Contents
What is sick sinus syndrome
Sick sinus syndrome — also known as sinus node disease or sinus node dysfunction — is the name for a group of heart rhythm problems (arrhythmias) in which the sinus node — the heart’s natural pacemaker — doesn’t work properly. Sick sinus syndrome is a group of abnormal heartbeats (arrhythmias) presumably caused by malfunction of the sinus node, the heart’s “natural” pacemaker. Although the term “sick sinus syndrome” was first used to describe the sluggish return of sinoatrial (SA) nodal activity following electrical cardioversion, it is now commonly used to describe the inability of the sinoatrial (SA) node to generate a heart rate commensurate with the physiologic needs of an individual.
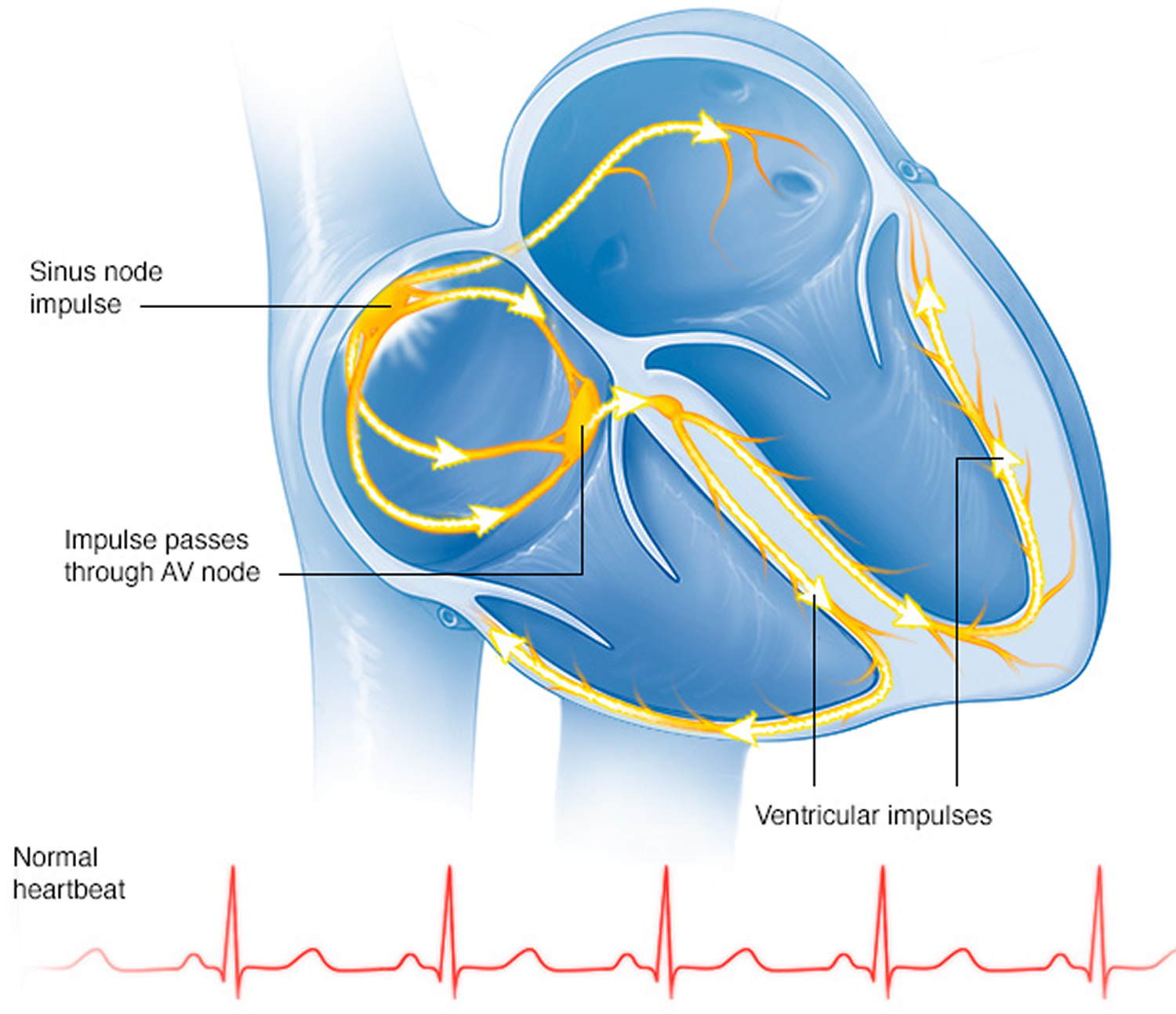
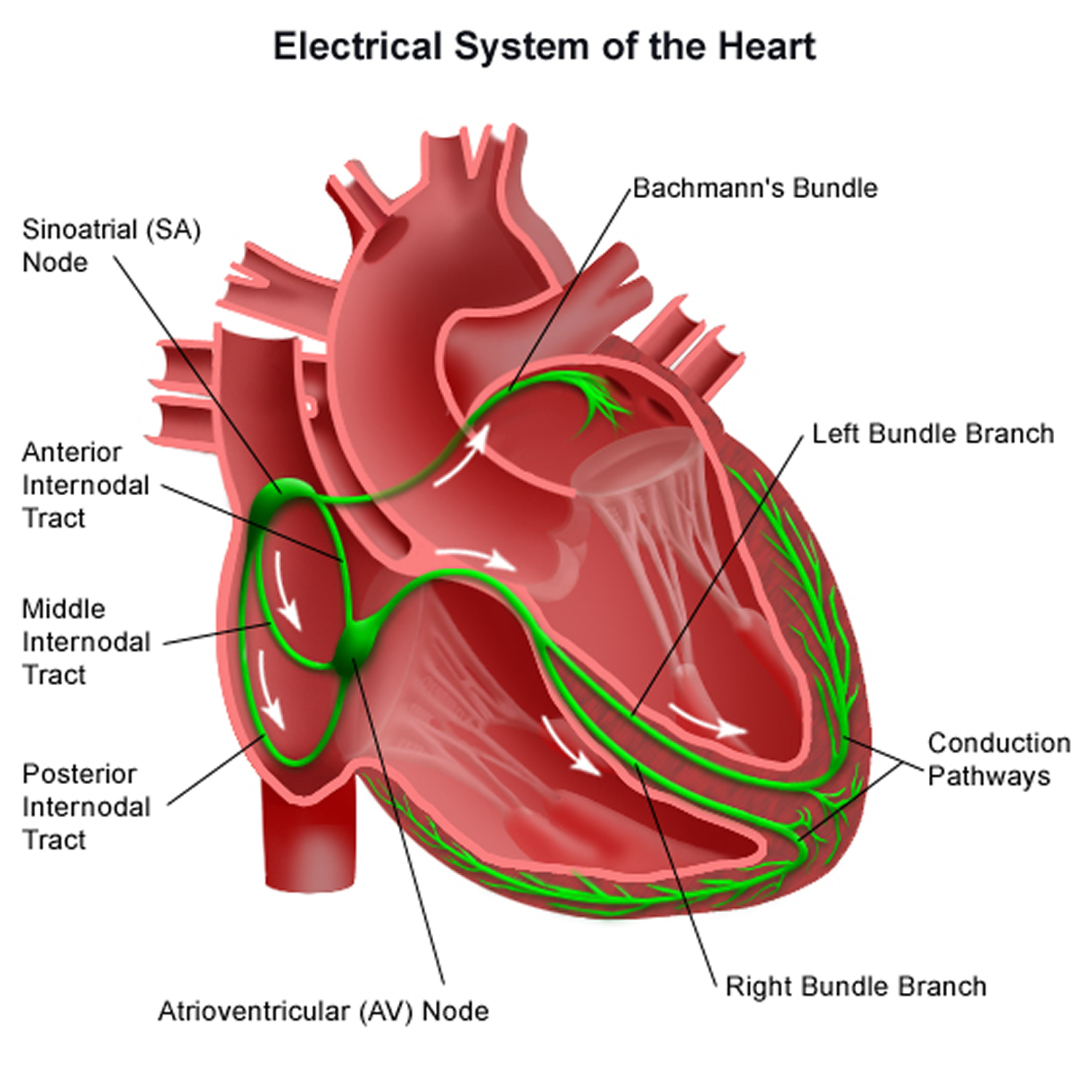
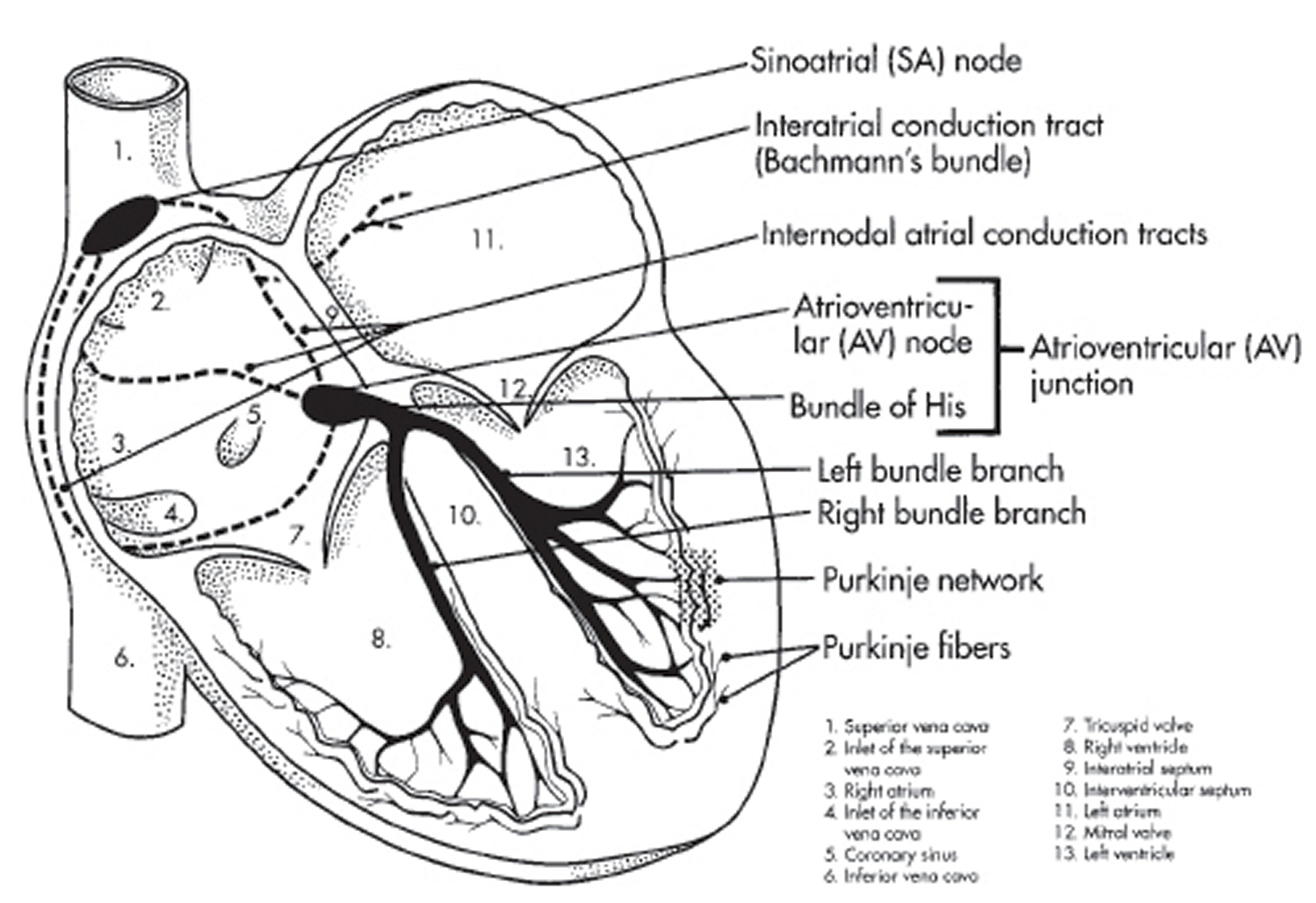
The sinus node is an area of specialized cells in the upper right chamber of the heart that controls the rhythm of your heart (see Figures 1). Normally, the sinoatrial (SA) node produces a steady pace of regular electrical impulses. In sick sinus syndrome, these signals are abnormally paced.
A person with sick sinus syndrome may have heart rhythms that are too fast, too slow, punctuated by long pauses — or an alternating combination of all of these rhythm problems. Sick sinus syndrome is relatively uncommon, but the risk of developing sick sinus syndrome increases with age. Sick sinus syndrome is more common in elderly adults, where the cause is often a non-specific, scar-like degeneration of the conduction system. Cardiac surgery, especially to the atria, is a common cause of sick sinus syndrome in children.
Many people with sick sinus syndrome eventually need a pacemaker to keep the heart in a regular rhythm.
The sinoatrial (SA) node is innervated by the parasympathetic and the sympathetic nervous systems; the balance between these systems controls the pacemaker rate. Parasympathetic input via the vagus nerves decreases the sinoatrial (SA) nodal pacemaker and is the dominant input at rest, wheras sympathetic nerve input, as well as the adrenal medullary release of catecholamines, increases the sinus rate during exercise and stress.
Sinus node dysfunction is characterized by dysfunction of the sinoatrial (SA) node that is often associated with senescence of the node and surrounding atrial myocardium 1. When sinus node dysfunction is associated with symptoms such as dizziness or syncope, sick sinus syndrome is a more clinically representative term. However, sinus node dysfunction and sick sinus syndrome are often used interchangeably.
