Contents
What is the thoracic duct
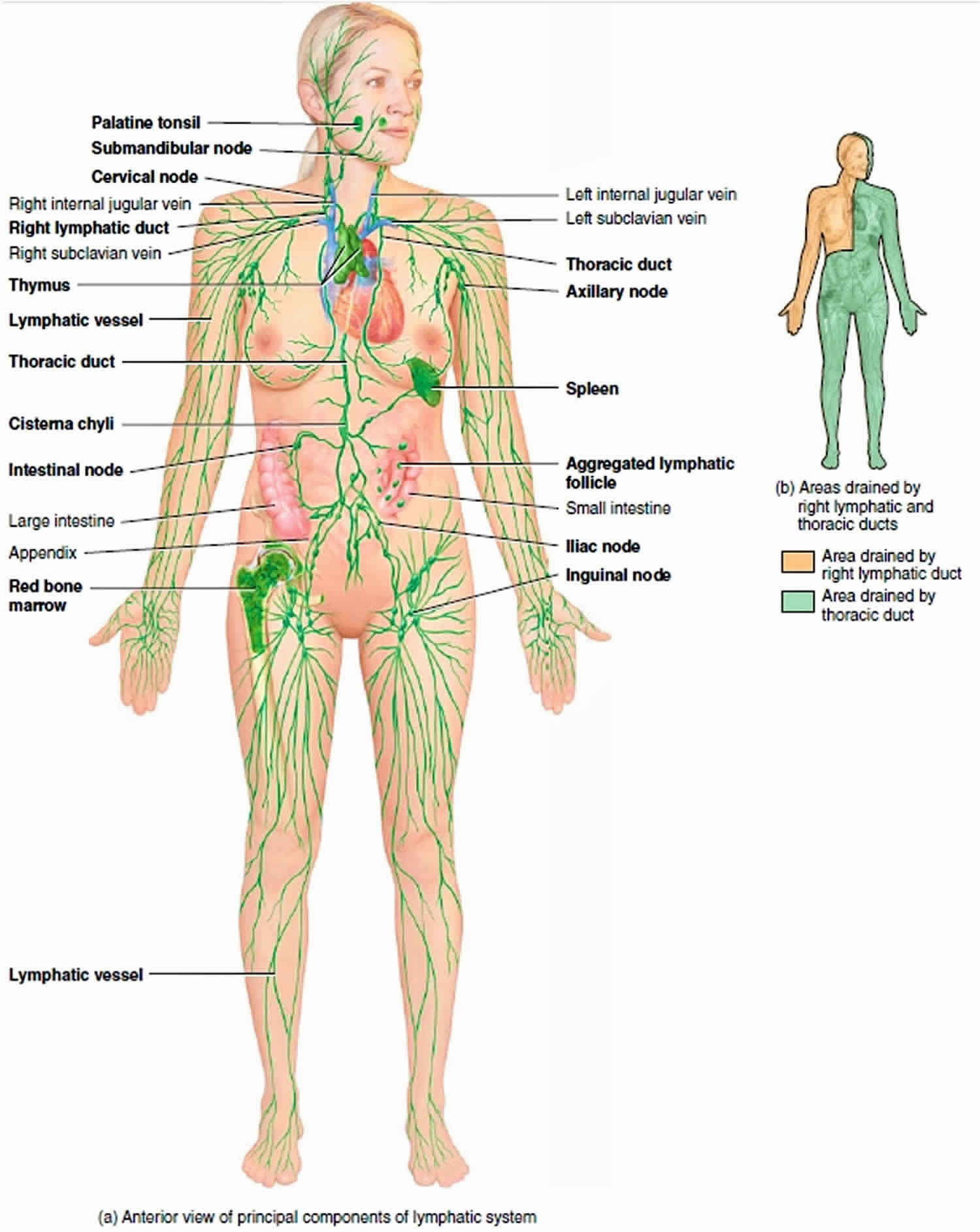
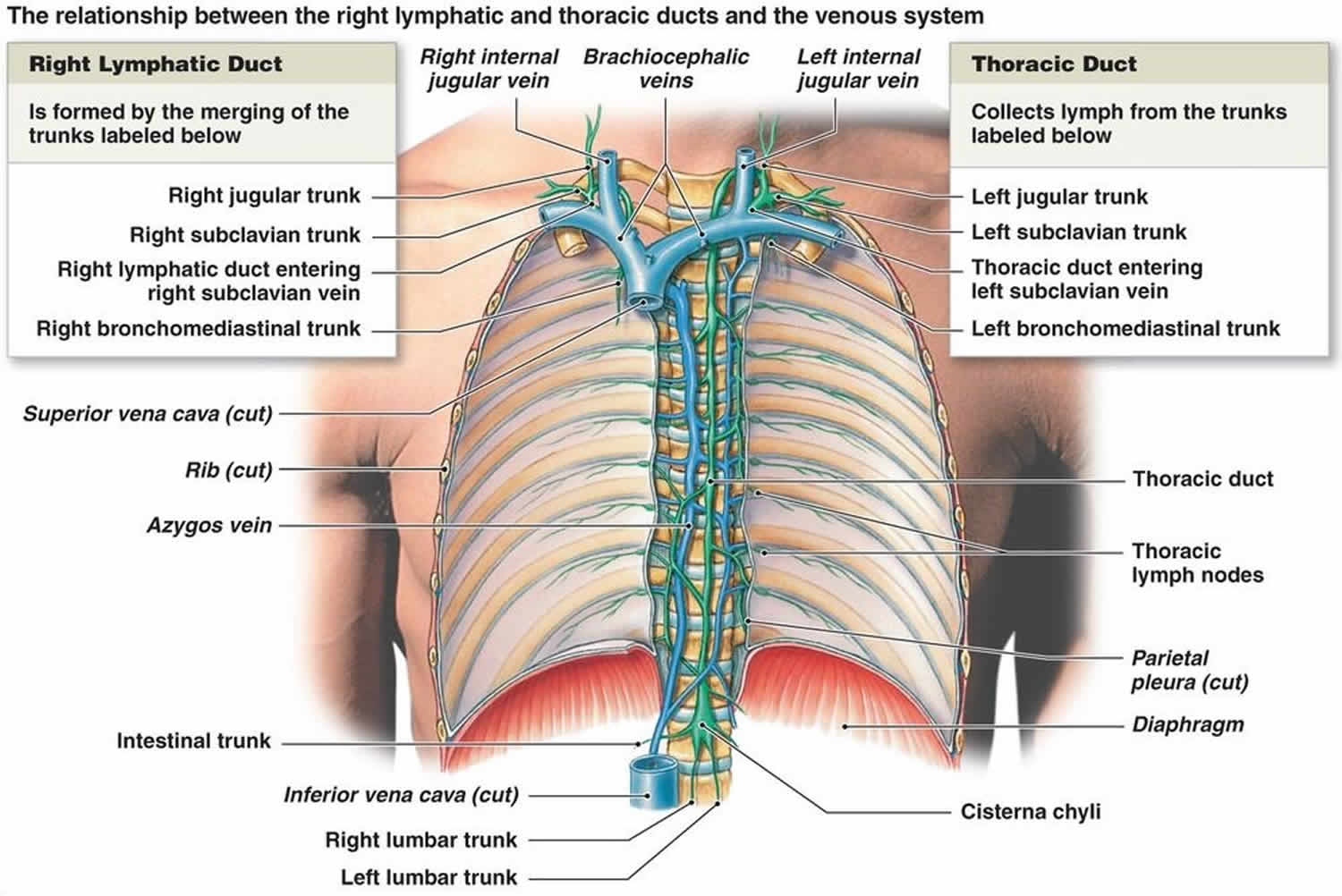
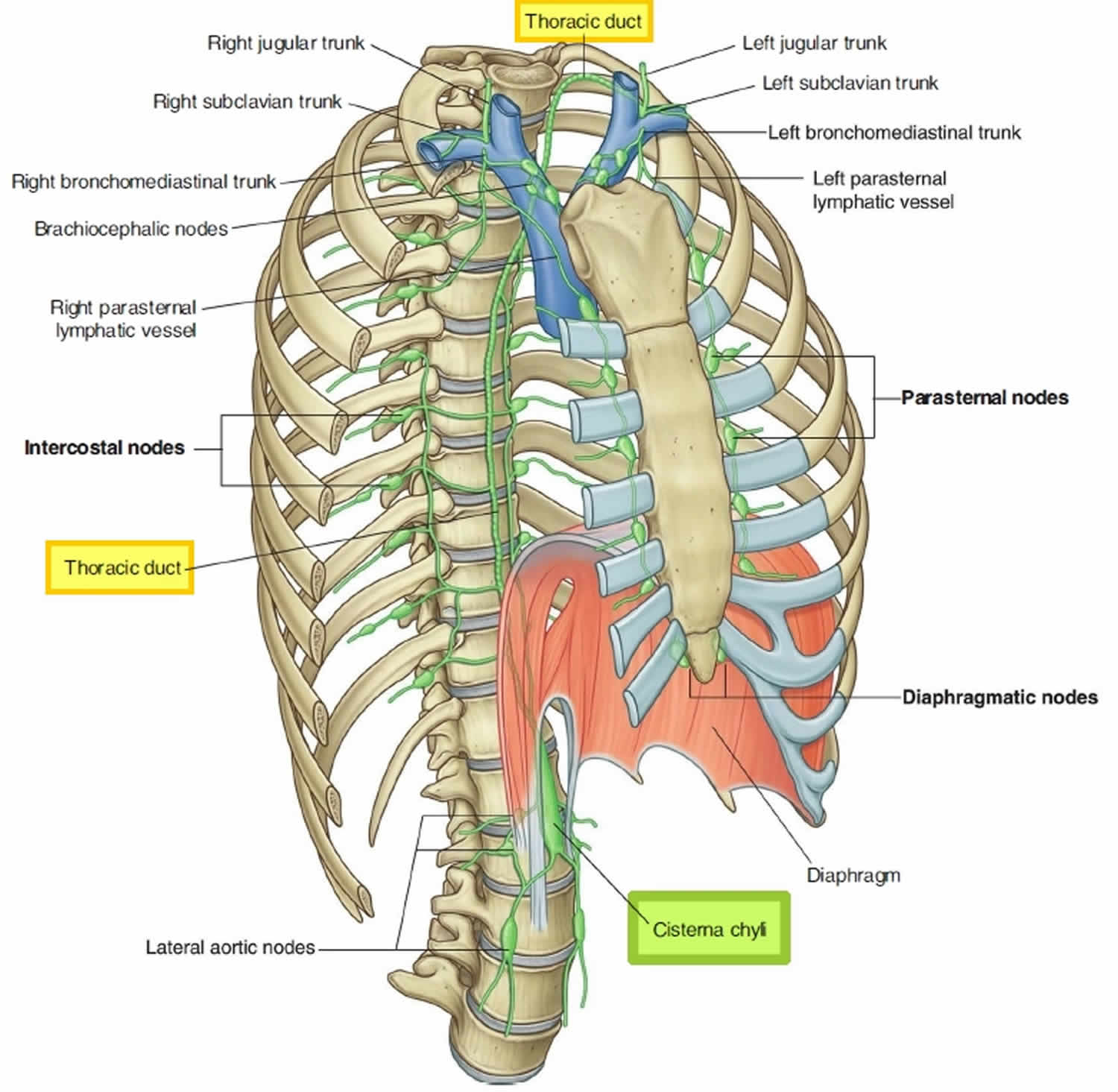
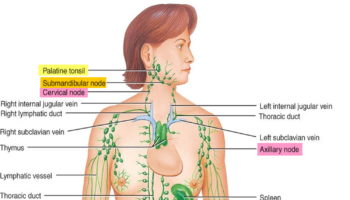
The thoracic duct is the main lymphatic channel for the return of chyle to the venous system. The thoracic duct drains lymph from both lower limbs, abdomen (except the convex area of the liver), left hemithorax, left upper limb and left face and neck. The thoracic duct is present in all individuals. The thoracic duct most inferior part, located at the union of the lumbar and intestinal trunks, is the cisterna chyli which lies on the bodies of vertebrae L1 and L2 (range T10-L3) (Figure 1). From there, the