Contents
- What is stomach spasm ?
- Abdominal Pain causes
- Non-abdominal causes:
- Abdominal or chest wall pain:
- Inflammatory conditions of the upper abdomen:
- Functional problems of the abdomen:
- Cancers of the upper abdomen:
- Vascular problems:
- Inflammatory conditions in the mid- and lower abdomen:
- Bowel obstruction:
- Urinary tract problems:
- Pelvic problems in women:
- Abdominal pain in infants and toddlers
- Abdominal pain in adolescents
- Abdominal pain in women
- Older patients with abdominal pain
- Diagnosis of abdominal pain
- What treatments are available for abdominal pain ?
- Abdominal Pain causes
What is stomach spasm ?
Abdominal pain or “stomach spasm” is a common presentation in the outpatient setting and is challenging to diagnose. Abdominal pain is pain that you feel anywhere between your chest and groin 1. This is often referred to as the stomach region or belly. Some people use the word stomach to refer to the area of the body between the chest and the pelvic area. The medical term for this area is the abdomen. For instance, some people with pain in this area would say they have a “stomach ache,” when in fact the pain could be coming from the appendix, small intestine, colon (large intestine) or other organs in the area. Doctors would call this symptom abdominal pain, because the stomach is only one of many organs in the abdomen.
Almost everyone has pain in the abdomen at some point. Most of the time, it is not serious.
Although most abdominal pain is benign, as many as 10 percent of patients in the emergency department setting and a lesser percentage in the outpatient setting have a severe or life-threatening cause or require surgery 2. Therefore, a thorough and logical approach to the diagnosis of abdominal pain is necessary.
Ordinarily, we are unaware of any of the actions of the organs in the abdomen or any discomfort from activities such as eating, movement of food through the intestines, or bowel movements. Nerves are constantly monitoring activities in the body, and when those messages are transmitted to the brain and come into consciousness as unpleasant sensations, we may sense pain or discomfort.
Pain is always abnormal, but it may not be a medical emergency. For example, you might have very bad abdominal pain if you have gas or stomach cramps due to viral gastroenteritis. Mild pain or chronic pain that is not associated with danger signs (“red flags”) should be discussed with your doctor when it is convenient. Severe pain or pain that is associated with red flags should be discussed with your doctor; he or she may want you to visit the office or even the emergency room, depending upon your specific complaints. Red flags that should prompt discussion with your doctor include fever, diarrhea, persistent constipation, blood in the stools, persistent nausea or vomiting, vomiting blood, severe tenderness of the belly, jaundice (yellowish discoloration of the skin) or swelling of the abdomen.
- How bad your pain is does not always reflect the seriousness of the condition causing the pain.
However, life-threatening conditions, such as colon cancer or early appendicitis, may only cause mild pain or no pain.
Get medical help immediately if:
- You have abdominal pain that is sudden and sharp
- You also have pain in your chest, neck or shoulder
- You’re vomiting blood or have blood in your stool
- Your abdomen is stiff, hard and tender to touch
- You can’t move your bowels, especially if you’re also vomiting
Other ways to describe pain in your abdomen include:
- Generalized pain: This means that you feel it in more than half of your belly. This type of pain is more typical for a stomach virus, indigestion, or gas. If the pain becomes more severe, it may be caused by a blockage of the intestines.
- Localized pain: This is pain found in only one area of your belly. It is more likely to be a sign of a problem in an organ, such as the appendix, gallbladder, or stomach.
- Cramp-like pain: This type of pain is not serious most of the time. It is likely to be due to gas and bloating, and is often followed by diarrhea. More worrisome signs include pain that occurs more often, lasts than 24 hours, or occurs with a fever.
- Colicky pain: This type of pain comes in waves. It very often starts and ends suddenly, and is often severe. Kidney stones and gallstones are common causes of this type of belly pain.
