Contents
What is zika virus
Zika virus is an infection that is spread by mosquitoes and/or sexual contact. Zika virus is spread mostly by the bite of an infected Aedes species mosquito (Aedes aegypti and Aedes albopictus) bites. These mosquitoes bite during the day and night, and can also carry dengue and yellow fever.
Zika virus might also be transmitted sexually. Zika virus was first identified in 1947 in rhesus monkeys and it was first described in humans in the 1960s in Nigeria, Uganda and the United Republic of Tanzania. Zika virus was first reported outside Africa in 2007 when a case was reported on the Island of Yap in Micronesia, but has recently gained attention because of new outbreaks in countries such as Brazil, and reported links between the virus and various birth defects.
Many people infected with Zika will have no symptoms or mild symptoms that last several days to a week. However, Zika infection during pregnancy can cause a serious birth defect called microcephaly and other severe fetal brain defects. Current research suggests that Guillain-Barre syndrome, an uncommon sickness of the nervous system, is strongly associated with Zika; however, only a small proportion of people with recent Zika virus infection get Guillain-Barre syndrome.
Once someone has been infected with Zika, it’s very likely they’ll be protected from future infections. There is no evidence that past Zika infection poses an increased risk of birth defects in future pregnancies.
Zika virus mosquito
Figure 1. Aedes aegypti mosquito
Figure 2. Aedes albopictus mosquito
About 4 in 5 people who have the zika virus infection have no symptoms. Those who do get symptoms might have fever, rash, tiredness, aches and pains. Zika virus infections in United States are most frequently reported in people who have traveled to a country where the virus is very common, such as in Central and South America and the Pacific. Public health authorities around the world including the Centers for Disease Control and Prevention (CDC) are closely monitoring the spread of Zika virus.
- Most people with Zika virus don’t notice anything. Some feel like they have the flu. In some cases it has been known to cause fever, rash, severe headache, joint pain and muscle or bone pain. The illness is usually mild with symptoms lasting up to a week, and many people do not have symptoms or will have only mild symptoms.
- Any symptoms come on about 3 to 12 days after infection. A blood test can be used to diagnose the infection.
- If you have the virus, get plenty of rest, drink plenty of water and treat any pain and fever as you normally would. If your symptoms gets worse, see your doctor.
- A person with Zika can pass it to his or her sex partners.
- Zika can also be passed from a pregnant woman to her fetus. A pregnant woman can pass Zika to her fetus during pregnancy or around the time of birth. Infection during pregnancy can cause certain birth defects called microcephaly and other severe brain defects. Pregnant women who have traveled to or live in places with risk of Zika should protect themselves by preventing mosquito bites and sexual transmission of Zika.
- There is NO vaccine to prevent infection by Zika virus.
The best prevention is to avoid mosquito bites in areas with known outbreaks. Mosquito bites can be avoided by wearing long-sleeved clothing, using insect repellents and bed nets and sleeping in rooms that are enclosed or air-conditioned.
Figure 3. Zika virus rash
Figure 4. Zika virus rash
How does Zika virus spread?
Zika virus spreads in several ways:
- Through mosquito bites. This is the most common way Zika spreads. You can get infected from a mosquito that carries the Zika virus, and a mosquito can get the virus by biting an infected person. The mosquito can then pass the virus by biting someone else. Zika infection usually stays in a person’s blood for a few days to a week after getting infected. The mosquito can’t pass the virus until 8 to 12 days after biting an infected person. The mosquitoes that carry Zika virus can live both inside and outside. They’re called day biters because they bite most often during the day, but they also bite at night.
- By passing it to your baby during pregnancy and birth. More research is needed, but experts think Zika virus can pass through the placenta to your baby. The placenta grows in your uterus (womb) and supplies your baby with food and oxygen through the umbilical cord.
- Through sex with an infected person. During sex, an infected male can pass Zika through semen. Zika stays in a man’s semen for at least 2 weeks and possibly more than 3 months after his signs and symptoms start. Semen contains sperm, which is what fertilizes an egg to get a woman pregnant. An infected woman can pass Zika to her partner during sex through vaginal fluids or blood from her menstrual period. Zika has been found in a woman’s cervical mucus up to 11 days after her signs and symptoms start. Cervical mucus is a body fluid that collects in the vagina.
- Through infected blood and body tissue, including semen. You may come in contact with infected blood or body tissue in a health care setting (like a laboratory) or if you have a blood transfusion. A blood transfusion is when you have new blood put into your body.
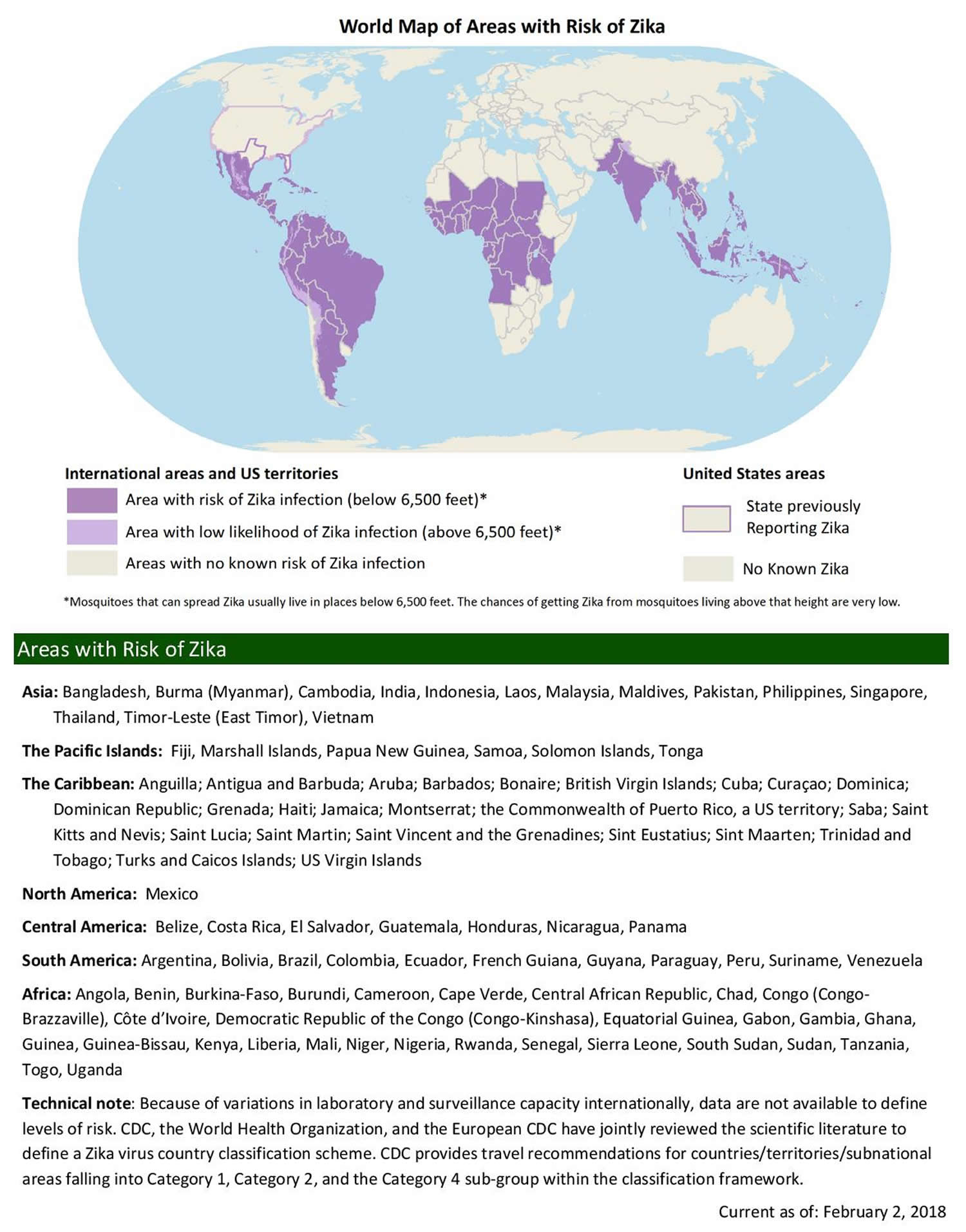
Where is zika virus
Figure 5. Zika virus map
For the latest Map of Areas with Risk of Zika please go here: https://wwwnc.cdc.gov/travel/page/world-map-areas-with-zika
