Contents
- What is esophagitis
- What is eosinophilic esophagitis?
- What is gastroesophageal reflux disease (GERD)?
- Gastroesophageal reflux disease causes
- Risk factors for gastroesophageal reflux disease
- Gastroesophageal reflux disease prevention
- Gastroesophageal reflux disease symptoms
- Gastroesophageal reflux disease complications
- Gastroesophageal reflux disease diagnosis
- Gastroesophageal reflux disease differential diagnosis
- Gastroesophageal reflux disease treatments
- Gastroesophageal reflux disease prognosis
What is esophagitis
Esophagitis is present when the lining of the esophagus becomes swollen, inflamed, or irritated 1. Esophagitis is also called erosive esophagitis or ulcerative esophagitis. Esophagitis can cause painful, difficult swallowing. Esophagitis can also lead to chest pain. Various things can cause esophagitis. Some common causes include stomach acids backing up into the esophagus, infection, medicines taken by mouth and allergies. Chronic acid reflux (GERD) is a common cause of esophagitis.
The esophagus is a hollow muscular tube that carries food from your throat (pharynx) to your stomach. The esophagus lies behind the trachea (windpipe) and in front of the spine. In adults, the esophagus is usually between 10 and 13 inches (25 to 33 centimeters [cm]) long and is about ¾ of an inch (2cm) across at its smallest point 2. The esophagus starts with a special ring of muscle called the upper esophageal sphincter, formed in part by the cricopharyngeus muscle, and ends with the lower esophageal sphincter, surrounded by the crural diaphragm 3. When food enters your mouth, it mixes with saliva. The actions of salivary enzymes convert food into a mass called a food bolus. Once the food bolus reaches your throat (pharynx), swallowing starts, and relaxation of the upper esophageal sphincter ensues to allow passage of the food bolus into the esophagus 3. When you swallow, food and liquids travel through the inside of your esophagus called the lumen aided by peristaltic contractions of the esophageal muscles to reach your stomach. The lower part of your esophagus that connects to your stomach is called the gastroesophageal (GE) junction. A special ring of muscle near the gastroesophageal junction, called the lower esophageal sphincter (LES), controls the movement of food from the esophagus into the stomach. Between meals, it closes to keep the stomach’s acid and digestive juices out of the esophagus. When the food bolus finally reaches the distal end of the esophageal body, it triggers relaxation of the lower esophageal sphincter (LES), which in turn permits entry of the food bolus into your stomach.
Esophagitis may feel like:
- A sore throat.
- Heartburn.
- Difficulty swallowing.
- Chest pain.
The pain may be mild to severe and may be constant or come and go.
Depending on the cause and the severity of esophagitis, you might also notice:
- Acid reflux.
- Regurgitations.
- Food getting stuck in your throat.
- Indigestion.
- Feeding difficulties in children.
- Nausea and vomiting.
- Blood in your vomit.
- Mouth sores.
Treatment for esophagitis depends on its exact cause and how badly the tissue that lines the esophagus is damaged. Without treatment, esophagitis can damage this lining. The esophagus may start to have trouble moving food and liquid from the mouth to the stomach. Esophagitis also can lead to other serious health issues. These include scarring or narrowing of the esophagus, unhealthy weight loss, and dehydration.
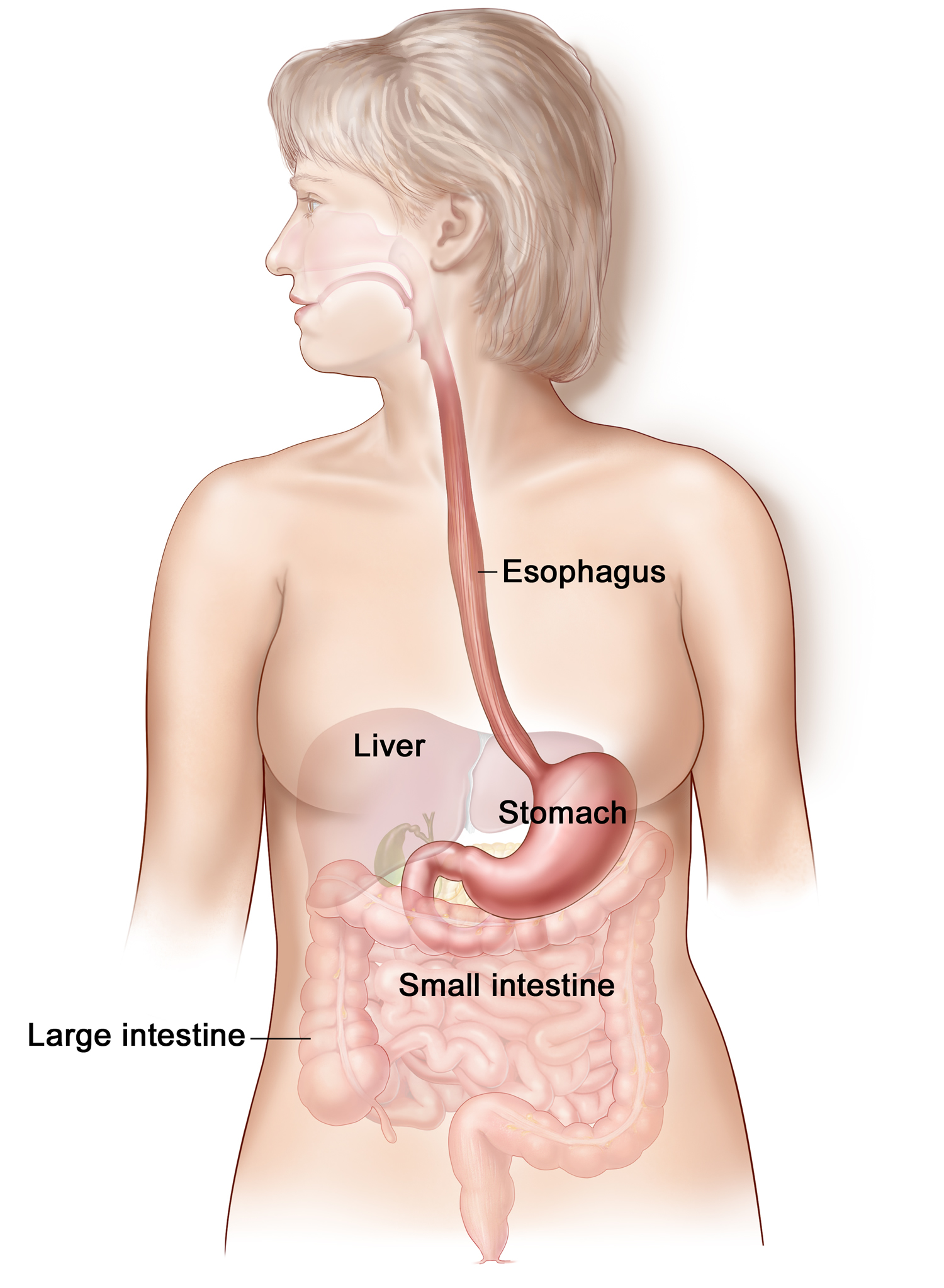
Figure 1. Esophagus
Most symptoms of esophagitis can be caused by a few different conditions that affect your digestive system.
See your doctor if your symptoms:
- Last more than a few days.
- Don’t get better after using medicines called antacids that are available without a prescription.
- Are bad enough to make it hard for you to eat or cause you to lose weight.
- Happen along with flu symptoms such as headache, fever and muscle aches.
Get emergency care if you:
- Have pain in your chest that lasts more than a few minutes.
- Think you have food stuck in your esophagus.
- Have a history of heart disease and feel chest pain.
- Feel pain in your mouth or throat when you eat.
- Have shortness of breath or chest pain that happens soon after eating.
- Vomit large amounts, often have forceful vomiting or have trouble breathing after vomiting.
- Notice that your vomit is yellow or green, looks like coffee grounds, or has blood in it.
Esophagitis causes
Esophagitis is often caused by stomach fluid that flows back into the food pipe. The fluid contains acid, which irritates the tissue. This problem is called gastroesophageal reflux (GER). An autoimmune disorder called eosinophilic esophagitis can also causes esophagitis.
The following increase your risk of esophagitis:
- Alcohol use
- Cigarette smoking
- Surgery or radiation to the chest (for example, treatment for lung cancer)
- Taking certain medicines without drinking plenty of water. These medicines include alendronate, doxycycline, ibandronate, risedronate, tetracycline, potassium tablets, and vitamin C
- Vomiting
People who have a weakened immune system may develop infections. Infections may lead to swelling of the food pipe. Infection may be due to:
- Fungi or yeast (most often Candida)
- Viruses, such as herpes or cytomegalovirus.
Reflux esophagitis
A valve called the lower esophageal sphincter (LES) usually keeps stomach acid out of your esophagus. But sometimes the lower esophageal sphincter (LES) doesn’t close properly. Or it opens when it shouldn’t. In some people, the upper part of the stomach bulges through the large muscle that separates the stomach and the chest. This is known as a hiatal hernia. It also can cause stomach acid to back up into the esophagus.
Gastroesophageal reflux disease (GERD) is a condition in which this backflow of acid is a frequent or ongoing problem. GERD can lead to ongoing swelling and tissue damage in the esophagus.
Eosinophilic esophagitis
Eosinophils are white blood cells that play a key role in allergic reactions. Eosinophilic esophagitis can happen if lots of these white blood cells build up in your esophagus. This most likely happens in response to a substance that causes an allergy, acid reflux or both.
Certain foods may trigger eosinophilic esophagitis, including:
- Milk.
- Eggs.
- Wheat.
- Soy.
- Peanuts.
- Seafood.
Typical allergy testing often is not able to spot these foods as being triggers.
People with eosinophilic esophagitis may have other allergies that aren’t caused by food. For example, sometimes allergens in the air, such as pollen, may be the cause. One common symptom of eosinophilic esophagitis is food getting stuck in the esophagus after swallowing. This is called food impaction. Another common symptom is trouble swallowing, also called dysphagia.
Lymphocytic esophagitis
Lymphocytic esophagitis is a rare condition of the esophagus. With lymphocytic esophagitis, a higher than typical number of white blood cells called lymphocytes build up in the lining of the esophagus. Lymphocytic esophagitis may be related to eosinophilic esophagitis or to gastroesophageal reflux disease (GERD).
Medicine-induced esophagitis
Medicine-induced esophagitis also called drug-induced esophagitis, happens when some medicines taken by mouth cause tissue damage in your esophagus. The damage happens if the medicines stay in contact with the lining of the esophagus for too long. For example, you might swallow a pill with little or no water. If you do that, the pill itself or residue from the pill may stay in the esophagus.
Medicines that have been linked to esophagitis include:
- Pain-relieving medicines such as aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
- Antibiotics such as tetracycline and doxycycline.
- Medicine called potassium chloride that is used to treat low levels of the mineral potassium.
- Medicines called bisphosphonates that treat bone conditions such as osteoporosis. These medicines include alendronate (Binosto, Fosamax).
- A treatment for heart conditions called quinidine.
