Contents
- What is atrial tachycardia
What is atrial tachycardia
Atrial tachycardia is a least common type of supraventricular tachycardia (SVT), constituting 5-15% of all SVTs, that does not require the atrioventricular (AV) junction, accessory pathways, or ventricular tissue for its initiation and maintenance. Atrial tachycardia may occur at any age, although it is more common in children and adults with congenital heart disease. Atrial tachycardia is generally seen in children with underlying heart disorders such as congenital heart disease, particularly those who’ve had heart surgery, particularly after surgery for repair or correction of congenital or valvular heart disease. Atrial tachycardia can also occur in persons with normal hearts. Atrial tachycardia occurs less commonly with heart attack, serious mitral valve disease. In patients with structurally normal hearts, atrial tachycardia is associated with a low mortality rate. Patients with underlying structural heart disease, congenital heart disease, or lung disease are less likely to be able to tolerate this rhythm disturbance. Atrial tachycardia has no known racial or ethnic predilection and no known predilection for either sex. There may be some association with pregnancy.
Atrial tachycardia may also be triggered by factors such as an infection or drug or alcohol use. For some people, atrial tachycardia increases during pregnancy or exercise.
A normal heart rate is 60 to 100 beats per minute. A heart rate of more than 100 beats per minute is called a tachycardia. This occurs when the electrical impulses that coordinate your heartbeats don’t work properly. It may feel like a fluttering or racing heart.
Atrial tachycardia episodes typically begin slowly, gradually increasing to more than 100 beats per minute before returning to a normal heart rate of around 60 to 80 beats per minute. In some cases, these episodes occur more abruptly or occur continuously. The rapid heartbeat does not allow enough time for your heart to fill before it contracts so blood flow to the rest of your body is compromised.
In adults, tachycardia is usually defined as a heart rate more than 100 beats per minute (bpm). In children, the definition of tachycardia varies because the normal heart rate is age dependent, as follows 1:
- Age 1-2 days: 123-159 bpm
- Age 3-6 days: 129-166 bpm
- Age 1-3 weeks: 107-182 bpm
- Age 1-2 months: 121-179 bpm
- Age 3-5 months: 106-186 bpm
- Age 6-11 months: 109-169 bpm
- Age 1-2 years: 89-151 bpm
- Age 3-4 years: 73-137 bpm
- Age 5-7 years: 65-133 bpm
- Age 8-11 years: 62-130 bpm
- Age 12-15 years: 60-119 bpm
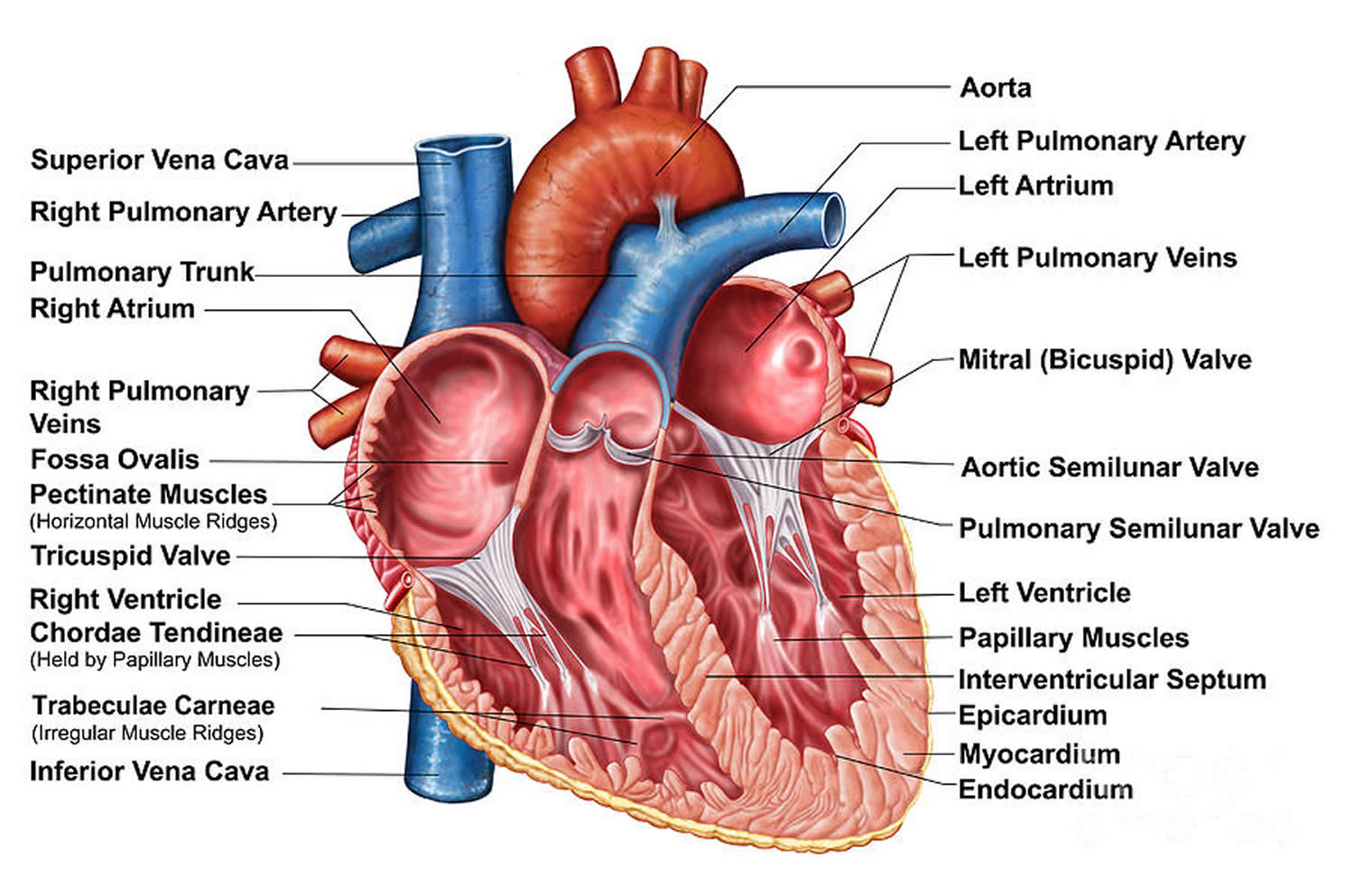
