Contents
What are blood thinners
Blood thinners (anticoagulants and antiplatelet agents) are medicines that prevent blood clots from forming. Blood thinners also keep existing blood clots from getting larger. Blood thinners are medicines that reduce blood clotting in an artery, a vein or the heart. Blood clots can block the blood flow to your heart muscle and cause a heart attack. Blood clots can also block blood flow to your brain, causing a stroke.
You may take a blood thinner if you have:
- Certain heart or blood vessel diseases
- An abnormal heart rhythm called atrial fibrillation (afib)
- A heart valve replacement
- A risk of blood clots after surgery
- Congenital heart defects
There are two main types of blood thinners:
- Anticoagulants such as heparin, warfarin (also called Coumadin), dabigitran, apixaban, and rivoraxaban, slow down your body’s process of making clots. Anticoagulants make it harder for clots to form or keep existing clots from growing in your heart, veins or arteries. Treatment should be managed by your healthcare provider.
- Warfarin is used for long-term therapy in patients with atrial fibrillation to prevent a thrombus from forming in the left atrium. Warfarin acts by inhibiting epoxide reductase. Epoxide reductase is a critical component in coagulation factor production because it helps recycle vitamin K. Without vitamin K more coagulation factors cannot be produced by the liver.
- Heparin is an anticoagulant used in hospital settings for deep venous thrombosis prophylaxis. Heparin binds and activates antithrombin. Antithrombin goes on to inactivate thrombin and factor Xa (Stuart-Prower factor).
- Antiplatelet drugs, such as aspirin, clopidogrel, dipyridamole and ticlopidine, prevent blood cells called platelets from clumping together to form a clot.
Anticoagulants are considered more aggressive drugs than antiplatelets. They are recommended primarily for people with a high risk of stroke and people with atrial fibrillation. More than 2.7 million Americans have atrial fibrillation (AF), an-arrhythmia of the heart where the atria (the heart’s pumping chambers) quiver instead of beat. As a result, not all of the blood is pumped out of the heart, allowing pools to collect in the heart chamber, where clots may form.
An embolic stroke is a type of ischemic stroke that occurs when a piece of an atrial blood clot (embolus) is pumped out of the heart, circulates to the brain and becomes lodged in an artery. The American Heart Association recommends that most atrial fibrillation patients over age 65 receive some sort of anticoagulant therapy.
Although anticoagulants tend to be more effective for atrial fibrillation patients, they are generally recommended only for patients with strokes caused by clots originating in the heart. Anticoagulants tend to be more expensive and carry a higher risk of serious side effects, including bruising and skin rash and bleeding in the brain, stomach and intestines.
When used as directed, however, anticoagulants have proven very effective for atrial fibrillation patients. Although the potential risks seem severe, the life-saving effects give these drugs a bright upside.
Other people who may benefit from anticoagulant therapy for stroke prevention are those with blood that clots easily, and in some cases, patients with intracranial artery blockages that surgery can’t remedy.
In comparison to antiplatelets, anticoagulants tend to be affected more by other drugs, vitamins and even certain foods, making anticoagulant therapy somewhat troublesome for stroke survivors. Because warfarin competes with Vitamin K, patients taking it should consult their doctors about possible dietary restrictions, as even some vegetables might cause an imbalance if eaten in excess.
When you take a blood thinner, follow directions carefully. Blood thinners may interact with certain foods, medicines, vitamins, and alcohol. Make sure that your healthcare provider knows all of the medicines and supplements you are using. You will probably need regular blood tests to check how well your blood is clotting. It is important to make sure that you’re taking enough medicine to prevent clots, but not so much that it causes bleeding.
There are several things you need to be aware of when taking anticoagulant medicines. If you’re going to have surgery or a test such as an endoscopy, make sure your doctor or surgeon is aware that you’re taking anticoagulants, as you may have to stop taking them for a short time.
Speak to your doctor, anticoagulant clinic or pharmacist before taking any other medications, including prescription and over-the-counter medicines, as some medications can affect how your anticoagulant works.
If you’re taking warfarin, you’ll also need to avoid making significant changes to what you normally eat and drink, as this can affect your medication.
- Most anticoagulant medicines aren’t suitable for pregnant women. Speak to your doctor or anticoagulant clinic if you become pregnant or are planning to try for a baby while taking anticoagulants.
Anticoagulant therapy with warfarin also requires regular blood tests to ensure the correct drug dose. A weak dosage increases the risk of stroke and heart attack, but too much puts someone at risk for bleeding. Generic brands may not be the same strength as the one prescribed by your doctor.
Side effects of anticoagulants
Like all medicines, there’s a risk of experiencing side effects while taking anticoagulants.
The main side effect is that you can bleed too easily, which can cause problems such as:
- passing blood in your urine
- passing blood when you poo or having black poo
- severe bruising
- prolonged nosebleeds
- bleeding gums
- vomiting blood or coughing up blood
- heavy periods in women
For most people, the benefits of taking anticoagulants will outweigh the risk of excessive bleeding.
