Contents
What is proctitis
Proctitis is inflammation of the anus and of the lining of the rectum. The rectum is a muscular tube that’s connected to the end of your colon. Stool passes through the rectum on its way out of the body via the anus. Proctitis can cause rectal pain and the continuous sensation that you need to have a bowel movement. Proctitis symptoms can be short-lived, or they can become chronic.
Proctitis is common in people who have inflammatory bowel diseases. Sexually transmitted infections are another frequent cause. Proctitis also can be a side effect of radiation therapy for certain cancers.
What the Rectum
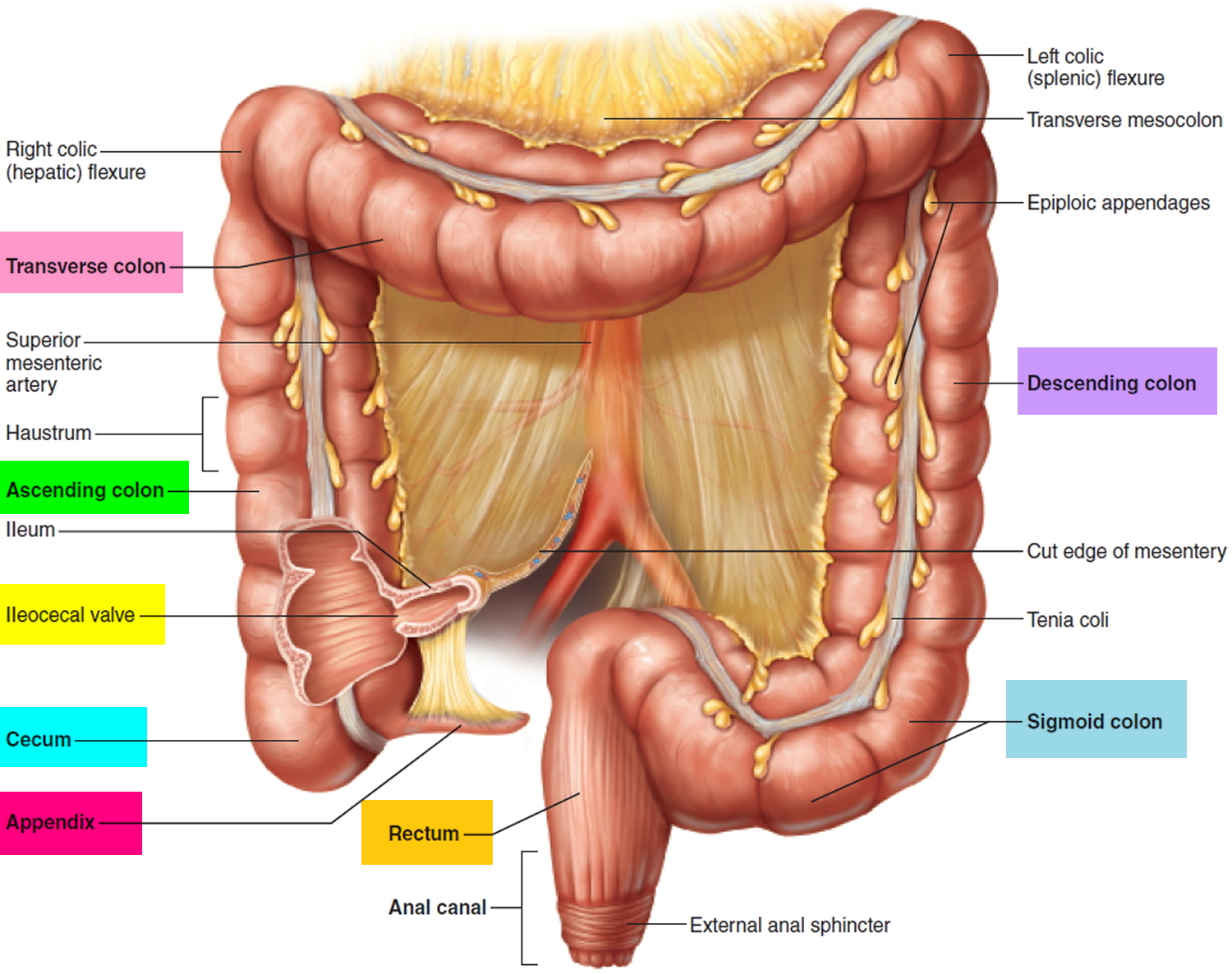
Extending from the sigmoid colon is the rectum. The rectum forms the last 15 cm (6 in.) of the large intestine. The rectum is an expandable organ for the temporary storage of feces. The rectum lies next to the sacrum and generally follows its curvature. The peritoneum firmly attaches the rectum to the sacrum. The rectum ends about 5 centimeters below the tip of the coccyx, where it becomes the anal canal.
The Anus and Anal Canal
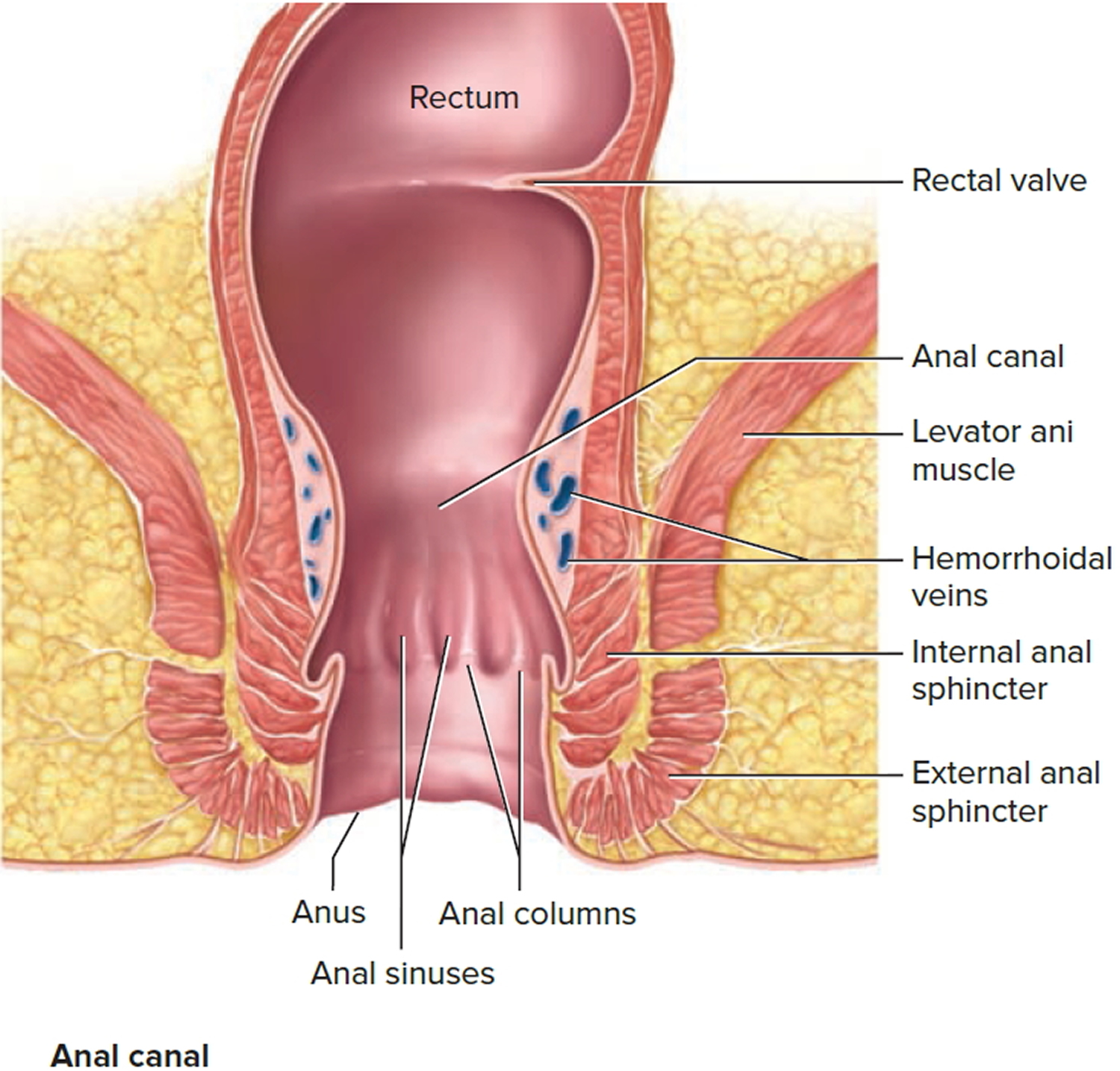
The anal canal is the continuation of the large intestine inferior to the rectum. The anal canal is about 3 cm long, it begins where the rectum passes through the levator ani, the muscle that forms the pelvic floor. At its distal end, the anal canal opens to the outside as the anus. Two sphincter muscles guard the anus—an internal anal sphincter muscle, composed of smooth muscle under involuntary control, and an external anal sphincter muscle, composed of skeletal muscle under voluntary control. A portion of the levator ani is responsible for maintaining the anorectal angle, an acute angle between the anus and the rectum that contributes to fecal continence. The anal canal lies entirely external to the abdominopelvic cavity in the perineum.
