Contents
- What Is Vascular Dementia ?
- Types of vascular dementia
- Multi-infarct dementia
- Causes of Multi-infarct dementia
- Symptoms of multi-infarct dementia
- The early symptoms of dementia can include:
- Exams and Tests for multi-infarct dementia
- Treatment for multi-infarct dementia
- Medications
- Outlook (Prognosis) of multi-infarct dementia
- Possible Complications of multi-infarct dementia
- Prevention of multi-infarct dementia
- Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
- Subcortical vascular dementia, also called Binswanger’s disease
- Symptoms of vascular dementia
- Causes of vascular dementia
- How to reduce your risk of getting vascular dementia
- Tests for vascular dementia
- Treatments for vascular dementia
- Vascular Dementia Life Expectancy
- What Is Mixed Dementia ?
- What is a Stroke ?
- Care plans
- Looking after someone with dementia
- Staying independent with dementia
- Working when you have dementia
- Driving
- Assistive technology for people with dementia
- Helping someone with dementia with everyday tasks
- Keeping up hobbies and interests when someone has dementia
- Maintaining good health and nutrition in someone with dementia
- Dealing with incontinence in someone with dementia
- Helping someone with dementia with their personal hygiene
- Safety when washing or bathing
- Continence services
- Helping someone with dementia sleep well
- Carers’ breaks and respite care
- Multi-infarct dementia
- Types of vascular dementia
What Is Vascular Dementia ?
Vascular dementia, considered the second most common form of dementia after Alzheimer’s disease. A growing number of experts prefer the term “vascular cognitive impairment” to “vascular dementia” because they feel it better expresses the concept that vascular thinking changes can range from mild to severe 1 and vascular cognitive impairment result from injuries to the vessels supplying blood to the brain, often after a stroke or series of strokes 2. Vascular dementia and vascular cognitive impairment arise as a result of risk factors that similarly increase the risk for cerebrovascular disease (such as stroke), including atrial fibrillation, hypertension (high blood pressure), diabetes, and high cholesterol. The symptoms of vascular dementia can be similar to those of Alzheimer’s disease and both conditions can occur at the same time (a condition called “mixed dementia”). Symptoms of vascular dementia can begin suddenly and worsen or improve during one’s lifetime.
This type of dementia is often managed with drugs to prevent strokes. The aim is to reduce the risk of additional brain damage. Some studies suggest that drugs that improve memory in Alzheimer’s disease might benefit people with early vascular dementia. Interventions that address risk factors may be incorporated into the management of vascular dementia.
Types of vascular dementia
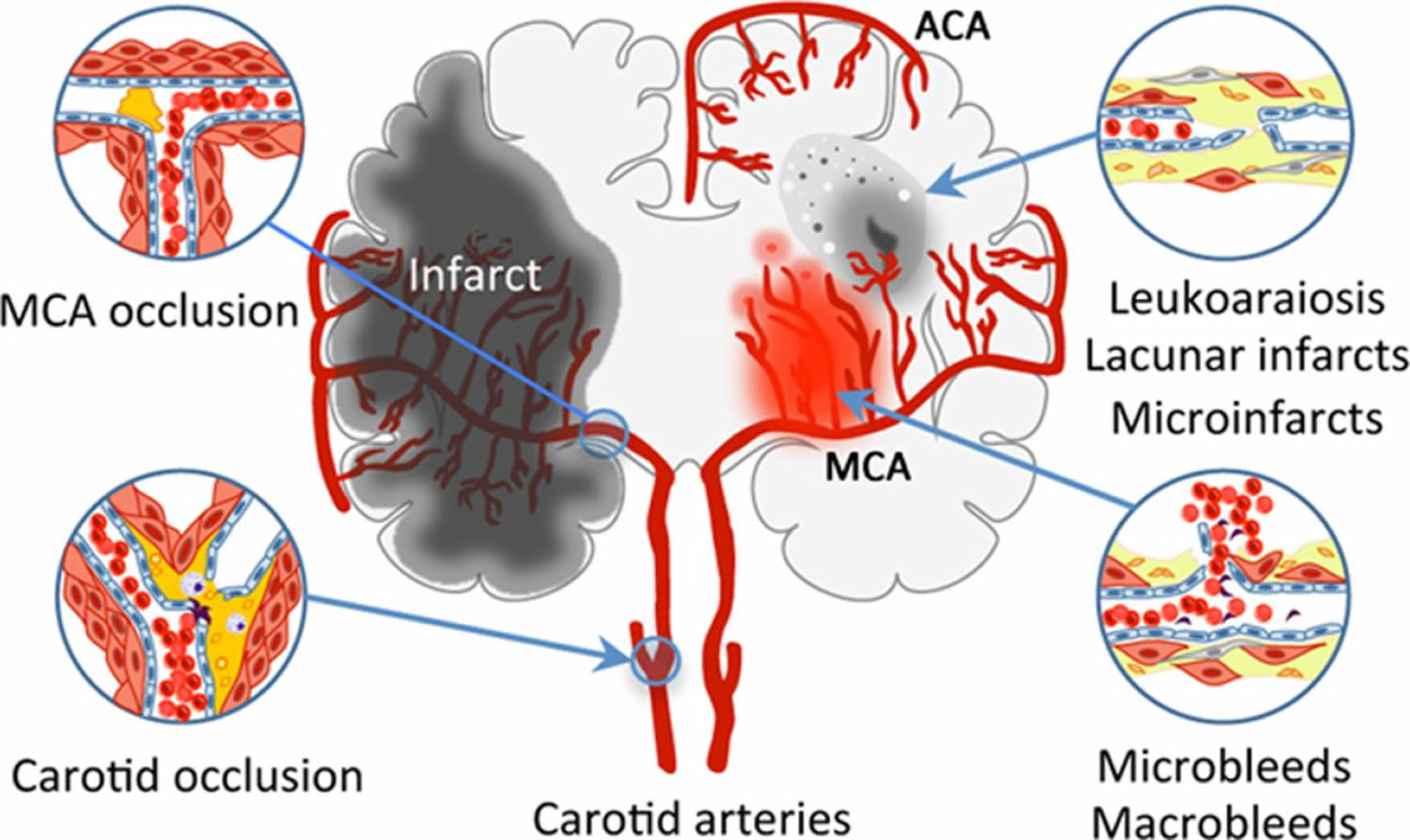
Multi-infarct dementia
This type of dementia occurs when a person has had many small strokes that damage brain cells. One side of the body may be disproportionally affected, and multi-infarct dementia may impair language or other functions, depending on the region of the brain that is affected. In classic multi-infarct dementia, the cognitive deterioration is stepwise rather than smoothly progressive 3. The cognitive changes vary, but memory loss is usually much less prominent than in Alzheimer’s disease. With each event (stroke) the patient suddenly worsens but then improves either completely or partially. As the disease progresses, the patient develops an accretion of abnormal neurologic signs such as asymmetric reflexes, pseudobulbar changes (i.e. swallowing and speech difficulties along with emotional lability), pathologic reflexes (e.g. Babinski signs), and sensory abnormalities. This condition is usually seen in hypertensive individuals and is caused by multiple small infarcts in the white matter of the brain as well as the basal ganglia and cortex. A variant of multi-infarct dementia is Binswanger subcortical arteriosclerotic encephalopathy (also called subcortical vascular dementia) in which the disease is confined to the white matter of the brain hemispheres and is usually reported as a fairly rapidly progressing dementia with significant neurologic and cognitive changes.
When the strokes occur on both sides of the brain, dementia is more likely than when stroke occurs on one side of the brain. In some cases, a single stroke can damage the brain enough to cause dementia. This so-called single-infarct dementia is more common when stroke affects the left side of the brain—where speech centers are located—and/or when it involves the hippocampus, the part of the brain that is vital for memory.
Causes of Multi-infarct dementia
Multi-infarct dementia is the second most common cause of dementia (after Alzheimer’s disease) in people over age 65 4. Multi-infarct dementia affects men more often than women. The disorder usually affects people between ages 55 and 75 4.
Multi-infarct dementia is caused by a series of small strokes.
A stroke is an interruption in or blockage of the blood supply to any part of the brain. A stroke is sometimes called an infarct. “Multi-infarct” means that many areas in the brain have been injured due to a lack of blood.
If blood flow is stopped for longer than a few seconds, the brain cannot get oxygen. Brain cells can die, causing permanent damage.
When these strokes affect a small area, there may be no symptoms of a stroke. These are often called silent strokes. Over time, as more areas of the brain are damaged, the symptoms of multi-infarct dementia begin to appear.
Not all strokes need to be “silent.” Larger strokes that have clear affects on strength, sensation, or other brain and nervous system (neurologic) function also can lead to multi-infarct dementia.
Risk factors for multi-infarct dementia include a history of:
- Diabetes
- Hardening of the arteries (atherosclerosis)
- High blood pressure (hypertension)
- Smoking
- Stroke
See also: Stroke risk factors and prevention
Symptoms of dementia in any one person may be caused by either Alzheimer’s disease or multi-infarct dementia. The symptoms for each problem are very similar, and multi-infarct dementia may be a risk factor for Alzheimer’s disease.
Symptoms of multi-infarct dementia
Symptoms may develop gradually or may progress after each small stroke.
The symptoms of the disorder may begin suddenly after each stroke. Some people with multi-infarct dementia may appear to improve for short periods of time, then decline after having more silent strokes.
The early symptoms of dementia can include:
- Difficulty performing tasks that used to come easily, such as balancing a checkbook, playing games (such as bridge), and learning new information or routines
- Getting lost on familiar routes
- Language problems, such as trouble finding the name of familiar objects
- Losing interest in things you previously enjoyed, flat mood
- Misplacing items
- Personality changes and loss of social skills.
