What is PMS
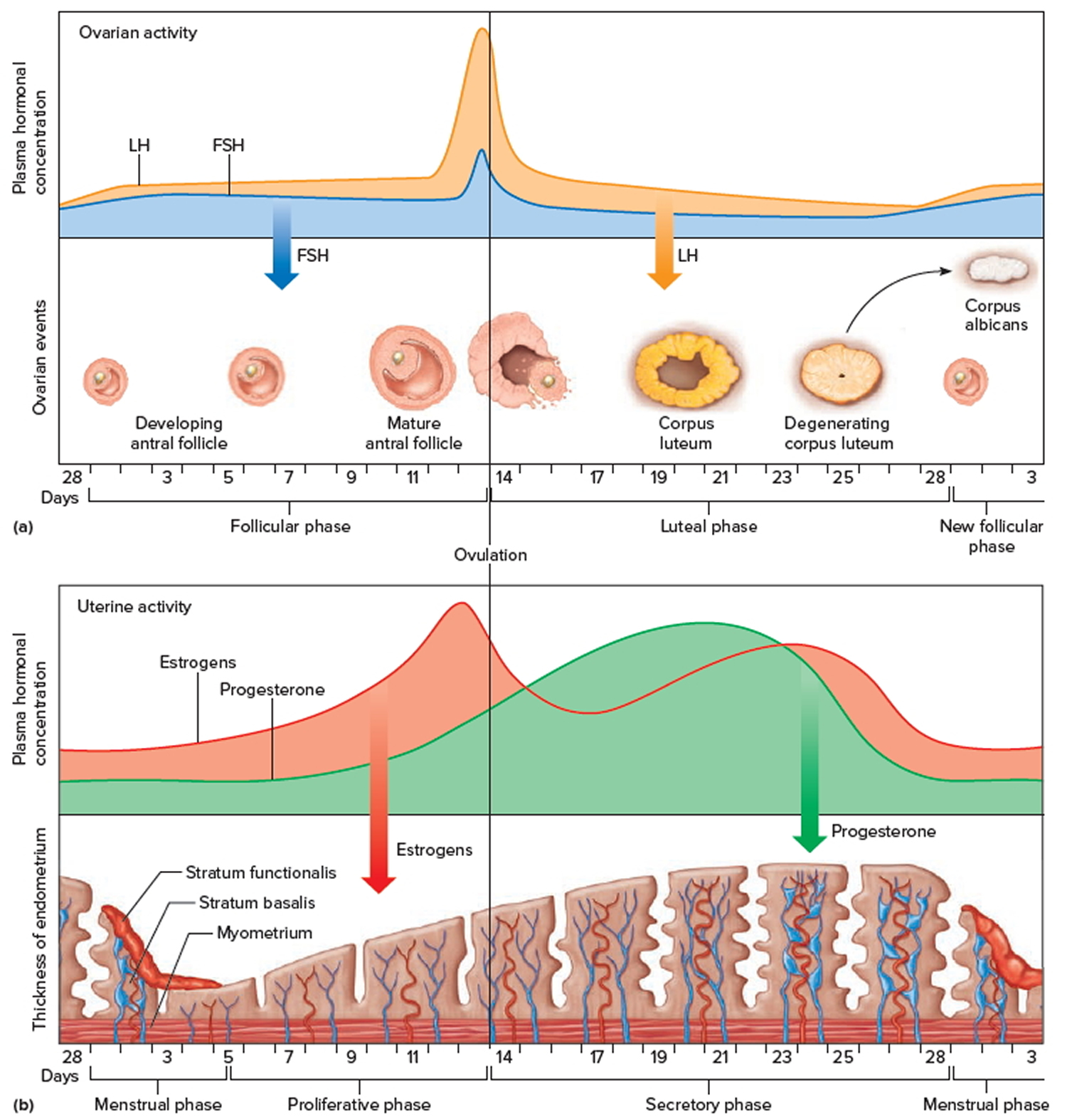
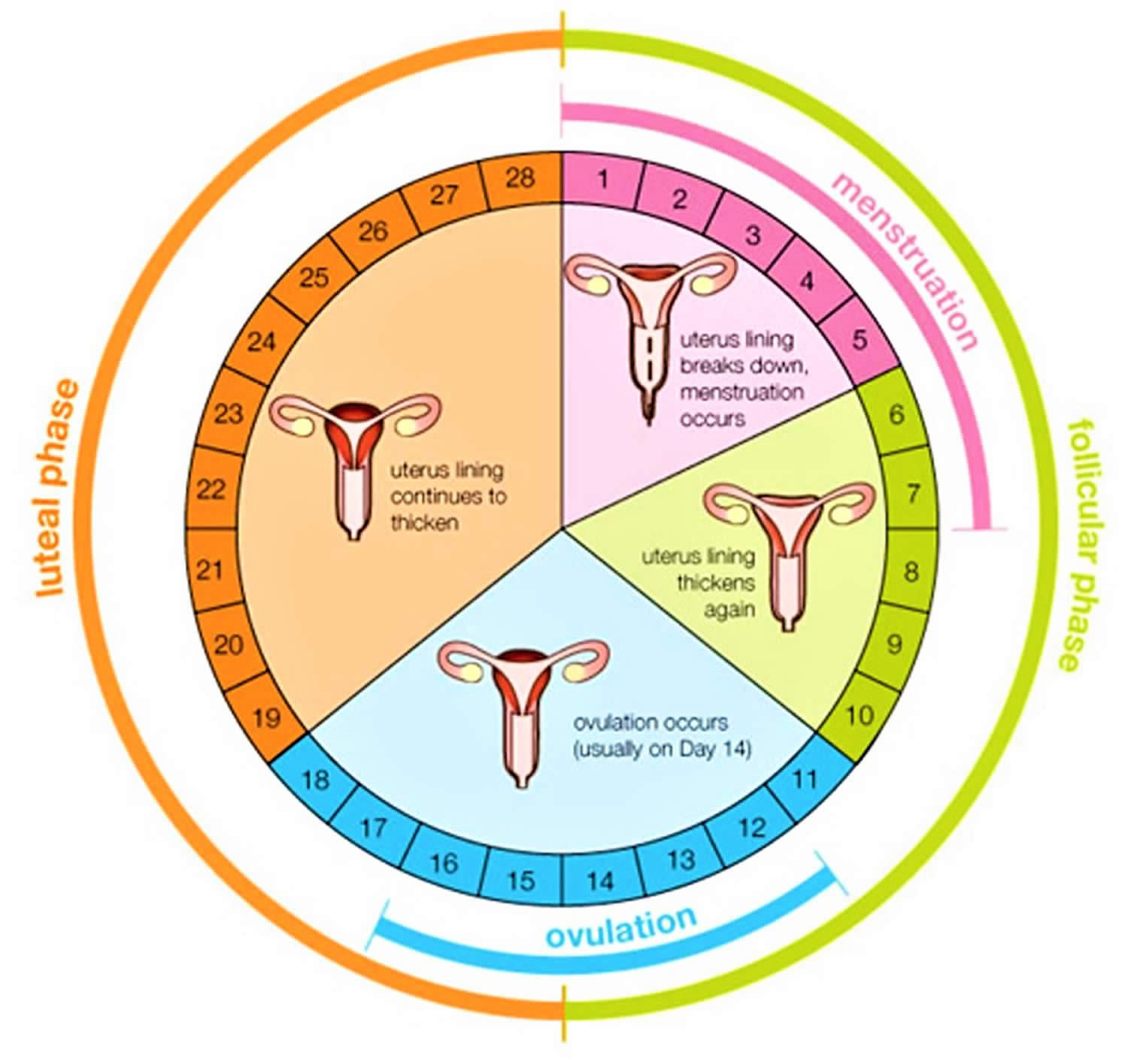
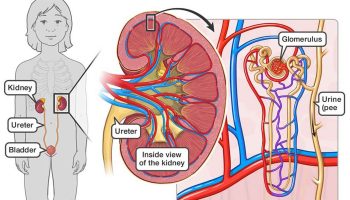
PMS commonly called premenstrual syndrome or premenstrual tension (PMT), is a group of symptoms that start one to two weeks before your period (after ovulation) and finishing during your period. PMS is a combination of physical and emotional symptoms that many women get after ovulation and before the start of their menstrual period. Researchers think that PMS happens in the days after ovulation because estrogen and progesterone levels begin falling dramatically if you are not pregnant (see Figure 2. Ovarian activity during the Menstrual cycle). PMS symptoms go away within a few days after a woman’s period starts as hormone levels begin rising again.
Most women, over 90%, have at least some symptoms of PMS, and the symptoms go away after your period start 1. For some women, the symptoms are severe enough to interfere with their lives. They have a type of PMS called premenstrual dysphoric disorder (PMDD). About 90% of women of childbearing age have some PMS problems. About 2% to 10% of women in this age group have PMDD (premenstrual dysphoric disorder).
Many women experience premenstrual symptoms, especially those between their 20s and 40s. Other women have such severe symptoms that their lives are disrupted for a week or two every month. PMS symptoms can often get worse when a woman is in her thirties and may continue to be a problem until menopause. PMS often improves after the menopause.
Some isolated reports indicate varying individual symptoms but not the overall prevalence of premenstrual symptoms among different racial groups. Although premenstrual clinics are reported to be almost exclusively attended by white women, community-based studies found no difference in the prevalence or severity of premenstrual symptoms between black women and white women. Black women tend to have a higher prevalence of food cravings than white women. White women are more likely than black women to report premenstrual mood changes and weight gain.
PMS settles completely once your period is over, so there is always a time in your menstrual cycle when you have no symptoms at all. If your PMS symptoms continue after your menstrual period, then the cause may be something other than PMS, like depression, approaching menopause or thyroid problems.
Common PMS symptoms include:
- Breast swelling and tenderness
- Acne
- Abdominal bloating and constipation
- Fluid retention and weight gain
- Pain – headache or joint pain
- Food cravings
- Irritability, mood swings, crying spells, depression – feeling down, tearful, irritable, anxious, angry
- Tiredness
- Nausea
- Food cravings
- Aches and pains
- Headaches (or even migraines)
- Difficulty concentrating
Although the causes of PMS are unknown, it is thought to be linked to changing hormone levels. No single PMS treatment works for everyone. Over-the-counter pain relievers such as ibuprofen, aspirin or naproxen may help ease cramps, headaches, backaches and breast tenderness. Exercising, getting enough sleep, and avoiding salt, caffeine, and alcohol can also help.