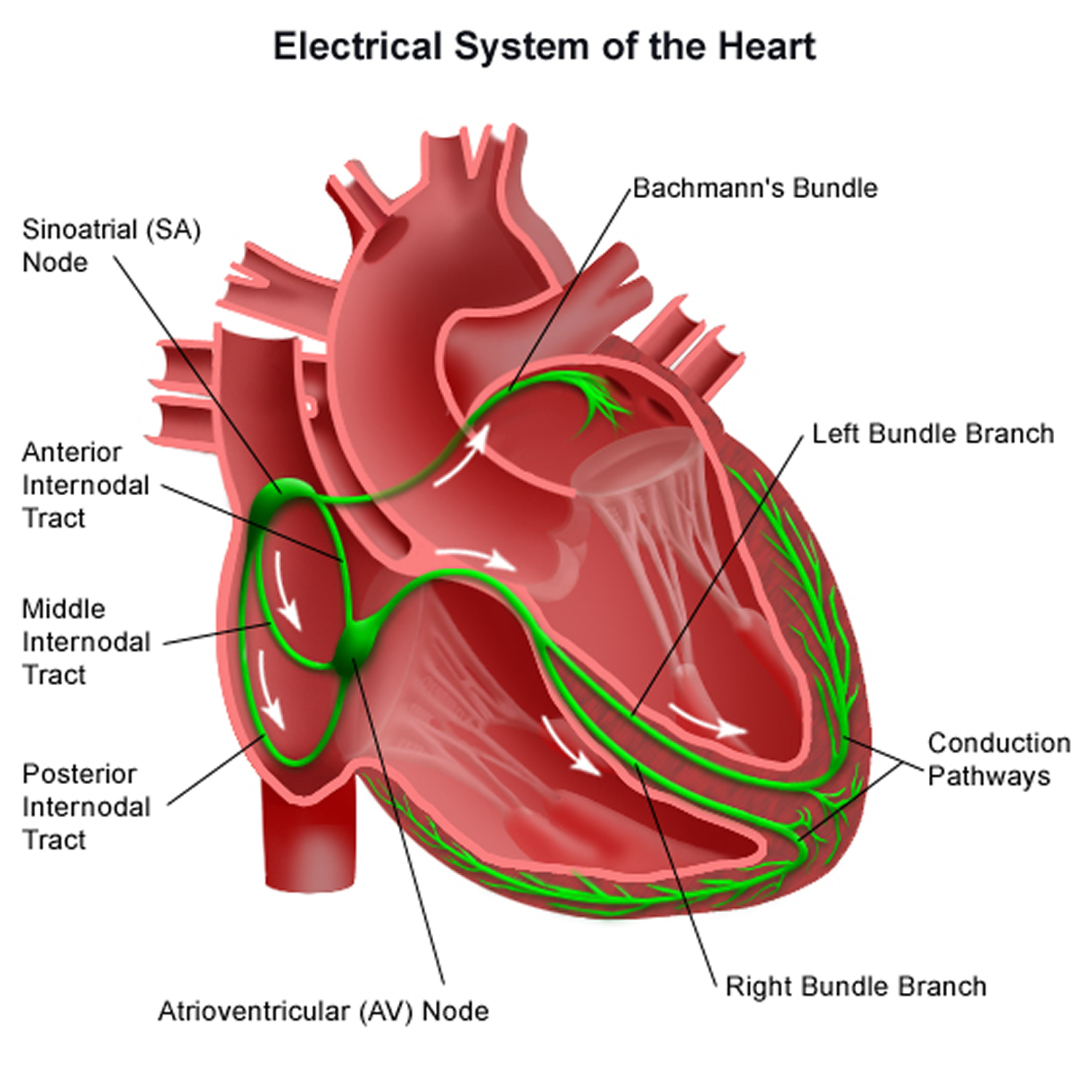
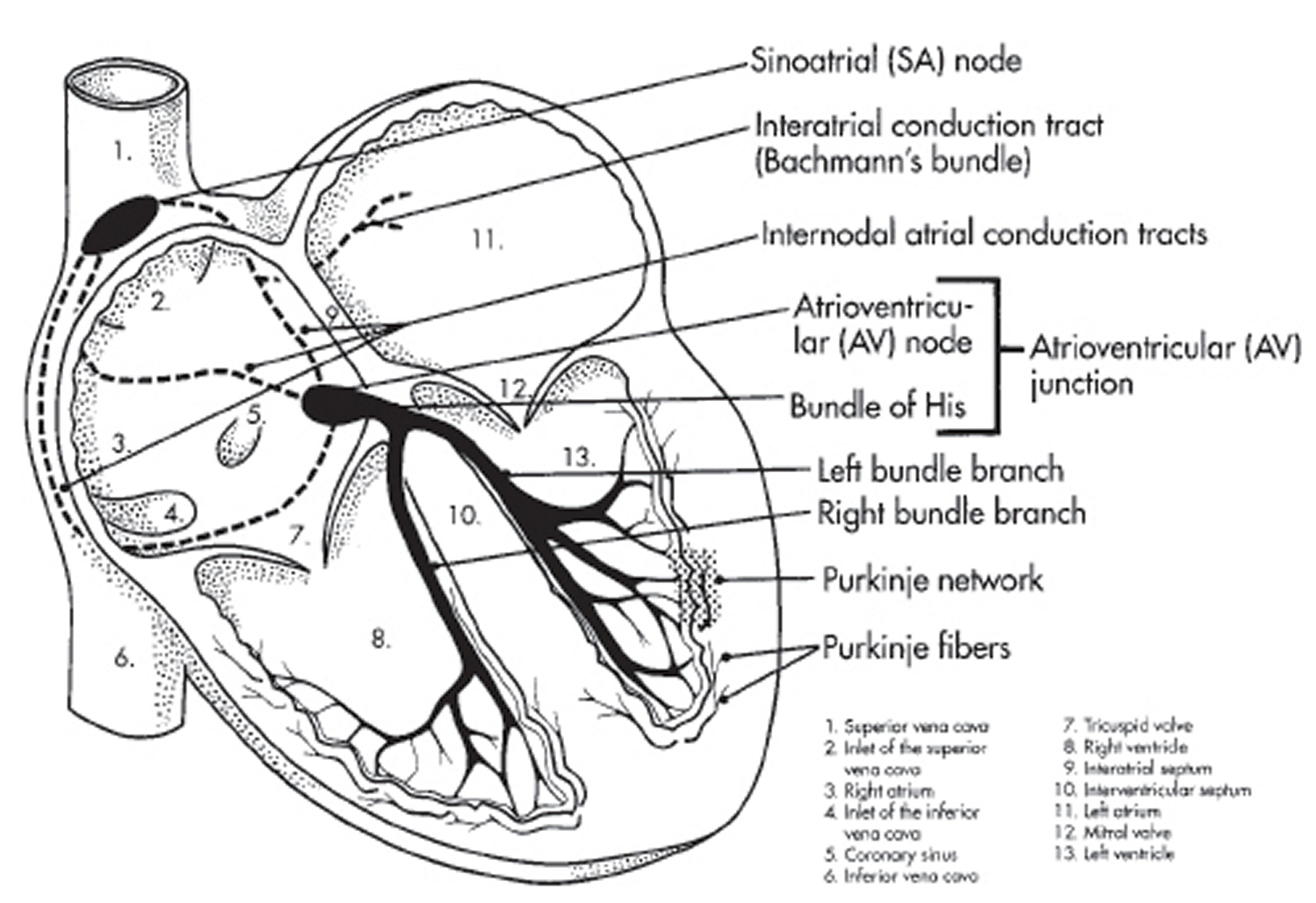
Heartbeats are normally initiated by a small group of cells at the top of the heart in the right atrium called the sinoatrial node (SA node), which acts as the heart’s natural pacemaker (see Figure 1).
The sinoatrial node (SA node) produces electrical signals that pass through the muscles of the upper heart chambers (atria), causing them to contract and pump blood into the lower heart chambers (ventricles).
The signal then passes into another group of cells in the middle of the heart called the atrioventricular (AV) node. From here, the signals travel into the ventricle muscles, causing them to contract and pump blood out of the heart.
Episodes of atrial tachycardia or supraventricular tachycardia (SVT) occur when a problem develops in the heart’s electrical system. This causes faster signals to be sent around the heart, increasing the speed at which the heart beats.
A number of methods are used to classify atrial tachycardia. Classification in terms of origin can be based on endocardial activation mapping data, pathophysiologic mechanisms, and anatomy.
On the basis of endocardial activation, atrial tachycardia may be divided into the following 2 groups:
- Focal atrial tachycardia: Arises from a localized area in the atria such as the crista terminalis, pulmonary veins, ostium of the coronary sinus, or intra-atrial septum. If it originates from the pulmonary veins, it may trigger atrial fibrillation and often forms a continuum of arrhythmias.
- Reentrant atrial tachycardias: Usually macroreentrant; reentrant atrial tachycardias most commonly occur in persons with either structural or complex heart disease, particularly after surgery involving atrial incisions or scarring. Electrophysiologically, these atrial tachycardias are similar to atrial flutters, typical or atypical. Often, the distinction is semantic, typically based on arbitrary cutoffs of atrial rate.
- Other methods of classification are as follows:
- Pathophysiologic mechanisms: Atrial tachycardia can be classified as the result of enhanced automaticity, triggered activity, or reentry
- Anatomy: Classification of atrial tachycardia can be based on the location of the arrhythmogenic focus.
Atrial tachycardia can have a right or left atrial origin. Some atrial tachycardias actually originate outside the usual anatomic boundaries of the atria, in areas such as the superior vena cava, pulmonary veins, and vein of Marshall, where fingers of atrial myocardium extend into these locations. Rare locations, such as the noncoronary aortic cusp 2 and hepatic veins, have been described, as well.