A conglomeration of electrocardiogram (ECG) abnormalities represent manifestation of sinus node dysfunction, including 1:
- Sinus bradycardia
- Sinus pause
- Sinus arrest
- SA nodal exit block
- Inadequate heart rate response to physiologic demands during activity (chronotropic incompetence)
- Supraventricular tachycardia (eg, atrial fibrillation, atrial flutter, and atrial tachycardia as part of the tachycardia-bradycardia syndrome) 2
The epidemiology of sick sinus syndrome is difficult to study, given its nature and varying manifestations, including nonspecific symptoms and electrocardiographic (ECG) findings. It is estimated that the incidence of sick sinus syndrome in the United States is approximately 1 in 600 cardiac patients older than 65 years 3. Due to its relationship with advanced age, sick sinus syndrome is more prevalent in countries where citizens have a longer life expectancy.
Symptomatic patients are generally older, in seventh or eighth decade of life, with frequent comorbidities. Only a few epidemiologic studies have been published.
A pooled analysis of 20,572 patients from 2 large epidemiology studies (the Atherosclerosis Risk in Communities and Cardiovascular Health Study trials) who were followed for an average of 17 years, 291 incident cases of sick sinus syndrome were noted, yielding an incidence rate of 0.8 cases per 1000 person-years 4. Although several variables were associated with the development of sick sinus syndrome (e.g, higher body mass index, hypertension, prior cardiovascular event), advancing age was the most significant risk factor for sick sinus syndrome (hazard ratio 1.73 for each additional 5 years of age) 4.
In major trials of pacing in this disorder, the median or mean age of the patients with sick sinus syndrome was 73 to 76 years. Men and women appear equally affected and, although less common, sick sinus syndrome can also occur in younger adults and children 5.
The Heart’s Electrical System
The heart’s electrical system controls the rate and rhythm of the heartbeat.
With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As the signal travels, it causes the heart to contract and pump blood.
Your heart’s electrical system controls all the events that occur when your heart pumps blood 6. The electrical system also is called the cardiac conduction system. If you’ve ever seen the heart test called an EKG (electrocardiogram), you’ve seen a graphical picture of the heart’s electrical activity.
Your heart’s electrical system is made up of three main parts:
- The Sinoatrial (SA) node, located in the right atrium of your heart
- The Atrioventricular (AV) node, located on the interatrial septum close to the tricuspid valve
- The His-Purkinje system, located along the walls of your heart’s ventricles
A heartbeat is a complex series of events. These events take place inside and around your heart. A heartbeat is a single cycle in which your heart’s chambers relax and contract to pump blood. This cycle includes the opening and closing of the inlet and outlet valves of the right and left ventricles of your heart.
Each heartbeat has two basic parts: diastole and systole. During diastole, the atria and ventricles of your heart relax and begin to fill with blood.
At the end of diastole, your heart’s atria contract (atrial systole) and pump blood into the ventricles. The atria then begin to relax. Your heart’s ventricles then contract (ventricular systole), pumping blood out of your heart.
Each electrical signal begins in a group of cells called the sinus node or sinoatrial (SA) node. The SA node is located in the heart’s upper right chamber, the right atrium. In a healthy adult heart at rest, the SA node fires off an electrical signal to begin a new heartbeat 60 to 100 times a minute. In a normal, healthy heart, each beat begins with a signal from the SA node. This is why the SA node sometimes is called your heart’s natural pacemaker. Your pulse, or heart rate, is the number of signals the SA node produces per minute.
The signal is generated as the vena cavae fill your heart’s right atrium with blood from other parts of your body. The signal spreads across the cells of your heart’s right and left atria.
The SA node (the sinus node) is a subepicardial structure normally located in the right atrial wall near the superior vena cava entrance on the upper end of the sulcus terminalis. It is formed by a cluster of cells capable of spontaneous depolarization. Normally, these pacemaker cells depolarize at faster rates than any other latent cardiac pacemaker cell inside the heart. Therefore, a healthy sinoatrial (SA) node directs the rate at which the heart beats. Electrical impulses generated in the sinoatrial (SA) node must then be conducted outside the sinoatrial (SA) node in order to depolarize the rest of the heart. From the SA node, the electrical signal travels through special pathways in the right and left atria. This causes the atria to contract and pump blood through the open valves from the atria into heart’s two lower chambers, the ventricles.
The electrical signal then moves down to a group of cells called the atrioventricular (AV) node, located between the atria and the ventricles. Here, the signal slows down just a little, allowing your heart’s right and left ventricles time to finish filling with blood.
The electrical signal then leaves the AV node and travels along a pathway called the bundle of His. This pathway divides into a right bundle branch and a left bundle branch. The signal goes down these branches to the ventricles, causing them to contract and pump blood to the lungs and the rest of the body.
From the bundle of His, the signal fibers divide into left and right bundle branches through the Purkinje fibers. These fibers connect directly to the cells in the walls of your heart’s left and right ventricles.
The signal spreads across the cells of your ventricle walls, and both ventricles contract. However, this doesn’t happen at exactly the same moment.
The left ventricle contracts an instant before the right ventricle. This pushes blood through the pulmonary valve (for the right ventricle) to your lungs, and through the aortic valve (for the left ventricle) to the rest of your body.
As the signal passes, the walls of the ventricles relax and await the next signal.
This process continues over and over as the atria refill with blood and more electrical signals come from the SA node.
Sinoatrial (SA) node activity is regulated by the autonomic nervous system. For example, parasympathetic stimulation causes sinus bradycardia, sinus pauses, or sinoatrial exit block. These actions decrease SA node (the sinus node) automaticity, thereby decreasing the heart rate.
Sympathetic stimulation, however, increases the slope of phase 4 spontaneous depolarizations. This increases the automaticity of the SA node (the sinus node), thereby increasing the heart rate. Blood supply to the sinoatrial (SA) node is provided by the right coronary artery in most cases.
A problem with any part of this process can cause an arrhythmia. For example, sick sinus syndrome (sinus node dysfunction) involves abnormalities in sinoatrial (SA) node impulse formation and propagation, which are often accompanied by similar abnormalities in the atrium and in the conduction system of the heart. Together, these abnormalities may result in inappropriately slow ventricular rates and long pauses at rest or during various stresses. When sick sinus syndrome is mild, patients are usually asymptomatic. As sick sinus syndrome becomes more severe, patients may develop symptoms due to organ hypoperfusion and pulse irregularity. Such symptoms include the following:
- Fatigue
- Dizziness
- Confusion
- Fall
- Syncope
- Angina
- Heart failure symptoms and palpitations
Figure 1. The heart’s electrical system
Natural history of sick sinus syndrome
The natural history of sick sinus syndrome typically involves intermittent and/or progressive cardiac rhythm disorders, which have been associated with higher rates of other cardiovascular events and higher mortality. There is a tendency for the rhythm disturbances associated with sick sinus syndrome to evolve over time, along with a higher likelihood of thromboembolic events and other cardiovascular events.
