Contents
- What is primary sclerosing cholangitis
- Bile ducts and human liver
- Primary biliary cirrhosis vs Primary sclerosing cholangitis
- Primary sclerosing cholangitis life expectancy
- Primary sclerosing cholangitis complications
- Primary sclerosing cholangitis causes
- Primary sclerosing cholangitis symptoms
- Primary sclerosing cholangitis diagnosis
- Primary sclerosing cholangitis treatment
What is primary sclerosing cholangitis
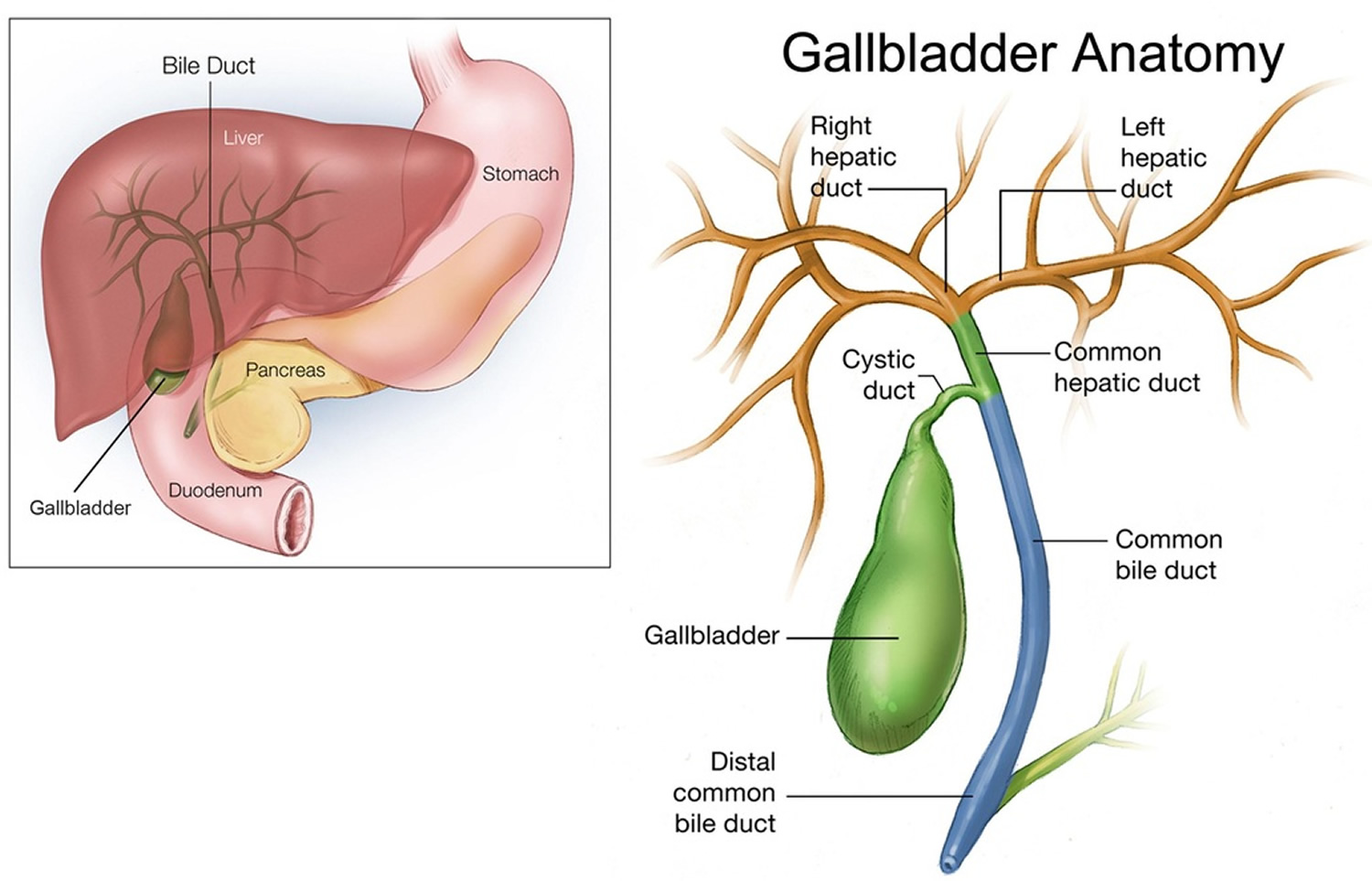
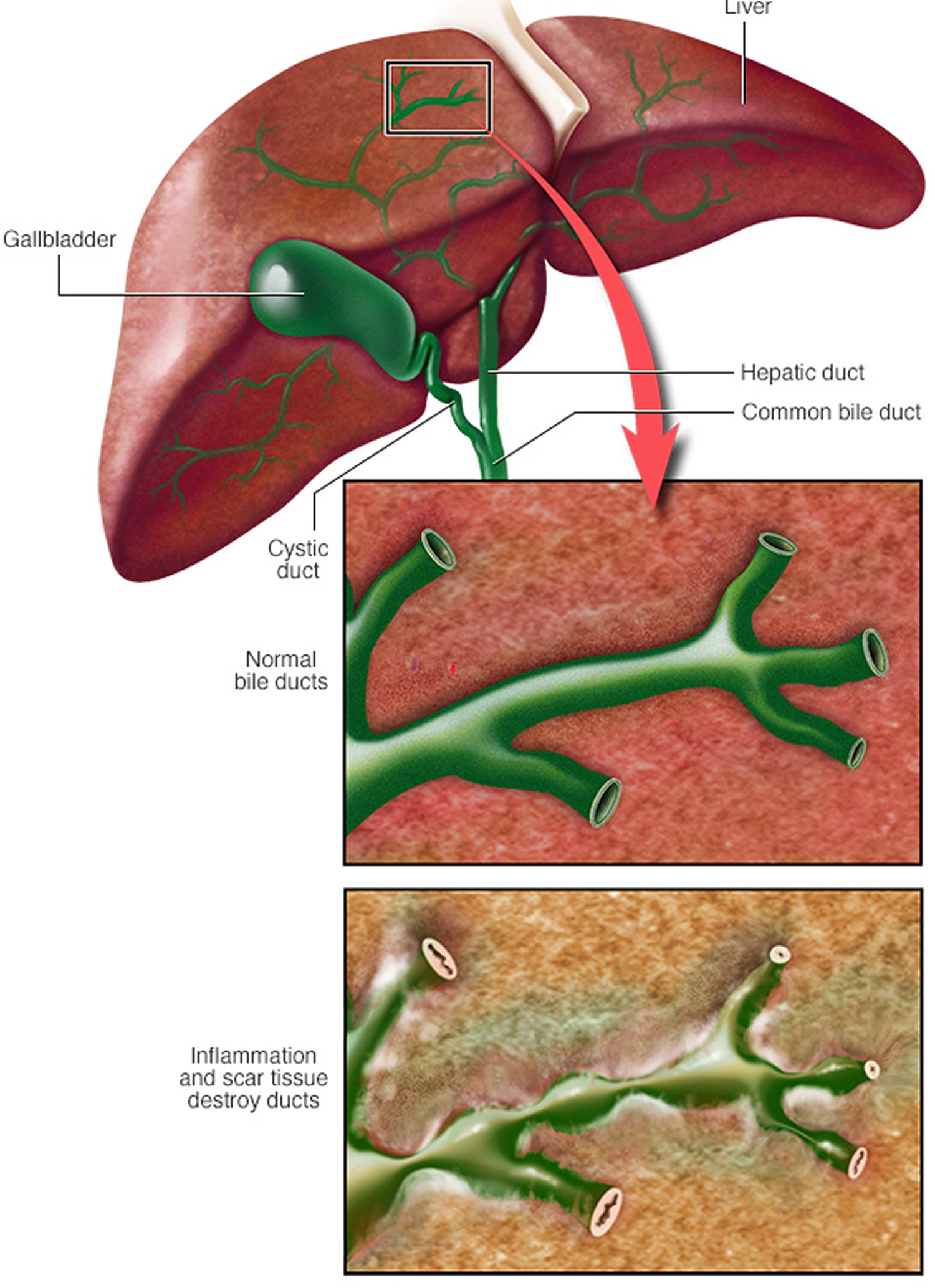
Primary sclerosing cholangitis (PSC) is a chronic disease in which the bile ducts inside and outside the liver become inflamed and scarred, and are eventually narrowed or blocked. Bile ducts carry bile (a fluid that helps to digest fats) from the liver, where bile is produced, to the gallbladder, where it is stored, and to the small intestine, where it aids in digestion. Primary sclerosing cholangitis occurs because of inflammation in the bile ducts (cholangitis) that leads to scarring (sclerosis) and narrowing of the ducts. As a result, bile cannot be released to the gallbladder and small intestine, and it builds up in the liver and causes liver damage. This damage can lead to cirrhosis and eventually liver failure. Medical experts believe that primary sclerosing cholangitis is an autoimmune disease , which means that your body’s immune system is overactive and attacks normal, healthy bile duct cells. Primary sclerosing cholangitis is strongly associated with inflammatory bowel disease (IBD), particularly ulcerative colitis 1. Primary sclerosing cholangitis is a premalignant condition, associated with higher rates of hepatobiliary and colorectal cancer in patients with ulcerative colitis 1.
