Contents
What is thymus cancer
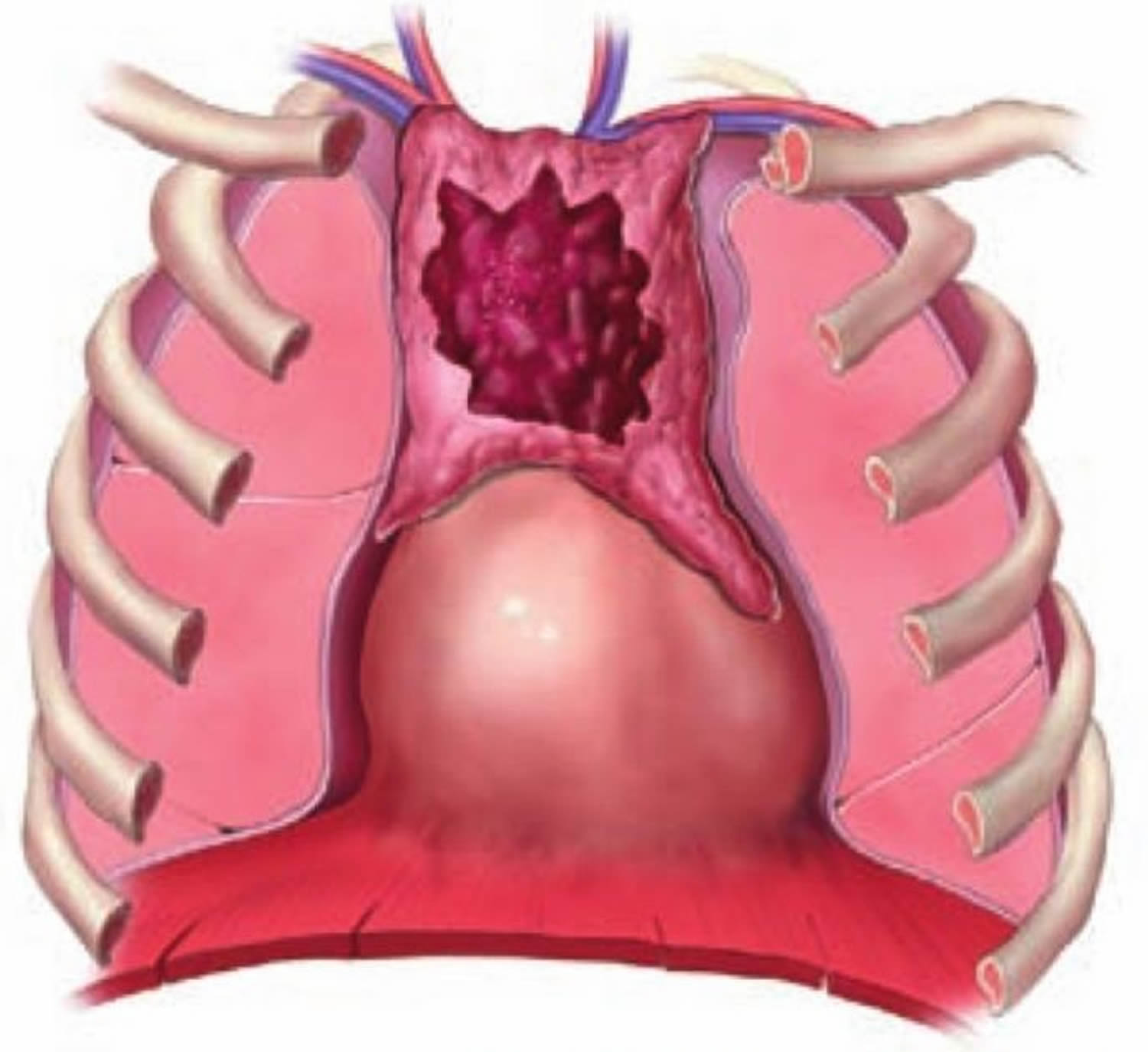
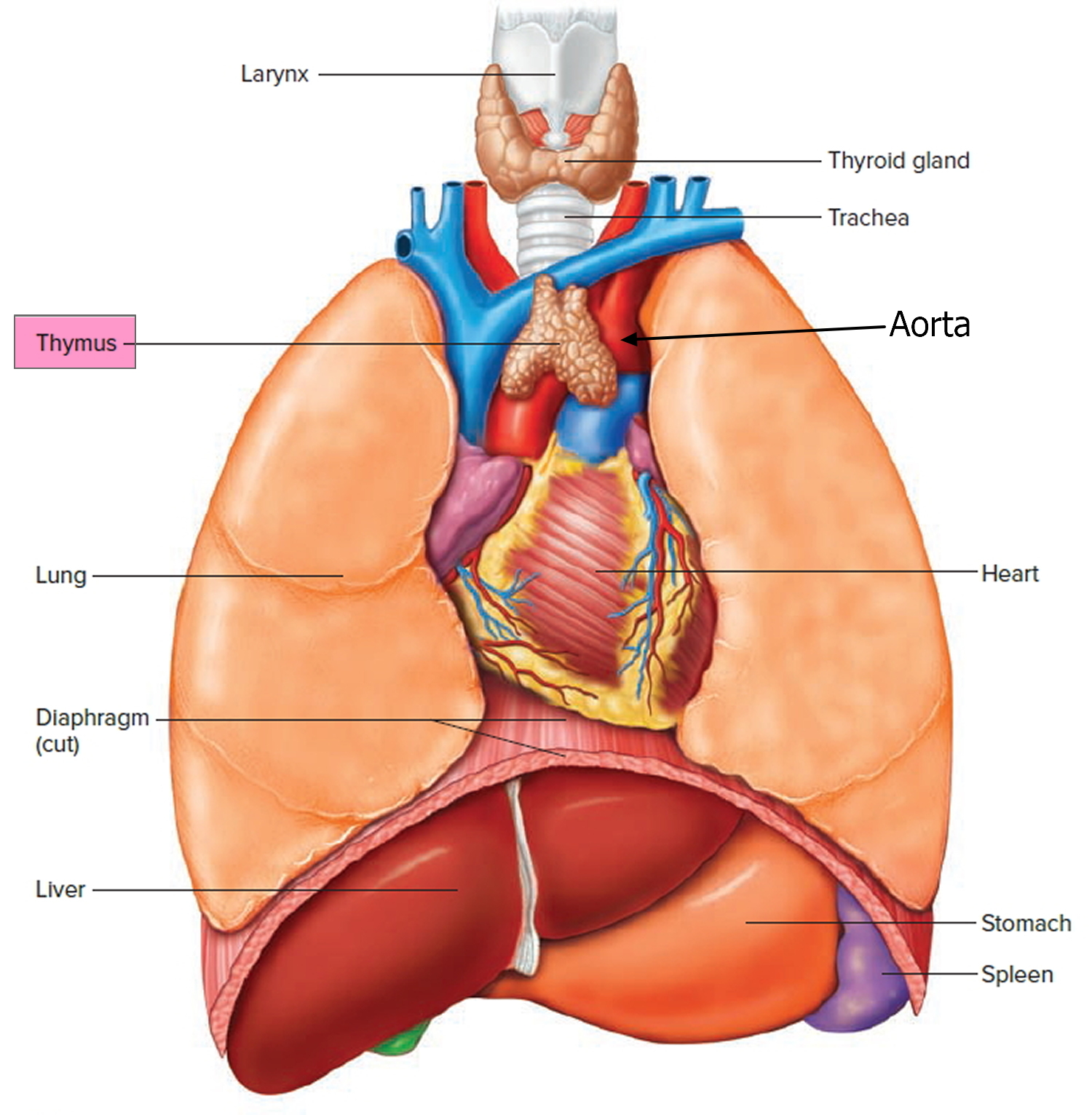
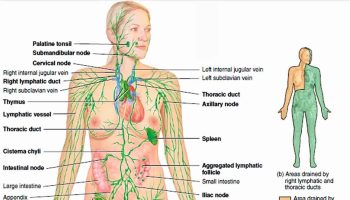
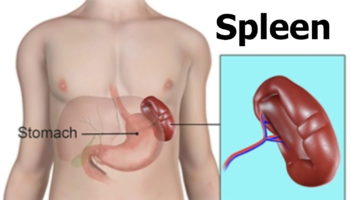
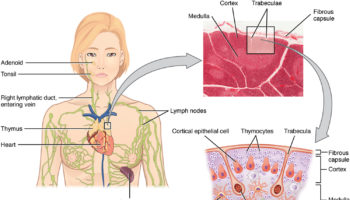
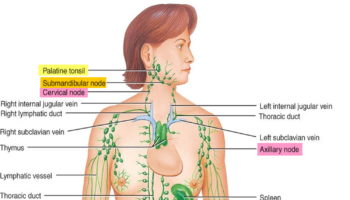
The thymus is a small organ in your upper chest, under your breastbone (see Figure 1 and 2). The thymus is in a part of the chest known as the mediastinum, the space in the chest between the lungs that also contains the heart, part of the aorta, the esophagus (the tube that connects the throat to the stomach), part of the trachea (windpipe), and many lymph nodes. The thymus sits just in front of the aorta and above the heart. Before birth and during childhood, the thymus helps the body make a type of white blood cell – T cells (T lymphocytes). These cells help protect you from infections.
Cancer of the thymus is rare. You are more likely to get it if you have other diseases such as myasthenia gravis, lupus or rheumatoid arthritis 1. Sometimes there are no symptoms. Other times, thymus cancer can cause:
- A cough that doesn’t go away
- Chest pain
- Trouble breathing
Although thymic tumors are the most common tumors in the anterior mediastinum (the front part of the chest cavity), overall they are rare. They occur at a rate of only 1.5 cases for every million people each year in the US. This works out to about 400 cases per year (the exact number diagnosed each year is not known) 2.
