Contents
What is digoxin toxicity
Digoxin toxicity also known as digitalis toxicity can be a problem with digitalis therapy. It may occur when you take too much of digoxin at one time. Digoxin toxicity can also occur when levels of the drug build up for other reasons. Digoxin is a relatively safe, cheap and effective therapy for relieving recurrent symptoms in patients with congestive heart failure. Digoxin is derived from the species Digitalis lanata and was first described by William Withering in 1785. Digoxin is sometimes used to increase cardiac contractility (positive inotrope) and as an anti-arrhythmic agent to control heart rate (e.g. in fast atrial fibrillation) 1). Superior rate-limiting agents, such as beta blockers, have now superseded digoxin as a first-line agent but its role remains important in atrial fibrillation (A Fib) associated with heart failure.
Symptoms of digoxin toxicity include:
- lethargy
- nausea and vomiting
- diarrhea
- abdominal pain
- visual disturbances
- hallucinations and delirium
- severe headache.
The clinical features of digoxin toxicity are often non-specific. They commonly include lethargy, confusion and gastrointestinal symptoms (anorexia, nausea, vomiting, diarrhea and abdominal pain) 2). Visual effects (blurred vision, color disturbances, haloes and scotomas) are rarer in contemporary practice 3). Cardiac arrhythmias account for most deaths 4).
Arrhythmias can occur even if the patient has no symptoms. Almost any arrhythmia can occur, with the exception of atrial tachyarrhythmias with a rapid ventricular response 5), because these usually require intact conduction in the atrioventricular (AV) node. Characteristic arrhythmias are those in which a tachyarrhythmia occurs simultaneously with sinus or atrioventricular node suppression, such as atrial and junctional tachycardia with atrioventricular block. However, sinus bradycardia, atrioventricular block and ventricular ectopy are more common 6). With severe toxicity, ventricular tachycardia (which may be bidirectional) and ventricular fibrillation can occur. ‘Reverse tick’ T-wave inversion is not a sign of toxicity.
Digoxin is an agent that is readily available, can be administered acutely and long-term, intravenously or orally, is safe and may be beneficial in both acute and chronic heart failure.
Digoxin toxicity can occur when serum digoxin concentration is within the therapeutic range and, as the presenting features are usually non-specific, the diagnosis can be difficult.
Digoxin toxicity can be caused by high levels of digoxin in the body. A lower tolerance to the drug can also cause digoxin toxicity. People with lower tolerance may have a normal level of digoxin in their blood. They may develop digoxin toxicity if they have other risk factors.
People with heart failure who take digoxin are commonly given medicines called diuretics. This drugs remove excess fluid from the body. Many diuretics can cause potassium loss. A low level of potassium in the body can increase the risk of digoxin toxicity. Digoxin toxicity may also develop in people who take digoxin and have a low level of magnesium in their body.
You are more likely to have digoxin toxicity if you take digoxin, digitoxin, or other digitalis medicines along with drugs that interact with it. Some of these drugs are quinidine, flecainide, verapamil, and amiodarone.
If your kidneys do not work well, digoxin can build up in your body. Normally, digoxin is removed through the urine. Any problem that affects how your kidneys work (including dehydration) makes digoxin toxicity more likely.
Some plants contain chemicals that can cause symptoms similar to digoxin toxicity if they are eaten. These include foxglove, oleander, and lily of the valley.
However, the incidence of digoxin toxicity has declined in recent years, as a result of a decreasing use and a reduced recommended therapeutic range, along with improved technology for monitoring of drug levels and increased awareness of drug interactions. Nevertheless, digoxin toxicity continues to be a problem in the United States because of the wide use of digoxin and its narrow therapeutic window.
Digoxin-specific antibody fragments are used when there is a risk of a life-threatening arrhythmia. The decision to use digoxin-specific antibody fragments is not dependent on knowledge of the serum digoxin concentration or the amount of digoxin ingested, but when either of these is known they should be used to calculate the dose. Further research is needed into optimal dosing protocols and whether digoxin-specific antibody fragments can be cost-effectively used for non-life-threatening toxicity.