Internally, the superior half of the anal canal contains longitudinal folds of mucosa, the anal columns. These columns contain the terminal portions of the superior rectal artery and vein (the hemorrhoidal vessels). Neighboring anal columns join each other inferiorly at crescent-shaped transverse folds called anal valves. The pockets just superior to these valves are anal sinuses, which release mucus when they are compressed by feces, providing lubrication that eases fecal passage during defecation. The horizontal line along which the anal valves lie is called the pectinate (“comb-shaped”) line. Because the mucosa superior to this line is innervated by visceral sensory fibers, it is relatively insensitive to pain. Inferior to the pectinate line, however, the mucosa is sensitive to pain because it is innervated by somatic nerves.
The wall of the anal canal contains two sphincter muscles: an internal anal sphincter of smooth muscle and an external anal sphincter of skeletal muscle. The former is a thickening of the circular layer of the muscularis, whereas the latter is a distinct muscle. The external sphincter contracts voluntarily to inhibit defecation, whereas the internal sphincter contracts involuntarily, both to prevent feces from leaking from the anus between defecations and to inhibit defecation during emotional stress. During toilet training, children learn to control the external anal sphincter.
Figure 1. Rectum
Figure 2. Rectum anatomy and Anus (anal canal)
Rectum function
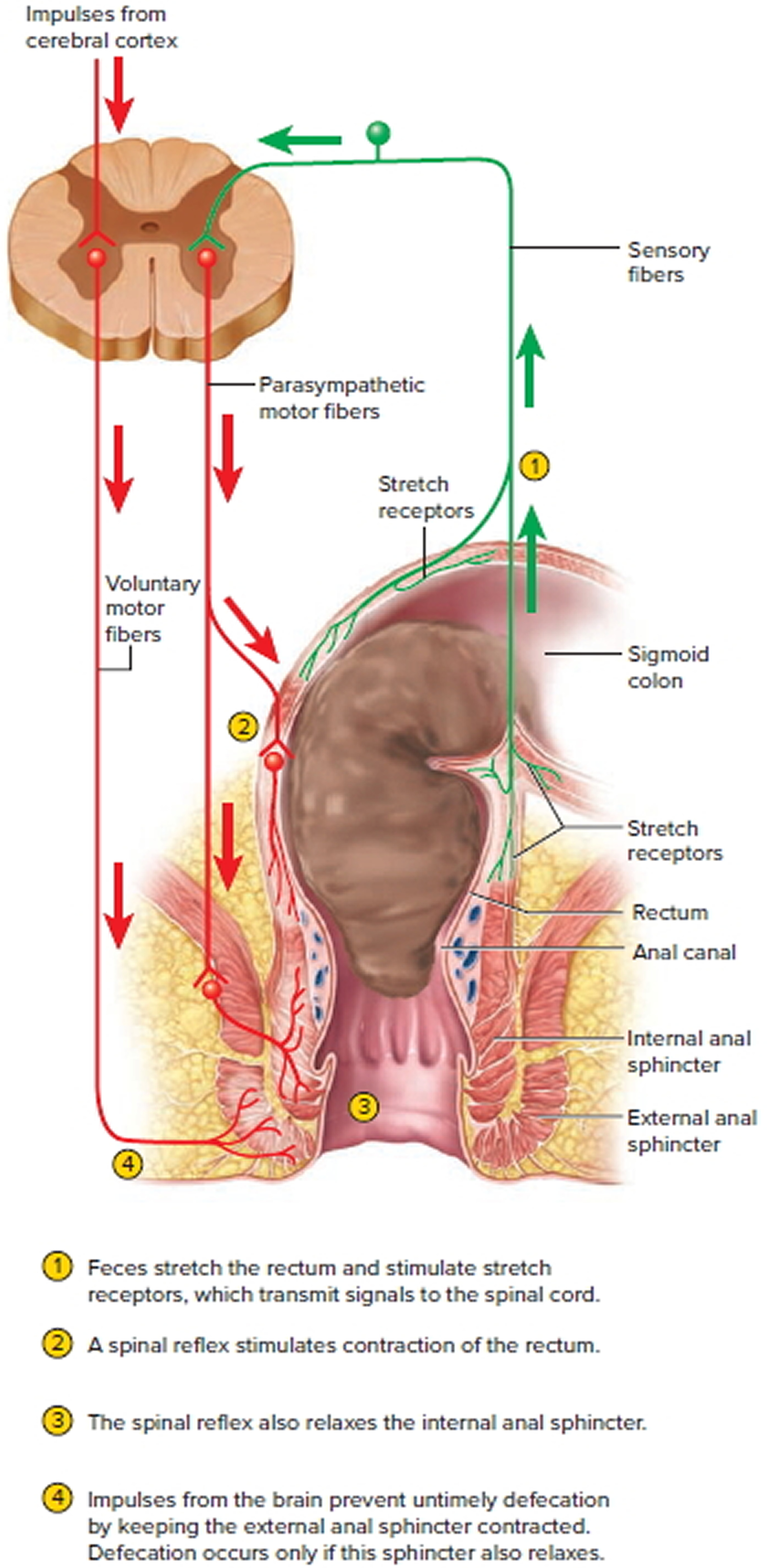
The rectum is usually empty and the anal sphincters contracted. When feces are squeezed into the rectum by mass peristaltic movements, the stretching of the rectal wall initiates the defecation reflex, which account for the urge to defecate that is often felt soon after a meal (Figure 3).
Figure 3. Rectum function and neural control of defecation
Ulcerative proctitis
Ulcerative colitis is a common chronic idiopathic inflammatory disease of the colon, which causes diarrhea, bleeding, and pain; its severity can range from mild to life-threatening. Ulcerative colitis typically extends proximally in a circumferential and uninterrupted manner that involves either all or only parts of the colon and sometimes is referred to with different terms, such as left-sided or pan colitis, depending upon the degree of colonic involvement. In approximately 30% of patients, the disease presents as ulcerative proctitis 1 with bowel inflammation limited to the rectum. Approximately 50% of patients with ulcerative proctitis have a relapsing-remitting course that is characterized by flares of varying severity and periods of remission during which patients are relatively asymptomatic 2. During flares, patients typically experience rectal bleeding, discomfort and urgency, pain, passage of mucous, tenesmus, and diarrhea.
In general, treatment of ulcerative proctitis is determined by the severity of symptoms and the extent of colonic involvement 3. Therapy is customarily tailored to the needs of individual patients and is designed to reduce inflammation, moderate symptoms, and maintain remission once achieved. Treatment usually begins with oral mesalamine or rectally administered (i.e., topical) mesalamine or glucocorticosteroids. The American College of Gastroenterology and the Toronto Consensus recommend that 5-aminosalicylate (5-ASA) preparations be used as initial treatment for patients with mild to moderate disease and for the prevention of relapse; in patients with disease confined to the rectosigmoid area, topical preparations may be useful 4.