Infectious esophagitis
An infection in tissues of the esophagus may cause esophagitis. The infection could be due to bacteria, viruses or funguses. Infectious esophagitis is fairly rare. It happens most often in people with weakened immune systems, such as people with HIV/AIDS or cancer.
A fungus usually present in the mouth called Candida albicans is a common cause of infectious esophagitis. This type of fungal infection often is linked with a weakened immune system, diabetes, cancer, or use of steroid or antibiotic medicines.
Risk factors for esophagitis
Risk factors for esophagitis vary depending on the cause of the esophagitis.
Reflux esophagitis
Factors that raise the risk of gastroesophageal reflux disease (GERD) also are factors in reflux esophagitis. These risk factors include the following:
- Eating right before going to bed.
- Eating meals that are too large and fatty.
- Smoking.
- Gaining extra weight, including from pregnancy.
Foods that can make symptoms of GERD or reflux esophagitis worse include:
- Caffeine.
- Alcohol.
- Fatty foods.
- Chocolate.
- Peppermint.
Eosinophilic esophagitis
Risk factors for this allergy-related esophagitis may include:
- A history of certain allergic reactions. These include asthma, atopic dermatitis and allergic rhinitis, also known as hay fever.
- A family history of eosinophilic esophagitis.
Medicine-induced esophagitis
Risk factors for medicine-induced esophagitis are often linked with issues that prevent quick and complete passage of a pill into your stomach. These factors include:
- Swallowing a pill with little or no water.
- Taking medicines while lying down.
- Taking medicines right before sleep. This risk factor likely is due in part to less saliva being made and less swallowing happening during sleep.
- Being older in age. This may be a factor because of age-related changes to the muscles of the esophagus or to glands making less saliva.
- Taking large or oddly shaped pills.
Infectious esophagitis
Risk factors for infectious esophagitis often relate to medicines such as steroids or antibiotics. People with diabetes also have a higher risk of esophagitis caused by a fungal candida infection in particular.
Other causes of infectious esophagitis may relate to poor immune system function. This may be due to an immune system condition, such as HIV/AIDS, or certain cancers. Also, certain cancer treatments may raise the risk of infectious esophagitis. So might medicines called immunosuppressants that block immune system reactions to transplanted organs.
Esophagitis symptoms
The infection or irritation may cause the food pipe to become inflamed. Sores called ulcers may form.
Common symptoms of esophagitis include:
- Cough
- Stomach acid that backs up into the esophagus, also called acid reflux.
- Difficulty swallowing
- Painful swallowing
- Swallowed food becoming stuck in the esophagus, also known as food impaction.
- Heartburn (acid reflux). It’s common to feel heartburn behind the breastbone while eating.
- Hoarseness
- Sore throat.
Babies and some children with esophagitis are too young to explain their discomfort or pain. Their symptoms can include:
- Feeding troubles, such as getting easily upset, arching of the back and not wanting to eat.
- Failure to thrive.
- Chest or belly pain in older children.
Esophagitis complications
If not treated, esophagitis may cause severe discomfort. Scarring (stricture) of the food pipe may develop. This can cause swallowing problems.
A condition called Barrett esophagus can develop after years of gastroesophageal reflux (GERD). Rarely, Barrett esophagus may lead to cancer of the food pipe.
Without treatment, esophagitis can lead to complications that include:
- Scarring or narrowing of the esophagus, known as a stricture.
- Tearing of the lining of the esophagus. This can be due to retching or to healthcare professionals passing medical tools through an inflamed esophagus during endoscopy. Endoscopy is a way for your doctor to check your digestive system.
- A condition called Barrett esophagus in which the cells lining the esophagus are damaged from acid reflux. This raises the risk of cancer that starts in the esophagus, also called esophageal cancer.
Esophagitis diagnosis
Your doctor may perform the following tests:
- Esophagogastroduodenoscopy (EGD) and removing a piece of tissue from the food pipe for examination (biopsy). Endoscopy is a test that’s used to check the digestive system. A healthcare professional guides a long, thin tube equipped with a tiny camera down the throat and into the esophagus. This tool is called an endoscope. Your healthcare professional can use an endoscope to see if the esophagus looks different than usual. Small tissue samples may be taken for testing. This is called a biopsy. The esophagus may look different depending on the cause of the swelling, such as medicine-induced or reflux esophagitis. Before this test, you receive medicine that helps you relax.
- Esophageal capsule. Esophageal capsule test can be done in your doctor’s office. It involves swallowing a capsule attached to a string. The capsule dissolves in the stomach and releases a sponge. Your doctor pulls the sponge out of your mouth with the string. As the sponge is pulled out, it samples the tissues of the esophagus. This may help your doctor figure out how inflamed your esophagus is without doing an endoscopy.
- Upper GI series (barium swallow x-ray). Barium X-ray involves drinking a solution or taking a pill that contains a compound called barium. Barium coats the lining of the esophagus and the stomach so that they show up on images taken. The images can help healthcare professionals find narrowing of the esophagus and other changes in structure. The images also can help spot a hiatal hernia, tumors or other conditions that may be causing symptoms.
- Esophageal manometry
- Biopsy. Small tissue samples removed during an endoscopic exam are sent to the lab for testing. Depending on the suspected cause of the condition, tests may be used to:
- Diagnose an infection caused by a bacterium, a virus or a fungus.
- Find out if allergy-related white blood cells called eosinophils have built up in the esophagus.
- Spot cells that aren’t regular. Such cells may be clues of esophageal cancer or changes that raise the risk of cancer.
Esophagitis treatment
Treatment depends on the cause. Treatments for esophagitis are intended to lessen symptoms, manage complications and treat the causes of the condition.
Common treatment options for esophagitis are:
- Medicines that reduce stomach acid in case of reflux disease
- Antibiotics to treat infections
- Medicines and diet changes to treat eosinophilic esophagitis
- Medicines to coat the lining of the food pipe to treat damage related to pills.
Esophagitis home remedies
Depending on the type of esophagitis you have, you may lessen symptoms or stop recurring problems by following these steps:
- Do not eat foods that may make reflux worse. Consuming large amounts of certain foods or drinks may make symptoms of acid reflux worse. These can include alcohol, drinks with caffeine, chocolate and mint-flavored foods.
- Use proper pill-taking habits. Take a pill with plenty of water and before eating a meal. Don’t lie down for at least 30 minutes after taking a pill.
- Lose extra weight. Talk with your doctor or dietitian about a diet and exercise routine to help you lose weight and stay at a healthy weight.
- If you smoke, quit. You can ask your doctor to help you end a smoking habit.
- Try not to stoop or bend, especially soon after eating.
- Do not lie down after eating. Wait at least three hours after eating to lie down or go to bed.
- Raise the head of your bed. Place wooden blocks under your bed to raise the head. Aim to raise it 6 to 8 inches (15 to 20 centimeters). If it’s not possible to elevate your bed, place a wedge between your mattress and box spring. This raises your body from the waist up. Raising your head by using only pillows doesn’t work.
Reflux esophagitis treatment
Treatment for reflux esophagitis may include:
- Medicines available without a prescription. These include antacids (Maalox, Mylanta, others); medicines called H-2-receptor blockers that lower stomach acid, such as cimetidine (Tagamet HB); and medicines called proton pump inhibitors that block stomach acid and heal the esophagus, such as lansoprazole (Prevacid 24 HR) and omeprazole (Prilosec OTC), among others.
- Prescription medicines. These include prescription-strength H-2-receptor blockers and proton pump inhibitors.
- Surgery. A type of surgery called fundoplication may improve the condition of the esophagus if other treatments don’t work. The surgeon wraps a portion of the stomach around the lower esophageal sphincter that separates the esophagus and stomach. This surgery can strengthen the sphincter and prevent acid from backing up into the esophagus.
Eosinophilic esophagitis treatment
Treatment for eosinophilic esophagitis involves staying away from the allergen that trigger symptoms. Treatment also involves easing the allergic reaction with medicines. Medicines may include:
- Proton pump inhibitors. Your doctor likely will first prescribe a proton pump inhibitor. You might take one such as esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec) or pantoprazole (Protonix).
- Steroids. Some studies show that swallowed steroids may act on the surface tissue of the esophagus to treat eosinophilic esophagitis. One steroid called budesonide (Eohilia) comes in a liquid form. Another steroid called fluticasone is sprayed into the mouth and then swallowed. Your doctor can tell you how to swallow the steroid solution so that it coats your esophagus. Swallowing a steroid solution is much less likely to cause serious side effects compared with taking steroid pills by mouth.
- Elimination and elemental diets. A reaction to a food allergen is likely the cause of eosinophilic esophagitis. So it may help to stop eating the food that seems to cause the allergy. Standard allergy tests can’t tell you for sure if you’re allergic to a certain food. For that reason, your healthcare professional may recommend that you remove common food allergens from your diet. Then you can slowly add foods back into your diet and note when symptoms come back. This is known as an elimination diet. It needs to be done with guidance from your allergy specialist. A more restrictive method is to remove all food from your diet for a time. Your allergy specialist replaces food with an amino acid-based formula. Over time, you slowly get back to eating food. This is called an elemental diet. It also must be done under the watch of a allergy specialist and dietitian.
- Monoclonal antibodies. This type of medicine works to block the action of certain proteins in the body that cause inflammation. A monoclonal antibody called dupilumab (Dupixent) may be a treatment option for people age 12 and older with eosinophilic esophagitis. Dupilumab is given as an injection every week or every two weeks depending on your weight.
Medicine-induced esophagitis treatment
Treatment for medicine-induced esophagitis involves not using the problem medicine when possible. It also involves lowering the risk of this condition with proper pill-taking habits.
Your doctor may recommend:
- Taking a different medicine that is less likely to cause medicine-induced esophagitis.
- Taking a liquid version of a medicine if possible.
- Sitting or standing for at least 30 minutes after taking a pill.
- Drinking an entire glass of water with a pill. But this option isn’t right for everyone. For instance, some people need to drink less fluid because of another condition, such as kidney disease.
Infectious esophagitis treatment
Your doctor may prescribe medicine to treat an infection that causes infectious esophagitis. Medicines can help clear up infections from viruses, bacteria or fungi.
Treating common complications
A doctor called a gastroenterologist who treats digestive conditions may use medical tools to expand the esophagus. This treatment is called esophageal dilation. It tends to be used only if the esophagus becomes very narrow or if food becomes stuck in the esophagus.
During esophageal dilation, your doctor guides small narrow tubes through the esophagus. Versions of these devices may be equipped with:
- A tapered tip that starts with a rounded point that gradually widens.
- A balloon that can be expanded after it’s placed in the esophagus.
Outlook (Prognosis) for Esophagitis
Most of the time, the disorders that cause swelling of the food pipe, respond to treatment.
What is eosinophilic esophagitis?
