Contents
What is Chiari malformation
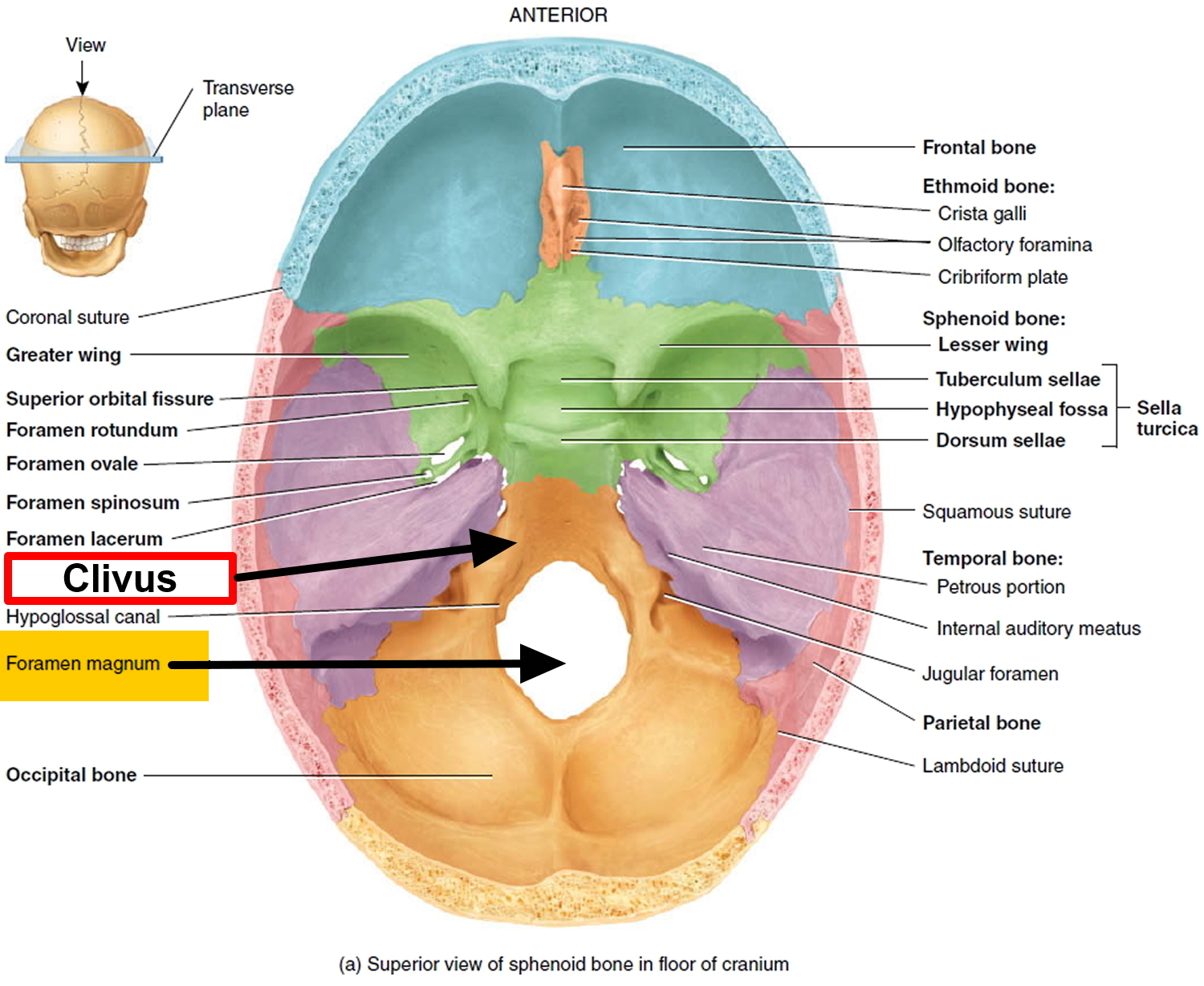
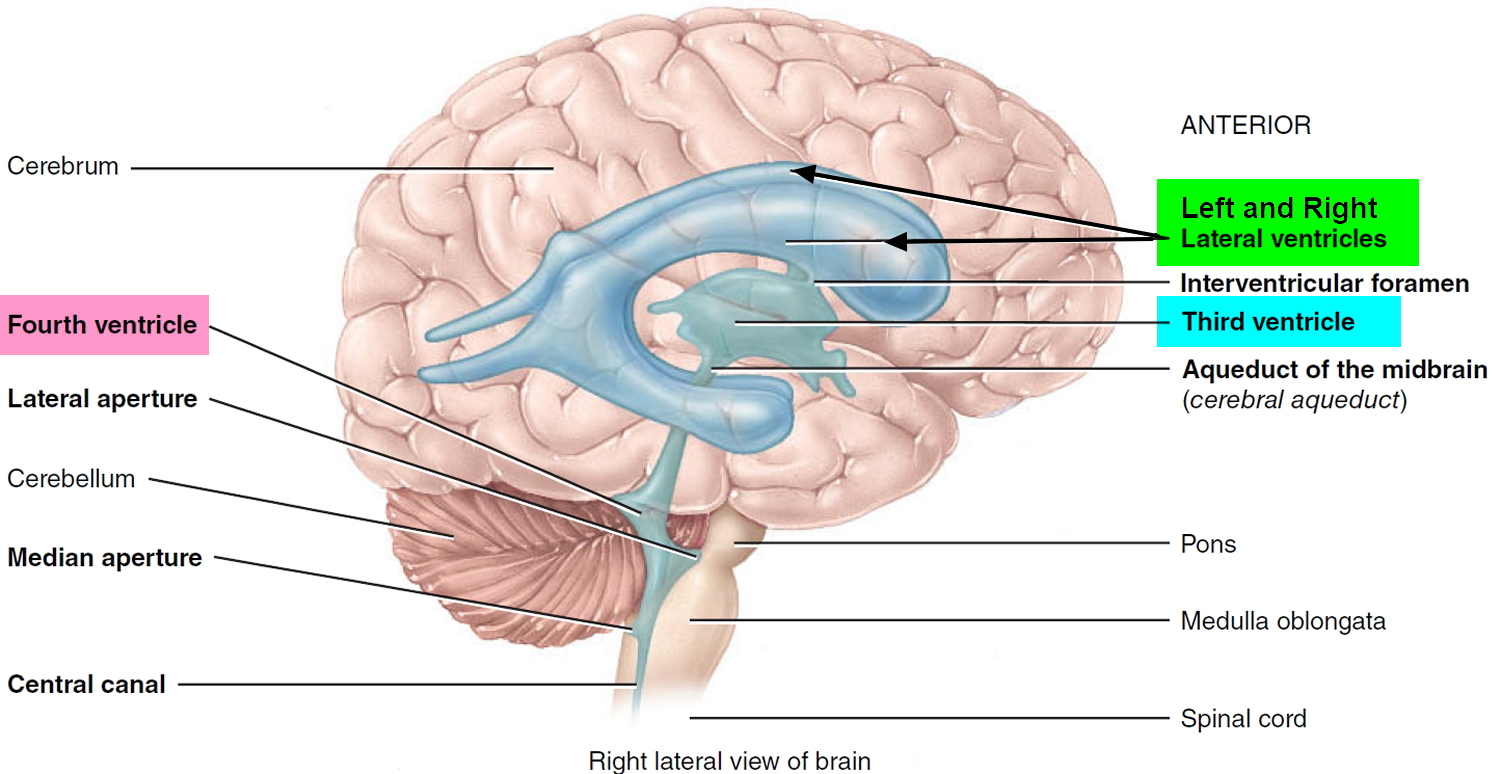
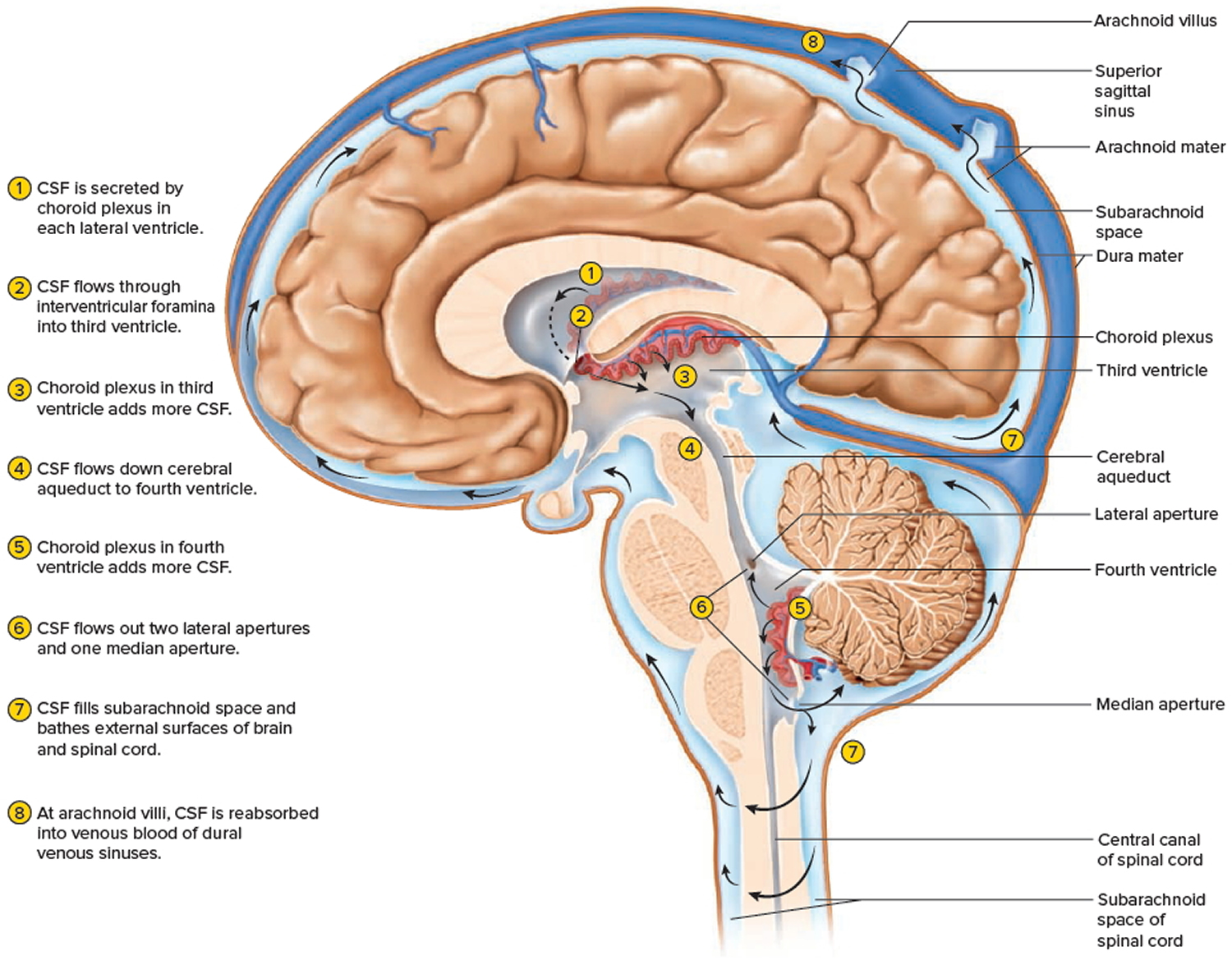
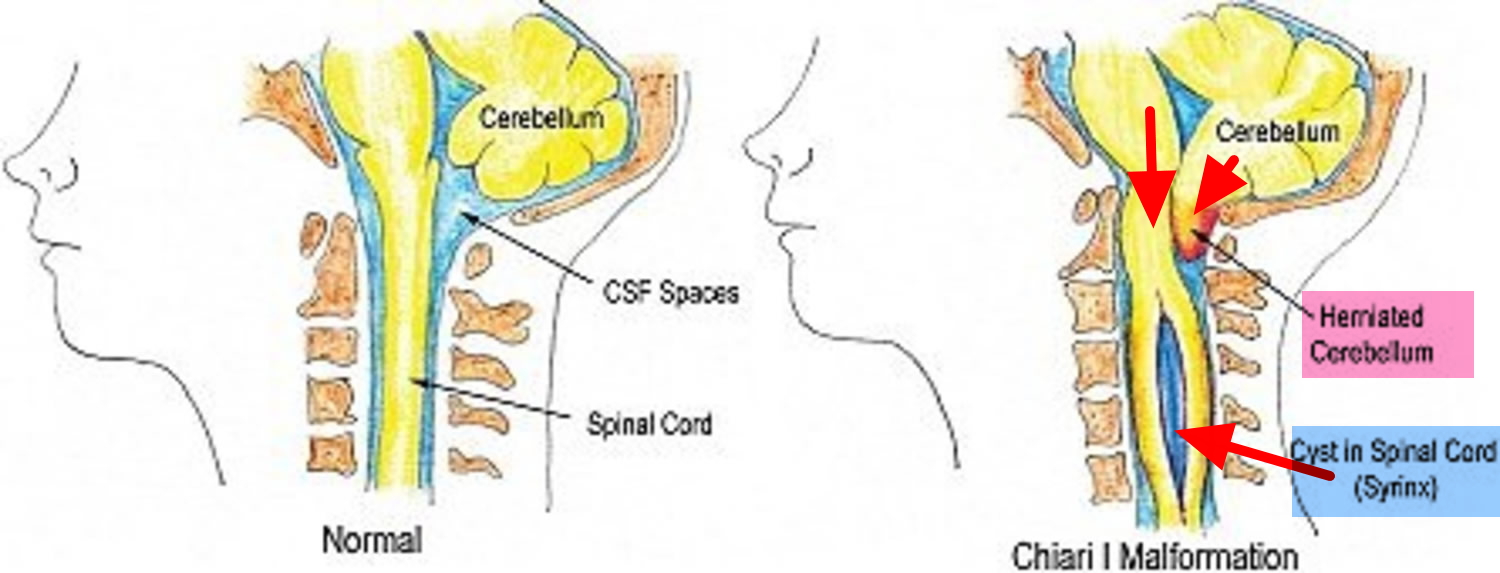
Chiari malformation is a group of congenital (present at birth) defects in which brain tissue (the cerebellum and brainstem) extend into the spinal canal. Chiari malformation occurs when part of your skull is abnormally small or misshapen, pressing on your brain and forcing it downward into the foramen magnum and the spinal canal. This causes pressure on the cerebellum and brain stem that may affect functions controlled by these areas and block the flow of cerebrospinal fluid (CSF)—the clear liquid that surrounds and cushions the brain and spinal cord. The cerebrospinal fluid (CSF) also circulates nutrients and chemicals filtered from the blood and removes waste products from the brain. Normally the cerebellum and parts of the brain stem sit above an opening in the skull that allows the spinal cord to pass through it (called the foramen magnum). When part of the cerebellum extends below the foramen magnum and into the upper spinal canal, it is called a Chiari malformation.
In the past, it was estimated that Chiari malformation occurs in about one in every 1,000 births. However, the increased use of diagnostic imaging has shown that Chiari malformation may be much more common. Complicating this estimation is the fact that some children who are born with this condition may never develop symptoms or show symptoms only in adolescence or adulthood. Chiari malformations occur more often in women than in men and Chiari type 2 malformations are more prevalent in certain groups, including people of Celtic descent.