As the dementia becomes worse, symptoms are more obvious and interfere with the ability to take care of yourself. The symptoms may include:
- Change in sleep patterns, often waking up at night
- Difficulty doing basic tasks, such as preparing meals, choosing proper clothing, or driving
- Forgetting details about current events
- Forgetting events in your own life history, losing awareness of who you are
- Having delusions, depression, or agitation
- Having hallucinations, arguments, striking out, or violent behavior
- Having more difficulty reading or writing
- Having poor judgment and loss of ability to recognize danger
- Using the wrong word, not pronouncing words correctly, or speaking in confusing sentences
- Withdrawing from social contact
Any of the neurologic problems that occur with a stroke may also be present.
Exams and Tests for multi-infarct dementia
Tests may be ordered to help determine whether other medical problems could be causing dementia or making it worse, such as:
- Anemia
- Brain tumor
- Chronic infection
- Drug and medication intoxication
- Severe depression
- Thyroid disease
- Vitamin deficiency
Neuropsychological testing is often helpful to find out what parts of thinking have been affected, and to guide other tests.
Tests that can show evidence of previous strokes in the brain may include:
- Head CT scan
- MRI of the brain
Treatment for multi-infarct dementia
There is no treatment to turn back damage to the brain caused by small strokes.
An important goal is to control symptoms and correct risk factors such as high blood pressure, smoking, and high cholesterol to prevent future strokes.
- Avoid fatty foods. Follow a healthy, low-fat diet.
- Do not drink more than 1 – 2 alcoholic drinks a day.
- Keep blood pressure less than 130/80 mm/Hg (ask your doctor what your blood pressure reading should be).
- Keep LDL “bad” cholesterol lower than 70 mg/dL.
- Quit smoking.
- Your doctor may suggest taking aspirin or another drug called clopidogrel (Plavix) to help prevent blood clots from forming in the arteries. These medicines are called antiplatelet drugs. DO NOT take aspirin without talking to your doctor first.
The goals of helping someone with dementia in the home environment are to:
- Manage behavior problems, confusion, sleep problems, and agitation
- Modify the home environment
- Support family members and other caregivers
- Hearing aids, glasses, or cataract surgery may be needed if the person has sensory problems.
See home care plan for information about taking care of a loved one with dementia.
Medications
Medications may be needed to control aggressive, agitated, or dangerous behaviors. The health care provider will usually prescribe these medicines in very low doses and adjust the dose as needed. Such medications may include:
- Antipsychotics (olanzapine, quetiapine)
- Serotonin-affecting drugs (trazodone, buspirone, or fluoxetine)
Medications used to treat Alzheimer’s disease have not been shown to work for multi-infarct dementia.
Outlook (Prognosis) of multi-infarct dementia
Some improvement may occur for short periods of time, but the disorder will generally get worse over time.
Possible Complications of multi-infarct dementia
Complications include the following:
- Future strokes
- Heart disease
- Loss of ability to function or care for self
- Loss of ability to interact
- Pneumonia, urinary tract infections, skin infections
- Pressure sores
Prevention of multi-infarct dementia
Control conditions that increase the risk of hardening of the arteries (atherosclerosis) by:
- Controlling high blood pressure
- Controlling weight
- Reducing saturated fats and salt in the diet
- Treating related disorders.
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
This inherited form of cardiovascular disease results in a thickening of the walls of small- and medium-sized blood vessels, eventually stemming the flow of blood to the brain. The muscle cells surrounding these blood vessels (vascular smooth muscle cells) are abnormal and gradually die 5. In the brain, the resulting blood vessel damage (arteriopathy) can cause migraines, often with visual sensations or auras, or recurrent seizures (epilepsy).
CADASIL is likely a rare condition; however, its prevalence is unknown 5.
In individuals with CADASIL, a stroke can occur at any time from childhood to late adulthood, but typically happens during mid-adulthood (U.S. National Library of Medicine. Genetics Home Reference. cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. https://ghr.nlm.nih.gov/condition/cerebral-autosomal-dominant-arteriopathy-with-subcortical-infarcts-and-leukoencephalopathy)). People with CADASIL often have more than one stroke in their lifetime. Recurrent strokes can damage the brain over time. Strokes that occur in the subcortical region of the brain, which is involved in reasoning and memory, can cause progressive loss of intellectual function (dementia) and changes in mood and personality.
Many people with CADASIL also develop leukoencephalopathy, which is a change in a type of brain tissue called white matter that can be seen with magnetic resonance imaging (MRI) (U.S. National Library of Medicine. Genetics Home Reference. cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. https://ghr.nlm.nih.gov/condition/cerebral-autosomal-dominant-arteriopathy-with-subcortical-infarcts-and-leukoencephalopathy)).
The age at which the signs and symptoms of CADASIL first begin varies greatly among affected individuals, as does the severity of these features (U.S. National Library of Medicine. Genetics Home Reference. cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. https://ghr.nlm.nih.gov/condition/cerebral-autosomal-dominant-arteriopathy-with-subcortical-infarcts-and-leukoencephalopathy)).
CADASIL is not associated with the common risk factors for stroke and heart attack, such as high blood pressure and high cholesterol, although some affected individuals might also have these health problems (U.S. National Library of Medicine. Genetics Home Reference. cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. https://ghr.nlm.nih.gov/condition/cerebral-autosomal-dominant-arteriopathy-with-subcortical-infarcts-and-leukoencephalopathy)).
CADASIL is associated with mutations of a gene called Notch3. CADASIL is associated with multi-infarct dementia, stroke, migraine with aura (migraine preceded by visual symptoms), and mood disorders. The first symptoms can appear in people between ages 20 and 40. Many people with CADASIL are undiagnosed. People with first-degree relatives who have CADASIL can be tested for genetic mutations to the Notch3 gene to determine their own risk of developing CADASIL.
Subcortical vascular dementia, also called Binswanger’s disease
Binswanger’s disease, also called subcortical vascular dementia, is a rare type of dementia caused by widespread, microscopic areas of damage to the deep layers of white matter in the brain 6. The damage is the result of the thickening and narrowing (atherosclerosis) of arteries that feed the subcortical areas of the brain. Atherosclerosis (commonly known as “hardening of the arteries”) is a systemic process that affects blood vessels throughout the body. It begins late in the fourth decade of life and increases in severity with age. As the arteries become more and more narrowed, the blood supplied by those arteries decreases and brain tissue dies. A characteristic pattern of Binswanger’s disease-damaged brain tissue can be seen with modern brain imaging techniques such as CT scans or magnetic resonance imaging (MRI). The symptoms associated with Binswanger’s disease are related to the disruption of subcortical neural circuits that control what neuroscientists call executive cognitive functioning: short-term memory, organization, mood, the regulation of attention, the ability to act or make decisions, and appropriate behavior. The most characteristic feature of Binswanger’s disease is psychomotor slowness – an increase in the length of time it takes, for example, for the fingers to turn the thought of a letter into the shape of a letter on a piece of paper. Other symptoms include forgetfulness (but not as severe as the forgetfulness of Alzheimer’s disease), changes in speech, an unsteady gait, clumsiness or frequent falls, changes in personality or mood (most likely in the form of apathy, irritability, and depression), and urinary symptoms that aren’t caused by urological disease. Brain imaging, which reveals the characteristic brain lesions of Binswanger’s disease, is essential for a positive diagnosis.
The symptoms of Binswanger’s disease are related to the disruption of subcortical neural circuits involving short-term memory, organization, mood, attention, decision making, and appropriate behavior. A characteristic feature of this disease is psychomotor slowness, such as an increase in the time it takes for a person to think of a letter and then write it on a piece of paper.
Treatment of Binswanger’s disease
There is no specific course of treatment for Binswanger’s disease. Treatment is symptomatic. People with depression or anxiety may require antidepressant medications such as the serotonin-specific reuptake inhibitors (SSRI) sertraline or citalopram. Atypical antipsychotic drugs, such as risperidone and olanzapine, can be useful in individuals with agitation and disruptive behavior. Recent drug trials with the drug memantine have shown improved cognition and stabilization of global functioning and behavior. The successful management of hypertension and diabetes can slow the progression of atherosclerosis, and subsequently slow the progress of Binswanger’s disease. Because there is no cure, the best treatment is preventive, early in the adult years, by controlling risk factors such as hypertension, diabetes, and smoking.
Prognosis for Binswanger’s disease
Binswanger’s disease is a progressive disease; there is no cure. Changes may be sudden or gradual and then progress in a stepwise manner. Binswanger’s disease can often coexist with Alzheimer’s disease. Behaviors that slow the progression of high blood pressure, diabetes, and atherosclerosis — such as eating a healthy diet and keeping healthy wake/sleep schedules, exercising, and not smoking or drinking too much alcohol — can also slow the progression of Binswanger’s disease.