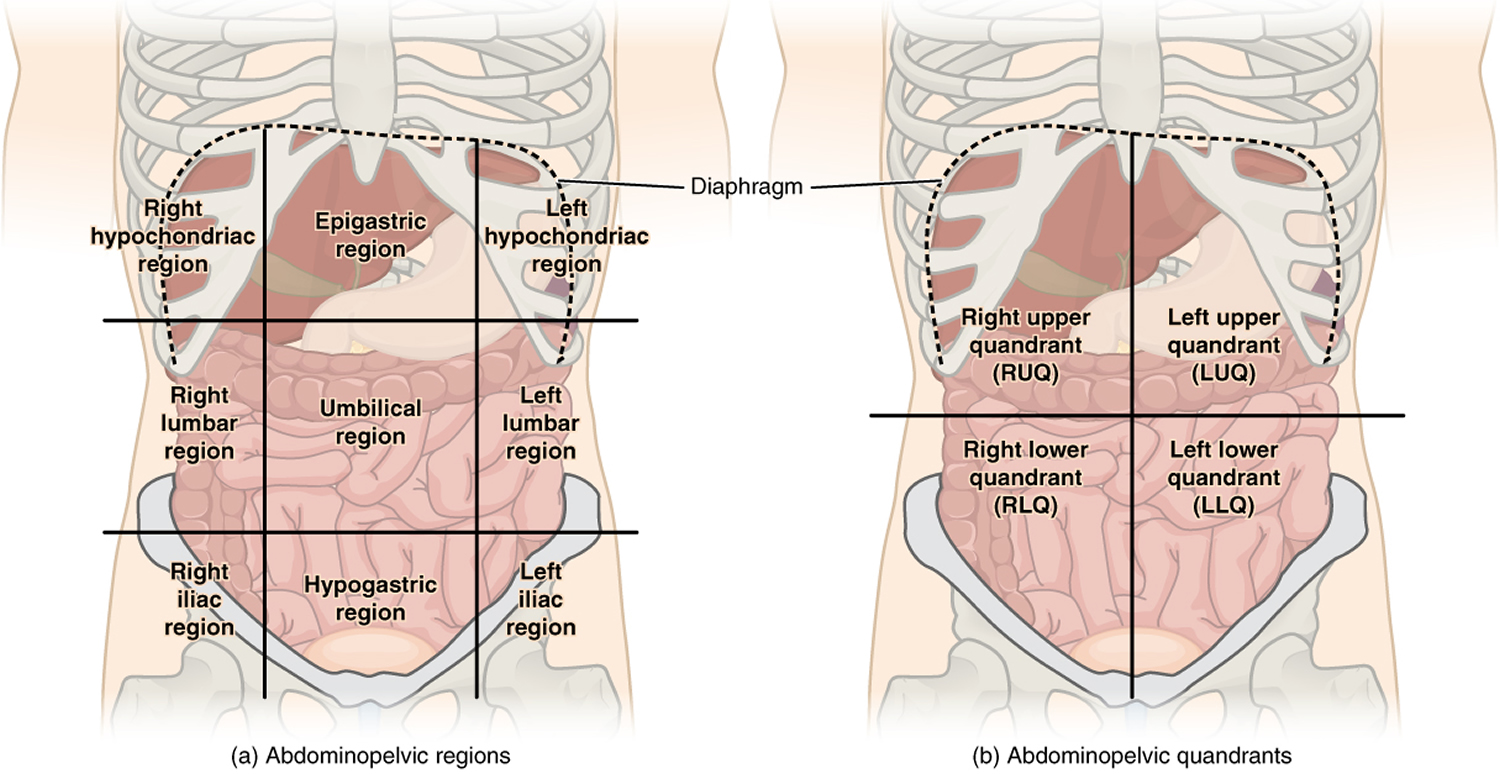
When evaluating a patient with acute abdominal pain, physicians usually focus on common conditions that cause abdominal pain as well as other more serious conditions. The location of pain should drive the evaluation (Figure 1). For some diagnoses, such as appendicitis, the location of pain has a very strong predictive value.
Figure 1. Quadrants of Abdomen
Abdominal Pain causes
Many different conditions can cause abdominal pain. The key is to know when you need to get medical care right away. Sometimes you may only need to see a health care provider if your symptoms continue.
Pain can arise from any of the structures within the abdomen or the abdominal wall. In addition, pain messages originating in the chest, back, or pelvis can sometimes be perceived as coming from the abdomen. For example, patients with heart attacks or pneumonia sometimes complain of upper abdominal pain rather than chest pain. There are many possible causes of abdominal pain. Tables 1 and 2 shows some of the more common causes of pain in adults and children.
