Contents
What is sinusitis
Sinusitis is an inflammation of the mucous membrane (the lining of the sinuses) of one or more paranasal sinuses. The sinuses are small, air-filled cavities behind your cheekbones and forehead. The mucus produced by your sinuses usually drains into your nose through small channels. In sinusitis, these channels become blocked because the sinus linings are inflamed (swollen).
Sinusitis may be caused by a microbial infection (virus, bacterium, or fungus), allergic reactions, nasal polyps, or a severely deviated nasal septum. However, sinusitis is usually caused by a viral infection and often improves within two or three weeks without the need for medical treatment. If the inflammation or an obstruction blocks the drainage of mucus into the nasal cavity, fluid pressure builds up in the paranasal sinuses, and a sinus headache may develop. Other symptoms may include nasal congestion, inability to smell, fever, and cough.
Sinusitis is a common symptom after colds and the flu. If you have sinusitis, your symptoms will usually get worse after five days, or will last for more than 10 days. In some cases, there is an infection in the sinuses caused by bacteria.
There are several types of sinusitis, including:
- Acute sinusitis, symptoms come on suddenly, which lasts up to 4 weeks
- Subacute sinusitis, symptoms which lasts 4 to 12 weeks
- Chronic sinusitis, symptoms last more than 12 weeks and can continue for months or even years
- Recurrent sinusitis, with several attacks within a year
Acute sinusitis often starts as a cold, which then turns into a bacterial infection. Allergies, nasal problems, and certain diseases can also cause acute and chronic sinusitis.
Symptoms of sinusitis can include fever, weakness, fatigue, cough, and congestion. There may also be mucus drainage in the back of the throat, called postnasal drip. Your health care professional diagnoses sinusitis based on your symptoms and an examination of your nose and face. You may also need imaging tests. Treatments include antibiotics, decongestants, and pain relievers. Using heat pads on the inflamed area, saline nasal sprays, and vaporizers can also help.
See your doctor if:
- your symptoms are severe or getting worse
- your symptoms haven’t started to improve after around 7-10 days
- you have frequent episodes of sinusitis.
Your doctor may prescribe medicines including regular pain relief, a saline nasal spray or a nasal decongestant. In some cases, your doctor may decide to give you inhaled steroids or an antibiotic. If you often get sinusitis, it could be due to an allergy so they may refer you to an ear, nose and throat (ENT) specialist.
Tell your doctor if you develop bleeding from the nose, a stiff neck, swelling, or problems with your vision.
If symptoms worsen or if they recur with clearing between episodes, physicians should reevaluate the patient to confirm the diagnosis of acute bacterial rhinosinusitis, exclude other causes of illness, and detect complications 1. People who are immunocompromised, seriously ill, or continue to deteriorate despite an extended course of antibiotics should be referred to a subspecialist 2. Complications of acute bacterial rhinosinusitis are estimated at approximately one in 1,000 episodes 1. Although rare in the United States, sinonasal cancer should also be included in the differential diagnosis 3. The box below summarizes indications for subspecialist referral in patients with acute bacterial rhinosinusitis 4.
