Contents
What is vulvodynia
Vulvodynia is chronic pain (lasting 3 months or longer) or discomfort of the vulva without an identifiable cause – not caused by an infection, skin disorder, or other medical condition. Vulvodynia is usually described as burning, stinging, irritation, or rawness. The location, constancy and severity of the pain vary among sufferers. Some women experience pain in only one area of the vulva, while others experience pain in multiple areas. The most commonly reported symptom is burning, but women’s descriptions of the pain vary. One woman reported her pain felt like “acid being poured on my skin,” while another described it as “constant knife-like pain.” Researchers and health care providers currently know little about why and how vulvodynia occurs—the condition and the pain have no known cause or cure 1. Therapies can help relieve symptoms of vulvodynia, but the condition can have some serious effects on women’s reproductive health and day-to-day life.
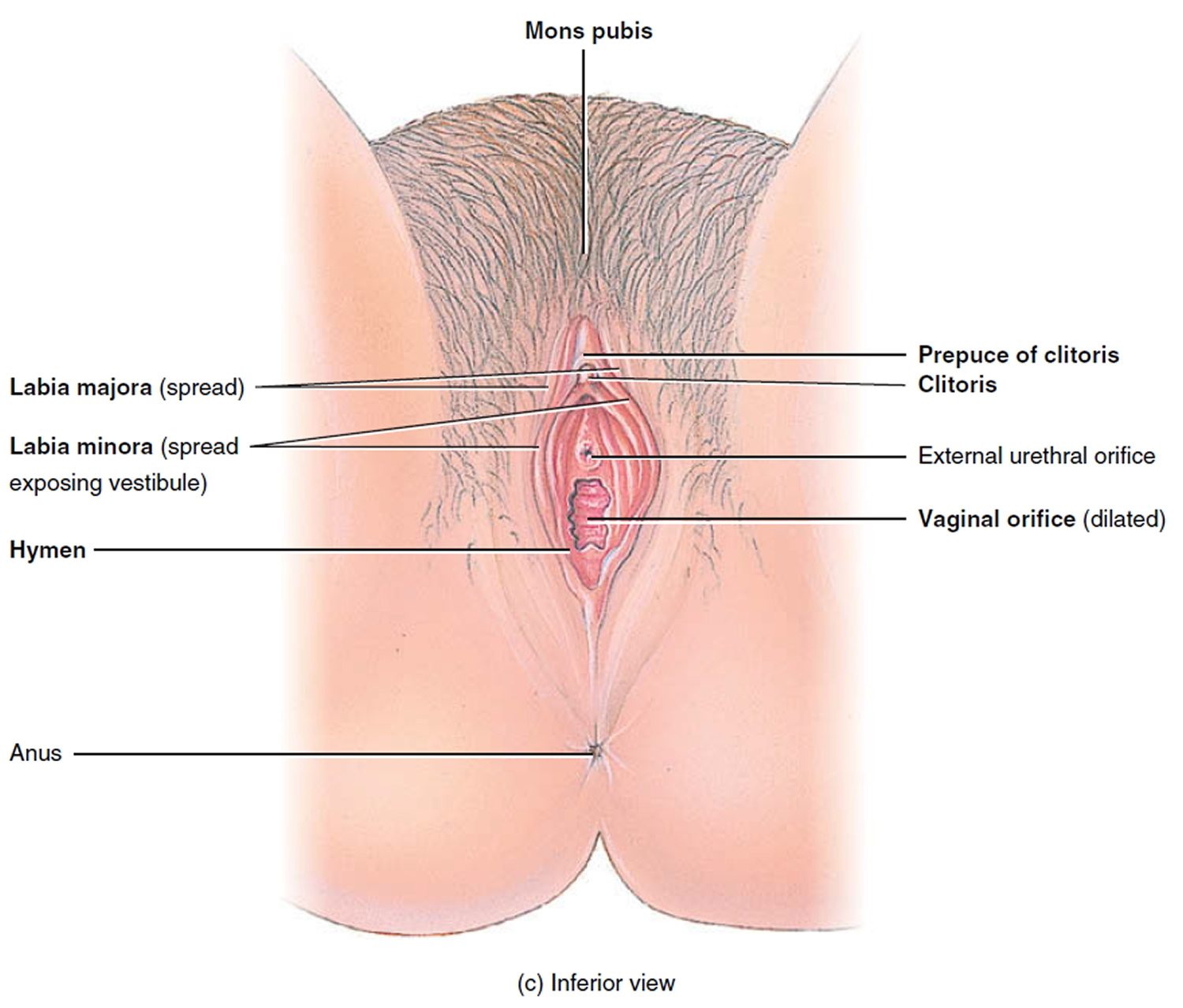
The vulva refers to the external female genitalia, including the labia (“lips” or folds of skin at the opening of the vagina), the clitoris, and the vaginal opening (see Figure 1).