Less serious causes of abdominal pain include:
- Constipation
- Irritable bowel syndrome
- Food allergies or intolerance (such as lactose intolerance)
- Food poisoning
- Stomach flu
Other possible causes include:
- Appendicitis
- Abdominal aortic aneurysm (bulging and weakening of the major artery in the body)
- Bowel blockage or obstruction
- Cancer of the stomach, colon (large bowel), and other organs
- Cholecystitis (inflammation of the gallbladder) with or without gallstones
- Decreased blood supply to the intestines (ischemic bowel)
- Diverticulitis (inflammation and infection of the colon)
- Heartburn, indigestion, or gastroesophageal reflux (GERD)
- Inflammatory bowel disease (Crohn disease or ulcerative colitis)
- Kidney stones
- Pancreatitis (swelling or infection of the pancreas)
- Ulcers.
Sometimes, abdominal pain may occur due to a problem somewhere else in your body, such as your chest or pelvic area. For example, you may have abdominal pain if you have:
- Severe menstrual cramps
- Endometriosis
- Muscle strain
- Pelvic inflammatory disease (PID)
- Tubal (ectopic) pregnancy
- Urinary tract infections.
Get medical help right away or call your local emergency number if you:
- Are currently being treated for cancer
- Are unable to pass stool, especially if you are also vomiting
- Are vomiting blood or have blood in your stool (especially if bright red, maroon or dark, tarry black)
- Have chest, neck, or shoulder pain
- Have sudden, sharp abdominal pain
- Have pain in, or between, your shoulder blades with nausea
- Have tenderness in your belly, or your belly is rigid and hard to the touch
- Are pregnant or could be pregnant
- Had a recent injury to your abdomen
- Have difficulty breathing
See your healthcare provider if you have:
- Abdominal discomfort that lasts 1 week or longer
- Abdominal pain that does not improve in 24 to 48 hours, or becomes more severe and frequent and occurs with nausea and vomiting
- Bloating that persists for more than 2 days
- Burning sensation when you urinate or frequent urination
- Diarrhea for more than 5 days
- Fever, over 100°F (37.7°C) for adults or 100.4°F (38°C) for children, with pain
- Prolonged poor appetite
- Prolonged vaginal bleeding
- Unexplained weight loss.
Non-abdominal causes:
- Pneumonia (lung infection)
- Myocardial infarction (heart attack)
- Pleurisy (irritation of the lining around the lungs)
- Pulmonary embolism (blood clots to the lungs)
Abdominal or chest wall pain:
- Shingles (herpes zoster infection)
- Costochondritis (inflammation of the rib cartilages)
- Injury (blunt trauma, muscle pulls)
- Nerve irritation (neuropathy)
- Hernias (protrusions of structures through the abdominal wall)
- Scars
Inflammatory conditions of the upper abdomen:
- Ulcer disease (duodenal ulcer, gastric ulcer)
- Esophagitis (gastroesophageal reflux disease)
- Gastritis (irritation of the lining of the stomach)
- Pancreatitis (inflammation of the pancreas)
- Cholecystitis (inflammation of the gall bladder)
- Choledocholithiasis (passage of gall stones through the bile duct)
- Hepatitis (infection or inflammation of the liver)
- Colitis (infection or inflammation of the colon)
Functional problems of the abdomen:
- Non-ulcer dyspepsia or indigestion (discomfort after eating not due to ulcers)
- Sphincter of Oddi dysfunction (problems with the bile duct valve)
- Functional abdominal pain (pain without clear cause)
- Irritable bowel syndrome (pain associated with bowel movements)
Cancers of the upper abdomen:
- Hepatoma (liver cancer)
- Cholangiocarcinoma (bile duct or gall bladder cancer)
- Pancreatic cancer
- Stomach cancer
- Lymphoma (cancer of the immune cells)
Vascular problems:
- Mesenteric vascular insufficiency (blocked arteries or veins)
- Abdominal aortic aneurysm (swelling of the main artery in the belly)
Inflammatory conditions in the mid- and lower abdomen:
- Enteritis (infections of the small bowel, Crohn’s disease)
- Colitis (infection or inflammation of the colon)
- Diverticulitis (inflammation of pouches that form in the colon)
- Appendicitis