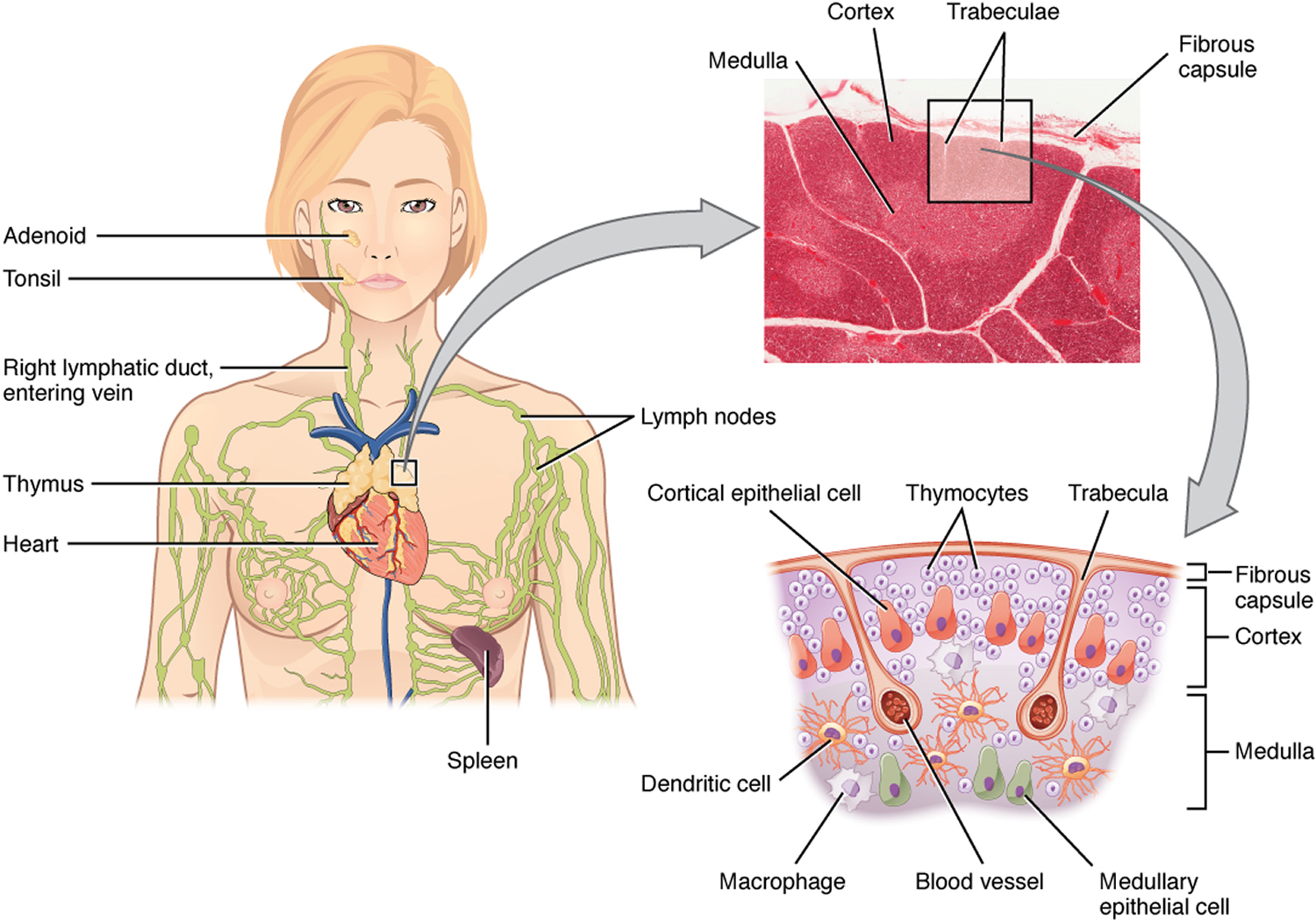
The thymus is an important part of your body’s immune system. During fetal development and childhood, the thymus is involved in the production and maturation of T lymphocytes (also known as T cells), a type of white blood cell. T lymphocytes develop in the thymus and then travel to lymph nodes (bean-sized collections of immune system cells) throughout the body. There they help the immune system protect the body from viruses, fungus, and other types of infections.
The thymus has different types of cells, each of which can develop into different types of cancer:
- Epithelial cells give the thymus its structure and shape. Thymomas and thymic carcinomas, develop from these cells.
- Lymphocytes make up most of the rest of the thymus. Whether in the thymus or in other parts of the body, these immune system cells can develop into cancers called Hodgkin disease and non-Hodgkin lymphoma.
- Kulchitsky cells, or neuroendocrine cells, are much less common cells that normally release certain hormones. These cells can give rise to cancers called carcinoid tumors.
Figure 1. The location and structure of the thymus
Figure 2. Thymus location
Thymomas and thymic carcinomas
Thymomas and thymic carcinomas are tumors that start from thymic epithelial cells 3. Not all doctors agree about the best way to describe and classify these tumors. In the past, thymomas were sometimes divided into benign (non-cancerous) thymomas and malignant (cancerous) thymomas, based on whether they had grown beyond the thymus into other tissues or organs. Now, most doctors think all thymomas are potentially cancerous and the best way to predict how likely they are to come back after treatment is to describe whether they have grown into tissues beyond the thymus (and if so, how far). This is done by the surgeon who notes whether or not the tumor appears attached to nearby organs and by the pathologist who looks at samples from the margins (edges) of the tumor under the microscope.
World Health Organization classification system for thymomas
Most doctors also classify thymomas by how they look under a microscope and by tests done on the tissue samples. This is called the histologic type. The system used for this classification, which was developed by the World Health Organization (WHO), assigns letters to the different types of thymomas.
Type A: The cells in these tumors are spindle-shaped or oval epithelial cells that appear to be fairly normal looking. This is the rarest type of thymoma, but it seems to have the best prognosis (outlook).
Type AB: This type, also known as a mixed thymoma, looks like type A except that there are also areas of lymphocytes mixed in the tumor.
Type B1: This type looks a lot like the normal structure of the thymus. It has a lot of lymphocytes along with normal-appearing thymus cells.
Type B2: This type also has a lot of lymphocytes, but the thymus epithelial cells are larger with abnormal nuclei (the DNA-containing part of the cell).
Type B3: This type has few lymphocytes and mostly consists of thymus epithelial cells that look pretty close to normal.
