotic therapy and mortality among medicare pneumonia inpatients in 10 western states : 1993, 1995, and 1997. Chest. 2001;119(5):1420–1426. doi: 10.1378/chest.119.5.1420[↩]
- Bartlett JG, et al. Practice guidelines for the management of community-acquired pneumonia in adults. Infectious Diseases Society of America. Clin Infect Dis. 2000;31(2):347–382. doi: 10.1086/313954[↩]
- Lim WS, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64(Suppl 3):iii1–55. doi: 10.1136/thx.2009.121434[↩]
- Mandell LA, et al. Canadian guidelines for the initial management of community-acquired pneumonia: an evidence-based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Canadian Community-Acquired Pneumonia Working Group. Clin Infect Dis. 2000;31(2):383–421. doi: 10.1086/313959[↩]
- Metlay JP, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–e67. doi: 10.1164/rccm.201908-1581ST[↩]
- Blot SI, Rodriguez A, Solé-Violán J, Blanquer J, Almirall J, Rello J; Community-Acquired Pneumonia Intensive Care Units (CAPUCI) Study Investigators. Effects of delayed oxygenation assessment on time to antibiotic delivery and mortality in patients with severe community-acquired pneumonia. Crit Care Med. 2007 Nov;35(11):2509-14. doi: 10.1097/01.CCM.0000287587.43801.9C[↩]
- Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, Dean N, File T, Fine MJ, Gross PA, Martinez F, Marrie TJ, Plouffe JF, Ramirez J, Sarosi GA, Torres A, Wilson R, Yu VL; American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001 Jun;163(7):1730-54. doi: 10.1164/ajrccm.163.7.at1010[↩]
- Dion CF, Ashurst JV. Streptococcus pneumoniae. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470537[↩]
- ANTIBIOTIC RESISTANCE THREATS IN THE UNITED STATES 2019. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf[↩]
- Active Bacterial Core Surveillance (ABCs) Report Emerging Infections Program Network. Streptococcus pneumoniae, 2019. https://www.cdc.gov/abcs/downloads/SPN_Surveillance_Report_2019.pdf[↩][↩][↩][↩][↩]
- Karlowsky JA, Thornsberry C, Jones ME, Evangelista AT, Critchley IA, Sahm DF; TRUST Surveillance Program. Factors associated with relative rates of antimicrobial resistance among Streptococcus pneumoniae in the United States: results from the TRUST Surveillance Program (1998-2002). Clin Infect Dis. 2003 Apr 15;36(8):963-70. doi: 10.1086/374052[↩]
- Song, J. H., Jung, S. I., Ko, K. S., Kim, N. Y., Son, J. S., Chang, H. H., Ki, H. K., Oh, W. S., Suh, J. Y., Peck, K. R., Lee, N. Y., Yang, Y., Lu, Q., Chongthaleong, A., Chiu, C. H., Lalitha, M. K., Perera, J., Yee, T. T., Kumarasinghe, G., Jamal, F., … Shibl, A. (2004). High prevalence of antimicrobial resistance among clinical Streptococcus pneumoniae isolates in Asia (an ANSORP study). Antimicrobial agents and chemotherapy, 48(6), 2101–2107. https://doi.org/10.1128/AAC.48.6.2101-2107.2004[↩]
- Pneumococcal Disease Drug Resistance. https://www.cdc.gov/pneumococcal/clinicians/drug-resistance.html[↩]
- Jones RN, Sader HS, Mendes RE, Flamm RK. Update on antimicrobial susceptibility trends among Streptococcus pneumoniae in the United States: report of ceftaroline activity from the SENTRY Antimicrobial Surveillance Program (1998-2011). Diagn Microbiol Infect Dis. 2013 Jan;75(1):107-9. doi: 10.1016/j.diagmicrobio.2012.08.024[↩]
- Hawser SP. Activity of tigecycline against Streptococcus pneumoniae, an important causative pathogen of community-acquired pneumonia (CAP). J Infect. 2010 Apr;60(4):306-8. doi: 10.1016/j.jinf.2010.02.003[↩]
- Jones RN, Jacobs MR, Sader HS. Evolving trends in Streptococcus pneumoniae resistance: implications for therapy of community-acquired bacterial pneumonia. Int J Antimicrob Agents. 2010 Sep;36(3):197-204. doi: 10.1016/j.ijantimicag.2010.04.013[↩]
- Jones, R. N., Schuchert, J. E., & Mendes, R. E. (2016). Dalbavancin Activity When Tested against Streptococcus pneumoniae Isolated in Medical Centers on Six Continents (2011 to 2014). Antimicrobial agents and chemotherapy, 60(6), 3419–3425. https://doi.org/10.1128/AAC.00116-16[↩]
- Henriques-Normark, B., & Tuomanen, E. I. (2013). The pneumococcus: epidemiology, microbiology, and pathogenesis. Cold Spring Harbor perspectives in medicine, 3(7), a010215. https://doi.org/10.1101/cshperspect.a010215[↩]
- Osowicki J, Steer AC. International survey of paediatric infectious diseases consultants on the management of community-acquired pneumonia complicated by pleural empyema. J Paediatr Child Health. 2019 Jan;55(1):66-73. doi: 10.1111/jpc.14128[↩]
- Jakhar SK, Pandey M, Shah D, Ramachandran VG, Saha R, Gupta N, Gupta P. Etiology and Risk Factors Determining Poor Outcome of Severe Pneumonia in Under-Five Children. Indian J Pediatr. 2018 Jan;85(1):20-24. doi: 10.1007/s12098-017-2514-y[↩]
- American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Community-Acquired Pneumonia, Smith MD, Fee C, Mace SE, Maughan B, Perkins JC Jr, Kaji A, Wolf SJ. Clinical Policy: Critical Issues in the Management of Adult Patients Presenting to the Emergency Department With Community-Acquired Pneumonia. Ann Emerg Med. 2021 Jan;77(1):e1-e57. https://www.acep.org/globalassets/new-pdfs/clinical-policies/cp-pneumonia.pdf[↩]
- Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, Whitley RJ. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004 Nov 1;39(9):1267-84. doi: 10.1086/425368[↩]
- van de Beek D, de Gans J, McIntyre P, Prasad K. Steroids in adults with acute bacterial meningitis: a systematic review. Lancet Infect Dis. 2004 Mar;4(3):139-43. doi: 10.1016/S1473-3099(04)00937-5[↩]
- Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, Joffe MD, Miller DT, Rosenfeld RM, Sevilla XD, Schwartz RH, Thomas PA, Tunkel DE. The diagnosis and management of acute otitis media. Pediatrics. 2013 Mar;131(3):e964-99. doi: 10.1542/peds.2012-3488. Epub 2013 Feb 25. Erratum in: Pediatrics. 2014 Feb;133(2):346. Dosage error in article text.[↩]
- Pneumococcal Infections (Streptococcus pneumoniae). https://emedicine.medscape.com/article/225811-overview#a3[↩][↩]
- Ajayi OO, Norton NB, Gress TW, Stanek RJ, Mufson MA. Three Decades of Follow-up of Adults After Recovery From Invasive Pneumococcal Pneumonia. Am J Med Sci. 2017 May;353(5):445-451. doi: 10.1016/j.amjms.2017.03.002[↩]