Contents
- What is premature ventricular contractions
What is premature ventricular contractions
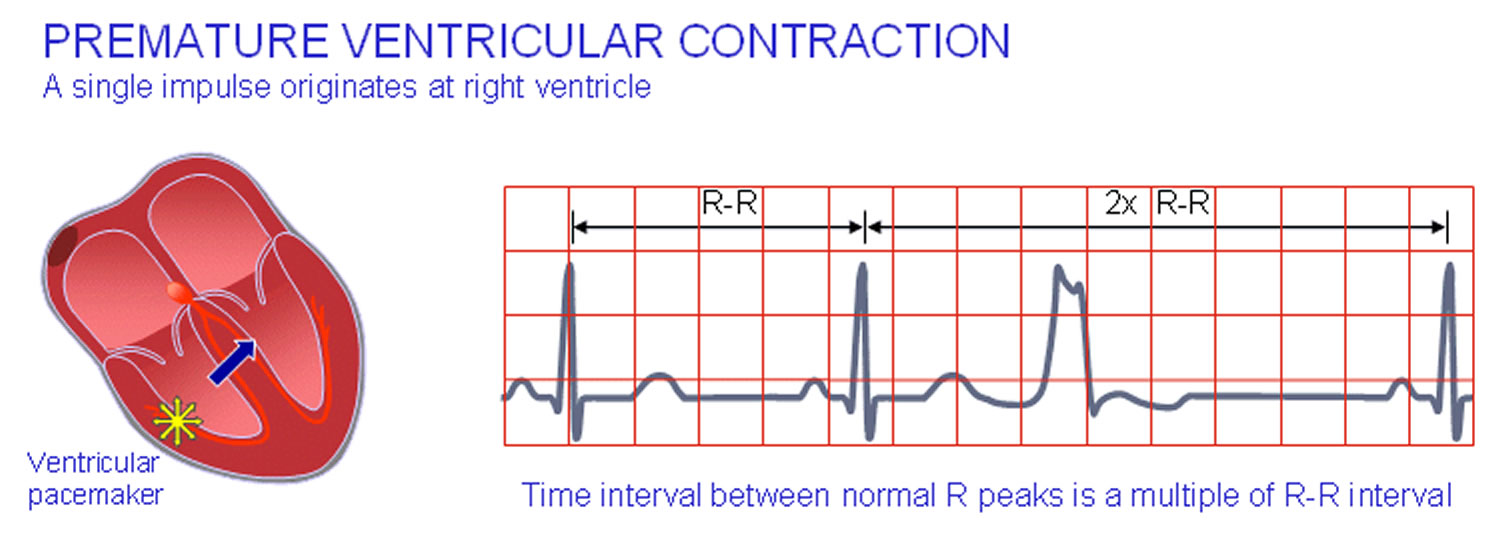
Premature ventricular contractions are extra heartbeats that is initiated by Purkinje fibers, an ectopic cardiac pacemaker located in the ventricles rather than by the sinoatrial node, the normal heartbeat initiator. These extra beats disrupt your regular heart rhythm, sometimes causing you to feel a fluttering or a “skipped beat” or felt as palpitations in your chest. The electrical events of the heart detected by the electrocardiogram (ECG) allow a premature ventricular contraction to be easily distinguished from a normal heart beat (see Figure 1 premature ventricular contractions ECG below). Although a premature ventricular contraction can be a sign of decreased oxygenation to the heart muscle, often premature ventricular contractions are benign and may even be found in otherwise healthy hearts.
In a normal heartbeat, the ventricles contract after the atria have helped to fill them by contracting; in this way the ventricles can pump a maximized amount of blood both to the lungs and to the rest of the body. In a premature ventricular contraction, the ventricles contract first and before the atria have optimally filled the ventricles with blood, which means that circulation is inefficient. However, single beat premature ventricular contraction abnormal heart rhythms do not usually pose a danger and can be asymptomatic in healthy individuals. A premature ventricular contraction is a type of ectopic heartbeat.
Premature ventricular contractions are characterized by premature and bizarrely shaped QRS complexes that are unusually long (typically >120 msec) and appear wide on the electrocardiogram (ECG). These complexes are not preceded by a P wave, and the T wave is usually large and oriented in a direction opposite the major deflection of the QRS. The clinical significance of premature ventricular contractions depends on their frequency, complexity, and hemodynamic response.