For many patients with sick sinus syndrome, there are variable, and often long, periods of normal sinoatrial (SA) node function. However, once present, in due course, sick sinus syndrome progresses in most patients, accompanied by a greater likelihood of developing atrial tachyarrhythmias. However, the time course of disease progression is difficult to predict; hence, most patients with symptomatic sick sinus syndrome are treated earlier in an attempt to alleviate symptoms.
As noted, sick sinus syndrome usually progresses over time. In a study of 52 patients with sick sinus syndrome and sinus bradycardia associated with sinoatrial (SA) block or sinus arrest, it took an average of 13 years (range, 7-29 years) for progression to total sinus arrest and an escape rhythm 7.
The incidence of atrial arrhythmias and conduction disturbances occurs more frequently over time, which may be due in part to a progressive pathologic process that affects the entire atrium and other parts of the heart. In a study comprising 213 patients with a history of symptomatic sick sinus syndrome who were treated with atrial pacing and followed for a median of 5 years, 7% developed atrial fibrillation and 8.5% developed high-grade atrioventricular block 8.
Patients with sick sinus syndrome, especially those with tachycardia-bradycardia, are at higher risk for thromboembolic events—even after pacemaker implantation. Asymptomatic episodes of atrial fibrillation resulting in thromboembolic events may contribute to cardiovascular events following pacemaker implantation.
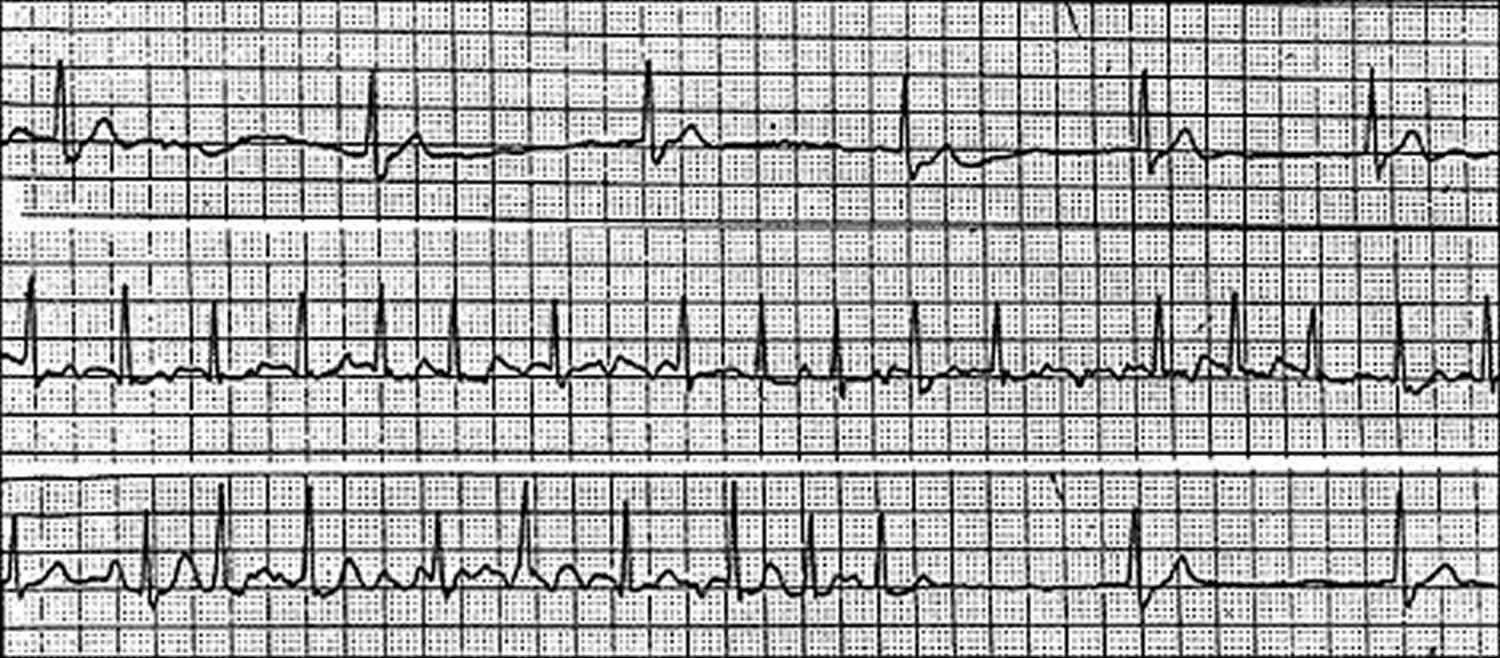
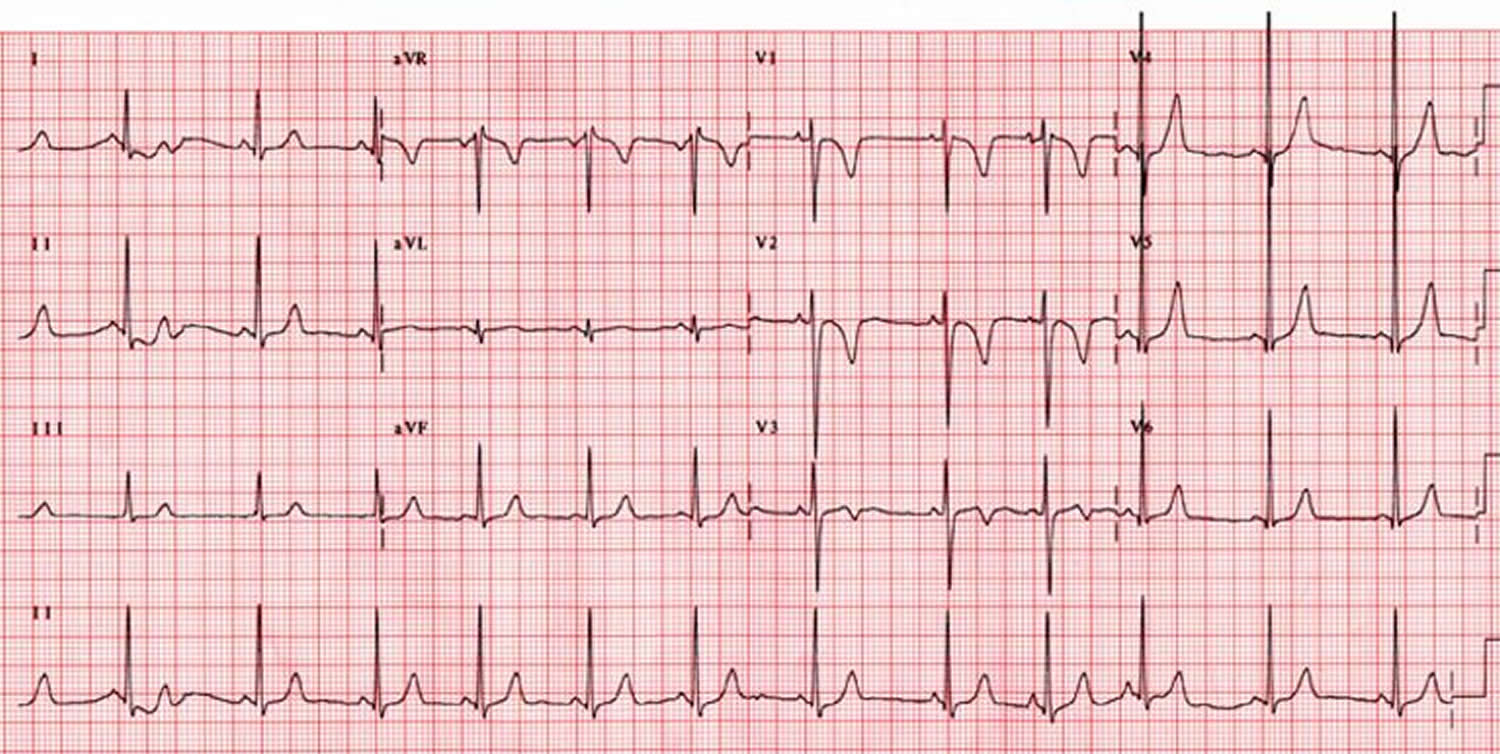
Figure 2. Sick sinus syndrome ECG – image below exhibits the alternating patterns of bradycardia and tachycardia