Because Zika infection during pregnancy can cause severe birth defects, pregnant women should not travel to the above areas. Partners of pregnant women and couples considering pregnancy should know the risks to pregnancy and take prevention steps. All travelers should strictly follow steps to prevent mosquito bites and prevent sexual transmission during and after the trip.
If I am traveling to an area with risk of Zika, should I be concerned about Zika?
Travelers who go to places with risk of Zika can be infected with Zika, and CDC has issued travel recommendations 1 for people traveling to areas with a CDC Zika Travel Notice. Many people will have mild or no symptoms. However, Zika can cause microcephaly and other severe birth defects. For this reason, pregnant women should not travel to any area with risk of Zika, and women trying to get pregnant should talk to their doctors before traveling or before their sex partners travel to an area with risk of Zika. It is especially important that women who wish to delay or avoid pregnancy consistently use the most effective method of birth control that they are able to use. Those traveling to areas with risk of Zika should take steps during and after they travel to prevent mosquito bites and sexual transmission of Zika.
Pregnant Women Should Not Travel to an Area with Risk of Zika
- Pregnant women should not travel to areas with risk of Zika (i.e., with documented or likely Zika virus transmission).
- Pregnant women should consider postponing travel to yellow cautionary areas in the United States.
Guidance for Areas with Local Zika Virus Transmission in the Continental United States and Hawaii
CDC has issued guidance for travel, prevention, testing, and preconception counseling related to risks for pregnant women and couples considering conception in areas of active Zika virus transmission in the continental United States and Hawaii. CDC has identified two types of geographic areas to describe where Zika virus-related domestic guidance applies: Zika active transmission areas (designated as red areas) and Zika cautionary areas (designated as yellow areas). The recommendations in the tables below are based on the CDC Zika Interim Response Plan, May 2017 2.
Red Areas
A Zika active transmission (red) area is a geographic area where local, state, and CDC officials have identified the presence of confirmed, multi-person local mosquito-borne transmission and have determined that the intensity of Zika virus transmission presents a significant risk of contracting mosquito-borne Zika and poses a risk to pregnant women and blood and tissue safety.
Yellow Areas
A Zika cautionary (yellow) area is a geographic area where local mosquito-borne transmission has been identified and pregnant women and blood and tissue safety are at some undetermined risk, but evidence is lacking on whether the intensity of transmission is widespread and sustained.
Recommendations for Red and Yellow Areas
Red Areas
- Pregnant women should not travel to red areas.
- Women and men who are planning to conceive in the near future should avoid nonessential travel to red areas.
Yellow Areas
- Pregnant women should consider postponing travel to yellow areas.
- Healthcare providers should discuss reproductive life plans with patients who are planning to conceive in the near future about the lower likelihood of Zika infection in yellow areas compared to red areas and the limited information about periconceptional infection risk.
Preconception Counseling
With Zika symptoms and/or diagnosis
Red and Yellow
Women and men who are planning to conceive in the near future should be advised to wait at least 8 weeks if a woman had Zika symptoms and/or diagnosis, and at least 6 months if a man had Zika symptoms and/or diagnosis, before attempting conception.
No Zika symptoms, and without ongoing exposure
Red
Women and men who are planning to conceive in the near future should be advised to wait at least 8 weeks if only the woman was exposed and at least 6 months if the man was exposed after the end date of the last possible exposure before attempting conception.
Yellow
Women and men who are planning to conceive in the near future should consider waiting at least 8 weeks if only the woman was exposed and at least 6 months if the man was exposed after the end date of the last possible exposure before attempting conception.
No Zika symptoms and with ongoing exposure
Red and Yellow
- Women and men who are planning to conceive in the near future should be counseled on the possible risk for Zika virus infection during the periconceptional period and about the potential consequences of Zika virus infection to the fetus during pregnancy. Healthcare providers should discuss reproductive life plans with patients and review factors that might influence pregnancy timing (e.g., duration of Zika virus outbreak, fertility, age, reproductive history, medical history, personal values and preferences).
- Women and men who live in or travel to red or yellow areas should be advised to remain aware of Zika virus transmission and strictly follow steps to prevent mosquito bites.
Please note: There are limited data about the persistence of Zika virus RNA in body fluids and the risk for adverse pregnancy outcomes associated with maternal Zika virus infection around the time of conception is currently unknown. Therefore, some couples in which one or both partners have had possible Zika virus exposure might choose to wait longer or shorter than the recommended period to conceive, depending on individual circumstances (e.g., age, fertility, details of possible exposure) and risk tolerance. Healthcare providers should work with couples to help them make informed decisions.
