Contents
- What is Prediabetes
- Who is more likely to develop prediabetes?
- What is insulin?
- How does insulin work?
- What is glucose?
- What is normal blood glucose levels?
- What is diabetes blood glucose levels?
- What happens when my blood sugar levels are too high?
- Why are good blood sugar levels important?
- What is HbA1c?
- What is insulin resistance?
- What are the most common symptoms of diabetes?
- What causes prediabetes?
- Risk factors for developing prediabetes
- How do I prevent getting prediabetes?
- Prediabetes signs and symptoms
- Prediabetes complications
- Prediabetes diagnosis
- Prediabetes treatment
- Prediabetes diet
What is Prediabetes
Prediabetes, also called borderline diabetes, means your blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes 1. In people with prediabetes, you can expect to see fasting blood glucose levels elevated between 100 mg/dL to 125 mg/dL (5.5 to 6.9 mmol/L) or 2 hours after eating blood glucose levels between 140 mg/dL to 199 mg/dL (7.8 to 11.0 mmol/L) 2, 3, 4. However, these blood sugar levels do not meet the required criteria for a diagnosis of diabetes mellitus (see below). For this reason, many people with prediabetes are not aware that they are living with prediabetes 5, 6, 7. Doctors sometimes refer to prediabetes as impaired glucose tolerance (IGT) or impaired fasting glucose (IFG), depending on what test was used when it was detected. Prediabetes puts you at a higher risk for developing type 2 diabetes, cardiovascular disease and stroke 4.
NOTE: Fasting means after not having anything to eat or drink (except water) for at least 8 hours before the test. This test is usually done first thing in the morning, before breakfast.
Healthy individuals, normal blood sugar levels are 8, 4:
- Between 70 to 99 mg/dL (4.0 to 5.4 mmol/L) when fasting.
- Up to 140 mg/dL (7.8 mmol/L) 2 hours after eating.
Blood sugar levels in diagnosing diabetes 2, 3:
- 126 mg/dL or higher (7.0 mmol/L or more) when fasting.
- 200 mg/dL or higher (11.1 mmol/L or more) 2 hours after eating.
- Random blood glucose test also called casual plasma glucose test (is a blood sugar check at any time of the day) of greater than or equal to 200 mg/dL (11.1 mmol/L or more).
NOTE: Fasting means after not having anything to eat or drink (except water) for at least 8 hours before the test. This test is usually done first thing in the morning, before breakfast.
Prediabetes usually occurs in people who already have some insulin resistance or whose beta cells in the pancreas aren’t making enough insulin to keep blood glucose in the normal range. Without enough insulin, extra glucose stays in your bloodstream rather than entering your cells. Over time, you could develop type 2 diabetes. Therefore, if you have prediabetes, you should be checked for type 2 diabetes every one to two years. If screening is negative for prediabetes, repeat screening should be carried out every 3 years as per the United States Preventive Services Task Force 4.
People with prediabetes often may show no signs or symptoms of diabetes, but will have blood sugar levels higher than normal, so you may have prediabetes and not know it.
Some people with prediabetes may have some of the symptoms of diabetes or even problems from diabetes already. You usually find out that you have prediabetes when being tested for diabetes.
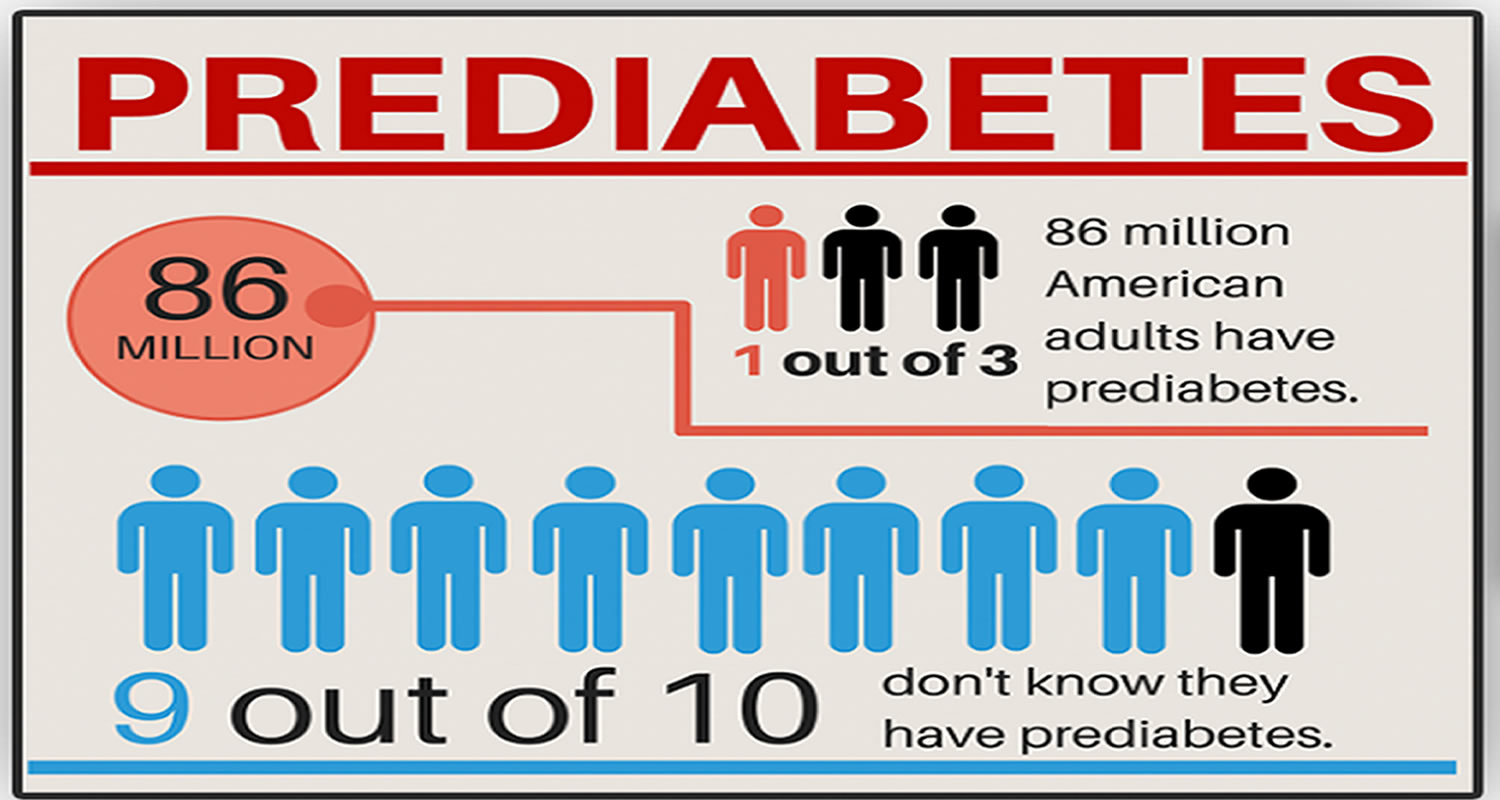
Approximately 96 million American adults (18 and older), that’s more than 1 in 3, have prediabetes 9. Of those with prediabetes, more than 80% don’t know they have it. Prediabetes puts you at increased risk of developing type 2 diabetes, heart disease, and stroke. Without lifestyle changes, a person with prediabetes is at high risk of going on to develop type 2 diabetes. People with prediabetes have up to a 50 percent chance of developing type 2 diabetes over the next 5 to 10 years. So if you’ve been told you have prediabetes, this is a warning sign that you are at high risk of developing type 2 diabetes. The good news is you don’t have it yet, and by making changes to your diet, increasing physical activity and losing weight, up to 70% of cases of type 2 diabetes can be prevented or delayed in some people 4.
