Contents
- Eye diseases
- Common Eye Disorders
- Refractive errors
- Degenerative eye disease
- Age-Related Macular Degeneration
- The Macula
- Who is at risk ?
- Does lifestyle make a difference ?
- How is age-related macular degeneration detected ?
- What are the stages of age-related macular degeneration ?
- How is age-related macular degeneration treated ?
- Advanced neovascular age-related macular degeneration
- Loss of Vision
- Charles Bonnet syndrome (Visual Hallucinations)
- Coping with age-related macular degeneration
- Age-Related Macular Degeneration
- Diabetic Eye Disease
- Diabetic Retinopathy
- What causes diabetic retinopathy ?
- What is diabetic macular edema ?
- Who is at risk for diabetic retinopathy ?
- What are the symptoms of diabetic retinopathy and diabetic macular edema ?
- How can people with diabetes protect their vision ?
- How is diabetic macular edema treated ?
- How is proliferative diabetic retinopathy treated ?
- What is a vitrectomy ?
- What if treatment doesn’t improve vision ?
- Cataract
- What causes cataracts ?
- How do cataracts affect vision ?
- When are you most likely to have a cataract ?
- Who is at risk for cataract ?
- What are the symptoms of a cataract ?
- Are there different types of cataract ?
- How is a cataract detected ?
- How is a cataract treated ?
- What are the risks of cataract surgery ?
- What if you have other eye conditions and need cataract surgery ?
- Can problems develop after surgery ?
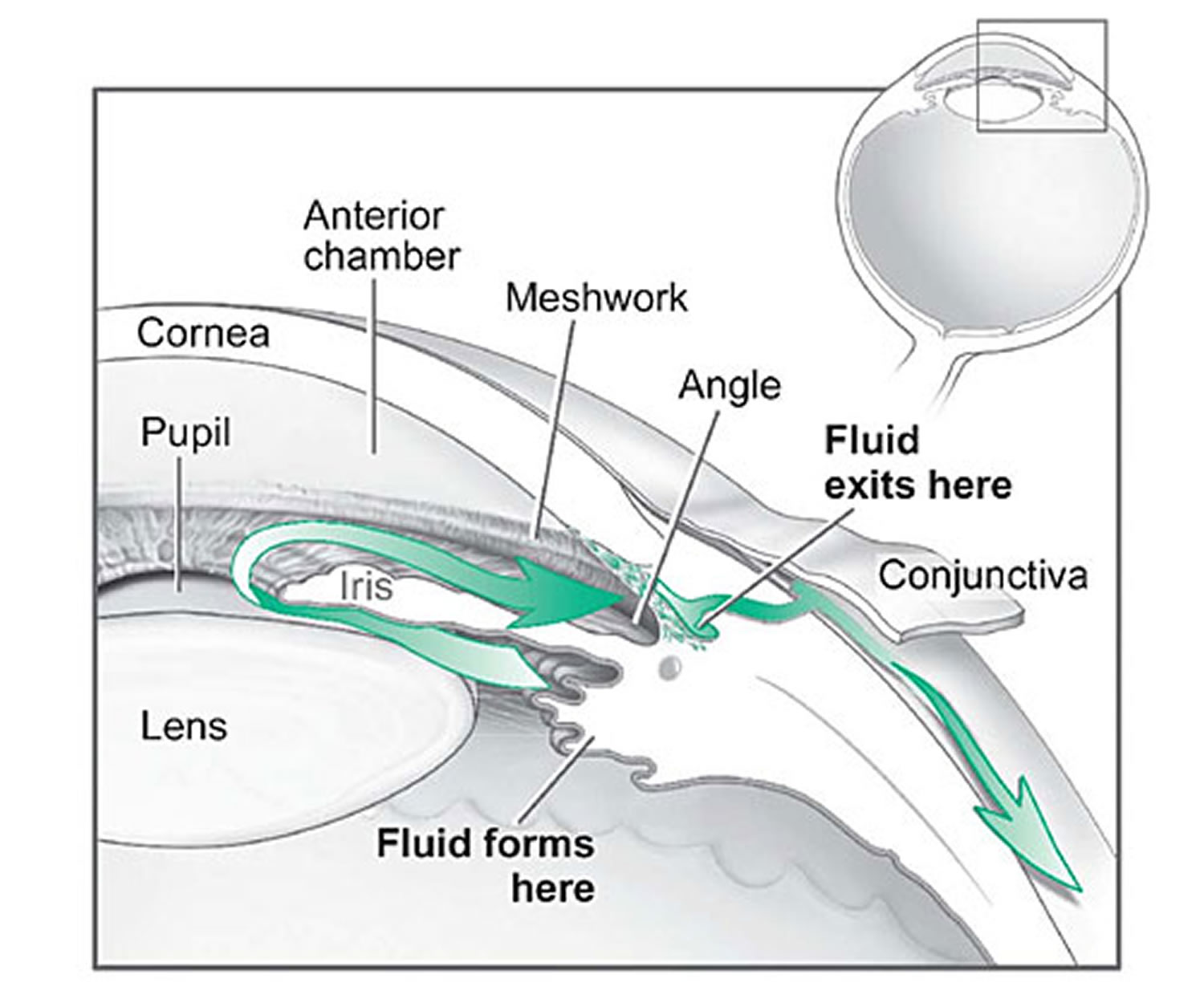
- Glaucoma
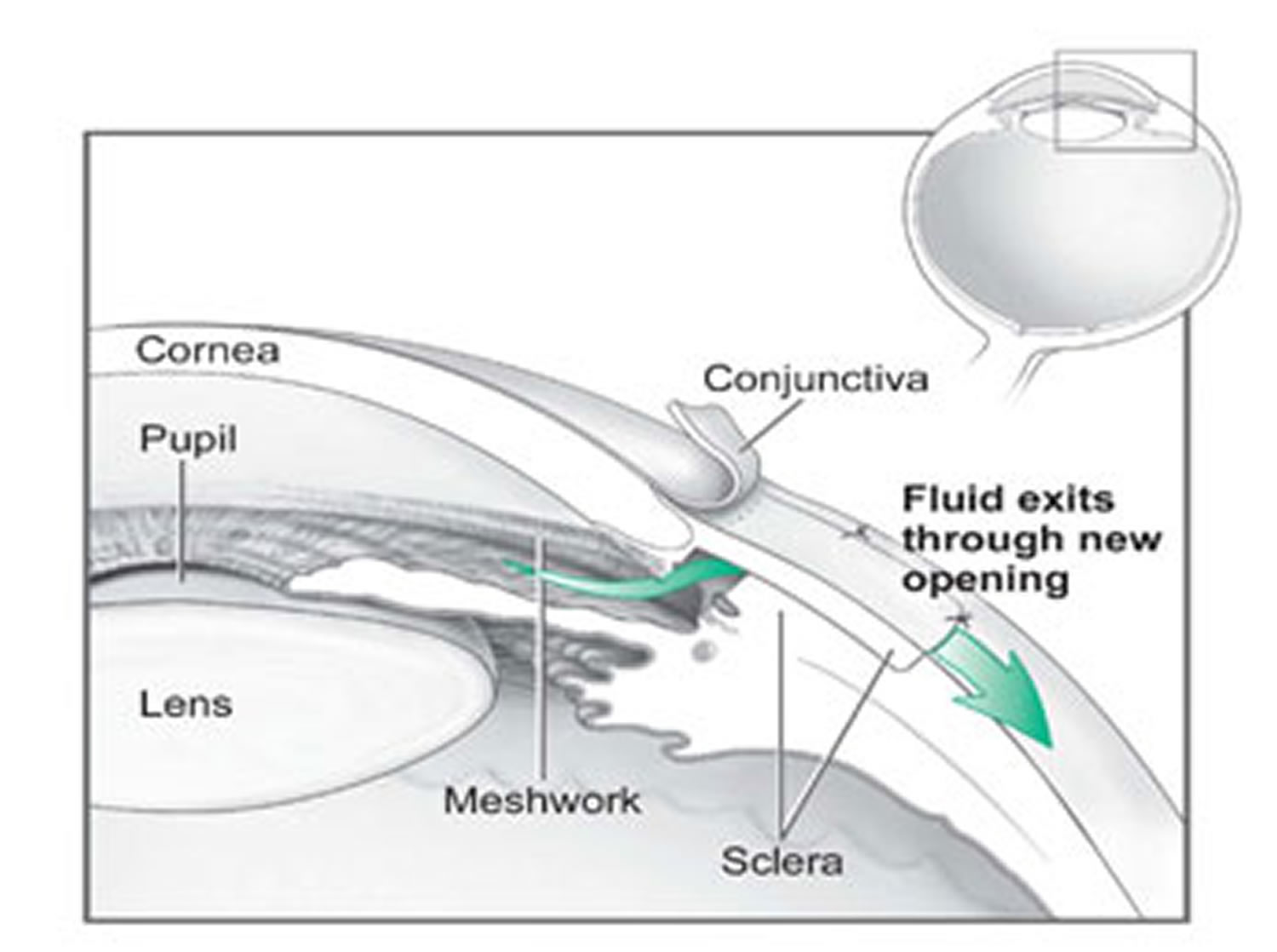
- How does the optic nerve get damaged by open-angle glaucoma ?
- Can you develop glaucoma if you have increased eye pressure ?
- Can you develop glaucoma without an increase in your eye pressure ?
- Who is at risk for open-angle glaucoma ?
- Glaucoma Symptoms
- How is glaucoma detected ?
- Can glaucoma be cured ?
- Glaucoma Treatments
- Laser trabeculoplasty
- Conventional surgery
- What are some other forms of glaucoma and how are they treated ?
- Thyroid eye disease
- Dry Eye
- Strabismus
- Types of strabismus
- Horizontal strabismus
- Vertical strabismus
- What causes strabismus ?
- How is strabismus related to poor vision ?
- Who develops strabismus as a child ?
- What adult disorders cause strabismus ?
- How does trauma cause strabismus ?
- How is strabismus treated ?
- What age is considered “too old” to have eye muscle surgery ?
- Can anything be done for adults with strabismus (misaligned eyes) ?
- Why do adults get strabismus ?
- Is eye straightening as an adult strictly cosmetic ?
- Is eye muscle surgery risky for adults ?
- How successful is eye muscle surgery ?
- How painful is this type of surgery ?
- Is hospitalization required for eye alignment surgery and how will this affect normal activities ?
- Amblyopia
- What causes amblyopia ?
- What is refractive amblyopia ?
- What is strabismic amblyopia ?
- What is deprivation amblyopia ?
- When should amblyopia be treated ?
- How old is TOO old for amblyopia treatment ?
- What happens if amblyopia is not treated ?
- How can you get early treatment for amblyopia ?
- How is amblyopia treated in children ?
- What happens if amblyopia treatment does not work ?
- Can surgery be performed to treat amblyopia ?
- Can amblyopia be treated in adults ?
- Conjunctivitis
- What is pink eye ?
- What causes pink eye (conjunctivitis) ?
- Is conjunctivitis contagious ?
- Does a pink eye always mean infection ?
- How you can prevent getting conjunctivitis ?
- How is pink eye diagnosed ?
- Viral Conjunctivitis
- Bacterial Conjunctivitis
- Allergic Conjunctivitis
- How is conjunctivitis treated ?
- Will there be any permanent effect on vision with conjunctivitis ?
- Can newborns get pink eye ?
- How is pink eye treated in newborns ?
- Diabetic Retinopathy
Eye diseases
Some eye problems are minor and don’t last long. But some can lead to a permanent loss of vision.
It is estimated that half of visual impairment and blindness can be prevented through early diagnosis and timely treatment. Despite cost-effective treatment and eye preservation interventions, the number of potentially blinding eye diseases continues to escalate. Increased awareness can help — remind family members and friends at higher risk for eye diseases and vision loss to have their eyes examined regularly.
The prevalence of blindness and visual impairment increases with age in all racial and ethnic groups. The major eye diseases among people 40 years and older are age-gelated macular degeneration, cataract, diabetic retinopathy, and glaucoma.
Common Eye Disorders
Approximately 11 million Americans aged 12 years and older could improve their vision through proper refractive correction 1. More than 3.3 million Americans aged 40 years and older are either legally blind (having best-corrected visual acuity of 6/60 or worse (=20/200) in the better-seeing eye) or are with low vision (having best-corrected visual acuity less than 6/12 (<20/40) in the better-seeing eye, excluding those who were categorized as being blind) 1. The leading causes of blindness and low vision in the United States are primarily age-related eye diseases such as age-related macular degeneration, cataract, diabetic retinopathy, and glaucoma. Other common eye disorders include amblyopia and strabismus.
Common eye problems include:
- Refractive errors
- Cataracts – clouded lenses
- Optic nerve disorders, including glaucoma
- Retinal disorders – problems with the nerve layer at the back of the eye
- Macular degeneration – a disease that destroys sharp, central vision (age-related macular degeneration)
- Diabetic eye problems (diabetic retinopathy)
- Strabismus
- Conjunctivitis – an infection also known as pinkeye.
How do your eyes work ?
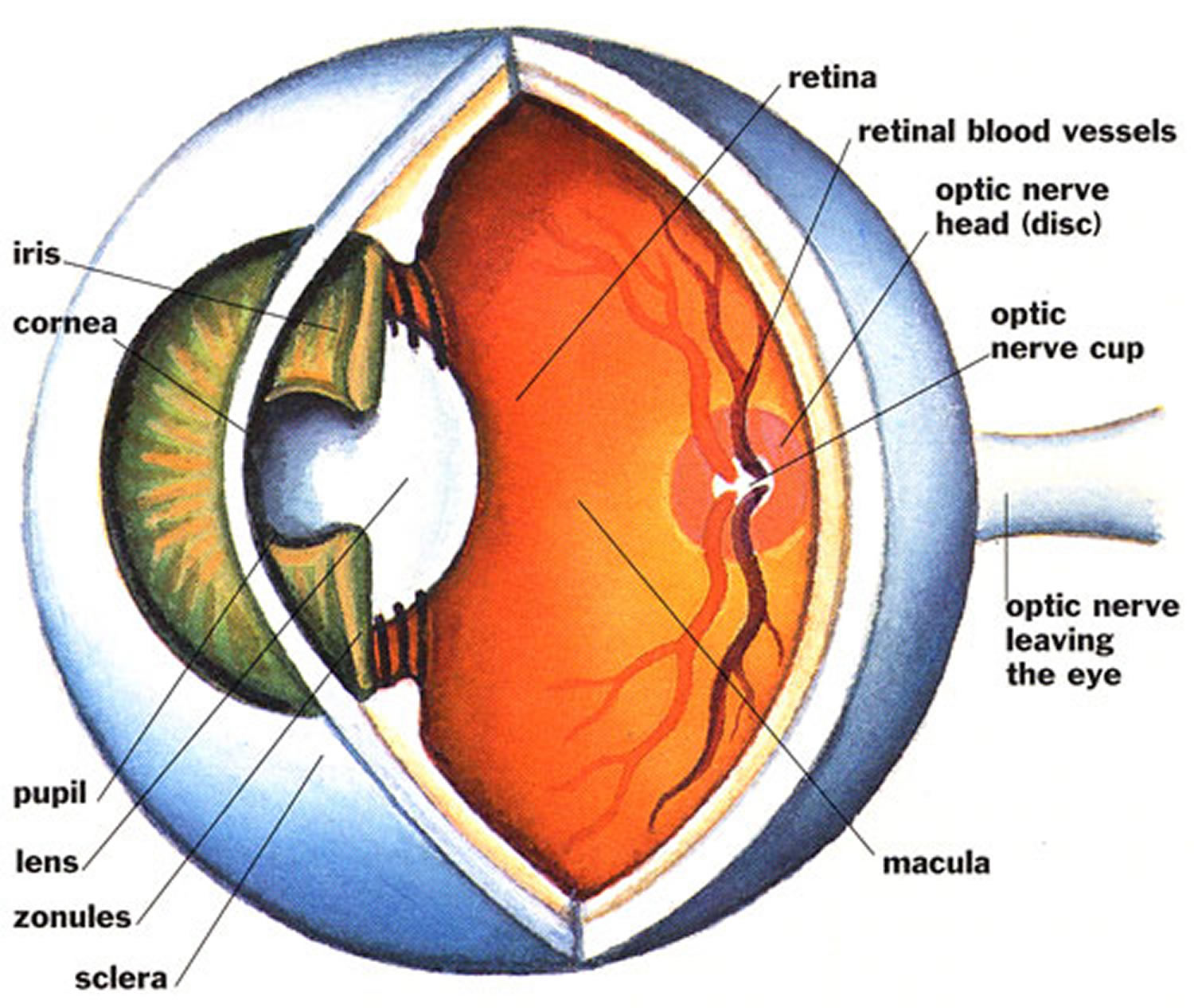
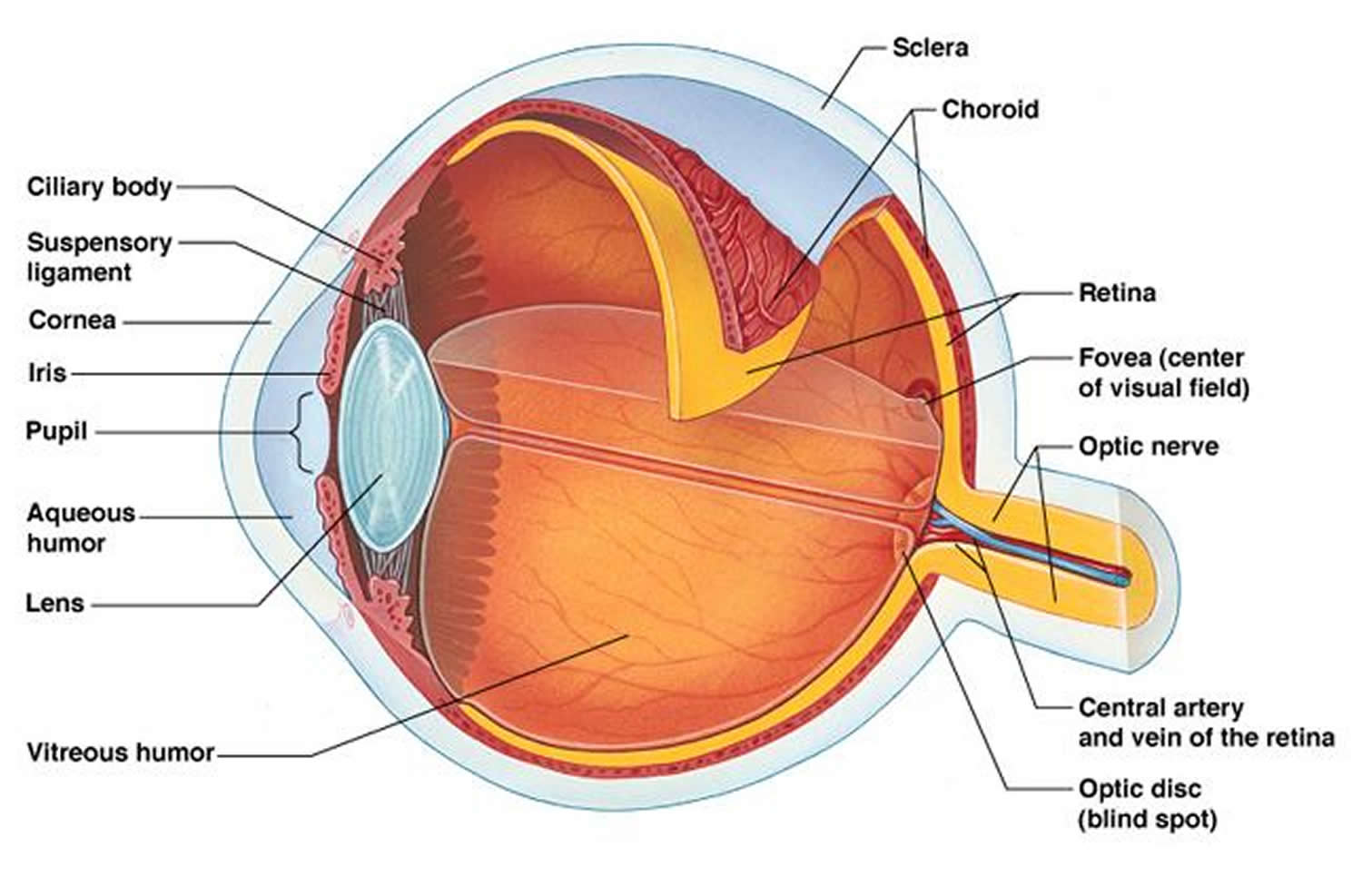
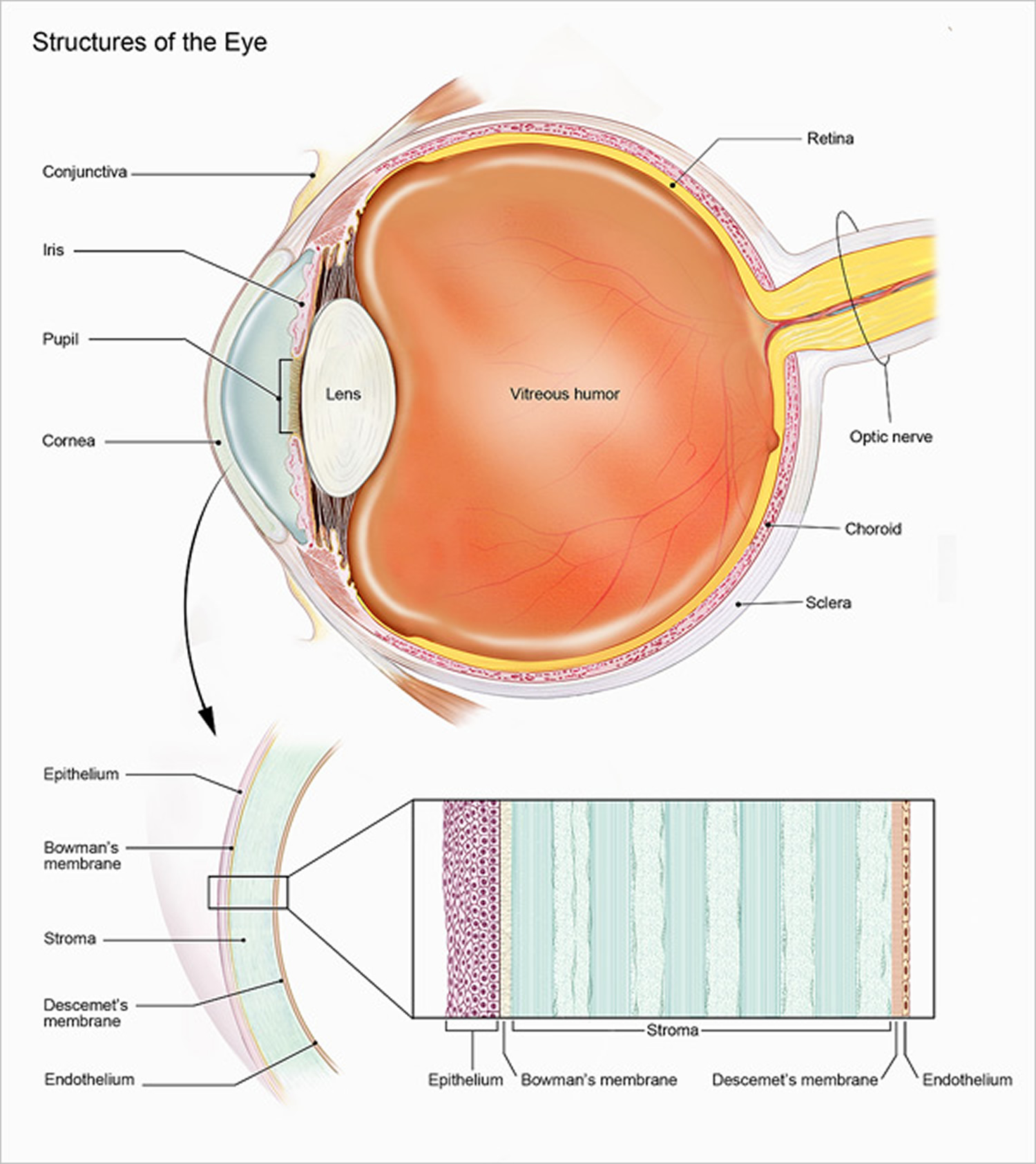
There are many different parts of the eye that help to create vision 2. We “see” with our brains; our eyes collect visual information and begin this complex process.
