Contents
What is ear infection
An ear infection is an inflammation of the middle ear, usually caused by bacteria, that occurs when fluid builds up behind the eardrum 1. Anyone can get an ear infection, but children get them more often than adults. Ear infections are the most common reason parents bring their child to a doctor. Three out of four children will have at least one ear infection by their third birthday 2. The scientific name for an ear infection is otitis media (OM).
Otitis media is among the most common issues faced by physicians caring for children. Approximately 80% of children will have at least one episode of acute otitis media (AOM), and between 80% and 90% will have at least one episode of otitis media with effusion (OME) before school age 3, 4.
Adults can also get ear infections, but they are less common.
Your health care provider will diagnose an ear infection by looking inside the ear with an instrument called an otoscope.
Often, ear infections go away on their own. Your health care provider may recommend pain relievers. Severe infections and infections in young babies may require antibiotics.
Children who get infections often may need surgery to place small tubes inside their ears. The tubes relieve pressure in the ears so that the child can hear again. However, tympanostomy tubes may increase the risk of long-term tympanic membrane abnormalities and reduced hearing compared with medical therapy 5.
Infants Eight Weeks or Younger
Young infants are at increased risk of severe sequelae from suppurative acute otitis media. Middle ear pathogens found in neonates younger than two weeks include group B streptococcus, gram-negative enteric bacteria, and Chlamydia trachomatis 6. Febrile neonates younger than two weeks with apparent AOM should have a full sepsis workup, which is indicated for any febrile neonate 6. Empiric amoxicillin is acceptable for infants older than two weeks with upper respiratory tract infection and acute otitis media who are otherwise healthy 7.
Ear infection in adults
There is little published information to guide the management of otitis media in adults 8. Adults with new-onset unilateral, recurrent acute otitis media (AOM) greater than two episodes per year or persistent otitis media with effusion (OME) greater than six weeks should receive additional evaluation to rule out a serious underlying condition, such as mechanical obstruction, which in rare cases is caused by nasopharyngeal carcinoma 8. Isolated acute otitis media or transient OME may be caused by eustachian tube dysfunction from a viral upper respiratory tract infection; however, adults with recurrent acute otitis media or persistent OME should be referred to an otolaryngologist 8.
The Ear
The ear, has outer, middle, and inner parts. The ear also functions in the sense of equilibrium.
Outer (External) Ear
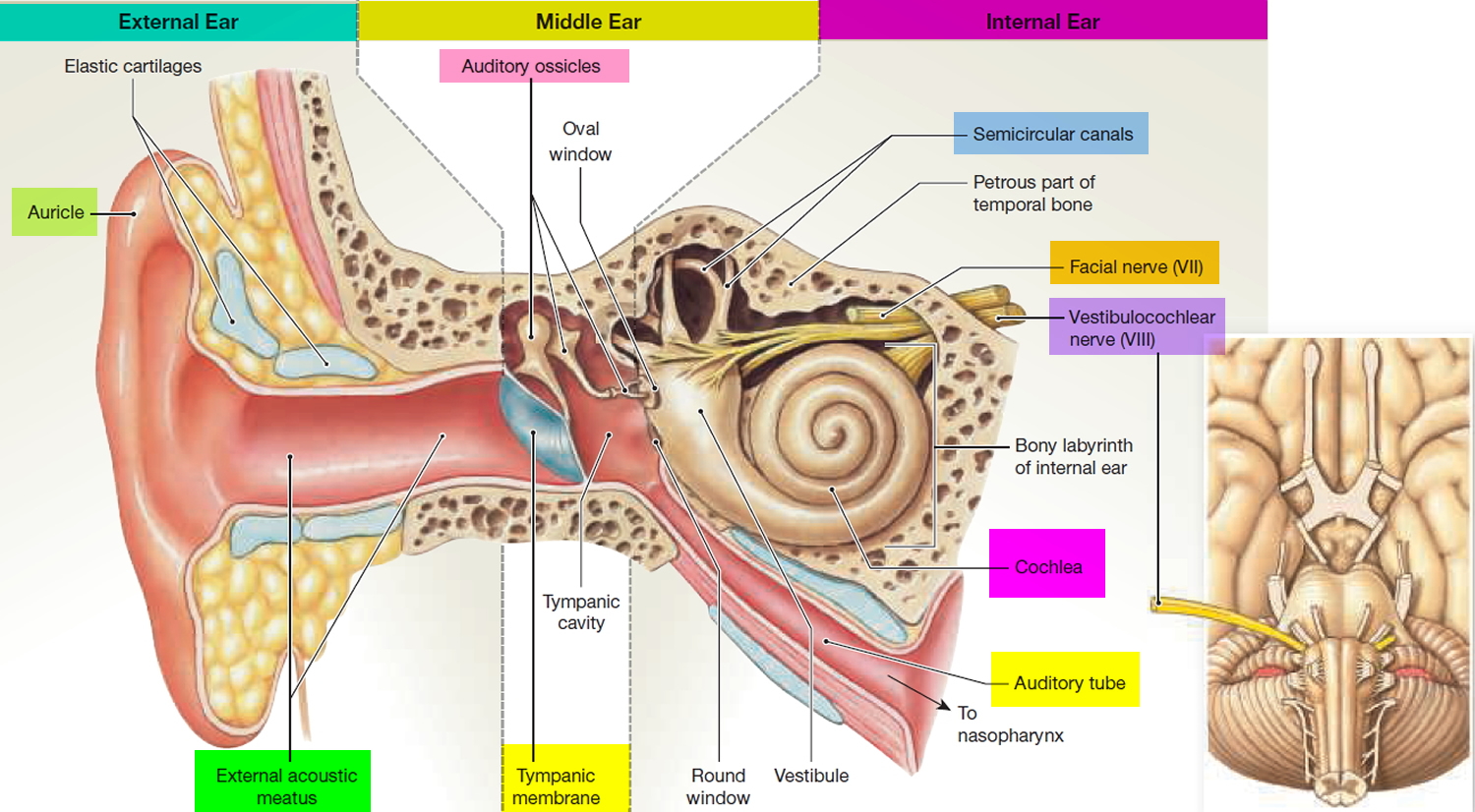
The outer ear consists of three parts. The first is an outer, funnel-like structure called the auricle or pinna. The second is an S-shaped tube called the external acoustic meatus or external auditory canal, that leads inward through the temporal bone for about 2.5 centimeters (Figure 1). The meatus terminates with the third part, the eardrum or tympanic membrane.