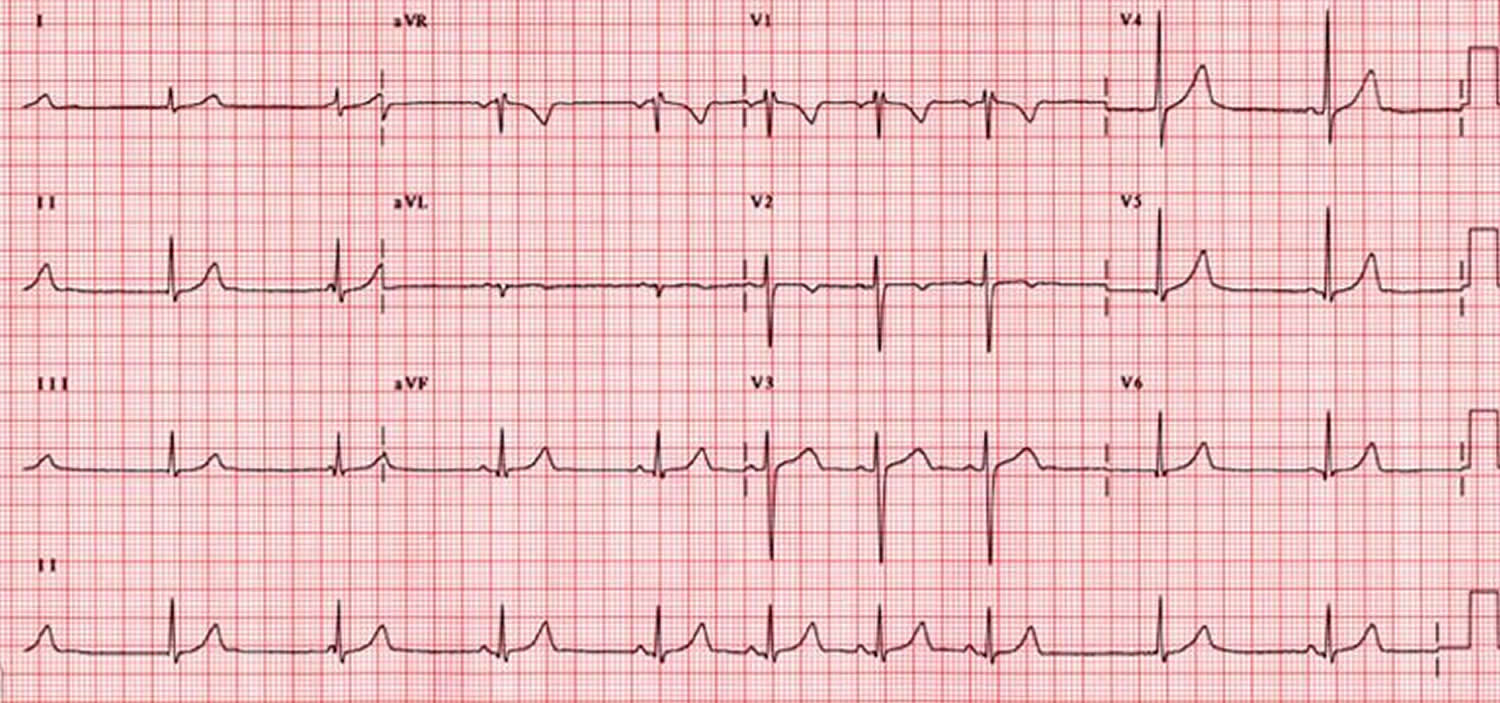
Figure 3. Sick sinus syndrome ECG – sinus arrhythmia
Figure 4. Sick sinus syndrome ECG – sinus bradycardia
Sick sinus syndrome prognosis
The prognosis of patients with sinus node dysfunction (sick sinus syndrome) is dependent on the underlying associated condition. The incidence of sudden cardiac death in patients with sick sinus syndrome is low 5. Pacemaker therapy does not appear to affect survival in patients with sick sinus syndrome 9.
Patients with tachy-brady syndrome have a worse prognosis than do patients with isolated sick sinus syndrome. The overall prognosis in patients with sick sinus syndrome and additional systemic ventricular dysfunction (e.g, numerous postoperative Mustard and Fontan patients) depends on their underlying ventricular dysfunction or degree of congestive heart failure.
In patients who have undergone a Fontan surgery and developed sick sinus syndrome, endocardial atrial leads can be implanted relatively safely and can permit low-energy thresholds for as long as 5 years after implantation 10.
Morbidity and mortality
The relationship between sick sinus syndrome and mortality is difficult to clearly understand, as many individuals with sick sinus syndrome have preexisting comorbidities (e.g, hypertension, diabetes mellitus, atrial fibrillation) that are known to increase all-cause mortality 11.
Sick sinus syndrome complications
The complications of sick sinus syndrome include the following:
- Sudden cardiac death
- Syncope
- Thromboembolic events, including stroke
- Heart failure
- Atrial tachyarrhythmias
When your heart’s natural pacemaker isn’t working properly, your heart can’t perform as efficiently as it should. This can lead to a very slow heart rate, which may cause fainting.