thoracic duct ascends along the vertebral bodies. In the superior thorax, the thoracic duct turns left and empties into the venous circulation at the junction of the left internal jugular and left subclavian veins. The thoracic duct is often joined by the left jugular, subclavian, and/or bronchomediastinal trunks just before it joins with the venous circulation. Alternatively, any or all of these three lymph trunks can empty separately into the nearby veins. When it is joined by the three trunks, the thoracic duct drains three-quarters of the body: the left side of the head, neck, and thorax; the left upper limb; and the body’s entire lower half (see Figure 2).
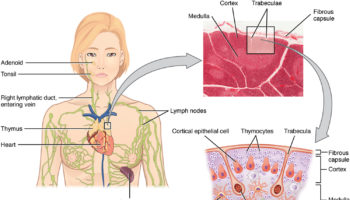
After leaving the lymph nodes, the largest collecting lymphatic vessels converge to form lymph trunks. The lymph trunks drain into the largest lymphatic vessels, the lymph ducts (Figures 1 and 2). Whereas some individuals have two lymph ducts, others have just one. Lymphatic ducts empty lymph fluid into the venous system. The two lymphatic ducts of the body are the right lymphatic duct and the thoracic duct. The thoracic duct is the larger of the two and responsible for lymph drainage from the entire body except for the right sides of the head and neck, the right side of the thorax, and the right upper extremity which are primarily drained by the right lymphatic duct (see Figure 2) 1.