What are new blood thinners
The U.S. Food and Drug Administration (FDA) has approved four blood thinners in recent years — dabigatran (Pradaxa), rivaroxaban (Xarelto), apixiban (Eliquis), and edoxaban (Savaysa). Along with warfarin, a drug approved 60 years ago, these drugs are used to prevent stroke in patients with atrial fibrillation.
There are some important differences among these drugs. Warfarin interacts with certain drugs and foods that make it less effective or more likely to cause bleeding, and so its effects must be monitored with periodic blood tests. The new drugs have fewer interactions and don’t require blood monitoring.
Although all anticoagulants reduce the risk of a stroke caused by clots from the heart, they increase the risk of a stroke caused by bleeding into the brain (a hemorrhagic stroke). The newer drugs cause fewer bleeding strokes than warfarin, and the overall rates of strokes (caused by blood clots or bleeding) are lower with some of the newer drugs.
Another difference is how fast the drugs start and stop working. When starting warfarin, it takes a few days before the drug takes effect. And when stopping warfarin, it takes a few days for its effects to wear off.
The new drugs start working rapidly, and their effects wear off fairly rapidly. For most patients, this is an advantage.
Rarely, however, when patients have life-threatening bleeding or need urgent surgery, it can be important to stop the effects of these drugs immediately.
For the rare patient with life-threatening bleeding, reversal agents can be used to counter the effects of anticoagulants. For example, Vitamin K is the reversal agent for warfarin. FDA recently approved the first reversal agent — Praxbind (idrucizumab) — for Pradaxa. Praxbind can be used in emergency situations when bleeding caused by Pradaxa’s anticoagulant effects can’t be controlled.
Who should take anticoagulants?
Your doctor may recommend anticoagulants to help prevent the above conditions if they feel you’re at risk.
This may be because you have:
- developed blood clots in the past
- recently had surgery that means you’re unable to move around much while you recover, such as a hip replacement or knee replacement
- had an aortic valve replacement – as blood clots can form on the surface of the new heart valve
- atrial fibrillation – a type of irregular heartbeat (arrhythmia) that can cause blood clots to form in the heart
- a condition where the blood has an increased tendency to form clots (thrombophilia), such as Factor V Leiden
- antiphospholipid syndrome – where the immune system attack fats and proteins in the blood vessels, causing the blood to clot
Anticoagulants are also sometimes used to treat blood clots, such as deep vein thrombosis (DVT) or a pulmonary embolism, by stopping the clot getting bigger while your body slowly reabsorbs it.
How long you’ll need to take anticoagulants for will depend on why they’re needed. You might only need to take them for a short time after a hip or knee replacement, but treatment may be lifelong if you have a long-term condition that increases your risk of blood clots.
Can you get a blood clot while on blood thinners?
Yes. Medications that are commonly called blood thinners — such as aspirin, warfarin (Coumadin, Jantoven), dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis) and heparin — significantly decrease your risk of blood clotting, but will not decrease the risk to zero.
These medications must be taken exactly as directed to work safely and effectively. Taking too little of these medications may not be effective, and taking too much can lead to serious bleeding.
Also, blood thinners may not be able to lessen the strong blood-clotting tendency of an underlying disease, such as cancer.
Interactions with other medications, food and alcohol are common with warfarin. These interactions are less so with other blood-thinning medications.
However, any interactions may decrease the effectiveness of your blood thinner, making you more likely to develop blood clots. If you take a blood thinner, be sure to follow your doctor’s advice on dosing and ask about foods and other medications — including over-the-counter drugs and herbal supplements — that may interfere with safety and efficacy of the blood thinner.
What happens when you stop taking blood thinners?
The most important and most effective thing any person can do is take their health into their own hands. This means eating a healthy diet, exercising daily, abstaining from smoking, taking prescribed medicines according to doctor’s orders and, of course, staying educated.
Blood thinners (antiplatelet and anticoagulant therapies) are at the heart of preventing blood clots from forming and therefore reduce your risk of recurrent strokes.
Depending on where the blood clot forms, this can lead to serious problems such as:
- strokes or transient ischemic attacks (“mini-strokes”)
- heart attacks
- deep vein thrombosis (DVT)
- pulmonary embolism
Your doctor has prescribed a blood thinner to prevent blood clots. Blood clots can put you at risk for heart attack, stroke, and other serious medical problems. Never stop taking your blood thinner unless your doctor has told you so, for example you may be advised to stop taking your blood thinner medication before surgery.
Bruising from blood thinners
Taking anticoagulant medicines can make you more prone to bleeding if you’re injured.
Try to avoid minor injuries and cuts and grazes by:
- taking care when brushing your teeth and shaving (consider using a soft toothbrush and an electric razor)
- using insect repellent to avoid insect bites or stings
- using protection when gardening, sewing or playing sports
Your doctor or anticoagulant clinic may advise you to avoid contact sports because of the risk of excessive bleeding.