Zika virus and pregnancy
Zika virus can be passed from a pregnant woman to her developing baby during pregnancy or around the time of birth. Zika virus infection during pregnancy is a cause of microcephaly and has been linked to other pregnancy problems and serious birth defects, including miscarriage, stillbirth, eye defects, hearing loss, and impaired growth. Zika is primarily spread through the bite of an infected Aedes aegypti or Aedes albopictus mosquito. However, Zika can also be spread during sex by a person infected with Zika to his or her sex partners.
What scientists know
- Zika virus can be passed from a pregnant woman to her fetus.
- Infection during pregnancy can cause a birth defect called microcephaly and other severe fetal brain defects. Microcephaly is a condition where a baby has a head that is smaller than expected. Microcephaly is a rare condition associated with mild to severe developmental delays and disability. Babies can be born with microcephaly or it can develop in their first few years. Microcephaly can affect a baby in different ways, including:
- delayed development or speech
- intellectual disability
- problems with coordination or balance
- seizures
- agitation or aggression
- problems with hearing or vision.
- Zika primarily spreads through infected mosquitoes. You can also get Zika through sex without a condom with someone infected by Zika, even if that person does not show symptoms of Zika.
- There is no vaccine to prevent or medicine to treat Zika.
The Centers for Disease Control and Prevention (CDC) has issued a travel notice (Level 2-Practice Enhanced Precautions) for people traveling to places where Zika virus is spreading. Specific areas where Zika is spreading are often difficult to determine and are likely to change over time. As more information becomes available, CDC’s Zika travel notices will be updated. Please check CDC’s Zika Travel Information website 1 frequently for the most up-to-date travel recommendations.
Pregnant women
- Should not travel to areas with Zika.
- Who must travel to one of these areas should talk to their doctor or healthcare provider first and strictly follow steps to prevent mosquito bites during the trip.
- Should talk with your doctor and consider postponing nonessential travel to countries in CDC’s special travel considerations.
- Who have a sex partner who lives in or has traveled to an area with Zika should protect themselves by using condoms correctly, from start to finish, every time they have sex, or they should not have sex during the pregnancy. This includes vaginal, anal, oral sex, and the sharing of sex toys.
Women trying to become pregnant
- Should consider avoiding nonessential travel to areas with Zika.
- Who must travel to one of these areas should consult with their healthcare provider first before traveling to areas with Zika, and they and their partners should strictly follow steps to prevent mosquito bites during the trip.
- Who have a sex partner who lives in or has traveled to an area with Zika should protect themselves from getting Zika during sex.
- Should review CDC’s guidance for men and women who are thinking about pregnancy in the context of the Zika outbreak.
Partners of pregnant women who live in or have traveled to an area with Zika
- Should take steps to prevent mosquito bites.
- Should use a condom correctly, from start to finish, every time they have sex, or not have sex during the pregnancy. This includes vaginal, anal, and oral sex and the sharing of sex toys. Condoms include male or female condoms. Not having sex is the only way to be sure that Zika will not spread through sex.
- Should talk to a healthcare provider about how to prevent sexual transmission of Zika during pregnancy and reduce the risk of birth defects related to Zika.
Should pregnant women travel to areas with risk of Zika?
No. Pregnant women should not travel to any area with risk of Zika. Travelers who go to places with risk of Zika can be infected with Zika, and Zika infection during pregnancy can cause microcephaly and other severe brain defects.
Zika Virus and Pregnancy Testing
Symptomatic
- Pregnant women should be offered testing for Zika virus infection. There are limitations to the interpretation of laboratory tests done on specimens drawn more than 12 weeks after the start date of the exposure.
- Men and non-pregnant women should be tested2 for Zika virus infection based on time of evaluation relative to symptom onset. There are limitations to the interpretation of laboratory tests done on specimens drawn more than 12 weeks after the start date of the exposure.
Asymptomatic with ongoing exposure (people with ongoing exposure include those who live in or frequently travel (e.g., daily, weekly) to a red or yellow area)
- Pregnant women should be offered testing for Zika virus infection.
- Testing is not recommended for men and non-pregnant women.
Zika virus testing is not recommended for asymptomatic non-pregnant persons with possible exposure to Zika virus because there is potential for false reassurance in the following ways: 1) a blood test may be performed after the virus is no longer in the blood but could still be present in semen, 2) the antibody test may be performed early after infection when the antibody levels are not yet high enough to be detected, 3) the antibody test may be performed later after infection when the antibody levels have fallen to undetectable levels, and 4) a test result can sometimes be negative in the setting of true infection.
Asymptomatic without ongoing exposure
Jurisdictional recommendations may take into account the epidemiology of Zika virus transmission and other epidemiologic considerations (e.g., seasonality and mosquito surveillance and control factors) in areas with risk for Zika virus transmission. Therefore, jurisdictions might include a routine recommendation to test asymptomatic pregnant women, particularly in areas where local, state, and CDC officials have identified the presence of confirmed, multi-person local mosquito-borne transmission and have determined that the intensity of Zika virus transmission presents a significant risk of Zika virus infection, posing a risk to pregnant women and blood and tissue safety (red areas). Please contact your state health department for state-specific guidance. Testing is not recommended for men and non-pregnant women.
Please note: Your healthcare providers should contact their state, local, or territorial health department to coordinate testing and interpret results. Healthcare providers should discuss the limitations of laboratory tests used to diagnose Zika virus infection with their patients.
Zika virus baby
Congenital Zika syndrome is a group of birth defects associated with Zika infection during pregnancy. Zika is a virus. If you get infected with Zika during pregnancy, the virus can pass through the placenta to your baby. The placenta grows in your uterus (womb) and supplies your baby with food and oxygen through the umbilical cord. Being infected with Zika before birth increases a baby’s risk for these conditions, but not all babies infected have these conditions.
About 1 in 10 pregnant women (10 percent) with Zika infection in the United States and the District of Columbia has a baby with birth defects. A birth defect is a health condition that is present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, in how the body develops or in how the body works. Pregnant women with Zika infection during the first trimester may be more likely to have a baby with birth defects than women infected later in pregnancy. In the United States, the birth defects most strongly linked to Zika infection during pregnancy (like microcephaly) have increased in Puerto Rico and south Florida and Texas where Zika has spread locally. Zika is still spreading in Puerto Rico. Spread of Zika is expected to be low in FLorida and Texas, but some people may still get infected.
Being infected with Zika before birth increases a baby’s risk for birth defects, but not all babies infected have them. Researchers are trying to find out more about babies who are infected or who may have been infected with Zika before birth. This research helps scientists learn how Zika may affect a baby’s health and development at birth and later in life. This is why It’s important for these babies to get early regular medical care.