- Anatomic defects causing obstruction
- Complications, such as orbital cellulitis, subperiosteal abscess, intraorbital abscess, altered mental status, meningitis, cavernous sinus thrombosis, intracranial abscess, Pott puffy tumor (osteomyelitis of frontal bone)
- Evaluation of immunotherapy for allergic rhinitis
- Frequent recurrences (three to four episodes per year)
- Fungal sinusitis, granulomatous disease, or possible neoplasm
- Immunocompromised host
- Nosocomial infection
- Severe infection with persistent fever greater than 102°F (39°C)
- Treatment failure after extended antibiotic courses
- Unusual or resistant bacteria
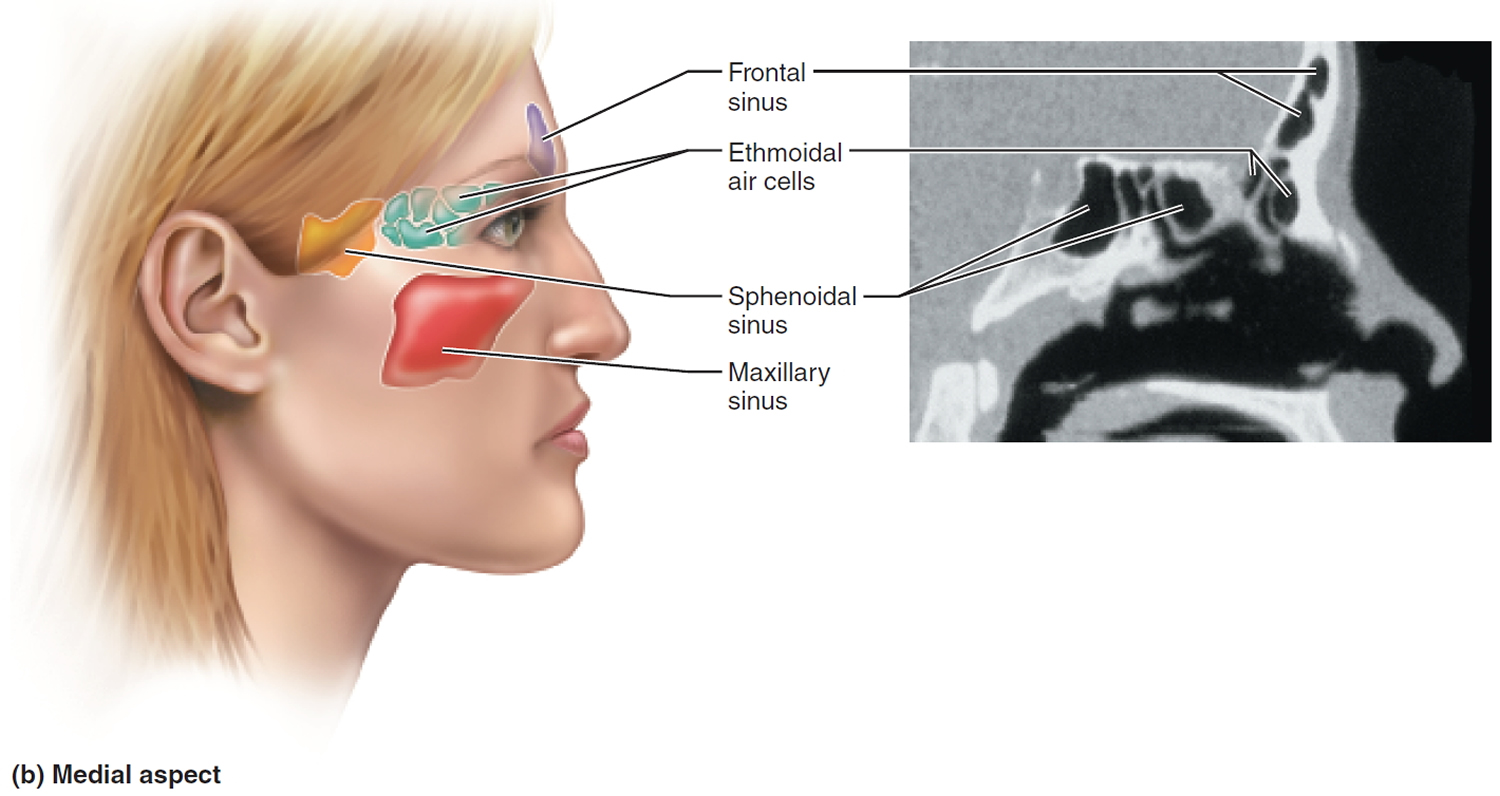
The sinuses
The paranasal sinuses are spaces in the bones of the skull which are mainly full of air. The paranasal sinuses include:
- the sphenoid sinus – in the centre of the head;
- the maxillary sinuses – situated in the cheekbones;
- the frontal sinuses – above the eyes; and
- the ethmoidal sinuses – on either side of the nose.
The lining of the sinuses produces clear fluid – mucus – which cleans them. This fluid passes through narrow drainage passages into the back of the nose and throat, from where it is swallowed. This happens continually, although we are usually unaware of it.
Because the drainage holes from the sinuses are narrow, they block up easily. So any excess mucus production can cause a blockage, and pressure builds up in the sinuses.
The 2 main causes of excess mucus production are:
- Infection; and
- Allergy.
Figure 1. Paranasal sinuses
Sinusitis symptoms
The main symptoms of sinusitis include:
- feeling of pressure inside the face;
- facial pain, particularly when leaning forward;
- either blocked nose or runny nose and/or postnasal drip (mucus running down the back of the throat causing irritation); and
- reduced sense of smell or taste.
Additional symptoms may include:
- a green or yellow discharge from your nose;
- facial tenderness;
- fever 38° C (100.4° F) or more;
- tiredness;
- bad breath (halitosis);
- headache;
- swelling around the eyes;
- swelling of the face;
- pain in the upper jaw and/or teeth; A sinus infection (sinusitis) or inflammation can cause a toothache — specifically in the upper rear teeth, which are close to the sinuses.
- cough;
- nausea;
- generally feeling unwell.
Symptoms of chronic sinusitis are similar to those of acute sinusitis, but last longer. Fever is generally not a feature of chronic sinusitis.
A sensation of partial deafness or blockage in the ear may also occur. This is because the Eustachian tube, which connects the middle ear to the back of the nose, blocks up in just the same way as the nearby sinus openings.
Sinusitis causes
Sinusitis is caused by too much mucus, or a swelling of the lining of the sinuses and nose, which can block the narrow channels. This can occur during a cold, or may be due to allergy (for example, hayfever) or irritation of the linings of the sinuses (for example, from chlorine in a swimming pool). Bacteria (germs) then grow inside the sinuses, causing pain, headache and sometimes fever. Mucus from infected sinuses can be yellow or green. Some people get sinusitis with most colds, while others get it rarely.