Bowel obstruction:
- Adhesions (scars in the belly that form after surgery or inflammation)
- Tumor
- Inflammation
- Colon Cancer
Urinary tract problems:
- Kidney stones
- Urinary tract infections (kidneys, bladder)
- Tumors of the kidneys or bladder
Pelvic problems in women:
- Ovarian cysts or cancer
- Infection of the tubes (salpingitis)
- Ectopic pregnancy
- Fibroid tumors of the uterus (womb)
- Malignant tumors of the uterus or cervix
- Endometriosis
- Adhesions (scars)
Table 1. Causes of Abdominal Pain in Adults
Pain location | Possible diagnoses |
| Right upper quadrant | Biliary: cholecystitis, cholelithiasis, cholangitis Colonic: colitis, diverticulitis Hepatic: abscess, hepatitis, mass Pulmonary: pneumonia, embolus Renal: nephrolithiasis, pyelonephritis |
| Epigastric | Biliary: cholecystitis, cholelithiasis, cholangitis Cardiac: myocardial infarction, pericarditis Gastric: esophagitis, gastritis, peptic ulcer Pancreatic: mass, pancreatitis Vascular: aortic dissection, mesenteric ischemia |
| Left upper quadrant | Cardiac: angina, myocardial infarction, pericarditis Gastric: esophagitis, gastritis, peptic ulcer Pancreatic: mass, pancreatitis Renal: nephrolithiasis, pyelonephritis Vascular: aortic dissection, mesenteric ischemia |
| Periumbilical | Colonic: early appendicitis Gastric: esophagitis, gastritis, peptic ulcer, small-bowel mass or obstruction Vascular: aortic dissection, mesenteric ischemia |
| Right lower quadrant | Colonic: appendicitis, colitis, diverticulitis, IBD, IBS Gynecologic: ectopic pregnancy, fibroids, ovarian mass, torsion, PID Renal: nephrolithiasis, pyelonephritis |
| Suprapubic | Colonic: appendicitis, colitis, diverticulitis, IBD, IBS Gynecologic: ectopic pregnancy, fibroids, ovarian mass, torsion, PID Renal: cystitis, nephrolithiasis, pyelonephritis |
| Left lower quadrant | Colonic: colitis, diverticulitis, IBD, IBS Gynecologic: ectopic pregnancy, fibroids, ovarian mass, torsion, PID Renal: nephrolithiasis, pyelonephritis |
| Any location | Abdominal wall: herpes zoster, muscle strain, hernia Other: bowel obstruction, mesenteric ischemia, peritonitis, narcotic withdrawal, sickle cell crisis, porphyria, IBD, heavy metal poisoning |
Table 2. Causes of Abdominal Pain in Children
| All ages | Infants and toddlers (0 to 4 years) | School age (5 to 11 years) | Adolescents (12 to 18 years) |
|---|---|---|---|
Appendicitis | Hirschsprung disease | Abdominal migraine | Ectopic pregnancy |
Bowel obstruction | Infantile colic | Functional pain | Functional pain |
Child abuse | Inguinal hernia | Henoch-Schönlein purpura | Inflammatory bowel disease |
Constipation | Intussusception | Intussusception | Irritable bowel syndrome |
Dietary indiscretions | Lactose intolerance | Lead poisoning | Menstrual-related condition |
Gallbladder disease | Lead poisoning | Mononucleosis | Mononucleosis |
Gastroenteritis | Malrotation of the midgut | Volvulus | Omental infarction |
Hemolytic uremic syndrome | Meckel diverticulum | Other pregnancy issues | |
Mesenteric adenitis | Volvulus | Ovarian or testicular torsion | |
Pancreatitis | Pelvic inflammatory disease | ||
Sickle cell crisis | Sexually transmitted infection | ||
Trauma | |||
Upper respiratory infection | |||
Urinary tract infection |
Abdominal pain in infants and toddlers
In infants and toddlers, acute abdominal pain may be caused by intussusception and congenital anomalies, including Meckel diverticulum, malrotation of the midgut, and inguinal hernias. Intussusception usually occurs before two years of age 5. Infants and toddlers may present with right lower quadrant tenderness, a sausage-shaped mass in the abdomen, and red currant jelly stool caused by venous congestion of intussuscepted bowel 5. However, the classic triad of colicky abdominal pain, vomiting, and bloody stool is found in less than 50% of cases 6. In children, 90% of cases of intussusception are idiopathic, with 10% of cases resulting from a lead point or sticky spot in the colon 5. Air or contrast enema can be diagnostic and therapeutic for intussusception.