If you have prediabetes, losing a small amount of weight if you’re overweight and getting regular physical activity can lower your risk for developing type 2 diabetes. A small amount of weight loss means around 5% to 7% of your body weight or just 10 to 14 pounds for a 200-pound person can significantly reduce your risk. There are lots of ways you can lose weight and it’s about finding what works best for you. If you need help with managing your weight, a dietitian can help you.
Regular physical activity means getting at least 150 minutes a week of brisk walking or a similar activity. That’s just 30 minutes a day, five days a week.
Making healthier food choices and being more active are both positive ways to start making positive changes that will benefit your health.
Some patients will need to take some medications. These patients include those that have failed to maintain adequate lifestyle therapy or are at high-risk for developing type 2 diabetes. The most common medications used for prediabetes are metformin and acarbose, which will help prevent the development of diabetes mellitus. These two drugs have minimal side effects and work well in prediabetic patients.
Figure 1. Prediabetes blood sugar levels
Who is more likely to develop prediabetes?
People who have genetic or lifestyle risk factors are more likely to develop insulin resistance or prediabetes. Risk factors include:
- overweight or obesity
- age 45 or older
- a parent, brother, or sister with diabetes
- African American, Alaska Native, American Indian, Asian American, Hispanic/Latino, Native Hawaiian, or Pacific Islander American ethnicity
- physical inactivity
- health conditions such as high blood pressure and abnormal cholesterol levels
- a history of gestational diabetes
- a history of heart disease or stroke
- polycystic ovary syndrome (PCOS)
People who have metabolic syndrome—a combination of high blood pressure, abnormal cholesterol levels, and large waist size—are more likely to have prediabetes.
Along with these risk factors, other things that may contribute to insulin resistance include:
- certain medicines, such as glucocorticoids, some antipsychotics, and some medicines for HIV
- hormonal disorders, such as Cushing’s syndrome and acromegaly
- sleep problems, especially sleep apnea
Although you can’t change risk factors such as family history, age, or ethnicity, you can change lifestyle risk factors around eating, physical activity, and weight. These lifestyle changes can lower your chances of developing insulin resistance or prediabetes.
What is insulin?
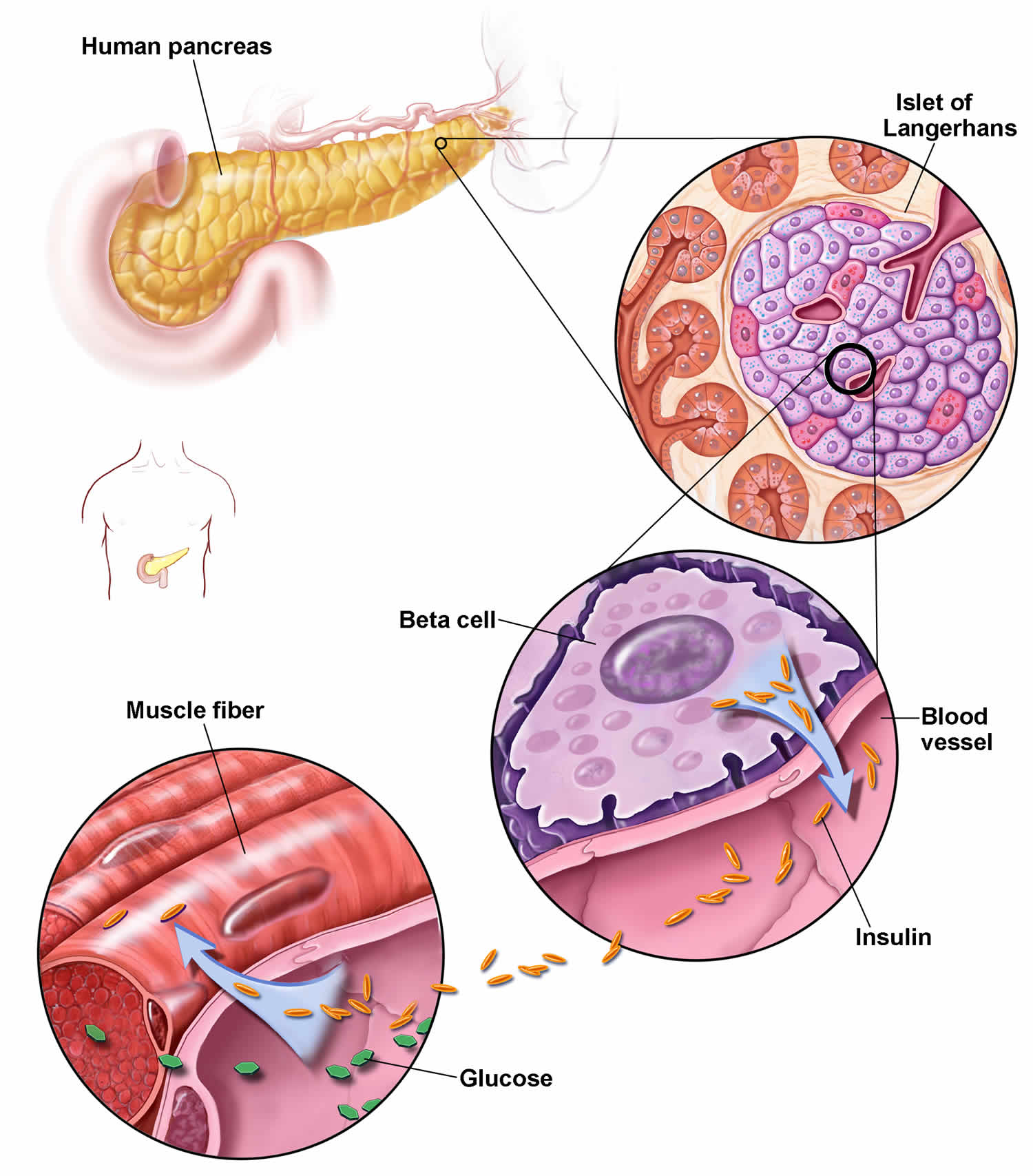
Insulin is a hormone that comes from your pancreas, a gland situated behind and below the stomach. The pancreas secretes insulin into the bloodstream. The insulin circulates, enabling sugar to enter your cells. Insulin lowers the amount of sugar in your bloodstream. As your blood sugar level drops, so does the secretion of insulin from your pancreas.