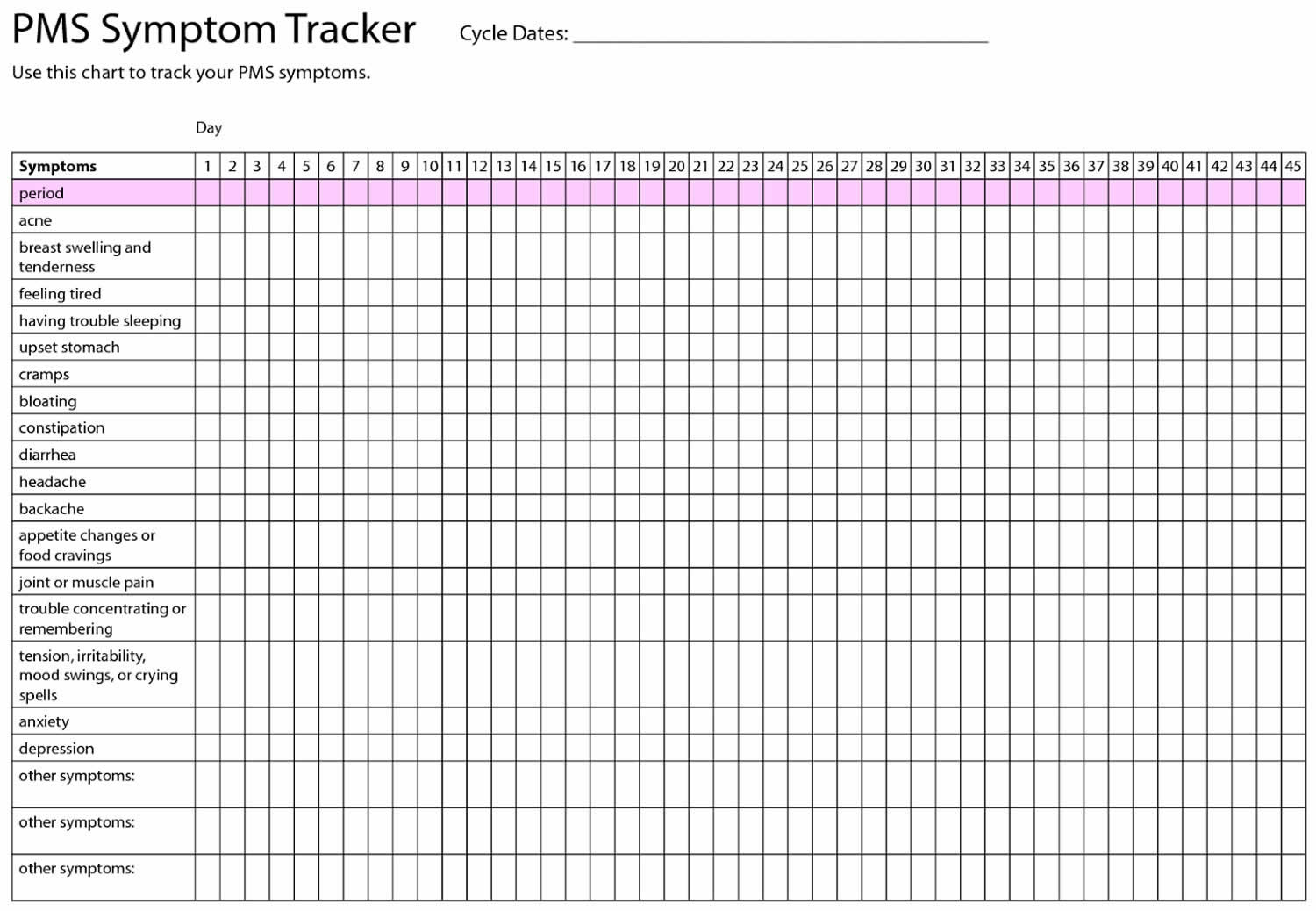
It may be useful to keep a calendar record of your menstrual cycle. This will help you to know when your symptoms usually start, so you can try to manage them or avoid the things that cause you stress around that time.
Try explaining the situation to the person or people you live with. This will help them to be more understanding of you at this time.
A healthy lifestyle seems to help with PMS symptoms. Eat plenty of fruit, vegetables and whole grains and cut down on salt, coffee, alcohol, sugar and cigarettes. Some women find that eating smaller meals more frequently helps as well.
Get some regular aerobic exercise – aim for half an hour every day. Get plenty of sleep. Try to lower your general stress level. Consider learning relaxation techniques, yoga, meditation or tai chi, or have a regular massage.
If your premenstrual syndrome symptoms are severe and you haven’t been able to manage your premenstrual syndrome with lifestyle changes and the symptoms of PMS are affecting your health and daily activities, you should discuss treatment options (including hormone therapy) with your doctor.
Figure 1. PMS symptoms tracker
Footnote: To help establish a premenstrual pattern, your doctor may have you record your signs and symptoms on a calendar or in a diary for at least two menstrual cycles. Note the day that you first notice PMS symptoms, as well as the day they disappear. Also be sure to mark the days your period starts and ends.
When does PMS start?
PMS symptoms usually start 7 to 14 days before your period and improve when your period starts.
How long does PMS last?
PMS symptoms usually start 7 to 14 days before your period and PMS settles completely once your period is over.
Does PMS change with age?
Yes. PMS symptoms may get worse as you reach your late 30s or 40s and approach menopause and are in the transition to menopause, called perimenopause 2.
This is especially true for women whose moods are sensitive to changing hormone levels during the menstrual cycle. In the years leading up to menopause, your hormone levels also go up and down in an unpredictable way as your body slowly transitions to menopause. You may get the same mood changes, or they may get worse.
PMS stops after menopause when you no longer get a period.
Who gets PMS?
As many as three in four women say they get PMS symptoms at some point in their lifetime 3. For most women, PMS symptoms are mild.
Less than 5% of women of childbearing age get a more severe form of PMS, called premenstrual dysphoric disorder (PMDD) 4.
PMS may happen more often in women who:
- Have high levels of stress 5
- Have a family history of depression 6
- Have a personal history of either postpartum depression or depression 7
How is PMS diagnosed?
There is no single test for PMS. Your doctor will talk with you about your symptoms, including when they happen and how much they affect your life.
You probably have PMS if you have symptoms that 8:
- Happen in the 5 days before your period for at least three menstrual cycles in a row
- End within 4 days after your period starts
- Keep you from enjoying or doing some of your normal activities
Keep track of which PMS symptoms you have and how severe they are for a few months. Write down your symptoms each day on a calendar or with an app on your phone. Take this information with you when you see your doctor.
Can other conditions mimic PMS?
Symptoms of other conditions can mimic PMS or overlap with PMS. Some of these conditions include the following:
- depression
- anxiety
- perimenopause
- chronic fatigue syndrome
- irritable bowel syndrome
- thyroid disease
Depression and anxiety disorders are the most common conditions that overlap with PMS. About one half of women seeking treatment for PMS have one of these disorders. The symptoms of depression and anxiety are much like the emotional symptoms of PMS. Women with depression, however, often have symptoms that are present all month long. These symptoms may worsen before or during their periods. Your health care provider will want to find out whether you have one of these conditions if you are having PMS symptoms.
Can PMS make other conditions worse?
In addition to depression and anxiety, symptoms of other disorders can get worse right before your period. Examples include seizure disorders, migraines, asthma, and allergies.
About half of women who need relief from PMS also have another health problem, which may get worse in the time before their menstrual period 9. These health problems share many symptoms with PMS and include:
- Depression and anxiety disorders.These are the most common conditions that overlap with PMS. Depression and anxiety symptoms are similar to PMS and may get worse before or during your period.
- Myalgic encephalomyelitis/chronic fatigue syndrome. Some women report that their symptoms often get worse right before their period. Research shows that women with myalgic encephalomyelitis/chronic fatigue syndrome may also be more likely to have heavy menstrual bleeding and early or premature menopause 10
- Irritable bowel syndrome (IBS). IBS causes cramping, bloating, and gas. Your IBS symptoms may get worse right before your period.
- Bladder pain syndrome. Women with bladder pain syndrome are more likely to have painful cramps during PMS.
Figure 2. Ovarian activity during the Menstrual cycle
Note: Major events in the female menstrual cycle. (a) Plasma hormonal concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) affect follicle maturation in the ovaries. (b) Plasma hormonal concentrations of estrogen and progesterone influence changes in the uterine lining.
PMS depression
PMS depression is more commonly called premenstrual dysphoric disorder (PMDD) is a more severe form of premenstrual syndrome (PMS) characterized by extreme mood swings, anxiety, irritability, and depression, occurring in the week or two before your period starts (the luteal phase), most commonly in the days preceding menstruation 11, 12, 13, 14. And your symptoms usually go away two to three days after your period starts. Premenstrual Dysphoric Disorder (PMDD) is considered a mood disorder affecting young adult women that causes significant emotional, psychological, and physical symptoms, with significant distress or impairment in menstruating women during the the second half of a menstrual cycle occurring after ovulation and before the next period of your menstrual cycle. Premenstrual Dysphoric Disorder (PMDD) symptoms include mood swings, irritability, depression and fatigue are usually so severe that the young or adult woman misses school, work and/or avoids her regular social activities.
The symptoms of premenstrual dysphoric disorder (PMDD) are:
- Sadness and crying
- Feeling nervous or anxious
- Anger or irritability
- Strong cravings for certain foods
- Problems paying attention and concentrating
- Fatigue, tiredness, loss of energy
- Physical problems such as breast tenderness, headaches, joint or muscle pain and swelling or bloating
- Trouble sleeping
- Very depressed mood, feeling hopeless
- Marked anxiety, tension, edginess
- Sudden mood shifts (crying easily, extreme sensitivity)
- Persistent, marked irritability, anger, increased conflicts
- Loss of interest in usual activities (work, school, socializing, etc.)
- Difficulty concentrating and staying focused
- Marked appetite change, overeating, food cravings
- Insomnia (difficulty sleeping) or sleeping too much
- Feeling out of control or overwhelmed
- Physical symptoms such as weight gain, bloating, breast tenderness or swelling, headache, and muscle or joint aches and pains
The cause of premenstrual dysphoric disorder (PMDD) isn’t clear. Underlying depression and anxiety are common in both PMS and premenstrual dysphoric disorder (PMDD), so it’s possible that the hormonal changes that trigger a menstrual period worsen the symptoms of mood disorders.
Epidemiological studies indicate that as many as 80% of women in the US experience emotional, behavioral, or physical premenstrual symptoms.
Worldwide, premenstrual dysphoric disorder (PMDD) affects 3-8% of women in their reproductive years, and has varying degrees of severity that interfere with work, social activities, or interpersonal relationships 15. Premenstrual dysphoric disorder (PMDD) is a multifactorial syndrome that imposes an enormous burden on women, their families, and the health care system. A recent study from India reported a similar frequency.
Women in the late third to middle fourth decades of life are most vulnerable to experiencing premenstrual dysphoric disorder.