Blood thinners and alcohol
Alcohol can affect your warfarin (Coumadin) dose and should be avoided. Check with your doctor or pharmacist about this issue and any questions you may have. If you’re taking warfarin, do not drink more than 1 or 2 alcoholic drinks a day and never binge drink.
Aspirin and alcohol — there is a risk of stomach problems, including stomach bleeding, for people who take aspirin regularly. Alcohol use can increase these stomach risks, so ask your doctor if it is safe for you to drink alcohol in moderation.
Types of blood thinners
There are two main types of blood thinners.
- Anticoagulants such as heparin or warfarin (also called Coumadin) slow down your body’s process of making clots.
- Antiplatelet drugs, such as aspirin and clopidogrel, prevent blood cells called platelets from clumping together to form a clot.
Anticoagulants
Anticoagulants are medicines that help prevent blood clots. Anticoagulants are given to people at a high risk of getting clots, to reduce their chances of developing serious conditions such as strokes and heart attacks.
A blood clot is a seal created by the blood to stop bleeding from wounds. While blood clots are useful in stopping bleeding, they can block blood vessels and stop blood flowing to organs such as the brain, heart or lungs if they form in the wrong place.
Anticoagulants work by interrupting the process involved in the formation of blood clots. They’re sometimes called “blood-thinning” medicines, although they don’t actually make the blood thinner.
Although they’re used for similar purposes, anticoagulants are different to antiplatelet medicines, such as low-dose aspirin and clopidogrel.
Types of anticoagulants
The most commonly prescribed anticoagulant is warfarin.
Newer types of anticoagulants are also available and are becoming increasingly common. These include:
- rivaroxaban (Xarelto)
- dabigatran (Pradaxa)
- apixaban (Eliquis)
- edoxaban (Lixiana)
Warfarin and the newer alternatives are taken as tablets or capsules. There’s also an anticoagulant called heparin that can be given by injection.
When anticoagulants are used?
If a blood clot blocks the flow of blood through a blood vessel, the affected part of the body will become starved of oxygen and will stop working properly.
Depending on where the blood clot forms, this can lead to serious problems such as:
- strokes or transient ischemic attacks (“mini-strokes”)
- heart attacks
- deep vein thrombosis (DVT)
- pulmonary embolism
Treatment with anticoagulants may be recommended if your doctor feels you’re at an increased risk of developing one of these problems. This may be because you’ve had blood clots in the past or you’ve been diagnosed with a condition such as atrial fibrillation that can cause blood clots to form.
You may also be prescribed an anticoagulant if you’ve recently had surgery, as the period of rest and inactivity you need during your recovery can increase your risk of developing a blood clot.
Anticoagulants precaution
If you’re prescribed anticoagulants, always follow the instructions of your doctor or another healthcare professional. Some of the main issues you’ll need to consider while taking your medication are outlined below.
Having surgery
If you’re taking anticoagulants and you need to have surgery or any kind of invasive procedure, make sure that the healthcare professionals treating you are aware of your medication. This includes procedures used to diagnose other conditions, such as an endoscopy or cystoscopy.
As anticoagulants reduce the ability of your blood to clot, there’s a risk you could experience heavy bleeding if any kind of cut (incision) is made during a procedure.
You may therefore be advised to stop taking your medication before surgery.
If you’re having a dental procedure, such as having a tooth removed, tell your dentist that you take anticoagulants. You may not need to stop taking your medication, but you might need to have a blood test before the procedure to make sure your blood clots at the right speed.
Only stop taking your medication on the advice of your doctor or another healthcare professional.
Pregnancy
Warfarin isn’t normally given to pregnant women because it can affect the unborn baby. Warfarin can cause birth defects or excessive bleeding from the placenta or fetus.
Warfarin may sometimes be used in the second trimester, but should never be taken during the first trimester and should ideally be avoided in the third trimester as well.
The newer anticoagulant medications apixaban (Eliquis), dabigatran (Pradaxa) and rivaroxaban (Xarelto) also are not recommended in pregnancy.
If you’re taking any of these medications, you should make sure you use contraception when having sex to avoid becoming pregnant.
If you’re on anticoagulants and find out you’re pregnant or plan to start trying for a baby, speak to your doctor or anticoagulant clinic about stopping or changing your prescription.
Injections of an anticoagulant called heparin can be given while you’re pregnant if necessary.
Breastfeeding
You can usually take warfarin while you’re breastfeeding, but you should discuss this with your doctor or midwife first.
Heparin is also safe to take while you’re breastfeeding.
Apixaban, dabigatran and rivaroxaban aren’t recommended if you’re breastfeeding because it’s not clear if they’re safe for the baby.
If you’re on anticoagulants and are breastfeeding or planning to breastfeed, speak to your doctor, anticoagulant clinic or midwife to find out if you need to change your prescription.
Other medications and remedies
If you’re taking anticoagulants, you should speak to your doctor, anticoagulant clinic or pharmacist before taking any other medication, remedy or supplement.
This includes prescription medicines, medicines bought over the counter without a prescription (such as aspirin), and any herbal remedies (such as St John’s Wort).
