Contents
What is transverse myelitis
Transverse myelitis is an inflammatory disorder of the spinal cord leading to loss of muscle power, sensory symptoms (pins and needles) and bladder and bowel dysfunction. The spinal cord carries nerve signals to and from the brain through nerves that extend from each side of the spinal cord and connect to nerves elsewhere in the body. The term myelitis refers to inflammation of the spinal cord; transverse refers to the pattern of changes in sensation—there is often a band-like sensation across the trunk of the body, with sensory changes below. Transverse myelitis is uncommon but not rare, the annual incidence (the number of new cases per year) of transverse myelitis in the United States is around 4.6 per million per year 1. The incidence of idiopathic transverse myelitis is about 1.34-4.6 per million per year 2. However, a study by Young and his co-workers found much higher numbers (3-5 times higher) in the Australian population 2. It is estimated that about 1,400 new cases of transverse myelitis are diagnosed each year in the United States.
Transverse myelitis has a bimodal distribution with two distinct peaks: between 10 and 19 years and 30 and 39 years. Transverse myelitis shows no racial, familial or gender predilection 3. About 28% of reported cases of transverse myelitis are in pediatric population 4.
Transverse myelitis does not appear to be genetic or run in families.
Transverse myelitis may occur alone or in combination with disease elsewhere in the nervous system. Causes of transverse myelitis include infections, immune system disorders, and other disorders that may damage or destroy myelin (demyelination), loss of the fatty tissue the insulating substance that covers nerve cell fibers. Inflammation within the spinal cord interrupts communications between nerve fibers in the spinal cord and the rest of your body, affecting sensation and nerve signaling below the injury. Similar symptoms may also occur in spinal cord ischemia (loss of blood flow). Transverse myelitis may occur as a complication of such disorders as neuromyelitis optica, multiple sclerosis, smallpox, measles, or chickenpox. In some patients, no cause can be found despite extensive investigation.
Symptoms include pain, sensory problems, weakness in the legs and possibly the arms, and bladder and bowel problems. The symptoms may develop suddenly (over a period of hours) or over days or weeks. Almost all patients with transverse myelitis develop leg weakness of varying degrees of severity. Fewer will experience arm problems. Pain and temperature appreciation are lessened in most patients. Progression to immobility may be rapid and patients may be immobile within hours or days of the onset of symptoms.
Although some people recover from transverse myelitis with minor or no residual problems, the healing process may take months to years. Others may suffer permanent impairments that affect their ability to perform ordinary tasks of daily living. Some individuals will have only one episode of transverse myelitis; other individuals may have a recurrence, especially if an underlying illness caused the disorder.
The diagnosis is made using a combination of clinical examination and investigations such as spinal cord MRI (magnetic resonance imaging). In the majority of patients, blood tests and a lumbar puncture will be required before a definite cause can be found.
There is no cure for transverse myelitis. Treatments to prevent or minimize permanent neurological deficits include corticosteroid and other medications that suppress the immune system, plasmapheresis (removal of proteins from the blood), or antiviral medications.
Spinal cord
The spinal cord is a slender column of nervous tissue that passes downward from the brain into the vertebral canal. Although continuous with the brain, the spinal cord begins where nervous tissue leaves the cranial cavity at the level of the foramen magnum.
The spinal cord is not uniform in diameter along its length. In the neck region, a thickening in the spinal cord, called the cervical enlargement, occurs in the region associated with the origins of spinal nerves from the cervical spines to thoracic spine T1 giving rise to nerves to the upper limbs. A similar thickening in the lower back, the lumbosacral enlargement, occurs in the region associated with the origins of spinal nerves thoracic spine T 11 to Sacral S3 giving rise to nerves to the lower limbs. The spinal cord tapers to a point and ends near the intervertebral disc that separates the first (L1) and second lumbar (L2) vertebrae, adults, although it can end as high as thoracic vertebra T12 or as low as the disc between vertebrae lumbar vertebrae L2 and L3. From this point, nervous tissue, including axons of both motor and sensory neurons, extends downward to become spinal nerves at the remaining lumbar and sacral levels forming a structure called the cauda equina (horse’s tail).
The distal end of the cord (the conus medullaris) is cone shaped. A fine filament of connective tissue (the pial part of the filum terminale) continues inferiorly from the apex of the conus medullaris.
A nerve is a cordlike organ composed of numerous nerve fibers (axons) bound together by connective tissue. If you compare a nerve fiber to a wire carrying an electrical current in one direction, a nerve would be comparable to an electrical cable composed of thousands of wires carrying currents in opposite directions. A nerve contains anywhere from a few nerve fibers to (in the optic nerve) a million. Nerves usually have a pearly white color and resemble frayed string as they divide into smaller and smaller branches. As we move away from the spinal nerves proper, the smaller branches are called peripheral nerves, and their disorders are collectively called peripheral neuropathy.