A number of aspects of the atrial anatomy can contribute to the substrate for arrhythmia. The orifices of the vena cava, pulmonary veins, coronary sinus, atrial septum, and mitral and tricuspid annuli are potential anatomic boundaries for reentrant circuits.
Anisotropic conduction in the atria due to complex fiber orientation may create the zone of slow conduction. Certain atrial tissues, such as the crista terminalis and pulmonary veins, are common sites for automaticity or triggered activity. Additionally, disease processes or age-related degeneration of the atria may give rise to the arrhythmogenic substrate.
- Abnormalities that have been reported at the sites of atrial tachycardia origin include the following 3 :
- Extensive myocardial fibrosis
- Myocyte hypertrophy
- Endocardial fibrosis
- Mononuclear cell infiltration
- Mesenchymal cell proliferation
- Islets of fatty tissue
- Thinning
- Blebs
Manifestations of atrial tachycardia include the following:
- Rapid pulse rate: In most atrial tachycardias, the rapid pulse is regular; it may be irregular in rapid atrial tachycardias with variable AV conduction and in multifocal atrial tachycardia (multifocal atrial tachycardia)
- Episodic or paroxysmal occurrence
- Sudden onset of palpitations
- Continuous, sustained, or repetitive tachycardia: If atrial tachycardia is due to enhanced automaticity
- Warm-up phenomenon: Tachycardia gradually speeds up soon after onset (may be clinically inapparent)
- Dyspnea, dizziness, lightheadedness, fatigue, or chest pressure: In tachycardic episodes accompanied by palpitations
- Syncope: With rapid rate and severe hypotension
- Heart-failure symptoms and reduced effort tolerance: Early manifestations of tachycardia-induced cardiomyopathy in patients with frequent or incessant tachycardia
The heart’s electrical system
To understand the causes of heart rate or rhythm problems such as tachycardia, it helps to understand how the heart’s internal electrical system works.
Your heart is made up of four chambers — two upper chambers (atria) and two lower chambers (ventricles). The rhythm of your heart is normally controlled by a natural pacemaker called the sinus node, which is located in the right atrium. The sinus node produces electrical impulses that normally start each heartbeat.
From the sinus node, electrical impulses travel across the atria, causing the atrial muscles to contract and pump blood into the ventricles.