Eosinophilic esophagitis is a disease characterized by the presence of a large number of a special type of white blood cell, called the eosinophil, that can cause inflammation in the esophagus 4. This inflammation can lead to stiffening or narrowing of the esophagus, which can lead to difficulty swallowing (dysphagia) or food getting stuck in the esophagus. Reflux of stomach acid contents into the esophagus can also cause eosinophils as well as inflammation in the esophagus. In eosinophilic esophagitis, the eosinophils are present even after acid reflux has been treated. Although eosinophils may be found in the rest of the gastrointestinal tract in a healthy person, when present in the esophagus, this usually suggests an abnormal condition. While other illnesses such as gastroesophageal reflux disease (GERD), parasitic diseases or inflammatory bowel disease may cause eosinophils in the esophagus, eosinophilic esophagitis is the most common cause of large numbers of eosinophils in the esophagus.
How common is eosinophilic esophagitis in adults?
While eosinophilic esophagitis was previously thought to be a rare disease, it has recently been recognized as one of the most common causes of difficulty swallowing and food impaction in young adults 4. This has become a global trend with increased cases of eosinophilic esophagitis being reported from five continents. The cause for this rise is likely a combination of increasing occurrences of eosinophilic esophagitis and a growing awareness of the condition among gastroenterologists, allergists and pathologists. It is thought that the disease may be increasing similar to the increases seen in other allergic disorders such as asthma and allergic rhinitis. Estimated occurrences of this condition in adults may be as high as 1-3 per 10,000 people, based on information from patients in Australia and Switzerland. Although some studies suggest that the disease is more common in the Caucasian population, cases have been seen in patients of African American, Asian and Hispanic descent. Eosinophilic esophagitis affects males three times more often than females.
Eosinophilic esophagitis causes
Currently the cause of eosinophilic esophagitis in adults has not been clearly identified. Some studies have suggested an allergic reaction to environmental and food allergens. There may also be a genetic cause that may lead to eosinophilic esophagitis in some patients. A recent study has identified an increase in a gene coding for a protein called eotaxin-3 in patients with eosinophilic esophagitis. Further support that there may be a genetic link is that some adults have a family history of allergic disorders and a family history of eosinophilic esophagitis.
A history of allergic conditions such as allergic rhinitis, asthma, eczema or food allergy has been seen in up to 70% of adults with eosinophilic esophagitis either by history or positive allergy testing. In one recent study, adults with eosinophilic esophagitis treated with dietary elimination improved their eosinophilic esophagitis, but recurrence of eosinophilic esophagitis happened when certain foods were added back to the diet. This suggests that food allergens play a role in some adults with eosinophilic esophagitis.
Eosinophilic esophagitis symptoms
The most common presenting symptoms in adults are difficulty swallowing solid food and food impactions in which food gets lodged in the esophagus and is unable to pass into the stomach 4. If patients develop a food impaction, an endoscopy is often needed to help relieve this obstruction. Most adults with symptoms are between the ages of 20 to 40, although there have been cases of adults presenting at much later ages. Other less common symptoms include heartburn and chest pain.
Eosinophilic esophagitis diagnosis
Currently, the only way to diagnose eosinophilic esophagitis is by performing an upper endoscopy with biopsy (taking tiny pieces of tissue) of the esophagus 4. During endoscopy, a thin, flexible tube with a camera, which allows the doctor to see the inside of your esophagus, is inserted into the esophagus while the patient is sedated (sleep caused by medication). Biopsies taken from the lining of the esophagus (mucosa) are later inspected under a microscope by a pathologist for characteristic changes of eosinophilic esophagitis. These changes include large numbers of eosinophils in the superficial portion of the tissue biopsy and signs of inflammation in the tissue. Sometimes scaring or fibrosis can be seen in the deeper portions of the tissue. In eosinophilic esophagitis, the eosinophils are limited to the esophagus and are not present in the stomach or duodenum.
Usually, there are characteristic features that the gastroenterologist can see in the esophagus of patients with eosinophilic esophagitis. These include linear furrows or creases in the esophagus and concentric rings of the superficial layer of the esophagus. Other features, including narrow esophagus, white spots on the esophageal tissue and short, very narrow segments of the esophagus called strictures, may also be seen. While these changes are suggestive of eosinophilic esophagitis, their presence alone does not diagnose the condition. The esophagus can also appear normal in adult patients with eosinophilic esophagitis.
Symptoms of gastroesophageal reflux disease (GERD) such as heartburn or regurgitation can overlap with symptoms of eosinophilic esophagitis. Since gastroesophageal reflux disease is much more common than eosinophilic esophagitis in the adult population and can also be a cause of eosinophils in the esophagus, it is important to distinguish the two. Therefore, if eosinophils are found on a tissue biopsy of the esophagus, it is suggested that the patient start treatment with acid reducers to see if the eosinophils go away once the reflux is treated. This requires another endoscopy. If the eosinophils are still in the tissue after reflux has been treated, then the patient most likely has eosinophilic esophagitis. Another method to identify if acid in the esophagus is contributing to the eosinophils is to complete a test called an esophageal pH test. In this test, a very thin tube is placed through the nose into the esophagus and stomach, or a temporary sensor is placed in the esophagus via endoscopy. Both allow levels of acid in the esophagus to be monitored for a period of time, usually 24 – 72 hours. If this test shows high levels of acid in the esophagus, it suggests that GERD may be the cause of the eosinophils in the esophagus. In more complicated situations, some patients have both GERD and eosinophilic esophagitis and therefore will need to have treatment for both conditions.
Eosinophilic esophagitis treatment
Currently, there is no one accepted therapy for all patients with eosinophilic esophagitis. Although dietary therapy is the most common treatment of pediatric eosinophilic esophagitis, this has not been widely accepted among gastroenterologists who treat adult patients. Many adult patients are initially treated with acid-blocking medications to rule out GERD. If this does not improve symptoms or tissue changes of the eosinophils, then steroids taken using an asthma inhaler, but swallowed rather than inhaled by the patient, have been tried with good, although limited results. This treatment tends to be well tolerated; side-effects of a fungal infection called thrush or candida of the esophagus are relatively rare.
Dietary treatment may consist of an elemental diet, a “six-food-elimination diet” or a targeted-elimination diet, usually for six weeks. After this point, if the disease improves, foods are reintroduced one at a time to help identify the food trigger. An elemental diet is another potential treatment. It is an amino-acid based formula, taken usually for six weeks. Elemental diet involve removing intact protein from the diet and replacing that with an amino acid–based formula 5. Elemental formula can have a poor taste and can be costly; therefore, a six-food-elimination diet is preferred by most patients.
A six-food-elimination diet is a diet that contains no milk protein, soy, egg, wheat, peanut/tree nuts, and seafood 6. These foods are the most common food allergens found in patients with eosinophilic esophagitis.
A targeted-elimination diet is a diet that is based on eliminating foods found to be positive on allergy testing.
Dietary therapy has been shown to be helpful in some adults with eosinophilic esophagitis and may be tried with motivated (willing to follow through with food avoidance) patients under the care of an experienced provider or dietician.
If patients do not respond to medical therapy or diet exclusion, an esophageal dilation or “stretching” is sometimes performed if there is narrowing of the esophagus. Although dilation may be helpful in the short term, repeated dilations may be needed to control symptoms. Because dilation alone does not affect the underlying inflammation in the esophagus, this procedure is usually performed in patients who are also being treated with medical or dietary therapy. The risks of esophageal dilation include chest pain after the procedure and in rare cases a perforation or tear of the esophagus. While dilation can be performed safely, it must be done with caution and is almost always performed after a trial of medical or dietary therapy has failed.
Eosinophilic esophagitis prognosis
There is limited information about the natural history of this disease in adults. Current studies suggest that it is a chronic, reoccurring condition. Patients have continued symptoms, although esophageal eosinophil levels may change over time. Complications, including esophageal strictures and food impactions, may occur. In very rare cases, forceful vomiting, prolonged food impactions and esophageal dilations may result in a perforation or tear of the esophagus which needs immediate medical attention. Currently treatment of eosinophilic esophagitis is directed at controlling symptoms, reducing eosinophil levels in the tissue, and preventing complications of the disease, such as food impactions.
What is gastroesophageal reflux disease (GERD)?
Gastroesophageal reflux disease also called GERD, gastro-oesophageal reflux disease (GORD), acid reflux or heartburn, is a condition that develops when there is a backward flow or reflux of stomach contents (acid from the food and liquid in your stomach) back up into your throat and esophagus causing troublesome symptoms and/or complications 7, 8, 9, 10, 11. Gastroesophageal reflux disease can present as non-erosive reflux disease or erosive esophagitis. It can occur at any age, even in babies. Many times, you or your doctor can determine the triggers for your reflux.
The main symptoms of gastroesophageal reflux disease (GERD) are:
- Heartburn – a burning sensation in the middle of your chest, usually after eating, which might be worse after eating, when lying down or when bending over.
- An unpleasant sour taste in your mouth, caused by stomach acid
You may also have:
- Cough or hiccups that keep coming back
- Hoarse voice
- Bad breath
- Bloating and feeling sick
If you have nighttime acid reflux, you might also experience:
- An ongoing cough
- Inflammation of the vocal cords (laryngitis)
- New or worsening asthma
Gastroesophageal reflux disease is caused by a weakened muscle at the end of your esophagus where it connects to your stomach called the lower esophageal sphincter (LES). The lower esophageal sphincter (LES) muscle doesn’t close properly, which allows acid to back up into your throat. Typically, when food is swallowed, the lower esophageal sphincter (a band of muscle around the bottom of the esophagus) relaxes to allow food and liquid to flow down into the stomach. Then the muscle tightens again. If the lower esophageal sphincter isn’t working as it should, stomach acid can flow back up into the esophagus (acid reflux) and cause heartburn. The acid backup may be worse when you’re bent over or lying down.
Sometimes gastroesophageal reflux disease is caused or made worse by:
- certain food and drink – such as coffee, tomatoes, alcohol, chocolate and fatty or spicy foods
- being overweight
- smoking
- pregnancy
- stress and anxiety
- an increase in some types of hormones, such as progesterone and estrogen
- taking certain medicines such as anti-inflammatory painkillers like ibuprofen
- a hiatus hernia – when part of your stomach moves up into your chest
- a stomach ulcer
- a bacterial infection in your stomach
In the United States, 20% of the population experience gastroesophageal reflux disease-related symptoms weekly and 7% daily 12, 13. The prevalence of gastroesophageal reflux disease is slightly higher in men compared to women 14. Several studies have demonstrated that patients with gastroesophageal reflux disease (GERD) have reduced health-related quality of life and work productivity 15.
The danger of untreated gastroesophageal reflux disease (GERD) is that it can cause health problems such as inflammation of the esophagus (esophagitis), which is a risk factor for esophageal cancer. Gastroesophageal reflux disease (GERD) also may lead to breathing problems such as asthma, fluid in the lungs, chest congestion, as well as damaging teeth.
Not everyone who has an episode of acid reflux has gastroesophageal reflux disease (GERD). Your doctor may have you undergo testing to see if you have gastroesophageal reflux disease (GERD). Such tests could include:
- Ambulatory acid (pH) probe test: This test measures the acid in your stomach for 24 hours. Your doctor will insert a small, thin tube into your nose and down into your throat. The tube is connected to a small computer you strap around your waist. Another version of this involves a small probe placed in your throat. The probe transmits a signal for a period of time. After 2 days, the probe falls off and is passed in your stool.
