Contents
Gentamicin
Gentamicin is a parenterally administered, broad spectrum aminoglycoside antibiotic typically used for moderate to severe bacterial infections, primarily gram negative bacteria and some aerobic gram positive organisms. Like other aminoglycosides, gentamicin is thought to act by binding to bacterial ribosomes and inhibiting protein synthesis. Nevertheless, gentamicin is considered bacteriocidal as well as bacteriostatic. Gentamicin and other aminoglycosides are typically used in combination with a penicillin or cephalosporin for treatment of severe infections with E. coli, Staphylococcus aureus, Enterobacter, Klebsiella, Serratia, Pseudomonas aeruginosa, and other gram negative bacteria resistant to less toxic antibiotics. Gentamicin is most commonly used for septicemia, bacterial endocarditis, peritonitis, meningitis, pelvic inflammatory disease and pneumonia. Gentamicin was first approved for use in the United States in 1970 and remains in wide use. Gentamicin is available in multiple generic parenteral formulations and the typical adult dose is 3 to 5 mg/kg per day intramuscularly (into a muscle) (IM) or intravenously (into a vein) (IV), usually in three divided doses and often after a loading dose. When gentamicin is injected intravenously, it is usually infused (injected slowly) over a period of 30 minutes to 2 hours once every 6 or 8 hours. Doses must be modified based upon renal function and monitoring of drug levels is advisable. The length of your treatment depends on the type of infection you have. Topical formulations are also available for local wound, tissue and ophthalmologic anti-bacterial therapy.
You may receive gentamicin injection in a hospital or you may administer the medication at home. If you will be receiving gentamicin injection at home, your healthcare provider will show you how to use the medication. Be sure that you understand these directions, and ask your healthcare provider if you have any questions.
You should begin to feel better during the first few days of treatment with gentamicin injection. If your symptoms do not improve or get worse, call your doctor.
Use gentamicin injection until you finish the prescription, even if you feel better. If you stop using gentamicin injection too soon or skip doses, your infection may not be completely treated and the bacteria may become resistant to antibiotics.
Gentamicin common side effects of gentamicin include dizziness, headache, confusion, nausea and skin rash. Important, dose related adverse effects include ototoxicity and nephrotoxicity, which are shared by all aminoglycosides.
Gentamicin may cause serious kidney problems. Kidney problems may occur more often in older people or in people that are dehydrated. Tell your doctor if you have or have ever had kidney disease. If you experience any of the following symptoms, call your doctor immediately: decreased urination; swelling of the face, arms, hands, feet, ankles, or lower legs; or unusual tiredness or weakness.
Gentamicin may cause serious hearing problems. Hearing problems may occur more often in older people. Hearing loss may be permanent in some cases. Tell your doctor if you have or have ever had dizziness, vertigo, hearing loss, or ringing in the ears. If you experience any of the following symptoms, call your doctor immediately: hearing loss, roaring or ringing in the ears, or dizziness.
Gentamicin may cause nerve problems. Tell your doctor if you have or have ever had burning or tingling in the hands, arms, feet, or legs; muscle twitching or weakness; or seizures.
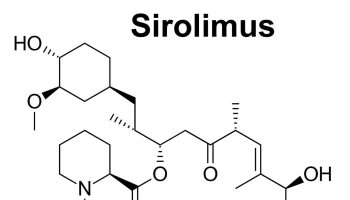
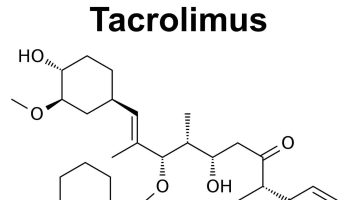
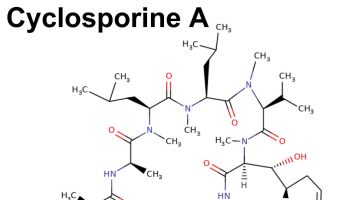
The risk that you will develop serious kidney, hearing, or other problems is greater if you are taking certain prescription or nonprescription medications. Tell your doctor and pharmacist if you are taking acyclovir (Zovirax, Sitavig); amphotericin (Abelcet, Ambisome, Amphotec); capreomycin (Capastat); certain cephalosporin antibiotics such as cefazolin (Ancef, Kefzol), cefixime (Suprax), or cephalexin (Keflex); cisplatin; colistin (Coly-Mycin S); cyclosporine (Gengraf, Neoral, Restasis, Sandimmune); diuretics (‘water pills’) such as bumetanide, ethacrynic acid (Edecrin), furosemide (Lasix), or torsemide (Demadex). other aminoglycoside antibiotics such as amikacin, kanamycin, neomycin (Neo-Fradin), paromomycin, streptomycin, and tobramycin; polymyxin B; or vancomycin (Vanocin). Your doctor may not want you to receive gentamicin injection.