Lymph Trunks
After leaving the lymph nodes, the largest collecting lymphatic vessels converge to form lymph trunks. These trunks drain large areas of the body and are large enough to be found by a skilled dissector. The five major lymph trunks, from inferior to superior, are as follows:
- Lumbar trunks. These paired trunks, which lie along the sides of the aorta in the inferior abdomen, receive all lymph draining from the lower limbs, the pelvic organs, and from some of the anterior abdominal wall.
- Intestinal trunk. This unpaired trunk, which lies near the posterior abdominal wall in the midline, receives fatty lymph (chyle) from the stomach, intestines, and other digestive organs.
- Bronchomediastinal trunks. Ascending near the sides of the trachea, these paired trunks collect lymph from the thoracic viscera and thoracic wall. Intercostal lymph nodes in the upper thorax also drain into bronchomediastinal trunks, whereas intercostal lymph nodes in the lower thorax drain into the thoracic duct.
- Subclavian trunks. Located near the base of the neck, these paired trunks receive lymph from the upper limbs; they also drain the inferior neck and the superior thoracic wall.
- Jugular trunks. Located at the base of each internal jugular vein, these paired trunks drain lymph from the head and neck.
Right Lymphatic Duct
The upper right quadrant of the body is drained by the right jugular, subclavian, and bronchomediastinal trunks. In about 20% of people, these ducts join to form a short right lymphatic duct. When present, right lymphatic duct empties into the neck veins at or near the junction of the right internal jugular and subclavian
veins (Figures 1 and 2). More commonly, the three trunks open independently into the neck veins.
Figure 1. Thoracic duct
Where does the thoracic duct drain?
The thoracic duct delivers lymph into junction between left subclavian and left internal jugular veins.
Right lymphatic duct delivers lymph into junction between right subclavian and right internal jugular veins.
Figure 2. Thoracic duct drainage
Thoracic duct anatomy
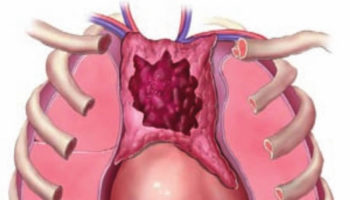
The thoracic duct is 38 to 45 centimeters long and 2 to 5 millimeters in diameter 2. The thoracic duct runs from the superior aspect of the cisterna chyli, a lymph sac at the L2 vertebral level, to the lower cervical spine. From the cisterna chyli, the thoracic duct continues superiorly, running between the aorta and the azygous vein and anterior to the vertebral column. The thoracic duct ascends through the aortic hiatus of the diaphragm entering the posterior mediastinum, still to the right of the vertebral column. It courses posterior to the esophagus at the T7 level and crosses over the midline to the left side of the thorax around the T5 vertebral level. As it continues upward, it runs behind the aorta and to the left of the esophagus ascending 2-3 cm above the clavicle. In the superior mediastinum, it passes behind the left common carotid artery, the vagus nerve, and the internal jugular vein. It then descends to empty into the junction of the left subclavian and internal jugular veins.
The wall of the thoracic duct has three layers: the intima, the media, and the adventitia. It also has a basement membrane. The media is composed of smooth muscle and connective tissue. The smooth muscle contracts regularly to move lymph flow forward. The thoracic duct also contains valves which may be unicuspid, bicuspid, or tricuspid, but are usually bicuspid. At the junction of the lymphatic and venous system, a bicuspid valve prevents venous backflow into the lymphatic system 3.
The thoracic duct course:
- The thoracic duct enters the thoracic cavity through the aortic hiatus
- Ascends to the right of the midline in the posterior mediastinum
- It crosses to the left of midline at the thoracic plane (range T4-T6 vertebral body)
Ascends posterior to the arch of the aorta
At the root of the neck, it arches forward behind the carotid sheath and its content crossing over the dome of the pleura anteriorly to enter the confluence of the left internal jugular and subclavian veins
The thoracic duct relations
Courses along anterior aspects of T12 to T4 vertebral bodies
In posterior mediastinum:
- between aorta and azygos vein
- posterior esophagus
- anterior to right posterior intercostal arteries and termination of hemizygos and accessory hemiazygos vein.