Type C: This is the most dangerous form and is also known as thymic carcinoma. It contains cells that have a very abnormal appearance under the microscope. The cells may no longer even look like thymus cells. These tumors have often grown into (invaded) nearby tissues and/or metastasized (spread to distant tissues and organs) at the time they are found. This type of thymoma has the worst prognosis (outlook) 3.
Type AB and type B2 are the most common types of thymoma, and type A is the least common. As you go from A to C, the outlook for survival tends to get worse, with type A having the best outlook, and type C having the worst. Still, for most types of thymoma, the stage (extent of growth and spread) is a better predictor of a person’s outcome.
What Causes Thymus Cancer ?
Not much is known about why thymus cancers develop in some people but not in others 4. Researchers have found some DNA changes that occur more often in thymus cancer cells than in normal cells. DNA is the chemical in each of our cells that makes up our genes — the instructions for how our cells function. However, they are still not certain why these changes occur in some people, exactly how the changes occur, and how the changes might cause cancer to form.
- Because we do not know what causes most thymus cancers, it is not yet possible to know how to prevent them.
What Are the Risk Factors for Thymus Cancer ?
A risk factor is anything that affects your chance of getting a disease such as cancer. Different cancers have different risk factors. For example, exposing the skin to strong sunlight is a risk factor for skin cancer. Smoking is a risk factor for lung cancer and many others.
But risk factors don’t tell us everything. Having a known risk factor, or even several risk factors, does not mean that you will get the disease. And many people who get the disease may not have had any known risk factors.
No specific inherited, environmental, or lifestyle risk factors have been strongly linked to thymoma or thymic carcinoma 5. Some studies have suggested a possible link with exposure to radiation to the upper chest area, but this has not been confirmed. The only known risk factors are age and ethnicity.
Age
The risk of this type of cancer goes up with age. This type of cancer is rare in children and young adults, is seen more often in middle-aged adults, and is most common in those in their 70s.
Ethnicity
In the US, this cancer most common in Asians and Pacific Islanders and least common in Whites and Latinos. It is more common in African Americans than in Whites.
Thymus cancer symptoms
Many thymic tumors are found on an x-ray or scan done for some other reason, before the patient has symptoms 6. The rest are brought to the attention of a doctor after a person starts to have symptoms. These may be related to the tumor itself, or they may be part of a paraneoplastic syndrome.
Although these signs and symptoms might be caused by thymus tumors, they can also be caused by other conditions. Still, if you have any of these problems, it’s important to see your doctor right away so the cause can be found and treated, if needed.
Symptoms caused by the thymus tumor
The thymus is in the middle of the chest, near the airways and certain blood vessels. Tumors in the thymus can press on nearby structures, causing symptoms such as:
- Shortness of breath
- Cough (which may bring up bloody sputum)
- Chest pain
- Trouble swallowing
- Loss of appetite
- Weight loss
The thymus is near the superior vena cava, the main blood vessel bringing blood from the head and upper body to the heart. Tumors that press on this vessel can cause symptoms of superior vena cava syndrome, which can include:
- Swelling in the face, neck, and upper chest, sometimes with a bluish color
- Swelling of the visible veins in this part of the body
- Headaches
- Feeling dizzy or light-headed
Paraneoplastic syndromes
These are conditions that are related to the cancer but that are not caused directly by the tumor mass. For example, people with thymomas may develop autoimmune diseases, where the immune system starts to attack the body itself. Part of the normal function of the thymus is to help keep the immune system in check, which may help explain why this happens.
Myasthenia gravis: About 30% to 65% of people with thymomas also have myasthenia gravis. This is by far the most common autoimmune disease associated with thymomas. In this disease, the immune system forms antibodies that block the chemical signals that signal the muscles to move. This causes severe muscle weakness. People with myasthenia gravis tire easily. They may notice problems climbing stairs or walking long distances.
Although patients have decreased muscle strength throughout the body, symptoms caused by weakness of the muscles of the eyes, neck, and chest may be the most troublesome. Weakness of the eye muscles can cause blurred or double vision and drooping eyelids, while weak neck muscles can lead to problems with swallowing. Weakness of the chest muscles and diaphragm can cause problems breathing and shortness of breath.
Many people with thymomas have myasthenia gravis, but most people with myasthenia gravis don’t have thymomas. Many people with myasthenia gravis have other, noncancerous abnormalities of the thymus gland. Myasthenia gravis can be treated by removing the thymus (whether or not a thymoma is present) or with medicines that either strengthen the chemical signals to muscles or weaken the immune attack on the muscles.
Red cell aplasia: Red cell aplasia, in which the body’s ability to make new red blood cells is severely reduced, occurs in about 5% of thymoma patients. Red blood cells carry oxygen from the lungs to other tissues of the body. Reduced red blood cell production causes anemia (low red blood cell counts). Symptoms of anemia can include weakness, dizziness, shortness of breath, and tiring easily. The usual treatment is to remove the thymus gland.
Hypogammaglobulinemia: Hypogammaglobulinemia is a disorder in which the body makes low amounts of infection-fighting antibodies (also known as gamma globulins). This leaves the person susceptible to infections. About 5% to 10% of thymoma patients develop hypogammaglobulinemia. About 10% of patients with hypogammaglobulinemia have a thymoma. Removing the thymus does not help correct this disease.
Other autoimmune diseases: Many other autoimmune diseases have also been linked to thymoma. However, they are much less common than myasthenia gravis, pure red cell aplasia, or hypogammaglobulinemia. Some examples include:
- Systemic lupus erythematosus
- Polymyositis
- Ulcerative colitis
- Rheumatoid arthritis
- Sjogren (Sjögren) syndrome
- Sarcoidosis
- Scleroderma
Most people who have these autoimmune diseases do not have a thymoma 6.
