Contents
What is trigeminal neuralgia
Trigeminal neuralgia, also known as tic douloureux, is a disorder of the trigeminal nerve (5th cranial nerve) — the nerve that supplies sensation to your face and controls some of the muscles involved in chewing (see Figure 1 below). More than one trigeminal nerve (5th cranial nerve) branch can be affected by the disorder. Rarely, both sides of the face may be affected at different times in an individual, or even more rarely at the same time (called bilateral trigeminal neuralgia). Trigeminal neuralgia causes episodes of intense facial pain, which can occur spontaneously or be brought on by certain triggers, such as brushing your teeth, shaving, eating, touching your face, or even smiling. Fully-developed trigeminal neuralgia is one of the most painful conditions known.
The pain of trigeminal neuralgia has been described as sharp and stabbing, or like an electric shock, and is most often felt in the jaw or cheek. It normally comes on suddenly and can last from several seconds to a couple of minutes. Trigeminal neuralgia usually affects only one side of the face at a time. Sometimes, people with trigeminal neuralgia have a dull ache in the affected side of their face after the shock-like pain has subsided, but most people have no symptoms between attacks.
The pain of trigeminal neuralgia tends to come and go — you may have several attacks a day for a few days, weeks or months, and then be pain-free for months or years.
Trigeminal neuralgia is a form of neuropathic pain (pain associated with nerve injury or nerve lesion.) The typical or “classic” form of the disorder (called “Type 1” or trigeminal neuralgia1) causes extreme, sporadic, sudden burning or shock-like facial pain that lasts anywhere from a few seconds to as long as two minutes per episode. These attacks can occur in quick succession, in volleys lasting as long as two hours. The “atypical” form of the disorder (called “Type 2” or trigeminal neuralgia2), is characterized by constant aching, burning, stabbing pain of somewhat lower intensity than Type 1. Both forms of pain may occur in the same person, sometimes at the same time. The intensity of pain can be physically and mentally incapacitating.
Trigeminal neuralgia occurs most often in people over age 50, although it can occur at any age, including infancy. The possibility of trigeminal neuralgia being caused by multiple sclerosis increases when it occurs in young adults. The incidence of new cases is approximately 12 per 100,000 people per year; trigeminal neuralgia is more common in women than in men.
In most people, trigeminal neuralgia improves with treatment or goes into remission on its own. However, recurrences do occur, often after a long pain-free period. Also, as with any ongoing painful condition, depression may occur, but there are treatments for depression that can help.
Support groups can provide information, reassurance and support to people living with trigeminal neuralgia.
Trigeminal Nerve
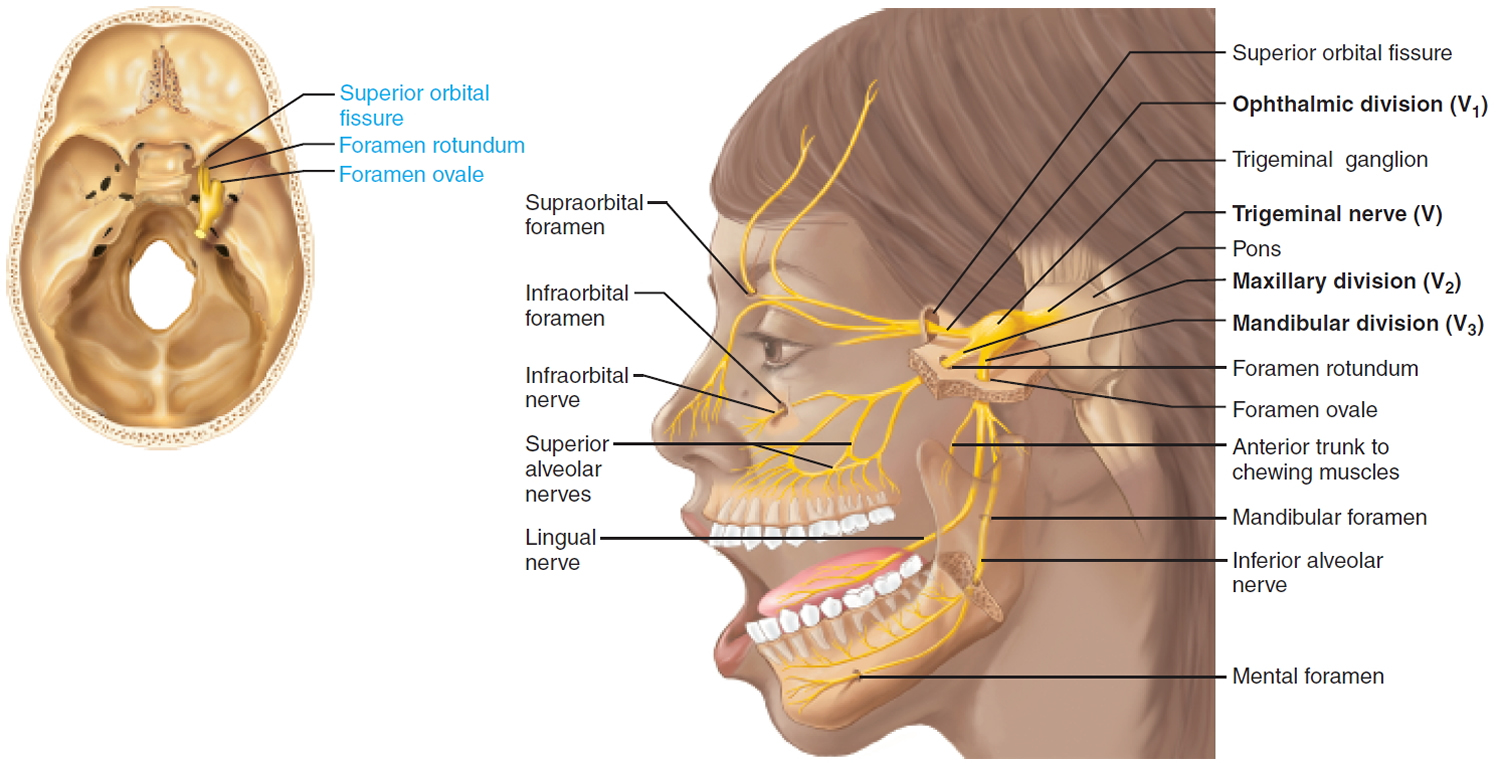
