Contents
Water and Electrolyte Balance
Two types of substances that are important in maintaining homeostasis in the body are water and electrolytes. Electrolytes are minerals in your body that have an electric charge. They are in your blood, urine and body fluids. Maintaining the right balance of electrolytes helps your body’s blood chemistry, the amount of water in your body, the acidity of your blood (pH), muscle action and other important processes 1. Sodium, calcium, potassium, chlorine, phosphate and magnesium are all electrolytes 2. You get them from the foods you eat and the fluids you drink.
Electrolytes can be acids, bases, or salts 3. They can be measured by different blood tests. Each electrolyte can be measured separately, such as:
- Ionized calcium
- Serum calcium
- Serum chloride
- Serum magnesium
- Serum phosphorus
- Serum potassium
- Serum sodium
Note: Serum is the part of blood that doesn’t contain cells.
Water retention, dehydration and water intoxication are among the more common disorders that involve a water imbalance in body fluids.
For homeostasis, water balance and electrolyte balance must be maintained; that is, the quantities entering the body must equal the quantities leaving it 4. In other word, homeostasis requires control of both water intake and water output. Water balance exists when water intake equals water output. Therefore, the body requires mechanisms to:
- Replace lost water and electrolytes, and
- Excrete any excess water and electrolytes.
Levels of electrolytes in your body can become too low or too high. That can happen when the amount of water in your body changes, causing dehydration or overhydration. Causes include some medicines, vomiting, diarrhea, sweating or kidney problems 2. Problems most often occur with levels of sodium, potassium or calcium.
Water balance and electrolyte balance are interdependent because electrolytes are dissolved in the water of body fluids. Consequently, anything that alters the concentrations of the electrolytes will alter the concentration of the water, either by adding solutes to it or by removing solutes from it. Likewise, anything that changes the concentration of water will change concentrations of the electrolytes by concentrating or diluting them.
Water balance
- Water Intake
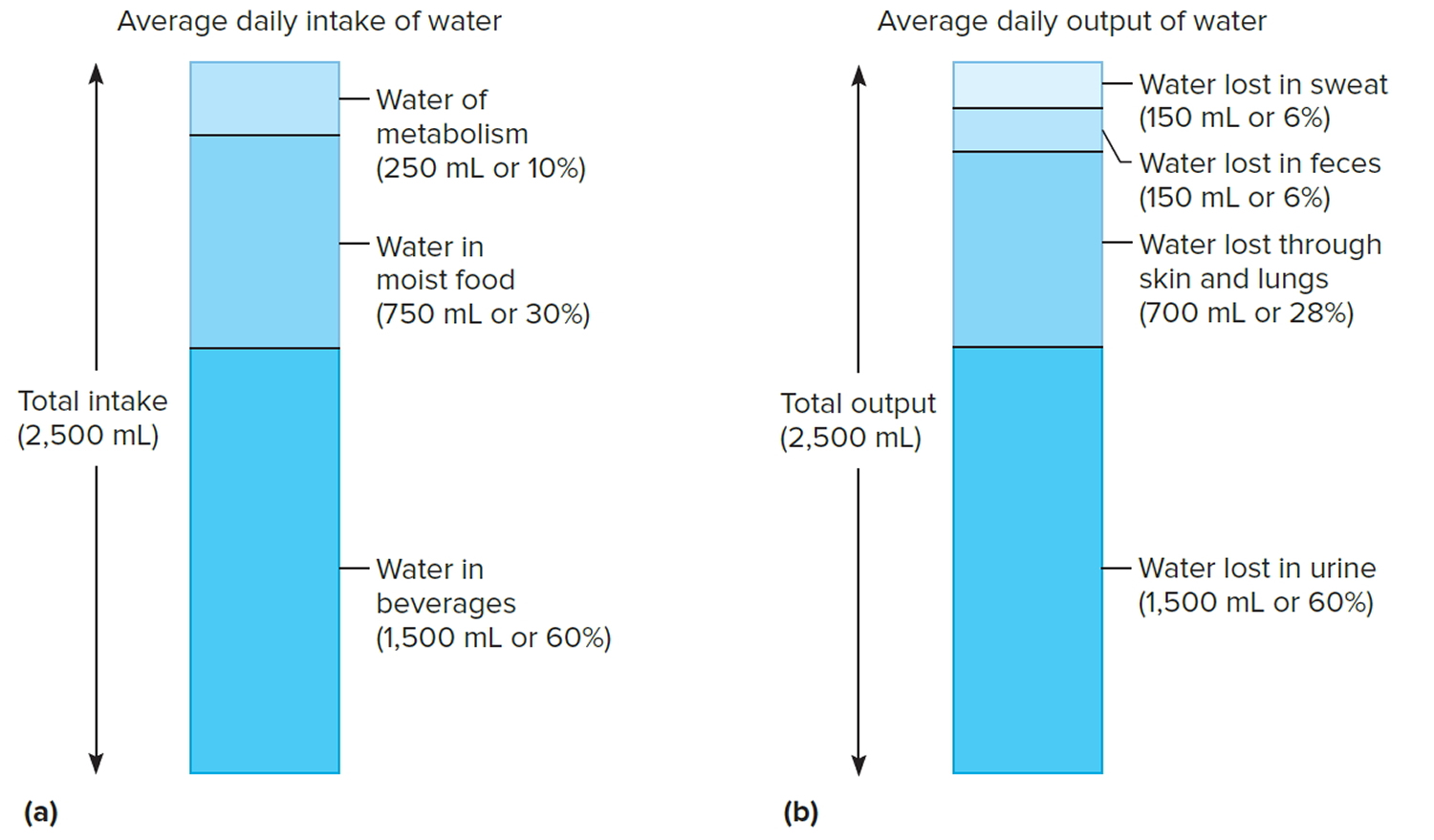
The volume of water gained each day varies among individuals. An average adult living in a moderate environment takes in about 2.5 liters. Probably 60% is obtained from drinking water or beverages, and another 30% comes from moist foods. The remaining 10% is a by-product of the oxidative metabolism of nutrients, called water of metabolism.
The primary regulator of water intake is thirst. The intense feeling of thirst derives from the osmotic pressure of extracellular fluids and both neural and hormonal input to the brain. As the body loses water, the osmotic pressure of extracellular fluids increases. Such a change stimulates osmoreceptors in the hypothalamus, and in response, the hypothalamus causes the person to feel thirsty and to seek water.
Thirst is a homeostatic mechanism, normally triggered when total body water decreases by as little as 1%. The act of drinking and the resulting distension of the stomach wall trigger impulses that inhibit the thirst mechanism. In this way, drinking stops even before the swallowed water is absorbed, preventing the person from drinking more than is required to replace the volume lost, avoiding development of an imbalance.
- Water Output
Water normally enters the body only through the mouth, but it can be lost by a variety of routes. These include obvious losses in urine, feces, and sweat (sensible perspiration), as well as evaporation of water from the skin (insensible perspiration) and from the lungs during breathing.
If an average adult takes in 2.5 liters of water each day, then 2.5 liters must be eliminated to maintain water balance. Of this volume, perhaps 60% is lost in urine, 6% in feces, and 6% in sweat. About 28% is lost by evaporation from the skin and lungs. These percentages vary with such environmental factors as temperature
and relative humidity and with physical exercise.
The primary means of regulating water output is urine production. The renal distal convoluted tubules of the nephrons and collecting ducts are the effectors of the mechanism that regulates urine volume. The epithelial linings in these structures remain relatively impermeable to water unless antidiuretic hormone (ADH) is present. Antidiuretic hormone (ADH) increases the permeability of the distal convoluted tubule and collecting duct, thereby increasing water reabsorption and reducing urine production. In the absence of antidiuretic hormone (ADH), less water is reabsorbed and more urine is produced.
Figure 1. Water balance
Note: Water balance. (a) Major sources of body water. (b) Routes by which the body loses water.
[Source 4]Electrolyte balance
Electrolyte balance exists when the quantities of electrolytes the body gains equal those lost. Homeostatic mechanisms maintain electrolyte balance. This involves keeping the associated ions in appropriate concentrations within the plasma and the interstitial fluid.
- Electrolyte Intake
The electrolytes of greatest importance to cellular functions dissociate to release sodium, potassium, calcium, magnesium, chloride, sulfate, phosphate, bicarbonate, and hydrogen ions. These electrolytes are primarily obtained from foods, but they may also be found in drinking water and other beverages. In addition, some electrolytes are by-products of metabolic reactions.
Ordinarily, a person obtains sufficient electrolytes by responding to hunger and thirst. However, a severe electrolyte deficiency may cause salt craving, which is a strong desire to eat salty foods.
- Electrolyte Output
The body loses some electrolytes by perspiring, with more lost in sweat on warmer days and during strenuous exercise. Varying amounts of electrolytes are lost in the feces. The greatest electrolyte output occurs as a result of kidney function and urine production. The kidneys alter electrolyte output to maintain the proper composition of body fluids, thereby promoting homeostasis.
Precise concentrations of positively charged ions, such as sodium (Na+), potassium (K+), and calcium (Ca+2), are required for impulse conduction along an axon, muscle fiber contraction, and maintenance of cell membrane potential. Sodium ions account for nearly 90% of positively charged ions in extracellular fluids. The kidneys and the hormone aldosterone regulate these ions. Aldosterone, which the adrenal cortex secretes, increases sodium ion reabsorption in the distal convoluted tubules of the kidneys’ nephrons and in the collecting ducts.
Aldosterone also regulates potassium ion concentration. A rising potassium ion concentration directly stimulates cells of the adrenal cortex to secrete aldosterone. This hormone enhances tubular secretion of potassium ions at the same time that it causes tubular reabsorption of sodium ions.
The calcium ion concentration dropping below normal directly stimulates the parathyroid glands to secrete parathyroid hormone. This hormone returns the concentration of calcium in extracellular fluids toward normal.
Generally the regulatory mechanisms that control positively charged ions secondarily control the concentrations of negatively charged ions. For example, chloride ions (Cl−), the most abundant negatively charged ions in extracellular fluids, are passively reabsorbed in response to the active tubular reabsorption of sodium ions. That is, the negatively charged chloride ions are electrically attracted to positively charged sodium ions and accompany them as they are reabsorbed. Water is then reabsorbed by osmosis.
Active transport mechanisms with limited transport capacities partially regulate some negatively charged ions, such as phosphate ions (PO4−3) and sulfate ions (SO4−2). Therefore, if the extracellular phosphate ion concentration is low, renal tubules reabsorb phosphate ions. On the other hand, if the renal plasma threshold is exceeded, excess phosphate is excreted in urine.