Can Thymus Cancer Be Found Early ?
Screening is testing for a disease like cancer in people without any symptoms. Thymus cancers are uncommon, and there are no widely recommended screening tests for them. Still, these cancers can sometimes be found early.
About 4 out of 10 people with thymomas have no symptoms when their tumor is found. In most of these cases the tumor is seen by chance on a test (like a chest x-ray or CT scan) that is done for some other reason 7.
Thymomas are often associated with symptoms that are not directly caused by the tumor mass itself. These are called paraneoplastic syndromes (tumor-related conditions). Some of these paraneoplastic syndromes, such as myasthenia gravis, red cell aplasia, and hypogammaglobulinemia. These conditions can be very important in diagnosing some thymomas early because they may be present while the tumor is still at an early stage.
Thymus cancer diagnosis
If there is a reason to think you might have a tumor of the thymus, your doctor will ask you about symptoms and use one or more exams or tests to find out if the disease is really present. Certain signs and symptoms might suggest that a person may have a thymus tumor, but tests are needed to confirm the diagnosis.
Medical history and physical exam
If you have signs or symptoms that suggest you might have a thymus tumor, your doctor will want to take a complete medical history to check for symptoms. You will also be asked about your general health.
A physical exam provides information about possible signs of thymus cancer and other health problems. Patients with thymic cancer will sometimes have a fullness that the doctor can feel in the lower neck area.
Thymomas are often suspected because the patient has signs and symptoms associated with myasthenia gravis, hypogammaglobulinemia, or red cell aplasia.
If symptoms and/or the results of the physical exam suggest a thymus tumor might be present, more tests probably will be done. These might include imaging tests, lab tests, and other procedures.
Imaging tests
Imaging tests use x-rays, magnetic fields, or radioactive substances to create pictures of the inside of your body. Imaging tests may be done for a number of reasons, including to help find a suspicious area that might be cancerous, to learn how far cancer may have spread, and to help determine if treatment has been effective.
Chest x-ray
A chest x-ray may be the first imaging test a doctor orders if he or she suspects a problem in the middle of the chest. It may be able to show if there is a tumor in the chest. In some cases, a chest x-ray may find tumors in people before they cause any symptoms (when the person is having the x-ray done for another reason). However, some thymomas are small or are in certain places that may not show up on a chest x-ray. If your doctor is still suspicious or if an abnormality appears on the chest x-ray, a CT scan may be ordered.
Computed tomography (CT) scan
The computed tomography (CT) scan is an x-ray procedure that produces detailed cross-sectional images of your body. Instead of taking one picture, like a regular x-ray, a CT scanner takes many pictures as it rotates around you while you are lying on a narrow platform. A computer then combines these into images of slices of the part of your body that is being studied.
Before the test, you may be asked to drink 1 to 2 pints of a liquid called oral contrast. This helps outline abnormal areas in the body. You may also receive an IV line through which a different kind of contrast dye (IV contrast) is injected. This helps better outline structures such as blood vessels in your body.
The injection can cause some flushing (redness and warm feeling that may last hours to days). A few people are allergic to the dye and get hives. Rarely, more serious reactions like trouble breathing and low blood pressure can occur. Medicine can be given to prevent and treat allergic reactions. Be sure to tell the doctor if you have ever had a reaction to any contrast material used for x-rays.
A CT scanner has been described as a large donut, with a narrow table in the middle opening. You will need to lie still on the table while the scan is being done. CT scans take longer than regular x-rays, and you might feel a bit confined by the ring while the pictures are being taken.
CT scans can have several uses:
- CT scans of the chest can spot very small tumors and help determine the exact location and extent of the tumors.
- CT scans can be helpful in staging a cancer (determining the extent of its spread). For example, they can show whether the cancer has spread to nearby lymph nodes or to the liver, kidneys, brain, or other organs.
- CT scans can also be used to guide a biopsy needle precisely into a suspected tumor or metastasis. For this procedure, called a CT-guided needle biopsy, the patient remains on the CT scanning table while a radiologist advances a biopsy needle through the skin and toward the location of the mass. CT scans are repeated until the needle is within the mass. A biopsy sample is then removed and looked at under a microscope.
- During or after treatment, CT scans may be used to see whether tumors are shrinking or have recurred (come back) in other parts of the body.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans provide detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. The energy from the radio waves is absorbed and then released in a pattern formed by the type of body tissue and by certain diseases. A computer translates the pattern into very detailed images of parts of the body. A contrast material called gadolinium is often injected into a vein before the scan to better see details.
MRI scans may be a little more uncomfortable than CT scans. They take longer — often up to an hour. You may be placed inside a large cylindrical tube, which is confining and can upset people with a fear of enclosed spaces (claustrophobia). For people who cannot tolerate a regular MRI machine, there are special, more open MRI machines that can be used instead in some cases. The MRI machine makes buzzing and clicking noises that you might find disturbing. Some places will provide earplugs to help block this out.
MRI of the chest may be done to look more closely at thymus tumors. They are most often used when the patient can’t have a CT scan for medical reasons (like problems with the IV contrast). MRI images are also particularly useful in looking for cancer that may have spread to the brain or spinal cord.