- Light passes through the cornea, the clear, dome-shaped surface that covers the front of the eye. The cornea bends – or refracts – this incoming light.
- The iris, the colored part of the eye, regulates the size of the pupil, the opening that controls the amount of light that enters the eye.
- Behind the pupil is the lens, a clear part of the eye that further focuses light, or an image, onto the retina.
- The retina is a thin, delicate, photosensitive tissue that contains the special “photoreceptor” cells that convert light into electrical signals.
- These electrical signals are processed further, and then travel from the retina of the eye to the brain through the optic nerve, a bundle of about one million nerve fibers.
How can you keep your eyes healthy ?
Incorporate your eye health as part of your regular health check-ups. Having a comprehensive dilated eye exam is one of the best things you can do to make sure that you’re seeing the best you can and that you’re keeping your eyes healthy.
Millions of people have problems with their vision every year. Some of these problems can cause permanent vision loss and even blindness, while others are common problems that can be easily corrected with glasses or contact lenses.
Tips for Keeping Your Eyes Healthy 2
- Have a comprehensive dilated eye exam. A dilated eye exam is the only way to detect many common eye diseases such as glaucoma, diabetic eye disease and age-related macular degeneration in their early stages.
- Know your family’s eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary. This will help to determine if you are at higher risk for developing an eye disease or condition.
- Eat right to protect your sight. Eating a diet rich in fruits and vegetables, particularly dark leafy greens such as spinach, kale, or collard greens is important for keeping your eyes healthy, too. Research has also shown there are eye health benefits from eating fish high in omega-3 fatty acids, such as salmon, tuna, and halibut.
- Maintain a healthy weight. Being overweight or obese increases your risk of developing diabetes and other systemic conditions, which can lead to vision loss, such as diabetic eye disease or glaucoma. If you are having trouble maintaining a healthy weight, talk to your doctor.
- Wear protective eyewear. Protective eyewear includes safety glasses and goggles, safety shields, and eye guards specially designed to provide the correct protection for a certain activity.
- Quit smoking or never start. Smoking is as bad for your eyes as it is for the rest of your body. Research has linked smoking to an increased risk of developing age-related macular degeneration, cataract, and optic nerve damage, all of which can lead to blindness.
- Be cool and wear your shades. Sunglasses are a great fashion accessory, but their most important job is to protect your eyes from the sun’s ultraviolet rays.
- When purchasing sunglasses, look for ones that block out 99 to 100 percent of both UV-A and UV-B radiation.
- Give your eyes a rest. If you spend a lot of time at the computer or focusing on any one thing, you sometimes forget to blink and your eyes can get fatigued.
- Try the 20-20-20 rule: Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain.
- Clean your hands and your contact lenses–properly. To avoid the risk of infection, always wash your hands thoroughly before putting in or taking out your contact lenses. Make sure to disinfect contact lenses as instructed and replace them as appropriate.
- Practice workplace eye safety. Employers are required to provide a safe work environment. When protective eyewear is required as a part of your job, make a habit of wearing the appropriate type at all times and encourage your coworkers to do the same.
What is a comprehensive dilated eye exam ?
A comprehensive dilated eye exam is a painless procedure in which an eye care professional examines your eyes to look for common vision problems and eye diseases, many of which have no early warning signs. Regular comprehensive eye exams can help you protect your sight and make sure that you are seeing your best.
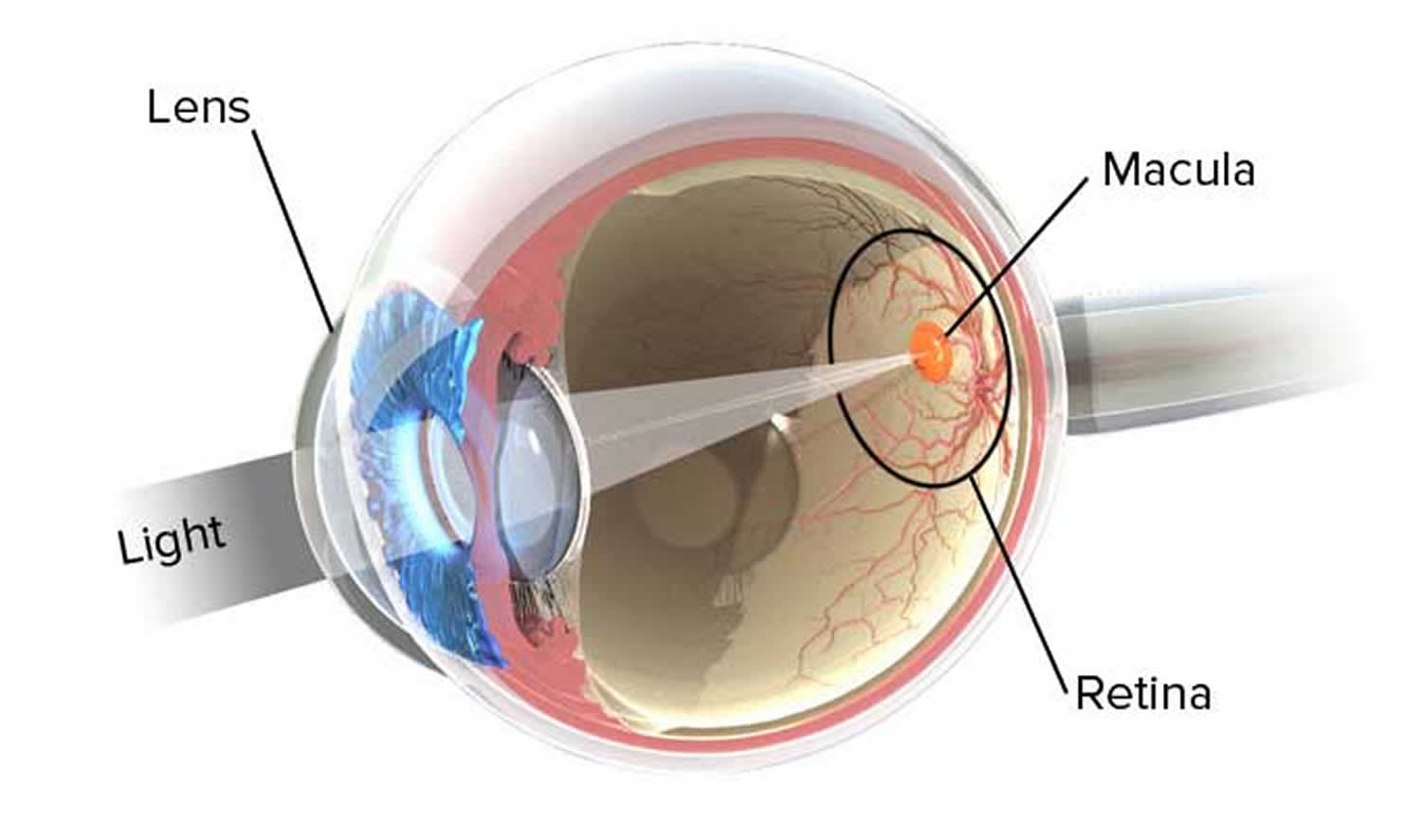
Figure 1. Eye anatomy
Figure 2. Normal eye refraction (perfect image on the Macula’s Fovea)
Refractive errors
Refractive errors occur when the shape of the eye prevents light from focusing directly on the retina. The length of the eyeball (longer or shorter), changes in the shape of the cornea, or aging of the lens can cause refractive errors. Refraction is the bending of light as it passes through one object to another. Vision occurs when light rays are bent (refracted) as they pass through the cornea and the lens. The light is then focused on the retina. The retina converts the light-rays into messages that are sent through the optic nerve to the brain. The brain interprets these messages into the images you see 3.
The most common vision problems are refractive errors, more commonly known as:
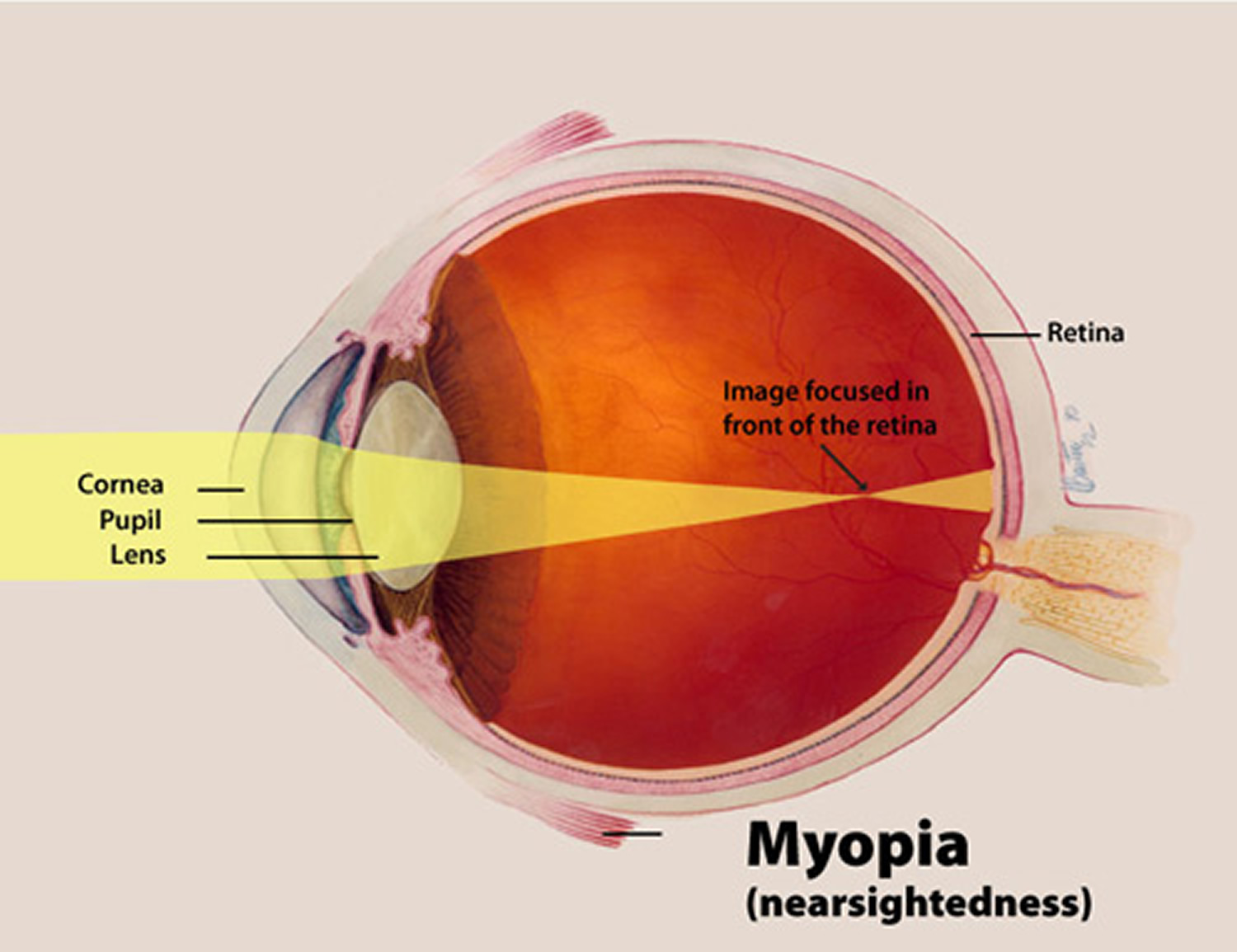
- Myopia or Nearsightedness, is a condition where objects up close appear clearly, while objects far away appear blurry. With myopia, light comes to focus in front of the retina instead of on the retina.
- Hyperopia or Farsightedness, is a common type of refractive error where distant objects may be seen more clearly than objects that are near. However, people experience hyperopia differently. Some people may not notice any problems with their vision, especially when they are young. For people with significant hyperopia, vision can be blurry for objects at any distance, near or far.
- Astigmatism is a condition in which the eye does not focus light evenly onto the retina, the light-sensitive tissue at the back of the eye. This can cause images to appear blurry and stretched out.
- Presbyopia is an age-related condition in which the ability to focus up close becomes more difficult. As the eye ages, the lens can no longer change shape enough to allow the eye to focus close objects clearly.
Myopia or Nearsightedness
Myopia, also known as nearsightedness, is a common type of refractive error where close objects appear clearly, but distant objects appear blurry 4.
When you look at an object, light rays reflect off that object and pass through the cornea and the lens of the eye, which bend (or refract) the light and focus it on the retina at the back of the eye. If you have perfect vision, the rays focus directly on the surface of the retina. But in a myopic eye, the eyeball is usually too long from front to back. This causes light rays to focus at a point in front of the retina, rather than directly on its surface. This makes distant objects blurry.
Myopia can also be the result of a cornea that is too curved for the length of the eyeball or a lens that is too thick. For some people, their myopia may be caused by a combination of problems in the cornea, lens, and length of the eyeball.
Figure 3. Nearsightedness (Myopia)
[Source 5]What are the symptoms of myopia ?
If you have myopia, you have trouble seeing things far away, but you can see nearby things clearly. This is why myopia is commonly called nearsightedness.
If you can see well enough to read what’s on your laptop or in a book, but you struggle to see what’s on the television or a movie screen, you may be nearsighted. Sometimes people with undiagnosed myopia will have headaches and eyestrain from struggling to clearly see things in the distance.