You can prevent congenital Zika syndrome in your baby by not getting infected with Zika before or during pregnancy. The Zika virus is spread mostly through infected mosquitoes. You also can get it by having unprotected sex with an infected person or by coming into contact with infected body fluids, like through a blood transfusion or if you work in a health care setting.
Congenital Zika syndrome includes these five birth defects:
- Severe microcephaly with a partly collapsed skull. Microcephaly is a birth defect in which a baby’’s head is smaller than expected, compared to babies of the same sex and age. Babies with mild microcephaly often don’t have problems other than small head size. A baby with severe microcephaly has a head that’s much smaller than expected and may have more serious health problems than a baby with mild microcephaly. A baby can develop microcephaly after birth if her head growth slows or doesn’t develop. We don’t know if a newborn who’s infected with Zika around the time of birth will develop microcephaly after birth.
- Less brain tissue than normal, with a specific pattern of brain damage that includes calcium deposits in the deep tissues of the brain. This calcium can build up and affect the way a baby’s brain works.
- Damage to the back of the eye, including macular scarring. The retina is the nerve tissue that lines the back of the eye. It senses light and sends images to your brain. The center of the retina is called the macula. The macula gives the sharp, central vision you need for reading, driving and seeing fine detail. Macular scarring happens when scar tissue forms on the macula.
- Problems with limbs or joints, including birth defects like arthrogryposis, club foot and congenital hip dysplasia. A joint is a part of the body where two or more bones come together, like the knee, hip, elbow or shoulder. A baby with arthrogryposis is born with joint problems that make it hard for her to move her hands or legs. Her joints may not move the right way or they may get stuck in one position. If a baby has clubfoot, one foot or both feet point down and turn in. Babies with clubfoot also may have abnormal foot bones, ankle joints and muscles. Babies born with hip dysplasia have an abnormal hip joint where the top of a hip bone doesn’t stay firmly in the hip socket.
- Hypertonia that limits a baby’s movement after birth. Hypertonia is when your baby has too much muscle tone, so his hands or legs may be stiff and hard to move.
If the Zika virus reaches your baby’s brain, it can slow brain growth and kill brain cells, and some parts of the brain may not develop. Problems in the brain that are linked to congenital Zika virus infection include:
- Brain atrophy. This is a loss of brain cells that can make the brain shrink. Sometimes all of the brain shrinks; other times only a small part of the brain shrinks.
- Brain structures that are missing or don’t develop properly. For example, some babies that may have been exposed to Zika during pregnancy have hypoplasia of the cerebellum. The cerebellum is the part of your brain that helps control your balance and how your body moves. Hypoplasia of the cerebellum is when the cerebellum is smaller than usual or it’s not fully developed.
- Neural tube defects (also called NTDs). An neural tube defect is a birth defect in a baby’s neural tube. The neural tube is part of a developing baby that becomes the brain and spine. Examples of neural tube defects are spina bifida and anencephaly.
- Fetal brain disruption sequence. Babies with this condition may have severe microcephaly, problems with the skull (including collapsed skull or skull bones that overlap), extra skin on the scalp and problems with the nervous system. Your baby’s nervous system is made up of the brain, spinal cord and nerves. The nervous system helps your baby move, think and feel.
- Smooth brain. A healthy brain has many folds and grooves in it. For some babies, the brain may be smooth with no folds or few folds. Some babies with smooth brain don’t have serious health problems, but others stop developing after 3 to 5 months and many die before they’re 2 years old.
- Thin cerebral cortex with enlarged ventricles and hydrocephalus. The cerebral cortex is the thin layer of cells that covers the brain. It helps the brain process information. Ventricles are spaces in the brain that fill with fluid. When fluid builds up, it causes pressure on the brain. This is called hydrocephalus.
Other health conditions linked to congenital Zika infection include:
- Cerebral Palsy. This is a group of conditions that affects the parts of the brain that control muscles. This can cause problems with movement, posture (standing up straight) and balance.
- Low birthweight. This is when a baby is born weighing less than 5 pounds, 8 ounces.
- Growth and development problems, including trouble swallowing (also called dysphagia), problems with balance and movement, trouble sitting up and intellectual and developmental disabilities. These are problems with how the brain works that can cause a person to have trouble or delays in physical development, learning, communicating, taking care of himself or getting along with others.
- Hearing loss and other hearing problems. Hearing loss is when your baby can’t hear sound in one or both ears.
- Nervous system problems, including epilepsy, hypotonia, hyperreflexia, severe fussiness and tremors (also called body shakes). Epilepsy is a seizure disorder that affects how the nerve cells in your brain work. A seizure is when the whole body or parts of the body move without control. Hypotonia is when your baby has too little muscle tone, so he may seem floppy and have poor head control (his head falls forward, backward or to the side). Hyperreflexia is when you baby has overactive reflexes.
- Sleeping problems
- Vision problems, including cataracts, colomba and congenital glaucoma. A cataract is a film or cloud that covers the eye’s lens and affects a baby’s vision. Columba is when there are missing pieces of tissues in the structures that form the eye. Congenital glaucoma is a group of diseases that damage the eye’s optic nerve. The optic nerve connects the retina to the brain. Glaucoma can lead to vision loss and blindness.
Congenital Zika syndrome diagnosis
Not all babies are checked for congenital Zika syndrome after birth. Your baby should get tested for Zika infection and health conditions that are part of congenital Zika syndrome if:
- Your baby has birth defects that are part of congenital Zika syndrome and you may have been exposed to Zika during pregnancy.
- Your baby doesn’t have birth defects that are part of congenital Zika syndrome, but lab tests show you possibly had Zika infection during pregnancy.
If you may have been exposed to Zika during pregnancy, but lab tests don’t show possible Zika infection and your baby doesn’t have birth defects that are part of congenital Zika syndrome, talk to your baby’s provider to decide if testing is right for your baby. Even if your baby looks and seems healthy at birth, he may have effects of congenital Zika syndrome as he gets older. So it’s important that you take him to all his medical checkups so his providers can make sure he’s doing well. Checkups also let providers spot and treat conditions early to help prevent health problems later on. Tell your provider if you’re worried about your baby’s health and development.
Your baby’s health care provider uses these tests to check for Zika infection and related health conditions:
- A blood and urine test for Zika. Your baby gets tested as soon as possible, ideally within the first few days after birth. Your baby’s spinal fluid may be tested for Zika, especially if your baby’s blood and urine tests are negative for Zika and your baby’s provider can’t find another cause of your baby’s birth defects.