- X-ray of the upper digestive system: The X-ray will look at the inside your upper digestive system (throat, stomach, and upper intestine). For this test, you will you be given a chalky liquid to swallow. This liquid coats your digestive tract to provide better views of the inside.
- Endoscopy or gastroscopy: This is where a thin tube with a camera inside it is passed down your throat and into your stomach. This allows your doctor to look inside your upper digestive tract. He or she may also take a sample of the tissue inside your tract for further testing, for example, tests to check for bacteria that can cause heartburn
- Esophageal motility test (manometry): This test measures the movement and pressure of your esophagus. It involves inserting small, thin tube through your nose and down your throat.
Based on endoscopic and histopathologic appearance, gastroesophageal reflux disease (GERD) is classified into three different types 16:
- Non-erosive reflux disease (NERD). Non-erosive reflux disease (NERD) is a subcategory of gastroesophageal reflux disease (GERD). It is characterized by troublesome reflux symptoms with abnormally increased gastroesophageal reflux observed on 24-hour ambulatory pH-impedance monitoring in the absence of esophageal mucosal injury confirmed on endoscopy.
- Erosive esophagitis. Erosive esophagitis is characterized by erosions or ulcers of the esophageal mucosa 17. Patients may be asymptomatic or can present with worsening symptoms of gastroesophageal reflux disease (GERD). The degree of esophagitis is endoscopically graded using the Los Angeles esophagitis classification system, which employs the A, B, C, D grading system based on variables that include length, location, and circumferential severity of mucosal breaks in the esophagus 18.
- Barrett’s esophagus. Barrett’s esophagus occurs as a result of chronic pathological acid exposure to the distal esophageal mucosa. It leads to a histopathological change of the distal esophageal mucosa, which is normally lined by stratified squamous epithelium to metaplastic columnar epithelium. Barrett’s esophagus is more commonly seen in Caucasian males above 50 years, obesity, and history of smoking and predisposes to the development of esophageal adenocarcinoma 17. Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s esophagus 19.
Non-erosive reflux disease (NERD) is the most prevalent type seen in 60-70% of patients followed by erosive esophagitis and Barrett’s esophagus seen in 30% and 6-12% of patients with gastroesophageal reflux disease (GERD), respectively 16, 15, 20.
If you have acid reflux, your doctor may prescribe a medicine called a proton pump inhibitor (PPI) or H-2 receptor blockers (Histamine-2 Receptor Antagonists) that reduces how much acid your stomach makes. You’ll usually need to take this type of medicine for 4 or 8 weeks, depending on how serious your acid reflux is.
Go back to your doctor if your symptoms return after stopping your medicine. You may need a long-term prescription.
In some cases, surgery may be required to treat acid reflux. This is when medicine doesn’t help, or if you want a long-term solution. Types of surgery may include:
- Nissen fundoplication: This surgery reinforces the lower muscle in the esophagus. A surgeon will wrap the very top of the stomach around the outside of the lower esophagus. This reduces reflux by putting pressure on your esophagus. This is a laparoscopic surgery. This means the surgeon makes three or four small cuts in the abdomen (stomach region). He or she will insert instruments, including a flexible tube with a tiny camera, through the cuts.
- Linx surgery: This surgery strengthens the muscle in the esophagus. The Linx device is a ring of tiny beads made of titanium. The surgery wraps the ring around the area between the stomach and esophagus. The magnetic attraction of the beads keeps the opening between the two closed. This helps keep acid from backing up into your throat. However, it’s weak enough to allow food to pass. The surgery is minimally invasive.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
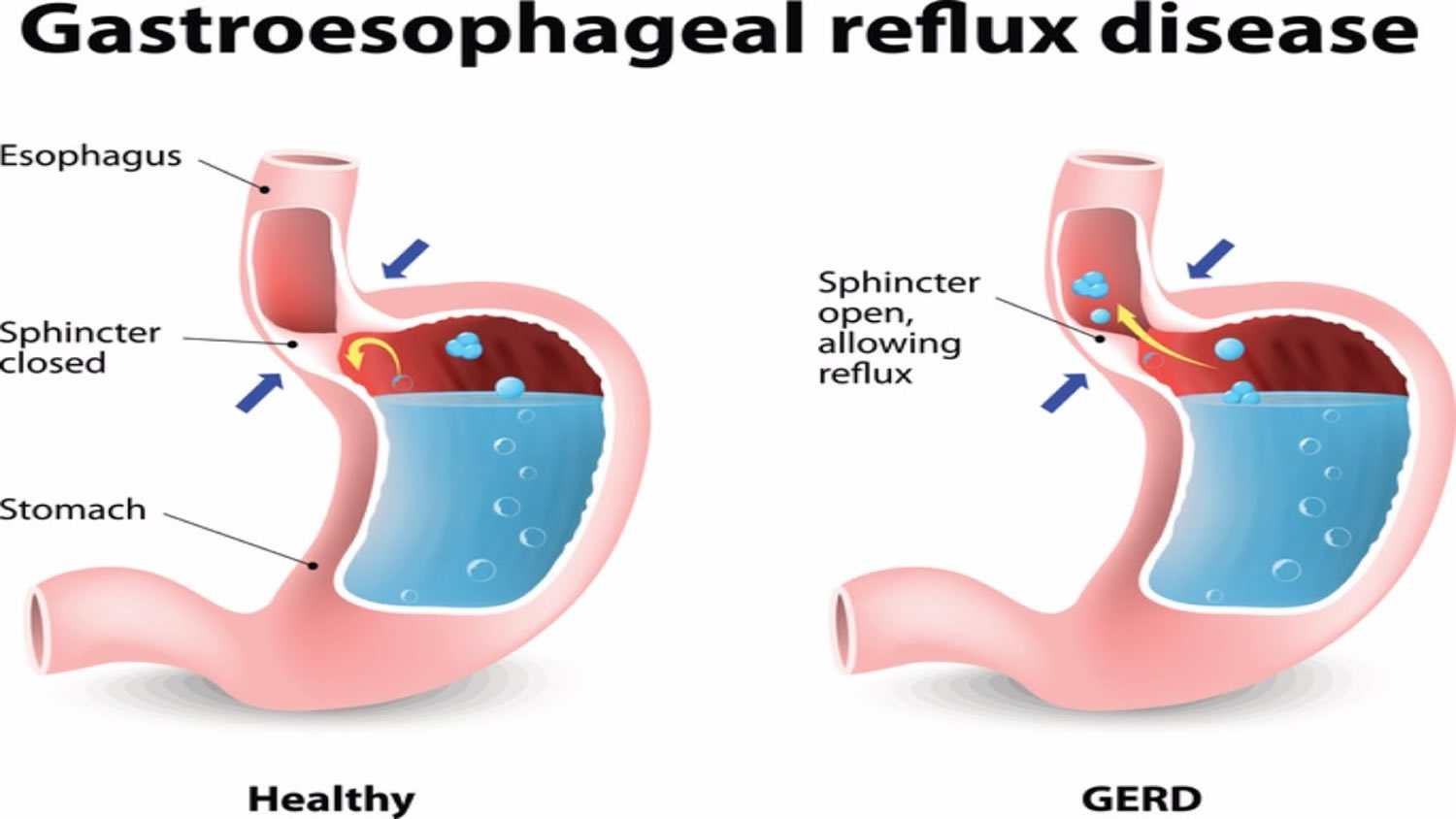
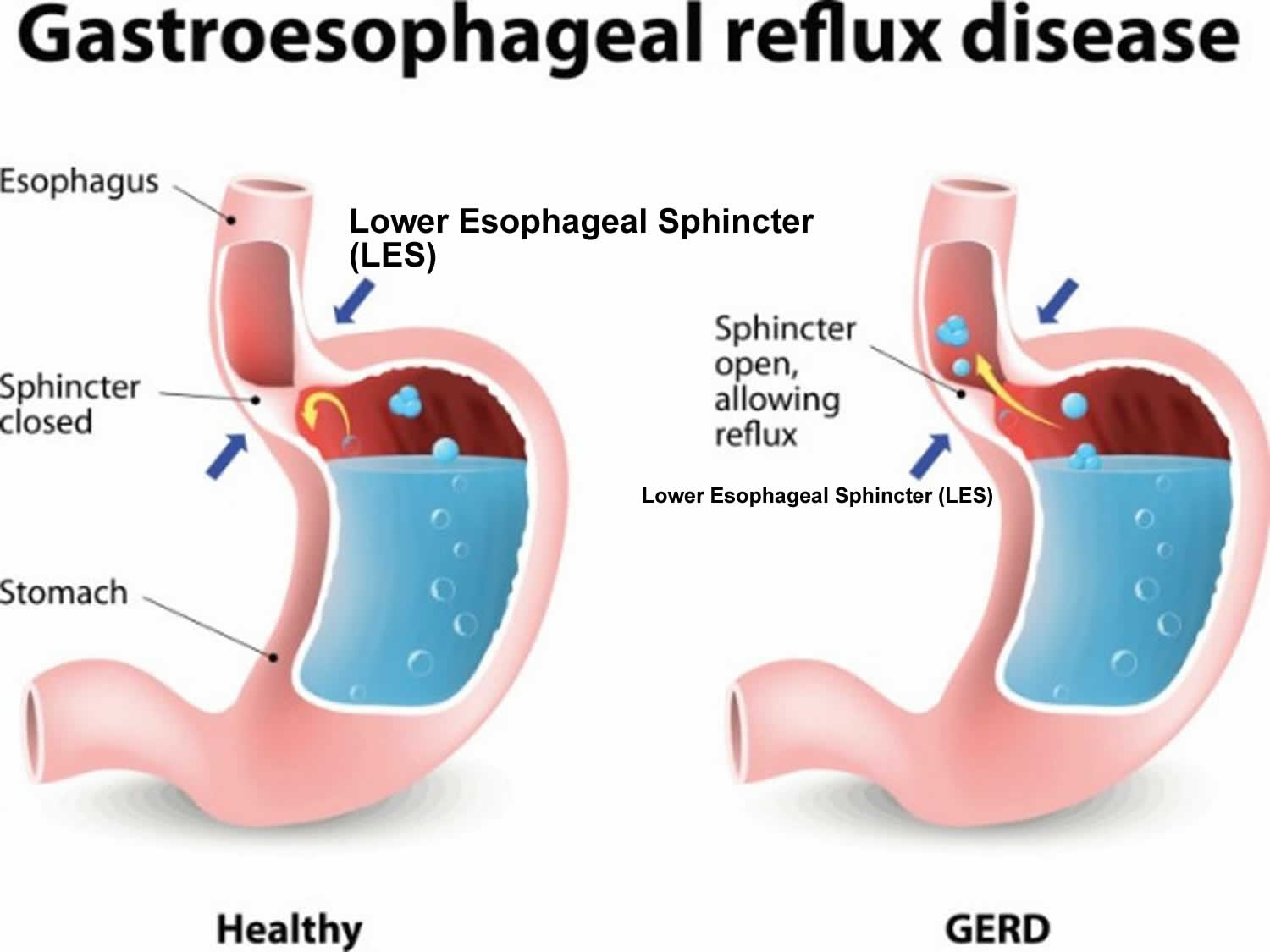
Figure 2. Gastroesophageal reflux disease (GERD)
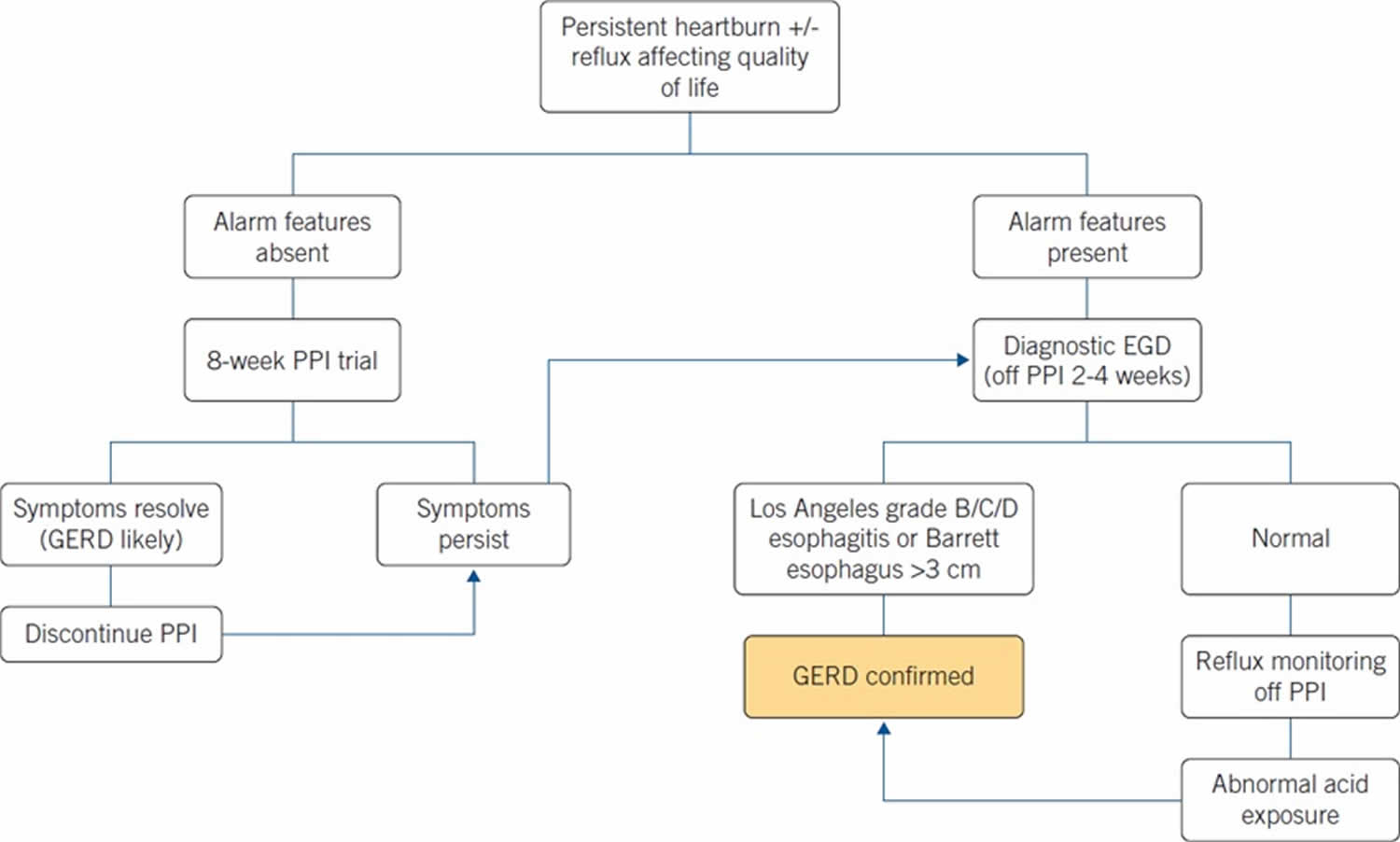
Figure 3. Gastroesophageal reflux disease diagnostic algorithm
[Source 21 ]Chest pain may be a symptom of a heart attack. Seek immediate medical care if you have severe chest pain or pressure, especially when combined with pain in the arm or jaw or difficulty breathing. These may be signs and symptoms of a heart attack.
Make an appointment with your doctor if:
- Heartburn occurs more than twice a week
- Symptoms persist despite use of nonprescription medications
- Take over-the-counter medications for heartburn more than twice a week
- Experience severe or frequent acid reflux symptoms
- You have difficulty swallowing
- You have persistent nausea or vomiting
- You have weight loss because of poor appetite or difficulty eating
Contact your doctor right away if pain is severe or accompanied by:
- If you are 55 or over
- Unintentional weight loss or loss of appetite
- Difficulty swallowing (dysphagia)
- Repeated vomiting or vomiting with blood
- Black, tarry stools
- Trouble swallowing that gets progressively worse
- Fatigue or weakness, which may indicate anemia
Seek immediate medical attention if you have:
- Shortness of breath, sweating or chest pain radiating to the jaw, neck or arm
- Chest pain on exertion or with stress
These symptoms can be a sign of something more serious.
IMPORTANT: Sometimes a heart attack can masquerade as heartburn. Seek medical attention right away if your heartburn is accompanied by sweating, shortness of breath or a tight, clenching feeling in your upper abdominal area.
Do you have GERD ?
Here’s a simple self-test developed by a panel of experts from the American College of Gastroenterology 22.
Take this “Acid Test” to see if you’re a GERD sufferer and are taking the right steps to treat it.
- Do you frequently have one or more of the following:
+ an uncomfortable feeling behind the breastbone that seems to be moving upward from the stomach?