If your body isn’t able to make enough insulin or if your body’s cells have trouble accepting insulin, your blood glucose level can rise to a dangerous level. This may lead to diabetes, a serious disease that can damage your body’s organs if it is not kept under control.
How does insulin work?
Insulin is a hormone that comes from the gland situated behind and below the stomach (pancreas). Insulin regulates how the body uses sugar in the following ways:
- Sugar in the bloodstream triggers the pancreas to secrete insulin.
- Insulin circulates in the bloodstream, enabling sugar to enter your cells.
- The amount of sugar in your bloodstream drops.
- In response to this drop, the pancreas releases less insulin.
What is glucose?
Glucose is the type of sugar that your body uses as its principal energy source. Glucose comes from two major sources: the food you eat and your liver. Your liver stores glucose as glycogen and makes glucose. The glucose enters your bloodstream and is taken up by your body’s cells with the help of a hormone called insulin.
If your body isn’t able to make enough insulin, or if your body’s cells have trouble accepting insulin, your blood glucose level can rise to a dangerous level. This may lead to diabetes, a serious disease that can damage your body’s organs if it is not kept under control.
When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
What is normal blood glucose levels?
A blood sugar level with blood sample taken at a random time (regardless of when you last ate) less than 140 mg/dL (7.8 mmol/L) is normal.
A fasting blood sugar level (a blood sample taken after an overnight fast) less than 100 mg/dL (5.6 mmol/L) is normal.
What is diabetes blood glucose levels?
A blood sugar level with blood sample taken at a random time (regardless of when you last ate) of 200 milligrams per deciliter (mg/dL) [11.1 millimoles per liter (mmol/L)] or higher suggests diabetes.
A fasting blood sugar level (a blood sample taken after an overnight fast) of 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes.
What happens when my blood sugar levels are too high?
If your blood sugar levels are slightly above your targets, there are usually no symptoms. But if your blood sugar levels become too high, you may experience some symptoms associated with a hyperglycemia (or hyper).
The blood sugar level at which symptoms begin to appear is different for everyone, but the common symptoms include passing more urine than normal, being very thirsty, having headaches and feeling tired and lethargic.
Why are good blood sugar levels important?
It is important that you control your blood glucose levels as well as you can as too high sugar levels for long periods of time increases the risk of diabetes complications developing.
Diabetes complications are health problems which include:
- Kidney disease
- Nerve damage
- Retinal disease
- Heart disease
- Stroke
What is HbA1c?
The HbA1c (hemoglobin A1c) also known as glycated hemoglobin (A1C) or glycohemoglobin measures the percentage of hemoglobin A in your blood that has glucose attached. The HbA1c (glycated hemoglobin A1C) test estimates how much glucose or blood sugar, has been in your bloodstream over the last two to three months. HbA1c is a marker for long-term glucose control and the HbA1c test can identify diabetes or keep track of how well diabetes is being controlled. Since red blood cells live about three months, your hemoglobin A1c test result corresponds to your average blood glucose level throughout the three months before your test.
The hemoglobin A1c (HbA1c) test is NOT used to diagnose gestational diabetes, a form of the disease that can develop during pregnancy.
Glucose has the ability to attach to hemoglobin in the blood and form hemoglobin A1c (HbA1c). Hemoglobin is the protein in red blood cells that carries oxygen. A measurement of hemoglobin A1c (HbA1c) reflects the percentage of hemoglobin A that is attached to glucose compared to the total amount of hemoglobin A in the blood.
The more glucose is in the blood, the more glucose can attach to hemoglobin. If your hemoglobin A1c (HbA1c) percentage is too high, this means that your average blood glucose in the previous months has been too high as well.
If you have diabetes, an ideal HbA1c level is 48mmol/mol (6.5%) or below. If you’re at risk of developing type 2 diabetes, your target HbA1c level should be below 42mmol/mol (6%).
The hemoglobin A1c (HbA1c) test may have several purposes:
- Screening for prediabetes and diabetes: Screening means checking for health conditions before a person experiences symptoms. If you are over 40 and are obese or overweight, or if you are otherwise at a high risk for diabetes, your doctor may want to screen you. The hemoglobin A1c test can be used for diabetes screening, but the results may need to be confirmed by repeating the test or using another type of test.
- Diagnosing prediabetes and diabetes: Diagnosis uses tests and procedures to find out the cause of health changes. Your doctor may order a hemoglobin A1c test for you, among other tests, if you have symptoms or show signs of diabetes. Diabetes symptoms can include excessive thirst, frequent urination, blurred vision, tingling or loss of sensation in the feet and hands, and feeling extremely tired.
- Monitoring diabetes: If you have been diagnosed with diabetes, your doctor may order a hemoglobin A1c test for you at least twice a year. This helps give your doctor an idea of how well your blood glucose has been controlled in the months between your appointments. Keeping track of your blood glucose allows your doctor to make adjustments to your treatment plan and lower your chance of health problems.
Table 1. HbA1c (A1c) test results
| A1c (HbA1c) Level | Indication |
|---|---|
| Less than 5.7% (39 mmol/mol) | Normal |
| 5.7% to 6.4% (39-46 mmol/mol) | Prediabetes |
| 6.5% (47 mmol/mol) or higher | Diabetes |
What is insulin resistance?
Insulin resistance also known as impaired insulin sensitivity, is when the insulin that you produce, or the insulin you inject, doesn’t work properly, making the insulin hormone less effective. Insulin resistance is when cells in your muscles, fat, and liver don’t respond well to insulin and can’t easily take up glucose from your blood. Insulin resistance is identified as an impaired biologic response to insulin stimulation of target tissues, primarily the liver, muscle, and adipose tissue 10. As a result, your pancreas makes more insulin and more insulin is needed to persuade fat and muscle cells to take up glucose and the liver to continue to store it. As long as your pancreas can make enough insulin to overcome your cells’ weak response to insulin, your blood glucose levels will stay in the healthy range.
However, the clinical definition of insulin resistance remains elusive as there is not a generally accepted test for insulin resistance 11. Clinically, insulin resistance is recognized via the metabolic consequences associated with insulin resistance as described in metabolic syndrome and insulin resistance syndrome 10. While insulin resistance is a hallmark of prediabetes and type 2 diabetes it can also affect those with type 1 diabetes.