The efficacy of these drugs has been demonstrated in randomized controlled trials. Most such studies, however, are placebo-controlled and do not involve active comparators; relatively little is therefore known about the comparative effectiveness of drugs that form the cornerstone of the treatment of ulcerative proctitis. Those few head-to-head clinical trials that have been conducted point to possible differences in effectiveness that may be important in clinical practice. For example, a small randomized trial of oral versus rectal mesalamine by Gionchetti and colleagues in 58 patients, aged >18 years, with active, histologically confirmed ulcerative proctitis, demonstrated the superiority of rectal drug administration, in terms of improvement in mean Disease Activity Index (DAI) score, as well as the rate of histologic remission 5. A similar trial by Kam and colleagues 6 reported equivalent efficacy for oral versus rectal administration of mesalamine in terms of the primary efficacy outcome (DAI score), but rectal administration reportedly was found to be superior on a number of secondary efficacy endpoints, such as both physician-rated and patient-rated global improvement. The percentage of patients experiencing adverse events also was higher in the oral mesalamine group. Another trial by Biddle and colleagues 7 found that the efficacy of oral and rectal mesalamine did not differ but reported that combined treatment was superior to either drug administered alone.
To shed light on this issue, Richter et al 2 undertook a retrospective study involving 548 patients with average age 47.3 years on the effectiveness of oral 5-aminosalicylate (5-ASA), mesalamine suppository, and mesalamine enema as initial therapy in patients newly presenting in clinical practice with ulcerative proctitis. Their findings confirm the relatively favorable natural history of distal colitis in a large community-based cohort of patients with newly presenting disease who were followed up for one year. There were few hospitalizations, and no one required surgery or was treated with a biological agent. Their results also confirm the observation that topical or rectal mesalamine may be superior to oral mesalamine 2. Although they measured treatment escalation rather than response to treatment, which is the more commonly studied outcome, it is a complementary endpoint 8. Treatment escalation in clinical practice represents the active judgment of the treating physician that prior treatment was unsatisfactory. Richter et al 2 could not determine if the treatment escalation was due to disease extension. In addition, it is a comparison of treatment options, rather than a comparison of a treatment to placebo, and addresses the relevant question of comparative effectiveness of treatments that practicing clinicians confront.
Radiation proctitis
Radiation proctitis or proctopathy is the radiation induced rectal mucosal injury, with an incidence rate varying from 5%–20% 9. Radiation proctitis is a common complication following radiation therapy of pelvic malignancies, like malignancies of prostate, cervix, uterus, bladder, testicles, rectum and lymphomas 10. Acute radiation proctitis occurs during or within three months of the radiotherapy treatment and are usually self limiting 11. Radiation proctitis is usually seen in about 13% of patients receiving radiotherapy, while 5-10% of patients develop chronic radiation proctitis 12. Chronic radiation proctitis either continues from the acute phase or begins after a latent period of at least 90 days. Chronic proctitis occurs generally in patients with severe acute proctitis and in those with predisposing conditions of diabetes mellitus, inflammatory bowel disease, hypertension, peripheral vascular disease, or even chemotherapy 11.
Radiation therapy leads to tissue changes including changes like loss of mucosa, endothelial swelling in the arterioles and subsequent fibrosis of connective tissue and arteriolar endarteritis 13. The management of radiation proctitis is extremely challenging as no recommended treatment guidelines are available. Treatment options include medical measures like anti-inflammatory agents (sulphasalazine, balsalazide, mesalazine), antioxidants, sucralfate, formalin, steroid enemas, sodium butyrate enemas, hyperbaric oxygen therapy, pentoxifylline, rebamipide enema therapy, oestrogen/ progesterone, sodium pentosan polysulphate and misoprostol 12.
Endoscopic therapies are considered as the treatment of choice in patients of chronic radition proctitis with troublesome bleeding 14. These may also be used along with medical therapies in treating the patients 15. The goal of endoscopic therapy, is the obliteration of telangiectasias, regardless of methodology 10. Options include contact methods, like the heater probe and bipolar electrocautery, and non-contact methods, such as laser therapy, argon plasma coagulation, radiofrequency ablation and cryotherapy 16. It appears, however, that non-contact methods are better in comparison to thermal contact methods of endoscopic treatment. The methods like heater probe and bipolar electrocautery have reported higher incidence of bleeding as a side effect of the treatment and they also require significantly longer sessions of the endoscopic treatment.
Now-a-days, argon plasma coagulation has rapidly become the preferred and first-line endoscopic therapy for haemorrhagic chronic radiation proctitis 16. Argon Plasma Coagulation uses inert argon gas as a conducting medium and bipolar diathermy current is delivered. Limited depth of coagulation (0.5-3mm), uniform and predictable application are some of the advantages seen with it’s use. The risks of perforation, stenosis and fistulisation are reduced. Another benefit is that, it can also be applied radially and axially, thus, allowing tangential coagulation of lesions 16. In addition, as argon plasma coagulation treatment is being delivered using the colonoscope, it can reach more proximally affected parts of the rectum 11.
It has been found that argon plasma coagulation has the potential to complement topical formalin application and can be used in combination to treat the proximal and distal rectum concurrently. This series has also found that all the patients failed initial conservative management for per rectal bleeding, and should thus be either offered empirical treatment at the time of diagnosis with formalin or argon plasma coagulation, or at least be followed up closely following a course of stool softeners and antibiotics such as metronidazole 11.
Most studies have shown benefit on using argon plasma coagulation for the management of chronic radiation proctitis. Improvement in rectal symptoms like tenesmus, diarrhoea has been noticed in 60%-75% of the cases. Argon plasma coagulation also alleviates rectal bleeding in 80%-90% of the cases [28]. Multiple treatment sessions are required in the diffuse lesions, usually ranging from one to five sessions 16.
Hortelano et al., have recently analysed the response of argon plasma coagulation in 30 patients of chronic radiation proctitis. Out of all, 77% patients demonstrated complete response while 16% patients revealed partial response. Transfusion was not required in any of the patients following therapy. Long-term (>6 weeks) grade 2 rectal ulceration and grade 2 rectal incontinence were seen in two patients 17.
Overall, the varied complication rates have been observed with the use of argon plasma coagulation. Overall morbidity was reported in 47%, post-treatment pain in 20% and severe complications (severe bleeding, extensive necrosis and perforation) in 10% of the patients 16. The commonest procedure-related complication observed is rectal or anal pain and it usually resolves spontaneously 16.. Rectal ulcers are common following argon plasma coagulation treatment. Therefore, recommendation is to give brief pulse treatment to the lesions 18. Occurrence of ulcers may be affected by the various factors, including the method of application, the time interval between the sessions of the treatment and the flow rate of the argon gas 19. Rare complications reported include urinary retention, necrosis and arteriovenous fistula 16. The occurrence of strictures is less common and varies among different studies, from 2%-13.3% 16.
Mesenchymal Stem Cells are isolated from bone marrow. They are the pluripotent progenitor cells and play an important role in the maintenance and regeneration of various connective tissues 20. Mesenchymal Stem Cells therapy is supposed to have role in extracellular matrix remodelling, proangiogenesis and inflammatory modulation. In a recent study by Linard et al. 20, on pigs, autologous MSCs (2 × 106 MSCs per kilogram in sterile phosphate-buffered saline) were given in the ear vein once a week on days 27, 34, and 41 postirradiation to assess the response in the radiation induced proctitis. In a pig model, repeated injections of mesenchymal stem cells have shown improvement in radiation induced fibrosis and inflammation. This therapy may be a light of hope to the patients suffering from severe proctitis and refractory to the nonsurgical interventions 20.
Fortunately, surgery is often a last resort to be used when severe complications occur, such as refractory bleeding, strictures leading to intestinal obstruction or sepsis. Surgery can range from a simple proximal diversion to a formal resection with or without an anastomosis 11. It is noteworthy that all the patients who underwent an anterior resection with proximal diversions ultimately had their stomas reversed and there were no leaks thereafter. Thus, when appropriately indicated, surgery can offer an effective solution 11.
Though, different options are available, exact utility and superiority of one line of treatment over other is yet to be found 14.
Stercoral proctitis
Stercoral proctitis is a rare life-threatening inflammatory process involving the rectal wall secondary to chronic constipation and fecal impaction with high morbidity 21 and 35-60% mortality 22; especially if complicated with ischemic colitis, stercoral ulcer formation and subsequent perforation 23. Stercoral colitis is defined as an inflammatory colitis that is caused by increased intraluminal pressure in the colon from the impacted feces and ischemic colitis is the condition that results when blood flow to the colon is reduced to a level insufficient to maintain cellular metabolic function.