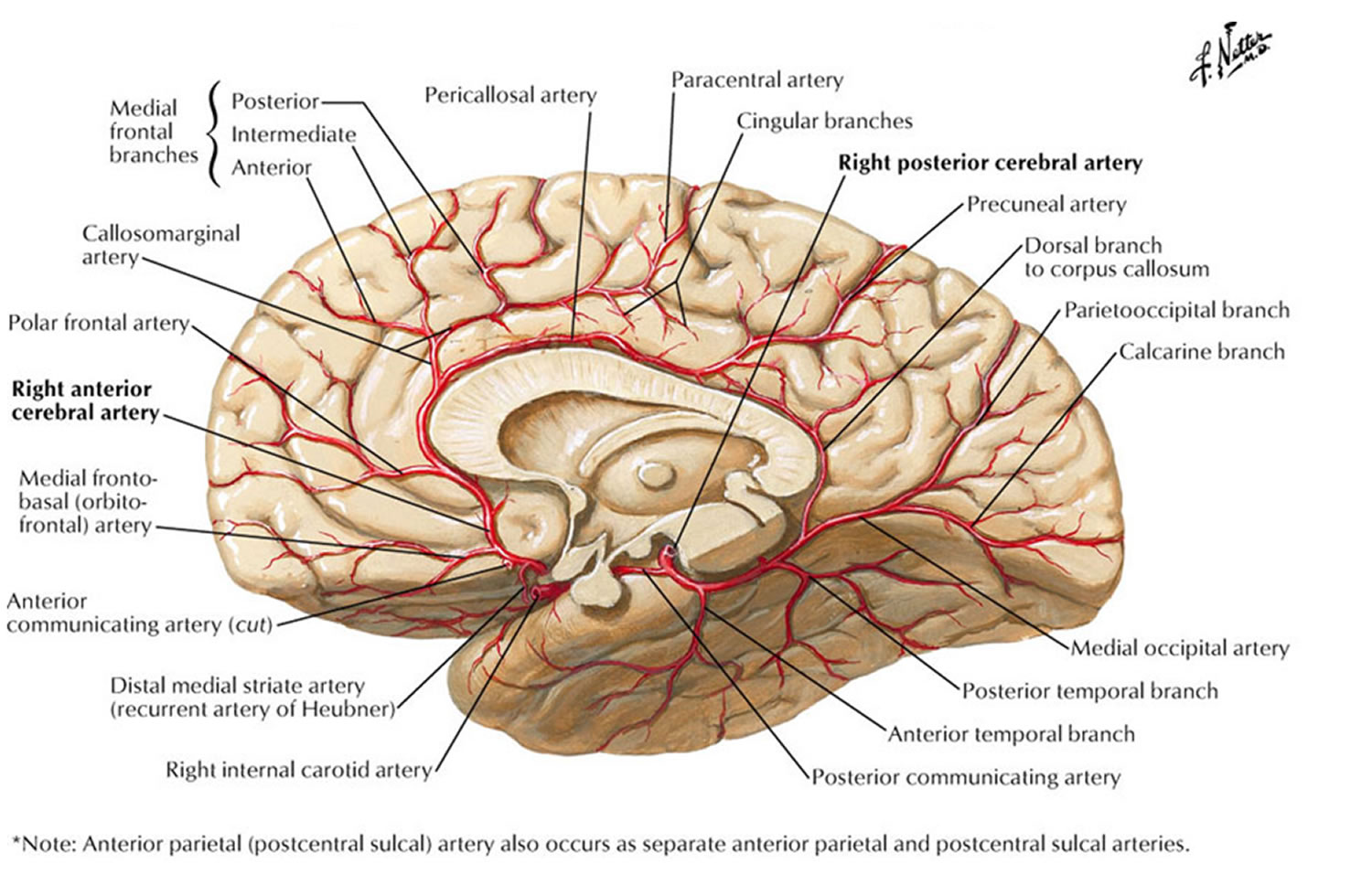
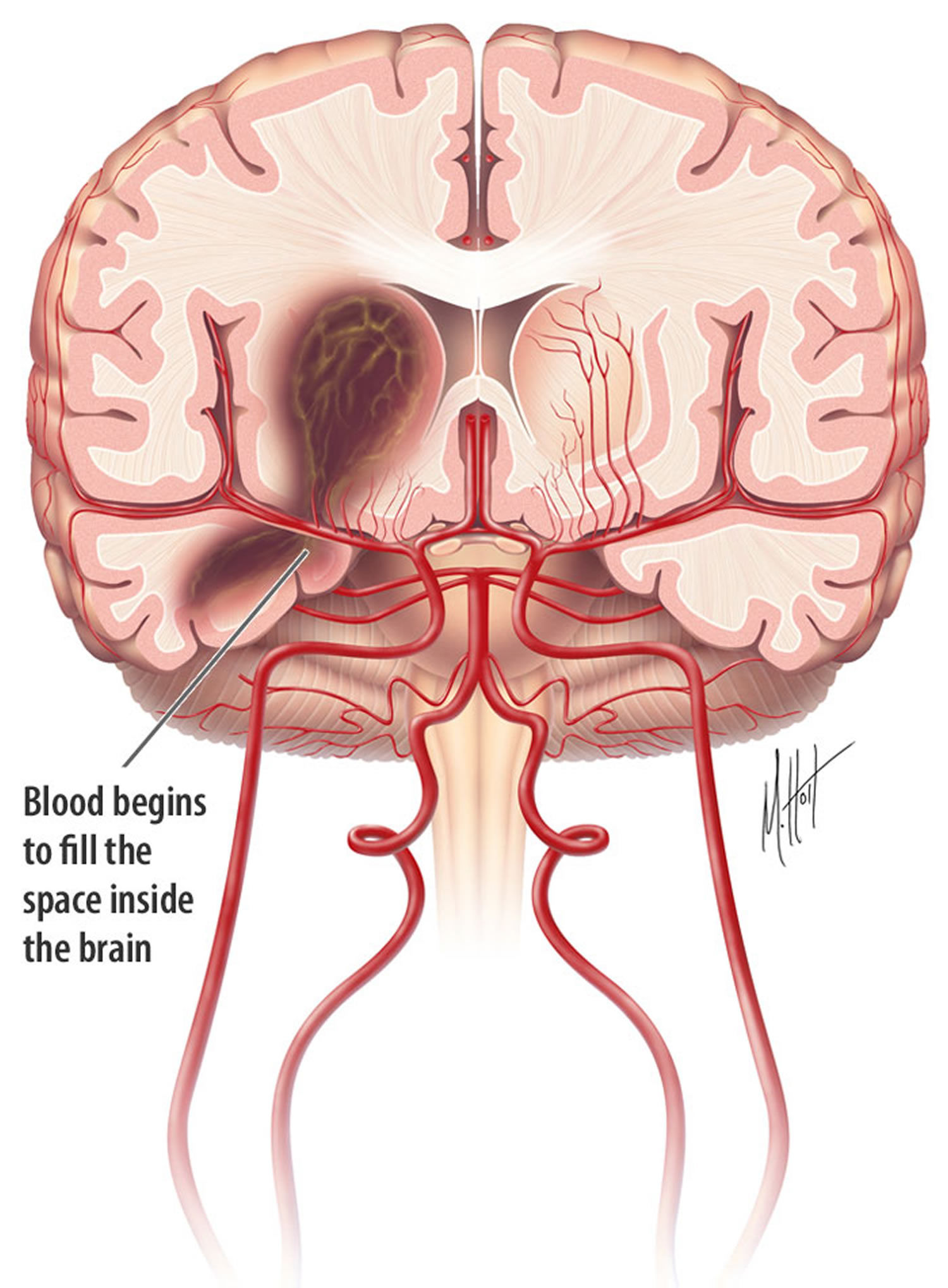
Figure 1. Brain Blood Supply (Vascular Anatomy) – looking through a brain sliced in the center
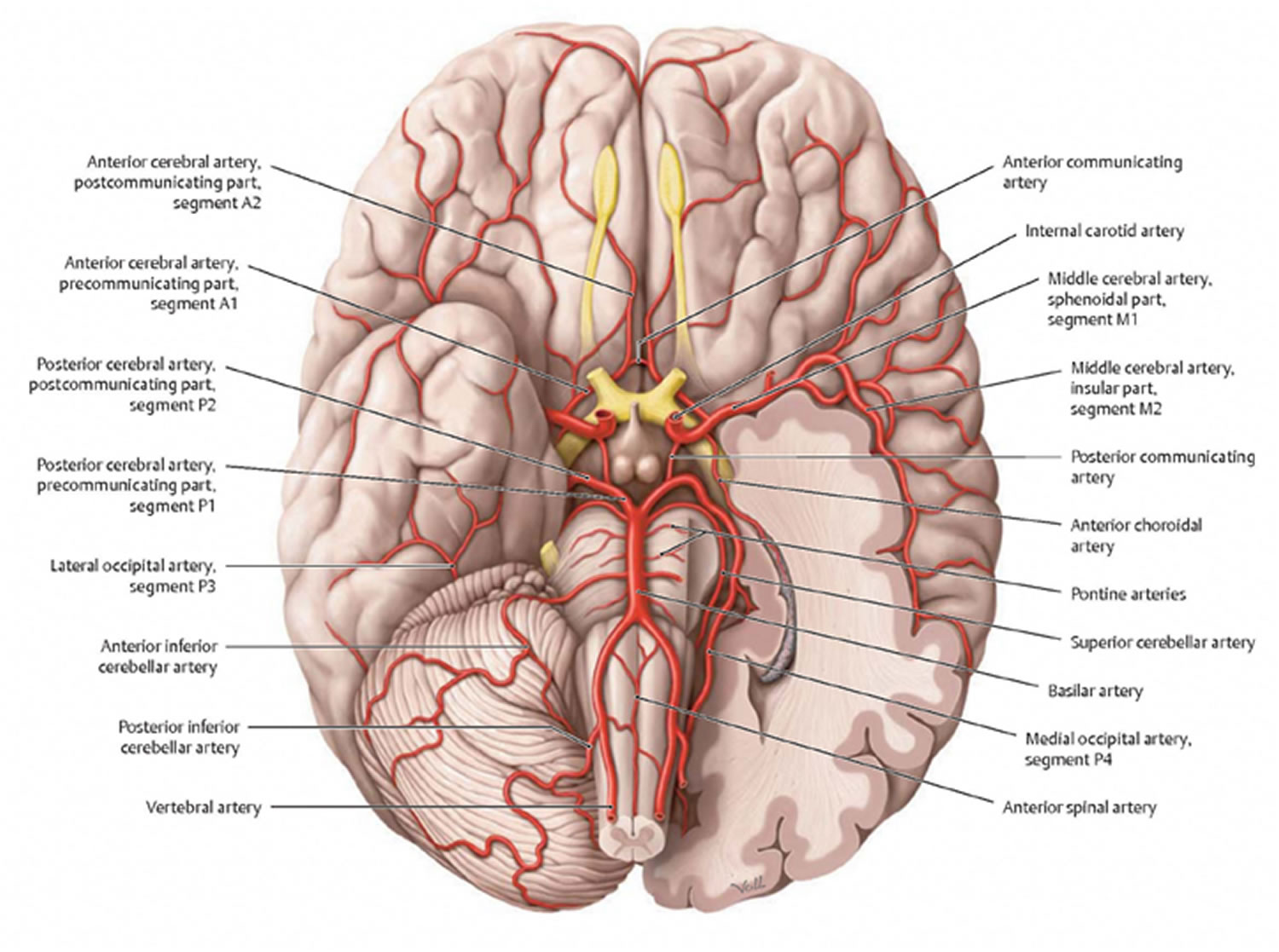
Figure 2. Brain Blood Supply (Vascular Anatomy) – looking from the base of the brain up
Symptoms of vascular dementia
Vascular dementia can start suddenly or come on slowly over time.