Some treatments can stop anticoagulants working or can increase the effect they have, which can be dangerous.
Some of the medicines that can affect anticoagulants include certain:
- antibiotics
- antidepressants
- corticosteroids (medications used to reduce inflammation)
- anticonvulsants (medications used to treat epilepsy)
- non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (take paracetamol instead if you need pain relief)
For a full list of medicines that you should avoid, check the patient information leaflet that comes with your medicine.
Food and drink
It’s important to have a healthy, balanced diet that includes lots of fruit and vegetables if you’re taking anticoagulants. But you should avoid making frequent changes to the amount of green vegetables you eat and cranberry juice you drink if you’re taking warfarin.
Foods with a lot of vitamin K, such as leafy green vegetables, chickpeas and liver, can interfere with how warfarin works. You can still include these in your diet while taking warfarin, as the clinic will adjust your dose accordingly, but it’s important to be consistent in the amount you eat.
Do not drink cranberry juice while you’re taking warfarin. It can increase the blood-thinning effect of warfarin.
You should also seek advice before taking supplements containing vitamin K.
The effect of warfarin is also affected by alcohol. If you’re taking warfarin, do not drink more than 1 or 2 alcoholic drinks a day and never binge drink.
These food and drink restrictions don’t usually apply if you’re taking apixaban, dabigatran and rivaroxaban, but you should check with your doctor, anticoagulant clinic or pharmacist if you’re not sure.
Dietary supplements and herbal medications
Many dietary supplements can alter the International Normalized Ratio (INR) such as: arnica, bilberry, butchers broom, cat’s claw, dong quai, feverfew, forskolin, garlic, ginger, ginkgo, horse chestnut, insositol hexaphosphate, licorice, melilot (sweet clover), pau d’arco, red clover, St. John’s wort, sweet woodruff, turmeric, willow bark, and wheat grass. Much is unknown about dietary supplements. The safest policy is for individuals on warfarin (Coumadin) to avoid all dietary supplements unless your physician approves. This includes any vitamin/mineral supplements that list vitamin K on the label. If they are taken regularly on a daily basis, they pose less of a problem than if taken off and on.
Vitamin E supplements
Evidence suggests that vitamin E has blood-thinning effects. Vitamin E intakes above 1,000 International Units (IU) per day may increase the risk of excess bleeding. Research suggests that doses up to 800 IU may be safe for individuals on warfarin (Coumadin), but the evidence is not conclusive. It is best to ask your physician about taking Vitamin E supplements while taking warfarin (Coumadin). Antibiotics Some antibiotics can either lower vitamin K levels in the body or interfere with the activity of warfarin (Coumadin). Check with your physician or pharmacist about whether you will need to adjust your vitamin K intake or warfarin (Coumadin) dose when you take antibiotics.
Antibiotics
Some antibiotics can either lower vitamin K levels in the body or interfere with the activity of warfarin (Coumadin). Check with your physician or pharmacist about whether you will need to adjust your vitamin K intake or warfarin (Coumadin) dose when you take antibiotics.
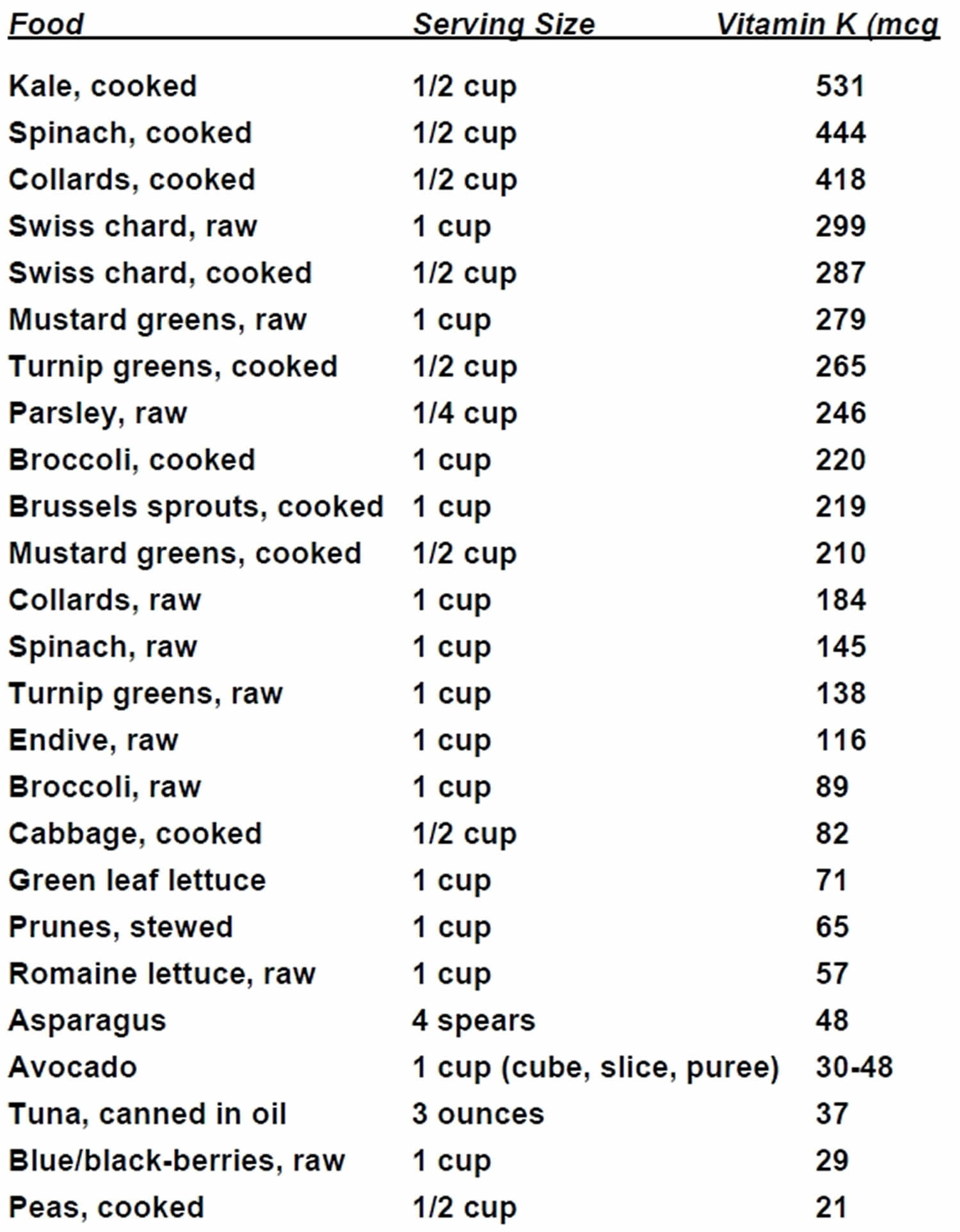
How do I keep my vitamin K intake consistent?