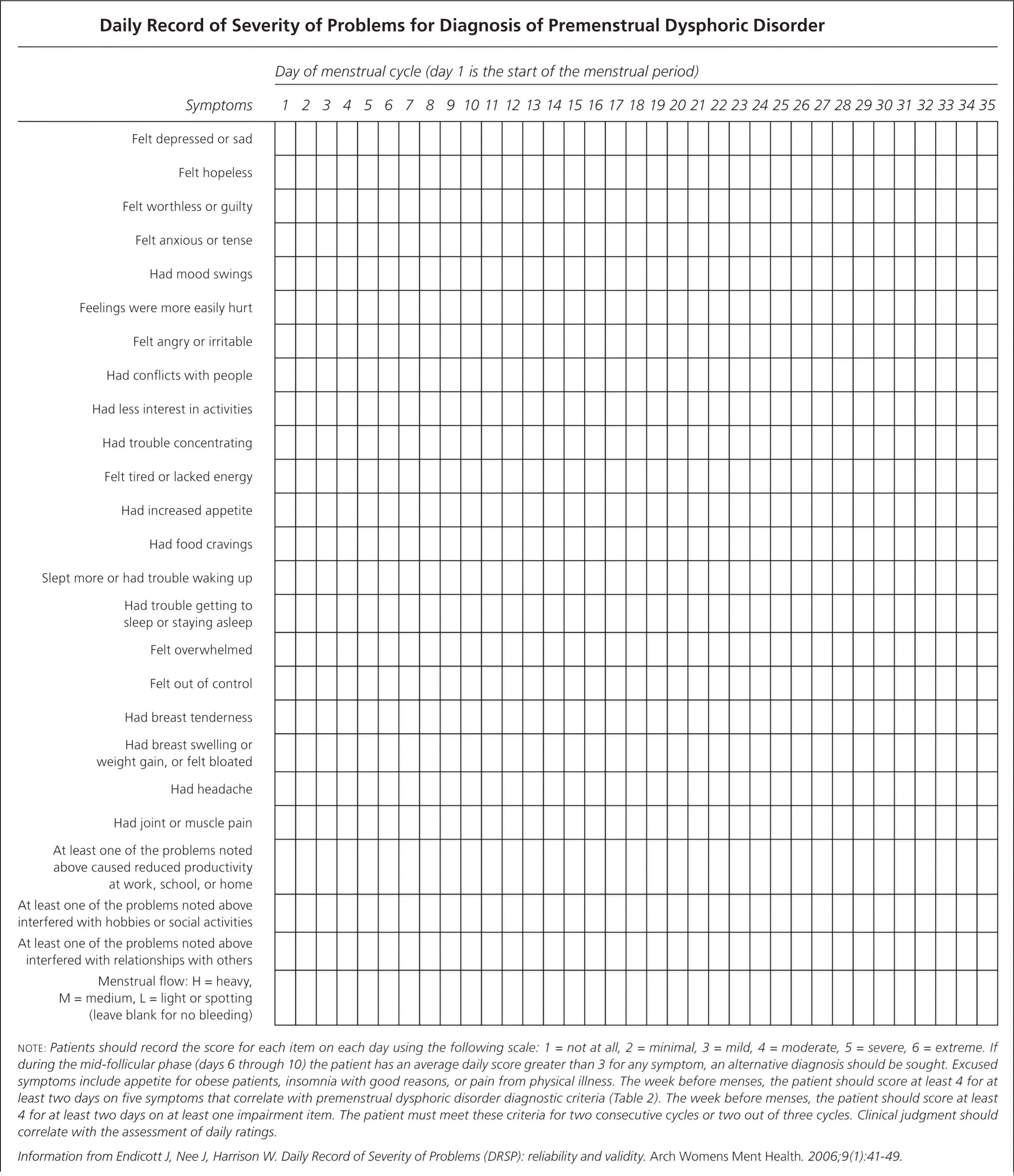
To help diagnose PMDD, your doctor may ask you to chart your symptoms (see sample chart in Figure 3 below).
Premenstrual Dysphoric Disorder (PMDD) affects up to 5% of women of childbearing age 16. If you suspect you have Premenstrual Dysphoric Disorder (PMDD), it’s important to talk to your doctor. A thorough medical evaluation may determine if your symptoms are due to premenstrual dysphoric disorder or some other condition. If you’re diagnosed with premenstrual dysphoric disorder (PMDD), your doctor can recommend specific treatments to help minimize your symptoms. Premenstrual Dysphoric Disorder (PMDD) treatment options may include dietary and lifestyle changes, medications such as antidepressants or birth control pills or other therapies.
Treatments for PMDD include:
- Diet and lifestyle changes. Regular exercise often reduces premenstrual symptoms. Cutting back on caffeine, avoiding alcohol and stopping smoking may ease symptoms, too. Getting enough sleep and using relaxation techniques, such as mindfulness, meditation and yoga, also may help. Avoid stressful and emotional triggers, such as arguments over financial issues or relationship problems, whenever possible.
- Nutritional supplements. Consuming 1,200 milligrams of calcium daily may possibly reduce symptoms of PMS and PMDD. Vitamin B6 (pyridoxine), magnesium and L-tryptophan also may help, but talk with your doctor for advice before taking any supplements.
- Herbal remedies. Some research suggests that chasteberry (Vitex agnus-castus) may possibly reduce irritability, mood swings, breast tenderness, swelling, cramps and food cravings associated with PMDD, but more research is needed. The U.S. Food and Drug Administration doesn’t regulate herbal supplements, so talk with your doctor before trying one.
- Antidepressants called selective serotonin reuptake inhibitors (SSRIs). SSRIs change serotonin levels in your brain. The Food and Drug Administration (FDA) approved three SSRIs to treat PMDD:
- Sertraline
- Fluoxetine
- Paroxetine
- Birth control pills. The FDA has approved a birth control pill containing drospirenone and ethinyl estradiol, to treat PMDD.
- Over-the-counter pain relievers may help relieve physical symptoms, such as cramps, joint pain, headaches, backaches, and breast tenderness. These include:
- Ibuprofen
- Naproxen
- Aspirin
- Stress management, such as relaxation techniques and spending time on activities you enjoy 17
Making healthy changes, such as eating a healthy combination of foods across the food groups, cutting back on salty and sugary foods, and getting more physical activity, may also help relieve some PMDD symptoms. But PMDD can be serious enough that some women should go to a doctor to discuss treatment options. According to a meta-analysis, women with PMDD have a fourfold higher risk of suicidal thoughts and a sevenfold higher risk of suicidal attempts 18. And, if you are thinking of hurting yourself or others, call your local emergency services number right away.
How do I know if I have PMS depression?
In both premenstrual dysphoric disorder (PMDD) and PMS, symptoms usually begin seven to 10 days before your period starts and continue for the first few days that you have your period. Both premenstrual dysphoric disorder and PMS may also cause bloating, breast tenderness, fatigue, and changes in sleep and eating habits. In premenstrual dysphoric disorder, however, at least one of these emotional and behavioral symptoms stands out:
- Sadness or hopelessness
- Anxiety or tension
- Extreme moodiness
- Marked irritability or anger
These symptoms can affect your relationships and work ability. If you have some of these symptoms 10 to 14 days before your period and they improve when your period starts, you might have premenstrual dysphoric disorder (PMDD).
The American Psychiatric Association 19 focuses predominantly on psychiatric symptoms in its diagnostic criteria for premenstrual dysphoric disorder (PMDD) see Table 1.
To meet the diagnostic criteria for premenstrual dysphoric disorder (PMDD), a patient must have at least five of the symptoms listed in Table 1 in the week before menses, and these symptoms must improve within a few days after the onset of menses 19.
Premenstrual dysphoric disorder symptoms are not always present. Symptoms disappear during or by the end of menses, and return at about the same time during following cycles. If symptoms are present every day, then they are unlikely to be due to premenstrual dysphoric disorder (PMDD).
To be considered premenstrual dysphoric disorder (PMDD), symptoms must be severe enough to impact on the functioning of daily life, that is, to interfere with work, school, social activities or interpersonal relationships.
Women with premenstrual dysphoric disorder (PMDD) may have associated medical or psychiatric disorders. Some of the more commonly associated conditions are mood (depression and bipolar [manic-depressive] disorder) and anxiety disorders. Sometimes, these conditions begin before the onset of premenstrual dysphoric disorder. Sometimes, they appear later. If there is a co-existing condition, it may get worse in the premenstrual phase of the cycle.
What causes PMS depression?
The exact cause of premenstrual dysphoric disorder (PMDD) is not known 13, 14. Changes in hormones related to your period may cause premenstrual dysphoric disorder. Several studies suggest that cyclical changes in estrogen and progesterone levels trigger the symptoms 20, 21, 22. However, premenstrual dysphoric disorder (PMDD) does not appear to be caused simply by an imbalance of female ovarian hormones. Research measuring estrogen and progesterone levels across the menstrual cycle found no difference between women with premenstrual dysphoric disorder (PMDD) and those without the disorder. On the other hand, hormones must play some role because premenstrual dysphoric disorder symptoms disappear if the ovaries are removed or not functioning (e.g. menopause). Recent evidence from research studies suggests that estrogen and progesterone hormone release patterns are normal in women with PMS or PMDD, but they have a heightened sensitivity to cyclical variations in levels of estrogen and progesterone hormones, which predisposes them to experience mood, behavioral, and somatic symptoms 22.
Postmenopausal women who had previously been diagnosed with PMS had recurrent psychiatric and physical symptoms when they received cyclical progestogen therapy 20. Furthermore, the suppression of estrogen with gonadotropin-releasing hormone (GnRH) analogues has been shown to significantly improve PMS symptoms 21.
Current theories suggest that normal ovarian function may trigger changes in brain chemistry in women predisposed to premenstrual dysphoric disorder (PMDD). One brain chemical that may be especially important is serotonin, a neurotransmitter. The serotonin system has a close relationship to the female hormones, and imbalances of the serotonin system may play an important role in causing premenstrual dysphoric disorder. Another tie-in is that medications most effective for treating premenstrual dysphoric disorder are those with specific effects on serotonin.
Changes in mood may be attributable to the effect estrogen and progesterone have on the serotonin, gamma-aminobutyric acid (GABA), and dopamine systems 22. These can also alter the renin-angiotensin-aldosterone system (RAAS), which could explain some of the bloating and swelling that occur during the luteal phase 22. Sex hormone levels alone cannot fully explain premenstrual disorders. Studies show that women diagnosed with a premenstrual disorder do not have higher levels of estrogen or progesterone than the general population, and accepted explanations as to why some women could be more sensitive to fluctuations in these sex hormones are lacking 16.
Premenstrual dysphoric disorder may also be inherited. Studies have shown that identical twins are more likely to share the disorder (93%) than non-identical twins (44%), and daughters of mothers with premenstrual dysphoric disorder are more likely to have it themselves. However, no specific genes have been identified to account for premenstrual dysphoric disorder 23. Therefore there may be a genetic predisposition to developing the disorder.
Psychological, social and cultural factors also may be involved in causing premenstrual dysphoric disorder or at least in the expression of premenstrual dysphoric disorder symptoms. Stressful life events and a family history of PMS or premenstrual dysphoric disorder may increase your chances of getting premenstrual dysphoric disorder. Major depression is common in women who have premenstrual dysphoric disorder. However, not all women who have premenstrual dysphoric disorder have major depression. Moreover, these factors alone are inadequate to explain the disorder, which almost certainly has a biological basis.
Risk factors for PMS depression
Proven Risk Factors
- Past traumatic events: Traumatic events and preexisting anxiety disorders are risk factors for the development of premenstrual dysphoric disorder (PMDD). The underlying mechanisms are unknown, making further investigation necessary 24.
- Cigarette smoking: There is a strong association of moderate-to-severe forms of PMS with current smoking status compared to non-smokers. The risk is elevated even for former smokers and the risk of incident PMS tends to increase with the quantity of cigarette smoking. Furthermore, the risk of premenstrual dysphoric disorder (PMDD) is significantly higher for women who began smoking during adolescence 25
- Obesity: There is a strong linear relationship between body mass index (BMI) at baseline and risk of incident PMS. For each 1 kg/m² increase, there was a significant associated increase (3%). The risk of PMS rose significantly in women with body mass index (BMI) at or higher than 27.5 kg/m² compared with women with a BMI of less than 20 kg/m². Relative risk in women with a BMI of 35.0 kg/m² was 1.66 26. Relative risk (RR) is a ratio of the probability of an event occurring in the exposed group versus the probability of the event occurring in the non-exposed group 27. In this example, in women with a BMI of 35.0 kg/m² a a relative risk of 1.66 means that the risk of an event occurring is 66% higher in the exposed group compared to the unexposed group.