Scientists are beginning to get a better understanding of how insulin resistance develops. For starters, several genes have been identified that make a person more or less likely to develop insulin resistance. It’s also known that older people are more prone to insulin resistance. Lifestyle can play a role, too. Being sedentary, overweight or obese and having too much fat around your stomach increases your risk for insulin resistance. Why? It’s not clear, but some researchers theorize that extra fat tissue may cause inflammation, physiological stress or other changes in the cells that contribute to insulin resistance. There may even be some undiscovered factor produced by fat tissue, perhaps a hormone, that signals the body to become insulin resistant. Just why a person fails to respond properly to insulin is still a mystery. But there are ways to make the body more receptive to insulin, which can help prevent or delay type 2 diabetes or help someone with type 1 diabetes manage their blood sugar (blood glucose).
In response to the body’s insulin resistance, the pancreas deploys greater amounts of the hormone to keep cells energized and blood glucose levels under control. This is why people with type 2 diabetes tend to have elevated levels of circulating insulin. The ability of the pancreas to increase insulin production means that insulin resistance alone won’t have any symptoms at first. Over time, though, insulin resistance tends to get worse, and the pancreatic beta cells that make insulin can wear out. Eventually, the pancreas no longer produces enough insulin to overcome the cells’ resistance. The result is higher blood sugar levels, and ultimately prediabetes or type 2 diabetes.
Insulin has other roles in the body besides regulating blood sugar levels, and the effects of insulin resistance are thought to go beyond diabetes. For example, some research has shown that insulin resistance, independent of diabetes, is associated with heart disease.
Insulin resistance is more likely to happen as a teenager when hormones are unpredictable and can be completely unrelated to your weight. To reduce your insulin resistance you might need to start oral medications alongside your insulin, making insulin more effective again. Your healthcare team will advise you on the best method to reduce your insulin resistance.
What are the most common symptoms of diabetes?
No individual is the same. The symptoms you experience won’t exactly match those of another person. However, the most common symptoms experienced by many people with diabetes are increased thirst, increased urination , feeling tired and losing weight. These symptoms occur because some or all of the glucose stays in your blood, and isn’t being used as fuel for energy. Your body tries to reduce blood glucose levels by flushing the excess glucose out of your body in your urine, making you more thirsty. High levels of glucose being passed in the urine are a perfect breeding ground for the fungal infection which causes thrush. But not everyone gets symptoms. In fact, 6 out of 10 people have no symptoms when they’re diagnosed with type 2 diabetes.
What causes prediabetes?
The exact cause of prediabetes is unknown. But family history and genetics appear to play an important role. Inactivity and excess fat — especially abdominal fat — also seem to be important factors.
Insulin is a hormone made by your pancreas beta cells that acts like a key to let blood sugar into cells for use as energy. If you have prediabetes, the cells in your body don’t respond normally to insulin (insulin resistance). Your pancreas makes more insulin to try to get cells to respond. Eventually your pancreas can’t keep up, and your blood sugar rises, setting the stage for prediabetes and type 2 diabetes down the road.
Researchers don’t fully understand what causes insulin resistance and prediabetes, but they think excess weight and lack of physical activity are major factors.
Excess weight
Experts believe obesity, especially too much fat in the abdomen and around the organs, called visceral fat, is a main cause of insulin resistance. A waist measurement of 40 inches or more for men and 35 inches or more for women is linked to insulin resistance. This is true even if your body mass index (BMI) falls within the normal range. However, research has shown that Asian Americans may have an increased risk for insulin resistance even without a high BMI.
Researchers used to think that fat tissue was only for energy storage. However, studies have shown that belly fat makes hormones and other substances that can contribute to chronic, or long-lasting, inflammation in the body. Inflammation may play a role in insulin resistance, type 2 diabetes, and cardiovascular disease.
Excess weight may lead to insulin resistance, which in turn may play a part in the development of fatty liver disease.
Physical inactivity
Not getting enough physical activity is linked to insulin resistance and prediabetes. Regular physical activity causes changes in your body that make it better able to keep your blood glucose levels in balance.
Risk factors for developing prediabetes
The same factors that increase the risk of developing type 2 diabetes increase the risk of developing prediabetes.
These factors include:
- Being overweight or obese. Being overweight or obese is a primary risk factor for prediabetes. The more fatty tissue you have — especially inside and between the muscle and skin around your abdomen — the more resistant your cells become to insulin.
- Physically inactive. The less active you are, the greater your risk of prediabetes. Physical activity helps you control your weight, uses up sugar for energy and makes the body use insulin more effectively.
- Poor diet. Eating red meat and processed meat, and drinking sugar-sweetened beverages, is associated with a higher risk of prediabetes. A diet high in fruits, vegetables, nuts, whole grains and olive oil is associated with a lower risk of prediabetes.
- Large waist size. A large waist size can indicate insulin resistance. The risk of insulin resistance goes up for men with waists larger than 40 inches and for women with waists larger than 35 inches.
- Having a close (first degree) relative with diabetes. Your risk of prediabetes increases if you have a parent or sibling with type 2 diabetes.
- Being a woman who delivered a baby weighing more than 9 pounds or with a history of gestational diabetes. If you’ve had gestational diabetes, your doctor will likely check your blood sugar levels at least once every three years.
- Being a woman with polycystic ovary syndrome (PCOS). Women with this common condition — characterized by irregular menstrual periods, excess hair growth and obesity — have a higher risk of prediabetes.
- Being of a high-risk race or ethnicity such as African American, Latino, Native American, Asian American, Pacific Islander
- Having high blood pressure (hypertension) or taking medication for high blood pressure
- Having an A1C equal to or above 5.7% or prediabetes identified by previous testing
- Having a history of cardiovascular disease
- Age. Although diabetes can develop at any age, the risk of prediabetes increases after age 45.
- People with obstructive sleep apnea — a condition that disrupts sleep repeatedly — have an increased risk of insulin resistance.
- Tobacco smoke. Smoking may increase insulin resistance. Smokers also seem to carry more weight around the middle.
Other conditions associated with prediabetes include:
- High blood pressure
- Low levels of high-density lipoprotein (HDL) cholesterol, the “good” cholesterol
- High levels of triglycerides — a type of fat in your blood
When these conditions occur with obesity, they are associated with insulin resistance. The combination of three or more of these conditions is often called metabolic syndrome.
Along with these risk factors, other things that may contribute to insulin resistance include:
- certain medicines, such as glucocorticoids, some antipsychotics, and some medicines for HIV
- hormonal disorders, such as Cushing’s syndrome and acromegaly
- sleep problems, especially sleep apnea
Although you can’t change risk factors such as family history, age, or ethnicity, you can change lifestyle risk factors around eating, physical activity, and weight. These lifestyle changes can lower your chances of developing insulin resistance or prediabetes.
How do I prevent getting prediabetes?
Healthy lifestyle choices can help you prevent prediabetes and its progression to type 2 diabetes, even if diabetes runs in your family. Try to:
- Eat healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains. Strive for variety to prevent boredom.
