Contents
- What is seborrheic keratosis
What is seborrheic keratosis
Seborrheic keratoses are common benign (noncancerous) wart-like growths of unknown cause seen in adults due to a thickening of an area of the top skin layer. A seborrheic keratosis usually looks like a waxy or wart-like growth. It typically appears on the face, chest, shoulders or back of the body. You may develop a single growth or cluster of them. Although seborrheic keratosis can occur anytime after puberty, almost everyone over 50 has one or more of these and they increase in number with age. Some families have an inherited tendency to grow multiple seborrheic keratosis. Men and women are equally as likely to develop seborrheic keratoses. Dark-skinned people are less affected than those with light skin; a variant seen in people with dark skin is called dermatosis papulosa nigra.
Seborrheic keratosis do not go away. Seborrheic keratosis do not turn into cancers, but some cancers resemble seborrheic keratosis.
No treatment is needed unless there is irritation from clothing with itching or bleeding.
The name seborrheic keratosis is misleading, because they are not limited to a seborrhoeic distribution (scalp, mid-face, chest, upper back) as in seborrhoeic dermatitis, nor are they formed from sebaceous glands, as is the case with sebaceous hyperplasia, nor are they associated with sebum — which is greasy.
Seborrhoeic keratoses are considered degenerative in nature. As time goes by, seborrhoeic keratoses become more numerous. Some people inherit a tendency to develop a very large number of them.
- There is no way to prevent new spots from forming.
