Contents
- Osler nodes
- Janeway lesions
- Splinter hemorrhages
- Osler’s nodes causes
- Osler’s nodes diagnosis
- Osler nodes differential diagnosis
- Osler nodes treatment
- What is endocarditis?
Osler nodes
Osler nodes also called Osler’s node are red-purple, slightly raised, tender or painful lumps, often with a pale center typically found on the tip of the fingers and/or toes 1, 2, 3. Pain often precedes the development of the visible lesion by up to 24 hours. Osler’s nodes can occur at any time during the course of bacterial endocarditis, usually subacute and last from hours to several days. Osler’s node was first described by William Osler 3.
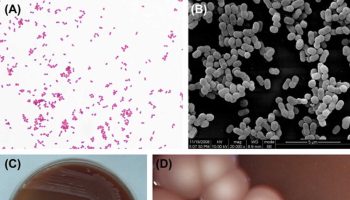
In contrast to Osler nodes, Janeway lesions are painless (non-tender) often hemorrhagic (bleeding into the skin) slightly nodular lesions that occur mostly on palms and soles on the thenar and hypothenar eminences (at the base of the thumb and little finger respectively) 4. Janeway lesions tend to last days to weeks before healing totally 5. Janeway lesions are more commonly seen in acute form of bacterial endocarditis, when bacteria such as Staphylococcus aureus may be cultured from them 5. The histology is usually consistent with microabscesses in the dermis (i.e. bacteria may be found within the blood in the capillaries with neutrophil infiltration) with thrombosis of small vessels, without evidence of vasculitis 6, 7, 8. Janeway lesions are associated with embolic events other than cerebral emboli 9.
Osler’s nodes are thought to be caused by localized immunological-mediated response while Janeway lesions are thought to be caused by septic microemboli 1. These findings frequently overlap and are difficult to differentiate 2. In preantibiotic era, Osler nodes appeared in 40–90% cases of infective endocarditis 10, however, recent prospective data report the incidence of Osler nodes to be 3–5% 11.
Distinguishing between Janeway lesions and Osler nodes is not that easy. Osler nodes disappear within a few days without consequences, occasionally in a few hours, while Janeway lesions tend to last days to weeks before healing completely 12. Bacterial cultures are often positive, leading to the conclusion that these lesions are caused by septic micro-emboli 7.
There are four peripheral signs of infective endocarditis: Roth spots, Osler nodes, Janeway lesions, and splinter hemorrhages 13. Sandre and Shafran 14 reported the incidence of peripheral signs of endocarditis as follows: 39% for splinter hemorrhages, 6.7% for Osler nodes, 2.2% for Janeway lesions, and 3% for Roth spots. Patients with dermatological manifestations of infective endocarditis have significantly higher complication rates 12.
Roth spots appear as white-centered retinal hemorrhages on a fundoscopic examination 15, 16, 16. The white center of a Roth spot is thought to be a platelet-fibrin plug 17, 18, 18. These platelet-fibrin plugs presumably form in response to vascular leaks brought about by elevated intravascular pressure, ischemia, increased capillary fragility, or combinations thereof 18. In most cases, emboli appear to play no role 19. Although Roth spots are a classic peripheral sign of endocarditis, they are also present in other conditions, including hematologic malignancies, connective tissue diseases, vasculitis, anemia, hypertension, diabetes mellitus, human immunodeficiency virus infections, and intracranial hemorrhages 19.
Splinter hemorrhage in the proximal nail plate is also a sign of bacterial endocarditis. Splinter hemorrhages are small areas of longitudinal bleeding (hemorrhage) under the fingernails or toenails and look like a wood splinter. Seen end-on, splinter hemorrhage is in the lower part of the nail plate or underneath it. Splinter hemorrhages in nails are formed by the hemorrhage of blood from the rupture of the longitudinally oriented blood vessels of the nail bed. Splinter hemorrhages look like thin, red to reddish-brown lines of blood under the nails. Splinter hemorrhages run in the direction of nail growth. The underlying blood will attach to the nail plate and seems to move up as the nail grows. Splinter hemorrhages can be single or multiple.
Osler nodes and Janeway lesions have also rarely been described in systemic lupus erythematosus (SLE), gonococcemia (gonorrhea), hemolytic anemia and typhoid fever. They are important as they may help in the earlier diagnosis of a serious medical disorder.
Table 1. Differentiating between Janeway lesions and Osler nodes
| Variables | Janeway lesion | Osler node |
|---|---|---|
| Location | Soles, palms, thenar and hypothenar eminences, plantar surfaces of the toe | Finger and toe tips, thenar and hypothenar eminences |
| Size and shape | Macules of variable size and irregular shape | Nodules of 1 mm to > 1 cm |
| Tender | No | Yes |
| Course | Days to weeks | Hours to days |
| Type of endocarditis | Acute | Subacute |
| Culture | Positive, usually | Negative, usually |
| Histology | Septic microemboli | Vasculitis |
Figure 1. Osler nodes
[Source 1 ]Figure 2. Osler node
Footnote: Right foot with a medial tender red-purple lesion, consistent with Osler node.
[Source 20 ]Figure 3. Osler nodes
Footnote: Multiple tender purple lesions, consistent with Osler nodes in the left hand.