Speculative Risk Factor
- Genetics: Twin studies have implicated heritable factors in the development of PMS (Premenstrual Syndrome) and premenstrual dysphoric disorder (PMDD). Recent studies have provided support for the involvement of the gene that codes for the serotonergic 5HT1A receptor 28 and genetic mutations of the estrogen receptor alpha gene (ESR1) in the development of PMS and PMDD 29.
PMS depression signs and symptoms
Premenstrual Dysphoric Disorder (PMDD) symptoms can include:
- Emotional or Mood symptoms
- Severe irritability with frequent conflicts with family members or at work
- Anger
- Anxiety or the feeling of being on edge all the time
- Depression
- Feelings of sadness, hopeless, worthless or despair
- Mood swings, suddenly feeling sad or tearful
- Feeling overwhelmed or out of control
- Crying spells.
- Cognitive symptoms
- Difficulty concentrating
- Lack of interest in normal activities
- Feeling overwhelmed.
- Physical symptoms
- Fatigue
- Changes in appetite or sleep
- Breast swelling or tenderness
- Bloating or weight gain
- Headaches
- Joint pain
- Muscle aches
- Lack of energy
- Fatigability
- Behavioral symptoms
- Social withdrawal
- Changes in libido
- Changes in appetite, either overeating or craving a specific food
- Changes in sleep pattern, either hypersomnia or insomnia
These symptoms typically begin in the week or two before menstruation and usually subside a few days after menstruation begins. The length of time for which the women experience symptoms of Premenstrual Dysphoric Disorder (PMDD) varies from a few days to 2 weeks. For most symptomatic women, symptoms intensify 6 days before and are the most severe 2 days before the menses 30, 31. Of all the symptoms mentioned, anger and irritability are the most distressing and are experienced slightly before the other symptoms 30. Premenstrual Dysphoric Disorder (PMDD) symptoms can be so severe that they can disrupt daily life, impacting relationships, work, and overall well-being.
PMS depression Complications
Premenstrual Dysphoric Disorder (PMDD) symptoms may be severe enough to interfere with a woman’s daily life. Women with depression may have worse symptoms during the second half of their cycle and may need changes in their medicine.
Some women with Premenstrual Dysphoric Disorder (PMDD) have suicidal thoughts. Suicide in women with depression is more likely to occur during the second half of their menstrual cycle. If you or someone you know is thinking about suicide call your local emergency services number right away. The Suicide and Crisis Lifeline provides free and confidential support 24/7, anytime day or night.
Premenstrual Dysphoric Disorder (PMDD) may be associated with eating disorders and smoking.
How is PMS depression diagnosed?
Your doctor will talk to you about your health history and do a physical examination. You will need to keep a calendar or diary of your symptoms to help your doctor diagnose PMDD. Your doctor may also want to perform some laboratory tests to exclude the possibility of any illness responsible for causing your symptoms. Illnesses that may cause similar symptoms include anemia, migraines, endometriosis, menopause, and thyroid disease. These tests include a blood test that will be analyzed to see the total number of the different types of cells (full blood count), thyroid function tests, and the level of follicle stimulating hormone (FSH) in the blood.
Premenstrual Dysphoric Disorder DSM-5 Diagnostic Criteria
- Criterion A. In the majority of menstrual cycles, at least five symptoms must be present in the final week before the onset of menses, start to improve within a few days after the onset of
menses, and become minimal or absent in the week postmenses. - Criterion B. One (or more) of the following symptoms must be present:
- Marked affective lability (e.g., mood swings: feeling suddenly sad or tearful, or increased sensitivity to rejection).
- Marked irritability or anger or increased interpersonal conflicts.
- Marked depressed mood, feelings of hopelessness, or self-deprecating thoughts.
- Marked anxiety, tension, and/or feelings of being keyed up or on edge.
- Criterion C. One (or more) of the following symptoms must additionally be present, to reach a total of five symptoms when combined with symptoms from Criterion B above.
- Decreased interest in usual activities (e.g., work, school, friends, hobbies).
- Subjective difficulty in concentration.
- Lethargy, easy fatigability, or marked lack of energy.
- Marked change in appetite; overeating; or specific food cravings.
- Hypersomnia or insomnia.
- A sense of being ovenwhelmed or out of control.
- Physical symptoms such as breast tenderness or swelling, joint or muscle pain, a sensation of “bloating,” or weight gain.
- Note: The symptoms in Criteria A-C must have been met for most menstrual cycles that occurred in the preceding year.
- Criterion D. The symptoms are associated with clinically significant distress or interference with work, school, usual social activities, or relationships with others (e.g., avoidance of social
activities; decreased productivity and efficiency at work, school, or home). - Criterion E. The disturbance is not merely an exacerbation of the symptoms of another disorder, such as major depressive disorder, panic disorder, persistent depressive disorder (dysthymia), or a personality disorder (although it may co-occur with any of these disorders).
- Criterion F. Criterion A should be confirmed by prospective daily ratings during at least two symptomatic cycles. (Note: The diagnosis may be made provisionally prior to this confirmation.)
- Criterion G. The symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication, other treatment) or another medical condition (e.g., hyperthyroidism).
Recording Procedures
If symptoms have not been confirmed by prospective daily ratings of at least two symptomatic cycles, “provisional” should be noted after the name of the diagnosis (i.e., “premenstrual dysphoric disorder, provisional”).
Diagnostic Features
The essential features of premenstrual dysphoric disorder (PMDD) are the expression of mood lability, irritability, dysphoria, and anxiety symptoms that occur repeatedly during the premenstrual
phase of the cycle and remit around the onset of menses or shortly thereafter. These symptoms may be accompanied by behavioral and physical symptoms. Symptoms must have occurred in most of the menstrual cycles during the past year and must have an adverse effect on work or social functioning. The intensity and/or expressivity of the accompanying symptoms may be closely related to social and cultural background characteristics of the affected female, family perspectives, and more specific factors such as religious beliefs, social tolerance, and female gender role issues.
Typically, symptoms peak around the time of the onset of menses. Although it is not uncommon for symptoms to linger into the first few days of menses, the individual must have a symptom-free period in the follicular phase after the menstrual period begins. While the core symptoms include mood and anxiety symptoms, behavioral and somatic symptoms commonly also occur. However, the presence of physical and/or behavioral symptoms in the absence of mood and/or anxious symptoms is not sufficient for a diagnosis. Symptoms are of comparable severity (but not duration) to those of another mental disorder, such as a major depressive episode or generalized anxiety disorder. In order to confirm a provisional diagnosis, daily prospective symptom ratings are required for at least two symptomatic cycles.
Associated Features Supporting Diagnosis
Delusions and hallucinations have been described in the late luteal phase of the menstrual cycle but are rare. The premenstrual phase has been considered by some to be a risk period for suicide.
[Source 19 ]Daily Record of Severity of Problems
To help diagnose premenstrual dysphoric disorder (PMDD), your family doctor may ask you to chart your symptoms (see sample chart below). The Daily Record of Severity of Problems for the diagnosis of premenstrual dysphoric disorder (PMDD) is a valid and reliable tool that can be used to diagnose PMS or PMDD 32. It is a daily log of symptoms that correlate with the diagnostic criteria for PMS and PMDD. Patients rate their symptoms through at least two menstrual cycles, which requires a significant investment of time and effort. Administering the Daily Record of Severity of Problems on the first day of menses may be an acceptable way to screen for premenstrual disorders. A cutoff value of 50 provides a positive predictive value of 63.4% and a negative predictive value of 90% 33.
Figure 3. PMS Depression Symptoms Chart
Footnotes: Patients should record the score for each item on each day using the following scale: 1 = not at all, 2 = minimal, 3 = mild, 4 = moderate, 5 = severe, 6 = extreme. If during the mid-follicular phase (days 6 through 10; day 1 is first day of your period) the patient has an average daily score greater than 3 for any symptom, an alternative diagnosis should be sought. Excused symptoms include appetite for obese patients, insomnia with good reasons, or pain from physical illness. The week before menses, the patient should score at least 4 for at least two days on five symptoms that correlate with premenstrual dysphoric disorder diagnostic criteria (DSM-5). The week before menses, the patient should score at least 4 for at least two days on at least one impairment item. The patient must meet these criteria for two consecutive cycles or two out of three cycles. Clinical judgment should correlate with the assessment of daily ratings.
[Source 34 ]PMS depression treatment
There are 3 broad approaches to treating premenstrual dysphoric disorder (PMDD). While most experts recommend a combination of all 3, there have been no scientific studies to determine if combination treatment is really the best approach. It is likely that the best approach or combination of approaches will vary from woman to woman based on things like symptom severity and which symptoms are most troublesome.
Here are the 3 approaches with some examples of each:
- Medications – including antidepressants, antianxiety drugs, analgesics, hormones and diuretics.
- Psychobehavioral – including exercise and psychotherapies (cognitive-behavioral therapy, coping skills training, relaxation).
- Nutritional – including diet modification, vitamins, minerals and herbal preparations.
Dietary and Lifestyle Changes
- Lifestyle changes. Regular exercise often reduces premenstrual symptoms. Getting enough sleep and using relaxation techniques, such as mindfulness, meditation and yoga, also may help. Avoid stressful and emotional triggers, such as arguments over financial issues or relationship problems, whenever possible.
- Dietary modifications: Increased intake of complex carbohydrates or proteins (“slow-burning fuels”) is believed to increase tryptophan availability, leading to increased serotonin levels. Cutting back caffeine, avoiding alcohol and stopping smoking may ease symptoms, too.
- Nutritional supplements. Consuming 1,200 milligrams of dietary and supplemental calcium daily may possibly reduce symptoms of PMS and premenstrual dysphoric disorder (PMDD) in some women, however the exact mechanism of action of calcium in PMS or PMDD is unknown 35. Randomized controlled trials have demonstrated the superiority of calcium in improving emotional and physical symptoms over placebo. A randomized controlled trial of 179 Tehran University students who met criteria for PMS without another psychiatric diagnosis found a 50% reduction in depression, appetite, and fatigue in women who received 500 mg of supplemental calcium carbonate twice daily for three months 36. This result was also demonstrated in a U.S. study of more than 400 women who supplemented with 1,200 mg of calcium carbonate daily 35. Vitamin B6 (pyridoxine), vitamin D, magnesium and L-tryptophan also may help. Vitamin D supplementation for treatment of PMS and PMDD symptoms was reviewed in a cross-sectional analysis of a large study 37. The cross-section analyzed was too small to make strong conclusions about the benefit of vitamin D 37. A separate study followed 401 women for 16 years and compared those who developed PMS with those who did not 38. The analysis concluded that low vitamin D levels were not associated with an increased risk of PMS 38. Further studies are needed to support the use of vitamin D as a treatment for symptoms of PMS and PMDD. Vitamin B6 (Pyridoxine) at a dosage of 80 mg per day has also been studied and recommended as treatment for primarily psychological symptoms of PMS, but these studies are small and more data is needed to recommend it as first-line treatment 39. Talk with your doctor for advice before taking any supplements.