Why does the eyeball grow too long ?
What causes the eyeball to grow too long isn’t completely known, but researchers are exploring a number of factors. For many people, myopia appears to be an inherited condition – in other words, if you have a parent with myopia you are at higher risk for developing it. Researchers are also looking at the effects of sex, age, ethnicity, and environmental exposures – such as sunlight and the amount of time spent doing close-up work – on the development of myopia. More recently, scientists have been considering the influence of circadian rhythms (sometimes referred to as our biological or body clock), which regulate systems in the body according to the daily cycles of light and dark, as a factor in the development of myopia.
How common is myopia ?
Based on a study published in 2008 6, experts at National Institutes of Health estimate that at least 33 percent of Americans are nearsighted. According to a 2009 study 7, the number of Americans with myopia has increased significantly from the 1970s to the early 2000s. The prevalence of myopia has also been increasing in many other countries around the world. It is particularly prominent among school-aged children living in urban areas in some Asian countries. In the past, people thought children might become myopic from spending too much time reading and writing, which require close-up vision, or from reading in poorly lit rooms. Recent studies 8 suggest that the increase of myopia in children could be related to a decrease in the amount of time they spend outdoors.
How is myopia diagnosed ?
An eye care professional can diagnose myopia during an eye exam, which usually begins with a visual acuity test. This test uses a standardized chart or card with rows of letters that decrease in size from top to bottom. Covering one eye, you will be asked to read out loud the smallest line of letters that you can see. When done, you will test the other eye. If the vision test shows that you are nearsighted, your doctor will use a retinoscope to shine light into your eyes and observe the reflection off the retina to determine the amount of refractive error you have.
What kinds of treatments are available for myopia ?
The most common way to treat myopia is to prescribe eyeglasses or contact lenses. Refractive surgery, once the eyes have stopped growing, has become another option for many people.
To find out the amount of myopia you have, an eye care professional uses a device called a phoropter to place a series of lenses in front of your eyes until you are seeing clearly. The combination of the results from both eyes is written as a prescription that will correct your vision to make it as normal as possible.
Eyeglasses use curved lenses to refocus light rays onto the retina, instead of in front of it.
Contact lenses correct vision in the same way as eyeglasses, except they rest directly on the eye.
Refractive surgery changes the shape of the cornea to correct myopia. There are different types of refractive surgery, but the most common are LASIK (Laser-assisted in-situ keratomileusis) and PRK (Photorefractive keratectomy).
Laser-assisted in-situ keratomileusis (LASIK) removes tissue from the inner layers of the cornea. To do this, a section of the outer corneal surface is cut and folded back to expose the inner cornea. A laser removes a precise amount of tissue to reshape the cornea and then the flap of outer tissue is placed back in position to heal. The correction possible with LASIK is limited by the amount of corneal tissue that can be safely removed.
Photorefractive keratectomy (PRK) removes a thin layer of tissue from the surface of the cornea to change its shape. This allows light to focus more accurately on the retina. Like LASIK surgery, with PRK there is a limit to how much tissue can safely be removed and the amount of nearsightedness that can be corrected.
Many people will experience dry eye symptoms after refractive surgery and a small number may develop chronic dry eye syndrome. Some people may also develop vision symptoms such as double vision/ghosting, starbursts, glare, and halos, especially at night. Ask your eye doctor to discuss with you the risks and benefits of LASIK or PRK surgery before you undergo either procedure.
Phakic intraocular lenses (IOLs) are a new option for people who are very nearsighted or whose corneas are too thin to allow the use of laser procedures such as LASIK and PRK. Phakic lenses are surgically placed inside the eye.
What is high myopia ?
High myopia is a severe form of myopia in which the eyeball continues to grow and becomes very long from front to back. It can increase the risk for retinal detachment, early development of cataracts and glaucoma.
What is degenerative myopia ?
Degenerative myopia (also called pathological or malignant myopia) is a rare and mostly inherited type of myopia that begins in early childhood. In degenerative myopia, the eyeball elongates rapidly and causes severe myopia, usually by the teenage or early adult years. Degenerative myopia may also progress far into the adult years. People with the condition have a significantly increased risk of retinal detachment and other degenerative changes in the back of the eye, including choroid neovascularization (abnormal blood vessel growth), and glaucoma.
Hyperopia or Farsightedness
Hyperopia, also known as farsightedness, is a common type of refractive error where distant objects may be seen more clearly than objects that are near 9. However, people experience hyperopia differently. Some people may not notice any problems with their vision, especially when they are young. For people with significant hyperopia, vision can be blurry for objects at any distance, near or far.
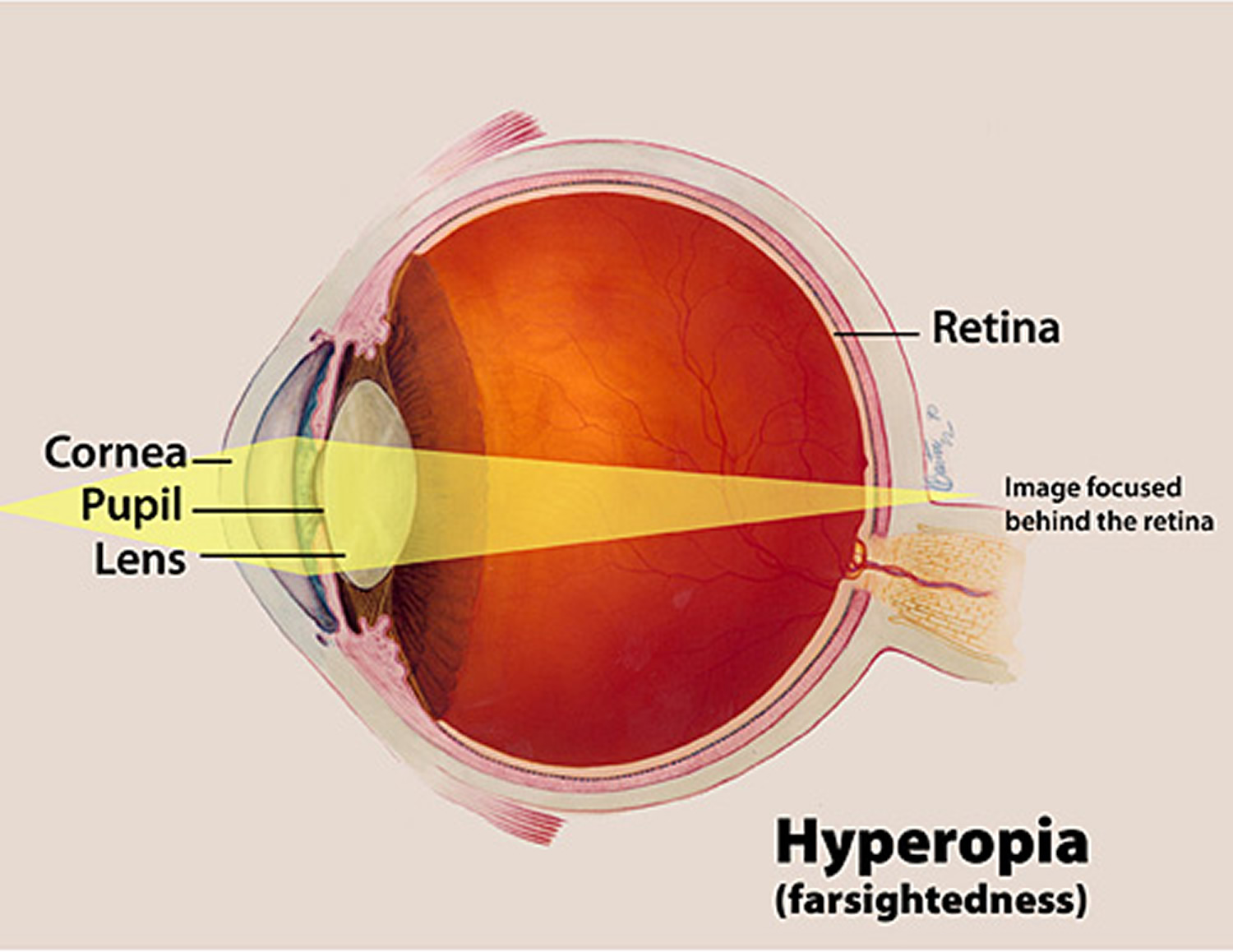
Figure 4. Farsightedness (Hyperopia)
[Source 10]How does hyperopia develop ?
Hyperopia develops in eyes that focus images behind the retina instead of on the retina, which can result in blurred vision. This occurs when the eyeball is too short, which prevents incoming light from focusing directly on the retina. It may also be caused by an abnormal shape of the cornea or lens.
Who is at risk for hyperopia ?
Hyperopia can affect both children and adults. It affects about 5 to 10 percent of Americans 9. People whose parents have hyperopia may also be more likely to get the condition.
What are the signs and symptoms of hyperopia ?
The symptoms of hyperopia vary from person to person. Your eye care professional can help you understand how the condition affects you.
Common signs and symptoms of hyperopia include:
- Headaches
- Eyestrain
- Squinting
- Blurry vision, especially for close objects.
How is hyperopia diagnosed ?
An eye care professional can diagnose hyperopia and other refractive errors during a comprehensive dilated eye examination. People with this condition often visit their eye care professional with complaints of visual discomfort or blurred vision.
How is hyperopia corrected ?
Hyperopia can be corrected with eyeglasses, contact lenses, or surgery 9.
Eyeglasses are the simplest and safest way to correct hyperopia. Your eye care professional can prescribe lenses that will help correct the problem and help you see your best.
Contact Lenses work by becoming the first refractive surface for light rays entering the eye, causing a more precise refraction or focus. In many cases, contact lenses provide clearer vision, a wider field of vision, and greater comfort. They are a safe and effective option if fitted and used properly. However, contact lenses are not right for everyone. Discuss this with your eye care professional.
Refractive Surgery aims to permanently change the shape of the cornea which will improve refractive vision. Surgery can decrease or eliminate dependency on wearing eyeglasses and contact lenses. There are many types of refractive surgeries and surgical options should be discussed with an eye care professional.
Astigmatism
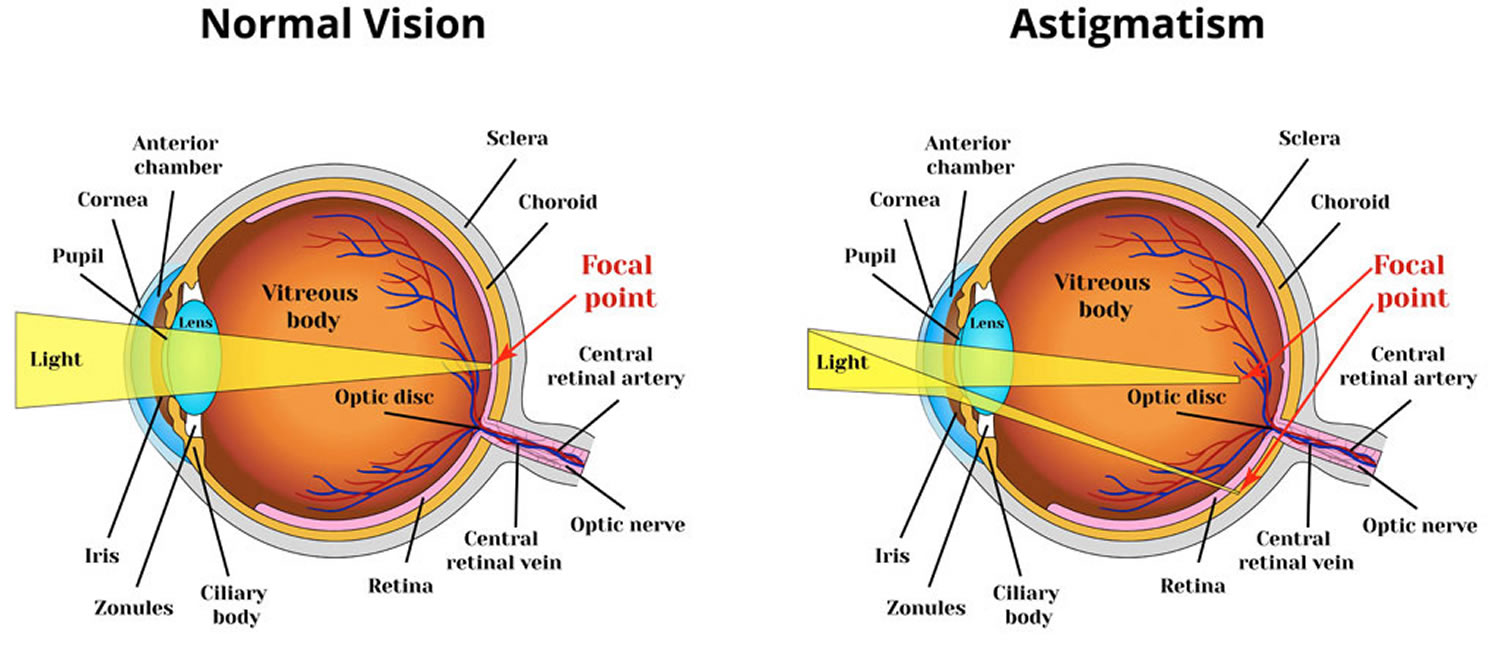
Astigmatism is a common type of refractive error. It is a condition in which the eye does not focus light evenly onto the retina, the light-sensitive tissue at the back of the eye 11.
Figure 5. In astigmatism, images focus in front of and beyond the retina, causing both close and distant objects to appear blurry.
How does astigmatism occur ?
Astigmatism occurs when light is bent differently depending on where it strikes the cornea and passes through the eyeball. The cornea of a normal eye is curved like a basketball, with the same degree of roundness in all areas. An eye with astigmatism has a cornea that is curved more like a football, with some areas that are steeper or more rounded than others. This can cause images to appear blurry and stretched out.
Who is at risk for astigmatism ?
Astigmatism can affect both children and adults. Some patients with slight astigmatism will not notice much change in their vision. It is important to have eye examinations at regular intervals in order to detect any astigmatism early on for children.
What are the signs and symptoms of astigmatism ?
Signs and symptoms include:
- Headaches
- Eyestrain
- Squinting
- Distorted or blurred vision at all distances
- Difficulty driving at night
If you experience any of these symptoms, visit your eye care professional. If you wear glasses or contact lenses and still have these issues, a new prescription might be needed.
How is astigmatism diagnosed ?
Astigmatism is usually found during a comprehensive dilated eye exam. Being aware of any changes in your vision is important. It can help in detecting any common vision problems. If you notice any changes in your vision, visit your eye care professional for a comprehensive dilated eye examination.
Can you have astigmatism and not know it ?
It is possible to have mild astigmatism and not know about it. This is especially true for children, who are not aware of their vision being other than normal. Some adults may also have mild astigmatism without any symptoms. It’s important to have comprehensive dilated eye exams to make sure you are seeing your best.
How is astigmatism corrected ?
Astigmatism can be corrected with eyeglasses, contact lenses, or surgery 11. Individual lifestyles affect the way astigmatism is treated.
Eyeglasses are the simplest and safest way to correct astigmatism. Your eye care professional will prescribe appropriate lenses to help you see as clearly as possible.
Contact Lenses work by becoming the first refractive surface for light rays entering the eye, causing a more precise refraction or focus. In many cases, contact lenses provide clearer vision, a wider field of vision, and greater comfort. They are a safe and effective option if fitted and used properly. However, contact lenses are not right for everyone. Discuss this with your eye care professional.
Refractive Surgery aims to change the shape of the cornea permanently. This change in eye shape restores the focusing power of the eye by allowing the light rays to focus precisely on the retina for improved vision. There are many types of refractive surgeries. Your eye care professional can help you decide if surgery is an option for you.
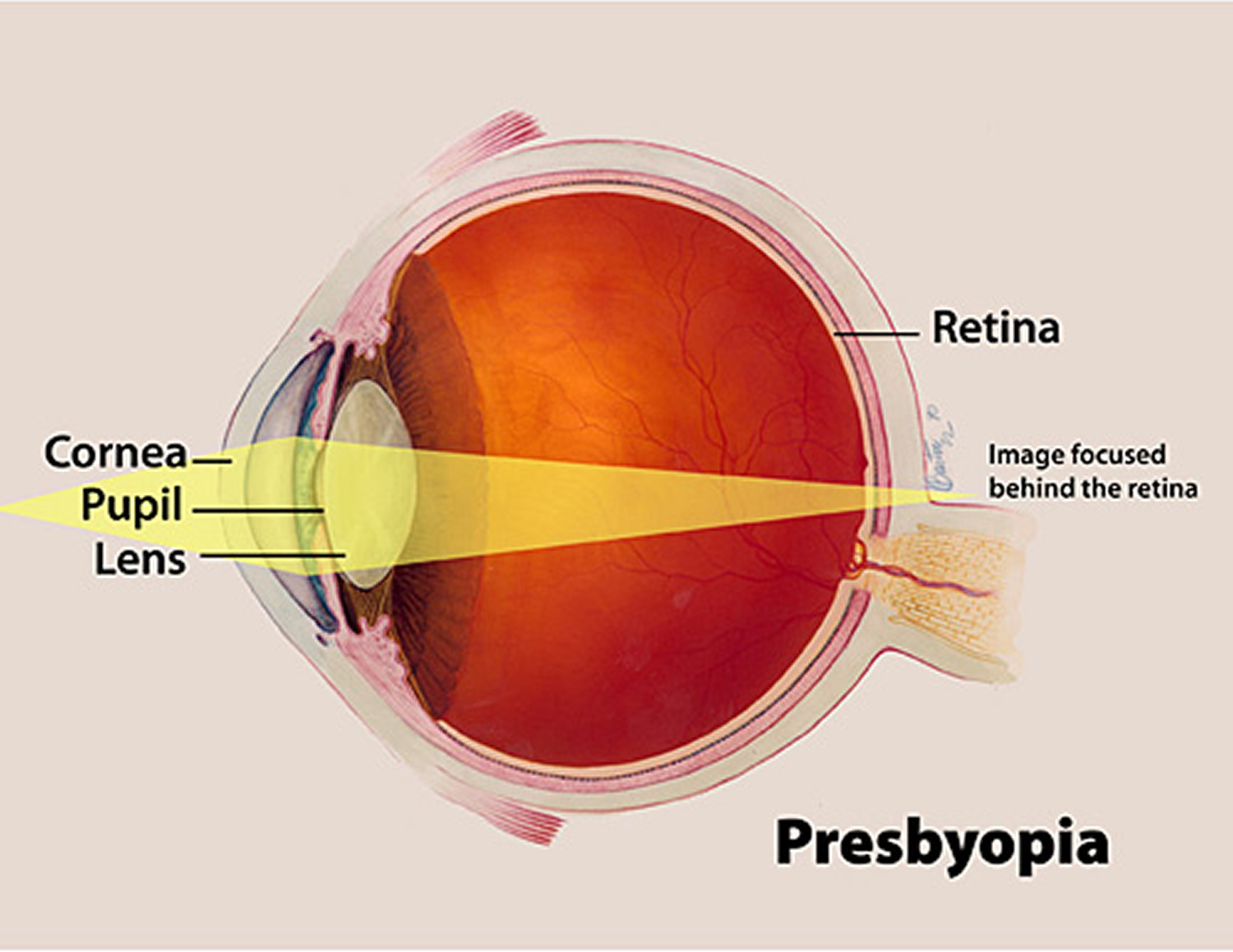
Presbyopia
Presbyopia is a common type of vision disorder that occurs as you age. It is often referred to as the aging eye condition. Presbyopia results in the inability to focus up close, a problem associated with refraction in the eye 12.
