Contents
- Type 2 Diabetes
- Who is more likely to develop type 2 diabetes?
- What is the difference between type 1 and type 2 diabetes?
- If I’m overweight, will I always develop type 2 diabetes?
- Do sugary drinks cause diabetes?
- How does insulin work?
- Is hyperinsulinemia a form of diabetes?
- What are blood sugar levels?
- Can I check my own blood sugar?
- Why test blood sugar levels?
- What happens when my blood sugar levels are too high?
- What happens when your blood sugar levels are too low?
- What happens if I don’t treat hypoglycemia?
- Is there a cure for diabetes?
- Is there a cure for type 1 diabetes?
- Is diabetes a serious disease?
- Do people with diabetes need to eat special foods?
- How to reverse type 2 diabetes?
- What is prediabetes?
- Type 2 diabetes and pregnancy
- What is gestational diabetes?
- Causes of type 2 diabetes
- Type 2 diabetes symptoms and signs
- Type 2 diabetes complications
- Type 2 diabetes prevention
- Type 2 diabetes diagnosis
- Type 2 diabetes treatment
- Type 2 diabetes diet
Type 2 Diabetes
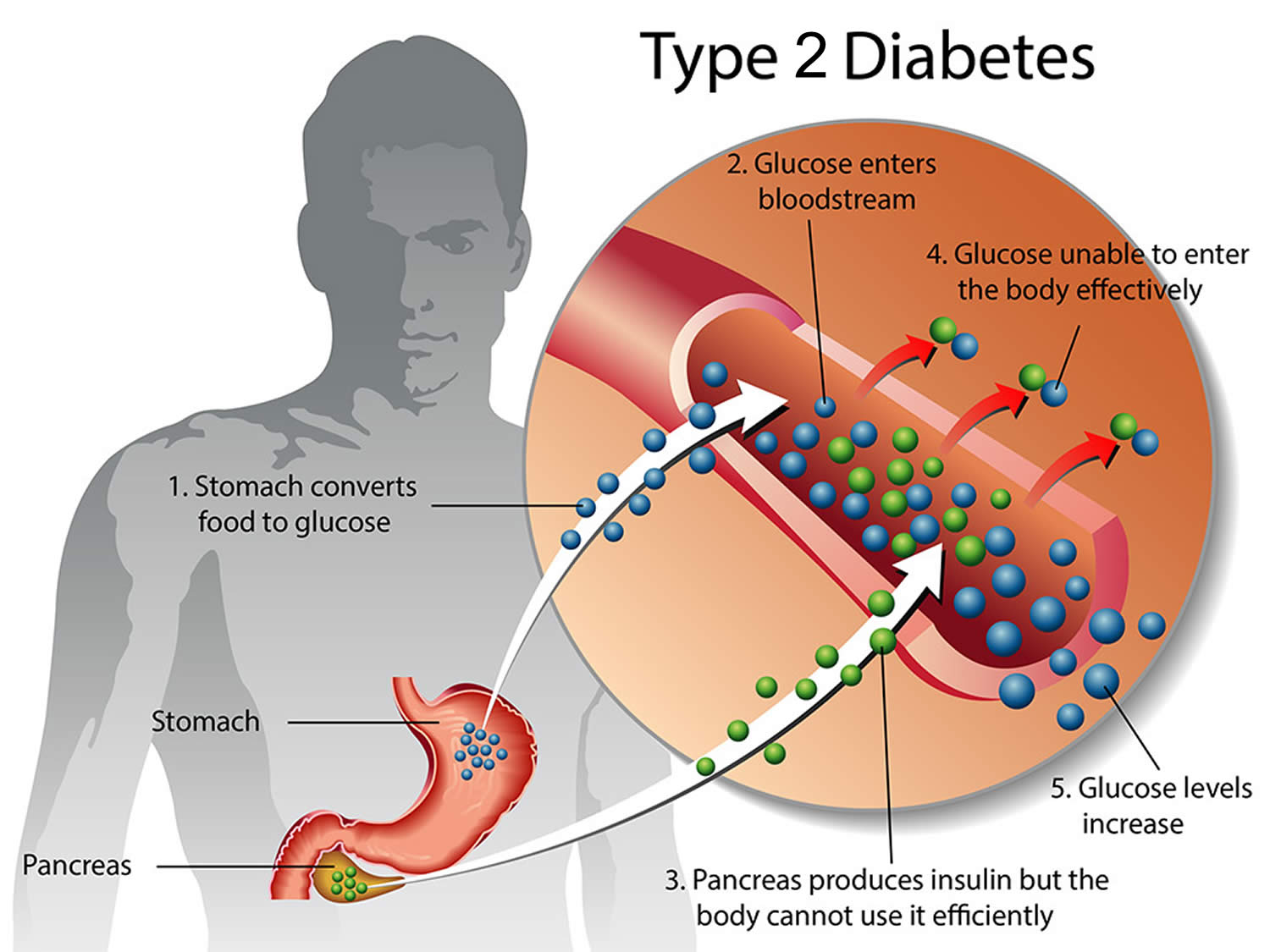
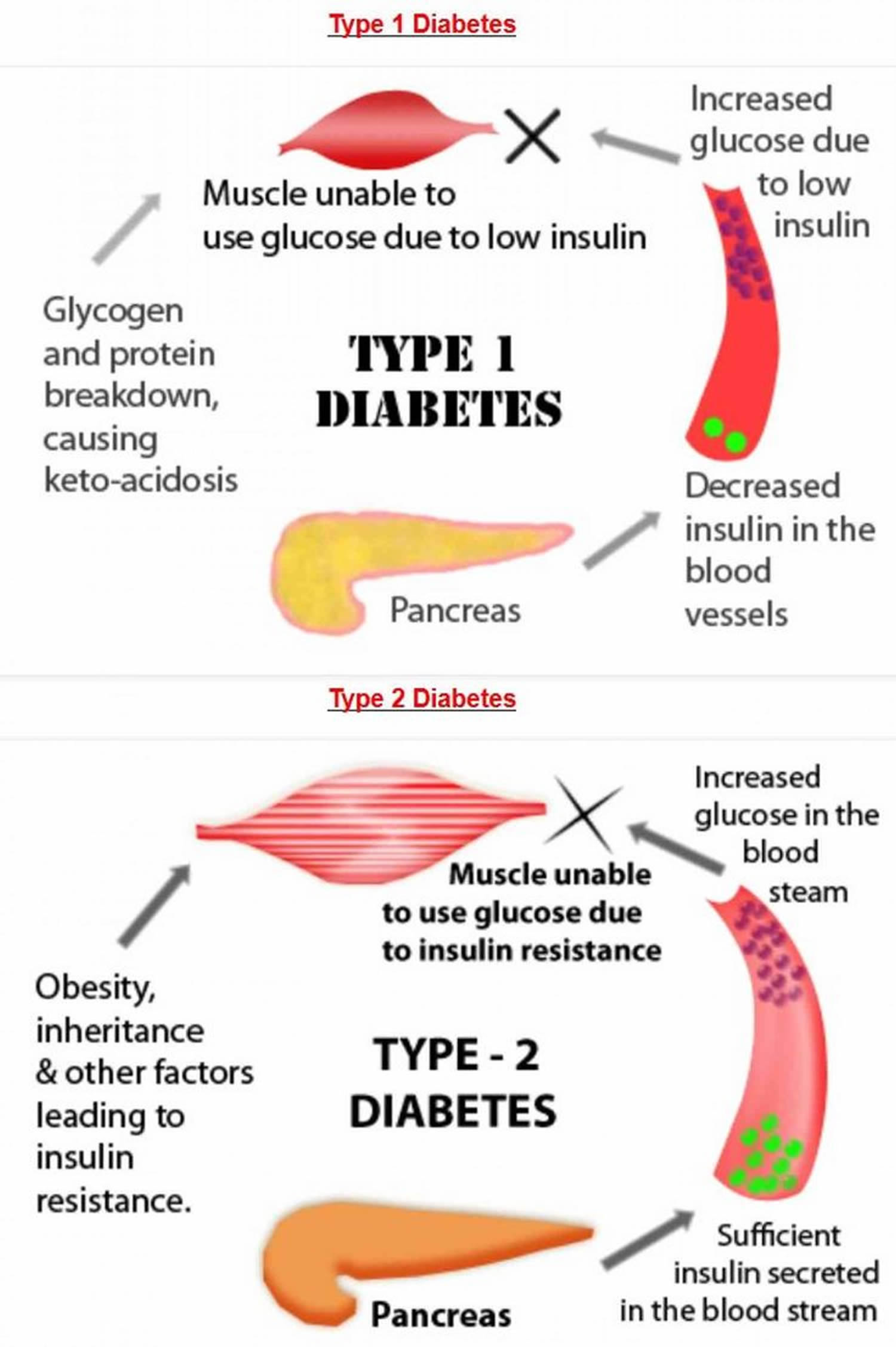
Type 2 diabetes develops when your body does not use insulin efficiently and gradually loses the ability to make enough insulin. In type 2 diabetes, there are primarily two interrelated problems at work – 1) your pancreas does not produce enough insulin and 2) your body’s cells respond poorly to insulin and take in less sugar. When you eat, your body breaks down sugar and starches from food into glucose to use for energy. Your pancreas (an organ behind your stomach) makes a hormone called insulin that controls the amount of glucose (sugar) in your blood. Insulin helps glucose (sugar) produced by the digestion of carbohydrates move from the blood into your body’s cells where it can be used for energy. When you have type 2 diabetes, your body doesn’t make enough insulin or can’t use insulin well, so you end up with too much sugar in your blood. In type 2 diabetes, the body’s cells do not respond effectively to insulin. This is known as insulin resistance, it causes glucose (sugar) to stay in your blood, leading to a higher than normal level of glucose in your blood (also known as hyperglycemia, usually above 7 mmol/L [126 mg/dL] before a meal and above 8.5 mmol/L [153 mg/dL] two hours after a meal) and not enough reaches your cells. The normal blood sugar level is between 4.0 mmol/L (72 mg/dL) and 5.5 mmol/L (99 mg/dL) when fasting (before meals), and less than 7.0 mmol/L [126 mg/dL] 2 hours after a meal. Eventually, high blood sugar levels can lead to serious health problems, like heart disease, kidney failure, blindness and disorders of the immune systems. People who have type 2 diabetes are also at greater risk of developing cardiovascular diseases such as heart attack, stroke or problems with circulation in their legs and feet (peripheral artery disease). These are the “macrovascular” complications of diabetes. “Macrovascular” means that these complications affect the larger blood vessels. This risk is especially high in people who also have high blood pressure.
Type 2 diabetes is the most common type of diabetes. More than 37 million Americans have diabetes (about 1 in 10), and approximately 90-95% of them have type 2 diabetes 1. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it.
Type 2 diabetes used to be referred to as “adult-onset” diabetes or or noninsulin-dependent diabetes mellitus (NIDDM) because it is often diagnosed later in life most often in middle-aged and older adults, but type 2 diabetes can appear in children, teens, and young people. More common in adults, type 2 diabetes increasingly affects children as childhood obesity increases.
With type 2 diabetes, your body either resists the effects of insulin — a hormone that regulates the movement of sugar into your cells — or doesn’t produce enough insulin to maintain a normal glucose level.
There’s no cure for type 2 diabetes, but losing weight and maintaining a healthy weight, eating well and exercising can help you manage the disease. If diet and exercise aren’t enough to manage your blood sugar well, you also may need diabetes medications or insulin therapy.
The severity of diabetes can vary quite a bit. Some people only have to make minor changes to their lifestyle after they are diagnosed. Just losing a little weight and getting some more exercise may be enough for them to manage their diabetes.
It also important to note that not everyone with type 2 diabetes is overweight, but weight gain and obesity are the most important risk factors for type 2 diabetes and the reason why type 2 has become a global epidemic that affects overweight people of all ages 2.
Other people who have type 2 diabetes need more permanent therapy that involves taking tablets or insulin. It is then especially important to have a good understanding of the disease and know what they can do to stay healthy 3.
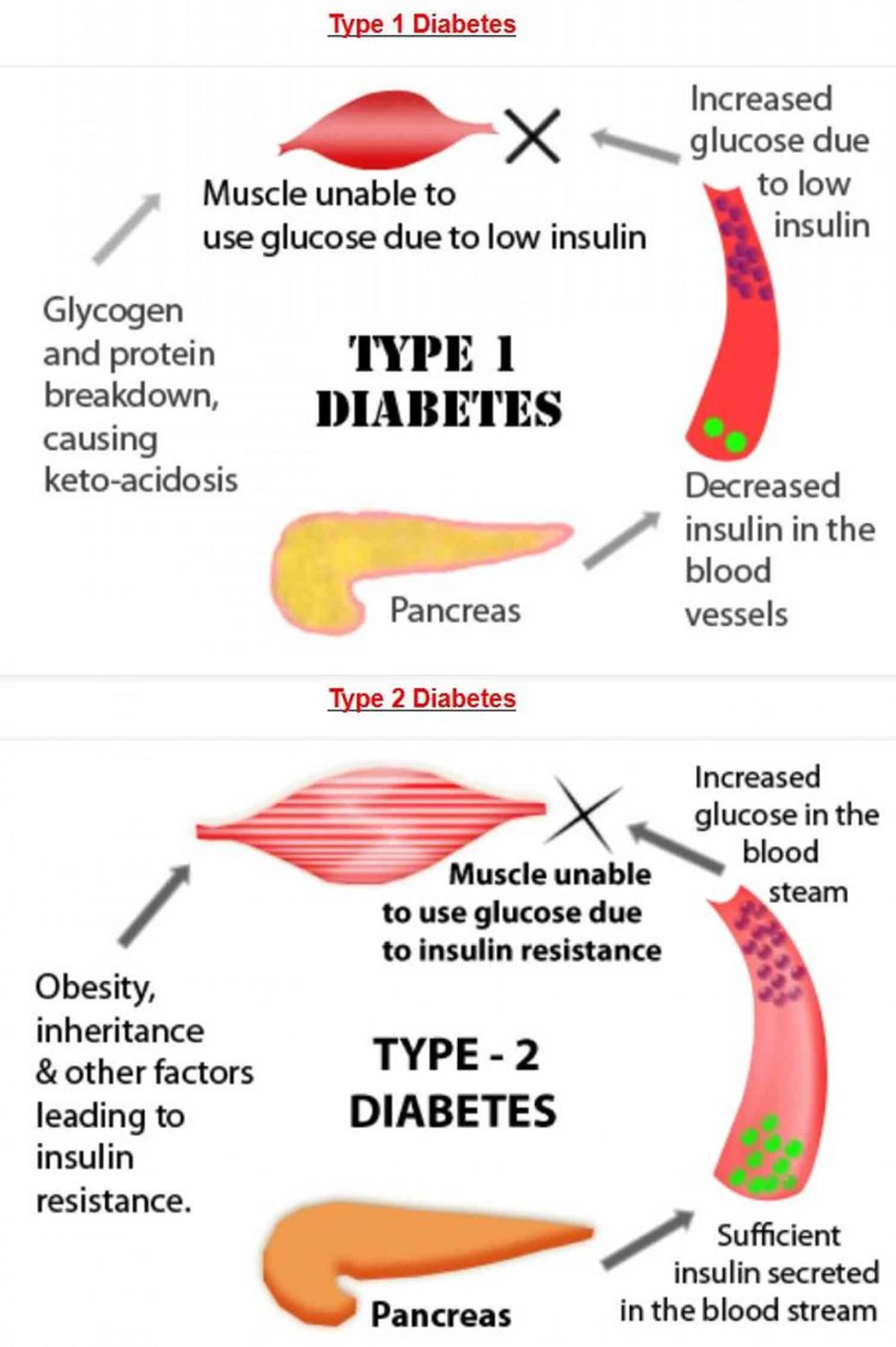
Figure 1. Type 2 diabetes
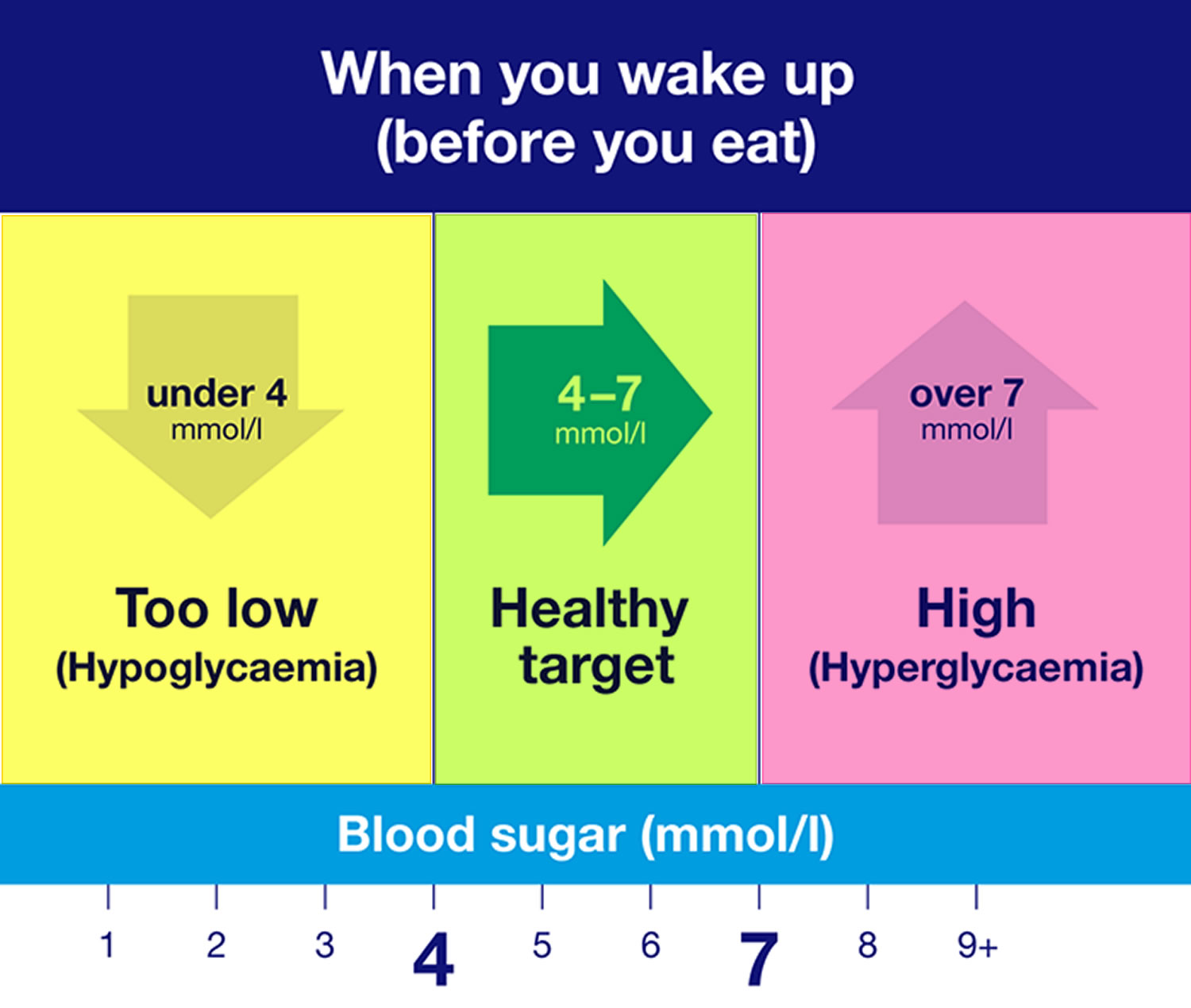
Figure 2. Blood sugar levels
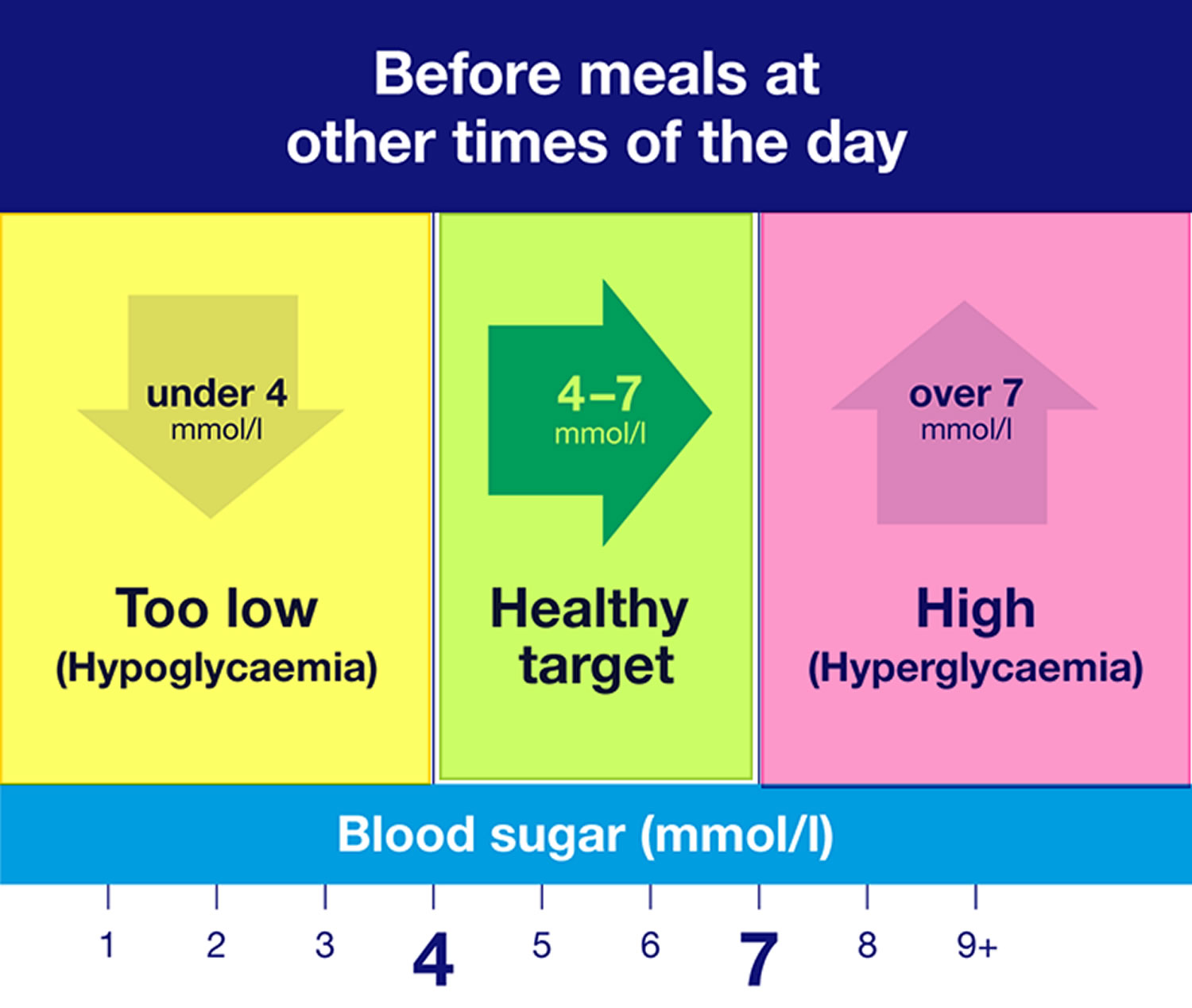
Footnotes: The images above show the general guidelines, but your individual target range for your blood sugar levels may be different. You’ll get different readings at different times of the day, depending on things like what you’ve eaten and how much you are moving around.