These problems can make daily activities increasingly difficult and someone with the condition may eventually be unable to look after themselves.
Early symptoms of vascular dementia
Early signs of vascular dementia can include mild:
- slowness of thought
- difficulty with planning
- trouble with understanding
- problems with concentration
- mood or behavioral changes
- problems with memory and language (but these aren’t as common as they are in people with Alzheimer’s disease)
As this point, these problems may be barely noticeable or mistaken for something else, such as depression. But they indicate some brain damage has occurred and that treatment is needed.
Later symptoms of vascular dementia
The symptoms often continue to get worse over time. This may happen slowly, or in sudden steps every few months or years.
The symptoms depend on the part of the brain that’s affected, but can include:
- significant slowness of thought
- feeling disorientated and confused
- memory loss and difficulty concentrating
- difficulty finding the right words
- severe personality changes, such as becoming aggressive
- depression, mood swings and lack of interest or enthusiasm
- finding it difficult to walk and keep balance, with frequent falls
- loss of bladder control (incontinence)
- increasing difficulty with daily activities
Some people also have some symptoms of Alzheimer’s disease.
If it’s spotted at an early stage, treatment may be able to stop the vascular dementia getting worse, or at least slow it down.
If you’re worried about someone else, encourage them to make an appointment with their doctor and perhaps suggest that you go with them.
Symptoms of dementia can have several causes. Your medical practitioner can do some simple checks to try to find out the cause and may refer you to a specialist for further tests.
Causes of vascular dementia
Vascular dementia is caused by reduced blood flow to the brain, which damages and eventually kills the brain cells.
This is usually due to:
- narrowing of the small blood vessels deep inside the brain – known as subcortical vascular dementia or small vessel disease.
- a stroke (where the blood supply to part of the brain is suddenly cut off, usually as the result of a blood clot) – called post-stroke dementia or single-infarct dementia.
- lots of “mini strokes” that cause tiny but widespread damage to the brain – known as multi-infarct dementia.
Some people with vascular dementia also have brain damage caused by Alzheimer’s disease. This is known as mixed dementia.
Things that can increase your chances of getting vascular dementia in later life include:
- high blood pressure (hypertension)
- smoking
- an unhealthy diet
- high blood cholesterol
- lack of exercise
- being overweight or obese
- diabetes
- excessive alcohol consumption
- atrial fibrillation (a type of irregular heartbeat) and other types of heart disease
These problems increase the risk of damage to the blood vessels in and around the brain, or cause blood clots to develop inside them.
How to reduce your risk of getting vascular dementia
By making healthy lifestyle changes – such as stopping smoking, lose excess body weight and exercising regularly – and treating any health conditions you have, you may be able to reduce your risk of vascular dementia. Tackling these might reduce your risk of vascular dementia in later life, although it’s not yet clear exactly how much your risk of dementia can be reduced.
This may also help slow down or stop the progression of vascular dementia if you’re diagnosed in the early stages. See treating vascular dementia for more information.
But there are some things you can’t change that can increase your risk of vascular dementia, such as:
- your age – the risk of vascular dementia increases as you get older, with people over 65 most at risk
- your family history – your risk of problems such as strokes is higher if a close family member has had them
- your ethnicity – if you have a south Asian, African or Caribbean background, your risk of vascular dementia is higher, as related problems such as diabetes and high blood pressure are more common in these groups
In rare cases, unavoidable genetic conditions can also increase your risk of vascular dementia.
Tests for vascular dementia
There’s no single test for vascular dementia.
The following are needed to make a diagnosis:
- an assessment of symptoms – for example, whether there are typical symptoms of vascular dementia
- a full medical history, including asking about a history of conditions related to vascular dementia, such as strokes or high blood pressure
- an assessment of mental abilities –this will usually involve a number of tasks and questions
- a brain scan, such as an MRI scan, CT scan or a single photon-emission computed tomography (SPECT) scan – this can detect signs of dementia and damage to the blood vessels in the brain.
- Transcranial Doppler – transcranial doppler sonography studies can now provide valuable information on cerebrovascular resistance, cerebrovascular reserve, and cerebral perfusion 7. Vascular resistance is calculated from the pulsative index (systolic/diastolic ratio); increased pulsative index indicates increased cerebrovascular resistance. Cerebrovascular reserve is calculated from the response of the cerebral vessels to a vasodilatory challenge either with CO2 elevation, as tested by breath holding, or with acetazolamide injection 8. Cerebral perfusion is assessed as a velocity measure of the individual vessels. Patients with vascular dementia secondary to small vessel disease have a significant increase in vascular resistance and a decrease in vascular reserve. In Alzheimer’s disease, vascular resistance and reserve are normal, and there is a decrease in perfusion through the middle cerebral artery secondary to the atrophic brain tissue that it supplies. Therefore, Doppler studies can be very helpful in sorting out the vascular factors and establishing the diagnosis in dementia patients with abnormal MRIs and a history compatible with cerebrovascular disease.
Treatments for vascular dementia
Treatment can help prevent further damage to the brain in people with vascular dementia and may slow down its progression.
But there’s currently no cure for the condition or a way to reverse the damage that’s already occurred.
Vascular Dementia Life Expectancy
Vascular dementia will usually get worse over time. This can happen in sudden steps, with periods in between where the symptoms don’t change much, but it’s difficult to predict when this will happen.
Home-based help will usually be needed, and some people will eventually need care in a nursing home.
Although treatment can help, vascular dementia can significantly shorten life expectancy. But this is highly variable and many people live for a number of years with the condition or die from some other cause.
What Is Mixed Dementia ?
It is common for people to have mixed dementia—a combination of two or more disorders, at least one of which is dementia 9. A number of combinations are possible. For example, some people have both Alzheimer’s disease and vascular dementia.
Some studies indicate that mixed dementia is the most common cause of dementia in the elderly. For example, autopsy studies looking at the brains of people who had dementia indicate that most people age 80 and older had mixed dementia—a combination of brain changes related to Alzheimer’s disease (amyloid and tau), cerebrovascular disease (such as stroke), and, in some instances, Lewy body dementia (Lewy bodies). These studies suggest that mixed dementia is caused by both Alzheimer’s-related neurodegenerative processes and vascular disease-related processes.
In a person with mixed dementia, it may not be clear exactly how many of a person’s symptoms are due to Alzheimer’s disease or another type of dementia. In one study, approximately 40 percent of people who were thought to have Alzheimer’s disease were found after autopsy to also have some form of cerebrovascular disease. In addition, several studies have found that many of the major risk factors for vascular disease also may be risk factors for Alzheimer’s disease.
Researchers are still working to understand how underlying disease processes in mixed dementia influence each other. It is not clear, for example, if symptoms are likely to be worse when a person has brain changes reflecting multiple types of dementia. Nor do we know if a person with multiple dementias can benefit from treating one type, for example, when a person with Alzheimer’s disease controls high blood pressure and other vascular disease risk factors.
What is a Stroke ?
A stroke is a medical emergency. Strokes happen when blood flow to your brain stops. Within minutes, brain cells begin to die 10. A stroke is also called cerebrovascular accident (CVA) or brain attack. There are two types – ischemic and hemorrhagic. Hemorrhagic stroke is the less common type ~ 13% 11. It happens when a blood vessel breaks and bleeds into the brain. Within minutes, brain cells begin to die. Causes include a bleeding aneurysm, an arteriovenous malformation (AVM), or an artery wall that breaks open.
Stroke can affect people of all ages, including children. Many people with ischemic strokes are older (60 or more years old), and the risk of stroke increases with age 12. Each year, about 55,000 more women than men have a stroke, and it is more common among African-Americans than members of other ethnic groups 12. Many people with stroke have other problems or conditions which put them at higher risk for stroke, such as high blood pressure (hypertension), heart disease, smoking, or diabetes.
In the United States, approximately 750,000 strokes occur each year 13. During a stroke, one or more areas of the brain can be damaged. Depending upon the area affected, a person may lose the ability to move one side of the body, the ability to speak, or a number of other functions. The damage may be temporary or permanent, and the function may be partially or completely lost. A person’s long term outcome depends upon how much brain is damaged, how quickly treatment begins, and a number of other factors.
Strokes are a leading cause of long-lasting injury, disability, and death. Early treatment and preventive measures can reduce the brain damage that occurs as a result of a stroke. The treatment of a stroke depends upon the type of stroke (eg, ischemic or hemorrhagic), the time since the first stroke symptoms occurred, and the patient’s underlying medical problems. General information about the treatment of hemorrhagic strokes is provided here.
Symptoms of stroke are
- Sudden numbness or weakness of the face, arm or leg (especially on one side of the body)
- Sudden confusion, trouble speaking or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden severe headache with no known cause
It is important to treat strokes as quickly as possible. With a hemorrhagic stroke, the first steps are to find the cause of bleeding in the brain and then control it. Surgery may be needed. In the case of ischemic stroke, blood thinners may be used to stop a stroke while it is happening by quickly dissolving the blood clot. Post-stroke rehabilitation can help people overcome disabilities caused by stroke damage.