Premature ventricular contractions often cause few or no symptoms. But you might feel an odd sensation in your chest, such as:
- Fluttering
- Pounding or jumping
- Skipped beats or missed beats
- Increased awareness of your heartbeat
Premature ventricular contractions are one of the most common arrhythmias and can occur in patients with or without heart disease. Their prevalence varies greatly, with estimates ranging from less than 3% to more than 60% in asymptomatic individuals. Data from large, population-based studies indicate that the prevalence ranges from less than 3% for young white women without heart disease to almost 20% for older African American individuals with hypertension.
Black race is associated with an increased frequency of premature ventricular contractions on routine monitoring 1. In a large population-based study of premature ventricular contraction prevalence, black race alone increased the risk of premature ventricular contractions by 30% in comparison with the risk in white individuals.
Ventricular ectopy is more prevalent in men than in women of the same age. Male sex alone increases the risk of identifying premature ventricular contractions on routine screening, with an odds ratio for male sex of 1.39 as compared with female sex.
Premature ventricular contraction frequency increases with age, reflecting the increased prevalence of hypertension and cardiac disease in aging populations.
Premature ventricular contractions are also called:
- Premature ventricular complexes
- Ventricular premature beats
- Ventricular extrasystoles
If you have occasional premature ventricular contractions, but you’re otherwise healthy, there’s probably no reason for concern, and no need for treatment. If you have frequent premature ventricular contractions or underlying heart disease, you might need treatment.
Figure 1. Premature ventricular contraction ECG
The heart’s electrical system
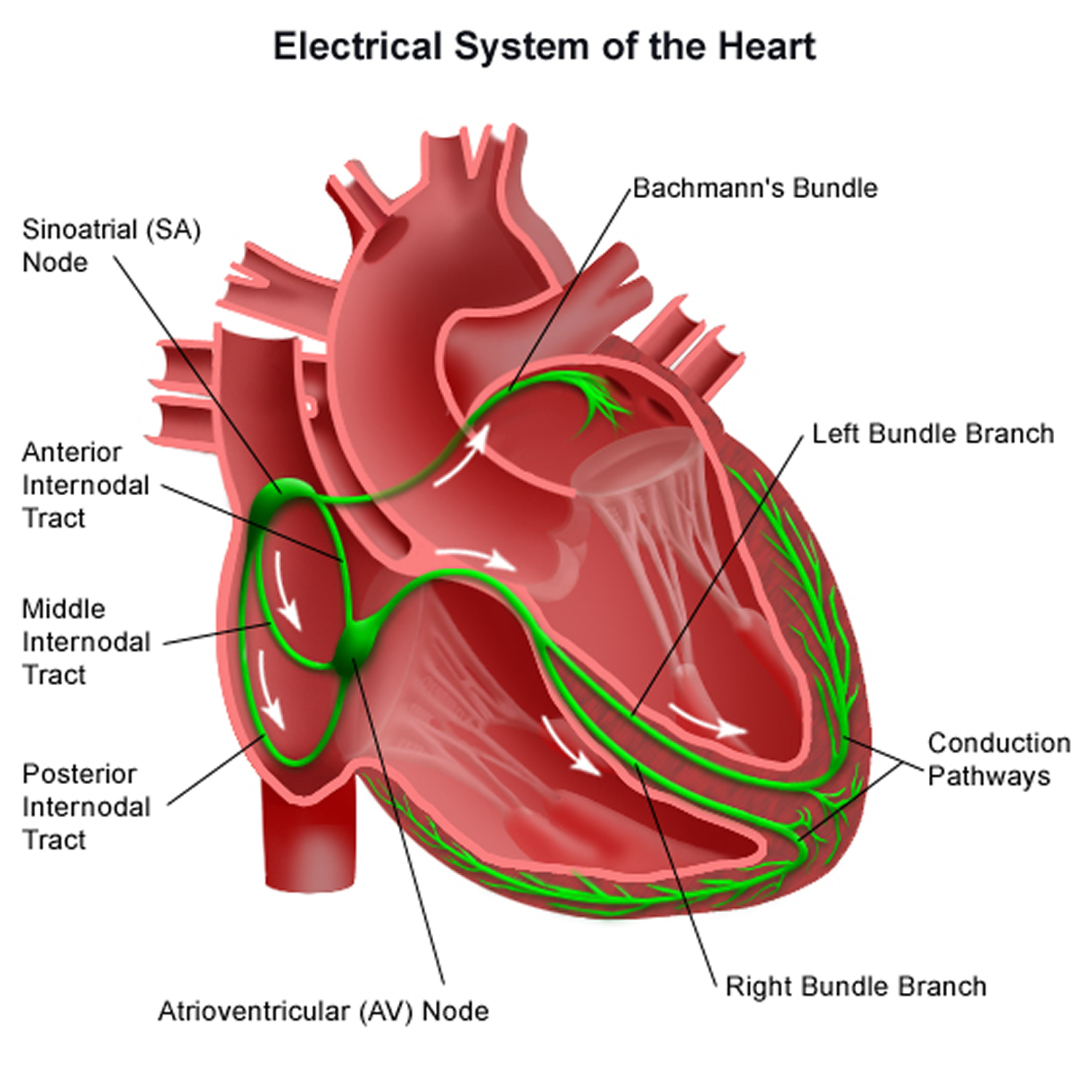
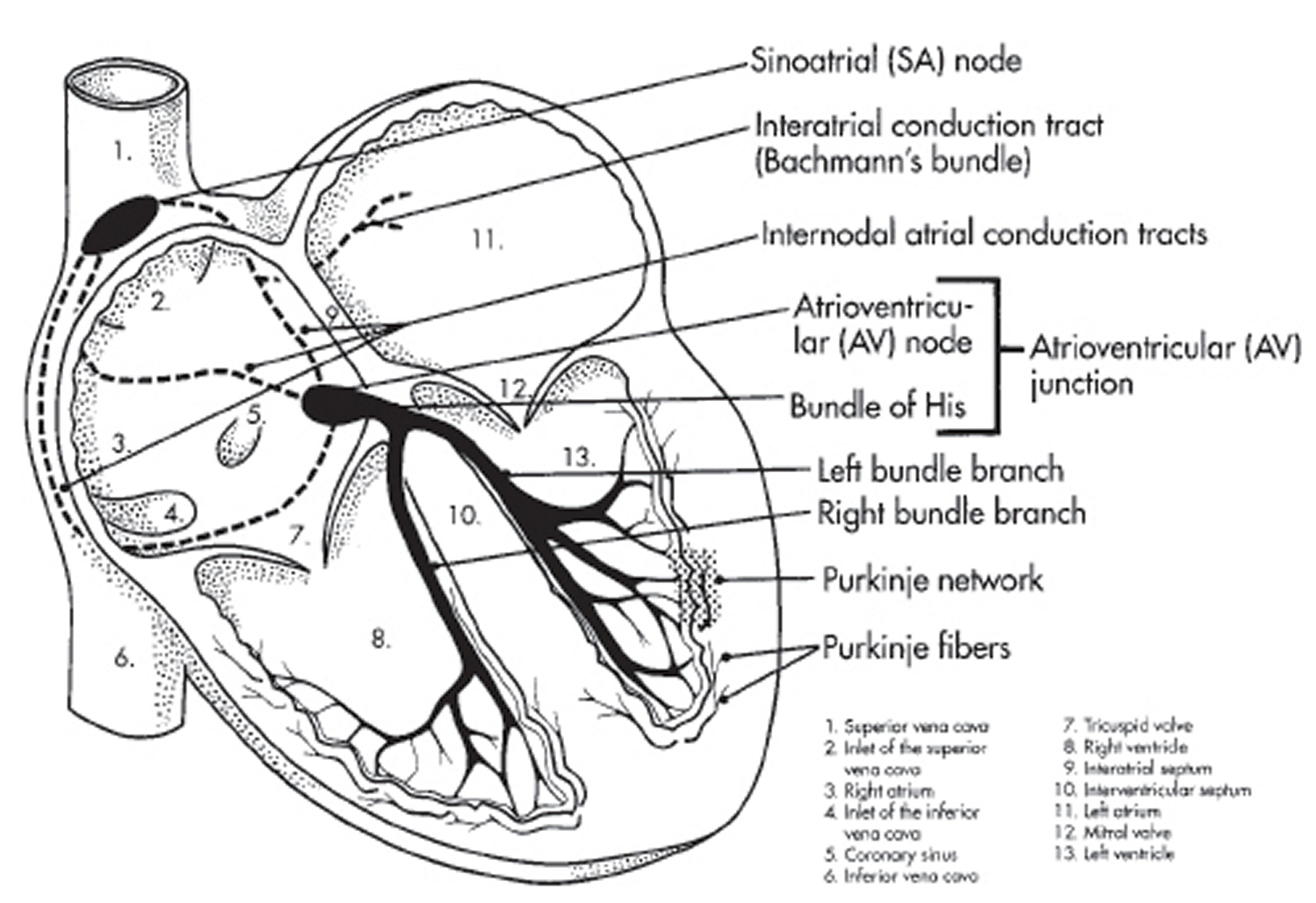
To understand the causes of heart rate or rhythm problems such as ectopic heartbeats, it helps to understand how the heart’s internal electrical system works.