- Some lotions with alpha hydroxyl acids may make the areas feel smoother with regular use but will not eliminate them.
- Over-the-counter (OTC) freezing techniques are available but usually not effective.
Seborrheic keratosis can be removed if you don’t want them, but removal is considered a cosmetic issue. Removal can be accomplished with freezing (cryosurgery), scraping (curettage), burning (electrocautery), lasers, or with acids. The doctor might conduct a biopsy if the growth looks unusual.
Figure 1. Seborrheic keratosis scalp
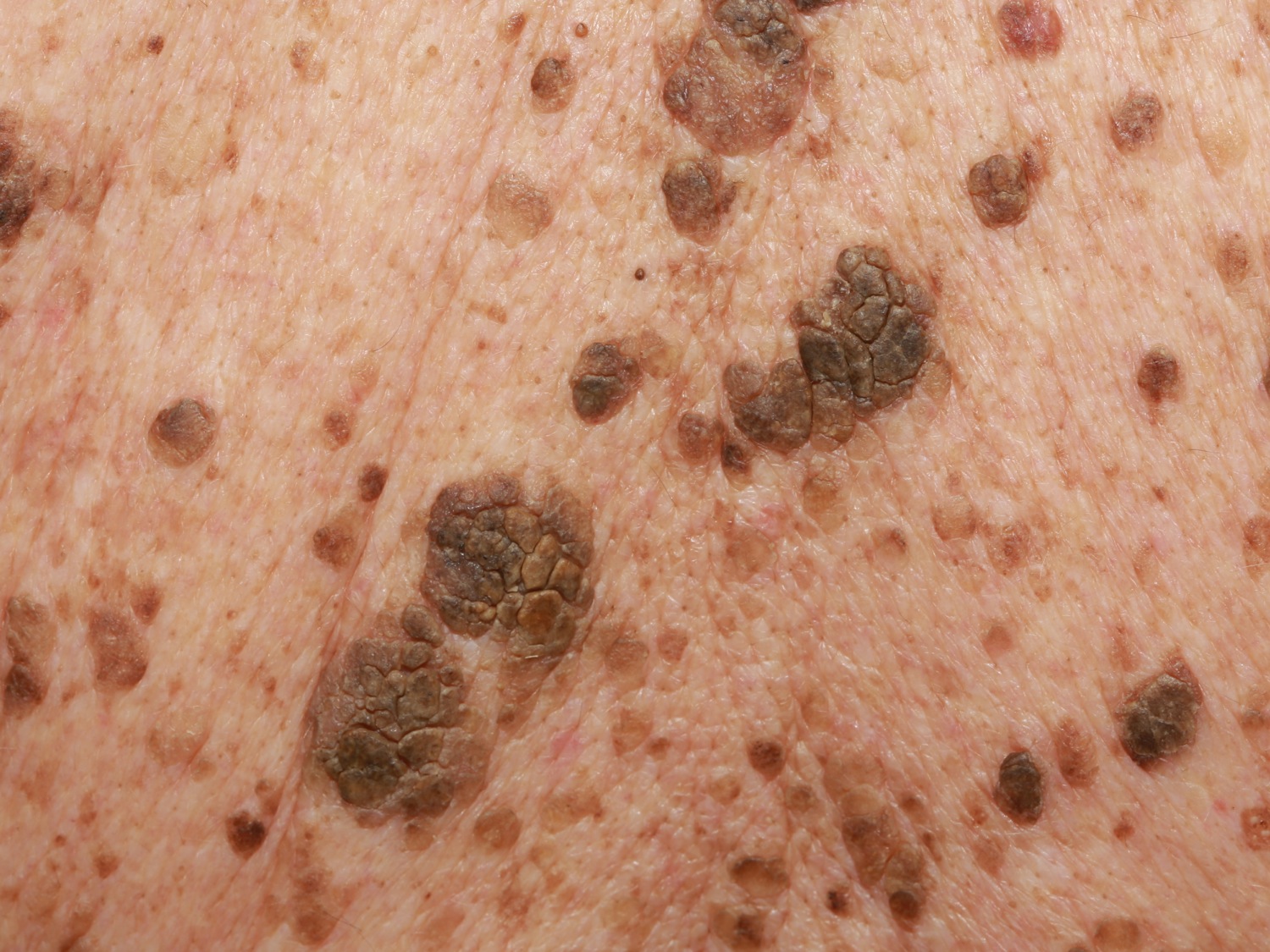
Figure 2. Seborrheic keratosis
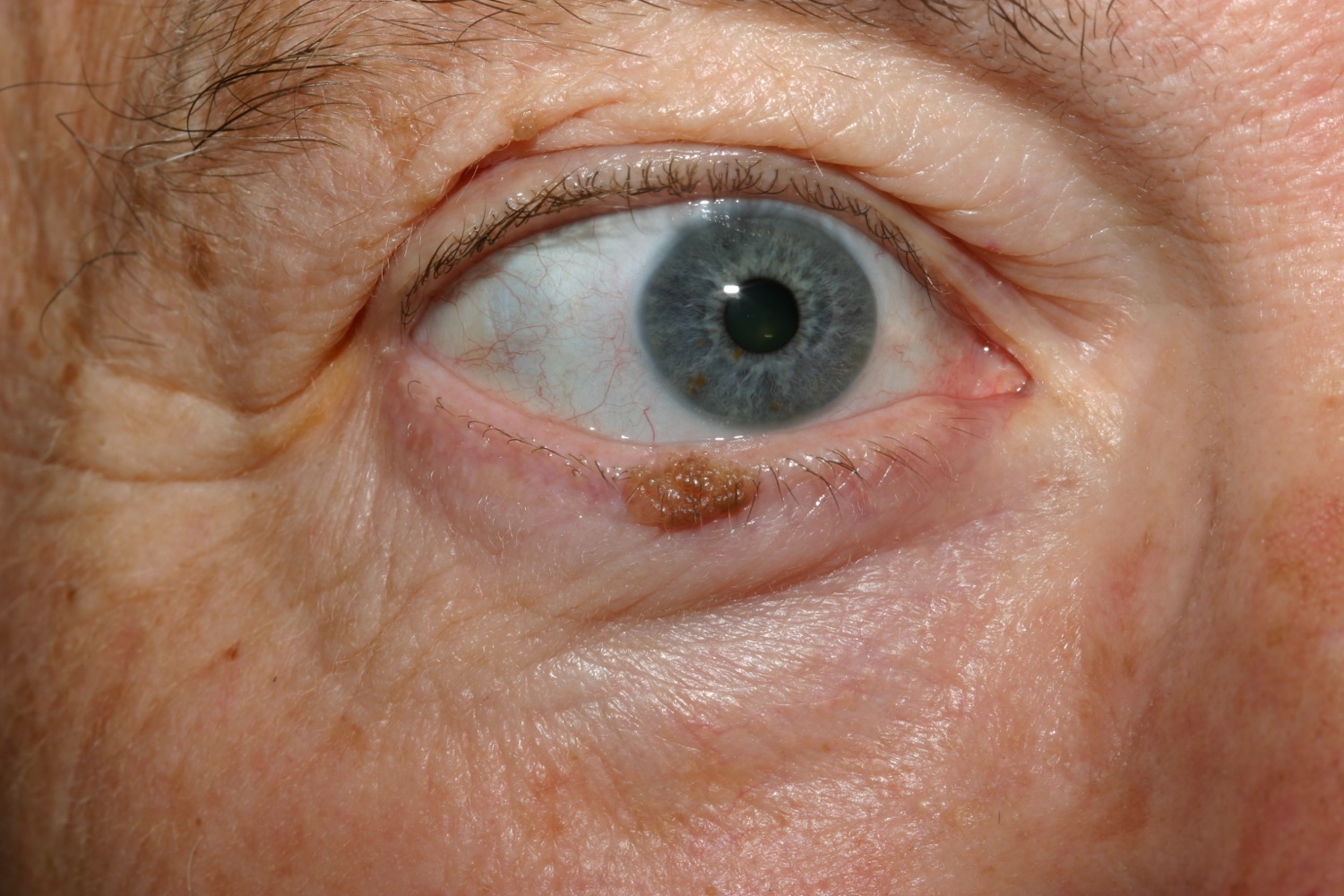
Figure 3. Irritated seborrheic keratosis
If a spot on the skin is growing, bleeding, painful, or itchy, see your doctor. Your doctor will need to examine it for skin cancer.
- A change in the appearance of the skin growth
- New growths
- A growth that looks like a seborrheic keratosis, but occurs by itself or has ragged borders and irregular color.
Seborrheic keratosis vs melanoma
Melanoma is a cancer that arises in pigment cells of the skin (melanocytes). Melanoma is the least common of the skin cancers, but it is the most serious. Melanoma can be life threatening if it spreads (metastasizes) to other parts of the body. The frequency of diagnosis of melanoma has been increasing in recent years, faster than any other cancer.
Melanoma starts in the color-producing cells (melanocytes) of the skin and may develop in an existing mole or may occur as a new mole. Early diagnosis and treatment can lead to a complete cure, while advanced forms are likely to have a poor outcome. Advanced melanoma can spread to lymph nodes as well as other areas in the body, typically the lungs, liver, and brain.