The transmission of vibrations through matter produces sound. These vibrations travel in waves, much like ripples on the surface of a pond. The higher the wave, the louder the sound. The more waves per second, the higher the frequency, or pitch, of the sound. Vibrating strings on a guitar or reeds on an oboe produce the sounds of these musical instruments, and vibrating vocal folds (vocal cords) in the larynx produce the voice. The auricle of the ear helps collect sound waves traveling through the air and directs them into the external acoustic meatus. At the end of the meatus, the sound waves reach the eardrum.
The eardrum is a semitransparent membrane covered by a thin layer of skin on its outer surface and by mucous membrane on the inside. It has an oval margin and is coneshaped, with the apex of the cone directed inward. The attachment of one of the auditory ossicles (the malleus) maintains the eardrum’s cone shape. Sound waves that enter the external acoustic meatus change the pressure on the eardrum, which vibrates back and forth in response and thus reproduces the vibrations of the sound-wave source.
Middle Ear
The middle ear, or tympanic cavity, is an air-filled space in the temporal bone. It contains three small bones called auditory ossicles: the malleus, the incus, and the stapes (Figure 1). Tiny ligaments attach them to the wall of the tympanic cavity, and they are covered by mucous membrane. These bones bridge the eardrum and the inner ear, transferring vibrations between these parts. Specifically, the malleus attaches to the eardrum, and when the eardrum vibrates, the malleus vibrates in unison. The malleus causes the incus to vibrate, and the incus passes the movement on to the stapes. An oval ligament holds the stapes to an opening in the wall of the tympanic cavity called the oval window, which leads into the inner ear. Vibration of the stapes at the oval window moves a fluid in the inner ear, which stimulates the hearing receptors.
The auditory ossicles help increase (amplify) the force of vibrations as they pass from the eardrum to the oval window, in addition to transferring vibrations. The vibrational force concentrates as it moves from the outer to the inner ear because the ossicles transmit vibrations from the relatively large surface of the eardrum to a much smaller area at the oval window. As a result, the pressure (per square millimeter) that the stapes applies on the oval window is many times greater than the pressure that sound waves exert on the eardrum.
Auditory Tube
An auditory tube or eustachian tube, connects each middle ear to the back of the nasal cavity (nasopharynx). This tube conducts air between the tympanic cavity and the outside of the body by way of the nose and mouth. The auditory tube helps maintain equal air pressure on both sides of the eardrum, which is necessary for normal hearing.
The function of the auditory tube is noticeable during rapid changes in altitude. As a person moves from a higher altitude to a lower one, air pressure on the outside of the eardrum increases. This may push the eardrum inward, impairing hearing. When the air pressure difference is great enough, air movement through the auditory tube equalizes the pressure on both sides of the eardrum, and the membrane moves back into its regular position. This restores normal hearing and is associated with a popping sound.
Inner (Internal) Ear
Next to the middle ear in the bone of the skull is a small compartment which contains the hearing and balance apparatus known as the inner ear. The inner ear is a complex system of communicating chambers and tubes called a labyrinth. Each ear has two parts to the labyrinth—the bony (osseus) labyrinth and the membranous labyrinth. The bony labyrinth is a cavity within the temporal bone. The membranous labyrinth is a tube of similar shape that lies within the bony labyrinth. Between the bony and membranous labyrinths is a fluid called perilymph, which is secreted by cells in the wall of the bony labyrinth. The membranous labyrinth contains another fluid, called endolymph.
The parts of the labyrinths include three membranous semicircular ducts within three bony semicircular canals, and a cochlea. The semicircular canals and associated structures provide a sense of equilibrium or balance. The cochlea functions in hearing.
The cochlea is shaped like a snail and is divided into two chambers by a membrane. The chambers are full of fluid which vibrates when sound comes in and causes the small hairs which line the membrane to vibrate and send electrical impulses to the brain.
The semi-circular canals are also known as the labyrinthine. These little canals are lined up at right angles (90°) to each other. This allows the brain to know in which direction the head is moving. These semi-circular canals are filled with fluid and have some small calcium crystals embedded in the lining.
Coming from the inner ear and running to the brain is the eighth cranial nerve, the auditory nerve. This nerve carries both balance and hearing information to the brain. Along with the eighth cranial nerve runs the seventh cranial nerve. The seventh cranial nerve is also known as the facial nerve because it supplies nerve impulses to the muscles of the face.
How does the hearing system work ?
The outer ear captures sound waves. The sound travels down the ear canal and hits the ear drum. The ear drum vibrates which causes the ossicles (middle ear bones) to vibrate. A piston action of the ossicles creates a wave in the fluid in the inner ear. The fluid wave stimulates the hair cells in the cochlea and an electrical impulse is sent through the eighth cranial nerve to the brain.
The balance system works by sending continuous electrical impulses to the brain. Moving the head causes the fluid in the semi-circular canals to shift. This in turn changes the electrical impulses to the brain. The brain uses this information to make any adjustments the body needs for balance.