Primary sclerosing cholangitis is usually diagnosed around age 40, and for unknown reasons, it affects men seven times as often as women (70% of patients affected are men).
An estimated 1 in 10,000 to 6 to 16 in 100,000 people have primary sclerosing cholangitis, and the condition is diagnosed in approximately 1 in 100,000 people per year worldwide 2. Interestingly, the incidence appears to be increasing with time 3. Many people have no signs or symptoms of primary sclerosing cholangitis when they are diagnosed, but routine blood tests reveal liver problems. When apparent, the earliest signs and symptoms of primary sclerosing cholangitis include extreme tiredness (fatigue), discomfort in the abdomen, and severe itchiness (pruritus). As the condition worsens, affected individuals may develop yellowing of the skin and whites of the eyes (jaundice) and an enlarged spleen (splenomegaly). Eventually, the buildup of bile damages the liver cells, causing chronic liver disease (cirrhosis) and liver failure. Without bile available to digest them, fats pass through the body. As a result, weight loss and shortages of vitamins that are absorbed with and stored in fats (fat-soluble vitamins) can occur. A fat-soluble vitamin called vitamin D helps absorb calcium and helps bones harden, and lack of this vitamin can cause thinning of the bones (osteoporosis) in people with primary sclerosing cholangitis.
You are more likely to get primary sclerosing cholangitis if you:
- are between the ages of 30 and 50
- are a man
- have inflammatory bowel disease (IBD), most commonly ulcerative colitis. About 7 out of 10 people who have primary sclerosing cholangitis also have inflammatory bowel disease (IBD) 4.
- have a family member who has primary sclerosing cholangitis
Primary sclerosing cholangitis is often associated with another condition called inflammatory bowel disease, which is characterized by inflammation of the intestines that causes open sores (ulcers) in the intestines and abdominal pain. However, the reason for this link is unclear. Approximately 70 percent of people with primary sclerosing cholangitis have inflammatory bowel disease, most commonly a form of the condition known as ulcerative colitis. In addition, people with primary sclerosing cholangitis are more likely to have an autoimmune disorder, such as type 1 diabetes, celiac disease, or thyroid disease, than people without the condition. Autoimmune disorders occur when the immune system malfunctions and attacks the body’s tissues and organs. People with primary sclerosing cholangitis also have an increased risk of developing cancer, particularly cancer of the bile ducts (cholangiocarcinoma).
In most people with primary sclerosing cholangitis, the disease progresses slowly. It can eventually lead to liver failure, repeated infections, and tumors of the bile duct or liver. Medications so far have not been effective in slowing or preventing the progression of primary sclerosing cholangitis. Care for primary sclerosing cholangitis focuses on monitoring liver function, managing symptoms and, when possible, doing procedures that temporarily open blocked bile ducts. A liver transplant is the only known cure for advanced primary sclerosing cholangitis. But primary sclerosing cholangitis may recur in the transplanted liver in a small number of patients.