Chiari malformation is usually present at birth, but can develop later in association with some tumors and spinal abnormalities. Abnormalities at the base of the brain may include the displacement of the lower portion of the brain (cerebellum) and/or brainstem through the opening in the back of the skull (foramen magnum) typically into the spinal canal. Some infants may also have abnormal accumulations of cerebrospinal fluid (CSF) in the skull (hydrocephalus). Other malformations of the brain and spinal cord (i.e., spina bifida) may also occur.
Symptoms often begin during infancy, although they are usually delayed until adolescence or adulthood. The resulting pressure on the cerebellum can block the flow of cerebrospinal fluid (CSF, the liquid that surrounds and protects the brain and spinal cord) and can cause a range of symptoms including dizziness, muscle weakness, numbness, headache, and problems with hearing, balance, and coordination. Symptoms may change for some individuals depending on buildup of cerebrospinal fluid (CSF) and any resulting pressure on tissue and nerves. These usually include headache in the occipital region, vomiting, muscle weakness in the head and face, difficulty swallowing, and varying degrees of mental impairment. Paralysis of the arms and legs may also occur. As they grow older, adults and adolescents with Chiari malformation who previously showed no symptoms may show signs of progressive brain impairment, such as involuntary, rapid, downward eye movements.
Many patients with Chiari malformation will also develop a cyst within the spinal cord (syringomyelia). These cysts are usually in the upper part of the cord near the Chiari malformation but may occur in any part of the spinal cord. These patients present with pain and numbness in the arms, legs, or trunk. In severe cases weakness and spasticity of the legs or arms also occurs. Patients may present with symptoms from syringomyelia and have no symptoms from the underlying Chiari malformation.
Chiari malformation was first described in 1891 by Hans Chiari, Austrian pathologist (1851-1916), based on the autopsies of children.