Actual incidence and prevalence of the stercoral colitis and its complications are not known. The estimated post mortem incidence of stercoral ulcer ranges from 0.04% to 2.3%. Per the study published by Maurer et al. 24, stercoral perforation of the colon was found in 0.5% of all surgical colorectal procedures, 1.2% of all emergency colorectal procedures, and 3.2% of all colonic perforations. When stercoral colitis is associated with colonic perforation, a 35% mortality rate has been reported in the literature 25. However, decreased morbidity and mortality have been observed in patients who were diagnosed earlier and managed appropriately.
Chronic constipation has been described as a risk factor for stercoral proctitis / colitis and colonic ischemia 26. Typical risk factors are chronic constipation, age >60, female sex, NSAIDs 27, heroin addiction 28, antacids, steroids, amitriptyline, and other constipating agents 29. It has also been reported in patients receiving dialysis 29, patients on immunosuppressive therapy after kidney transplant 30, and those with spinal cord injury 31:1054–1058. https://www.ncbi.nlm.nih.gov/pubmed/7202964)). Perforation commonly occurs in the sigmoid colon (50%) and rectosigmoid junction (24%) 27. The diagnosis should be suspected in anyone with a history of constipation who presents with an acute abdomen. Typical pathologic findings include areas of ischemic necrosis surrounded by nonspecific inflammatory changes 32.
To date, less than 200 cases of stercoral colitis have been reported in the literature with a focus on the radiographic characteristics of stercoral colitis and management of abdominal perforation as a complication of colitis. Intestinal perforation and solitary stercoral ulcers are commonly reported complications of stercoral colitis 33. However, only a few cases of ischemic colitis that are complicated by stercoral colitis have been published so far 34. Only 3 case reports and 2 case series of localized ischemic colitis with lactic acidosis are reported in total 35. Extensive ischemic colitis involving right colon associated with stercoral colitis is only reported in one case report 36.
The mechanism by which fecal impaction and chronic constipation can lead to stercoral inflammation, ulceration, and subsequently perforation is proposed to be distention of the colonic lumen and increased pressure from dry desiccated fecal material (also called fecaloma) which, if left untreated may result in perforation and peritonitis 35. The mechanism by which stercoral proctitis / colitis leads to ischemia and colonic wall perforation is a result of increased intraluminal pressure from fecal impaction leading to ischemia of the bowel 23. Subsequently, ulceration may occur in perforation that can lead to severe hemodynamic compromise. Patients usually present with acute abdomen and are diagnosed by a CT scan of the abdomen and performing a colonoscopy. Diagnostic delay may lead to perforation and septic shock with a mortality rate as high as 60% 37.
Common locations for stercoral colitis are anterior rectum, anti-mesenteric border of the recto sigmoid junction, and the apex of the sigmoid colon which are described as the “watershed” area of the colon. The recto-sigmoid junction has a relatively low blood supply from and often inefficient or absent anastomosis between the branch of the inferior mesenteric artery and the branch of the superior rectal artery, referred to as Sudeck’s point. Therefore, these patients are at risk of ischemia, particularly related to hypoperfusion.
The usual presentation of stercoral colitis complicated with ischemic colitis is the colicky abdominal pain, which may be diffuse or localized in a patient with a history of chronic constipation. Patients can also be asymptomatic or can present with vague symptoms that could be confused with diverticulitis, a more common condition in elderly. Physical examination findings are consistent with tenderness on palpation with signs of focal or diffuse peritonitis. The CT scan findings of stercoral colitis include dilated sigmoid colon and/or rectum with subsequent thickening of the wall. This likely symbolizes edema caused by focal ischemia, necrosis and ulceration. Additionally, stranding of the peri-colonic fat in an area that shows fecal impaction suggests ischemic colitis or wall edema. While the presence of intramural or extra luminal air loculi, bubbles of gas, or an abscess, suggests colonic perforation. Endoscopic features of stercoral enterocolitis complicated with ischemic colitis include mucosal edema, erythema, ulceration and obstructing large fecolith at the angulation of sigmoid-descending colon junction as reported by Cohen et al. 38.
Non-operative management with bowel regimen, enemas, manual fecal disimpaction via per rectal examination or endoscopy considered standard of care. However, endoscopic guided disimpaction is considered the standard of care 39. Operative management is reserved for patient presenting with signs of peritonitis secondary to colonic wall perforation and includes surgical resection of the dilated colon. Hence, early diagnosis and treatment with bowel cleansing and fecal disimpaction are essential to avoid the fatal consequence of such condition.
Proctitis complications
Proctitis that isn’t treated or that doesn’t respond to treatment may lead to complications, including:
- Anemia. Chronic bleeding from your rectum can cause anemia. With anemia, you don’t have enough red blood cells to carry adequate oxygen to your tissues. Anemia causes you to feel tired, and you may also experience dizziness, shortness of breath, headache, pale skin and irritability.
- Ulcers. Chronic inflammation in the rectum can lead to open sores (ulcers) on the inside lining of the rectum.
- Fistulas. Sometimes ulcers extend completely through the intestinal wall, creating a fistula, an abnormal connection that can occur between different parts of your intestine, between your intestine and skin, or between your intestine and other organs, such as the bladder and vagina.
Proctitis causes
Several diseases and conditions can cause the lining of the rectum to become inflamed (proctitis). They include:
- Inflammatory bowel disease. About 30 percent of people with inflammatory bowel disease (Crohn’s disease or ulcerative colitis) have inflammation of the rectum.
- Infections. Sexually transmitted infections, spread particularly by people who engage in anal intercourse, can result in proctitis. Sexually transmitted infections that can cause proctitis include gonorrhea, genital herpes and chlamydia. Infectious proctitis is also associated with HIV. Infections associated with foodborne illness, such as salmonella, shigella and campylobacter infections, also can cause proctitis.
- Radiation therapy for cancer. Radiation therapy directed at your rectum or nearby areas, such as the prostate, can cause inflammation of the lining of your rectum. Radiation proctitis can begin during radiation treatment and last for a few months after treatment. Or it can occur years after treatment.
- Antibiotics. Sometimes antibiotics used to treat an infection can kill helpful bacteria in the bowels, allowing the harmful Clostridium difficile bacteria to grow in the rectum.
- Diversion proctitis. Proctitis can occur in people following some types of colon surgery in which the passage of stool is diverted from the rectum.
- Food protein-induced proctitis. This can occur in infants who drink either cow’s milk- or soy-based formula, and in those who are breastfed by mothers who eat dairy products.
- Eosinophilic proctitis. A form of proctitis caused by accumulation of a kind of white blood cell (eosinophil) in the lining of the rectum that affects only children younger than 2.
Risk factors for proctitis
Risk factors for proctitis include:
- Unsafe sex. Practices that increase your risk of a sexually transmitted infection (STI) can increase your risk of proctitis. Your risk of contracting an STI increases if you have multiple sex partners, don’t use condoms and have sex with a partner who has an STI.
- Inflammatory bowel diseases. Having an inflammatory bowel disease (ulcerative colitis or Crohn’s disease) increases your risk of proctitis.
- Radiation therapy for cancer. Radiation therapy directed at or near your rectum (such as for rectal, ovarian or prostate cancer) increases your risk of proctitis.
Proctitis prevention
To reduce your risk of proctitis, take steps to protect yourself from sexually transmitted infections (STIs). The surest way to prevent an STI is to abstain from sex, especially anal sex. If you choose to have sex, reduce your risk of an sexually transmitted infection by:
- Limiting your number of sex partners
- Using a latex condom during each sexual contact
- Not having sex with anyone who has any unusual sores or discharge in the genital area
If you’re diagnosed with a sexually transmitted infection, stop having sex until after you’ve completed treatment. That way you can avoid passing the infection to your partner. Ask your doctor when it’s safe to have sex again.
Proctitis symptoms
Proctitis signs and symptoms may include:
- A frequent or continuous feeling that you need to have a bowel movement
- Rectal bleeding
- The passing of mucus through your rectum
- Rectal pain
- Pain on the left side of your abdomen
- A feeling of fullness in your rectum
- Diarrhea
- Pain with bowel movements
Proctitis diagnosis
Tests and procedures used to diagnose proctitis include:
- Blood tests. These can detect blood loss or infections.