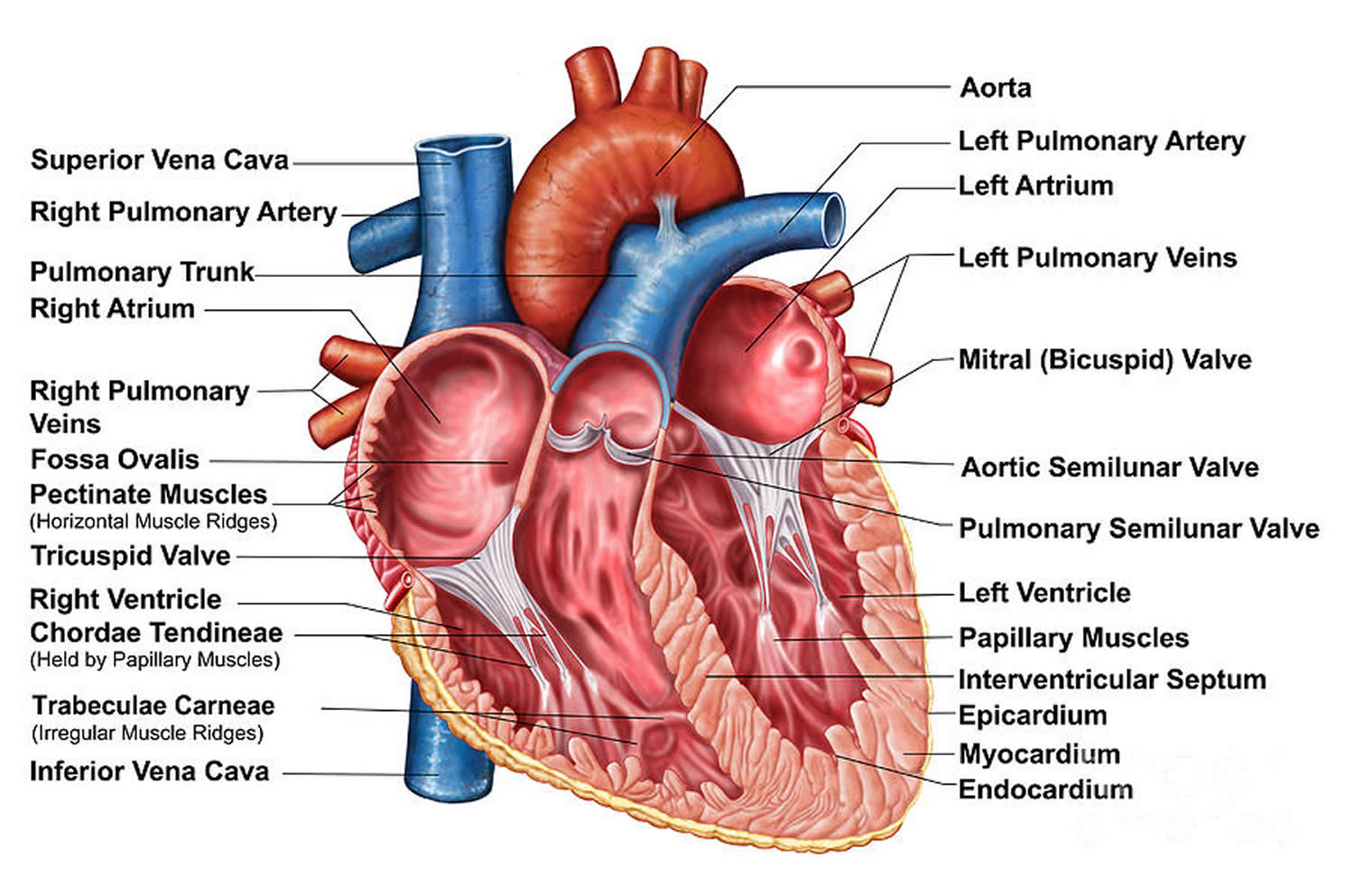
Your heart is made up of four chambers — two upper chambers (atria) and two lower chambers (ventricles). The rhythm of your heart is normally controlled by a natural pacemaker called the sinoatrial (SA) node — or sinus node — an area of specialized cells in the right atrium. The sinoatrial (SA) node produces electrical impulses that normally start each heartbeat. This natural pacemaker produces the electrical impulses that trigger the normal heartbeat. From the sinus node, electrical impulses travel across the atria to the ventricles, causing them to contract and pump blood to your lungs and body.