Tell your doctor if you are pregnant or plan to become pregnant. If you become pregnant while using gentamicin injection, call your doctor immediately. Gentamicin may harm the fetus.
Keep all appointments with your doctor and the laboratory. Your doctor will order certain tests, including hearing tests, before and during treatment to check your body’s response to gentamicin.
Gentamicin drops
- Gentamicin ophthalmic preparations are used to treat infections of the eye.
- Gentamicin otic preparations are used to treat infections of the ear canal.
Gentamicin is available only with your doctor’s prescription.
Gentamicin otic preparations
To use:
- Lie down or tilt the head so that the infected ear faces up. Gently pull the earlobe up and back for adults (down and back for children) to straighten the ear canal. Drop the medicine into the ear canal. Keep the ear facing up for about 1 or 2 minutes to allow the medicine to come into contact with the infection. A sterile cotton plug may be gently inserted into the ear opening to prevent the medicine from leaking out.
- To keep the medicine as germ-free as possible, do not touch the applicator tip to any surface (including the ear). Also, keep the container tightly closed.
To help clear up your infection completely, keep using this medicine for the full time of treatment, even if your symptoms have disappeared. Do not miss any doses.
Gentamicin ophthalmic preparations
For patients using the eye drop form of this medicine:
The bottle is only partially full to provide proper drop control.
To instill the eye drops, follow these steps:
- Wash your hands thoroughly with soap and water.
- Check the dropper tip to make sure that it is not chipped or cracked.
- Avoid touching the dropper tip against your eye or anything else; eye drops and droppers must be kept clean.
- While tilting your head back, pull down the lower lid of your eye with your index finger to form a pocket.
- Hold the dropper (tip down) with the other hand, as close to the eye as possible without touching it.
- Brace the remaining fingers of that hand against your face.
- While looking up, gently squeeze the dropper so that a single drop falls into the pocket made by the lower eyelid. Remove your index finger from the lower eyelid.
- Close your eye for 2 to 3 minutes and tip your head down as though looking at the floor. Try not to blink or squeeze your eyelids.
- Place a finger on the tear duct and apply gentle pressure.
- Wipe any excess liquid from your face with a tissue.
- If you are to use more than one drop in the same eye, wait at least 5 minutes before instilling the next drop.
- Replace and tighten the cap on the dropper bottle. Do not wipe or rinse the dropper tip.
- Wash your hands to remove any medication.
For patients using the eye ointment form of this medicine:
To apply the eye ointment, follow these steps:
- Wash your hands thoroughly with soap and water.
- Use a mirror or have someone else apply the ointment.
- Avoid touching the tip of the tube against your eye or anything else. The ointment must be kept clean.
- Tilt your head forward slightly.
- Holding the tube between your thumb and index finger, place the tube as near as possible to your eyelid without touching it.
- Brace the remaining fingers of that hand against your cheek or nose.
- With the index finger of your other hand, pull the lower lid of your eye down to form a pocket.
- Place a small amount of ointment into the pocket made by the lower lid and the eye. A 1/2-inch (1.25-centimeter) strip of ointment usually is enough unless otherwise directed by your doctor.
- Gently close your eyes and keep them closed for 1 to 2 minutes to allow the medication to be absorbed.
- Replace and tighten the cap right away.
- Wipe off any excess ointment from your eyelids and lashes with a clean tissue. Wash your hands again.
To help clear up your infection completely, keep using this medicine for the full time of treatment, even if your symptoms have disappeared. Do not miss any doses.
Gentamicin mechanism of action
Gentamicin has bactericidal activity in which it binds to the bacteria ribosomal 30S subunit 1. Specifically, gentamicin is believed to bind to the A-site on the 16S rRNA, a component of the ribosomal 30S subunit. Through this binding, the genetic code gets misread, and the translation is disrupted, leading to the bacteria being unable to carry out protein synthesis 2.
Gentamicin contraindications
Gentamicin should be avoided in patients with myasthenia gravis because of the risk of prolonged neuromuscular blockade.