+ a burning sensation in the back of your throat?
+ a bitter acid taste in your mouth? - Do you often experience these problems after meals?
- Do you experience heartburn or acid indigestion two or more times per week?
- Do you find that antacids only provide temporary relief from your symptoms?
- Are you taking prescription medication to treat heartburn, but still having symptoms?
If you said yes to two or more of the above, you may have GERD. To know for sure, see your doctor or a gastrointestinal specialist. They can help you live pain free.
Gastroesophageal reflux disease causes
Currently, there is no known cause to explain the development of gastroesophageal reflux disease 11. Over the years, several risk factors have been identified and implicated in the pathogenesis of gastroesophageal reflux disease 23. Gastroesophageal reflux disease is caused by frequent acid reflux or reflux of nonacidic content from the stomach. When you swallow, a circular band of muscle around the bottom of your esophagus called the lower esophageal sphincter relaxes to allow food and liquid to flow into your stomach. Then the sphincter closes again. If the lower esophageal sphincter does not relax as it should or it weakens, stomach acid can flow back into your esophagus. This constant backwash of acid irritates the lining of your esophagus, often causing it to become inflamed.
A meta-analysis by Hampel H et al. 24 concluded that obesity was associated with an increased risk of developing gastroesophageal reflux disease (GERD) symptoms, erosive esophagitis, and esophageal cancer. The study by Malfertheiner et al. 25 evaluated the predictive factors for erosive reflux disease in more than 6000 patients with GERD and noted that the odds ratio for the erosive disease increased with the body mass index (BMI). Several other risk factors have been independently associated with the development of GERD symptoms that include age ≥50 years, low socioeconomic status, tobacco use, consumption of excess alcohol, connective tissue disorders, pregnancy, postprandial supination, and different classes of drugs which include anticholinergic drugs, benzodiazepines, NSAID or aspirin use, nitroglycerin, albuterol, calcium channel blockers, antidepressants, and glucagon 26, 27, 10.
Risk factors for gastroesophageal reflux disease
The following factors can lead to the onset of gastroesophageal reflux disease or aggravate acid reflux:
- Certain diseases, such as Zollinger-Ellison syndrome or scleroderma.
- Increased abdominal pressure due to obesity or pregnancy.
- Increased production of gastrin, a hormone that regulates the release of stomach acid.
- Hiatal hernia, a condition where the upper part of the stomach moves up into the chest through an opening in the diaphragm. This condition lowers the pressure in the esophageal sphincter.
- Certain medications, including asthma medicine, calcium channel blockers, antihistamines, painkillers, sedatives, and antidepressants.
- Certain foods and beverages, such as fried, spicy, or fatty foods, chocolate, peppermint, coffee, or alcoholic beverages.
- Smoking or inhaling second-hand smoke.
- Delayed stomach emptying.
Factors that can aggravate acid reflux include:
- Smoking
- Eating large meals or eating late at night
- Eating certain foods (triggers) such as fatty or fried foods
- Drinking certain beverages, such as alcohol or coffee
- Taking certain medications, such as aspirin, ibuprofen and naproxen.
Gastroesophageal reflux disease prevention
There are ways to prevent gastroesophageal reflux disease and acid reflux. To start, you need to know your body and how it reacts to different food and drinks. Spicy and acidic foods and carbonated drinks can trigger acid reflux. Try to avoid those things when possible. Eat smaller meals throughout the day, and don’t eat too late at night. Don’t lie down too soon after eating. Limit the use of alcohol. If you use tobacco, try to quit. Stress and lack of sleep also can worsen symptoms.
There are many dietary and lifestyle changes you can make to reduce or eliminate acid reflux, including:
- Not drinking alcohol
- Not smoking
- Avoid these foods and drinks that are commonly known to be heartburn triggers
- Fried foods
- Fast foods
- Pizzas
- Potato chips and other processed snacks
- Chili powder and pepper (white, black, cayenne)
- Fatty meats such as bacon and sausage
- Cheese
- Alcohol
- Carbonated beverages
- Caffeine
- Acidic foods
- Peppermints
- Not eating too close to bedtime
- Losing weight
- Not wearing tight clothing
- Eating smaller meals or avoiding overeating
Foods that help prevent acid reflux
Ginger is one of the best digestive aids because of its medicinal properties. Ginger is alkaline in nature and anti-inflammatory, which eases irritation in the digestive tract. Try sipping ginger tea when you feel heartburn coming on.
High-fiber foods
Fibrous foods make you feel full so you’re less likely to overeat, which may contribute to heartburn. So, load up on healthy fiber from these foods:
- Whole grains such as oatmeal, couscous and brown rice.
- Root vegetables such as sweet potatoes, carrots and beets.
- Green vegetables such as asparagus, broccoli and green beans.
Alkaline foods
Foods that have a low pH are acidic and more likely to cause reflux. Those with higher pH are alkaline and can help offset strong stomach acid. Alkaline foods include:
- Bananas
- Melons
- Cauliflower
- Fennel
- Nuts
Watery foods
Eating foods that contain a lot of water can dilute and weaken stomach acid. Choose foods such as:
- Celery
- Cucumber
- Lettuce
- Watermelon
- Broth-based soups
- Herbal tea
Gastroesophageal reflux disease symptoms
The main symptom of gastroesophageal reflux disease (GERD) is heartburn, often described as a burning feeling in the back of your throat, in the middle of your chest, or behind the sternum (breastbone), and regurgitating sour or bitter liquid to the throat or mouth 11, 17. The combination of heartburn and regurgitation is such a common characteristic of gastroesophageal reflux disease (GERD) that formal testing may be unnecessary 28.