Keep your intake of foods rich in vitamin K about the same each day. For example, you may plan to eat only ½ cup of these foods per day. If you like these foods and eat them often, you can eat more, but be consistent.
Do not a make any major changes in your intake of foods rich in vitamin K. For example, if you typically have a spinach salad daily, do not stop eating it entirely.
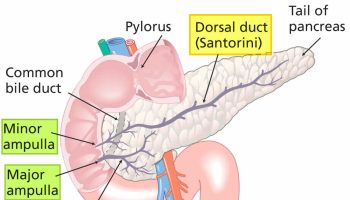
Figure 1. Foods rich in vitamin K
How to take anticoagulants
Your doctor or nurse should tell you how much of your anticoagulant medicine to take and when to take it.
Most people need to take their tablets or capsules once or twice a day with water or food.
The length of time you need to keep taking your medicine for depends on why it’s been prescribed. In many cases, treatment will be lifelong.
If you’re unsure how to take your medicine, or are worried that you missed a dose or have taken too much, check the patient information leaflet that comes with it or ask your doctor, anticoagulant clinic or pharmacist what to do.
Anticoagulant dosage
For most people, anticoagulant tablets or capsules should be taken at the same time once or twice a day. It’s important to take your medicine as scheduled because the effect of some anticoagulants can start to wear off within a day.
Warfarin, apixaban (Eliquis) and dabigatran (Pradaxa) should be taken with water. Rivaroxaban (Xarelto) is normally taken with food.
Depending on your dose, you may need to take more than one tablet or capsule at a time.
Warfarin tablets come in different colors (white, brown, blue and pink) to indicate their strength. You may need to take a combination of different coloured tablets to reach your total dose. Other anticoagulants come in different strengths and colors.
Your doctor or nurse will explain how many tablets you need to take, when to take them, and what the different colors mean.
Missed or extra doses
Warfarin
If you’re taking warfarin and you miss one of your doses, you should skip the dose you missed and wait to take your next scheduled dose as normal. Don’t take a double dose to make up for the one you missed.
If you accidentally take a dose that was much higher than recommended, contact your anticoagulant clinic or doctor for advice.
Newer anticoagulants
If you’re taking apixaban or dabigatran twice a day and you miss one of your doses, you should take it as soon as you remember if it’s still more than 6 hours until your next scheduled dose. If it’s less than 6 hours until your next dose, skip the dose you missed and take the next scheduled dose as normal.
If you accidentally take a double dose, skip your next scheduled dose and take the following dose the next day as scheduled.
If you’re taking rivaroxaban once a day and you miss one of your doses, you should take it as soon as you remember if it’s still more than 12 hours until your next scheduled dose. If it’s less than 12 hours until your next dose, skip the dose you missed and take the next scheduled dose as normal.
If you accidentally take a double dose, take your next dose the next day as scheduled.
Monitoring your dose
Warfarin
If you’re taking warfarin, you will need regular blood tests to check how quickly your blood clots. This is measured using the International Normalized Ratio (INR).
Your International Normalized Ratio (INR) will be regularly tested at your doctor or anticoagulant clinic to make sure your blood doesn’t clot too slowly or too quickly. Your warfarin dose will be adjusted until your INR is in the correct range.