The large trigeminal nerve forms three divisions (trigeminal = threefold): ophthalmic (V1), maxillary (V2), and mandibular (V3) divisions.
This mixed nerve is the general somatic sensory nerve of the face for touch, temperature, and pain. The mandibular division supplies somatic motor innervation to the chewing muscles.
Sensory function:
- V1 The ophthalmic, or upper, branch supplies sensation to most of the scalp, forehead, and front of the head. General somatic sensation from skin of anterior scalp and forehead, upper eyelid and nose, nasal cavity mucosa, cornea, and lacrimal gland.
- V2 The maxillary, or middle, branch stimulates the cheek, upper jaw, top lip, teeth and gums, and to the side of the nose. General somatic sensation from skin of cheek, upper lip, and lower eyelid, nasal cavity mucosa, palate, upper teeth.
- V3 The mandibular, or lower, branch supplies nerves to the lower jaw, teeth and gums, and bottom lip. General somatic sensation from skin of chin and temporal region of scalp, anterior tongue and lower teeth.
Somatic motor function: V3 Innervate the muscles of mastication: temporalis, masseter, pterygoids, anterior belly of digastric. Afferent proprioceptor fibers return from these muscles.
Clinical significance: Anesthesia for Upper and Lower Jaws. Dentists desensitize upper and lower jaws by injecting local anesthetic (such as Novocain) into alveolar branches of the maxillary and mandibular divisions of the trigeminal nerve, respectively. This blocks pain-transmitting fibers from the teeth, and the surrounding tissues become numb.
Origin: Sensory receptors in skin and mucosa of face. Motor fibers from trigeminal motor nucleus in pons.
Pathway: Cell bodies of sensory neurons of all three divisions located in the large trigeminal ganglion. Fibers extend to trigeminal nuclei in the pons.
Through the Skull: V1 Superior orbital fissure. Cutaneous Branch: Supraorbital foramen.
Through the Skull: V2 Foramen rotundum. Cutaneous Branch: Infraorbital foramen.
Through the Skull: V3 Foramen ovale and Mandibular foramen. Cutaneous Branch: Mental foramen.
Figure 1. Trigeminal nerve (Cranial nerve 5)
Trigeminal neuralgia causes
What causes trigeminal neuralgia
Trigeminal neuralgia is associated with a variety of conditions. Compression of the root of the trigeminal nerve as it exits the brain stem by an abnormally positioned blood vessel is commonly implicated as a cause of trigeminal neuralgia. This compression causes the wearing away or damage to the protective coating around the nerve (the myelin sheath). The pressure on the nerve causes it to misfire, resulting in pain. Occasionally, the compression is caused by a tumor, tangle of arteries and veins called an arteriovenous malformation and often there is no obvious cause found. Injury to the trigeminal nerve (perhaps the result of sinus surgery, oral surgery, stroke, or facial trauma) may also produce neuropathic facial pain. Other, rarer causes of trigeminal neuralgia include multiple sclerosis (a disease that causes deterioration of the trigeminal nerve’s myelin sheath) and strokes affecting the lower part of the brain.