Distribution of Body Fluids
Body fluids are not uniformly distributed. Instead, they occupy regions, or compartments, of different volumes that contain fluids of varying compositions. The movement of water and electrolytes between these compartments is regulated to stabilize both the distribution and the composition of body fluids.
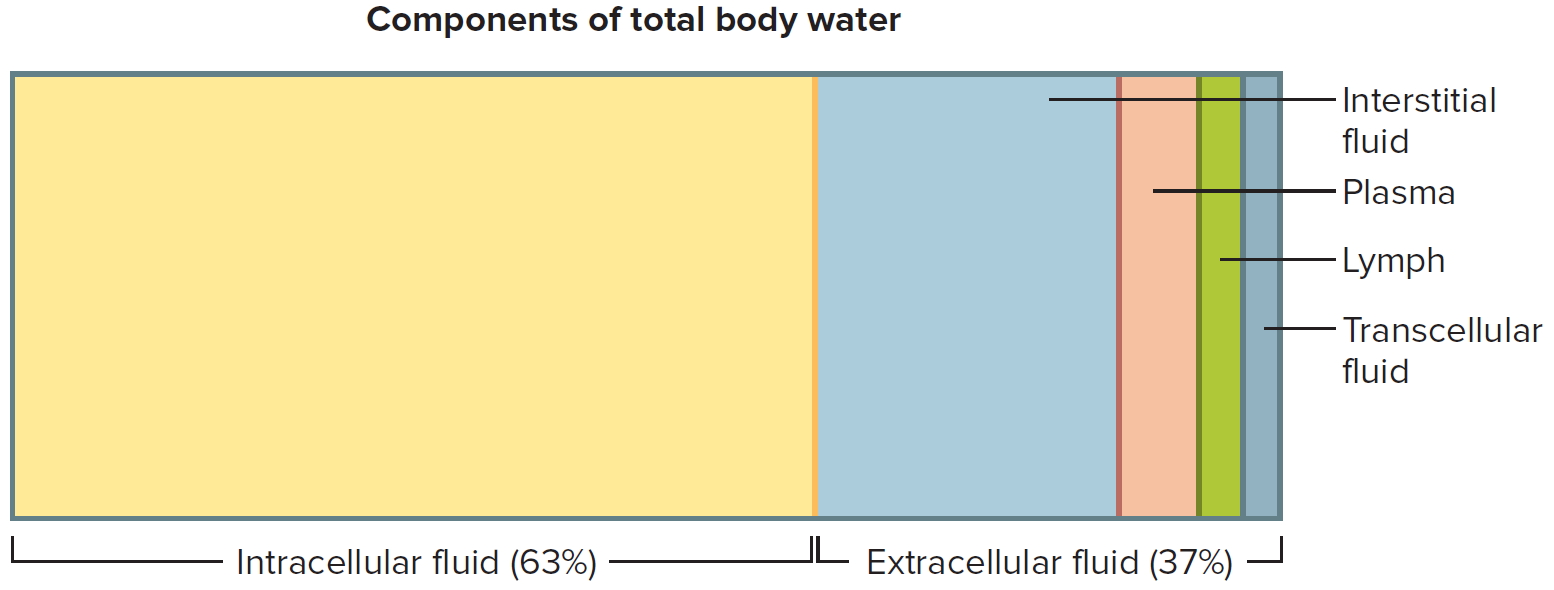
Fluid Compartments
The body of an average adult female is about 52% water by weight and that of an average male is about 63% water by weight. The reason for this difference is that females generally have more adipose tissue, which contains little water 4. Males generally have proportionately more muscle tissue, which contains a great deal of water. Water in the adult human body (about 40 liters), with its dissolved electrolytes, is distributed into two major compartments: an intracellular fluid compartment and an extracellular fluid compartment. The intracellular fluid compartment includes all the water and electrolytes that cell membranes enclose. In other words, intracellular fluid is the fluid inside cells. In an adult it accounts for about 63% by volume of total body water.
The extracellular fluid compartment includes all the fluid outside of cells—in tissue spaces (interstitial fluid), blood vessels (plasma), and lymphatic vessels (lymph). Transcellular fluid, a type of extracellular fluid, is found in cavities separated from other extracellular fluids by epithelial or connective tissue membranes. Transcellular fluid includes cerebrospinal fluid of the central nervous system, aqueous and vitreous humors of the eyes, synovial fluid of the joints, and serous fluid in the body cavities. The fluids of the extracellular compartment constitute about 37% by volume of total body water.
Figure 2. Components of total body water
[Source 4]Body Fluid Composition
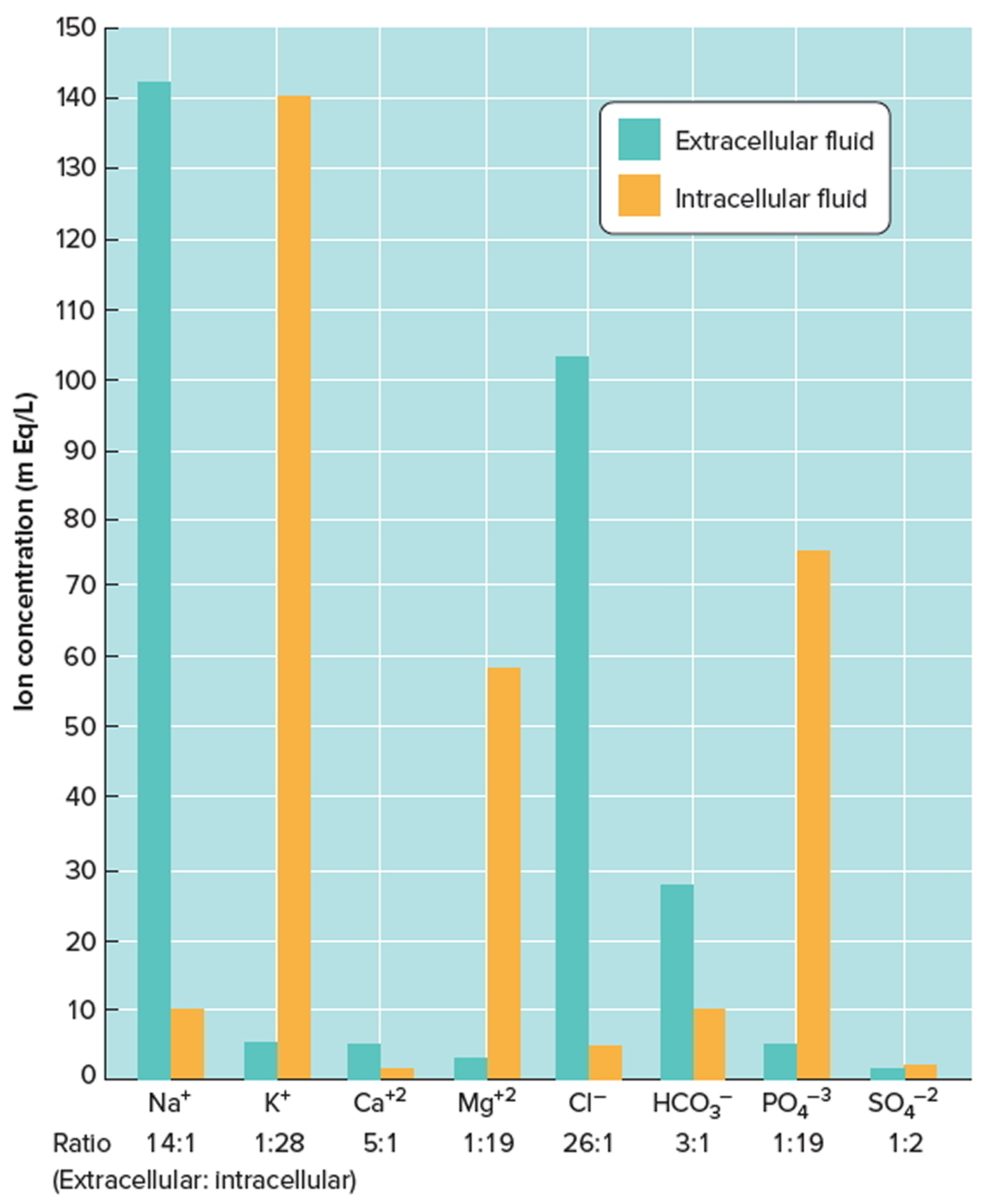
- Extracellular fluids generally are similar in composition, including high concentrations of sodium, chloride, calcium, and bicarbonate ions and lesser concentrations of potassium, magnesium, phosphate, and sulfate ions. The blood plasma portion of extracellular fluid has considerably more protein than does either interstitial fluid or lymph.
- Intracellular fluid has high concentrations of potassium, phosphate, and magnesium ions. It includes a greater concentration of sulfate ions and lesser concentrations of sodium, chloride, calcium, and bicarbonate ions than does extracellular fluid. Intracellular fluid also has a greater concentration of protein than does plasma. Figure 2 shows these relative concentrations.
Figure 3. Intracellular and extracellular fluid electrolyte concentrations
Note: Extracellular fluids have relatively high concentrations of sodium (Na+), calcium (Ca+2), chloride (Cl−), and bicarbonate (HCO3−) ions. Intracellular fluid has relatively high concentrations of potassium (K+), magnesium (Mg+2), phosphate (PO4−3), and sulfate (SO4−2) ions.