From the sinus node, electrical impulses travel across the atria, causing the atrial muscles to contract and pump blood into the ventricles.
The electrical impulses then arrive at a cluster of cells called the atrioventricular (AV) node — usually the only pathway for signals to travel from the atria to the ventricles.
The atrioventricular (AV) node slows down the electrical signal before sending it to the ventricles. This slight delay allows the ventricles to fill with blood. When electrical impulses reach the muscles of the ventricles, they contract, causing them to pump blood either to the lungs or to the rest of the body.
When anything disrupts this complex system, it can cause the heart to beat too fast (tachycardia), too slow (bradycardia) or with an irregular rhythm.
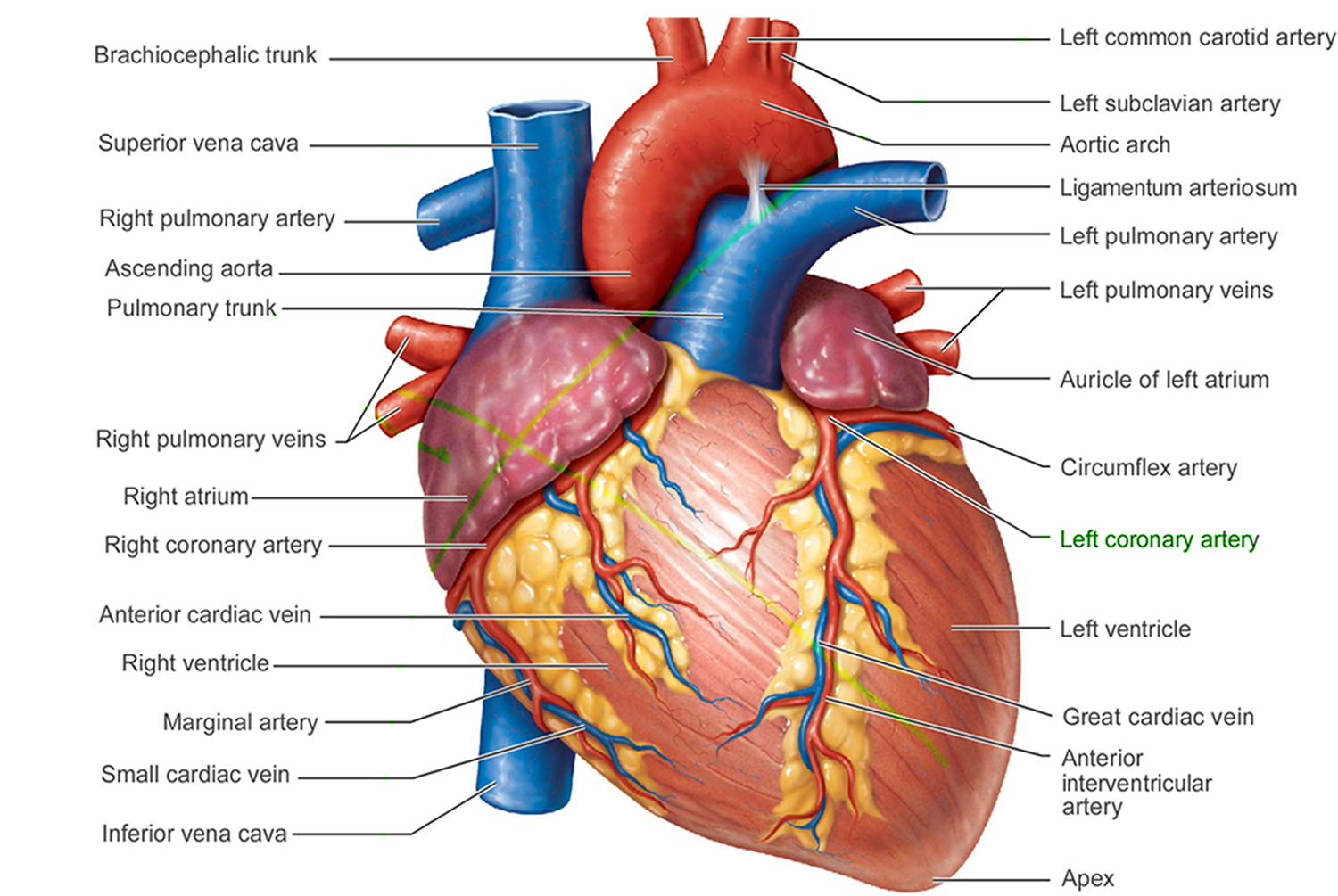
Figure 2. The anatomy of the heart
Premature ventricular contractions causes
Premature ventricular contractions are abnormal contractions that begin in the ventricles. These extra contractions usually beat sooner than the next expected regular heartbeat. And they often interrupt the normal order of pumping, which is the atria first, then the ventricles.