The exact number of women with vulvodynia is unknown. Researchers estimate that 9% to 18% of women between the ages of 18 and 64 may experience vulvar pain during their lifetimes 2.
The evidence suggests that many women either do not seek help at all or go from doctor to doctor seeking a diagnosis and treatment without receiving answers 3.
Figure 1. The vulva – the outer part of the female genitalia
Sometimes, vulvodynia is described with more specific terms:
- Generalized vulvodynia is pain or discomfort that can be felt in the entire vulvar area.
- Localized vulvodynia is felt in only one place on the vulva.
- Provoked vulvodynia is pain triggered by an activity or contact with the area, such as having sex, using a tampon, having a gynecological exam, or even wearing tight-fitting pants. Alternatively, spontaneous vulvodynia occurs when the pain is not initiated by any known trigger 4.
- Provoked vestibulodynia is vulvodynia with provoked pain that occurs in the vestibular region of the vulva, or the entry point to the vagina. This condition has formerly been called vulvar vestibulitis syndrome, focal vulvitis, vestibulodynia, or vulvar vestibulitis 4.
Localized Vulvodynia
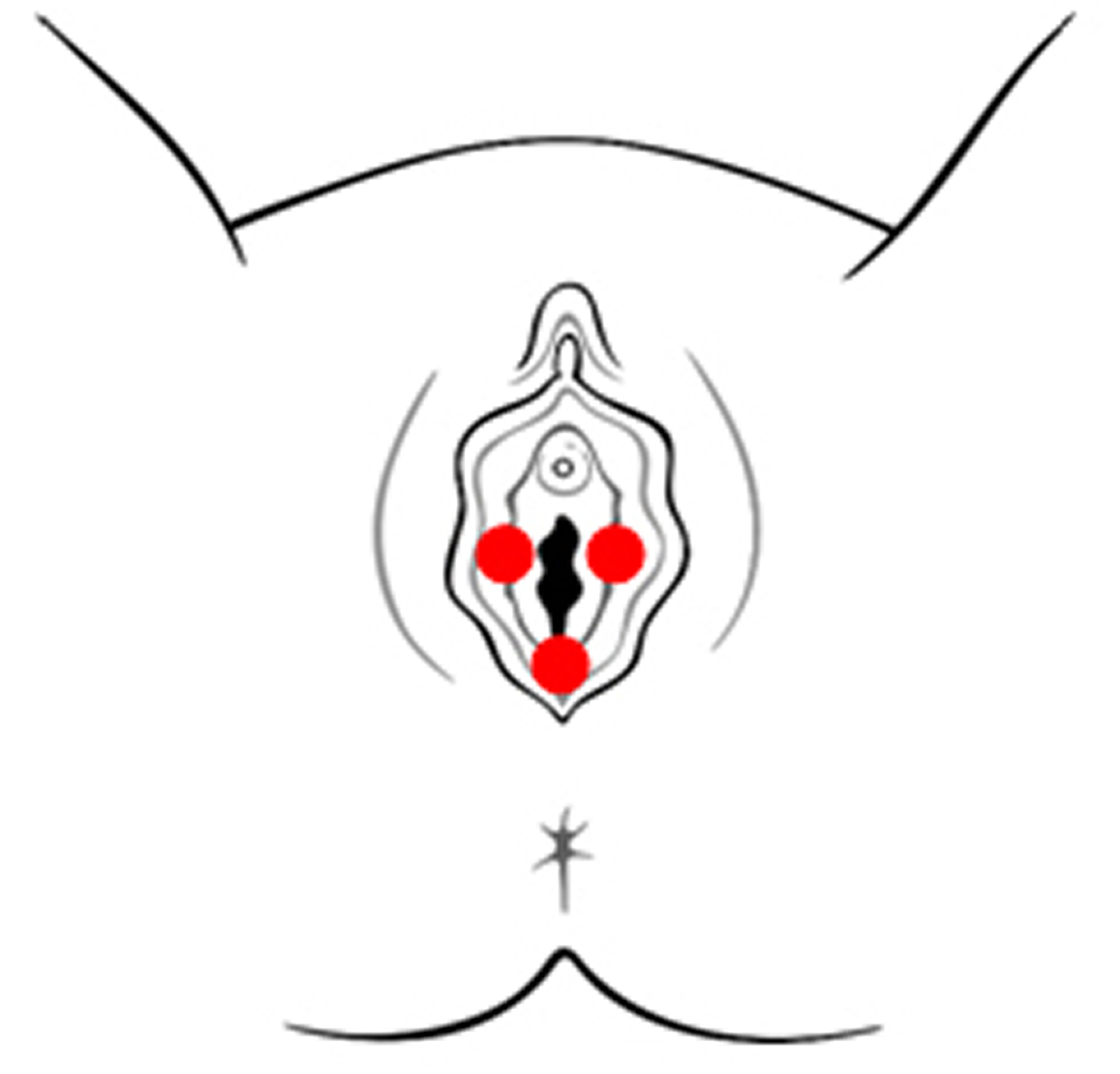
Most women have pain at only one vulvar site. If the pain is in the vestibule, the tissue surrounding the vaginal opening, the diagnosis is vestibulodynia (formerly known as vulvar vestibulitis syndrome) (see Figure 2)
Figure 2. Localized vulvodynia
The majority of women with localized vulvodynia have provoked vestibulodynia, in which pain occurs during or after pressure is applied to the vestibule, e.g., with:
- sexual intercourse,
- tampon insertion,
- a gynecologic examination,
- prolonged sitting, and/or
- wearing fitted pants.