[Source 20 ]Figure 4. Janeway lesions
Footnote: Right foot with multiple non-tender macular erythematous lesions, consistent with Janeway lesions
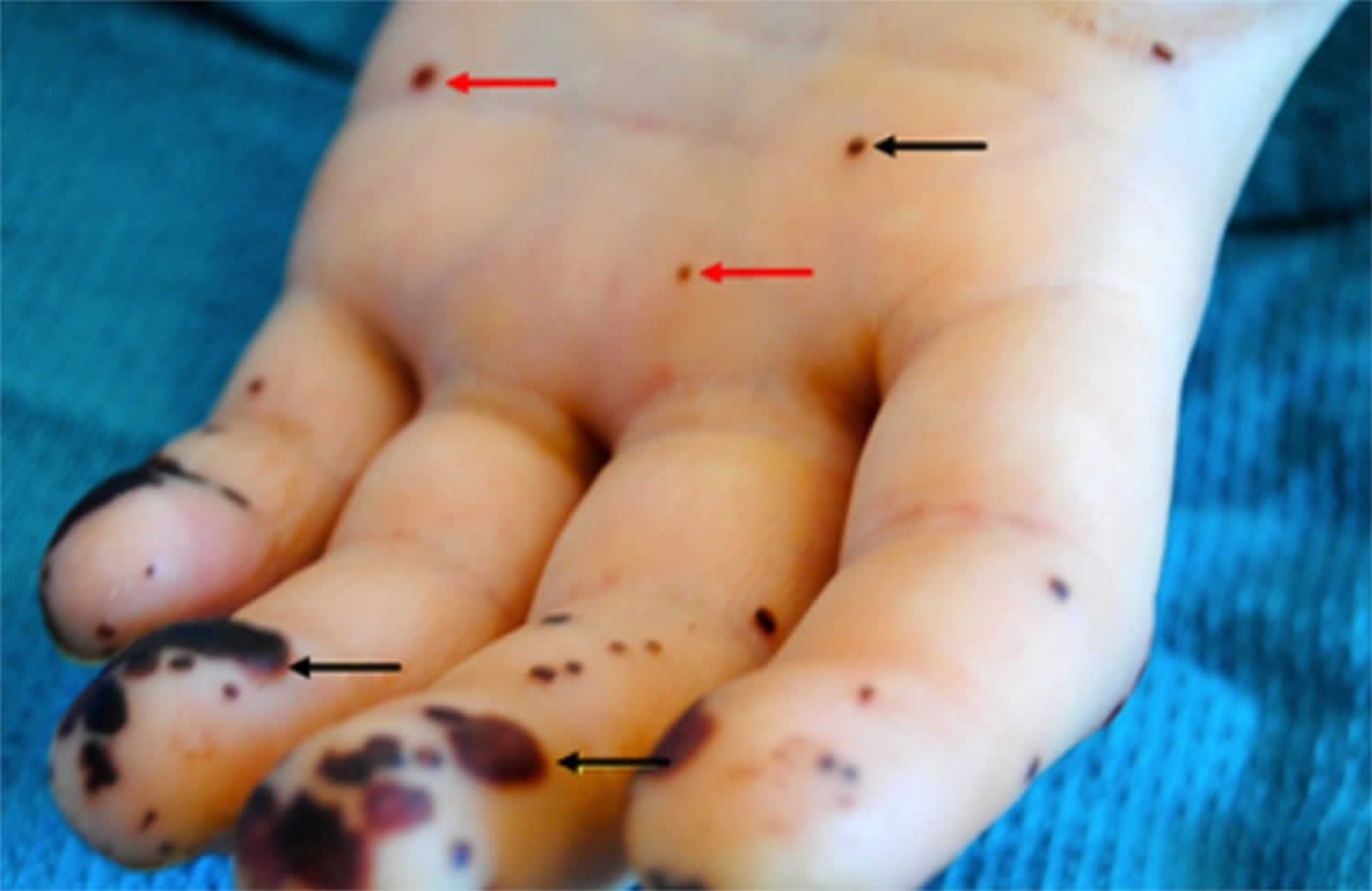
[Source 20 ]Figure 5. Osler nodes and Janeway lesions
Footnote: Osler nodes (black arrow) seen in the palm of the left hand, and Janeway lesions (red arrow) seen on the finger pulp and palm of the left hand.
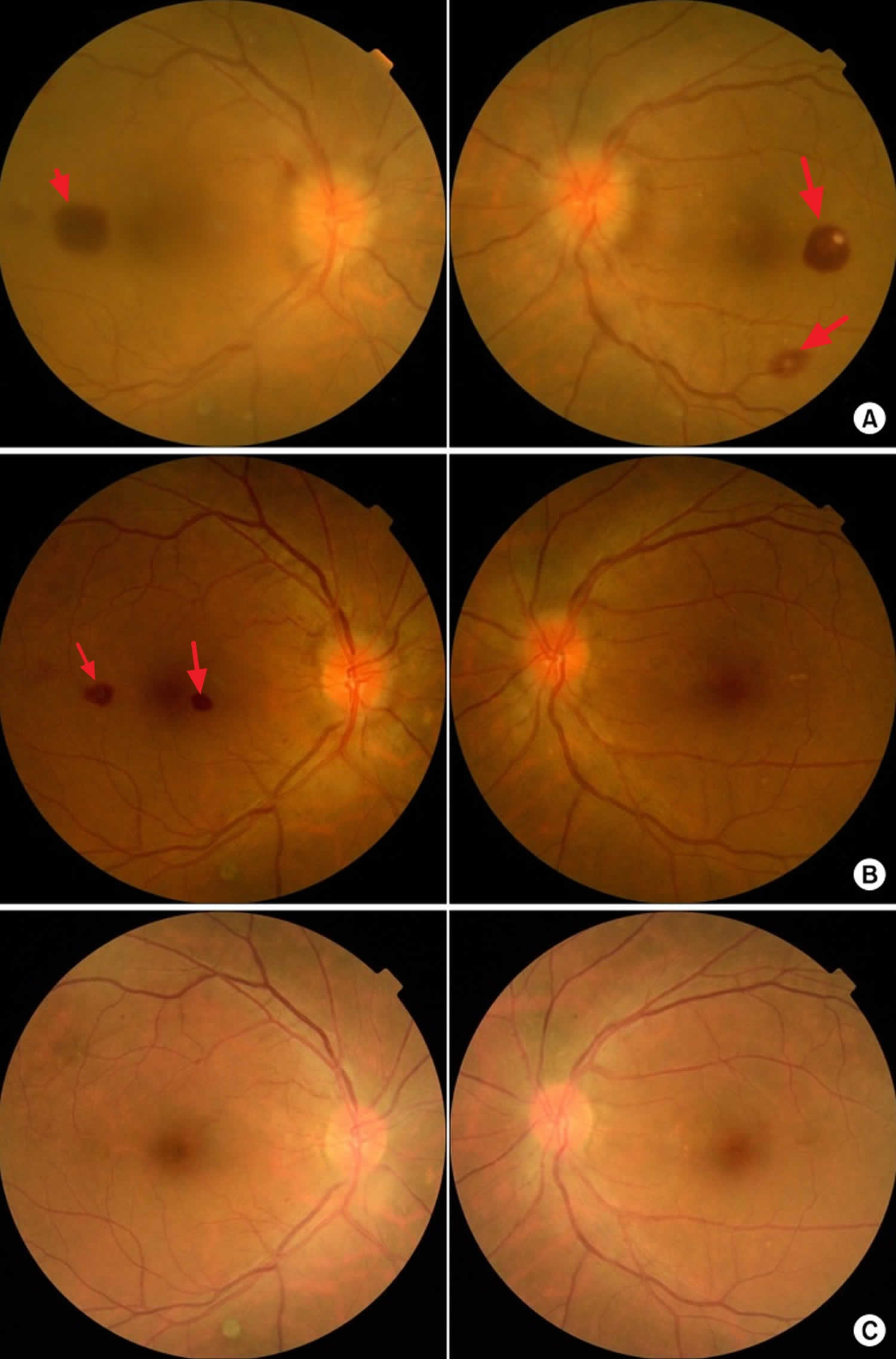
[Source 21 ]Figure 6. Roth spots
Footnote: Fundoscopic findings of Roth spots. (A) Preoperative findings. (B) 2 weeks postoperatively. (C) 6 weeks postoperatively.