Get more physical activity. Aim for about 30 minutes of moderate aerobic activity on most days of the week, or at least 150 minutes of moderate aerobic activity a week. - Lose excess pounds. If you’re overweight, losing even 7% of your body weight — for example, 14 pounds (6.4 kilograms) if you weigh 200 pounds (90.7 kilograms) — can reduce the risk of diabetes. Don’t try to lose weight during pregnancy, however. Talk to your doctor about how much weight is healthy for you to gain during pregnancy. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits. Motivate yourself by remembering the benefits of losing weight, such as a healthier heart, more energy and improved self-esteem.
- Get at least 150 minutes of moderate aerobic physical activity a week, or about 30 minutes on most days of the week.
- Control your blood pressure and cholesterol.
- Don’t smoke.
Physical activity and losing weight may help your body respond better to insulin. Taking small steps, such as eating healthier foods and moving more to lose weight, can help reverse insulin resistance and prevent or delay type 2 diabetes in people with prediabetes.
The Diabetes Prevention Program research studies 12, 13, showed that for people at high risk of developing diabetes, losing 5 to 7 percent of their starting weight helped reduce their chance of developing the disease 13. That’s 10 to 14 pounds for someone who weighs 200 pounds. People in the study lost weight by changing their diet and being more physically active.
The Diabetes Prevention Program research studies 12, 13 also showed that taking metformin, a medicine used to treat type 2 diabetes, could delay diabetes. Metformin worked best for women with a history of gestational diabetes, younger adults, and people with obesity. Ask your doctor if metformin might be right for you.
How you can lower your chances of developing type 2 diabetes
Research such as the Diabetes Prevention Program shows that you can do a lot to reduce your chances of developing type 2 diabetes. Here are some things you can change to lower your risk:
- Lose weight and keep it off. You may be able to prevent or delay diabetes by losing 5 to 7 percent of your starting weight.1 For instance, if you weigh 200 pounds, your goal would be to lose about 10 to 14 pounds.
- Move more. Get at least 30 minutes of physical activity 5 days a week. If you have not been active, talk with your health care professional about which activities are best. Start slowly to build up to your goal.
- Eat healthy foods most of the time. Eat smaller portions to reduce the amount of calories you eat each day and help you lose weight. Choosing foods with less fat is another way to reduce calories. Drink water instead of sweetened beverages.
In 8 randomized clinical trials 14 with 2241 participants randomized to exercise and diet intervention and 2509 participants to standard recommendation. Furthermore, 178 participants were randomised to an exercise only intervention and 167 participants to a diet only intervention. The duration of the interventions in the trials ranged from one year to six years. Interventions varied between studies but mainly consisted of caloric restriction if the person was overweight, low fat content (especially saturated fat), high carbohydrate content and the increase of fibre intake. Physical activity varied but on average at least 150 minutes each week of brisk walking or other activities such as cycling or jogging were recommended. Interventions were mainly delivered by frequent individual counseling by a physiotherapist, an exercise physiologist and a dietitian. Interventions aimed at increasing exercise combined with diet are able to decrease the incidence of type 2 diabetes mellitus in high risk groups (people with impaired glucose tolerance or the metabolic syndrome) by 37% with exercise and diet. This had favorable effects on body weight, waist circumference and blood pressure 14.
Ask your health care professional about what other changes you can make to prevent or delay type 2 diabetes.
Most often, your best chance for preventing type 2 diabetes is to make lifestyle changes that work for you long term.
Prediabetes signs and symptoms
Prediabetes doesn’t have any signs or symptoms. One possible sign of prediabetes is darkened skin (a patch of velvety brown pigmentation) around your neck, armpits and groin regions called acanthosis nigricans (see Figure 2). A lot of people don’t get any symptoms when it comes to type 2 diabetes, or don’t notice them. If you start to have any of the symptoms of type 2 diabetes it means you have probably already developed it.
Classic signs and symptoms that suggest you’ve moved from prediabetes to type 2 diabetes include:
- Increased thirst
- Going to the toilet to urinate more often, especially at night
- Increased hunger
- Feeling more tired, because your body can’t get enough glucose in to your cells for energy
- Blurred vision
- Numbness or tingling in the feet or hands
- Frequent infections
- Slow-healing sores or cuts and wounds taking longer to heal
- Losing weight without trying
- Genital itching or thrush.
Figure 2. Acanthosis nigricans
Prediabetes complications
People with prediabetes may already have damage to their eyes, kidneys, blood vessels, and heart. Evidence from numerous studies suggests that the chronic complications of type 2 diabetes start to develop during the prediabetic state. So by the time you have prediabetes, it may already too late to prevent organ damage, so best to prevent prediabetes in the first place, and the earlier the better.
The most serious consequence of prediabetes is progression to type 2 diabetes. That’s because type 2 diabetes can lead to:
- High blood pressure
- High cholesterol
- Heart disease
- Stroke
- Kidney disease
- Blindness
- Amputations
Research indicates that prediabetes is often associated with heart attacks and can damage your kidneys, even if you haven’t progressed to type 2 diabetes.
Prediabetes diagnosis
Screening and diagnostic tests are the same as those used for type 2 diabetes. Monitoring is not generally indicated, but the American Diabetes Association recommends that people with prediabetes be screened for the development of type 2 diabetes on a yearly basis. The American Diabetes Association also recommends that diabetes screening for most adults begin at age 35. And if you’ve had gestational diabetes, your doctor will likely check your blood sugar levels at least once every three years.
Doctors most often use the fasting plasma glucose (FPG) test or the A1C (HbA1c) test to find out if someone has prediabetes. Less often, doctors use the oral glucose tolerance test (OGTT), which is more expensive and not as easy to give.
Doctors don’t usually test for insulin resistance. The most accurate test for insulin resistance is complicated and used mostly for research.
You should be tested for prediabetes if you are overweight or have obesity and have one or more other risk factors for diabetes, or if your parents, siblings, or children have type 2 diabetes. Even if you don’t have risk factors, you should start getting tested once you reach age 35.