In rare cases, long periods of slow heart rate or fast heart rate can keep your heart from pumping enough blood to meet your body’s needs — a condition called heart failure.
If you have a type of sick sinus syndrome called bradycardia-tachycardia syndrome, you also may be at a higher risk of developing a blood clot in your heart that may lead to a stroke. That’s because the fast heart rhythm that occurs in bradycardia-tachycardia syndrome is often atrial fibrillation.
Atrial fibrillation is a chaotic rhythm of the upper chambers of the heart that can cause blood pooling in the heart. Blood clots are more likely to form when blood flow through the heart is altered in any way. A blood clot can break loose and travel to the brain, causing a stroke.
About 50% of patients with sick sinus syndrome develop tachy-brady syndrome over a lifetime; such patients have a higher risk of stroke and death. However, the incidence of sudden death owing directly to sick sinus syndrome is extremely low 5.
Sick sinus syndrome causes
Sinus node dysfunction (sick sinus syndrome) occurs as a result of disorders in automaticity, conduction, or both of the sinoatrial (SA) node 12. Local cardiac pathology, systemic diseases that involve the heart, and medications or toxins can all be responsible for abnormal SA node function and may result in sick sinus syndrome 12.
Abnormal automaticity (sinus arrest)
Abnormal automaticity, or sinus arrest, refers to a failure of sinus impulse generation. Abnormal conduction, or SA delay or block, is a failure of impulse transmission. In such cases, the sinus impulse is generated normally, but it is abnormally conducted to the neighboring atrial tissue. Both abnormal automaticity and abnormal conduction may result from one of several different mechanisms, including fibrosis, atherosclerosis, and inflammatory or infiltrative myocardial processes.
Sinus node degeneration resulting in fibrosis, calcification, or amyloidosis
The most common cause of sick sinus syndrome is the replacement of sinus node tissue by scar tissue, which may be accompanied by degeneration and fibrosis of other parts of the conduction system as well, including the atrioventricular (AV) node. The transitional junction between the sinoatrial (SA) node and atrial tissue may also be involved, and there may be degeneration of the nerve ganglia.
Medications and toxins
A number of medications and toxins can depress sinus node function, resulting in symptoms and electrocardiographic (ECG) changes consistent with sick sinus syndrome. The most commonly used prescription medications that alter myocardial conduction and may potentially result in sick sinus syndrome include:
- Beta blockers
- Non-dihydropyridine calcium channel blockers (eg, diltiazem, verapamil)
- Digoxin
- Antiarrhythmic medications
- Ivabradine
- Acetylcholinesterase inhibitors (eg, donepezil, rivastigmine) used in the treatment of Alzheimer disease
- Parasympathomimetic agents
- Sympatholytic drugs (eg, methyldopa, clonidine)
- Lithium
- Poisoning by grayanotoxin, which is produced by some plants (eg, Rhododendron species) and found in certain varieties of honey, has been associated with depressed sinoatrial (SA) node function
Childhood and familial diseases
Although rare in children, when sick sinus syndrome presents in this population, it is most often seen in those with congenital and acquired heart disease, particularly after corrective cardiac surgery. Familial sick sinus syndrome is rare, with mutations in the cardiac sodium channel gene SCN5A 13 and the HCN4 gene 14 (thought to contribute to the sinoatrial node pacemaker current) responsible for some familial cases.
In a series of 30 children and young adults (age range: 3 days to 25 years) with sick sinus syndrome, 22 had significant cardiac disease, and 13 developed sick sinus syndrome after cardiac surgery 15. The causes of sick sinus syndrome were inappropriate sinus bradycardia, sinus arrest, and SA exit block 15.
In a study of 10 children from 7 families with familial sick sinus syndrome, in which genomic DNA encoding the alpha subunit of the cardiac sodium channel was screened for mutations, compound heterozygous nucleotide changes were identified in 5 children from 3 families, but not in any of over 75 control subjects 16.
In a series of 38 patients with clinical evidence of Brugada syndrome, 4 had SCN5A mutations. Of these 4 patients, 3 had sick sinus syndrome with multiple affected family members. However, mutations in SCN5A are not pathognomonic for sick sinus syndrome, as different SCN5A mutations are associated with other cardiac abnormalities including Brugada syndrome, congenital long QT syndrome type 3, familial AV block, and familial dilated cardiomyopathy with conduction defects and susceptibility to atrial fibrillation (AF) 13.
Infiltrative diseases
The SA node may be affected by infiltrative disease, such as amyloidosis, sarcoidosis, scleroderma, hemochromatosis, and rarely tumor.
Inflammatory diseases
Rheumatic fever, pericarditis, diphtheria, Chagas disease, and other disorders may depress SA nodal function.
SA nodal artery disease
The sinoatrial (SA) node is perfused by branches of the right coronary artery in 55-60% of cases, and by the left circumflex artery in the remaining 40-45%. Stenosis of the SA nodal artery may occur due to atherosclerosis or inflammatory processes, resulting in ischemia; the latter may also occur with embolic events. Approximately 5% of patients with myocardial infarction (heart attack) (usually inferior wall heart attack) show sick sinus syndrome that tends to be reversible 17.
Genetic mutations
Mutations in HCN4 can produce both symptomatic and asymptomatic sick sinus syndrome, as illustrated by numerous reports of sinus bradycardia in family members with such mutations 18.
Trauma
Cardiac trauma may affect either the SA node directly or its blood supply.
Miscellaneous
Other disorders that can cause sick sinus syndrome include hypothyroidism, hypothermia, hypoxia, and muscular dystrophies. Some infections (eg, leptospirosis, trichinosis, Salmonella typhi infection) are associated with relative sinus bradycardia; however, these usually do not result in permanent sick sinus syndrome 19.
In addition, sick sinus syndrome is seen in children with congenital and acquired heart disease, particularly after corrective surgery. The cause of sick sinus syndrome in these children is likely related to the underlying structural heart disease and surgical trauma to the sinoatrial (SA) node and/or sinoatrial (SA) node artery.
Emery-Dreifuss muscular dystrophy is an X-linked muscle disorder associated with sick sinus syndrome and AV conduction defects. If AV conduction defects are present, sudden cardiac death may result unless the condition is treated with permanent pacing. Males and females may be affected with equal frequency.
Sinus venosus atrial septal defect (ASD), Ebstein anomaly, and heterotaxy syndromes, particularly left atrial isomerism, can also lead to sick sinus syndrome.
Surgical causes, especially from operations involving the right atrium
Gradual loss of sinus rhythm occurs after the Mustard, Senning, and all varieties of the Fontan operation. This is thought to be secondary to direct injury to the sinoatrial (SA) node during surgery and also due to later, chronic hemodynamic abnormalities. Paroxysmal atrial tachycardias are frequently associated with sick sinus syndrome, and loss of sinus rhythm appears to increase the risk of sudden death. Patients with transposition of the great arteries now undergo the arterial switch operation, which avoids the extensive atrial suture lines that lead to sinoatrial (SA) node damage.