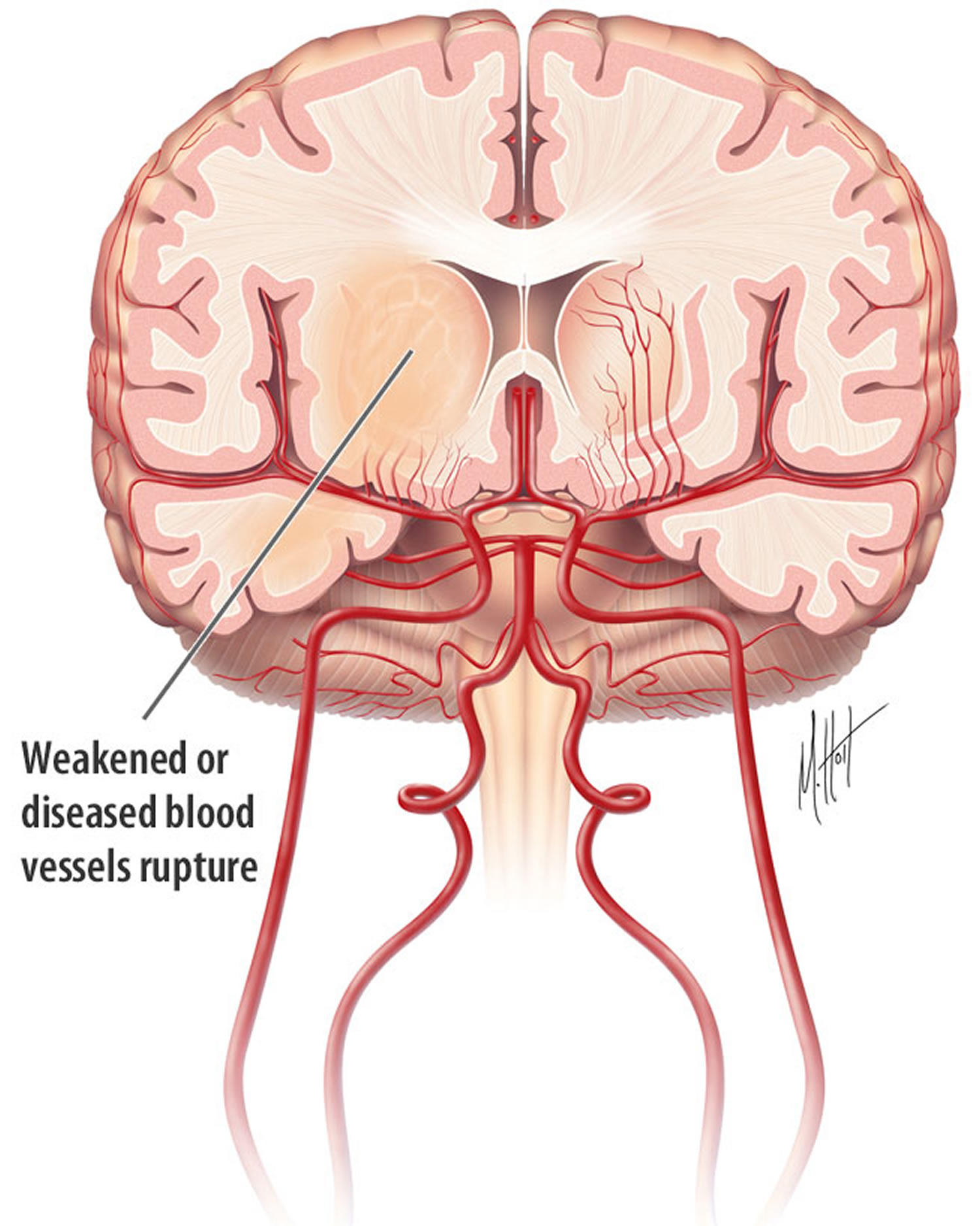
What is Hemorrhagic Stroke (13 percent of strokes)
Hemorrhage is the medical term for bleeding. Hemorrhagic stroke occurs when blood vessels in the brain leak or rupture, causing bleeding in or around the brain. About 13 percent of strokes are hemorrhagic strokes. Damage can occur quickly due to the pressure of increasing amounts of blood or because of the blood itself. Blood is irritating to the brain tissue, causing it to swell. Blood collects in the brain tissue is toxic for the brain tissue causing the cells in that area to weaken and die 11.
Bleeding around the brain is referred to as subarachnoid hemorrhage (SAH) and is often caused by rupture of an abnormal blood vessel (aneurysm) on the surface of the brain. Bleeding into the brain is called intracerebral hemorrhage (ICH) and is often caused by high blood pressure.
2 types hemorrhagic strokes
There are two kinds of hemorrhagic stroke. In both, a blood vessel ruptures, disrupting blood flow to part of the brain.
1. Intracerebral hemorrhages or ICH (most common type of hemorrhagic stroke):
- Occur when a blood vessel bleeds or ruptures into the tissue deep within the brain.
- Are most often caused by chronically high blood pressure or aging blood vessels.
- Are sometimes caused by an arteriovenous malformation (AVM). An AVM is a cluster of abnormally formed blood vessels. Any one of these vessels can rupture, also causing bleeding into the brain.
Intracerebral hemorrhage occurs when a diseased blood vessel within the brain bursts, allowing blood to leak inside the brain 11. (The name means within the cerebrum or brain). The sudden increase in pressure within the brain can cause damage to the brain cells surrounding the blood. If the amount of blood increases rapidly, the sudden buildup in pressure can lead to unconsciousness or death. Intracerebral hemorrhage usually occurs in selected parts of the brain, including the basal ganglia, cerebellum, brain stem, or cortex.
The most common cause of intracerebral hemorrhage is high blood pressure (hypertension) 11. Since high blood pressure by itself often causes no symptoms, many people with intracranial hemorrhage are not aware that they have high blood pressure, or that it needs to be treated. Less common causes of intracerebral hemorrhage include trauma, infections, tumors, blood clotting deficiencies, and abnormalities in blood vessels (such as arteriovenous malformations).
How are hemorrhagic strokes diagnosed ?
When someone has shown symptoms of a stroke or a transient ischemic attack (TIA), a doctor will gather information and make a diagnosis. He or she will review the events that have occurred and will:
- get a medical history
- do a physical and neurological examination
- have certain laboratory (blood) tests done
- get a CT or MRI scan of the brain
- study the results of other diagnostic tests that might be needed
Diagnostic tests examine how the brain looks, works and gets its blood supply. They can outline the injured brain area. Diagnostic tests fall into three categories.
- Imaging tests give a picture of the brain similar to X-rays.
- Electrical tests record the electrical impulses of the brain, also called an EEG.
- Blood flow tests show any problem that may cause changes in blood flow to the brain.
How are hemorrhagic strokes treated ?
Because hemorrhages may be life-threatening, hospital care is required. Medication is used to control high blood pressure. Other medicine may be given to reduce the brain swelling that follows a stroke.
Surgery may be needed depending on the cause and type of the hemorrhage. Surgery is often recommended to either place a metal clip at the base of an aneurysm or to remove the abnormal vessels that make up an arteriovenous malformation.
Some procedures are less invasive and use of a catheter that goes in through a major artery in the leg or arm. The catheter is guided to the aneurysm or arteriovenous malformation where it places a device, such as a coil, to prevent rupture.
Figure 3. Intracerebral hemorrhage
2. Subarachnoid hemorrhage (SAH):
Subarachnoid hemorrhage occurs when a blood vessel just outside the brain ruptures 14. The area of the skull surrounding the brain (the subarachnoid space) rapidly fills with blood. A patient with subarachnoid hemorrhage may have a sudden severe or intense headache, neck pain or worse near the back of the head, and nausea or vomiting. Sometimes this is described as the worst headache ever (often called thunderclap headache) 15. The headache may start after a popping or snapping feeling in the head. The sudden buildup of pressure outside the brain may also cause rapid loss of consciousness or death.
Subarachnoid hemorrhage can occur at any age, including in teenagers and young adults and is slightly more common in women than men.
Other symptoms:
- Decreased consciousness and alertness
- Eye discomfort in bright light (photophobia)
- Mood and personality changes, including confusion and irritability
- Muscle aches (especially neck pain and shoulder pain)
- Nausea and vomiting
- Numbness in part of the body
- Seizure
- Stiff neck
- Vision problems, including double vision, blind spots, or temporary vision loss in one eye
Other symptoms that may occur with subarachnoid hemorrhage:
- Eyelid drooping
- Pupil size difference
- Sudden stiffening of back and neck, with arching of the back (opisthotonos; not very common)
Subarachnoid hemorrhage can be caused by 15 :
- Occur when an aneurysm (a blood-filled pouch that balloons out from an artery) on or near the surface of the brain ruptures and bleeds into the space between the brain and the skull. The cause of cerebral aneurysms is not known 14. They may develop from birth or in childhood and grow very slowly. Some people have multiple aneuryms 14.
- Bleeding from a tangle of blood vessels called an arteriovenous malformation (AVM)
- Bleeding disorder
- Head injury: Subarachnoid hemorrhage caused by injury is often seen in the older people who have fallen and hit their head. Among the young, the most common injury leading to subarachnoid hemorrhage is motor vehicle crashes 15.
- Use of blood thinners
- Unknown cause (idiopathic)
- Are often caused by high blood pressure.
In addition to high blood pressure, factors that increase the risk of hemorrhagic strokes include:
- cigarette smoking
- use of oral contraceptives (particularly those with high estrogen content)
- excessive alcohol intake
- use of illegal drugs
- Aneurysm in other blood vessels
- Fibromuscular dysplasia (FMD) and other connective tissue disorders
- History of polycystic kidney disease.
A strong family history of aneurysms may also increase your risk.
The goals of treatment are to:
- Save your life
- Repair the cause of bleeding
- Relieve symptoms
- Prevent complications such as permanent brain damage (stroke)
Surgery may be done to:
- Remove large collections of blood or relieve pressure on the brain if the hemorrhage is due to an injury
- Repair the aneurysm if the hemorrhage is due to an aneurysm rupture
If the person is critically ill, surgery may have to wait until the person is more stable.
Surgery may involve:
- Craniotomy (cutting a hole in the skull) and aneurysm clipping, to close the aneurysm
- Endovascular coiling, placing coils in the aneurysm and stents in the blood vessel to cage the coils reduces the risk of further bleeding
If no aneurysm is found, the person should be closely watched by a health care team and may need more imaging tests.