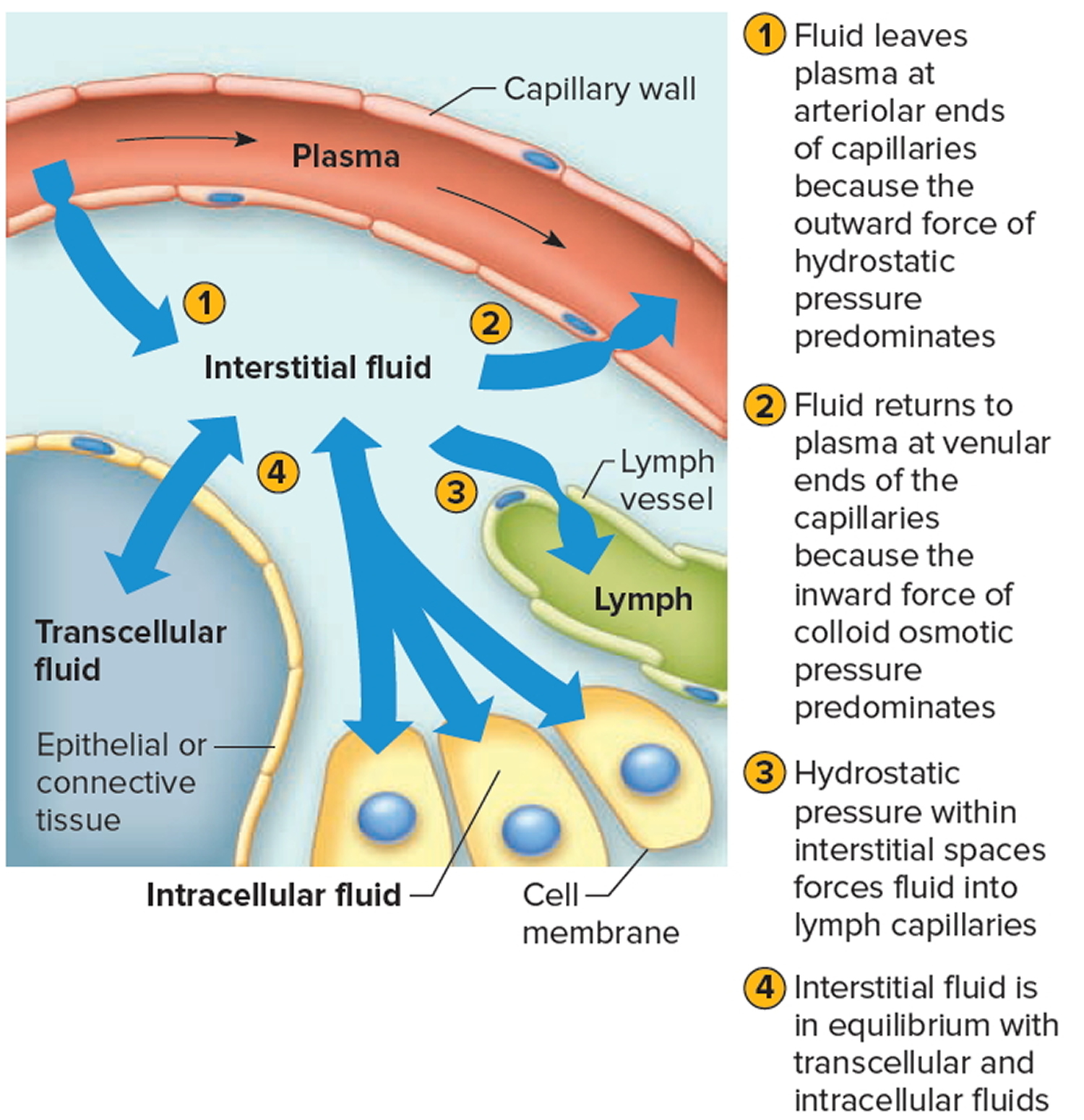
[Source 4]Movement of Fluid Between Compartments
Two major factors contribute to the movement of fluid from one compartment to another: hydrostatic pressure and osmotic pressure (Figure 4). For example, blood vessels, fluid leaves the plasma at the arteriolar ends of capillaries and enters the interstitial spaces because of the net outward force of hydrostatic pressure (blood pressure). Fluid returns to the plasma from the interstitial spaces at the venular ends of capillaries because of the net inward force of colloid osmotic pressure due to the plasma proteins. Likewise, tissue fluid and lymph, fluid leaves the interstitial spaces and enters the lymph capillaries due to the hydrostatic pressure of the interstitial fluid. The circulation of lymph returns interstitial fluid to the plasma.
Hydrostatic pressure in the cells and surrounding interstitial fluid is ordinarily equal and remains stable. Therefore, any net fluid movement is likely to be the result of changes in osmotic pressure.
The total solute concentration in extracellular and intracellular fluids is normally equal. However, a decrease in extracellular sodium ion concentration causes a net movement of water from the extracellular compartment into the intracellular compartment by osmosis. The cells swell. Conversely, if the extracellular sodium ion concentration increases, cells shrink as they lose water by osmosis.
Figure 4. Net movements of fluids between compartments result from differences in hydrostatic and osmotic pressures
[Source 4]Regulation of water balance
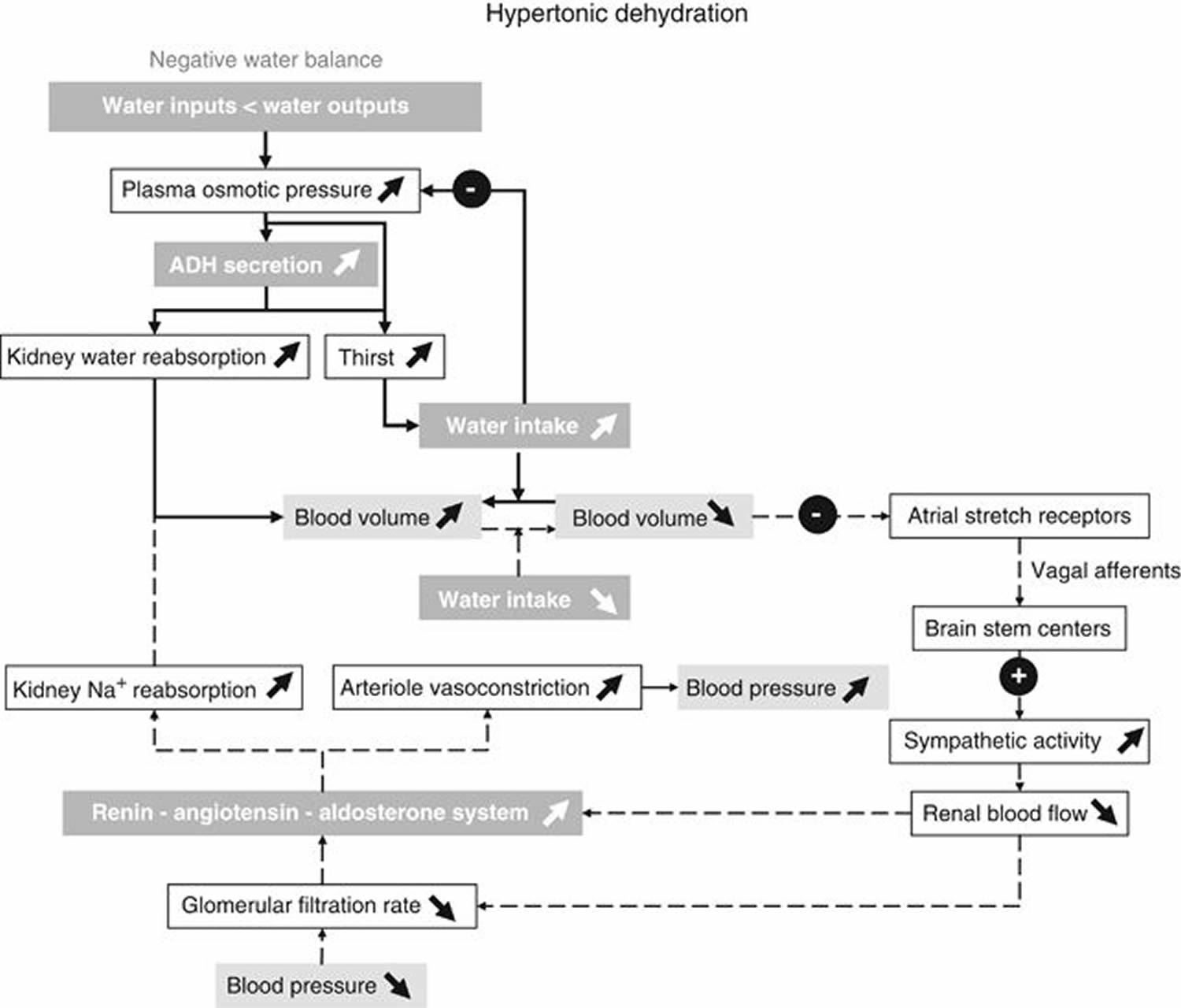
The intake of water is partially determined by thirst. When water losses exceed water intake, the osmotic pressure of extracellular fluid (ECF) increases. By activation of hypothalamic osmoreceptors, an antidiuretic hormone (ADH) is released from the posterior pituitary gland 5. Both the increased ECF osmotic pressure and antidiuretic hormone (ADH) elicit the feeling of thirst (Figure 2). The receptors that elicit thirst have an osmotic threshold higher than the osmoreceptors involved in ADH release. Thus, ADH can act on the kidneys to increase water reabsorption before thirst is elicited. Thirst is often blunted in elderly subjects who are at risk of having an insufficient water intake in conditions of elevated ambient temperature and humidity 6. Thirst is triggered by an increase in plasma and ECF osmolarity, by reductions in plasma volume at water deficits that correspond to a body weight loss of 1–3% 7. During rehydration, thirst can disappear before water balance is reached.
Figure 5. Water balance regulation in your body
Note: Feedback loops for water balance: main perturbations and physiological responses to hypertonic dehydration due to a negative water balance. Solid arrows show the responses induced by osmoreceptors when plasma osmotic pressure increases. Dashed arrows show the corrective mechanisms induced by insufficient water intake and a decreased blood volume to restore blood volume and blood pressure. Note that in the case of hypotonic dehydration due to a positive water balance, all perturbations and physiological responses that are induced occur in the reverse direction.
[Source 8]The set point of plasma osmolarity above which antidiuretic hormone (ADH) secretion is stimulated is about 280 mosm/l. Furthermore, the sensitivity of antidiuretic hormone (ADH) response to a rise in plasma osmolarity is enhanced when the circulating blood volume is lowered 5.
Kidneys are the main regulators of water losses. They have the unique property to modify the osmotic pressure of urine within a large range in response to minute changes in plasma osmotic pressure.
There are two conditions that induce the production of a large volume of urine, and therefore a large water loss. Water diuresis occurs when water is ingested in excess of body requirements. This leads to a small decrease in plasma osmolarity, with a suppression of ADH secretion. As a result, a large volume of hypotonic urine is produced. In contrast, osmotic diuresis results from a filtered load of a solute that exceeds the renal tubules’ maximum reabsorption capacity for this solute.
In summary, both deficit and excess water intakes are counterbalanced by subtle hormonal changes (ADH, aldosterone and atrial natriuretic peptide) that contribute to buffer the deleterious effects of these abnormal conditions. In the end, the final and precise regulation of water balance is dependent on thirst and on ADH release, with its predominant role in water reabsorption in the kidneys (Figure 1). Therefore, voluntary drinking of water is a key behavior for maintaining water balance. Consequently, drinking water before being thirsty is a good habit for maintaining a good body hydration status.