Sick sinus syndrome was described in 15% of patients who had undergone the Ross operation for aortic valve disease or complex left-sided heart disease, 2.6 to 11 years earlier 20. Other arrhythmias, such as complete AV block and ventricular tachycardia, were present as well after the Ross operation.
When repairing atrial septal defects, especially sinus venosus atrial septal defects, sick sinus syndrome frequently occurs because of the proximity of the defect with sinoatrial (SA) node tissue.
Other surgically related causes of sick sinus syndrome include the following:
- Patients who have undergone surgery for endocardial cushion defects (ECDs) may later develop sick sinus syndrome
- Sick sinus syndrome may be caused by a Blalock-Hanlon atrial septectomy
- Sick sinus syndrome may occur after repair of partial anomalous pulmonary venous return or total anomalous pulmonary venous return
- Cannulation of the superior vena cava, usually performed for cardiopulmonary bypass or extracorporeal membrane oxygenation, may damage sinoatrial (SA) node tissue
- Ischemic cardiac arrest may cause sick sinus syndrome
Other
Rheumatic fever is another cause of sick sinus syndrome. Such dysfunction may also result from central nervous system (CNS) disease, which is usually secondary to increased intracranial pressure with a subsequent increase in the parasympathetic tone.
Endocrine-metabolic diseases (hypothyroidism and hypothermia) and electrolyte imbalances (hypokalemia and hypocalcemia) are other conditions that can contribute to sick sinus syndrome.
A study by Sunaga et al 21 involving 202 subjects indicated that in patients with persistent atrial fibrillation, those with low-amplitude fibrillatory waves and a large left atrial volume index are at an increased risk for the appearance of concealed sick sinus syndrome after catheter ablation has restored sinus rhythm.
Sick sinus syndrome signs and symptoms
Most people with sick sinus syndrome initially have few or no symptoms. In some cases, symptoms may come and go.
Most patients with sick sinus syndrome present with one or more of the following nonspecific symptoms, primarily due to bradycardia, sinus pause, and sinus arrest:
- Fatigue
- Dizziness or lightheadedness
- A sensation of rapid, fluttering heartbeats (palpitations)
- Fainting or near fainting
- Dyspnea on exertion
- Chest pains or discomfort
- Slower than normal pulse (bradycardia)
- Shortness of breath
Many of these signs and symptoms are caused by reduced blood flow to the brain when the heart beats too fast or too slowly.
Sick sinus syndrome diagnosis
Symptoms of sick sinus syndrome — such as dizziness, shortness of breath and fainting — are also symptoms of many other diseases and conditions.
However, in sick sinus syndrome, these symptoms only occur when the heart is beating abnormally. In order to diagnose and treat sick sinus syndrome, your doctor will need to establish a connection between your symptoms and an abnormal heart rhythm.
Electrocardiogram
Testing for sick sinus syndrome usually starts with a standard electrocardiogram (ECG). However, if your abnormal heart rhythms tend to come and go, they may not be detected during the brief time a standard ECG is recording. You may need additional types of ECG:
- Standard ECG. During this test, sensors (electrodes) are attached to your chest and limbs to create a record of the electrical signals traveling through your heart. The test may show patterns that indicate sick sinus syndrome, including fast heart rate, slow heart rate or a long pause in the heartbeat (asystole) after a fast heart rate.
- Holter monitor. This portable device is carried in your pocket or in a pouch on a belt or shoulder strap. It automatically records your heart’s activity for an entire 24- to 48-hour period, which provides your doctor with an extended look at your heart rhythms. This type of monitoring can be very helpful for diagnosing sick sinus syndrome.
- Event recorder. This portable electrocardiogram device can also be carried in your pocket or worn on a belt or shoulder strap for home monitoring of your heart’s activity. You will often be given this device to use for up to a month. When you feel symptoms, you push a button, and a brief ECG recording is saved. This allows your doctor to see your heart rhythm at the time of your symptoms, which can help pinpoint sick sinus syndrome.
- Implantable loop recorder. This small device is implanted just under the skin of your chest and is used for continuous, long-term monitoring of your heart’s electrical activity. An implantable loop recorder may be worn from months to years. This device is automatically triggered by an irregular heart rhythm (arrhythmia) or may be triggered manually when you feel symptoms.
Electrophysiologic testing
This test isn’t commonly used to screen for sick sinus syndrome. However, in some cases, electrophysiologic testing can help check the function of your sinus node, as well as other electrical properties of your heart.
During this test, thin, flexible tubes (catheters) tipped with electrodes are threaded through your blood vessels to various spots along the electrical pathways in your heart. Once in place, the electrodes can precisely map the spread of electrical impulses during each beat and may identify the source of heart rhythm problems.
Sick sinus syndrome treatment
Treatment for sick sinus syndrome focuses on eliminating or reducing unpleasant symptoms. If you aren’t bothered by symptoms, you may only need regular checkups to monitor your condition. For people who are bothered by symptoms, the treatment of choice is usually an implanted electronic pacemaker.
Medication changes
Your doctor may start by looking at your current medications to see if any of them could be interfering with the function of your sinus node. Medications used to treat high blood pressure or heart disease — such as beta blockers or calcium channel blockers — can worsen abnormal heart rhythms. In some cases, adjusting these medications can relieve symptoms.
Pacing the heart
Most people with sick sinus syndrome eventually need a permanent artificial pacemaker to maintain a regular heartbeat. This small, battery-powered electronic device is implanted under the skin near your collarbone during a minor surgical procedure. The pacemaker is programmed to stimulate or “pace” your heart as needed to keep it beating normally.
The type of pacemaker you need depends on the type of irregular heart rhythm you’re experiencing. Some rhythms can be treated with a single chamber pacemaker, which uses only one wire (lead) to pace one chamber of the heart — in this case, the atrium. However, most people with sick sinus syndrome benefit from dual chamber pacemakers, in which one lead paces the atrium and one lead paces the ventricle.
You’ll be able to resume normal or near-normal activities after you recover from pacemaker implantation surgery. The risk of complications, such as swelling or infection in the area where the pacemaker was implanted, is small.
Additional treatments for fast heart rate
If you have rapid heart rate as part of your sick sinus syndrome, you may need additional treatments to control these rhythms:
- Medications. If you have a pacemaker and your heart rate is still too fast, your doctor may prescribe anti-arrhythmia medications to prevent fast rhythms. If you have atrial fibrillation or other abnormal heart rhythms that increase your risk of stroke, you may need a blood-thinning medicine, such as warfarin (Coumadin) or dabigatran (Pradaxa).