The electrical impulses then arrive at a cluster of cells called the atrioventricular (AV) node — usually the only pathway for signals to travel from the atria to the ventricles.
The AV node slows down the electrical signal before sending it to the ventricles. This slight delay allows the ventricles to fill with blood. When electrical impulses reach the muscles of the ventricles, they contract, causing them to pump blood either to the lungs or to the rest of the body.
When anything disrupts this complex system, it can cause the heart to beat too fast (tachycardia), too slow (bradycardia) or with an irregular rhythm.
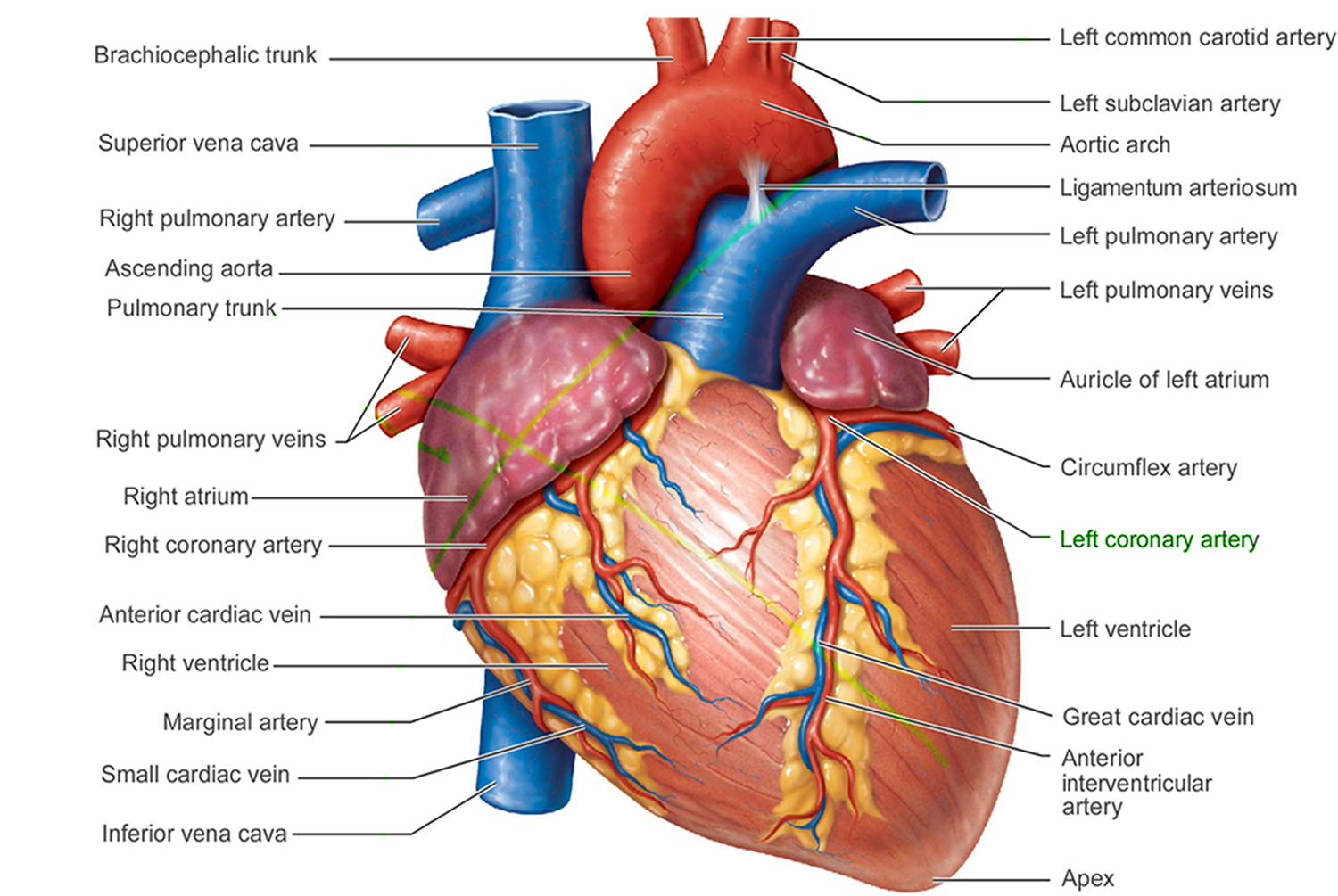
Figure 1. The anatomy of the heart
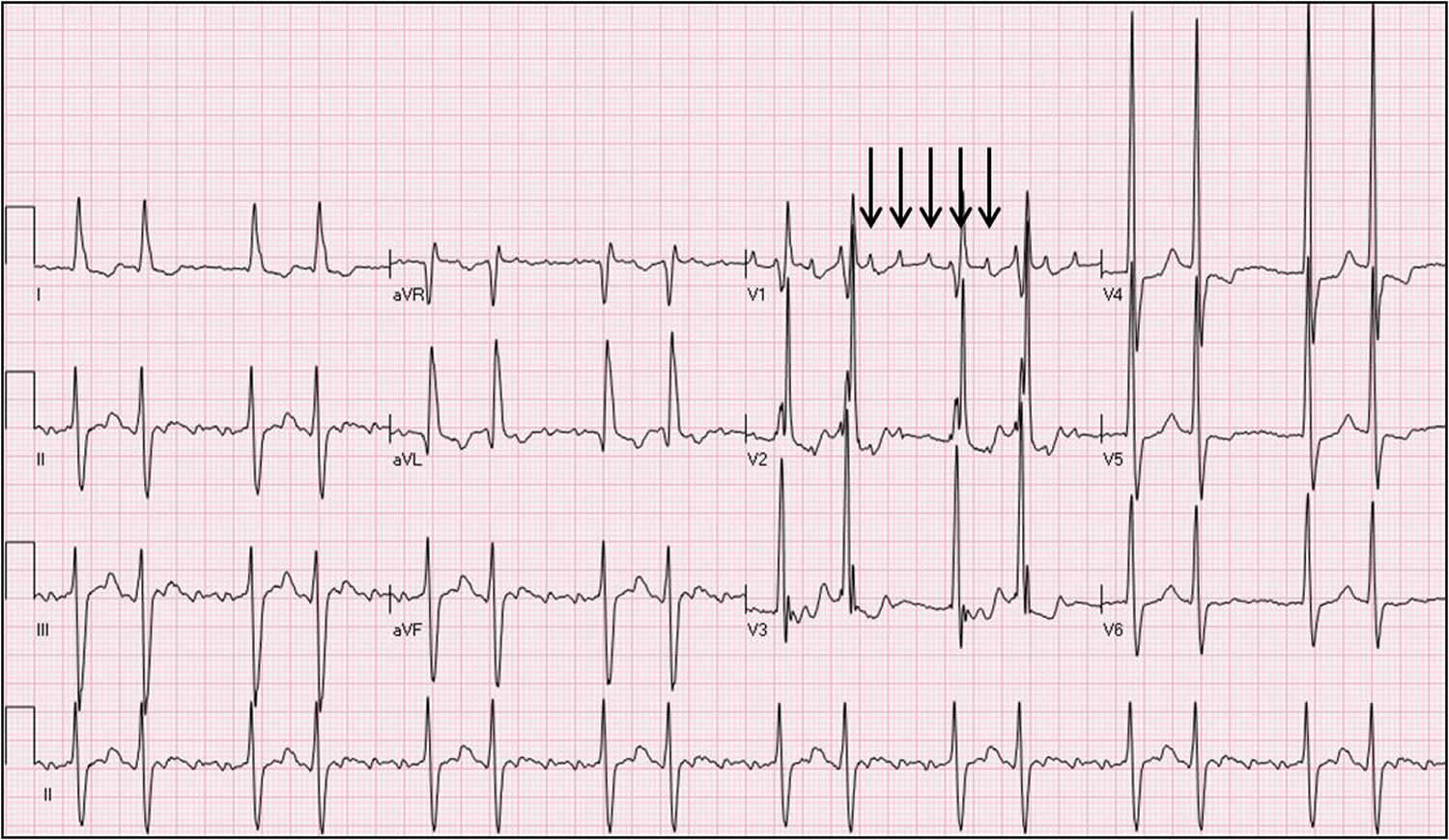
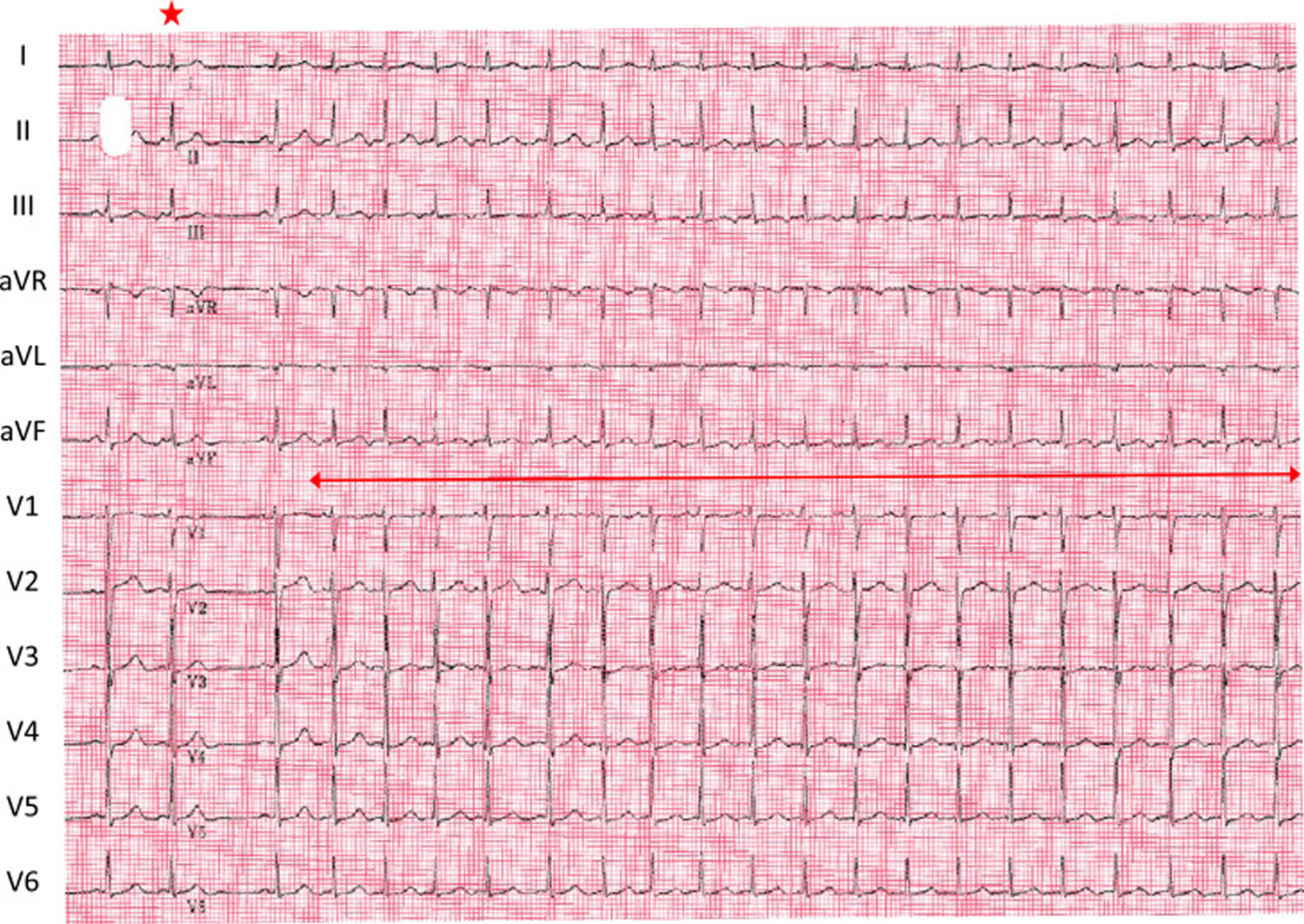
Figure 4. Atrial tachycardia ECG
Atrial tachycardia prognosis
In patients with structurally normal hearts, atrial tachycardia is associated with a low mortality rate. However, tachycardia-induced cardiomyopathies have developed in patients with persistent or frequent atrial tachycardia. Patients with underlying structural heart disease, congenital heart disease, or lung disease are less likely to be able to tolerate atrial tachycardia. Other morbidity is associated with lifestyle changes and associated symptoms.
A study by Chung et al 4 indicated that in patients with acute ischemic stroke and nonsustained atrial tachycardia, an enlarged left atrium is a risk factor for stroke recurrence. The study involved 252 patients, who were followed up for a mean period of 35 months.
Atrial tachycardia causes
Atrial tachycardia can occur in individuals with structurally normal hearts or in patients with organic heart disease. When it arises in patients with congenital heart disease who have undergone corrective or palliative cardiac surgery, such as a Fontan procedure, an atrial tachycardia can have potentially life-threatening consequences 5).
The atrial tachycardia that manifests in association with exercise, acute illness with excessive catecholamine release, alcohol ingestion, altered fluid states, hypoxia, metabolic disturbance, or drug use (e.g., caffeine, albuterol, theophylline, cocaine) is associated with automaticity or triggered activity. Digitalis intoxication is an important cause of atrial tachycardia, with triggered activity being the underlying mechanism.