- Stool test. You may be asked to collect a stool sample for testing. A stool test may help determine if your proctitis is caused by a bacterial infection.
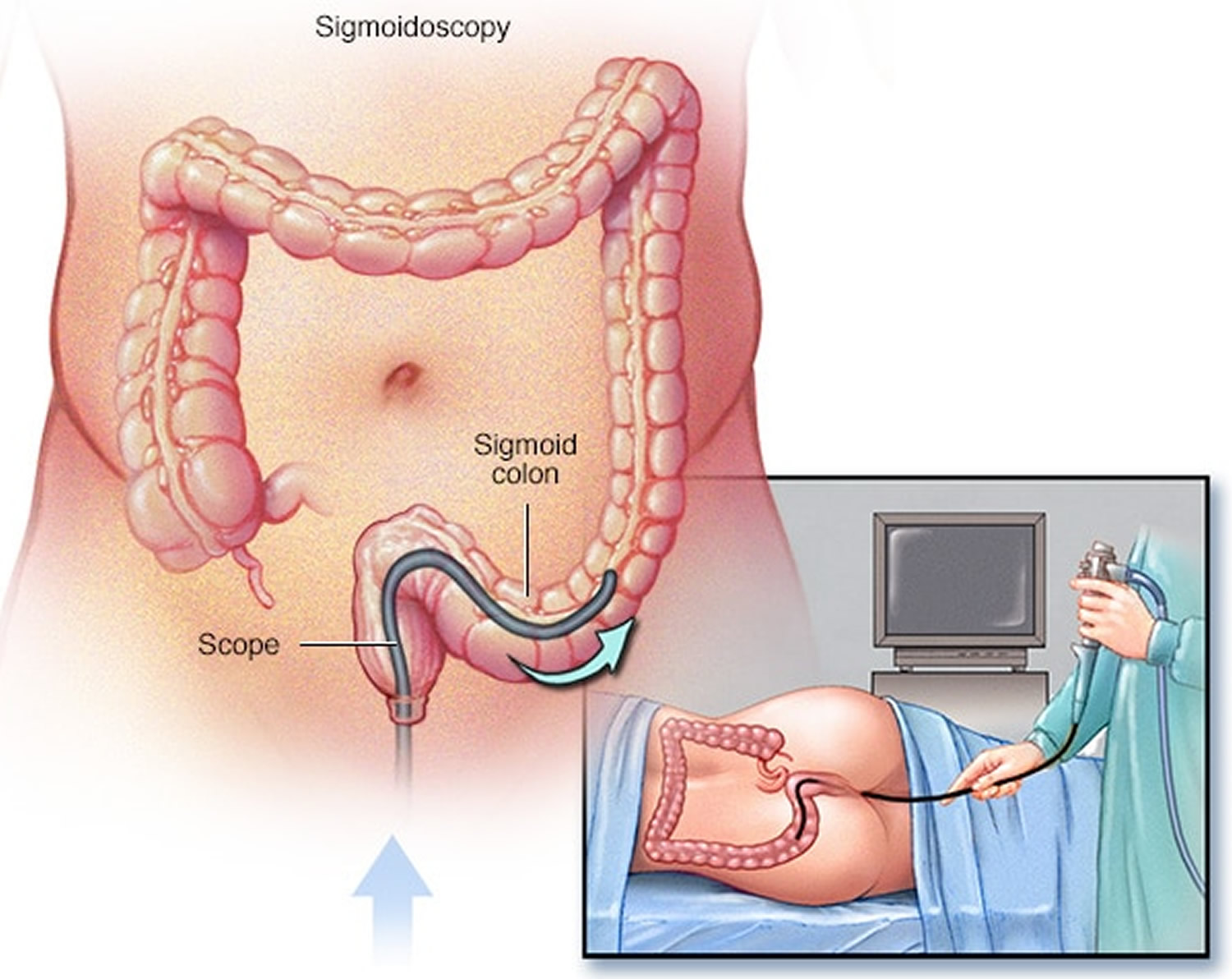
- Scope exam of the final portion of your colon. During a flexible sigmoidoscopy, your doctor uses a slender, flexible, lighted tube to examine the sigmoid, the last part of your colon — including the rectum. During the procedure, your doctor can also take small samples of tissue (biopsy) for laboratory analysis.
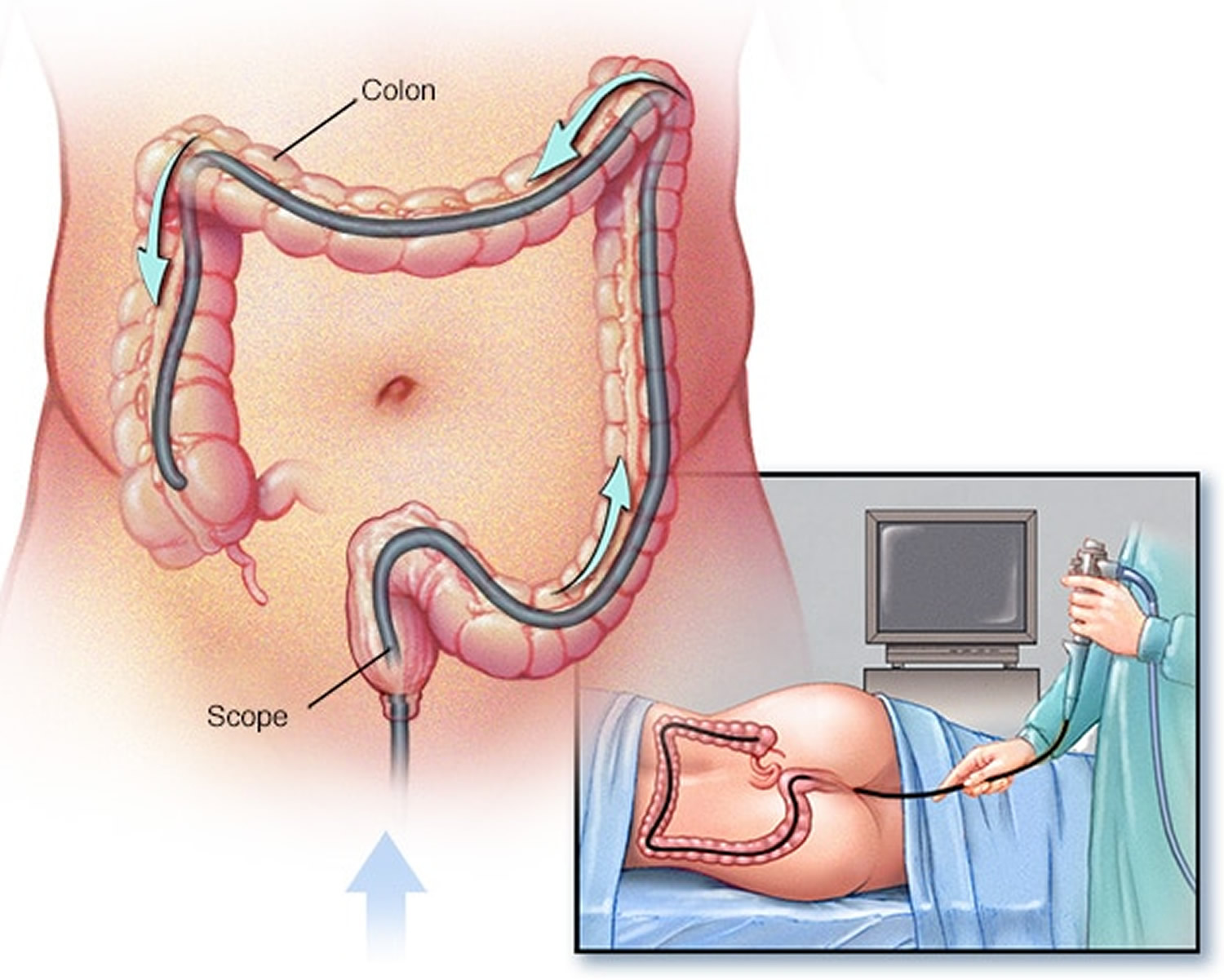
- Scope exam of your entire colon. A colonoscopy allows your doctor to view your entire colon using a thin, flexible, lighted tube with an attached camera. Your doctor can also take a biopsy during this test.