Figure 1. Human brain
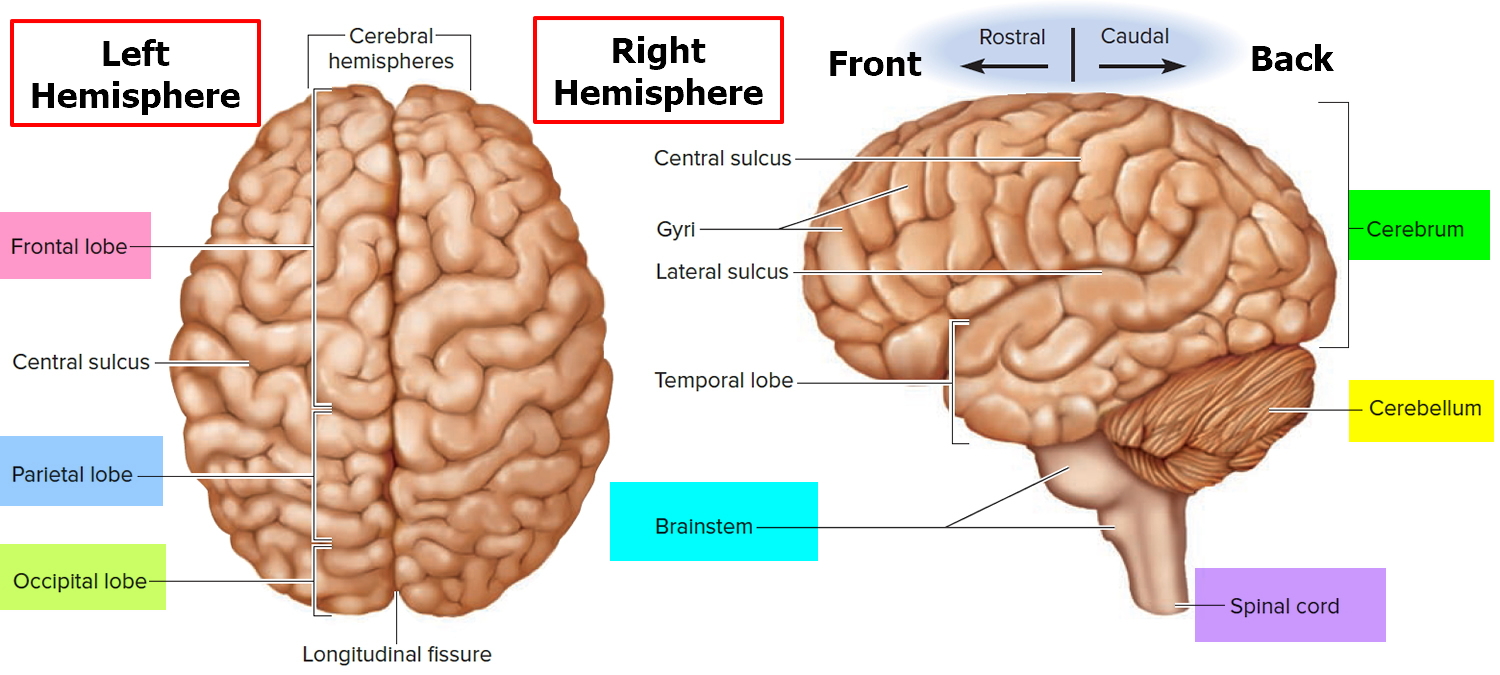
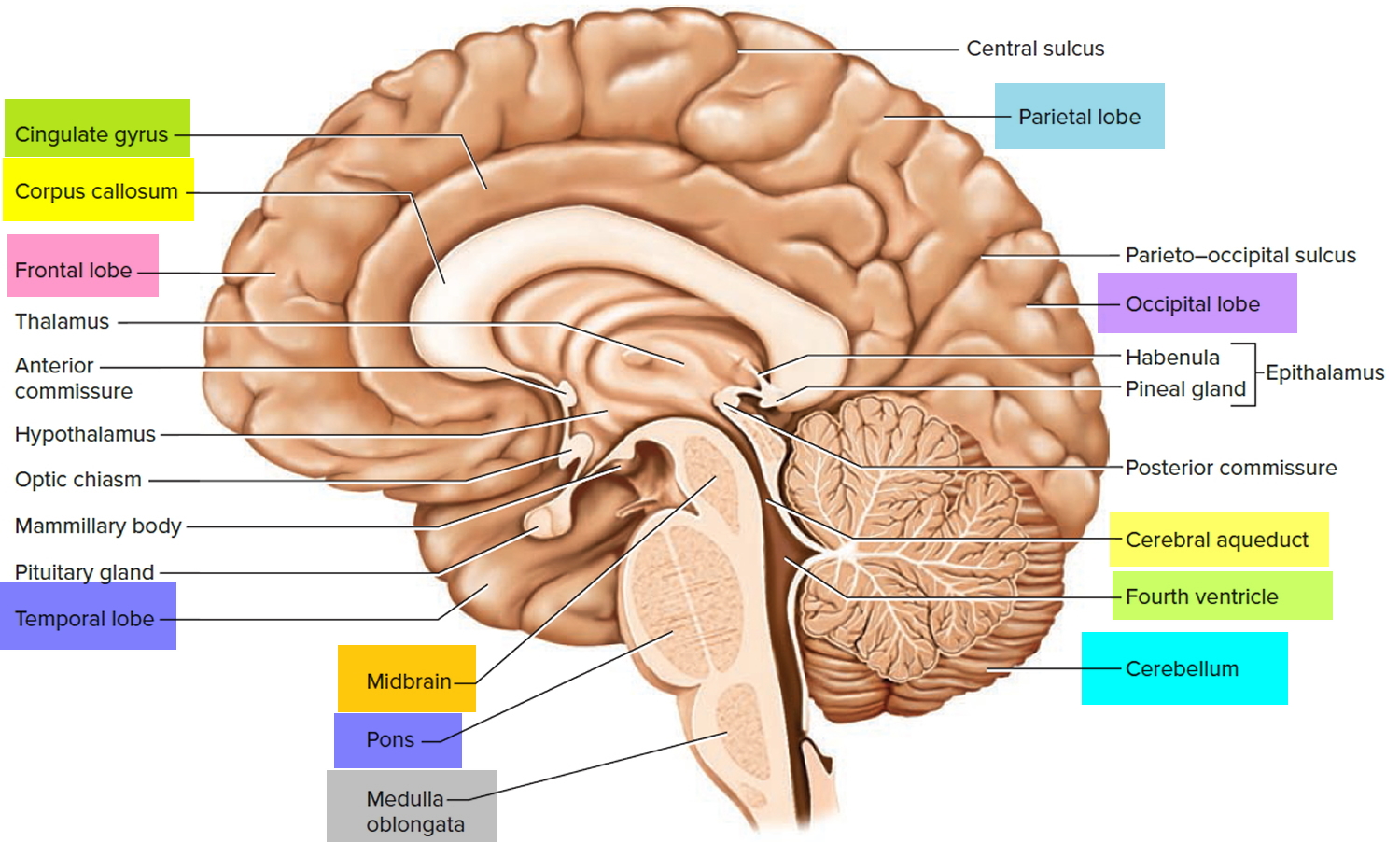
Figure 2. Medial aspect of the human brain
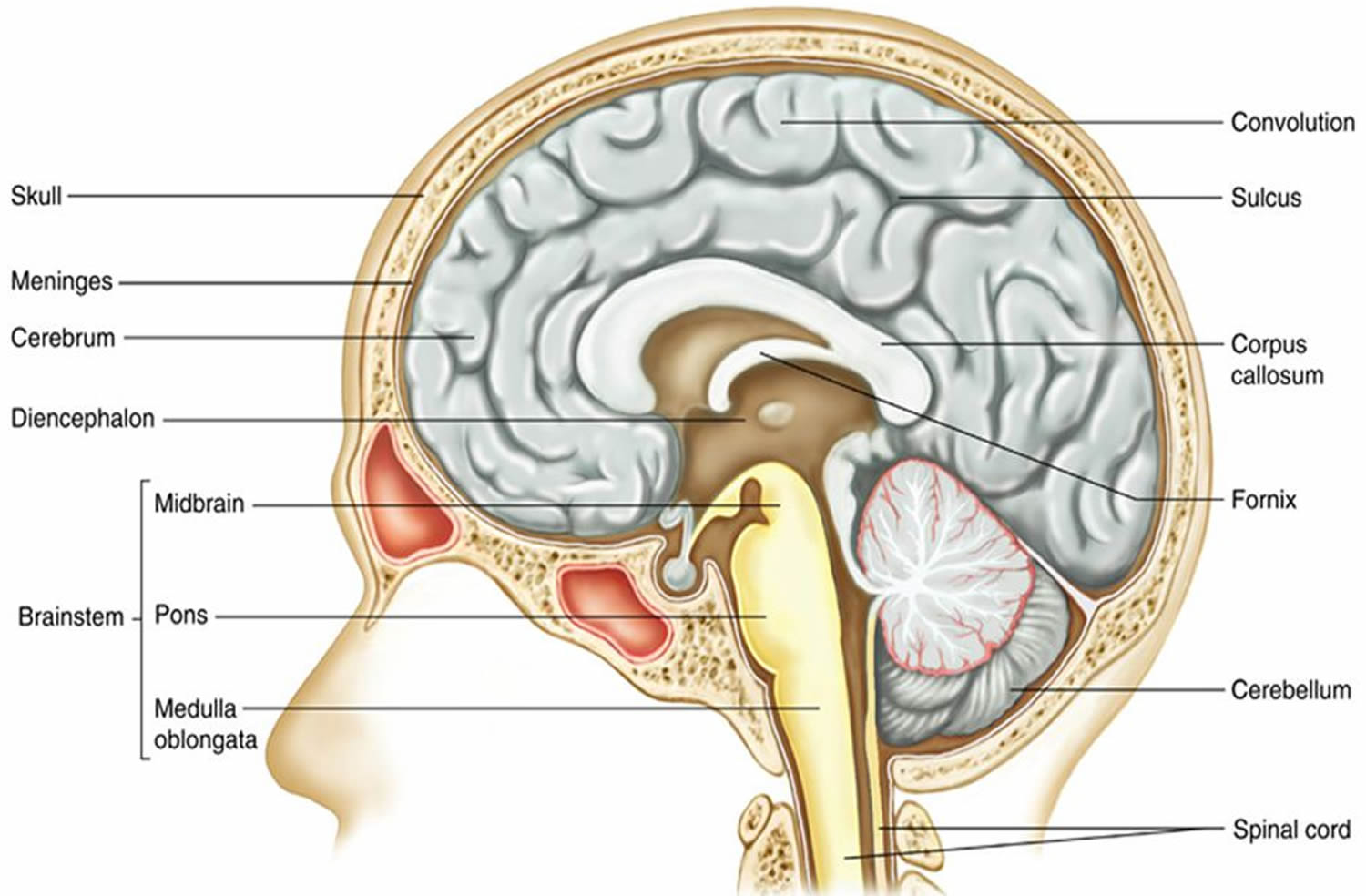
Figure 3. Normal brain and skull
Figure 4. Base of skull
Figure 5. Ventricles of the brain
Figure 6. Cerebrospinal fluid formation, absorption and circulation around and within the brain
Figure 7. Chiari malformation
Chiari malformation types
Chiari malformations are a group of defects associated with congenital caudal (inferior) ‘displacement’ of the cerebellum and brainstem extend into the spinal canal.