Figure 6. Presbyopia
[Source 12]Can you have presbyopia and another type of refractive error at the same time ?
Yes. It is common to have presbyopia and another type of refractive error at the same time. There are several other types of refractive errors: myopia (nearsightedness), hyperopia (farsightedness), and astigmatism 12.
An individual may have one type of refractive error in one eye and a different type of refractive error in the other.
How does presbyopia occur ?
Presbyopia happens naturally in people as they age. The eye is not able to focus light directly on to the retina due to the hardening of the natural lens. Aging also affects muscle fibers around the lens making it harder for the eye to focus on up close objects. The ineffective lens causes light to focus behind the retina, causing poor vision for objects that are up close.
When you are younger, the lens of the eye is soft and flexible, allowing the tiny muscles inside the eye to easily reshape the lens to focus on close and distant objects.
Who is at risk for presbyopia ?
Anyone over the age of 35 is at risk for developing presbyopia. Everyone experiences some loss of focusing power for near objects as they age, but some will notice this more than others.
What are the signs and symptoms of presbyopia ?
Some of the signs and symptoms of myopia include:
- Hard time reading small print
- Having to hold reading material farther than arm’s distance
- Problems seeing objects that are close to you
- Headaches
- Eyestrain
If you experience any of these symptoms you may want to visit an eye care professional for a comprehensive dilated eye examination. If you wear glasses or contact lenses and still have these issues, a new prescription might be needed.
How is presbyopia diagnosed ?
Presbyopia can be found during a comprehensive dilated eye exam. If you notice any changes in your vision, you should visit an eye care professional. Exams are recommended more often after the age 40 to check for age-related conditions.
How is presbyopia corrected ?
Eyeglasses are the simplest and safest means of correcting presbyopia. Eyeglasses for presbyopia have higher focusing power in the lower portion of the lens. This allows you to read through the lower portion of the lens and see properly at distant through the upper portion of the lens. It is also possible to purchase reading eyeglasses. These types of glasses do not require a prescription and can help with reading vision.
Degenerative eye disease
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) usually occurs in people who are age 50 and older 13. About 1,600,00 Americans aged 50 years and older have age-related macular degeneration. As people get older, the risk increases. Other risk factors include the following:
- Smoking. Research shows that smoking increases the risk of age-related macular degeneration two-fold.
- Race. Caucasians are much more likely to get age-related macular degeneration than people of African descent.
- Family history. People with a family history of age-related macular degeneration are at higher risk.
Age-related macular degeneration causes damage to the macula, a small spot near the center of the retina and the part of the eye needed for sharp, central vision, which lets us see objects that are straight ahead 14.
In some people, age-related macular degeneration advances so slowly that vision loss does not occur for a long time. In others, the disease progresses faster and may lead to a loss of vision in one or both eyes. As age-related macular degeneration progresses, a blurred area near the center of vision is a common symptom. Over time, the blurred area may grow larger or you may develop blank spots in your central vision. Objects also may not appear to be as bright as they used to be.
Age-related macular degeneration by itself does not lead to complete blindness, with no ability to see. However, the loss of central vision in age-related macular degeneration can interfere with simple everyday activities, such as the ability to see faces, drive, read, write, or do close work, such as cooking or fixing things around the house.
The Macula
The macula is made up of millions of light-sensing cells that provide sharp, central vision. It is the most sensitive part of the retina, which is located at the back of the eye. The retina turns light into electrical signals and then sends these electrical signals through the optic nerve to the brain, where they are translated into the images we see. When the macula is damaged, the center of your field of view may appear blurry, distorted, or dark.
Who is at risk ?
Age is a major risk factor for age-related macular degeneration. The disease is most likely to occur after age 60, but it can occur earlier. Other risk factors for age-related macular degeneration include:
- Smoking. Research shows that smoking doubles the risk of age-related macular degeneration.
- Race. AMD is more common among Caucasians than among African-Americans or Hispanics/Latinos.
- Family history and Genetics. People with a family history of age-related macular degeneration are at higher risk. At last count, researchers had identified nearly 20 genes that can affect the risk of developing age-related macular degeneration. Many more genetic risk factors are suspected. You may see offers for genetic testing for age-related macular degeneration. Because age-related macular degeneration is influenced by so many genes plus environmental factors such as smoking and nutrition, there are currently no genetic tests that can diagnose age-related macular degeneration, or predict with certainty who will develop it. The American Academy of Ophthalmology 15 currently recommends against routine genetic testing for AMD, and insurance generally does not cover such testing.
Does lifestyle make a difference ?
Researchers have found links between age-related macular degeneration and some lifestyle choices, such as smoking. You might be able to reduce your risk of age-related macular degeneration or slow its progression by making these healthy choices:
- Avoid smoking
- Exercise regularly
- Maintain normal blood pressure and cholesterol levels
- Eat a healthy diet rich in green, leafy vegetables and fish
The early and intermediate stages of age-related macular degeneration usually start without symptoms. Only a comprehensive dilated eye exam can detect age-related macular degeneration. The eye exam may include the following:
- Visual acuity test. This eye chart measures how well you see at distances.
- Dilated eye exam. Your eye care professional places drops in your eyes to widen or dilate the pupils. This provides a better view of the back of your eye. Using a special magnifying lens, he or she then looks at your retina and optic nerve for signs of AMD and other eye problems.
- Amsler grid. Your eye care professional also may ask you to look at an Amsler grid. Changes in your central vision may cause the lines in the grid to disappear or appear wavy, a sign of AMD.
- Fluorescein angiogram. In this test, which is performed by an ophthalmologist, a fluorescent dye is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your eye. This makes it possible to see leaking blood vessels, which occur in a severe, rapidly progressive type of AMD (see below). In rare cases, complications to the injection can arise, from nausea to more severe allergic reactions.
- Optical coherence tomography. You have probably heard of ultrasound, which uses sound waves to capture images of living tissues. OCT is similar except that it uses light waves, and can achieve very high-resolution images of any tissues that can be penetrated by light—such as the eyes. After your eyes are dilated, you’ll be asked to place your head on a chin rest and hold still for several seconds while the images are obtained. The light beam is painless.
During the exam, your eye care professional will look for drusen, which are yellow deposits beneath the retina. Most people develop some very small drusen as a normal part of aging. The presence of medium-to-large drusen may indicate that you have age-related macular degeneration.
Another sign of age-related macular degeneration is the appearance of pigmentary changes under the retina. In addition to the pigmented cells in the iris (the colored part of the eye), there are pigmented cells beneath the retina. As these cells break down and release their pigment, your eye care professional may see dark clumps of released pigment and later, areas that are less pigmented. These changes will not affect your eye color.
Questions to ask your eye care Professional
Below are a few questions you may want to ask your eye care professional to help you understand your diagnosis and treatment. If you do not understand your eye care professional’s responses, ask questions until you do understand.
- What is my diagnosis and how do you spell the name of the condition?
- Can my age-related macular degeneration be treated?
- How will this condition affect my vision now and in the future?
- What symptoms should I watch for and how should I notify you if they occur?
- Should I make lifestyle changes?
There are three stages of AMD defined in part by the size and number of drusen under the retina. It is possible to have age-related macular degeneration in one eye only, or to have one eye with a later stage of age-related macular degeneration than the other.
- Early age-related macular degeneration. Early AMD is diagnosed by the presence of medium-sized drusen, which are about the width of an average human hair. People with early age-related macular degeneration typically do not have vision loss.
- Intermediate age-related macular degeneration. People with intermediate age-related macular degeneration typically have large drusen, pigment changes in the retina, or both. Again, these changes can only be detected during an eye exam. Intermediate age-related macular degeneration may cause some vision loss, but most people will not experience any symptoms.
- Late age-related macular degeneration. In addition to drusen, people with late age-related macular degeneration have vision loss from damage to the macula. There are two types of late age-related macular degeneration:
- In geographic atrophy (also called dry age-related macular degeneration), there is a gradual breakdown of the light-sensitive cells in the macula that convey visual information to the brain, and of the supporting tissue beneath the macula. These changes cause vision loss.
- In neovascular age-related macular degeneration (also called wet age-related macular degeneration), abnormal blood vessels grow underneath the retina. (“Neovascular” literally means “new vessels.”) These vessels can leak fluid and blood, which may lead to swelling and damage of the macula. The damage may be rapid and severe, unlike the more gradual course of geographic atrophy. It is possible to have both geographic atrophy and neovascular age-related macular degeneration in the same eye, and either condition can appear first.
Age-related macular degeneration has few symptoms in the early stages, so it is important to have your eyes examined regularly. If you are at risk for age-related macular degeneration because of age, family history, lifestyle, or some combination of these factors, you should not wait to experience changes in vision before getting checked for age-related macular degeneration.
Not everyone with early age-related macular degeneration will develop late age-related macular degeneration. For people who have early age-related macular degeneration in one eye and no signs of age-related macular degeneration in the other eye, about five percent will develop advanced age-related macular degeneration after 10 years. For people who have early age-related macular degeneration in both eyes, about 14 percent will develop late age-related macular degeneration in at least one eye after 10 years. With prompt detection of age-related macular degeneration, there are steps you can take to further reduce your risk of vision loss from late age-related macular degeneration.
If you have late age-related macular degeneration in one eye only, you may not notice any changes in your overall vision. With the other eye seeing clearly, you may still be able to drive, read, and see fine details. However, having late age-related macular degeneration in one eye means you are at increased risk for late age-related macular degeneration in your other eye. If you notice distortion or blurred vision, even if it doesn’t have much effect on your daily life, consult an eye care professional.
- Early age-related macular degeneration
Currently, no treatment exists for early age-related macular degeneration, which in many people shows no symptoms or loss of vision. Your eye care professional may recommend that you get a comprehensive dilated eye exam at least once a year. The exam will help determine if your condition is advancing.
As for prevention, age-related macular degeneration occurs less often in people who exercise, avoid smoking, and eat nutritious foods including green leafy vegetables and fish. If you already have age-related macular degeneration, adopting some of these habits may help you keep your vision longer.
- Intermediate and late age-related macular degeneration
Researchers at the National Eye Institute tested whether taking nutritional supplements could protect against age-related macular degeneration in the Age-Related Eye Disease Studies (AREDS and AREDS2). They found that daily intake of certain high-dose vitamins and minerals can slow progression of the disease in people who have intermediate age-related macular degeneration, and those who have late age-related macular degeneration in one eye.
The first AREDS trial showed that a combination of vitamin C, vitamin E, beta-carotene, zinc, and copper can reduce the risk of late age-related macular degeneration by 25 percent. The AREDS2 trial tested whether this formulation could be improved by adding lutein, zeaxanthin or omega-3 fatty acids. Omega-3 fatty acids are nutrients enriched in fish oils. Lutein, zeaxanthin and beta-carotene all belong to the same family of vitamins, and are abundant in green leafy vegetables.
The AREDS2 trial found that adding lutein and zeaxanthin or omega-three fatty acids to the original AREDS formulation (with beta-carotene) had no overall effect on the risk of late age-related macular degeneration. However, the trial also found that replacing beta-carotene with a 5-to-1 mixture of lutein and zeaxanthin may help further reduce the risk of late age-related macular degeneration. Moreover, while beta-carotene has been linked to an increased risk of lung cancer in current and former smokers, lutein and zeaxanthin appear to be safe regardless of smoking status.
Here are the ingredients based on AREDS and AREDS2 research:
- 500 milligrams (mg) of vitamin C
- 400 international units of vitamin E
- 80 mg zinc as zinc oxide
- 2 mg copper as cupric oxide
- 10 mg lutein and 2 mg zeaxanthin
If you have intermediate or late age-related macular degeneration, you might benefit from taking supplements containing these ingredients. But first, be sure to review and compare the labels. Many supplements have different ingredients, or different doses, from those tested in the AREDS trials. Also, consult your doctor or eye care professional about which supplement, if any, is right for you. For example, if you smoke regularly, or used to, your doctor may recommend that you avoid supplements containing beta-carotene.
Even if you take a daily multivitamin, you should consider taking an AREDS supplement if you are at risk for late age-related macular degeneration. The formulations tested in the AREDS trials contain much higher doses of vitamins and minerals than what is found in multivitamins. Tell your doctor or eye care professional about any multivitamins you are taking when you are discussing possible AREDS formulations.
You may see claims that your specific genetic makeup (genotype) can influence how you will respond to AREDS supplements. Some recent studies have claimed that, depending on genotype, some patients will benefit from AREDS supplements and others could be harmed. These claims are based on a portion of data from the AREDS research. The National Eye Institute investigators have done comprehensive analyses of the complete AREDS data. Their findings to date indicate that AREDS supplements are beneficial for patients of all tested genotypes. Based on the overall data, the American Academy of Ophthalmology 15 does not support the use of genetic testing to guide treatment for AMD.
Finally, remember that the AREDS formulation is not a cure. It does not help people with early age-related macular degeneration, and will not restore vision already lost from age-related macular degeneration. But it may delay the onset of late age-related macular degeneration. It also may help slow vision loss in people who already have late age-related macular degeneration.
Neovascular age-related macular degeneration typically results in severe vision loss. However, eye care professionals can try different therapies to stop further vision loss. You should remember that the therapies described below are not a cure. The condition may progress even with treatment.
- Injections. One option to slow the progression of neovascular AMD is to inject drugs into the eye. With neovascular AMD, abnormally high levels of vascular endothelial growth factor (VEGF) are secreted in your eyes. VEGF is a protein that promotes the growth of new abnormal blood vessels. Anti-VEGF injection therapy blocks this growth. If you get this treatment, you may need multiple monthly injections. Before each injection, your eye will be numbed and cleaned with antiseptics. To further reduce the risk of infection, you may be prescribed antibiotic drops. A few different anti-VEGF drugs are available. They vary in cost and in how often they need to be injected, so you may wish to discuss these issues with your eye care professional.
- Photodynamic therapy. This technique involves laser treatment of select areas of the retina. First, a drug called verteporfin will be injected into a vein in your arm. The drug travels through the blood vessels in your body, and is absorbed by new, growing blood vessels. Your eye care professional then shines a laser beam into your eye to activate the drug in the new abnormal blood vessels, while sparing normal ones. Once activated, the drug closes off the new blood vessels, slows their growth, and slows the rate of vision loss. This procedure is less common than anti-VEGF injections, and is often used in combination with them for specific types of neovascular AMD.
- Laser surgery. Eye care professionals treat certain cases of neovascular AMD with laser surgery, though this is less common than other treatments. It involves aiming an intense “hot” laser at the abnormal blood vessels in your eyes to destroy them. This laser is not the same one used in photodynamic therapy which may be referred to as a “cold” laser. This treatment is more likely to be used when blood vessel growth is limited to a compact area in your eye, away from the center of the macula, that can be easily targeted with the laser. Even so, laser treatment also may destroy some surrounding healthy tissue. This often results in a small blind spot where the laser has scarred the retina. In some cases, vision immediately after the surgery may be worse than it was before. But the surgery may also help prevent more severe vision loss from occurring years later.
Loss of Vision
Coping with AMD and vision loss can be a traumatic experience. This is especially true if you have just begun to lose your vision or have low vision. Having low vision means that even with regular glasses, contact lenses, medicine, or surgery, you find everyday tasks difficult to do. Reading the mail, shopping, cooking, and writing can all seem challenging.
However, help is available. You may not be able to restore your vision, but low vision services can help you make the most of what is remaining. You can continue enjoying friends, family, hobbies, and other interests just as you always have. The key is to not delay use of these services.
What is vision rehabilitation ?
To cope with vision loss, you must first have an excellent support team. This team should include you, your primary eye care professional, and an optometrist or ophthalmologist specializing in low vision. Occupational therapists, orientation and mobility specialists, certified low vision therapists, counselors, and social workers are also available to help. Together, the low vision team can help you make the most of your remaining vision and maintain your independence.
Second, talk with your eye care professional about your vision problems. Ask about vision rehabilitation, even if your eye care professional says that “nothing more can be done for your vision.” Vision rehabilitation programs offer a wide range of services, including training for magnifying and adaptive devices, ways to complete daily living skills safely and independently, guidance on modifying your home, and information on where to locate resources and support to help you cope with your vision loss.
What are some low vision devices ?
Because low vision varies from person to person, specialists have different tools to help patients deal with vision loss. They include:
- Reading glasses with high-powered lenses
- Handheld magnifiers
- Video magnifiers
- Computers with large-print and speech-output systems
- Large-print reading materials
- Talking watches, clocks, and calculators
- Computer aids and other technologies, such as a closed-circuit television, which uses a camera and television to enlarge printed text
For some patients with end-stage AMD, an Implantable Miniature Telescope (IMT) may be an option. This FDA-approved device can help restore some lost vision by refocusing images onto a healthier part of the retina. After the surgery to implant the IMT, patients participate in an extensive vision rehabilitation program.
Keep in mind that low vision aids without proper diagnosis, evaluation, and training may not work for you. It is important that you work closely with your low vision team to get the best device or combination of aids to help improve your ability to see.
Charles Bonnet syndrome (Visual Hallucinations)
People with impaired vision sometimes see things that are not there, called visual hallucinations. They may see simple patterns of colors or shapes, or detailed pictures of people, animals, buildings, or landscapes. Sometimes these images fit logically into a visual scene, but they often do not.
This condition can be alarming, but don’t worry—it is not a sign of mental illness. It is called Charles Bonnet syndrome, and it is similar to what happens to some people who have lost an arm or leg. Even though the limb is gone, these people still feel their toes or fingers or experience itching. Similarly, when the brain loses input from the eyes, it may fill the void by generating visual images on its own.
Charles Bonnet syndrome is a common side effect of vision loss in people with AMD. However, it often goes away a year to 18 months after it begins. In the meantime, there are things you can do to reduce hallucinations. Many people find the hallucinations occur more frequently in evening or dim light. Turning on a light or television may help. It may also help to blink, close your eyes, or focus on a real object for a few moments.
Age-related macular degeneration and vision loss can profoundly affect your life. This is especially true if you lose your vision rapidly.