- A physical exam to check your baby’s head size, weight and length
- An eye exam before your baby’s 1 month old to check for vision problems
- A hearing test called automated auditory brainstem response (also called AABR). Your baby gets this test before she’s 1 month old, if she didn’t have automated auditory brainstem response as part of newborn screening. Automated auditory brainstem response (AABR) uses patches called electrodes and a computer to check how your baby’s nerves in the brain react to sounds. Your baby gets newborn screening before she leaves the hospital after birth. Newborn screening checks for serious but rare conditions that your baby has at birth. It includes blood, hearing and heart screening.
- Ultrasound of the head before your baby’s 1 month old to check her skull and brain. An ultrasound uses sound waves and a computer screen to show a picture of the inside of your baby’s body.
If your baby was infected with Zika before birth, was born with congenital Zika syndrome or may have congenital Zika syndrome, does he need special medical care?
Yes. If your baby was infected before birth or has or may have congenital Zika syndrome, a team of health care providers cares for your baby. The kind of checkups and medical care your baby needs depend on his condition at birth.
Zika Care Connect 3 is a website that offers up-to-date information about caring for babies and children who have been exposed to Zika and may have congenital Zika syndrome. It also offers a database of providers who care for these babies and children. You can search the database by things like location, kind of provider, the language the provider speaks and the insurance the provider takes. Use Zika Care Connect 3 to find the right providers to take care of your baby.
The team of providers caring for your baby knows how to treat health conditions that come with congenital Zika syndrome. They work together to coordinate your baby’s care to make sure she gets regular medical checkups as she grows, as well as treatment she needs for conditions that come with congenital Zika syndrome. Depending on your baby’s condition, she may need long-term treatment.
Your baby’s health care team is led by the provider who gives your baby general medical care. This may be your baby’s regular health care provider, or it may be a provider who has more experience taking care of babies with congenital Zika syndrome.
If your baby has congenital Zika syndrome, the lead provider may be a:
- Pediatrician. This is a doctor who has training to take care of babies and children.
- Family practice doctor (also called a family physician). This is a doctor who takes care of every member of the family. A family practice doctor can be your health care provider before, during and after pregnancy, and your baby’s provider, too.
- Neonatologist. This is a doctor who takes care of sick newborns, including premature babies (babies born before 37 weeks of pregnancy) and babies with birth defects.
- Pediatric nurse practitioner (also called PNP). This is a registered nurse who has advanced training to take care of babies and children.
- Family nurse practitioner (also called FNP). This is a registered nurse with advanced training to take care of every member of your family.
Providers who treat problems with digestion and feeding
- Gastroenterologist. This doctor treats digestion and feeding problems. Digestion is the process of how your baby’s body breaks down food after she eats.
- Lactation consultant. This person is trained to help women breastfeed, even women who have breastfeeding problems.
- Nutritionist. This person can help make sure your baby gets all the nutrients she needs for healthy growth and development.
- Pulmonologist. This doctor treats lung conditions, like aspiration. Aspiration is when your baby sucks food or drink into her airway.
- Otolaryngologist (also called an ear, nose and throat specialist or ENT). This doctor may treat your baby if she has feeding problems, like poor suck, trouble swallowing, reflux or aspiration. Reflux is when the milk or food your baby swallows comes back up into her esophagus. The esophagus is the tube that carries food and drink from your baby’s mouth to her stomach.
Providers who treat problems with the eyes and ears
- Audiologist. This provider has training to treat hearing problems and hearing loss.
- Ophthalmologist. This is a doctor who treats eye problems.
- Otolaryngologist (also called an ear, nose and throat specialist or ENT). This doctor treats problems of the ears, nose and throat.
Providers who treat problems with the brain, nerves, spine, bones and joints
- Endocrinologist. This doctor treats gland or hormone problems. A gland is an organ that makes hormones (chemicals) that help your baby’s body work. Babies with brain development problems may have problems with their glands and hormones.
- Neurologist. This doctor treats brain, spine and nerve problems.
- Orthopedist. This doctor treats bone and joint problems.
- Physiatrist. This doctor treats health conditions that affect the brain, nerves, bones and muscles. He also has special training in treating patients with disabilities.
- Radiologist. This doctor uses imaging tests to diagnose and treat disease, like microcephaly and other problems. Imaging tests include ultrasound and magnetic resonance imaging (also called MRI). MRI is a medical test that makes a detailed picture of the inside of your baby.
Providers who treat developmental conditions
- Developmental pediatrician. This doctor has training in child development and taking care of children with special needs. If your baby has developmental delays, he may need to see a developmental pediatrician. Developmental delays are when your child doesn’t reach developmental milestones when expected. Milestones are skills or activities that most children can do at a certain age. Milestones include sitting, walking, talking, having social skills and having thinking skills.
- Occupational therapist. This person trained to help people learn to do everyday activities. For children, this may be things like brushing teeth, getting dressed, putting on shoes or learning to use a pencil. If your baby has feeding problems, she may need treatment from an occupational therapist.
- Physical therapist. This provider creates exercise programs to help build strength and help with movement. If your baby has a condition like hypertonia, clubfoot or arthrogryposis, physical therapy may help these conditions.
- Speech therapist. This provider helps people with speech and language problems. A speech therapist also may help your baby if she has feeding problems.
Other providers who treat conditions caused by congenital Zika syndrome
- Infectious disease specialist. This doctor diagnoses and treats infections. He checks your baby for infections that may cause problems for your baby, including syphilis, toxoplasmosis, rubella, cytomegalovirus and herpes.
- Clinical geneticist. This doctor tries to find out the causes of birth defects and other genetic conditions (health conditions caused by genes). If your baby has microcephaly, a clinical geneticist may check to see if it’s caused by something other than Zika infection.
Providers who help families take care of a sick baby and cope with the stress of having a sick baby
- Mental health professional. This provider helps people with emotional or mental health problems, like depression. She can help people cope with the stress of caring for a baby with health conditions that come with congenital Zika syndrome. Mental health providers include social workers, therapists, counselors, psychologists, psychiatrists and psychiatric nurse practitioners.
- Social worker. A social worker help people solve problems and make their lives better. Most hospitals have social workers who can help connect you with the resources you need to care for your baby.
If my baby has developmental delays, does she need early intervention services?