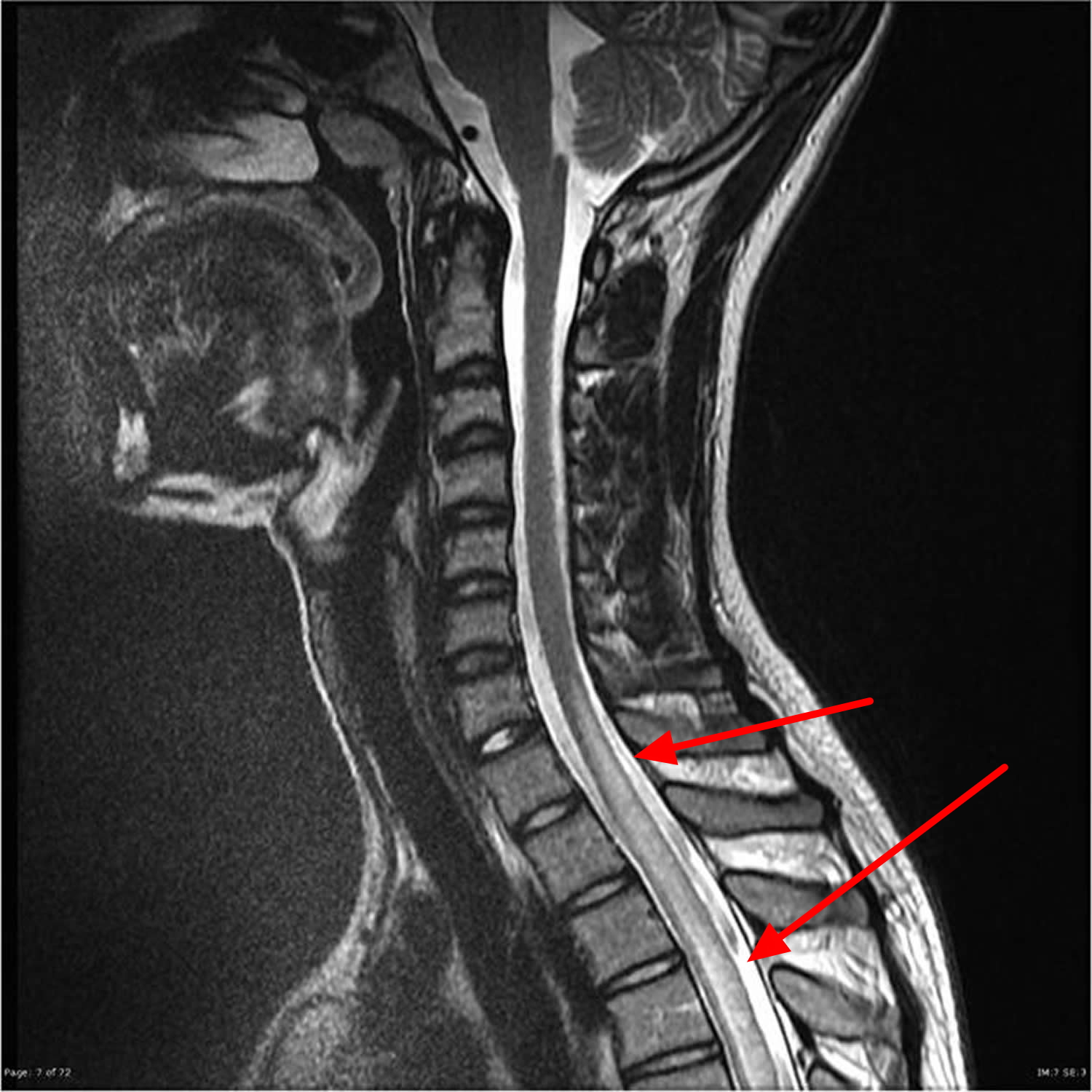
Figure 1. Spinal cord
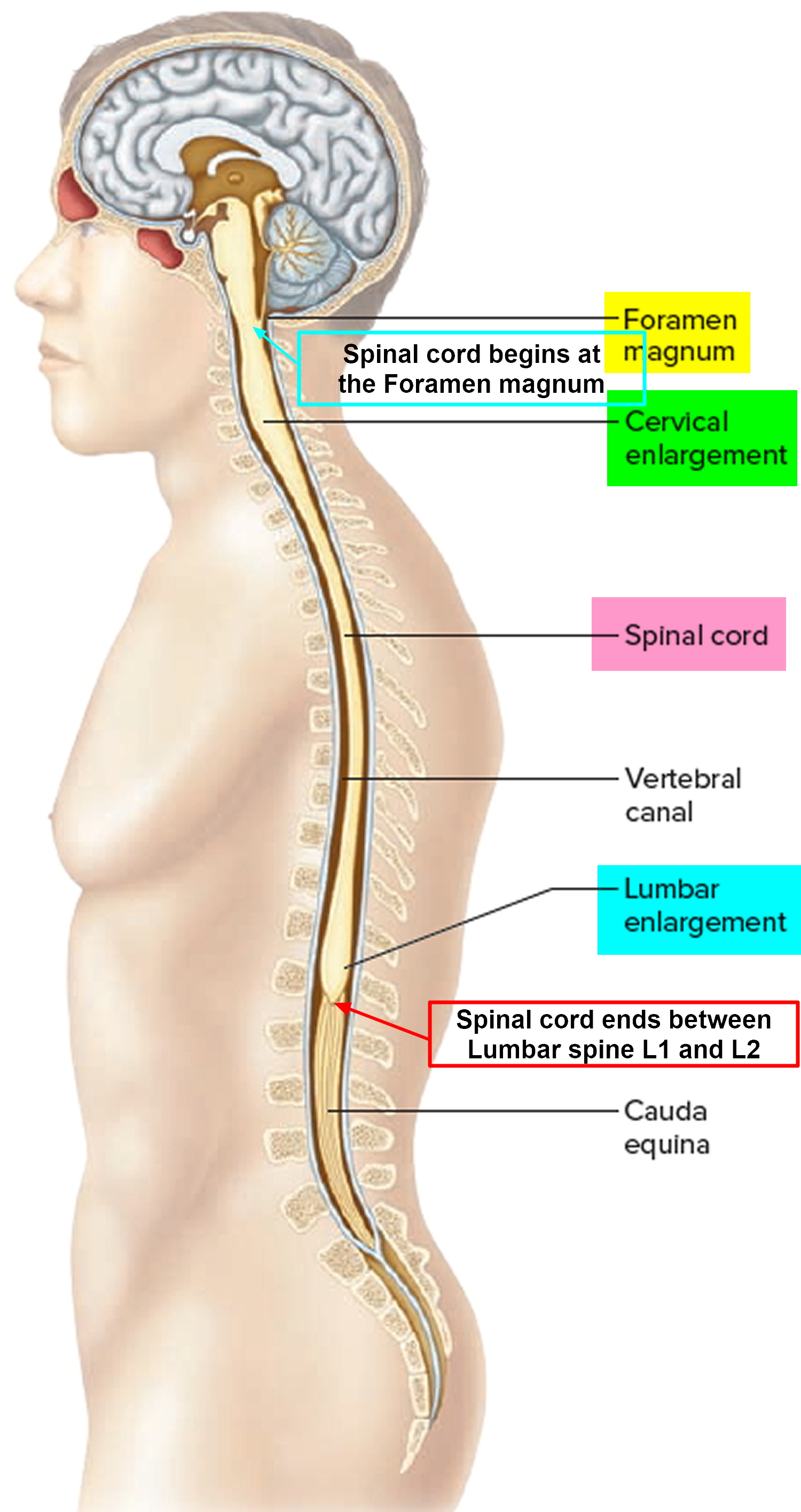
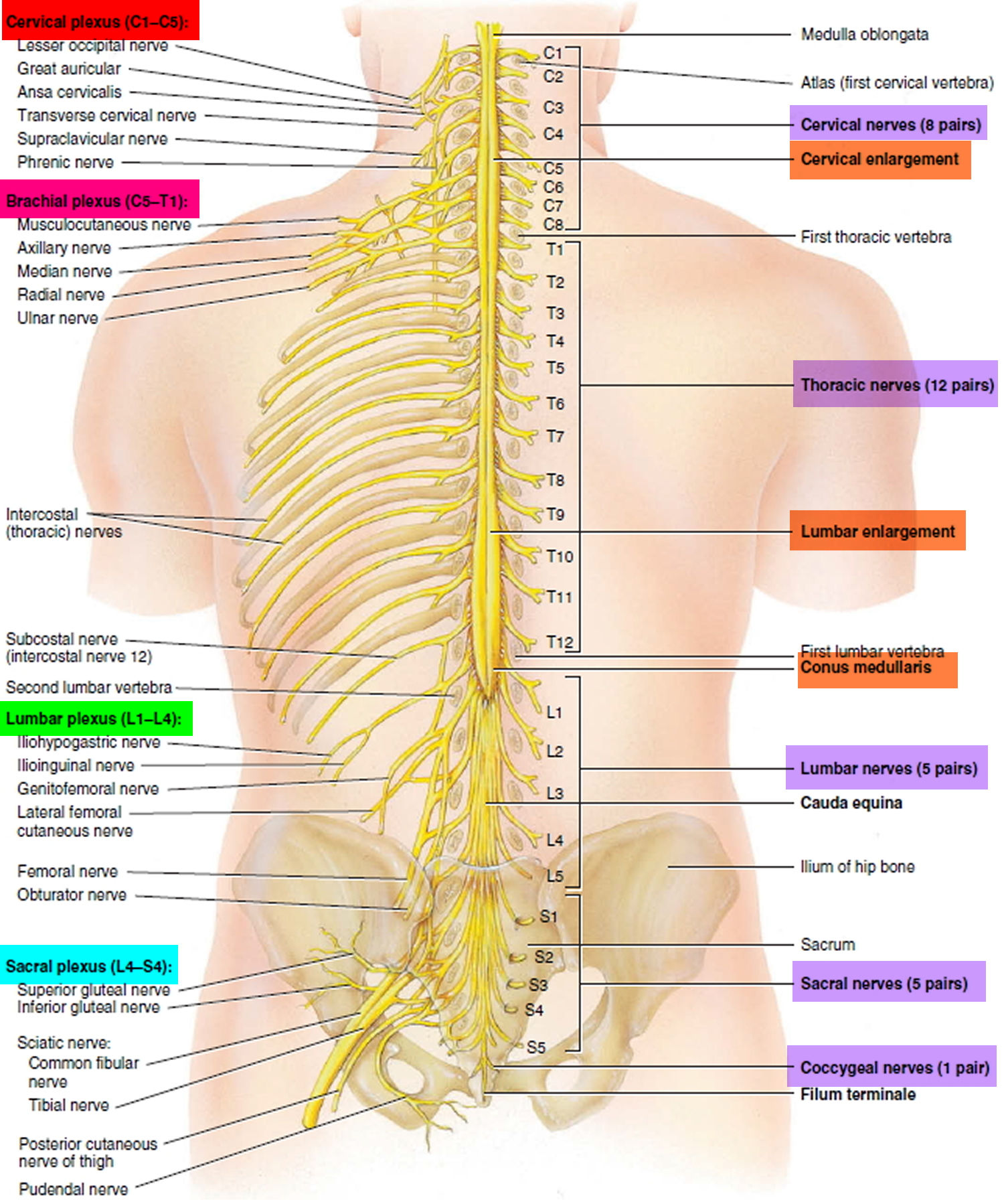
Figure 2. Spinal cord segments
Figure 3. Dermatome (spinal nerves sensory innvervation)
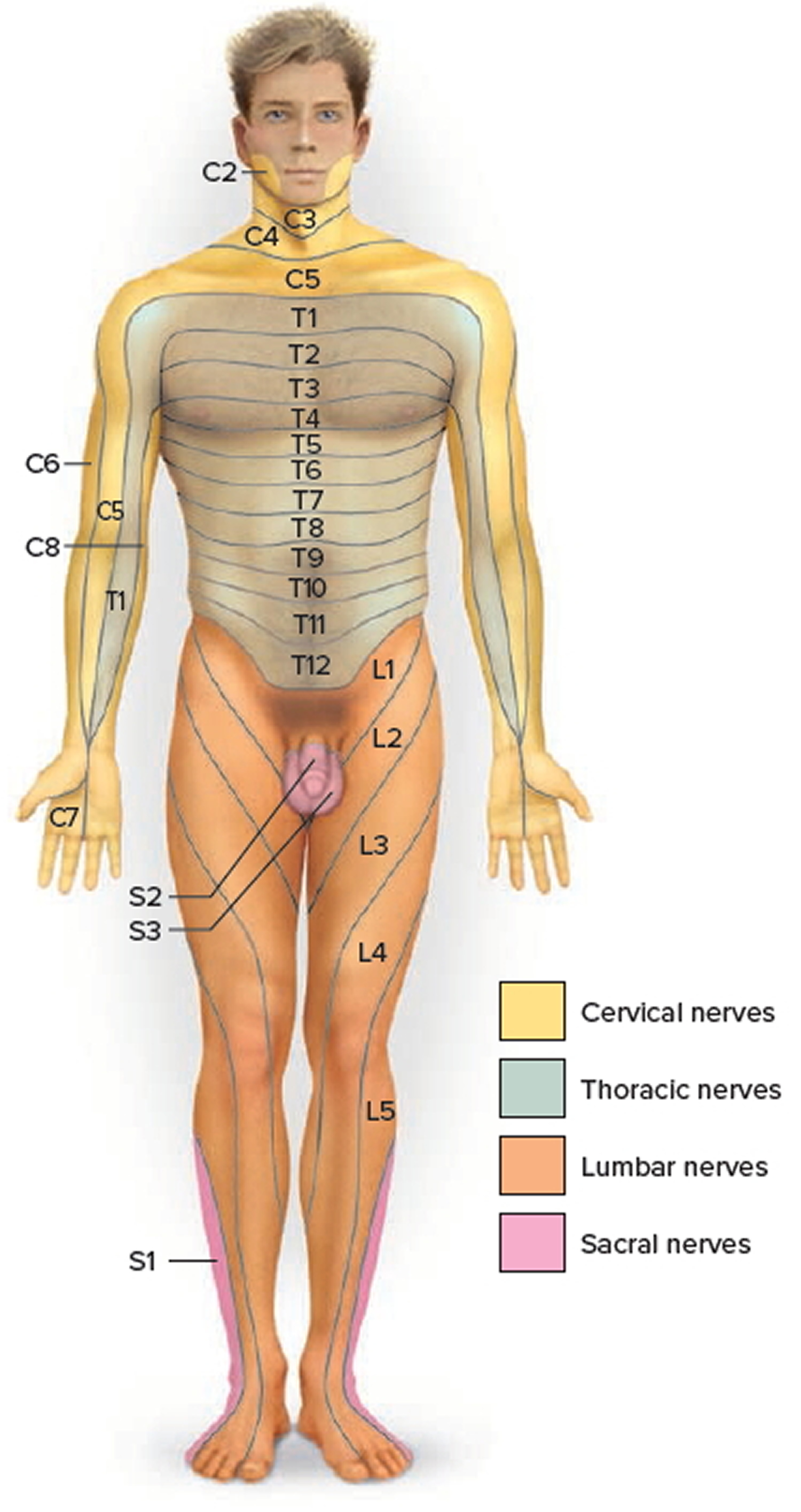
Figure 4. Transverse myelitis – MRI showing mild swelling (blue arrows) involves most of the conus, more patchy towards the tip
Transverse myelitis causes
The exact cause of transverse myelitis and extensive damage to nerve fibers of the spinal cord is unknown in many cases. Cases in which a cause cannot be identified are called idiopathic transverse myelitis. However, looking for a cause is important, as some will change treatment decisions.
The discovery of circulating antibodies to the proteins aquaporin-4 and anti-myelin oligodendrocyte point to a definite cause in some individuals