Symptomatic Meckel diverticulum can present with gastrointestinal bleeding, diverticulitis, bowel obstruction, peritonitis, intussusception, or volvulus. One-half of such cases occur in children younger than four years 7. Malrotation of the midgut leading to volvulus causes bilious vomiting, pain, diarrhea, and bloody stools in more advanced cases. Incarcerated inguinal hernias present with a tender groin mass.
Abdominal pain in adolescents
In adolescents, acute abdominal pain may result from a gonad- or pregnancy-related pathology. Ovarian torsion presents with intermittent, nonradiating unilateral lower abdominal pain with an enlarged adnexa on ultrasonography or CT scan 8. Testicular torsion commonly presents with a tender scrotum and enlarged testis in adolescents, but boys may present with a complaint of hip or abdominal pain with nausea or vomiting.
Ectopic pregnancy and early pregnancy loss must be considered in adolescent girls. Both conditions may present with vaginal bleeding, cramping pain, and abdominal tenderness. An intrauterine pregnancy should be visualized with transvaginal ultrasonography when the beta human chorionic gonadotropin level is 1,500 to 2,000 mIU per mL (1,500 to 2,000 IU per L) 9. Early pregnancy loss may be seen as an empty gestational sac or gestational sac without fetal heart activity on transvaginal ultrasonography 10. Repeat ultrasonography and serial beta human chorionic gonadotropin testing may be required to confirm pregnancy loss.
Abdominal pain in women
Abdominal pain in women may be related to pathology in the pelvic organs. Ovarian cysts, uterine fibroids, tuboovarian abscesses, and endometriosis are common causes of lower abdominal pain in women. In women of reproductive age, special attention to pregnancy, including ectopic pregnancy, and loss of pregnancy is critical in forming an appropriate differential diagnosis. The possibility of pregnancy modifies the likelihood of disease and significantly changes the diagnostic approach (e.g., avoidance of radiation exposure in diagnostic testing).
Older patients with abdominal pain
Older patients with abdominal pain present a particular diagnostic challenge. Disease frequency and severity may be exaggerated in this population (e.g., a higher incidence of diverticular disease or sepsis in those with urinary tract infection). Presentation may differ in older patients, and poor patient recall or a reduction in symptom severity may cause misdiagnosis. There are several diseases that should be considered in all older patients with abdominal pain because of the increased incidence and high risk of morbidity and mortality in these patients. Occult urinary tract infection, perforated viscus, and ischemic bowel disease are potentially fatal conditions commonly missed or diagnosed late in older patients.
Diagnosis of abdominal pain
The patient’s history provides the most helpful information that a doctor uses to determine the cause of abdominal pain 11. The characteristics of the pain (sharp, dull, cramping, burning, twisting, tearing, penetrating), its location and relation to eating or to having a bowel movement are important clues. Additional factors that are useful include the pattern of pain, its duration, radiation (spread) to other areas of the body, and its association with other symptoms, such as jaundice (yellow skin), nausea, vomiting, bleeding, diarrhea or constipation.
Findings on physical examination also are helpful. Key findings include areas of tenderness, the presence or absence of bowel sounds or abdominal distention, masses, organ enlargement, and evidence of blood in the stools.
Based on the history and physical examination the doctor may or may not have a clear idea about the cause of pain. Sometimes a diagnosis is made and treatment can be started. In other circumstances diagnostic tests are used to confirm or to exclude a specific diagnosis. Many tests can be ordered for these purposes. Frequently used tests include analysis of blood, urine and stool samples, x-rays of the abdomen, and endoscopy.