What is water retention
Water retention or edema is an abnormal accumulation of extracellular fluid in the interstitial spaces. The condition called edema arises when part of the body becomes swollen because fluid gathers in the tissue. Although edema can affect any part of your body, it’s most commonly noticed in the hands, arms, feet, ankles and legs 9.
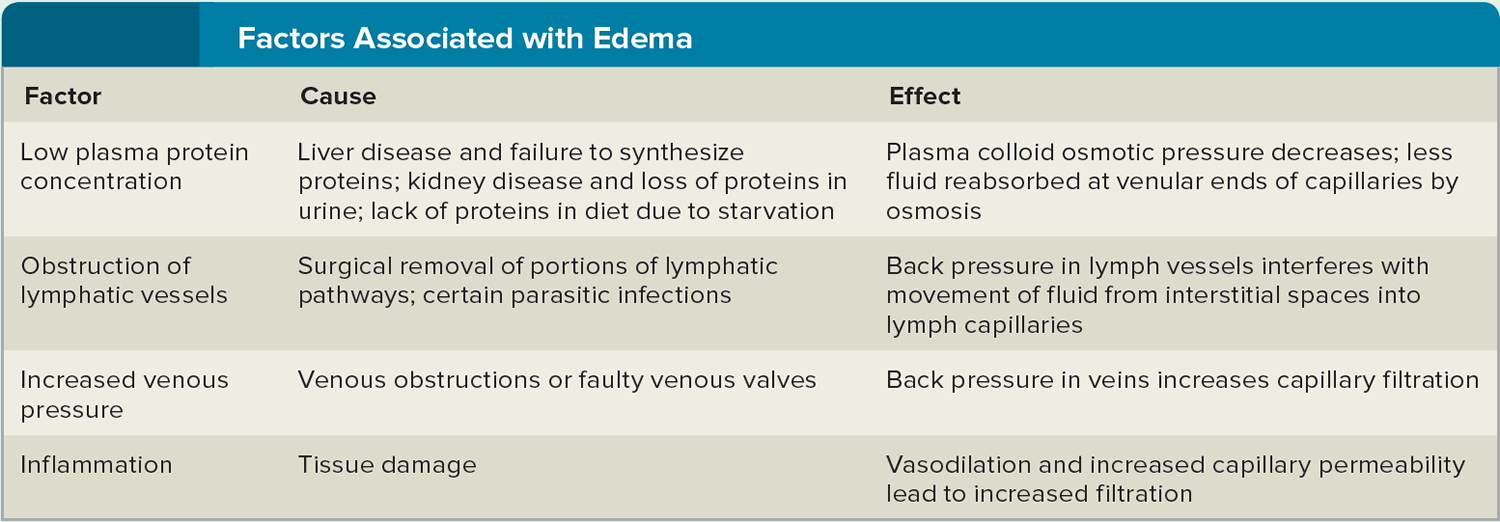
Causes of edema include a decrease in the plasma protein concentration (hypoproteinemia), obstructions in lymphatic vessels, increased venous pressure, and increased capillary permeability.
Hypoproteinemia may result from failure of the liver to synthesize plasma proteins; kidney disease that damages glomerular capillaries, allowing proteins to enter the urine; or starvation, in which amino acid intake is insufficient to support synthesis of plasma proteins. In each of these instances, the plasma protein concentration is decreased, which decreases plasma colloid osmotic pressure, reducing the normal return of tissue fluid to the venular ends of capillaries. Consequently, tissue fluid accumulates in the interstitial spaces.
Water retention (edema) may also result from lymphatic obstructions due to surgery or parasitic infections of lymphatic vessels.
Lymph Movement
Back pressure develops in the lymphatic vessels, which interferes with the normal movement of tissue fluid into them. At the same time, proteins that are usually removed by the lymphatic circulation accumulate in interstitial spaces, raising the osmotic pressure of interstitial fluid. This effect draws still more fluid into the interstitial spaces. If blood outflow from the liver into the inferior vena cava is blocked, the venous pressure in the liver and portal blood vessels greatly increases. As a result, fluid with a high protein concentration is exuded from the surfaces of the liver and intestine into the peritoneal cavity. The protein buildup elevates the osmotic pressure of the abdominal fluid, which in turn draws more water into the peritoneal cavity by osmosis, causing the painful condition ascites.
Edema may also result from increased capillary permeability accompanying inflammation. Inflammation is a response to tissue damage and usually releases chemicals such as histamine from damaged cells. Histamine causes vasodilation and increased capillary permeability. As a result, excess fluid leaks out of the capillary and enters the interstitial spaces.
Figure 6. Factors associated with edema
[Source 4]What causes water retention
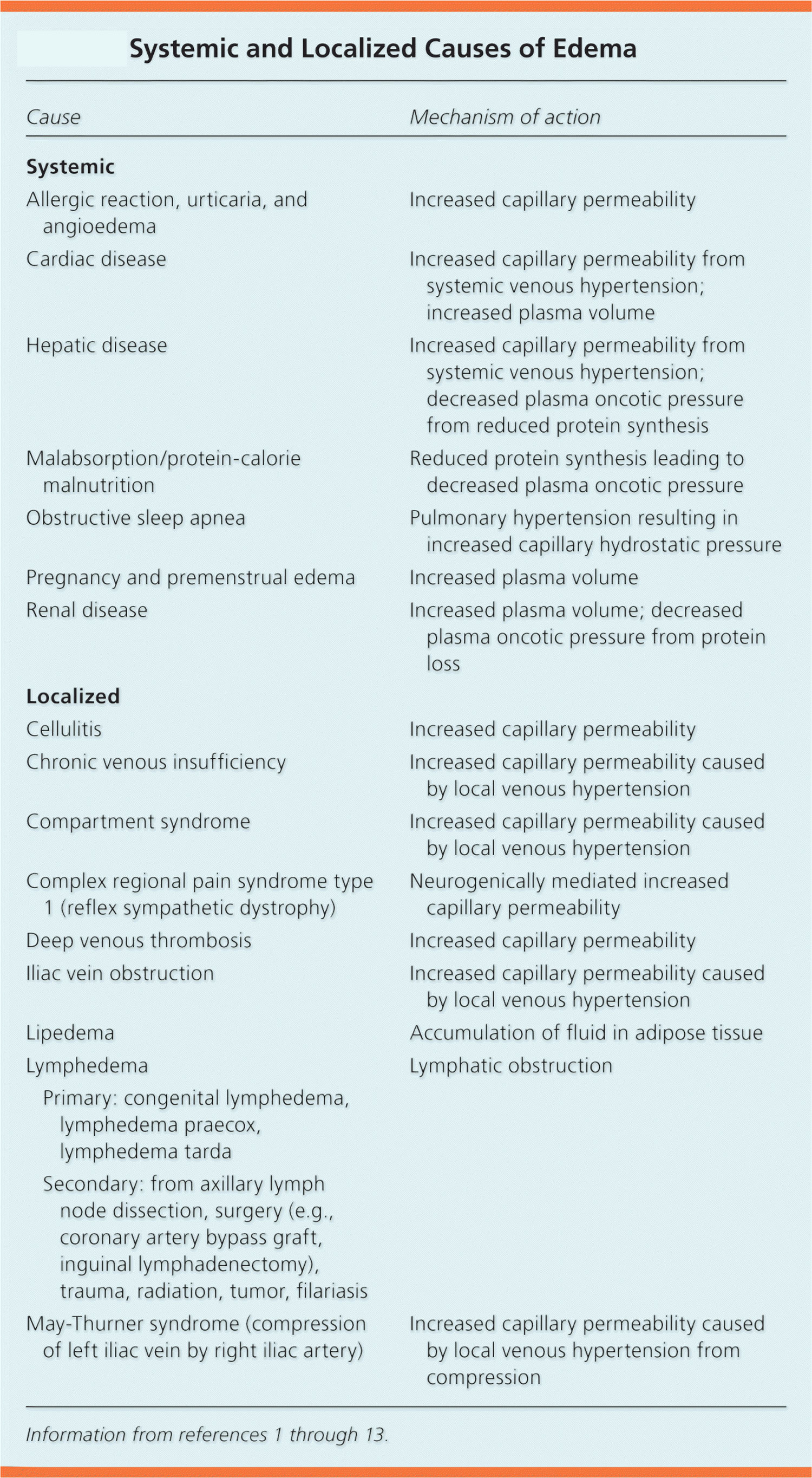
Edema can have various causes 10. Edema is an accumulation of fluid in the intercellular tissue that results from an abnormal expansion in interstitial fluid volume. The fluid between the interstitial and intravascular spaces is regulated by the capillary hydrostatic pressure gradient and the oncotic pressure gradient across the capillary 11, 12, 13. The accumulation of fluid occurs when local or systemic conditions disrupt this equilibrium (Figure 7 and Table 1), leading to increased capillary hydrostatic pressure, increased plasma volume, decreased plasma oncotic pressure (hypoalbuminemia), increased capillary permeability, or lymphatic obstruction. It is important to see a doctor and check what is causing it to make sure it gets treated correctly 10.