with transverse myelitis. Antibodies are proteins produced by cells of the immune system that bind to bacteria, viruses, and foreign chemicals to prevent them from harming the body. In autoimmune disorders, antibodies incorrectly bind to normal body proteins. Aquaporin-4 is a key protein that carries water through the cell membrane of neural cells. The myelin oligodendrocyte glycoprotein sits on the outer layer of myelin.
A number of conditions appear to cause transverse myelitis, including:
- Immune system disorders. These disorders appear to play an important role in causing damage to the spinal cord. Such disorders are:
- aquaporin-4 autoantibody associated neuromyelitis optica
- multiple sclerosis (MS)
- post-infectious or post-vaccine autoimmune phenomenon, in which the body’s immune system mistakenly attacks the body’s own tissue while responding to the infection or, less commonly, a vaccine
- an abnormal immune response to an underlying cancer that damages the nervous system; or
- other antibody-mediated conditions that are still being discovered.
- Viral infections. It is often difficult to know whether direct viral infection or a post-infectious response to the infection causes the transverse myelitis. Associated viruses include herpes viruses such as varicella zoster (the virus that causes chickenpox and shingles), herpes simplex, cytomegalovirus, and Epstein-Barr; flaviviruses such as West Nile and Zika; influenza, echovirus, hepatitis B, mumps, measles, and rubella.
- Bacterial infections such as syphilis, tuberculosis, actinomyces, pertussis, tetanus, diphtheria, and Lyme disease. Bacterial skin infections, middle-ear infections, campylobacter jejuni gastroenteritis, and mycoplasma bacterial pneumonia have also been associated with the condition.
- Fungal infections in the spinal cord, including Aspergillus, Blastomyces, Coccidioides, and Cryptococcus.
- Parasities, including Toxoplasmosis, Cysticercosis, Shistosomiasis, and Angtiostrongyloides.
- Other inflammatory disorders that can affect the spinal cord, such as sarcoidosis, systemic lupus erythematosus, Sjogren’s syndrome, mixed connective tissue disease, scleroderma, and Bechet’s syndrome.
- Vascular disorders such as arteriovenous malformation, dural arterial-venous fistula, intra spinal cavernous malformations, or disk embolism.
- Vaccinations for infectious diseases — including hepatitis B, measles-mumps-rubella and diphtheria-tetanus vaccines — have occasionally been associated as a possible trigger. However, at this time the association is not strong enough to warrant limiting any vaccine.