- Herbal remedies. Some research suggests that Chaster-berry or Vitex agnus-castus (a herb also known as Chaste Tree and Monk’s Pepper) may possibly reduce irritability, mood swings, breast tenderness, swelling, cramps and food cravings associated with premenstrual dysphoric disorder (PMDD) by exerting some dopaminergic effect, but more research is needed 40, 13. The Food and Drug Administration doesn’t regulate herbal supplements, so talk with your doctor before trying one.
- Stress management: Relaxation/ meditation/ yoga/ breathing techniques.
- Cognitive Behavioral Therapy (CBT). A 2009 meta-analysis analyzed seven trials, three of which were randomized controlled trials, and showed improvement in functioning and depression scores for patients with PMS or PMDD 41. The frequency and duration of cogntive behavioral therapy (CBT) were not defined. However, the results suggest that mindfulness-based exercises and acceptance-based cognitive behavior therapy may be helpful for reducing symptoms. Further studies are needed to support the use of cognitive behavior therapy as first-line therapy.
Medications
Treatment of premenstrual dysphoric disorder is directed at preventing or minimizing symptoms and may include:
- Antidepressants.
- In the United States, selective serotonin reuptake inhibitors (SSRIs) are approved as first-line treatment for severe symptoms of PMS and PMDD. Although SSRIs are considered psychiatric medications, when used to treat premenstrual disorders they improve physical and psychiatric symptoms in most patients 42. Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac), citalopram (Celexa), escitalopram (Lexapro), paroxetine (Paxil) and sertraline (Zoloft), may reduce symptoms such as emotional symptoms, fatigue, food cravings and sleep problems 42, 43, 44. You can reduce symptoms of premenstrual dysphoric disorder by taking SSRIs all month or only in the interval between ovulation and the start of your period. SSRI treatment probably increases your risk of adverse events, with the most common being nausea, weakness or lack of energy and drowsiness or excessive sleepiness 42.
- Antidepressants that predominantly affect noradrenergic transmission are not as effective for PMDD as SSRIs, which means that the effect of SSRIs in PMDD is not just an antidepressant effect 45, 46. This is supported by the fact that the beneficial effect of SSRIs begins rapidly in PMDD, whereas antidepressant effect takes several weeks. Therefore, clinicians can use SSRIs intermittently from mid-cycle to menses to treat symptoms of PMDD as opposed to continuous treatment 47. Side effects of SSRIs are usually mild. Nausea is the most common adverse effect, but it usually wears off in a couple of days after starting the therapy and doesn’t reappear even if the therapy is intermittent. Reduced libido and difficulty in achieving orgasm (anorgasmia) are other common side effects, but they are absent in drug-free intervals.
- Other antidepressants that are linked with the relief of symptoms include a tricyclic antidepressant (TCA) called Clomipramine 48, 49 and serotonin-norepinephrine reuptake inhibitors (SNRIs) like venlafaxine (Effexor).
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) such as venlafaxine (Effexor) have been used off-label to treat PMDD in women with predominantly psychological symptoms 50. The effect is achieved over a relatively short period, three to four weeks, and sustained throughout subsequent menstrual cycles 50.
- Benzodiazepines: Benzodiazepines like alprazolam have been found to be effective only in women with severe anxiety and premenstrual insomnia. However, since there is a risk of dependence, careful monitoring is required, especially in cases with reported prior substance abuse 51, 52.
- Hormonal therapies: For very severe symptoms, your doctor can use hormonal therapies to provide relief. The aim of hormonal therapy is to inhibit the hypothalamic-gonadal cycle; however, this causes medical menopause and leads to hot flashes and an increased risk of osteoporosis. Therefore, to prevent these adverse effects, women are also started back on estrogen and gestagen (a hormone with progesterone-like activity). Some patient reports suggesting recurrence of symptoms with the add-back gestagen (a hormone with progesterone-like activity) therapy. Hence, as an alternative, clinicians can combine gonadotropin hormone-releasing hormone (GnRH) agonist with tibolone (a synthetic steroid with weak estrogenic, progestogenic, and androgenic activity). Guidelines from the International Society of Premenstrual Disorders addressed gonadotropin-releasing hormone (GnRH) agonists as potential treatment of PMS and PMDD by eliminating luteal phase symptoms 53. Although these medications have been used since the 1980s and are effective, they are not practical for long-term use because of the increased heart and blood vessels disease and osteoporosis risks associated with extended use 53. Long-term users often need hormone add-back therapy to counteract many of their hypoestrogenic effects, which may cause a return of PMS symptoms 54.
- Birth control pills or oral contraceptive pills (OCPs). Taking birth control pills with no pill-free interval or with a shortened pill-free interval may reduce PMS and premenstrual dysphoric disorder (PMDD) symptoms for some women. Although oral birth control pills are widely used in clinical practice, their efficacy in treating PMDD has not been strongly supported by evidence. Studies have suggested that oral contraceptives provide benefit when treating physical and psychiatric symptoms of PMS or PMDD. Researchers analyzed four moderate-quality trials of continuous oral contraceptive use (90 mcg levonorgestrel/20 mcg ethinyl estradiol) in women who tracked their symptoms on the Daily Record of Severity of Problems 55. Although results were somewhat inconsistent, an improvement in depressive and physical symptoms (from 30% to 59%) was identified. A higher placebo response occurred in women with PMDD, which suggests that a greater improvement occurred in women with predominantly psychiatric symptoms at baseline 55, 56. A separate PMDD trial found that continuous treatment for 112 days resulted in the most improvement in Daily Record of Severity of Problems scores 56. Women on oral birth control pills experience more hormone-related symptoms on hormone-free days, and hence oral birth control pills treatment with fewer hormone-free days might be beneficial to these women.
- Drospirenone (a man-made progesterone) was particularly found to be effective in treating PMDD symptoms because of its anti-aldosterone and anti-androgenic effects. A 2023 Cochrane review of oral contraceptives containing drospirenone evaluated five trials with 858 women 57. Combined oral contraceptives with drospirenone and ethinylestradiol 20 μg may improve premenstrual symptoms in women with premenstrual dysphoric disorder (PMDD) 57. However, a powerful placebo effect was evident: in one trial, symptoms were reduced for 48% of the combined oral contraceptives containing drospirenone group versus 36% of the placebo group. The difference may not be clinically significant. Furthermore, combined oral contraceptives containing drospirenone may lead to more adverse effects compared to placebo. The effectiveness after three cycles is unknown. Little evidence exists for treating less severe symptoms, and determining whether combined oral contraceptives containing drospirenone work any better than other combined oral contraceptives that contain a different progestogen 57.
- Danazol: This is a synthetic partial androgen agonist/antagonist and gonadotropin inhibitor that has also been shown to be efficacious in treating PMDD by inhibiting ovulation. However, it is associated with hirsutism and teratogenicity and thus not preferred as an initial agent.
PMS depression prognosis
When undergoing treatment for premenstrual dysphoric disorder, symptoms tend to improve rapidly and you’re able to enjoy your life more fully. After cessation of treatment, symptoms recur rapidly, and their reemergence is more predictable than that with other mood disorders such as major depressive disorder. Symptoms do not usually recur after removal of the ovaries. Most women don’t have symptoms after menopause.
PMS signs and symptoms
The list of potential signs and symptoms for premenstrual syndrome is long, but most women only experience a few of these three main types of PMS symptoms; physical, psychological, and emotional.
Physical PMS signs and symptoms can include:
- tender breasts
- backache
- abdominal pain or swelling
- a bloated feeling in your tummy
- weight gain related to fluid retention
- swollen ankles
- swollen breasts
- headaches
- poor coordination or clumsiness
- tiredness, lethargy, insomnia
- acne flare-ups
- constipation and/or diarrhea
- food cravings
- alcohol intolerance
Psychological and emotional premenstrual syndrome symptoms can include:
- irritability or anger
- depressed mood
- mood swings
- crying spells
- anxiety/nervous tension
- having a short temper
- lack of confidence and feeling you can’t cope
- heightened emotions (such as crying for no reason)
- feeling aggressive
- having poor concentration
- feeling more tired than usual
- lower libido
- appetite changes and food cravings
- trouble falling asleep (insomnia)
- social withdrawal
For some, the physical pain and emotional stress are severe enough to affect their daily lives. Regardless of symptom severity, the signs and symptoms generally disappear within four days of the start of the menstrual period for most women.
But a small number of women with premenstrual syndrome have disabling symptoms every month. This form of PMS is called premenstrual dysphoric disorder (PMDD).
Premenstrual dysphoric disorder (PMDD) signs and symptoms include depression, mood swings, anger, anxiety, feeling overwhelmed, difficulty concentrating, irritability and tension.
PMS causes
The exact cause of PMS is not known but it seems to have something to do with the way hormonal changes in the last part of your menstrual cycle affecting your body 58.
- Cyclic changes in hormones. Signs and symptoms of premenstrual syndrome change with hormonal fluctuations and disappear with pregnancy and menopause.
- Chemical changes in the brain. Fluctuations of serotonin, a brain chemical (neurotransmitter) that’s thought to play a crucial role in mood states, could trigger PMS symptoms. Insufficient amounts of serotonin may contribute to premenstrual depression, as well as to fatigue, food cravings and sleep problems.
- Depression. Some women with severe premenstrual syndrome have undiagnosed depression, though depression alone does not cause all of the symptoms.
PMS Diagnosis
There are no unique physical findings or lab tests to positively diagnose premenstrual syndrome. Your doctor may attribute a particular symptom to PMS if it’s part of your predictable premenstrual pattern.
Certain conditions may mimic PMS, including chronic fatigue syndrome, thyroid disorders and mood disorders, such as depression and anxiety. Your health care provider may order tests, such as a thyroid function test or mood screening tests to help provide a clear diagnosis.
Establishing the timing of symptoms is essential when evaluating for PMS and premenstrual dysphoric disorder (PMDD). Symptoms must occur during the second half of your menstrual cycle (luteal phase) and resolve shortly after the onset of menstruation. Other conditions, such as depression or anxiety, may worsen during the luteal phase, but these can be distinguished from PMS because they persist throughout the menstrual cycle. Migraines, anemia, endometriosis, and hypothyroidism may produce symptoms similar to PMS or premenstrual dysphoric disorder and should also be considered. Diagnostic laboratory testing or imaging should be directed at ruling out alternative medical diagnoses.
The American College of Obstetricians and Gynecologists 59 includes psychiatric and physical symptoms in describing premenstrual syndrome (PMS) see Table 2.
Table 2. Diagnostic Criteria for PMS (Premenstrual Syndrome)
| Premenstrual syndrome can be diagnosed if the patient reports at least one of the following affective and somatic symptoms during the five days before menses in each of the three previous menstrual cycles* | |
|---|---|
| Affective symptoms | Somatic symptoms |
Angry outbursts | Abdominal bloating |
Anxiety | Breast tenderness or swelling |
Confusion | Headache |
Depression | Joint or muscle pain |
Irritability | Swelling of extremities |
Social withdrawal | Weight gain |
*—These symptoms must be relieved within four days of the onset of menses, without recurrence until at least day 13 of the cycle, and must be present in the absence of any pharmacologic therapy, hormone ingestion, or drug or alcohol use. The symptoms must occur reproducibly during two cycles of prospective recording. The patient must exhibit identifiable dysfunction in social, academic, or work performance.