Gentamicin special precautions
Before using gentamicin injection:
- tell your doctor and pharmacist if you are allergic to gentamicin injection; other aminoglycoside antibiotics such as amikacin, kanamycin, neomycin, paromomycin, streptomycin, or tobramycin; sulfites; any other medications; or any of the ingredients in gentamicin injection. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, and nutritional supplements, you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following: other antibiotics such as amoxicillin (Amoxil, Larotid, Moxatag, in Augmentin, in Prevpac), ampicillin, or penicillin; dimenhydrate (Dramamine); meclizine (Bonine); or nonsteroidal anti-inflammatory drugs such as indomethacin (Indocin, Tivorbex). Your doctor may need to change the doses of your medications or monitor you carefully for side effects. Many other medications may also interact with gentamicin, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list.
- tell your doctor if you are or have or have ever had cystic fibrosis (an inherited condition that affects the lungs and digestive system), problems with your muscles such as myasthenia gravis or Parkinson’s disease.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are using gentamicin injection.
Pregnancy
Pregnancy Category D: Studies in pregnant women have demonstrated a risk to the fetus. However, the benefits of therapy in a life threatening situation or a serious disease, may outweigh the potential risk.
Using gentamicin while you are pregnant can harm your unborn baby. Use an effective form of birth control to keep you from getting pregnant. If you think you have become pregnant while using gentamicin, tell your doctor right away.
Comments:
- Therapeutic blood levels in the mother do not equate with safety for the fetus.
- Some experts recommend: Aminoglycosides should be considered potentially ototoxic and nephrotoxic to the fetus.
- If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential harm to the fetus.
Breastfeeding
Studies in women suggest that this medication poses minimal risk to the infant when used during breastfeeding.
Comments:
- The American Academy of Pediatrics considers this drug compatible with breastfeeding.
- The WHO (World Health Organization) considers this drug compatible with breastfeeding; breastfed infants should be monitored for thrush and diarrhea.
- Breastfed infants should be monitored for candidiasis and gastrointestinal side effects (e.g., diarrhea, thrush, diaper rash, antibiotic-associated colitis).
Gentamicin Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are receiving gentamicin, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using gentamicin with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Ataluren
Using gentamicin with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Agalsidase Alfa
- Alcuronium
- Atracurium
- Cholera Vaccine, Live
- Cidofovir
- Cisatracurium
- Colistimethate Sodium
- Decamethonium
- Digoxin
- Doxacurium
- Ethacrynic Acid
- Fazadinium
- Foscarnet
- Furosemide
- Gallamine
- Hexafluorenium
- Lysine
- Metocurine
- Mivacurium
- Pancuronium
- Pipecuronium
- Rapacuronium
- Rocuronium
- Succinylcholine
- Tubocurarine
- Vancomycin
- Vecuronium
Using gentamicin with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Indomethacin
- Methoxyflurane
- Polygeline
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of gentamicin. Make sure you tell your doctor if you have any other medical problems, especially:
- Asthma or
- Sulfite allergy, history of—This medicine contains sodium metabisulfite which may cause an allergic reaction in patients with these conditions.
- Hypocalcemia (low calcium in the blood) or
- Hypokalemia (low potassium in the blood) or
- Hypomagnesemia (low magnesium in the blood)—Should be corrected before receiving this medicine. If these conditions are not corrected, this medicine may increase risk for more serious side effects.
- Kidney disease—Use with caution. The effects may be increased because of slower removal of this medicine from the body.
- Muscle problems or
- Myasthenia gravis (severe muscle weakness) or
- Nerve problems—Use with caution. May make these conditions worse.
Gentamicin uses
Gentamicin injection is used to treat certain serious infections that are caused by bacteria such as meningitis (infection of the membranes that surround the brain and spinal cord) and infections of the blood, abdomen (stomach area), lungs, skin, bones, joints, and urinary tract.
Gentamicin is also sometimes used to treat pelvic inflammatory disease, granuloma inguinale (donovanosis; a sexually transmitted disease), and other serious infections such as the plague and tularemia. Talk to your doctor about the risks of using this medication for your condition.
Antibiotics such as gentamicin injection will not work for colds, flu, or other viral infections. Taking antibiotics when they are not needed increases your risk of getting an infection later that resists antibiotic treatment.
Monitoring
Therapeutic drug monitoring is necessary with gentamicin to optimize patient outcome and limit toxicity. However, there is no universal agreement on the method of monitoring. Therapeutic drug monitoring has shown to reduce hospital stay duration and toxicities. Studies also suggest that therapeutic drug monitoring reduces mortality. It is important to note that monitoring clearance should be considered in critically ill, burn, and obese patients due to their abnormal distribution volume 3.