Your INR may need to be tested every other day at first until you’re on the right dose. Once your INR stabilizes in the correct range, these tests will be needed less frequently.
There are now home testing kits to monitor your INR. These mean you don’t need to go to your doctor or anticoagulant clinic for the INR test. This kit may be useful for some people, but you’ll need training to use it and you’ll usually need to pay for one yourself. Speak to your doctor or nurse if you’re considering using a home testing kit.
Newer anticoagulants
If you’re taking apixaban, dabigatran or rivaroxaban, you won’t need to have regular blood tests to monitor your INR.
However, you should still have appointments every few months to check you’re taking your medication correctly and to discuss whether you’ve experienced any side effects.
Antiplatelets
Blood platelets are actually fragments of cells – meaning they don’t contain all the necessary cellular equipment. When a person gets a cut or scratch, platelets release thromboxane, a chemical that signals other platelets to “help out”. Without the release of thromboxane, the platelets won’t come (stick) together, no clot will form, and the cut will continue to bleed. If you have a wound, thromboxane is an indispensable self-sealing material; but if you’re a stroke survivor, thromboxane’s ability to round up “help” to form a blood clot becomes potentially life-threatening.
Antiplatelet agents, including aspirin, clopidogrel, dipyridamole and ticlopidine, work by inhibiting the production of thromboxane. Aspirin is highly recommended for preventing a first stroke, but it and other antiplatelets also have an important role in preventing recurrent strokes. Because of aspirin low cost, availability and effectiveness, aspirin is the most prescribed and used drug in antiplatelet therapy. Currently, aspirin plus extended-release dipyridamole (an antiplatelet) is the only FDA-approved combination therapy for preventing recurrent stroke.
According to a statement by the American Heart Association, taking aspirin within two days of an ischemic stroke reduces the severity of the stroke. In some cases, it prevents death. For long-term (meaning for the rest of your life unless otherwise specified by your doctor) prevention, antiplatelet therapy is recommended primarily for people who have had a transient ischemic attack (TIA or “mini” stroke) or acute ischemic stroke.
The American Heart Association also recommends that people at high risk of heart attack should take a daily low-dose of aspirin [usually 75mg] (if told to by your healthcare provider) and that heart attack survivors regularly take low-dose aspirin. However, you should not start aspirin therapy without first consulting your healthcare provider. The risks and benefits of aspirin therapy vary for each person. Aspirin shouldn’t be given to anyone under 16 years old without medical supervision because aspirin may cause Reye’s syndrome (a serious condition in which fat builds up on the brain, liver, and other body organs) in children and teenagers, especially if they have a virus such as chicken pox or the flu.
Long-term treatment with low doses of aspirin – usually 75mg – has an antiplatelet effect, which means it makes the blood less sticky and can stop blood clots developing.
A doctor may recommend this if you have or have had:
- a heart attack or angina
- a stroke or transient ischemic attack (TIA)
- peripheral arterial disease
- coronary artery bypass surgery or another operation on your heart or blood vessels
Aspirin may also be prescribed for children after heart surgery or to treat Kawasaki disease.
Despite the potential benefits, antiplatelet therapy is not for everyone. People with a history of liver or kidney disease, gastrointestinal disease or peptic ulcers, high blood pressure, bleeding disorders or asthma may not be able to take aspirin or may require special dosage adjustments.
Types of antiplatelet medicines
There are many different types of antiplatelet medicines. Even though each type works in a different way, all antiplatelet medicines help to keep platelets from sticking together and forming blood clots.
- Aspirin is the most common type of antiplatelet medicine. Some patients who are recovering from a heart attack are given aspirin to prevent further blood clots from forming in the coronary arteries. Low-dose aspirin (sometimes called “baby aspirin”) may prevent heart attacks and strokes in people who take it every day.
- Adenosine diphosphate receptor inhibitors are usually given to patients who have had a recent heart attack or stroke, because these patients have a greater risk of having another heart attack or stroke. Doctors may also give this medicine to patients with mitral valve disease or those who have had heart valve replacement. Some patients with peripheral vascular disease may also be good candidates for adenosine diphosphate receptor inhibitors, because poor blood circulation in the legs can lead to blood clots.
- Adenosine reuptake inhibitors are usually given to patients in combination with an anticoagulant. Patients may also take this type of antiplatelet therapy in combination with aspirin if they have a heart condition that increases their risk of blood clots.
- Glycoprotein IIB/IIIA inhibitors are given by an intravenous (IV) needle directly into the bloodstream, so patients must be in the hospital to receive them. Patients usually receive this type of antiplatelet medicine to prevent blood clots that sometimes form during angioplasty and stent procedures. They are also used in patients with angina who are going to have an angioplasty or stent procedure.
- Phosphodiesterase inhibitors is most often used in patients with peripheral vascular disease to reduce leg pain that comes with walking (called intermittent claudication). Patients with peripheral vascular disease have a greater risk of developing blood clots in their legs, so some peripheral vascular disease patients need to take antiplatelet medicines. Patients with heart failure should not take this type of antiplatelet medicine, because studies have shown it can lead to death.