The reasons aren’t always clear. Certain triggers, heart diseases or changes in the body can make cells in the ventricles electrically unstable. Heart disease or scarring may also cause electrical impulses to be misrouted.
Premature ventricular contractions can be associated with:
- Certain medications, including decongestants and antihistamines
- Alcohol or illegal drugs
- Increased levels of adrenaline in the body that may be caused by caffeine, tobacco, exercise or anxiety
- Injury to the heart muscle from coronary artery disease, congenital heart disease, high blood pressure or heart failure
Cardiac causes of premature ventricular contractions include the following:
- Acute myocardial infarction (heart attack) or myocardial ischemia
- Myocarditis
- Cardiomyopathy, dilated or hypertrophic 2 – Two consistent predictors of of premature ventricular contraction-induced cardiomyopathy are premature ventricular contraction burden and premature ventricular contraction QRS duration 3
- Myocardial contusion
- Mitral valve prolapse
Other causes of premature ventricular contractions include the following:
- Hypoxia and/or hypercapnia
- Medications (eg, digoxin, sympathomimetics, tricyclic antidepressants, aminophylline, caffeine)
- Illicit substances (eg, cocaine, amphetamines, alcohol, tobacco)
- Hypomagnesemia, hypokalemia, hypercalcemia
Risk factors for premature ventricular contractions
The following can increase your risk of premature ventricular contractions:
- Caffeine , tobacco, alcohol and illicit drugs
- Exercise — if you have certain types of premature ventricular contractions
- High blood pressure (hypertension)
- Anxiety
- Heart disease, including congenital heart disease, coronary artery disease, heart attack, heart failure and a weakened heart muscle (cardiomyopathy)
Premature ventricular contractions prognosis
In asymptomatic patients without underlying heart disease, the long-term prognosis is similar to that of the general population. Asymptomatic patients with ejection fractions greater than 40% have a 3.5% incidence of sustained ventricular tachycardia or cardiac arrest. Therefore, in patients with no evidence of heart disease on noninvasive workup, reassurance is appropriate.
One caveat to this is that emerging data suggest that very frequent ventricular ectopy (>4000/24 hr) may be associated with the development of cardiomyopathy related to abnormal electrical activation of the heart. This mechanism is thought to be similar to that of chronic right ventricular pacing associated cardiomyopathy.
In the setting of acute coronary ischemia/infarction, patients with simple premature ventricular contractions rarely progress to malignant arrhythmias. However, persistent complex ectopy after heart attack is associated with increased risk of sudden death and may be an indication for electrophysiologic studies.
In patients with underlying chronic structural heart disease (e.g, cardiomyopathy, infarction, valvular disease) and complex ectopy (eg, >10 premature ventricular contractions/hr), mortality is significantly increased. The following points should be kept in mind:
First, understanding of the role of antiarrhythmic therapy in the months after myocardial infarction (heart attack) is poor. The Cardiac Arrhythmia Suppression Trial 4 studied patients with ventricular ectopy after myocardial infarction (heart attack) to see if antiarrhythmic therapy improved survival rates. Despite suppression of ectopy on Holter monitoring, patients treated with encainide, flecainide, or moricizine had increased rates of sudden death and death from all causes. Findings have suggested a role for amiodarone in this patient population and have had significant reductions in rates of post-myocardial infarction (heart attack) ventricular arrhythmias and death. Moricizine was discontinued in July 2007 because of diminished market demand.