American College of Obstetricians and Gynecologists 59 has defined PMS as a condition in which a woman experiences at least one affective symptom and one somatic symptom that cause dysfunction in social, academic, or work performance. These symptoms must be cyclical, beginning after ovulation and resolving shortly after the onset of menstruation (Table 2) 59.
Prospective questionnaires are the most accurate way to diagnose PMS and premenstrual dysphoric disorder (PMDD) because patients greatly overestimate the cyclical nature of symptoms, when in fact they are erratic or simply exacerbated during their luteal phase 59. The Daily Record of Severity of Problems (see Figure 3. PMS Depression Symptoms Chart) is a valid and reliable tool that can be used to diagnose PMS or premenstrual dysphoric disorder (PMDD) 60. It is a daily log of symptoms that correlate with the diagnostic criteria for PMS and premenstrual dysphoric disorder. Patients rate their symptoms through at least two menstrual cycles, which requires a significant investment of time and effort. Administering the Daily Record of Severity of Problems (see Figure 3. PMS Depression Symptoms Chart) on the first day of menses may be an acceptable way to screen for premenstrual disorders. A cutoff value of 50 provides a positive predictive value of 63.4% and a negative predictive value of 90% 61.
Premenstrual syndrome treatment
Treatment of premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) focuses on relieving physical and psychiatric symptoms. Many of the medications used address the body’s hormonal activity through suppression of ovulation, whereas others affect the concentration of neurotransmitters such as serotonin, norepinephrine, or dopamine in the brain. The success of medications in relieving symptoms varies among women. A third group of complementary or alternative agents with varying mechanisms of action are also used. In the United States, selective serotonin reuptake inhibitors (SSRIs) are approved for primary treatment. Although SSRIs are considered psychiatric medications, when used to treat premenstrual disorders they improve physical and psychiatric symptoms in most patients 62. Physicians often tailor therapy based on patient tolerance and response to each medication.
Home remedies
Your diet and lifestyle
There are several ways to reduce your symptoms of PMS by eating and drinking the right things. You could:
- Eat little and often. Eating smaller meals throughout the day can help avoid that bloated feeling. Your stomach will feel comfortably full throughout the day. It’s better than waiting until you feel hungry and eating large meals that may fill you up too much.
- Avoid foods that are high in salt as salt retains fluid, which can make you feel bloated.
- Drink water and avoid alcohol and caffeine as these also cause bloating, mood swings, headaches and tiredness.
- Eat foods such as fruit, vegetables, and whole grains. These contain complex carbohydrates which release energy slowly so you don’t feel so tired or hungry.
- Eat plenty of vitamin-rich food, such as fresh fruit and vegetables, as these can ease symptoms and give the body an overall boost.
- Choose foods rich in calcium. If you can’t tolerate dairy products or aren’t getting adequate calcium in your diet, a daily calcium supplement may help.
- Maintain your weight at a healthy level.
- Smoking or breathing in other people’s smoke can make symptoms worse. Try to avoid being around people who are smoking. If you smoke, try to cut down or quit. In one large study, women who smoked reported more PMS symptoms and worse PMS symptoms than women who did not smoke 63.
Exercise
Exercise is a great way to improve your mood if PMS makes you feel tired, angry, depressed or emotional. Exercising raises the level of a chemical called serotonin, which makes us feel happier.
For many women, regular aerobic exercise lessens PMS symptoms. It may reduce fatigue and depression. Aerobic exercise, which includes brisk walking, running, cycling, and swimming, increases your heart rate and lung function. Exercise regularly, not just during the days that you have symptoms.
It is recommended that adults do at least half an hour (30 minutes) of exercise five times a week. It will not only improve the way you feel when you have PMS, it will also help prevent the onset of conditions such as heart disease, stroke, and diabetes.
Exercises such as pilates, yoga and other stretching techniques, can help reduce your feelings of stress and tension. They can also increase your circulation and flexibility, help ease cramps, and improve sleep patterns.
When you do any type of exercise (e.g., brisk walking, cycling, swimming or other aerobic activity), it is important that you listen to your body. If you feel any discomfort or pain you should stop immediately and rest. Never continue if you feel dizzy or faint as you could hurt yourself. Remember to drink plenty of water to replace any fluids that are lost through sweating.
Reduce stress
- Get plenty of sleep.
- Practice progressive muscle relaxation or deep-breathing exercises to help reduce headaches, anxiety or trouble sleeping (insomnia).
- Try yoga 64, meditation 65 or massage 66 to relax and relieve stress.
Vitamins and minerals
If you are considering taking vitamin and mineral supplements, you are advised to speak with your doctor or pharmacist first. The doctor or pharmacist will want to check that any condition you may have or medicine you are taking will not interact with the supplements. They may also suggest alternative supplements or techniques to ease symptoms.
Water retention treatment
Premenstrual water retention is likely caused by fluctuations in your hormones. Your diet also might play a role.
Most women who menstruate experience symptoms such as bloating one to two days before the start of their periods. Others regularly experience symptoms during the five days before their periods that interfere with some of their normal activities. This is called premenstrual syndrome (PMS).
To reduce premenstrual water retention, consider:
- Limiting salt in your diet. Eating a lot of salty food might make water retention worse.
- Magnesium. Taking magnesium supplements might help reduce water retention. Talk to your doctor before taking a supplement.
- Water pills (diuretics). These medications are available by prescription to help reduce fluid buildup. Spironolactone (Aldactone) is a diuretic that can help ease some of the symptoms of PMS.
- Be aware that taking nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others), and diuretics at the same time can cause kidney damage.
Some evidence also suggests that regular aerobic exercise and relaxation techniques, such as breathing exercises, meditation, yoga and massage, can lessen PMS symptoms.
If you continue to be troubled by monthly water retention, consult your doctor. He or she might suggest that you keep a symptom diary for a few months. This can help confirm that your symptoms are related to your menstrual cycle, rather than other causes. Your doctor can also help determine the best treatment for you.
Medications
Many women don’t need medication once they recognize their PMS and make some lifestyle changes. However, some women can find medications are helpful.
- Over-the-counter pain relievers you can buy in most stores may help lessen physical symptoms, such as cramps, headaches, backaches, and breast tenderness. These include:
- Ibuprofen
- Naproxen
- Aspirin
- Some women find that taking an over-the-counter pain reliever right before their period starts lessens the amount of pain and bleeding they have during their period.
- Calcium supplements (600mg calcium carbonate twice daily): Studies show that calcium can help reduce some PMS symptoms, such as fatigue, cravings, and depression 67, 68. Calcium is found in foods such as milk, cheese, and yogurt. Some foods, such as orange juice, cereal, and bread, have calcium added (fortified). You can also take a calcium supplement.
- Vitamin B6. Vitamin B6 may help with PMS symptoms, including moodiness, irritability, forgetfulness, bloating, and anxiety. Vitamin B6 can be found in foods such as fish, poultry, potatoes, fruit (except for citrus fruits), and fortified cereals. You can also take it as a dietary supplement.
- Magnesium. Magnesium may help relieve some PMS symptoms, including migraines 67. If you get menstrual migraines, talk to your doctor about whether you need more magnesium. Magnesium is found in green, leafy vegetables such as spinach, as well as in nuts, whole grains, and fortified cereals. You can also take a supplement.
- Polyunsaturated fatty acids (omega-3 and omega-6). Studies show that taking a supplement with 1 to 2 grams of polyunsaturated fatty acids may help reduce cramps and other PMS symptoms 69. Good sources of polyunsaturated fatty acids include flaxseed, nuts, fish, and green leafy vegetables.
- Chasteberry extract (Vitex agnus-castus): Dried ripe chasteberry is used to prepare liquid extracts or pills that some women take to relieve PMS symptoms. Some evidence that this therapy, which has been used by women for many years, is effective at reducing PMS symptoms 70.
- A few preliminary studies found that chasteberry may improve some symptoms of premenstrual syndrome but the evidence isn’t firm.
- Researchers have studied chasteberry for breast pain and infertility, but there isn’t enough reliable scientific evidence to know if it helps.
- There’s no evidence that chasteberry helps with menopausal symptoms.
- What scientists know about chasteberry extract safety?
- When used in limited amounts, chasteberry appears to be generally well tolerated. Few side effects have been reported.
- Women on birth control pills or hormone replacement therapy, or who have a hormone-sensitive condition (such as breast cancer) should not use chasteberry.
- People taking dopamine-related medications, such as certain antipsychotic drugs and Parkinson’s disease medications should avoid using chasteberry.
- What scientists know about chasteberry extract safety?
- The combined oral contraceptive pill: may help relieve symptoms for some women. This might be a good option if you need contraception as well. Because the birth control pill stops ovulation and tends to make periods lighter and less painful many women find that it improves their symptoms of PMS. Some of the newer pills can reduce fluid retention as well, so if this is a problem for you, the doctor may suggest one of these pills. Other hormonal contraceptive methods such as the contraceptive injection or implant may also work to reduce PMS in some women.
- Selective Serotonin Reuptake Inhibitors (SSRIs): used for many years to treat depression. We now know that when they are taken in low doses in the last half of the cycle, they can be very effective at treating the mood disturbance symptoms of PMS in some women. These medications can have side-effects and some women complain of sleeplessness, nausea and dizziness while using them.
In the past, high doses of Vitamin B, Evening Primrose Oil 71, and progesterone creams and tablets have all been suggested as treatments for PMS. There is very little evidence that any of these are effective.
Black cohosh. The underground stems and root of black cohosh are used fresh or dried to make tea, capsules, pills, or liquid extracts 72. Black cohosh is most often used to help treat menopausal symptoms 73, and some women use it to help relieve PMS symptoms.
If your symptoms are very severe, you should discuss this with your doctor. Some women can have very severe symptoms that may require specialist help.
Serotonergic Antidepressants
Selective Serotonin Reuptake Inhibitors (SSRIs) are first-line treatment for severe symptoms of PMS and premenstrual dysphoric disorder (PMDD). Sertraline (Zoloft), paroxetine (Paxil), fluoxetine (Prozac), citalopram (Celexa), and escitalopram (Lexapro) can be used to treat the psychiatric symptoms of PMS and premenstrual dysphoric disorder and have been shown to relieve some of the physical symptoms 62. A 2013 Cochrane review analyzed 31 randomized controlled trials that compared SSRIs with placebo for symptom relief of PMS 62. Each of the five SSRIs studied had statistically significant benefits on patient-reported symptoms when taken continuously or only during the luteal phase, but more direct studies comparing luteal phase administration with continuous administration are needed 62. Adverse effects include nausea, asthenia, fatigue, and sexual dysfunction 62. All SSRI doses seemed to be effective for psychiatric symptoms, and ultimately could be titrated to the patient’s tolerability 62. Higher doses are needed for relief of physical symptoms. Bupropion (Wellbutrin) was not effective for symptom relief of PMS or premenstrual dysphoric disorder 62.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs). SNRIs such as venlafaxine have been used off-label to treat premenstrual dysphoric disorder in women with predominantly psychological symptoms 74. The effect is achieved over a relatively short period, three to four weeks, and sustained throughout subsequent menstrual cycles 74.
Quetiapine (Seroquel). This antipsychotic has been studied as an adjunctive treatment with an SSRI or SNRI in patients with PMS or premenstrual dysphoric disorder. The goal was to improve luteal phase mood in women who did not respond to SSRI or SNRI therapy alone 75. In a small study, 20 women were started on 25 mg of quetiapine and followed for three menstrual cycles 75. Luteal phase mood lability, anxiety, and irritability were reduced in the quetiapine group 75.