Yes. If your baby has developmental delays, it’s important to get early intervention services as soon as possible. Developmental delays are when your child doesn’t reach developmental milestones when expected. A developmental milestone is a skill or activity that most children can do at a certain age. Milestones include sitting, walking, talking, having social skills and having thinking skills. Early intervention services can help improve your child’s development. They can help children from birth through 3 years old learn important skills. Services include therapy to help a child talk, walk, learn self-help skills and interact with others.
The CDC program 4 Learn the signs. Act early, offers tools and information for parents who think their child may have developmental delays. You can find your state’s contact information for early intervention services. You don’t need a doctor’s referral or a medical diagnosis to ask for a free screening.
If my baby has congenital Zika syndrome, is it OK to breastfeed?
Yes. Breast milk is the best food for most babies for the first year of life. If your baby has problems swallowing or feeding, his provider may refer you to a lactation consultant for help. Even if your baby breastfeeds well after birth in the hospital, he may have feeding problems after you’re home. If you’re worried about your baby’s feeding, tell his provider.
Zika virus prevention
- Pregnant women and their partners who live in or travel to red or yellow areas should be counseled to consistently and correctly use condoms every time they have sex (including vaginal, anal, and oral sex) to prevent Zika virus infection or they should not have sex during the pregnancy.
- Couples in which one or both partners have had exposure1 who want to reduce their risk for spreading Zika through sex to the uninfected partner should be advised to use condoms consistently and correctly or abstain from sex for:
- At least 8 weeks after symptom onset or last possible Zika virus exposure, (if only the woman was exposed), or
- At least 6 months after symptom onset or last possible Zika virus exposure (if the man was exposed)
- If couples are asymptomatic and possible exposure to Zika is ongoing, Healthcare providers should discuss reproductive life plans with their patients (See “Preconception counseling” above)
- All women and men who live in or travel to red or yellow areas should be advised to remain aware of Zika virus transmission and strictly follow steps to prevent mosquito bites.
- All travelers to red or yellow areas should be advised to use insect repellent for 3 weeks after returning home to prevent passing Zika to mosquitoes that could infect others.
- All travelers to red or yellow areas should be counseled on the potential consequences of Zika virus infection to the fetus during pregnancy and the traveler’s role in preventing transmission to pregnant women in their communities.
- Stay in air-conditioned or well-screened housing. The mosquitoes that carry the Zika virus are most active from dawn to dusk, but they can also bite at night. Consider sleeping under a mosquito bed net, especially if you are outside.
- Wear protective clothing. When you go into mosquito-infested areas, wear a long-sleeved shirt, long pants, socks and shoes.
- Use mosquito repellent. Permethrin can be applied to your clothing, shoes, camping gear and bed netting. You also can buy clothing made with permethrin already in it. For your skin, use a repellent containing at least a 10 percent concentration of DEET. When used as directed, insect repellents that are registered with the Environmental Protection Agency (EPA) are proven safe and effective for pregnant and breast-feeding women.
- Reduce mosquito habitat. The mosquitoes that carry the Zika virus typically live in and around houses, breeding in standing water that can collect in such things as animal dishes, flower pots and used automobile tires. Reduce the breeding habitat to lower mosquito populations.
Zika virus transmitted through blood transfusion
All blood donations are now screened for Zika virus. To further reduce the risk of transmitting Zika virus through blood transfusion in areas where there are no active Zika virus outbreaks, the Food and Drug Administration recommends not donating blood for four weeks if you:
- Have a history of Zika virus infection
- Traveled or lived in an area with active Zika virus transmission
- Have symptoms that are suggestive of Zika virus infection within two weeks of travel from an area with Zika virus
- Have had sexual contact with a male partner who has been diagnosed with Zika virus infection
- Have had sexual contact with a male partner who has traveled or lived in an area with active Zika virus transmission in the past three months
If you or your partner have or may have Zika, when is it OK to get pregnant?
Remember, most people who have Zika don’t have signs or symptoms. If you think you or your partner may have Zika but haven’t had signs or symptoms, talk to your provider.
The CDC says:
| Affected Partner | Timeframe to Prevent Sexual Transmission |
|---|---|
| If a couple has a male partner and only he travels to an area with risk of Zika | The couple should consider using condoms or not having sex for at least 6 months
|
| If a couple has a female partner and only she travels to an area with risk of Zika | The couple should consider using condoms or not having sex for at least 8 weeks
|
| If the couple contains both a male and female partner and both travel to an area with risk of Zika | The couple should consider using condoms or not having sex for at least 6 months
|
The CDC recommends that you wait at least this long to be sure you and your partner aren’t infected with Zika virus when you try to get pregnant. If you live in or often travel to a Zika-affected area, talk to your health care provider about getting tested for Zika before you try to get pregnant. Zika infection usually stays in your blood for a few days to a week, but it can stay in blood for more than 12 weeks and it has been found in an infected man’s semen more than 3 months after symptoms started.
Mosquito Bites Prevention
Protect yourself and your family from mosquito bites
Use Insect Repellent
Use Environmental Protection Agency 5-registered insect repellents with one of the active ingredients below. When used as directed, EPA-registered insect repellents 5 are proven safe and effective, even for pregnant and breastfeeding women.
- DEET
- Picaridin (known as KBR 3023 and icaridin outside the US)
- IR3535
- Oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD)
- 2-undecanone
Always use as directed. Insect repellents containing DEET and picaridin are safe for pregnant and breastfeeding women and children older than 2 months when used according to the product label.
Find the insect repellent that’s right for you by using EPA’s search tool 6.
Tips for Everyone
- Always follow the product label instructions.
- Reapply insect repellent as directed.
- Do not spray repellent on the skin under clothing.
- If you are also using sunscreen, apply sunscreen first and insect repellent second.
- Use permethrin-treated clothing and gear (such as boots, pants, socks, and tents.
- Use bed nets as necessary.
- Stay and sleep in screened-in or air-conditioned rooms.
Tips for Babies & Children
- Always follow instructions when applying insect repellent to children.
- Do not use insect repellent on babies younger than 2 months old.
- Do not apply insect repellent onto a child’s hands, eyes, mouth, and cut or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- Do not use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
Protect your baby or child
- Dress your child in clothing that covers arms and legs.
- Cover crib, stroller, and baby carrier with mosquito netting.
Natural insect repellents (repellents not registered with EPA)
- Scientists do not know the effectiveness of non-EPA registered insect repellents, including some natural repellents.
- To protect yourself against diseases spread by mosquitoes, CDC and EPA recommend using an EPA-registered insect repellent.
- Choosing an EPA-registered repellent ensures the EPA has evaluated the product for effectiveness.