What is digoxin
Digoxin is a cardiac glycoside extracted from foxglove leaves. Digoxin is used in heart failure because of its ability to increase the force of myocardial contraction (positive inotropy) and, simultaneously, decrease oxygen consumption.
Digoxin increases intracellular calcium in myocardial cells indirectly, by inhibiting the sodium/potassium-ATPase (sodium–potassium pump) in the cell membrane. Increased intracellular calcium increases cardiac contractility, but also the risk of tachyarrhythmias 7). Inhibition of this pump causes the hyperkalaemia commonly seen in toxicity. Digoxin also causes an increase in vagal activity, reducing activity in the sinus node and prolonging conduction in the atrioventricular node.
After a dose of digoxin, distribution to the tissues takes several hours. This means that the serum digoxin concentration is inaccurate unless taken at least six hours after the last dose. Only a post-distribution measurement reflects the severity of intoxication and this is the measurement that can help when calculating the dose of digoxin-specific antibody 8). This applies in both acute and chronic poisoning.
The elimination of digoxin is mainly by renal clearance and is prolonged in patients with renal impairment. Transport by P-glycoprotein also contributes to elimination 9). Consequently, a higher serum digoxin concentration for a given dose occurs in patients with renal impairment, lower body weight and in those taking amiodarone, verapamil, macrolides, azole antifungals and cyclosporin, which inhibit P-glycoprotein transport 10).