Positron emission tomography (PET) scan
For a PET scan, you receive an injection of a substance that contains a radioactive atom. This is usually glucose (a type of sugar), but other substances that are attracted to thymoma cells may also be used. The amount of radioactivity is very low. The cancer cells in the body absorb large amounts of the radioactive substance. A special camera can then be used to create a picture of areas of radioactivity in the body. The picture is not finely detailed like a CT or MRI scan, but it can provide helpful information about your whole body.
A PET scan can help give the doctor a better idea of whether an abnormal area seen on another imaging test is a tumor or not. If you have already been diagnosed with cancer, your doctor may use this test to see if the cancer has spread to lymph nodes or other parts of the body. A PET scan can also be useful if your doctor thinks the cancer may have spread but doesn’t know where.
Certain machines are able to perform both a PET and CT scan at the same time (PET/CT scan). This lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed appearance of that area on the CT. Combined PET/CT is used more often than PET (alone) in looking at thymomas.
Blood tests
Blood tests can’t be used to diagnose thymomas directly, but they may still be helpful in some situations. For example, tests may be done to look for certain antibodies in the blood of people who may have myasthenia gravis or other autoimmune disorders. Other blood tests may be done to make sure a mass in the middle of the chest isn’t a germ cell tumor or part of the thyroid gland.
If a thymoma is diagnosed, blood cell counts and blood chemistry tests are done to get an idea of a person’s overall health, especially if surgery is planned. Also, tests for myasthenia gravis (MG) will be done before any surgery. This is because MG is very common in patients with a thymoma, and, if left untreated, it can cause problems with anesthesia during surgery. People getting chemotherapy also have regular blood tests to make sure the drugs aren’t having unwanted effects on the bone marrow, kidneys, or other organs.
Types of biopsy procedures
Although signs, symptoms, and imaging tests can suggest that a thymic tumor is likely to be present, doctors can’t be certain of the diagnosis without looking at the tumor under a microscope.
For most cancers, removal of a small sample of the tumor (known as a biopsy) is needed to confirm whether a tumor is present and, if so, to determine its type. For thymomas, this is rarely done because doctors can usually tell that the tumor is very likely a thymoma based on how it looks on imaging tests. Because of this, doctors often remove the entire tumor rather than do a biopsy. If the doctor suspects a different type of tumor, a biopsy may be done before surgery. Most often, a needle biopsy is done. A biopsy may also be done to confirm the diagnosis if the tumor can’t be removed completely with surgery. This can allow the cancer to be treated with things other than surgery.
Needle biopsy
Tumors in the chest are sometimes sampled by needle biopsy. A long, hollow needle is passed through the skin in the chest. Imaging tests such as CT scans are used to guide the needle into the tumor so that a small sample can be removed to be looked at under the microscope. This procedure is done without a surgical incision or overnight hospital stay.
A possible downside of this test is that it might not always get enough of a sample to make an accurate diagnosis or allow the doctor to get a good sense of the extent of the tumor.
Surgical biopsy
In most cases, if the doctor believes that the patient has thymoma (based on CT findings and lab tests, especially in a patient with a paraneoplastic syndrome) and it can be removed with surgery, the doctor may operate without any biopsy. This can both provide enough of a sample for a diagnosis and treat the tumor at the same time. The specimen is sent to the lab after surgery to confirm the diagnosis.
How Is Thymus Cancer Staged ?
Staging is the process of finding out if and how far a cancer has spread. Your treatment and prognosis (the outlook for chances of survival) depend, to a large extent, on the cancer’s stage.
Masaoka staging system 8
There is no single staging system for thymomas that all doctors agree on, perhaps because these tumors are so uncommon 8. The system most often used to stage thymomas is the Masaoka system, although other systems exist. Staging in the Masaoka system is based on:
- The extent of disease as seen on imaging tests such as CT or MRI scans
- Whether the surgeon finds the tumor hard to separate from nearby tissues (indicating the tumor is invasive)
- Whether the doctor sees tumor cells beyond the thymus when looking at the tumor sample under the microscope
The Masaoka system has 4 main stages.
Stage I
The thymoma is non-invasive. That is, it has not spread into the capsule (outer layer) of the thymus.
Stage II, which is divided into IIA and IIB
- Stage IIA: The thymoma is growing into the capsule (the outer layer of tissue of the thymus).
- Stage IIB: The tumor has grown through the capsule into the nearby fatty tissue, and may be stuck to the mediastinal pleura (the thin layer covering the space between the 2 lungs) or the pericardium (the tissue sac containing the heart).
Stage III
The thymoma is growing into nearby tissues or organs of the lower neck or upper chest area, including the pericardium (the tissue sac containing the heart), the lungs, or the main blood vessels going into or exiting from the heart (the superior vena cava and aorta).
Stage IV, which is divided into IVA and IVB
- Stage IVA: The thymoma has spread widely throughout the pleura (lining of the lungs and chest wall) and/or pericardium.
- Stage IVB: The thymoma has spread to distant organs. The most common sites of spread are bone, the liver, and the lungs.
Resectable versus unresectable cancer
The Masaoka staging system divides thymomas into different groups that help give doctors an idea about a person’s prognosis (outlook). But for treatment purposes, doctors often use a simpler system based on whether these cancers are likely to be resectable (where all visible tumor can be removed by surgery) or unresectable.
In general terms, almost all stage I and II thymomas, most stage III thymomas, and even some stage IV thymomas are potentially resectable, but there are exceptions. Resectability is based on whether the tumor appears to have grown into nearby tissues or spread to distant sites, as well as on whether or not a person is healthy enough to have surgery.