Table 1. Systemic and Localized Causes of Edema (water or fluid retention)
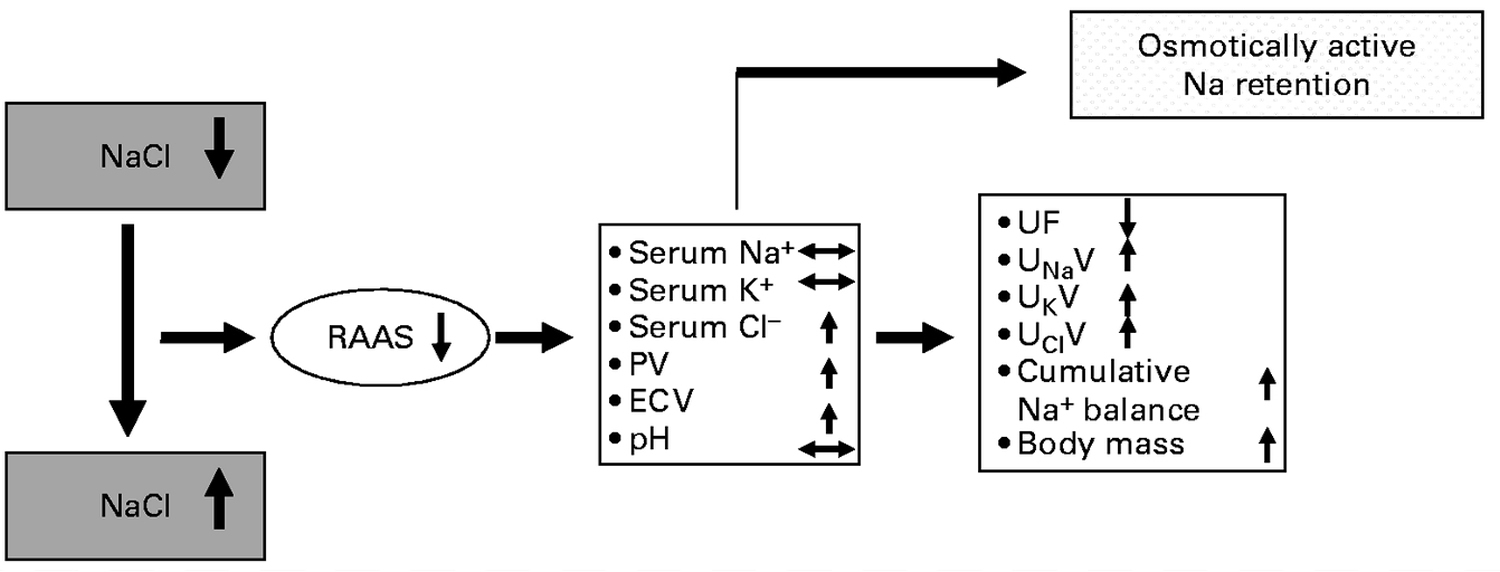
[Source: American Family Physician 14]Figure 7. Model of Na (sodium) regulation dependent on different levels of NaCl (table salt) intake sodium and fluid retention
Note: Na (sodium) and fluid retention when increasing NaCl (table salt) intake from a low to a high level leading to osmotically active Na retention. Increasing Na (sodium) intake from low to average normal intake levels leads to positive cumulative Na balance accompanied by plasma volume (PV) rise and an increase in extracellular volume (ECV), indicating an isotonic increase in the intravascular and interstitial volumes. This could be described as osmotically active Na retention. In this case, the renin–angiotensin system (RAAS) is very much suppressed. PV, plasma volume; ECV, extracellular volume; UF, urine flow; UNaV, urinary Na excretion; UKV, urinary K excretion; UClV, urinary Cl excretion.
[Source 15]Edema can be 10:
- a mild and temporary water retention problem that goes away by itself,
- a symptom of a serious disease that needs treatment,
- a condition that could become chronic and severe (like lymphedema after cancer treatment or leg edema in one leg following deep vein thrombosis), or
- an adverse effect of medication or an allergic reaction.
Mild cases of edema 9 may result from:
- Sitting or staying in one position for too long
- Eating too much salty food
- Premenstrual signs and symptoms
- Pregnancy.
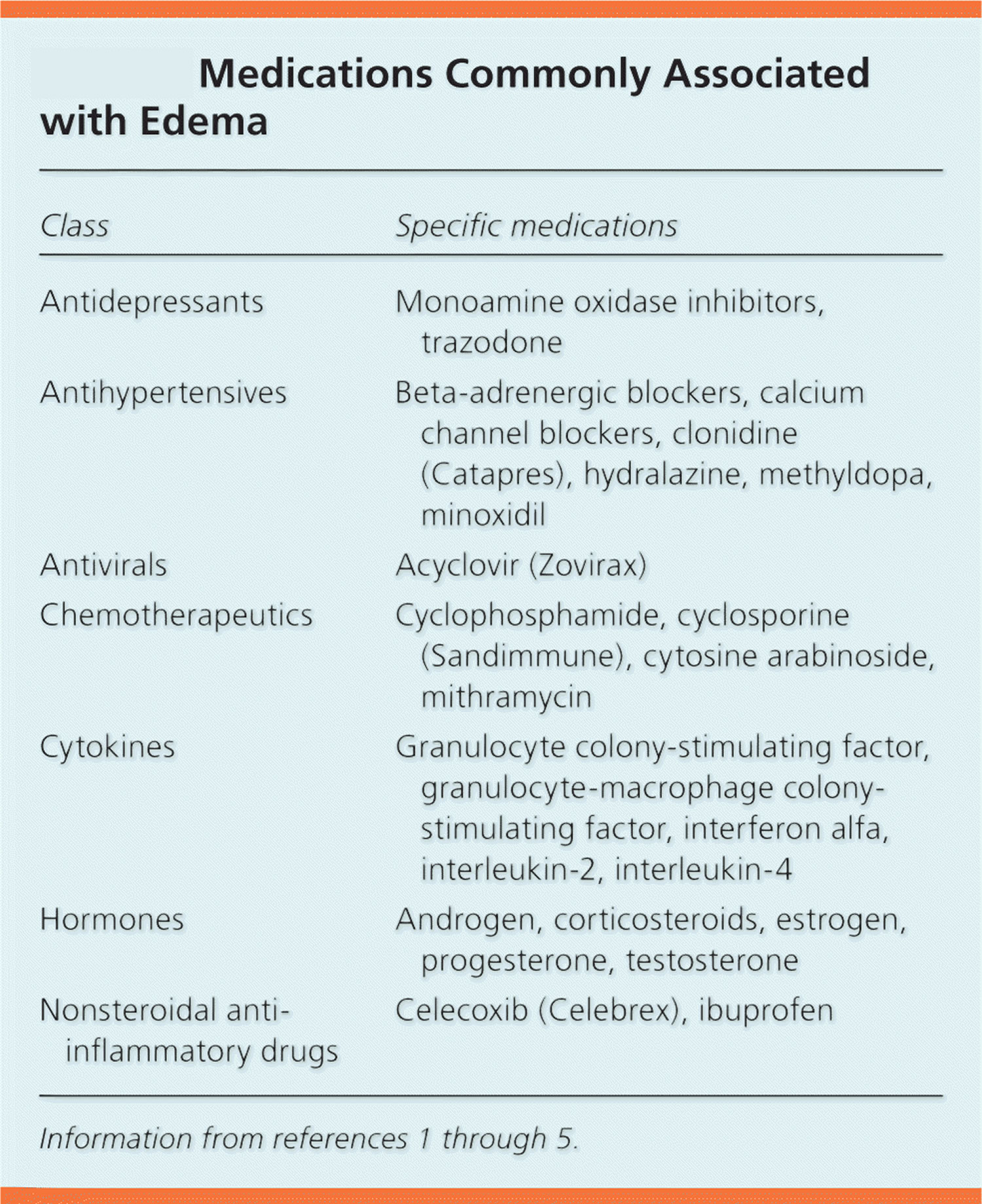
Edema can be a side effect of some medications 9, including:
- High blood pressure medications
- Nonsteroidal anti-inflammatory drugs
- Steroid drugs
- Estrogens
- Certain diabetes medications called thiazolidinediones
In some cases, however, edema may be a sign of a more serious underlying medical condition 9.
Diseases and conditions that may cause edema include:
- Congestive heart failure. When one or both of your heart’s lower chambers lose their ability to pump blood effectively — as happens in congestive heart failure — the blood can back up in your legs, ankles and feet, causing edema. Heart failure can also cause swelling in your abdomen. Sometimes it can cause fluid to accumulate in your lungs (pulmonary edema), which can lead to shortness of breath.
- Cirrhosis. Fluid may accumulate in your abdominal cavity (ascites) and in your legs as a result of liver damage (cirrhosis).
- Kidney disease. When you have kidney disease, extra fluid and sodium in your circulation may cause edema. The edema associated with kidney disease usually occurs in your legs and around your eyes.
- Kidney damage. Damage to the tiny, filtering blood vessels in your kidneys can result in nephrotic syndrome. In nephrotic syndrome, declining levels of protein (albumin) in your blood can lead to fluid accumulation and edema.
- Weakness or damage to veins in your legs. Chronic venous insufficiency, in which the one-way valves in your leg veins are weakened or damaged, allows blood to pool in the leg veins and cause swelling. Abrupt onset of swelling in one leg accompanied by pain in your calf can be due to a clot in one of your leg veins. Seek medical help promptly.
- Inadequate lymphatic system. Your body’s lymphatic system helps clear excess fluid from tissues. If this system is damaged — for example, by cancer surgery — the lymph nodes and lymph vessels draining an area may not work correctly and edema results.
Due to the fluid needed by the fetus and placenta, a pregnant woman’s body retains more sodium and water than usual, increasing the risk of edema 9.
If you have a chronic illness such as heart failure, liver or kidney disease, your risk of edema increases, as well. Surgery can sometimes obstruct a lymph node, leading to swelling in an arm or leg, usually on just one side.
If left untreated, edema can cause:
- Increasingly painful swelling
- Difficulty walking
- Stiffness
- Stretched skin, which can become itchy and uncomfortable
- Increased risk of infection in the swollen area
- Scarring between layers of tissue
- Decreased blood circulation
- Decreased elasticity of arteries, veins, joints and muscles
- Increased risk of skin ulcers
Unless you’re already under a specialist’s care for a current medical condition, you’ll probably start by seeing your family doctor or regular health care provider to begin evaluation for what could be causing your symptoms.
General puffiness or swelling caused by water retention
Signs of this kind of edema include puffiness of the hands, feet and / or face. This kind of edema is temporary and goes away without treatment. It can happen because you have been standing or sitting for too long. Edema is common after a long flight, for example, or in people who have to stand for long periods at work. Many women experience edema during their monthly period (menstruation) or during pregnancy. Edema in pregnancy is usually harmless, although it can be a sign of other problems if blood pressure is also high.
Fluid Retention over the Menstrual Cycle
Self-reported “fluid retention,” commonly described as bloating, is one element of the clinical symptom of premenstrual syndrome (PMS) and diagnosis of premenstrual symptoms. Many women perceive changes in fluid retention or “bloating” over the course of their menstrual cycle. As early as 1934, Sweeney 16 reported a pattern of “menstrual edema,” premenstrual weight gain peaking at the onset of flow, in a subgroup of student nurses. For most women, water retention is just a monthly bother — but in some cases, it can be severe enough to interfere with daily activities.
Premenstrual water retention causes a bloated, heavy feeling the week or two before your period begins. What causes water retention and other PMS symptoms is unclear, but hormonal changes seem to play a major role. Heredity might be a factor as well. Your diet — such as a lack of certain vitamins or too much salt — might also contribute to water retention.
Several prospective daily rating studies reported peak fluid retention at the onset of menstrual flow 17, 18, but the hormonal factors underlying these changes remain poorly understood. In particular, it is not clear whether ovulation is necessary, or whether similar changes also occur in anovulatory cycles of normal length.