Figure 3. Type 2 diabetes blood sugar levels
Who is more likely to develop type 2 diabetes?
You can develop type 2 diabetes at any age, even during childhood. However, type 2 diabetes occurs most often in middle-aged and older people. You are more likely to develop type 2 diabetes if you are age 45 or older, have a family history of diabetes, or are overweight or have obesity. Diabetes is more common in people who are African American, Hispanic/Latino, American Indian, Asian American, or Pacific Islander.
Physical inactivity and certain health problems such as high blood pressure affect your chances of developing type 2 diabetes. You are also more likely to develop type 2 diabetes if you have prediabetes or had gestational diabetes when you were pregnant.
The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
- People younger than 35 who are overweight or obese and have one or more risk factors associated with diabetes
- Women who have had gestational diabetes
- People who have been diagnosed with prediabetes
- Children who are overweight or obese and who have a family history of type 2 diabetes or other risk factors
What is the difference between type 1 and type 2 diabetes?
The main difference between the type 1 and type 2 diabetes is that type 1 diabetes is a genetic condition that often shows up early in life, and type 2 is mainly lifestyle-related and develops over time. Type 1 diabetes is an auto-immune disease where your immune system is attacking and destroying the insulin-producing cells in your pancreas. In type 1 diabetes, people produce little or no insulin, as the insulin-producing cells have been destroyed by the body’s immune system. Approximately 5-10% of the people who have diabetes have type 1 diabetes. Currently, no one knows how to prevent type 1 diabetes.
In type 2 diabetes, the body may make enough insulin early in the disease, but doesn’t respond to it effectively. As type 2 diabetes progresses, the pancreas gradually loses the ability to produce enough insulin. Type 2 diabetes is associated with inherited factors and lifestyle risk factors such as being overweight or obese, poor diet, and insufficient physical activity. Type 2 diabetes most often develops in people over age 45, but more and more children, teens, and young adults are also developing it because the increase in the number of children with obesity.
Type 1 diabetes affects 8% of everyone with diabetes. While type 2 diabetes affects about 90% of people with diabetes.
Although type 1 and type 2 diabetes both have things in common, there are lots of differences. Like what causes them, who they affect, and how you should manage them.
A big difference between the two is that type 1 diabetes isn’t affected by your lifestyle. Or your weight. That means you can’t affect your risk of developing type 1 diabetes by lifestyle changes.
It’s different for type 2 diabetes. Scientists know some things put you at more risk:
- If you’re overweight or obese. Being overweight or obese is a main risk.
- Fat distribution. Storing fat mainly in your abdomen (waist size is too large) — rather than your hips and thighs — indicates a greater risk. Your risk of type 2 diabetes rises if you’re a man with a waist circumference above 40 inches (101.6 centimeters) or a woman with a measurement above 35 inches (88.9 centimeters).
- How to measure your waist: Find the top of your hip bone and the bottom of your ribcage. In the middle of these two points is where you need to measure. For many people, the belly button is a good guide, but this might not be the case for you, so it’s best to find that midpoint between your ribcage and hip. If you’re still not sure, watch the video below.
- What is a healthy waist size? This all depends on your gender and ethnicity. For a healthy measurement you need to aim to be less than:
- 80 cm (31.5 in) for all women
- 94 cm (37 in) for most men
- 90cm (35in) for South Asian men. This is because you have a higher risk of type 2 diabetes if you are of black or South Asian background.
- Inactivity. The less active you are, the greater your risk. Physical activity helps control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. The risk of type 2 diabetes increases if your parent, brother or sister has type 2 diabetes.
- Race and ethnicity. Although it’s unclear why, people of certain races and ethnicities — including African Caribbean, Black African, Hispanic, Native American and Asian people (Indian, Pakistani, Bangladeshi or Chinese), and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
- Blood lipid levels. An increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — and high levels of triglycerides.
- Age. You’re more at risk if you’re white and over 40, or over 25 if you’re African Caribbean, Black African, or South Asian (Indian, Pakistani or Bangladeshi).
- Medical history. For example if you have a history of high blood pressure, heart attack or strokes, gestational diabetes or severe mental illness.
- Prediabetes. Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes.
- Pregnancy-related risks. Your risk of developing type 2 diabetes increases if you developed gestational diabetes when you were pregnant or if you gave birth to a baby weighing more than 9 pounds (4 kilograms).
- Polycystic ovary syndrome (PCOS). Having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
- Smoking. Smoking is associated with a higher risk of type 2 diabetes, and also increases the risk of other health conditions such as heart disease and cancer.
- Areas of darkened skin, usually in the armpits and neck. This condition, called acanthosis nigricans. This condition often indicates insulin resistance. Acanthosis nigricans is most common in those who are overweight, have darker skin, and have diabetes or pre-diabetic conditions. Acanthosis nigricans is not contagious. It is not harmful. Acanthosis nigricans is a warning sign of a health problem that requires medical attention.
Scientists also know that there are things you can do to reduce your risk of developing type 2 diabetes. Things like eating healthily, being active and maintaining a healthy weight can help you to prevent type 2 diabetes.
Some people still get confused between type 1 and type 2 diabetes. Below is a guide to some of the main differences between type 1 and type 2 diabetes. The main thing to remember is that both are as serious as each other. Having high blood glucose (or sugar) levels can lead to serious health complications, no matter whether you have type 1 or type 2 diabetes. So if you have either condition, you need to take the right steps to manage it.
Table 1. Type 1 and type 2 diabetes differences
| Type 1 diabetes | Type 2 diabetes | |
|---|---|---|
| What is happening? | Your body attacks the cells in your pancreas which means it cannot make any insulin. | Your body is unable to make enough insulin or the insulin you do make doesn’t work properly. |
| Risk factors | Scientists don’t currently know what causes type 1 diabetes. | Scientists know some things can put you at risk of having type 2 like weight and ethnicity. |
| Symptoms | The symptoms for type 1 appear more quickly. | Type 2 symptoms can be easier to miss because they appear more slowly. |
| Management | Type 1 is managed by taking insulin to control your blood sugar. | You can manage type 2 diabetes in more ways than type 1. These include through medication, exercise and diet. People with type 2 can also be prescribed insulin. |
| Cure and Prevention | Currently there is no cure for type 1 but research continues. | Type 2 cannot be cured but there is evidence to say in many cases it can be prevented and put into remission. If you have obesity or overweight, your type 2 diabetes is more likely to go into remission if you lose a substantial amount of weight – 15kg (or 2 stone 5lbs) – as quickly and safely as possible following diagnosis. Type 2 diabetes remission is when your blood sugar levels are below the diabetes range and you don’t need to take diabetes medication anymore. Remission is when your HbA1c — a measure of long-term blood glucose levels — remains below 48mmol/mol or 6.5% for at least three months, without diabetes medication 4. |
If I’m overweight, will I always develop type 2 diabetes?
Being overweight is a risk factor for developing diabetes, but other risk factors such as how much physical activity you get, family history, ethnicity, and age also play a role. Unfortunately, many people think that weight is the only risk factor for type 2 diabetes, but many people with type 2 diabetes are at a normal weight or only moderately overweight.
Do sugary drinks cause diabetes?
Research has also shown that drinking sugary drinks is linked to type 2 diabetes. The American Diabetes Association recommends that people avoid drinking sugar-sweetened beverages and switch to water whenever possible to help prevent type 2 diabetes.
Sugary drinks also raise blood sugar and can provide several hundred calories in just one serving. Just one 12-ounce can of regular soda has about 150 calories and 40 grams of sugar, a type of carbohydrate (carb). This is the same as 10 teaspoons of sugar.
Sugar-sweetened beverages include beverages like:
- Regular soda
- Fruit punch
- Fruit drinks
- Energy drinks
- Sports drinks
- Sweet tea
- Sweetened coffee drinks
- Other sugary drinks
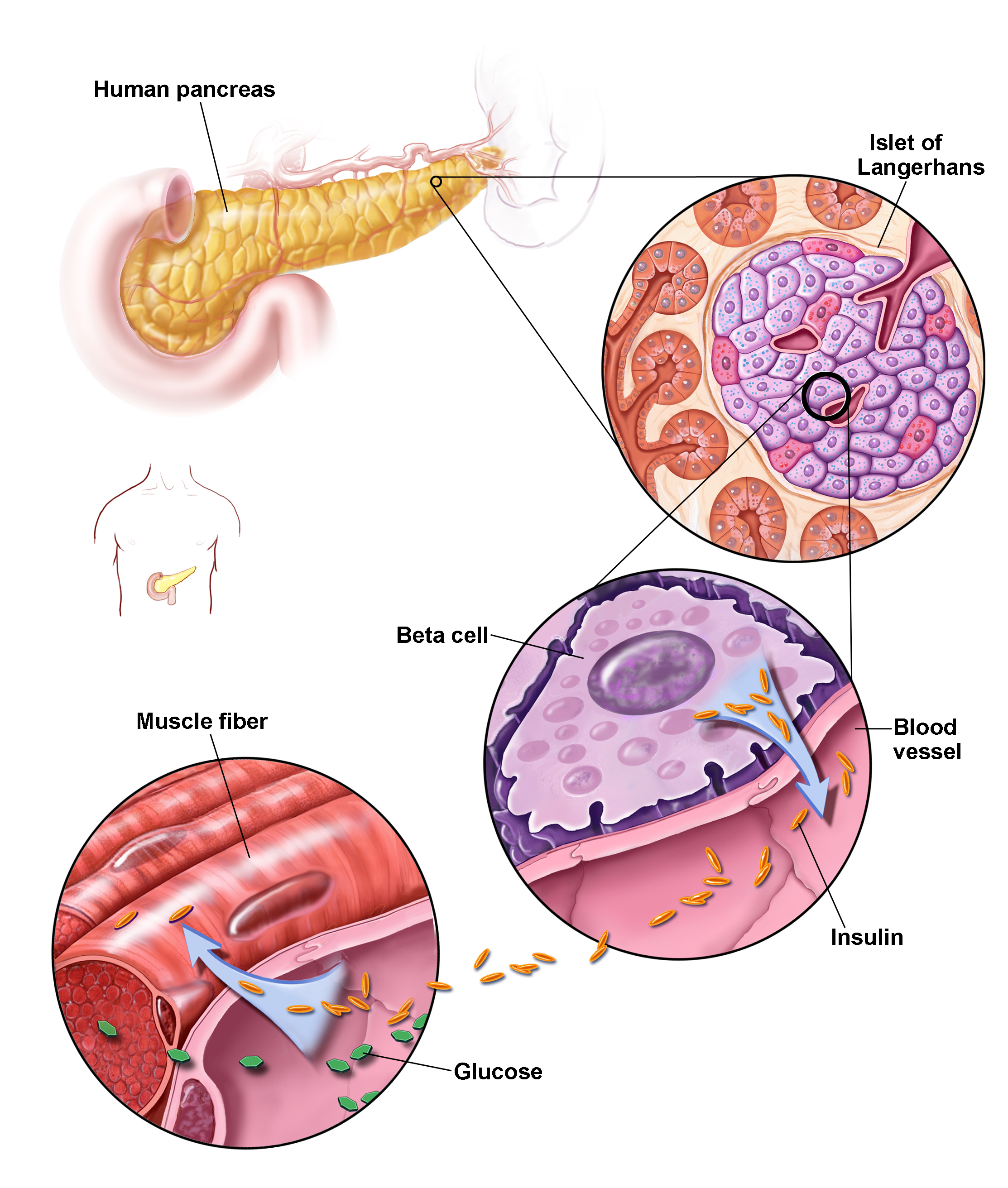
How does insulin work?
Insulin is a hormone that comes from the pancreas, a gland situated behind and below your stomach. Insulin regulates how your body uses sugar in the following ways:
- Sugar in the bloodstream triggers the pancreas to secrete insulin.
- Insulin circulates in the bloodstream, enabling sugar to enter your cells.
- The amount of sugar in your bloodstream drops.
- In response to this drop, the pancreas releases less insulin.
Is hyperinsulinemia a form of diabetes?
Hyperinsulinemia means the amount of insulin in your blood is higher than what’s considered healthy. On its own, hyperinsulinemia isn’t diabetes. But hyperinsulinemia often is associated with type 2 diabetes.
Insulin is a hormone that the pancreas makes. It helps control blood sugar. Hyperinsulinemia is connected to insulin resistance — a condition in which the body doesn’t respond as it should to the effects of insulin. In that situation, the pancreas makes more insulin in order to overcome the resistance, leading to higher levels of insulin in the blood. Type 2 diabetes develops when the pancreas can no longer make the large amounts of insulin needed to keep blood sugar at a healthy level.
Rarely, hyperinsulinemia is caused by:
- A tumor of the cells in the pancreas that make insulin. These tumors are called insulinomas.
- Too many cells in the pancreas that make insulin or too much growth of those cells. This condition is called nesidioblastosis.
Hyperinsulinemia usually doesn’t cause symptoms in people with insulin resistance. In people who have insulinomas, hyperinsulinemia may lead to low blood sugar, a condition called hypoglycemia.
Treatment of hyperinsulinemia is directed at the problem that’s causing it.
What are blood sugar levels?