Although the serum digoxin concentration does predict the likelihood of toxicity 11), several conditions increase sensitivity to digoxin. They at least partly account for patients who develop digoxin toxicity when their serum digoxin concentration is within the therapeutic range 12). These conditions include hypokalemia, hypomagnesemia, hypercalcemia, myocardial ischemia, hypoxemia and acid–base disturbances 13).
Digoxin toxicity ECG
Digoxin toxicity causes a variety of arrhythmias. With digoxin toxicity, ECG changes are T-wave inversion and almost any dysrrhythmia may occur except sinus tachycardia, superventricular tachycardia (SVT) and rapid atrial fibrillation (A Fib). Digoxin toxicity may also cause sinus bradycardia, slow or regularized atrial fibrillation, AV blocks, premature ventricular contractions (PVCs) or ventricular tachycardia (VT).
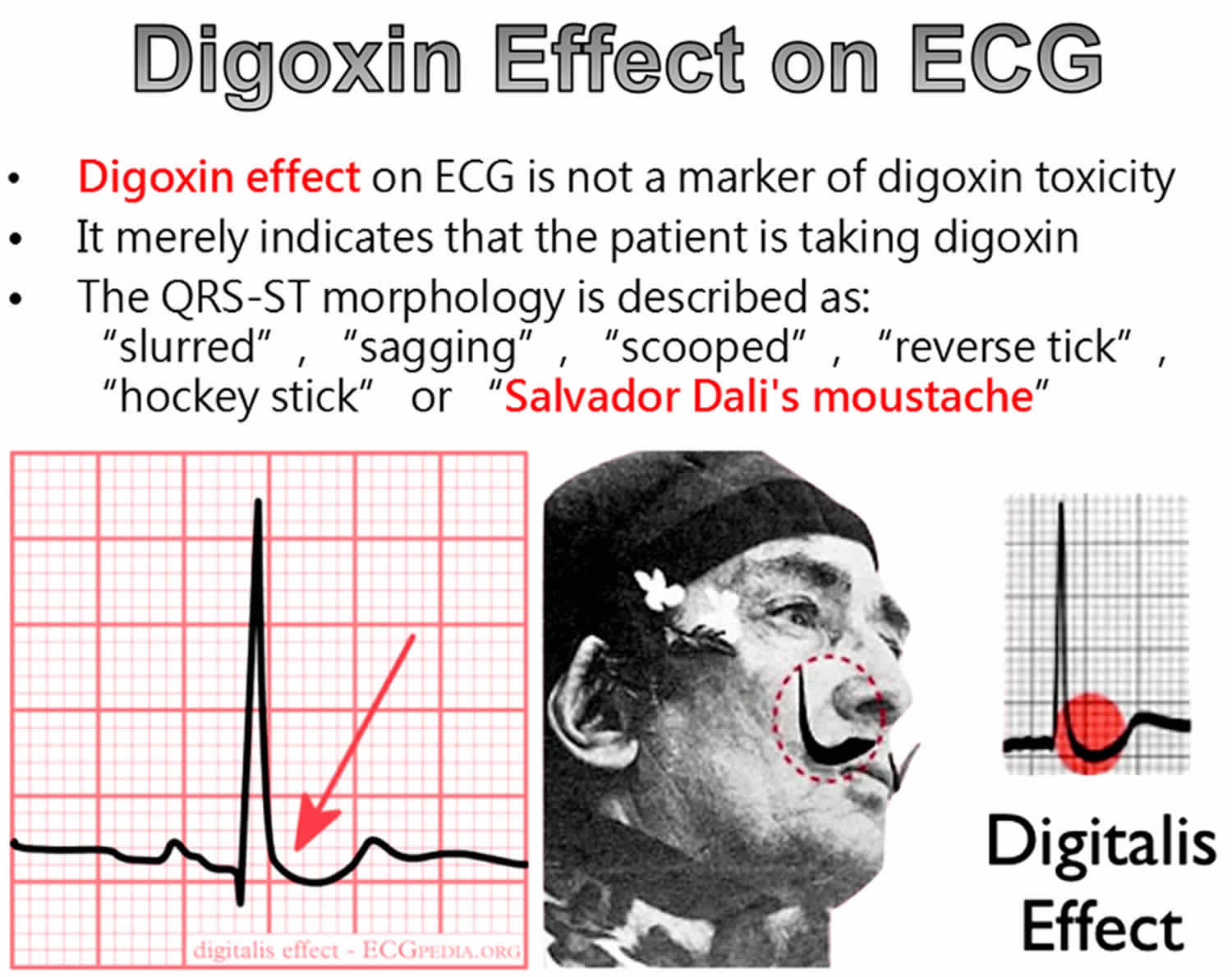
Digoxin toxicity should be separated from the normal digoxin effect that can occur in patients taking the expected dose of digoxin. The digoxin effect includes sagging ST segment depression, abnormal T waves (flat, inverted or biphasic) and a short QT.
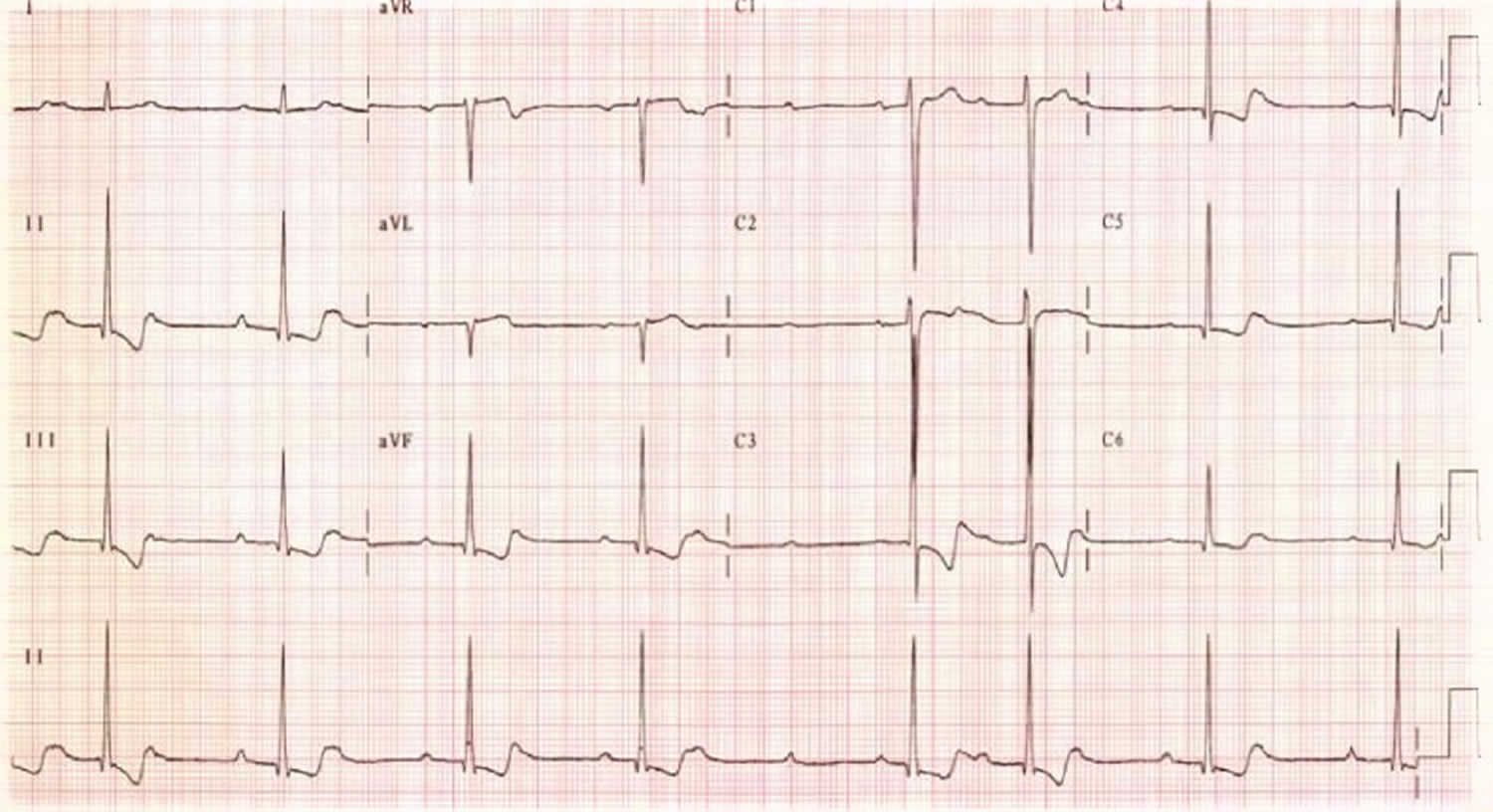