Surgery is typically part of the treatment plan whenever possible. In some cases, other forms of treatment such as radiation therapy or chemotherapy may be recommended as well.
Other prognostic factors
The prognosis (the outlook for chances of survival) after treatment of a thymoma depends to a large extent on its stage. But other features are important as well, such as its cellular classification and whether the surgeon is able to remove the entire tumor.
Thymus cancer treatment
Factors important in choosing a treatment include the type and stage of the cancer, whether or not it is resectable (able to be completely removed with surgery), and whether you have any other serious medical problems. Whether or not a thymus cancer is considered resectable (removable by surgery) is one of the most important factors in determining treatment options. The type of tumor is also important. Thymic carcinomas are more likely to grow and spread quickly than thymomas and often require more aggressive treatment. Because thymic cancer is rare, it has been hard to do large studies looking at treatments and comparing one against another. That’s why in many cases the best way to treat this cancer is not always clear
Selecting a treatment plan is an important decision, and you should take the time to think about all of your choices. If time permits, it is often a good idea to seek a second opinion. A second opinion can provide more information and help you feel more confident about the treatment plan chosen.
The main treatments for thymus cancer are:
- Surgery
- Radiation
- Chemotherapy
Surgery
Surgery is the removal of the tumor and some surrounding healthy tissue during an operation. For thymoma, surgery is usually done by a thoracic surgeon, a doctor who specializes in surgery of the chest.
Surgery is the most common treatment for early-stage thymoma 9. For early-stage thymoma, it is also often the only treatment needed. The most common type of surgery for thymoma is called a median sternotomy. During a median sternotomy, the breastbone is split, and the thymoma and the tissue surrounding the tumor are removed. Sometimes, for smaller, early-stage tumors, a less invasive type of surgery using smaller incisions and a laparoscope may be an option. A laparoscope is a thin, lighted tube with a small camera on the end. With some laparoscopes, the surgeon can work with small instruments through the tube.
Later-stage thymoma treatment options may include surgery to remove as much of the tumor as possible when the entire thymoma cannot be removed with surgery. This is called debulking surgery and may provide some relief of symptoms. If the thymoma has spread to the lining of the lung, surgery may also include the removal of the lung lining or a portion of the lung.
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. A radiation therapy regimen (schedule) usually consists of a specific number of treatments given over a set period of time.
External-beam radiation therapy can be used as the only treatment after surgery. Or, it may be combined with chemotherapy. For patients with later-stage disease, radiation therapy is often recommended after the thymoma has been surgically removed.
Side effects from radiation therapy may include fatigue, mild skin reactions, difficulty swallowing, upset stomach, and loose bowel movements. Most side effects go away soon after treatment is finished.
Chemotherapy
Chemotherapy is the use of drugs to destroy cancer cells, usually by stopping the cancer cells’ ability to grow and divide. Chemotherapy is given by a medical oncologist, a doctor who specializes in treating cancer with medication.
Systemic chemotherapy gets into the bloodstream to reach cancer cells throughout the body. Common ways to give chemotherapy include an intravenous (IV) tube placed into a vein using a needle or in a pill or capsule that is swallowed (orally).
A chemotherapy regimen (schedule) usually consists of a specific number of cycles given over a set period of time. A patient may receive 1 drug at a time or combinations of different drugs at the same time. Common drugs for thymoma or thymus carcinoma include 9.:
- Carboplatin (Paraplatin)
- Cisplatin (Platinol)
- Cyclophosphamide (Neosar)
- Doxorubicin (Adriamycin)
- Etoposide (Toposar, VePesid)
- Ifosfamide (Ifex)
- Octreotide (Sandostatin)
- Paclitaxel (Taxol)
- Pemetrexed (Alimta)
The common drug combinations for thymoma or thymic carcinoma include:
- Carboplatin and paclitaxel
- Cyclophosphamide, doxorubicin, and cisplatin
- Etoposide and cisplatin
These chemotherapy combinations are sometimes used to shrink the tumor before surgery if the thymoma is found at a later stage 9. Chemotherapy may also be used for people who have stage IVB/advanced thymoma or recurrent thymoma that cannot be completely removed with surgery. Recurrent thymoma is thymoma that has come back after treatment.
The side effects of chemotherapy depend on the individual, the type of drug, and the dose used, but they can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away once treatment is finished.
Targeted therapy
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells.
Recent studies show that not all tumors have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumor. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, many research studies are taking place now to find out more about specific molecular targets and new treatments directed at them.
For thymus tumors, anti-angiogenesis therapy may be an option 9. Anti-angiogenesis therapy is a type of targeted therapy. It is focused on stopping angiogenesis, which is the process of making new blood vessels. Because a tumor needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to “starve” the tumor. The 2 targeted therapies used for thymic tumors include 9:
- Everolimus (Afinitor, Zortress)
- Sunitinib (Sutent).
Metastatic thymus cancer
If cancer spreads to another part in the body from where it started, doctors call it metastatic cancer. If this happens, it is a good idea to talk with doctors who have experience in treating it. Doctors can have different opinions about the best standard treatment plan. Also, clinical trials might be an option. Learn more about getting a second opinion before starting treatment, so you are comfortable with your treatment plan chosen.
Your treatment plan may include a combination of surgery, radiation therapy, chemotherapy, and targeted therapy. Sometimes, when thymoma is metastatic and growing very slowly, your health care team may recommend no treatment for a period of time. You will be closely monitored during this time. When thymoma has spread to another location in the body, it is unlikely that any of the treatments will make the cancer go away forever. Palliative care will also be important to help relieve symptoms and side effects.