Figure 4. Melanoma
Melanoma usually occurs on areas of the skin that are exposed to the sun, but it may be found anywhere on the body, including the eye, mouth, and genital area.
- Men are most likely to develop melanoma on the head, neck, and trunk.
- Women are most likely to develop melanoma on the legs and arms.
A helpful tool to help you identify a mole that may be melanoma is the ABCDE checklist:
- A – Asymmetry: One half of the mole does not look like the other half.
- B – Border: The outline of the mole is irregular.
- C – Color: More than one color can be seen, such as brown, black, red, blue, and white.
- D – Diameter: A mole larger than 6 mm (1/4 inch), which is roughly the size of a pencil eraser.
- E – Evolving: Changes in the mole over time.
You have an increased risk of developing melanoma if you have:
- A family history of melanoma – Having someone in your family with melanoma increases your risk tenfold.
- Fair skin, light eyes, and a tendency to freckle – The risk of getting melanoma is 1 in 50 for whites, 1 in 200 for Hispanics, and 1 in 1,000 for people of African descent.
- A large number of moles, especially unusual appearing moles.
- History of frequent sun exposure, especially in childhood.
- History of sunburns.
- Decreased immune system, such as transplant patients and patients with HIV/AIDS.
Melanoma may be seen at any age, but it is most often diagnosed during middle age.
Sunlamps and tanning beds may increase your risk of melanoma, especially if they cause sunburn.