- AV node ablation. This procedure can also control fast heart rhythms in people with pacemakers. It involves applying radiofrequency energy through a long, thin tube (catheter) to destroy (ablate) the tissue around the atrioventricular (AV) node between the atria and the ventricles. This stops fast heart rates from reaching the ventricles and causing problems.
- Radiofrequency ablation of atrial fibrillation. This procedure is similar to AV node ablation. However, in this case, ablation targets the tissue that triggers atrial fibrillation. This actually eliminates atrial fibrillation itself, rather than just preventing it from reaching the ventricles.
Lifestyle and home remedies
In some cases, inflammation and narrowed arteries caused by underlying heart disease can cause sick sinus syndrome. Your doctor may suggest that, in addition to other treatments, you make lifestyle changes that will keep your heart as healthy as possible.
Take the following steps to treat or eliminate risk factors that may lead to heart disease:
- Exercise and eat a healthy diet. Live a heart-healthy lifestyle by exercising regularly and eating a healthy, low-fat diet that’s rich in fruits, vegetables and whole grains.
- Maintain a healthy weight. Being overweight increases your risk of developing heart disease.
- Keep blood pressure and cholesterol under control. Make lifestyle changes and take medications as prescribed to correct high blood pressure (hypertension) or high cholesterol.
- Don’t smoke. If you smoke and can’t quit on your own, talk to your doctor about strategies or programs to help you break a smoking habit.
- If you drink, do so in moderation. If you drink alcohol, drink in moderation. For some conditions it’s recommended that you completely avoid alcohol. Ask your doctor for advice specific to your condition. If you can’t control your alcohol use, talk to your doctor about a program to quit drinking and manage other behaviors related to alcohol abuse.
- Don’t use illegal drugs. Talk to your doctor about an appropriate program for you if you need help ending illegal drug use.
- Control stress. Avoid unnecessary stress and learn coping techniques to handle normal stress in a healthy way.
- Go to scheduled checkups. Have regular physical exams and report any signs or symptoms to your doctor.
- [Guideline] Epstein AE, DiMarco JP, Ellenbogen KA, et al, for the American College of Cardiology Foundation, American Heart Association Task Force on Practice Guidelines, et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2013 Jan 22. 61 (3):e6-75.[↩][↩]
- Zhao J, Liu T, Li G. Relationship between two arrhythmias: sinus node dysfunction and atrial fibrillation. Arch Med Res. 2014 May. 45(4):351-5.[↩]
- Rodriguez RD, Schocken DD. Update on sick sinus syndrome, a cardiac disorder of aging. Geriatrics. 1990 Jan. 45(1):26-30, 33-6.[↩]
- Jensen PN, Gronroos NN, Chen LY, et al. Incidence of and risk factors for sick sinus syndrome in the general population. J Am Coll Cardiol. 2014 Aug 12. 64 (6):531-8.[↩][↩]
- Lamas GA, Lee KL, Sweeney MO, et al, for the Mode Selection Trial in Sinus-Node Dysfunction. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. 2002 Jun 13. 346 (24):1854-62.[↩][↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Your Heart’s Electrical System. https://www.nhlbi.nih.gov/health/health-topics/topics/hhw/electrical[↩]
- Lien WP, Lee YS, Chang FZ, Lee SY, Chen CM, Tsai HC. The sick sinus syndrome: natural history of dysfunction of the sinoatrial node. Chest. 1977 Nov. 72 (5):628-34.[↩]
- Brandt J, Anderson H, Fahraeus T, Schuller H. Natural history of sinus node disease treated with atrial pacing in 213 patients: implications for selection of stimulation mode. J Am Coll Cardiol. 1992 Sep. 20 (3):633-9.[↩]
- Menozzi C, Brignole M, Alboni P, et al. The natural course of untreated sick sinus syndrome and identification of the variables predictive of unfavorable outcome. Am J Cardiol. 1998 Nov 15. 82 (10):1205-9.[↩]
- Shah MJ, Nehgme R, Carboni M, Murphy JD. Endocardial atrial pacing lead implantation and midterm follow-up in young patients with sinus node dysfunction after the fontan procedure. Pacing Clin Electrophysiol. 2004 Jul. 27(7):949-54.[↩]
- Guideline] Zipes DP, DiMarco JP, Gillette PC, et al. Guidelines for clinical intracardiac electrophysiological and catheter ablation procedures. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Clinical Intracardiac Electrophysiologic and Catheter Ablation Procedures), developed in collaboration with the North American Society of Pacing and Electrophysiology. J Am Coll Cardiol. 1995 Aug. 26 (2):555-73.[↩]
- Choudhury M, Boyett MR, Morris GM. Biology of the sinus node and its disease. Arrhythm Electrophysiol Rev. 2015 May. 4 (1):28-34.[↩][↩]
- Makiyama T, Akao M, Tsuji K, et al. High risk for bradyarrhythmic complications in patients with Brugada syndrome caused by SCN5A gene mutations. J Am Coll Cardiol. 2005 Dec 6. 46 (11):2100-6.[↩][↩]
- Ishikawa T, Ohno S, Murakami T, et al. Sick sinus syndrome with HCN4 mutations shows early onset and frequent association with atrial fibrillation and left ventricular non-compaction. Heart Rhythm. 2017 Jan 16.[↩]
- Yabek SM, Jarmakani JM. Sinus node dysfunction in children, adolescents, and young adults. Pediatrics. 1978 Apr. 61 (4):593-8.[↩][↩]
- Benson DW, Wang DW, Dyment M, et al. Congenital sick sinus syndrome caused by recessive mutations in the cardiac sodium channel gene (SCN5A). J Clin Invest. 2003 Oct. 112 (7):1019-28.[↩]
- Alboni P, Baggioni GF, Scarfo S, et al. Role of sinus node artery disease in sick sinus syndrome in inferior wall acute myocardial infarction. Am J Cardiol. 1991 Jun 1. 67 (15):1180-4.[↩]
- Nof E, Luria D, Brass D, et al. Point mutation in the HCN4 cardiac ion channel pore affecting synthesis, trafficking, and functional expression is associated with familial asymptomatic sinus bradycardia. Circulation. 2007 Jul 31. 116 (5):463-70.[↩]
- Cunha BA. The diagnostic significance of relative bradycardia in infectious disease. Clin Microbiol Infect. 2000 Dec. 6 (12):633-4.[↩]
- Pasquali SK, Marino BS, Kaltman JR, et al. Rhythm and conduction disturbances at midterm follow-up after the ross procedure in infants, children, and young adults. Ann Thorac Surg. 2008 Jun. 85(6):2072-8.[↩]
- Sunaga A, Masuda M, Kanda T, et al. A low fibrillatory wave amplitude predicts sinus node dysfunction after catheter ablation in patients with persistent atrial fibrillation. J Interv Card Electrophysiol. 2015 Sep. 43 (3):253-61.[↩]