Areas of controversy
The pathogenesis of primary sclerosing cholangitis is unclear, and competing theories exist surrounding toxic bile acids, enhanced homing of particular T cells from the gut to the liver and increased passage of toxins to the liver through a permeable bowel wall. It is unclear whether the higher rate of colonic cancer in primary sclerosing cholangitis with ulcerative colitis also occurs in primary sclerosing cholangitis with Crohn’s disease. Ursodeoxycholic acid (UDCA) therapy reduces liver enzymes but has not been shown to improve survival. It may reduce the prevalence of bowel cancer.
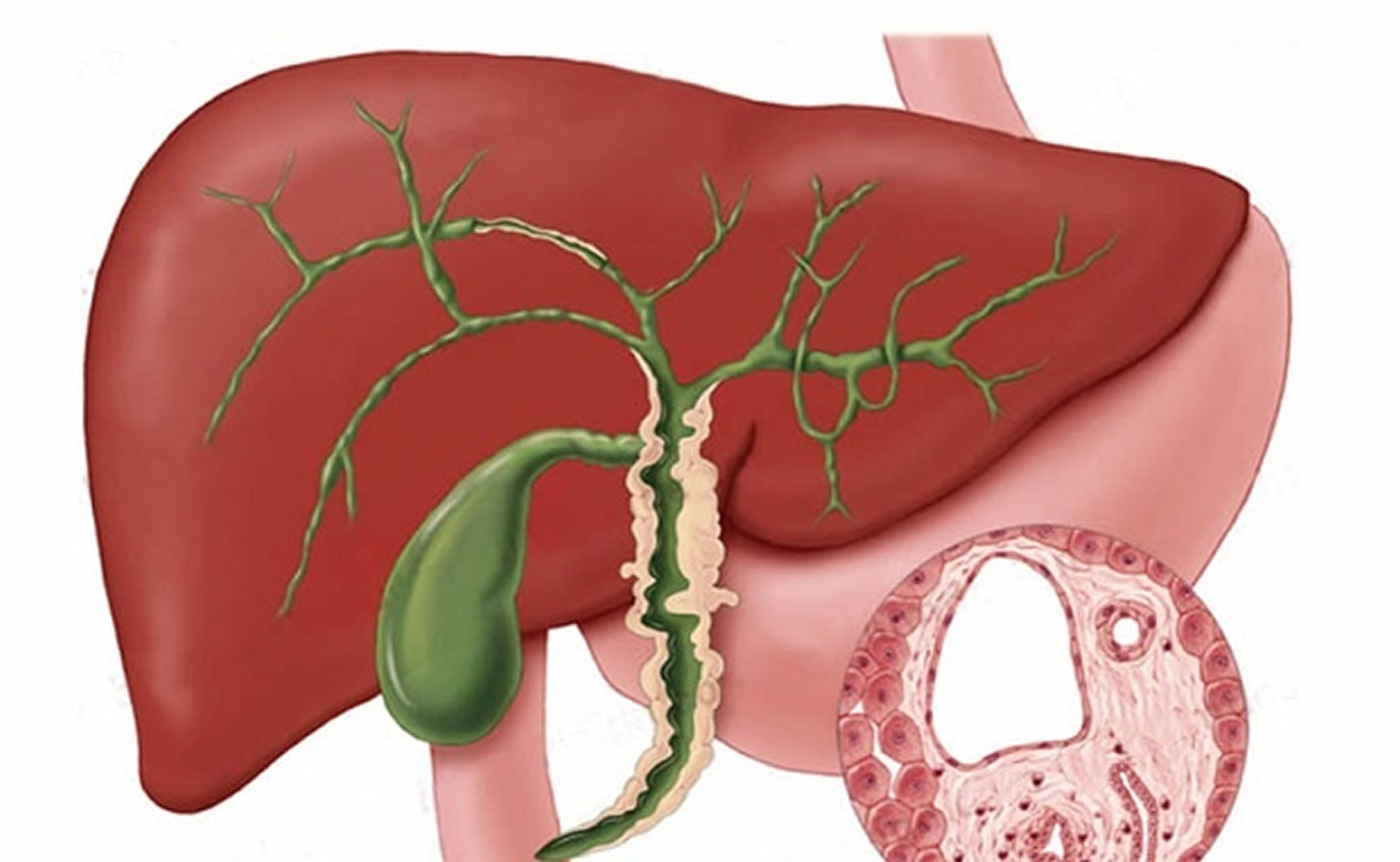
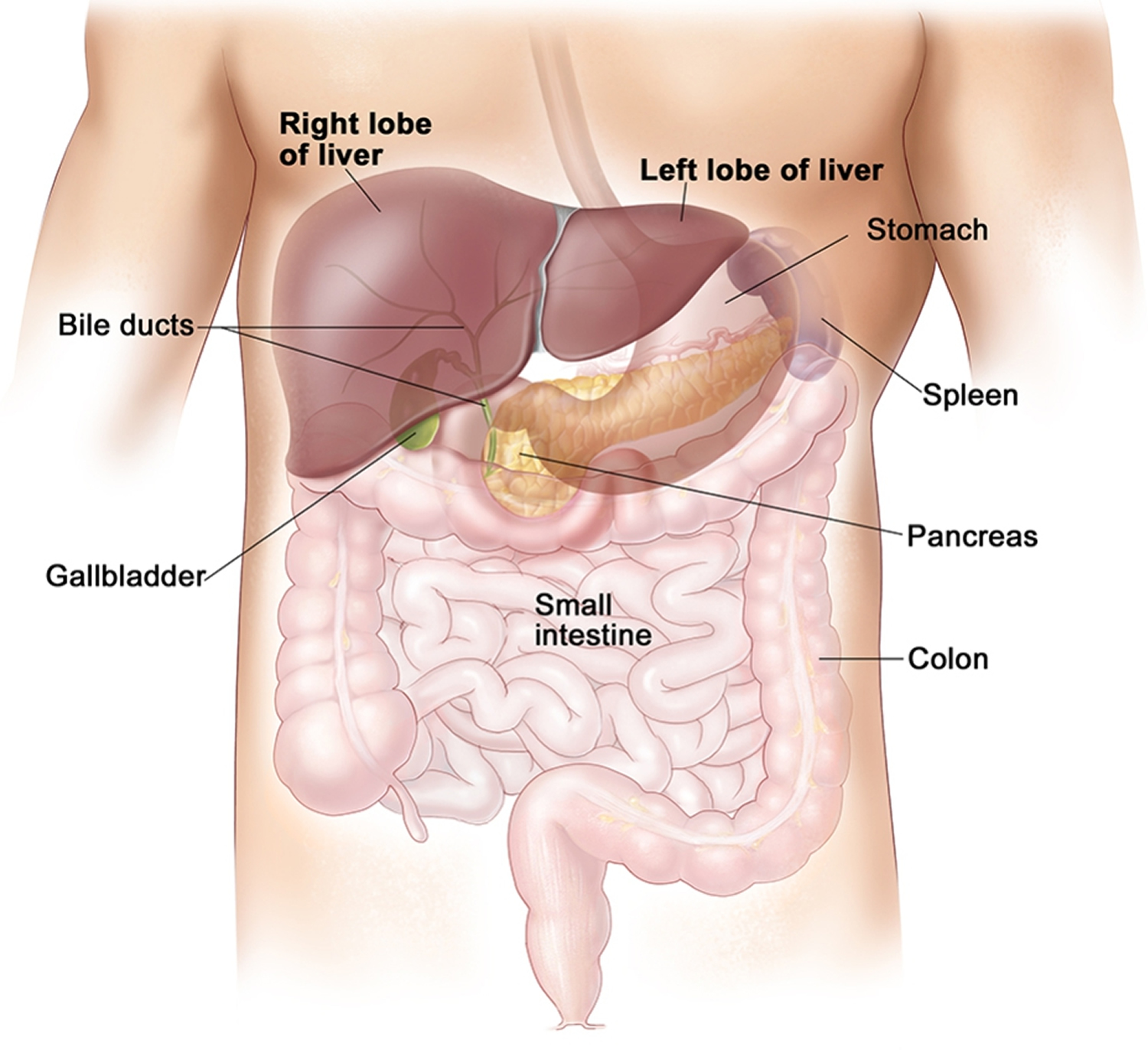
Bile ducts and human liver
Your liver is the largest organ inside your body, weighing about 1.4 kg (3 pounds) in an average adult. The liver is in the right upper quadrant of the abdominal cavity, just inferior to the diaphragm in the right superior part of the abdominal cavity and under your right ribs just beneath your right lung – filling much of the right hypochondriac and epigastric regions and extending into the left hypochondriac region. The liver is partially surrounded by the ribs, and extends from the level of the fifth intercostal space to the lower margin of the right rib cage, which protects this highly vascular organ from blows that could rupture it. The liver is shaped like a wedge, the wide base of which faces right and the narrow apex of which lies just inferior to the level of the left nipple. The reddish-brown liver is well supplied with blood vessels.
The liver also has two minor lobes, the quadrate lobe and the caudate lobe. Each lobe is separated into many tiny hepatic lobules, the liver’s functional units (Figure 2). A lobule consists of many hepatic cells radiating outward from a central vein. Blood-filled channels called hepatic sinusoids separate platelike groups of these cells from each other. Blood from the digestive tract, carried in the hepatic portal vein, brings newly absorbed nutrients into the sinusoids and nourishes the hepatic cells.
Within the hepatic lobules are many fine bile canaliculi, which carry secretions from hepatic cells to bile ductules (see Figure 2). The ductules of neighboring lobules converge to ultimately form the hepatic ducts. These ducts merge, in turn, to form the common hepatic duct.
Bile is a yellowish-green liquid continuously secreted from hepatic cells. In addition to water, bile contains bile salts, bile pigments (bilirubin and biliverdin), cholesterol, and electrolytes. Of these, bile salts are the most abundant and are the only bile components that have a digestive function.
Bile pigments are breakdown products of hemoglobin from red blood cells and are normally secreted in the bile.
Jaundice, a yellowing of the skin and mucous membranes due to accumulation of bile pigment, has several causes. In obstructive jaundice bile ducts are blocked, perhaps by scar tissues like in primary sclerosing cholangitis. In hepatocellular jaundice the liver is diseased, as in cirrhosis or hepatitis.
Figure 1. Location of the human liver
Figure 2. Liver lobule
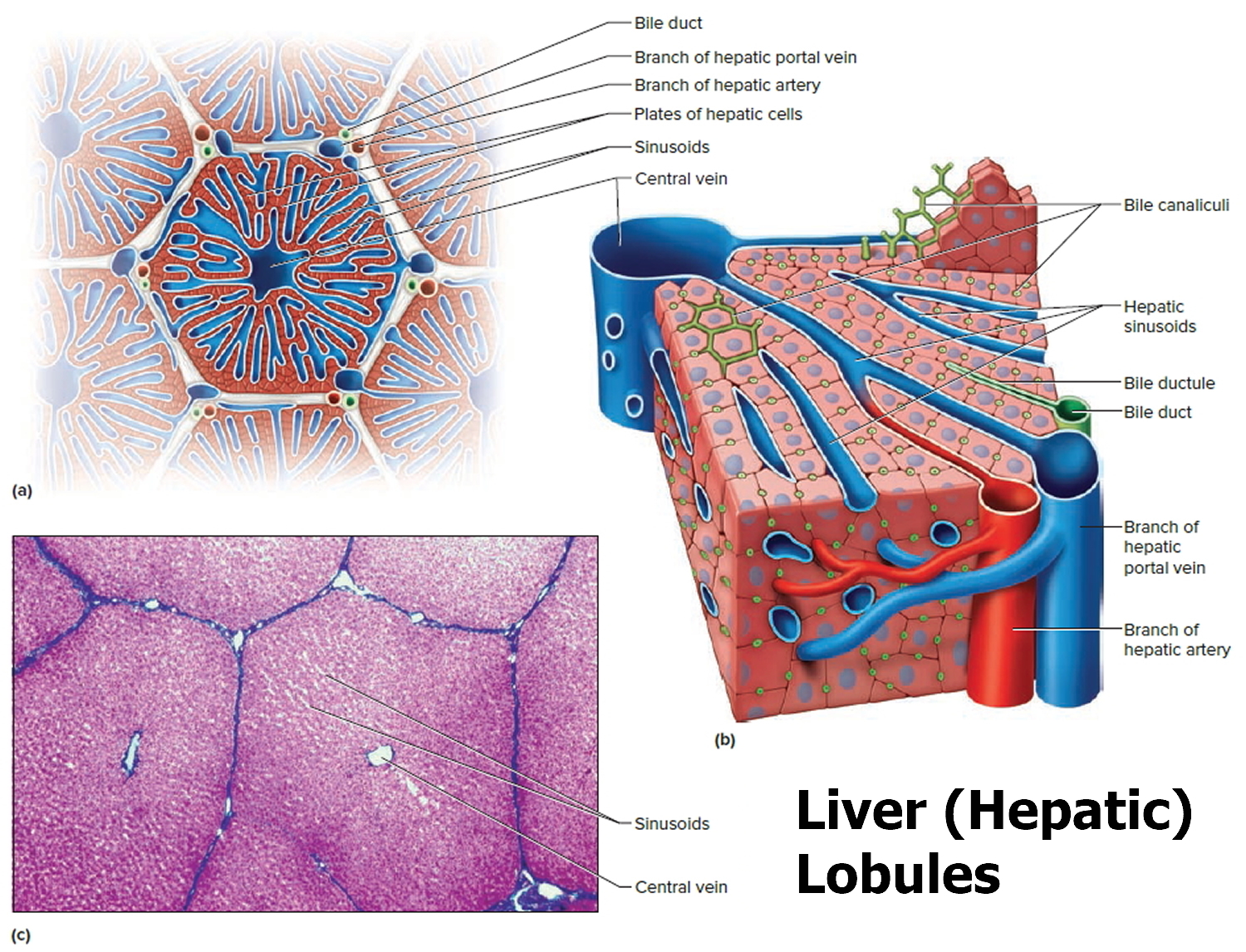 Note: (a) Cross section of a hepatic lobule. (b) Enlarged longitudinal section of a hepatic lobule. (c) Light micrograph of hepatic lobules in cross section.