Reentrant atrial tachycardia tends to occur in patients with structural heart disease, including ischemic, congenital, postoperative, and valvular disorders. Iatrogenic atrial tachycardias have become more common and typically result from ablative procedures in the left atrium. Several typical origination sites for these tachycardias have been identified, including the mitral isthmus (between the left lower pulmonary vein and mitral annulus), the roof of the left atrium, and, for reentry, around the pulmonary veins.
The most common reason for postablation tachycardias is gaps in the ablation lines, allowing for slow conduction and initiation reentry circuits or circuits excluded by the set of ablation lines. Typically, these patients have undergone an atrial fibrillation ablation procedure. This is true for catheter ablation and surgical epicardial ablation. Similarly, patients with prior surgical procedures involving the left atrium may have surgical incision lines and, hence, the potential for macroreentrant circuits.
multifocal atrial tachycardia is often related to underlying illnesses, frequently occurring in patients experiencing an exacerbation of chronic obstructive pulmonary disease (COPD) 6, a pulmonary thromboembolism, an exacerbation of heart failure, or severe illness, especially under critical care with inotropic infusion. multifocal atrial tachycardia is often associated with hypoxia and sympathetic stimulation. Digitalis toxicity also may be present in persons with multifocal atrial tachycardia, with triggered activity as the mechanism.
Other underlying conditions that are commonly associated with multifocal atrial tachycardia are the following:
- Valvular heart disease
- Diabetes mellitus
- Hypokalemia
- Hypomagnesemia
- Azotemia
- Postoperative state
- Sepsis
- Methylxanthine toxicity
- Myocardial infarction
- Pneumonia
Unusual forms of atrial tachycardias can be seen in patients with an infiltrative process involving the pericardium and, by extension, the atrial wall.
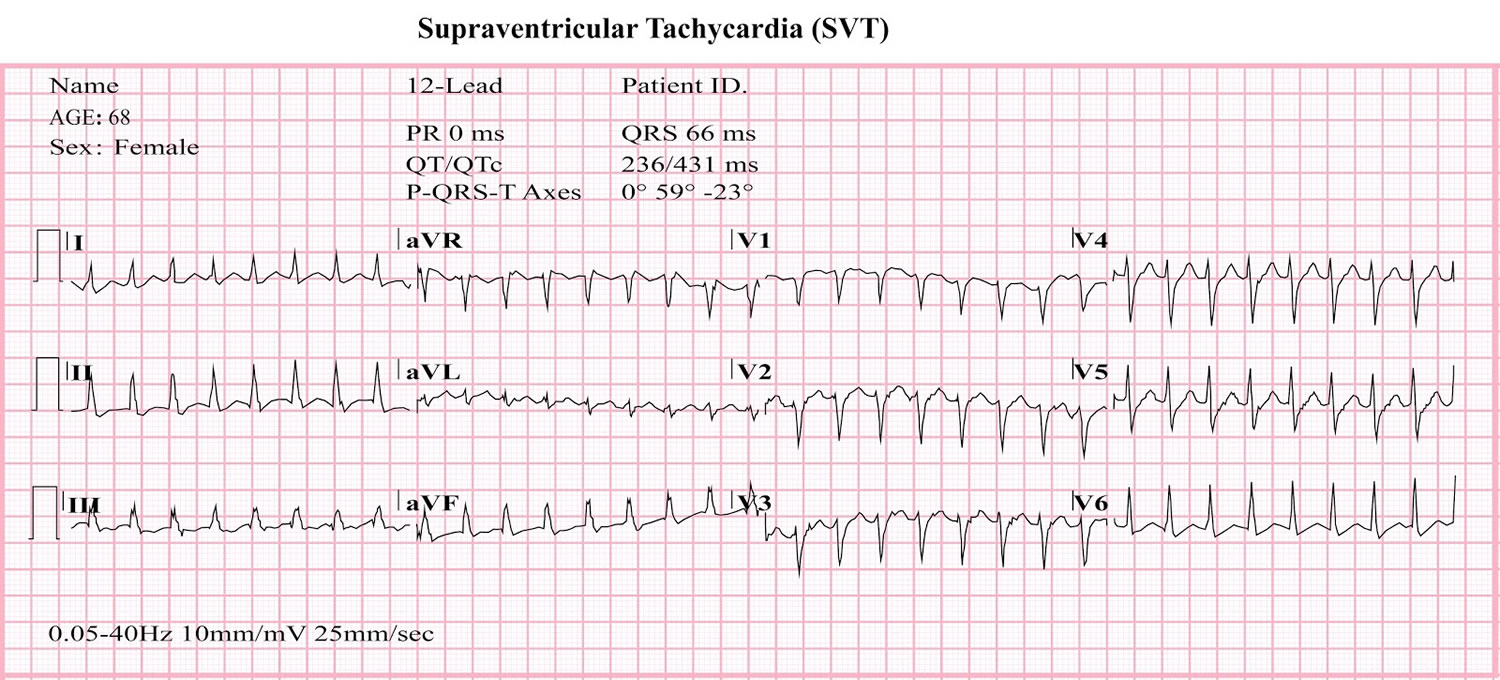
Atrial tachycardia vs SVT
SVT (supraventricular tachycardia) is an abnormally fast heart rate of over 100 heartbeats a minute. Supraventricular tachycardia (SVT) is a rapid heart rate (tachycardia, or a heart rate above 100 beats per minute) that is caused by electrical impulses that originate above the heart’s ventricles. Many doctors and other health care professional include all of the many tachycardias that involve the atrioventricular node (AV node) under this classification, but others do not.
Supraventricular tachycardia does not include those tachycardia rhythms that originate from the ventricles (ventricular tachycardias) such as ventricular tachycardia or ventricular fibrillation.
SVT is also called paroxysmal supraventricular tachycardia (PSVT), is defined as an abnormally fast heartbeat. SVT (supraventricular tachycardia) is a broad term that includes many forms of heart rhythm problems (heart arrhythmias) that originate above the ventricles (supraventricular) in the atria or AV node.
You’ll usually feel your heart suddenly start racing and going very fast, then stop or slow down abruptly. You may also experience:
- chest pain
- dizziness
- light-headedness
- breathlessness
- fatigue (tiredness)
Episodes of SVT can last for seconds, minutes, hours or even days, in rare cases. They may occur several times a day, or only once or twice a year.
SVT occurs when there’s a problem with the heart’s electrical system, which controls your heart rhythm. This causes the heart to beat much faster than normal.
In some people, SVT results from an extra electrical connection in the heart present from birth (Wolff-Parkinson-White syndrome), but it can also occur in hearts that are otherwise normal.
SVT can occur in anyone at any age and often starts for the first time in children or young adults. Generally, the fast heart rate happens more frequently and lasts longer the older you get.
SVT can be triggered by the extra heartbeats (ectopic heartbeats) that most people experience, but some episodes are brought on by things like drinking large amounts of alcohol or caffeine, stress, or smoking lots of cigarettes.
Most people with rare episodes of supraventricular tachycardia live healthy lives without restrictions or interventions. For others, treatment and lifestyle changes can often control or eliminate rapid heartbeats.
In most cases, the problem is temporary and lasts for a few seconds, minutes, or in some cases hours.
Types of SVT
There are several different types of SVT, which are classified by the specific problem in the heart that disrupts the electrical system.
- Atrial tachycardia
- Atrioventricular nodal reentry tachycardia. Atrioventricular nodal reentry tachycardia is the most common type of supraventricular tachycardia (SVT). Episodes often start and end suddenly, and occur because of a reentrant circuit — also called an accessory pathway — located in or near the AV node that causes the heart to beat prematurely. Atrioventricular nodal reentry tachycardia tends to occur more often in young women, but it can affect both males and females of any age.
- Another type of SVT called Wolff-Parkinson-White syndrome occurs as a result of an abnormal electrical connection between the atria and ventricles, which creates a short circuit in the heart’s electrical system. This happens because people with Wolff-Parkinson-White syndrome are born with an extra strand of muscle tissue between these chambers.
- In other cases of SVT, a short circuit occurs, even though the heart is otherwise normal.
- SVT can also be caused by an electrical signal from another part of the heart overriding the signal from the sinoatrial node.