[Source 17 ]Janeway lesions
Janeway lesions are painless (non-tender) often hemorrhagic (bleeding into the skin) slightly nodular lesions that occur mostly on palms and soles on the thenar and hypothenar eminences (at the base of the thumb and little finger respectively) 4. Janeway lesions tend to last days to weeks before healing totally 5. Janeway lesions are more commonly seen in acute form of bacterial endocarditis, when bacteria such as Staphylococcus aureus may be cultured from them 5. The histology is usually consistent with microabscesses in the dermis (i.e. bacteria may be found within the blood in the capillaries with neutrophil infiltration) with thrombosis of small vessels, without evidence of vasculitis 6, 7, 8. Janeway lesions are associated with embolic events other than cerebral emboli 9.
Splinter hemorrhages
Splinter hemorrhages are small areas of longitudinal bleeding (hemorrhage) under the fingernails or toenails and look like a wood splinter. Seen end-on, splinter hemorrhage is in the lower part of the nail plate or underneath it. Splinter hemorrhages in nails are formed by the hemorrhage of blood from the rupture of the longitudinally oriented blood vessels of the nail bed. Splinter hemorrhages look like thin, red to reddish-brown lines of blood under the nails. Splinter hemorrhages run in the direction of nail growth. The underlying blood will attach to the nail plate and seems to move up as the nail grows. Splinter hemorrhages can be single or multiple.
They are named splinter hemorrhages because they look like a wood splinter under the fingernail. The hemorrhages may be caused by tiny clots that damage the small capillaries under the nails.
Splinter hemorrhages occur commonly in psoriasis but may be seen with infection of the heart valves (infective endocarditis), rheumatic heart disease, valvular replacement, SLE (systemic lupus erythematosus), antiphospholipid syndrome, IV drug abusers, and congenital heart diseases 22. Splinter hemorrhages may be caused by vessel damage from swelling of the blood vessels (vasculitis) or tiny clots that damage the small capillaries (microemboli). A simultaneous occurrence in multiple nails is indicative of a systemic cause 23.
Other common systemic causes of splinter hemorrhages include dermatoses (e.g., psoriasis and lichen planus), connective tissue diseases, vasculitis, drugs, particularly kinase inhibitors, infectious diseases, such as acute endocarditis and meningococcemia and renal failure 24 and congenital heart diseases 22. In addition, splinter hemorrhages may be idiopathic, as seen in elderly, or they can be caused by various types of trauma, such as playing percussion instruments, housework, sports, and habits/tics.
In people with systemic diseases, splinter hemorrhages will often reappear, sometimes in different locations. The hemorrhages are usually 1 to 3 millimeters in length, and the streaks are typically red or reddish-brown.
Splinter hemorrhages may be asymptomatic or tender. In most instances, a splinter hemorrhage is not painful. However, if splinter hemorrhages are painful, they are more likely to be the result of a systemic disease.
Also, splinter hemorrhages close to the nail plate (proximal splinter hemorrhages) and on several fingers are more likely due to a systemic disease, especially in women.
Splinter hemorrhages under the distal third of the nail plate are frequent and are usually a result of trauma such as a sports injury. They may be associated with subungual hematoma and nail splitting.
Men experience splinter hemorrhages more often than women. People with a darker complexion may also have a greater risk of splinter hemorrhages.
Figure 7. Splinter hemorrhages
Figure 8. Splinter hemorrhage with bacterial endocarditis
Osler’s nodes causes
The underlying cause of the nodes has been debated since Osler first proposed micro-embolisation as a cause (this is the scattering of tiny particles around the bloodstream). Early reports favoured an allergic or immunological cause, but more recent reports have isolated bacteria from within the nodules.
A skin biopsy (histology) may reveal a neutrophilic vasculitis (inflammation of blood vessels) affecting the glomus apparatus of the ends of the fingers, or microabscess formation without evidence of vasculitis. It has been postulated that early biopsies show bacteria within the microabscesses and as time progresses, the nodes become sterile and hypersensitivity vasculitis or small vessel vasculitis develops, mediated by the immune system.
Osler’s nodes diagnosis
A careful search for endocarditis is made. Endocarditis can be difficult to diagnose. To find out if you have endocarditis, your doctor will:
- Ask about your medical history, including your symptoms, recent illnesses, and other health conditions that affect your chance of developing endocarditis.
- Do a physical exam.
- Likely order tests, such as:
- Blood culture test to check for signs of infection, bacteria, or fungi in your blood. Results from this test help determine the antibiotic or combination of antibiotics to use for treatment.
- Complete blood count. This test can determine if there’s a lot of white blood cells, which can be a sign of infection. A complete blood count can also help diagnose low levels of healthy red blood cells (anemia), which can be a sign of endocarditis. Other blood tests also may be done.
- Chest x-rays.
- An echocardiogram (heart ultrasound scan) can show an abnormal bacterial growth on the valve.
- In a standard (transthoracic) echocardiogram, a wandlike device (transducer) is moved over the chest area. The device directs sound waves at the heart and records them as they bounce back.
- In a transesophageal echocardiogram (TEE), a flexible tube containing a transducer is guided down the throat and into the tube connecting the mouth to the stomach (esophagus). A transesophageal echocardiogram provides much more detailed pictures of the heart than is possible with a standard echocardiogram.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. During an ECG, sensors (electrodes) are attached to the chest and sometimes to the arms or legs. It isn’t specifically used to diagnose endocarditis, but it can show if something is affecting the heart’s electrical activity.
- Chest X-ray. A chest X-ray shows the condition of the lungs and heart. It can help determine if endocarditis has caused heart swelling or if any infection has spread to the lungs.
- Computerized tomography (CT) scan or magnetic resonance imaging (MRI). You may need scans of your brain, chest or other parts of your body if your provider thinks that infection has spread to these areas.
A skin biopsy may be helpful to confirm the diagnosis of the Osler nodes.
Osler nodes differential diagnosis
Differential diagnoses include meningitis, bacteremia, pneumonia, sepsis, vasculitis, marantic endocarditis, thrombotic nonbacterial endocarditis, septic pulmonary infarction, temporal arteritis, connective tissue disease, antiphospholipid syndrome, fever of unknown origin, intra-abdominal infections, tricuspid regurgitation and primary cardiac neoplasms.