Note: (a) Cross section of a hepatic lobule. (b) Enlarged longitudinal section of a hepatic lobule. (c) Light micrograph of hepatic lobules in cross section.Figure 3. Gallbladder anatomy
Primary biliary cirrhosis vs Primary sclerosing cholangitis
Primary biliary cirrhosis is now called primary biliary cholangitis. Primary biliary cirrhosis (primary biliary cholangitis) is a chronic inflammatory disease in which the small bile ducts in the liver become injured and inflamed and are eventually destroyed. Primary biliary cirrhosis is characterized by chronic inflammation and progressive destruction and fibrosis of the bile ducts leading to an obstruction to bile flow from the liver and cirrhosis. When there are no bile ducts, bile builds up and causes liver damage. This damage can lead to liver scarring, cirrhosis, and eventually liver failure. Primary biliary cholangitis is believed to be an autoimmune disease , which means that the immune system is overactive and attacks normal, healthy bile duct cells.
Researchers estimate that in the United States, about 65 out of every 100,000 women and about 12 out of every 100,000 men have primary biliary cholangitis 5.
The exact cause of primary biliary cirrhosis (primary biliary cholangitis) is unknown. Experts think that a person’s tendency to have an overactive immune system, which may be genetic , and unknown environmental triggers play a role in causing primary biliary cholangitis. Possible environmental triggers include:
- infections
- cigarette smoking. In contrast to primary biliary cirrhosis (primary biliary cholangitis), primary sclerosing cholangitis is predominantly a disease of non-smokers, with multiple studies showing only 5% of patients with primary sclerosing cholangitis smoke compared with 25% of controls 6. The high rate of non-smoking is irrespective of the presence of underlying inflammatory bowel disease. Additionally, coffee may potentially also play a protective role 7.
- exposure to certain chemicals
Anti-mitochondrial antibodies (AMA) are found in the blood of about 95 percent of people with primary biliary cirrhosis 8.
You are more likely to get primary biliary cirrhosis (primary biliary cholangitis) if you:
- are a woman
- are older than age 35
- have a parent or sibling—particularly an identical twin—with primary biliary cirrhosis
- are of Northern European descent
People with primary biliary cholangitis may have certain autoimmune diseases, including:
- autoimmune hepatitis
- autoimmune thyroid diseases—conditions in which the immune system attacks the thyroid gland
- Celiac disease
- Raynaud’s disease
- Sjögren’s syndrome
- scleroderma
Some people with primary biliary cirrhosis may also have symptoms of another condition, such as an underactive thyroid (hypothyroidism). People with primary biliary cholangitis may also have frequent urinary tract infections.
Common complications of primary biliary cirrhosis (primary biliary cholangitis) include:
- high blood cholesterol levels
- osteoporosis
- fat-soluble vitamin deficiencies (e.g. vitamins A, D, E and K)
These common complications can be prevented and treated.
Similar to primary sclerosing cholangitis, primary biliary cholangitis can also lead to cirrhosis and liver failure.
Because both primary biliary cirrhosis (primary biliary cholangitis) and primary sclerosing cholangitis affect the bile ducts, their symptoms are very similar. People with primary biliary cirrhosis may have higher-than-normal cholesterol levels, which may be a sign that their liver is not working properly.
The most common early symptoms of primary biliary cirrhosis (primary biliary cholangitis) are:
- feeling tired
- itchy skin
Other common early symptoms may include:
- abdominal pain
- nausea
- poor appetite
- weight loss
- arthritis / bone or joint aches
- dizziness when standing up (postural or orthostatic hypotension)
- dry eyes and mouth
Symptoms can range from mild to severe, and this isn’t always related to the degree of liver damage you have.
Some people with primary biliary cirrhosis have severe symptoms but their liver isn’t severely damaged, while others may have significant liver damage but no symptoms or only mild ones.
Advanced primary biliary cirrhosis
Medication can usually help to delay liver damage in people with primary biliary cirrhosis, but as the liver slowly becomes more scarred and damaged (eventually ending up with cirrhosis), you may have additional symptoms.
These can include:
- weakness
- nausea
- weight loss
- diarrhea
- build-up of fluid in your abdomen that can make you look heavily pregnant (ascites)
- a build-up of fluid in the legs, ankles and feet (edema)
- dark urine
- pale stools
- yellowish eyes and skin, called jaundice
- the formation of small fatty deposits on the skin called xanthomas, usually around your eyes (xanthelasmata)
- a tendency to bleed and bruise more easily
- problems with memory and concentration
Many people have no symptoms when they are first diagnosed with primary biliary cirrhosis. Doctors diagnose up to 6 in 10 people with primary biliary cirrhosis before symptoms begin 9. People with primary biliary cirrhosis and no symptoms are identified through blood tests. Some people do not have symptoms for years after they have been diagnosed with primary biliary cirrhosis.
Doctors treat primary biliary cirrhosis with medicines. Your doctor may prescribe ursodeoxycholic acid (UDCA) or ursodiol (Actigall, Urso). Although ursodiol does not cure primary biliary cirrhosis, it can slow the progression of liver damage. People who respond to ursodiol early in the course of primary biliary cirrhosis can live longer without needing a liver transplant.
If you do not respond to ursodiol, your doctor may prescribe obeticholic acid (Ocaliva). However obeticholic acid does not improve symptoms, and further research is needed to show whether it slows liver disease progression.
Obeticholic acid (Ocaliva) may be offered as an option for treating primary biliary cirrhosis, either:
- in combination with ursodeoxycholic acid (UDCA) – if ursodeoxycholic acid (UDCA) isn’t working well enough
- on its own – for people who can’t take ursodeoxycholic acid (UDCA)
People who may need obeticholic acid will first need assessment by a specialist team with experience in treating primary biliary cirrhosis.
One possible side effect of obeticholic acid is itching. If itching is a problem, your dose may be lowered or you may be offered medication to treat the itching. People with very advanced liver disease may be prescribed a lower dose of obeticholic acid, or it may not be recommended.
Primary sclerosing cholangitis life expectancy
Because there are currently no treatments that halt primary sclerosing cholangitis disease progression, average duration to fulminant liver failure can range between 9 and 12 years. Several features correlate with a poor prognosis. These include: an enlarged liver or spleen, anemia, cirrhosis, female sex and older age. Increasing bilirubin also correlates with disease progression. The natural history of primary sclerosing cholangitis is highly variable among patients. Alkaline phosphatase (ALP) [a liver enzyme] levels tend to fluctuate over time, but a persistently low alkaline phosphatase (ALP) (e.g. <1.5 times the upper limit of normal) has been shown to confer a good clinical outcome 10. In one study of hyperbilirubinemic patients, the survival of patients with primary sclerosing cholangitis whether symptomatic or asymptomatic is reported to be below the normal population. Whilst initial studies suggested the median time from diagnosis to death or liver transplantation is 10–12 years, a recent population study from the Netherlands gave a much more optimistic view of a median time of 21.3 years from diagnosis to primary sclerosing cholangitis-related death or liver transplantation 11. This is likely a better estimate, as it represents a large population, as opposed to tertiary centres with potential referral bias (see Figure 5). Mortality rates are as high as 30% at 6 years from diagnosis, with cancer as the main cause (40–50% of deaths), followed by liver failure (30–40%). Around 15% of patients will require liver transplantation 12.