A less common form of localized vulvodynia, known as clitorodynia (pain in the clitoris), can be very painful.
Provoked vestibulodynia is further classified as primary or secondary.
Women with primary provoked vestibulodynia have experienced vestibular pain since the first attempt at vaginal penetration.
Women with secondary provoked vestibulodynia have experienced pain-free sexual intercourse prior to the development of vulvar pain.
Generalized Vulvodynia
For women with generalized vulvodynia (GV), pain occurs spontaneously and is relatively constant, but there can be some periods of symptom relief.
Activities that apply pressure to the vulva, such as prolonged sitting or sexual intercourse, typically exacerbate symptoms.
Vulva anatomy
The vulva is the outer part of the female genitals. The vulva includes the opening of the vagina (sometimes called the vestibule), the labia majora (outer lips), the labia minora (inner lips), and the clitoris (Figure 1).
Around the opening of the vagina, there are 2 sets of skin folds. The inner set, called the labia minora, are small and hairless. The outer set, the labia majora, are larger, with hair on the outer surface. (Labia is Latin for lips.) The inner and outer labia meet, protecting the vaginal opening and, just above it, the opening of the urethra (the short tube that carries urine from the bladder). The Bartholin glands are found just inside the opening of the vagina — one on each side. These glands produce a mucus-like fluid that acts as a lubricant during sex.