Trigeminal neuralgia triggers
A variety of triggers may set off the pain of trigeminal neuralgia, including:
- Shaving
- Touching your face
- Eating
- Drinking
- Brushing your teeth
- Talking
- Putting on makeup
- Encountering a breeze
- Smiling
- Washing your face
Trigeminal neuralgia symptoms
Pain varies, depending on the type of trigeminal neuralgia, and may range from sudden, severe, and stabbing to a more constant, aching, burning sensation. The intense flashes of pain can be triggered by vibration or contact with the cheek (such as when shaving, washing the face, or applying makeup), brushing teeth, eating, drinking, talking, or being exposed to the wind. The pain may affect a small area of the face or may spread. Bouts of pain rarely occur at night, when the affected individual is sleeping.
Trigeminal neuralgia is typified by attacks that stop for a period of time and then return, but the condition can be progressive. The attacks often worsen over time, with fewer and shorter pain-free periods before they recur. Eventually, the pain-free intervals disappear and medication to control the pain becomes less effective. The disorder is not fatal, but can be debilitating. Due to the intensity of the pain, some individuals may avoid daily activities or social contacts because they fear an impending attack.
Trigeminal neuralgia symptoms may include one or more of these patterns:
- Episodes of severe, shooting or jabbing pain that may feel like an electric shock
- Spontaneous attacks of pain or attacks triggered by things such as touching the face, chewing, speaking or brushing teeth
- Bouts of pain lasting from a few seconds to several minutes
- Episodes of several attacks lasting days, weeks, months or longer — some people have periods when they experience no pain
- Constant aching, burning feeling that may occur before it evolves into the spasm-like pain of trigeminal neuralgia
- Pain in areas supplied by the trigeminal nerve, including the cheek, jaw, teeth, gums, lips, or less often the eye and forehead
- Pain affecting one side of the face at a time, though may rarely affect both sides of the face
- Pain focused in one spot or spread in a wider pattern
- Attacks that become more frequent and intense over time.
Trigeminal neuralgia diagnosis
Trigeminal neuralgia diagnosis is based primarily on the person’s history and description of symptoms, along with results from physical and neurological examinations. Your doctor will ask about the pain and perform a physical examination, testing the nerves of your head and neck. Other disorders that cause facial pain should be ruled out before trigeminal neuralgia is diagnosed. Some disorders that cause facial pain include post-herpetic neuralgia (nerve pain following an outbreak of shingles), cluster headaches, and temporomandibular joint disorder (TMJ, which causes pain and dysfunction in the jaw joint and muscles that control jaw movement). Because of overlapping symptoms and the large number of conditions that can cause facial pain, obtaining a correct diagnosis is difficult, but finding the cause of the pain is important as the treatments for different types of pain may differ.
Your doctor will diagnose trigeminal neuralgia mainly based on your description of the pain, including:
- Type. Pain related to trigeminal neuralgia is sudden, shock-like and brief.
- Location. The parts of your face that are affected by pain will tell your doctor if the trigeminal nerve is involved.
- Triggers. Trigeminal neuralgia-related pain usually is brought on by light stimulation of your cheeks, such as from eating, talking or even encountering a cool breeze.
Your doctor may conduct many tests to diagnose trigeminal neuralgia and determine underlying causes for your condition, including:
Most people with trigeminal neuralgia eventually will undergo a magnetic resonance imaging (MRI) scan to rule out a tumor or multiple sclerosis as the cause of their pain. This scan may or may not clearly show a blood vessel compressing the nerve. In some cases, your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow (magnetic resonance angiogram). Special magnetic resonance angiogram can reveal the presence and severity of compression of the nerve by a blood vessel.
A diagnosis of classic trigeminal neuralgia may be supported by an individual’s positive response to a short course of an antiseizure medication. Diagnosis of trigeminal neuralgia 2 is more complex and difficult, but tends to be supported by a positive response to low doses of tricyclic antidepressant medications (such as amitriptyline and nortriptyline), similar to other neuropathic pain diagnoses.
Trigeminal neuralgia treatment
Trigeminal neuralgia medication
Regular pain medicines are generally not helpful in treating trigeminal neuralgia because the episodes of pain are brief and recurrent. However, anticonvulsant medications — the same medicines that are used to control seizures in people with epilepsy — have been found to be effective in relieving this type of nerve pain.