Your blood sugar levels also known as blood glucose levels, are a measurement that show how much glucose (sugar) you have in your blood. Glucose is a sugar that you get from food and drink. Your blood sugar levels go up and down throughout the day and for people living with diabetes these changes are larger and happen more often than in people who don’t have diabetes.
Can I check my own blood sugar?
You can do blood sugar level check by doing a finger-prick test or by using an electronic blood sugar monitor called a flash glucose monitor. You can do this several times a day – helping you keep an eye on your levels as you go about your life and help you work out what to eat and how much medication to take. Find out your ideal target range.
Not everyone with diabetes needs to check their levels like this. You’ll need to if you take certain diabetes medication. Always talk to your healthcare team if you’re not sure whether that’s you – they’ll give you advice on whether to check them yourself and how often.
And there’s also something called an HbA1c, which is a blood test to measure your average blood sugar level over the last three months. Everyone with diabetes is entitled to this check.
High blood sugar levels increase your risk of developing serious complications. However you manage your diabetes, stay in the know about your blood sugar levels
Why test blood sugar levels?
Testing your blood sugar levels will help you stay healthy and prevent serious diabetes complications now and in the future. By complications, we mean serious problems in places like your feet and your eyes. This happens because too much sugar in the blood damages your blood vessels, making it harder for blood to flow around your body. This can lead to very serious problems like sight loss and needing an amputation.
Furthermore, if you take certain medication, like insulin or sulphonylureas, checking your blood sugars is a vital part of living with diabetes. It can help you work out when you need to take more medication, when you need to eat something or for when you want to get up and move around more.
Routine checks can help you know when you might be starting to go too low (called a hypoglycemia or hypo) or too high (called a hyperglycemia or hyper). It’s a way of getting to know your body and how it works. It can help you and your healthcare team spot patterns too. Do you write your results down? You might find that helpful.
What happens when my blood sugar levels are too high?
If your blood sugar levels are slightly above your targets, there are usually no symptoms. But if your blood sugar levels become too high, you may experience some symptoms associated with a hyperglycemia (or hyper). High blood sugar levels are usually considered hyperglycemia when they are above 15mmol/L (270 mg/dL). Hyperglycemia can be caused by not enough insulin, eating too much carbohydrate food, sickness or infection, stress or reduced physical activity.
The blood sugar level at which symptoms begin to appear is different for everyone, but the common symptoms include passing more urine than normal, being very thirsty, having headaches and feeling tired and lethargic.
Symptoms of hyperglycemia:
- Excessive thirst
- Lethargy
- Frequent urination
- Blurred vision
- Lack of concentration
- Change in behavior (usually irritable).
Over time, high blood glucose levels can lead to diabetes related complications. If your blood glucose levels are regularly above your target range, make an appointment to see your diabetes health team.
What happens when your blood sugar levels are too low?
Low blood sugar level also known as hypoglycemia, a ‘hypo’ or ‘low’, is when your blood glucose level is below 4 mmol/L (less than 72 mg/dL). Ask your doctor what’s considered a low blood sugar level for you. People taking insulin or certain types of diabetes medication are at risk of hypoglycemia. Hypos require immediate treatment with glucose to raise your blood glucose levels above 4mmol/L (above 72 mg/dL), otherwise your blood sugar levels will drop further. If this happens, you may experience a severe hypo and need emergency treatment.
Hypos can be caused by missing a meal, not eating enough carbohydrates for a given dose of insulin, unplanned physical activity, strenuous exercise, drinking alcohol, some medications or injecting too much insulin.
There are many different symptoms of a hypoglycemia, so it’s important that you are aware of the signs in case your blood sugar level gets too low. Test your blood sugar if you think your blood sugar levels are low. When in doubt, always test your blood sugar!
Symptoms of a hypo are:
- Weakness, trembling or shaking
- Sweating
- Light headedness/headache
- Lack of concentration or difficulty concentrating
- Behavior change
- Dizziness
- Tearfulness/crying
- Irritability or anxiety
- Tingling or numbness around the lips, tongue, cheek or fingers
- Hunger
- Looking pale (pallor)
- An irregular or fast heartbeat
- Feeling weak and having no energy (fatigue)
- Headache
Nighttime hypoglycemia may cause you to wake with sweat-soaked pajamas or a headache. Nighttime hypoglycemia sometimes might cause an unusually high blood sugar reading first thing in the morning.
If diabetic hypoglycemia isn’t treated, symptoms of hypoglycemia worsen and can include:
- Confusion, unusual behavior or both, such as the inability to complete routine tasks
- Loss of coordination
- Difficulty speaking or slurred speech
- Blurry or tunnel vision
- Inability to eat or drink
- Muscle weakness
- Drowsiness
Severe hypoglycemia may cause:
- Convulsions or seizures
- Unconsciousness
- Death, rarely
You can raise your blood sugar quickly by eating or drinking a simple sugar source, such as glucose tablets, hard candy or fruit juice. Tell family and friends what symptoms to look for and what to do if you’re not able to treat the condition yourself.
If a blood glucose meter isn’t readily available, treat for low blood sugar anyway if you have symptoms of hypoglycemia, and then test as soon as possible.
Inform people you trust about hypoglycemia. If others know what symptoms to look for, they might be able to alert you to early symptoms. It’s important that family members and close friends know where you keep glucagon and how to give it so that a potentially serious situation can be easier to safely manage. Glucagon is a hormone that stimulates the release of sugar into the blood.
Here’s some emergency information to give to others. If you’re with someone who is not responding (loses consciousness) or can’t swallow due to low blood sugar:
- Don’t inject insulin, as this will cause blood sugar levels to drop even further
- Don’t give fluids or food, because these could cause choking
- Give glucagon by injection or a nasal spray
- Call your local emergency services number in your area for immediate treatment if glucagon isn’t on hand, you don’t know how to use it or the person isn’t responding
Hypoglycemia unawareness
Some people may lose the ability to sense that their blood sugar levels are getting low. This is called hypoglycemia unawareness. The body no longer reacts to a low blood sugar level with symptoms such as lightheadedness or headaches. The more you experience low blood sugar, the more likely you are to develop hypoglycemia unawareness.
If you can avoid having a hypoglycemic episode for several weeks, you may start to become more aware of coming lows. Sometimes increasing the blood sugar target (for example, from 80 to 120 mg/DL to 100 to 140 mg/DL) at least for a short time can also help improve low blood sugar awareness.
Hypoglycemia treatment
Hypoglycemia is treated by having quick-acting glucose, such as Lucozade, 6 to 7 jellybeans, 3 teaspoons of honey, 100mls of full-strength soft drink or 150-200mls of fruit juice.
Wait 15 minutes, re-check your blood glucose levels to see if your blood glucose level has risen above 4mmol/L (above 72 mg/dL). If your blood glucose level is still below 4mmol/L (less than 72 mg/dL), repeat Step 1 by having another quick-acting glucose.
If your blood glucose level has risen above 4mmol/L, eat a snack or meal with longer acting carbohydrate such as a slice of bread, 1 glass of milk, 1 piece of fruit, 2-3 pieces of dried apricots, figs or other dried fruit OR 1 tub of natural low-fat yogurt.
It’s important to tell your family, friends and colleagues about hypos, how to recognize the symptoms when you’re hypoglycemic and how to treat it. Make sure they know to call your local emergency services number if you become unconscious, drowsy or unable to swallow, stating that it is a diabetes emergency.
It is important that your support person does not try to feed you; instead they should lay you on your side and check that your airway is clear. Then they should wait with you until the ambulance arrives. It is recommended that you wear a medical alert ID. This will help emergency services personnel to act appropriately and quickly.
What happens if I don’t treat hypoglycemia?
If not treated quickly, your blood glucose level can continue to drop, which may result in the brain not getting enough glucose. This can cause unconsciousness or fitting.
If a person with diabetes is unconscious, drowsy or unable to swallow: THIS IS AN EMERGENCY.
Do not give them any food or drink by mouth, treat as follows:
- Place them on their side making sure their airway is clear
- Give an injection of Glucagon if available and you are trained to give it
- Phone for an ambulance stating the person is unconscious AND that the person has diabetes
- Wait with them until the ambulance arrives.
Is there a cure for diabetes?
Unfortunately, there’s currently no permanent cure for either type 1 or type 2 diabetes, but scientists are working on a ground-breaking weight management study, to help people put their type 2 diabetes into remission. There’s evidence that some people with type 2 can put their diabetes into remission by losing weight. Following a very low-calorie diet under medical supervision, or having weight loss surgery (bariatric surgery) are some ways you can put your type 2 diabetes into remission. Remission is when blood glucose (or blood sugar) levels are in a normal range again. This doesn’t mean diabetes has gone for good. It’s still really important for people in remission to get regular healthcare checks. But being in remission can be life changing.
Is there a cure for type 1 diabetes?
In type 1 diabetes, insulin-producing beta cells in the pancreas are destroyed by the immune system. This means you can’t make the insulin you need to live. To stop type 1 diabetes scientists need to disrupt the immune system’s attack on beta cells. Currently scientists are working on it. They’re aiming to develop and test treatments – called immunotherapies – that target the immune system to stop it destroying beta cells.
Is diabetes a serious disease?
Yes. Diabetes causes more deaths per year than breast cancer and AIDS combined and having diabetes nearly doubles your chance of having a heart attack. The good news is that managing your diabetes can reduce your risk for diabetes complications.
Common diabetes health complications include heart disease, chronic kidney disease, nerve damage, and other problems with feet, oral health, vision, hearing, and mental health.
- Heart and blood vessel (cardiovascular) disease. Diabetes majorly increases the risk of many heart problems. These can include coronary artery disease with chest pain (angina), heart attack, stroke and narrowing of arteries (atherosclerosis). If you have diabetes, you’re more likely to have heart disease or stroke.
- Nerve damage (diabetic neuropathy). Too much sugar can injure the walls of the tiny blood vessels (capillaries) that nourish the nerves, especially in the legs. This can cause tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward. Damage to the nerves related to digestion can cause problems with nausea, vomiting, diarrhea or constipation. For men, it may lead to erectile dysfunction.
- Kidney damage (diabetic nephropathy). The kidneys hold millions of tiny blood vessel clusters (glomeruli) that filter waste from the blood. Diabetes can damage this delicate filtering system.
- Eye damage (diabetic retinopathy). Diabetes can damage the blood vessels of the eye (diabetic retinopathy). This could lead to blindness.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of many foot complications.
- Skin and mouth conditions. Diabetes may leave you more prone to skin problems, including bacterial and fungal infections.
- Hearing impairment. Hearing problems are more common in people with diabetes.
- Alzheimer’s disease. Type 2 diabetes may increase the risk of dementia, such as Alzheimer’s disease.
- Depression. Depression symptoms are common in people with type 1 and type 2 diabetes.
Do people with diabetes need to eat special foods?
No, you don’t need special food. Packaged foods with special “diabetes-friendly” claims may still raise blood glucose levels, be more expensive, and/or contain sugar alcohols that can have a laxative effect.
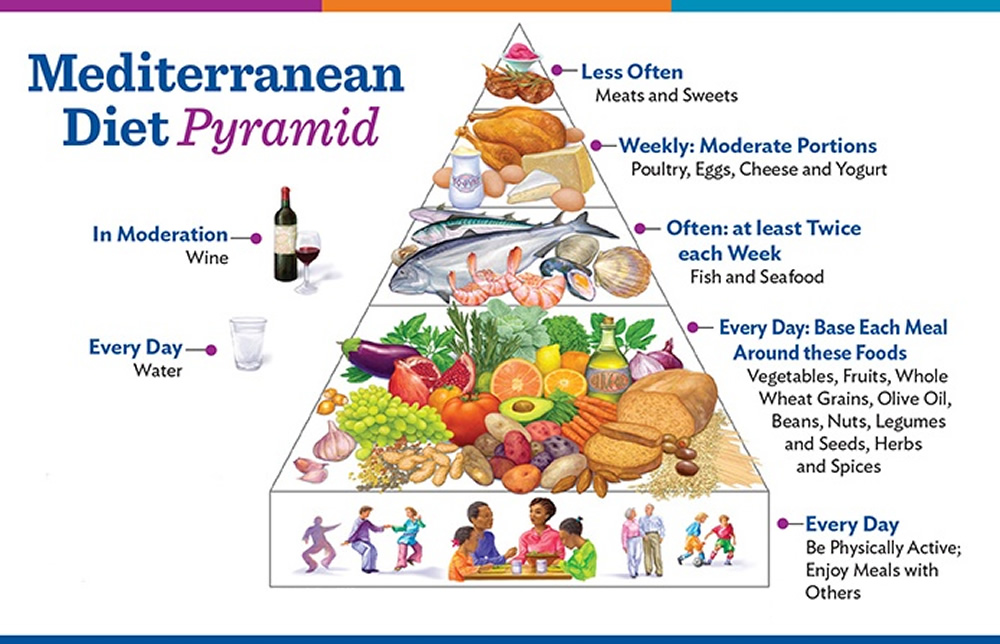
A healthy meal plan for people with diabetes is generally the same as healthy eating for anyone. In fact, there are a lot of different eating plans that can help you manage your diabetes. In general, a healthy eating plan for diabetes will include lots of non-starchy vegetables, limit added sugars, swap refined grains for whole grains and prioritize whole foods over highly processed foods when possible.
How to reverse type 2 diabetes?
The strongest evidence we have at the moment suggests that type 2 diabetes can be reversed or put into remission is by weight loss 5. If you have obesity or overweight, your diabetes is more likely to go into remission if you lose a substantial amount of weight – 15kg (or 2 stone 5lbs) – as quickly and safely as possible following diagnosis. Type 2 diabetes remission is when your blood sugar levels are below the diabetes range and you don’t need to take diabetes medication anymore. Remission is when your HbA1c — a measure of long-term blood glucose levels — remains below 48mmol/mol or 6.5% for at least three months, without diabetes medication 4. This definition has been agreed by a team of international experts at Diabetes UK, the American Diabetes Association and the European Association for the Study of Diabetes. Some people call this ‘reversing type 2 diabetes’, but experts use the term remission because your blood sugar levels can rise again and there’s no guarantee that your diabetes has gone forever. If your regular blood tests show your HbA1c remaining below 48 mmol/mol or 6.5%, talk to your healthcare team to discuss diabetes remission and how this applies to you. Remission is more likely if you lose weight as soon as possible after your diabetes diagnosis. However, scientists do know of people who have put their diabetes into remission 25 years after diagnosis.
There is no such thing as a special diet for people with diabetes or those aiming for diabetes reversal. There are a lot of different ways to lose weight – but there’s no one-size-fits-all diet. Some people have lost a substantial amount of weight and put their diabetes into remission through lifestyle and diet changes or by having weight loss surgery (called bariatric surgery). Scientists do know that some people have put their diabetes into remission by losing weight through following the Mediterranean diet or a low-carb diet 6, 7, 8.
It’s important to know that not everyone who loses this much weight will be able to put their diabetes into remission. But losing 15kg comes with a lot of health benefits, even if you don’t lead to remission. Research shows that getting support to lose just 5% of your body weight can have huge benefits for your health. People with obesity have an increased risk of serious health conditions, including heart attack, stroke and certain cancers. Research has shown that losing just 5% of your body weight can lead to:
- fewer medications
- better blood sugar levels
- lowering your blood pressure and cholesterol levels
- a lower risk of complications.
Scientists believe that just as storing fat around the liver and pancreas affects how type 2 diabetes develops, losing fat affects remission.
To understand how losing weight can help someone go into remission, you need to understand why obesity or overweight can lead to type 2 diabetes. If someone’s carrying extra weight around their waist, fat can build up around important organs like the liver and pancreas. This makes it more difficult for those organs to work properly, leading to type 2 diabetes.
But not everyone who develops type 2 diabetes lives with obesity or overweight. There are other factors, like age, ethnicity and family history that play a role in our risk of type 2 too. These factors influence how well the liver and pancreas work, and also where you store your fat. You can’t change those things, but you can usually change your weight.
Diabetes remission is quite a new idea. A lot of research is needed before we fully understand it. Diabetes experts don’t have enough evidence that remission is permanent. It needs to be maintained and in many cases, blood sugar levels can rise again, which is why it is so important to continue your diabetes appointments while in remission, because there’s always a chance that your diabetes might return. So, you’ll need ongoing support to keep an eye on your weight, and if it starts to creep up again, ask for extra support to adjust your eating pattern and activity levels.
You’ll also want to ensure that your HbA1c levels stay below 48 mmol/L or 6.5%.
Be sure to have regular health checks with your healthcare team at least once a year, including retinal screening. That way, your healthcare team can follow up on existing complications, pick up on new complications and give you support as soon as possible if your HbA1c levels go up again.
What is prediabetes?
Prediabetes means your blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes. Approximately 96 million American adults (18 and older), more than 1 in 3, have prediabetes. Of those with prediabetes, more than 80% don’t know they have it. Prediabetes puts you at increased risk of developing type 2 diabetes, heart disease, and stroke. Without lifestyle changes, a person with prediabetes is at high risk of going on to develop type 2 diabetes. People with prediabetes have up to a 50 percent chance of developing type 2 diabetes over the next 5 to 10 years. So if you’ve been told you have prediabetes, this is a warning sign that you are at high risk of developing type 2 diabetes. The good news is you don’t have it yet, and by making changes to your diet, increasing physical activity and losing weight, up to 50% of cases of type 2 diabetes can be prevented or delayed in some people.
If you have prediabetes, losing a small amount of weight if you’re overweight and getting regular physical activity can lower your risk for developing type 2 diabetes. A small amount of weight loss means around 5% to 7% of your body weight or just 10 to 14 pounds for a 200-pound person can significantly reduce your risk. There are lots of ways you can lose weight and it’s about finding what works best for you. If you need help with managing your weight, a dietitian can help you.
Regular physical activity means getting at least 150 minutes a week of brisk walking or a similar activity. That’s just 30 minutes a day, five days a week.
Making healthier food choices and being more active are both positive ways to start making positive changes that will benefit your health.
Healthy lifestyle choices can help you prevent prediabetes and its progression to type 2 diabetes, even if diabetes runs in your family. Try to:
- Eat healthy foods
- Get at least 150 minutes of moderate aerobic physical activity a week, or about 30 minutes on most days of the week
- Lose excess weight
- Control your blood pressure and cholesterol
- Don’t smoke
What causes prediabetes?