In some people, transverse myelitis represents the first symptom of an autoimmune or immune-mediated disease such as multiple sclerosis or neuromyelitis optica.
- Multiple sclerosis (MS), is disease that causes distinctive lesions, or plaques, that primarily affect parts of the brain, spinal cord, and optic nerve—the nerve that carries information from the eye to the brain.
- Neuromyelitis optica (Devic’s disease), is an autoimmune disease of the central nervous system that predominantly affects the optic nerves and spinal cord. Transverse myelitis associated with neuromyelitis optica usually affects both sides of your body. In addition to transverse myelitis, you may experience symptoms of damage to myelin of the optic nerve, including pain in the eye with movement and temporary vision loss. This can happen with or separately from transverse myelitis symptoms. However, some people with neuromyelitis optica don’t experience eye-related problems and might have only recurrent episodes of transverse myelitis. Transverse myelitis associated with an autoimmune disorder may be a warning sign of neuromyelitis optica. Neuromyelitis optica occurs more frequently in people with other autoimmune diseases.
- ”Partial” myelitis—affecting only a portion of the cord cross-section—is more characteristic of multiple sclerosis. Neuromyelitis optica is much more likely as an underlying condition when the myelitis is “complete” (causing severe paralysis and numbness on both sides of the spinal cord).
Transverse myelitis prognosis
The prognosis is variable but in the majority of cases there will be some residual impairment in limb function. Recovery usually begins between 2 and 12 weeks after onset. For some people, recovery may continue for up to 2 years (and in some cases, longer). However, if there is no improvement within the first 3 to 6 months, complete recovery is unlikely (although partial recovery can still occur and still requires rehabilitation). Aggressive acute treatment and physical therapy have been shown to improve outcomes. Some individuals are left with moderate disability (such as trouble walking, nerve sensitivity, and bladder and bowel problems) while others may have permanent weakness, spasticity, and other complications. Myelitis attacks with neuromyelitis optica spectrum disorder tend to be more severe and are associated with less recovery than attacks with multiple sclerosis.
It’s difficult to predict the course of transverse myelitis. Generally, research has shown that a rapid onset of signs and symptoms generally results in poorer recovery and a worse prognosis than do those with a relatively slower onset.
About one-third of people with transverse myelitis fall into one of three categories after an attack:
- No or slight disability. These people experience only minimal lingering symptoms.
- Moderate disability. These people are mobile, but may have difficulty walking, numbness or tingling, and bladder and bowel problems.
- Severe disability. Some people may permanently need a wheelchair and require ongoing assistance with daily care and activities.
Many people with transverse myelitis experience only one episode although recurrent or relapsing transverse myelitis does sometimes occur, particularly when an underlying cause (such as MS or neuromyelitis optica spectrum disorder) can be found. Some people recover completely and then experience a relapse. Others begin to recover and then suffer worsening of symptoms before recovery continues. In all cases of transverse myelitis, physicians will evaluate possible underlying causes such as multiple sclerosis (MS), neuromyelitis optica spectrum disorder, or sarcoidosis, since most people with these underlying conditions can experience a relapse or worsen when acute treatment is discontinued. These individuals should be treated with preventative care to reduce the chance of future relapses.
Transverse myelitis complications
People with transverse myelitis usually experience only one episode. However, complications often linger, including the following:
- Pain, one of the most common debilitating long-term complications of the disorder.
- Stiffness, tightness or painful spasms in your muscles (muscle spasticity). This is most common in the buttocks and legs.
- Partial or total paralysis of your arms, legs or both. This may persist after the first symptoms.
- Sexual dysfunction, a common complication of transverse myelitis. Men may experience difficulty achieving an erection or reaching orgasm. Women may have difficulty reaching orgasm.
- Depression or anxiety, which is common in those with long-term complications because of the significant changes in lifestyle, the stress of chronic pain or disability, and the impact of sexual dysfunction on relationships.
Transverse myelitis symptoms
Transverse myelitis may be either acute (developing over hours to several days) or subacute (usually developing over one to four weeks).
Four classic features of transverse myelitis are:
- Weakness of the legs and arms. People with transverse myelitis may have weakness in the legs that progresses rapidly. If the myelitis affects the upper spinal cord it affects the arms as well. Individuals may develop paraparesis (partial paralysis of the legs) that may progress to paraplegia (complete paralysis of the legs), requiring the person to use a wheelchair.
- Pain. Initial symptoms usually include lower back pain or sharp, shooting sensations that radiate down the legs or arms or around the torso. Pain symptoms vary based on on the part of your spinal cord that’s affected.