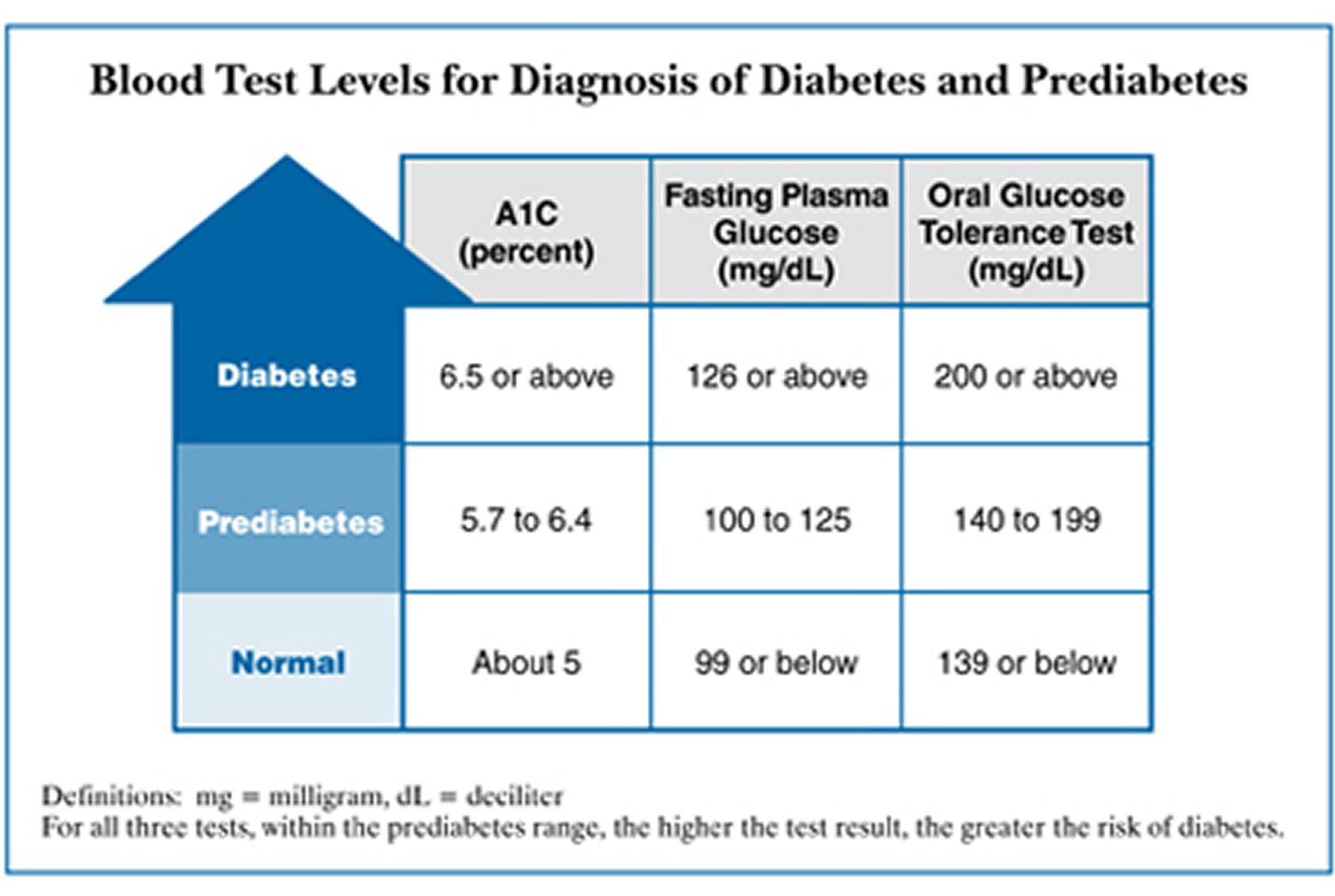
The following test results show prediabetes 15:
- A1C (HbA1c): 5.7 to 6.4 percent
- Fasting plasma glucose (FPG): 100 to 125 mg/dL (5.6 to 6.9 mmol/L)
- Oral glucose tolerance test (OGTT): 140 to 199 mg/dL (7.8 to 11.1 mmol/L)
If the results are normal but you have other risk factors for diabetes, you should be retested at least every 3 years (testing might occur more frequently if you have additional risk factors for diabetes) 15.
Prediabetes A1c
Glycated hemoglobin (A1C or HbA1c) test shows your average blood sugar level for the past three months. A1C (HbA1c) test measures the percentage of blood sugar attached to the oxygen-carrying protein in red blood cells called hemoglobin. The higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached.
Glycated hemoglobin (A1C) test in general:
- An A1C level below 5.7% is considered normal
- An A1C level between 5.7% and 6.4% is considered prediabetes
- An A1C level of 6.5% or higher on two separate tests indicates type 2 diabetes
Certain conditions can make the A1C test inaccurate — such as if you’re pregnant or have an uncommon form of hemoglobin.
Fasting plasma glucose (FPG) test
With fasting blood sugar test (FPG) a blood sample is taken after you fast for at least eight hours or overnight.
In general:
- A fasting blood sugar level below 100 milligrams per deciliter (mg/dL) — 5.6 millimoles per liter (mmol/L) — is considered normal.
- A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 7.0 mmol/L) is considered prediabetes. This result is sometimes called impaired fasting glucose.
- A fasting blood sugar level of 126 mg/dL (7.0 mmol/L) or higher indicates type 2 diabetes. Individuals who have a fasting blood glucose level greater than or equal to 7.0 mmol/L (126 mg/dl) will be retested and if the results are consistent, diagnosed with diabetes.
Oral glucose tolerance test (OGTT)
Oral glucose tolerance test (OGTT) is usually used to diagnose diabetes only during pregnancy. A blood sample is taken after you fast for at least eight hours or overnight. Then you’ll drink a sugary solution, and your blood sugar level will be measured again after two hours.
In general:
- A blood sugar level less than 140 mg/dL (7.8 mmol/L) is considered normal.
- A blood sugar level from 140 to 199 mg/dL (7.8 to 11.0 mmol/L) is considered prediabetes. This is sometimes referred to as impaired glucose tolerance.
- A blood sugar level of 200 mg/dL (11.1 mmol/L) or higher indicates type 2 diabetes.
If you have prediabetes, your doctor will typically check your blood sugar levels at least once a year.
Children and prediabetes testing
Type 2 diabetes is becoming more common in children and adolescents, likely due to the rise in childhood obesity. The American Diabetes Association recommends prediabetes testing for children who are overweight or obese and who have one or more other risk factors for type 2 diabetes.
These other risk factors include:
- Family history of type 2 diabetes.
- Race. Children who are African American, Hispanic, Native American, Asian American and Pacific Islander are at higher risk.
- Low birth weight.
- Being born to a mother who had gestational diabetes.
The ranges of blood sugar level considered normal, prediabetic and diabetic are the same for children and adults.
Children who have prediabetes should be tested annually for type 2 diabetes — or more often if the child experiences a change in weight or develops signs or symptoms of diabetes, such as increased thirst, increased urination, fatigue or blurred vision.
What test numbers tell you if you have diabetes or prediabetes?
Each test to detect diabetes and prediabetes uses a different measurement. Usually, the same test method needs to be repeated on a second day to diagnose diabetes. Your doctor may also use a second test method to confirm that you have diabetes.
If you had diabetes while you were pregnant, you should get tested 6 to 12 weeks after your baby is born to see if you have type 2 diabetes.