Table 3. Clinical Features of Selected Causes of Acute Abdominal Pain in Children
| Condition | Clinical findings | Age | Comments |
|---|---|---|---|
Abdominal migraine | Anorexia, nausea, vomiting, headache, photophobia | 3 to 10 years | Boys and girls equally affected |
Colic | Persistent crying without apparent cause | Younger than 3 months | Nonacute abdominal examination |
Constipation | Hard, infrequent stooling | All age groups | May be most common cause of abdominal pain1 |
Gastroenteritis or colitis | Diarrhea, with vomiting or fever | All age groups | Campylobacter, Cryptosporidium, Escherichia coli, Salmonella, Shigella, rotavirus |
Hirschsprung disease | Constipation, severe diarrhea, bowel obstruction, perforation, sepsis | Infant | Delayed passage of meconium (more than 24 hours) in about 57% of cases |
Inflammatory bowel disease | Bloody diarrhea | Primarily adolescents | Childhood prevalence of Crohn disease is 43 per 100,000; of ulcerative colitis, 28 per 100,000 |
Omental infarction | Lower abdominal pain, vomiting, diarrhea | School-aged, overweight males | Self-limiting, diagnosed on computed tomography |
Ovarian cyst | Lower abdominal pain | Adolescent females | Types include hemorrhagic, ruptured, and ovulatory, and torsion of a cyst |
Pneumonia | Cough, shortness of breath, fever, tachypnea | All age groups | Lower lobe pneumonia |
Pyelonephritis | Flank tenderness, fever, nausea and vomiting | All age groups | Oral antibiotics for 10 to 14 days as effective as intravenous antibiotics |
Sexually transmitted infection | Vaginal or penile discharge, fever | Adolescent | Chlamydia trachomatis, Neisseria gonorrhoeae |
Streptococcal pharyngitis | Sore throat, fever | Older than 3 years | Rapid strep test or culture |
Urinary tract infection | Dysuria, urinary frequency, urinary urgency, hematuria | All age groups, primarily females and uncircumcised infants | Point prevalence in children older than one year is 7.8% |
[Source 4]
Tests that may be done include:
- Barium enema
- Blood, urine, and stool tests
- CT scan
- Colonoscopy or sigmoidoscopy (tube through the rectum into the colon)
- EKG (electrocardiogram) or heart tracing
- Ultrasound of the abdomen
- Upper endoscopy (tube through the mouth into the esophagus, stomach and upper small intestine)
- Upper GI (gastrointestinal) and small bowel series
- X-rays of the abdomen
Blood Tests
Blood tests include complete blood counts (analysis of the numbers of white cells that fight infections, red cells that carry oxygen and that are reduced in anemia, and platelets that help the blood to clot), chemistry tests (liver and kidney tests, blood mineral levels, and enzymes released when organs like the liver or pancreas are injured), and serology tests that measure antibody levels to various infections.
Urine tests include urinalysis (measurement of characteristics and chemicals in urine along with microscopic inspection of a drop of urine), and urine culture for bacterial infection.
Stools can be analyzed for blood and pus (markers of inflammation, infections, or tumors), fat (evidence of impaired digestion and absorption of food), and the presence of germs.
X-ray and Imaging Tests
Many different kinds of x-ray and imaging tests are used to make pictures of the interior of the body. These include barium studies in which barium sulfate (a material that shows up on x-rays) is swallowed (barium swallow, upper gastrointestinal series, small bowel follow-through examination) or injected by a tube into the small intestine (enteroclysis) or colon (barium enema). Computerized tomography (CT scan) is a very sophisticated technique for reconstructing cross-sectional x-ray images of the body with the help of a computer. Magnetic resonance imaging is a similar technique in which radio waves and magnets are used to make pictures of the internal organs. Sonography uses high frequency sound waves to peer into the body and to visualize the internal structures. Nuclear medicine scans use isotopes to identify body parts and to examine their function.
Endoscopy
Endoscopy involves the use of special instruments to look into the hollow organs of the digestive tract. Upper gastrointestinal endoscopy uses a flexible tube with a television camera in its tip and a lighting system to examine the esophagus, stomach, and duodenum (the part of the intestine just beyond the stomach). Special tools can be passed through the tube to remove polyps or to obtain biopsy specimens to be viewed under a microscope. Longer tubes can reach well into the small intestine and similar tubes can be introduced through the rectum to view the colon (colonoscopy).