A liver transplantation is considered for patients with a more advanced disease, a transplantation has a 90% survival rate over years. But the disease may recur in the transplanted liver in a small number of patients.
Figure 5. Primary sclerosing cholangitis life expectancy
[Source 13]Primary sclerosing cholangitis complications
Complications of primary sclerosing cholangitis may include:
- Liver disease and failure. Chronic inflammation of the bile ducts throughout your liver can lead to tissue scarring (cirrhosis), liver cell death and, eventually, loss of liver function.
- Repeated bile duct infections. If scarring of the bile ducts slows or stops the flow of bile out of the liver, you may experience frequent infections in the bile ducts. The risk of infection is particularly high after you’ve had a surgical procedure to expand a badly scarred bile duct or remove a stone blocking a bile duct.
- Portal hypertension. Your portal vein is the major route for blood flowing from your digestive system into your liver. Portal hypertension refers to high blood pressure in this vein. Portal hypertension can cause fluid from the liver to leak into your abdominal cavity (ascites). It can also divert blood from the portal vein to other veins, causing these veins to become swollen (varices). Varices are weak veins and tend to bleed easily, which can be life-threatening.
- Thinning bones. People with primary sclerosing cholangitis may experience thinning bones (osteoporosis). Your doctor may recommend a bone density exam to test for osteoporosis every few years. Calcium and vitamin D supplements may be prescribed to help prevent bone loss.
- Bile duct cancer. If you have primary sclerosing cholangitis, you have an increased risk of developing cancer in the bile ducts or gallbladder.
- Gallbladder cancer.
- Colon cancer. People with primary sclerosing cholangitis associated with inflammatory bowel disease have an increased risk of colon cancer. If you’ve been diagnosed with primary sclerosing cholangitis, your doctor may recommend testing for inflammatory bowel disease, even if you have no signs or symptoms, since the risk of colon cancer is elevated if you have both diseases.
Cancer is common, occurring in up to 25% of patients, and primary sclerosing cholangitis is considered to be a premalignant condition. Initially, the prevalence of colorectal cancer in the setting of ulcerative colitis/primary sclerosing cholangitis was purported to be as high as 9% at 10 years, 31% at 20 years and 50% at 25 years 14, though subsequent studies have suggested a more modest prevalence. A recent Danish study, however, analysed a large number of patients and found that the relative risk of developing colorectal cancer in patients with primary sclerosing cholangitis/ulcerative colitis was 9.13 compared with patients with ulcerative colitis alone. Only one small study suggests an increased risk of colorectal cancer in the setting of primary sclerosing cholangitis with Crohn’s disease, but further studies contradict this, indicating no increased risk for colorectal cancer in the setting of primary sclerosing cholangitis/Crohn’s disease 15. It appears that the diagnosis of colorectal cancer can occur very soon after the diagnosis of primary sclerosing cholangitis (a median time of only 1.3 years in the Scandinavian study); hence, the treating physician must be proactive in detecting and potentially preventing this. Accordingly, international guidelines recommend annual surveillance colonoscopy for all patients with primary sclerosing cholangitis and inflammatory bowel disease, beginning at the time of diagnosis of primary sclerosing cholangitis. Additionally, patients with primary sclerosing cholangitis without inflammatory bowel disease at index colonoscopy should have 5-yearly colonoscopies screening for the development of inflammatory bowel disease given its quiescent nature in primary sclerosing cholangitis, as well as the potential for malignancy should it occur.
Most liver transplantation centers regard the diagnosis of cholangiocarcinoma as an absolute contraindication to liver transplantation, as very poor survival rates have been shown in studies. The Mayo Clinic experience of neo-adjuvant chemoradiation for unresectable perihilar cholangiocarcinoma prior to liver transplantation in highly selected patients has shown promising results, in non-metastatic tumours less than 3 cm in diameter. These results have been replicated in other centers 16.
Gallbladder cancer is also more prevalent in patients with primary sclerosing cholangitis—around 2–3% prevalence, warranting annual ultrasound surveillance. International guidelines recommend cholecystectomy in the setting of gallbladder polyps as around 50% are malignant 17. There is recent literature to suggest that small gallbladder polyps less than 0.8 cm are benign, and surveillance may be an option, especially if the risk of complications from the surgery is significant due to underlying advanced liver disease 18. The risk of hepatocellular carcinoma also is increased in patients with cirrhosis.
Primary sclerosing cholangitis causes
It’s not clear what causes primary sclerosing cholangitis. Primary sclerosing cholangitis is thought to arise from a combination of genetic and environmental factors such as an immune system reaction to an infection or toxin may trigger primary sclerosing cholangitis in people who are genetically predisposed to it. Researchers believe that genetic changes play a role in this condition because it often occurs in several members of a family and because immediate family members of someone with primary sclerosing cholangitis have an increased risk of developing the condition. It is likely that specific genetic variations increase a person’s risk of developing primary sclerosing cholangitis, and then exposure to certain environmental factors triggers the disorder. However, the genetic changes that increase susceptibility and the environmental triggers remain unclear.
A large proportion of people with primary sclerosing cholangitis also have inflammatory bowel disease, an umbrella term that includes ulcerative colitis and Crohn’s disease.
Primary sclerosing cholangitis and inflammatory bowel disease don’t always appear at the same time, though. In some cases, primary sclerosing cholangitis is present for years before inflammatory bowel disease occurs. If primary sclerosing cholangitis is diagnosed, it’s important to look for inflammatory bowel disease because there is a greater risk of colon cancer.
Somewhat less often, people being treated for inflammatory bowel disease turn out to have primary sclerosing cholangitis as well. And rarely, people with primary sclerosing cholangitis develop inflammatory bowel disease only after having a liver transplant.
There is also evidence that variations in certain genes involved in immune function influence the risk of developing primary sclerosing cholangitis. The most commonly associated genes belong to a family of genes called the human leukocyte antigen (HLA) complex. The HLA complex helps the immune system distinguish the body’s own proteins from proteins made by foreign invaders (such as viruses and bacteria). Each HLA gene has many different normal variations, allowing each person’s immune system to react to a wide range of foreign proteins. Specific variations of several HLA genes seem to be present more often in people with primary sclerosing cholangitis than in people who do not have the disorder. These variations may dysregulate the body’s immune response, leading to the inflammation of the bile ducts in people with primary sclerosing cholangitis. However, the mechanism is not well understood. Researchers are also studying variations in other genes related to the body’s immune function to understand how they contribute to the risk of developing this condition.
Risk Factors for primary sclerosing cholangitis
Factors that may increase the risk of primary sclerosing cholangitis include:
- Your age. Primary sclerosing cholangitis can occur at any age, but it’s most often diagnosed between the ages of 30 and 50.
- Your sex. Primary sclerosing cholangitis occurs more often in men.
- Inflammatory bowel disease. A large proportion of people with primary sclerosing cholangitis also have inflammatory bowel disease.
- Your geographical location. People with Northern European heritage have a higher risk of primary sclerosing cholangitis.
- AIDS (acquired immunodeficiency syndrome)
Primary sclerosing cholangitis symptoms
Primary sclerosing cholangitis is often diagnosed before symptoms appear when a routine blood test or an X-ray taken for an unrelated condition shows liver abnormalities.
Early symptoms often include:
- Fatigue
- Feeling tired or weak
- Itching
Other symptoms may include:
- losing weight without trying
- poor appetite
- fever
- pain in the abdomen
Many people diagnosed with primary sclerosing cholangitis before they have symptoms continue to feel generally well for several years. But there’s no reliable way to predict how quickly or slowly the disease will progress for any individual.
As the disease gets worse, you may get symptoms of cirrhosis and liver failure, such as:
- bloating
- bruising and bleeding easily
- confusion, difficulty thinking, or memory loss
- redness in the palms of your hands
- swelling in your legs, ankles, or feet
- yellowish eyes and skin, called jaundice.
Primary sclerosing cholangitis diagnosis
Doctors diagnose primary sclerosing cholangitisbased on your medical and family history, a physical exam, and the results of medical tests.