At the front of the vagina, the labia minora meet to form a fold or small hood of skin called the prepuce. The clitoris is beneath the prepuce. The clitoris is an approximately ¾-inch structure of highly sensitive tissue that becomes swollen with blood during sexual stimulation. The labia minora also meet at a place just beneath the vaginal opening, at the fourchette. Beyond the fourchette is the anus, the opening to the rectum. This is where stool comes out of the body. The space between the vagina and the anus is called the perineum.
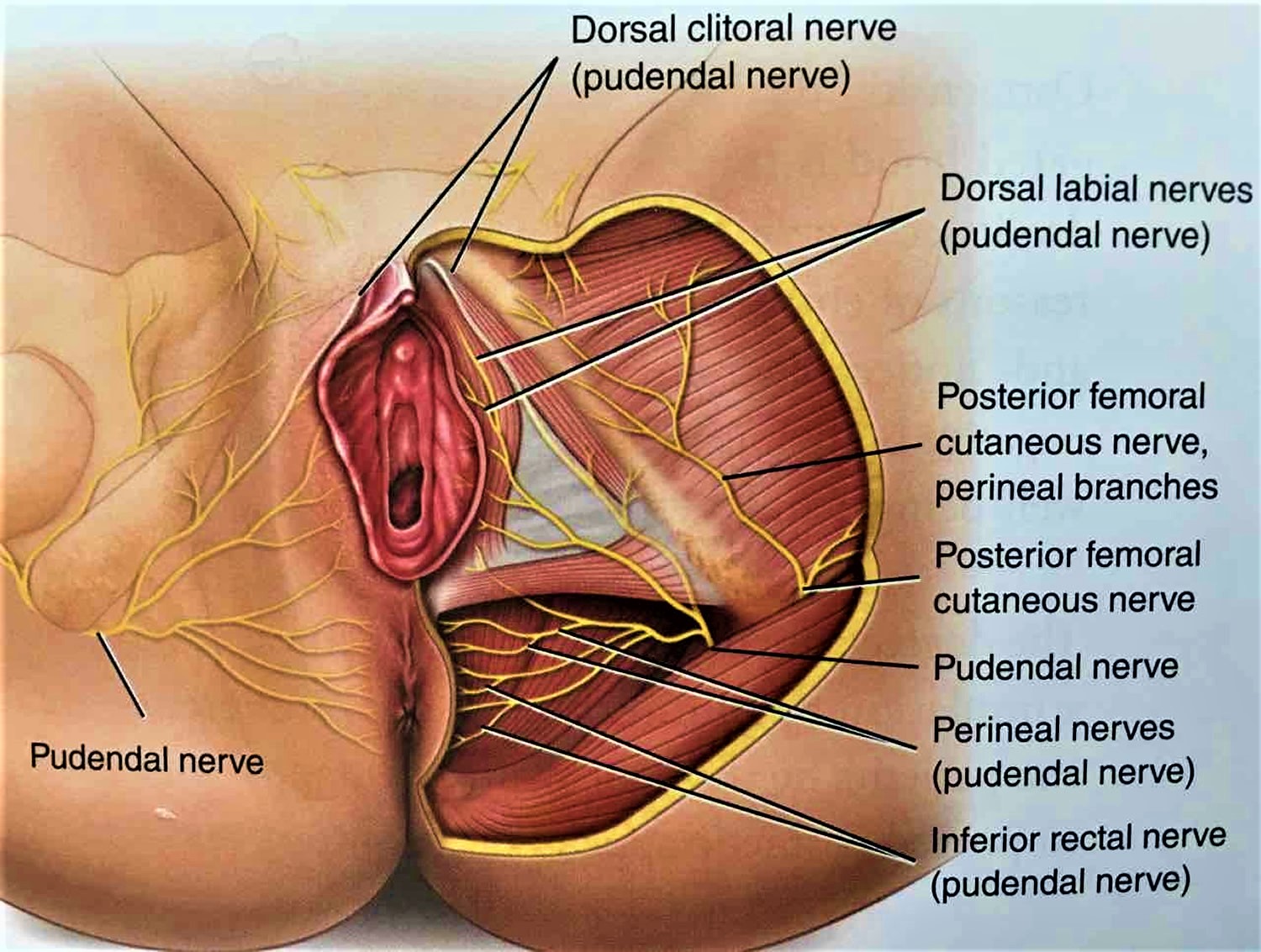
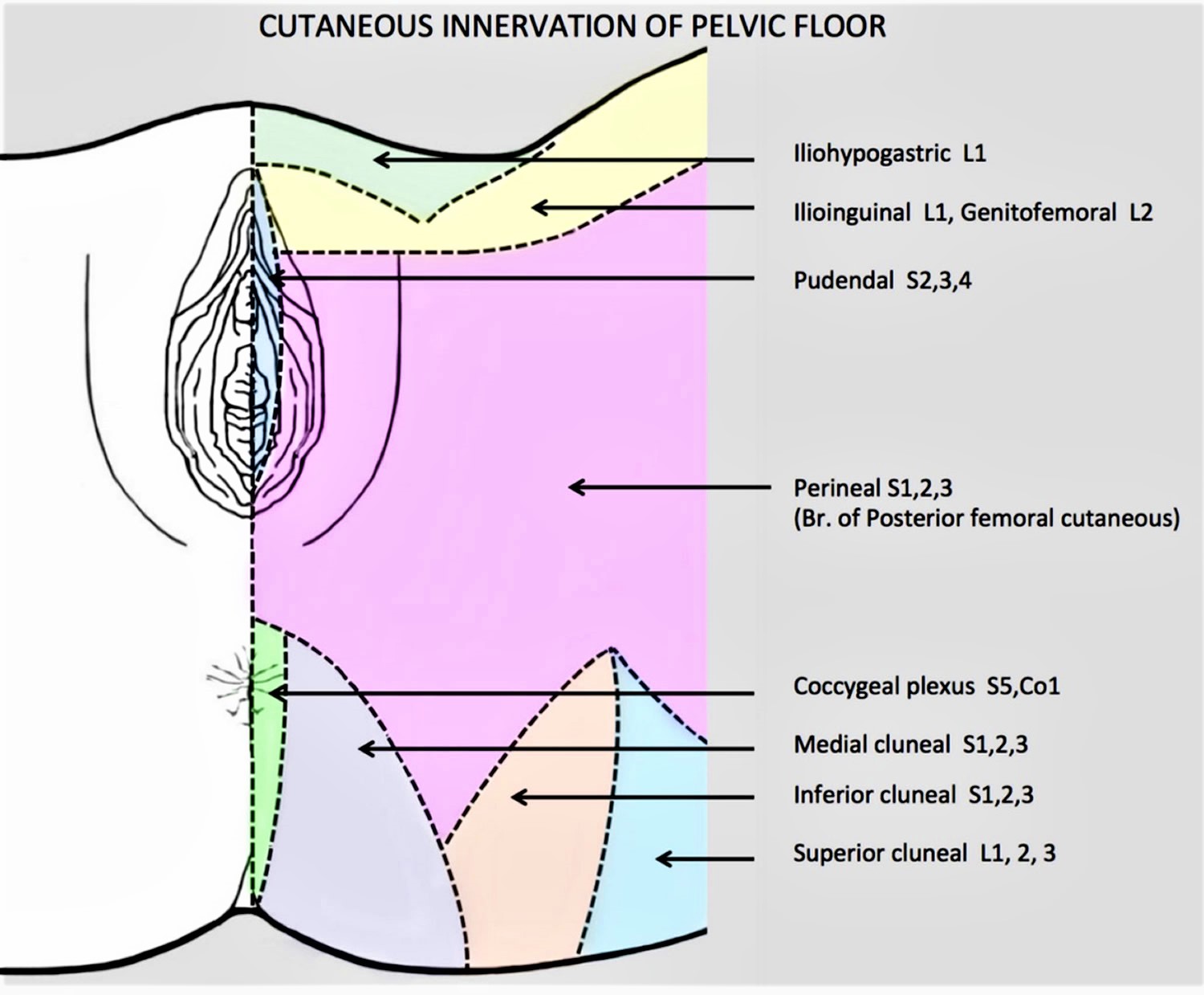
The pudendal nerve transmits pain messages and other sensations from the vulva (Figures 3 and 4). The pudendal nerve originates from the sacral spine, which is located directly below the low back area. The nerve passes through the pelvis and enters the vulvar region near the ischial spine, which is part of the hip bone. From there, it branches off into the inferior rectal nerve, perineal nerve and dorsal nerve of the clitoris. The pudendal nerve is responsible for proper functioning and control of urination, defecation and orgasm in both males and females.
Figure 3. Nerve supply of the vulva
Figure 4. Nerve supply of the vulva
Vulvodynia causes
Vulvodynia is not caused by an active infection or a sexually transmitted disease. Vulvodynia tends to be diagnosed when other causes of vulvar pain, such as infection or skin diseases, are ruled out. Through continued research efforts, scientists move closer to discovering the underlying cause(s) of vulvodynia. Vulvodynia is likely caused by many factors working together.
Researchers speculate that one or more of the following may cause, or contribute to, vulvodynia:
- An injury to, or irritation of, the nerves that transmit pain from the vulva to the spinal cord
- Inflammation of the vulva
- Long-term reactions to certain infections
- Certain genetic disorders
- Sensitivity to certain foods