Oral Contraceptives
Studies have suggested that oral birth control pills provide benefit when treating physical and psychiatric symptoms of PMS or premenstrual dysphoric disorder. Researchers analyzed four moderate-quality trials of continuous oral contraceptive use (90 mcg levonorgestrel/20 mcg ethinyl estradiol) in women who tracked their symptoms on the PMS Depression Symptoms Chart 76. Although results were somewhat inconsistent, an improvement in depressive and physical symptoms (from 30% to 59%) was identified. A higher placebo response occurred in women with premenstrual dysphoric disorder, which suggests that a greater improvement occurred in women with predominantly psychiatric, placebo-responsive symptoms at baseline 76. A separate premenstrual dysphoric disorder trial found that continuous treatment for 112 days resulted in the most improvement in PMS Depression Symptoms Chart scores 77.
A 2012 Cochrane review of oral contraceptives containing drospirenone evaluated five trials with 1,920 women 78. High drop-out rates were noted in all but one trial. Results showed that the drospirenone combination pill reduced impairments in productivity and social functioning in women with premenstrual dysphoric disorder, but there was insufficient evidence of benefit for those with PMS 78. Oral contraceptives with and without drospirenone seem to be effective at relieving abdominal bloating, mastalgia (breast pain), headache, weight gain, and swelling of extremities. Trials that extend beyond three months are needed for further analysis 78.
Other Medications
Calcium supplementation has been evaluated as treatment for PMS. Women with PMS and mood instability have been noted to have associated cyclic changes in their calcium levels; the exact mechanism of action is unknown 79. A randomized controlled trial of 179 Tehran University students who met criteria for PMS without another psychiatric diagnosis found a 50% reduction in depression, appetite, and fatigue in women who received 500 mg of supplemental calcium carbonate twice daily for three months 80. This result was also demonstrated in a U.S. study of more than 400 women who supplemented with 1,200 mg of calcium carbonate daily 79.
Vitamin D supplementation for treatment of PMS and premenstrual dysphoric disorder (PMDD) symptoms was reviewed in a cross-sectional analysis of a large study 81. The cross-section analyzed was too small to make strong conclusions about the benefit of vitamin D 81. A separate study followed 401 women for 16 years and compared those who developed PMS with those who did not 82. The analysis concluded that low vitamin D levels were not associated with an increased risk of PMS 82. Further studies are needed to support the use of vitamin D as a treatment for symptoms of PMS and premenstrual dysphoric disorder. Vitamin B6 at a dosage of 80 mg per day has also been studied and recommended as treatment for primarily psychological symptoms of PMS, but these studies are small and more data is needed to recommend it as first-line treatment 83.
Guidelines from the International Society of Premenstrual Disorders addressed gonadotropin-releasing hormone agonists as potential treatment of PMS and premenstrual dysphoric disorder (PMDD) by eliminating luteal phase symptoms 84. Although these medications have been used since the 1980s and are effective, they are not practical for long-term use because of the increased cardiovascular and osteoporosis risks associated with extended use 84. Long-term users often need hormone add-back therapy to counteract many of their hypoestrogenic effects, which may cause a return of PMS symptoms 85.
Alternative and complementary treatments
Herbal Preparations and Acupuncture
Many small, poorly conducted studies have reviewed the effectiveness of Chinese herbal supplements and acupuncture in the treatment of premenstrual symptoms 86. This evidence is too limited and study quality is too poor to suggest benefit 86. A 2010 Cochrane review of Chinese herbal supplements for PMS also did not find evidence that was strong enough to support their use 87. The studies evaluated use of saffron, St. John’s wort, ginkgo, vitex agnus-castus, peppermint, angelica root, dragon’s teeth, turmeric, tangerine leaf, and bitter orange, among others 86. Larger, more extensive trials are needed to support the use of these agents as first-line treatment.
Cognitive Behavior Therapy (CBT)
A 2009 meta-analysis analyzed seven trials, three of which were randomized controlled trials, and showed improvement in functioning and depression scores for patients with PMS or premenstrual dysphoric disorder 88. The frequency and duration of therapy were not defined. However, the results suggest that mindfulness-based exercises and acceptance-based cognitive behavior therapy may be helpful for reducing symptoms. Further studies are needed to support the use of cognitive behavior therapy as first-line therapy.
- Winer, S. A., Rapkin, A. J. (2006). Premenstrual disorders: prevalence, etiology and impact. Journal of Reproductive Medicine; 51(4 Suppl):339-347. https://www.ncbi.nlm.nih.gov/pubmed/16734317[↩]
- Pinkerton, J.V., Guico-Pabia, C.J., Taylor, H.S. (2010). Menstrual cycle-related exacerbation of disease. American Journal of Obstetrics and Gynecology; 202(3): 221-231. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3107848/[↩]
- Steiner, M. (2000). Premenstrual syndrome and premenstrual dysphoric disorder: guidelines for management. Journal of Psychiatry and Neuroscience; 25(5): 459–468. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1408015/[↩]
- Potter, J., Bouyer, J., Trussell, J., Moreau, C. (2009). Premenstrual Syndrome Prevalence and Fluctuation over Time: Results from a French Population Survey. Journal of Women’s Health; 18(1): 31–39. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3196060/[↩]
- Gollenberg, A.L., Hediger, M.L., Mumford, S.L., Whitcomb, B.W., Hovey, K.M., Wactawski-Wende, J., et al. (2010). Perceived Stress and Severity of Perimenstrual Symptoms: The BioCycle Study. Journal of Women’s Health; 19(5): 959-967. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2875955/[↩]
- Endicott, J., Amsterdam, J., Eriksson, E., Frank, E., Freeman, E., Hirschfeld, R. et al. (1999). Is premenstrual dysphoric disorder a distinct clinical entity? Journal of Women’s Health & Gender-Based Medicine; 8(5): 663-79. https://www.ncbi.nlm.nih.gov/pubmed/10839653/[↩]
- Richards, M., Rubinow, D.R., Daly, R.C., Schmidt, P.J. (2006). Premenstrual symptoms and perimenopausal depression. American Journal of Psychiatry; 163(1): 133-7. https://www.ncbi.nlm.nih.gov/pubmed/16390900/[↩]
- American College of Obstetricians and Gynecologists. (2015). Premenstrual Syndrome (PMS). https://www.acog.org/Patients/FAQs/Premenstrual-Syndrome-PMS[↩]
- Premenstrual Syndrome (PMS). https://www.acog.org/Patients/FAQs/Premenstrual-Syndrome-PMS[↩]
- Boneva, R. S., Lin, J. M., & Unger, E. R. (2015). Early menopause and other gynecologic risk indicators for chronic fatigue syndrome in women. Menopause, 22, 826–834. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5745581/[↩]
- Hofmeister S, Bodden S. Premenstrual Syndrome and Premenstrual Dysphoric Disorder. Am Fam Physician. 2016 Aug 1;94(3):236-40. https://www.aafp.org/pubs/afp/issues/2016/0801/p236.html[↩]
- Liguori F, Saraiello E, Calella P. Premenstrual Syndrome and Premenstrual Dysphoric Disorder’s Impact on Quality of Life, and the Role of Physical Activity. Medicina (Kaunas). 2023 Nov 20;59(11):2044. doi: 10.3390/medicina59112044[↩]
- Mishra S, Elliott H, Marwaha R. Premenstrual Dysphoric Disorder. [Updated 2023 Feb 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532307[↩][↩][↩]
- Reid RL. Premenstrual Dysphoric Disorder (Formerly Premenstrual Syndrome) [Updated 2017 Jan 23]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279045[↩][↩]
- Mishell DR Jr. Premenstrual disorders: epidemiology and disease burden. Am J Manag Care. 2005;11(16 suppl):S473–S479.[↩]
- Potter J, Bouyer J, Trussell J, Moreau C. Premenstrual syndrome prevalence and fluctuation over time: results from a French population-based survey. J Womens Health (Larchmt). 2009 Jan-Feb;18(1):31-9. doi: 10.1089/jwh.2008.0932[↩][↩]
- Premenstrual Dysphoric Disorder Treatment & Management. https://emedicine.medscape.com/article/293257-treatment#d7[↩]
- Prasad D., Wollenhaupt-Aguiar B., Kidd K.N., de Azevedo Cardoso T., Frey B.N. Suicidal Risk in Women with Premenstrual Syndrome and Premenstrual Dysphoric Disorder: A Systematic Review and Meta-Analysis. J. Womens Health. 2021;30:1693–1707. doi: 10.1089/jwh.2021.0185[↩]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.[↩][↩][↩]
- Hammarbäck S, Bäckström T, Holst J, von Schoultz B, Lyrenäs S. Cyclical mood changes as in the premenstrual tension syndrome during sequential estrogen-progestagen postmenopausal replacement therapy. Acta Obstet Gynecol Scand. 1985;64(5):393-7. doi: 10.3109/00016348509155154[↩][↩]
- Kumar P, Sharma A. Gonadotropin-releasing hormone analogs: Understanding advantages and limitations. J Hum Reprod Sci. 2014 Jul;7(3):170-4. doi: 10.4103/0974-1208.142476[↩][↩]
- Halbreich U. The etiology, biology, and evolving pathology of premenstrual syndromes. Psychoneuroendocrinology. 2003 Aug;28 Suppl 3:55-99. doi: 10.1016/s0306-4530(03)00097-0[↩][↩][↩][↩]
- Jahanfar S, Lye MS, Krishnarajah IS. The heritability of premenstrual syndrome. Twin Res Hum Genet. 2011 Oct;14(5):433-6. doi: 10.1375/twin.14.5.433[↩]
- Wittchen HU, Perkonigg A, Pfister H. Trauma and PTSD – an overlooked pathogenic pathway for premenstrual dysphoric disorder? Arch Womens Ment Health. 2003 Nov;6(4):293-7. doi: 10.1007/s00737-003-0028-2[↩]
- Bertone-Johnson ER, Hankinson SE, Johnson SR, Manson JE. Cigarette smoking and the development of premenstrual syndrome. Am J Epidemiol. 2008 Oct 15;168(8):938-45. doi: 10.1093/aje/kwn194[↩]