Your doctor will ask you about your symptoms. He or she may also ask whether:
- you have a history of inflammatory bowel disease, particularly ulcerative colitis
- one of your parents or siblings has primary sclerosing cholangitis
- you have a history of autoimmune disease, such type 1 diabetes, celiac disease, and thyroid diseases
During a physical exam, your doctor may:
- use a stethoscope to listen to sounds in your abdomen
- tap or press on specific areas of your abdomen
- look for symptoms of cirrhosis and liver failure
- check to see if your liver and spleen are larger than they should be
- check for tenderness or pain in your abdomen
Your doctor may also check for and ask about symptoms of a bile duct infection, which may include:
- fever
- chills
- nausea
- vomiting
- yellowish eyes and skin, called jaundice
Tests and procedures used to diagnose primary sclerosing cholangitis include:
- Liver function blood tests. A blood test to check your liver function, including levels of your liver enzymes, can give your doctor clues about your diagnosis.
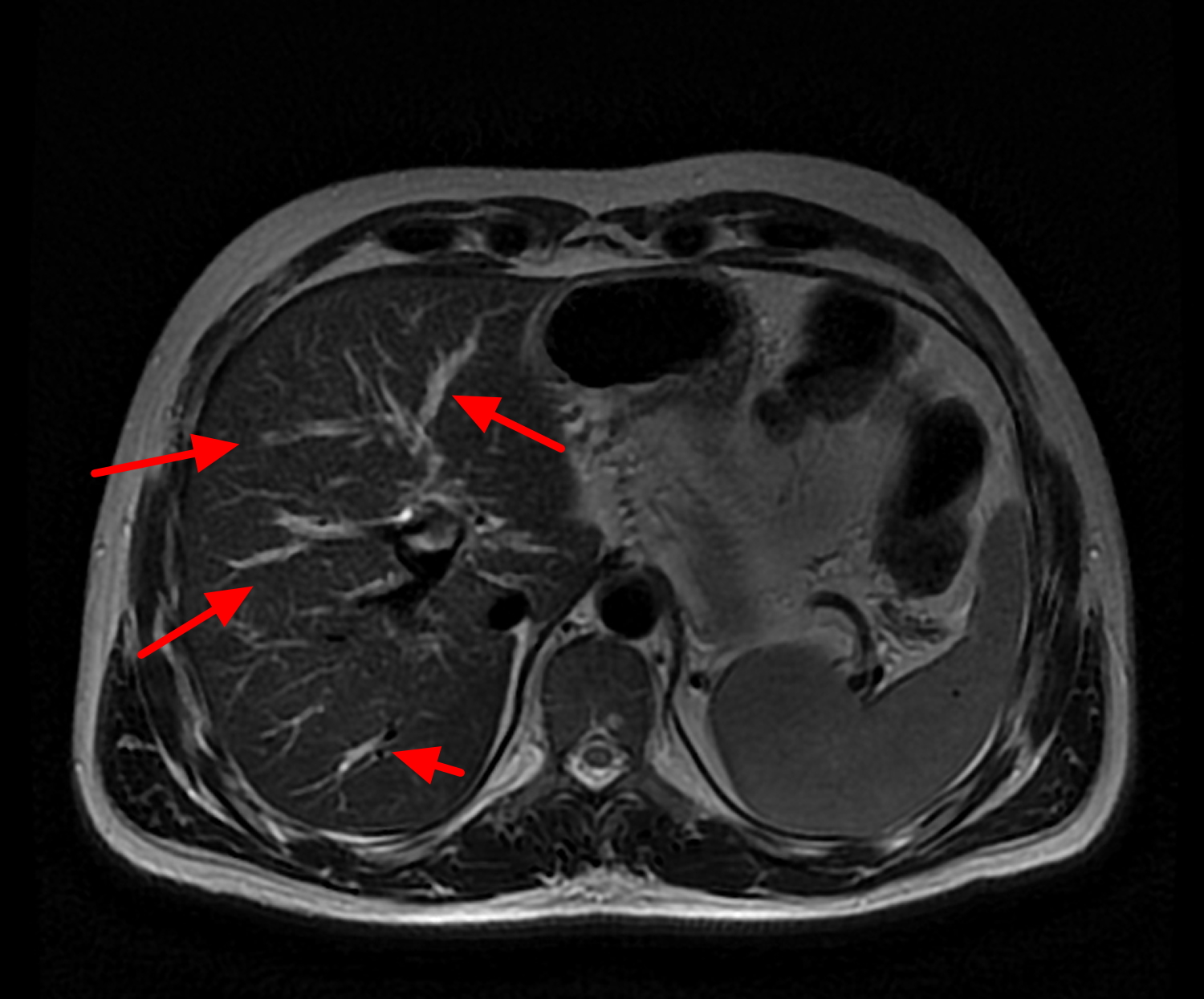
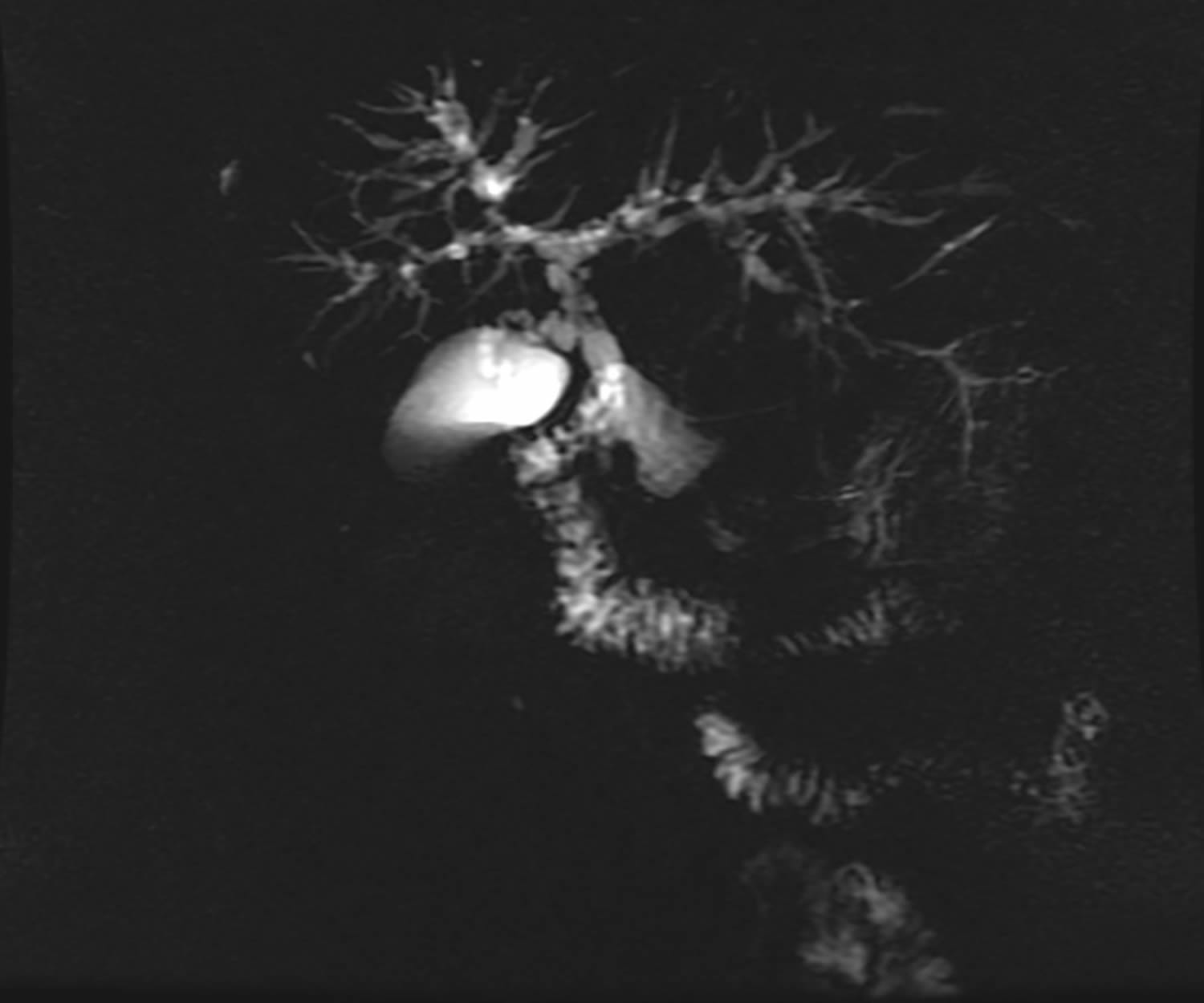
- MRI of your bile ducts. Magnetic resonance cholangiopancreatography uses magnetic resonance imaging (MRI) to make images of your liver and bile ducts and is the test of choice to diagnose primary sclerosing cholangitis.