Other symptoms of gastroesophageal reflux disease include 29, 30, 31:
- An acid taste in your mouth.
- A dry cough, asthma, and difficulty swallowing (these may occur without the burning sensation)
- Excessive saliva and a sore throat that doesn’t go away
You may also have:
- Non-burning chest pain, which is usually located in the middle of the chest and radiates to the back
- Difficulty swallowing (dysphagia)
- Atypical reflux symptoms relating to the throat, larynx or lungs:
- Sore throat
- Coughing or hiccups that keep coming back
- Increased salivation
- Shortness of breath
- A hoarse voice
- Bad breath
- Bloating and feeling sick
Symptoms are often worse after eating, when lying down or when bending over.
Gastroesophageal reflux disease complications
Gastroesophageal reflux disease can sometimes lead to the following complications:
- Swelling of the vocal cords, also known as reflux laryngitis
- Inflammation of the tissue in the esophagus (esophagitis). Stomach acid can break down tissue in the esophagus, causing inflammation, bleeding, and sometimes an open sore (ulcer). Esophagitis can cause pain and make swallowing difficult.
- Narrowing of the esophagus (esophageal stricture), caused by scar tissues that develop due to repeated ulcerations. Damage to the lower esophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing. American College of Gastroenterology guidelines recommend esophageal dilation and continue proton pump inhibitor (PPI) therapy to prevent the need for repeated dilations 32.
- Barrett’s esophagus, a precancerous changes to the esophagus tissue caused by long-lasting gastroesophageal reflux disease which increases the risk of esophageal cancer. Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s esophagus 19.
- Lung damage which may include pulmonary fibrosis and bronchiectasis
- Worsening of asthma
- Bronchospasm (irritation and spasm of the airways due to acid)
- Chronic cough or hoarseness
- Dental problems
- Ulcers in the esophagus, caused by burning from stomach acid.
Peptic Stricture
This results from chronic acid injury and scarring of the lower esophagus. Patients complain of food sticking in the lower esophagus. Heartburn symptoms may actually lessen as the esophageal opening narrows down preventing acid reflux. Stretching of the esophagus and proton pump inhibitor medication are needed to control and prevent peptic strictures.
Barrett’s Esophagus
A serious complication of chronic GERD is Barrett’s esophagus. Here the lining of the esophagus changes to resemble the intestine. Patients may complain of less heartburn with Barrett’s esophagus — that’s the good news. Unfortunately, this is a pre-cancerous condition: patients with Barrett’s esophagus have approximately a 30-fold increased risk of developing esophageal cancer. These patients should be followed by endoscopy by a trained gastroenterologist familiar with this disease.
Esophageal Cancer
Recent scientific reports have confirmed that if GERD is left untreated for many years, it could lead to this most serious complication — Barrett’s esophagus and esophageal cancer. Frequent heartburn symptoms with a duration of several years cannot simply be dismissed — there can be severe consequences of delaying diagnosis and treatment. This increased risk of chronic, longstanding GERD sufferers to develop cancer demonstrates the true severity of heartburn. In patients with chronic heartburn, an endoscopy will often be recommended to visually monitor the condition of the lining of the esophagus and identify or confirm the absence of any suspicious or pre-malignant lesions, such as Barrett’s esophagus. So, do not ignore your heartburn. If you are having heartburn two or more times a week, it is time to see your physician and in all likelihood a gastrointestinal specialist. In most cases an endoscopy should be performed to evaluate the severity of GERD and identify the possible presence of the pre-malignant condition — Barrett’s esophagus. The preventative strategy is to treat GERD. If it goes untreated and cancer does develop, the survival rate for esophageal cancer, at this time, is dismal.
Study links duration of heartburn to severity of esophageal disease
Esophageal disease may be perceived in many forms, with heartburn being the most common. The severity of heartburn is measured by how long a given episode lasts, how often symptoms occur, and/or their intensity. Since the esophageal lining is sensitive to stomach contents, persistent and prolonged exposure to these contents may cause changes such as inflammation, ulcers, bleeding and scarring with obstruction. A pre-cancerous condition called Barrett’s esophagus may also occur. Barrett’s esophagus causes severe damage to the lining of the esophagus when the body attempts to protect the esophagus from acid by replacing its normal lining with cells that are similar to the intestinal lining.
Research was conducted to determine whether the duration of heartburn symptoms increases the risk of having esophageal complications. The study found that inflammation in the esophagus not only increased with the duration of reflux symptoms, but that Barrett’s esophagus likewise was more frequently diagnosed in these patients. Those patients with reflux symptoms and a history of inflammation in the past were more likely to have Barrett’s esophagus than those without a history of esophageal inflammation.
Study links chronic heartburn to esophageal cancer
Over the past 20 years, the incidence of esophageal cancer, a highly fatal form of cancer, has rapidly increased in the United States. A recent research study has linked chronic, longstanding, untreated heartburn with an increased risk of developing esophageal cancer. As reported by Lagergren et al. in the study that was published in the New England Journal of Medicine, patients who experienced chronic, unresolved heartburn markedly increase the risk of esophageal cancer, a rare but often deadly malignancy. According to the study, the incidence of adenocarcinoma of the esophagus was nearly eight times more likely among frequent heartburn sufferers (two times a week or more) compared to individuals without symptoms, while among patients with longstanding, severe and unresolved heartburn (e.g. frequent symptoms 20 years duration), the risk of developing esophageal cancer was 43.5 times as great as for those without chronic heartburn.
Persistent symptoms of heartburn and reflux should not be ignored. By seeing your doctor early, the physical cause of GERD can be treated and more serious problems avoided.
Gastroesophageal reflux disease diagnosis
A diagnosis of gastroesophageal reflux disease (GERD) starts with a thorough medical history during which you describe your signs and symptoms and physical examination. If the typical symptoms of acid reflux disease are present, including heartburn and regurgitation, your doctor may begin treatment without performing specific diagnostic tests.
However, tests may be performed if:
- Your symptoms are atypical
- The severity of acid reflux raises concerns about esophageal damage
- Symptoms do not respond to initial treatment
- Your doctor is considering anti-reflux surgery
To confirm a diagnosis of gastroesophageal reflux disease (GERD) or to check for complications, your doctor might recommend:
- Upper endoscopy or gastroscopy. Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat. The endoscope helps your provider see inside your esophagus and stomach. Test results may not show problems when reflux is present, but an endoscopy may detect inflammation of the esophagus (esophagitis) or other complications. An endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications such as Barrett esophagus. In some instances, if a narrowing is seen in the esophagus, it can be stretched or dilated during this procedure. This is done to improve trouble swallowing (dysphagia).
- Transnasal esophagoscopy. This test is done to look for any damage in your esophagus. A thin, flexible tube with a video camera is put through your nose and moved down your throat into the esophagus. The camera sends pictures to a video screen.
- Reflux testing (wireless pH/pH impedance). Ambulatory acid (pH) probe is placed in your esophagus to identify when, and for how long, stomach acid regurgitates there. The monitor connects to a small computer that you wear around your waist or with a strap over your shoulder. The monitor might be a thin, flexible tube (catheter) that’s threaded through your nose into your esophagus. Or it might be a clip that’s placed in your esophagus during an endoscopy. The clip passes into your stool after about two days.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- Your doctor performs an endoscopy and places a small chip in your lower esophagus
- The chip records the acid level in your esophagus for 48 hours.
- The chip transmits your acid level to a wireless recording device that you wear around your belt.
- The data from the recording device can gauge your reflux severity.
- 24-Hour pH Impedance. Your doctor may order this procedure to evaluate your reflux. This procedure monitors your pH level (level of acidity) for a prolonged period. During pH impedance:
- Your doctor places a thin, flexible catheter with an acid-sensitive tip through your nose into your esophagus. The catheter is placed in separate recording spots to evaluate the flow of liquid from your stomach into your esophagus.
- The catheter stays in your nose for a period of 24 hours.
- Your doctor is able to evaluate whether you have GERD, the severity of your reflux, the presence of non-acid reflux and the correlation between your reflux and symptoms. This procedure helps in the design of a course of treatment for you.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- X-ray of the upper digestive system. X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus and stomach. This is particularly useful for people who are having trouble swallowing. You may also be asked to swallow a barium pill that can help diagnose a narrowing of the esophagus that may interfere with swallowing.
- Esophageal manometry also known as esophageal motility (movement) studies. This test measures the rhythmic muscle contractions in your esophagus when you swallow. Esophageal manometry also measures the coordination and force exerted by the muscles of your esophagus. This is typically done in people who have trouble swallowing. An esophageal manometry is an essential part of the assessment process prior to anti-reflux surgery.
- During an esophageal manometry your doctor places a pressure-sensitive catheter into the esophagus. This may be performed right before esophageal pH impedance studies, as it determines where your doctor should place the catheter. The catheter evaluates the strength and coordination of your muscle contractions. It also tests the strength and relaxation function of the lower esophageal sphincter.
- Barium esophagram also called barium swallow, is an imaging test that checks for problems in your upper gastrointestinal tract. Your upper gastrointestinal tract includes your mouth, back of the throat, esophagus, stomach, and first part of your small intestine. The test uses a special type of x-ray called fluoroscopy. Fluoroscopy is a kind of X-ray “movie.” A barium esophagram also evaluates the coordination of your esophageal motor function. While it does not test for the presence of reflux, it is useful for evaluating injury to your esophagus.
- During barium contrast radiography:
- You swallow a contrast solution called barium.
- The barium coats your esophagus and gastrointestinal tract, making it easier for the doctor to detect abnormalities.
- An X-ray is taken.
- During the X-ray, your doctor looks for a narrowing in the esophagus called a stricture.
- During barium contrast radiography:
Gastroesophageal reflux disease differential diagnosis
Gastroesophageal reflux disease (GERD) differential diagnoses may include 33:
- Chest Pain: Patients with GERD may have chest pain similar to angina or heart pain. Usually, they also have other symptoms like heartburn and acid regurgitation. If your doctor says your chest pain is not coming from the heart, don’t forget the esophagus. On the other hand, if you have chest pain, you should not assume it is your esophagus. All chest pain should be checked by a doctor!
- Asthma: Acid reflux may aggravate asthma. Recent studies suggest that the majority of asthmatics have acid reflux. Clues that GERD may be worsening your asthma include: 1) asthma that appears for the first time during adulthood; 2) asthma that gets worse after meals, lying down or exercise; and 3) asthma that is mainly at night. Treatment of acid reflux may cure asthma in some patients and decrease the need for asthmatic medications in others.
- Ear, Nose and Throat Problems: Acid reflux may be a cause of chronic cough, sore throat, laryngitis with hoarseness, frequent throat clearing, or growths on the vocal cords. If these problems do not get better with standard treatments, think about GERD.