Even if you experience gradual vision loss, you may not be able to live your life the way you used to. You may need to cut back on working, volunteering, and recreational activities. Your relationships may change, and you may need more help from family and friends than you are used to. These changes can lead to feelings of loss, lowered self-esteem, isolation, and depression.
In addition to getting medical treatment for AMD, there are things you can do to cope:
Learn more about your vision loss.
- Visit a specialist in low vision and get devices and learning skills to help you with the tasks of everyday living.
- Try to stay positive. People who remain hopeful say they are better able to cope with AMD and vision loss.
- Stay engaged with family and friends.
- Seek a professional counselor or support group. Your doctor or eye care professional may be able to refer you to one.
Diabetic Eye Disease
Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of diabetes. People with diabetes are at risk for diabetic retinopathy, diabetic macular edema (DME), cataract, and glaucoma 16.
What is diabetic eye disease ?
Diabetic eye disease is a group of eye conditions that can affect people with diabetes.
- Diabetic retinopathy affects blood vessels in the light-sensitive tissue called the retina that lines the back of the eye. It is the most common cause of vision loss among people with diabetes and the leading cause of vision impairment and blindness among working-age adults.
- Diabetic macular edema. A consequence of diabetic retinopathy, diabetic macular edema is swelling in an area of the retina called the macula.
Diabetic eye disease also includes cataract and glaucoma:
- Cataract is a clouding of the eye’s lens. Adults with diabetes are 2-5 times more likely than those without diabetes to develop cataract. Cataract also tends to develop at an earlier age in people with diabetes.
- Glaucoma is a group of diseases that damage the eye’s optic nerve—the bundle of nerve fibers that connects the eye to the brain. Some types of glaucoma are associated with elevated pressure inside the eye. In adults, diabetes nearly doubles the risk of glaucoma.
All forms of diabetic eye disease have the potential to cause severe vision loss and blindness.
Diabetic Retinopathy
Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness among working-age (ages 20–74) Americans 17. It is caused by changes in the blood vessels of the retina 18.
In some people with diabetic retinopathy, blood vessels may swell and leak fluid. In other people, abnormal new blood vessels grow on the surface of the retina. The retina is the light-sensitive tissue at the back of the eye. A healthy retina is necessary for good vision.
If you have diabetic retinopathy, at first you may not notice changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
What causes diabetic retinopathy ?
Chronically high blood sugar from diabetes is associated with damage to the tiny blood vessels in the retina, leading to diabetic retinopathy. The retina detects light and converts it to signals sent through the optic nerve to the brain. Diabetic retinopathy can cause blood vessels in the retina to leak fluid or hemorrhage (bleed), distorting vision. In its most advanced stage, new abnormal blood vessels proliferate (increase in number) on the surface of the retina, which can lead to scarring and cell loss in the retina.
Diabetic retinopathy may progress through four stages:
- Mild nonproliferative retinopathy. Small areas of balloon-like swelling in the retina’s tiny blood vessels, called microaneurysms, occur at this earliest stage of the disease. These microaneurysms may leak fluid into the retina.
- Moderate nonproliferative retinopathy. As the disease progresses, blood vessels that nourish the retina may swell and distort. They may also lose their ability to transport blood. Both conditions cause characteristic changes to the appearance of the retina and may contribute to diabetic macular edema.
- Severe nonproliferative retinopathy. Many more blood vessels are blocked, depriving blood supply to areas of the retina. These areas secrete growth factors that signal the retina to grow new blood vessels.
- Proliferative diabetic retinopathy. At this advanced stage, growth factors secreted by the retina trigger the proliferation of new blood vessels, which grow along the inside surface of the retina and into the vitreous gel, the fluid that fills the eye. The new blood vessels are fragile, which makes them more likely to leak and bleed. Accompanying scar tissue can contract and cause retinal detachment—the pulling away of the retina from underlying tissue, like wallpaper peeling away from a wall. Retinal detachment can lead to permanent vision loss.
What is diabetic macular edema ?
Diabetic macular edema is the build-up of fluid (edema) in a region of the retina called the macula. The macula is important for the sharp, straight-ahead vision that is used for reading, recognizing faces, and driving. Diabetic macular edema is the most common cause of vision loss among people with diabetic retinopathy. About half of all people with diabetic retinopathy will develop diabetic macular edema. Although it is more likely to occur as diabetic retinopathy worsens, diabetic macular edema can happen at any stage of the disease.
Who is at risk for diabetic retinopathy ?
People with all types of diabetes (type 1, type 2, and gestational) are at risk for diabetic retinopathy. Risk increases the longer a person has diabetes. Between 40 and 45 percent of Americans diagnosed with diabetes have some stage of diabetic retinopathy, although only about half are aware of it. Women who develop or have diabetes during pregnancy may have rapid onset or worsening of diabetic retinopathy.
What are the symptoms of diabetic retinopathy and diabetic macular edema ?
The early stages of diabetic retinopathy usually have no symptoms. The disease often progresses unnoticed until it affects vision. Bleeding from abnormal retinal blood vessels can cause the appearance of “floating” spots. These spots sometimes clear on their own. But without prompt treatment, bleeding often recurs, increasing the risk of permanent vision loss. If diabetic macular edema occurs, it can cause blurred vision.
How are diabetic retinopathy and diabetic macular edema detected ?
Diabetic retinopathy and diabetic macular edema are detected during a comprehensive dilated eye exam that includes:
- Visual acuity testing. This eye chart test measures a person’s ability to see at various distances.
- Tonometry. This test measures pressure inside the eye.
- Pupil dilation. Drops placed on the eye’s surface dilate (widen) the pupil, allowing a physician to examine the retina and optic nerve.
- Optical coherence tomography (OCT). This technique is similar to ultrasound but uses light waves instead of sound waves to capture images of tissues inside the body. OCT provides detailed images of tissues that can be penetrated by light, such as the eye.
A comprehensive dilated eye exam allows the doctor to check the retina for:
- Changes to blood vessels
- Leaking blood vessels or warning signs of leaky blood vessels, such as fatty deposits
- Swelling of the macula (diabetic macular edema)
- Changes in the lens
- Damage to nerve tissue
If diabetic macular edema or severe diabetic retinopathy is suspected, a fluorescein angiogram may be used to look for damaged or leaky blood vessels. In this test, a fluorescent dye is injected into the bloodstream, often into an arm vein. Pictures of the retinal blood vessels are taken as the dye reaches the eye.
How can people with diabetes protect their vision ?
Vision lost to diabetic retinopathy is sometimes irreversible. However, early detection and treatment can reduce the risk of blindness by 95 percent. Because diabetic retinopathy often lacks early symptoms, people with diabetes should get a comprehensive dilated eye exam at least once a year. People with diabetic retinopathy may need eye exams more frequently. Women with diabetes who become pregnant should have a comprehensive dilated eye exam as soon as possible. Additional exams during pregnancy may be needed.
Studies such as the Diabetes Control and Complications Trial (DCCT) have shown that controlling diabetes slows the onset and worsening of diabetic retinopathy. DCCT study participants who kept their blood glucose level as close to normal as possible were significantly less likely than those without optimal glucose control to develop diabetic retinopathy, as well as kidney and nerve diseases. Other trials have shown that controlling elevated blood pressure and cholesterol can reduce the risk of vision loss among people with diabetes.
Treatment for diabetic retinopathy is often delayed until it starts to progress to proliferative diabetic retinopathy, or when diabetic macular edema occurs. Comprehensive dilated eye exams are needed more frequently as diabetic retinopathy becomes more severe. People with severe nonproliferative diabetic retinopathy have a high risk of developing proliferative diabetic retinopathy and may need a comprehensive dilated eye exam as often as every 2 to 4 months.
How is diabetic macular edema treated ?
Diabetic macular edema can be treated with several therapies that may be used alone or in combination.
Anti-VEGF Injection Therapy. Anti-VEGF drugs are injected into the vitreous gel to block a protein called vascular endothelial growth factor (VEGF), which can stimulate abnormal blood vessels to grow and leak fluid. Blocking VEGF can reverse abnormal blood vessel growth and decrease fluid in the retina. Available anti-VEGF drugs include Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (aflibercept). Lucentis and Eylea are approved by the U.S. Food and Drug Administration (FDA) for treating diabetic macular edema. Avastin was approved by the FDA to treat cancer, but is commonly used to treat eye conditions, including diabetic macular edema.
Diabetic Retinopathy Clinical Research Network compared Avastin, Lucentis, and Eylea in a clinical trial. The study found all three drugs to be safe and effective for treating most people with diabetic macular edema. Patients who started the trial with 20/40 or better vision experienced similar improvements in vision no matter which of the three drugs they were given. However, patients who started the trial with 20/50 or worse vision had greater improvements in vision with Eylea.
Most people require monthly anti-VEGF injections for the first six months of treatment. Thereafter, injections are needed less often: typically three to four during the second six months of treatment, about four during the second year of treatment, two in the third year, one in the fourth year, and none in the fifth year. Dilated eye exams may be needed less often as the disease stabilizes.
Avastin, Lucentis, and Eylea vary in cost and in how often they need to be injected, so patients may wish to discuss these issues with an eye care professional.
Focal/grid macular laser surgery. In focal/grid macular laser surgery, a few to hundreds of small laser burns are made to leaking blood vessels in areas of edema near the center of the macula. Laser burns for diabetic macular edema slow the leakage of fluid, reducing swelling in the retina. The procedure is usually completed in one session, but some people may need more than one treatment. Focal/grid laser is sometimes applied before anti-VEGF injections, sometimes on the same day or a few days after an anti-VEGF injection, and sometimes only when diabetic macular edema fails to improve adequately after six months of anti-VEGF therapy.
Corticosteroids. Corticosteroids, either injected or implanted into the eye, may be used alone or in combination with other drugs or laser surgery to treat diabetic macular edema. The Ozurdex (dexamethasone) implant is for short-term use, while the Iluvien (fluocinolone acetonide) implant is longer lasting. Both are biodegradable and release a sustained dose of corticosteroids to suppress diabetic macular edema. Corticosteroid use in the eye increases the risk of cataract and glaucoma. DME patients who use corticosteroids should be monitored for increased pressure in the eye and glaucoma.
How is proliferative diabetic retinopathy treated ?
For decades, proliferative diabetic retinopathy has been treated with scatter laser surgery, sometimes called panretinal laser surgery or panretinal photocoagulation. Treatment involves making 1,000 to 2,000 tiny laser burns in areas of the retina away from the macula. These laser burns are intended to cause abnormal blood vessels to shrink. Although treatment can be completed in one session, two or more sessions are sometimes required. While it can preserve central vision, scatter laser surgery may cause some loss of side (peripheral), color, and night vision. Scatter laser surgery works best before new, fragile blood vessels have started to bleed. Recent studies have shown that anti-VEGF treatment not only is effective for treating diabetic macular edema, but is also effective for slowing progression of diabetic retinopathy, including proliferative diabetic retinopathy, so anti-VEGF is increasingly used as a first-line treatment for proliferative diabetic retinopathy.
What is a vitrectomy ?
A vitrectomy is the surgical removal of the vitreous gel in the center of the eye. The procedure is used to treat severe bleeding into the vitreous, and is performed under local or general anesthesia. Ports (temporary water-tight openings) are placed in the eye to allow the surgeon to insert and remove instruments, such as a tiny light or a small vacuum called a vitrector. A clear salt solution is gently pumped into the eye through one of the ports to maintain eye pressure during surgery and to replace the removed vitreous. The same instruments used during vitrectomy also may be used to remove scar tissue or to repair a detached retina.
Vitrectomy may be performed as an outpatient procedure or as an inpatient procedure, usually requiring a single overnight stay in the hospital. After treatment, the eye may be covered with a patch for days to weeks and may be red and sore. Drops may be applied to the eye to reduce inflammation and the risk of infection. If both eyes require vitrectomy, the second eye usually will be treated after the first eye has recovered.
What if treatment doesn’t improve vision ?
An eye care professional can help locate and make referrals to low vision and rehabilitation services and suggest devices that may help make the most of remaining vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairment. A nearby school of medicine or optometry also may provide low vision and rehabilitation services.
Cataract
A cataract is a clouding of the lens in the eye that affects vision 19. Cataracts are a major cause of vision loss. Among Americans aged 40 years and older, 20.5 million, have cataracts 17. Cataract removal surgery can restore vision, and this surgery is highly cost-effective; however, among African Americans, unoperated senile cataracts remain a major cause of blindness. Some possible risk factors other than age could be diabetes, smoking, and prolonged exposure to sunlight.
Most cataracts are related to aging. Cataracts are very common in older people. By age 80, more than half of all Americans either have a cataract or have had cataract surgery.
A cataract can occur in either or both eyes. It cannot spread from one eye to the other.
The lens lies behind the iris and the pupil. It works much like a camera lens. It focuses light onto the retina at the back of the eye, where an image is recorded. The lens also adjusts the eye’s focus, letting us see things clearly both up close and far away. The lens is made of mostly water and protein. The protein is arranged in a precise way that keeps the lens clear and lets light pass through it.
But as we age, some of the protein may clump together and start to cloud a small area of the lens. This is a cataract. Over time, the cataract may grow larger and cloud more of the lens, making it harder to see.
Smoking and diabetes contribute to the development of cataract. Or, it may be that the protein in the lens just changes from the wear and tear it takes over the years.
What causes cataracts ?
The lens lies behind the iris and the pupil. It works much like a camera lens. It focuses light onto the retina at the back of the eye, where an image is recorded. The lens also adjusts the eye’s focus, letting us see things clearly both up close and far away. The lens is made of mostly water and protein. The protein is arranged in a precise way that keeps the lens clear and lets light pass through it.
But as we age, some of the protein may clump together and start to cloud a small area of the lens. This is a cataract. Over time, the cataract may grow larger and cloud more of the lens, making it harder to see.
Researchers suspect that there are several causes of cataract, such as smoking and diabetes. Or, it may be that the protein in the lens just changes from the wear and tear it takes over the years.
How do cataracts affect vision ?
Age-related cataracts can affect your vision in two ways:
Clumps of protein reduce the sharpness of the image reaching the retina. The lens consists mostly of water and protein. When the protein clumps up, it clouds the lens and reduces the light that reaches the retina. The clouding may become severe enough to cause blurred vision. Most age-related cataracts develop from protein clumpings. When a cataract is small, the cloudiness affects only a small part of the lens. You may not notice any changes in your vision. Cataracts tend to “grow” slowly, so vision gets worse gradually. Over time, the cloudy area in the lens may get larger, and the cataract may increase in size. Seeing may become more difficult. Your vision may get duller or blurrier.
The clear lens slowly changes to a yellowish/brownish color, adding a brownish tint to vision. As the clear lens slowly colors with age, your vision gradually may acquire a brownish shade. At first, the amount of tinting may be small and may not cause a vision problem. Over time, increased tinting may make it more difficult to read and perform other routine activities. This gradual change in the amount of tinting does not affect the sharpness of the image transmitted to the retina. If you have advanced lens discoloration, you may not be able to identify blues and purples. You may be wearing what you believe to be a pair of black socks, only to find out from friends that you are wearing purple socks.
When are you most likely to have a cataract ?
The term “age-related” is a little misleading. You don’t have to be a senior citizen to get this type of cataract. In fact, people can have an age-related cataract in their 40s and 50s. But during middle age, most cataracts are small and do not affect vision. It is after age 60 that most cataracts cause problems with a person’s vision.
Who is at risk for cataract ?
The risk of cataract increases as you get older. Other risk factors for cataract include:
- Certain diseases (for example, diabetes).
- Personal behavior (smoking, alcohol use).
- The environment (prolonged exposure to ultraviolet sunlight).
What are the symptoms of a cataract ?
The most common symptoms of a cataract are:
- Cloudy or blurry vision.
- Colors seem faded.
- Glare. Headlights, lamps, or sunlight may appear too bright. A halo may appear around lights.
- Poor night vision.
- Double vision or multiple images in one eye. (This symptom may clear as the cataract gets larger.)
- Frequent prescription changes in your eyeglasses or contact lenses.
These symptoms also can be a sign of other eye problems. If you have any of these symptoms, check with your eye care professional.
Are there different types of cataract ?
Yes. Although most cataracts are related to aging, there are other types of cataract:
- Secondary cataract. Cataracts can form after surgery for other eye problems, such as glaucoma. Cataracts also can develop in people who have other health problems, such as diabetes. Cataracts are sometimes linked to steroid use.
- Traumatic cataract. Cataracts can develop after an eye injury, sometimes years later.
- Congenital cataract. Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may be so small that they do not affect vision. If they do, the lenses may need to be removed.
- Radiation cataract. Cataracts can develop after exposure to some types of radiation.
How is a cataract detected ?
Cataract is detected through a comprehensive eye exam that includes:
- Visual acuity test. This eye chart test measures how well you see at various distances.
- Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry. An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
Your eye care professional also may do other tests to learn more about the structure and health of your eye.
How is a cataract treated ?
The symptoms of early cataract may be improved with new eyeglasses, brighter lighting, anti-glare sunglasses, or magnifying lenses. If these measures do not help, surgery is the only effective treatment. Surgery involves removing the cloudy lens and replacing it with an artificial lens.
A cataract needs to be removed only when vision loss interferes with your everyday activities, such as driving, reading, or watching TV. You and your eye care professional can make this decision together. Once you understand the benefits and risks of surgery, you can make an informed decision about whether cataract surgery is right for you. In most cases, delaying cataract surgery will not cause long-term damage to your eye or make the surgery more difficult. You do not have to rush into surgery.
Sometimes a cataract should be removed even if it does not cause problems with your vision. For example, a cataract should be removed if it prevents examination or treatment of another eye problem, such as age-related macular degeneration or diabetic retinopathy.
If you choose surgery, your eye care professional may refer you to a specialist to remove the cataract.
If you have cataracts in both eyes that require surgery, the surgery will be performed on each eye at separate times, usually four weeks apart.
Is cataract surgery effective?
Cataract removal is one of the most common operations performed in the United States. It also is one of the safest and most effective types of surgery. In about 90 percent of cases, people who have cataract surgery have better vision afterward.
What are the risks of cataract surgery ?
As with any surgery, cataract surgery poses risks, such as infection and bleeding. Before cataract surgery, your doctor may ask you to temporarily stop taking certain medications that increase the risk of bleeding during surgery. After surgery, you must keep your eye clean, wash your hands before touching your eye, and use the prescribed medications to help minimize the risk of infection. Serious infection can result in loss of vision.
Cataract surgery slightly increases your risk of retinal detachment. Other eye disorders, such as high myopia (nearsightedness), can further increase your risk of retinal detachment after cataract surgery. One sign of a retinal detachment is a sudden increase in flashes or floaters. Floaters are little “cobwebs” or specks that seem to float about in your field of vision. If you notice a sudden increase in floaters or flashes, see an eye care professional immediately. A retinal detachment is a medical emergency. If necessary, go to an emergency service or hospital. Your eye must be examined by an eye surgeon as soon as possible. A retinal detachment causes no pain. Early treatment for retinal detachment often can prevent permanent loss of vision. The sooner you get treatment, the more likely you will regain good vision. Even if you are treated promptly, some vision may be lost.