Osler nodes treatment
Treatment of Osler nodes is aimed at the bacterial endocarditis and involves intravenous antibiotics and sometimes valve surgery.
The skin lesions tend to heal spontaneously without scarring.
What is endocarditis?
Endocarditis also called infective endocarditis, is a rare but life-threatening inflammation of the lining inside your heart’s chambers and valves (the endocardium). Endocarditis is usually caused by germs that get into your bloodstream and travel to your heart. Once germs get inside your heart, the germs can attach to the lining or get trapped in the valves (the endocardium). They start to grow, causing an infection. If not treated quickly, the infection can cause damage to the heart and lead to serious health problems.
Bacterial endocarditis is an infection of the lining of the heart (the endocardium) caused by various bacteria. The responsible bacteria include various species of staphylococcus, streptococcus, pseudomonas, bartonella and several other organisms. Bacterial endocarditis most often affects the heart valves. Most commonly, infective endocarditis affects the aortic and mitral valves, less commonly the tricuspid vale, and in approximately 10% of cases affects more than one valve 25. The bacteria gain access to the heart via the bloodstream; an infection elsewhere in the body may or may not be apparent. While some bacteria can cause infection in normal heart valves, bacterial endocarditis more commonly affects patients with abnormal valves as a result of previous rheumatic fever, valve surgery/replacement, or congenital abnormalities.
Your risk of endocarditis is increased by having:
- Congenital heart disease
- Previous endocarditis. Endocarditis can damage heart tissue, which increases your risk of getting it again.
- Heart valve replacement
- Heart valve disease – either stenosis (a narrowed valve) or regurgitation (a leaking valve)
- Heart devices (such as a pacemaker or ICD)
- Intravenous drug use (intravenous users of heroin, cocaine or amphetamine) 26.
If you have a problem with a heart valve or you have man-made materials in your heart, it is easier for bacteria to lodge there, and your body may not be able to fight off the infection. Intravenous drug users are at risk even if they don’t have heart problems.
The factors predisposing to infective endocarditis are an elderly age of > 65 years, male gender, history of a rheumatic disease, presence of a prosthetic heart valve, diabetes mellitus, HIV infection, long-term presence of catheters in central veins, dialysis treatment, immunosuppression, and intravenous drug use by addicts 25. The most common complications of infective endocarditis include heart failure, renal failure, ischemic stroke, interstitial bleeding, and septic shock 25.
Bacterial endocarditis is often divided into ‘acute bacterial endocarditis’ and ‘subacute bacterial endocarditis’ depending on the speed that it progresses. The symptoms may include fever, lethargy, shortness of breath, chest pain or palpitations. These symptoms require prompt assessment and investigation by a doctor.
What causes endocarditis?
Bacterial infections cause most endocarditis. Normally, many bacteria live in your mouth, on your skin, or in other parts of the body. Sometimes these bacteria can get into your bloodstream from injuries such cuts or scrapes. Dental work and certain surgeries can also allow small amounts of bacteria to enter your bloodstream.
In some cases, fungal infections cause endocarditis. The fungi, such as yeast, can live in parts of your body. Fungal infections generally happen in people who have weakened immune systems that can’t stop the fungus from growing. This includes people who have HIV.
In general, endocarditis is rare. If you’re healthy, your immune system usually destroys the germs in your bloodstream before they can cause harm. But your chance of developing endocarditis may be higher than most people if you:
- Have certain heart conditions. Damaged or abnormal heart tissue and devices in your heart can trap germs more easily than healthy heart tissue. That means your risk of endocarditis is higher if you have:
- Heart valve disease.
- Certain congenital heart defects.
- A pacemaker or an implantable defibrillator.
- A heart valve replacement.
- Are older. Age-related changes to the heart valves, such as mitral valve prolapse or calcium deposits in the aortic valve, create places for germs to attach to the heart.
- Inject illegal drugs. Unclean needles may carry bacteria into the bloodstream.
- Have a condition that weakens your immune system.
- Don’t take care of your teeth and gums. Poor dental health makes it easier for germs to get into your bloodstream through your gums and mouth.
- Have a long-term central venous line, a tube that stays in a large vein for weeks or months for medical treatment.
- Have already had endocarditis. Endocarditis can damage heart tissue, which increases your risk of getting it again.
Risk factors for endocarditis
Many different things can cause germs to get into the bloodstream and lead to endocarditis. Having a faulty, diseased or damaged heart valve increases the risk of the condition. However, endocarditis may occur in those without heart valve problems.
Risk factors for endocarditis include:
- Older age. Endocarditis occurs most often in adults over age 60.
- Artificial heart valves. Germs are more likely to attach to an artificial (prosthetic) heart valve than to a regular heart valve.
- Damaged heart valves. Certain medical conditions, such as rheumatic fever or infection, can damage or scar one or more of the heart valves, increasing the risk of infection. A history of endocarditis also increases the risk of infection.
- Congenital heart defects. Being born with certain types of heart defects, such as an irregular heart or damaged heart valves, raises the risk of heart infections.
- Implanted heart device. Bacteria can attach to an implanted device, such as a pacemaker, causing an infection of the heart’s lining.
- Illegal IV drug use. Using dirty IV needles can lead to infections such as endocarditis. Contaminated needles and syringes are a special concern for people who use illegal IV drugs, such as heroin or cocaine.
- Poor dental health. A healthy mouth and healthy gums are essential for good health. If you don’t brush and floss regularly, bacteria can grow inside your mouth and may enter your bloodstream through a cut on your gums. Some dental procedures that can cut the gums also may allow bacteria to get in the bloodstream.
- Long-term catheter use. A catheter is a thin tube that’s used to do some medical procedures. Having a catheter in place for a long period of time (indwelling catheter) increases the risk of endocarditis.
If you’re at risk of endocarditis, tell your health care providers. You may want to request an endocarditis wallet card from the American Heart Association (https://www.heart.org/-/media/files/health-topics/infective-endocarditis/infective-endocarditis-wallet-card.pdf?la=en).
Endocarditis prevention
If you have a higher chance of developing endocarditis than most people, you can reduce your risk if you:
- Take good care of your teeth and gums every day
- Have dental exams and cleaning at your dentist’s office every 6 months
- Make heart-healthy habits part of your daily life to help prevent heart disease
- See your doctor right away if you have symptoms that could be endocarditis
- Don’t use illegal IV drugs. Dirty needles can send bacteria into the bloodstream, increasing the risk of endocarditis.