Who can and can’t take aspirin?
Most people can take aspirin safely. But you should get advice from a pharmacist or doctor before taking it if you:
- have had an allergic reaction to aspirin or non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, in the past
- have asthma
- have had stomach ulcers in the past
- have severe liver or kidney problems
- have hemophilia or another bleeding disorder
- have uncontrolled high blood pressure
- are looking for medication for a child under 16 – medication containing aspirin shouldn’t be given to children under 16
- are over 65 years of age
- are pregnant, breastfeeding or trying to get pregnant
- are taking other medications – see Interactions with other medicines, below
You may still be able to take aspirin in these cases, but you should only do so if advised that it’s safe by a healthcare professional.
If you can’t take aspirin, a different medicine, such as paracetamol (for pain) or clopidogrel (to prevent blood clots), may be recommended instead.
How to take aspirin
Your pharmacist or doctor can tell you how often to take your aspirin and how much you should take. You can also check the recommendations in the leaflet that comes with your medicine.
Generally speaking, low-dose aspirin [usually 75mg] (to prevent blood clots) is taken once a day, usually for the rest of your life.
Some medicine leaflets advise taking aspirin with water, while others may recommend taking it before or after food. Follow the instructions in the leaflet or label that comes with your medicine. Ask your pharmacist if you’re not sure.
Missed or extra doses
If you’re taking aspirin to reduce your risk of blood clots and you forget to take a dose, take that dose as soon as you remember and then continue to take your course of aspirin as normal.
If it’s almost time for the next dose, skip the missed dose and continue your regular schedule. Don’t take a double dose to make up for a missed one.
If you think you’ve taken too much aspirin (overdose) and have any concerns, speak to your doctor or pharmacist
Aspirin interactions with other medicines, food and alcohol
Aspirin can potentially interact with other medications, including some complementary and herbal medicines, which could alter their effects or increase your risk of side effects. The risk of bleeding in the stomach may be higher if you drink alcohol while taking aspirin, so you may want to consider reducing how much you drink or avoiding alcohol completely.
Medicines that can interact with aspirin include:
- NSAIDs – such as ibuprofen or naproxen
- steroid medication – such as prednisolone
- anticoagulant medicines – such as warfarin or heparin
- SSRI antidepressants – such as citalopram, fluoxetine or paroxetine
- some medications used to treat high blood pressure – such as ACE inhibitors or diuretics
- some medicines used to treat epilepsy – such as phenytoin
- other medicines containing aspirin – including cold and flu remedies where aspirin is one of the ingredients
This is not a complete list. If you want to check whether a medicine is safe to take with aspirin, ask your doctor or pharmacist, or read the leaflet that comes with the medicine.
There are no known interactions between aspirin and food.
What do blood thinners do
Anticoagulants (warfarin, apixaban, dabigatran and rivaroxaban ) target clotting factors, which are blood proteins that are crucial to the blood-clotting process. Clotting factors are proteins made in the liver. These proteins can’t be created in the liver without Vitamin K – a common vitamin found in cabbage, cauliflower, spinach and other leafy green vegetables. Anticoagulants, such as warfarin (Coumadin) and heparin, slow clot formation by competing with Vitamin K. This inhibits the circulation of certain clotting factors with the exotic names of factors 2, 7, 9 and 10. Within the past 3 years, new anticoagulants have been approved by the U.S. Food and Drug Administration (FDA): dabigitran, apixaban, and rivaroxaban. All of these are simpler to use and less risky than warfarin (bleeding risk is lower).
Antiplatelet agents, including aspirin, clopidogrel, dipyridamole and ticlopidine, work by inhibiting the production of thromboxane. Aspirin is highly recommended for preventing a first stroke, but it and other antiplatelets also have an important role in preventing recurrent strokes.
What are blood thinners used for
Anticoagulants are used if you’re at risk of developing blood clots that could potentially block a blood vessel and disrupt the flow of blood around your body.
This can lead to several serious conditions, including:
- strokes – where a blood clot restricts the flow of blood to your brain, causing brain cells to die and possibly resulting in permanent brain damage or death
- transient ischaemic attacks (TIAs) – also called “mini-strokes”, these have similar symptoms to a stroke, but the effects usually last less than 24 hours
- heart attacks – where a blood clot blocks a blood vessel supplying your heart, starving it of oxygen and causing chest pain and sometimes death
- deep vein thrombosis (DVT) – where a blood clot forms in one of the deep veins in your body, usually your legs, causing pain and swelling
- pulmonary embolism – where a blood clot blocks one of the blood vessels around the lungs, stopping the supply of blood to your lungs
Anticoagulants are used for:
- Anticoagulants reduce your risk for heart attack, stroke, and blockages in your arteries and veins by preventing clumps of blood (blood clots) from forming or growing. However, anticoagulants cannot break up blood clots that have already formed.