- Dysfunction of the muscles of the pelvic floor
- Conditions that affect nearby muscles or bones
- An increase in the number and sensitivity of pain-sensing nerve fibers in the vulva
- Elevated levels of inflammatory substances in the vulva
- An abnormal response of different types of vulvar cells to environmental factors such as infection or trauma
- Genetic factors such as susceptibility to chronic vestibular inflammation, chronic widespread pain and/or inability to combat vulvovaginal infection
- Pelvic floor muscle weakness, spasm or instability
- Injury to or irritation of the nerves that transmit pain and other sensations from the vulva
- Altered hormone receptor expression in the vulvar tissue
- Localized hypersensitivity to Candida or other vulvovaginal organisms.
Other causes of vulval pain
Pain in the vulva isn’t always vulvodynia. It can have a number of other causes, such as:
- persistent vaginal thrush or other vaginal infections
- sensitivity to something touching the vulva, such as soap, bubble bath or medicated creams (known as irritant contact dermatitis)
- a drop in the hormone oestrogen causing dryness of the vulva, particularly during the menopause
- a recurrent herpes infection
- lichen sclerosus or lichen planus (skin conditions that can cause intense irritation and soreness of the vulva)
- in rare cases, Behcet’s disease (a condition of the blood vessels that can cause genital ulcers) or Sjogren’s syndrome (a disorder of the immune system that can cause vaginal dryness)
Your doctor may want to rule out these conditions before treating you for vulvodynia. Some women can have a combination of problems, for example recurrent thrush and vulvodynia, with both needing proper treatment to reduce pain.