Estradiol lowers the operating point for osmoregulation of arginine vasopressin and thirst and increases plasma volume. Although total body water and sodium content are only mildly affected, data presented in this study 19 suggest that reproductive hormones alter homeostatic set points for body fluid and tonicity.
Hypothalamic causes for ovulation disturbances include situational stresses 20, dietary restraint (vegetarian vs non-vegetarian diets) 21, travel, and increases in strenuous exercise with inadequate energy intake 22. In previous study, it was shown that increasing exercise training decreases fluid retention within ovulatory cycles 23. Prospective studies have shown decreases in fluid retention with increasing exercise in both sedentary women 24 and in fit women who increased their training in preparation for a marathon 23. Sedentary women just starting exercise showed the largest decreases in fluid retention. A rebound increase in fluid retention with decreasing exercise, however, has been reported in the exercise literature 25.
Although there is a clear menstrual pattern in fluid retention, this study 26 shows the peak day of average fluid retention was the first day of flow rather than premenstrually. Fluid retention around flow was similar between anovulatory and ovulatory cycles; therefore self-perceived fluid retention/bloating is unlikely to be due to the actions of progesterone. Heavier and less physically active women tend to have more fluid retention 26.
A variety of diseases can cause edema. Most of the time, the edema is not a serious illness, but it may be a sign for one. Here are some examples:
- Venous insufficiency
Venous insufficiency can cause edema in the feet and ankles, because the veins are having trouble transporting enough blood all the way to the feet and back to the heart. This means that it gathers in the legs, and fluid is forced out of the blood vessels into the surrounding tissue. Edema can also be caused by varicose veins.
- Congestive heart failure
Congestive heart failure can cause both peripheral edema and abdominal edema (ascites). This is because the heart is too weak to pump blood around the body properly, so the blood gathers in front of the heart. Because of this, and due to the increased blood pressure in the veins, fluid seeps out into the surrounding tissue. This may cause swelling in the legs or a build-up of fluid in the abdomen. If the person spends a lot of time lying down, the edema might show up on his or her back (called sacral edema). Congestive heart failure can also cause edema in the lungs (pulmonary edema). This is not common, but the condition is life-threatening. It means the lungs are filling with fluid because the left side of the heart is not strong enough to pump the blood returning from the lungs. The blood gathers in the blood vessels of the lung, and fluid seeps out into the lung tissue. The signs are shortness of breath and rapid, shallow breathing or coughing.
- Kidney disease
Kidney disease could cause edema in the legs and around the eyes, because when the kidneys do not remove enough sodium and water from the body, the pressure in the blood vessels starts building up, which can lead to edema.
- Low protein levels in the blood
If there is a lack of the protein albumin in the blood, fluid can leak out of blood vessels more easily. Low protein in the blood can be caused by extreme malnutrition, as well as kidney and liver diseases which mean that the body loses too much or produces too little protein.
- Liver diseases
Scarring of liver tissue (liver cirrhosis) due to, for instance, long-term alcohol abuse or a liver inflammation, can cause edema in the abdomen (called ascites). This is because cirrhosis causes a lack of proteins and congestion in the liver, which can lead to increased pressure in the blood vessels. As a result, fluid seeps out into the abdomen.
- Severe lung conditions like emphysema can also cause edema in the legs and feet if the pressure in the lungs and heart gets very high.
Lymphedema
This is caused by damage to the lymphatic system. It usually affects only one part of the body, like an arm. The most common cause of lymphedema in countries like Germany is cancer treatment in which lymph nodes have been removed or destroyed. It could be temporary after cancer surgery, but it can also develop into a chronic condition that can become severe.
Water retention signs and symptoms
Common early signs and symptoms of peripheral edema 10 include the following:
- Swelling or puffiness of the tissue directly under your skin.
- Stretched or shiny skin.
- The skin near the edema feels tight or warm.
- When you press the swelling, it leaves a dent.
- An arm or leg starts feeling full or heavy.
- The arm or leg starts to look swollen.
- Increased abdominal size.
- Your clothing or jewelry starts to feel tight and uncomfortable.
- It becomes harder to move any joints that are affected.
- There is a sensation of tautness or even pain in the surrounding area.
Make an appointment to see your doctor if you have swelling, stretched or shiny skin, or skin that retains a dimple after being pressed. Seek immediate medical attention if you experience:
- Shortness of breath
- Difficulty breathing
- Chest pain
These symptoms can be a sign of pulmonary edema, which requires prompt treatment.
If you’ve been sitting for a prolonged period, such as on a long flight, and you develop swelling and pain in a leg that won’t go away, call your doctor. Persistent leg pain and swelling can be a sign of a blood clot deep in your veins (deep vein thrombosis, or DVT) 9.
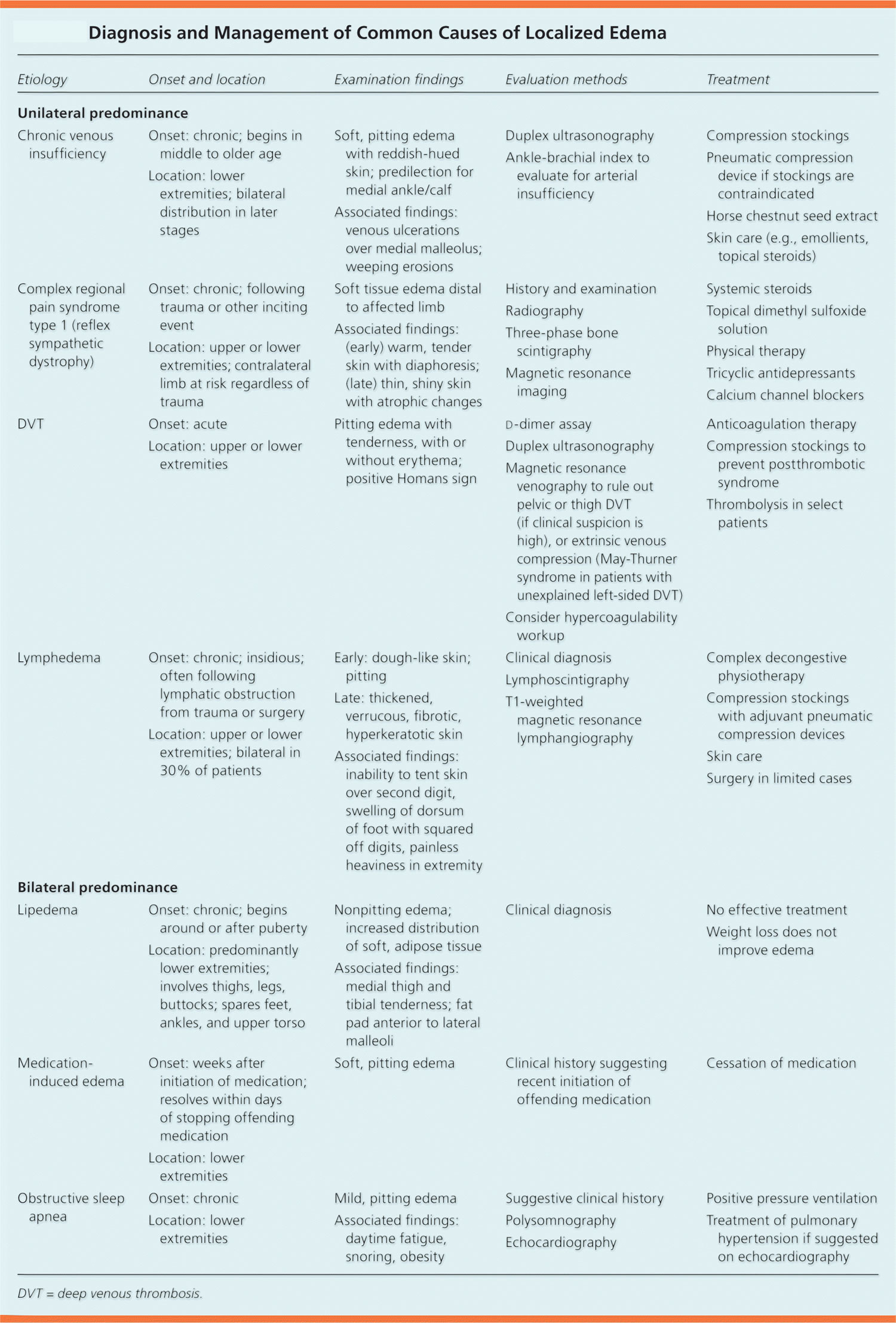
Water retention diagnosis
The history should include the timing of the edema, whether it changes with position, and if it is unilateral or bilateral, as well as a medication history and an assessment for systemic diseases (Table 2). Acute swelling of a limb over a period of less than 72 hours is more characteristic of deep venous thrombosis (DVT), cellulitis, ruptured popliteal cyst, acute compartment syndrome from trauma, or recent initiation of calcium channel blockers. The chronic accumulation of more generalized edema is due to the onset or exacerbation of chronic systemic conditions, such as congestive heart failure (CHF), renal disease, or hepatic disease 27, 28.
Gravity dependent edema caused by venous insufficiency is more likely to improve with elevation and worsen with gravity 29. Edema associated with decreased plasma oncotic pressure (e.g., malabsorption, liver failure, nephrotic syndrome) does not change with gravity.
Unilateral swelling from compression or compromise of venous or lymphatic drainage can result from DVT, venous insufficiency, venous obstruction by tumor (e.g., tumor obstruction of the iliac vein), lymphatic obstruction (e.g., from a pelvic tumor or lymphoma), or lymphatic destruction (e.g., congenital vs. secondary from a tumor, radiation, or filariasis). Bilateral or generalized swelling suggests a systemic cause, such as congestive heart failure (especially right-sided), pulmonary hypertension, chronic renal or hepatic disease (causing hypoalbuminemia), protein-losing enteropathies, or severe malnutrition 11, 27, 28.
Table 2. Diagnosis and management of localized edema
[Source: American Family Physician 14]Edema can be an adverse effect of certain medications (Table 3). The mechanism often includes the retention of salt and water with increased capillary hydrostatic pressure. Diuretic use may cause volume depletion and reflex stimulation of the reninangiotensin system.
Table 3. Medications commonly associated with edema
[Source: American Family Physician 14]Physical examination
The physical examination should assess for systemic causes of edema, such as heart failure (e.g., jugular venous distention, crackles), renal disease (e.g., proteinuria, oliguria), hepatic disease (e.g., jaundice, ascites, asterixis), or thyroid disease (e.g., exophthalmos, tremor, weight loss). Edema should also be evaluated for pitting, tenderness, and skin changes.