Talk to your eye care professional about these risks. Make sure cataract surgery is right for you.
What if you have other eye conditions and need cataract surgery ?
Many people who need cataract surgery also have other eye conditions, such as age-related macular degeneration or glaucoma. If you have other eye conditions in addition to cataract, talk with your doctor. Learn about the risks, benefits, alternatives, and expected results of cataract surgery.
What happens before surgery ?
A week or two before surgery, your doctor will do some tests. These tests may include measuring the curve of the cornea and the size and shape of your eye. This information helps your doctor choose the right type of intraocular lens (IOL).
You may be asked not to eat or drink anything 12 hours before your surgery.
What happens during surgery ?
At the hospital or eye clinic, drops will be put into your eye to dilate the pupil. The area around your eye will be washed and cleansed.
The operation usually lasts less than one hour and is almost painless. Many people choose to stay awake during surgery. Others may need to be put to sleep for a short time. If you are awake, you will have an anesthetic to numb the nerves in and around your eye.
After the operation, a patch may be placed over your eye. You will rest for a while. Your medical team will watch for any problems, such as bleeding. Most people who have cataract surgery can go home the same day. You will need someone to drive you home.
What happens after surgery ?
Itching and mild discomfort are normal after cataract surgery. Some fluid discharge is also common. Your eye may be sensitive to light and touch. If you have discomfort, your doctor can suggest treatment. After one or two days, moderate discomfort should disappear.
For a few weeks after surgery, your doctor may ask you to use eyedrops to help healing and decrease the risk of infection. Ask your doctor about how to use your eyedrops, how often to use them, and what effects they can have. You will need to wear an eye shield or eyeglasses to help protect your eye. Avoid rubbing or pressing on your eye.
When you are home, try not to bend from the waist to pick up objects on the floor. Do not lift any heavy objects. You can walk, climb stairs, and do light household chores.
In most cases, healing will be complete within eight weeks. Your doctor will schedule exams to check on your progress.
Can problems develop after surgery ?
Problems after surgery are rare, but they can occur. These problems can include infection, bleeding, inflammation (pain, redness, swelling), loss of vision, double vision, and high or low eye pressure. With prompt medical attention, these problems can usually be treated successfully.
Sometimes the eye tissue that encloses the IOL becomes cloudy and may blur your vision. This condition is called an after-cataract. An after-cataract can develop months or years after cataract surgery.
An after-cataract is treated with a laser. Your doctor uses a laser to make a tiny hole in the eye tissue behind the lens to let light pass through. This outpatient procedure is called a YAG laser capsulotomy. It is painless and rarely results in increased eye pressure or other eye problems. As a precaution, your doctor may give you eyedrops to lower your eye pressure before or after the procedure.
When will your vision be normal again ?
You can return quickly to many everyday activities, but your vision may be blurry. The healing eye needs time to adjust so that it can focus properly with the other eye, especially if the other eye has a cataract. Ask your doctor when you can resume driving.
If you received an IOL, you may notice that colors are very bright. The IOL is clear, unlike your natural lens that may have had a yellowish/brownish tint. Within a few months after receiving an IOL, you will become used to improved color vision. Also, when your eye heals, you may need new glasses or contact lenses.
What can you do if you already have lost some vision from cataract ?
If you have lost some vision, speak with your surgeon about options that may help you make the most of your remaining vision.
What can you do to protect your vision ?
Wearing sunglasses and a hat with a brim to block ultraviolet sunlight may help to delay cataract. If you smoke, stop. Researchers also believe good nutrition can help reduce the risk of age-related cataract. They recommend eating green leafy vegetables, fruit, and other foods with antioxidants.
If you are age 60 or older, you should have a comprehensive dilated eye exam at least once every two years. In addition to cataract, your eye care professional can check for signs of age-related macular degeneration, glaucoma, and other vision disorders. Early treatment for many eye diseases may save your sight.
Glaucoma
Glaucoma is a group of diseases that can damage the eye’s optic nerve and result in vision loss and blindness 20. It usually happens when fluid builds up in the front part of your eye. That extra fluid increases the pressure in your eye, damaging the optic nerve. Open-angle glaucoma, is the most common form of the disease.
How does the optic nerve get damaged by open-angle glaucoma ?
Several large studies have shown that eye pressure is a major risk factor for optic nerve damage. In the front of the eye is a space called the anterior chamber. A clear fluid flows continuously in and out of the chamber and nourishes nearby tissues. The fluid leaves the chamber at the open angle where the cornea and iris meet. When the fluid reaches the angle, it flows through a spongy meshwork, like a drain, and leaves the eye.
In open-angle glaucoma, even though the drainage angle is “open”, the fluid passes too slowly through the meshwork drain. Since the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma-and vision loss—may result. That’s why controlling pressure inside the eye is important.
Another risk factor for optic nerve damage relates to blood pressure. Thus, it is important to also make sure that your blood pressure is at a proper level for your body by working with your medical doctor.
Figure 7. Flow and absorption of fluid in the front of the eye
[Source 20]Can you develop glaucoma if you have increased eye pressure ?
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher levels of eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important. It can help your eye care professional determine what level of eye pressure is normal for you.
Can you develop glaucoma without an increase in your eye pressure ?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is a type of open-angle glaucoma.
Who is at risk for open-angle glaucoma ?
Anyone can develop glaucoma. Some people, listed below, are at higher risk than others:
- African Americans over age 40
- Everyone over age 60, especially Mexican Americans
- People with a family history of glaucoma
A comprehensive dilated eye exam can reveal more risk factors, such as high eye pressure, thinness of the cornea, and abnormal optic nerve anatomy. In some people with certain combinations of these high-risk factors, medicines in the form of eyedrops reduce the risk of developing glaucoma by about half.
Glaucoma Symptoms
At first, open-angle glaucoma has no symptoms. It causes no pain. Vision stays normal. Glaucoma can develop in one or both eyes.
Without treatment, people with glaucoma will slowly lose their peripheral (side) vision. As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. They seem to be looking through a tunnel. Over time, straight-ahead (central) vision may decrease until no vision remains.
How is glaucoma detected ?
Glaucoma is detected through a comprehensive dilated eye exam that includes the following:
- Visual acuity test. This eye chart test measures how well you see at various distances.
- Visual field test. This test measures your peripheral (side vision). It helps your eye care professional tell if you have lost peripheral vision, a sign of glaucoma.
- Dilated eye exam. In this exam, drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry is the measurement of pressure inside the eye by using an instrument called a tonometer. Numbing drops may be applied to your eye for this test. A tonometer measures pressure inside the eye to detect glaucoma.
- Pachymetry is the measurement of the thickness of your cornea. Your eye care professional applies a numbing drop to your eye and uses an ultrasonic wave instrument to measure the thickness of your cornea.
Can glaucoma be cured ?
No. There is no cure for glaucoma. Vision lost from the disease cannot be restored.
Glaucoma Treatments
Immediate treatment for early-stage, open-angle glaucoma can delay progression of the disease. That’s why early diagnosis is very important.
Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma.
Medicines
Medicines, in the form of eyedrops or pills, are the most common early treatment for glaucoma. Taken regularly, these eyedrops lower eye pressure. Some medicines cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye.
Before you begin glaucoma treatment, tell your eye care professional about other medicines and supplements that you are taking. Sometimes the drops can interfere with the way other medicines work.
Glaucoma medicines need to be taken regularly as directed by your eye care professional. Most people have no problems. However, some medicines can cause headaches or other side effects. For example, drops may cause stinging, burning, and redness in the eyes.
Many medicines are available to treat glaucoma. If you have problems with one medicine, tell your eye care professional. Treatment with a different dose or a new medicine may be possible.
Because glaucoma often has no symptoms, people may be tempted to stop taking, or may forget to take, their medicine. You need to use the drops or pills as long as they help control your eye pressure. Regular use is very important.
Make sure your eye care professional shows you how to put the drops into your eye.
Laser trabeculoplasty
Laser trabeculoplasty helps fluid drain out of the eye. Your doctor may suggest this step at any time. In many cases, you will need to keep taking glaucoma medicines after this procedure.
Laser trabeculoplasty is performed in your doctor’s office or eye clinic. Before the surgery, numbing drops are applied to your eye. As you sit facing the laser machine, your doctor holds a special lens to your eye. A high-intensity beam of light is aimed through the lens and reflected onto the meshwork inside your eye. You may see flashes of bright green or red light. The laser makes several evenly spaced burns that stretch the drainage holes in the meshwork. This allows the fluid to drain better.
Like any surgery, laser surgery can cause side effects, such as inflammation. Your doctor may give you some drops to take home for any soreness or inflammation inside the eye. You will need to make several follow-up visits to have your eye pressure and eye monitored.
If you have glaucoma in both eyes, usually only one eye will be treated at a time. Laser treatments for each eye will be scheduled several days to several weeks apart.
Studies show that laser surgery can be very good at reducing the pressure in some patients. However, its effects can wear off over time. Your doctor may suggest further treatment.
Conventional surgery
Conventional surgery makes a new opening for the fluid to leave the eye. Your doctor may suggest this treatment at any time. Conventional surgery often is done after medicines and laser surgery have failed to control pressure.
Conventional surgery, called trabeculectomy, is performed in an operating room. Before the surgery, you are given medicine to help you relax. Your doctor makes small injections around the eye to numb it. A small piece of tissue is removed to create a new channel for the fluid to drain from the eye. This fluid will drain between the eye tissue layers and create a blister-like “filtration bleb.”
For several weeks after the surgery, you must put drops in the eye to fight infection and inflammation. These drops will be different from those you may have been using before surgery.
Conventional surgery is performed on one eye at a time. Usually the operations are four to six weeks apart.
Conventional surgery is about 60 to 80 percent effective at lowering eye pressure. If the new drainage opening narrows, a second operation may be needed. Conventional surgery works best if you have not had previous eye surgery, such as a cataract operation.
Sometimes after conventional surgery, your vision may not be as good as it was before conventional surgery. Conventional surgery can cause side effects, including cataract, problems with the cornea, inflammation, infection inside the eye, or low eye pressure problems. If you have any of these problems, tell your doctor so a treatment plan can be developed.
Figure 8. Conventional surgery for glaucoma
[Source 20]What are some other forms of glaucoma and how are they treated ?
Open-angle glaucoma is the most common form. Some people have other types of the disease.
In low-tension or normal-tension glaucoma, optic nerve damage and narrowed side vision occur in people with normal eye pressure. Lowering eye pressure at least 30 percent through medicines slows the disease in some people. Glaucoma may worsen in others despite low pressures.
A comprehensive medical history is important to identify other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma.
In angle-closure glaucoma, the fluid at the front of the eye cannot drain through the angle and leave the eye. The angle gets blocked by part of the iris. People with this type of glaucoma may have a sudden increase in eye pressure. Symptoms include severe pain and nausea, as well as redness of the eye and blurred vision. If you have these symptoms, you need to seek treatment immediately. This is a medical emergency. If your doctor is unavailable, go to the nearest hospital or clinic. Without treatment to restore the flow of fluid, the eye can become blind. Usually, prompt laser surgery and medicines can clear the blockage, lower eye pressure, and protect vision.
In congenital glaucoma, children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have obvious symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines are not effective and can cause more serious side effects in infants and be difficult to administer. Surgery is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision.
Secondary glaucomas can develop as complications of other medical conditions. For example, a severe form of glaucoma is called neovascular glaucoma, and can be a result from poorly controlled diabetes or high blood pressure. Other types of glaucoma sometimes occur with cataract, certain eye tumors, or when the eye is inflamed or irritated by a condition called uveitis. Sometimes glaucoma develops after other eye surgeries or serious eye injuries. Steroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in some people. There are two eye conditions known to cause secondary forms of glaucoma.
Pigmentary glaucoma occurs when pigment from the iris sheds off and blocks the meshwork, slowing fluid drainage.
Pseudoexfoliation glaucoma occurs when extra material is produced and shed off internal eye structures and blocks the meshwork, again slowing fluid drainage.
Depending on the cause of these secondary glaucomas, treatment includes medicines, laser surgery, or conventional or other glaucoma surgery.
Thyroid eye disease
Thyroid eye disease also known as Graves’ ophthalmopathy is a condition that occurs when the immune system attacks the muscles and other tissues around the eyes 21.
The result is inflammation and a buildup of tissue and fat behind the eye socket, causing the eyeballs to bulge out. Rarely, inflammation is severe enough to compress, or push on, the optic nerve that leads from the eye to the brain, causing vision loss.
Symptoms of thyroid eye disease
Besides bulging eyes, other GO symptoms are
- dry, gritty, and irritated eyes
- puffy or retracted eyelids
- double vision
- light sensitivity
- pressure or pain in the eyes
- trouble moving the eyes
About one in three people with Graves’ disease develop mild Graves’ ophthalmopathy, and about 5 percent develop severe Graves’ ophthalmopathy 22. This eye condition usually lasts 1 to 2 years and often improves on its own.
Thyroid eye disease can occur before, at the same time as, or after other symptoms of hyperthyroidism develop. Eye problems sometimes develop long after Graves’ disease has been treated, but this happens rarely. Thyroid eye disease may even occur in people whose thyroid function is normal. Smoking makes thyroid eye disease worse.
Treatment of thyroid eye disease
The eye problems of Graves’ disease may not improve after thyroid treatment, so doctors often treat the two problems separately.
Eye drops can relieve dry, gritty, irritated eyes—the most common of the milder symptoms. If pain and swelling occur, your doctor may prescribe a steroid such as prednisone . Other medicines that reduce your body’s immune response, such as rituximab , may also provide relief.
Sunglasses can help with light sensitivity. Special eyeglass lenses may help reduce double vision. If you have puffy eyelids, your doctor may advise you to sleep with your head raised to reduce swelling. If your eyelids do not fully close, taping them shut at night can help prevent dry eyes.
Your doctor may recommend surgery to improve bulging of your eyes and correct the vision changes caused by pressure on the optic nerve. A procedure called orbital decompression makes the eye socket bigger and gives the eye room to sink back to a more normal position. Eyelid surgery can return retracted eyelids to their normal position.
Rarely, doctors treat Graves’ eye disease with radiation therapy to the muscles and tissues around the eyes.
Dry Eye
Dry eye occurs when the eye does not produce tears properly, or when they evaporate too quickly 23. Experts estimate that dry eye affects millions of adults in the United States. The risk of developing dry eye increases with advancing age. Women have a higher prevalence of dry eye compared with men. Dry eye can make it difficult to do some activities, such as using a computer or reading for an extended period of time, and it can decrease tolerance for dry environments, such as the air inside an airplane.
What are the symptoms of dry eye ?
Dry eye causes a scratchy sensation or the feeling that something is in the eye. Other symptoms include stinging or burning, episodes of excess tearing that follow periods of dryness, discharge, pain, and redness in the eye. People with dry eye may also feel as if their eyelids are heavy and may experience blurred vision.
What are tears and how do they relate to dry eye ?
In a healthy eye, lubricating tears called basal tears continuously bathe the cornea, the clear, dome-shaped outer surface of the eye. With every blink of the eye, basal tears flow across the cornea, nourishing its cells and providing a layer of liquid protection from the environment. When the glands nearby each eye fail to produce enough basal tears, or when the composition of the tears changes, the health of the eye and vision are compromised. Vision may be affected because tears on the surface of the eye play an important role in focusing light.
Tears are a complex mixture of fatty oils, water, mucus, and more than 1500 different proteins that keep the surface of the eye smooth and protected from the environment, irritants, and infectious pathogens. Tears form in three layers:
- An outer, oily (lipid) layer, produced by the Meibomian glands, keeps tears from evaporating too quickly and helps tears remain on the eye.
- A middle (aqueous) layer contains the watery portion of tears as well as water-soluble proteins. This layer is produced by the main lacrimal gland and accessory lacrimal glands. It nourishes the cornea and the conjunctiva, the mucous membrane that covers the entire front of the eye and the inside of the eyelids.
- An inner (mucin) layer, produced by goblet cells, binds water from the aqueous layer to ensure that the eye remains wet.
Figure 9. Tear production
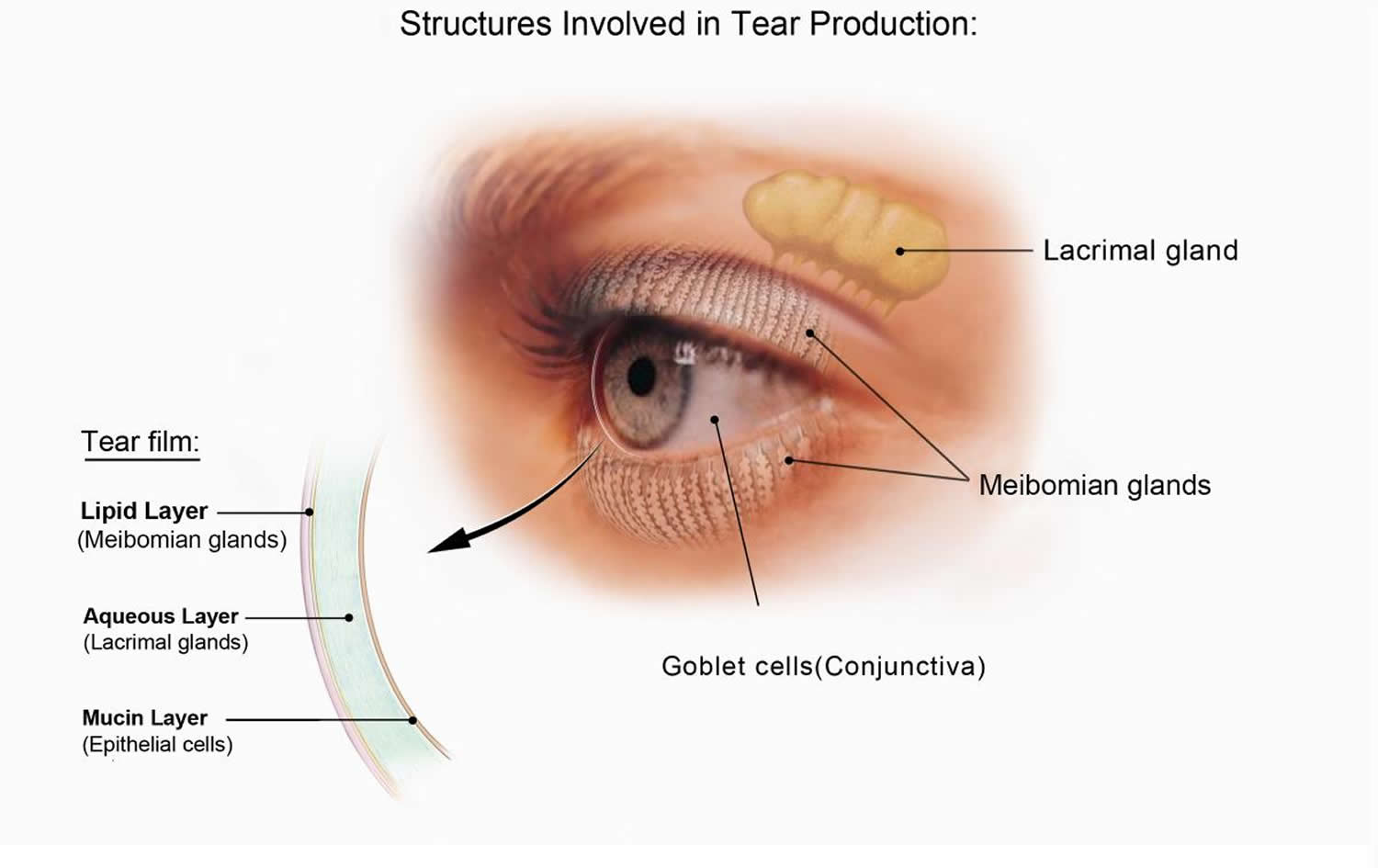
What causes dry eye ?