Insulin is a hormone made by your pancreas beta cells that acts like a key to let blood sugar into cells for use as energy. If you have prediabetes, the cells in your body don’t respond normally to insulin (insulin resistance). Your pancreas makes more insulin to try to get cells to respond. Eventually your pancreas can’t keep up, and your blood sugar rises, setting the stage for prediabetes and type 2 diabetes down the road.
Researchers don’t fully understand what causes insulin resistance and prediabetes, but they think excess weight and lack of physical activity are major factors.
Excess weight
Experts believe obesity, especially too much fat in the abdomen and around the organs, called visceral fat, is a main cause of insulin resistance. A waist measurement of 40 inches or more for men and 35 inches or more for women is linked to insulin resistance. This is true even if your body mass index (BMI) falls within the normal range. However, research has shown that Asian Americans may have an increased risk for insulin resistance even without a high BMI.
Researchers used to think that fat tissue was only for energy storage. However, studies have shown that belly fat makes hormones and other substances that can contribute to chronic, or long-lasting, inflammation in the body. Inflammation may play a role in insulin resistance, type 2 diabetes, and cardiovascular disease.
Excess weight may lead to insulin resistance, which in turn may play a part in the development of fatty liver disease.
Physical inactivity
Not getting enough physical activity is linked to insulin resistance and prediabetes. Regular physical activity causes changes in your body that make it better able to keep your blood glucose levels in balance.
How do I prevent getting prediabetes?
Physical activity and losing weight may help your body respond better to insulin. Taking small steps, such as eating healthier foods and moving more to lose weight, can help reverse insulin resistance and prevent or delay type 2 diabetes in people with prediabetes.
The Diabetes Prevention Program research studies 9, 10, showed that for people at high risk of developing diabetes, losing 5 to 7 percent of their starting weight helped reduce their chance of developing the disease 10. That’s 10 to 14 pounds for someone who weighs 200 pounds. People in the study lost weight by changing their diet and being more physically active.
The Diabetes Prevention Program research studies 9, 10 also showed that taking metformin, a medicine used to treat type 2 diabetes, could delay diabetes. Metformin worked best for women with a history of gestational diabetes, younger adults, and people with obesity. Ask your doctor if metformin might be right for you.
What are prediabetes signs and symptoms?
You can have prediabetes for years but have no clear symptoms, so it often goes undetected until serious health problems such as type 2 diabetes show up. Some people with prediabetes may have darkened skin in the armpit or on the back and sides of the neck, a condition called acanthosis nigricans. Many small skin growths called skin tags often appear in these same areas. Even though blood glucose levels are not high enough to cause symptoms for most people, a few research studies have shown that some people with prediabetes may already have early changes in their eyes that can lead to retinopathy. This problem more often occurs in people with diabetes. It’s important to talk to your doctor about getting your blood sugar tested if you have any of the risk factors for prediabetes, which include:
- Being overweight
- Being 45 years or older
- Having a parent, brother, or sister with type 2 diabetes
- Being physically active less than 3 times a week
- Ever having gestational diabetes (diabetes during pregnancy) or giving birth to a baby who weighed more than 9 pounds
- Having polycystic ovary syndrome (PCOS)
- People who have metabolic syndrome (a combination of high blood pressure, abnormal cholesterol levels, and large waist size) are more likely to have prediabetes.
Race and ethnicity are also a factor: African Americans, Hispanic/Latino Americans, American Indians, Pacific Islanders, and some Asian Americans are at higher risk.
Along with these risk factors, other things that may contribute to insulin resistance include:
- certain medicines, such as glucocorticoids, some antipsychotics, and some medicines for HIV
- hormonal disorders, such as Cushing’s syndrome and acromegaly
- sleep problems, especially sleep apnea
Although you can’t change risk factors such as family history, age, or ethnicity, you can change lifestyle risk factors around eating, physical activity, and weight. These lifestyle changes can lower your chances of developing insulin resistance or prediabetes.
Complications of Prediabetes
People with prediabetes may already have damage to their eyes, kidneys, blood vessels, and heart. Evidence from numerous studies suggests that the chronic complications of type 2 diabetes start to develop during the prediabetic state. So by the time we have prediabetes, it may already too late to prevent organ damage, so best to prevent prediabetes in the first place, and the earlier the better.
The most serious consequence of prediabetes is progression to type 2 diabetes. That’s because type 2 diabetes can lead to:
- High blood pressure
- High cholesterol
- Heart disease
- Stroke
- Kidney disease
- Blindness
- Amputations
Research indicates that prediabetes is often associated with heart attacks and can damage your kidneys, even if you haven’t progressed to type 2 diabetes.
How is prediabetes diagnosed?
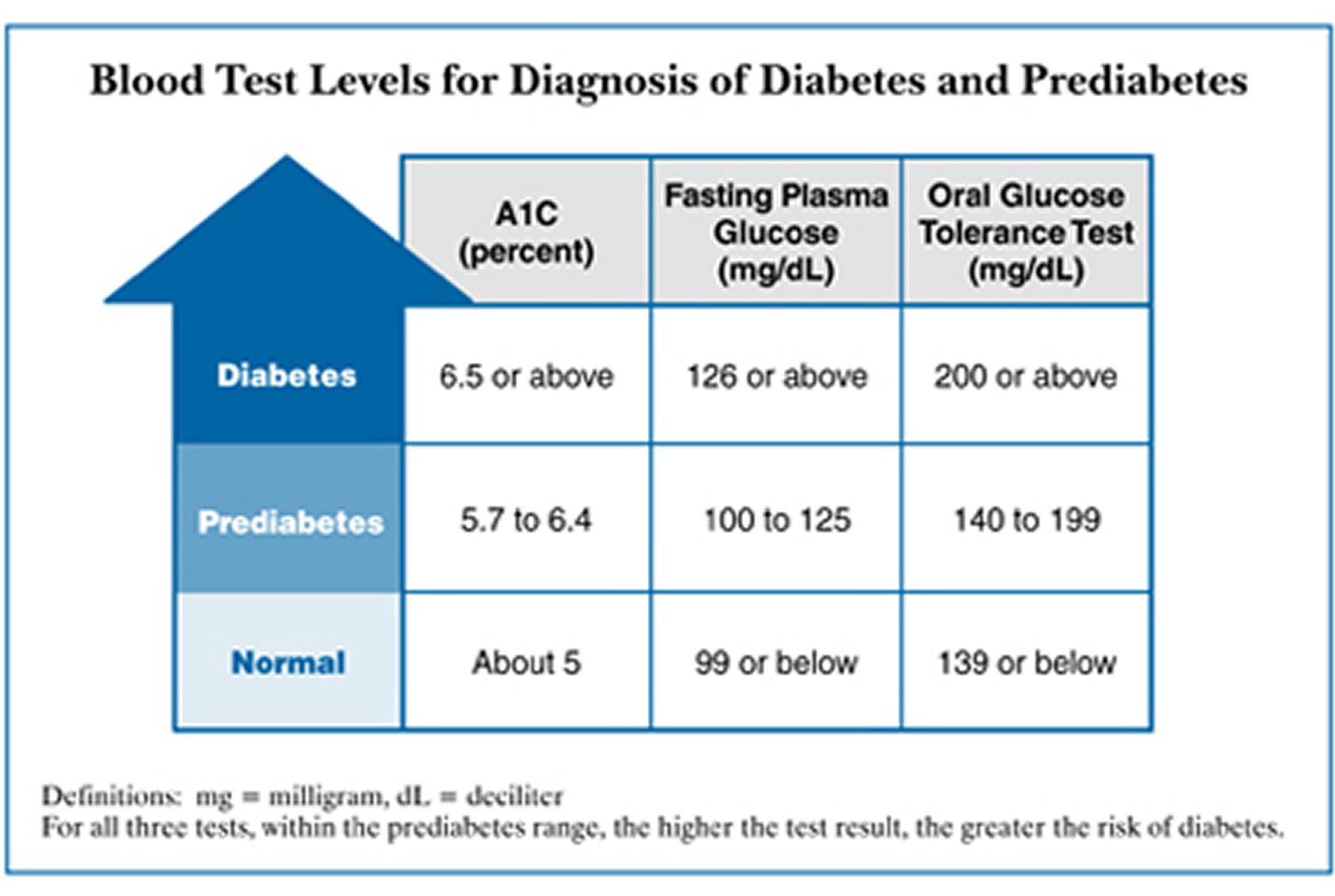
Doctors most often use the fasting plasma glucose (FPG) test or the A1C (HbA1C) test to find out if someone has prediabetes. Less often, doctors use the oral glucose tolerance test (OGTT), which is more expensive and not as easy to give.
Doctors don’t usually test for insulin resistance. The most accurate test for insulin resistance is complicated and used mostly for research.
You should be tested for prediabetes if you are overweight or have obesity and have one or more other risk factors for diabetes, or if your parents, siblings, or children have type 2 diabetes. Even if you don’t have risk factors, you should start getting tested once you reach age 45.
The following test results show prediabetes 11:
- A1C (HbA1C): 5.7 to 6.4 percent
- Fasting plasma glucose (FPG): 100 to 125 mg/dL (5.6 to 6.9 mmol/L)
- Oral glucose tolerance test (OGTT): 140 to 199 mg/dL (7.8 to 11.1 mmol/L)
If the results are normal but you have other risk factors for diabetes, you should be retested at least every 3 years (testing might occur more frequently if you have additional risk factors for diabetes) 11.
Prediabetes treatment
Healthy lifestyle choices can help you bring your blood sugar level back to normal, or at least keep it from rising toward the levels seen in type 2 diabetes.
To prevent prediabetes from progressing to type 2 diabetes, try to:
- Eat healthy foods. Choose foods low in fat and calories and high in fiber. Focus on fruits, vegetables and whole grains. Strive for variety to help you achieve your goals without compromising taste or nutrition.
- Be more active. Aim for 30 to 60 minutes of moderate physical activity most days of the week.
- Lose excess weight. If you’re overweight, losing just 5 to 10 percent of your body weight — only 10 to 20 pounds (4.5 to 9 kilograms) if you weigh 200 pounds (91 kilograms) — can reduce the risk of developing type 2 diabetes. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits. Motivate yourself by remembering the benefits of losing weight, such as a healthier heart, more energy and improved self-esteem.
- Stop smoking.
- Take medications as needed. If you’re at high risk of diabetes, your doctor might recommend metformin (Glucophage, others). Medications to control cholesterol and high blood pressure might also be prescribed.
Alternative medicine
Many alternative therapies have been touted as possible ways to treat or prevent type 2 diabetes, including:
- Banaba
- Cassia cinnamon
- Fenugreek
- Ginseng
- Gymnema
- Mangesium
- White mulberry
Although some of these substances have shown promise in early trials, there’s no definitive evidence that any of these alternative therapies are effective.
Talk to your doctor if you’re considering dietary supplements or other alternative therapies to treat or prevent prediabetes. Some of these supplements or alternative therapies might be harmful if combined with certain prescription medications. Your doctor can help you weigh the pros and cons of specific alternative therapies.
Children and prediabetes treatment
Children with prediabetes should undertake the lifestyle changes recommended for adults with type 2 diabetes, including:
- Medication generally isn’t recommended for children with prediabetes.
- Losing weight.
- Eating fewer refined carbohydrates and fats, and more fiber.
- Spending at least one hour every day in physical activity.
Type 2 diabetes and pregnancy
Preexisting diabetes also called pregestational diabetes means you have diabetes before you get pregnant. This is different from gestational diabetes, which is a kind of diabetes that some women get during pregnancy. In the United States, about 1 to 2 percent of pregnant women have preexisting diabetes. The number of women with diabetes during pregnancy has increased in recent years. High blood sugar can be harmful to your baby during the first few weeks of pregnancy when his brain, heart, kidneys and lungs begin to form. There is a chance that some of the potential complications of diabetes, like eye disease (diabetic retinopathy) and kidney disease (diabetic nephropathy), may develop while you are pregnant. Your doctors will keep an eye on this. If you are pregnant or planning a pregnancy, visit an ophthalmologist during each trimester of your pregnancy, one year postpartum or as advised. There is also a risk of developing pre-eclampsia, a condition involving high blood pressure during pregnancy, which can cause problems for the baby.
If you have type 1 or type 2 diabetes and are planning a family, you should plan your pregnancy as much as possible. Controlling your blood sugars before conception and throughout pregnancy gives you the best chance of having a trouble-free pregnancy and birth and a healthy baby. Most women with diabetes have a healthy baby.
Having diabetes means that you and your baby are more at risk of serious health complications during pregnancy and childbirth. The good news is that by planning ahead and getting support from your doctor and diabetes team, you can really reduce the risks involved. So you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby.
If you have diabetes and your pregnancy is unplanned, there’s still plenty you can do to give your baby the best start in life.
Women with type 2 diabetes will likely need to change their treatment plans and adhere to diets that carefully controls carbohydrate intake. Many women will need insulin therapy during pregnancy and may need to discontinue other treatments, such as blood pressure medications.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of signs and symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar (hyperglycemia). Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Signs and symptoms include:
- Frequent urination
- Increased thirst
- Dry mouth
- Blurred vision
- Fatigue
- Headache
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L). Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Signs and symptoms of hyperglycemic hyperosmolar nonketotic syndrome (HHNS) include:
- Dry mouth
- Extreme thirst
- Drowsiness
- Confusion
- Dark urine
- Seizures
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medications — including the diabetes medications called SGLT2 inhibitors.
Although diabetic ketoacidosis is usually less severe in type 2 diabetes, the toxicity of the acids can be life-threatening. In addition to the signs and symptoms of low blood sugar (hypoglycemia), such as frequent urination and increased thirst, ketoacidosis may result in:
- Nausea
- Vomiting
- Abdominal pain
- Shortness of breath
- Fruity-smelling breath
Low blood sugar (hypoglycemia). If your blood sugar level drops below your target range, it’s known as low blood sugar (hypoglycemia). Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physical activity than usual. Signs and symptoms include:
- Sweating
- Shakiness
- Weakness
- Hunger
- Irritability
- Dizziness
- Headache
- Blurred vision
- Heart palpitations
- Slurred speech
- Drowsiness
- Confusion
If you have signs or symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level — fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, repeat the sugar intake. Eat a meal after levels return to normal.
If you lose consciousness, you will need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
What is gestational diabetes?
Gestational diabetes also called gestational diabetes mellitus (GDM) is a type of diabetes that some women get during pregnancy who don’t already have diabetes. Diabetes is a condition in which your body has too much sugar (also called glucose) in your blood. As gestational diabetes is a condition that occurs during pregnancy, it is not the same as having pre-existing diabetes during your pregnancy. Gestational diabetes occurs when your body can’t make enough insulin during your pregnancy. Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into the cells in your body for use as energy. This leads to higher than normal levels of sugar in the blood, which can be unhealthy for both you and the baby. Typically, women with gestational diabetes have no symptoms. Your medical history and whether you have any risk factors may suggest to your doctor that you could have gestational diabetes, but you’ll need to be tested to know for sure. Most women are diagnosed after routine tests during pregnancy. Most pregnant women get tested for gestational diabetes at 24 to 28 weeks of pregnancy.
During pregnancy, your body makes more hormones and goes through other changes, such as weight gain. These changes cause your body’s cells to use insulin less effectively, a condition called insulin resistance. Insulin resistance increases your body’s need for insulin.
All pregnant women have some insulin resistance during late pregnancy. However, some women have insulin resistance even before they get pregnant. They start pregnancy with an increased need for insulin and are more likely to have gestational diabetes.
Every year, 7 out of every 100 pregnancies in the United States are affected by gestational diabetes. You’re more likely than other women to have gestational diabetes (GDM) if you’re Asian, South Asian, African-American or African Caribbean, Middle Eastern, Native American, Hispanic or Pacific Islander.
Most of the time it can be controlled and treated during pregnancy. If it’s not treated, gestational diabetes can cause problems for you and your baby.
Having gestational diabetes increases your risk of developing it again in future pregnancies. It also increases your risk of developing type 2 diabetes after giving birth or later in life.
Babies born to women with diabetes are at risk of being born larger than average, or with a birth defect. They may also be born prematurely or even stillborn. They are also at risk of becoming overweight and going on to develop type 2 diabetes as an adult.
These risks are greatly reduced if you keep your blood sugars under good control.
Managing gestational diabetes will help make sure you have a healthy pregnancy and a healthy baby. This will include eating well and keeping active.
Gestational diabetes usually goes away after you have your baby.
If I have gestational diabetes, how can I prevent getting diabetes later in life?
For most people, gestational diabetes goes away after giving birth. But having it makes you more likely to develop type 2 diabetes later in life. Type 2 diabetes is the most common kind of diabetes.
Here’s what you can do to help reduce your risk of developing type 2 diabetes after pregnancy:
- Get tested for diabetes 4 to 12 weeks after your baby is born. If the test is normal, get tested again every 1 to 3 years.
- Get to and stay at a healthy weight.
- Talk to your provider about medicine that may help prevent type 2 diabetes.
Can gestational diabetes increase my risk for problems during pregnancy?
Yes. If not treated, gestational diabetes can increase your risk for pregnancy complications and procedures, including:
- Macrosomia. This means your baby weighs more than 8 pounds, 13 ounces (4,000 grams) at birth. Babies who weigh this much are more likely to be hurt during labor and birth, and can cause damage to his or her mother during delivery.
- Shoulder dystocia or other birth injuries (also called birth trauma). Complications for birthing parents caused by shoulder dystocia include postpartum hemorrhage (heavy bleeding). For babies, the most common injuries are fractures to the collarbone and arm and damage to the brachial plexus nerves. These nerves go from the spinal cord in the neck down the arm. They provide feeling and movement in the shoulder, arm and hand.
- High blood pressure and preeclampsia. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy. Preeclampsia is when a pregnant person has high blood pressure and signs that some of their organs, such as the kidneys and liver, may not be working properly.
- Perinatal depression. This is depression that happens during pregnancy or in the first year after having a baby (also called postpartum depression). Depression is a medical condition that causes feelings of sadness and a loss of interest in things you like to do. It can affect how you think, feel, and act and can interfere with your daily life.
- Preterm birth. This is birth before 37 weeks of pregnancy. Most women who have gestational diabetes have a full-term pregnancy that lasts between 39 and 40 weeks. However, if there are complications, your health care provider may need to induce labor before your due date. This means your provider will give you medicine or break your water (amniotic sac) to make your labor begin.