Figure 1. Digoxin toxicity ECG
Footnote: An example of an ECG after a digoxin overdose in a very unwell patient with all the digoxin toxicity symptoms and digoxin levels of 4.7 ug/L (therapeutic range 1–2 ug/L). Note the irregular bradycardia, atrioventricular block and T-wave inversion.
The ST-T complexes here are ‘scooping’ – consistent with a digitalis ‘effect’. In the digitalis effect, the ST segments are often likened to a ‘reverse tick’.
[Source 14) ]Figure 2. Digoxin effect ECG
Digoxin toxicity prevention
If you take digoxin, you should have your blood level checked regularly. Blood tests should also be done to check for conditions that make digoxin toxicity more common.
Potassium supplements may be prescribed if you take diuretics and digoxin together. A potassium-sparing diuretic may also be prescribed.
Signs and symptoms of digoxin toxicity
Patients can have an asymptomatic period of from several minutes to several hours after the oral ingestion of a single toxic dose. Clinical signs may be subtle or obvious, depending on the severity of toxicity. Acute toxicity is rarely subtle, whereas chronic toxicity may be difficult to diagnose. Nausea, vomiting, and drowsiness are among the most common extracardiac manifestations. Visual changes usually affect patients with chronic toxicity. Emphasis should be placed on the vital signs and the neurologic and cardiovascular findings.