People with the highest risk for bacterial endocarditis need antibiotics before dental visits or certain medical or surgical procedures. You may want to request an endocarditis wallet card from the American Heart Association (https://www.heart.org/-/media/files/health-topics/infective-endocarditis/infective-endocarditis-wallet-card.pdf?la=en). Ask your doctor if you’re part of the highest risk group. If so, let all your healthcare providers know about your risk.
If you’re at high risk of endocarditis, the American Heart Association recommends taking antibiotics an hour before having any dental work done (https://www.heart.org/-/media/files/health-topics/infective-endocarditis/infective-endocarditis-wallet-card.pdf?la=en).
Antibiotic prophylaxis is reasonable before dental procedures that involve manipulation of the gingival tissue, manipulation of the periapical region of teeth, or perforation of the oral mucosa in patients with valvular heart disease who have any of the following (https://www.heart.org/-/media/files/health-topics/infective-endocarditis/infective-endocarditis-wallet-card.pdf?la=en):
- Prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts
- Prosthetic material used for cardiac valve repair, such as annuloplasty rings, chords or clips
- Previous bacterial endocarditis
- Unrepaired cyanotic congenital heart defect (CHD) or repaired congenital heart defect, with residual shunts or valvular regurgitation at the site of or adjacent to the site of a prosthetic patch or prosthetic device*
- A heart transplant with valve regurgitation due to a structurally abnormal valve
*Except for the conditions listed above, antibiotic prophylaxis before dental procedures is not recommended for any other types of congenital heart defect.
If you have endocarditis or any type of congenital heart disease, talk to your dentist and other care providers about your risks and whether you need preventive antibiotics.
What are the symptoms of endocarditis?
The symptoms of endocarditis can be hard to notice and unclear, developing slowly over weeks or sometimes months. In some cases, however, they can develop suddenly.
The most common symptoms of endocarditis are:
- Flu-like symptoms which don’t go away – these include having a temperature, tiredness, headaches, chills, a cough and sore throat. Flu symptoms tend to get better within 10 days, while endocarditis continues.
- Shivers, shakes and night sweats (fever in the night, so sheets or nightclothes may be wet when you wake). This is an important symptom to tell your doctor about.
- Poor appetite or unexplained weight loss
- Pale skin
- Aching muscles and joints
- Heart murmurs (an abnormal heart sound).
Other rarer symptoms you may see or feel include:
- small dark-colored spots on the skin (Osler nodes)
- unusual dark lines under your fingernails (splinter hemorrhages)
- red lumps on the fingers or toes that might be painful (Janeway lesions).
If you’ve been told you’re at high risk of developing endocarditis and you have flu-like symptoms with a high temperature for more than a week, see your doctor immediately. Early diagnosis makes treatment easier and more successful.
Endocarditis complications
When the germs are in your heart, they can clump together with blood cells. These clumps are called vegetations. These clumps can break off and travel through your bloodstream. They may block blood flow, spread infection, or damage your organs, including your brain, lungs, kidneys, and spleen. They can also travel to the arms and legs.
Endocarditis may sometimes lead to sepsis, a medical emergency that happens when your body has an extreme response to the infection.
Complications of endocarditis may include:
- Heart valve damage
- Heart failure
- Arrhythmia (a problem with the rate or rhythm of your heartbeat)
- Stroke
- Pockets of collected pus (abscesses) that develop in the heart, brain, lungs and other organs
- Blood clot in a lung artery (pulmonary embolism)
- Kidney damage
- Enlarged spleen
What are the long-term effects of endocarditis?
A lot of people with endocarditis need surgery, due to damage to the heart valves caused by the infection. There are potential complications including stroke. Infection can spread from the valve to places such as the joints or bones of the back, which may cause ongoing joint or back pain. One in five people die from endocarditis during a hospital stay.
How is endocarditis diagnosed?
Endocarditis can be difficult to diagnose. To find out if you have endocarditis, your doctor will:
- Ask about your medical history, including your symptoms, recent illnesses, and other health conditions that affect your chance of developing endocarditis.
- Do a physical exam.
- Likely order tests, such as:
- Blood culture test to check for signs of infection, bacteria, or fungi in your blood. Results from this test help determine the antibiotic or combination of antibiotics to use for treatment.
- Complete blood count. This test can determine if there’s a lot of white blood cells, which can be a sign of infection. A complete blood count can also help diagnose low levels of healthy red blood cells (anemia), which can be a sign of endocarditis. Other blood tests also may be done.
- Chest x-rays.
- An echocardiogram (heart ultrasound scan) can show an abnormal bacterial growth on the valve.
- In a standard (transthoracic) echocardiogram (TTE), a wandlike device (transducer) is moved over the chest area. The device directs sound waves at the heart and records them as they bounce back.
- In a transesophageal echocardiogram (TEE), a flexible tube containing a transducer is guided down the throat and into the tube connecting the mouth to the stomach (esophagus). A transesophageal echocardiogram provides much more detailed pictures of the heart than is possible with a standard echocardiogram.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. During an ECG, sensors (electrodes) are attached to the chest and sometimes to the arms or legs. It isn’t specifically used to diagnose endocarditis, but it can show if something is affecting the heart’s electrical activity.
- Chest X-ray. A chest X-ray shows the condition of the lungs and heart. It can help determine if endocarditis has caused heart swelling or if any infection has spread to the lungs.
- Computerized tomography (CT) scan or magnetic resonance imaging (MRI). You may need scans of your brain, chest or other parts of your body if your provider thinks that infection has spread to these areas.
Duke Criteria for the diagnosis of infective endocarditis
The Duke diagnostic criteria were developed by Durack and colleagues as a guide for reaching a valid definitive diagnosis of infective endocarditis 27. The Duke criteria combine the clinical, microbiologic, pathologic, and echocardiographic characteristics of a specific case 28, 25, 29, 30, 31.