SVT triggers
SVT is usually triggered by extra heartbeats (ectopic beats), which everyone has. It may also be triggered by:
- Some medications, including asthma medications, herbal supplements and cold remedies
- Drinking large amounts of caffeine (or caffeinated substances)
- Tiredness, stress or emotional upset
- Smoking lots of cigarettes
- More common in women, but may occur in either sex
- Anxious young people
- People who are physically fatigued
However, in the majority of cases, there’s no identifiable trigger for SVT.
In many cases, symptoms of supraventricular tachycardia (SVT) stop quickly and no treatment is needed.
However, if necessary, treatment is available to stop an episode of SVT and prevent future episodes.
Stopping an SVT episode
Vagal manoeuvres
Vagal manoeuvres are techniques designed to stimulate the vagus nerve. Stimulating this nerve can reduce the speed of the electrical impulses in your heart and stop episodes of SVT. However, these techniques work in less than one in three cases.
One of the main vagal manoeuvres used is called the Valsalva manoeuvre. There’s no standard way to perform this manoeuvre, but it often involves holding your nose, closing your mouth and trying to exhale hard while straining as if you were on the toilet. If you’re in hospital, you may be asked to blow hard into a tube instead.
You can perform a simple version of the Valsalva manoeuvre at home to try to stop an episode of SVT. You can also try dipping your face into a bowl of cold water, as this can have a similar effect.
An alternative vagal manoeuvre is a carotid sinus massage. This involves massaging an area of your neck called the carotid sinus in an attempt to stimulate the vagus nerve. However, this should only be carried out by a healthcare professional and shouldn’t be attempted at home.
Medication
If vagal manoeuvres are unsuccessful, you may need an injection of a medication called adenosine in hospital. This medication blocks the abnormal electrical impulses in your heart.
Side effects of adenosine are relatively common, but usually short-lived. After an injection, you may experience nausea (feeling sick), dizziness, chest tightness or shortness of breath.
An injection of verapamil may sometimes be used instead of adenosine, but only usually if adenosine is unsuitable (for example, if you have asthma). This is because there’s a risk of more serious side effects, including low blood pressure.
Cardioversion
If a prolonged episode of SVT doesn’t respond to vagal manoeuvres or medication, or if these treatments are unsuitable, a treatment called cardioversion may be used.
Cardioversion is a relatively simple procedure that uses a defibrillator to apply an electrical current to your chest. This shocks the heart back into a normal rhythm.
It’s usually carried out under general anaesthetic and you should be able to go home the same day.
Cardioversion is a very effective procedure and serious complications are uncommon. However, your chest muscles may feel sore afterwards and the areas of skin where the electrical shocks were applied may be red and irritated for a few days.
Preventing future SVT episodes
There are also some treatments that reduce your chances of having further SVT episodes.
Lifestyle changes
Some SVT episodes are triggered by things like tiredness, drinking lots of alcohol or caffeine, or smoking lots of cigarettes.
Cutting down on the amount of caffeine or alcohol you drink, stopping or limiting how many cigarettes you smoke, and making sure you get enough rest can reduce your chances of having further episodes.
Medication
If necessary, medication can be prescribed to prevent further episodes of SVT by slowing down the electrical impulses in your heart. These medications are taken as a daily tablet and include digoxin, verapamil and beta-blockers.
Common side effects of these medications can include dizziness, diarrhoea and blurred vision. Tiredness can occur with beta-blockers and men may experience problems getting erections. Less common side effects include difficulty getting to sleep (insomnia) and depression.
If the medication you’re prescribed doesn’t work or has unpleasant side effects, a more suitable alternative can often be found.
Catheter ablation
If you have repeated episodes of SVT, an operation called catheter ablation is the recommended treatment option. This prevents further episodes of SVT by destroying the tiny parts of the heart causing the problems in the heart’s electrical system.
Catheter ablation is a safe and highly effective treatment, and means you no longer need to take medication. It cures SVT in over 95% of people and is the recommended treatment worldwide.
During catheter ablation, a thin wire called a catheter is inserted into a vein in your upper leg or groin, before being guided to your heart by an electrophysiologist (a heart specialist who specialises in abnormal heartbeats and rhythms). When the wire reaches the heart, it records the electrical activity to pinpoint the precise location of the problem.
When the problem area is found, high-frequency radiowaves are transmitted to the catheter tip to destroy it, producing a small scar.
You’ll remain awake during this procedure, but will be given a sedative to relax you. Local anaesthetic will be used to numb the area where the catheter is inserted.
The procedure lasts about an hour and a half and you can usually go home on the same day you have the procedure. However, there may be instances where you need to stay in hospital overnight – for example, if you’re operated on in the late afternoon.
Catheter ablation is very effective at preventing future episodes of SVT (19 out of every 20 people treated will never have the problem again), but like all operations it carries a risk of complications. These include bruising and bleeding where the catheter was inserted. Any bruising will usually be small, but even if you have a large bruise it won’t require any treatment and will disappear within two weeks.
There’s also a small risk (less than 1 in 100) of the heart’s normal electrical system being damaged. This is known as heart block, and if it happens you may need a permanent pacemaker to control your heart rhythm.
You should discuss potential benefits and risks of catheter ablation with your surgeon (the electrophysiologist) before the procedure.
Multifocal atrial tachycardia
Multifocal atrial tachycardia is a rapid heart rate. It occurs when too many signals (electrical impulses) are sent from the upper heart (atria) to the lower heart (ventricles).
Multifocal atrial tachycardia causes
The human heart gives off electrical impulses, or signals, which tell it to beat. Normally, these signals begin in an area of the upper right chamber called the sinoatrial node (sinus node or SA node). This node is considered the heart’s “natural pacemaker.” It helps control the heartbeat. When the heart detects a signal, it contracts (or beats).
The normal heart rate in adults is about 60 to 100 beats per minute. The normal heart rate is faster in children.
In multifocal atrial tachycardia, many locations in the atria fire signals at the same time. Too many signals lead to a rapid heart rate. It most often ranges between 100 to 130 beats per minute or more in adults. The rapid heart rate causes the heart to work too hard and not move blood efficiently. If the heartbeat is very fast, there is less time for the heart chamber to fill with blood between beats. Therefore, not enough blood is pumped to the brain and the rest of the body with each contraction.
Multifocal atrial tachycardia is most common in people age 50 and over. It is often seen in people with conditions that lower the amount of oxygen in the blood.
These conditions include:
- Bacterial pneumonia
- Chronic obstructive pulmonary disease (COPD)
- Congestive heart failure
- Lung cancer
- Lung failure
- Pulmonary embolism
You may be at higher risk for multifocal atrial tachycardia if you have:
- Coronary heart disease
- Diabetes
- Had surgery within the last 6 weeks
- Overdosed on the drug theophylline
- Sepsis
When the heart rate is less than 100 beats per minute, the arrhythmia is called “wandering atrial pacemaker.”
Multifocal atrial tachycardia outlook (prognosis)
Multifocal atrial tachycardia itself is seldom life threatening. The condition is transient and resolves when the underlying condition improves. The prognosis depends on the prognosis of any comorbid disease.
Many patients with multifocal atrial tachycardia have significant comorbidities, especially COPD and respiratory failure, that often require treatment in an intensive care unit. Consequently, a high mortality rate (up to 45%) is associated with this arrhythmia, although the mortality is not a direct consequence of the rhythm abnormality.
Potential complications of multifocal atrial tachycardia include development of tachycardia-induced cardiomyopathy if the arrhythmia is persistent. Other complications include the following:
- Atrial thrombi with embolization and subsequent stroke
- Myocardial infarction from incongruous myocardial supply and demand
- Pulmonary emboli
Multifocal atrial tachycardia possible complications
Complications may include:
- Cardiomyopathy
- Congestive heart failure
- Reduced pumping action of the heart
Multifocal atrial tachycardia symptoms
Some people may have no symptoms. When symptoms occur, they can include:
- Chest tightness
- Lightheadedness
- Fainting
- Sensation of feeling the heart is beating irregularly or too fast (palpitations)
- Shortness of breath
- Weight loss and failure to thrive in infants
Other symptoms that can occur with this disease:
- Breathing difficulty when lying down
- Dizziness
Multifocal atrial tachycardia diagnosis
A physical exam shows a fast irregular heartbeat of over 100 beats per minute. Blood pressure is normal or low. There may be signs of poor circulation.