- Computed tomography (CT) scans
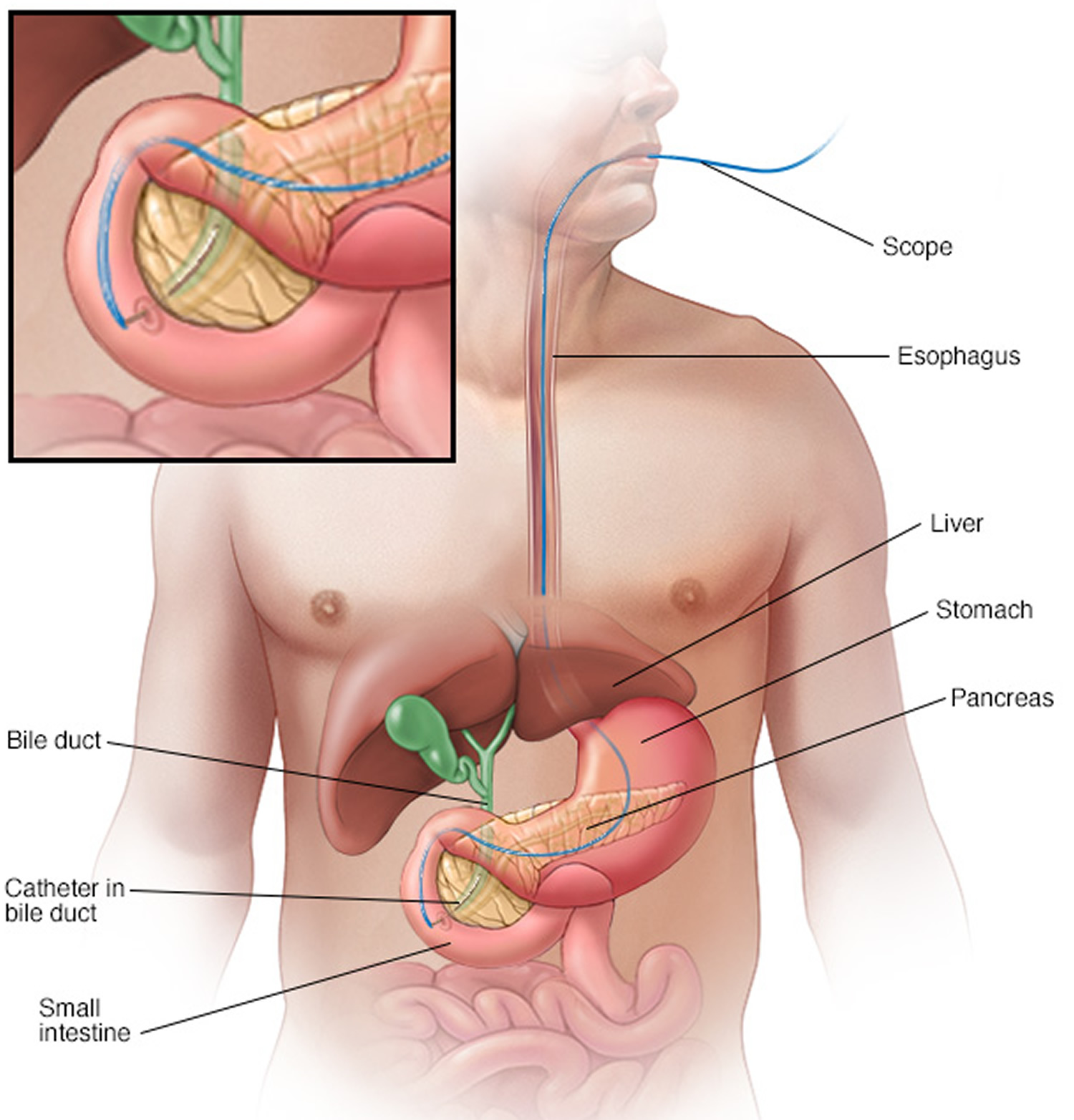
- X-rays of your bile ducts. A type of bile duct X-ray called endoscopic retrograde cholangiopancreatography (ERCP) in addition to, or instead of, an MRI may be needed. But this test is rarely used for diagnosis because of the risk of complications. To make your bile ducts visible on an X-ray, your doctor uses a flexible tube passed down your throat to inject dye into the area of your small intestine where your bile ducts empty. An ERCP is the test of choice if signs and symptoms persist despite no abnormalities on an MRI. An ERCP is often the initial test if you’re unable to have an MRI because of a metal implant in your body.
- Percutaneous transhepatic cholangiography (PTC). PTC is an x-ray of the bile ducts. A special dye injected into the bile ducts lets a doctor see the bile ducts on the x-ray. PTC can show narrowing or blockage in the bile ducts.
- Transient elastography, a special ultrasound that measures the stiffness of your liver
- Testing a sample of liver tissue. A liver biopsy is a procedure to remove a piece of liver tissue for laboratory testing. Your doctor inserts a needle through your skin and into your liver to extract a tissue sample. A liver biopsy can help determine the extent of damage to your liver. The test is used only when the diagnosis of primary sclerosing cholangitis is still uncertain after less invasive tests.
Figure 6. Primary sclerosing cholangitis – MRI of liver and bile ducts
Figure 7. Primary sclerosing cholangitis – magnetic resonance cholangiopancreatography (MRCP) image showing typical features in primary sclerosing cholangitis with stricturing, beading and dilatation of both intra- and extrahepatic ducts.
Figure 8. Primary sclerosing cholangitis – endoscopic retrograde cholangiopancreatography (ERCP)
Primary sclerosing cholangitis treatment
Treatments for primary sclerosing cholangitis focus on managing complications and monitoring liver damage. Many medications have been studied in people with primary sclerosing cholangitis, but so far none have been found to slow or reverse the liver damage associated with this disease.
Treatment for narrowed or blocked bile ducts
If your bile ducts are narrowed or blocked, your doctor may use medical procedures, such as endoscopic retrograde cholangiopancreatography (ERCP) and percutaneous transhepatic cholangiography, to open them and help keep them open.
Treatment for itching
Your doctor may recommend over-the-counter products and medicines or prescribe medicines to treat itchy skin. Over-the-counter products and medicines include skin creams and antihistamines. For mild itchy skin, your doctor may prescribe hydroxyzine. For severe itchy skin, your doctor may prescribe cholestyramine.
- Skin creams and lotions that contain camphor, menthol, pramoxine, or capsaicin
- Bile acid sequestrants. Medications that bind to bile acids — the substances thought to cause itching in liver disease — are the first line treatment for itching in primary sclerosing cholangitis.
- Antibiotics. If you have trouble tolerating a bile acid-binding drug or if it doesn’t help, your doctor may prescribe rifampin (Rifadin, Rimactane, others), an antibacterial drug. Exactly how rifampin reduces itching is unknown, but it may block the brain’s response to itch-inducing chemicals in your circulation.
- Antihistamines. This type of medication may help reduce mild itching caused by primary sclerosing cholangitis. Whether these medications are effective for this condition is unknown. Antihistamines may worsen the liver disease symptoms of dry eyes and dry mouth. On the other hand, antihistamines can help with sleep if itching keeps you awake.
- Opioid antagonists. Itching related to liver disease may also respond to opioid antagonist drugs, such as naltrexone. Like rifampin, these drugs seem to reduce the itch sensation by acting on your brain.
- Ursodeoxycholic acid (UDCA). Also known as ursodiol, UDCA is a naturally occurring bile acid that may help relieve itching symptoms caused by liver disease by increasing the absorbability of bile. One possible side effect of ursodeoxycholic acid (UDCA) is weight gain. People gain an average of 2.3kg (5lbs) during the first year of taking the medication, although most people don’t gain any more weight after this. Other side effects can include diarrhea, nausea, vomiting and thinning hair.
Treatment for infections
Bile that backs up in narrowed or blocked ducts causes frequent bacterial infections. To prevent and treat these infections, people with primary sclerosing cholangitis may take repeated courses of antibiotics or continue taking antibiotics for long periods.
Before any procedure that could cause an infection, such as an endoscopic procedure or abdominal surgery, you’ll also need to take antibiotics.