Figure 1. The Ear showing outer (auricle), middle and inner parts
Figure 2. Normal ear drum (tympanic membrane) (otoscopic view)
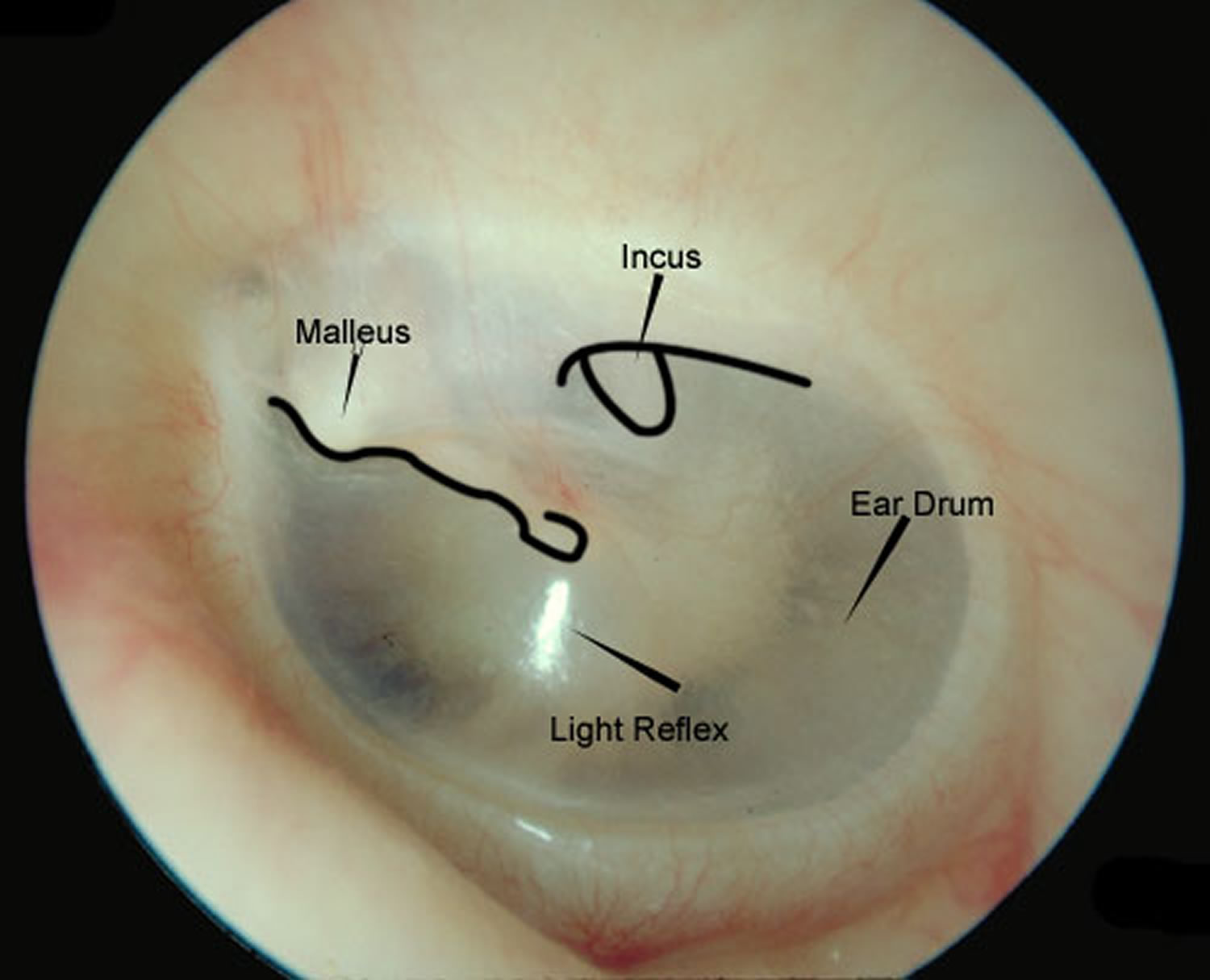
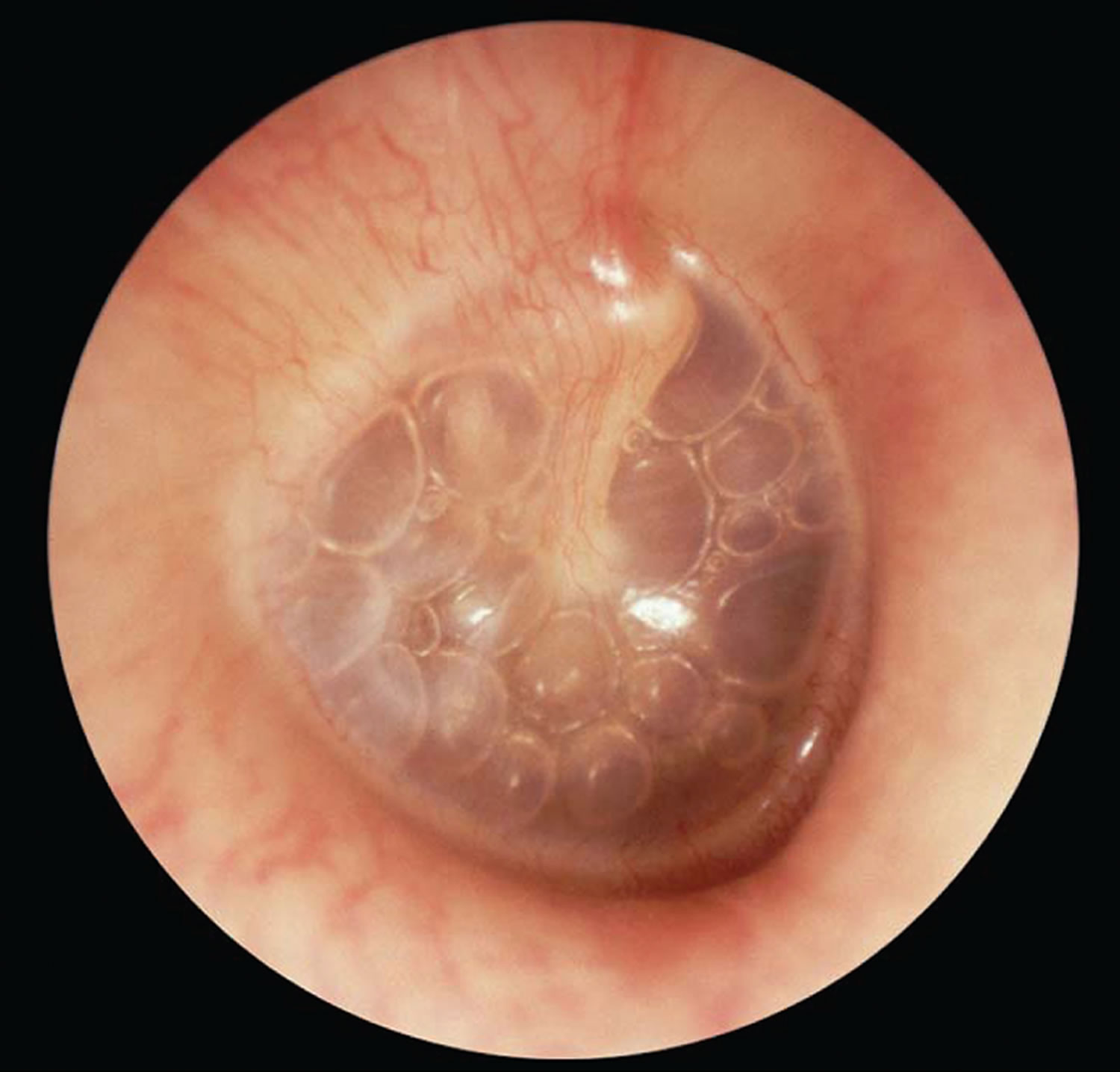
Figure 3. Middle Ear Infection or Otitis Media with Effusion (OME) (otoscopic view)
Causes of ear infection
Usually, acute otitis media is a complication of eustachian tube dysfunction that occurred during an acute viral upper respiratory tract infection 8. An ear infection usually is caused by bacteria and often begins after a child has a sore throat, cold, or other upper respiratory infection. If the upper respiratory infection is bacterial, these same bacteria may spread to the middle ear; if the upper respiratory infection is caused by a virus, such as a cold, bacteria may be drawn to the microbe-friendly environment and move into the middle ear as a secondary infection. Because of the infection, fluid builds up behind the eardrum.