Tests to diagnose multifocal atrial tachycardia include:
- ECG
- Electrophysiologic study
Heart monitors are used to record the rapid heartbeat. These include:
- 24-hour Holter monitor
- Portable, long-term loop recorders that allow you to start recording if symptoms occur
If you are in the hospital, your heart rhythm will be monitored 24 hours a day, at least at first.
Multifocal atrial tachycardia treatment
If you have a condition that can lead to multifocal atrial tachycardia, that condition should be treated first.
Treatment for multifocal atrial tachycardia includes:
- Improving blood oxygen levels
- Giving magnesium or potassium through a vein
- Stopping medicines, such as theophylline, which can increase heart rate
- Taking medicines to slow the heart rate (if the heart rate is too fast), such as calcium channel blockers (verapamil, diltiazem) or beta-blockers.
Ectopic atrial tachycardia
Ectopic atrial tachycardia occurs at a rate of 5%–20% among children with supraventricular tachycardia (SVT) 7 that often resists medical therapy. Untreated, it may progress to tachycardia-induced cardiomyopathy 8, and differentiating it from dilated cardiomyopathy is sometimes difficult. Atrial appendages are the most frequent focus in children, differing from the situation in adults 9. However, ectopic atrial tachycardia originating from aneurysms of the right atrial appendage is very rare and in fact has not yet been clearly defined.
Ectopic atrial tachycardia is thought to be caused by rapid discharges from an automatic atrial focus distinct from the sinus node. Histologic studies have shown that spontaneous activity arises from a single focus of abnormal cells. In adults, the foci of ectopic atrial tachycardia most often occur along the crista terminalis 10, the tricuspid annulus 11, the coronary sinus ostium 12, the perinodal region 13, and the pulmonary veins 14.
In contrast, in studies involving children showed that the ectopic focus more often is located in one of the atrial appendages. This difference in location of the ectopic focus suggests a possible difference in underlying substrate for ectopic atrial tachycardia between children and adults. In younger children, the focus often may be a remnant of the original embryonic cells with abnormal automaticity. In this regard, the right atrial appendage originates from the primitive atrium, and the left atrial appendage is the remnant of the original embryonic left atrium that develops during the third week of gestation. Some scientists suggest that in children, persisting autorhythmic tissue may be the source of the arrhythmia. Of 12 patients younger than 3 years in this study 15, 6 (50%) had ectopic atrial tachycardia originating from the right atrial appendage.
As a focus for ectopic atrial tachycardia, the crista terminalis is unlikely in children. The crista terminalis is an area of marked anisotropy due to poor transverse cell-to-cell coupling 16. By creating a region of slow conduction, such anisotropy favors the development of microreentry. In addition, the normal sinus pacemaker complex is distributed along the long axis of the crista terminalis 17. Hence, cells with spontaneous automaticity are to be found in this region. In our study, patients with crista terminalis-related ectopic atrial tachycardia were older than 7 years, suggesting that the substrate of ectopic atrial tachycardia originating in the crista terminalis might be acquired with age 15.
Adenosine-sensitive and microreentrant atrial tachycardias have been reported 18, with origins in the perinodal region and atrioventricular valve annulus in adults. The atrioventricular annulus (tricuspid annulus, mitral annulus) was the usual origin for ectopic atrial tachycardia in our study, the mechanism being automaticity, not reentry. In 9 of 10 patients, ectopic atrial tachycardia originated from a site in the free wall of the tricuspid annulus or mitral annulus. The one exception arose from the tricuspid posterior septal region.
Ectopic atrial tachycardia is characterized by 11:
- (1) atrial activation originating in a small area and spreading centrifugally;
- (2) a range of activation time less than the tachycardia cycle length, with the first few beats showing progressive shortening;
- (3) atrioventricular block possibly occurring in the presence of persisting SVT;
- (4) ventriculoatrial dissociation during ventricular pacing at the cycle length of the SVT without a change in the atrial activation sequence; and
- (5) typical inability to induce or terminate tachycardia with standard pacing protocols.
Tachycardias were considered to arise from the tricuspid or mitral annulus based on the following criteria 11:
- (1) radiofrequency catheter ablation catheter positioned in an annular location when viewed in right and left anterior oblique fluoroscopic views with characteristic annular motion of the catheter tip and
- (2) an atrioventricular ratio less than 1.
Radiofrequency catheter ablation of SVT in children has been successful, with a low risk of significant complications 19.
Atrial tachycardia vs sinus tachycardia
Sinus tachycardia is a normal increase in the heart rate. The heart rate is fast, but the heart beats properly.
Causes of sinus tachycardia
A rapid heartbeat may be your body’s response to common conditions such as:
- Fever
- Anxiety
- Some medicinal and street drugs
- Severe emotional distress
- Fright
- Strenuous exercise
Other causes but less commonly, it may indicate:
- Anemia (low blood count)
- Increased thyroid activity
- Heart muscle damage from heart attack or heart failure
- Hemorrhage (severe bleeding)
Symptoms of sinus tachycardia
Your heart beats faster than usual.
Treatments for sinus tachycardia
Your doctor should consider and treat the cause of sinus tachycardia rather than the condition itself. If your rapid heartbeat is a symptom of a more serious or longer term problem, simply slowing the heart rate could cause more harm and leave the underlying condition untreated.
Atrial tachycardia symptoms
Some people have no symptoms; others may feel:
- Fainting (syncope)
- Lightheadedness or dizziness
- Rapid heartbeat or “palpitations” or fluttering feeling in chest or bounding pulse
- Angina (chest pain), pressure or tightness
- Shortness of breath
- Fatigue/tiredness
In extreme cases, atrial tachycardia or SVT may cause:
- Unconsciousness
- Cardiac arrest
In patients with multifocal atrial tachycardia, the history may disclose an underlying illness that is causing the tachycardia. Such illnesses include pulmonary, cardiac, metabolic, and endocrinopathic disorders. Chronic obstructive pulmonary disease (COPD) is the most common underlying disease process (60%) in multifocal atrial tachycardia.
Reentrant atrial tachycardia is not uncommon in patients with a history of a surgically repaired atrial septal defect. The scar tissue in the atrium may give rise to the formation of a reentrant circuit.
On physical examination, the primary abnormal finding is a rapid pulse rate. The rate is usually regular, but it may be irregular in rapid atrial tachycardias with variable AV conduction and in multifocal atrial tachycardia. Blood pressure may be low in patients presenting with fatigue, lightheadedness, or presyncope.
Atrial tachycardia diagnosis
Workup for atrial tachycardia can employ the following diagnostic tools:
- 12-lead electrocardiography with rhythm strip: To help identify, locate, and differentiate atrial tachycardia
- Holter monitoring: To analyze the onset and termination of atrial tachycardia, identify the AV conduction block during the episode, and correlate the symptoms to atrial tachycardia
The following laboratory studies may be indicated to exclude systemic causes of sinus tachycardia:
- Serum chemistry: To exclude electrolyte disorders
- Blood hemoglobin level and red blood cell (RBC) counts: To seek evidence of anemia
- Blood tests to check thyroid function, heart disease or other conditions that may trigger atrial tachycardia
- Arterial blood gas level: To define pulmonary status
- Serum digoxin assay: When digitalis intoxication is suspected
The following imaging studies can be useful in the evaluation of patients with atrial tachycardia:
- Chest radiography: In patients with tachycardia-induced cardiomyopathy or complex congenital heart disease
- Computed tomography (CT) scanning: To exclude pulmonary embolism, assess the anatomy of pulmonary veins, and provide images prior to ablative procedure
- Echocardiography: To rule out structural heart disease and assess left atrial size, pulmonary arterial pressure, left ventricular function, and pericardial pathology
Your doctor might also try to trigger an episode with other tests, which may include:
- Stress test, which is typically done on a treadmill or stationary bicycle while your heart activity is monitored
- Electrophysiological testing and mapping, which allows your doctor to see the precise location of the arrhythmia
Atrial tachycardia treatment
Treatment of atrial tachycardia depends on the severity of the condition and the factors that trigger it. In addition to managing any underlying conditions that could trigger your atrial tachycardia, your doctor may recommend or try:
- Carotid sinus massage: gentle pressure on the neck, where the carotid artery splits into two branches. Must be performed by a healthcare professional to minimize risk of stroke, heart or lung injury from blood clots.