Melanoma prevention
Protective measures, such as avoiding skin exposure to sunlight during peak sun hours (10 AM to 4 PM), wearing protective clothing, and applying high-SPF broad spectrum sunscreen (SPF 30+), are essential for reducing exposure to harmful ultraviolet (UV) light. These protective measures are especially important in children because 80% of our lifetime exposure to UV light occurs before age 18.
Once a month, you should perform a self-exam to look for signs of skin cancer. It is best to perform the exam in a well-lit area after a shower or bath. Use a full-length mirror with the added assistance of a hand mirror when necessary. Using a hair dryer can help you examine any areas of skin covered by hair, such as your scalp.
- In front of a full-length mirror, inspect the front of your body, making sure to look at the front of your neck, chest (including under breasts), legs, and genitals.
- With your arms raised, inspect both sides of your body, making sure to examine your underarms.
- With your elbows bent, examine the front and back of your arms as well as your elbows, hands, fingers, area between your fingers, and fingernails.
- Inspect the tops and bottoms of your feet, the area between your toes, and toenails.
- With your back to the mirror and holding a hand mirror, inspect the back of your body, including the back of your neck, shoulders, legs, and buttocks.
- Using a hand mirror, examine your scalp and face.
As you perform your monthly self-exam, familiarize yourself with the moles, freckles, and other marks on your body, and look for any changes in them, including shape, size, color, or other changes, such as bleeding or itching.
Melanoma treatment
Prognosis and treatment of melanoma depend on how deep the tumor has grown into the skin. If you have a melanoma that is very thin (less than 1 mm) and has been completely removed with the excision, this may be all the treatment you need.
For thicker melanomas, your doctor will probably recommend a biopsy of your lymph nodes to determine if they contain melanoma cells. This is called a sentinel node biopsy. If these lymph nodes do have melanoma cells, you may need to have other lymph nodes surgically removed.
If you have lymph nodes that contain melanoma, your doctor will also need to determine if the melanoma has spread to other parts of your body. You may have to have a chest X-ray, a CT scan, an MRI, and/or other tests to determine this.
Treatment for melanoma that has spread to the lymph nodes or other parts of the body may include chemotherapy. For patients with melanoma that has metastasized, immunotherapy is another treatment that can help the body’s own immune system to destroy cancer cells. Types of immunotherapy include vaccines, cytokines (proteins that boost the immune system), and interferon-alpha.
If you have previously been diagnosed and treated for melanoma, you are at increased risk of developing another melanoma, especially in the first 3 years after diagnosis. Therefore, it is essential that you regularly follow up with your doctor to have a thorough skin examination.
Actinic keratosis vs seborrheic keratosis
Actinic keratosis, also known as solar keratosis, are small rough or scaly areas of skin due to damage from sun exposure. Some actinic keratosis can turn into squamous cell skin cancer, so it is important to perform self-examinations often and catch them early.
People with fair skin who sunburn easily; have trouble tanning; have blue, green, or hazel eyes; and red or blond hair are most at risk for developing actinic keratoses. Those who have had a lot of sun exposure in their youth are at a high risk as well. Those with a weak immune system due to chemotherapy, HIV, or an organ transplant are at higher risk.
Actinic keratosis spots usually appear in those who are older (over 50), but they can start appearing in younger adults who have had a lot of sun exposure. Darker-skinned individuals are rarely affected.
Figure 5. Actinic keratosis
Figure 6. Actinic keratosis
Actinic keratosis signs and symptoms
The sun-exposed areas of the face, scalp (where balding), ears, neck, forearms, and backs of the hands are most commonly affected with actinic keratoses, but any skin area frequently exposed to sun can be involved.
Patches are usually less than an inch in size with slight scale (sometimes thick like a wart) and a pink, red, or brownish color. They are slightly rough to the touch, like fine sandpaper, and may be a bit sensitive.
- Mild – one or two spots, not thick or hard
- Moderate – scattered, few spots
- Severe – numerous or thick, hard, or bleeding spots
Actinic keratosis prevention
Prevention is very important. Sun protection can reduce the number of new areas occurring and may help small lesions go away on their own.