Chiari malformations are classified by the severity of the disorder and the parts of the brain that protrude into the spinal canal.
Chiari malformation type 1
Chiari I malformation happens when the lower part of the cerebellum (called the cerebellar tonsils) extends into the foramen magnum. This is believed to be due to a mismatch between size and content of the posterior fossa. Normally, only the spinal cord passes through this opening. Chiari malformation type 1—which may not cause symptoms—is the most common form of Chiari malformation. It is usually first noticed in adolescence or adulthood, often by accident during an examination for another condition. Adolescents and adults who have Chiari malformation but no symptoms initially may develop signs of the disorder later in life.
Chiari I malformations needs to be distinguished from low-lying cerebellar tonsils (benign tonsillar ectopia) which is an asymptomatic and incidental finding in normal individuals, whereby the cerebellar tonsils protrude through the foramen magnum by no more than 3-5 mm 1.
Chiari I malformation is the most common variant of the Chiari malformations, and it is characterized by a caudal descent of the cerebellar tonsil (and brainstem in its subtype, Chiari 1.5) through the foramen magnum. Chiari I malformations are more frequently encountered in females 1.
Unlike Chiari II, III and IV malformations, Chiari I malformations often remain asymptomatic until adulthood. Symptoms are proportional to the degree of descent. Brainstem (medulla) compression and syringomyelia with associated symptoms and signs account for clinical presentation.
Symptoms may include a headache and those associated with syrinx or scoliosis.
The likelihood of Chiari I malformation becoming symptomatic is proportional to the degree of descent of the cerebellar tonsils. All patients who have greater than 12 mm of descent were symptomatic, whereas approximately 30% of those whose descent measured between 5 and 10 mm were asymptomatic 2.
MRI is the imaging modality of choice. Treatment with posterior decompression is usually reserved for symptomatic patients or those with a syrinx.
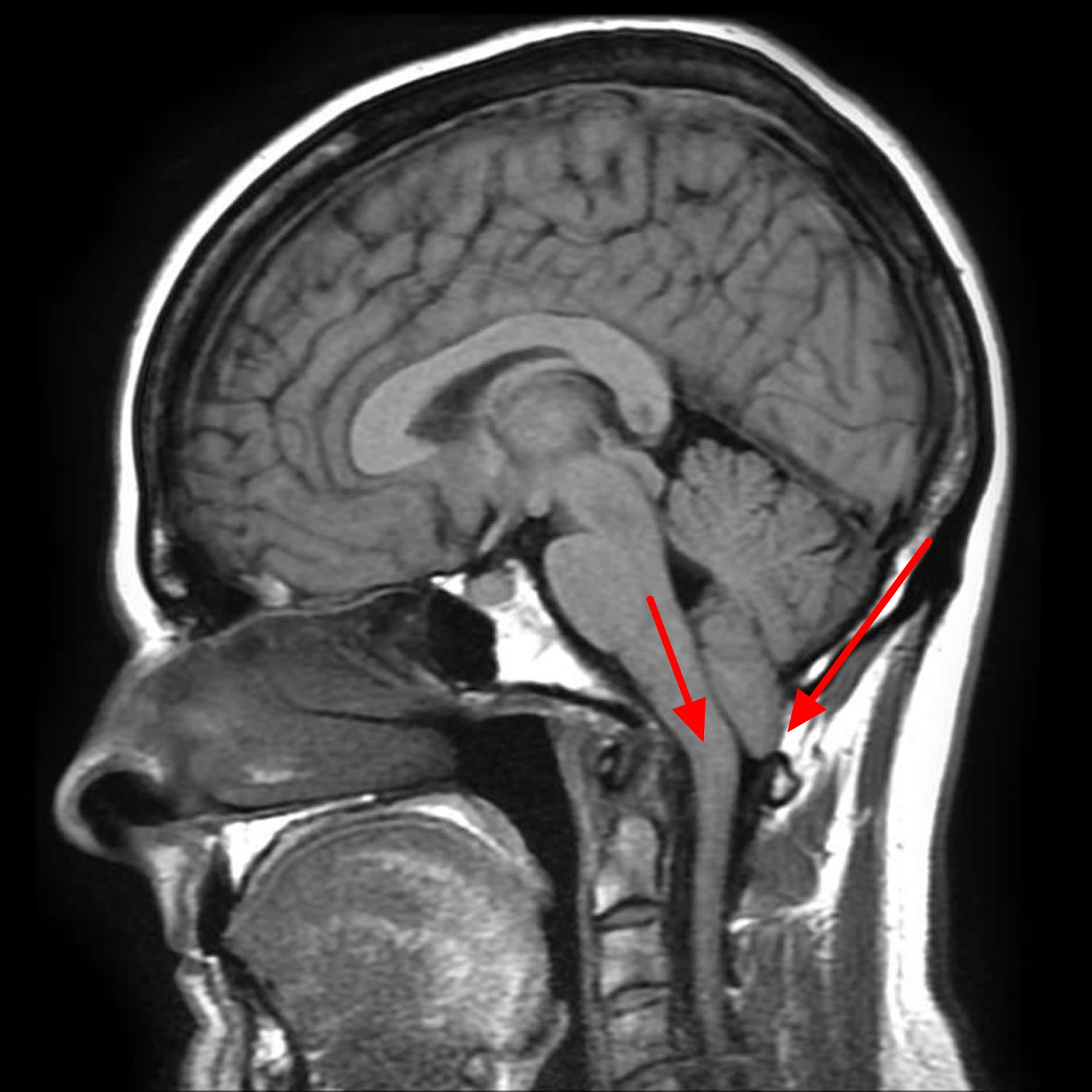
Figure 8. Chiari malformation MRI scan (Chiari malformation type 1 with cerebellar tonsil and/or brainstem herniation through the foramen magnum)
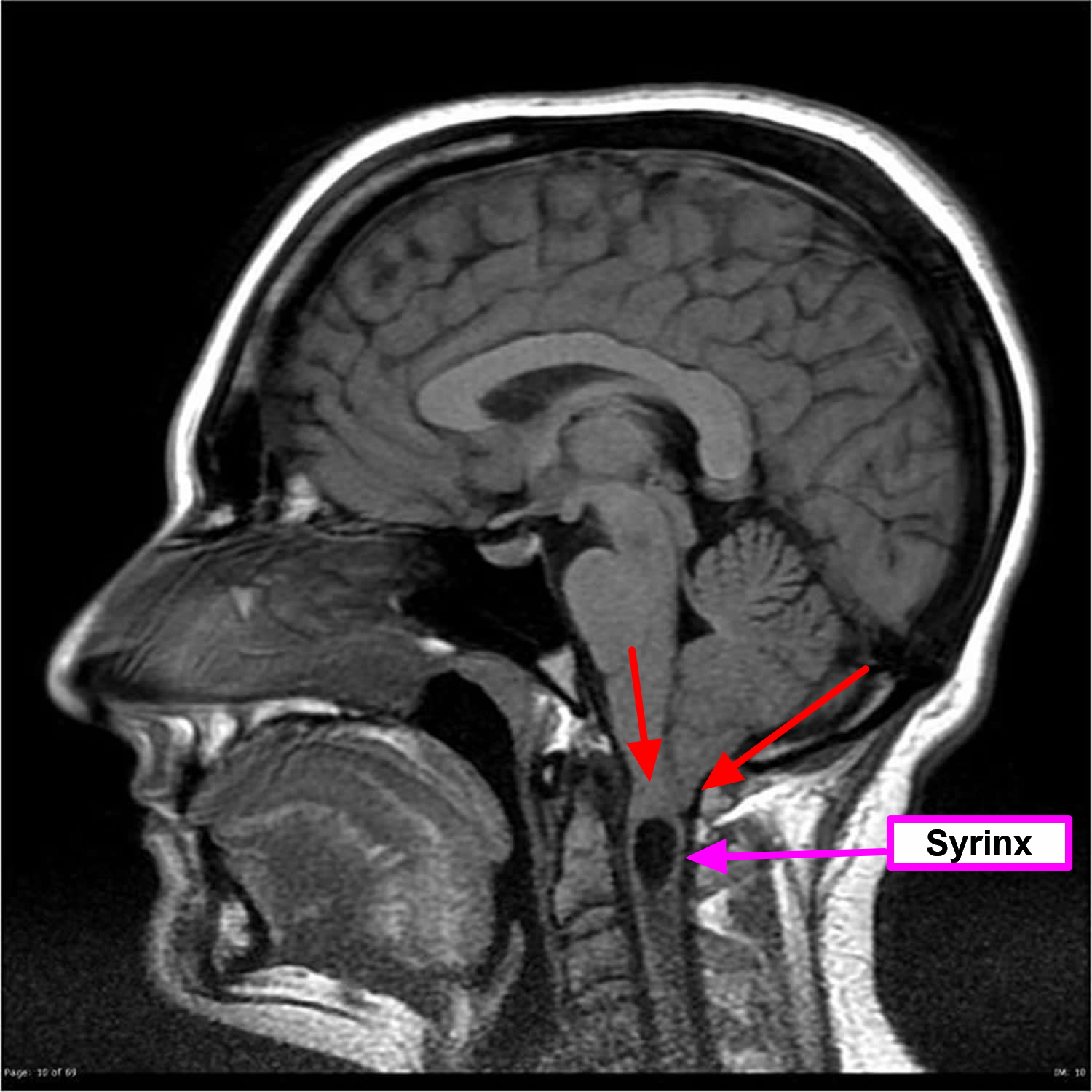
Figure 9. Chiari malformation type 1 with focal syrinx
Although Chiari I malformations are often isolated abnormalities; however, some associated anomalies have been described:
- cervical cord syrinx is present in ~35% (range 20-56%): more common in symptomatic patients
- hydrocephalus in up to 30% 2 of cases and
- both are thought to result from abnormal CSF flow dynamics through the central canal of the cord and around the medulla
- In ~35% (range 23-45%) of cases there are associated skeletal anomalies 2:
- platybasia/basilar invagination
- atlanto-occipital assimilation
- Sprengel deformity
- Syndromic associations
- Klippel-Feil syndrome
- Crouzon syndrome
- Hajdu-Cheney syndrome
Chiari I malformations can be divided into three stages (although not frequently used in day to day practice):
- I: asymptomatic
- II: brainstem compression
- III: syrinx
Treatment is usually reserved only for symptomatic patients or those with a syrinx. It consists of decompressing the posterior fossa, by removing part of the occipital bone, and posterior arch of C1 (cervical spine #1) as well as performing a duroplasty.
Chiari malformation type 2
Chiari 2 malformation also called classic Chiari malformation or Arnold-Chiari malformation with a small posterior fossa with a descent of both the brainstem and cerebellar tonsils into the foramen magnum and it is usually accompanied by a myelomeningocele — a form of spina bifida that occurs when the spinal canal and backbone do not close before birth, causing the spinal cord to protrude through an opening in the back. Spina bifida is a disorder characterized by the incomplete development of the brain, spinal cord, and/or their protective covering. A myelomeningocele usually results in partial or complete paralysis of the area below the spinal opening.
The term Arnold-Chiari malformation (named after two pioneering researchers) is specific to Type 2 Chiari malformations.
Individuals with Chiari malformation type 2 have symptoms that are generally more severe than in Chiari malformation type 1 and usually appear during childhood. This disorder can cause life-threatening complications during infancy or early childhood, and treating it requires surgery.
Chiari 2 malformations are encountered relatively commonly with an incidence of ~1:1000 live births 3. When a child is born with a myelomeningocoele the vast majority (~95%) have an associated Chiari 2 malformation.
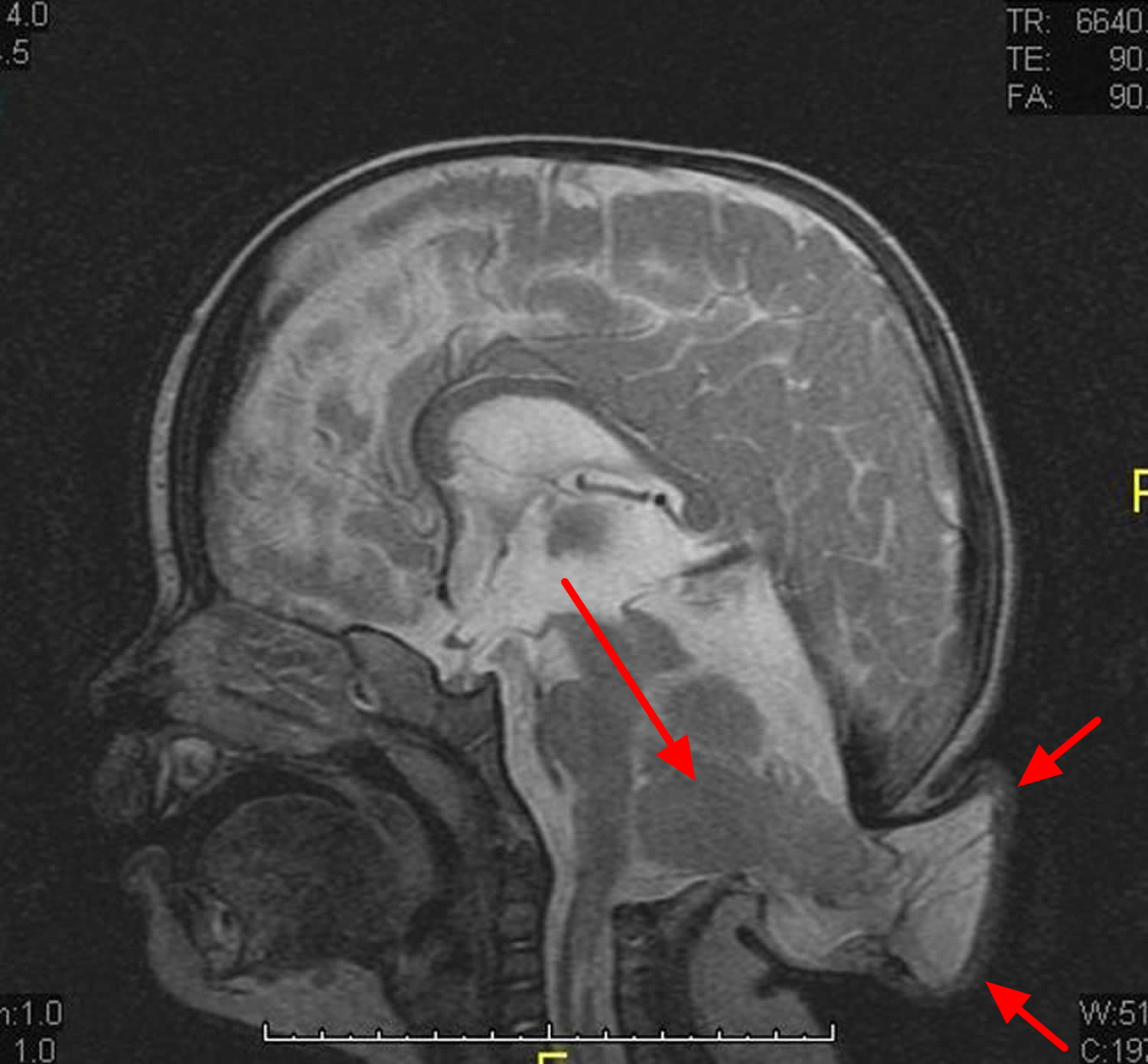
While Chiari 1 malformation is thought to result from a small posterior fossa, Chiari malformation type 2 occurs due to in utero malformation of the spine and cranial structures resulting in characteristic displacement of the medulla, fourth ventricle, and cerebellum through the foramen magnum.