Vulvodynia complications
Because it can be painful and frustrating and can keep you from wanting sex, vulvodynia can cause emotional problems. For example, fear of having sex can cause spasms in the muscles around your vagina (vaginismus). Other complications might include:
- Anxiety
- Depression
- Sleep disturbances
- Sexual dysfunction
- Altered body image
- Relationship problems
- Decreased quality of life
Vulvodynia symptoms
The main symptom of vulvodynia is pain. The type of pain can be different for each woman.
Vulvodynia can cause burning, stinging, irritation, or rawness of the vulva. Some women may also have itching, aching, soreness, throbbing, or swelling. These symptoms may be caused by pressure on the vulvar area, such as during sex or when inserting a tampon. Symptoms may occur during exercise, after urinating, or even while sitting or resting 5.
Pain may move around or always be in the same place. It can be constant, or it can come and go.
Vulvodynia diagnosis
If you have vulvar pain, your gynecologist or other health care professional will try to rule out the most common causes of vulvar pain first. You may be asked questions about your symptoms, sexual history, and medical and surgical history. You may be asked when symptoms occur, what treatments you have tried, and whether you have any allergies, chronic infections, or skin problems.
Your gynecologist also will examine the vulva and vagina carefully. Your gynecologist may use a moist cotton swab to touch areas of the vulva. The goal is to find where the pain is and whether it is mild, moderate, or severe. Your provider should carefully examine the vaginal secretions to rule out an active infection or skin disorder. Routine cultures for yeast and bacterial infections should be performed. Your provider may also recommend that you have blood drawn to assess levels of estrogen, progesterone and testosterone. He/she will likely perform a cotton-swab test (pictured on the right). During the test, gentle pressure is applied to various vulvar sites and you’re asked to rate the severity of the pain. If any areas of skin appear suspicious, your provider may examine them with a magnifying instrument or take a biopsy of the area.
You also may have a biopsy of the vulvar skin.
Vulvodynia treatment
Since vulvodynia is not simply a gynecological condition, many experts favor a multi-disciplinary approach to its management.
Vulvodynia treatment may involve visiting a:
- gynecologist or vulvovaginal specialist,
- dermatologist,
- neurologist,
- pain management specialist,
- urogynecologist, and/or
- physical therapist.
Also, because vulvodynia typically affects a woman’s sexual relationships and emotional well-being, your provider may recommend a psychologist or couples/sex therapist.
Many kinds of treatment are available. No one method works all the time for everyone and it may take time to find a treatment or combination of treatments, that alleviates your pain. It can take a few months before any relief is noticed. Keeping a pain diary can help you track your symptoms and how they respond to different therapies. In some cases, your gynecologist or other health care professional may refer you to a pain specialist. A pain specialist may use techniques such as ultrasound and electrical stimulation to relieve pain.
Treatments are directed towards alleviating symptoms and usually provides moderate pain relief. Some women experience relief with a particular treatment, while others do not respond or experience unacceptable side effects.
Vulvar pain can have an emotional or psychological aspect, and some women benefit from psychological counseling, sex therapy, or both.
Women with provoked vestibulodynia may be candidates for surgery. Success rates for surgery vary from 60% – 90%.
Current vulvodynia treatments include:
- Discontinuation of Irritants
- Oral “Pain-Blocking” Medications
- Tricyclic Antidepressants
- Serotonin-Norepinephrine Reuptake Inhibitors
- Anticonvulsants
- Opioids
- Topical Medications
- Topical Hormonal Creams (e.g., estrogen, testosterone)
- Topical Anesthetics (e.g., lidocaine)
- Topical Compounded Formulations (e.g., anticonvulsant, antidepressant)
- Pelvic Floor Muscle Therapy
- Nerve Blocks
- Neurostimulation and Spinal Infusion Pump
- Surgery (for women with Provoked Vestibulodynia)
- Complementary or Alternative Medicine (including relaxation, massage, homeopathy, and acupuncture). But there is little evidence about the effectiveness of these approaches.
An expert panel, convened in 2016, recommended against the use of antidepressants or corticosteroids for vulvodynia 6.
Vulvodynia pain relief
Prescription medication
Several medications can be used to treat vulvodynia. Medications can be taken in pill form (oral), injected into the affected area, or applied to the skin (topical). The following medications have been found to be helpful in treating vulvodynia:
- Local anesthetics —These medications are applied to the skin. They may be used before sexual intercourse to provide short-term pain relief, or they can be used for extended periods.
- Antidepressants and antiseizure drugs —Drugs used to treat depression and to prevent seizures also may help with the symptoms of vulvodynia. It may take a few weeks for these medications to work. Some types of antidepressants can be provided in the form of a cream that is applied to the skin.
- Hormone creams —Estrogen cream applied to the vulva may help relieve vulvodynia in some cases.