- Stillbirth. This is the death of a baby after 20 weeks of pregnancy.
- Cesarean birth also called C-section. This is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus. You may need to have a c-section if you have complications during pregnancy, or if your baby is very large (also known as macrosomia). Most people who have gestational diabetes can have a vaginal birth. But they’re more likely to have a c-section than people who don’t have gestational diabetes.
Gestational diabetes also can cause health complications for your baby after birth, including:
- Breathing problems, including respiratory distress syndrome. This can happen when babies don’t have enough surfactant in their lungs. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing.
- Jaundice. This is a medical condition in which the baby’s liver isn’t fully developed or isn’t working well. A jaundiced baby’s eyes and skin look yellow.
- Low blood sugar (hypoglycemia)
- Obesity later in life
- Diabetes later in life
What causes gestational diabetes?
Scientists believe gestational diabetes, a type of diabetes that develops during pregnancy, is caused by the hormonal changes of pregnancy along with genetic and lifestyle factors.
When you are pregnant, your placenta produces hormones to help the baby grow. Pregnancy hormones you produce block the action of insulin in your body (called insulin resistance). This puts you at an increased risk of insulin resistance, and some women can’t produce enough insulin to overcome it. This makes it difficult to use glucose (sugar) properly for energy, so it stays in your blood and the sugar levels rise. This then leads to gestational diabetes.
- Insulin resistance: Hormones produced by the placenta contribute to insulin resistance, which occurs in all women during late pregnancy. Most pregnant women can produce enough insulin to overcome insulin resistance, but some cannot. Gestational diabetes occurs when the pancreas can’t make enough insulin.
- Extra weight is linked to gestational diabetes. Women who are overweight or obese may already have insulin resistance when they become pregnant. Gaining too much weight during pregnancy may also be a factor.
- Genes and family history: Having a family history of diabetes makes it more likely that a woman will develop gestational diabetes, which suggests that genes play a role. Genes may also explain why the disorder occurs more often in African Americans, American Indians, Asians, and Hispanics/Latinas.
You are at higher risk of developing gestational diabetes if you:
- are overweight or obese and not physically active or gaining too much weight in the first half of pregnancy
- are over the age of 35 years
- have a family history (parent, brother or sister) of type 2 diabetes
- come from a racial or ethnic group that has a higher prevalence of diabetes that isn’t entirely explained by race or ethnicity, such as Black, American Indian, Alaska Native, Asian, Hispanic/Latino or Pacific Islander
- have had gestational diabetes before
- have prediabetes. This means your blood glucose levels are higher than normal but not high enough to be diagnosed with diabetes.
- have had polycystic ovary syndrome (PCOS). This is a hormone problem that can affect reproductive and overall health.
- have had a large baby (macrosomia) in a past pregnancy
- are taking some types of anti-psychotic or steroid medications
- have high blood pressure or you’ve had heart disease.
Gestational diabetes symptoms
Many women with gestational diabetes have no noticeable symptoms.
As some of the signs of diabetes are like symptoms experienced in pregnancy anyway – like feeling more tired or going to the toilet more – most gestational diabetes cases are diagnosed during screening for gestational diabetes. This is called a Glucose Tolerance Test, also known as an Oral Glucose Tolerance Test (OGTT).
What are complications of gestational diabetes?
Most women who have gestational diabetes deliver healthy babies. However, untreated or uncontrolled blood sugar levels can cause problems for you and your baby.
Complications in your baby can be caused by gestational diabetes, including:
- Excess growth (also known as macrosomia). Extra glucose can cross the placenta. Extra glucose triggers the baby’s pancreas to make extra insulin. This can cause your baby to grow too large. It can lead to a difficult birth and sometimes the need for a C-section.
- Low blood sugar (hypoglycemia). Sometimes babies of mothers with gestational diabetes develop low blood sugar (hypoglycemia) shortly after birth. This is because their own insulin production is high.
- Type 2 diabetes later in life. Babies of mothers who have gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.
- Death. Untreated gestational diabetes can lead to a baby’s death either before or shortly after birth.
Complications in the mother also can be caused by gestational diabetes, including:
- Preeclampsia. Symptoms of this condition include high blood pressure, too much protein in the urine, and swelling in the legs and feet.
- Gestational diabetes. If you had gestational diabetes in one pregnancy, you’re more likely to have it again with the next pregnancy.
How is gestational diabetes diagnosed?
All women are tested for gestational diabetes, usually at 24 to 28 weeks of pregnancy. If you are at higher risk, you may be tested earlier.
The test for gestational diabetes is called an ‘oral glucose tolerance test’ (OGTT). You need to fast for 10 hours (generally overnight, missing breakfast). A blood test is taken, followed by a 75g glucose drink and further blood tests at 1 and 2 hours later. You will be required to remain at the laboratory for the 2-hour test.
Taking a Oral Glucose Tolerance Test
Your test preparation depends on whether a one-step or two-step glucose tolerance test is done. American College of Obstetricians and Gynecologists (ACOG) and the National Institutes of Health (NIH) consensus conference currently recommend the two-step approach, while the Endocrine Society recommends the one-step approach, and the American Diabetes Association (ADA) says either the one-step or two-step approach is appropriate.
- One-step 2-hour oral glucose tolerance test: you will need to fast (usually overnight) before an initial blood sample is drawn. You will then be given a 75-gram dose of glucose to drink and your blood will be drawn at 1 hour and 2 hours after the dose. Only one of the values (including the fasting glucose level) needs to be above a cutoff value for diagnosis of diabetes to be made.
- Two-step oral glucose tolerance test:
- Glucose challenge test: you do not need to fast. You will be given a 50-gram glucose dose to drink and your blood is drawn after 1 hour.
- If the challenge test is abnormal, a 3-hour oral glucose tolerance test will be performed. You will need to fast before an initial blood sample is drawn. Then you will be given a 100-gram glucose dose and your blood drawn at 1 hour, 2 hours, and 3 hours after the dose. If at least 2 of the glucose levels at fasting, 1 hour, 2 hours, or 3 hours are above a certain level, then a diagnosis of gestational diabetes is made.
The following tables summarize the meaning of gestational diabetes glucose tolerance testing results.
Table 2. Gestational Diabetes One-Step Approach test results
| Time of sample collection | Glucose level |
|---|---|
| Fasting | Equal to or greater than 92 mg/dL (5.1 mmol/L) |
| 1 hour | Equal to or greater than 180 mg/dL (10.0 mmol/L) |
| 2 hour | Equal to or greater than 153 mg/dL (8.5 mmol/L) |
Footnote: Samples drawn fasting and then 1 hour and 2 hours after a 75-gram glucose drink. Diagnosis of gestational diabetes is made when any of the values meet or exceed the limit.
Table 3. Gestational Diabetes Two-Step Approach: Step One (Glucose Challenge Screen) test results
| Glucose Level | Interpretation |
|---|---|
| Less than 140* mg/dL (7.8 mmol/L) | Normal screen |
| 140* mg/dL (7.8 mmol/L) or greater | Abnormal, needs OGTT (see Step Two below) |
Footnote: Sample drawn 1 hour after a 50-gram glucose drink. *Some experts recommend a cutoff of 130 mg/dL (7.2 mmol/L) because that identifies 90% of women with gestational diabetes, compared to 80% identified using the threshold of 140 mg/dL (7.8 mmol/L). The American College of Obstetricians and Gynecologists (ACOG) recommends a lower threshold of 135 mg/dL (7.5 mmol/L) in high-risk ethnic groups with higher prevalence of gestational diabetes.
Table 4. Gestational Diabetes Two-Step Approach: Step Two (Diagnostic OGTT) test results
| Time of sample collection | Target levels** |
|---|---|
| Fasting (prior to glucose load) | 95 mg/dL (5.3 mmol/L) |
| 1 hour after glucose load | 180 mg/dL (10.0 mmol/L) |
| 2 hours after glucose load | 155 mg/dL (8.6 mmol/L) |
| 3 hours after glucose load | 140 mg/dL (7.8 mmol/L) |
Footnote: **Some labs may use different numbers. Samples drawn at fasting and then 1, 2 and 3 hours after a 100-gram glucose drink. If two or more values meet or exceed the target level, gestational diabetes is diagnosed.
How is gestational diabetes treated?
If you are diagnosed with gestational diabetes, it’s important to follow your doctor’s advice. Managing the condition and keeping your blood glucose levels under control helps avoid complications for both you and your baby.
You may be referred to an obstetrician and dietitian and may need more frequent antenatal appointments and regular monitoring of your blood sugar levels.
If you have gestational diabetes, your prenatal care provider will want to see you more often at prenatal care checkups so they can monitor you and your baby closely to help prevent problems. You’ll probably have tests to make sure you and your baby are doing well. These include a nonstress test and a biophysical profile. The nonstress test checks your baby’s heart rate. The biophysical profile is a nonstress test with an ultrasound.
Your provider also may ask you to do kick counts (also called fetal movement counts). This is way for you to keep track of how often you can feel your baby move. Here are two ways to do kick counts:
- Every day, time how long it takes for your baby to move 10 times. If it takes longer than 2 hours, tell your provider.
- See how many movements you feel in 1 hour. Do this 3 times each week. If the number changes, tell your provider.
If you have gestational diabetes, your provider tells you how often to check your blood sugar, what your levels should be and how to manage them during pregnancy. Blood sugar is affected by pregnancy, what you eat and drink, and how much physical activity you get. You may need to eat differently and be more active. You also may need to take insulin shots or other medicines.
Treatment for gestational diabetes can help reduce your risk for pregnancy complications. Your provider begins treatment with monitoring your blood sugar levels, healthy eating, and physical activity. If this doesn’t do enough to control your blood sugar, you may need medicine. Insulin is the most common medicine for gestational diabetes. It’s safe to take during pregnancy.
Here’s what you can do to help manage gestational diabetes:
- Go to all your prenatal care checkups, even if you’re feeling fine.
- Follow your provider’s directions about how often to check your blood sugar. Your provider shows you how to check your blood sugar on your own. They tell you how often to check it and what to do if it’s too high. Keep a log that includes your blood sugar level every time you check it. Share it with your provider at each checkup. Most parents can check their blood sugar four times each day: once after fasting (first thing in the morning before you’ve eaten) and again after each meal.
- Eat healthy foods. Talk to your provider about the right kinds of foods to eat to help control your blood sugar.
- Do something active every day. Try to get 30 minutes of moderate-intensity activity at least 5 days each week. Talk to your provider about activities that are safe during pregnancy, like walking.
- If you take medicine for diabetes, take it exactly as your provider tells you to. If you take insulin, your provider teaches you how to give yourself insulin shots. Tell your provider about any medicine you take, even if it’s medicine for other health conditions. Some medicines can be harmful during pregnancy, so your provider may need to change them to ones that are safer for you and your baby. Don’t start or stop taking any medicine during pregnancy without talking to your provider first.
- Check your weight gain during pregnancy. Gaining too much weight or gaining weight too fast can make it harder to manage your blood sugar. Talk to your provider about the right amount of weight to gain during pregnancy.
Monitoring your blood glucose levels
Your medical team will give you a target range for your blood glucose levels. You will need to check these at home while you are pregnant.
You can purchase a blood glucose measuring kit from your local pharmacy or diabetes center.
To test your blood glucose levels, you prick your finger with a lancet and put a small drop of blood onto a testing strip. Then you insert the strip into a meter, which reads your blood glucose level.
Healthy diet
If you are diagnosed with gestational diabetes you should be referred to a dietitian for individual advice. If this has not happened ask your maternity care team to refer you.
Understanding your diet and eating healthily is an important part of your treatment for gestational diabetes. It will help you keep your blood sugar levels in the safe range so you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby.
These healthy eating tips for women with gestational diabetes are general. Your care team should talk to you about making changes to your diet and refer you to a dietitian for individual advice that’s right for you.
Following a healthy eating plan is important in managing gestational diabetes. Eat small amounts often and try not to put on too much weight. A healthy diet for women with gestational diabetes includes:
- a carbohydrate with every meal and snack (spread your carbohydrate intake over 3 small meals and 2 to 3 snacks each day)
- a variety of foods that contain the nutrients you need during pregnancy
- high-fiber foods
- avoiding foods and drinks that contain a lot of sugar
- limiting fat, especially saturated fats
Exercise
Moderate intensity physical activity — physical activity that raises your breathing or heart rate — can help you manage your blood glucose levels and reduces insulin resistance.
The best form of exercise if you have gestational diabetes is to build walking into your daily routine. Always check with your doctor first before you start exercising while you are pregnant.
Medication
If your blood sugar levels remain high despite changes to your diet and an exercise regime, you may need medication to lower your blood sugar levels.
Both insulin injections and metformin pills have been shown to be safe for the unborn baby. If you already have diabetes when you become pregnant, discuss with your doctor whether you will need to change any of your medicines.
If you are worried about taking medicines while you are pregnant, discuss the risks with your doctor. Remember, the risks of not treating your gestational diabetes could be much higher for both you and your baby.
Causes of type 2 diabetes
Type 2 diabetes is primarily the result of two interrelated problems:
- Cells in muscle, fat and the liver become resistant to insulin. Because these cells don’t interact in a normal way with insulin, they don’t take in enough sugar.
- The pancreas is unable to produce enough insulin to manage blood sugar levels.
Exactly why this happens is unknown, but being overweight and inactive are key contributing factors.
Glucose (a sugar) is a main source of energy for the cells that make up muscles and other tissues. The use and regulation of glucose includes the following:
- Glucose comes from two major sources: food and your liver.
- Glucose is absorbed into the bloodstream, where it enters cells with the help of insulin.
- Your liver stores and makes glucose.
- When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
In type 2 diabetes, this process doesn’t work well. Instead of moving into your cells, sugar builds up in your bloodstream. As blood sugar levels increase, the insulin-producing beta cells in the pancreas release more insulin. Eventually these cells become impaired and can’t make enough insulin to meet the body’s demands.
Risk factors for developing type 2 diabetes
Some things can increase your chance of getting type 2 diabetes. Because the symptoms of type 2 diabetes are not always obvious, it’s really important to be aware of these risk factors. Factors that may increase your risk of type 2 diabetes include:
- Weight. Being overweight or obese is a main risk.
- Fat distribution. Storing fat mainly in your abdomen (waist size is too large) — rather than your hips and thighs — indicates a greater risk. Your risk of type 2 diabetes rises if you’re a man with a waist circumference above 40 inches (101.6 centimeters) or a woman with a measurement above 35 inches (88.9 centimeters).
- How to measure your waist: Find the top of your hip bone and the bottom of your ribcage. In the middle of these two points is where you need to measure. For many people, the belly button is a good guide, but this might not be the case for you, so it’s best to find that midpoint between your ribcage and hip. If you’re still not sure, watch the video below.
- What is a healthy waist size? This all depends on your gender and ethnicity. For a healthy measurement you need to aim to be less than:
- 80 cm (31.5 in) for all women
- 94 cm (37 in) for most men
- 90cm (35in) for South Asian men. This is because you have a higher risk of type 2 diabetes if you are of black or South Asian background.
- Inactivity. The less active you are, the greater your risk. Physical activity helps control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. The risk of type 2 diabetes increases if your parent, brother or sister has type 2 diabetes.
- Race and ethnicity. Although it’s unclear why, people of certain races and ethnicities — including African Caribbean, Black African, Hispanic, Native American and Asian people (Indian, Pakistani, Bangladeshi or Chinese), and Pacific Islanders — are more likely to develop type 2 diabetes than white people are.
- Blood lipid levels. An increased risk is associated with low levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — and high levels of triglycerides.
- Age. You’re more at risk if you’re white and over 40, or over 25 if you’re African Caribbean, Black African, or South Asian (Indian, Pakistani or Bangladeshi).
- Medical history. For example if you have a history of high blood pressure, heart attack or strokes, gestational diabetes or severe mental illness.
- Prediabetes. Prediabetes is a condition in which your blood sugar level is higher than normal, but not high enough to be classified as diabetes. Left untreated, prediabetes often progresses to type 2 diabetes.
- Pregnancy-related risks. Your risk of developing type 2 diabetes increases if you developed gestational diabetes when you were pregnant or if you gave birth to a baby weighing more than 9 pounds (4 kilograms).
- Polycystic ovary syndrome (PCOS). Having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
- High blood pressure. Having blood pressure over 140/90 millimeters of mercury (mm Hg) is linked to an increased risk of type 2 diabetes.
- Abnormal cholesterol and triglyceride levels. If you have low levels of high-density lipoprotein (HDL), or “good,” cholesterol, your risk of type 2 diabetes is higher. Triglycerides are another type of fat carried in the blood. People with high levels of triglycerides have an increased risk of type 2 diabetes. Your doctor can let you know what your cholesterol and triglyceride levels are.
- Smoking. Smoking is associated with a higher risk of type 2 diabetes, and also increases the risk of other health conditions such as heart disease and cancer.
- Areas of darkened skin, usually in the armpits and neck. This condition, called acanthosis nigricans. This condition often indicates insulin resistance. Acanthosis nigricans is most common in those who are overweight, have darker skin, and have diabetes or pre-diabetic conditions. Acanthosis nigricans is not contagious. It is not harmful. Acanthosis nigricans is a warning sign of a health problem that requires medical attention.
Figure 4. Acanthosis nigricans
Type 2 diabetes symptoms and signs
Many people with type 2 diabetes do not experience any symptoms at first and it may go undiagnosed for years. In fact, you can be living with type 2 diabetes for years and not know it.
Signs and symptoms of type 2 diabetes often develop slowly. When signs and symptoms are present, they may include:
- Increased thirst or being very thirsty
- Frequent urination (passing more urine). Excess sugar building up in your bloodstream causes fluid to be pulled from the tissues. This may leave you thirsty. As a result, you may drink and urinate more than usual.
- Increased hunger. Without enough insulin to move sugar into your cells, your muscles and organs become depleted of energy. This triggers intense hunger.
- Unintended weight loss. Despite eating more than usual to relieve hunger, you may lose weight. Without the ability to metabolize glucose, the body uses alternative fuels stored in muscle and fat. Calories are lost as excess glucose is released in the urine.
- Fatigue (feeling tired). If your cells are deprived of sugar, you may become tired and irritable.
- Blurred vision. If your blood sugar is too high, fluid may be pulled from the lenses of your eyes. This may affect your ability to focus.