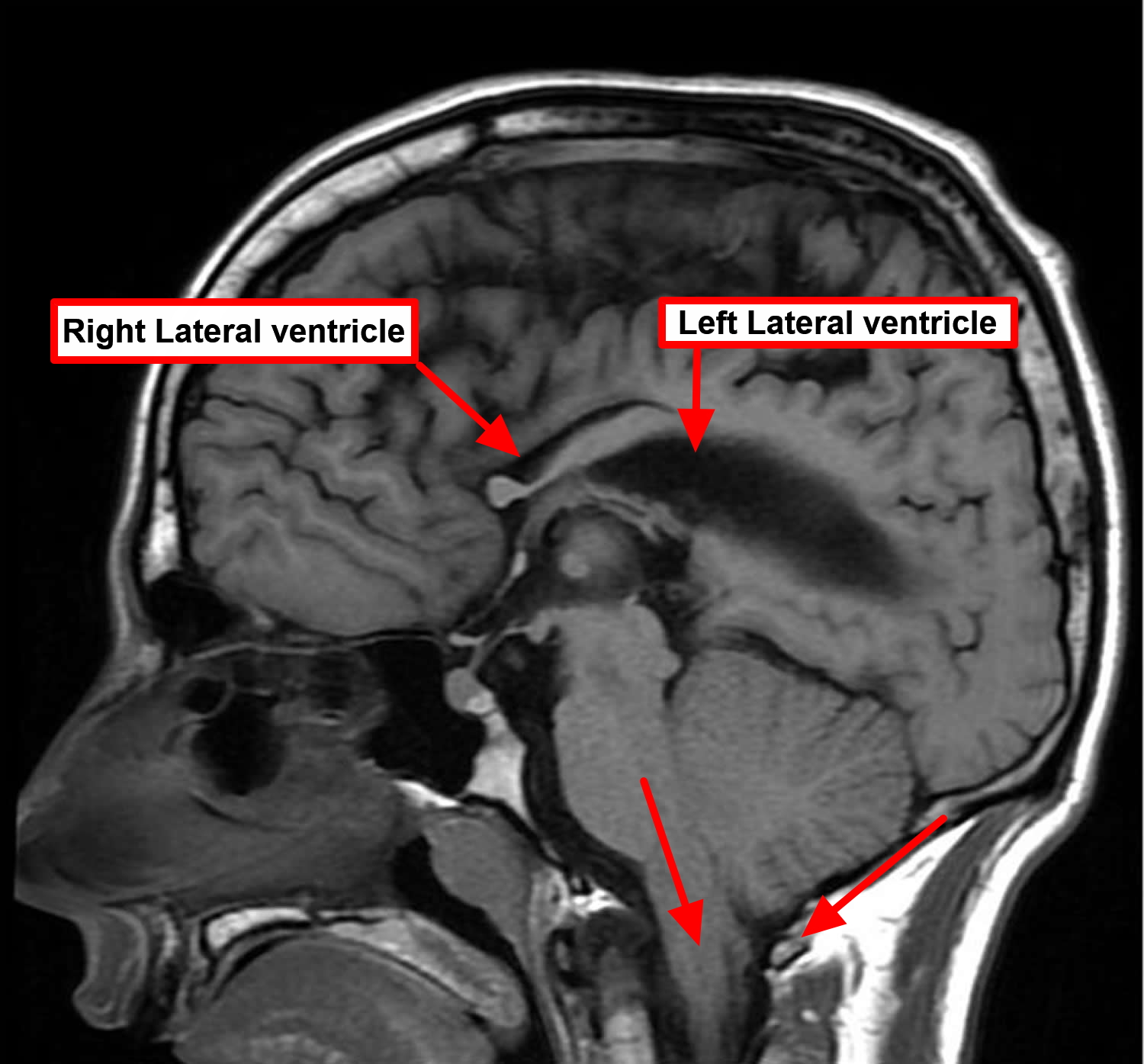
Figure 10. Chiari malformation type 2 (this patient was born with a sacral myelomeningocoele which was reparied in the neonatal period. Hydrocephalus, a common complication, is also present and has required shunting)
Chiari 2 malformations clinical features:
- displacement of the medulla, fourth ventricle and cerebellar vermis through the foramen magnum
- usually with associated with a lumbosacral spinal myelomeningocoele
As almost all neonatal patients with Chari malformation type 2 have a myelomeningocoele it has been suggested that the underlying aetiology is that of in utero CSF leak due to open spinal dysraphism. Older patients with Chiari II without a myelomeningocoele are thought to have had either a smaller neural tube defect or subsequent closure of the defect in utero.
Given the wide range of anatomical severity as well as a large number of associated abnormalities which are sometimes encountered, it should be no surprise that the clinical presentation of patients with Chiari 2 malformations is also varied both in character and severity. The presentation can be divided according to the age of the individual (although most will have life long sequelae) as follows 3:
- Neonatal
- myelomeningocoele
- brainstem dysfunction resulting in cranial nerve palsies
- neurogenic bladder
- Child
- musculoskeletal
- hydrocephalus
- Young adult
- syrinx and scoliosis
Chiari malformation type 2 is associated with these conditions:
spinal
- syringohydromyelia
- scoliosis
- segmentational anomalies: 50% 3
- Klippel-Feil syndrome
- atlanto-axial assimilation
- diastematomyelia
cerebral
- dysgenesis of corpus callosum
- absent septum pellucidum
- obstructive hydrocephalus
- fenestration of the falx with interdigitated gyri or absent falx; heart shape incisura
- stenogyria/polymicrogyria [probably not the same as polymicrogyia encountered in schizencephaly 3]
- tectal beaking
cranial vault
- scalloping of petrous temporal bone 4
- enlarged foramen magnum
- Luckenschadel skull
- small posterior fossa
skeletal
- clubfoot
Treatment of patients with Chiari 2 malformation is complex due to the variable form and severity of malformations:
- myelomeningocoele repair and management of neurogenic bladder
- is being performed on the in utero fetus at some centers in select cases to improve outcomes 5
- ventricular shunting (usually ventriculoperitoneal)
- hydrocephalus usually requires shunting and can help ameliorate cranial nerve and brainstem dysfunction
- craniovertebral decompression
- may also be required in neonates which brainstem dysfunction if hydrocephalus is not present or symptoms and signs do not improve with shunting
- older patients with hind brain herniation or syringohydromyelia may also benefit
Chiari malformation type 3
Chiari 3 malformation is the most serious form of Chiari malformation with features that are similar to Chiari 2 malformation but with an occipital and/or high cervical encephalocoele.
Chiari malformation type 3 is an extremely rare anomaly characterized by a low occipital and high cervical encephalocele with herniation of posterior fossa contents, that is, the cerebellum and/or the brainstem, occipital lobe, and fourth ventricle, through an abnormal opening in the back of the skull.
The symptoms of Chiari malformation type 3 appear in infancy and can cause debilitating and life-threatening complications. Babies with Chiari malformation type 3 can have many of the same symptoms as those with Chiari malformation type 2 but can also have additional severe neurological defects such as mental and physical delays, and seizures.
Chiari malformation type 3 is associated with these conditions:
- agenesis of the corpus callosum
- syringohydromyelia of the cervical cord
Figure 11. Chiari malformation type 3 (MRI image reveals a sub-occipital encephalocele with herniation of cerebellum in 2 month old baby)
Chiari malformation type 4
Chiari malformation type 4 was a term some authors gave to describe an incomplete or underdeveloped cerebellum (a condition known as cerebellar hypoplasia). In this rare form of Chiari malformation, the cerebellum is located in its normal position but parts of it are missing, and portions of the skull and spinal cord may be visible. Chiari malformation type 4 can be associated with hypoplasia of pons as well as a small funnel shaped posterior fossa. It is now considered to be an obsolete term.
Chiari malformation type 0
Researchers have determined that some individuals with a Chiari malformation have minimal or no herniation of the cerebellar tonsils through the foramen magnum. These individuals often have syringomyelia despite the lack of cerebellar tonsil herniation. Occipital headaches may also occur. Symptoms in these cases are most likely due to abnormalities in the flow of cerebrospinal fluid at the level of the foramen magnum at the skull base, although there is often no identifiable cause. Individuals with this condition have improved after decompression surgery. The addition of Chiari malformation type 0 as a classification for Chiari malformations is controversial; some physicians believe that, for a diagnosis of a Chiari malformation, tonsillar herniation must be present.
Other conditions are associated with Chiari malformations
- Hydrocephalus is an excessive buildup of CSF in the brain. A Chiari malformation can block the normal flow of this fluid and cause pressure within the head that can result in mental defects and/or an enlarged or misshapen skull. Severe hydrocephalus, if left untreated, can be fatal. The disorder can occur with any type of Chiari malformation, but is most commonly associated with Chiari malformation type 2.
- Spina bifida is the incomplete closing of the backbone and membranes around the spinal cord. In babies with spina bifida, the bones around the spinal cord do not form properly, causing defects in the lower spine. While most children with this birth defect have such a mild form that they have no neurological problems, individuals with Type 2 Chiari malformation usually have myelomeningocele, and a baby’s spinal cord remains open in one area of the back and lower spine. The membranes and spinal cord protrude through the opening in the spine, creating a sac on the baby’s back. This can cause a number of neurological impairments such as muscle weakness, paralysis, and scoliosis.
- Syringomyelia is a disorder in which a CSF-filled tubular cyst, or syrinx, forms within the spinal cord’s central canal. The growing syrinx destroys the center of the spinal cord, resulting in pain, weakness, and stiffness in the back, shoulders, arms, or legs. Other symptoms may include a loss of the ability to feel extremes of hot or cold, especially in the hands. Some individuals also have severe arm and neck pain.