Pitting describes an indentation that remains in the edematous area after pressure is applied (Figure 8). This occurs when fluid in the interstitial space has a low concentration of protein, which is associated with decreased plasma oncotic pressure and disorders caused by increased capillary pressure (e.g., DVT, CHF, iliac vein compression) 30. Pitting edema also occurs in the early stages of lymphedema because of an influx of protein-rich fluid into the interstitium, before fibrosis of the subcutaneous tissue; therefore, its presence should not exclude the diagnosis of lymphedema 31. Tenderness to palpation over the edematous area is associated with deep venous thrombosis (DVT) and complex regional pain syndrome type 1 (i.e., reflex sympathetic dystrophy). Conversely, lymphedema generally does not elicit pain with palpation.
Figure 8. Pitting edema, bilateral, as observed in a patient with congestive heart failure

Changes in skin temperature, color, and texture provide clues to the cause of edema. For example, acute deep venous thrombosis (DVT) and cellulitis may produce increased warmth over the affected area. Because of the deposition of hemosiderin, chronic venous insufficiency is often associated with skin that has a brawny, reddish hue and commonly involves the medial malleolus 32. As venous insufficiency progresses, it can result in lipodermatosclerosis, which is associated with marked sclerotic and hyperpigmented tissue, and characterized by fibrosis and hemosiderin deposition that can lead to venous ulcers over the medial malleolus. These ulcers may progress to deep, weeping erosions. Myxedema from hypothyroidism presents with a generalized dry, thick skin with nonpitting periorbital edema and yellow to orange skin discoloration over the knees, elbows, palms, and soles. Localized pretibial myxedema may be caused by Graves disease (Figure 9). In the late stages of complex regional pain syndrome, the skin may appear shiny with atrophic changes. In the early stages of lymphedema, the skin has a doughy appearance, whereas in the later stages, it becomes fibrotic, thickened, and verrucous.
Figure 9. Pretibial myxedema causing a peau d’orange appearance in a patient with Graves disease

The following laboratory tests are useful for diagnosing systemic causes of edema: brain natriuretic peptide measurement (for congestive heart failure), creatinine measurement and urinalysis (for renal disease), and hepatic enzyme and albumin measurement (for hepatic disease). In patients who present with acute onset of unilateral upper or lower extremity swelling, a d-dimer enzyme-linked immunosorbent assay can rule out deep venous thrombosis (DVT) in low-risk patients. However, this test has a low specificity, and d-dimer concentrations may be elevated in the absence of thrombosis 33, 34, 35.
Ultrasonography
Venous ultrasonography is the imaging modality of choice in the evaluation of suspected deep venous thrombosis (DVT). Compression ultrasonography with or without Doppler waveform analysis has a high sensitivity (95%) and specificity (96%) for proximal thrombosis; however, the sensitivity is lower for calf veins (73%) 36. Duplex ultrasonography can also be used to confirm the diagnosis of chronic venous insufficiency.
Lmyphoscintigraphy
Lymph flow cannot be detected with ultrasonography. Therefore, indirect radionuclide lymphoscintigraphy, which shows absent or delayed filling of lymphatic channels, is the method of choice for evaluating lymphedema when the diagnosis cannot be made clinically 37.
Magnetic Resonance Imaging (MRI)
Patients with unilateral lower extremity edema who do not demonstrate a proximal thrombosis on duplex ultrasonography may require additional imaging to diagnose the cause of edema if clinical suspicion for DVT remains high. Magnetic resonance angiography with venography of the lower extremity and pelvis can be used to evaluate for intrinsic or extrinsic pelvic or thigh DVT 38. Compression of the left iliac vein by the right iliac artery (May-Thurner syndrome) should be suspected in women between 18 and 30 years of age who present with edema of the left lower extremity 39. Magnetic resonance imaging may aid in the diagnosis of musculoskeletal etiologies, such as a gastrocnemius tear or popliteal cyst. T1-weighted magnetic resonance lymphangiography can be used to directly visualize the lymphatic channels when lymphedema is suspected 40.
Other studies
Echocardiography to evaluate pulmonary arterial pressures is recommended for patients with obstructive sleep apnea and edema.27,28 In one study of patients with obstructive sleep apnea, 93% of those with edema had elevated right arterial pressures 41. Pulmonary hypertension has long been thought to be the cause of edema associated with obstructive sleep apnea. However, one study found that although a high proportion of patients with edema had obstructive sleep apnea (more than two-thirds), nearly one-third of these patients did not have pulmonary hypertension, which suggests a stronger correlation between edema and obstructive sleep apnea than can be explained by the presence of pulmonary hypertension alone 42.
Water retention remedies
To understand what might be causing your edema, your doctor will perform a physical exam and ask you questions about your medical history. This information is often enough to determine the underlying cause of your edema. In some cases, X-rays, ultrasound exams, blood tests or urine analysis may be necessary.
- Mild edema usually goes away on its own, particularly if you help things along by raising the affected limb higher than your heart.
- More severe edema may be treated with drugs that help your body expel excess fluid in the form of urine (diuretics or water pills). One of the most common diuretics is furosemide (Lasix). These medications — sometimes referred to as water pills — are available by prescription to help reduce fluid buildup. Diuretics do have some side effects, however and it’s rare that water retention alone would warrant use of this type of medication. Be aware that taking ibuprofen or other nonsteroidal anti-inflammatory drugs and diuretics at the same time can cause kidney damage.
- Birth control pills. Some research suggests that oral contraceptives — which prevent ovulation — can help reduce the physical symptoms of PMS 43.
Long-term management typically focuses on treating the underlying cause of the swelling. If edema occurs as a result of medication use, your doctor may adjust your prescription or check for an alternative medication that doesn’t cause edema.
The following may help decrease edema and keep it from coming back 44. Before trying these self-care techniques, talk to your doctor about which ones are right for you.
- Lose weight if you need to.
- Eat a healthy diet. Eat plenty of fruits, vegetables, nuts, seeds and whole grains.
- Avoid caffeine and alcohol.
- Reduce salt intake to less than 1 g/day. Follow your doctor’s suggestions about limiting how much salt you consume. Salt can increase fluid retention and worsen edema. A low-salt diet, which may reduce fluid buildup and swelling. Patients with sodium retention often benefit from restriction of dietary sodium. Patients with heart failure should eliminate salt in cooking and at the table and avoid prepared foods with added salt. Patients with advanced cirrhosis or nephrotic syndrome often require more severe sodium restriction (≤ 1 g/day). Potassium salts are often substituted for sodium salts to make sodium restriction tolerable; however, care should be taken, especially in patients receiving potassium-sparing diuretics, ACE inhibitors, or angiotensin II receptor blockers and in those with a kidney disorder because potentially fatal hyperkalemia can result 45.
- Include physical activity in your daily routine. Women who participate in regular physical activity generally report fewer premenstrual (PMS) symptoms.
- Movement. Moving and using the muscles in the part of your body affected by edema may help pump the excess fluid back to your heart. Ask your doctor about exercises you can do that may reduce swelling.
- Elevation. Hold the swollen part of your body above the level of your heart several times a day. In some cases, elevating the affected body part while you sleep may be helpful.
- Massage. Stroking the affected area toward your heart using firm, but not painful, pressure may help move the excess fluid out of that area.
- Compression. If one of your limbs is affected by edema, your doctor may recommend you wear compression stockings, sleeves or gloves. These garments keep pressure on your limbs to prevent fluid from collecting in the tissue.
- Protection. Keep the affected area clean, moisturized and free from injury. Dry, cracked skin is more prone to scrapes, cuts and infection. Always wear protection on your feet if that’s where the swelling typically occurs.
- Lymphedema
The mainstay of lymphedema treatment involves complex decongestive physiotherapy, which is composed of manual lymphatic massage and multilayer bandages. The initial goal is to improve fluid resorption until a maximum therapeutic response is reached. The maintenance phase of treatment includes compression stockings at 30 to 40 mm Hg 46, 47. Pneumatic compression devices have been shown to augment standard therapies. One randomized controlled trial of women with breast cancer–related lymphedema showed statistically significant improvement in lymphatic function following one hour of pneumatic compression therapy 48. In a study of 155 patients with cancer- and non–cancer-related lymphedema, 95% of patients noted reduction in limb edema after using pneumatic compression devices at home 49. Surgical debulking or bypass procedures are limited to severe refractory cases 50. Diuretics do not have a role in the treatment of lymphedema.
- Deep venous thrombosis (DVT)
Acute thrombotic events are treated with anticoagulation therapy (unfractionated or low-molecular-weight heparin or warfarin [Coumadin]) to prevent progression of a clot or the development of postthrombotic syndrome 33. Postthrombotic syndrome is characterized by chronic leg swelling, pain, cramping, and skin changes including telangiectasias, which occur in 20% to 50% of patients within five years of a thrombotic event 51, 52. In addition to anticoagulation, compression stockings should be used after a DVT to prevent postthrombotic syndrome. In a Cochrane review of two randomized controlled trials comparing elastic compression stockings (20 to 30 mm Hg) with placebo in patients with DVT, those who wore compression stockings had a statistically significant reduction in the risk of developing postthrombotic syndrome after two years 53. A randomized controlled trial of 209 patients with proximal DVT showed that those who received catheter-directed thrombolysis in addition to conservative therapy with compression stockings and anticoagulation had a lower prevalence of postthrombotic syndrome after 24 months compared with conservative therapy alone, suggesting that thrombolysis may be a treatment option for select patients 54.