The patient’s mentation may change according to the severity of digoxin toxicity, as well as associated comorbid conditions. Although the patient may note visual changes, the pupils are spared and objective findings are few. Drug-induced fever does not occur.
The pulse may be irregular if the patient has atrial fibrillation or arrhythmia arising from the digoxin toxicity itself. Hypotension may be observed if the patient has chronic heart failure or dehydration secondary to decreased oral intake. Neck findings include increased jugular venous pressure.
Hemodynamic instability is related directly to the presence of a dysrhythmia or to acute exacerbation of chronic heart failure (CHF). Associated cardiomegaly may be identified. Cardiovascular findings on physical examination relate to the severity of CHF, dysrhythmias, or hemodynamic instability.
The respiratory rate is sometimes increased. Basal crepitations are associated with CHF. Although GI symptoms are common, the abdominal examination is usually nonspecific. An enlarged liver secondary to CHF (ie, hepatic congestion) may be palpated. Hepatojugular reflux is present. Pedal edema is noted if the patient has renal failure or decompensated CHF.
Neurologic findings are related to changes in sensorium or mental status. Lateralizing findings usually indicate another disease process.
These are symptoms of digoxin toxicity:
- Confusion
- Irregular pulse
- Loss of appetite
- Nausea, vomiting, diarrhea
- Fast heartbeat
- Vision changes (unusual), including blind spots, blurred vision, changes in how colors look, or seeing spots
Other digoxin toxicity symptoms may include:
- Decreased consciousness
- Decreased urine output
- Difficulty breathing when lying down
- Excessive nighttime urination
- Overall swelling
Digitalis toxicity produces CNS (central nervous system), visual, gastrointestinal, and cardiac manifestations. Nausea, vomiting, and drowsiness are among the most common extracardiac manifestations.
CNS symptoms of digitalis toxicity include the following:
- Drowsiness
- Lethargy
- Fatigue
- Neuralgia
- Headache
- Dizziness
- Confusion or giddiness
- Hallucinations
- Seizures (rare)
- Paresthesias and neuropathic pain
Visual aberration often is an early indication of digitalis toxicity. Yellow-green distortion is most common, but red, brown, blue, and white distortions also occur. Drug intoxication also may cause the following:
- Snowy vision
- Photophobia
- Photopsia
- Decreased visual acuity
- Yellow halos around lights (xanthopsia)
- Transient amblyopia or scotomata
Gastrointestinal symptoms in acute or chronic toxicity include the following:
- Anorexia
- Weight loss
- Failure to thrive (in pediatric patients)
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
- Mesenteric ischemia (a rare complication of rapid IV infusion)
Cardiac symptoms
Cardiac symptoms include the following:
- Palpitations
- Shortness of breath
- Syncope
- Swelling of lower extremities
- Bradycardia
- Hypotension
- Dyspnea
Digoxin toxicity possible complications
Digoxin toxicity complications may include:
- Irregular heart rhythms, which may be deadly
- Heart failure
Digoxin toxicity diagnosis
Your health care provider will examine you. Your heart rate may be rapid, or slow and irregular.
An ECG is done to check for irregular heartbeats.
Blood tests that will be done include:
- Blood chemistry
- Kidney function tests, including BUN (blood urea nitrogen) and creatinine
- Digitoxin and digoxin test to check levels
- Potassium level
- Magnesium level
Serum digoxin level
- Therapeutic levels are 0.6-1.3 to 2.6 ng/mL. In general, normal values range from 0.5 to 1.9 nanograms per milliliter of blood. But the right level for some people may vary depending on the situation.
- Levels associated with toxicity overlap between therapeutic and toxic ranges
- False-negative assay results may occur with acute ingestion of nondigoxin cardiac glycosides (e.g., herbal compunds, such as foxglove or oleander)
- Levels determined less than 6-8 hours after an acute ingestion do not necessarily predict toxicity
The best way to guide therapy is to follow the digoxin level and correlate it with serum potassium concentrations and the patient’s clinical and ECG findings.