For toxicity purposes, renal function and cochlear function require monitoring. Serial audiometry may be considered to prevent irreversible hearing loss. Additionally, monitoring serum creatinine must be done to assess for nephrotoxicity in patients requiring gentamicin therapy 4.
Gentamicin dose
Gentamicin injection dose
A nurse or other trained health professional will give you the gentamicin injection. Gentamicin is given as a shot into a muscle or into a vein.
To help clear up your infection completely, keep using gentamicin for the full time of treatment, even if you begin to feel better after a few days. Also, gentamicin works best when there is a constant amount in the blood. To help keep the amount constant, you must receive gentamicin on a regular schedule.
To keep your kidneys working well and help prevent kidney problems, drink extra fluids so you will pass more urine while you or your child are receiving gentamicin.
Your doctor will check your progress closely while you or your child are receiving gentamicin. This will allow your doctor to see if the gentamicin is working properly and to decide if you or your child should continue to receive it. Blood, urine, hearing, and nerve tests may be needed to check for unwanted effects.
Adult dose
- Systemic infections: 1 mg/kg IM or IV infusion (over 30 to 120 minutes) every 8 hours
- Duration of therapy: 7 to 10 days
Children dose
- Premature and full-term neonates 1 week of age or less: 2.5 mg/kg IM or IV every 12 hours
- Neonates and infants: 2.5 mg/kg IM or IV every 8 hours
- Children: 2 to 2.5 mg/kg IM or IV every 8 hours
- Duration of therapy: 7 to 10 days
American Academy of Pediatrics (AAP) Recommendations:
Severe Infections:
- 7 days or younger and 2 kg or less: 5 mg IM or IV every 48 hours
- 7 days or younger and greater than 2 kg: 4 mg IM or IV every 24 hours
- 8 to 28 days and 2 kg or less: 5 mg IM or IV every 24 hours
- 8 to 28 days and greater than 2 kg: 4 to 5 mg IM or IV every 24 hours
- Older than 28 days: 6 to 7.5 mg IM or IV in 2 to 3 doses OR 5 to 7.5 mg IM or IV once a day
Gentamicin ophthalmic dose
The amount of gentamicin that you take depends on the strength of the gentamicin. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take gentamicin depend on the medical problem for which you are using the gentamicin.
For gentamicin ophthalmic ointment dosage form:
- For eye infections: Adults and children—Use every eight to twelve hours.
For ophthalmic solution (eye drops) dosage form:
- For mild to moderate eye infections: Adults and children—One to two drops every four hours.
- For severe eye infections: Adults and children—One to two drops as often as once every hour as directed by your doctor.
Missed Dose
If you miss a dose of gentamicin, apply it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule.
Gentamicin otic dose
The amount of gentamicin that you take depends on the strength of the gentamicin. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take gentamicin depend on the medical problem for which you are using the gentamicin.
For gentamicin ear drops dosage form:
- For ear infections:
- Adults and children 6 years of age and older—Place three or four drops in the infected ear three times a day.
- Children younger than 6 years of age—Use and dose must be determined by your doctor.
Missed Dose
If you miss a dose of gentamicin, apply it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule.
Gentamicin side effects
The main noted adverse effects of gentamicin are ototoxicity (toxic to the ear), nephrotoxicity (toxic to the kidneys) and neuromuscular blockade. Therefore, patients should be educated to look out for warning signs of these adverse effects before the initiation of gentamicin therapy 5.
Gentamicin-induced ototoxicity has been reported to occur in 2 to 45% of adults. The ototoxicity can be vestibular and/or cochlear and is typically dose-dependent. Gentamicin, streptomycin, and tobramycin more commonly cause vestibular damage while amikacin and kanamycin result in more cochlear damage 6. Studies have found that gentamicin seems to create reactive oxygen species within the inner ear; this, in turn, causes damage to the vestibular and cochlear sensory cells along with cochlear neurons. Often the vestibular loss is salvageable while hearing loss is irreversible 7.
Nephrotoxicity due to gentamicin may appear 10 to 25% of patients. In patients receiving gentamicin therapy, renal tubular toxicity decreased blood flow to the kidneys, and reduced GFR most commonly causes the nephrotoxicity seen. Renal effects with gentamicin generally are reversible. Furthermore, there are risk factors associated with the development of gentamicin-induced nephrotoxicity including dehydration, pregnancy, and hepatic dysfunction. Taking other medications concurrently with gentamicin that can cause nephrotoxicity, such as nonsteroidal anti-inflammatory drugs (NSAIDs), cyclosporine, and diuretics, also put a patient at risk for renal problems. It is important to monitor patient renal function when taking gentamicin 4.