Wear long-sleeved shirts and long pants
- Treat items, such as boots, pants, socks, and tents, with permethrin* or buy permethrin-treated clothing and gear.
- Permethrin-treated clothing will protect you after multiple washings. See product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do not use permethrin products directly on skin.
*In some places, such as Puerto Rico, where permethrin products have been used for years in mosquito control efforts, mosquitoes have become resistant to it. In areas with high levels of resistance, use of permethrin is not likely to be effective.
Take steps to control mosquitoes inside and outside your home
- Use screens on windows and doors. Repair holes in screens to keep mosquitoes outside.
- Use air conditioning when available.
- Sleep under a mosquito bed net if air conditioned or screened rooms are not available or if sleeping outdoors.
- Once a week, empty and scrub, turn over, cover, or throw out items that hold water, such as tires, buckets, planters, toys, pools, birdbaths, flowerpots, or trash containers. Check inside and outside your home. Mosquitoes lay eggs near water.
Sexual Transmission and Prevention
Zika Can Be Passed Through Sex
- Zika can be passed through sex from a person with Zika to his or her partners.
- Sex includes vaginal, anal, and oral sex and the sharing of sex toys.
- Zika can be passed through sex even in a committed relationship.
- The timeframes that men and women can pass Zika through sex are different because Zika virus can stay in semen longer than in other body fluids.
Infected People Can Pass Zika Through Sex Even When They Don’t Have Symptoms
- Many people infected with Zika virus won’t have symptoms or will only have mild symptoms, and they may not know they have been infected.
- Zika can also be passed from a person before their symptoms start, while they have symptoms, and after their symptoms end.
How to Protect Yourself During Sex
- Condoms can reduce the chance of getting Zika from sex.
- Condoms include male and female condoms.
- To be effective, condoms should be used from start to finish, every time during vaginal, anal, and oral sex and the sharing of sex toys
- Dental dams may also be used for certain types of oral sex (mouth to vagina or mouth to anus).
- Not sharing sex toys can also reduce the risk of spreading Zika to sex partners.
- Not having sex eliminates the risk of getting Zika from sex.
Pregnant Couples
- Pregnant women should NOT travel to areas with risk of Zika. If a pregnant woman must travel to one of these areas, she should talk to her healthcare provider first.
- If a pregnant woman or her partner travel to an area with risk of Zika, the couple should use condoms from start to finish every time they have sex or not have sex for the entire pregnancy, even if the traveler does not have symptoms of Zika or feel sick.
- Pregnant couples should use condoms from start to finish every time they have sex, or they should not have sex for the entire pregnancy.
Couples Interested in Pregnancy
| Affected Partner | Timeframe to Prevent Sexual Transmission |
|---|---|
| If a couple has a male partner and only he travels to an area with risk of Zika | The couple should consider using condoms or not having sex for at least 6 months
|
| If a couple has a female partner and only she travels to an area with risk of Zika | The couple should consider using condoms or not having sex for at least 8 weeks
|
| If the couple contains both a male and female partner and both travel to an area with risk of Zika | The couple should consider using condoms or not having sex for at least 6 months
|
Living in an area with risk of Zika
Uninfected couples living in an area with risk of Zika can use condoms or not have sex if they are concerned with passing or getting Zika through sex.
Decisions about having sex and using condoms depend on each person’s understanding of the risks and benefits, including
- The mild nature of the illness for many people
- Their possible exposure to mosquitoes while in an area with risk of Zika
- Their plans for pregnancy (if appropriate) and access to birth control
- Their access to condoms
- Their desire for intimacy, including willingness to use condoms or not have sex
- Their ability to use condoms or not have sex
If either partner develops symptoms of Zika or has concerns, they should talk to a healthcare provider.
Zika virus symptoms
Most people with Zika (about 80 percent or 4 in 5 people) don’t get sick and have no signs or symptoms. If you do get sick with Zika, it’s usually a mild illness, and you may not even know you’re infected.
If you do have signs or symptoms of Zika, they usually begin 2 to 7 days after you’ve been exposed to the virus. Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. You can be sick with Zika for several days to a week.
Signs and symptoms of Zika include:
- Headache
- Fever (You may or may not have a fever if you have Zika.)
- Joint or muscle pain
- Pink eye (also called conjunctivitis) or pain behind the eyes
- Rash
- Throwing up
There are no medicines to treat Zika. If you have signs or symptoms, you can:
- Get plenty of rest.
- Drink plenty of fluids.
- Take acetaminophen (Tylenol®) to relieve fever and pain.
If you or anyone in your family has or may have Zika, protect yourselves from mosquito bites. This can help prevent Zika virus from spreading to others.
How Zika is Diagnosed
- To diagnose Zika, a doctor or other healthcare provider will ask about any recent travel and any signs and symptoms. A blood or urine test can confirm a Zika infection.
- The doctor or other healthcare provider may order blood or urine tests to look for Zika or other viruses like dengue or chikungunya.
- Make sure to receive your Zika test results even if you are feeling better.
Only Some People Need Zika Testing
Zika virus testing is recommended only for certain people. If you have questions or think you should be tested, talk to your healthcare provider.
If You Have Symptoms
Zika testing is recommended if you have symptoms of Zika and
- You live in or traveled to an area with risk of Zika or
- You had sex without a condom with a partner who lives in or traveled to an area with risk of Zika.
Pregnant Women
Zika testing is recommended for pregnant women who don’t have Zika symptoms in certain cases. You should be tested for Zika if you are pregnant and
- You have ongoing exposure to Zika because you live in or frequently travel to an area with risk of Zika or
- Your doctor sees Zika-associated abnormalities on an ultrasound or you deliver a baby with birth defects that may be related to Zika.
Testing Guidance for Symptomatic Pregnant Women
Pregnant women who report signs or symptoms consistent with Zika virus disease (acute onset of fever, rash, arthralgia, conjunctivitis) should be tested for Zika virus infection. For symptomatic pregnant women who live in or traveled to an area with risk of Zika or had sex without a condom with a partner who lived in or traveled to an area with risk of Zika, concurrent testing of serum and urine by RNA NAT and Zika virus IgM testing of serum is recommended as soon as possible up through 12 weeks after symptoms began.
- A positive RNA NAT result on both serum and urine, regardless of IgM results, should be interpreted as an acute maternal Zika virus infection.
- A positive RNA NAT result on either serum or urine, in conjunction with a positive Zika IgM, should be interpreted as evidence of acute Zika virus infection.
- A negative RNA NAT result in conjunction with a non-negative Zika virus IgM test result should be followed by plaque reduction neutralization test (PRNT).