Treatment for coma or decreased alertness includes:
- Draining tube placed in the brain to relieve pressure
- Life support
- Methods to protect the airway
- Special positioning
A person who is conscious may need to be on strict bed rest. The person will be told to avoid activities that can increase pressure inside the head, including:
- Bending over
- Straining
- Suddenly changing position
Treatment may also include:
- Medicines given through an IV line to control blood pressure
- Medicine to prevent artery spasms
- Painkillers and anti-anxiety medicines to relieve headache and reduce pressure in the skull
- Medicines to prevent or treat seizures
- Stool softeners or laxatives to prevent straining during bowel movements
Outlook (Prognosis) with subarachnoid hemorrhage
How well a person with subarachnoid hemorrhage does depends on a number of different factors, including:
- Location and amount of bleeding
- Complications
Older age and more severe symptoms can lead to a poorer outcome.
People can recover completely after treatment. But some people die, even with treatment.
Possible Complications
Repeated bleeding is the most serious complication. If a cerebral aneurysm bleeds for a second time, the outlook is much worse.
Changes in consciousness and alertness due to a subarachnoid hemorrhage may become worse and lead to coma or death.
Other complications include:
- Complications of surgery
- Medicine side effects
- Seizures
- Stroke
What is Ischemic Stroke (87 percent of strokes)
Ischemic stroke (also called embolic stroke or thrombotic stroke), is the most common type of stroke. It is usually caused by a blood clot that blocks or plugs a blood vessel in the brain 16. This keeps blood from flowing to the brain. Within minutes, brain cells begin to die. Another cause is stenosis or narrowing of the artery 16. The majority of strokes occur when blood vessels to the brain become narrowed or clogged with fatty deposits called plaque. This cuts off blood flow to brain cells. A stroke caused by lack of blood reaching part of the brain is called an ischemic
stroke. High blood pressure is the most important risk factor for ischemic stroke that you can change. Transient ischemic attacks (TIAs) occur when the blood supply to the brain is interrupted briefly. Having a TIA can mean you are at risk for having a more serious stroke.
There are two types of ischemic strokes:
- Thrombotic strokes – are caused by a blood clot (thrombus) in an artery going to the brain. The clot blocks blood flow to part of the brain. Blood clots
usually form in arteries damaged by plaque 17.
- Embolic strokes – are caused by a wandering clot (embolus) that’s formed elsewhere (usually in the heart or neck arteries). Clots are carried in the bloodstream and block a blood vessel in or leading to the brain 17.
What causes Ischemic Stroke ?
Ischemic stroke can be caused by several different kinds of diseases. The most common problem is narrowing of the arteries in the neck or head 18. This is most often caused by atherosclerosis, or gradual cholesterol deposition. If the arteries become too narrow, blood cells may collect and form blood clots. These blood clots can block the artery where they are formed (thrombosis), or can dislodge and become trapped in arteries closer to the brain (embolism). Another cause of stroke is blood clots in the heart, which can occur as a result of irregular heartbeat (for example, atrial fibrillation), heart attack, or abnormalities of the heart valves. While these are the most common causes of ischemic stroke, there are many other possible causes. Examples include use of street drugs, traumatic injury to the blood vessels of the neck, or disorders of blood clotting.
How are ischemic strokes diagnosed ?
When someone has shown symptoms of a stroke or a TIA (transient ischemic attack), a doctor will gather information and make a diagnosis. He or she will review the events that have occurred and will:
- get a medical history from you or a family member
- do a physical and neurological examination
- have certain laboratory (blood) tests done
- get a CT or MRI scan of the brain
- study the results of other diagnostic tests that might be needed.
How are ischemic strokes treated ?
Acute treatment is the immediate treatment given by the healthcare team when a stroke happens. The goal of acute treatment is to keep the amount of brain injury as small as possible. This is done by restoring blood flow to the part of the brain where the blockage was quickly.
The only FDA approved drug to treat ischemic stroke is tissue plasminogen activator (tPA). It is a clot busting drug. tPA must be given within 3 to 4.5 hours of the first symptoms of stroke. Medication may also be used to treat brain swelling that sometimes occurs after a stroke. For people with blood clots in larger arteries, tPA often does not dissolve them completely. In this case, a procedure , called mechanical thrombectomy, should be done within six hours of the first symptoms
of stroke. In most cases this is done only after the patient receives IV tPA. To remove the clot, doctors thread a catheter (thin tube) with a stent through an artery in the groin up to the blocked artery in the brain. The stent opens and grabs the clot. The doctors then remove the stent with the trapped clot. If necessary, other devices may also be used. When someone has a stroke, they are at risk of another. Once the medical team identifies what caused the stroke, they may prescribe treatments or procedures to reduce the risk of a second stroke, such as:
- Antiplatelet agents such as aspirin and anticoagulants such as warfarin, dabigitran, apixabanm rivoraxaban or edoxaban interfere with the blood’s ability to clot. This can play an important role in preventing a stroke.
- Carotid endarterectomy is a procedure in which blood vessel blockage (blood clot or fatty plaque) is surgically removed from the carotid artery in the neck. This reopens the artery and the blood flow to the brain. This is only done in people who have a large blockage.
- Doctors sometimes use balloon angioplasty and implantable steel screens called stents to treat and reduce fatty buildup clogging a vessel that may make it
easy for clots to form in the bloodstream.
Sometimes a stroke is the first sign a person has of other health conditions, such as high blood pressure, diabetes, atrial fibrillation (a heart rhythm disorder), or
other vascular disease. If any of these are diagnosed, the healthcare team will prescribe appropriate treatment.
What is Transient Ischemic Attack ?
A transient ischemic attack (TIA) is a stroke lasts only a few minutes 19. It happens when the blood supply to part of the brain is briefly blocked 19. Since it doesn’t cause permanent damage, it might seem like no big deal. But ignoring it is a big mistake. That’s because a transient ischemic attack (TIA) may signal a full-blown stroke ahead 20. TIAs are often labeled “mini-strokes,” because they can be relatively benign in terms of immediate consequences. But the term “warning stroke” is more appropriate for these temporary episodes, because they can indicate the likelihood of a coming stroke 20. Like most strokes, TIAs are caused by a clot or blockage in the brain. TIAs should be taken very seriously. If you suspect a TIA or stroke of kind, be sure to call for an ambulance and go to the hospital emergency room immediately.
Symptoms of a transient ischemic attack (TIA) are like other stroke symptoms, but do not last as long. They happen suddenly, and include
- Numbness or weakness, especially on one side of the body
- Confusion or trouble speaking or understanding speech
- Trouble seeing in one or both eyes
- Difficulty walking
- Dizziness
- Loss of balance or coordination
Most symptoms of a TIA disappear within an hour, although they may last for up to 24 hours. Because you cannot tell if these symptoms are from a TIA or a stroke, you should go to the hospital right away. About a third of the people who have a TIA go on to have a more severe stroke within a year.
TIAs are often a warning sign for future strokes. Taking medicine, such as blood thinners, may reduce your risk of a stroke. Your doctor might also recommend surgery. You can also help lower your risk by having a healthy lifestyle. This includes not smoking, not drinking too much, eating a healthy diet, and exercising. It is also important to control other health problems, such as high blood pressure and cholesterol.
Treatment of Transient Ischemic Attack
Because there is no way to tell whether symptoms are from a TIA or an acute stroke, patients should assume that all stroke-like symptoms signal an emergency and should not wait to see if they go away 21. A prompt evaluation (within 60 minutes) is necessary to identify the cause of the TIA and determine appropriate therapy. Depending on a patient’s medical history and the results of a medical examination, the doctor may recommend drug therapy or surgery to reduce the risk of stroke in people who have had a TIA. The use of antiplatelet agents, particularly aspirin, is a standard treatment for patients at risk for stroke. People with atrial fibrillation (irregular beating of the heart) may be prescribed anticoagulants.
Prognosis of Transient Ischemic Attack
Transient Ischemic Attacks are often warning signs that a person is at risk for a more serious and debilitating stroke. About one-third of those who have a TIA will have an acute stroke some time in the future. Many strokes can be prevented by heeding the warning signs of TIAs and treating underlying risk factors. The most important treatable factors linked to TIAs and stroke are high blood pressure, cigarette smoking, heart disease, carotid artery disease, diabetes, and heavy use of alcohol. Medical help is available to reduce and eliminate these factors. Lifestyle changes such as eating a balanced diet, maintaining healthy weight, exercising, and enrolling in smoking and alcohol cessation programs can also reduce these factors.
Care plans
A care plan (sometimes called a care and support plan, or support plan if you’re a carer) sets out how your care and support needs will be met. Before treatment starts, your current and future health and social care needs will be assessed and a care plan drawn up.
This is a way of ensuring you receive the right treatment for your needs. It involves identifying areas where you may need some assistance, such as:
- what support you or your carer need for you to remain as independent as possible – including whether you might need care at home or in a nursing home
- whether there are any changes that need to be made to your home to make it easier to live in
- whether you need any financial assistance
You should be fully involved in the preparation of your care plan, and you and anyone else you request should also get a written copy. The care plan must set out:
- the needs identified by the assessment
- whether, and to what extent, the needs meet the eligibility criteria
- the needs that the authority is going to meet, and how it intends to do so
- for a person needing care, for which of the desired outcomes care and support could be relevant
- for a carer, the outcomes the carer wishes to achieve, and their wishes around providing care, work, education and recreation where support could be relevant
- the personal budget
- information and advice on what can be done to reduce the needs in question, and to prevent or delay the development of needs in the future
- where needs are being met via a direct payment, the needs to be met via the direct payment and the amount and frequency of the payments
Your care plan should be individual to you, and you should be allowed to have as much involvement in the development of your plan as you wish.
Care and support should help you to:
- live independently
- have as much control over your life as possible
- participate in society on an equal level, with access to employment and a family life
- have the best possible quality of life
- keep as much dignity and respect as possible
It’s worth remembering that if there are different options that would meet your assessed needs equally well, the local authority can choose what it believes are the most cost-effective options.
Reviews of your care plan
Your care plan should be reviewed by social services within the first three months, and then at least annually.