- DuBose TD. Disorders of acid-base balance. In: Taal MW, Chertow GM, Marsden PA, et al, eds. Brenner and Rector’s The Kidney. 9th ed. Philiadelphia, PA: Elsevier Saunders; 2012:chap16.[↩]
- U.S. National Library of Medicine. Fluid and Electrolyte Balance. https://medlineplus.gov/fluidandelectrolytebalance.html[↩][↩]
- Chernecky CC, Berger BJ. Electrolytes panel – blood. In: Chernecky CC, Berger BJ, eds. Laboratory Tests and Diagnostic Procedures. 6th ed. St. Louis, MO: Elsevier Saunders; 2013:464-467.[↩]
- Hole’s Essentials of Human Anatomy and Physiology 13th edition. Published by McGraw-Hill Education, 2 Penn Plaza, New York, NY 10121.[↩][↩][↩][↩][↩][↩][↩]
- Ganong WF (2005). Review of Medical Physiology, 22nd edn, LANGE-Science: New York.[↩][↩]
- Phillips PA, Rolls BJ, Ledingham JG, Forsling ML, Morton JJ, Crowe MJ et al. (1984). Reduced thirst after water deprivation in healthy elderly men. N Engl J Med 311, 753–759. https://www.ncbi.nlm.nih.gov/pubmed/6472364[↩]
- EFSA (2008). Draft dietary reference values for water. Scientific Opinion of the Panel on Dietetic Products, Nutrition and Allergies.[↩]
- Water as an essential nutrient: the physiological basis of hydration. European Journal of Clinical Nutrition (2010) 64, 115–123; doi:10.1038/ejcn.2009.111; published online 2 September 2009. http://www.nature.com/ejcn/journal/v64/n2/full/ejcn2009111a.html[↩]
- Mayo Foundation for Medical Education and Research. Edema. http://www.mayoclinic.org/diseases-conditions/edema/basics/definition/CON-20033037[↩][↩][↩][↩][↩][↩]
- National Center for Biotechnology Information. Institute for Quality and Efficiency in Health Care. Causes and signs of edema. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072593/[↩][↩][↩][↩][↩]
- Braunwald E, Loscalzo J. Edema. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2011. http://accessmedicine.mhmedical.com/Content.aspx?bookId=331§ionId=40726754[↩][↩]
- O’Brien JG, Chennubhotla SA, Chennubhotla RV. Treatment of edema. Am Fam Physician. 2005;71(11):2111–2117.[↩]
- Cho S, Atwood JE. Peripheral edema. Am J Med. 2002;113(7):580–586.[↩]
- Edema: Diagnosis and Management. Am Fam Physician. 2013 Jul 15;88(2):102-110. http://www.aafp.org/afp/2013/0715/p102.html[↩][↩][↩][↩][↩]
- Increasing sodium intake from a previous low or high intake affects water, electrolyte and acid–base balance differently. British Journal of Nutrition, Volume 101, Issue 9, May 2009 , pp. 1286-1294. https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/increasing-sodium-intake-from-a-previous-low-or-high-intake-affects-water-electrolyte-and-acidbase-balance-differently/3EFD00612B339DB8731C9EEBB54A40E2/core-reader[↩]
- Sweeney JS. Menstrual edema: preliminary report. Journal of the American Medical Association. 1934;103(4):234–236.[↩]
- The timing of menstruation-related symptoms assessed by a daily symptom rating scale. Taylor JW. Acta Psychiatr Scand. 1979 Jul; 60(1):87-105. https://www.ncbi.nlm.nih.gov/pubmed/573049/[↩]
- Timing and severity of symptoms associated with the menstrual cycle in a community-based sample in the Midwestern United States. Meaden PM, Hartlage SA, Cook-Karr J. Psychiatry Res. 2005 Mar 30; 134(1):27-36. https://www.ncbi.nlm.nih.gov/pubmed/15808287/[↩]
- Stachenfeld NS. Sex Hormone Effects on Body Fluid Regulation. Exercise and sport sciences reviews. 2008;36(3):152-159. doi:10.1097/JES.0b013e31817be928. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2849969/[↩]
- Ovulatory disturbances. Causative factors among Japanese student nurses in a dormitory. Nagata I, Kato K, Seki K, Furuya K. J Adolesc Health Care. 1986 Jan; 7(1):1-5. https://www.ncbi.nlm.nih.gov/pubmed/3080392/[↩]
- Vegetarian vs nonvegetarian diets, dietary restraint, and subclinical ovulatory disturbances: prospective 6-mo study. Barr SI, Janelle KC, Prior JC. Am J Clin Nutr. 1994 Dec; 60(6):887-94. https://www.ncbi.nlm.nih.gov/pubmed/7985629/[↩]
- Induction of menstrual disorders by strenuous exercise in untrained women. Bullen BA, Skrinar GS, Beitins IZ, von Mering G, Turnbull BA, McArthur JW. N Engl J Med. 1985 May 23; 312(21):1349-53. https://www.ncbi.nlm.nih.gov/pubmed/3990734/[↩]
- Conditioning exercise decreases premenstrual symptoms: a prospective, controlled 6-month trial. Prior JC, Vigna Y, Sciarretta D, Alojado N, Schulzer M. Fertil Steril. 1987 Mar; 47(3):402-8. https://www.ncbi.nlm.nih.gov/pubmed/3549364/[↩][↩]
- Conditioning exercise decreases premenstrual symptoms. A prospective controlled three month trial. Prior JC, Vigna Y, Alojada N. Eur J Appl Physiol Occup Physiol. 1986; 55(4):349-55. https://www.ncbi.nlm.nih.gov/pubmed/3758033/[↩]
- Reproduction for the athletic woman. New understandings of physiology and management. Prior JC, Vigna YM, McKay DW. Sports Med. 1992 Sep; 14(3):190-9. https://www.ncbi.nlm.nih.gov/pubmed/1439394/[↩]
- White CP, Hitchcock CL, Vigna YM, Prior JC. Fluid Retention over the Menstrual Cycle: 1-Year Data from the Prospective Ovulation Cohort. Obstetrics and Gynecology International. 2011;2011:138451. doi:10.1155/2011/138451. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3154522/[↩][↩]
- Yale SH, Mazza JJ. Approach to diagnosing lower extremity edema. Compr Ther. 2001;27(3):242–252.[↩][↩]
- Ely JW, Osheroff JA, Chambliss ML, Ebell MH. Approach to leg edema of unclear etiology. J Am Board Fam Med. 2006;19(2):148–160.[↩][↩]
- Topham EJ, Mortimer PS. Chronic lower limb oedema. Clin Med. 2002;2(1):28–31.[↩]
- Villeco JP. Edema: a silent but important factor. J Hand Ther. 2012;25(2):153–162.[↩]
- Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007;59(4):464–472.[↩]
- Alguire PC, Mathes BM. Chronic venous insufficiency and venous ulceration. J Gen Intern Med. 1997;12(6):374–383.[↩]
- Kesieme E, Kesieme C, Jebbin N, Irekpita E, Dongo A. Deep vein thrombosis: a clinical review. J Blood Med. 2011;2:59–69.[↩][↩]
- Gorman WP, Davis KR, Donnelly R. ABC of arterial and venous disease. Swollen lower limb-1: general assessment and deep vein thrombosis [published correction appears in BMJ. 2000;321(7256):266]. BMJ. 2000;320(7247):1453–1456.[↩]
- Brotman DJ, Segal JB, Jani JT, Petty BG, Kickler TS. Limitations of d-dimer testing in unselected inpatients with suspected venous thromboembolism. Am J Med. 2003;114(4):276–282.[↩]
- Kearon C, Julian JA, Newman TE, Ginsberg JS. Noninvasive diagnosis of deep venous thrombosis. McMaster Diagnostic Imaging Practice Guidelines Initiative [published correction appears in Ann Intern Med. 1998;129(5):425]. Ann Intern Med. 1998;128(8):663–677.[↩]
- Studdiford J, Lamb K, Stonehouse A. Evaluating edema of the hands. J Musculoskel Med. 2009;26(1):30–36.[↩]
- American College of Radiology. ACR Appropriateness Criteria: suspected lower extremity deep vein thrombosis. gm.acr.org/[↩]
- Naik A, Mian T, Abraham A, Rajput V. Iliac vein compression syndrome: an underdiagnosed cause of lower extremity deep venous thrombosis. J Hosp Med. 2010;5(7):E12–E13.[↩]
- Lawenda BD, Mondry TE, Johnstone PA. Lymphedema: a primer on the identification and management of a chronic condition in oncologic treatment. CA Cancer J Clin. 2009;59(1):8–24.[↩]
- O’Hearn DJ, Gold AR, Gold MS, Diggs P, Scharf SM. Lower extremity edema and pulmonary hypertension in morbidly obese patients with obstructive sleep apnea. Sleep Breath. 2009;13(1):25–34.[↩]
- Blankfield RP, Zyzanski SJ. Bilateral leg edema, pulmonary hypertension, and obstructive sleep apnea: a cross-sectional study. J Fam Pract. 2002;51(6):561–564.[↩]
- Mayo Foundation for Medical Education and Research. Water retention treatment. http://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/water-retention/art-20044983?pg=2[↩]
- Trayes KP, Studdiford JS, Pickle S, Tully AS. Edema: Diagnosis and management. Am Fam Phys. 2013;88(2):102-110.[↩]
- Merck Sharp & Dohme Corp. Merck Manual. Edema. https://www.merckmanuals.com/professional/cardiovascular-disorders/symptoms-of-cardiovascular-disorders/edema[↩]
- Stanisic MG, Gabriel M, Pawlaczyk K. Intensive decongestive treatment restores ability to work in patients with advanced forms of primary and secondary lower extremity lymphoedema. Phlebology. 2012;27(7):347–351.[↩]
- Badger C, Preston N, Seers K, Mortimer P. Physical therapies for reducing and controlling lymphoedema of the limbs. Cochrane Database Syst Rev. 2004;(4):CD003141.[↩]
- Adams KE, Rasmussen JC, Darne C, et al. Direct evidence of lymphatic function improvement after advanced pneumatic compression device treatment of lymphedema. Biomed Opt Express. 2010;1(1):114–125.[↩]
- Ridner SH, McMahon E, Dietrich MS, Hoy S. Home-based lymphedema treatment in patients with cancer-related lymphedema or noncancer-related lymphedema. Oncol Nurs Forum. 2008;35(4):671–680.[↩]
- Tiwari A, Cheng KS, Button M, Myint F, Hamilton G. Differential diagnosis, investigation, and current treatment of lower limb lymphedema. Arch Surg. 2003;138(2):152–161.[↩]
- Kahn SR. Post-thrombotic syndrome after deep venous thrombosis: risk factors, prevention, and therapeutic options. Clin Adv Hematol Oncol. 2009;7(7):433–435.[↩]
- Prandoni P, Kahn SR. Post-thrombotic syndrome: prevalence, prognostication and need for progress. Br J Haematol. 2009;145(3):286–295.[↩]
- Kolbach DN, Sandbrink MW, Hamulyak K, Neumann HA, Prins MH. Non-pharmaceutical measures for prevention of post-thrombotic syndrome. Cochrane Database Syst Rev. 2004;(1):CD004174.[↩]
- Enden T, Haig Y, Kløw NE, et al. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. Lancet. 2012;379(9810):31–38.[↩]