In superior mediastinum:
- posterior to arch of aorta and left subclavian artery
Tributaries:
- posterior mediastinal nodes
- left intercostal nodes
- left bronchomediastinal trunk,
- left jugular nodes
- left subclavian nodes
Thoracic duct anatomic variants
The typical anatomy described above is present in only about 50% of individuals. There are many anatomic variations of the thoracic duct. A cisterna chyli is present in about half of individuals. When embryologic lymphatic trunks converge above the T12 vertebral level, the cisterna chyli is generally absent, but there may be dilation of lower lumbar trunks.
The thoracic duct has variant anatomy in ~40% (range 30-50%) of the population
- double thoracic ducts (i.e. multiple ducts) (~20%)
- aberrant termination: left internal jugular vein, left external jugular vein, azygos vein, brachiocephalic vein or left subclavian vein
- multiple terminal channels from single duct with a typical course (~20%)
- continues on the right to terminate in the right internal jugular vein
In the embryo, portions of a bilateral system of lymphatic trunks anastomose and develop while portions atrophy. Failure of the typical pattern leads to anatomic variations of the thoracic duct. A common variation is a bifid lower aspect of the trunk caused by embryonic right and left lymphatic trunks failing to fuse. Another variation is the lower thoracic duct being replaced by a plexus of lymphatic vessels and forming a single duct higher in the mediastinum. Two rare variations include complete bilateral thoracic ducts and termination of the duct into the azygous system.
Variations in termination also exist. In the majority of cases, the duct terminates on the left side. In 2% to 3% of cases, the duct empties on the right, and bilaterally in up to 1.5% of cases. In over 95% of cases, the thoracic duct terminates in the internal jugular vein, the subclavian vein, or the angle between the two. The remaining 5% include termination in the external jugular vein, vertebral vein, brachiocephalic vein, suprascapular vein, and transverse cervical vein. The thoracic duct can also terminate as a single vessel (up to 87.5%), bilateral ducts (up to 25%), or several terminal branches (up to 7%).
The thoracic duct displays physiologic adaptation to certain disease processes by increasing in diameter. These disease states include congestive heart failure, cirrhosis or the liver, portal hypertension, and malignancy 4.
Thoracic duct function
The function of the thoracic duct is to transport lymph back into the circulatory system. Interstitial fluid is collected by lymph capillaries from the interstitial space. Lymph then moves through lymphatic vessels to lymph nodes. Lymphatic vessels merge to create the lymphatic ducts which drain into the venous system. The thoracic duct delivers an estimated 1.38 mL/kg/hour of lymph to the venous system.
Thoracic duct and right lymphatic duct functions:
- Return excess interstitial fluid (tissue fluid) to the bloodstream.
- Transports absorbed dietary lipids (fats) from the gastrointestinal tract to the blood.
- Return leaked proteins to the blood.
Moreover, in addition to their roles as lymph filters, the lymph nodes along lymphatic collecting vessels fight disease in their roles as lymphoid organs.
As a central structure to lymphatic flow and movement, thoracic duct dysfunction and resulting chyle accumulation is concerning for malignancy. Lymph from organs can drain directly into the thoracic duct without passing a lymph node. This anodal route has been observed for the diaphragm, esophagus, and parts of the lungs. The drainage pattern may play a role in the prognosis of cancers of these organs. This pattern may also explain the presence of distant metastases without lymph node involvement.
The Virchow node, a lymph node located at the base of the neck where the duct generally terminates, can be enlarged in cases of malignancy and may obstruct drainage of the thoracic duct. When there is an obstruction of the thoracic duct, lymph collects in the pleural cavity. This formation of chylothorax can be the first sign of malignancy.
- Rizvi S, Law MA. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jan 25, 2019. Anatomy, Thorax, Mediastinum Superior and Great Vessels.[↩]
- Ilahi M, Ilahi TB. Anatomy, Thorax, Thoracic Duct. [Updated 2018 Dec 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513227[↩]
- Ndiaye A, Di-Marino V, Ba PS, Ndiaye A, Gaye M, Nazarian S. Anatomical variations in lymphatic drainage of the right lung: applications in lung cancer surgery. Surg Radiol Anat. 2016 Dec;38(10):1143-1151[↩]
- Sarkaria IS, Finley DJ, Bains MS, Adusumilli PS, Rizk NP, Huang J, Downey RJ, Rusch VW, Jones DR. Chylothorax and Recurrent Laryngeal Nerve Injury Associated With Robotic Video-Assisted Mediastinal Lymph Node Dissection. Innovations (Phila). 2015 May-Jun;10(3):170-3[↩]