Testing Partners of Pregnant Women
CDC recommends Zika virus testing for anyone who is not pregnant who has been exposed to Zika and who also has Zika symptoms, including sex partners of pregnant women.
Testing does not determine how likely a person is to pass Zika virus through sex. Because Zika virus can remain in some fluids (e.g., semen) longer than blood, someone might have a negative blood test, but still carry Zika in their genital secretions.
Further, intermittent shedding in semen can occur with other viruses and the pattern of Zika virus shedding in semen is unknown. In addition, the detection of Zika virus RNA in semen might not indicate the presence of infectious virus in semen. Testing semen and vaginal fluids for Zika virus is not currently available outside of the research setting. Studies are underway to better understand the performance of these tests, the persistence of Zika virus in these fluids, and how best to interpret the results.
If You Have Tested Positive for Zika
- If you are pregnant, you can pass Zika to your fetus.
- You can pass Zika to your sex partner(s).
- You can pass Zika to mosquitoes, which can bite you, get infected with Zika virus, and spread the virus to other people.
Testing for Zika Virus
Zika virus testing is performed at CDC, at several state, local, and territorial health departments, and at some commercial laboratories. Several tests are available to help determine if a person is infected with Zika virus. Healthcare providers should contact their state or local health department to facilitate testing.
Testing Guidance
CDC recommends Zika virus testing for:
- Anyone with possible Zika virus exposure* who has or recently experienced symptoms of Zika.
- Symptomatic pregnant women with possible Zika virus exposure
- Asymptomatic pregnant women with ongoing possible Zika virus exposure
- Pregnant women with possible Zika virus exposure who have a fetus with prenatal ultrasound findings consistent with congenital Zika virus infection
Zika testing may be considered for:
- Asymptomatic pregnant women with recent possible but no ongoing exposure to Zika virus (i.e., travelers)
Zika virus testing is not recommended for:
- Non-pregnant asymptomatic individuals
- Preconception screening
*Possible exposure includes living in, traveling to, or having unprotected sex with someone who lives in or traveled to an area with risk of Zika.
Testing Guidance for Non-Pregnant Symptomatic Individuals
Non-pregnant symptomatic individuals with possible exposure to Zika virus should receive testing of serum and urine by Zika virus ribonucleic acid (RNA) nucleic acid testing (NAT) and Zika virus and/or dengue virus IgM testing of serum. NAT testing is dependent on the timing of specimen collection. NAT testing should be performed on specimens collected <14 days after symptom onset. Zika virus and dengue virus IgM serology testing should be performed on NAT negative samples collected <14 days after onset of symptoms or on samples collected ≥14 days after onset of symptoms. NAT testing is not recommended on specimens collected ≥ 14 days after symptom onset.
Testing Guidance for Asymptomatic Pregnant Women
- Asymptomatic pregnant women with ongoing possible Zika virus exposure (i.e., residence in or frequent travel to an area with risk of Zika) should be tested. NAT testing is recommended three times during pregnancy. IgM serology testing is not routinely recommended. Recommendations for the timing of NAT testing are at the initial prenatal care visit, followed by two additional NAT tests performed during pregnancy, coinciding with non-consecutive prenatal visits. Timing of additional NAT testing may be informed by jurisdictional trends in Zika virus transmission, the expected length of Zika virus nucleic acid detection in serum, and the duration of exposure during pregnancy. Although not routinely recommended, after pre-test counseling and individualized risk assessment, physicians and patients, through a shared decision-making model, may collaboratively elect to have IgM testing performed concurrent with NAT testing. For women who have a positive NAT test during pregnancy, additional NAT testing is not recommended. If a patient has previously been confirmed positive for Zika virus infection, no additional IgM serology testing is recommended.
- Asymptomatic pregnant women with recent possible exposure to Zika virus but no ongoing exposure (i.e., travelers) may be considered for testing. Although not routinely recommended, testing may be considered on a case-by-case basis using a shared physician-patient decision-making model and in line with jurisdictional recommendations. If testing of asymptomatic pregnant women is performed, the same algorithm as for symptomatic pregnant women should be followed using the timeframe from the last possible exposure to Zika virus.
Note: Jurisdictions may take into account local epidemiologic considerations (e.g., seasonality, geography, and mosquito surveillance and control factors) in making recommendations for Zika virus testing for this group of pregnant women; therefore, testing recommendations for this group of pregnant women may differ by jurisdiction. Please contact your state, tribal, local, or territorial health department for jurisdiction specific guidance.
- Pregnant women with possible exposure to Zika virus and who have a fetus with prenatal ultrasound findings consistent with congenital Zika virus infection should be tested. NAT and IgM testing should be performed on maternal serum and urine following the algorithm for symptomatic pregnant women. If amniocentesis is being performed as part of clinical care, NAT testing of amniocentesis specimens should also be performed. Testing of placental and fetal tissues may also be considered.
Sexual Transmission and Testing
A blood or urine test can confirm Zika infection from sexual transmission; however, testing blood, semen, vaginal fluids, or urine is not recommended to determine how likely a person is to pass Zika virus through sex.
Zika virus treatment
Zika virus disease is usually relatively mild. Currently, there is no cure or specific treatment for Zika virus. Treatment aims to ease symptoms and reduce the risk of complications while the person recovers. If you have visited a country with active Zika virus transmission and have symptoms that could be caused by Zika infection, you should seek medical care and advice, especially as there could be other causes of your symptoms.
People diagnosed with Zika virus infection should:
- get plenty of rest
- drink enough fluids
- treat pain and fever with common medicines such as paracetamol
- do not take aspirin or other non-steroidal anti-inflammatory drugs unless advised by your doctor, as these can be associated with a risk of bleeding if there is a dengue infection present.
If symptoms worsen, seek further medical care and advice.
No vaccine exists to prevent Zika virus.
- Zika Travel Information. https://wwwnc.cdc.gov/travel/page/zika-travel-information[↩][↩]
- CDC Zika Interim Response Plan. https://www.cdc.gov/zika/public-health-partners/cdc-zika-interim-response-plan.html[↩]
- Zika Care Connect. https://www.zikacareconnect.org/[↩][↩]
- Learn the Signs. Act Early. https://www.cdc.gov/ncbddd/actearly[↩]
- Repellents: Protection against Mosquitoes, Ticks and Other Arthropods. https://www.epa.gov/insect-repellents[↩][↩]
- Find the Repellent that is Right for You. https://www.epa.gov/insect-repellents/find-repellent-right-you[↩]