A definitive clinical diagnosis can be made on the basis of the following 27:
- Clinical criteria
- Two major criteria; OR
- One major criterion and 3 minor criteria; OR
- Five minor criteria
- Pathologic criteria
- Microorganisms demonstrated by culture or histologic examination of a vegetation, a vegetation that has embolized, or an intracardiac abscess specimen; or
- Pathologic lesions; vegetation or intracardiac abscess confirmed by histologic examination showing active endocarditis
Major criteria
- Blood culture positive for infective endocarditis
- Typical microorganisms consistent with infective endocarditis from 2 separate blood cultures:
- Viridans streptococci, Streptococcus bovis, HACEK group, Staphylococcus aureus; or
- Community-acquired enterococci, in the absence of a primary focus; or
- Microorganisms consistent with infective endocarditis from persistently positive blood cultures, defined as follows:
- At least 2 positive cultures of blood samples drawn >12 hour apart; or
- All of 3 or a majority of ≥4 separate cultures of blood (with first and last sample drawn at least 1 hour apart)
- Single positive blood culture for Coxiella burnetii or antiphase I IgG antibody titer >1:800
- Evidence of endocardial involvement
- Echocardiogram positive for infective endocarditis (transesophageal echocardiography (TEE) recommended in patients with prosthetic valves, rated at least “possible infective endocarditis” by clinical criteria, or complicated infective endocarditis [paravalvular abscess]; transthoracic echocardiography (TTE) as first test in other patients), defined as follows:
- Oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation; or
- Myocardial abscess; or
- Development of partial dehiscence of a prosthetic valve
- New valvular regurgitation (worsening or changing of pre-existing murmur not sufficient)
- Echocardiogram positive for infective endocarditis (transesophageal echocardiography (TEE) recommended in patients with prosthetic valves, rated at least “possible infective endocarditis” by clinical criteria, or complicated infective endocarditis [paravalvular abscess]; transthoracic echocardiography (TTE) as first test in other patients), defined as follows:
Minor criteria
Minor criteria for infective endocarditis include the following:
- Predisposing heart condition or intravenous drug use
- Fever of 38°C (100.4°F) or higher
- Vascular phenomenon, including major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage, or Janeway lesions
- Immunologic phenomenon such as glomerulonephritis, Osler nodes, Roth spots, or rheumatoid factor
- Positive blood culture results not meeting major criteria or serologic evidence of active infection with an organism consistent with infective endocarditis
- Echocardiogram results consistent with infective endocarditis but not meeting major echocardiographic criteria
How is endocarditis treated?
If you have endocarditis, it’s important to get treatment quickly. Treatments may include 32, 33:
- Medicines
- Antibiotics to treat bacterial infections. Antibiotics are usually started through an intravenous (IV) line in the hospital.
- Antifungal medicine to treat fungal infections. Your doctor may suggest taking antifungal medicine for the rest of your life to prevent the infection from coming back.
- Heart surgery may be needed to repair or replace damaged valves and heart tissue. Surgery may also be done to remove infected tissue.
- Dental care, especially cleanings, can help reduce the amount of bacteria that grows in your mouth.
Treatment may last weeks, and you may need tests to make sure it’s working. Your doctor will also check you for problems that could develop from endocarditis, such as heart failure or an irregular heartbeat.
Many people with endocarditis are successfully treated with antibiotics. Sometimes, surgery may be needed to fix or replace damaged heart valves and clean up any remaining signs of the infection.
Endocarditis prognosis
Endocarditis prognosis largely depends on whether or not complications develop. Early detection and appropriate treatment of this uncommon disease can be lifesaving. The overall mortality rate has remained stable at 14.5% 34. There has been no overall improvement in outcomes of infective endocarditis of congenital heart disease 35.
Cure rates for appropriately managed (including both medical and surgical therapies) native valve endocarditis are as follows:
- For Streptococcus viridans and Streptococcus bovis infection, the rate is 98%.
- For enterococci and Staphylococcus aureus infection in individuals who abuse intravenous drugs, the rate is 90%.
- For community-acquired Staphylococcus aureus infection in individuals who do not abuse intravenous drugs, the rate is 60-70%.
- For infection with aerobic gram-negative organisms, the rate is 40-60%.
- For infection with fungal organisms, the rate is lower than 50%.
For prosthetic valve endocarditis, the cure rates are as follows:
- Rates are 10-15% lower for each of the above categories, for both early and late prosthetic valve endocarditis.
- Surgery is required far more frequently.
- Approximately 60% of early coagulase-negative staphylococcal prosthetic valve endocarditis cases and 70% of late coagulase-negative staphylococcal prosthetic valve endocarditis cases are curable.
Anecdotal reports describe the resolution of right-sided valvular infection caused by S aureus infection in individuals who abuse IV drugs after just a few days of oral antibiotics.
The role of early valvular surgery in reducing mortality among patients with infective endocarditis has become somewhat clearer. Challenges to resolving this question include the necessity of performing multicentered studies with an apparent difficulty of ensuring that the patients’ preoperative assessments and surgical approaches are comparable. The largest study to date indicates that in cases of infective endocarditis complicated by heart failure, valvular surgery reduces the 1-year mortality rate 36. More recent studies document that early surgery in patients, especially those with large vegetations, significantly reduces the risk for death from any cause 36, 37, 38, 39, 40, 41, 42, 43.
Mortality rates in native valve endocarditis range from 16% to 27%, and mortality rates in patients with prosthetic valve endocarditis are higher. More than 50% of these infections occur within 2 months after surgery. The fatality rate of pacemaker infective endocarditis ranges up to 34% 44, 45, 46, 47
Increased mortality rates are associated with older age, infection involving the aortic valve, development of congestive heart failure, central nervous system complications, and underlying disease such as diabetes mellitus 48. Catastrophic neurological events of all types as a result of infective endocarditis are highly predictive of morbidity and mortality.
Mortality rates also vary with the infecting organism. Acute endocarditis caused by Staphylococcus aureus is associated with a high mortality rate (30-40%), except when it is associated with IV drug use, whereas infective endocarditis resulting from streptococci has a mortality rate of approximately 10% 49, 50.