Second, left ventricular dysfunction has a stronger association with increased mortality rate than do premature ventricular contractions. Many now believe that premature ventricular contractions reflect the severity of heart disease rather than contribute to arrhythmogenesis. Some studies in recent years suggest that increased variability of the premature ventricular contraction coupling interval in patients with underlying heart diseases, including left ventricular dysfunction, is a predictor of cardiac death; however, this remains a matter of debate 5.
Third, electrophysiologic studies has a primary role in risk stratification of patients with frequent or complex premature ventricular contractions. Patients with premature ventricular contractions that are noninducible (ie, unable to trigger ventricular tachycardia during stimulation) have a low risk of sudden death.
Frequent premature ventricular contractions may be associated with increased risk of stroke in patients who do not have hypertension and diabetes 6.
Mortality/morbidity
The clinical significance of premature ventricular contractions depends on the clinical context in which they occur, as follows:
- Premature ventricular contractions in young, healthy patients without underlying structural heart disease are usually not associated with any increased mortality
- Premature ventricular contractions in older patients, in particular those with underlying heart disease, are associated with an increased risk of adverse cardiac events, particularly sustained ventricular dysrhythmias and sudden death
- In patients who have had a myocardial infarction (heart attack), the risk of malignant ventricular arrhythmias and sudden death is related to the complexity and frequency of the premature ventricular contractions; patients with premature ventricular contractions in Lown classes 3-5 are at greatest risk.
Premature ventricular contractions complications
Having frequent premature ventricular contractions or certain patterns of them might increase your risk of developing heart rhythm problems (arrhythmias) or weakening of the heart muscle (cardiomyopathy).
Rarely, when accompanied by heart disease, frequent premature contractions can lead to chaotic, dangerous heart rhythms and possibly sudden cardiac death.
Premature ventricular contractions symptoms
Premature ventricular contractions often cause few or no symptoms. But you might feel an odd sensation in your chest, such as:
- Fluttering
- Pounding or jumping
- Skipped beats or missed beats
- Increased awareness of your heartbeat
Premature ventricular contractions diagnosis
An electrocardiogram (ECG) can detect the extra beats and identify the pattern and source.
Electrocardiogram
Depending on the frequency and timing of your premature ventricular contractions, different types of ECG testing options are available.
- Standard ECG. Sensors (electrodes) are attached to your chest and limbs to create a graphical record of the electrical signals traveling through your heart. This brief test usually is done in a clinic or hospital setting.
If you have infrequent premature ventricular contractions, they may not be detected during the brief time a standard ECG is being done. In such cases, you may need to use a portable monitoring device for 24 hours or more to capture any abnormal rhythms. Common types of portable ECGs include:
- Holter monitor. You carry this device in your pocket or in a pouch on a belt or shoulder strap. It automatically records your heart’s activity for 24 or 48 hours, which provides your doctor with an extended look at your heart rhythms.
- Event recorder. This device can be carried in your pocket or worn on a belt or shoulder strap for home monitoring of your heart’s activity. When you feel symptoms, you push a button, and a brief ECG strip recording is made. The recorder, which can be used for several weeks, allows your doctor to see your heart rhythm at the time of your symptoms.
- Exercise stress ECG. This test uses electrocardiography to record your heart’s electrical activity while you walk on a treadmill or pedal an exercise bike. It can help determine whether exercise triggers your premature ventricular contractions.
- Echocardiography is useful not only in evaluating the ejection fraction, which is important in determining the prognosis and also in identifying valvular disease or ventricular hypertrophy.
Premature ventricular contractions treatment
For most people, premature ventricular contractions with an otherwise normal heart won’t need treatment. However, if you have frequent premature ventricular contractions, your doctor might recommend treatment.
In some cases, if you have heart disease that could lead to more-serious rhythm problems, you might need the following:
Lifestyle changes. Eliminating common premature ventricular contraction triggers — such as caffeine or tobacco — can decrease the frequency and severity of your symptoms.
- Medications. Beta blockers, which are often used to treat high blood pressure and heart disease can suppress premature contractions. Other medications, such as calcium channel blockers, or anti-arrhythmic drugs, such as amiodarone (Pacerone) or flecainide (Tambocor), also might be used if you have ventricular tachycardia or frequent premature ventricular contractions that interfere with your heart’s function. Amiodarone 7 is also a useful agent for suppressing ectopy or ventricular tachycardia (if hemodynamically significant); additional beneficial effects include coronary vasodilation and increased cardiac output via a reduction in systemic vascular resistance.