Bacteria can be isolated from middle ear fluid cultures in 50% to 90% of cases of acute otitis media (AOM) and otitis media with effusion (OME). Streptococcus pneumoniae, Haemophilus influenzae (nontypable), and Moraxella catarrhalis are the most common organisms 9, 10. H. influenzae has become the most prevalent organism among children with severe or refractory acute otitis media following the introduction of the pneumococcal conjugate vaccine 11, 12. Risk factors for acute otitis media are listed in Table 1.
Table 1. Risk Factors for Acute Otitis Media 13, 14
Age (younger) |
Allergies |
Craniofacial abnormalities |
Exposure to environmental smoke or other respiratory irritants |
Exposure to group day care |
Family history of recurrent acute otitis media |
Gastroesophageal reflux |
Immunodeficiency |
No breastfeeding |
Pacifier use |
Upper respiratory tract infections |
Why are children more likely than adults to get ear infections ?
There are several reasons why children are more likely than adults to get ear infections.
Eustachian tubes are smaller and more level in children than they are in adults. This makes it difficult for fluid to drain out of the ear, even under normal conditions. If the eustachian tubes are swollen or blocked with mucus due to a cold or other respiratory illness, fluid may not be able to drain.
A child’s immune system isn’t as effective as an adult’s because it’s still developing. This makes it harder for children to fight infections.
As part of the immune system, the adenoids respond to bacteria passing through the nose and mouth. Sometimes bacteria get trapped in the adenoids, causing a chronic infection that can then pass on to the eustachian tubes and the middle ear.
Can ear infections be prevented ?
Currently, the best way to prevent ear infections is to reduce the risk factors associated with them. Here are some things you might want to do to lower your child’s risk for ear infections 1.
- Vaccinate your child against the flu. Make sure your child gets the influenza, or flu, vaccine every year.
- It is recommended that you vaccinate your child with the 13-valent pneumococcal conjugate vaccine (PCV13). The PCV13 protects against more types of infection-causing bacteria than the previous vaccine, the PCV7. If your child already has begun PCV7 vaccination, consult your physician about how to transition to PCV13. The Centers for Disease Control and Prevention (CDC) recommends that children under age 2 be vaccinated, starting at 2 months of age. Studies have shown that vaccinated children get far fewer ear infections than children who aren’t vaccinated. The vaccine is strongly recommended for children in daycare.
- Wash hands frequently. Washing hands prevents the spread of germs and can help keep your child from catching a cold or the flu.
- Avoid exposing your baby to cigarette smoke. Studies have shown that babies who are around smokers have more ear infections.
- Never put your baby down for a nap, or for the night, with a bottle.
- Don’t allow sick children to spend time together. As much as possible, limit your child’s exposure to other children when your child or your child’s playmates are sick.
Ear infection symptoms
The infection usually affects the middle ear and is called otitis media. The tubes inside the ears become clogged with fluid and mucus. This can affect hearing, because sound cannot get through all that fluid.
If your child isn’t old enough to say “My ear hurts,” here are a few things to look for 2:
- Tugging at ears
- Crying more than usual
- Fluid draining from the ear
- Trouble sleeping
- Balance difficulties
- Hearing problems.
Signs of ear infection
There are three main types of ear infections 1. Each has a different combination of symptoms.
- Acute otitis media (AOM) is the most common ear infection. Parts of the middle ear are infected and swollen and fluid is trapped behind the eardrum. This causes pain in the ear—commonly called an earache. Your child might also have a fever.
- Otitis media with effusion (OME) sometimes happens after an ear infection has run its course and fluid stays trapped behind the eardrum. A child with OME may have no symptoms, but a doctor will be able to see the fluid behind the eardrum with a special instrument.
- Chronic otitis media with effusion (COME) happens when fluid remains in the middle ear for a long time or returns over and over again, even though there is no infection. COME makes it harder for children to fight new infections and also can affect their hearing.
How does a doctor diagnose a middle ear infection ?
The first thing a doctor will do is ask you about your child’s health. Has your child had a head cold or sore throat recently ? Is he having trouble sleeping ? Is she pulling at her ears ? If an ear infection seems likely, the simplest way for a doctor to tell is to use a lighted instrument, called an otoscope, to look at the eardrum. A red, bulging eardrum indicates an infection.
A doctor also may use a pneumatic otoscope, which blows a puff of air into the ear canal, to check for fluid behind the eardrum. A normal eardrum will move back and forth more easily than an eardrum with fluid behind it.
Tympanometry, which uses sound tones and air pressure, is a diagnostic test a doctor might use if the diagnosis still isn’t clear. A tympanometer is a small, soft plug that contains a tiny microphone and speaker as well as a device that varies air pressure in the ear. It measures how flexible the eardrum is at different pressures.