Conventional painkillers such as paracetamol won’t usually relieve the pain of vulvodynia. But several medications available on prescription can help, including:
- antidepressants called amitriptyline and nortriptyline – possible side effects include drowsiness, weight gain and dry mouth
- anti-epilepsy medicines called gabapentin and pregabalin – possible side effects include dizziness, drowsiness and weight gain
Your doctor will probably start you on a low dose and gradually increase it until your pain subsides. You may need to take the medication for several months.
If you have pain in a specific area of your vulva, injections of local anesthetic and steroid medication into a nearby nerve may provide temporary pain relief.
Physical therapy
Physical therapy is another option for treating vulvodynia. This type of therapy can relax tissues in the pelvic floor and release tension in muscles and joints. Biofeedback is a form of physical therapy that trains you to strengthen the pelvic floor muscles. Strengthening these muscles may help lessen your pain.
A physiotherapist can teach you some pelvic floor exercises (such as squeezing and releasing your pelvic floor muscles) to help relax the muscles around your vagina.
Another technique to relax the muscles in the vagina and desensitize it involves using a set of vaginal trainers. These are smooth cones of gradually increasing size and length which can be inserted into your vagina in the privacy of your own home.
Some physiotherapists may also suggest trying TENS (transcutaneous electrical nerve stimulation) to reduce your pain. This is where a machine is used to deliver a mild electrical current to the painful area.
Trigger point therapy
Trigger point therapy is a form of massage therapy. A trigger point is a small area of tightly contracted muscle. Pain from a trigger point travels to nearby areas. Trigger point therapy involves soft tissue massage to relax the tight area of muscle. A combination of an anesthetic drug and a steroid also can be injected into the trigger point to provide relief.
Physical therapy and biofeedback also can be helpful for women with vulvodynia 7. Physical therapy for vulvodynia may include exercise, education, or manual therapies, such as massage, joint mobilization, or soft-tissue mobilization. Other forms of physical therapy can involve ultrasound, electrical stimulation, or biofeedback techniques.
Nerve block
A nerve block is a type of anesthesia in which an anesthetic drug is injected into the nerves that carry pain signals from the vulva to the spinal cord. This treatment interrupts the pain signals and can provide short-term and sometimes long-term pain relief. Injection of a drug called botulinum toxin A (also known as Botox) has been used to treat vulvodynia. This drug relaxes muscles of the pelvic floor. Current evidence regarding the efficacy of the botulinum toxin A treatment is mixed, and further clinical trials are needed.
Cognitive behavioral therapy
Cognitive behavioral therapy may be suggested if you have vulvodynia. A counselor can help you learn to cope with chronic pain. This may reduce stress and help you feel more in control of your symptoms. Sexual counseling can provide support and education about this condition for you and your partner. A randomized, controlled clinical trial found that women who had cognitive behavioral therapy reported a 30% decrease in vulvar pain that occurs with intercourse 6.
Surgery
Surgery is usually considered a last resort and may be an option for women with severe pain from vulvar vestibulitis who have not found relief through other treatment options 8. A vestibulectomy is the removal of the painful tissue from the part of the vulva called the vestibule and may help relieve pain and improve sexual comfort. It can be used for women who have vulvodynia specific to this area and for whom other treatments have not worked. It is not recommended for women with generalized vulvodynia that is not limited to the vestibule 7.
Vulvodynia home remedies
If you have vulvodynia, gentle care of the vulva can help provide some pain relief for some women 9. Avoid products and other items that may be irritating. The following may be helpful in relieving or reducing symptoms:
- Wear 100% cotton underwear.
- Do not wear underwear while sleeping.
- Avoid tightfitting pantyhose and nylon underwear. Tight clothing restricts airflow to your genital area, often leading to increased temperature and moisture that can cause irritation.
- Soak in a sitz bath. Two to three times a day, sit in comfortable, lukewarm (not hot) or cool water with Epsom salts or colloidal oatmeal for five to 10 minutes.
- Avoid douching.
- Avoid irritants, such as perfumes, dyes, shampoos, detergents, and deodorants.
- Clean the vulva with water only.
- Switch to 100% cotton pads if regular pads are irritating.
- Use lubricants during sex, but avoid lubricants with flavor or cooling/warming sensation.
- Rinse and pat the vulva dry after urinating.
- After bathing, apply a thin layer of a preservative-free oil or petroleum jelly to hold in moisture and protect the skin.
- Avoid using a hair dryer to dry the vulvar area.
- Try cold compresses or gel packs on the vulva.
- Avoid exercises that put pressure directly on the vulva, such as bicycling.