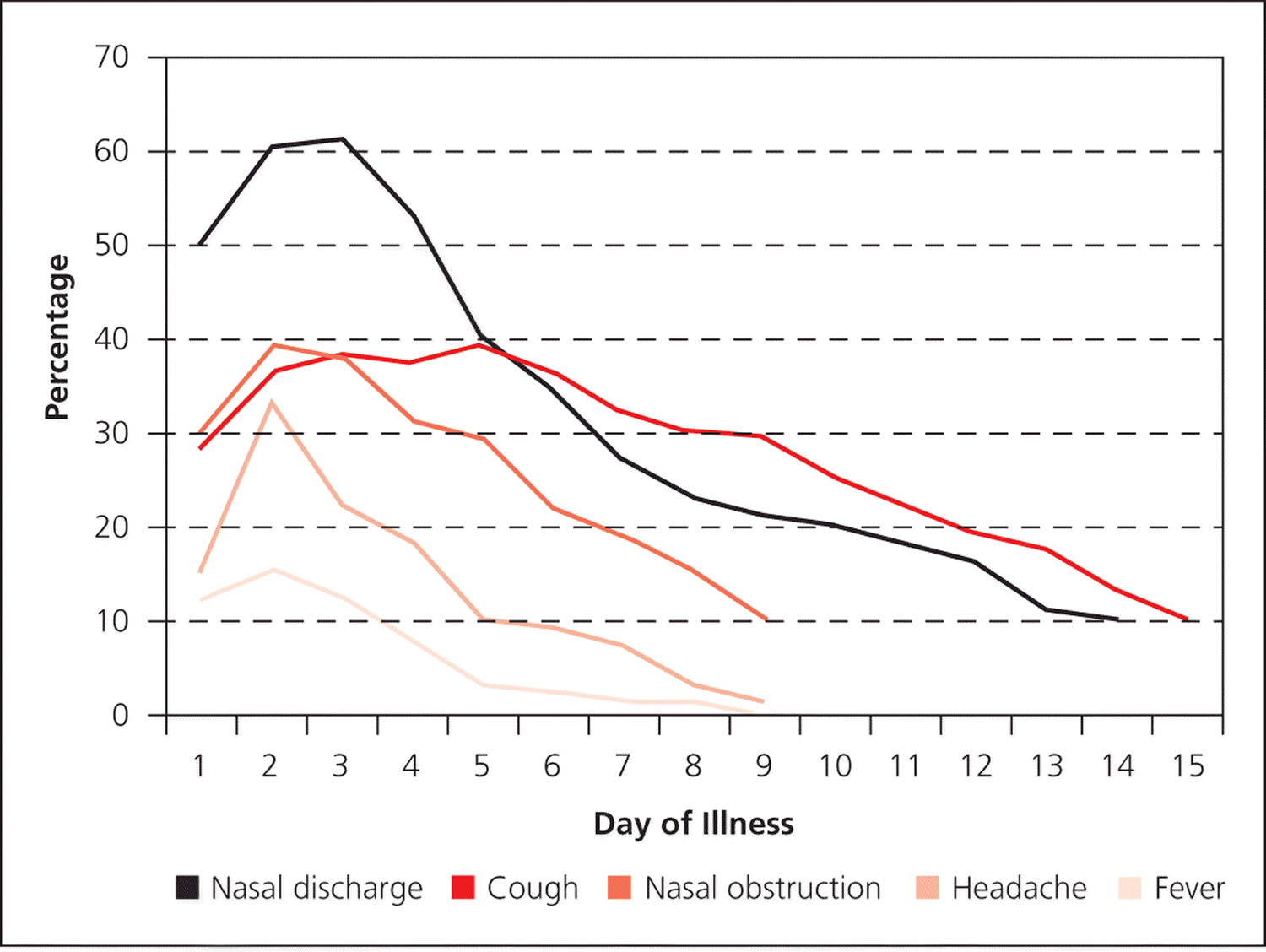
In the first three to four days of illness, viral rhinosinusitis cannot be differentiated from early acute bacterial rhinosinusitis 5. Figure 2 summarizes the natural course of signs and symptoms associated with rhinovirus infections 5. A pattern of initial improvement followed by a worsening of symptoms—called double sickening—between days 5 and 10 of the illness is consistent with acute bacterial rhinosinusitis 5.
Physicians should not rely solely on colored nasal drainage as an indication for antibiotic therapy because it does not predict the likelihood of sinus infection (positive likelihood ratio = 1.5; negative likelihood ratio = 0.5) 6. Local sinus pain with unilateral predominance in addition to purulent rhinorrhea had an overall reliability of 85% for diagnosing sinusitis according to one study 7. Another study showed that four signs and symptoms with a high likelihood ratio for acute bacterial sinusitis are double sickening, purulent rhinorrhea, an erythrocyte sedimentation rate greater than 10 mm per hour, and purulent secretion in the nasal cavity. A combination of at least three of these four signs and symptoms has a specificity of 81% and sensitivity of 66% for acute bacterial rhinosinusitis 8. Diagnosis of acute bacterial rhinosinusits is indicated when signs or symptoms of acute rhinosinusitis persist without evidence of improvement for at least 10 days beyond the onset of upper respiratory symptoms 5. After 10 days of upper respiratory symptoms, the probability of bacterial rhinosinusitis is 60% 9.
Figure 2. Natural course of symptom prevalence for rhinovirus infections
[Source 5]Causes of infective sinusitis include:
- viral infections such as the common cold;
- bacterial infections (usually a complication of viral sinusitis);
- fungal infections (usually seen in people with an underlying problem with their sinuses or immune system).
Risk factors for sinusitis
Factors that can increase your risk of developing sinusitis include:
- obstruction in the nose or sinuses (due to problems such as nasal polyps – small benign growths in the nose, or a deviated septum after a fractured nose);
- allergy (hay fever, or allergic rhinitis);
- a medical condition such as cystic fibrosis;
- problems with your immune system.
Sinusitis diagnosis
Your doctor will usually be able to diagnose sinusitis based on your symptoms and physical examination. In some cases, tests may be necessary if the sinusitis is persistent.
During the past decade, expert panels have created evidence-based guidelines for the diagnosis (Table 1) and management of acute rhinosinusitis in adults 5.