The updated American Academy of Pediatrics guideline recently endorses more stringent otoscopic criteria for diagnosis of acute otitis media 13. An acute otitis media diagnosis requires moderate to severe bulging of the tympanic membrane (Figure 4), new onset of otorrhea (ear discharge) not caused by otitis externa, or mild bulging of the tympanic membrane associated with recent onset of ear pain (less than 48 hours) or erythema. Acute otitis media should not be diagnosed in children who do not have objective evidence of middle ear effusion 13. An inaccurate diagnosis can lead to unnecessary treatment with antibiotics and contribute to the development of antibiotic resistance.
Otitis media with effusion (OME) is defined as middle ear effusion in the absence of acute symptoms 15, 16. If otitis media with effusion is suspected and the presence of effusion on otoscopy is not evident by loss of landmarks, pneumatic otoscopy, tympanometry, or both should be used 16. Pneumatic otoscopy is a useful technique for the diagnosis of acute otitis media and otitis media with effusion 17 and is 70% to 90% sensitive and specific for determining the presence of middle ear effusion. By comparison, simple otoscopy is 60% to 70% accurate 16. Inflammation with bulging of the tympanic membrane on otoscopy is highly predictive of acute otitis media. Pneumatic otoscopy is most helpful when cerumen is removed from the external auditory canal.
Tympanometry and acoustic reflectometry are valuable adjuncts to otoscopy or pneumatic otoscopy 16. Tympanometry has a sensitivity and specificity of 70% to 90% for the detection of middle ear fluid, but is dependent on patient cooperation 18. Combined with normal otoscopy findings, a normal tympanometry result may be helpful to predict absence of middle ear effusion. Acoustic reflectometry has lower sensitivity and specificity in detecting middle ear effusion and must be correlated with the clinical examination 19. Tympanocentesis is the preferred method for detecting the presence of middle ear effusion and documenting bacterial etiology, but is rarely performed in the primary care setting 13.
Figure 4. Otoscopic view of acute otitis media
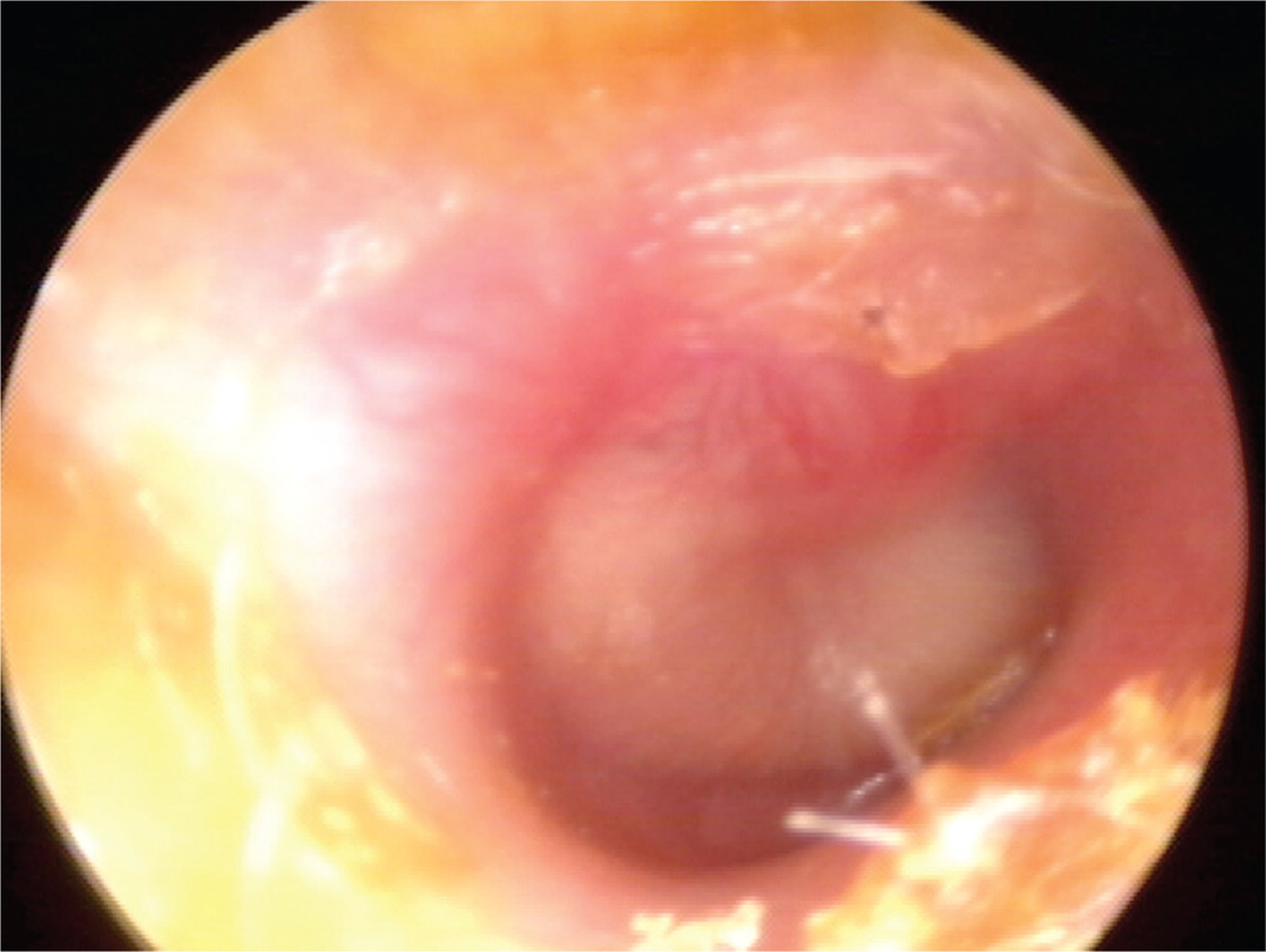
Note: Erythema (redness) and bulging of the tympanic membrane with loss of normal landmarks.