The following table helps you understand what your test numbers mean if you are not pregnant.
| Diagnosis | A1C (percent) | Fasting plasma glucose (FPG)a | Oral glucose tolerance test (OGTT)ab | Random plasma glucose test (RPG)a |
|---|---|---|---|---|
| Normal | below 5.7% | 99 mg/dL or below | 139 mg/dL or below | |
| Prediabetes | 5.7 to 6.4% | 100 to 125 mg/dL | 140 to 199 mg/dL | |
| Diabetes | 6.5% or above | 126 mg/dL or above | 200 mg/dL or above | 200 mg/dL or above |
Footnotes: aGlucose values are in milligrams per deciliter, or mg/dL.bAt 2 hours after drinking 75 grams of glucose. To diagnose gestational diabetes, health care professionals give more glucose to drink and use different numbers as cutoffs.
[Source 16 ]Prediabetes treatment
The primary focus of treatment for prediabetes and prevention of progression to type 2 diabetes is lifestyle changes 4. Weight loss, eating a healthy diet, and regular physical activity can help prevent or delay the development of type 2 diabetes and reduce blood glucose levels. In some cases, oral diabetes medications may also be prescribed.
Research shows that you can lower your risk for type 2 diabetes by 58% by 17, 18, 19:
- Losing 7% of your body weight (or 15 pounds if you weigh 200 pounds)
- Exercising moderately (such as brisk walking) 30 minutes a day, five days a week
Don’t worry if you can’t get to your ideal body weight. Losing even 10 to 15 pounds can make a huge difference.
To prevent prediabetes from progressing to type 2 diabetes, try to:
- Eat healthy foods. Choose foods low in fat and calories and high in fiber. Focus on fruits, vegetables and whole grains. Eat a variety of foods to help you achieve your goals without compromising taste or nutrition.
- Be more active. Aim for at least 150 minutes of moderate or 75 minutes of vigorous aerobic activity a week.
- Lose excess weight. If you’re overweight, losing just 5% to 7% of your body weight — about 14 pounds (6.4 kilograms) if you weigh 200 pounds (91 kilograms) — can reduce the risk of type 2 diabetes. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits.
- Stop smoking. Smoking may up your risk of developing type 2 diabetes.
- Take medications as needed. If you’re at high risk of diabetes, your doctor might recommend metformin (Glumetza, others). This is usually prescribed for older adults who are obese and unable to lower blood sugar levels with lifestyle changes. Medications to control cholesterol and high blood pressure might also be prescribed.
Children prediabetes treatment
Children with prediabetes should undertake the lifestyle changes recommended for adults with type 2 diabetes, including:
- Losing weight
- Eating fewer refined carbohydrates and fats, and more fiber
- Reducing portion sizes
- Eating out less often
- Spending at least one hour every day in physical activity
Medication generally isn’t recommended for children with prediabetes unless lifestyle changes aren’t improving blood sugar levels. If medication is needed, metformin (Glumetza, others) is usually the recommended drug.
Alternative medicine
Many alternative therapies have been touted as possible ways to treat or prevent type 2 diabetes. But there’s no definitive evidence that any alternative treatments are effective. Therapies that have been said to be helpful in type 2 diabetes and are also likely to be safe, include:
- Cassia cinnamon
- Flaxseed
- Ginseng
- Magnesium
- Oats
- Soy
- Xanthan gum
Talk to your health care provider if you’re considering dietary supplements or other alternative therapies to treat or prevent prediabetes. Some supplements or alternative therapies might be harmful if combined with certain prescription medications. Your health care provider can help you weigh the pros and cons of specific alternative therapies.
Prediabetes diet
There is no specific diet for prediabetes. But the foods you eat not only make a difference to how you manage your diabetes, but also to how well you feel and how much energy you have.
Fruit and vegetables
Fruit and veg are naturally low in calories and packed full of vitamins, minerals and fiber. They also add flavor and variety to every meal. Fruit and vegetables can help protect against stroke, heart disease, high blood pressure and some cancers – and when you have diabetes, you’re more at risk of developing these conditions.
Fruit and vegetables benefits
- Help to keep your digestive system working well
- Help protect the body from heart disease, stroke and some cancers
Examples of what to try:
- sliced melon or grapefruit topped with unsweetened yogurt, or a handful of berries, or fresh dates, apricots or prunes for breakfast
- mix carrots, peas and green beans into your pasta bake
- add an extra handful of peas to rice, spinach to lamb or onions to chicken
- try mushrooms, cucumber, spinach, cabbage, cauliflower, broccoli, celery and lettuce for lower carb vegetable options
- try avocados, blackberries, raspberries, strawberries, plums, peaches and watermelon for lower carb fruit options
Fresh, frozen, dried and canned – they all count. Go for a rainbow of colors to get as wide a range of vitamins and minerals as possible. Try to avoid fruit juices and smoothies as they don’t have as much fiber.
Everyone should aim to eat at least five portions a day. A portion is roughly what fits in the palm of your hand.
Starchy foods
Starchy foods are things like potatoes, rice, pasta, bread, chapattis, naan and plantain. They all contain carbohydrate, which is broken down into glucose and used by our cells as fuel. The problem with some starchy foods is that it can raise blood glucose levels quickly, which can make it harder for you to manage your diabetes. These foods have something called a high glycemic index (GI).
There are some better options for starchy foods – ones that affect blood glucose levels more slowly. These are foods with a low glycemic index (GI), like wholegrain bread, whole-wheat pasta and basmati, brown or wild rice. They also have more fiber, which helps to keep your digestive system working well. So if you’re trying to cut down on carbs, cut down on things like white bread, pasta and rice first.
Starchy foods benefits
- The fiber helps to keep your digestive system healthy
- Some affect your blood sugar levels more slowly
- Wholegrains help protect your heart
Examples of what to try
- two slices of multigrain toast with a bit of spread and Marmite or peanut butter
- brown rice, pasta or noodles in risottos, salads or stir-fries
- baked sweet potato with the skin left on – add toppings like cottage cheese or beans
- boiled cassava, flavored with chilli and lemon
- chapatti made with brown or wholemeal atta.
Proteins
Meat and fish are high in protein, which keeps your muscles healthy. But a healthy diet means less red and processed meat – they’ve been linked to cancer and heart disease. Oily fish like mackerel, salmon and sardines have a lot of omega-3 oil, which can help protect the heart.
Protein foods benefits
- Helps keep your muscles healthy
- Oily fish protects your heart
Aim to have some food from this group every day. Specifically at least 1 or 2 portions of oily fish each week. But you don’t need to eat meat every day.
Examples of what to try
- a small handful of raw nuts and seeds as a snack or chopped with a green salad
- using beans and pulses in a casserole to replace some – or all – of the meat
- eggs scrambled, poached, dry fried or boiled – the choice is yours
- grilled fish with masala, fish pie, or make your own fishcakes
- chicken grilled, roasted or stir-fried
Dairy foods
Milk, cheese and yogurt have lots of calcium and protein in – great for your bones, teeth and muscles. But some dairy foods are high in fat, particularly saturated fat, so choose lower-fat alternatives.