Over-the-counter gels and lubricants
Applying the anesthetic gel lidocaine to your vulva about 10 minutes before sex may make it more comfortable. To stop the gel getting on your partner, either wipe it off just before having sex or ask your partner to wear a condom (if using condoms, use latex-free ones as latex condoms can be damaged by lidocaine).
If your pain is more constant, applying lidocaine regularly throughout the day may help. Lidocaine can also be used overnight. A tip is to put some on a cotton make-up removal pad and put it onto the sore area so it’s held in place by your underwear.
It’s very common to have some burning when the lidocaine is initially applied which can last several minutes before going numb. Try to give the lidocaine time it to work, but if the burning continues for 10 minutes, wash it off thoroughly.
Tubes of 5% lidocaine gel, cream or ointment can be bought over the counter from a pharmacy, although it’s a good idea to get a doctor’s advice before trying it.
Vaginal lubricants and aqueous cream (also available over the counter) may soothe the area and help moisturize the vulva if it’s dry. Speak to your pharmacist about these treatments.
Coping and support
You might find talking to other women who have vulvodynia helpful because it can provide information and make you feel less alone. If you don’t want to join a support group, your doctor might be able to recommend a counselor in your area who has experience helping women cope with vulvodynia.
Sex therapy or couples therapy might help you and your partner cope with vulvodynia’s affect on your relationship.
Vulvodynia diet
Some patients find that following a diet that is low in oxalates and taking calcium citrate supplements is helpful, although the evidence to support this approach is limited 10. Foods that are high in oxalates include greens, nuts, tea, chocolate, and soy products 11. Food high in oxalates may produce urine that is irritating, which contributes to the vulvar pain 12.
- National Vulvodynia Association. (2016). Vulvodynia: A common and under-recognized pain disorder in women and female adolescents – Integrating current knowledge into clinical practice. https://cme.dannemiller.com/articles/activity?id=570&f=1[↩]
- Arnold, L. D., Bachmann, G. A., Rosen, R., & Rhoads, G. G. (2007). Assessment of vulvodynia symptoms in a sample of U.S. women: A prevalence survey with a nested case control study. American Journal of Obstetrics and Gynecology, 196(2), 128e1-128e6[↩]
- Harlow, B. L., Kunitz, C. G., Nguyen, R. H. N., Rydell, S. A., Turner, R. M., & MacLehose, R. F. (2014). Prevalence of symptoms consistent with a diagnosis of vulvodynia: Population-based estimates from two geographical regions. American Journal of Obstetrics and Gynecology, 210(1), 40.e1–40.e8.[↩]
- National Vulvodynia Association. (2012). What is vulvodynia? https://www.nva.org/what-is-vulvodynia/[↩][↩]
- American College of Obstetricians and Gynecologists. (2014). Vulvodynia. Frequently Asked Questions (FAQ 127). https://www.acog.org/Patients/FAQs/Vulvodynia[↩]
- Bergeron, S., Binik, Y. M., Khalifé, S., Pagidas, K., Glazer, H. I., Meana, M., & Amsel, R. (2001). A randomized comparison of group cognitive-behavioral therapy, surface electromyographic biofeedback, and vestibulectomy in the treatment of dyspareunia resulting from vulvar vestibulitis. Pain, 91, 297–306.[↩][↩]
- Reed, B. D. (2006). Vulvodynia: Diagnosis and management. American Family Physician, 73, 1231–1238. https://www.aafp.org/afp/2006/0401/p1231.html[↩][↩]
- American College of Obstetricians and Gynecologists. (2011). Vulvodynia. Frequently Asked Questions (FAQ 127). Washington, DC: American College of Obstetricians and Gynecologists. https://www.acog.org/-/media/For-Patients/faq127.pdf?dmc=1&ts=20160817T1318087562[↩]
- Haefner, H. K., Collins, M. E., Davis, G. D., Edwards, L., Foster, D. C., Hartmann, E. H., et al. (2005). The vulvodynia guideline. Journal of Lower Genital Tract Disease, 9, 40–51[↩]
- Reed, B.D. (2006). Vulvodynia: Diagnosis and management. American Family Physician, 73, 1231–1238.[↩]
- Mayo Clinic. Kidney stones: Prevention. https://www.mayoclinic.org/diseases-conditions/kidney-stones/symptoms-causes/syc-20355755[↩]
- American College of Obstetricians and Gynecologists. (2011). Vulvodynia. Frequently Asked Questions (FAQ 127). Washington, DC: American College of Obstetricians and Gynecologists. https://www.acog.org/-/media/For-Patients/faq127.pdf?dmc=1&ts=20160817T1318087562 [↩]