Ear infection treatment
Table 2. Treatment Strategy for Acute Otitis Media
Initial presentation |
Diagnosis established by physical examination findings and presence of symptoms |
Treat pain |
Children six months or older with otorrhea or severe signs or symptoms (moderate or severe otalgia, otalgia for at least 48 hours, or temperature of 102.2°F [39°C] or higher): antibiotic therapy for 10 days |
Children six to 23 months of age with bilateral acute otitis media without severe signs or symptoms: antibiotic therapy for 10 days |
Children six to 23 months of age with unilateral acute otitis media without severe signs or symptoms: observation or antibiotic therapy for 10 days |
Children two years or older without severe signs or symptoms: observation or antibiotic therapy for five to seven days |
Persistent symptoms (48 to 72 hours) |
Repeat ear examination for signs of otitis media |
If otitis media is present, initiate or change antibiotic therapy |
If symptoms persist despite appropriate antibiotic therapy, consider intramuscular ceftriaxone (Rocephin), clindamycin, or tympanocentesis |
PAIN RELIEF
Analgesics are recommended for symptoms of ear pain, fever, and irritability 13, 20. Analgesics are particularly important at bedtime because disrupted sleep is one of the most common symptoms motivating parents to seek care. Ibuprofen and acetaminophen have been shown to be effective 21. Ibuprofen is preferred, given its longer duration of action and its lower toxicity in the event of overdose 4. Topical analgesics, such as benzocaine, can also be helpful 22.
OBSERVATION VS. ANTIBIOTIC THERAPY
Antibiotic-resistant bacteria remain a major public health challenge. A widely endorsed strategy for improving the management of acute otitis media involves deferring antibiotic therapy in patients least likely to benefit from antibiotics 23. Antibiotics should be routinely prescribed for children with acute otitis media who are six months or older with severe signs or symptoms (i.e., moderate or severe ear pain, ear pain for at least 48 hours, or temperature of 102.2°F [39°C] or higher), and for children younger than two years with bilateral acute otitis media regardless of additional signs or symptoms 13.
Among children with mild symptoms, observation may be an option in those six to 23 months of age with unilateral acute otitis media, or in those two years or older with bilateral or unilateral acute otitis media 13, 15, 24. A large prospective study of this strategy found that two out of three children will recover without antibiotics 25. Recently, the American Academy of Family Physicians recommended not prescribing antibiotics for otitis media in children two to 12 years of age with nonsevere symptoms if observation is a reasonable option 26, 27. If observation is chosen, a mechanism must be in place to ensure appropriate treatment if symptoms persist for more than 48 to 72 hours. Strategies include a scheduled follow-up visit or providing patients with a backup antibiotic prescription to be filled only if symptoms persist 28.
ANTIBIOTIC SELECTION
Table 3 summarizes the antibiotic options for children with acute otitis media 13. High-dose amoxicillin should be the initial treatment in the absence of a known allergy 13, 15, 29. The advantages of amoxicillin include low cost, acceptable taste, safety, effectiveness, and a narrow microbiologic spectrum. Children who have taken amoxicillin in the past 30 days, who have conjunctivitis, or who need coverage for β-lactamase–positive organisms should be treated with high-dose amoxicillin/clavulanate (Augmentin) 13.
Table 3. Antibiotic options for children with acute otitis media 30
| Initial immediate or delayed antibiotic treatment | Antibiotic treatment after 48–72 h of failure of initial antibiotic treatment | ||||
|---|---|---|---|---|---|
| Recommended first-line treatment | Alternative treatment (if penicillin allergy) | Recommended first-line treatment | Alternative treatment | ||
|
|
|
| ||
NOTE: Cefdinir, cefuroxime, cefpodoxime, and ceftriaxone are highly unlikely to be associated with cross-reactivity with penicillin allergy on the basis of their distinct chemical structures.
IM = intramuscular; IV = intravenous.
*—May be considered in patients who have received amoxicillin in the previous 30 d or who have the otitis-conjunctivitis syndrome.
†—Perform tympanocentesis/drainage if skilled in the procedure, or seek a consultation from an otolaryngologist for tympanocentesis/drainage. If the tympanocentesis reveals multidrug-resistant bacteria, seek an infectious disease specialist consultation.
Oral cephalosporins, such as cefuroxime (Ceftin), may be used in children who are allergic to penicillin. Recent research indicates that the degree of cross reactivity between penicillin and second- and third-generation cephalosporins is low (less than 10% to 15%), and avoidance is no longer recommended 31. Because of their broad-spectrum coverage, third-generation cephalosporins in particular may have an increased risk of selection of resistant bacteria in the community 32. High-dose azithromycin (Zithromax; 30 mg per kg, single dose) appears to be more effective than the commonly used five-day course, and has a similar cure rate as high-dose amoxicillin/clavulanate 13, 33, 34. However, excessive use of azithromycin is associated with increased resistance, and routine use is not recommended 13. Trimethoprim/sulfamethoxazole is no longer effective for the treatment of acute otitis media due to evidence of S. pneumoniae resistance 35.
Intramuscular or intravenous ceftriaxone (Rocephin) should be reserved for episodes of treatment failure or when a serious comorbid bacterial infection is suspected 4. One dose of ceftriaxone may be used in children who cannot tolerate oral antibiotics because it has been shown to have similar effectiveness as high-dose amoxicillin 36, 37. A three-day course of ceftriaxone is superior to a one-day course in the treatment of nonresponsive AOM caused by penicillin-resistant S. pneumoniae 37. Although some children will likely benefit from intramuscular ceftriaxone, overuse of this agent may significantly increase high-level penicillin resistance in the community 4. High-level penicillin-resistant pneumococci are also resistant to first- and third-generation cephalosporins.
Antibiotic therapy for acute otitis media is often associated with diarrhea 38. Probiotics and yogurts containing active cultures reduce the incidence of diarrhea and should be suggested for children receiving antibiotics for acute otitis media 38. There is no compelling evidence to support the use of complementary and alternative treatments in acute otitis media 13.
PERSISTENT OR RECURRENT EAR INFECTION
Children with persistent, significant acute otitis media symptoms despite at least 48 to 72 hours of antibiotic therapy should be reexamined 13. If a bulging, inflamed tympanic membrane is observed, therapy should be changed to a second-line agent 4. For children initially on amoxicillin, high-dose amoxicillin/clavulanate is recommended 13.
For children with an amoxicillin allergy who do not improve with an oral cephalosporin, intramuscular ceftriaxone, clindamycin, or tympanocentesis may be considered 13. If symptoms recur more than one month after the initial diagnosis of acute otitis media, a new and unrelated episode of acute otitis media should be assumed 15. For children with recurrent AOM (i.e., three or more episodes in six months, or four episodes within 12 months with at least one episode during the preceding six months) with middle ear effusion, tympanostomy tubes may be considered to reduce the need for systemic antibiotics in favor of observation, or topical antibiotics for tube otorrhea 15. However, tympanostomy tubes may increase the risk of long-term tympanic membrane abnormalities and reduced hearing compared with medical therapy 5. Other strategies may help prevent recurrence (Table 4).