- Avoid direct sun in the middle of the day (10 AM to 4 PM). Remember: snow and water reflect light to the skin, and clouds still let a lot of light through, so you may still be exposed to ultraviolet light even on cloudy days.
- Use a hat with a wide brim. A baseball hat does not give much protection.
- Cover up with tightly woven clothing. Some manufacturers make specialty clothing with a high sun protection factor (SPF) rating, or you can purchase a special ingredient to be added to your washer that can “wash” SPF into your clothing.
- Use sunscreen on all exposed skin areas, including the lips, before going outdoors. A broad spectrum (blocks UVB and UVA light), with an SPF of at least 30, is best. Apply generously 30 minutes before going outdoors and reapply every 2 hours or after swimming or sweating a lot.
- Do not use tanning beds!
- A low-fat diet (less than 21% calories from fat) has been shown to reduce the incidence of actinic keratoses.
Once a month, you should perform a self-exam to look for signs of skin cancer. It is best to perform the exam in a well-lit area after a shower or bath. Use a full-length mirror with the added assistance of a hand mirror, when necessary. Using a hair dryer can help you examine any areas of skin covered by hair, such as your scalp.
- In front of a full-length mirror, inspect the front of your body making sure to look at the front of your neck, chest (including under breasts), legs, and genitals.
- With your arms raised, inspect both sides of your body making sure to examine your underarms.
- With your elbows bent, examine the front and back of your arms as well as your elbows, hands, fingers, area between your fingers, and fingernails.
- Inspect the tops and bottoms of your feet, the area between your toes, and toenails.
- With your back to the mirror and holding a hand mirror, inspect the back of your body, including the back of your neck, shoulders, legs, and buttocks.
- Using a hand mirror, examine your scalp and face.
As you perform your monthly self-exam, familiarize yourself with the moles, freckles, and other marks on your body, and look for any changes in them from month to month, including shape, size, color, or other changes, such as bleeding or itching.
Actinic keratosis treatments
- Local destruction with freezing (cryosurgery), scraping (curettage), burning (electrocautery), dermabrasion, or a laser
- Creams with either tretinoin, adapalene, fluorouracil, diclofenac, or imiquimod
- Chemical peeling
- Photodynamic therapy
Seborrheic keratosis causes
Seborrheic keratosis is a benign form of skin tumor. The cause is unknown. The condition commonly appears after age 40. Seborrheic keratosis aren’t contagious. They tend to run in some families, so inheritance may play a role.
Researchers have noted:
- Eruptive seborrhoeic keratoses can follow sunburn or dermatitis.
- Skin friction may be the reason they appear in body folds.
- Viral cause (eg human papillomavirus) seems unlikely.
- Stable and clonal mutations or activation of FRFR3, PIK3CA, RAS, AKT1 and EGFR genes are found in seborrhoeic keratoses.
- Seborrhoeic keratosis can arise from solar lentigo.
- FRFR3 mutations also arise in solar lentigines. These mutations are associated with increased age and location on the head and neck, suggesting a role of ultraviolet radiation in these lesions.
- Seborrhoeic keratoses do not harbour tumor suppressor gene mutations.
- Epidermal growth factor receptor inhibitors (used to treat cancer) often result in an increase in verrucal (warty) keratoses.
Risk factors for seborrheic keratosis
You can develop seborrheic keratoses at any age, but you’re generally more likely to develop them if you’re over age 50. You’re also more likely to have them if you have a family history of the condition.
Seborrheic keratosis outlook (prognosis)
Removing the growths is simple and usually does not cause scars. You may have patches of lighter skin where growths on the torso have been removed.
Growths usually DO NOT return after they are removed. You may develop more growths in the future if you are prone to the condition.
Seborrheic keratosis possible complications
These complications may occur:
- Irritation, bleeding, or discomfort of growths
- Mistake in diagnosis (growths may look like skin cancer tumors)
- Distress due to physical appearance.