Table 1. Summary of Guidelines for the Diagnosis of Acute Rhinosinusitis in Adults
| Guideline | Signs and symptoms | Diagnostic criteria | ||
|---|---|---|---|---|
Clinical Practice Guideline (update): Adult Sinusitis 5 | Purulent nasal discharge with nasal obstruction, facial pain, or facial pressure | Presumed acute viral rhinosinusitis: | ||
Symptoms last less than seven days and do not worsen | ||||
Presumed acute bacterial rhinosinusitis: | ||||
Severe symptoms in first three to four days of illness; symptoms persist seven days or longer after initial presentation; symptoms worsen within seven days of initial presentation | ||||
European Position Paper on Rhinosinusitis and Nasal Polyps 2012 10 | Inflammation of the nasal cavity and paranasal sinus, characterized by either nasal congestion or obstruction or nasal discharge with or without facial pain or pressure with or without decreased sense of smell | Presumed acute viral rhinosinusitis: | ||
Symptoms last less than 10 days and do not worsen | ||||
Presumed acute bacterial rhinosinusitis: | ||||
Symptoms persist more than 10 days after start of URI; symptoms worsen after five days | ||||
IDSA Clinical Practice Guideline 2011 2 | Two major symptoms or one major and more than two minor symptoms | Presumed acute viral rhinosinusitis: | ||
Major symptoms: Purulent nasal discharge, nasal congestion or obstruction, facial congestion or fullness, facial pain or pressure, decreased sense of smell, fever | For mild symptoms, watchful waiting for first three days of illness | |||
Minor symptoms: Headache; ear pain, pressure, fullness; halitosis; dental pain; cough; fever; fatigue | Presumed acute bacterial rhinosinusitis: | |||
Severe symptoms in first three to four days of illness; symptoms persist more than 10 days after start of URI; symptoms worsen after three to four days | ||||
Joint Task Force on Practice Parameters 2005 11 | Nasal congestion, purulent rhinorrhea, facial-dental pain, postnasal drainage, headache, cough, tenderness over sinuses, dark circles under eyes | Presumed acute viral rhinosinusitis: | ||
Symptoms last less than 10 days and do not worsen | ||||
Presumed acute bacterial rhinosinusitis: | ||||
Symptoms persist more than 10 to 14 days | ||||
Severe symptoms: fever with purulent nasal discharge, facial pain or tenderness, periorbital swelling | ||||
Rhinosinusitis Initiative 2004 12 | Two or more major symptoms or one major and two or more minor symptoms (see IDSA symptom lists above) | Presumed acute bacterial rhinosinusitis: | ||
Severe symptoms in first three to four days of illness; symptoms persist more than 10 days after start of URI; symptoms worsen within 10 days of initial improvement | ||||
IDSA = Infectious Diseases Society of America; URI = upper respiratory infection.
Tests that can help diagnose sinusitis and determine the cause include:
- Imaging tests, such as CT scan or MRI (magnetic resonance imaging) of the paranasal sinuses, are sometimes used when symptoms are severe or chronic sinusitis is not improving.
- Nasal endoscopy, where a narrow lighted tube with a camera is used to look at the nasal cavity and sinuses. It can show excess mucus, inflammation and swelling of the inner lining of the nose and sinuses, and problems such as polyps.
- Microbiology tests: a nasal swab is sent for testing to try to confirm if there is an infection and what type. This type of test is only performed when sinusitis is not responding to treatment.
- Allergy tests, to determine whether allergies are contributing to your sinusitis.
LABORATORY TESTS
Erythrocyte sedimentation rate and C-reactive protein (CRP) are somewhat useful tests for diagnosing acute bacterial maxillary sinusitis. In a study of 173 patients using antral puncture as the reference standard, 30 of 38 (79%) of those with a CRP level greater than 49 mg per L (466.7 nmol per L) had acute maxillary sinusitis compared with 37 of 61 (61%) of those with a CRP level of 11 to 49 mg per L (104.8 to 466.7 nmol per L) and only 25 of 74 (34%) of those with a CRP level less than 11 mg/L 14.
IMAGING
Radiography is not recommended in the evaluation of acute uncomplicated rhinosinusitis 5. It is somewhat helpful in ruling out the presence of fluid when the results are negative. Positive results are not helpful because they cannot differentiate between viral and bacterial sinusitis.
For patients with recurrent acute or chronic rhinosinusitis, computed tomography (CT) of the sinuses without contrast media is the imaging method of choice 5. CT of the sinuses should be performed only after completing maximal medical therapy. CT is primarily used to define the anatomy of the sinuses before surgery, as well as to assess the extent, pattern, and a probable mechanical cause of the recurrent or chronic rhinosinusitis. A thickened mucosa of 5 mm or greater on CT is a significant sign of sinus infection 8. Antral puncture data from patients with CT evidence of fluid in the maxillary sinus were associated with demonstrated pus or mucopus by sinus lavage in 90% of patients reviewed 8.
Sinusitis treatment
Treatments for sinusitis include:
- Self-care measures such as rest, drinking plenty of fluids, steam inhalations, and applying a warm compress to your forehead.
- Pain relievers such as paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs).
- Saline nasal sprays and nasal irrigation are useful in relieving nasal congestion.
- Corticosteroid nasal sprays can also help improve symptoms. Oral corticosteroid tablets are also occasionally used to treat acute and chronic sinusitis.
- Decongestants: decongestant nasal sprays can provide relief but should not be used for longer than 3 days or in young children. Decongestant tablets can also be used to ease symptoms, but should not be used for more than a few days.
- Hay fever treatment, including antihistamine nasal spray or tablets, is recommended when allergic rhinitis is contributing to sinusitis. Immunotherapy for ongoing hay fever is another treatment option.
Watchful waiting
Watchful waiting is appropriate in place of antibiotics for seven to 10 days after upper respiratory symptoms appear when there is assurance of follow-up 5. Antibiotic therapy should be considered if the patient’s condition does not improve by seven to 10 days after initial presentation or if symptoms worsen at any time 5. Symptomatic therapies should be offered to patients who are under observation. Physicians may also provide these patients with a safety net antibiotic prescription (also called a delayed prescription), with instructions describing when to fill the prescription 5. Watchful waiting is supported by four meta-analyses that were published after the 2007 American Academy of Otolaryngology–Head and Neck Surgery clinical practice guideline was released 15, 16, 17, 18. These studies did not provide evidence confirming or disproving the American Academy of Otolaryngology–Head and Neck Surgery position that patients with more severe acute bacterial rhinosinusitis should initially be treated with antibiotics.