- Anticonvulsants. Doctors usually prescribe carbamazepine (Tegretol, Carbatrol, others) for trigeminal neuralgia, and it’s been shown to be effective in treating the condition. Other anticonvulsant drugs that may be used to treat trigeminal neuralgia include oxcarbazepine (Trileptal), lamotrigine (Lamictal) and phenytoin (Dilantin, Phenytek). Other drugs, including clonazepam (Klonopin) and gabapentin (Neurontin, Gralise, others), also may be used. If the anticonvulsant you’re using begins to lose effectiveness, your doctor may increase the dose or switch to another type. Side effects of anticonvulsants may include dizziness, confusion, drowsiness and nausea.
- Antispasmodic agents. Muscle-relaxing agents such as baclofen (Gablofen, Lioresal) may be used alone or in combination with carbamazepine. Side effects may include confusion, nausea and drowsiness.
- Botox injections. Small studies have shown that onabotulinumtoxinA (Botox) injections may reduce pain from trigeminal neuralgia in people who are no longer helped by medications. However, more research needs to be done before this treatment is widely used for this condition.
Your doctor will most likely prescribe an anticonvulsant such as carbamazepine for the initial treatment of trigeminal neuralgia. Carbamazepine has been shown to be effective in relieving pain in people with trigeminal neuralgia. However, in some people, this medicine is not well tolerated because of side effects, or becomes less effective in controlling the pain over time. Also, carbamazepine can trigger a serious drug reaction in some people, mainly those of Asian descent, so genetic testing may be recommended before you start carbamazepine. Other anticonvulsants can also be used, either as initial treatment or if carbamazepine is ineffective.
Another medicine that can be used is baclofen, which is normally used to control muscle spasms. Baclofen may be used in combination with an anticonvulsant.
Trigeminal neuralgia surgery
Surgery is an option if your trigeminal neuralgia is the result of a blood vessel compressing your trigeminal nerve. In this type of surgery, any blood vessels that are compressing the trigeminal nerve are removed or relocated. Surgery is more commonly performed in younger people who are in good overall health.
Surgical options for trigeminal neuralgia include:
- Microvascular decompression. Microvascular decompression is the most invasive of all surgeries for trigeminal neuralgia, but also offers the lowest probability that pain will return. About half of individuals undergoing microvascular decompression for trigeminal neuralgia will experience recurrent pain within 12 to 15 years. This procedure involves relocating or removing blood vessels that are in contact with the trigeminal root to stop the nerve from malfunctioning. This inpatient procedure, which is performed under general anesthesia, requires that a small incision be made through the mastoid bone behind the ear on the side of your pain. Then, while viewing the trigeminal nerve through a microscope or endoscope through a small hole in your skull, your surgeon moves any arteries that are in contact with the trigeminal nerve away from the nerve, and places a soft cushion between the nerve and the arteries. If a vein is compressing the nerve, your surgeon may remove it. Doctors may also cut part of the trigeminal nerve (neurectomy) during this procedure if arteries aren’t pressing on the nerve. Microvascular decompression can successfully eliminate or reduce pain most of the time, but pain can recur in some people. Microvascular decompression has some risks, including decreased hearing, facial weakness, facial numbness, a stroke or other complications. Most people who have this procedure have no facial numbness afterward. Individuals generally recuperate for several days in the hospital following the procedure, and will generally need to recover for several weeks after the procedure.
- Brain stereotactic radiosurgery (Gamma knife). In this procedure, a surgeon directs a focused dose of radiation to the root of your trigeminal nerve where the trigeminal nerve exits the brain stem. This procedure uses radiation to damage the trigeminal nerve and reduce or eliminate pain. People usually leave the hospital the same day or the next day following treatment but won’t typically experience relief from pain for several weeks (or sometimes several months) following the procedure. The International RadioSurgery Association reports that between 50 and 78 percent of people with trigeminal neuralgia who are treated with Gamma Knife radiosurgery experience “excellent” pain relief within a few weeks following the procedure. For individuals who were treated successfully, almost half have recurrence of pain within three years. If pain recurs, the procedure can be repeated. Facial numbness can be a side effect.
Other procedures may be used to treat trigeminal neuralgia, such as a rhizotomy. In a rhizotomy, your surgeon destroys nerve fibers to reduce pain, and this causes some facial numbness. Types of rhizotomy include:
- Glycerol injection. Glycerol injection isgenerally an outpatient procedure in which the individual is sedated with intravenous medication. A thin needle is passed through the cheek, next to the mouth, and guided through the opening in the base of the skull where the third division of the trigeminal nerve (mandibular) exits. The needle is moved into the pocket of spinal fluid (cistern) that surrounds the trigeminal nerve center (or ganglion, the central part of the nerve from which the nerve impulses are transmitted to the brain). The procedure is performed with the person sitting up, since glycerol is heavier than spinal fluid and will then remain in the spinal fluid around the ganglion. The glycerol injection bathes the ganglion and damages the insulation of trigeminal nerve fibers. This procedure often relieves pain. However, this form of rhizotomy is likely to result in recurrence of pain within a year to two years and many experience facial numbness or tingling. However, the procedure can be repeated multiple times.