- Your doctor may prescribe an anticoagulant if you have had a heart valve replaced or if you have atrial fibrillation, phlebitis, congestive heart failure, or, in some cases, if you are obese.
Antiplatelets are a group of medicines that stop blood cells (called platelets) from sticking together and forming a blood clot. Antiplatelet medicines can stop blood clots from forming.
Patients are usually given antiplatelets if they have a history of:
- Coronary artery disease (CAD)
- Heart attack
- Angina
- Stroke or transient ischemic attacks (TIAs)
- Peripheral vascular disease
Antiplatelets may also be given to patients during and after angioplasty and stent procedures and after coronary artery bypass surgery. Some patients with atrial fibrillation or valve disease also take antiplatelets.
Side effects of blood thinners
Anticoagulants side effects
A possible side effect of anticoagulants is excessive bleeding (hemorrhage), because these medicines increase the time it takes for blood clots to form. Some people also experience other side effects.
Excessive bleeding
Signs of excessive bleeding can include:
- passing blood in your pee
- passing blood when you poo or having black poo
- severe bruising
- prolonged nosebleeds (lasting longer than 10 minutes)
- bleeding gums
- vomiting blood or coughing up blood
- sudden severe back pain
- difficulty breathing or chest pain
- in women, heavy or increased bleeding during your periods, or any other bleeding from your vagina
If you notice any severe or recurrent bleeding, seek medical attention immediately. Contact your doctor or go to your nearest emergency department.
You should also seek immediate medical attention if you:
- are involved in a major accident
- experience a significant blow to the head
- are unable to stop any bleeding
If you’re taking warfarin, you’ll have regular blood tests to check if you’re at a high risk of excessive bleeding by measuring how quickly your blood clots. If your blood clots too slowly, your dose may be increased.
Other side effects
Other side effects of anticoagulants vary depending on which medication you’re taking.
For a full list of potential side effects for your medicine, check the leaflet that comes with it.
Possible other side effects include:
- diarrhea or constipation
- feeling and being sick
- indigestion
- dizziness
- headaches
- rashes
- itchy skin
- hair loss
- jaundice (yellowing of the skin and whites of the eyes)
Speak to your doctor or anticoagulant clinic if you have any persistent troublesome side effects. Contact them immediately if you develop jaundice.
Aspirin side effects
Like all medications, there’s a risk of side effects from aspirin.
The most common side effects of aspirin are:
- indigestion and stomach aches – taking your medicine with food may help reduce this risk
- bleeding or bruising more easily than normal
Tell your doctor if any of these symptoms are severe or do not go away.
Uncommon and rare side effects include:
- hives – a raised, itchy rash
- tinnitus (ringing in the ears) – hearing sounds that come from inside your body
- breathing difficulties, wheezing or an asthma attack
- an allergic reaction – this can cause breathing problems, swelling of the mouth, eyes, face, lips, tongue, or throat, and a sudden rash
- bleeding in the stomach – this can cause dark, tar-like stools or vomiting blood or vomit that looks like coffee grounds
- bleeding in the brain – this can cause a sudden, severe headache, vision problems and stroke symptoms, such as slurred speech and weakness on one side of the body
- hoarseness
- fast heartbeat
- fast breathing
- cold, clammy skin
- loss of hearing
Speak to your doctor if you experience any concerning or troublesome side effects while taking aspirin.
Call your local emergency services number for an ambulance or go to your nearest emergency room if you think you’re having a severe allergic reaction, or you have symptoms of bleeding in your stomach or brain.
Antiplatelets side effects
Sometimes a medicine causes unwanted effects. These are called side effects. Not all of the side effects for antiplatelet therapy are listed here. If you feel these or any other effects, you should check with your doctor.
Common side effects:
- Extreme tiredness (fatigue)
- Heartburn
- Headache
- Upset stomach and nausea
- Stomach pain
- Diarrhea
- Nosebleed
Rare side effects:
- Allergic reaction, with swelling of the face, throat, tongue, lips, hands, feet, or ankles
- Skin rash, itching, or hives
- Throwing up, especially if the vomit has blood in it or looks like coffee grounds
- Dark or bloody stools or blood in the urine
- Trouble breathing or swallowing
- Trouble speaking or slowed speech
- Unusual bleeding or bruising
- Fever, chills, or sore throat
- Fast heartbeat (arrhythmia)
- Yellowing of your skin or eyes (jaundice)
- Joint pain
- Weakness or numbness of your arm or leg
- Confusion or hallucinations
Again, tell your doctor right away if you have any of these side effects. Do not stop taking your medicine unless your doctor tells you to. If you stop taking your medicine without checking with your doctor, it can make your condition worse.
You may need to take antiplatelet medicines for the rest of your life, depending on your condition. You will need to have your blood tested regularly to see how your blood is clotting. Keep all your appointments with your doctor and the lab, so that your body’s response to antiplatelet therapy can be closely monitored.
You should wear a medical alert bracelet or carry a card in your wallet or purse, so that in the event of an accident, emergency responders will know that you are taking antiplatelet medicines.