A Cochrane review showed that the symptoms of bacterial rhinosinusitis had resolved in 47% of all patients after seven days with or without antibiotic therapy (Lemiengre MB, van Driel ML, Merenstein D, Young J, De Sutter AI. Antibiotics for clinically diagnosed acute rhinosinusitis in adults. Cochrane Database Syst Rev. 2012;(10):CD006089.()). In addition, approximately 70% of patients improved within two weeks without antibiotics 17. Antibiotic therapy did increase cure rates for patients between seven and 15 days compared with placebo; however, the clinical benefit was small, with only 5% of patients having a faster cure 17. Moreover, analysis of individual patient data found that it was not possible to identify which patients with rhinosinusitis would benefit from antibiotics based on the presence of common clinical signs and symptoms 15. The number needed to treat was estimated to be 11 to 15.1,22,24 Adverse effects occurred more often with antibiotics than with placebo (number needed to harm = 8) 16. The risk of harm outweighs the potential benefit of antibiotic therapy. As a result of this research, the 2015 American Academy of Otolaryngology–Head and Neck Surgery guideline recommends offering watchful waiting to patients regardless of illness severity 5.
Sinusitis Antibiotics
Antibiotics are sometimes needed to treat sinusitis when a bacterial infection is suspected. Acute bacterial sinusitis is suspected when:
- symptoms are getting worse after initial improvement;
- you have a high fever, symptoms are severe and have lasted for more than 3 days; or
- symptoms of rhinosinusitis have lasted for longer than 7 days.
Chronic sinusitis may also sometimes need antibiotic treatment.
Antibiotics for the treatment of acute bacterial rhinosinusitis are outlined in Table 2. Most guidelines recommend amoxicillin with or without clavulanate as a first-line antibiotic for adults because of its safety, effectiveness, low cost, and narrow microbiologic spectrum 5. Amoxicillin/clavulanate (Augmentin) should be used in patients who are at high risk of bacterial resistance or who have comorbid conditions, as well as in those with moderate to severe infection 5. No significant differences in acute bacterial rhinosinusitis cure rates are noted between different antibiotic classes 5.
Table 2. Oral Antibiotics for the Treatment of Acute Bacterial Sinusitis
| Antibiotic | Clinical effectiveness (%) | Dosage | |||
| First line for most patients | |||||
| Amoxicillin (regular dose) | 83 to 88 | 500 mg every eight hours for five to 10 days | |||
| or | |||||
| 875 mg every 12 hours for five to 10 days | |||||
| First line for coverage of beta lactamase–producing Haemophilus influenzae and Moraxella (Branhamella) catarrhalis | |||||
| Amoxicillin/clavulanate (Augmentin; regular dose) | 90 to 92 | 500 mg/125 mg every eight hours for five to 10 days | |||
| or | |||||
| 875 mg/125 mg every 12 hours for five to10 days | |||||
| For possible Streptococcus pneumoniae resistance (e.g., child in household who attends day care) | |||||
| Amoxicillin (high dose) | 83 to 88 | 1 g every eight hours for five to 10 days | |||
| or | |||||
| 1 g four times per day for five to 10 days | |||||
| For moderate to severe disease, high risk of resistance, recent antibiotic use, or treatment failure | |||||
| Amoxicillin/clavulanate, extended release (Augmentin XR) | 90 to 92 | 2,000 mg/125 mg twice per day for 10 days | |||
| For patients with penicillin allergy or as second-line antibiotic | |||||
| Doxycycline | 77 to 81 | 100 mg twice per day or 200 mg once per day for five to 10 days | |||
| Levofloxacin (Levaquin)‡ | 90 to 92 | 500 mg per day for 10 to 14 days | |||
| or | |||||
| 750 mg every day for five days | |||||
| Moxifloxacin (Avelox)‡ | 90 to 92 | 400 mg per day for 10 days | |||
| Non–type I penicillin allergy or second-line antibiotic | |||||
| Clindamycin | 77 to 81 | 300 mg three times per day for five to10 days | |||
| plus | |||||
| Cefixime (Suprax) | 83 to 88 | 400 mg per day for 10 days | |||
| or | |||||
| Cefpodoxime | 83 to 88 | 200 mg twice per day for 10 days | |||
†—May be available at discounted prices at one or more national retail chains.
‡—Fluoroquinolones should be reserved for those who do not have alternative treatment options.
Respiratory fluoroquinolones are not recommended as first-line antibiotics because they conferred no benefit over beta-lactam antibiotics and are associated with a variety of adverse effects 5. According to a recent U.S. Food and Drug Administration safety alert, fluoroquinolones should be reserved for patients who do not have other treatment options 20. Macrolides, including azithromycin (Zithromax), trimethoprim/sulfamethoxazole, and second- or third-generation cephalosporins, are no longer recommended as initial therapy for acute bacterial rhinosinusitis because of high rates of resistance in S. pneumoniae and H. influenzae 5.
The recommended duration of therapy for uncomplicated acute bacterial rhinosinusitis is five to 10 days for most adults 5. This recommendation is based primarily on findings from a meta-analysis of 12 randomized controlled trials 21. A shorter treatment course (median of five days) may be just as effective as a longer course of treatment (median of 10 days) and is associated with fewer adverse effects 21. Regardless, clinicians should assess disease and symptom response before stopping antibiotic therapy prematurely, especially in older adults and in patients with underlying disease.
Treatment failure occurs when a patient’s symptoms do not improve by seven days after diagnosis or when they worsen at any time, with or without antibiotic therapy 5. If treatment failure occurs following initial antibiotic therapy, an alternative antibiotic with a broader spectrum is required. High-dose amoxicillin/clavulanate, a respiratory fluoroquinolone, or the combination of clindamycin plus a third-generation oral cephalosporin may be considered 5.
Adjunctive symptomatic treatment
Current guidelines consider analgesics, intranasal corticosteroids, and saline nasal irrigation to be options for the management of rhinosinusitis symptoms 22. They are recommended for use within the first 10 days but may be continued if antibiotics are initiated. Selection of interventions should be based on shared decision making. Decongestants, antihistamines, and guaifenesin are not recommended for patients with acute bacterial rhinosinusitis because of their unproven effectiveness, potential adverse effects, and cost 2. Table 2 summarizes adjunctive therapies for acute rhinosinusitis 23, 24, 25.