- Tethered cord syndrome occurs when a child’s spinal cord abnormally attaches to the tissues around the bottom of the spine. This means the spinal cord cannot move freely within the spinal canal. As a child grows, the disorder worsens, and can result in permanent damage to the nerves that control the muscles in the lower body and legs. Children who have a myelomeningocele have an increased risk of developing a tethered cord later in life.
- Spinal curvature is common among individuals with syringomyelia or Chiari malformation Type 1. The spine either may bend to the left or right (scoliosis) or may bend forward (kyphosis).
Chiari malformation complications
In some people, Chiari malformation can become a progressive disorder and lead to serious complications. In others, there may be no associated symptoms, and no intervention is necessary. The complications associated with this condition include:
- Hydrocephalus. An accumulation of excess fluid within your brain (hydrocephalus) may require placement of a flexible tube (shunt) to divert and drain the cerebrospinal fluid to another area of your body.
- Spina bifida. Spina bifida, a condition in which your spinal cord or its covering isn’t fully developed, may occur in Chiari malformation. Part of the spinal cord is exposed, which can cause serious conditions such as paralysis. People with Chiari malformation type II usually have a form of spina bifida called myelomeningocele.
- Syringomyelia. Some people with Chiari malformation also develop a condition called syringomyelia, in which a cavity or cyst (syrinx) forms within the spinal column.
- Tethered cord syndrome. In this condition, your spinal cord attaches to your spine and causes your spinal cord to stretch. This can cause serious nerve and muscle damage in your lower body.
Chiari malformation life expectancy
Many people with Type1 Chiari malformation do not show symptoms and do not know they have the condition. Symptoms may change for some individuals, depending on the compression of the tissue and nerves and on the buildup of crebrospinal fluid pressure. Many individuals with the more severe types of Chiari malformation and have surgery see a reduction in their symptoms and/or prolonged periods of relative stability, although paralysis is generally permanent.
Most patients who have surgery experience a reduction or stabilisation of their symptoms. Some patients may experience prolonged periods of relative stability. Infants with very severe malformations may have life-threatening complications.
Chiari malformation causes
The exact cause of Chiari malformations is unknown. These malformations and the associated central nervous system abnormalities are extremely complex. There’s some evidence that Chiari malformation runs in some families. However, research into a possible hereditary component is still in its early phase.
Chiari malformation has several different causes. Most often it is caused by structural defects in the brain and spinal cord that occur during fetal development. This can be the result of genetic mutations or a maternal diet that lacked certain vitamins or nutrients. This is called primary or congenital Chiari malformation. It can also be caused later in life if spinal fluid is drained excessively from the lumbar or thoracic areas of the spine either due to traumatic injury, disease, or infection. This is called acquired or secondary Chiari malformation. Primary Chiari malformation is much more common than secondary Chiari malformation.
The exact cause of primary Chiari malformations is unknown. These malformations and the associated central nervous system abnormalities are extremely complex. Chiari malformations appear to be due to a developmental failure of the brainstem and upper spinal cord (cervical region) within a developing fetus with no known cause. Some investigators believe that an abnormally small posterior fossa, which is the space in which the cerebellum normally resides, contributes to the development of a Chiari malformation. In many individuals, the posterior fossa is abnormally small, which may lead to the growing brain being pushed down through the normal opening (foramen magnum) where the brain and spinal cord meet.
The specific parts of the cerebellum that are affected are the cerebellar tonsils. The cerebellum is the part of the brain that plays a role in maintaining balance and posture as well as coordinating voluntary movements. The cerebellar tonsils are small peg-like structures at the base of the cerebellum. When the tonsils protrude through the foramen magnum, they block the proper flow of cerebrospinal fluid between the skull and the spinal cord, potentially compressing the brainstem (pons medulla) and the upper portion of the spinal cord.
There have been numerous reports in the medical literature of families in which more than one family member was affected by a Chiari malformation. This suggests that in some cases genetic factors play a role in the development of a Chiari malformation. Research is ongoing to determine the specific genetic components (e.g., gene mutations) that influence the development of Chiari malformations in some people.
In extremely rare cases, Chiari malformations have been acquired during life. Generally, any condition that takes up space within the skull, especially within the posterior fossa of the skull, can cause an acquired Chiari malformation. Such conditions include tumors, an arachnoid cyst, and hematomas. Hydrocephalus and intracranial hypertension (pseudotumor cerebri) have also been linked to Chiari malformations. Abnormalities that affect the upper cervical portion of the spine, such as basilar invagination, can also cause a Chiari malformation. Basilar invagination occurs when the upper vertebrae are located upward, blocking the foramen magnum and thereby blocking the flow of cerebrospinal fluid.
Leakage or drainage of CSF including the prolonged use of a lumboperitoneal shunt, which is often used to treat hydrocephalus, has been linked to the development of an acquired Chiari malformation. One theory states that if too much cerebrospinal fluid is drained, it might create a pressure imbalance between the cranial and spinal fluid compartments. Consequently, this pressure imbalance is theorized to suck or draw the cerebellar tonsils downward through the foramen magnum.
Some researchers have speculated that, in a specific subset of individuals, a Chiari malformation may be caused by a tethered cord. Such individuals have a normal-sized posterior fossa. Tethered cord syndrome is a stretch-induced functional disorder associated with the fixation (tethering) effect of inelastic tissue (filum terminale) on the lower end of the spinal cord, limiting its normal upward movement. This abnormal attachment is associated with progressive stretching and increased tension of the spinal cord as a child grows, potentially resulting in a variety of neurological and other symptoms. While some individuals have both a tethered cord and a Chiari malformation, the exact relationship between these two disorders is not understood. Whether tethered cord syndrome is a distinct cause of Chiari malformations in certain cases is unproven and controversial.
Chiari malformations can also occur as part of a larger syndrome such as Goldenhar syndrome, Albright hereditary osteodystrophy (pseudohypoparathyroidism), Hajdu-Cheney syndrome, achondroplasia and hereditary connective tissue diseases such as Ehlers-Danlos syndrome.
Many of the symptoms of a Chiari malformation are believed to be due to abnormalities affecting the flow of cerebrospinal fluid (CSF) in the skull and spinal canal. Syringomyelia, which is often associated with a Chiari malformation, most likely develops due to partial obstruction of the normal flow of CSF between the brain and spinal cord. Some symptoms associated with a Chiari malformation or syringomyelia result from direct compression of portions of the brainstem or spinal cord. Researchers have determined that the length of herniation (i.e., the amount of the cerebellar tonsils that protrudes through the foramen magnum) does not necessarily correspond to the severity of a Chiari malformation.
Chiari malformation symptoms
Headache is the hallmark sign of Chiari malformation, especially after sudden coughing, sneezing, or straining. Other symptoms may vary among individuals and may include:
- neck pain
- hearing or balance problems
- muscle weakness or numbness
- dizziness
- difficulty swallowing or speaking
- vomiting
- ringing or buzzing in the ears (tinnitus)
- curvature of the spine (scoliosis)
- insomnia
- depression
- problems with hand coordination and fine motor skills.
Some individuals with Chiari malformation may not show any symptoms. Symptoms may change for some individuals, depending on the compression of the tissue and nerves and on the buildup of CSF pressure.
Infants with a Chiari malformation may have difficulty swallowing, irritability when being fed, excessive drooling, a weak cry, gagging or vomiting, arm weakness, a stiff neck, breathing problems, developmental delays, and an inability to gain weight.
Chiari malformation type 1 symptoms
Headaches, often severe, are the classic symptom of Chiari malformation. They generally occur after sudden coughing, sneezing or straining. People with Chiari malformation type 1 can also experience:
- Neck pain
- Unsteady gait (problems with balance)
- Poor hand coordination (fine motor skills)
- Numbness and tingling of the hands and feet
- Dizziness
- Difficulty swallowing, sometimes accompanied by gagging, choking and vomiting
- Vision problems (blurred or double vision)
- Speech problems, such as hoarseness
Less often, people with Chiari malformation may experience:
- Ringing or buzzing in the ears (tinnitus)
- Weakness
- Slow heart rhythm
- Curvature of the spine (scoliosis) related to spinal cord impairment
- Abnormal breathing, such as central sleep apnea, characterized by periods of breathing cessation during sleep
Chiari malformation type 2 symptoms
In Chiari malformation type 2, a greater amount of tissue extends into the spinal canal compared with Chiari malformation type 1.
The signs and symptoms can include those related to a form of spina bifida called myelomeningocele that nearly always accompanies Chiari malformation type 2. In myelomeningocele, the backbone and the spinal canal haven’t closed properly before birth.
Symptoms may include:
- Changes in breathing pattern
- Swallowing problems, such as gagging
- Quick downward eye movements
- Weakness in arms
Chiari malformation type 3 symptoms
In one of the most severe types of the condition, Chiari malformation type 3, a portion of the lower back part of the brain (cerebellum) or the brainstem extends through an abnormal opening in the back of the skull. This form of Chiari malformation is diagnosed at birth or by an ultrasound during pregnancy.