Very rarely, eruptive seborrhoeic keratoses may denote an underlying internal malignancy, most often gastric adenocarcinoma. The paraneoplastic syndrome is known as the sign of Leser-Trélat. Eruptive seborrhoeic keratoses that are not associated with cancer are sometimes described as having pseudo-sign of Leser-Trélat.
Eruptive and irritated seborrhoeic keratoses may also arise as an adverse reaction to a medication, such as adalimumab, vemurafenib, dabrafenib, 5-fluorouracil and many chemotherapy drugs.
An irritated seborrhoeic keratosis is an inflamed, red and crusted lesion. It may give rise to eczematous dermatitis around the seborrhoeic keratosis. Dermatitis may also trigger new seborrhoeic keratoses to appear.
Seborrheic keratosis signs and symptoms
One or more spots can occur anywhere on the body, except for palms, soles, and mucous membranes (e.g, in the mouth or rectum). Seborrheic keratosis do not go away. Seborrheic keratosis do not turn into cancers, but some cancers resemble seborrheic keratosis.
Seborrheic keratosis start as light brown to skin-colored, flat areas, which are round to oval and of varying size (usually less than a half inch, but sometimes much larger). As they grow thicker and rise above the skin surface, seborrheic keratoses may become dark brown to almost black with a “stuck on” appearance. The surface may feel smooth or rough.
Symptoms of seborrheic keratosis are skin growths that:
- Are located on the face, chest, shoulders, back, or other areas
- Are painless, but may become irritated and itch
- Are most often tan, brown, or black
- Have a slightly raised, flat surface
- May have a rough texture (like a wart)
- Often have a waxy surface
- Are round or oval in shape
- May look like a piece of bee’s wax that has been “pasted-on” the skin
- Often appear in clusters
Seborrheic keratosis diagnosis
Your health care provider will look at the growths to determine if you have the condition. You may need a skin biopsy to confirm the diagnosis.
Seborrheic keratosis treatment
Treatment of seborrheic keratoses usually isn’t necessary. You may want them removed if they become irritated, if they bleed because your clothing rubs against them, or if you simply don’t like how they look or feel.
Your doctor can remove seborrheic keratoses using several methods, including:
- Freezing with liquid nitrogen (cryosurgery). Cryosurgery can be an effective way to remove seborrheic keratoses. It doesn’t always work on raised growths, and it may lighten treated skin.
- Scraping the skin’s surface with a special instrument (curettage). Sometimes curettage is used along with cryosurgery to treat thinner or flat growths. It may be used with electrocautery.
- Burning with an electric current (electrocautery). Electrocautery can be effective in removing seborrheic keratoses. It can be used alone or with curettage. This procedure can leave scars if it’s not done properly, and it may take longer than other removal methods.
- Vaporizing the growth with a laser (ablation). Different types of laser treatments are available to treat seborrheic keratoses.
- Focal chemical peel with trichloracetic acid or hydrogen peroxide
On average, dermatologists treat 43% of their seborrheic keratosis patients to remove lesions. Cryosurgery is the most common removal method.
Cryotherapy
Cryotherapy is quick and effective in the majority of cases, however, significant postinflammatory hyperpigmentation may occur e.g., in Asians or darker-skinned individuals on the face or below the knee.
Electrocautery
Light electrocautery (and curettage if needed) after local anesthesia can provide excellent cosmetic results, perhaps with less risk of pigmentary change.
Hydrogen Peroxide
The has approved ESKATA™, a 40% hydrogen peroxide topical solution for the treatment of raised seborrheic keratoses. In a study of facial seborrheic keratoses treated up to 2 times, 68% of patients were judged to be clear or near clear 1. It is applied in the office, not by the patient.
Laser
One study of 42 patients compared one-time freezing vs. Er:YAG laser treatment on matched, same-patient lesions 2. Complete healing occurred in all laser-treated lesions while the healing rate was only 68% in the cryotherapy group. Both hyperpigmentation and erythema post-healing were higher with cryotherapy.
All methods have disadvantages. Treatment-induced loss of pigmentation is a particular issue for dark skinned patients. There is no easy way to remove multiple lesions on a single occasion.