- Slow-healing sores or having cuts that heal slowly.
- Frequent infections. Type 2 diabetes affects your ability to heal and resist infections.
- Numbness or tingling in the hands or feet (diabetic neuropathy). Diabetic neuropathy is when diabetes causes damage to your nerves. It can affect different types of nerves in your body, including in your feet, organs and muscles.
- Areas of darkened skin, usually in the armpits and neck. Some people with type 2 diabetes have patches of dark, velvety skin in the folds and creases of their bodies — usually in the armpits and neck. This condition, called acanthosis nigricans, may be a sign of insulin resistance.
Over time, diabetes can lead to complications, which can then cause other symptoms.
Blood glucose testing is important for detecting pre-diabetes and type 2 diabetes before complications arise.
Type 2 diabetes complications
Type 2 diabetes affects many major organs, including your heart, blood vessels, nerves, eyes and kidneys. Also, factors that increase the risk of diabetes are risk factors for other serious chronic diseases. Managing diabetes and controlling your blood sugar can lower your risk for these complications or coexisting conditions (comorbidities).
Potential complications of type 2 diabetes and frequent comorbidities include:
- Heart and blood vessel disease. Diabetes is associated with an increased risk of heart disease, stroke, high blood pressure and narrowing of blood vessels (atherosclerosis).
- Nerve damage (neuropathy) in limbs. High blood sugar over time can damage or destroy nerves, resulting in tingling, numbness, burning, pain or eventual loss of feeling that usually begins at the tips of the toes or fingers and gradually spreads upward.
- Other nerve damage. Damage to nerves of the heart can contribute to irregular heart rhythms. Nerve damage in the digestive system can cause problems with nausea, vomiting, diarrhea or constipation. For men, nerve damage may cause erectile dysfunction.
- Kidney disease (diabetic nephropathy). Diabetes may lead to chronic kidney disease or irreversible end-stage kidney disease, which may require dialysis or a kidney transplant.
- Eye damage. Diabetes increases the risk of serious eye diseases, such as cataracts and glaucoma, and may damage the blood vessels of the retina, potentially leading to blindness.
- Skin conditions. Diabetes may leave you more susceptible to skin problems, including bacterial and fungal infections.
- Slow healing. Left untreated, cuts and blisters can become serious infections, which may heal poorly. Severe damage might require toe, foot or leg amputation.
- Hearing impairment. Hearing problems are more common in people with diabetes.
- Sleep apnea. Obstructive sleep apnea is common in people living with type 2 diabetes. Obesity may be the main contributing factor to both conditions. It’s not clear whether treating sleep apnea improves blood sugar control.
- Dementia. Type 2 diabetes seems to increase the risk of Alzheimer’s disease and other disorders that cause dementia. Poor control of blood sugar levels is linked to more-rapid decline in memory and other thinking skills.
Type 2 diabetes prevention
Healthy lifestyle choices can help prevent type 2 diabetes, and that’s true even if you have biological relatives living with diabetes. If you’ve received a diagnosis of prediabetes, lifestyle changes may slow or stop the progression to diabetes.
Prevention of diabetes through healthy lifestyle includes:
- Eating healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains.
- Getting active. Aim for 150 or more minutes a week of moderate to vigorous aerobic activity, such as a brisk walk, bicycling, running or swimming.
- Losing weight. Losing a modest amount of weight and keeping it off can delay the progression from prediabetes to type 2 diabetes. If you have prediabetes, losing 7% to 10% of your body weight can reduce the risk of diabetes.
- Avoiding inactivity for long periods. Sitting still for long periods can increase your risk of type 2 diabetes. Try to get up every 30 minutes and move around for at least a few minutes.
For people with prediabetes, metformin (Fortamet, Glumetza, others), an oral diabetes medication, may be prescribed to reduce the risk of type 2 diabetes. This is usually prescribed for older adults who are obese and unable to lower blood sugar levels with lifestyle changes.
How to reduce your waist size
Unfortunately, there are no quick fixes when it comes to reducing your waist size. It comes down to eating well and moving more. Start by setting some realistic, achievable changes to suit your lifestyle. You can become more active by making small changes to your lifestyle. You can fit them around your daily life and in your budget. Here are three top tips to help make your life more active:
- Set clear goals to move more – setting goals can help you break down what you need to do and how to do it. This could be aiming to walk more, taking up a new activity or learning a new skill such as swimming or running.
- Plan ahead – we all have busy lives, so try to plan what you’re going to eat and what activity you’re going to do this week, fitting it around your social life. You can always squeeze in an activity during your lunch hour or go for walk instead of getting another form of transport.
- Start by making small changes – it’s time to put your plan into action. Start small and do something you enjoy. Doing just a little bit more each day will still make a difference. It also means you’re more likely to stick to it. Just remember, small changes to your routine won’t have such a big impact, so start small and grow.
Manage your weight
If you are living with overweight or obesity and are at high risk of type 2 diabetes, losing just 5% of your body weight can significantly reduce your risk. There are lots of ways you can lose weight and it’s about finding what works best for you.
Making healthier food choices and being more active are both positive ways to start making these changes. If you need help with managing your weight, a dietitian can help you. Your family physician may also be able to help you find weight management services in your local area.
Eat a healthy and balanced diet
There’s no one special diet for all people at high risk of developing type 2 diabetes. Everyone is individual, so there isn’t a one size fits all way of eating for everyone. But, the food and drink you have in your overall diet is linked to your risk of developing type 2 diabetes. For example, if your overall diet is made up of food and drinks that are in high fat, have a high GI (glycemic index) and low fiber content, this is linked to an increased risk of type 2 diabetes. But the good news is that by changing some of your food and drink choices, you can reduce your risk of type 2 diabetes.
All of these ways of eating have been linked with a decreased risk of type 2 diabetes:
- Mediterranean diet.
- Dietary Approaches to Stop Hypertension (DASH) diet
- Vegetarian and vegan diets
- Nordic diet
- Moderately cutting down on carbohydrates.
This is because they are made up of healthy foods like fruits, vegetables, wholegrains and lean proteins and it’s the overall balance of your diet that is important in keeping you healthy.
Additionally, there are some foods experts recommend reducing your intake of, as these have been associated with an increased risk. These foods include:
- sugar sweetened drinks
- red and processed meats
- refined carbohydrates (like sugary snacks, white bread, sugary cereals)
- potatoes (particularly French fries)
So, to reduce your risk, aim to eat more of the foods linked with a decreased risk.
Research has shown that the following foods and drinks can be associated with a decreased risk:
- total fruit and veg intake (including specifically green leafy veg, blueberries, grapes and apples)
- wholegrains
- yogurt and cheese
- unsweetened tea and coffee
Be more active
If you spend a lot of time sitting down, this is known as a sedentary lifestyle. Being sedentary is linked with an increased risk of type 2 diabetes. So being active in your daily life can help to reduce your risk of type 2 diabetes. This doesn’t mean you need to take up a new sport or join the gym. You could make small changes so that you are being more active every day. Think about taking phone calls standing up, using stairs instead of the lift, and going for a walk on your lunch break.
Type 2 diabetes diagnosis
If your doctor thinks you may have type 2 diabetes, you will probably need to have a blood test.
You may be asked to take a fasting blood glucose test, where you don’t eat for 8 hours before the test, or a random blood glucose test, where you don’t need to fast.
You may also need to have an oral glucose tolerance test (OGTT) where you have blood glucose tests after you drink a sugary drink.
You may also be asked to have your urine tested for glucose and ketones.
A1C or HbA1C test
Type 2 diabetes is usually diagnosed using the glycated hemoglobin (A1C or HbA1C) test. The A1C test measures your average blood glucose for the past two to three months. Results are interpreted as follows 12:
- Below 5.7% is normal.
- 5.7% to 6.4% is diagnosed as prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
If the A1C test isn’t available, or if you have certain conditions — such as if you’re pregnant or have an uncommon form of hemoglobin (known as a hemoglobin variant) — that can make the A1C test inaccurate, your doctor may use the following tests to diagnose diabetes:
Random blood sugar test
Random blood sugar test also called casual plasma glucose test is a blood check at any time of the day when you have severe diabetes symptoms.
- Diabetes is diagnosed at blood glucose of greater than or equal to 11.1 mmol/L (200 mg/dL)
Blood sugar values are expressed in milligrams of sugar per deciliter (mg/dL) or millimoles of sugar per liter (mmol/L) of blood. Regardless of when you last ate, a level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially if you also have signs and symptoms of diabetes, such as frequent urination and extreme thirst.
Fasting blood sugar test
A blood sample is taken after an overnight fast. Results are interpreted as follows:
- Less than 100 mg/dL (5.6 mmol/L) is normal.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is diagnosed as prediabetes.
- 126 mg/dL (7 mmol/L) or higher on two separate tests is diagnosed as diabetes.
Oral glucose tolerance test (OGTT)
Oral glucose tolerance test is less commonly used than the others, except during pregnancy. You’ll need to fast overnight and then drink a sugary liquid at the doctor’s office. Blood sugar levels are tested periodically for the next two hours. Results are interpreted as follows:
- Less than 140 mg/dL (7.8 mmol/L) is normal.
- 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) is diagnosed as prediabetes.
- 200 mg/dL (11.1 mmol/L) or higher after two hours suggests diabetes.
After a diagnosis
If you’re diagnosed with diabetes, your doctor or health care provider may do other tests to distinguish between type 1 and type 2 diabetes — since the two conditions often require different treatments.
Your health care provider will repeat the test A1C levels at least two times a year and when there are any changes in treatment. Target A1C goals vary depending on your age and other factors. For most people, the American Diabetes Association recommends an A1C level below 7%.
You will also receive regular diagnostic tests to screen for complications of diabetes or comorbid conditions.
Type 2 diabetes treatment
Nutrition and physical activity are important parts of a healthy lifestyle when you have diabetes.
Management of type 2 diabetes includes:
- Healthy eating
- Regular exercise
- Weight loss
- Blood sugar monitoring
- Possibly, diabetes medication or insulin therapy
These steps will help keep your blood sugar level closer to normal, which can delay or prevent complications.
Following a healthy meal plan and being active can help you keep your blood sugar level in your target range. To manage your blood glucose, you need to balance what you eat and drink with physical activity and diabetes medicine, if you take any. What you choose to eat, how much you eat, and when you eat are all important in keeping your blood glucose level in the range that your health care team recommends.
Becoming more active and making changes in what you eat and drink can seem challenging at first. You may find it easier to start with small changes and get help from your family, friends, and health care team.
Eating well and being physically active most days of the week can help you:
- keep your blood glucose level, blood pressure, and cholesterol in your target ranges
- lose weight or stay at a healthy weight
- prevent or delay diabetes problems
- feel good and have more energy
Physical activity
Exercise is important for losing weight or maintaining a healthy weight. It also helps with regulating your blood sugar levels.
Being active has many health benefits:
- lowers blood glucose levels
- lowers blood pressure
- improves blood flow
- burns extra calories so you can keep your weight down if needed
- improves your mood
- can prevent falls and improve memory in older adults
- may help you sleep better
Talk to your primary health care provider before starting or changing your exercise program to ensure that activities are safe for you.
- Aerobic exercise. Choose an aerobic exercise that you enjoy, such as walking, swimming, biking or running. Adults should aim for 30 minutes or more of moderate aerobic exercise on most days of the week, or at least 150 minutes a week. Children should have 60 minutes of moderate to vigorous aerobic exercise daily.
- Resistance exercise. Resistance exercise increases your strength, balance and ability to perform activities of daily living more easily. Resistance training includes weightlifting, yoga and calisthenics.
Adults living with type 2 diabetes should aim for two to three sessions of resistance exercise each week. Children should engage in activities that build strength and flexibility at least three days a week. This can include resistance exercises, sports and climbing on playground equipment.
Limit inactivity. Breaking up long bouts of inactivity, such as sitting at the computer, can help control blood sugar levels. Take a few minutes to stand, walk around or do some light activity every 30 minutes.
If you are overweight, combining physical activity with a reduced-calorie eating plan can lead to even more benefits. In the Look AHEAD: Action for Health in Diabetes study, overweight adults with type 2 diabetes who ate less and moved more had greater long-term health benefits compared to those who didn’t make these changes 13, 14. These benefits included improved cholesterol levels, less sleep apnea, and being able to move around more easily.
Even small amounts of physical activity can help. Experts suggest that you aim for at least 30 minutes of moderate or vigorous physical activity 5 days of the week.3 Moderate activity feels somewhat hard, and vigorous activity is intense and feels hard. If you want to lose weight or maintain weight loss, you may need to do 60 minutes or more of physical activity 5 days of the week.3
Be patient. It may take a few weeks of physical activity before you see changes in your health.
Weight loss
Weight loss results in better control of blood sugar levels, cholesterol, triglycerides and blood pressure. If you’re overweight, you may begin to see improvements in these factors after losing as little as 5% of your body weight. However, the more weight you lose, the greater the benefit to your health and disease management.
Your health care provider or dietitian can help you set appropriate weight-loss goals and encourage lifestyle changes to help you achieve them.
Medications for type 2 diabetes
If you can’t maintain your target blood sugar level with diet and exercise, you may need type 2 diabetes medicines, which may include pills or medicines you inject under your skin, such as insulin. Over time, you may need more than one diabetes medicine to manage your blood glucose. Even if you don’t take insulin, you may need it at special times, such as during pregnancy or if you are in the hospital. You also may need medicines in addition to diabetes medications for high blood pressure, high cholesterol, or other conditions, as well as low-dose aspirin, to help prevent heart and blood vessel disease.
Drug treatments for type 2 diabetes include the following.
Metformin
Metformin (Fortamet, Glumetza, others) is generally the first medication prescribed for most people with type 2 diabetes. Metformin comes as a liquid, a tablet, and an extended-release (long-acting) tablet to take by mouth. Metformin works primarily by lowering glucose production in the liver and improving your body’s sensitivity to insulin so that your body uses insulin more effectively. This drug may help you lose a small amount of weight.
Your doctor may start you on a low dose of metformin and gradually increase your dose not more often than once every 1–2 weeks. You will need to monitor your blood sugar carefully so your doctor will be able to tell how well metformin is working.
Some people on metformin may experience B-12 deficiency and may need to take supplements.
Other possible side effects of metformin, which may improve over time, include:
- Nausea
- Abdominal pain
- Bloating
- Diarrhea
Alpha-glucosidase inhibitors
Alpha-glucosidase inhibitors pills help your body digest sugar more slowly by blocking the breakdown of starches, such as bread, potatoes, and pasta in the intestine. Acarbose (Precose) and miglitol (Glyset) are alpha-glucosidase inhibitors. These drugs help the body to lower blood glucose levels. They also slow the breakdown of some sugars, such as table sugar. Their action slows the rise in blood glucose levels after a meal. They should be taken with the first bite of a meal. These drugs may have side effects, including gas and diarrhea.
Sulfonylureas
Sulfonylureas help your body secrete more insulin. Examples include glyburide (DiaBeta, Glynase), glipizide (Glucotrol) and glimepiride (Amaryl).
Possible side effects of sulfonylureas include:
- Low blood sugar
- Weight gain
Meglitinides
Meglitinides or glinides stimulate the pancreas to secrete more insulin. They’re faster acting than sulfonylureas, and the duration of their effect in the body is shorter. Examples include repaglinide (Prandin) and nateglinide (Starlix).
Possible side effects of meglitinides include:
- Low blood sugar
- Weight gain
Thiazolidinediones
Thiazolidinediones make the body’s tissues more sensitive to insulin. Examples include rosiglitazone (Avandia) and pioglitazone (Actos). Possible side effects include:
- Risk of congestive heart failure
- Risk of bladder cancer (pioglitazone)
- Risk of bone fractures
- High cholesterol (rosiglitazone)
- Weight gain
DPP-4 inhibitors
DPP-4 inhibitors help reduce blood sugar levels but tend to have a very modest effect. Examples include sitagliptin (Januvia), saxagliptin (Onglyza) and linagliptin (Tradjenta). Possible side effects include:
- Risk of pancreatitis
- Joint pain
GLP-1 receptor agonists
GLP-1 receptor agonists are injectable medications that slow digestion and help lower blood sugar levels. Their use is often associated with weight loss, and some may reduce the risk of heart attack and stroke. Examples include exenatide (Byetta, Bydureon), liraglutide (Saxenda, Victoza) and semaglutide (Rybelsus, Ozempic). Possible side effects include:
- Risk of pancreatitis
- Nausea
- Vomiting
- Diarrhea
SGLT2 inhibitors
SGLT2 inhibitors affect the blood-filtering functions in your kidneys by inhibiting the return of glucose to the bloodstream. As a result, glucose is excreted in the urine. These drugs may reduce the risk of heart attack and stroke in people with a high risk of those conditions. Examples include canagliflozin (Invokana), dapagliflozin (Farxiga) and empagliflozin (Jardiance). Possible side effects include:
- Risk of amputation (canagliflozin)
- Risk of bone fractures (canagliflozin)
- Risk of gangrene
- Vaginal yeast infections
- Urinary tract infections
- Low blood pressure
- High cholesterol
Dopamine-2 agonists
Dopamine-2 agonist bromocriptine (Cycloset and Parlodel) helps lower blood glucose levels after a meal. Dopamine-2 agonist affects a chemical called dopamine in your cells. It is not clear how this pill works for diabetes.
Common side effects of bromocriptine:
- Nausea
- Headache
- Feel very tired
- Feel dizzy
- Vomiting
Bile acid sequestrants
Bile acid sequestrants colesevelam (Welchol) is a cholesterol-lowering medication that also reduces blood glucose levels in patients with diabetes. Bile acid sequestrants help remove cholesterol from the body, particularly LDL cholesterol (“bad cholesterol”), which is often elevated in people with diabetes. The medications reduce LDL cholesterol by binding with bile acids in the digestive system; the body in turn uses cholesterol to replace the bile acids, which lowers cholesterol levels. The mechanism by which colesevelam lowers glucose levels is not well understood. Because bile acid sequestrants are not absorbed into the bloodstream, they are usually safe for use by patients who may not be able to use other medications because of liver problems. Because of the way they work, side effects of bile acid sequestrants can include flatulence and constipation.