Electrolytes
- In acute toxicity, hyperkalemia is common
- Chronic toxicity is often accompanied by hypokalemia and hypomagnesemia
Electrocardiography
Digoxin toxicity may cause almost any dysrhythmia.
Classically, dysrhythmias associated with increased automaticity and decreased AV conduction occur
Sinus bradycardia and AV conduction blocks are the most common ECG changes in the pediatric population, while ventricular ectopy is more common in adults
Nonparoxysmal atrial tachycardia with heart block and bidirectional ventricular tachycardia are particularly characteristic of severe digitalis toxicity
Digoxin toxicity treatment
If the person has stopped breathing, call your local emergency number, then start CPR.
If the person is having trouble breathing, call your local emergency number.
At the hospital, symptoms will be treated as appropriate.
There are no evidence-based guidelines for the management of mild to moderate digoxin toxicity so there is a wide variation in treatment 15). Severe digoxin toxicity requires hospital admission and consideration of the need for digoxin-specific antibody fragments. Although digoxin-specific antibody fragments are safe and effective, randomized trials have not been performed.
The antibody fragments form complexes with the digoxin molecules. These complexes are then excreted in the urine.
Management
Supportive care of digoxin toxicity includes the following:
- Hydration with IV fluids
- Oxygenation and support of ventilatory function
- Discontinuation of the drug, and, sometimes, the correction of electrolyte imbalances
Gastrointestinal decontamination
- Activated charcoal is indicated for acute overdose or accidental ingestion
- Binding resins (e.g., cholestyramine) may bind enterohepatically-recycled digoxin
Treatment of electrolyte imbalance
- For hyperkalemia, use insulin plus glucose, and sodium bicarbonate if the patient is acidotic
- Treatment with digoxin Fab fragments is indicated for a K+ level greater than 5 mEq/L
- Hemodialysis may be necessary for uncontrolled hyperkalemia
- Correct hypokalemia (usually in chronic intoxication)
- Concomitant hypomagnesemia may result in refractory hypokalemia
Digoxin-specific antibody fragments
Digoxin-specific antibody fragments is considered the first-line treatment for significant dysrhythmias from digitalis toxicity.
Indications for digoxin-specific antibody fragments
The indications for digoxin-specific antibody fragments are inconsistent. Four contemporary sources 16), 17), 18), 19) recommend administration for strongly suspected or known digoxin toxicity with:
- life-threatening arrhythmia
- cardiac arrest
- potassium >5.0 mmol/L (significant hyperkalaemia is a strong indication for treatment because of its association with a poor prognosis if digoxin-specific antibody fragments are not given) 20).
However, the same sources vary in their recommendations for administration when there is:
- acute ingestion of >10 mg in adults or >4 mg in children
- evidence of end-organ dysfunction
- moderate to severe gastrointestinal symptoms
- serum digoxin concentration >12 nanogram/mL (i.e., 6-8 hours after acute ingestion or at baseline in chronic toxicity)
- significant clinical features of digoxin toxicity with serum digoxin concentration >1.6 nanogram/mL.
Such disagreements over when to use digoxin-specific antibody fragments arise from cost–benefit, not harm–benefit, considerations. The cost is roughly $1000 per ampoule and several ampoules may be used. However, economic arguments have been made for their use in non-life-threatening toxicity, as the duration of hospitalization may be reduced 21).
Dose and administration
Each ampoule contains 40 mg of powdered digoxin-specific antibody and is reconstituted with 4 mL of water. This can be given as a slow push in cardiac arrest, but otherwise the total dose is diluted further with normal saline and infused over 30 minutes.
The response begins about 20 minutes (range 0–60 min) after administration. A complete response occurs in 90 minutes (range 30–360 min) 22).
Conventional dosing protocols aim to neutralise total body digoxin completely. The total dose is usually expressed in vials. It depends on whether the post-distribution serum digoxin concentration is known, the amount ingested is known, or neither is known 23).