- Abnormal sensations. Transverse myelitis can cause paresthesias (abnormal sensations such as burning, tickling, pricking, numbness, coldness, or tingling) in the legs, and sensory loss. Some are especially sensitive to the light touch of clothing or to extreme heat or cold. You may feel as if something is tightly wrapping the skin of your chest, abdomen or legs. Abnormal sensations in the torso and genital region are common. Sometimes the shooting sensations occur when the neck is bent forward and resolve when the neck is brought back to normal position (a condition called Lhermitte’s phenomenon).
- Bowel and bladder dysfunction. Common symptoms include an increased frequency or urge to use the toilet, incontinence, difficulty voiding, and constipation.
Many individuals also report experiencing muscle spasms, a general feeling of discomfort, headache, fever, and loss of appetite, while some people experience respiratory problems. Other symptoms may include sexual dysfunction and depression and anxiety caused by lifestyle changes, stress, and chronic pain.
The segment of the spinal cord at which the damage occurs determines which parts of the body are affected. Damage at one segment will affect function at that level and below. In individuals with transverse myelitis, myelin damage most often occurs in nerves in the upper back, causing problems with leg movement and bowel and bladder control, which require signals from the lower segments of the spinal cord.
Transverse myelitis diagnosis
Physicians diagnose transverse myelitis by taking a medical history and performing a thorough neurological examination. The first step in evaluating a spinal cord condition is to rule out causes that require emergency intervention, such as trauma or a mass putting pressure on the cord. Other problems to rule out include herniated or slipped discs, stenosis (narrowing of the canal that holds the spinal cord), abscesses, abnormal collections of blood vessels, and vitamin deficiencies. Tests that can indicate a diagnosis of transverse myelitis and rule out or evaluate underlying causes include:
- Magnetic resonance imaging (MRI) uses a strong magnetic field and radio waves to produce a cross sectional view or three-dimensional image of tissues, including the brain and spinal cord. A spinal MRI will almost always confirm the presence of a lesion within the spinal cord, whereas a brain MRI may provide clues to other underlying causes, especially MS. In some instances, computed tomography (CT), which uses x-rays and a computer to produce cross-section images of the body or an organ, may be used. Often an injection of a contrast agent is given in the middle of the scan to determine whether the contrast agent leaks out into the spinal cord. Such leakage is a telltale feature of inflammation.
- Blood tests may be performed to rule out various disorders such as HIV infection, vitamin B12 deficiency, and many others. Blood is tested for the presence of autoantibodies (anti- aquaporin-4, anti-myelin oligodendrocyte) and a host of antibodies associated with cancer (paraneoplastic antibodies) that may be found in people with transverse myelitis.
- Lumbar puncture (also called spinal tap) uses a needle to remove a small sample of the cerebrospinal fluid that surrounds the brain and spinal cord. In some people with transverse myelitis, the cerebrospinal fluid contains more protein than usual and an increased number of white blood cells (leukocytes) that help the body fight infections. A spinal tap is important to identify or rule out infectious causes.
If none of these tests suggests a specific cause, the person is presumed to have idiopathic transverse myelitis. In occasional cases, initial testing using MRI and lumbar puncture may show normal results but may need to be repeated in 5-7 days.
Transverse myelitis treatment
The treatment depends on the underlying cause and may include the use of intravenous steroids and other drugs to suppress inflammation. Pain and spasm can be treated with medication if they occur.
Treatments are designed to address infections that may cause the disorder, reduce spinal cord inflammation, and manage and alleviate symptoms.
Initial treatments and management of the complications of transverse myelitis
- Intravenous corticosteroid drugs may decrease swelling and inflammation in the spine and reduce immune system activity. Such drugs may include methylprednisolone or dexamethasone (usually administered for 3 to 7 days and sometimes followed by a tapering off period). These medications may also be given to reduce subsequent attacks of transverse myelitis in individuals with underlying disorders.
- Plasma exchange therapy (plasmapheresis) may be used for people who don’t respond well to intravenous steroids. Plasmapheresis is a procedure that reduces immune system activity by removing plasma (the fluid in which blood cells and antibodies are suspended) and replacing it with special fluids, thus removing the antibodies and other proteins thought to be causing the inflammatory reaction.
- Intravenous immunoglobulin (IVIG) is a treatment thought to reset the immune system. IVIG is a highly concentrated injection of antibodies pooled from many healthy donors that bind to the antibodies that may cause the disorder and remove them from circulation.
- Pain medicines that can lessen muscle pain include acetaminophen, ibuprofen, and naproxen. Nerve pain may be treated with certain antidepressant drugs (such as duloxetine), muscle relaxants (such as baclofen, tizanidine, or cyclobenzaprine), and anticonvulsant drugs (such as gabapentin or pregabalin).