- Hirai T, Koster M. Osler’s nodes, Janeway lesions and splinter haemorrhages. Case Reports 2013;2013:bcr2013009759[↩][↩][↩]
- Marrie TJ. Osler’s nodes and Janeway lesions. Am J Med 2008;2013:105–6.[↩][↩]
- Osler W. Chronic infectious endocarditis. Q J Med 1909;2:219–30.[↩][↩]
- Silverman ME, Upshaw CB., Jr Extracardiac manifestations of infective endocarditis and their historical descriptions. Am J Cardiol. 2007;100(12):1802–7. doi: 10.1016/j.amjcard.2007.07.034[↩][↩]
- Beaulieu A, Rehman HU. Janeway lesions. CMAJ. 2010 Jul 13;182(10):1075. doi: 10.1503/cmaj.091528[↩][↩][↩][↩]
- Gunson, T.H. and Oliver, G.F. (2007), Osler’s nodes and Janeway lesions. Australasian Journal of Dermatology, 48: 251-255. https://doi.org/10.1111/j.1440-0960.2007.00397.x[↩][↩][↩]
- Sethi K, Buckley J, de Wolff J. Splinter haemorrhages, Osler’s nodes, Janeway lesions and Roth spots: the peripheral stigmata of endocarditis. Br J Hosp Med (Lond). 2013 Sep;74(9):C139-42.[↩][↩][↩]
- KERR, A., JR. and TAN, J.S. (1979), Biopsies of the Janeway Lesion of Infective Endocarditis. Journal of Cutaneous Pathology, 6: 124-129. https://doi.org/10.1111/j.1600-0560.1979.tb01113.x[↩][↩]
- Misin A, Di Bella S, Priolo L, Luzzati R. Image of the month: ‘Diagnostic hands’: Janeway lesions. Clin Med (Lond). 2017 Jul;17(4):373-374. doi: 10.7861/clinmedicine.17-4-373[↩][↩]
- Yee J, McAllister CK. Osler’s nodes and the recognition of infective endocarditis: a lesion of diagnostic importance. South Med J. 1987 Jun;80(6):753-7. doi: 10.1097/00007611-198706000-00020[↩]
- Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falcó V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF, Utili R, Wang A, Woods CW, Cabell CH; International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) Investigators. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009 Mar 9;169(5):463-73. doi: 10.1001/archinternmed.2008.603[↩]
- Servy A, Valeyrie-Allanore L, Alla F, Lechiche C, Nazeyrollas P, Chidiac C, Hoen B, Chosidow O, Duval X; Association Pour l’Etude et la Prévention de l’Endocardite Infectieuse Study Group. Prognostic value of skin manifestations of infective endocarditis. JAMA Dermatol. 2014 May;150(5):494-500. doi: 10.1001/jamadermatol.2013.8727[↩][↩]
- Habib G, Lancellotti P, Iung B. 2015 ESC Guidelines on the management of infective endocarditis: a big step forward for an old disease. Heart. 2016 Jul 1;102(13):992-4. doi: 10.1136/heartjnl-2015-308791[↩]
- Sandre RM, Shafran SD. Infective endocarditis: review of 135 cases over 9 years. Clin Infect Dis. 1996;22:276–86. doi: 10.1093/clinids/22.2.276[↩]
- Sapira JD. The art & science of bedside diagnosis. Baltimore: Urban & Schwarzenberg, Inc.; 1990. p. 197–8.[↩]
- Van Uitert RL, Solomon GE. White-centered retinal hemorrhages: a sign of intracranial hemorrhage. Neurology. 1979 Feb;29(2):236-9. doi: 10.1212/wnl.29.2.236[↩][↩]
- Chong Y, Han SJ, Rhee YJ, Kang SK, Yu JH, Na MH. Classic Peripheral Signs of Subacute Bacterial Endocarditis. Korean J Thorac Cardiovasc Surg. 2016 Oct;49(5):408-412. doi: 10.5090/kjtcs.2016.49.5.408[↩][↩]
- Duane TD, Osher RH, Green WR. White centered hemorrhages: their significance. Ophthalmology. 1980 Jan;87(1):66-9. doi: 10.1016/s0161-6420(80)35277-9[↩][↩][↩]
- Fred HL. Little black bags, ophthalmoscopy, and the Roth spot. Tex Heart Inst J. 2013;40(2):115-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3649782[↩][↩]
- Sachdeva AS, Gomez JO, Wattanakit K. A Case of Aortic Valve Infective Endocarditis with Dermatological Findings of Infective Endocarditis. Cureus. 2022 Mar 10;14(3):e23044. doi: 10.7759/cureus.23044[↩][↩][↩]
- Tikoo M, Bardia A, Gupta A, Pandey A. Dermatological Manifestations of Infective Endocarditis. J Gen Intern Med. 2015 Aug;30(8):1229-30. doi: 10.1007/s11606-015-3256-z[↩]
- Singal A, Arora R. Nail as a window of systemic diseases. Indian Dermatol Online J. 2015;6(2):67-74. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/[↩][↩]
- Lawry M, Daniel CR., 3rd . Nails in systemic disease. In: Scher RK, Daniel CR, editors. Nails: Diagnosis, Therapy, Surgery. 3rd ed. Philadelphia: Elsevier Science Limited; 2005. pp. 147–69.[↩]
- Haber R., Khoury R., Kechichian E., Tomb R. Splinter hemorrhages of the nails: a systematic review of clinical features and associated conditions. International Journal of Dermatology. 2016;55(12):1304–1310. doi: 10.1111/ijd.13347[↩]
- Guzek A, Braksator W, Gąsior Z, Kuśmierczyk M, Różański J, Rybicki Z. Infective endocarditis – can we treat it more effectively? Kardiochir Torakochirurgia Pol. 2020 Mar;17(1):8-14. doi: 10.5114/kitp.2020.94184[↩][↩][↩][↩]
- Yanagawa B, Bahji A, Lamba W, Tan DH, Cheema A, Syed I, Verma S. Endocarditis in the setting of IDU: multidisciplinary management. Curr Opin Cardiol. 2018 Mar;33(2):140-147. doi: 10.1097/HCO.0000000000000493[↩]
- Jennifer S. Li, Daniel J. Sexton, Nathan Mick, Richard Nettles, Vance G. Fowler, Jr., Thomas Ryan, Thomas Bashore, G. Ralph Corey, Proposed Modifications to the Duke Criteria for the Diagnosis of Infective Endocarditis, Clinical Infectious Diseases, Volume 30, Issue 4, April 2000, Pages 633–638, https://doi.org/10.1086/313753[↩][↩]
- Hackett AJ, Stuart J. Infective endocarditis: identification and management in the emergency department. Emerg Med Pract. 2020 Sep;22(9):1-24. https://www.ebmedicine.net/topics/cardiovascular/infective-endocarditis[↩]
- Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994 Mar;96(3):200-9. doi: 10.1016/0002-9343(94)90143-0[↩]
- Brusch JL. Infective endocarditis and its mimics in the critical care unit. Cunha BA, ed. Infectious Diseases in Critical Care. 2nd ed. New York, NY: Informa Healthcare; 2007. 261-2.[↩]
- Karchmer AW. Infective endocarditis. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 7th ed. WB Saunders Co; 2005. 1633-1658.[↩]