Oral combination therapy
Because the drugs listed above act in different ways to lower blood glucose levels, they may be used together. For example, a biguanide and a sulfonylurea may be used together. Many combinations can be used. Though taking more than one drug can be more costly and can increase the risk of side effects, combining oral medications can improve blood glucose control when taking only a single pill does not have the desired effects. Switching from one single pill to another is not as effective as adding another type of diabetes medicine.
Insulin therapy
Insulin is a naturally occurring hormone secreted by your pancreas. Some people who have type 2 diabetes need insulin therapy. In the past, insulin therapy was used as a last resort, but today it may be prescribed sooner if blood sugar targets aren’t met with lifestyle changes and other medications.
There are many different types of insulin sold in the United States, which differ on how quickly they begin to work and how long they have an effect. Long-acting insulin, for example, is designed to work overnight or throughout the day to keep blood sugar levels stable. Short-acting insulin might be used at mealtime.
Here’s a quick look at the different types of insulin. If you need a mix of two types, you can talk to your doctor about getting a premixed supply.
- Rapid-acting insulin begins to work about 15 minutes after injection, peaks in about 1 hour, and continues to work for 2 to 4 hours
- Regular or short-acting insulin usually reaches the bloodstream within 30 minutes after injection, peaks anywhere from 2 to 3 hours after injection, and is effective for approximately 3 to 6 hours
- Intermediate-acting insulin generally reaches the bloodstream about 2 to 4 hours after injection, peaks 4 to 12 hours later, and is effective for about 12 to 18 hours
- Long-acting insulin reaches the bloodstream several hours after injection and tends to lower glucose levels fairly evenly over a 24-hour period
Your doctor will determine what type of insulin is appropriate for you and when you should take it. Your insulin type, dosage and schedule may change depending on how stable your blood sugar levels are. Most types of insulin are taken by injection.
When it comes to syringes, your doctor will advise on which capacity you need based on your insulin dose. In general, smaller capacity syringes can be easier to read and draw an accurate dose. Here are some tips:
- If your largest dose is close to the syringe’s maximum capacity, consider buying the next size up in case your dosage changes
- If you need to measure doses in half units, be sure to choose a syringe that has these markings
- If you’re traveling outside of the United States, be certain to match your insulin strength with the correct size syringe
Side effects of insulin include the risk of low blood sugar (hypoglycemia), diabetic ketoacidosis and high triglycerides.
Weight-loss surgery
Weight-loss surgery also known as bariatric surgery changes the shape and function of your digestive system. This surgery may help you lose weight and manage type 2 diabetes and other conditions related to obesity. There are various surgical procedures, but all of them help you lose weight by limiting how much food you can eat. Some procedures also limit the amount of nutrients you can absorb.
Weight-loss surgery is only one part of an overall treatment plan. Your treatment will also include diet and nutritional supplement guidelines, exercise and mental health care.
Generally, weight-loss surgery may be an option for adults living with type 2 diabetes who have a body mass index (BMI) of 35 or higher. BMI is a formula that uses weight and height to estimate body fat. Depending on the severity of diabetes or comorbid conditions, surgery may be an option for someone with a BMI lower than 35.
Weight-loss surgery requires a lifelong commitment to lifestyle changes. Long-term side effects include nutritional deficiencies and osteoporosis.
Alternative medicine
Many alternative medicine treatments claim to help people living with diabetes. According to the National Center for Complementary and Integrative Health, studies haven’t provided enough evidence to recommend any alternative therapies for blood sugar management. Research has shown the following results about popular supplements for type 2 diabetes:
- Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage, muscular problems and skin reactions.
- Magnesium supplements have shown benefits for blood sugar control in some but not all studies. Side effects include diarrhea and cramping. Very large doses — more than 5,000 mg a day — can be fatal.
- Cinnamon, in some studies, has lowered fasting glucose levels but not A1C levels. Therefore, there’s no evidence of overall improved glucose management. Most cinnamon contains a substance called coumarin that may cause or worsen liver disease.
Talk to your doctor before starting a dietary supplement or natural remedy. Do not replace your prescribed diabetes medication with alternative medicines.
Monitoring your blood sugar
Your health care provider will advise you on how often to check your blood sugar level to make sure you remain within your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to do this multiple times a day.
Monitoring is usually done with a small, at-home device called a blood glucose meter, which measures the amount of sugar in a drop of your blood. You should keep a record of your measurements to share with your health care team.
Continuous glucose monitoring is an electronic system that records glucose levels every few minutes from a sensor placed under your skin. Information can be transmitted to a mobile device such as your phone, and the system can send alerts when levels are too high or too low.
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of signs and symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar (hyperglycemia)
Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar (hyperglycemia).
High blood sugar (hyperglycemia) signs and symptoms include:
- Frequent urination
- Increased thirst
- Dry mouth
- Blurred vision
- Fatigue
- Headache
Hyperglycemic hyperosmolar nonketotic syndrome
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L). Hyperglycemic hyperosmolar nonketotic syndrome may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination.
Hyperglycemic hyperosmolar nonketotic syndrome signs and symptoms include:
- Dry mouth
- Extreme thirst
- Drowsiness
- Confusion
- Dark urine
- Seizures
Diabetic ketoacidosis
Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medications — including the diabetes medications called SGLT2 inhibitors.
Although diabetic ketoacidosis is usually less severe in type 2 diabetes, the toxicity of the acids can be life-threatening. In addition to the signs and symptoms of hypoglycemia, such as frequent urination and increased thirst, diabetic ketoacidosis may result in:
- Nausea
- Vomiting
- Abdominal pain
- Shortness of breath
- Fruity-smelling breath
Low blood sugar (hypoglycemia)
If your blood sugar level drops below your target range, it’s known as low blood sugar (hypoglycemia). Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physical activity than usual.
Low blood sugar (hypoglycemia) signs and symptoms include:
- Sweating
- Shakiness
- Weakness
- Hunger
- Irritability
- Dizziness
- Headache
- Blurred vision
- Heart palpitations
- Slurred speech
- Drowsiness
- Confusion
If you have signs or symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level — fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, repeat the sugar intake. Eat a meal after levels return to normal.
If you lose consciousness, you will need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
Type 2 diabetes diet
There is no such thing as a ‘diabetic diet’ or a special diet exclusively for people with type 2 diabetes 5, 15. No two people with diabetes are the same. So there isn’t a one-size-fits-all way of eating for everyone with diabetes. In the past, people with type 2 diabetes were sent away after their diagnosis with a list of foods they weren’t allowed to eat, or often told to cut out sugar. But the best advice is to make healthier choices more often, and only have treats occasionally and in small portions. Because experts know that making healthier food choices is important to managing your diabetes and to reducing your risk of diabetes complications, like heart problems and strokes, and other health conditions including certain types of cancers.
Healthy eating centers around:
- A regular schedule for meals and healthy snacks
- Smaller portion sizes
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains
- Fewer refined grains, starchy vegetables and sweets
- Modest servings of low-fat dairy, low-fat meats and fish
- Healthy cooking oils, such as olive oil or canola oil
- Fewer calories
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy choices among your food preferences
- Plan well-balanced, nutritional meals
- Develop new habits and address barriers to changing habits
- Monitor carbohydrate intake to keep your blood sugar levels more stable
Try and make changes to your food choices that are realistic and achievable so you’ll stick with them. This will be different for everyone, depending on what you eat now and the goals you want to achieve.
Breakfast. Here are some healthy breakfast ideas to choose from:
- a bowl of wholegrain cereal with milk
- two slices of wholegrain toast with olive oil-based spread
- a pot of natural unsweetened yogurt and fruit
- two slices of avocado with a hardboiled egg.
Lunch. Here are some healthy lunch ideas to choose from:
- a chicken or tuna salad sandwich
- a small pasta salad
- soup with or without a wholegrain roll
- a piece of salmon or tuna steak and salad.
Think about having a piece of fruit or a pot of natural unsweetened yogurt afterwards too.
Dinner. Here are some healthy dinner ideas to choose from:
- lasagne and salad
- roast chicken and vegetables, with or without potatoes
- beef stir-fry and vegetables, with or without brown rice
- chicken tortillas and salad
- salmon and vegetables, with or without noodles
- curry with chickpeas and brown rice
Mediterranean diet
The Mediterranean Diet is a way of eating rather than a formal diet plan. The Mediterranean Diet features foods eaten in more than 20 countries bordering the Mediterranean Sea including Greece, Spain, southern Italy, Portugal, Morocco, Cyprus, Croatia and France and each has their own unique culture and cuisine. In reality there is no “one” Mediterranean Diet 16, which in 2010 was recognized by UNESCO as an intangible cultural heritage of humanity. The “Mediterranean diet” encompasses all of them—it’s not one size fits all 17. Despite regional variations, common components and cultural aspects can be identified, namely olive oil as the main source of lipids, the consumption of large amounts of seasonal vegetables, fruits and aromatic herbs (some of them gathered from the wild), as well as small intakes of meat and fish, often replaced or complemented with pulses, as sources of protein.
A Mediterranean-style diet typically includes:
- plenty of fruits, vegetables, bread and other grains, potatoes, beans, nuts and seeds are eaten daily and make up the majority of food consumed;
- olive oil as a primary fat source, may account for up to 40% of daily calories; and
- small portions of cheese or yogurt are usually eaten each day, along with a serving of fish, poultry, or eggs.
Fish and poultry are more common than red meat in the Mediterranean diet. The Mediterranean diet also centers on minimally processed, plant-based foods. Wine may be consumed in low to moderate amounts, usually with meals. Fruit is a common dessert instead of sweets.
Main meals consumed daily should be a combination of three elements: cereals, vegetables and fruits, and a small quantity of legumes, beans or other (though not in every meal). Cereals in the form of bread, pasta, rice, couscous or bulgur (cracked wheat) should be consumed as one–two servings per meal, preferably using whole or partly refined grains. Vegetable consumption should amount to two or more servings per day, in raw form for at least one of the two main meals (lunch and dinner). Fruit should be considered as the primary form of dessert, with one–two servings per meal. Consuming a variety of colors of both vegetables and fruit is strongly recommended to help ensure intake of a broad range of micronutrients and phytochemicals. The less these foods are cooked, the higher the retention of vitamins and the lower use of fuel, thus minimizing environmental impact.
The Mediterranean Diet is characterized by 18:
- An abundance of plant food (fruit, vegetables, breads, cereals, potatoes, beans, nuts, and seeds);
- Minimally processed, seasonally fresh, locally grown foods;
- Desserts comprised typically of fresh fruit daily and occasional sweets containing refined sugars or honey;
- Olive oil (high in polyunsaturated fat) as the principal source of fat;
- Daily dairy products (mainly cheese and yogurt) in low to moderate amounts;
- Fish and poultry in low to moderate amounts;
- Up to four eggs weekly;
- Red meat rarely; and
- Wine in low to moderate amounts with meals.
Here are some things you can do to switch from a traditional Western-style diet to a more Mediterranean way of eating.
- Dip bread in a mix of olive oil and fresh herbs instead of using butter.
- Add avocado slices to your sandwich instead of bacon.
- Have fish for lunch or dinner instead of red meat. Brush it with olive oil, and broil or grill it.
- Sprinkle your salad with seeds or nuts instead of cheese.
- Cook with olive or canola oil instead of butter or oils that are high in saturated fat.
- Choose whole-grain bread, pasta, rice, and flour instead of foods made with white flour.
- Add ground flaxseed to cereal, low-fat yogurt, and soups.
- Cut back on meat in meals. Instead of having pasta with meat sauce, try pasta tossed with olive oil and topped with pine nuts and a sprinkle of Parmesan cheese.
- Dip raw vegetables in a vinaigrette dressing or hummus instead of dips made from mayonnaise or sour cream.
- Have a piece of fruit for dessert instead of a piece of cake.
- Use herbs and spices instead of salt to add flavor to foods.
A Mediterranean-style diet can help you achieve the American Heart Association’s recommendations for a healthy dietary pattern that:
- emphasizes vegetables, fruits, whole grains, beans and legumes;
- includes low-fat or fat-free dairy products, fish, poultry, non-tropical vegetable oils and nuts; and
- limits added sugars, sugary beverages, sodium, highly processed foods, refined carbohydrates, saturated fats, and fatty or processed meats.
This style of eating can play a big role in preventing heart disease and stroke and reducing risk factors such as obesity, diabetes, high cholesterol and high blood pressure. There is some evidence that a Mediterranean diet rich in virgin olive oil may help the body remove excess cholesterol from arteries and keep blood vessels open.
The traditional Mediterranean dietary pattern is of particular interest to healthcare providers and dietary scientists, because of observations from the 1960s that populations in countries of the Mediterranean region, such as Greece and Italy, had lower mortality from cardiovascular disease compared with northern European populations or the US, probably as a result of different eating habits.
However, adherence to the Mediterranean diet dietary pattern has been rapidly decreasing in the region since 2000, particularly in Greece, Portugal and Spain – due to the wide dissemination of the fast-food culture. These observations point to a nutrition transition period that encompasses considerable changes in diet and physical activity patterns, which may be leading to an increase in the incidence of chronic and degenerative diseases in the Mediterranean region.
Traditionally characterized by vegetables, legumes, beans, fruits, nuts, seeds, olives, lots of extra virgin olive oil, high-fiber breads and whole grains and fish, this way of eating not only involves a low consumption of processed food, processed carbohydrates, sweets, chocolate and red meat. The recommended foods are rich with monounsaturated fats, fiber, and omega-3 fatty acids.
The Mediterranean Diet is associated with a lower incidence of mortality from all-causes 19 and is also related to lower incidence of cardiovascular diseases 20, type 2 diabetes 21, certain types of cancer 22, and neurodegenerative diseases 23. The Mediterranean diet is now recognized as one of the most healthy food patterns in the world.
The Mediterranean diet is like other heart-healthy diets in that it recommends eating plenty of fruits, vegetables, and high-fiber grains. But in the Mediterranean diet, an average of 35% to 40% of calories can come from fat. Most other heart-healthy guidelines recommend getting less than 35% of your calories from fat. The fats allowed in the Mediterranean diet are mainly from unsaturated oils such as fish oils, olive oil, and certain nut or seed oils (such as canola, soybean, or flaxseed oil) and from nuts (walnuts, hazelnuts, and almonds). These types of oils may have a protective effect on the heart.
Mediterranean Diet Food List
There’s no one “Mediterranean diet food list” because there are more than 20 countries bordering the Mediterranean Sea. Diets vary between these countries and also between regions within a country. Many differences in culture, ethnic background, religion, economy and agricultural production result in different diets. But the common Mediterranean dietary meal plan (source 24) has these characteristics:
- High consumption of fruits, vegetables, bread and other cereals, potatoes, beans, nuts and seeds
- Olive oil is an important monounsaturated fat source
- Dairy products, fish and poultry are consumed in low to moderate amounts, and little red meat is eaten
- Eggs are consumed zero to four times a week
- Wine is consumed in low to moderate amounts
Mediterranean Diet Meal Plan:
- Eating a variety of fruits and vegetables each day, such as grapes, blueberries, tomatoes, broccoli, peppers, figs, olives, spinach, eggplant, beans, lentils, and chickpeas.
- Eating a variety of whole-grain foods each day, such as oats, brown rice, and whole wheat bread, pasta, and couscous.
- Choosing healthy (unsaturated) fats, such as nuts, olive oil, and certain nut or seed oils like canola, soybean, and flaxseed. About 35% to 40% of daily calories can come from fat, mainly from unsaturated fats. More than half the fat calories in a Mediterranean diet come from monounsaturated fats (mainly from olive oil). Monounsaturated fat doesn’t raise blood cholesterol levels the way saturated fat does. (source 24).
- Limiting unhealthy (saturated) fats, such as butter, palm oil, and coconut oil. And limit fats found in animal products, such as meat and dairy products made with whole milk.
- Eating mostly vegetarian meals that include whole grains, beans, lentils, and vegetables.
- Eating fish at least 2 times a week, such as tuna, salmon, mackerel, lake trout, herring, or sardines.
- Eating moderate amounts of low-fat dairy products each day or weekly, such as milk, cheese, or yogurt.
- Eating moderate amounts of poultry and eggs every 2 days or weekly.
- Limiting red meat to only a few times a month in very small amounts. For example, a serving of meat is 3 ounces. This is about the size of a deck of cards.
- Limiting sweets and desserts to only a few times a week. This includes sugar-sweetened drinks like soda.
Low-carb diet
There are many different types of low-carb diets. Eating a low-carb diet means cutting down on the amount of carbohydrates (carbs) you eat to less than 130 grams a day 25, 26. A low-carb diet focuses on foods high in protein and fat. But low-carb eating shouldn’t be no-carb eating. Some carbohydrate foods contain essential vitamins, minerals and fiber, which form an important part of a healthy diet 27.
A low-carb diet is generally used for weight loss. Some low-carb diets may have health benefits beyond weight loss, such as lowering your risk of type 2 diabetes and metabolic syndrome.
There are three macronutrients, carbohydrates (4 kcal/g), fat (9 kcal/g), and protein (4 kcal/g) found in food. Therefore, studies have defined low carbohydrate as a percent of daily macronutrient intake or total daily carbohydrate load. This article will define it as 28:
- Very low-carbohydrate (less than 10% carbohydrates) or 20 to 50 g/day
- Low-carbohydrate (less than 26% carbohydrates) or less than 130 g/day
- Moderate-carbohydrate (26% to 44%)
- High-carbohydrate (45% or greater)
For reference, the institute of medicine proposes Americans obtain 45% to 65% of calories from carbohydrates 29.
To put this into context, a medium-sized slice of bread is about 15 to 20g of carbs, which is about the same as a regular apple. On the other hand, a large jacket potato could have as much as 90g of carbs, as does one liter of orange juice.
A low-carb diet limits the amount of carbohydrates you eat. Carbs are grouped as:
- Simple natural, such as lactose in milk and fructose in fruit.
- Simple refined, such as table sugar.
- Complex natural, such as whole grains or beans.
- Complex refined, such as white flour.
Common sources of natural carbohydrates include:
- Grains.
- Fruits.
- Vegetables.
- Milk.
- Nuts.
- Seeds.
- Legumes, such as beans, lentils and peas.
In general, you digest complex carbs more slowly. Complex carbs also have less effect on blood sugar than refined carbs do. They also offer fiber.
Refined carbs such as sugar or white flour are often added to processed foods. Examples of foods with refined carbs are white breads and pasta, cookies, cake, candy, and sugar-sweetened sodas and drinks.