Table 3. Adjunctive Therapies for Acute Rhinosinusitis
| Treatment | Evidence summary | Comment |
|---|---|---|
Intranasal corticosteroids | Two systematic reviews of randomized controlled trials showed minimal benefit and symptom relief occurred late (at 15 to 21 days) 24 | Some agents available over the counter |
Saline nasal irrigation | One small randomized controlled trial found hypertonic saline decreased nasal symptoms 26 | Available in a low-pressure method using a spray or squeeze bottle or a gravity-flow method using a vessel with a nasal spout |
Another study found no significant difference between groups receiving no treatment vs. those treated with saline nasal solutions, topical decongestants, and intranasal corticosteroids 27 | ||
Oral decongestants | No clinical trial evidence for patients with acute sinusitis | Significant adverse effects; phenylephrine is similar in effectiveness to placebo for nasal congestion due to seasonal allergic rhinitis 23 |
Topical decongestants | One comparative trial found no significant difference in improvement among groups receiving no treatment vs. those treated with saline nasal solutions, topical decongestants, and intranasal corticosteroids 27 | May cause rebound congestion when used for prolonged periods |
Intranasal Corticosteroids
Intranasal corticosteroids may be helpful in reducing mucosal swelling of inflamed tissue and facilitating sinus drainage because of an anti-inflammatory effect 5. However, data on intranasal corticosteroids as monotherapy for symptomatic relief in patients with acute sinusitis are limited 17. Several studies suggest that they provide additional benefit in symptom improvement when used with antibiotics in patients with acute sinusitis 28. A meta-analysis of six trials 25 concluded that intranasal corticosteroids offered a modest therapeutic benefit in patients with acute sinusitis (number needed to treat = 13).
Similarly, a 2013 Cochrane review found that patients receiving intranasal corticosteroids were more likely to experience symptom improvement after 15 to 21 days compared with those receiving placebo (73% vs. 66.4%; number needed to treat = 15) 24. Higher doses of intranasal corticosteroids had a greater effect on symptom relief than lower doses. Even though their benefits are only marginal,3 intranasal corticosteroids are often used as an adjunct to antibiotic therapy in the symptomatic treatment of acute bacterial sinusitis. They are likely most beneficial in patients with concurrent allergic rhinitis 2.
Saline Nasal Irrigation
Intranasal irrigations with either physiologic or hypertonic saline have been shown to improve mucociliary clearance and may be beneficial for the treatment of acute rhinosinusitis 27. One randomized controlled trial of 76 patients with frequent sinusitis found that daily hypertonic saline nasal irrigation decreases nasal symptoms and medication use 29. A Cochrane review concluded that saline nasal irrigation may relieve symptoms of upper respiratory infection 30. Despite limited evidence regarding effectiveness, saline nasal irrigation can be a safe and inexpensive adjunctive therapy for symptom relief in acute rhinosinusitis. It is important to inform patients to prepare irrigations using distilled, boiled, or filtered water because there have been reports of amebic encephalitis due to contaminated tap water rinses 31.
Decongestants
Oral decongestants have been shown to be modestly effective for short-term relief of symptoms in adults with the common cold by reducing nasal airway resistance 32. However, the effect of decongestants in the nasal cavity does not extend to the paranasal sinuses 33. There are currently no randomized controlled trials evaluating the effectiveness of decongestants in patients with sinusitis. Oral decongestants should be used with caution in patients with hypertension or cardiovascular disease. Topical decongestants should not be used for longer than 72 hours, owing to the potential for rebound congestion (rhinitis medicamentosa).
Antihistamines
Antihistamines are often used to relieve symptoms of excessive secretions and sneezing. However, there are no studies to support the effectiveness of antihistamine in acute rhinosinusitis 5. Antihistamines may also worsen congestion by overdrying the nasal mucosa. Current guidelines do not recommend antihistamines as an adjunctive therapy for acute bacterial rhinosinusitis, except in patients with a history of allergy 2.
Sinusitis Surgery
Sometimes surgery is necessary to drain a chronically blocked sinus, or to enlarge the drainage passage. This is most commonly done using an endoscope (a thin, flexible tube with an attached light), which is passed through the nose.
How to treat sinusitis at home yourself
If you are looking after yourself, the tips below may help relieve the symptoms:
- Decongestant medicines – available as tablets, nasal sprays or drops – may be helpful, but do not take them for longer than instructed.
- Always follow the manufacturer’s instructions when taking or giving someone else any medicines.
- It is important to stay well hydrated so drink plenty of water. If you have an existing medical condition check with your doctor about how much water is right for you.
- Gently blow your nose one nostril at a time.
- Place a warm or cool cloth, whichever helps, over the aching area.
- Use a saline nasal spray. Saline washes or sprays can remove thick secretions and allow the sinuses to drain.
- Use a neti pot. A neti pot is a container designed to rinse debris or mucus from your nasal cavity. Neti pots are often available in pharmacies and health food stores, as well as online. Talk to your doctor to see if nasal rinsing is right for you.
- Rest and avoid heavy activity until symptoms go away.
- Keep the room at a comfortable temperature.
- Smoking or breathing in other people’s smoke can make symptoms worse. Try to avoid being around people who are smoking. If you are a smoker, try to cut down or quit. For advice on quitting smoking, visit our quit smoking article.
- Find advice on suitable medicines for pain.
- Find out more about self-care tips if you have a high temperature (fever).
Most people with acute sinusitis get better without antibiotics. However, if your symptoms are severe or last longer than a few days, talk to your doctor.