Probiotics, particularly in infants, have been suggested to reduce the incidence of infections during the first year of life. Although available evidence has not demonstrated that probiotics prevent respiratory infections 39, probiotics do not cause adverse effects and need not be discouraged. Antibiotic prophylaxis is not recommended 13.
Table 4. Strategies for Preventing Recurrent Otitis Media
Check for undiagnosed allergies leading to chronic rhinorrhea |
Eliminate bottle propping and pacifiers 40 |
Eliminate exposure to passive smoke 41 |
Routinely immunize with the pneumococcal conjugate and influenza vaccines 42 |
Use xylitol gum in appropriate children (two pieces, five times a day after meals and chewed for at least five minutes) 43 |
[Source 8]
Treatment of Otitis Media with Effusion (OME)
Management of otitis media with effusion (OME) is summarized in Table 5. Two rare complications of OME are transient hearing loss potentially associated with language delay, and chronic anatomic injury to the tympanic membrane requiring reconstructive surgery 16. Children should be screened for speech delay at all visits. If a developmental delay is apparent or middle ear structures appear abnormal, the child should be referred to an otolaryngologist 16. Antibiotics, decongestants, and nasal steroids do not hasten the clearance of middle ear fluid and are not recommended 16, 44.
Table 5. Diagnosis and Treatment of Otitis Media with Effusion 16
Evaluate tympanic membranes at every well-child and sick visit if feasible; perform pneumatic otoscopy or tympanometry when possible (consider removing cerumen) |
If transient effusion is likely, reevaluate at three-month intervals, including screening for language delay; if there is no anatomic damage or evidence of developmental or behavioral complications, continue to observe at three- to six-month intervals; if complications are suspected, refer to an otolaryngologist |
For effusion that appears to be associated with anatomic damage, such as adhesive otitis media or retraction pockets, reevaluate in four to six weeks; if abnormality persists, refer to an otolaryngologist |
Antibiotics, decongestants, and nasal steroids are not indicated |
Tympanostomy Tube Placement
Tympanostomy tubes are appropriate for children six months to 12 years of age who have had bilateral otitis media with effusion (OME) for three months or longer with documented hearing difficulties, or for children with recurrent acute otitis media who have evidence of middle ear effusion at the time of assessment for tube candidacy. Tubes are not indicated in children with a single episode of otitis media with effusion (OME) of less than three months’ duration, or in children with recurrent acute otitis media who do not have middle ear effusion in either ear at the time of assessment for tube candidacy. Children with chronic otitis media with effusion (OME) who did not receive tubes should be reevaluated every three to six months until the effusion is no longer present, hearing loss is detected, or structural abnormalities of the tympanic membrane or middle ear are suspected 45.
Children with tympanostomy tubes who present with acute uncomplicated otorrhea should be treated with topical antibiotics and not oral antibiotics. Routine, prophylactic water precautions such as ear plugs, headbands, or avoidance of swimming are not necessary for children with tympanostomy tubes 45.
- National Institute on Deafness and Other Communication Disorders, National Institutes of Health. Ear Infections in Children. https://www.nidcd.nih.gov/health/ear-infections-children[↩][↩][↩]
- U.S. National Library of Medicine. Medline Plus. Ear Infections. https://medlineplus.gov/earinfections.html[↩][↩]
- Tos M. Epidemiology and natural history of secretory otitis. Am J Otol. 1984;5(6):459–462.[↩]
- Burrows HL, Blackwood RA, Cooke JM, et al.; Otitis Media Guideline Team. University of Michigan Health System otitis media guideline. http://www.med.umich.edu/1info/FHP/practiceguides/om/OM.pdf[↩][↩][↩][↩][↩]
- Stenstrom R, Pless IB, Bernard P. Hearing thresholds and tympanic membrane sequelae in children managed medically or surgically for otitis media with effusion [published correction appears in Arch Pediatr Adolesc Med. 2006;160(6):588]. Arch Pediatr Adolesc Med. 2005;159(12):1151–1156.[↩][↩]
- Nozicka CA, Hanly JG, Beste DJ, et al. Otitis media in infants aged 0–8 weeks: frequency of associated serious bacterial disease. Pediatr Emerg Care. 1999;15(4):252–254.[↩][↩]
- Turner D, Leibovitz E, Aran A, et al. Acute otitis media in infants younger than two months of age: microbiology, clinical presentation and therapeutic approach. Pediatr Infect Dis J. 2002;21(7):669–674.[↩]
- Otitis Media: Diagnosis and Treatment. Am Fam Physician. 2013 Oct 1;88(7):435-440. http://www.aafp.org/afp/2013/1001/p435.html[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Jacobs MR, Dagan R, Appelbaum PC, Burch DJ. Prevalence of antimicrobial-resistant pathogens in middle ear fluid. Antimicrob Agents Chemother. 1998;42(3):589–595.[↩]
- Arrieta A, Singh J. Management of recurrent and persistent acute otitis media: new options with familiar antibiotics. Pediatr Infect Dis J. 2004;23(2 suppl):S115–S124.[↩]
- Block SL, Hedrick J, Harrison CJ, et al. Community-wide vaccination with the heptavalent pneumococcal conjugate significantly alters the microbiology of acute otitis media. Pediatr Infect Dis J. 2004;23(9):829–833.[↩]
- Coker TR, Chan LS, Newberry SJ, et al. Diagnosis, microbial epidemiology, and antibiotic treatment of acute otitis media in children: a systematic review. JAMA. 2010;304(19):2161–2169.[↩]
- Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964–e999.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Daly KA, Giebink GS. Clinical epidemiology of otitis media. Pediatr Infect Dis J. 2000;19(5 suppl):S31–S36.[↩]