The body uses carbs as its main energy source. During digestion, complex carbs are broken down into simple sugars, also called glucose, and released into your blood. This is called blood glucose.
Insulin is released to help glucose enter the body’s cells, where it can be used for energy. Extra glucose is stored in the liver and in muscles. Some is changed to body fat.
A low-carb diet is meant to cause the body to burn stored fat for energy, which leads to weight loss 30, 31.
A low-carb diet isn’t for everyone. The evidence shows they can be safe and effective in helping people with type 2 diabetes manage their weight, blood glucose (sugar) levels and risk of heart disease in the short term 32. But the evidence also shows they can affect growth in children, and so should not be recommended for them. And there is little evidence to show the benefits of this type of diet in people with type 1 diabetes.
If you do decide to follow a low-carb diet, it’s important to know all the potential benefits and how to manage any potential risks.
One hypothesis of why low-carb diet produces rapid weight loss compared to other diets is that fats and protein increase the feeling of fullness (satiety) and produce less concomitant hypoglycemia. This increase in satiety and less rebound hypoglycemia reduces hunger and overall food intake and produces a caloric deficit 28. Another hypothesis contends that low-carb diets can produce a higher metabolic burn than high-carb diets. In recent studies, there appears to be a metabolic advantage of approximately 200 to 300 more calories burned compared to an iso-caloric high-carb diet 30, 33. However, these theories remain controversial 34.
Typical foods for a low-carb diet
In broad terms, a low-carb diet focuses on proteins and some nonstarchy vegetables 35. A low-carb diet generally limits grains, legumes, fruits, breads, sweets, pastas and starchy vegetables, and sometimes nuts and seeds. But some low-carb diet plans allow small amounts of fruits, vegetables and whole grains.
A daily limit of 0.7 to 2 ounces (20 to 57 grams) of carbohydrates is typical with a low-carb diet. These amounts of carbohydrates provide 80 to 240 calories. Some low-carb diets greatly limit carbs during the early phase of the diet. Then those diets allow more carbs over time.
In contrast, the Dietary Guidelines for Americans recommend that carbohydrates make up 45% to 65% of your total daily calorie intake 36. So if you eat or drink 2,000 calories a day, carbs would account for between 900 and 1,300 calories a day.
Side effects of low-carb diet
A sudden and large drop in carbs can cause short term side effects, such as:
- Constipation.
- Headache.
- Muscle cramps.
Severe carb limits can cause your body to break down fat into ketones for energy. This is called ketosis. Ketosis can cause side effects such as bad breath, headache, fatigue and weakness.
It’s not clear what kind of possible long-term health risks a low-carb diet may pose. If you limit carbs in the long term, it may cause you to have too little of some vitamins or minerals and to have digestive issues.
Some health experts think that if you eat large amounts of fat and protein from animal sources, your risk of heart disease or certain cancers may go up.
If you opt to follow a low-carb diet, think about the fats and proteins you choose. Limit foods with saturated and trans fats, such as meat and high-fat dairy products. These foods may make your risk for heart disease go up.
Type 2 diabetes food list
You may worry that having diabetes means going without foods you enjoy. The good news is that you can still eat your favorite foods, but you might need to eat smaller portions or enjoy them less often. Your health care team will help create a diabetes meal plan for you that meets your needs and likes.
The key to eating with diabetes is to eat a variety of healthy foods from all food groups, in the amounts your meal plan outlines.
The food groups are:
- Vegetables
- nonstarchy: includes broccoli, carrots, greens, peppers, and tomatoes
- starchy: includes potatoes, corn, and green peas
- Fruits—includes oranges, melon, berries, apples, bananas, and grapes
- Grains—at least half of your grains for the day should be whole grains
- includes wheat, rice, oats, cornmeal, barley, and quinoa
- examples: bread, pasta, cereal, and tortillas
- Protein
- lean meat
- chicken or turkey without the skin
- fish
- eggs
- nuts and peanuts
- dried beans and certain peas, such as chickpeas and split peas
- meat substitutes, such as tofu
- Dairy—nonfat or low fat
- milk or lactose-free milk if you have lactose intolerance
- yogurt
- cheese
- Heart-healthy fats. Eat foods with heart-healthy fats, which mainly come from these foods:
- oils that are liquid at room temperature, such as canola and olive oil
- nuts and seeds
- heart-healthy fish such as salmon, tuna, and mackerel
- avocado
Use oils when cooking food instead of butter, cream, shortening, lard, or stick margarine.
Foods and drinks to limit include:
- fried foods and other foods high in saturated fat and trans fat
- foods high in salt, also called sodium
- sweets, such as baked goods, candy, and ice cream
- beverages with added sugars, such as juice, regular soda, and regular sports or energy drinks
Drink water instead of sweetened beverages. Consider using a sugar substitute in your coffee or tea.
If you drink alcohol, drink moderately—no more than one drink a day if you’re a woman or two drinks a day if you’re a man. If you use insulin or diabetes medicines that increase the amount of insulin your body makes, alcohol can make your blood glucose level drop too low. This is especially true if you haven’t eaten in a while. It’s best to eat some food when you drink alcohol.
Low Calorie Diet on Weight Loss and the Metabolic Profile of Obese Patients with Type 2 Diabetes Mellitus
A small study 37 with 60 patients (23 males and 37 postmenopausal females) who have type 2 diabetes and are obese, to compare the effects of low calorie diet (1800 kcal/day) plus intensive insulin therapy (4 insulin injections/day) versus low calorie diet (1800 kcal/day) plus conventional insulin therapy (2/3 insulin injections/day). At 6 months post-interventions, there were significant reductions were observed in the body weight, body mass index (BMI), HbA1c for all participants and cholesterol. At 1 year, median body weight reduction was 4.5 kg for patients on low calorie diet (1800 kcal/day) plus intensive insulin therapy and 4.8 kg for those on low calorie diet (1800 kcal/day) plus conventional insulin therapy. The conclusion was a 12-month 1800-kcal low calorie dietary intervention achieved significant body weight loss and HbA1c reductions irrespectively of insulin regimen. The low calorie diet (1800 kcal/day) plus conventional insulin therapy was associated with body weight loss greater than 8.0%, whereas low calorie diet (1800 kcal/day) plus intensive insulin therapy was associated with higher rates of normoglycemia 37.
Very Low Calorie Diet in Obese Type 2 Diabetes
A small study was conducted with fifty-one obese subjects (24 with diabetes and 27 obese without diabetes) to compare weight loss and change in body composition in obese subjects with and without type 2 diabetes mellitus during a very-low-calorie diet (VLCD) program 38. After 24 weeks of intervention, there was no difference in weight loss between the 2 groups. Both groups completing the study per protocol had near-identical weight change during the program, with similar weight loss at 24 weeks (diabetes: 8.5 ± 1.3 kg vs control: 9.4 ± 1.2 kg). Change in fat mass index correlated with change in body mass index (BMI) in both groups, but change in fat mass index per unit change in BMI was less in the diabetic group compared with controls, which persisted after adjusting for age, sex, and baseline BMI. Insulin concentrations remained higher and peak β-hydroxybutyrate concentrations were lower in the diabetic compared with the control group. The conclusion was while following a 24-week very-low-calorie diet program, obese subjects with and without diabetes achieved comparable weight loss; but the decrease in body fat per unit weight loss was less in diabetic subjects. Hyperinsulinemia may have inhibited lipolysis in the diabetic group; however, further investigation into other factors is needed 38.
Low Carbohydrate Low Calorie Diet in type 2 Diabetes
In a very small study 39 comparing the effects of low carbohydrate low calorie diet (1800 kcal for men and 1600 kcal for women, distributed as 20 % carbohydrates, 30 % protein and 50 % fat) and high carbohydrate low calorie diet (1600-1800 kcal for men and 1400-1600 kcal for women, consisted of approximately 60 % carbohydrates, 15 % protein and 25 % fat) in two groups of obese patients with type 2 diabetes. The diets were tested with regard to glycaemic control and bodyweight. A group of 16 obese patients with type 2 diabetes was advised on a low-carbohydrate diet, Fifteen obese diabetes patients on a high-carbohydrate diet were control group. Positive effects on the glucose levels were seen very soon. After 6 months a marked reduction in bodyweight of patients in the low-carbohydrate diet group was observed, and this remained one year later. After 6 months the mean changes in the low-carbohydrate group and the control (high carbohydrate low calorie diet) group respectively were fasting blood glucose: -3.4 and -0.6 mmol/l; HBA1c: -1.4 % and -0.6 %; Body Weight: -11.4 kg and -1.8 kg; BMI: -4.1 kg/m2 and -0.7 kg/m2. In conclusion, a low-carbohydrate diet is an effective tool in the treatment of obese patients with type 2 diabetes 39.
- Type 2 Diabetes. https://www.cdc.gov/diabetes/basics/type2.html[↩]
- Diabetes UK. Research spotlight – low-calorie diet for Type 2 diabetes. https://www.diabetes.org.uk/Research/Research-round-up/Research-spotlight/Research-spotlight-low-calorie-liquid-diet/[↩]
- National Center for Biotechnology Information. PubMed Health. Type 2 Diabetes. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024703/[↩]
- Diabetes remission. https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/treating-your-diabetes/type2-diabetes-remission[↩][↩]
- Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, Mitri J, Pereira RF, Rawlings K, Robinson S, Saslow L, Uelmen S, Urbanski PB, Yancy WS Jr. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019 May;42(5):731-754. doi: 10.2337/dci19-0014[↩][↩]
- Westman EC, Yancy WS Jr. Using a low-carbohydrate diet to treat obesity and type 2 diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2020 Oct;27(5):255-260. doi: 10.1097/MED.0000000000000565[↩]
- Gepner Y, Shelef I, Komy O, Cohen N, Schwarzfuchs D, Bril N, Rein M, Serfaty D, Kenigsbuch S, Zelicha H, Yaskolka Meir A, Tene L, Bilitzky A, Tsaban G, Chassidim Y, Sarusy B, Ceglarek U, Thiery J, Stumvoll M, Blüher M, Stampfer MJ, Rudich A, Shai I. The beneficial effects of Mediterranean diet over low-fat diet may be mediated by decreasing hepatic fat content. J Hepatol. 2019 Aug;71(2):379-388. doi: 10.1016/j.jhep.2019.04.013[↩]
- Kirkpatrick CF, Bolick JP, Kris-Etherton PM, Sikand G, Aspry KE, Soffer DE, Willard KE, Maki KC. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J Clin Lipidol. 2019 Sep-Oct;13(5):689-711.e1. doi: 10.1016/j.jacl.2019.08.003[↩]
- Diabetes Prevention Program Outcomes Study Research Group; Orchard TJ, Temprosa M, Barrett-Connor E, Fowler SE, Goldberg RB, Mather KJ, Marcovina SM, Montez M, Ratner RE, Saudek CD, Sherif H, Watson KE. Long-term effects of the Diabetes Prevention Program interventions on cardiovascular risk factors: a report from the DPP Outcomes Study. Diabet Med. 2013 Jan;30(1):46-55. doi: 10.1111/j.1464-5491.2012.03750.x[↩][↩]
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015 Nov;3(11):866-75. doi: 10.1016/S2213-8587(15)00291-0[↩][↩][↩]
- American Diabetes Association. Standards of Medical Care in Diabetes-2017 Abridged for Primary Care Providers. Clin Diabetes. 2017 Jan;35(1):5-26. doi: 10.2337/cd16-0067[↩][↩]
- Understanding A1C. https://diabetes.org/diabetes/a1c/diagnosis[↩]
- Wing, R.R. and (2021), Does Lifestyle Intervention Improve Health of Adults with Overweight/Obesity and Type 2 Diabetes? Findings from the Look AHEAD Randomized Trial. Obesity, 29: 1246-1258. https://doi.org/10.1002/oby.23158[↩]
- Kaze AD, Santhanam P, Musani SK, Ahima R, Echouffo-Tcheugui JB. Metabolic Dyslipidemia and Cardiovascular Outcomes in Type 2 Diabetes Mellitus: Findings From the Look AHEAD Study. J Am Heart Assoc. 2021 Apr 6;10(7):e016947. doi: 10.1161/JAHA.120.016947. Epub 2021 Mar 17. Erratum in: J Am Heart Assoc. 2021 Jul 20;10(14):e020749[↩]
- Food for Thought. Key Takeaways from ADA’s Nutrition Consensus Report. https://diabetes.org/sites/default/files/2019-10/ADV_2019_Consumer_Nutrition_One%20Pager.pdf[↩]
- Altomare, R., Cacciabaudo, F., Damiano, G., Palumbo, V. D., Gioviale, M. C., Bellavia, M., Tomasello, G., & Lo Monte, A. I. (2013). The mediterranean diet: a history of health. Iranian journal of public health, 42(5), 449–457. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3684452[↩]
- Castro-Quezada, I., Román-Viñas, B., & Serra-Majem, L. (2014). The Mediterranean diet and nutritional adequacy: a review. Nutrients, 6(1), 231–248. https://doi.org/10.3390/nu6010231[↩]
- F.B. Hu. The Mediterranean Diet and mortality—olive oil and beyond. N Engl J Med, 348 (2003), pp. 2595-2596[↩]
- Sofi F., Macchi C., Abbate R., Gensini G.F., Casini A. Mediterranean diet and health. Biofactors. 2013;39:335–342. doi: 10.1002/biof.1096[↩]
- Estruch R., Ros E., Salas-Salvadó J., Covas M.I., Corella D., Arós F., Gómez-Gracia E., Ruiz-Gutiérrez V., Fiol M., Lapetra J., et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303[↩]
- Mitrou P.N., Kipnis V., Thiébaut A.C., Reedy J., Subar A.F., Wirfält E., Flood A., Mouw T., Hollenbeck A.R., Leitzmann M.F., et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH-AARP Diet and Health Study. Arch. Intern. Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461[↩]
- Couto E., Boffetta P., Lagiou P., Ferrari P., Buckland G., Overvad K., Dahm C.C., Tjønneland A., Olsen A., Clavel-Chapelon F., et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer. 2011;104:1493–1499. doi: 10.1038/bjc.2011.106[↩]
- Sofi F., Abbate R., Gensini G.F., Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010;92:1189–1196. doi: 10.3945/ajcn.2010.29673[↩]
- American Heart Association – Mediterranean Diet – http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Nutrition/Mediterranean-Diet_UCM_306004_Article.jsp[↩][↩]
- Hite, A.H., Berkowitz, V.G. and Berkowitz, K. (2011), Low-Carbohydrate Diet Review. Nutrition in Clinical Practice, 26: 300-308. https://doi.org/10.1177/0884533611405791[↩]
- Adam-Perrot, A., Clifton, P. and Brouns, F. (2006), Low-carbohydrate diets: nutritional and physiological aspects. Obesity Reviews, 7: 49-58. https://doi.org/10.1111/j.1467-789X.2006.00222.x[↩]
- Freire R. Scientific evidence of diets for weight loss: Different macronutrient composition, intermittent fasting, and popular diets. Nutrition. 2020 Jan;69:110549. doi: 10.1016/j.nut.2019.07.001[↩]
- Oh R, Gilani B, Uppaluri KR. Low Carbohydrate Diet. [Updated 2022 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537084[↩][↩]
- Trumbo P, Schlicker S, Yates AA, Poos M; Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002 Nov;102(11):1621-30. doi: 10.1016/s0002-8223(02)90346-9. Erratum in: J Am Diet Assoc. 2003 May;103(5):563.[↩]
- Ebbeling CB, Feldman HA, Klein GL, Wong JMW, Bielak L, Steltz SK, Luoto PK, Wolfe RR, Wong WW, Ludwig DS. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial. BMJ. 2018 Nov 14;363:k4583. doi: 10.1136/bmj.k4583. Erratum in: BMJ. 2020 Nov 3;371:m4264[↩][↩]
- Raynor HA, Champagne CM. Position of the Academy of Nutrition and Dietetics: Interventions for the Treatment of Overweight and Obesity in Adults. J Acad Nutr Diet. 2016 Jan;116(1):129-147. doi: 10.1016/j.jand.2015.10.031[↩]
- Shan Z, Guo Y, Hu FB, Liu L, Qi Q. Association of Low-Carbohydrate and Low-Fat Diets With Mortality Among US Adults. JAMA Intern Med. 2020 Apr 1;180(4):513-523. doi: 10.1001/jamainternmed.2019.6980[↩]
- Ebbeling CB, Swain JF, Feldman HA, Wong WW, Hachey DL, Garcia-Lago E, Ludwig DS. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA. 2012 Jun 27;307(24):2627-34. doi: 10.1001/jama.2012.6607[↩]
- Hall KD, Bemis T, Brychta R, Chen KY, Courville A, Crayner EJ, Goodwin S, Guo J, Howard L, Knuth ND, Miller BV 3rd, Prado CM, Siervo M, Skarulis MC, Walter M, Walter PJ, Yannai L. Calorie for Calorie, Dietary Fat Restriction Results in More Body Fat Loss than Carbohydrate Restriction in People with Obesity. Cell Metab. 2015 Sep 1;22(3):427-36. doi: 10.1016/j.cmet.2015.07.021[↩]
- Duyff RL. Carbs: Sugars, starches, and fiber. In: Academy of Nutrition and Dietetics Complete Food and Nutrition Guide. 5th ed. Houghton Mifflin Harcourt; 2017.[↩]
- 2015-2020 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines[↩]
- Adv Ther. 2016 Mar;33(3):447-59. doi: 10.1007/s12325-016-0300-2. Epub 2016 Feb 17. Obese Patients with Type 2 Diabetes on Conventional Versus Intensive Insulin Therapy: Efficacy of Low-Calorie Dietary Intervention. https://www.ncbi.nlm.nih.gov/pubmed/26886777[↩][↩]
- Metabolism. 2012 Jun;61(6):873-82. doi: 10.1016/j.metabol.2011.10.017. Epub 2011 Dec 5. Less fat reduction per unit weight loss in type 2 diabetic compared with nondiabetic obese individuals completing a very-low-calorie diet program. https://www.ncbi.nlm.nih.gov/pubmed/22146094?dopt=Abstract[↩][↩]
- Ups J Med Sci. 2005;110(1):69-73. Lasting improvement of hyperglycaemia and bodyweight: low-carbohydrate diet in type 2 diabetes–a brief report. https://www.ncbi.nlm.nih.gov/pubmed/15801687?dopt=Abstract[↩][↩]