- Radiofrequency catheter ablation. For premature ventricular contractions that don’t respond to lifestyle changes or medications, your doctor might recommend ablation therapy. This procedure uses radiofrequency energy to destroy the area of heart tissue that is causing your irregular contractions. Guidelines on the use of catheter ablation in ventricular arrhythmia are available from the European Heart Rhythm Association (EHRA) and the Heart Rhythm Society (HRS) in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA) 8.Fichtner et al 9 evaluated the outcome and success of premature ventricular contraction ablation in 408 patients in the German Ablation Registry from March 2007 to May 2011. The acute ablation success rate was 82%; all patients were discharged alive after a median of 3 days; and no patient suffered a heart attack, stroke, or major bleeding. After 12 months of follow-up, 99% of patients were still alive, and 76% showed significantly improved symptoms.Im et al investigated ECG criteria for predicting successful ablation of premature ventricular contractions from the right coronary cusp. They found that the presence of a dominant positive lead I, an R-wave duration index (RWDI) higher than 43.6%, and an S-wave amplitude lower than 0.95mV in aVL predicted right coronary cusp premature ventricular contractions in patients with a sensitivity of 83% and a specificity of 94% 10.
Home remedies
The following self-care strategies can help control premature ventricular contractions and improve your heart health:
- Track your triggers. If you have frequent symptoms, you might want to take note of your symptoms and your activities. This can help identify substances or actions that may trigger premature ventricular contractions.
- Modify your substance use. Caffeine, alcohol, tobacco and other recreational drugs are known triggers of premature ventricular contractions. Reducing or avoiding these substances can reduce your symptoms.
- Manage stress. Anxiety can trigger abnormal heartbeats. If you think anxiety is contributing to your condition, try stress-reduction techniques, such as biofeedback, meditation or exercise, or talk to your doctor about anti-anxiety medications.
- Simpson RJ, Cascio WE, Schreiner PJ, et al. Prevalence of premature ventricular contractions in a population of African American and white men and women: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2002 Mar. 143(3):535-40.[↩]
- Cha YM, Lee GK, Klarich KW, Grogan M. Premature ventricular contraction-induced cardiomyopathy: a treatable condition. Circ Arrhythm Electrophysiol. 2012 Feb 1. 5(1):229-36.[↩]
- Lee AK, Deyell MW. Premature ventricular contraction-induced cardiomyopathy. Curr Opin Cardiol. 2016 Jan. 31 (1):1-10.[↩]
- CAST Investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. The Cardiac Arrhythmia Suppression Trial (CAST) Investigators. N Engl J Med. 1989 Aug 10. 321(6):406-12.[↩]
- Lee CH, Park KH, Nam JH, et al. Increased variability of the coupling interval of premature ventricular contractions as a Predictor of cardiac mortality in patients with left ventricular dysfunction. Circ J. 2015 Oct 23. 79 (11):2360-6.[↩]
- Agarwal SK, Heiss G, Rautaharju PM, Shahar E, Massing MW, Simpson RJ Jr. Premature ventricular complexes and the risk of incident stroke: the Atherosclerosis Risk In Communities (ARIC) Study. Stroke. 2010 Apr. 41(4):588-93.[↩]
- Cairns JA, Connolly SJ, Roberts R, Gent M. Randomised trial of outcome after myocardial infarction in patients with frequent or repetitive ventricular premature depolarisations: CAMIAT. Canadian Amiodarone Myocardial Infarction Arrhythmia Trial Investigators. Lancet. 1997 Mar 8. 349(9053):675-82.[↩]
- [Guideline] Aliot EM, Stevenson WG, Almendral-Garrote JM, Bogun F, Calkins CH, Delacretaz E, et al. EHRA/HRS Expert Consensus on Catheter Ablation of Ventricular Arrhythmias: developed in a partnership with the European Heart Rhythm Association (EHRA), a Registered Branch of the European Society of Cardiology (ESC), and the Heart Rhythm Society (HRS); in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA). Europace. 2009 Jun. 11(6):771-817.[↩]
- Fichtner S, Senges J, Hochadel M, Tilz R, Willems S, Eckardt L, et al. Safety and efficacy in ablation of premature ventricular contraction: data from the German ablation registry. Clin Res Cardiol. 2017 Jan. 106 (1):49-57.[↩]
- Im SI, Park KM, Park SJ, Kim JS, On YK. New electrocardiographic criteria for predicting successful ablation of premature ventricular contractions from the right coronary cusp. Int J Cardiol. 2016 Sep 16. 224:199-205.[↩]