Gentamicin have also demonstrated correlations with neuromuscular blockade. Although this is less common than ototoxicity and nephrotoxicity, patients with diseases affecting the neuromuscular junction and patients using medications prolonging neuromuscular blockade, most notably calcium channel blockers, should be cautious when using gentamicin 8.
Gentamicin may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- vomiting
- diarrhea
- decreased appetite
- pain at the injection site
- headache
- fever
- joint pain
- unusual tiredness
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- rash
- peeling or blistering of the skin
- itching
- hives
- swelling of the eyes, face, throat, tongue, or lips
- difficulty breathing or swallowing
- hoarseness
Incidence not known
- abdominal or stomach cramps or pain
- agitation
- back pain
- black, tarry stools
- blood in the urine
- blurred or double vision
- burning, numbness, tingling, or painful sensations
- change in frequency of urination or amount of urine
- chest pain
- chills
- coma
- confusion
- continuing ringing or buzzing or other unexplained noise in the ears
- cough
- difficult or troubled breathing
- difficulty with swallowing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- drowsiness
- dry mouth
- eye pain
- fast heartbeat
- fever with or without chills
- hallucinations
- headache
- hearing loss
- hives
- hoarseness
- increased thirst
- irregular heartbeats
- irregular, fast or slow, or shallow breathing
- irritability
- itching
- joint pain
- loss of appetite
- mood or mental changes
- muscle cramps in the hands, arms, feet, legs, or face
- muscle pain or weakness
- muscle spasms (tetany) or twitching
- nausea or vomiting
- nervousness
- numbness and tingling around the mouth, fingertips, or feet
- pale or blue lips, fingernails, or skin
- pale skin
- pinpoint red spots on the skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- right upper abdominal or stomach pain and fullness
- seizures
- sensation of spinning
- skin rash
- slow or fast heartbeat
- slow or irregular breathing
- sore throat
- sores, ulcers, or white spots on the lips or in the mouth
- stiff neck
- sweating
- swelling of the feet or lower legs
- swollen glands
- tightness in the chest
- trembling
- unusual bleeding or bruising
- unusual tiredness or weakness
- weight chest discomfort
- weight loss
- wheezing
Gentamicin may cause other side effects. Call your doctor if you have any unusual problems while using gentamicin.
Gentamicin toxicity
There is no antidote for toxicities of gentamicin. However, agents with protective effects on the ear and kidney may help prevent gentamicin-induced toxicity. In particular, N-acetylcysteine demonstrates promising protective effects on patients using gentamicin 9.
- Block M, Blanchard DL. Aminoglycosides. [Updated 2019 May 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541105[↩]
- Krause KM, Serio AW, Kane TR, Connolly LE. Aminoglycosides: An Overview. Cold Spring Harb Perspect Med. 2016 Jun 01;6, 6[↩]
- Roberts JA, Norris R, Paterson DL, Martin JH. Therapeutic drug monitoring of antimicrobials. Br J Clin Pharmacol. 2012 Jan;73(1):27-36[↩]
- Wargo KA, Edwards JD. Aminoglycoside-induced nephrotoxicity. J Pharm Pract. 2014 Dec;27(6):573-7[↩][↩]
- Avent ML, Rogers BA, Cheng AC, Paterson DL. Current use of aminoglycosides: indications, pharmacokinetics and monitoring for toxicity. Intern Med J. 2011 Jun;41(6):441-9[↩]
- Leis JA, Rutka JA, Gold WL. Aminoglycoside-induced ototoxicity. CMAJ. 2015 Jan 06;187(1):E52[↩]
- Guthrie OW. Aminoglycoside induced ototoxicity. Toxicology. 2008 Jul 30;249(2-3):91-6.[↩]
- Barrons RW. Drug-induced neuromuscular blockade and myasthenia gravis. Pharmacotherapy. 1997 Nov-Dec;17(6):1220-32[↩]
- Vural A, Koçyiğit İ, Şan F, Eroğlu E, Ketenci İ, Ünal A, Tokgöz B, Ünlü Y. Long-Term Protective Effect of N-Acetylcysteine against Amikacin-Induced Ototoxicity in End-Stage Renal Disease: A Randomized Trial. Perit Dial Int. 2018 Jan-Feb;38(1):57-62[↩]