Dry eye can occur when basal tear production decreases, tear evaporation increases, or tear composition is imbalanced. Factors that can contribute to dry eye include the following:
- Medications including antihistamines, decongestants, antidepressants, birth control pills, hormone replacement therapy to relieve symptoms of menopause, and medications for anxiety, Parkinson’s disease, and high blood pressure have been associated with dry eye.
- Advancing age is a risk factor for declines in tear production. Dry eye is more common in people age 50 years or older.
Rosacea (an inflammatory skin disease) and blepharitis (an inflammatory eyelid disease) can disrupt the function of the Meibomian glands. - Autoimmune disorders such as Sjögren’s syndrome, lupus, scleroderma, and rheumatoid arthritis and other disorders such as diabetes, thyroid disorders, and Vitamin A deficiency are associated with dry eye.
- Women are more likely to develop dry eye. Hormonal changes during pregnancy and after menopause have been linked with dry eye. Women also have an increased risk for autoimmune disorders.
- Windy, smoky, or dry environments increase tear evaporation.
- Seasonal allergies can contribute to dry eye.
- Prolonged periods of screen time encourage insufficient blinking.
- Laser eye surgery may cause temporary dry eye symptoms.
How is dry eye diagnosed and treated ?
People experiencing dry eye symptoms should consult an eye care professional to determine the cause, which guides treatment strategy.
Change medications. Consult a physician about switching medications to alternative ones that are not associated with dry eye. This may alleviate dry eye symptoms.
Over-the-counter (OTC) topical medications. Mild dry eye symptoms may be treated with over-the-counter medications such as artificial tears, gels, and ointments.
Environmental and lifestyle changes. Cutting back on screen time and taking periodic eye breaks may help. Closing the eyes for a few minutes, or blinking repeatedly for a few seconds, may replenish basal tears and spread them more evenly across the eye. Sunglasses that wrap around the face and have side shields that block wind and dry air can reduce symptoms in windy or dry conditions.
In cases of Meibomian gland dysfunction, warm lid compresses and scrubs may be helpful.
Smoking cessation and limiting exposure to secondhand smoke also may help.
Prescription dry eye medications. Cyclosporine and lifitegrast are the only prescription medications approved by the U.S. Food and Drug Administration for treating dry eye. Corticosteroid eye drops also may be prescribed short-term to reduce eye inflammation.
Devices. FDA-approved devices provide temporary relief from dry eye by stimulating glands and nerves associated with tear production.
Surgical options. Punctal plugs made of silicone or collagen may be inserted by an eye care professional to partially or completely plug the tear ducts at the inner corners of the eye to keep tears from draining from the eye. In severe cases, surgical closure of the drainage ducts by thermal punctal cautery may be recommended to close the tear ducts permanently.
Future treatment options
In a healthy eye, only one-tenth of a degree of cooling from evaporation is needed for activation of nerves that trigger basal tearing. Researchers are investigating factors that influence the ability of corneal nerves to sense tear evaporation. Such research may lead to the development of topical corneal nerve stimulators, or products that increase nerve sensitivity to drying.
The protein lacritin in tears promotes basal tearing (via nerve stimulation) and eye health. Some people with dry eye have low levels of lacritin in their tears. A topical, synthetic form of the protein has been developed for initial testing in people with dry eye.
Since corneal nerve number, length, and function are substantially diminished in dry eye, another research goal is to devise ways to promote their regrowth. Such a product could also help individuals suffering from dry eye after corneal laser surgery, such as LASIK.
Other research is exploring the role of stem cells in the natural development of lacrimal glands. This early-stage research may eventually enable use of a patient’s own stem cells to rebuild or replace tear-producing lacrimal glands.
Investigation is ongoing into the molecular composition of the tear lipid layer, and factors that either stabilize or destabilize it. Treatments to stabilize it may help reduce tear evaporation.
Strabismus
Strabismus involves an imbalance in the positioning of the two eyes. Strabismus can cause the eyes to cross in (esotropia) or turn out (exotropia) 1. Strabismus is caused by a lack of coordination between the eyes. As a result, the eyes look in different directions and do not focus simultaneously on a single point. In most cases of strabismus in children, the cause is unknown 1. In more than half of these cases, the problem is present at or shortly after birth (congenital strabismus) 1. It is estimated that 4% of the U.S. population has strabismus 24. When the two eyes fail to focus on the same image, there is reduced or absent depth perception and the brain may learn to ignore the input from one eye, causing permanent vision loss in that eye (one type of amblyopia).
Types of strabismus
There are many different types of strabismus. Strabismus is most commonly described by the direction of the eye misalignment; common types of strabismus are 24:
- esotropia (inward turning of the eyes),
- exotropia (outward turning of the eye),
- hypotropia, and
- hypertropia.
Strabismus can also be described by its cause. The 3 cranial nerves (III, IV, VI) responsible for eye movement can be weak or palsied and cause strabismus. Some examples of paralytic strabismus include third nerve palsy and superior oblique palsy.
Special patterns of strabismus can have unique names such as Brown syndrome, and Duane syndrome.
Horizontal strabismus
Esotropia is inward turning of the eyes (aka “crossed eyes”). Types of esotropia include infantile esotropia, accommodative esotropia, and sixth nerve palsy. Exotropia is the term used to describe outward turning of the eyes (aka “wall-eyed”) [See figures 10 and 11].
Figure 10. Strabismus (Esotropia aka “crossed eyes”)

Figure 11. Strabismus (Exotropia aka “wall-eyed”)

Vertical strabismus
The terms hypertropia and hypotropia are used to describe vertical misalignment. Hypertropia is an abnormal eye higher than the normal eye. Hypotropia is when the abnormal eye is lower than the normal eye. The terms can generally be interchanged.
What causes strabismus ?
Most strabismus is the result of an abnormality of the poorly understood neuromuscular (including brain) control of eye movement. Less commonly, a problem with the actual eye muscle causes strabismus.
Eye misalignment can cause amblyopia in children. When the eyes are oriented in different directions, the brain receives 2 different visual images. The brain may ignore the image from the misaligned eye to avoid double vision, resulting in poor vision development of that eye. Also, an eye that sees poorly tends to be misaligned.
Who develops strabismus as a child ?
Strabismus often occurs in children who are otherwise completely normal. However, disorders that affect the brain such as cerebral palsy, Down syndrome, hydrocephalus and brain tumor are more likely to develop strabismus.
What adult disorders cause strabismus ?
Stroke is the leading cause of strabismus in adults. Trauma, neurological problems, and Graves disease (thyroid eye disorders) are other common causes of strabismus.
How does trauma cause strabismus ?
Trauma can cause strabismus by 1) brain damage that impairs control of eye movement, 2) damage of the nerves that control eye movement and/or 3) damage of the eye muscles either directly or secondarily from trauma to the eye socket.
How is strabismus treated ?
The goal of strabismus treatment is to improve eye alignment which allows for the eyes to better work together (binocular vision). Treatment may involve eye glasses, eye exercises, prism, and/ or eye muscle surgery. Problems associated with strabismus (including amblyopia, ptosis, and cataract) are usually treated prior to eye muscle surgery.
What age is considered “too old” to have eye muscle surgery ?
Eyes can be straightened at any age and should be considered as a treatment option if it is likely to improve symptoms and enhance quality of life 25. In most cases, eye muscle surgery is a successful, safe, and effective treatment for strabismus in adults of all ages. The good news is that it is never too late for surgery. Even patients in their 90’s have benefited from surgical correction 25.
Can anything be done for adults with strabismus (misaligned eyes) ?
Yes. Adults can benefit from some of the same treatment options that are available to children for treating strabismus. Treatment options may include prismatic glasses and surgery 25. Most adults with misaligned eyes are able to have successful surgical correction. It is important consult with an eye surgeon who specializes in strabismus surgery.
Why do adults get strabismus ?
Adults may have strabismus either from a residual childhood strabismus or they may acquire strabismus in adulthood 25. New strabismus that develops in an adult can result from conditions such as thyroid eye disease, stroke or tumors, but often there is no identifiable cause 25.
Is eye straightening as an adult strictly cosmetic ?
No. Eye alignment surgery is performed in adults for several reasons. Adults frequently have disabling double vision because of eye misalignment. Prism glasses or surgery will likely improve the double vision and depth perception 25. Heavy prism glasses can be uncomfortable and causes distorted vision, surgery can be evaluated by your surgeon to decrease the dependence on prism glasses.
Also, strabismus affects adults in emotional, social, and economical ways. Realigning the eyes can “reconstruct” the abnormal appearance of the eyes providing a better quality of life 25.
Is eye muscle surgery risky for adults ?
Every surgical procedure has some risks. For strabismus surgery, the most common risks are residual misalignment of the eyes and double vision. Most double vision that occurs after strabismus surgery is temporary; however, persistent double vision is possible. Fortunately, the more serious risks are rare. These risks include anesthetic complications, infection, bleeding, retinal detachment, and decreased vision. Health risks vary with the general health of the individual. For those in poor health, surgery under local anesthesia instead of general anesthesia may be considered.
How successful is eye muscle surgery ?
Most individuals have significant improvement in eye alignment with one surgery. Occasionally the surgery is only partially successful, or changes in ocular alignment may occur over time after initially successful surgery. Additional surgery may be indicated. Correction of residual double vision may be improved with the use of prism glasses.
How painful is this type of surgery ?
Discomfort after eye muscle surgery is usually not severe. Headache, pulling sensation with eye movement and foreign body sensation in the eye are the most common complaints. These symptoms typically last only several days. Over-the-counter pain medication often reduces the discomfort, although stronger medication is sometimes prescribed. Most patients return to full activity in several days. Some surgeons limit swimming and heavy physical activity for up to several weeks after surgery.
Is hospitalization required for eye alignment surgery and how will this affect normal activities ?
Eye alignment surgery is usually performed as an outpatient procedure although the need for hospitalization varies depending upon general health and surgeon preference 25. Following surgery, most individuals return to nearly all normal activities within several days.
Amblyopia
Amblyopia, also referred to as “lazy eye,” is the most common cause of vision impairment in children 1. Amblyopia is the medical term used when the vision in one of the eyes is reduced because the eye and the brain are not working together properly 26. The eye itself looks normal, but it is not being used normally because the brain is favoring the other eye. Vision loss occurs because nerve pathways between the brain and the eye aren’t properly stimulated. The brain “learns” to see only blurry images with the amblyopic eye even when glasses are used. As a result, the brain favors one eye, usually due to poor vision in the other eye.
Conditions leading to amblyopia include strabismus, an imbalance in the positioning of the two eyes; more nearsighted (myopia), farsighted (hyperopia), or astigmatic in one eye than the other eye (astigmatism), and rarely other eye conditions such as cataract. These terms refer to the ability of the eye to focus light on the retina. Farsightedness, or hyperopia, occurs when the distance from the front to the back of the eye is too short. Eyes that are farsighted tend to focus better at a distance but have more difficulty focusing on near objects. Nearsightedness, or myopia, occurs when the eye is too long from front to back. Eyes with nearsightedness tend to focus better on near objects. Eyes with astigmatism have difficulty focusing on far and near objects because of their irregular shape.
Unless it is successfully treated in early childhood amblyopia usually persists into adulthood, and is the most common cause of permanent one-eye (monocular) vision impairment among children and young and middle-aged adults. Amblyopia is the most common cause of visual impairment among children, affecting approximately 2 to 3 out of every 100 children 27.
What causes amblyopia ?
Normal vision develops during the first few years of life. At birth infants, have very poor vision, however as they use their eyes the vision improves because the vision centers in the brain are developing. If infants are not able to use their eyes from various reasons the vision centers do not develop properly and the vision is decreased despite normal appearance of the structures of the eyes.
Amblyopia can result from any condition that prevents the eye from focusing clearly. Amblyopia can be caused by the misalignment of the two eyes—a condition called strabismus. With strabismus, the eyes can cross in (esotropia) or turn out (exotropia). Occasionally, amblyopia is caused by a clouding of the front part of the eye, a condition called cataract.
The most common cause is refractive error in one or both eyes that is not corrected early in childhood resulting in poor development of the visual function in the affected eye/s. This is called refractive amblyopia 27. Amblyopia can occur when one eye is more nearsighted, more farsighted, or has more astigmatism. These terms refer to the ability of the eye to focus light on the retina. Farsightedness, or hyperopia, occurs when the distance from the front to the back of the eye is too short. Eyes that are farsighted tend to focus better at a distance but have more difficulty focusing on near objects. Nearsightedness, or myopia, occurs when the eye is too long from front to back. Eyes with nearsightedness tend to focus better on near objects. Eyes with astigmatism have difficulty focusing on far and near objects because of their irregular shape.
Another common cause is strabismus or eye misalignment. This is called strabismic. Rarely there is a structural anomaly that impairs the visual function like a droopy eyelid or opacity in the visual axis like cataract or corneal scar. This is called deprivation amblyopia. Multiple causative factors can coexist.
What is refractive amblyopia ?
Refractive amblyopia happens when there is a large or unequal amount of refractive error (glasses strength) between a child’s eyes. The brain learns how to see well from the eye that has less need for glasses and does NOT learn to see well from the eye that has a greater need for glasses. The vision problem may be invisible because the child does not complain of blurry vision. The child sees well with the better seeing eye. Additionally, the amblyopic eye may not look any different from the normal seeing eye. Therefore, parents and pediatricians may not think there is a problem because the child’s eyes look normal. For these reasons, this kind of amblyopia in children may not be found until the child has a vision test. This kind of amblyopia can affect one or both eyes and can be best helped if the problem is found early.
What is strabismic amblyopia ?
Strabismic amblyopia develops when the eyes are not straight. One eye may turn in, out, up or down. When this happens, the brain begins to ignore, or “turns off” the eye that is not straight and the vision subsequently drops in that eye.
What is deprivation amblyopia ?
Deprivation amblyopia develops when cataracts or similar conditions “deprive” young children’s eyes of visual experience. If not treated very early, these children never learn to see very well and can have very poor vision. Sometimes this kind of amblyopia can affect both eyes.
When should amblyopia be treated ?
Early treatment is always best 28. If necessary, children with refractive errors (nearsightedness, farsightedness or astigmatism) can wear glasses or contact lenses when they are as young as one week old. Children with cataracts or other “amblyogenic” conditions are usually treated promptly in order to minimize the development of amblyopia.
How old is TOO old for amblyopia treatment ?
A recent National Institutes of Health study confirmed that SOME improvement in vision can be attained with amblyopia therapy initiated in younger teenagers (through age 14 years) 28. Better treatment success is achieved when treatment starts early, however.
What happens if amblyopia is not treated ?
If amblyopia is not treated the vision in the affected eye/s will be permanently decreased causing deficits in depth perception and peripheral vision. Moreover if the good eye becomes injured or affected by a disease, significant lifetime disability may result.
The ophthalmologist will give the instructions and monitor the progress but the patient and the family will do the hard work of actually performing the treatment. Children do not like to have their good eye patched, especially if the vision in the amblyopic eye is very low, but parents must stand by them and help them do what’s best. Parents play probably the most important role in a successful treatment.
How can you get early treatment for amblyopia ?
Some forms of amblyopia, such as that associated with large-deviation strabismus, may be easily detected by parents. Other types of amblyopia (from high refractive error) might cause a child to move very close to objects or squint his or her eyes. Still other forms of amblyopia may NOT be obvious to parents and therefore must be detected by Vision Screening.
How is amblyopia treated in children ?
Treating amblyopia involves forcing the child to use the eye with weaker vision. There are two common ways to treat amblyopia 27:
Patching
An adhesive patch is worn over the stronger eye for weeks to months. This therapy forces the child to use the eye with amblyopia. Patching stimulates vision in the weaker eye and helps parts of the brain involved in vision develop more completely.
An National Eye Institute study 29 showed that patching the unaffected eye of children with moderate amblyopia for two hours daily works as well as patching for six hours daily 27. Shorter patching time can lead to better compliance with treatment and improved quality of life for children with amblyopia. However, a recent study 30 showed that children whose amblyopia persists despite two hours of daily patching may improve if daily patching is extended to 6 hours.
Previously, eye care professionals thought that treating amblyopia would be of little benefit to older children. However, results from a nationwide clinical trial 31 showed that many children from ages seven to 17 years old benefited from treatment for amblyopia. This study shows that age alone should not be used as a factor to decide whether or not to treat a child for amblyopia.
During which activities should patching be performed ?
There is no particular activity that will improve the vision more than another activity. The most important part of treatment is keeping the patch on for the prescribed treatment time. As long as the child is conscious and has his or her eyes open, visual input will be processed by the amblyopic eye. On the other hand, the child may be more cooperative or more open to bargaining if patching is performed during certain, favorite activities (such as watching a preferred television program or video). Some eye doctors believe that the performance of near activities (reading, coloring, hand-held computer games) during treatment may be more stimulating to the brain and produce better or more rapid recovery of vision.
Should patching be performed during school hours ?
In many instances, school is an excellent time to patch, taking advantage of a nonparental authority figure. Patching during school hours gives the class an opportunity to learn valuable lessons about accepting differences between children. While in most instances, children may not need to modify their school activities while patching, sometimes adjustments such as sitting in the front row of the classroom will be necessary. If the patient, teacher, and classmates are educated appropriately, school patching need not be a socially stigmatizing experience. On the other hand, frequently a parental or other family figure may be more vigilant in monitoring patching than is possible in the school setting. Parents should be flexible in choosing when to schedule patching.
What if my child refuses to wear the patch ?
Many children will resist wearing a patch at first. Successful patching may require persistence and plenty of encouragement from family members, neighbors, teachers, etc. Children will often throw a temper-tantrum, but then they eventually learn not to remove the patch. Another way to help is to provide a reward to the child for keeping the patch on for the prescribed time period.