- Matthew E. Falagas, Katerina G. Manta, Fotinie Ntziora, Konstantinos Z. Vardakas, Linezolid for the treatment of patients with endocarditis: a systematic review of the published evidence, Journal of Antimicrobial Chemotherapy, Volume 58, Issue 2, August 2006, Pages 273–280, https://doi.org/10.1093/jac/dkl219[↩]
- Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, Douglas PS, Faxon DP, Gillam LD, Kimball TR, Kussmaul WG, Pearlman AS, Philbrick JT, Rakowski H, Thys DM, Antman EM, Smith SC Jr, Alpert JS, Gregoratos G, Anderson JL, Hiratzka LF, Hunt SA, Fuster V, Jacobs AK, Gibbons RJ, Russell RO; American College of Cardiology; American Heart Association; American Society of Echocardiography. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003 Sep 2;108(9):1146-62. doi: 10.1161/01.CIR.0000073597.57414.A9[↩]
- Mendiratta, P., Tilford, J.M., Prodhan, P., Cleves, M.A. and Wei, J.Y. (2009), Trends in Hospital Discharge Disposition for Elderly Patients with Infective Endocarditis: 1993 to 2003. Journal of the American Geriatrics Society, 57: 877-881. https://doi.org/10.1111/j.1532-5415.2009.02224.x[↩]
- Ortiz-Bautista C, López J, García-Granja PE, Vilacosta I, Sevilla T, Sarriá C, Olmos C, Ferrera C, Sáez C, Puerto A, San Román JA. Right-sided infective endocarditis in cardiac device carriers: Clinical profile and prognosis. Med Clin (Barc). 2017 Dec 7;149(11):477-482. English, Spanish. doi: 10.1016/j.medcli.2017.03.055[↩]
- Sonneville R, Mirabel M, Hajage D, Tubach F, Vignon P, Perez P, Lavoué S, Kouatchet A, Pajot O, Mekontso Dessap A, Tonnelier JM, Bollaert PE, Frat JP, Navellou JC, Hyvernat H, Hssain AA, Tabah A, Trouillet JL, Wolff M; ENDOcardite en REAnimation Study Group. Neurologic complications and outcomes of infective endocarditis in critically ill patients: the ENDOcardite en REAnimation prospective multicenter study. Crit Care Med. 2011 Jun;39(6):1474-81. doi: 10.1097/CCM.0b013e3182120b41[↩][↩]
- Kiefer T, Park L, Tribouilloy C, Cortes C, Casillo R, Chu V, Delahaye F, Durante-Mangoni E, Edathodu J, Falces C, Logar M, Miró JM, Naber C, Tripodi MF, Murdoch DR, Moreillon P, Utili R, Wang A. Association between valvular surgery and mortality among patients with infective endocarditis complicated by heart failure. JAMA. 2011 Nov 23;306(20):2239-47. doi: 10.1001/jama.2011.1701[↩]
- Kang DH, Kim YJ, Kim SH, Sun BJ, Kim DH, Yun SC, Song JM, Choo SJ, Chung CH, Song JK, Lee JW, Sohn DW. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012 Jun 28;366(26):2466-73. doi: 10.1056/NEJMoa1112843[↩]
- Thuny F, Grisoli D, Collart F, Habib G, Raoult D. Management of infective endocarditis: challenges and perspectives. Lancet. 2012 Mar 10;379(9819):965-975. doi: 10.1016/S0140-6736(11)60755-1[↩]
- Wallace SM, Walton BI, Kharbanda RK, Hardy R, Wilson AP, Swanton RH. Mortality from infective endocarditis: clinical predictors of outcome. Heart. 2002 Jul;88(1):53-60. doi: 10.1136/heart.88.1.53[↩]
- Durante-Mangoni E, Bradley S, Selton-Suty C, Tripodi MF, Barsic B, Bouza E, Cabell CH, Ramos AI, Fowler V Jr, Hoen B, Koneçny P, Moreno A, Murdoch D, Pappas P, Sexton DJ, Spelman D, Tattevin P, Miró JM, van der Meer JT, Utili R; International Collaboration on Endocarditis Prospective Cohort Study Group. Current features of infective endocarditis in elderly patients: results of the International Collaboration on Endocarditis Prospective Cohort Study. Arch Intern Med. 2008 Oct 27;168(19):2095-103. doi: 10.1001/archinte.168.19.2095[↩]
- Chu VH, Cabell CH, Benjamin DK Jr, Kuniholm EF, Fowler VG Jr, Engemann J, Sexton DJ, Corey GR, Wang A. Early predictors of in-hospital death in infective endocarditis. Circulation. 2004 Apr 13;109(14):1745-9. doi: 10.1161/01.CIR.0000124719.61827.7F[↩]
- Prophylaxis against infective endocarditis: antimicrobial prophylaxis against infective endocarditis in adults and children undergoing interventional procedures. https://www.nice.org.uk/guidance/cg64[↩]
- Cengiz Özcan, Jakob Raunsø, Morten Lamberts, Lars Køber, Tommi Bo Lindhardt, Niels Eske Bruun, Marie Louise Laursen, Christian Torp-Pedersen, Gunnar Hilmar Gislason, Morten Lock Hansen, Infective endocarditis and risk of death after cardiac implantable electronic device implantation: a nationwide cohort study, EP Europace, Volume 19, Issue 6, June 2017, Pages 1007–1014, https://doi.org/10.1093/europace/euw404[↩]
- Cresti A, Chiavarelli M, Scalese M, Nencioni C, Valentini S, Guerrini F, D’Aiello I, Picchi A, De Sensi F, Habib G. Epidemiological and mortality trends in infective endocarditis, a 17-year population-based prospective study. Cardiovasc Diagn Ther. 2017 Feb;7(1):27-35. doi: 10.21037/cdt.2016.08.09[↩]
- Janga KC, Sinha A, Greenberg S, Sharma K. Nephrologists Hate the Dialysis Catheters: A Systemic Review of Dialysis Catheter Associated Infective Endocarditis. Case Rep Nephrol. 2017;2017:9460671. doi: 10.1155/2017/9460671[↩]
- Baddour LM, Epstein AE, Erickson CC, Knight BP, Levison ME, Lockhart PB, Masoudi FA, Okum EJ, Wilson WR, Beerman LB, Bolger AF, Estes NA 3rd, Gewitz M, Newburger JW, Schron EB, Taubert KA; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee; Council on Cardiovascular Disease in Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Nursing; Council on Clinical Cardiology; Interdisciplinary Council on Quality of Care; American Heart Association. Update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. Circulation. 2010 Jan 26;121(3):458-77. doi: 10.1161/CIRCULATIONAHA.109.192665[↩]
- Eknoyan G, Lister BJ, Kim HS, Greenberg SD. Renal complications of bacterial endocarditis. Am J Nephrol. 1985;5(6):457-69. doi: 10.1159/000166984[↩]
- Pruitt AA, Rubin RH, Karchmer AW, Duncan GW. Neurologic complications of bacterial endocarditis. Medicine (Baltimore). 1978 Jul;57(4):329-43. doi: 10.1097/00005792-197807000-00004[↩]
- Soong G, Chun J, Parker D, Prince A. Staphylococcus aureus activation of caspase 1/calpain signaling mediates invasion through human keratinocytes. J Infect Dis. 2012 May 15;205(10):1571-9. doi: 10.1093/infdis/jis244[↩]