- Testing for sexually transmitted infections. This involves obtaining a sample of discharge from your rectum or from the tube that drains urine from your bladder (urethra). If the cause of your proctitis is likely to be an sexually transmitted infection, your doctor may insert a narrow swab into the end of your urethra or anus to obtain the sample, which is then tested for the presence of bacteria or other infectious organisms. The results can be used to select the most effective treatment.
Figure 4. Flexible sigmoidoscopy
Figure 5. Colonoscopy
Proctitis treatment
Treatment for proctitis depends on the underlying cause of the inflammation.
Treatment for proctitis caused by an infection
Your doctor may recommend medications to treat your infection. Options may include:
- Antibiotics. For proctitis caused by bacterial infections, your doctor may recommend an antibiotic, such as doxycycline (Periostat, Vibramycin).
- Antivirals. For proctitis caused by viral infections, such as the sexually transmitted virus herpes, your doctor may prescribe an antiviral medication, such as acyclovir (Sitavig, Zovirax, others).
Treatment for proctitis caused by radiation therapy
Mild cases of radiation proctitis may not require treatment. In other cases, radiation proctitis can cause severe pain and bleeding that requires treatment. Your doctor may recommend treatments such as:
- Medications. Medications are given in pill, suppository or enema form. They include sucralfate (Carafate), mesalamine (Asacol, Canasa, others) and sulfasalazine (Azulfidine), and metronidazole (Flagyl). These medications can help control inflammation and reduce bleeding.
- Stool softeners and dilation. These can help open up obstructions in the bowel.
- Treatment to destroy damaged tissue. These techniques improve proctitis symptoms by destroying abnormal tissue (ablation) that is bleeding. Ablation procedures used to treat proctitis include argon plasma coagulation (APC), electrocoagulation and other therapies.
Proctitis caused by inflammatory bowel disease
Treatment of proctitis related to Crohn’s disease or ulcerative colitis is aimed at reducing the inflammation in your rectum. Treatment may include:
- Medications to control rectal inflammation. Your doctor may prescribe anti-inflammatory medications, either by mouth or as a suppository or enema — such as mesalamine (Asacol, Canasa, others) — or corticosteroids — such as prednisone (Rayos) or budesonide (Entocort EC, Uceris). Inflammation in people with Crohn’s disease often requires treatment with a medication that suppresses the immune system, such as azathioprine (Azasan, Imuran) or infliximab (Remicade).
- Surgery. If drug therapy doesn’t relieve your signs and symptoms, your doctor may recommend surgery to remove a damaged portion of your digestive tract.
Home remedies
For temporary relief of mild pain and inflammation, try the following self-care measures:
- Ask your doctor before using over-the-counter (OTC) diarrhea medicines. Don’t take OTC anti-diarrhea drugs, such as loperamide (Imodium A-D), without your doctor’s OK.
- Avoid food just before bedtime. Eating just before going to bed may stimulate your digestive system and cause you to have bowel movements and discomfort at night.
- Take over-the-counter pain relievers. Acetaminophen (Tylenol, others) may be helpful, but ask your doctor before taking aspirin or ibuprofen (Advil, Motrin IB, others), as in some cases these may make your proctitis worse.
- Use a sitz bath with warm water. A sitz bath fits over the toilet. You can get one at a medical supply store or some pharmacies. This may provide some comfort if you experience anal inflammation.
Ulcerative proctitis diet
Temporarily eating a low-residue or low-fiber diet can sometimes help improve symptoms of ulcerative colitis during a flare-up. These diets are designed to reduce the amount and frequency of the stools you pass.
Examples of foods that can be eaten as part of a low-residue diet include:
- white bread
- refined (non-wholegrain) breakfast cereals, such as cornflakes
- white rice, refined pasta and noodles
- cooked vegetables (but not the peel, seeds or stalks)
- lean meat and fish
- eggs
If you’re considering trying a low-residue diet, make sure you talk to your care team first.
Other dietary measures
- Eat small meals. You may find you feel better eating five or six small meals a day rather than two or three larger ones.
- Drink plenty of liquids. Try to drink plenty of fluids daily. Water is best. Alcohol and beverages that contain caffeine stimulate your intestines and can make diarrhea worse, while carbonated drinks frequently produce gas.
- Talk to a dietitian. If you begin to lose weight or your diet has become very limited, talk to a registered dietitian.
In studies involving people with chronic inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis, the anti-Inflammatory diet (IBD-AID) has been used as an adjunct dietary therapy for the treatment of inflammatory bowel diseases (IBD) 40. The goal of the anti-Inflammatory diet (IBD-AID) is to assist with a decreased frequency and severity of flares, obtain and maintain remission in people with inflammatory bowel diseases (IBD). Dysbiosis, or altered bacterial flora, is one of the theories behind the development of anti-Inflammatory diet (IBD-AID), in that certain carbohydrates in the lumen of the gut provide pathogenic bacteria a substrate on which to proliferate 41, 42.
The anti-Inflammatory diet (IBD-AID) has five basic components:
- The first of which is the modification of certain carbohydrates, (including lactose, and refined or processed complex carbohydrates)
- The second places strong emphasis on the ingestion of pre- and probiotics (e.g.; soluble fiber, leeks, onions, and fermented foods) to help restore the balance of the intestinal flora 43, 44, 45
- The third distinguishes between saturated, trans, mono- and polyunsaturated fats 46, 47,
- The fourth encourages a review of the overall dietary pattern, detection of missing nutrients, and identification of intolerances.
- The last component modifies the textures of the foods (e.g.; blenderized, ground, or cooked) as needed (per patient symptomology) to improve absorption of nutrients and minimize intact fiber.
The phases indicated in Table 1 are examples of the modification of texture complexity, so that dietitian and patient can expand the diet as the patient’s tolerance and absorption improves. Some sensitivities common to many patients (not just those with IBD), are eased through supplementation of digestive enzymes or avoidance. A senior dietitian advised the patient and either family or spouse regarding the details of the diet during regular clinic visits. Patients taking supplements (probiotics, vitamin/minerals, omega-3 fatty acids) were advised to continue or discontinue, depending on the needs of the individual and the dietary intake 48.
The anti-Inflammatory diet (IBD-AID) consists of lean meats, poultry, fish, omega-3, eggs, particular sources of carbohydrate, select fruits and vegetables, nut and legume flours, limited aged cheeses (made with active cultures and enzymes), fresh cultured yogurt, kefir, miso and other cultured products (rich with certain probiotics) and honey. Prebiotics, in the form of soluble fiber (containing beta-glucans and inulin, such as bananas, oats, blended chicory root, and flax meal) are suggested. In addition, the patient is advised to begin at a texture phase of the diet matching with symptomology, starting with phase one if in an active flare. Many patients require foods to be softened and textures mechanically altered by pureeing the foods, and avoiding foods with stems and seeds when starting the diet (see phases 1–3 of Table 1), as intact fiber can be problematic for those with strictures and highly active mucosal inflammation. Some patients will require lifelong avoidance of intact fiber. Food irritants are not limited to intact fiber, but may include certain foods, processing agents and flavorings to which IBD patients may be reactive.