This type of Chiari malformation has a higher mortality rate and may also cause neurological problems.
Chiari malformations diagnosis
Currently, no test is available to determine if a baby will be born with a Chiari malformation. Since Chiari malformations are associated with certain birth defects like spina bifida, children born with those defects are often tested for malformations. However, some malformations can be seen on ultrasound images before birth.
Many people with Chiari malformations have no symptoms and their malformations are discovered only during the course of diagnosis or treatment for another disorder. The doctor will perform a physical exam and check the person’s memory, cognition, balance (functions controlled by the cerebellum), touch, reflexes, sensation, and motor skills (functions controlled by the spinal cord). The physician may also order one of the following diagnostic tests:
- Magnetic resonance imaging (MRI) is the imaging procedure most often used to diagnose a Chiari malformation. It uses radio waves and a powerful magnetic field to painlessly produce either a detailed three-dimensional picture or a two-dimensional “slice” of body structures, including tissues, organs, bones, and nerves.
- X-rays use electromagnetic energy to produce images of bones and certain tissues on film. An X-ray of the head and neck cannot reveal a CM but can identify bone abnormalities that are often associated with the disorder.
- Computed tomography (CT) uses X-rays and a computer to produce two-dimensional pictures of bone and blood vessels. CT can identify hydrocephalus and bone abnormalities associated with Chiari malformation.
Chiari malformation treatment
Some Chiari malformations do not show symptoms and do not interfere with a person’s activities of daily living. In these cases, doctors may only recommend regular monitoring with MRI. When individuals experience pain or headaches, doctors may prescribe medications to help ease symptoms and/or massage therapy or a reduction in activities, particularly those involving heavy lifting or straining. Physical therapy may be tried in some cases, but some physicians argue against its use stating that physical therapy for individuals with a Chiari malformation is not always effective.
Medications may ease certain symptoms, such as pain, when present. In many cases, surgery is the only treatment available to improve or stabilize symptoms or halt the progression of damage to the central nervous system. There are no specific criteria or objective tests that can be used to determine when to undergo surgery or the best procedures to choose. The procedure that is best may differ for children and adults. More than one surgery may be needed to treat the condition. Surgery may include a procedure to create more space for the cerebellum or removing part of the cerebellar tonsils that may reach through the skull opening (the cerebellar tonsils do not have a recognized function and can be removed without causing any known neurological problems).
Children with Chiari malformation that is associated with spina bifida may require surgery to repair the myelomeningocele. Hydrocephalus may be treated with surgical implantation of a shunt to relieve increased pressure on the brain. Patients with symptomatic Chiari malformation or syringomyelia may benefit from surgery in which the opening in the base of the skull is enlarged to relieve the pressure on the medulla and to allow normal flow of the cerebrospinal fluid (CSF).
Chiari malformation surgery
In many cases, surgery is the only treatment available to ease symptoms or halt the progression of damage to the central nervous system. Surgery can improve or stabilize symptoms in most individuals. More than one surgery may be needed to treat the condition.
However, neurosurgeons and other physicians may disagree as to the best approach to treat a Chiari malformation. There is no specific, agreed-upon therapy or treatment regimen. Different neurosurgeons may recommend different surgical techniques or treatment regimens.
The most common surgery to treat Chiari malformation is posterior fossa decompression. It creates more space for the cerebellum and relieves pressure on the spinal cord. The surgery involves making an incision at the back of the head and removing a small portion of the bone at the bottom of the skull (craniectomy). In some cases the arched, bony roof of the spinal canal, called the lamina, may also be removed (spinal laminectomy). Your neurosurgeon will insert an artificial plate over the area where the skull was removed. The surgery should help restore the normal flow of CSF, and in some cases it may be enough to relieve symptoms.
Next, the surgeon may make an incision in the dura, the protective covering of the brain and spinal cord. Some surgeons perform a Doppler ultrasound test during surgery to determine if opening the dura is even necessary. If the brain and spinal cord area is still crowded, the surgeon may use a procedure called electrocautery to remove the cerebellar tonsils, allowing for more free space. These tonsils do not have a recognized function and can be removed without causing any known neurological problems. Electrocautery is more invasive and is not advocated by all neurosurgeons, but appears necessary for at least some patients.
The final step is to sew a dura patch (duraplasty) in place to enlarge the covering and provide more room for your brain to expand the space around the tonsils, similar to letting out the waistband on a pair of pants. The patch used in a duraplasty may be an artificial material or it could be tissue harvested from another part of your body. A duraplasty is performed to provide even more room for decompression, although some physicians argue against the necessity of this step. It may not be necessary in children.
Your doctor may also remove a small portion of the spinal column to relieve pressure on your spinal cord and allow more space for the spinal cord.
Surgical treatment of a Chiari malformation has variable results. One study found that more than 80 percent of adults reported significant improvement in symptoms after surgery. However, response to therapy is highly variable. Symptoms related to a Chiari malformation may respond differently from symptoms related to an associated syringomyelia. Although some individuals experience significant improvement, others may have symptoms that persist including residual pain, muscle weakness, and loss of sensation. In addition, surgery carries risks such as leakage of cerebrospinal fluid or infection.
Infants and children with myelomeningocele may require surgery to reposition the spinal cord and close the opening in the back. Findings from the National Institutes of Health show that this surgery is most effective when it is done prenatally (while the baby is still in the womb) instead of after birth. The prenatal surgery reduces the occurrence of hydrocephalus and restores the cerebellum and brain stem to a more normal alignment.
The surgical technique may vary, depending on whether a fluid-filled cavity (syrinx) is present, or if you have fluid in your brain (hydrocephalus). If you have a syrinx or hydrocephalus, you may need a tube (shunt) to drain the excess fluid and relieves pressure inside your head. A sturdy tube, surgically inserted into the head, is connected to a flexible tube placed under the skin. These tubes drain the excess fluid into either the chest cavity or the abdomen so it can be absorbed by the body.
An alternative surgical treatment in some individuals with hydrocephalus is third ventriculostomy, a procedure that improves the flow of CSF out of the brain. A small hole is made at the bottom of the third ventricle (brain cavity) and the CSF is diverted there to relieve pressure. Similarly, in cases where surgery was not effective, doctors may open the spinal cord and insert a shunt to drain a syringomyelia or hydromyelia (increased fluid in the central canal of the spinal cord).
Untethering – some children with a Chiari malformation type 1 have a tethered spinal cord, which means it is abnormally attached within the spine. Untethering involves separating the spinal cord and releasing tension in the spine.
Spinal fixation – some people with Chiari malformation type 1 will have a hypermobility syndrome, such as Ehlers-Danlos syndrome, and may require surgery to stabilise their spine.
Syringomyelia associated with a Chiari malformation usually does not require direct treatment. In most cases, syringomyelia improves on its own after surgery to correct a Chiari malformation because the normal flow of cerebrospinal fluid is restored.
An acquired Chiari malformation requires treatment of the underlying condition. In many cases, a Chiari malformation may resolve without further treatment in such cases.
Genetic counseling may be of benefit for affected individuals and their families. Additional treatment is symptomatic and supportive.
Surgical risks and follow-up
Surgery involves risks, including the possibility of infection, fluid in your brain, paralysis, stroke, cerebrospinal fluid leakage or problems with wound healing. Discuss the pros and cons with your doctor when deciding whether surgery is the most appropriate alternative for you.
The surgery reduces symptoms in most people, but if nerve injury in the spinal canal has already occurred, this procedure won’t reverse the damage.
After the surgery, you’ll need regular follow-up examinations with your doctor, including periodic imaging tests to assess the outcome of surgery and the flow of cerebrospinal fluid.
Symptoms may recur after a successful surgery, usually within the first two years. Most likely, this is due to the development of scar tissue or an opening around the duraplasty covering the brain. Children required periodic MRI examinations because of the normal continued growth of the brain and skull.
- Ketonen L, Hiwatashi A, Sidhu R. Pediatric brain and spine, an atlas of MRI and spectroscopy. Springer Verlag. (2005) ISBN:3540213406.[↩][↩]
- Elster AD, Chen MY. Chiari I malformations: clinical and radiologic reappraisal. Radiology. 1992;183 (2): 347-53. https://www.ncbi.nlm.nih.gov/pubmed/1561334[↩][↩][↩]
- Maixner WJ. Spina Bifida, Management and Outcome. Springer. (2008) ISBN:8847006511.[↩][↩][↩][↩]
- Naidich TP, Pudlowski RM, Naidich JB et-al. Computed tomographic signs of the Chiari II malformation. Part I: Skull and dural partitions. Radiology. 1980;134 (1): 65-71. https://www.ncbi.nlm.nih.gov/pubmed/7350637[↩]
- Adzick NS. Fetal surgery for myelomeningocele: trials and tribulations. Isabella Forshall Lecture. (2012) Journal of pediatric surgery. 47 (2): 273-81. doi:10.1016/j.jpedsurg.2011.11.021 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278714/[↩]