The review looks at whether the outcomes identified in the care plan are being met. It should also review these goals to make sure they’re still appropriate (and for instance, that your care and support needs haven’t changed), and check that any risk assessments are up to date.
If, after the review, it is clear that things have changed that affect the detail within the care plan, then the local authority will conduct a revision of the plan. This may also involve a needs assessment and financial assessment.
If it’s decided that you no longer qualify for local authority support, you should receive written reasons for this, with information about other help available, including funding your own care.
Lifestyle changes
The main aim of treatment for vascular dementia is to treat the underlying cause to help stop the condition getting worse.
This will usually involve making healthy lifestyle changes, such as:
- eating healthily, for example, you may be advised to follow a low-salt diet to manage high blood pressure
- losing weight if you’re overweight
- stopping smoking
- getting fit
- cutting down on alcohol
Medication
Medication may also be offered to treat the underlying cause of vascular dementia and help stop it getting worse.
These include:
- medication for high blood pressure
- statins to treat high cholesterol
- medicines such as aspirin or clopidogrel to reduce the risk of blood clots and further strokes
- anticoagulant medication, such as warfarin, which can also reduce the risk of blood clots and further strokes
- medication for diabetes
Some medicines may also help with some of the symptoms of vascular dementia. For example, antidepressants can help relieve depression.
Alzheimer’s disease medications such as donepezil (Aricept), galantamine (Reminyl) or rivastigmine (Exelon) aren’t used to treat vascular dementia, but may be used in people with a combination of vascular dementia and Alzheimer’s disease.
Support and other therapies
There are also a number of therapies and practical measures that can help make everyday living easier for someone with dementia.
These include:
- occupational therapy to identify problem areas in everyday life, such as getting dressed, and help work out practical solutions
- speech and language therapy to help improve any communication problems
- physiotherapy to help with movement difficulties
- psychological therapies, such as cognitive stimulation (activities and exercises designed to improve memory, problem-solving skills and language ability)
- relaxation techniques, such as massage and music or dance therapy
- social interaction, leisure activities and other dementia activities, such as memory cafés (drop-in sessions for people with memory problems and their carers to get support and advice)
- home modifications, such as removing loose carpets and potential trip hazards, ensuring the home is well lit, and adding grab bars and handrails
It may also be helpful to get in touch with a support group, such as the Alzheimer’s Society or Dementia Organization.
End of life and legal issues
If you’ve been diagnosed with dementia, you might want to make arrangements for your care that take into account the decline in your mental abilities.
This may include ensuring that your wishes are upheld if you’re not able to make decisions for yourself.
You may want to consider:
- drawing up an advance decision – this makes your treatment preferences known in case you’re unable to do this in the future
- having a preferred place of care plan – this outlines where you would like to receive treatment
- giving a relative lasting power of attorney – this is the power to make decisions about you if you’re unable to.
Looking after someone with dementia
If you have dementia, or you are looking after someone who has dementia, you are likely to face many practical issues in your daily life.
The symptoms of dementia will usually get gradually worse. How quickly this occurs will depend on the general health of the person with dementia and on the type of dementia they have.
Over time, people with dementia will need help to cope at home, and they may even need residential care in a nursing home eventually. It is natural to feel worried about the future, but you are not alone – whether you have dementia or you care for someone with the condition. The National Institutes of Health, National Institute on Aging social services and voluntary organisations can all provide advice and support to help you and your family.
People with dementia can feel vulnerable as their condition progresses and they increasingly rely on other people to do things for them. It is important that people who have dementia feel reassured and supported, while retaining some level of independence.
Although some symptoms are common to many people with dementia, each person’s experience of the disease and how they cope with it will be different.
Staying independent with dementia
Being diagnosed with dementia will have a big impact on your life. You and your family may worry about how long you can care for yourself, particularly if you live alone. People with dementia can remain independent for some time, but will need support from family and friends.
Living at home when you have dementia
In the early stages of dementia, many people are able to look after their homes in the same way as before their diagnosis. However, as the illness gets worse, it is likely that someone who has dementia will find it difficult to look after their home and they may need help with daily activities, such as housework and shopping. The home of a person with dementia may also need to be adapted to enable them to stay safe, mobile and independent.
Living alone with dementia
It’s good to stay independent for as long as possible. Many people with dementia continue to live successfully on their own for some time. However, be aware that, as your condition progresses, you will need extra support to help you cope, and it’s better to get this in place early.
Talk to family, friends and health professionals about how they can help you to stay independent. They can advise on how to cope with practical tasks, such as shopping. Find out about the local support services that can help you manage in your home – for example, by doing laundry and supervising meals.
Working when you have dementia
Coping at work can be worrying for people with dementia. You should speak to your employer as soon as you feel ready. You can also get advice from the disability employment adviser at your local job centre, your trade union or your local Citizens Advice Bureau. If you decide to leave work, seek advice about your pensions and benefits.
You could continue to work or return to work by asking your employer if you can change your workload. Your local disability employment adviser can help and advise you.
Driving
Some people with dementia prefer to give up driving because they find it stressful, but others continue driving for some time. To continue driving, you must inform the Driver and Vehicle Licensing Authority (DMV) that you have dementia.
The DMV will ask for medical reports and possibly a special driving assessment to decide whether you can continue driving.
Read more about driving and dementia on the Alzheimer’s Society website.
People with dementia must give up driving when their symptoms become bad enough to make them unsafe on the road. This is to protect themselves, their passengers and other road users.
Assistive technology for people with dementia
Assistive technology is available for people with dementia or other conditions that affect memory. AT Dementia is an organisation that provides access to technology aimed specifically at people with dementia, including:
- daily living aids – special utensils to help people eat and drink
- stand-alone devices – aids that can be used without being linked to a monitoring centre or carer
- telecare – sensors or detectors that automatically send a signal to a carer or monitoring centre by telephone.
Helping someone with dementia with everyday tasks
When a person with dementia finds that their mental abilities are declining, they’re likely to feel anxious, stressed and scared. They may be aware of their increasing clumsiness and inability to remember things, and this can be very frustrating and upsetting for them.
If you are looking after someone with dementia, you can help them feel more secure by creating a regular daily routine in a relaxed environment, where they’re encouraged and not criticised.
Involving the person you look after in everyday tasks may make them feel useful and improve their sense of self-worth. They could help with the shopping, laying the table or sweeping leaves in the garden, for example.
As the illness progresses, these tasks may become harder for them to manage independently, and you may need to give them more support.
How you can help
The main way you can help someone with dementia is by offering support sensitively and try not to be critical of what they do. It can be very important for the person with dementia to feel that they’re still useful.
In the early stages, memory aids can be used around the home to help the person remember where things are.
For example, you could put pictures on cupboard doors of what’s inside, such as cups and saucers. This may help to trigger their memory and enable them to retain their independence a little longer.
Keeping up hobbies and interests when someone has dementia
Many people with dementia will still enjoy their hobbies or interests. For example, if they like cooking, they may be able to help make a meal. Going for a walk or gardening is a simple way to get some exercise and a sense of achievement. Or they may prefer listening to music or playing a board game. Caring for a pet cat or dog can bring a lot of pleasure to some people.
If the person you care for was very sociable and outgoing, or if they have a large family, they may really enjoy visits from one or two family members or friends. However, they may struggle to keep up with conversations if they have a lot of visitors at the same time.
Maintaining good health and nutrition in someone with dementia
It’s important that the person you care for has a healthy, balanced diet and gets some exercise. The longer they stay fit and healthy, the better their quality of life will be. If you want some easy exercises, try these sitting exercises.
If the person you care for doesn’t eat enough or eats unhealthy food, they can become susceptible to other illnesses. People with dementia can become more confused if they get ill.
Common food-related problems for people with dementia include:
- not recognising foods
- forgetting what food they like
- refusing or spitting out food
- resisting being fed
- asking for strange food combinations
This behaviour is usually due to confusion, or irritation in the mouth caused by dental problems, rather than wanting to be awkward. If you’re concerned about the person’s eating behaviour, speak to your GP.
How you can help
Involve the person you care for. For example, if they cannot feed themselves, you could put the cutlery in their hand and help guide it to their mouth. You could also involve them in preparing food, if they are able to.
Try to stay calm. If you feel stressed at mealtimes, the person you care for will probably be stressed too. Make sure you have plenty of time for meals, so you can deal with any problems that arise.
Try to accommodate behaviour changes. It’s likely that the person you care for will change their eating patterns and habits over time. Being aware of this and trying to be flexible will make mealtimes less stressful for both of you.
If you think the person you care for may have health or dental problems, get help from your GP or dentist. You could also contact a local carers’ group to speak to other people who may have experienced similar difficulties.
If the person with dementia smokes, replace matches with disposable lighters to lower the risk of them accidentally causing a fire.
If the person you care for drinks alcohol, check if this is recommended alongside any medication they make take. If in doubt, ask your GP.
Dealing with incontinence in someone with dementia
Incontinence can be difficult to deal with and can be very upsetting for the person you care for. It’s common for people with dementia to experience incontinence. This can be due to urinary tract infections, constipation causing added pressure on the bladder, or medication.
A person with dementia may also simply forget to go to the toilet, or may forget where the toilet is. They may also have lost the ability to tell when they need the toilet.
How you can help
It’s important to be understanding, retain a sense of humour and remember that it’s not their fault. You may also want to try the following:
- Put a sign on the toilet door, such as a photo of the toilet.
- Keep the toilet door open and make sure that the person you care for can access it easily.
- Make sure they can remove their clothes – some people with dementia can struggle with buttons and zips.
- Look out for signs that they may need to go to the toilet, such as fidgeting and standing up and down.
- Get adaptations to the toilet if necessary – you may be able to get these through a care and support needs assessment.
If you’re still having problems with incontinence, ask your GP to refer you to a continence advisor, who can advise on things like waterproof bedding or incontinence pads.
Helping someone with dementia with their personal hygiene
People with dementia can become anxious about certain aspects of personal hygiene and may need help with washing. For example, they may be scared of falling when getting out of the bath, or they may become disorientated in the shower.