There are many over-the-counter saline (salt water) solutions available, but you can make your own saline solution at home:
- 1 quart (4 cups) boiled or distilled water
- 1 teaspoon baking soda
- 1 teaspoon non-iodized salt
If you make your own rinse, use water that’s contaminant-free — distilled, sterile, previously boiled and cooled, or filtered using a filter with an absolute pore size of 1 micron or smaller — to make up the irrigation solution. Also be sure to rinse the irrigation device after each use with contaminant-free water, and let air-dry.
Over-the-counter medicines for pain
An over-the-counter analgesic, such as acetaminophen or a nonsteroidal anti-inflammatory drug, is often sufficient to relieve pain or fever in acute rhinosinusitis. Narcotics are not recommended because of potential adverse effects 5.
There are a range of pain relief medicines that can be bought without prescription as over-the-counter pain relievers, including paracetamol (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and aspirin. Always use over-the-counter products as directed.
Use caution when giving aspirin to children or teenagers. Children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. This is because aspirin has been linked to Reye’s syndrome, a rare but potentially life-threatening condition, in such children.
Just because they are available over-the-counter does not mean that they are completely free of side effects and you should always check with your pharmacist or doctor if you are unsure whether these drugs are safe for you or not.
If you have allergies, chronic illness or are on any other medicines always check first before taking these medicines. The pharmacist can help in giving medication advice in these cases. Always if your pain persists or you are concerned see your doctor.
Paracetamol (acetaminophen)
Paracetamol (acetaminophen) is effective for mild to moderate pain, if used correctly. When you take paracetamol, check that none of your other medicines contain the same active ingredient, as it can cause serious liver damage if taken in larger doses than recommended. Arthritis medicines and over-the-counter cold and flu medicines can contain paracetamol.
Paracetamol (acetaminophen) can be given to children from the age of one month for pain and symptoms of fever. Paracetamol for children can only be bought at pharmacies. Make sure you’ve got the right strength for your child’s age and weight as overdosing can be dangerous. Read and follow the directions on the label carefully. If you are not sure, check with your doctor or pharmacist.
Ibuprofen
Non-steroidal anti-inflammatory (NSAIDs) drugs, such as ibuprofen, are effective against mild to moderate pain. Use these at the lowest dose that improves your symptoms and only use them for a short time. These medicines may not be suitable for people with stomach troubles, heart problems, kidney impairment, high blood pressure or asthma. See your doctor if you need to take these drugs for more than one week. The use of oral NSAIDs in older people is not recommended.
Ibuprofen can be given for pain and symptoms of fever in children aged three months and over who weigh more than 5kg. Ibuprofen for children can only be bought at pharmacies. Make sure you’ve got the right strength for your child’s age and weight as overdosing can be dangerous. Read and follow the directions on the label carefully. If you are not sure, check with your doctor or pharmacist. Avoid ibuprofen if your child has asthma, unless advised by your doctor.
If you have a high temperature there are a number of things you can do to help manage the condition:
- it’s important to stay well hydrated so drink plenty of clear non-alcoholic fluids
- ice blocks or iced drinks may be soothing
- wear lightweight clothing and avoid using blankets or quilts in bed as this may make you too hot and increase your temperature
- keep the room at a comfortable temperature
- rest and avoid heavy activity until your symptoms go away
- Rinse your nasal passages. Use a specially designed squeeze bottle (Sinus Rinse, others) or neti pot. This home remedy, called nasal lavage, can help clear your sinuses. If you make your own rinse, use water that’s contaminant-free — distilled, sterile, previously boiled and cooled, or filtered using a filter with an absolute pore size of 1 micron or smaller — to make up the irrigation solution. Also be sure to rinse the irrigation device after each use with contaminant-free water and leave open to air-dry.
- Moisten your sinus cavities. Drape a towel over your head as you breathe in the vapor from a bowl of hot water. Keep the vapor directed toward your face. Or take a hot shower, breathing in the warm, moist air. This will help ease pain and help mucus drain.
- Apply warm compresses to your face. Place warm, damp towels around your nose, cheeks and eyes to ease facial pain.
- Sleep with your head elevated. This will help your sinuses drain, reducing congestion.
- Smoking or breathing in other people’s smoke can make symptoms worse. Try to avoid being around people who are smoking. If you are a smoker, try to cut down or quit. For advice on quitting smoking, visit our quit smoking article.
- avoid cool baths or sponging – this can actually make you or your child feel more uncomfortable
- see your doctor if your fever persists or you are concerned.
Medicines you can take if you have a high temperature
There is no need to take medicines for fever unless you are experiencing discomfort.
If you are experiencing discomfort consider:
- paracetamol (acetaminophen)
- ibuprofen.
Before taking any medicine, you should check that it’s safe to take them:
- with any medical conditions that you may have
- with any other medicines that you are taking
- if you are pregnant or breastfeeding.
You can do this by reading the information leaflet inside the packet or asking a pharmacist.