Primary sclerosing cholangitis diet
Primary sclerosing cholangitis makes it difficult for your body to absorb certain fat-soluble vitamins – vitamin A, vitamin D, vitamin E and vitamin K. Even though you may eat a healthy diet, you may find that you can’t get all the nutrients you need.
If you have low levels of fat-soluble vitamins in your body, your doctor may recommend eating foods that are high in vitamins A, D, E, and K. Follow your doctor’s instructions on the type and amount of vitamins you should take. Your doctor may recommend vitamin supplements that you take as tablets or that you receive as an infusion through a vein in your arm. If the disease weakens your bones, you may take calcium and vitamin D supplements as well.
You should eat well-balanced meals that give you enough calories and nutrients. A health care professional such as a dietitian or nutritionist can help you plan meals that are good sources of fat-soluble vitamins – vitamin A, vitamin D, vitamin E and vitamin K.
What should I avoid eating if I have primary sclerosing cholangitis?
You should avoid eating raw shellfish such as oysters, which can have bacteria that may cause severe infections in people with liver disease. Your doctor may recommend that you avoid foods that are high in salt, fat, and carbohydrates, especially those with added sugars.
Your doctor will recommend that you stop drinking alcohol, or at least limit your intake to no more than one or two drinks per week. If you have primary sclerosing cholangitis and cirrhosis, your doctor will recommend that you don’t drink any alcohol at all.
Take steps to care for your liver, such as:
- Don’t drink alcohol.
- Quit smoking if you smoke.
- Get vaccinated against hepatitis A and B.
- Use care with chemicals at home and at work.
- Maintain a healthy weight.
- Follow directions on all medications, both prescription and over-the-counter. Make sure your pharmacist and any doctor prescribing for you know that you have a liver disease.
- Talk to your doctor about any herbs or supplements you’re taking since some can be harmful to your liver.
- The damage to your liver can affect its ability to process certain medications. This means you may need to avoid certain medicines – for example, non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen.
Treatment for bile duct blockages
Blockages that occur in your bile ducts may be due to disease progression but can be a sign of cancer of the bile duct. Endoscopic retrograde cholangiopancreatography (ERCP) can help determine the cause, and bile duct blockage can be treated with:
- Balloon dilation. This procedure can open blockages in the larger bile ducts outside the liver. In balloon dilation, your doctor runs a slender tube with an inflatable balloon at its tip (balloon catheter) through an endoscope and into a blocked bile duct. Once the balloon catheter is in place, the balloon is inflated.
- Stent placement. In this procedure, your doctor uses an endoscope and attached instruments to place a small plastic tube called a stent in a blocked bile duct to hold the duct open.
Cirrhosis
If your primary sclerosing cholangitis has caused cirrhosis, your doctor may treat the health problems related to cirrhosis with medicines, surgery, and other medical procedures. If cirrhosis leads to liver failure, you may need a liver transplant.
Liver transplant
Your doctor may consider a liver transplant if your primary sclerosing cholangitis has caused liver failure. Doctors consider liver transplants only after all other treatment options have failed.
A liver transplant is the only treatment known to cure primary sclerosing cholangitis. During a liver transplant, surgeons remove your diseased liver and replace it with a healthy liver from a donor.
A liver transplant is reserved for people with liver failure or other severe complications of primary sclerosing cholangitis. Though uncommon, it’s possible for primary sclerosing cholangitis to recur after a liver transplant.
Home remedies
No alternative medicine treatments have been found to treat primary sclerosing cholangitis. But some complementary and alternative therapies may help you cope with the signs and symptoms of the disease. Talk to your doctor about your options.
Fatigue is common in people with primary sclerosing cholangitis. While doctors can treat some factors that may contribute to fatigue, your signs and symptoms may still persist. You might find relief with complementary and alternative treatments that have shown some benefit for fatigue, such as:
- Exercise, such as walking 30 minutes most days of the week
- Spending time with friends and family
- Stress management techniques, such as meditation and relaxation exercises
- Yoga
- Primary sclerosing cholangitis: a clinical update. Br Med Bull. 2015 Jun;114(1):53-64. doi: 10.1093/bmb/ldv019. Epub 2015 May 16. https://academic.oup.com/bmb/article/114/1/53/246353[↩][↩]
- Eaton JE, Talwalkar JA, Lazaridis KN, Gores GJ, Lindor KD. Pathogenesis of primary sclerosing cholangitis and advances in diagnosis and management. Gastroenterology. 2013;145(3):521–536.[↩]
- Incidence of primary sclerosing cholangitis: a systematic review and meta-analysis. Hepatology. 2011 May;53(5):1590-9. doi: 10.1002/hep.24247. https://aasldpubs.onlinelibrary.wiley.com/doi/pdf/10.1002/hep.24247[↩]
- Trivedi PJ, Chapman RW. PSC, AIH and overlap syndrome in inflammatory bowel disease. Clinics and Research in Hepatology and Gastroenterology. 2012;36(5):420–436.[↩]
- Pyrsopoulos NT. Primary biliary cholangitis (primary biliary cirrhosis). https://emedicine.medscape.com/article/171117-overview[↩]
- Primary sclerosing cholangitis is associated with nonsmoking: a case-control study. Gastroenterology. 1996 May;110(5):1496-502. https://www.ncbi.nlm.nih.gov/pubmed/8613055[↩]
- Effects of coffee consumption, smoking, and hormones on risk for primary sclerosing cholangitis. Clin Gastroenterol Hepatol. 2014 Jun;12(6):1019-28. doi: 10.1016/j.cgh.2013.09.024. Epub 2013 Sep 25. https://www.ncbi.nlm.nih.gov/pubmed/24076415[↩]
- Prince MI, Chetwynd, Craig WL, Metcalf JV, James OFW. Asymptomatic primary biliary cirrhosis: clinical features, prognosis, and symptom progression in a large population based cohort. Gut. 2004;53(6):865‒870.[↩]
- Poupon R. Clinical manifestations, diagnosis, and prognosis of primary biliary cholangitis (primary biliary cirrhosis). https://www.uptodate.com/contents/clinical-manifestations-diagnosis-and-prognosis-of-primary-biliary-cholangitis-primary-biliary-cirrhosis[↩]
- Al Mamari S Djordjevic J Halliday JSet al. Improvement of serum alkaline phosphatase to <1.5 upper limit of normal predicts better outcome and reduced risk of cholangiocarcinoma in primary sclerosing cholangitis. J Hepatol 2013;58:329–34. https://www.ncbi.nlm.nih.gov/pubmed/23085647[↩]
- Rupp C Roessler A Halibasic Eet al. Reduction in alkaline phosphatase is associated with longer survival in primary sclerosing cholangitis, independent of dominant stenosis. Aliment Pharmacol Ther 2014;40:1292–301. https://www.ncbi.nlm.nih.gov/pubmed/25316001[↩]
- Bergquist A Ekbom A Olsson Ret al. Hepatic and extrahepatic malignancies in primary sclerosing cholangitis. J Hepatol 2002;36:321–7. https://www.ncbi.nlm.nih.gov/pubmed/11867174[↩]
- Boonstra K Weersma RK van Erpecum KJet al. Population-based epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis. Hepatology 2013;58:2045–55. https://www.ncbi.nlm.nih.gov/pubmed/23775876[↩]
- Broome U Lofberg R Veress Bet al. Primary sclerosing cholangitis and ulcerative colitis: evidence for increased neoplastic potential. Hepatology 1995;22:1404–8. https://www.ncbi.nlm.nih.gov/pubmed/7590655[↩]
- Braden B Halliday J Aryasingha Set al. Risk for colorectal neoplasia in patients with colonic Crohn’s disease and concomitant primary sclerosing cholangitis. Clin Gastroenterol Hepatol 2012;10:303–8. https://www.ncbi.nlm.nih.gov/pubmed/22037429[↩]
- Darwish Murad S Kim WR Harnois DMet al. Efficacy of neoadjuvant chemoradiation, followed by liver transplantation, for perihilar cholangiocarcinoma at 12 US centers. Gastroenterology 2012;143:88–98.e3; quiz e14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3846443/[↩]
- Buckles DC Lindor KD Larusso NFet al. In primary sclerosing cholangitis, gallbladder polyps are frequently malignant. Am J Gastroenterol 2002;97:1138–42.[↩]
- Eaton JE Thackeray EW Lindor KD. Likelihood of malignancy in gallbladder polyps and outcomes following cholecystectomy in primary sclerosing cholangitis. Am J Gastroenterol 2012;107:431–9.[↩]