The person you care for may not want to be left alone or they may resist washing, because they find the lack of privacy undignified and embarrassing. Try to do what’s best for them.
Poor hygiene can cause skin complaints and infections, and be a source of discomfort and low self-esteem.
How to maintain daily hygiene
To maintain daily personal hygiene, you should make sure:
- your hands are washed after you’ve used the toilet
- your genitals and anal area are washed every day
- your face is washed daily
- you’re fully bathed or showered at least twice a week
- your teeth are brushed twice a day
It is also important that you have regular dental checks. Find out more about dental treatment for people with special needs.
Help with washing and bathing
For most people, washing is a very private activity. If you are helping someone else wash or bathe, be sensitive and try to maintain their dignity. You may feel awkward and embarrassed, especially at first.
To make bathing and washing as pleasant and comfortable as possible, you might consider:
- using pleasant-smelling shampoo, bubble bath or soap
- playing music the person you care for likes and is familiar with
- if the person you’re washing is confused, explaining what’s happening as you go along
- being sensitive to their mood
Overhead showers can be frightening to some people. If you have no bath or there is a good reason for using a shower rather than a bath, use a handheld shower.
Ask the person how they would prefer to be helped and allow them as much independence as you think is safe. If they had a routine before you began caring for them, find out what it was and stick to it as much as you can. Find out which shampoo, shower gel or soap they prefer to make the experience more familiar to them.
Many people become self-conscious when undressed in front of others. Be sensitive to the situation and approach it in the way you think is most appropriate. The person you care for may feel isolated if you leave them alone. How you handle this depends on your relationship with them. Have clothes and towels with you so you don’t have to leave them alone in the bathroom if they don’t want you to.
Safety when washing or bathing
If you find it difficult to help someone move around, your local authority has a responsibility to consider your needs as a carer and the needs of the person you care for. Contact the local authority and ask for an assessment for the person you look after, as well as a carer’s assessment to help you. For advice and guidance on moving and handling, ask for an occupational therapy assessment.
If you or the person you’re looking after has limited mobility or problems balancing, make sure:
- the floor is not slippery (dry it if necessary)
- the room is a comfortable temperature
- the water is comfortably warm – older people particularly feel the cold, so bear this in mind when adjusting the temperature
- the locks are removed from the door – you or the person you care for may want privacy, but other people may need access in an emergency
Before attempting to move someone, ask yourself:
- Do they need help to move?
- Do they require help or supervision?
- Have you told them you’re moving them?
- How heavy are they?
- Are you healthy and strong enough to move them?
- Is there anyone who could help you?
- How long will it take?
- Is there enough space around you?
- Are there any obstacles in the way?
Are you wearing suitable clothing and shoes – for example, if you are on a slippery or damp surface?
If you have assessed the situation and have decided to move the person, make sure you:
- never lift above shoulder height
- make sure your feet are stable
- take a firm hold
- keep any weight close to your body
- keep your back straight and bend your knees
- lift as smoothly as possible.
Buying equipment
You may decide you need specialist moving equipment. Before you buy any equipment, get advice from a healthcare professional such as an occupational therapist or a social worker.
Try all equipment before you buy it. If you’re considering buying an expensive item, ask to use the equipment for a trial period in the home of the person you’re looking after.
Going to the toilet
Going to the toilet (toileting) is an important part of personal hygiene, regardless of whether you or the person you’re looking after is able to control their bladder and bowels (continent) or not.
Incontinence can create feelings of shame or embarrassment for both the carer and the person being cared for. Sometimes people may be in denial about their incontinence or refuse to accept help. Reassure them it’s not their fault and approach the issue in a calm, reassuring way.
Giving a bed bath
If the person you care for cannot move or has extremely limited mobility, you may need to give them a bed bath. You will need to be extra careful when moving or handling them. Specialist disposable baths are available for people who need a bath where you are put fully in the water.
Continence services
As many as one in three people have difficulty controlling their flow of urine. And while you may not have a problem controlling your bowel or bladder, a mobility problem can make successfully visiting the toilet difficult.
Continence problems can cause physical problems such as skin irritation and infection, as well as embarrassment and loss of confidence.
A continence adviser may be able to provide many small items and other equipment that can help with continence, including:
- plastic or PVC covers to protect beds
- disposable or washable continence pads
- waterproof pants
Your social services department should be able to provide small aids and adaptations for the home, including:
- hand rails
- commodes
- raised toilet seats.
Helping someone with dementia sleep well
People with dementia often experience disturbed sleep. They may wake up during the night or be restless. These problems may get worse as the illness progresses. People with dementia may also have painful illnesses such as arthritis that cause, or contribute to, sleep problems.
Some medication can cause sleepiness during the day and interfere with sleep at night. Sleeping pills can be used with care in people with dementia.
Carers’ breaks and respite care
Your carer’s assessment may identify that you need a break from caring from time to time. Equally, the person you care for may also want to have a break without you.
Replacement care is designed to replace the care that you, as a carer, would normally be giving the person you care for. It may be needed so you can look after your own health and wellbeing, and to take a break from caring. For example, it may be that regular replacement overnight care is needed so you can catch up on your own sleep.
In certain situations, respite (temporary) care may be provided by your local authority after your carer’s assessment or after the person you care for has had an assessment. You can use the directory of local carers’ services to find your nearest local carers’ centre or respite service. Your local authority or local carers’ centre can give you information about local support.
You might want to consider:
- homecare services – these can either be day services that give you the chance to do an activity inside or outside the home, or night services that can help you get a proper night’s sleep, or helpers coming to the home of the person you’re caring for. Different types of help can be organised, including sitting with the person you care for and keeping them company, preparing meals, and helping them to get up, washed and dressed. The care workers who come to your home can also provide social activities, such as taking the person you care for to the cinema, pub or shopping.
- residential or nursing care – this is where the person you’re looking after goes for a short stay in a residential or nursing home. If you can, visit the care or nursing home beforehand so you can see what it’s like.
- day care – this is where the person you’re looking after goes to a day centre or takes part in activities away from home.
If the replacement care provided is essentially a homecare service for the person needing care and allows you to take a break, it should be considered a service provided to the cared-for person and should therefore be charged to them, not you as the carer.
- Alzheimer’s Association. Vascular Dementia. http://www.alz.org/dementia/vascular-dementia-symptoms.asp[↩]
- National Institutes of Health. National Institute on Aging. What Is Vascular Dementia ? https://www.nia.nih.gov/health/what-vascular-dementia[↩]
- Multi-infarct dementia. A cause of mental deterioration in the elderly. Hachinski VC, Lassen NA, Marshall J. Lancet. 1974 Jul 27; 2(7874):207-10. https://www.ncbi.nlm.nih.gov/pubmed/4135618/[↩]
- U.S. National Library of Medicine. MedlinePlus. Multi-infarct dementia. https://wwwqa.nlm.nih.gov/medlineplus/275/ency/article/000746.htm[↩][↩]
- U.S. National Library of Medicine. Genetics Home Reference. cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. https://ghr.nlm.nih.gov/condition/cerebral-autosomal-dominant-arteriopathy-with-subcortical-infarcts-and-leukoencephalopathy[↩][↩]
- The National Institute of Neurological Disorders and Stroke. Binswanger’s disease. https://www.ninds.nih.gov/Disorders/All-Disorders/Binswangers-Disease-Information-Page[↩]
- Strub RL. Vascular Dementia. The Ochsner Journal. 2003;5(1):40-43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3314418/[↩]
- Sattel H., Forstl H., Biedert S. Senile dementia of Alzheimer type and multi-infarct dementia investigated by transcranial Doppler sonography. Dementia. 1996;7:41–46. https://www.ncbi.nlm.nih.gov/pubmed/8788081[↩]
- National Institutes of Health. National Institute on Aging. What Is Mixed Dementia ? https://www.nia.nih.gov/health/what-mixed-dementia[↩]
- U.S. National Library of Medicine. Stroke. https://medlineplus.gov/stroke.html [↩]
- American Heart Association. Let’s Talk About Hemorrhagic Stroke. http://www.heart.org/HEARTORG/Conditions/Lets-Talk-About-Hemorrhagic-Stroke_UCM_313389_Article.jsp[↩][↩][↩][↩]
- The Internet Stroke Center. Ischemic Stroke. http://www.strokecenter.org/patients/about-stroke/ischemic-stroke/ [↩][↩]
- Wolters Kluwer. UpToDate. Patient education: Hemorrhagic stroke treatment. https://www.uptodate.com/contents/hemorrhagic-stroke-treatment-beyond-the-basics[↩]
- The Internet Stroke Center. Subarachnoid Hemorrhage. http://www.strokecenter.org/patients/about-stroke/subarachnoid-hemorrhage/[↩][↩][↩]
- U.S. National Library of Medicine. Medline Plus. Subarachnoid hemorrhage. https://medlineplus.gov/ency/article/000701.htm[↩][↩][↩]
- U.S. National Library of Medicine. Medline Plus. Ischemic Stroke. https://medlineplus.gov/ischemicstroke.html[↩][↩]
- American Heart Association. American Stroke Association. Ischemic Stroke. http://www.strokeassociation.org/idc/groups/stroke-public/@wcm/@hcm/documents/downloadable/ucm_309725.pdf[↩][↩]
- The Internet Stroke Center. Ischemic Stroke. http://www.strokecenter.org/patients/about-stroke/ischemic-stroke/[↩]
- U.S. National Library of Medicine. Transient Ischemic Attack. https://medlineplus.gov/transientischemicattack.html[↩][↩]
- American Heart Association. Transient Ischemic Attack. http://www.strokeassociation.org/STROKEORG/AboutStroke/TypesofStroke/TIA/Transient-Ischemic-Attack-TIA_UCM_492003_SubHomePage.jsp[↩][↩]
- National Institute of Neurological Disorders and Stroke. Transient Ischemic Attack Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Transient-Ischemic-Attack-Information-Page[↩]