Resectable thymus cancers
For patients with resectable cancers (almost all stage I and II thymus cancers, most stage III cancers, and small number of stage IV cancers), surgery offers the best chance for long-term survival if it can be tolerated. This typically includes removal of the entire thymus and, depending on the extent of the disease, maybe parts of nearby organs or blood vessels as well.
Early stage thymomas (such as stage I and II) do not usually require further treatment after surgery as long as the tumor was removed completely. For early thymomas, radiation therapy may be considered if there is concern that any tumor was left behind.
Patients with more advanced stage thymomas (such as stages III and IV) may be treated with radiation after surgery, even if all of the tumor was removed. If the tumor couldn’t be removed completely, radiation therapy is usually given after surgery. Depending on how much cancer was left behind, chemotherapy (chemo) may be added as well.
Thymic carcinomas are more likely to come back after treatment. Patients with stage I tumors may not need further treatment if the tumor was removed completely. If the tumor is more advanced, or some might have been left behind, patients are typically treated with radiation after surgery. The radiation may be given with chemo as well, especially if some of the cancer is left behind after surgery.
Unresectable thymus cancers
Unresectable cancers are those that cannot be removed with surgery. This group includes cancers that are too close to vital structures or that have spread too far to be removed completely (which includes many stage III and most stage IV cancers), as well as cancers in people who are too ill for surgery.
In some cases, doctors may advise giving chemo, radiation therapy, or both first to try to make the tumor resectable. If it shrinks enough, surgery is done. This is then followed by further treatment with chemo or radiation therapy.
Surgery may be the first treatment for some unresectable cancers, to try to remove as much of the tumor as possible. This is known as debulking. Radiation therapy and/or chemo are then given. The hope is that the surgery may help the other treatments work better and may help people live longer, even if it doesn’t cure the cancer. Studies of this approach have had mixed results.
For patients who can’t have surgery, either because the cancer has spread too far or because they are too sick from other serious medical conditions, chemo and radiation therapy are the main treatment options.
Because unresectable cancers can be hard to treat, taking part in a clinical trial of a newer form of treatment may be a reasonable option.
Recurrent thymus cancer
When cancer comes back after treatment it is called recurrent. Recurrence can be local (in or near the same place it started) or distant (spread to organs such as the liver or bone).
Thymomas most often come back locally. Thymic carcinomas can also come back locally and in nearby lymph nodes, but they may also spread to liver, lungs, and bone.
Treatment for thymus cancer that has recurred (come back) after initial treatment depends on the location of the recurrence and on what the original treatment was. If the recurrence is not too widespread, surgery may be an option and would offer the best chance for long-term survival. But in most cases, the treatment options may be limited to radiation therapy and/or chemo. These treatments can often be effective in controlling the cancer for a time, although they are very unlikely to result in a cure.
Because recurrent cancers can often be hard to treat, clinical trials of new types of treatment may be a good option.
Thymus cancer survival rate
The 5-year survival rate refers to the percentage of patients who live at least 5 years after their cancer is diagnosed 10. Of course, many people live much longer than 5 years (and many are cured). Although many patients live much longer than this, it isn’t always an indication that the cancer has been cured, as some thymus tumors are very slow growing, and others may return in some people several years after treatment.
To get 5-year survival rates, doctors have to look at people who were treated at least 5 years ago. Treatment may have improved since then which could result in a more favorable outlook for people now being diagnosed with thymus cancer.
Because thymus cancers are not common, it is hard to find accurate survival rates based on the stage of the cancer. The numbers below come from a large series of patients treated in Japan between 1990 and 1994. They look separately at patients with thymoma (types A, AB, and B) and thymic carcinoma (type C thymoma). Also, these are observed survival rates. People with thymus cancer can die of other things, and these numbers don’t take that into account.
Table 1. Thymoma stages and 5 year survival rate
| Stage of thymoma | 5-year observed survival rate |
| I | 74% |
| II | 73% |
| III | 64% |
| IV | 45% |
Table 2. Thymus carcinoma stages and 5 year survival rate
| Stage of thymic carcinoma | 5-year observed survival rate |
| I and II | 74% |
| III | 33% |
| IV | 24% |
- Thymus Cancer. Medline Plus. https://medlineplus.gov/thymuscancer.html[↩]
- What Are the Key Statistics About Thymus Cancers ? American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/about/key-statistics.html[↩]
- What Is Thymus Cancer ? American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/about/what-is-thymus-cancer.html[↩][↩]
- What Causes Thymus Cancer ? American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/causes-risks-prevention/what-causes.html[↩]
- What Are the Risk Factors for Thymus Cancer ? American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/causes-risks-prevention/risk-factors.html[↩]
- Signs and Symptoms of Thymus Cancers. American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/detection-diagnosis-staging/signs-symptoms.html[↩][↩]
- Can Thymus Cancer Be Found Early ? American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/detection-diagnosis-staging/detection.html[↩]
- How Is Thymus Cancer Staged ? American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/detection-diagnosis-staging/staging.html[↩][↩]
- Thymoma: Treatment Options. American Society of Clinical Oncology. http://www.cancer.net/cancer-types/thymoma/treatment-options[↩][↩][↩][↩][↩]
- Survival Rates for Thymus Cancer. American Cancer Society. https://www.cancer.org/cancer/thymus-cancer/detection-diagnosis-staging/survival-rates.html[↩][↩][↩]