Special endoscopes have been designed to look at the bile ducts and pancreatic duct and to obtain sonograms from inside the gut ERCP (Endoscopic Retrograde Cholangiopancreatography) and EUS (Endoscopic Ultrasound), respectively. Another diagnostic test is capsule endoscopy in which a capsule containing a tiny camera, broadcasting station and antenna sends pictures to a special belt that is worn around the abdomen. Pictures can be obtained from throughout the small intestine as the device is propelled through the gut.
While the technology behind these tests is impressive, a cause for abdominal pain can be made in most patients by means of a history, physical examination, and a few simple tests. Every patient does not require a full panel of diagnostic tests.
What treatments are available for abdominal pain ?
Once a diagnosis is made, treatment can proceed for that condition. Sometimes medications are used to reduce inflammation or affect the function of an organ, thereby relieving pain. For example, ulcers can be treated by taking medications that reduce stomach acid secretion. As the ulcer heals, pain is reduced. Sometimes an operation is needed to correct a problem. For example, pain due to cholecystitis (inflammation of the gall bladder) is usually treated by removal of the gall bladder (cholecystectomy).
Occasionally, pain must be treated with drugs that reduce pain (analgesics). Simple analgesics like aspirin and ibuprofen should not be used ordinarily for undiagnosed abdominal pain because they may cause other problems, such as ulcers. Narcotic drugs are sometimes prescribed by doctors for abdominal pain, but their use can lead to constipation and other abdominal symptoms. Another approach is to use pain-modifying drugs to change the way that pain signals are processed in the spinal cord and brain. The drugs used most commonly for this purpose are antidepressant drugs, like amitriptyline or trazodone, that can be taken in very low doses that minimize side effects and have little or no antidepressant effects. In some cases pain management physicians use nerve blocks to identify and treat the mechanism of pain.
Signs Indicating the Possible Need for Surgery in Patients with Acute Abdominal Pain
- Absent bowel sounds
- Bilious vomiting
- Bloody diarrhea or occult blood in stool
- Elevated temperature (≥ 100.4°F [38.0°C])
- Rebound tenderness
- Rigidity (involuntary guarding)
- Voluntary guarding.
- Abdominal pain. Medline Plus. https://medlineplus.gov/ency/article/003120.htm[↩]
- Kamin RA, Nowicki TA, Courtney DS, Powers RD. Pearls and pitfalls in the emergency department evaluation of abdominal pain. Emerg Med Clin North Am. 2003;21(1):61–72.[↩]
- Evaluation of Acute Abdominal Pain in Adults. Am Fam Physician. 2008 Apr 1;77(7):971-978. http://www.aafp.org/afp/2008/0401/p971.html[↩]
- Acute Abdominal Pain in Children. Am Fam Physician. 2016 May 15;93(10):830-837. http://www.aafp.org/afp/2016/0515/p830.html[↩][↩]
- Pepper VK, Stanfill AB, Pearl RH. Diagnosis and management of pediatric appendicitis, intussusception, and Meckel diverticulum. Surg Clin North Am. 2012;92(3):505–526, vii.[↩][↩][↩]
- Mendez D, Caviness AC, Ma L, Macias CC. The diagnostic accuracy of an abdominal radiograph with signs and symptoms of intussusception. Am J Emerg Med. 2012;30(3):426–431.[↩]
- Saito JM. Beyond appendicitis: evaluation and surgical treatment of pediatric acute abdominal pain. Curr Opin Pediatr. 2012;24(3):357–364.[↩]
- Appelbaum H, Abraham C, Choi-Rosen J, Ackerman M. Key clinical predictors in the early diagnosis of adnexal torsion in children. J Pediatr Adolesc Gynecol. 2013;26(3):167–170.[↩]
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin no. 94. Medical management of ectopic pregnancy. Obstet Gynecol. 2008;111(6):1479–1485.[↩]
- Committee on Practice Bulletins—Gynecology. American College of Obstetricians and Gynecologists Practice Bulletin no. 150. Early pregnancy loss. Obstet Gynecol. 2015;125(5):1258–1267.[↩]
- Abdominal Pain Syndrome. American College of Gastroenterology. http://patients.gi.org/topics/abdominal-pain/[↩]