Table 1. The Anti-Inflammatory Diet (IBD-AID) Food Phase chart
| Phase type | Phase I | Phase II | Phase III | Phase IV |
|---|---|---|---|---|
| Soft, well-cooked or cooked then pureed foods, no seeds | Soft Textures: well-cooked or pureed foods, no seeds, choose floppy or tender foods | May still need to avoid stems, choose floppy greens or other greens depending on individual tolerance | If in remission with no strictures | |
| Vegetables | Butternut Squash, Pumpkin, Sweet Potatoes, Onions | Carrots, Zucchini, Eggplant, Peas, Snow peas, Spaghetti squash, Green beans, Yellow beans, Microgreens (2 week old baby greens), Watercress, Arugula, Fresh flat leaf parsley and cilantro, Seaweed, Algae | Butter lettuce, Baby spinach, Peeled cucumber, Olives, Leeks Bok Choy, Bamboo shoots, Collard greens, Beet greens, Sweet peppers, Kale, Fennel bulb | Artichokes, Asparagus, Tomatoes, Lettuce, Brussels sprouts, Beets, Cabbage, Kohlrabi, Rhubarb, Pickles, Spring onions, Water chestnuts, Celery, Celeriac, Cauliflower, Broccoli, Radish, Green pepper, Hot pepper |
| Pureed vegetables: Mushrooms, Phase II vegetables (pureed) | Pureed vegetables: all except cruciferous | Pureed vegetables: all from Phase IV, Kimchi | ||
| Fruits | Banana, Papaya, Avocado, Pawpaw | Watermelon (seedless), Mangoes, Honeydew, Cantaloupe, May need to be cooked: Peaches, Plums, Nectarines, Pears, (Phase III fruits are allowed if pureed and seeds are strained out) | Strawberries, Cranberries, Blueberries, Apricots, Cherries, Coconut, Lemons, Limes, Kiwi, Passion fruit, Blackberries, Raspberries, Pomegranate (May need to strain seeds from berries) | Grapes, Grapefruit, Oranges, Currants, Figs, Dates, Apples (best cooked), Pineapple, Prunes |
| Meats and fish | All fish (no bones), Sardines (small bones ok), Turkey and ground beef, Chicken, Eggs | Scallops | Lean cuts of Beef, Lamb, Duck, Goose | Shrimp, Prawns, Lobster |
| Non dairy unsweetened | Coconut milk, Almond milk, Oat milk, Soy milk | |||
| Dairy, unsweetened | Yogurt, Kefir | Farmers cheese (dry curd cottage cheese), Cheddar cheese | Aged cheeses | |
| Nuts/Oils/Legumes/Fats | Miso (refrigerated), Tofu, Olive oil, Canola oil, Flax oil, Hemp oil, Walnut oil, Coconut oil | Almond flour, Peanut flour, Soy flour, Sesame oil, Grapeseed oil, Walnut oil, Pureed nuts, Safflower oil, Sunflower oil | Whole nuts, Soybeans, Bean flours, Nut butters, Well-cooked lentils (pureed), Bean purees (e.g. hummus) | Whole beans and lentils |
| Grains | Ground flax or Chia Seeds (as tolerated) | Steel cut oats (well-cooked as oatmeal) | Rolled well-cooked oats | |
| Spices | Basil, Sage, Oregano, Salt, Nutmeg, Cumin, Cinnamon, Turmeric, Saffron, Mint, Bay leaves, Tamari (wheat free soy sauce), Fenugreek tea, Fennel tea, Vanilla | Dill, Thyme, Rosemary Tarragon, Cilantro, Basil, Parsley | Mint, Ginger, Garlic (minced), Paprika, Chives, Daikon, Mustard | Wasabi, Tamarind, Horseradish, Fenugreek, Fennel |
| Sweeteners | Stevia, Maple syrup, Honey (local), Unsweetened fruit juice | Lemon and lime juice | ||
| Misc. | Capsule or liquid supplements, Cocoa powder | Baking powder (no cornstarch), Baking soda, Unflavored gelatin | Ghee, Light mayonnaise, Vinegar | Ketchup (sugar free), Hot sauce (sugar free) |
- Bello C., Belaiche J., Louis E., Reenaers C. Evolution and predictive factors of relapse in ulcerative colitis patients treated with mesalazine after a first course of corticosteroids. Journal of Crohn’s and Colitis. 2011;5(3):196–202. doi: 10.1016/j.crohns.2010.12.011. https://www.ncbi.nlm.nih.gov/pubmed/21575881[↩]
- Richter JM, Arshi NK, Oster G. Oral 5-Aminosalicylate, Mesalamine Suppository, and Mesalamine Enema as Initial Therapy for Ulcerative Proctitis in Clinical Practice with Quality of Care Implications. Canadian Journal of Gastroenterology & Hepatology. 2016;2016:6928710. doi:10.1155/2016/6928710. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4904649/[↩][↩][↩][↩]
- Kornbluth A., Sachar D. B., Practice Parameters Committee of the American College of Gastroenterology Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. The American Journal of Gastroenterology. 2010;105(3):501–523. doi: 10.1038/ajg.2009.727. https://www.ncbi.nlm.nih.gov/pubmed/20068560[↩]
- Kornbluth A., Sachar D. B., Practice Parameters Committee of the American College of Gastroenterology Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. The American Journal of Gastroenterology. 2010;105(3):501–523. doi: 10.1038/ajg.2009.727 https://www.ncbi.nlm.nih.gov/pubmed/20068560[↩]
- Gionchetti P., Rizzello F., Venturi A., et al. Comparison of oral with rectal mesalazine in the treatment of ulcerative proctitis. Diseases of the Colon and Rectum. 1998;41(1):93–97. doi: 10.1007/bf02236902. https://www.ncbi.nlm.nih.gov/pubmed/9510317[↩]
- Kam L., Cohen H., Dooley C., Rubin P., Orchard J. A comparison of mesalamine suspension enema and oral sulfasalazine for treatment of active distal ulcerative colitis in adults. American Journal of Gastroenterology. 1996;91(7):1338–1342. https://www.ncbi.nlm.nih.gov/pubmed/8677990[↩]
- Biddle W. L., Greenberger N. J., Swan J. T., McPhee M. S., Miner P. B., Jr. 5-Aminosalicylic acid enemas: effective agent in maintaining remission in left-sided ulcerative colitis. Gastroenterology. 1988;94(4):1075–1079. https://www.ncbi.nlm.nih.gov/pubmed/3278942[↩]
- Cohen R. D., Woseth D. M., Thisted R. A., Hanauer S. B. A meta-analysis and overview of the literature on treatment options for left-sided ulcerative colitis and ulcerative proctitis. American Journal of Gastroenterology. 2000;95(5):1263–1276. doi: 10.1016/S0002-9270(00)00732-2 https://www.ncbi.nlm.nih.gov/pubmed/10811338[↩]
- Wong MTC, Lim JF, Ho KS, Ooi BS, Tang CL, Eu KW. Radiation proctitis: a decade’s experience. Singapore Med J. 2010;51(4):315–19 https://www.ncbi.nlm.nih.gov/pubmed/20505910[↩]
- Hong JJ, Park W, Ehrenpreis ED. Review article: current therapeutic options for radiation proctopathy. Aliment Pharmacol Ther. 2001;15(9):1253–52. https://www.ncbi.nlm.nih.gov/pubmed/11552895[↩][↩]
- Wong MTC, Lim JF, Ho KS, Ooi BS, Tang CL, Eu KW. Radiation proctitis: a decade’s experience. Singapore Med J. 2010;51(4):315–19. https://www.ncbi.nlm.nih.gov/pubmed/20505910[↩][↩][↩][↩][↩][↩]
- Linard C, Busson E, Holler V, Strup-Perrot C, Lacave-Lapalun JV, Lhomme B, et al. Repeated autologous bone marrow derived mesenchymal stem cell injections improve radiation-induced proctitis in pigs. Stem Cells. Transl Med. 2013;2(11):916–27 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3808206/[↩][↩]
- Radiation-induced proctosigmoiditis (editorial) Lancet. 1983;1:1082–83. https://www.ncbi.nlm.nih.gov/pubmed/6133109[↩]
- Bansal N, Soni A, Kaur P, Chauhan AK, Kaushal V. Exploring the Management of Radiation Proctitis in Current Clinical Practice. Journal of Clinical and Diagnostic Research : JCDR. 2016;10(6):XE01-XE06. doi:10.7860/JCDR/2016/17524.7906. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4963751/[↩][↩]
- Shadad AK, Sullivan FJ, Martin JD, Egan LJ. Gastrointestinal radiation injury: Prevention and treatment. World J Gastroenterol. 2013;19(2):199–98. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3547575/[↩]
- Rustagi T, Mashimo H. Endoscopic management of chronic radiation proctitis. World J Gastroenterol. 2011;17(41):4554–62 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3225092/[↩][↩][↩][↩][↩][↩][↩][↩]