- Achalasia
- Acute gastritis
- Antral web cholelithiasis
- Chronic gastritis
- Coronary artery disease
- Esophageal cancer
- Esophageal motility disorders
- Esophageal spasm
- Esophagitis
- Gallstones (cholelithiasis)
- Helicobacter Pylori infection
- Hiatal hernia
- Intestinal malrotation
- Intestinal motility disorders
- Irritable Bowel Syndrome (IBS)
- Peptic Ulcer disease.
Gastroesophageal reflux disease treatments
If your symptoms are mild, treatment may not be necessary. Your doctor is likely to recommend that you first try lifestyle changes and nonprescription medications. If you don’t experience relief within a few weeks, your doctor might recommend prescription medication and additional testing.
Over-the-counter medicine is effective for treating mild cases of acid reflux. These medicines include:
- Antacids: This is a quick-acting medicine that reduces stomach acid. Unfortunately, antacids alone won’t heal the damage stomach acid causes in your esophagus. Sometimes, overusing antacids can cause diarrhea or constipation.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists): These medicines reduce acid production. They don’t work as quickly as antacids. However, they provide longer relief (up to 12 hours). Stronger versions of these medications are available by prescription from your doctor.
- Proton pump inhibitors (PPIs): These medicines block acid production and heal the damage in your throat. They are stronger than H2-receptor blockers.
If these medicines are not providing relief after a few weeks, contact your doctor. Your doctor may give you a prescription version of H2 receptor blockers or proton pump inhibitors. Additionally, your doctor may prescribe medicine to strengthen the lower esophageal sphincter. The medicine may decrease the number of times your muscle relaxes. It is often used for severe reflux. Side effects include fatigue or confusion. Another medicine your doctor may prescribe helps your stomach empty faster. This will cause the food to move along the digestive tract and not back up into your throat. Your doctor may combine more than one medicine, depending upon the severity of your reflux.
In some cases, surgery may be required to treat acid reflux. This is when medicine doesn’t help, or if you want a long-term solution. Types of surgery may include:
- Nissen fundoplication: This surgery reinforces the lower muscle in the esophagus. A surgeon will wrap the very top of the stomach around the outside of the lower esophagus. This reduces reflux by putting pressure on your esophagus. This is a laparoscopic surgery. This means the surgeon makes three or four small cuts in the abdomen (stomach region). He or she will insert instruments, including a flexible tube with a tiny camera, through the cuts.
- Linx surgery: This surgery strengthens the muscle in the esophagus. The Linx device is a ring of tiny beads made of titanium. The surgery wraps the ring around the area between the stomach and esophagus. The magnetic attraction of the beads keeps the opening between the two closed. This helps keep acid from backing up into your throat. However, it’s weak enough to allow food to pass. The surgery is minimally invasive.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Lifestyle and home remedies for acid reflux
You can ease, stop or reduce heartburn and acid reflux yourself by doing the following:
- Eat smaller, more frequent meals.
- Eat food slowly and chew thoroughly. Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Lose weight if you’re overweight. Excess weight put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your esophagus.
- Try to find ways to relax
- Avoid foods or drinks that trigger your heartburn — such as alcohol, fried or fatty foods, chocolate, and peppermint.
- Don’t eat within 3 or 4 hours before bed. Wait at least three hours after eating before lying down or going to bed.
- Avoid tight-fitting clothing that are tight around your waist or abdomen. Clothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
- Don’t smoke or use tobacco. Smoking decreases the lower esophageal sphincter’s ability to function properly.
- Don’t drink alcohol
- Don’t stop taking any prescribed medicine without speaking to a doctor first
Elevate the head of your bed. You may find that using wood, bricks or books under the feet at the head end of your bed to raise the head of your bed by around 10 to 20 cm, so your chest and head are above your waist, helps relieve symptoms. This can help stop stomach acid traveling up towards your throat. If you can’t elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows isn’t effective as this can increase pressure on your abdomen and make your symptoms worse. When you go to bed, start by lying on your left side to help make it less likely that you will have reflux.
Alternative medicine
Some complementary and alternative therapies, such as ginger, chamomile and slippery elm, may be recommended to treat gastroesophageal reflux disease. However, none have been proved to treat gastroesophageal reflux disease or reverse damage to the esophagus. Talk to your doctor if you’re considering taking alternative therapies to treat GERD.
Nonprescription medications
If necessary, occasional acid reflux can be treated with nonprescription medication, options include:
- Antacids that neutralize stomach. Antacids containing calcium carbonate such as Mylanta, Rolaids and Tums, may provide quick relief. But antacids alone won’t heal an inflamed esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or sometimes kidney problems.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists) to reduce acid production, such as cimetidine (Tagamet HB), famotidine (Pepcid AC) or nizatidine (Axid AR). H-2 blockers don’t act as quickly as antacids, but they provide longer relief and may decrease acid production from the stomach for up to 12 hours. Stronger versions are available by prescription.
- Proton pump inhibitors (PPIs) block acid production and heal the esophagus. Proton pump inhibitors are stronger acid blockers than H-2 blockers and allow time for damaged esophageal tissue to heal. Nonprescription proton pump inhibitors include lansoprazole (Prevacid 24 HR), omeprazole (Prilosec OTC) and esomeprazole (Nexium 24 HR).
If you suspect that you have gastroesophageal reflux disease (GERD), your symptoms worsen, or you have nausea, vomiting or difficulty swallowing, talk to your doctor. Prescription medications might help. In a few cases, gastroesophageal reflux disease (GERD) might be treated with surgery or other procedures.
Prescription medications
Prescription-strength treatments for gastroesophageal reflux disease (GERD) include:
- Prescription-strength proton pump inhibitors. Prescription-strength proton pump inhibitors include esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix), rabeprazole (Aciphex) and dexlansoprazole (Dexilant). Although generally well tolerated, prescription-strength proton pump inhibitors might cause diarrhea, headaches, nausea, or in rare instances, low vitamin B-12 or magnesium levels.
- Prescription-strength H-2 blockers. Prescription-strength H-2 blockers include prescription-strength famotidine and nizatidine. Side effects from these medications are generally mild and well tolerated.
Multiple studies have demonstrated that proton-pump inhibitors (PPIs) provide superior therapeutic efficacy in the management of GERD than other antireflux medications such as H-2 receptor antagonists 34. Overall, proton-pump inhibitors (PPIs) demonstrate an unsurpassed rates of symptomatic relief and healing of esophageal inflammation as well as significant improvement in health-related quality of life in patients with erosive esophagitis 35, 36.
Table 1. Summary of Effectiveness of Therapies for GERD
| Class of Drugs | How It Works | Eliminate Symptoms | Heal Esophagitis | Manage or Prevent Complications | Maintain Remission |
|---|---|---|---|---|---|
| Antacids | neutralize acid | +1 | 0 | 0 | 0 |
| H2 Blockers Over-the-counter | mildly suppress acid | +1 | 0 | 0 | 0 |
| Promotility | increase LES pressure; move acid from esophagus and stomach | +2 | +1 | 0 | +1 |
| H2 Blockers Prescription | moderately suppress acid | +2 | +2 | +1 | +1 |
| H2 Blockers + Promotility | moderately suppress acid; move acid from esophagus to stomach | +3 | +3 | +1 | +1 |
| High Dose H2 Blockers | moderately suppress acid | +3 | +3 | +2 | +2 |
| Proton Pump Inhibitors | markedly suppress acid | +4 | +4 | +3 | +4 |
| Surgery | improve barrier between stomach and esophagus to prevent acid reflux | +4 | +4 | +3 | +4 |
Footnote: Rating Scale: 0 (no effect) to +4 (nearly 100%)
[Source 37]H2 Receptor Antagonists
Since the mid 1970’s, acid suppression agents, known as H2 receptor antagonists or H2 blockers, have been used to treat GERD. H2 blockers improve the symptoms of heartburn and regurgitation and provide an excellent means of decreasing the flow of stomach acid to aid in the healing process of mild-to-moderate irritation of the esophagus, known as “esophagitis.” Symptoms are eliminated in up to 50% of patients with twice a day prescription dosage of the H2 blockers. Healing of esophagitis may require higher dosing. These agents maintain remission in about 25% of patients.
H2 blockers are generally less expensive than proton pump inhibitors and can provide adequate initial treatment or serve as a maintenance agent in GERD patients with mild symptoms. Current treatment guidelines also recognize the appropriateness and in some cases desirability of using proton pump inhibitors as first-line therapy for some patients, particularly those with more severe symptoms or esophagitis on endoscopy. Proton pump inhibitors will be required to achieve effective long-term maintenance therapy in a significant percentage of heartburn/GERD patients.
Proton Pump lnhibitors
Proton pump inhibitors (PPIs), have been found to heal erosive esophagitis (a serious form of GERD) more rapidly than H2 blockers. Proton pump inhibitors provide not only symptom relief, but also elimination of symptoms in most cases, even in those with esophageal ulcers. Studies have shown proton pump inhibitor therapy can provide complete endoscopic mucosal healing of esophagitis at 6 to 8 weeks in 75% to 100% of cases. Although healing of the esophagus may occur in 6 to 8 weeks, it should not be misunderstood that gastroesophageal reflux can be cured in that amount of time. The goal of therapy for GERD is to keep symptoms comfortably under control and prevent complications. As noted above, current guidelines recognize that heartburn and GERD are typically relapsing, potentially chronic conditions, that symptoms and mucosal injury will often reoccur when medications are withdrawn, and hence that a strategy for long-term maintenance therapy is generally required. Occasionally, a health care plan seeks to limit use of proton pump inhibitors to a fixed duration of perhaps 2-3 months and others have even cited FDA’s approval of proton pump inhibitors for up to one year, as if that means that this therapy should be withdrawn after one year. There is no well-established scientific reason that supports withdrawing proton pump inhibitors after one year as these patients will invariably relapse. All gastroenterologists have patients who continue to do very well on proton pump inhibitors after many years’ use without adverse side effects. Efforts by payors to limit access to these medications are generally a cost-saving initiative. Daily proton pump inhibitor treatment provides the best long-term maintenance therapy of esophagitis, particularly in keeping symptoms and the disease in remission for those patients with moderate to severe esophagitis, plus this form of treatment has been shown to retain remission for up to five years.
Promotility Agents
Promotility drugs are effective in the treatment of mild to moderately symptomatic GERD. These drugs increase lower esophageal sphincter pressure, which helps prevent acid reflux, and improves the movement of food from the stomach. They can decrease heartburn symptoms, especially at night, by improving the clearance of acid from the esophagus. Recent developments have greatly limited the availability of one of these agents, i.e. cisapride. Cisapride had been used widely for several years in treating night-time heartburn and was also used by some practitioners in the treatment of GERD symptoms in children. More recently, rare but potentially serious complications have been reported in some patients taking cisapride. These complications seem to be related to usage in patients on contraindicated medications or in patients with contraindicated medical conditions, such as underlying heart disease. In March of 2000, the manufacturer announced that it had reached a decision in consultation with the FDA to discontinue the marketing of the drug. The product will remain available only through a limited-access program. This program has been established for patients who fail other treatment options and who meet clearly defined eligibility criteria.