Known digoxin concentration
If the post-distribution concentration is known (in either acute or chronic ingestion), knowing the amount ingested is unnecessary. The dose is:
number of vials = post-distribution serum digoxin concentration (nanogram/mL) x weight (kg)/100
(multiply by 0.78 if SI units are used for post-distribution serum digoxin concentration).
Known amount ingested
If the quantity of digoxin ingested is known, but the post-distribution serum digoxin concentration is unknown, the dose is:
number of vials = amount ingested (mg) x 2 x 0.7
(0.7 is the bioavailability of digoxin tablets).
Unknown data
When neither the post-distribution serum digoxin concentration nor the amount ingested is known, use empiric dosing. Repeat in 30 minutes if the response is inadequate. The dose is:
- for adults and children greater than 20 kg
- five vials if hemodynamically stable
- 10 vials if unstable
- for children less than 20 kg
- one vial.
Other regimens
Some authors have argued for modification of the calculated doses to be given as an initial half dose followed by either further doses as required 24) or an infusion 25). These suggestions follow from the view that full dosing is unnecessary to achieve tolerable concentrations of digoxin and may be undesirable in patients who need digoxin 26). There are also concerns that significant amounts of digoxin-specific antibody fragments may be eliminated before full removal of digoxin from tissue stores 27). Furthermore, in practice many hospitals will not stock sufficient ampoules for the full calculated dose. In this case specialist toxicological advice should be sought on the adequacy of modified dosing.
Management of dysrhythmias
In hemodynamically stable patients, bradyarrhythmias and supraventricular arrhythmias may be treated with supportive care.
Short-acting beta blockers (eg, esmolol) may be helpful for supraventricular tachyarrhythmias with rapid ventricular rates, but may precipitate advanced or complete AV block in patients with sinoatrial or AV node depression
Phenytoin and lidocaine are useful for ventricular tachycardia if immune therapy is ineffective or unavailable
Phenytoin may suppress digitalis-induced tachydysrhythmias
Atropine has proved helpful in reversing severe sinus bradycardia
Magnesium sulfate may terminate dysrhythmias, but is contraindicated in the setting of bradycardia or AV block and should be used cautiously in patients with renal failure
Cardioversion for severe dysrhythmias due to digitalis can precipitate ventricular fibrillation and asystole but may be used if the patient is hemodynamically unstable and has a wide, complex tachycardia and if fascicular tachycardia has been ruled out
Criteria for hospital admission
- New cardiac dysrhythmias
- Severe bradyarrhythmias
- Advanced AV block
- Acute prolongation of the QRS interval
- Severe electrolyte abnormalities, especially hypokalemia or hyperkalemia
- Dehydration
- Inability to care for self
- Suicidal ideation
Digoxin toxicity side effects
Hypomagnesemia and, more importantly, hypokalemia (common with diuretic use) should be corrected before or during administration because digoxin-specific antibody fragments will further lower potassium 28). Hypokalemia occurs as a result of treatment in about 4% of patients.21 Serum potassium should be frequently monitored 29).
‘Rebound’ toxicity 30) is the reappearance of toxicity after an initial response to digoxin-specific antibody fragments. This occurs in about 2% of patients given a full neutralizing dose 31). It can develop 12–24 hours after treatment, but up to 10 days later in patients with renal failure 32). Serum digoxin concentration is of no use in diagnosis, because it measures the digoxin in the complexes with antibody fragments as well as unbound digoxin. The concentration therefore rises many fold after digoxin-specific antibody fragments are given even in the absence of rebound toxicity 33).
Heart failure or atrial fibrillation with rapid ventricular response (presumed re-emergent due to removal of digoxin effect) occurs in up to 3% of patients 34). Allergic reactions occur in about 1% of infusions 35).
Digoxin toxicity prognosis
How well a person does depends on the severity of the toxicity and if it has caused an irregular heart rhythm.
References [ + ]