- Hortelano E, Gómez-Iturriaga A, Ortiz-de-Zárate R, Zaballa M, Barturen Á, Casquero F, et al. Is argon plasma coagulation an effective and safe treatment option for patients with chronic radiation proctitisafter high doses of radiotherapy? Rev Esp Enferm Dig. 2014;106(3):165–70 https://www.ncbi.nlm.nih.gov/pubmed/25007015[↩]
- Villavicencio RT, Rex DK, Rahmani E. Efficacy and complications of argon plasma coagulation for hematochezia related to radiation proctopathy. Gastrointest Endosc. 2002;55:70–74 https://www.ncbi.nlm.nih.gov/pubmed/11756918[↩]
- Ravizza D, Fiori G, Trovato C, Crosta C. Frequency and outcomes of rectal ulcers during argon plasma coagulation for chronic radiation-induced proctopathy. Gastrointest Endosc. 2003;57:519–25. https://www.ncbi.nlm.nih.gov/pubmed/12665762[↩]
- Linard C, Busson E, Holler V, Strup-Perrot C, Lacave-Lapalun JV, Lhomme B, et al. Repeated autologous bone marrow derived mesenchymal stem cell injections improve radiation-induced proctitis in pigs. Stem Cells. Transl Med. 2013;2(11):916–27. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3808206/[↩][↩][↩]
- Stercoral colitis leading to fatal peritonitis: CT findings. Heffernan C, Pachter HL, Megibow AJ, Macari M. AJR Am J Roentgenol. 2005 Apr; 184(4):1189-93. https://www.ncbi.nlm.nih.gov/pubmed/15788592/[↩]
- Mouchli MA, Meehan AM. Stercoral Ulcer-Associated Perforation and Chemotherapy. Case Reports in Oncology. 2017;10(2):442-446. doi:10.1159/000475756. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5597916/[↩]
- Naseer M, Gandhi J, Chams N, Kulairi Z. Stercoral colitis complicated with ischemic colitis: a double-edge sword. BMC Gastroenterology. 2017;17:129. doi:10.1186/s12876-017-0686-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5704496/[↩][↩]
- Maurer CA, Renzulli P, Mazzucchelli L, Egger B, Seiler CA, Büchler MW. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Dis Colon rectum. 2000;43:991–8. https://www.ncbi.nlm.nih.gov/pubmed/10910249[↩]
- SP R, Horton KM, Fishman EK. MDCT and CT angiography evaluation of rectal bleeding: the role of volume visualization. AJR Am J Roentgenol. 2013;201(3):589–597. doi: 10.2214/AJR.12.10357. https://www.ncbi.nlm.nih.gov/pubmed/23971451[↩]
- Saksonov M, Bachar GN, Morgenstern S, Zeina A-R, et al. Stercoral colitis: a lethal disease computed Tomographic findings and clinical characteristic. J Comput Assist Tomogr. 2014;38:721–726. doi: 10.1097/RCT.0000000000000117. https://www.ncbi.nlm.nih.gov/pubmed/24887575[↩]
- Chakravartty S, Chang A, Nunoo-Mensah J. A systematic review of stercoral perforation. Colorectal Dis. 2013;15:930–935 https://www.ncbi.nlm.nih.gov/pubmed/23331762[↩][↩]
- Tessier DJ, et al. Stercoral perforation of the colon in a heroin addict. Int J Colorectal Dis. 2002;17:435–437 https://www.ncbi.nlm.nih.gov/pubmed/12355222[↩]
- Velitchkov N, et al. Stercoral perforation of the normal colon: report of five cases. Sao Paulo Med J. 1996;114:1317–1323 https://www.ncbi.nlm.nih.gov/pubmed/9269107[↩][↩]
- Aguilo JJ, et al. Intestinal perforation due to fecal impaction after renal transplantation. J Urol. 1976;116:153–155 https://www.ncbi.nlm.nih.gov/pubmed/781315[↩]
- Gekas P, Schuster MM. Stercoral perforation of the colon: case report and review of the literature. Gastroenterology. 1981;80((Pt 1[↩]
- Maurer CA, et al. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Dis Colon Rectum. 2000;43:991–998 https://www.ncbi.nlm.nih.gov/pubmed/10910249[↩]
- Hudson J, Malik A. A fatal faecaloma stercoral colitis: a rare complication of chronic constipation. BMJ Case Rep. 2015. doi:10.1136/bcr-2015-211732. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4567767/[↩]
- Heffernan C, Leon Pachter H, Megibow AJ, Macari M. Stercoral colitis leading to fatal peritonitis: CT findings. AJR Am J Roentgenol. 2005;184:1189–1193. doi: 10.2214/ajr.184.4.01841189 https://www.ncbi.nlm.nih.gov/pubmed/15788592[↩]
- Canders CP, Shing R, Rouhani A. Stercoral Colitis in Two Young Psychiatric Patients Presenting with Abdominal Pain. J Emerg Med. 2015;49(4):e99–e103. doi:10.1016/j.jemermed.2015.04.026. Epub 2015 Jul 3. https://www.ncbi.nlm.nih.gov/pubmed/26145886[↩][↩]
- Mesurolle B, Milne C, Mignon F, Loutfi A, Roy A. What is your diagnosis? Severe ischemic colitis with extensive ischemic necrosis of the right colon with perforation and stercoral peritonitis. J Radiol. 2004;85(7–8):1077–1079. doi: 10.1016/S0221-0363(04)97724-4. https://www.ncbi.nlm.nih.gov/pubmed/15332014[↩]
- Hsiao TF, Chou YH. Stercoral perforation of colon: a rare but important mimicker of acute appendicitis. Am J Emerg Med. 2010;28(1):112.e1–112.e2. doi: 10.1016/j.ajem.2009.02.024. https://www.ncbi.nlm.nih.gov/pubmed/20006219[↩]
- Cohen S, Ascunce G, Kasmin F, Carr-Locke D. Endoscopic diagnosis and treatment of Stercoral colitis. Pract Gastroenterol. 2012;35(11):48–51.[↩]
- Mohamed AM, Caines A, Mohamed MM, Mumtaz S, Khan O. A complicated case of constipation. J Clin Med Case Rep. 2016;2(11):1–7.[↩]
- Olendzki BC, Silverstein TD, Persuitte GM, Ma Y, Baldwin KR, Cave D. An anti-inflammatory diet as treatment for inflammatory bowel disease: a case series report . Nutrition Journal. 2014;13:5. doi:10.1186/1475-2891-13-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3896778/[↩][↩]
- Vermeire S, Schreiber S, Sandborn WJ, Dubois C, Rutgeerts P. Correlation between the Crohn’s disease activity and Harvey-Bradshaw indices in assessing Crohn’s disease severity. Clin Gastroenterol Hepatol. 2010;8:357–363. doi: 10.1016/j.cgh.2010.01.001. https://www.ncbi.nlm.nih.gov/pubmed/20096379[↩]
- Bosscher D, Breynaert A, Pieters L, Hermans N. Food-based strategies to modulate the composition of the intestinal microbiota and their associated health effects. J Physiol Pharmacol. 2009;60(Suppl 6):5–11. https://www.ncbi.nlm.nih.gov/pubmed/20224145[↩]
- Jia W, Whitehead RN, Griffiths L, et al. Is the abundance of Faecalibacterium prausnitzii relevant to Crohn’s disease? Ross F, ed. Fems Microbiology Letters. 2010;310(2):138-144. doi:10.1111/j.1574-6968.2010.02057.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2962807/[↩]
- McFarland LV. Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World Journal of Gastroenterology : WJG. 2010;16(18):2202-2222. doi:10.3748/wjg.v16.i18.2202. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2868213/[↩]
- Lorea Baroja M, Kirjavainen PV, Hekmat S, Reid G. Anti-inflammatory effects of probiotic yogurt in inflammatory bowel disease patients. Clinical and Experimental Immunology. 2007;149(3):470-479. doi:10.1111/j.1365-2249.2007.03434.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2219330/[↩]
- Hou JK, Abraham B, El-Serag H. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol. 2011;106:563–573. doi: 10.1038/ajg.2011.44. https://www.ncbi.nlm.nih.gov/pubmed/21468064[↩]
- Wall R, Ross RP, Fitzgerald GF, Stanton C. Fatty acids from fish: the anti-inflammatory potential of long-chain omega-3 fatty acids. Nutrition reviews. 2010;68:280–289. doi: 10.1111/j.1753-4887.2010.00287.x. https://www.ncbi.nlm.nih.gov/pubmed/20500789[↩]
- Olendzki BC, Silverstein TD, Persuitte GM, Ma Y, Baldwin KR, Cave D. An anti-inflammatory diet as treatment for inflammatory bowel disease: a case series report. Nutrition Journal. 2014;13:5. doi:10.1186/1475-2891-13-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3896778/[↩]