- Valsalva maneuver: holding your nostrils closed while blowing air through your nose or coughing.
- Dive reflex: the body’s response to sudden immersion in water, especially cold water e.g. dunking your face in ice water.
- Medications. Your doctor may suggest intravenous or oral medication to control your heart rate or restore a normal heart rhythm.
- Cutting down on coffee or other caffeinated substances.
- Cutting down on alcohol.
- Quitting tobacco use.
- Getting more rest.
- Cardioversion. If your arrhythmia (irregular heart beat) does not respond to vagal maneuvers or medication — and if there’s no identifiable, treatable condition triggering it to occur — your doctor may use electrical cardioversion. In the procedure, a shock is delivered to your heart through paddles or patches on your chest. The current affects the electrical impulses in your heart and can restore a normal rhythm.
- Catheter ablation. In some cases, your doctor may recommend catheter ablation. For this procedure, your doctor threads one or more catheters through your blood vessels to your heart. Electrodes at the catheter tips can use heat, extreme cold or radiofrequency energy to damage (ablate) a small spot of heart tissue and create an electrical block along the pathway that’s causing your arrhythmia.
- Pacemaker. If you experience frequent episodes of atrial tachycardia and all other treatment options are unsuccessful, your doctor may suggest implanting a small device called a pacemaker to emit electrical impulses that stimulate your heart to beat at a normal rate. For people with atrial tachycardia, this procedure is typically followed by an ablation of the AV node.
- Song MK, Baek JS, Kwon BS, et al. Clinical spectrum and prognostic factors of pediatric ventricular tachycardia. Circ J. 2010 Sep. 74(9):1951-8.[↩]
- Weber R, Letsas KP, Arentz T, Kalusche D. Adenosine sensitive focal atrial tachycardia originating from the non-coronary aortic cusp. Europace. 2009 Jun. 11(6):823-6.[↩]
- Hirai Y, Nakano Y, Yamamoto H, et al. Pulmonary artery mapping for differential diagnosis of left-sided atrial tachycardia. Circ J. 2013. 77(2):345-51.[↩]
- Chung H, Joung B, Lee KY, et al. Left atrial volume index predicts recurrence of stroke in patients with nonsustained atrial tachycardia. J Stroke Cerebrovasc Dis. 2015 Oct. 24(10):2408-15.[↩]
- Law IH, Alam O, Bove EL, et al. Follow-up of a prospective surgical strategy to prevent intra-atrial reentrant tachycardia after the Fontan operation. Circ Arrhythm Electrophysiol. 2016 Dec. 9(12[↩]
- McCord J, Borzak S. Multifocal atrial tachycardia. Chest. 1998 Jan. 113(1):203-9.[↩]
- Naganuma T., Miura M., Tamame T., Chinen S., Matsuoka M., Yokoyama S., Ooki H., Sibuya K. A study on different clinical manifestation of ectopic atrial tachycardia in infants and children. Nihon Shoni Junkanki Gakkai Zasshi. 2011;27:199–205.[↩]
- Tachycardia-mediated cardiomyopathy secondary to focal atrial tachycardia: long-term outcome after catheter ablation. Medi C, Kalman JM, Haqqani H, Vohra JK, Morton JB, Sparks PB, Kistler PM. J Am Coll Cardiol. 2009 May 12; 53(19):1791-7. https://www.ncbi.nlm.nih.gov/pubmed/19422986/[↩]
- Toyohara K., Fukuhara H., Yoshimoto J., Ozaki N., Nakamura Y. Electrophysiologic studies and radiofrequency catheter ablation of ectopic atrial tachycardia in children. Pediatr Cardiol. 2011;32:40–46. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3018255/[↩]
- Kalman JM, Olgin JE, Karch MR, Hamdan M, Lee RJ, Lesh MD. “Cristal tachycardias”: origin of right atrial tachycardias from the crista terminalis identified by intracardiac echocardiography. J Am Coll Cardioi. 1998;31:451–459. doi: 10.1016/S0735-1097(97)00492-0. https://www.ncbi.nlm.nih.gov/pubmed/9462592[↩]
- Morton J, Sanders P, Das A, Vohra J, Sparks P, Kalman J. Focal atrial tachycardia arising from the tricuspid annulus: electrophysiologic and electrocardiographic characteristics. J Cardiovasc Electrophysiol. 2001;12:653–659. doi: 10.1046/j.1540-8167.2001.00653.x. https://www.ncbi.nlm.nih.gov/pubmed/11405398[↩][↩][↩]
- Kistler PM, Fynn SP, Haqqani H, Stevenson H, Vohra JK, Morton JB, et al. Focal atrial tachycardia from the ostium of the coronary sinus: electrocardiographic and electrophysiological characterization and radiofrequency ablation. J Am Coll Cardiol. 2005;45:1488–1493. doi: 10.1016/j.jacc.2005.01.042. https://www.ncbi.nlm.nih.gov/pubmed/15862424[↩]
- Lai LP, Lin JL, Chen TF, Ko WC, Lien WP. Clinical, electrophysiological characteristics, and radiofrequency catheter ablation of atrial tachycardia near the apex of Koch’s triangle. PACE. 1998;21:367–374. https://www.ncbi.nlm.nih.gov/pubmed/9507537[↩]
- Kistler PM, Prashanthan S, Fynn S, Stevenson I, Hussin A, Vohra J, et al. Electrophysiological and electrocardiographic characteristics of focal atrial tachycardia originating from the pulmonary veins: acute and long-term outcomes of radiofrequency ablation. Circulation. 2003;108:1968–1975. doi: 10.1161/01.CIR.0000095269.36984.75. http://circ.ahajournals.org/content/108/16/1968.long[↩]
- Toyohara K, Fukuhara H, Yoshimoto J, Ozaki N, Nakamura Y. Electrophysiologic Studies and Radiofrequency Catheter Ablation of Ectopic Atrial Tachycardia in Children. Pediatric Cardiology. 2011;32(1):40-46. doi:10.1007/s00246-010-9809-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3018255/[↩][↩]
- Saffitz JE, Kanter HL, Green KG, Tolley TK, Beyer EC. Tissue-specific determinants of anisotropic conduction velocity in canine atrial and ventricular myocardium. Circ Res. 1994;74:1065–1070. http://circres.ahajournals.org/content/74/6/1065.long[↩]
- Boineau JP, Canavan TE, Schuessler RB, Cain ME, Corr PB, Cox JL. Demonstration of a widely distributed atrial pacemaker complex in the human heart. Circulation. 1988;77:1221–1237. https://www.ncbi.nlm.nih.gov/pubmed/3370764[↩]
- Iesaka Y, Takahashi A, Goya M, Soejima Y, Okamoto Y, Fujiwara H, et al. Adenosine-sensitive atrial reentrant tachycardia originating from the atrioventricular nodal transitional area. J Cardiovasc Electrophysiol. 1997;8:854–864. doi: 10.1111/j.1540-8167.1997.tb00846.x. https://www.ncbi.nlm.nih.gov/pubmed/9261711[↩]
- Blaufox AD, Felix GL, Saul JP. Radiofrequency catheter ablation registry. Radiofrequency catheter ablation in infants ≤18 months old: when is it done and how do they fare? Short-term data from the pediatric ablation registry. Circulation. 2001;104:2803–2808. doi: 10.1161/hc4801.100028. http://circ.ahajournals.org/content/104/23/2803.long[↩]