- Hwang PH. A 51-year-old woman with acute onset of facial pressure, rhinorrhea, and tooth pain: review of acute rhinosinusitis. JAMA. 2009;301(17):1798–1807.[↩][↩]
- Chow AW, Benninger MS, Brook I, et al.; Infectious Diseases Society of America. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72–e112.[↩][↩][↩][↩][↩]
- Turner JH, Reh DD. Incidence and survival in patients with sinonasal cancer: a historical analysis of population-based data. Head Neck. 2012;34(6):877–885.[↩]
- Fokkens WJ, Lund VJ, Mullol J, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl. 2012;(23):1–298[↩]
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 suppl):S1–S39.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Williams JW Jr, Simel DL, Roberts L, Samsa GP. Clinical evaluation for sinusitis. Making the diagnosis by history and physical examination. Ann Intern Med. 1992;117(9):705–710.[↩]
- Berg O, Carenfelt C. Analysis of symptoms and clinical signs in the maxillary sinus empyema. Acta Otolaryngol. 1988;105(3–4):343–349.[↩]
- Lindbaek M, Hjortdahl P, Johnsen UL. Use of symptoms, signs, and blood tests to diagnose acute sinus infections in primary care: comparison with computed tomography. Fam Med. 1996;28(3):183–188.[↩][↩][↩]
- van den Broek MF, Gudden C, Kluijfhout WP, et al. No evidence for distinguishing bacterial from viral acute rhinosinusitis using symptom duration and purulent rhinorrhea: a systematic review of the evidence base. Otolaryngol Head Neck Surg. 2014;150(4):533–537.[↩]
- Fokkens WJ, Lund VJ, Mullol J, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl. 2012;(23):1–298.[↩]
- Slavin RG, Spector SL, Bernstein IL, et al.; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. The diagnosis and management of sinusitis: a practice parameter update. J Allergy Clin Immunol. 2005;116(6):S13–S47.[↩]
- Meltzer EO, Hamilos DL, Hadley JA, et al.; American Academy of Allergy, Asthma and Immunology; American Academy of Otolaryngic Allergy; American Academy of Otolaryngology—Head and Neck Surgery; American College of Allergy, Asthma and Immunology; American Rhinologic Society. Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol. 2004;114(6 suppl):155–212.[↩]
- Current Concepts in Adult Acute Rhinosinusitis. Am Fam Physician. 2016 Jul 15;94(2):97-105. https://www.aafp.org/afp/2016/0715/p97.html[↩]
- Hansen JG, Schmidt H, Rosborg J, Lund E. Predicting acute maxillary sinusitis in a general practice population. BMJ. 1995;311(6999):233–236.[↩]
- Young J, De Sutter A, Merenstein D, et al. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet. 2008;371(9616):908–914.[↩][↩]
- Falagas ME, Giannopoulou KP, Vardakas KZ, Dimopoulos G, Karageorgopoulos DE. Comparison of antibiotics with placebo for treatment of acute sinusitis: a meta-analysis of randomised controlled trials. Lancet Infect Dis. 2008;8(9):543–552.[↩][↩]
- Lemiengre MB, van Driel ML, Merenstein D, Young J, De Sutter AI. Antibiotics for clinically diagnosed acute rhinosinusitis in adults. Cochrane Database Syst Rev. 2012;(10):CD006089.[↩][↩][↩][↩]
- Rosenfeld RM, Singer M, Jones S. Systematic review of antimicrobial therapy in patients with acute rhinosinusitis. Otolaryngol Head Neck Surg. 2007;137(3 suppl):S32–S45.[↩]
- Anon JB, Jacobs MR, Poole MD, et al.; Sinus And Allergy Health Partnership. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis [published correction appears in Otolaryngol Head Neck Surg. 2004; 130(6):794–796]. Otolaryngol Head Neck Surg. 2004;130(1 suppl):1–45.[↩]
- U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together. https://www.fda.gov/Drugs/DrugSafety/ucm500143.htm[↩]
- Falagas ME, Karageorgopoulos DE, Grammatikos AP, Matthaiou DK. Effectiveness and safety of short vs. long duration of antibiotic therapy for acute bacterial sinusitis: a meta-analysis of randomized trials. Br J Clin Pharmacol. 2009;67(2):161–171.[↩][↩]
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 suppl):S1–S39.[↩]
- Meltzer EO, Ratner PH, McGraw T. Oral phenylephrine HCl for nasal congestion in seasonal allergic rhinitis: a randomized, open-label, placebo-controlled study. J Allergy Clin Immunol Pract. 2015;3(5):702–708.[↩][↩]
- Zalmanovici Trestioreanu A, Yaphe J. Intranasal steroids for acute sinusitis. Cochrane Database Syst Rev. 2013;(12):CD005149.[↩][↩][↩]
- Hayward G, Heneghan C, Perera R, Thompson M. Intranasal corticosteroids in management of acute sinusitis: a systematic review and meta-analysis. Ann Fam Med. 2012;10(3):241–249.[↩][↩]
- Rabago D, Zgierska A, Mundt M, Barrett B, Bobula J, Maberry R. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: a randomized controlled trial. J Fam Pract. 2002;51(12):1049–1055.[↩]
- Inanli S, Oztürk O, Korkmaz M, Tutkun A, Batman C. The effects of topical agents of fluticasone propionate, oxymetazoline, and 3% and 0.9% sodium chloride solutions on mucociliary clearance in the therapy of acute bacterial rhinosinusitis in vivo. Laryngoscope. 2002;112(2):320–325.[↩][↩][↩]
- Meltzer EO, Orgel HA, Backhaus JW, et al. Intranasal flunisolide spray as an adjunct to oral antibiotic therapy for sinusitis. J Allergy Clin Immunol. 1993;92(6):812–823.[↩]
- Rabago D, Zgierska A, Mundt M, Barrett B, Bobula J, Maberry R. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: a randomized controlled trial. J Fam Pract. 2002;51(12):1049–1055[↩]
- King D, Mitchell B, Williams CP, Spurling GK. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst Rev. 2015;(4):CD006821.[↩]
- Cope JR, Ratard RC, Hill VR, et al. The first association of a primary amebic meningoencephalitis death with culturable Naegleria fowleri in tap water from a US treated public drinking water system. Clin Infect Dis. 2015;60(8):e36–e42.[↩]
- Taverner D, Danz C, Economos D. The effects of oral pseudoephedrine on nasal patency in the common cold: a double-blind single-dose placebo-controlled trial. Clin Otolaryngol Allied Sci. 1999;24(1):47–51.[↩]
- Caenen M, Hamels K, Deron P, Clement P. Comparison of decongestive capacity of xylometazoline and pseudoephedrine with rhinomanometry and MRI. Rhinology. 2005;43(3):205–209.[↩]