Surgery and other procedures for GERD
Gastroesophageal reflux disease (GERD) can usually be controlled with medication. But if medications don’t help or you wish to avoid long-term medication use, your doctor might recommend surgical measures to prevent reflux or if complications occur such as bleeding, recurrent stricture, or metaplasia (abnormal transformation of cells lining the esophagus), which is progressive. The surgical technique improves the natural barrier between the stomach and the esophagus that prevents acid reflux from occurring. Consultation with both a gastroenterologist and a surgeon is recommended prior to such a decision.
- Fundoplication. The surgeon wraps the top of your stomach around the lower esophageal sphincter, to tighten the muscle and prevent reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. The wrapping of the top part of the stomach can be complete (Nissen fundoplication) or partial. The most common partial procedure is the Toupet fundoplication. Your surgeon will recommend the type that is best for you.
- LINX device. A ring of tiny magnetic beads is wrapped around the junction of the stomach and esophagus. The magnetic attraction between the beads is strong enough to keep the junction closed to refluxing acid, but weak enough to allow food to pass through. The LINX device can be implanted using minimally invasive surgery. The magnetic beads do not have an effect on airport security or magnetic resonance imaging.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
There are two new endoscopic techniques for treating GERD — suturing and the Stretta radio frequency technique — which have recently been approved by the FDA for use with patients. Because these treatments are so new, doctors do not have any real information concerning their long-term effectiveness. They were approved by the FDA largely based on data showing that they could help reduce GERD for at least six months after treatment. At least in the foreseeable future, until long-term outcomes can be evaluated, most patients and physicians will likely be sticking with the treatment options about which there is a much greater wealth of experience, e.g. medical treatment with proton pump inhibitors and other acid suppression medications, and surgery.
Because obesity can be a risk factor for gastroesophageal reflux disease (GERD), your doctor may suggest weight-loss surgery as an option for treatment. Talk with your doctor to find out if you’re a candidate for weight-loss surgery.
Gastroesophageal reflux disease prognosis
Most people with GERD respond to lifestyle changes and medicines. However, a relapse after cessation of medical therapy is common and indicates the need for long-term maintenance therapy 38. Many people need to continue taking medicines to control their symptoms.
Identifying the subgroup of patients who may develop the most serious complications of GERD and treating them aggressively is important 38. Surgery at an early stage is most likely indicated in these patients 38. After a laparoscopic Nissen fundoplication, symptoms resolve in approximately 92% of patients 38.
The LOTUS trial—a 5-year, exploratory randomized, open, parallel-group trial—demonstrated that with antireflux therapy for GERD, either using drug-induced acid suppression with esomeprazole or laparoscopic antireflux surgery, most patients achieve remission and remain in remission at 5 years 39.
Most cases of gastroesophageal reflux in infants and very young children are benign and respond to conservative nonpharmacologic treatment (developmental disabilities represent an important diagnostic exception); 80% resolve by age 18 months (55% resolve by age 10 months) 38. Some patients require a “step-up” to acid-reducing medications, and only a very small minority require surgery 38. Because symptomatic gastroesophageal reflux after age 18 months likely represents a chronic condition, long-term risks are increased. For patients whose gastroesophageal reflux persists into later childhood, long-term therapy with antisecretory agents is often required 38.
In refractory cases or when complications related to reflux disease are identified (eg, stricture, aspiration, airway disease, Barrett esophagus), surgical treatment (fundoplication) is typically necessary. The prognosis with surgery is considered excellent. The surgical morbidity and mortality is higher in patients who have complex medical problems in addition to gastroesophageal reflux.
- Esophagitis. Medline Plus. https://medlineplus.gov/ency/article/001153.htm[↩]
- What Is Cancer of the Esophagus? https://www.cancer.org/cancer/types/esophagus-cancer/about/what-is-cancer-of-the-esophagus.html[↩]
- Bajwa SA, Toro F, Kasi A. Physiology, Esophagus. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519011[↩][↩]
- Eosinophilic Esophagitis. American College of Gastroenterology. http://patients.gi.org/topics/eosinophilic-esophagitis/[↩][↩][↩][↩]
- Kelly, K.J., Lazenby, A.J., Rowe, P.C. et al. Eosinophilic esophagitis attributed to gastroesophageal reflux: improvement with amino acid-based formula. Gastroenterology. 1995; 109: 1503–1512. https://www.ncbi.nlm.nih.gov/pubmed/7557132[↩]
- Effect of Six-Food Elimination Diet on Clinical and Histologic Outcomes in Eosinophilic Esophagitis. September 2006Volume 4, Issue 9, Pages 1097–1102. http://dx.doi.org/10.1016/j.cgh.2006.05.026. http://www.cghjournal.org/article/S1542-3565(06)00495-2/fulltext[↩]
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x[↩]
- Hungin APS, Molloy-Bland M, Scarpignato C. Revisiting Montreal: new insights into symptoms and their causes, and implications for the future of GERD. Am J Gastroenterol. 2019;114:414–421. doi: 10.1038/s41395-018-0287-1[↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589[↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018 Mar;67(3):430-440. doi: 10.1136/gutjnl-2016-313589[↩][↩]
- Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441938[↩][↩][↩]
- Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997 May;112(5):1448-56. doi: 10.1016/s0016-5085(97)70025-8[↩]
- Nebel OT, Fornes MF, Castell DO. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis. 1976 Nov;21(11):953-6. doi: 10.1007/BF01071906[↩]
- Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Prevalence of gastro-oesophageal reflux symptoms and the influence of age and sex. Scand J Gastroenterol. 2004 Nov;39(11):1040-5. doi: 10.1080/00365520410003498[↩]
- Fass R, Frazier R. The role of dexlansoprazole modified-release in the management of gastroesophageal reflux disease. Therap Adv Gastroenterol. 2017 Feb;10(2):243-251. doi: 10.1177/1756283X16681701[↩][↩]
- Fass R, Ofman JJ. Gastroesophageal reflux disease–should we adopt a new conceptual framework? Am J Gastroenterol. 2002 Aug;97(8):1901-9. doi: 10.1111/j.1572-0241.2002.05912.x[↩][↩]
- Kellerman R, Kintanar T. Gastroesophageal Reflux Disease. Prim Care. 2017 Dec;44(4):561-573. doi: 10.1016/j.pop.2017.07.001[↩][↩][↩]
- Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ, Tytgat GN, Wallin L. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999 Aug;45(2):172-80. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1727604/pdf/v045p00172.pdf[↩]
- Wang KK, Sampliner RE; Practice Parameters Committee of the American College of Gastroenterology. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett’s esophagus. Am J Gastroenterol. 2008 Mar;103(3):788-97. doi: 10.1111/j.1572-0241.2008.01835.x[↩][↩]
- Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007 Feb;41(2):131-7. doi: 10.1097/01.mcg.0000225631.07039.6d[↩]
- Provenza D, Gillette C, Peacock B, Rejeski J. Managing heartburn and reflux in primary care. JAAPA. 2024 Mar 1;37(3):24-29. doi: 10.1097/01.JAA.0001005620.54669.f4[↩]
- American College of Gastroenterology. http://patients.gi.org/topics/acid-reflux/[↩]
- Argyrou A, Legaki E, Koutserimpas C, Gazouli M, Papaconstantinou I, Gkiokas G, Karamanolis G. Risk factors for gastroesophageal reflux disease and analysis of genetic contributors. World J Clin Cases. 2018 Aug 16;6(8):176-182. doi: 10.12998/wjcc.v6.i8.176[↩]
- Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005 Aug 2;143(3):199-211. doi: 10.7326/0003-4819-143-3-200508020-00006[↩]
- Malfertheiner P, Nocon M, Vieth M, Stolte M, Jaspersen D, Koelz HR, Labenz J, Leodolter A, Lind T, Richter K, Willich SN. Evolution of gastro-oesophageal reflux disease over 5 years under routine medical care–the ProGERD study. Aliment Pharmacol Ther. 2012 Jan;35(1):154-64. doi: 10.1111/j.1365-2036.2011.04901.x[↩]
- El-Serag HB, Hashmi A, Garcia J, Richardson P, Alsarraj A, Fitzgerald S, Vela M, Shaib Y, Abraham NS, Velez M, Cole R, Rodriguez MB, Anand B, Graham DY, Kramer JR. Visceral abdominal obesity measured by CT scan is associated with an increased risk of Barrett’s oesophagus: a case-control study. Gut. 2014 Feb;63(2):220-9. doi: 10.1136/gutjnl-2012-304189[↩]
- Mohammed I, Nightingale P, Trudgill NJ. Risk factors for gastro-oesophageal reflux disease symptoms: a community study. Aliment Pharmacol Ther. 2005 Apr 1;21(7):821-7. doi: 10.1111/j.1365-2036.2005.02426.x[↩]
- Gastroesophageal Reflux Disease (GERD). https://www.hopkinsmedicine.org/health/conditions-and-diseases/gastroesophageal-reflux-disease-gerd[↩]
- Sandhu DS, Fass R. Current Trends in the Management of Gastroesophageal Reflux Disease. Gut Liver. 2018 Jan 15;12(1):7-16. doi: 10.5009/gnl16615[↩]
- Hom C, Vaezi MF. Extraesophageal manifestations of gastroesophageal reflux disease. Gastroenterol Clin North Am. 2013 Mar;42(1):71-91. doi: 10.1016/j.gtc.2012.11.004[↩]
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006 Aug;101(8):1900-20; quiz 1943. doi: 10.1111/j.1572-0241.2006.00630.x[↩]
- Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013 Mar;108(3):308-28; quiz 329. doi: 10.1038/ajg.2012.444. Epub 2013 Feb 19. Erratum in: Am J Gastroenterol. 2013 Oct;108(10):1672.[↩]
- Gastroesophageal Reflux Disease Differential Diagnoses. https://emedicine.medscape.com/article/176595-differential[↩]
- Chiba N, De Gara CJ, Wilkinson JM, Hunt RH. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology. 1997 Jun;112(6):1798-810. doi: 10.1053/gast.1997.v112.pm9178669[↩]
- Hershcovici T, Fass R. Pharmacological management of GERD: where does it stand now? Trends Pharmacol Sci. 2011 Apr;32(4):258-64. doi: 10.1016/j.tips.2011.02.007[↩]
- Fass R, Shapiro M, Dekel R, Sewell J. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease–where next? Aliment Pharmacol Ther. 2005 Jul 15;22(2):79-94. doi: 10.1111/j.1365-2036.2005.02531.x[↩]
- Acid Reflux. American College of Gastroenterology. http://patients.gi.org/topics/acid-reflux/[↩]
- Gastroesophageal Reflux Disease. https://emedicine.medscape.com/article/176595-overview#a7[↩][↩][↩][↩][↩][↩][↩]
- Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, Långström G, Lind T, Lundell L; LOTUS Trial Collaborators. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. 2011 May 18;305(19):1969-77. doi: 10.1001/jama.2011.626[↩]