- Shekelle PG, Takata G, Newberry SJ, et al. Management of acute otitis media: update. Evid Rep Technol Assess (Full Rep). 2010;(198):1–426.[↩][↩][↩][↩][↩]
- American Academy of Family Physicians; American Academy of Otolaryngology-Head and Neck Surgery; American Academy of Pediatrics Subcommittee on Otitis Media with Effusion. Otitis media with effusion. Pediatrics. 2004;113(5):1412–1429.[↩][↩][↩][↩][↩][↩][↩][↩]
- Pelton SI. Otoscopy for the diagnosis of otitis media. Pediatr Infect Dis J. 1998;17(6):540–543.[↩]
- Watters GW, Jones JE, Freeland AP. The predictive value of tympanometry in the diagnosis of middle ear effusion. Clin Otolayngol Allied Sci. 1997;22(4):343–345.[↩]
- Kimball S. Acoustic reflectometry: spectral gradient analysis for improved detection of middle ear effusion in children. Pediatr Infect Dis J. 1998;17(6):552–555.[↩]
- American Academy of Pediatrics. Committee on Psychosocial Aspects of Child and Family Health; Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108(3):793–797.[↩]
- Bertin L, Pons G, d’Athis P, et al. A randomized, double-blind, multi-centre controlled trial of ibuprofen versus acetaminophen and placebo for symptoms of acute otitis media in children. Fundam Clin Pharmacol. 1996;10(4):387–392.[↩]
- Hoberman A, Paradise JL, Reynolds EA, et al. Efficacy of Auralgan for treating ear pain in children with acute otitis media. Arch Pediatr Adolesc Med. 1997;151(7):675–678.[↩]
- Venekamp RP, Sanders S, Glasziou PP, et al. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2013;(1):CD000219.[↩]
- Little P, Gould C, Moore M, et al. Predictors of poor outcome and benefits from antibiotics in children with acute otitis media: pragmatic randomised trial. BMJ. 2002;325(7354):22.[↩]
- Marchetti F, Ronfani L, Nibali SC, et al.; Italian Study Group on Acute Otitis Media. Delayed prescription may reduce the use of antibiotics for acute otitis media: a prospective observational study in primary care. Arch Pediatr Adolesc Med. 2005;159(7):679–684.[↩]
- American Academy of Family Physicians. Choosing Wisely. Otitis media. http://www.aafp.org/about/initiatives/choosing-wisely.html[↩]
- Siwek J, Lin KW. Choosing Wisely: more good clinical recommendations to improve health care quality and reduce harm. Am Fam Physician. 2013;88(3):164–168. http://www.aafp.org/afp/recommendations/search.htm[↩]
- Siegel RM, Kiely M, Bien JP, et al. Treatment of otitis media with observation and a safety-net antibiotic prescription. Pediatrics. 2003;112(3 pt 1):527–531.[↩]
- Piglansky L, Leibovitz E, Raiz S, et al. Bacteriologic and clinical efficacy of high dose amoxicillin for therapy of acute otitis media in children. Pediatr Infect Dis J. 2003;22(5):405–413.[↩]
- Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e983.[↩]
- Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol. 2010;105(4):259–273.[↩]
- Arguedas A, Dagan R, Leibovitz E, et al. A multicenter, open label, double tympanocentesis study of high dose cefdinir in children with acute otitis media at high risk of persistent or recurrent infection. Pediatr Infect Dis J. 2006;25(3):211–218.[↩]
- Dagan R, Johnson CE, McLinn S, et al. Bacteriologic and clinical efficacy of amoxicillin/clavulanate vs. azithromycin in acute otitis media [published correction appears in Pediatr Infect Dis J. 2000;19(4):275]. Pediatr Infect Dis J. 2000;19(2):95–104.[↩]
- Arrieta A, Arguedas A, Fernandez P, et al. High-dose azithromycin versus high-dose amoxicillin-clavulanate for treatment of children with recurrent or persistent acute otitis media. Antimicrob Agents Chemother. 2003;47(10):3179–3186.[↩]
- Doern GV, Pfaller MA, Kugler K, et al. Prevalence of antimicrobial resistance among respiratory tract isolates of Streptococcus pneumoniae in North America: 1997 results from the SENTRY antimicrobial surveillance program. Clin Infect Dis. 1998;27(4):764–770.[↩]
- Green SM, Rothrock SG. Single-dose intramuscular ceftriaxone for acute otitis media in children. Pediatrics. 1993;91(1):23–30.[↩]
- Leibovitz E, Piglansky L, Raiz S, et al. Bacteriologic and clinical efficacy of one day vs. three day intramuscular ceftriaxone for treatment of nonresponsive acute otitis media in children. Pediatr Infect Dis J. 2000;19(11):1040–1045.[↩][↩]
- Johnston BC, Goldenberg JZ, Vandvik PO, et al. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev. 2011(11):CD004827.[↩][↩]
- Weichert S, Schroten H, Adam R. The role of prebiotics and probiotics in prevention and treatment of childhood infectious diseases. Pediatr Infect Dis J. 2012;31(8):859–862.[↩]
- Niemelä M, Pihakari O, Pokka T, et al. Pacifier as a risk factor for acute otitis media: a randomized, controlled trial of parental counseling. Pediatrics. 2000;106(3):483–488.[↩]
- Etzel RA, Pattishall EN, Haley NJ, et al. Passive smoking and middle ear effusion among children in day care. Pediatrics. 1992;90(2 pt 1):228–232.[↩]
- Fireman B, Black SB, Shinefield HR, et al. Impact of the pneumococcal conjugate vaccine on otitis media [published correction appears in Pediatr Infect Dis J. 2003;22(2):163]. Pediatr Infect Dis J. 2003;22(1):10–16.[↩]
- Azarpazhooh A, Limeback H, Lawrence HP, et al. Xylitol for preventing acute otitis media in children up to 12 years of age. Cochrane Database Syst Rev. 2011(11):CD007095.[↩]
- Gluth MB, McDonald DR, Weaver AL, et al. Management of eustachian tube dysfunction with nasal steroid spray: a prospective, randomized, placebo-controlled trial. Arch Otolaryngol Head Neck Surg. 2011;137(5):449–455.[↩]
- Rosenfeld RM, Schwartz SR, Pynnonen MA, et al. Clinical practice guideline: tympanostomy tubes in children. Otolaryngol Head Neck Surg. 2013;149(1 suppl):S1–S35.[↩][↩]