How long does amblyopia patching therapy take to work ?
Although vision improvement frequently occurs within weeks of beginning patching treatment, optimal results often take many months. Once vision has been improved, less (maintenance) patching or periodic use of atropine eyedrops may be required to keep the vision from slipping or deteriorating. This maintenance treatment may be advisable for several months to years.
Atropine
A drop of a drug called atropine is placed in the stronger eye to temporarily blur vision so that the child will use the eye with amblyopia, especially when focusing on near objects. National Eye Institute-supported research 32 has shown that atropine eye drops, when placed in the unaffected eye once a day, work as well as eye patching. Atropine eye drops are sometimes easier for parents and children to use.
However, not all children benefit from eye drop treatment for amblyopia. Eye drops (such as atropine) do not work as well when the stronger eye is nearsighted or when the degree of amblyopia is severe 28.
What happens if amblyopia treatment does not work ?
In some cases, treatment for amblyopia may not succeed in substantially improving vision. It is hard to decide to stop treatment, but sometimes it is best for both the child and the family. Children who have amblyopia in one eye and good vision only in their other eye can wear safety glasses and sports goggles to protect the normal eye from injury. As long as the good eye stays healthy, these children function normally in most aspects of society
In most cases loss of vision from amblyopia can be prevented or successfully treated if started early enough and if the degree of amblyopia is not extreme.
Can surgery be performed to treat amblyopia ?
There is no surgery to improve the vision for amblyopia. Surgery can be performed to straighten misaligned eyes such as crossing. Surgery to make the eyes straight can only help enable the eyes to work together as a team. Children with strabismic amblyopia still need close monitoring and treatment for the amblyopia, and this treatment is usually performed before strabismus surgery is considered.
Children who are born with cataracts may need surgery to take out the cataracts. After surgery, the child will usually need vision correction with glasses or contact lenses and patching.
Can amblyopia be treated in adults ?
Studies are very limited at this time, and scientists don’t know the success rate for treating amblyopia in adults. During the first seven to ten years of life, the visual system develops rapidly. Important connections between the eye and the brain are created during this period of growth and development. Scientists are exploring whether treatment for amblyopia in adults can improve vision.
Conjunctivitis
Pink eye or conjunctivitis is one of the most common and treatable eye conditions in children and adults; about 3 million cases of pink eye occur in the United States each year 33. Conjunctivitis or “pink eye” is a condition where the eyes look pink or red and may have discharge. Symptoms may include burning, itching, irritation, discharge, or crusting of the lashes. Treatment is not always needed and the course of treatment depends on the underlying cause. Conjunctivitis caused by bacteria or viruses is contagious [See figure 12].
Figure 12. Conjunctivitis (pink eye)

What is pink eye ?
Pink eye, also known as conjunctivitis, involves inflammation of the conjunctiva, the thin, clear tissue that lines the inside of the eyelid and covers the white part of the eye, or sclera. The inflammation makes blood vessels more visible, giving the eye a pink or reddish appearance. The affected eye(s) may be painful, itchy or have a burning sensation. The eyes can also tear or have a discharge that forms a crust during sleep causing the eyes to be “stuck shut” in the morning. Other signs or symptoms that may accompany pink eye include:
- Swelling of the conjunctiva
- Feeling like a foreign body is in the eye(s)
- Sensitivity to bright light
- Enlargement and/or tenderness of the lymph node in front of the ear. This enlargement may feel like a small lump when touched. (Lymph nodes act as filters in the body, collecting and destroying viruses and bacteria.)
- Contact lenses that do not stay in place on the eye and/or feel uncomfortable due to bumps that may form under the eyelid
What causes pink eye (conjunctivitis) ?
Pink eye is most often caused by bacterial or viral infections. Allergic reactions or exposure to irritants can also cause pink eye. Pinpointing the cause may be difficult because the signs and symptoms tend to be similar regardless of the underlying cause.
- Viral conjunctivitis is caused by a wide variety of viruses, but adenovirus and herpesvirus are the most common viruses that cause pink eye. Viral conjunctivitis may also occur along with an upper respiratory tract infection, cold, or sore throat.
- Bacterial conjunctivitis is caused by infection of the eye with bacteria such as Staphylococcus aureus, Streptococcus pneumonia, or Haemophilus. It is a common reason for children to stay home sick from day care or school.
- Allergic conjunctivitis can be caused by allergies to pollen, dust mites, molds, or animal dander.
- Irritants such as contact lenses and lens solutions, chlorine in a swimming pool, smog or cosmetics may also be an underlying cause of conjunctivitis.
Is conjunctivitis contagious ?
Conjunctivitis caused by bacteria or viruses is contagious.
Does a pink eye always mean infection ?
No. Sometimes a pink eye can indicate other eye problems including allergy, foreign body, contact lens reaction, inflammation or glaucoma.
How you can prevent getting conjunctivitis ?
Hand washing is the most important preventive measure. Never touching your eyes or the facial area unless you have just washed your hands is also important. If you wear contact lenses, hand washing is especially important, as well as disinfecting lenses/disposing lenses on schedule. Never store your lenses in a solution other than the commercially prepared solutions. Never swim in a lake or hot tub with your lenses on.
Viral and bacterial conjunctivitis are highly contagious and can be easily spread from person to person. Allergic conjunctivitis is not contagious.
If you or someone around you has infectious (viral or bacterial) conjunctivitis, limit its spread by following these steps:
- Wash your hands often with soap and warm water. And wash up immediately if you’ve touched an affected person’s eyes, linens or clothes (for example, when caring for a child who has pink eye). If soap and water are not available, use an alcohol-based hand sanitizer that contains at least 60 percent alcohol.
- Avoid touching or rubbing your eyes.
- If you have conjunctivitis, wash any discharge from around the eyes several times a day.
- Do not use the same eye drop dispenser/bottle for infected and non-infected eyes—even for the same person.
- Avoid sharing articles like towels, blankets, and pillowcases.
- Clean your eyeglasses.
- Clean, store, and replace your contact lenses as instructed by your eye health professional.
- Do not share eye makeup, face makeup, makeup brushes, contact lenses or containers, or eyeglasses.
- Use a clean towel or tissue each time you wipe your face and eyes.
- Wash your hands very often. Always wash them before and after you eat, when you go to the bathroom, or after you sneeze or cough.
- Try not to touch your eyes. If you do, wash your hands right away.
There are also steps you can take to avoid re-infection once the infection goes away:
- Throw away any eye or face makeup or applicators you used while infected.
- Throw away contact lens solutions you used while infected.
- Throw away contact lenses and cases you used.
- Clean your eyeglasses and cases.
How is pink eye diagnosed ?
Conjunctivitis can be diagnosed with an eye examination by a healthcare provider. In some cases, the type of conjunctivitis can be determined by assessing the person’s signs, symptoms, and recent health history (such as whether the person has recently been exposed to someone with conjunctivitis or has a pattern of seasonal allergy). Most cases resolve with time, and there is usually no need for treatment or laboratory tests, unless the person’s history suggests bacterial conjunctivitis.
Viral Conjunctivitis
Viral conjunctivitis is often diagnosed based on a person’s history and symptoms. It tends to occur in both eyes and often accompanies a common cold or respiratory tract infection. Laboratory tests usually are not needed to diagnose viral conjunctivitis; however, testing may be done if a more severe form of viral conjunctivitis is suspected. More severe causes include herpes simplex virus (which usually involves blisters on the skin), varicella-zoster virus (chickenpox and shingles), rubella or rubeola (measles). This testing is performed using a sample of the discharge from an infected eye.
Bacterial Conjunctivitis
Bacterial conjunctivitis tends to occur in one eye and may accompany an ear infection. A sample of the discharge from the affected eye may be obtained for laboratory tests to determine which type of bacteria is causing the pink eye and how best to treat it.
Allergic Conjunctivitis
Allergic conjunctivitis tends to occur in both eyes and often accompanies allergy symptoms, such as an itchy nose, sneezing, and scratchy throat. Allergic conjunctivitis may occur seasonally when pollen counts are high, and it can cause the person’s eyes to itch intensely. A detailed health history may help determine the source of the allergic reaction.
How is conjunctivitis treated ?
Most cases of pink eye are mild and will resolve on their own without prescription treatment. In many cases, symptom relief can be achieved by using artificial tears for the dryness and cold packs for the inflammation. (Artificial tears can be purchased without a doctor’s prescription.)
However, you should seek medical attention if you have any of following symptoms:
- Moderate to severe pain in the eye(s)
- Vision problems, such as sensitivity to light or blurred vision, that do not improve when any discharge present is wiped from the eye(s)
- Intense redness in the eye(s)
- Symptoms that become worse or persist when severe viral conjunctivitis is suspected
Also seek medical attention if you have signs of conjunctivitis and you have a weakened immune system from HIV infection, cancer treatment, or other medical conditions or treatments.
Viral Conjunctivitis
Most cases of viral conjunctivitis are mild and will clear up in 7–14 days without treatment and without any long-term consequences. In some cases, however, viral conjunctivitis can take two or more weeks to resolve, especially if complications arise.
Antiviral medication can be prescribed by a physician to treat more serious forms of conjunctivitis, such as those caused by herpes simplex virus or varicella-zoster virus. Antibiotics will not improve viral conjunctivitis as these drugs are not effective against viruses.
Bacterial Conjunctivitis
Mild bacterial conjunctivitis may get better without antibiotic treatment and without causing any severe complications.
Antibiotics can help shorten the illness and reduce the spread of infection to others. Your healthcare provider may prescribe antibiotic eye drops or ointment, which should resolve the infection within several days.
Consult your healthcare provider if you have been given antibiotics for bacterial conjunctivitis and symptoms have not improved after 24 hours of treatment.
Allergic Conjunctivitis
Conjunctivitis caused by an allergy usually improves by eliminating or significantly reducing contact with the allergen (such as pollen or animal dander). Allergy medications and certain eye drops can also provide relief.
Conjunctivitis caused by an irritant often clears up by eliminating the irritant. If you develop conjunctivitis and you wear contacts, stop using them temporarily until the conjunctivitis resolves. In some cases, your healthcare provider may also prescribe drug treatments to improve symptoms.
Will there be any permanent effect on vision with conjunctivitis ?
Most infections will clear without complications. Any neglected infection can result in secondary vision problems. Viral eye infections, especially herpes, can affect vision.
Can newborns get pink eye ?
Newborns can develop pink eye, which is called neonatal conjunctivitis, or less commonly, ophthalmia neonatorum. Common symptoms include eye discharge and puffy, red eyelids within one day to two weeks after birth. Newborn conjunctivitis may be caused by infection, irritation, or a blocked tear duct. A mother can pass on infectious conjunctivitis to her newborn during childbirth, even she has no symptoms herself, because she may carry bacteria or viruses in the birth canal. When caused by an infection, neonatal conjunctivitis can be very serious. The most common types of neonatal conjunctivitis include:
- Chlamydial (or inclusion) conjunctivitis is caused by the bacterium Chlamydia trachomatis and can cause swelling of the eyelids with purulent (pus) discharge. Symptoms often appear 5-12 days after birth but may present at any time during the first month of life.
- Gonococcal conjunctivitis is caused by Neisseria gonorrhoeae, the bacterium that causes gonorrhea. Gonococcal conjunctivitis causes pus discharge and swelling of eyelids, which may appear 2-4 days after birth.
- Chemical conjunctivitis can be caused by eye drops or ointment given to newborns to help prevent bacterial eye infections. Symptoms include red eyes and eyelid swelling, and usually resolve in 24-36 hours. Most hospitals are required by state law to put drops or ointment in a newborn’s eyes to prevent disease. The benefits of preventing a more serious type of conjunctivitis are thought to outweigh the risks of chemical conjunctivitis.
- Other bacteria and viruses can also cause conjunctivitis in a newborn. Bacteria that normally live in a woman’s vagina and that are not sexually transmitted can cause neonatal conjunctivitis. The viruses that cause genital and oral herpes can also cause neonatal conjunctivitis and severe eye damage. Such viruses may be passed to the baby during childbirth.
How is pink eye treated in newborns ?
Bacterial conjunctivitis may be treated with topical antibiotic eye drops and ointments, oral antibiotics, or intravenous (given through a vein) antibiotics.
A combination of topical and oral, or topical and intravenous treatments are sometimes used at the same time. A saline solution may be prescribed for rinsing the baby’s eye(s) to remove pus, if necessary.
- Chlamydial conjunctivitis in newborns is usually treated with oral antibiotics such as erythromycin. Parents are usually treated as well.
- Gonococcal conjunctivitis in newborns is usually treated with intravenous antibiotics. If untreated, this condition can lead to corneal ulcers and blindness.
- Other types of bacterial and viral conjunctivitis are usually treated with antibiotic eye drops or ointments. A warm compress to the eye may also help relieve swelling and irritation.
- Blocked tear ducts may cause conjunctivitis. If a tear duct is blocked, a gentle warm massage between the eye and nasal area may help. If the blocked tear duct is not cleared by one year of age, surgery may be required.
- Chemical Conjunctivitis usually resolves in 24-36 hours without treatment.
- Centers for Disease Control and Prevention. Common Eye Disorders. https://www.cdc.gov/visionhealth/basics/ced/index.html[↩][↩][↩][↩][↩][↩]
- The National Eye Institute, National Institutes of Health. Healthy Eyes Facts. https://nei.nih.gov/health/healthyeyes[↩][↩]
- The National Eye Institute, National Institutes of Health. Facts About Refractive Errors. https://nei.nih.gov/health/errors/errors[↩]
- The National Eye Institute, National Institutes of Health. Facts About Myopia. https://nei.nih.gov/health/errors/myopia[↩]
- The National Eye Institute, the National Institutes of Health. Myopia. https://nei.nih.gov/health/myopia[↩]
- Vitale S, Ellwein L, Cotch MF, Ferris FL, Sperduto R. Prevalence of refractive error in the United States, 1999–2004. Archives of ophthalmology. 2008;126(8):1111-1119. doi:10.1001/archopht.126.8.1111. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2772054/[↩]
- Vitale S, Sperduto RD, Ferris FL. Increased Prevalence of Myopia in the United States Between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632–1639. doi:10.1001/archophthalmol.2009.303. http://jamanetwork.com/journals/jamaophthalmology/fullarticle/424548[↩]
- Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012 Oct;119(10):2141-51. doi: 10.1016/j.ophtha.2012.04.020. Epub 2012 Jul 17. https://www.ncbi.nlm.nih.gov/pubmed/22809757[↩]
- The National Eye Institute, the National Institutes of Health. Facts About Hyperopia. https://nei.nih.gov/health/errors/hyperopia[↩][↩][↩]
- The National Eye Institute, the National Institutes of Health. Hyperopia. https://nei.nih.gov/health/hyperopia[↩]
- The National Eye Institute, the National Institutes of Health. Facts About Astigmatism. https://nei.nih.gov/health/errors/astigmatism[↩][↩]
- The National Eye Institute, the National Institutes of Health. Facts About Presbyopia. https://nei.nih.gov/health/errors/presbyopia[↩][↩][↩]
- The National Eye Institute, National Institutes of Health. Age-Related Macular Degeneration (AMD). https://nei.nih.gov/health/maculardegen[↩]
- The National Eye Institute, National Institutes of Health. Facts About Age-Related Macular Degeneration. https://nei.nih.gov/health/maculardegen/armd_facts[↩]
- American Academy of Ophthalmology. https://www.aao.org[↩][↩]
- The National Eye Institute, National Institutes of Health. Facts About Diabetic Eye Disease. https://nei.nih.gov/health/diabetic/retinopathy[↩]
- Centers for Disease Control and Prevention. Basics of Vision and Eye Health FAQs. https://www.cdc.gov/visionhealth/faq.htm[↩][↩]
- The National Eye Institute, National Institutes of Health. Diabetic Eye Disease. https://nei.nih.gov/health/diabetic/[↩]
- The National Eye Institute, National Institutes of Health. Facts About Cataract. https://nei.nih.gov/health/cataract/cataract_facts[↩]
- The National Eye Institute, National Institutes of Health. Facts About Glaucoma. https://nei.nih.gov/health/glaucoma/glaucoma_facts[↩][↩][↩]
- The National Institute of Diabetes and Digestive and Kidney Diseases. Graves’ Disease. https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease[↩]
- Burch HB, Cooper DS. Management of Graves disease: a review. JAMA. 2015;314(243):2544-2554.[↩]
- The National Eye Institute, National Institutes of Health. Facts About Dry Eye. https://nei.nih.gov/health/dryeye/dryeye[↩][↩]
- American Association for Pediatric Ophthalmology and Strabismus. Strabismus. https://aapos.org/terms/conditions/100[↩][↩]
- American Association for Pediatric Ophthalmology and Strabismus. Adult Strabismus. https://aapos.org/terms/conditions/11[↩][↩][↩][↩][↩][↩][↩][↩]
- The National Eye Institute, National Institutes of Health. Amblyopia. https://nei.nih.gov/health/amblyopia/[↩]
- The National Eye Institute, National Institutes of Health. Facts About Amblyopia. https://nei.nih.gov/health/amblyopia/amblyopia_guide[↩][↩][↩][↩]
- American Association for Pediatric Ophthalmology and Strabismus. Amblyopia. https://aapos.org/terms/conditions/21[↩][↩][↩]
- Repka MX, Beck RW, Holmes JM, Birch EE, Chandler DL, Cotter SA, Hertle RW, Kraker RT, Moke PS, Quinn GE, Scheiman MM, Pediatric Eye Disease Investigator Group. A Randomized Trial of Patching Regimens for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2003 May. https://www.ncbi.nlm.nih.gov/pubmed/12742836[↩]
- Pediatric Eye Disease Investigator Group, Wallace DK, Lazar EL, et al. A Randomized Trial of Increasing Patching for Amblyopia. Ophthalmology. 2013;120(11):10.1016/j.ophtha.2013.04.008. doi:10.1016/j.ophtha.2013.04.008. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3833469/[↩]
- Scheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, Crouch ER Jr, Cruz OA, Davitt BV, Donahue S, Holmes JM, Lyon DW, Repka MX, Sala NA, Silbert DI, Suh DW, Tamkins SM, Pediatric Eye Disease Investigator Group. Randomized Trial of Treatment of Amblyopia in Children Aged 7 to 17 Years. Arch Ophthalmol. 2005 Apr. https://www.ncbi.nlm.nih.gov/pubmed/15824215[↩]
- Pediatric Eye Disease Investigator Group. A Randomized Trial of Atropine Vs. Patching for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2002 Mar. https://www.ncbi.nlm.nih.gov/pubmed/11879129[↩]
- The National Eye Institute, National Institutes of Health. Facts About Pink Eye. https://nei.nih.gov/health/pinkeye/pink_facts[↩]