- Balloon compression. In balloon compression, your doctor inserts a hollow needle through your face and guides it to a part of your trigeminal nerve that goes through the base of your skull. Then, your doctor threads a thin, flexible tube (catheter) with a balloon on the end through the needle. Your doctor inflates the balloon with enough pressure to damage the trigeminal nerve and block pain signals. Balloon compression successfully controls pain in most people, at least for a period of time – pain relief usually lasts one to two years. Most people undergoing this procedure experience at least some transient facial numbness. Balloon compression is generally an outpatient procedure, although sometimes the patient may be kept in the hospital overnight.
- Radiofrequency thermal lesioning. This procedure selectively destroys nerve fibers associated with pain. While you’re sedated, your surgeon inserts a hollow needle through your face and guides it to a part of the trigeminal nerve that goes through an opening at the base of your skull. Once the needle is positioned, your surgeon will briefly wake you from sedation. Your surgeon inserts an electrode through the needle and sends a mild electrical current through the tip of the electrode. You’ll be asked to indicate when and where you feel tingling. When your neurosurgeon locates the part of the nerve involved in your pain, you’re returned to sedation. Then the electrode is heated until it damages the nerve fibers, creating an area of injury (lesion). The procedure can be repeated until the desired amount of sensory loss is obtained; usually a blunting of sharp sensation, with preservation of touch. If your pain isn’t eliminated, your doctor may create additional lesions. Radiofrequency thermal lesioning usually results in some temporary facial numbness after the procedure. Pain may return after three to four years. Approximately half of the people have symptoms that reoccur three to four years following radiofrequency thermal lesioning. Production of more numbness can extend the pain relief even longer, but the risks of anesthesia dolorosa also increase.
- A neurectomy (also called partial nerve section), which involves cutting part of the nerve, may be performed near the entrance point of the nerve at the brain stem during an attempted microvascular decompression if no vessel is found to be pressing on the trigeminal nerve. Neurectomies also may be performed by cutting superficial branches of the trigeminal nerve in the face. When done during microvascular decompression, a neurectomy will cause more long-lasting numbness in the area of the face that is supplied by the nerve or nerve branch that is cut. However, when the operation is performed in the face, the nerve may grow back and in time sensation may return. With neurectomy, there is risk of creating anesthesia dolorosa.
Surgical treatment for trigeminal neuralgia 2 is usually more problematic than for trigeminal neuralgia 1, particularly where vascular compression is not detected in brain imaging prior to a proposed procedure. Many neurosurgeons advise against the use of microvascular decompression or rhizotomy in individuals for whom trigeminal neuralgia 2 symptoms predominate over trigeminal neuralgia1, unless vascular compression has been confirmed. Microvascular decompression for trigeminal neuralgia2 is also less successful than for trigeminal neuralgia 1.
Trigeminal neuralgia natural treatment
Alternative treatments for trigeminal neuralgia generally haven’t been as well-studied as medications or surgical procedures, so there’s often little evidence to support their use.
Some people find that low-impact exercise, yoga, creative visualization, aroma therapy, or meditation may be useful in promoting well-being. Other options include acupuncture, upper cervical chiropractic, biofeedback, vitamin therapy, and nutritional therapy. Some people report modest pain relief after injections of botulinum toxin to block activity of sensory nerves. Be sure to check with your doctor before trying an alternative treatment because it may interact with your other treatments.
Coping and support
Living with trigeminal neuralgia can be difficult. The disorder may affect your interaction with friends and family, your productivity at work, and the overall quality of your life.
Chronic pain from trigeminal neuralgia is frequently very isolating and depressing for the individual. Conversely, depression and sleep disturbance may render individuals more vulnerable to pain and suffering. Some individuals benefit from supportive counseling or therapy by a psychiatrist or psychologist. However, there is no evidence that trigeminal neuralgia is psychogenic in origin or caused by depression, and persons with trigeminal neuralgia require effective medical or surgical treatment for their pain.
You may find encouragement and understanding in a support group. Group members often know about the latest treatments and tend to share their own experiences. If you’re interested, your doctor may be able to recommend a group in your area.