- Antiviral medications may help those individuals who have a viral infection of the spinal cord.
- Medications can treat other symptoms and complications, including incontinence, painful muscle contractions called tonic spasms, stiffness, sexual dysfunction, and depression.
Following initial therapy, it is critical part to keep the person’s body functioning while hoping for either complete or partial spontaneous recovery of the nervous system. This may require placing the person on a respirator in the uncommon scenario where breathing is significantly affected. Treatment is most often given in a hospital or in a rehabilitation facility where a specialized medical team can prevent or treat problems that afflict paralyzed individuals.
Prevention of future transverse myelitis episodes
Most transverse myelitis only occurs once (called monophasic). In some cases chronic (long-term) treatment with medications to modify the immune system response is needed. Examples of underlying disorders that may require long-term treatment include multiple sclerosis and neuromyelitis optica. Treatment of MS with immumodulatory or immunosuppressant medications may be considered when it is the cause of myelitis. These medications include alemtuzumab, dimethyl fumarate, fingomilod, glatiramer acetate, interferon-beta, natalizumab, and teriflunomide, among others.
Immunosuppressant treatments are used for neuromyelitis optica spectrum disorder and recurrent episodes of transverse myelitis that are not caused by multiple sclerosis. They are aimed at preventing future myelitis attacks (or attacks at other sites) and include steroid-sparing drugs such as mycophenolate mofetil, azathioprine, and rituximab.
Rehabilitative and long-term therapy
Many forms of long-term rehabilitative therapy are available for people who have disabilities resulting from transverse myelitis. Strength and functioning may improve with rehabilitative services, even years after the initial episode. Rehabilitative therapy teaches people strategies for carrying out activities in new ways in order to overcome, circumvent, or compensate for permanent disabilities. Although rehabilitation cannot reverse the physical damage resulting from transverse myelitis, it can help people, even those with severe paralysis, become as functionally independent as possible and attain the best possible quality of life.
Common neurological deficits resulting from transverse myelitis include severe weakness, spasticity, or paralysis; incontinence, and chronic pain. In some cases these may be permanent. Such deficits can substantially interfere with a person’s ability to carry out everyday activities such as bathing, dressing, and performing household tasks. Individuals with lasting neurological defects from transverse myelitis typically consult with a range of rehabilitation specialists, who may include physiatrists (physicians specializing in physical medicine and rehabilitation), physical therapists, occupational therapists, vocational therapists, and mental health care professionals.
- Physical therapy can help retain muscle strength and flexibility, improve coordination, reduce spasticity, regain greater control over bladder and bowel function, and increase joint movement. It also can help to reduce the likelihood of pressure sores developing in immobilized areas. Individuals are also taught to use assistive devices such as wheelchairs, canes, or braces as effectively as possible.
- Occupational therapy teaches people new ways to maintain or rebuild their independence by participating in meaningful, self-directed, everyday tasks such as bathing and dressing. Therapists teach people how to function at the highest level possible, by developing coping strategies, suggesting changes in their homes to improve safety (such as installing grab bars in bathrooms), and changing obstacles in their environment that interfere with normal activity.
- Vocational therapy involves offering instructions to help people develop and promote work skills, identify potential employers, and assist in job searches. Vocational therapists act as mediators between employees and employers to secure reasonable workplace accommodations.
- Psychotherapy for people living with permanent includes strategies and tools to deal with stress and a wide range of emotions and behaviors.
- Transverse myelitis support group: The Transverse Myelitis Association (https://myelitis.org/)
- Jeffery DR, Mandler RN, Davis LE. Transverse myelitis. Retrospective analysis of 33 cases, with differentiation of cases associated with multiple sclerosis and parainfectious events. Arch. Neurol. 1993;50(5):532–535. https://www.ncbi.nlm.nih.gov/pubmed/8489410[↩]
- Young J, Quinn S, Hurrell M, Taylor B. Clinically isolated acute transverse myelitis: prognostic features and incidence. Mult. Scler. 2009;15(11):1295–302. https://www.ncbi.nlm.nih.gov/pubmed/19812117[↩][↩]
- Krishnan C, Kaplin AI, Deshpande DM, Pardo CA, Kerr DA. Transverse Myelitis: pathogenesis, diagnosis and treatment. Front. Biosci. 2004;9:1483–1499. https://www.ncbi.nlm.nih.gov/pubmed/14977560[↩]
- Pidcock FS, Krishnan C, Crawford TO, Salorio CF, Trovato M, Kerr DA. Acute transverse myelitis in childhood: center-based analysis of 47 cases. Neurology. 2007;68(18):1474–1480. https://www.ncbi.nlm.nih.gov/pubmed/17470749[↩]