Check for added sugar in lower-fat versions of dairy foods, like yoghurt. It’s better to go for unsweetened yoghurt and add some berries if you want it sweeter. If you prefer a dairy alternative like soya milk, choose one that’s unsweetened and calcium-fortified.
Dairy foods Benefits
- Good for bones and teeth
- Keeps your muscles healthy
Examples of what to try
- a glass of milk straight, flavored with a little cinnamon or added to porridge
- natural or unsweetened yogurt with fruit or on curry
- cottage cheese scooped on carrot sticks
- a bowl of breakfast cereal in the morning, with skimmed or semi-skimmed milk
- a cheese sandwich for lunch, packed with salad
- a refreshing lassi or some plain yogurt with your evening meal
Oils and fats
You need some healthy fat in your diet but you need less saturated fat. This is because some saturated fats can increase cholesterol in your blood, increasing your risk of heart diseases and stroke. These less healthy options are butter, palm nut oil and coconut oil.
Healthier unsaturated fats are foods like olive oil, vegetable oil, rapeseed oil, spreads made from these oils, and nut butters.
Examples of what to try
- A drizzle of olive oil on your salad
- Peanut butter on your wholemeal toast
Avoid foods high in saturated fat, salt and sugar
You don’t need any of these as part of a healthy diet. The less often, the better. But we know you’re bound to eat these foods from time to time, so it’s really important to know how they might affect your body.
These foods include biscuits, crisps, chocolates, cakes, ice cream, butter and sugary drinks. These sugary foods and drinks are high in calories and raise blood sugar levels, so go for diet, light or low-calorie alternatives. And the best drink to choose is water – it’s calorie free.
They’re also high in unhealthy saturated fats, so they aren’t good for cholesterol levels and your heart.
And they can also be full of salt – processed foods especially. Too much salt can make you more at risk of high blood pressure and stroke. You should have no more than 1 tsp (6g) of salt a day.
Experts don’t recommend ‘diabetic’ ice cream or sweets. It’s now against the law to label any food as diabetic and there’s no evidence to suggest that food for diabetics offer any benefits over eating a healthy balanced diet.
Tips for cutting out saturated fat, salt and sugar
- Cook more meals from scratch at home, where you can control the amount of salt you use.
- Check food labels – look for green and orange colors.
- Try unsweetened teas and coffees – they’re better than fruit juices and smoothies as they don’t add any extra calories and carbs.
- Banish the salt shaker from the table – black pepper, herbs and spices are great ways of adding extra flavor to your food.
- Making your own sauces, like tomato ketchup and tandoori marinades.
- What is prediabetes? https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance#prediabetes[↩]
- Blood Sugar Level Ranges. https://www.diabetes.co.uk/diabetes_care/blood-sugar-level-ranges.html[↩][↩]
- Diabetes Diagnosis. https://diabetes.org/diabetes/a1c/diagnosis[↩][↩]
- Alvarez S, Coffey R, Algotar AM. Prediabetes. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459332[↩][↩][↩][↩][↩][↩]
- Horstman C, Aronne L, Wing R, Ryan DH, Johnson WD. Implementing an Online Weight-Management Intervention to an Employee Population: Initial Experience with Real Appeal. Obesity (Silver Spring). 2018 Nov;26(11):1704-1708. doi: 10.1002/oby.22309[↩]
- Moin T, Damschroder LJ, AuYoung M, Maciejewski ML, Havens K, Ertl K, Vasti E, Weinreb JE, Steinle NI, Billington CJ, Hughes M, Makki F, Youles B, Holleman RG, Kim HM, Kinsinger LS, Richardson CR. Results From a Trial of an Online Diabetes Prevention Program Intervention. Am J Prev Med. 2018 Nov;55(5):583-591. doi: 10.1016/j.amepre.2018.06.028[↩]
- Stepanek L, Horakova D, Nakladalova M, Cibickova L, Karasek D, Zadrazil J. Significance of prediabetes as a nosological entity. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2018 Sep 24. doi: 10.5507/bp.2018.057[↩]
- Type 2 diabetes: prevention in people at high risk. National Institute for Health and Care Excellence. Public health guideline 12 July 2012. https://www.nice.org.uk/guidance/ph38/resources/type-2-diabetes-prevention-in-people-at-high-risk-pdf-1996304192197[↩]
- National Diabetes Statistics Report. https://www.cdc.gov/diabetes/data/statistics-report/index.html[↩]
- Freeman AM, Pennings N. Insulin Resistance. [Updated 2021 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507839[↩][↩]
- Bothou C, Beuschlein F, Spyroglou A. Links between aldosterone excess and metabolic complications: A comprehensive review. Diabetes Metab. 2020 Feb;46(1):1-7. doi: 10.1016/j.diabet.2019.02.003[↩]
- Diabetes Prevention Program Outcomes Study Research Group; Orchard TJ, Temprosa M, Barrett-Connor E, Fowler SE, Goldberg RB, Mather KJ, Marcovina SM, Montez M, Ratner RE, Saudek CD, Sherif H, Watson KE. Long-term effects of the Diabetes Prevention Program interventions on cardiovascular risk factors: a report from the DPP Outcomes Study. Diabet Med. 2013 Jan;30(1):46-55. doi: 10.1111/j.1464-5491.2012.03750.x[↩][↩]
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015 Nov;3(11):866-75. doi: 10.1016/S2213-8587(15)00291-0[↩][↩][↩]
- Cochrane Review 16 July 2008. Exercise or exercise and diet for preventing type 2 diabetes mellitus. http://www.cochrane.org/CD003054/ENDOC_exercise-or-exercise-and-diet-for-preventing-type-2-diabetes-mellitus[↩][↩]
- American Diabetes Association. Standards of Medical Care in Diabetes-2017 Abridged for Primary Care Providers. Clin Diabetes. 2017 Jan;35(1):5-26. doi: 10.2337/cd16-0067[↩][↩]
- Adapted from American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care. 2016;39(1):S14–S20, tables 2.1, 2.3.[↩]
- Blackett P, George M, Wilson DP. Integrating lipid screening with ideal cardiovascular health assessment in pediatric settings. J Clin Lipidol. 2018 Nov-Dec;12(6):1346-1357. doi: 10.1016/j.jacl.2018.08.009[↩]
- Kamble PS, Collins J, Harvey RA, Prewitt T, Kimball E, Deluzio T, Allen E, Bouchard JR. Understanding Prediabetes in a Medicare Advantage Population Using Data Adaptive Techniques. Popul Health Manag. 2018 Dec;21(6):477-485. doi: 10.1089/pop.2017.0165[↩]
- Lim WY, Ma S, Heng D, Tai ES, Khoo CM, Loh TP. Screening for diabetes with HbA1c: Test performance of HbA1c compared to fasting plasma glucose among Chinese, Malay and Indian community residents in Singapore. Sci Rep. 2018 Aug 20;8(1):12419. doi: 10.1038/s41598-018-29998-z[↩]