- Bertone-Johnson ER, Hankinson SE, Willett WC, Johnson SR, Manson JE. Adiposity and the development of premenstrual syndrome. J Womens Health (Larchmt). 2010 Nov;19(11):1955-62. doi: 10.1089/jwh.2010.2128[↩]
- Tenny S, Hoffman MR. Relative Risk. [Updated 2023 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430824[↩]
- Dhingra V, Magnay JL, O’Brien PM, Chapman G, Fryer AA, Ismail KM. Serotonin receptor 1A C(-1019)G polymorphism associated with premenstrual dysphoric disorder. Obstet Gynecol. 2007 Oct;110(4):788-92. doi: 10.1097/01.AOG.0000284448.73490.ac[↩]
- Huo L, Straub RE, Roca C, Schmidt PJ, Shi K, Vakkalanka R, Weinberger DR, Rubinow DR. Risk for premenstrual dysphoric disorder is associated with genetic variation in ESR1, the estrogen receptor alpha gene. Biol Psychiatry. 2007 Oct 15;62(8):925-33. doi: 10.1016/j.biopsych.2006.12.019[↩]
- Pearlstein T, Yonkers KA, Fayyad R, Gillespie JA. Pretreatment pattern of symptom expression in premenstrual dysphoric disorder. J Affect Disord. 2005 Apr;85(3):275-82. doi: 10.1016/j.jad.2004.10.004[↩][↩]
- Meaden PM, Hartlage SA, Cook-Karr J. Timing and severity of symptoms associated with the menstrual cycle in a community-based sample in the Midwestern United States. Psychiatry Res. 2005 Mar 30;134(1):27-36. doi: 10.1016/j.psychres.2005.01.003[↩]
- Endicott J, Nee J, Harrison W. Daily Record of Severity of Problems (DRSP): reliability and validity. Arch Womens Ment Health. 2006 Jan;9(1):41-9. doi: 10.1007/s00737-005-0103-y[↩]
- Borenstein JE, Dean BB, Yonkers KA, Endicott J. Using the daily record of severity of problems as a screening instrument for premenstrual syndrome. Obstet Gynecol. 2007 May;109(5):1068-75. doi: 10.1097/01.AOG.0000259920.73000.3b[↩]
- Premenstrual Syndrome and Premenstrual Dysphoric Disorder. Am Fam Physician. 2016 Aug 1;94(3):236-240. https://www.aafp.org/afp/2016/0801/p236.html[↩]
- Thys-Jacobs S, Starkey P, Bernstein D, Tian J. Calcium carbonate and the premenstrual syndrome: effects on premenstrual and menstrual symptoms. Premenstrual Syndrome Study Group. Am J Obstet Gynecol. 1998 Aug;179(2):444-52. doi: 10.1016/s0002-9378(98)70377-1[↩][↩]
- Ghanbari Z, Haghollahi F, Shariat M, Foroshani AR, Ashrafi M. Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwan J Obstet Gynecol. 2009 Jun;48(2):124-9. doi: 10.1016/S1028-4559(09)60271-0[↩]
- Bertone-Johnson ER, Chocano-Bedoya PO, Zagarins SE, Micka AE, Ronnenberg AG. Dietary vitamin D intake, 25-hydroxyvitamin D3 levels and premenstrual syndrome in a college-aged population. J Steroid Biochem Mol Biol. 2010 Jul;121(1-2):434-7. doi: 10.1016/j.jsbmb.2010.03.076[↩][↩]
- Bertone-Johnson ER, Hankinson SE, Forger NG, Powers SI, Willett WC, Johnson SR, Manson JE. Plasma 25-hydroxyvitamin D and risk of premenstrual syndrome in a prospective cohort study. BMC Womens Health. 2014 Apr 12;14:56. doi: 10.1186/1472-6874-14-56[↩][↩]
- Kashanian M, Mazinani R, Jalalmanesh S, Babayanzad Ahari S. Pyridoxine (vitamin B6) therapy for premenstrual syndrome. Int J Gynaecol Obstet. 2007 Jan;96(1):43-4. doi: 10.1016/j.ijgo.2006.09.014. Epub 2006 Dec 21. Erratum in: Int J Gynaecol Obstet. 2020 Jul;150(1):135. doi: 10.1002/ijgo.13157[↩]
- Cerqueira RO, Frey BN, Leclerc E, Brietzke E. Vitex agnus castus for premenstrual syndrome and premenstrual dysphoric disorder: a systematic review. Arch Womens Ment Health. 2017 Dec;20(6):713-719. doi: 10.1007/s00737-017-0791-0[↩]
- Lustyk MK, Gerrish WG, Shaver S, Keys SL. Cognitive-behavioral therapy for premenstrual syndrome and premenstrual dysphoric disorder: a systematic review. Arch Womens Ment Health. 2009 Apr;12(2):85-96. doi: 10.1007/s00737-009-0052-y[↩]
- Jespersen C, Lauritsen MP, Frokjaer VG, Schroll JB. Selective serotonin reuptake inhibitors for premenstrual syndrome and premenstrual dysphoric disorder. Cochrane Database Syst Rev. 2024 Aug 14;8(8):CD001396. doi: 10.1002/14651858.CD001396.pub4[↩][↩][↩]
- Wikander I, Sundblad C, Andersch B, Dagnell I, Zylberstein D, Bengtsson F, Eriksson E. Citalopram in premenstrual dysphoria: is intermittent treatment during luteal phases more effective than continuous medication throughout the menstrual cycle? J Clin Psychopharmacol. 1998 Oct;18(5):390-8. doi: 10.1097/00004714-199810000-00007[↩]
- Ravindran LN, Woods SA, Steiner M, Ravindran AV. Symptom-onset dosing with citalopram in the treatment of premenstrual dysphoric disorder (PMDD): a case series. Arch Womens Ment Health. 2007;10(3):125-7. doi: 10.1007/s00737-007-0181-0[↩]
- Freeman EW, Rickels K, Sondheimer SJ, Polansky M. Differential response to antidepressants in women with premenstrual syndrome/premenstrual dysphoric disorder: a randomized controlled trial. Arch Gen Psychiatry. 1999 Oct;56(10):932-9. doi: 10.1001/archpsyc.56.10.932[↩]
- Pearlstein TB, Stone AB, Lund SA, Scheft H, Zlotnick C, Brown WA. Comparison of fluoxetine, bupropion, and placebo in the treatment of premenstrual dysphoric disorder. J Clin Psychopharmacol. 1997 Aug;17(4):261-6. doi: 10.1097/00004714-199708000-00004[↩]
- Sundblad C, Wikander I, Andersch B, Eriksson E. A naturalistic study of paroxetine in premenstrual syndrome: efficacy and side-effects during ten cycles of treatment. Eur Neuropsychopharmacol. 1997 Aug;7(3):201-6. doi: 10.1016/s0924-977x(97)00404-5[↩]
- Sundblad C, Hedberg MA, Eriksson E. Clomipramine administered during the luteal phase reduces the symptoms of premenstrual syndrome: a placebo-controlled trial. Neuropsychopharmacology. 1993 Sep;9(2):133-45. doi: 10.1038/npp.1993.52[↩]
- Sundblad C, Modigh K, Andersch B, Eriksson E. Clomipramine effectively reduces premenstrual irritability and dysphoria: a placebo-controlled trial. Acta Psychiatr Scand. 1992 Jan;85(1):39-47. doi: 10.1111/j.1600-0447.1992.tb01440.x[↩]
- Hsiao MC, Liu CY. Effective open-label treatment of premenstrual dysphoric disorder with venlafaxine. Psychiatry Clin Neurosci. 2003 Jun;57(3):317-21. doi: 10.1046/j.1440-1819.2003.01123.x[↩][↩]
- Smith S, Rinehart JS, Ruddock VE, Schiff I. Treatment of premenstrual syndrome with alprazolam: results of a double-blind, placebo-controlled, randomized crossover clinical trial. Obstet Gynecol. 1987 Jul;70(1):37-43.[↩]
- Harrison WM, Endicott J, Nee J. Treatment of premenstrual dysphoria with alprazolam. A controlled study. Arch Gen Psychiatry. 1990 Mar;47(3):270-5. doi: 10.1001/archpsyc.1990.01810150070011[↩]
- Nevatte T, O’Brien PM, Bäckström T, et al.; Consensus Group of the International Society for Premenstrual Disorders. ISPMD consensus on the management of premenstrual disorders. Arch Womens Ment Health. 2013 Aug;16(4):279-91. doi: 10.1007/s00737-013-0346-y[↩][↩]
- Imai A, Ichigo S, Matsunami K, Takagi H. Premenstrual syndrome: management and pathophysiology. Clin Exp Obstet Gynecol. 2015;42(2):123-8.[↩]
- Freeman EW, Halbreich U, Grubb GS, Rapkin AJ, Skouby SO, Smith L, Mirkin S, Constantine GD. An overview of four studies of a continuous oral contraceptive (levonorgestrel 90 mcg/ethinyl estradiol 20 mcg) on premenstrual dysphoric disorder and premenstrual syndrome. Contraception. 2012 May;85(5):437-45. doi: 10.1016/j.contraception.2011.09.010[↩][↩]
- Halbreich U, Freeman EW, Rapkin AJ, Cohen LS, Grubb GS, Bergeron R, Smith L, Mirkin S, Constantine GD. Continuous oral levonorgestrel/ethinyl estradiol for treating premenstrual dysphoric disorder. Contraception. 2012 Jan;85(1):19-27. doi: 10.1016/j.contraception.2011.05.008[↩][↩]
- Ma S, Song SJ. Oral contraceptives containing drospirenone for premenstrual syndrome. Cochrane Database Syst Rev. 2023 Jun 23;6(6):CD006586. doi: 10.1002/14651858.CD006586.pub5[↩][↩][↩]
- Dickerson, L., Mazyck, P., Hunter, M. (2002). Premenstrual Syndrome. American Family Physician; 67(8): 1743–1752. https://www.aafp.org/afp/2003/0415/p1743.html[↩]
- American College of Obstetricians and Gynecologists. Guidelines for Women’s Health Care: A Resource Manual. 4th ed. Washington, DC: American College of Obstetricians and Gynecologists; 2014:607–613.[↩][↩][↩][↩][↩]
- Endicott J, Nee J, Harrison W. Daily Record of Severity of Problems (DRSP): reliability and validity. Arch Womens Ment Health. 2006;9(1):41–49.[↩]
- Borenstein JE, Dean BB, Yonkers KA, Endicott J. Using the daily record of severity of problems as a screening instrument for premenstrual syndrome. Obstet Gynecol. 2007;109(5):1068–1075.[↩]
- Marjoribanks J, Brown J, O’Brien PM, Wyatt K. Selective serotonin reup-take inhibitors for premenstrual syndrome. Cochrane Database Syst Rev. 2013;(6):CD001396.[↩][↩][↩][↩][↩][↩][↩]
- Dennerstein, L., Lehert, P., Heinemann, K. (2011). Global epidemiological study of variation of premenstrual symptoms with age and sociodemographic factors. Menopause International; 17(3): 96–101. https://www.ncbi.nlm.nih.gov/pubmed/21903713[↩]
- Tsai S-Y. Effect of Yoga Exercise on Premenstrual Symptoms among Female Employees in Taiwan. Mawson AR, ed. International Journal of Environmental Research and Public Health. 2016;13(7):721. doi:10.3390/ijerph13070721. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4962262/[↩]
- Arias, A. J., Steinberg, K., Banga, A., Trestman, R. L. (2006). Systematic review of the efficacy of meditation techniques as treatments for medical illness. Journal of Alternative and Complementary Medicine; 12(8):817-32. https://doi.org/10.1089/acm.2006.12.817[↩]
- Hernandez-Reif, M., Martinez, A., Field, T., Quintero, O., Hart, S., Burman, I. (2000). Premenstrual symptoms are relieved by massage therapy. J Psychosom Obstet Gynaecol; 21(1):9-15. https://www.ncbi.nlm.nih.gov/pubmed/10907210[↩]
- Canning S, Waterman M, Dye L. Dietary supplements and herbal remedies for premenstrual syndrome (PMS): a systematic research review of the evidence for their efficacy. Journal of Reproductive and Infant Psychology 2006; 24(4): 363-378[↩][↩]
- Ghanbari, Z., Haghollahi, F., Shariat, M., Foroshani, A.R., Ashrafi, M. (2009). Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwanese Journal of Obstetrics and Gynecology; 48(2): 124–129. https://www.ncbi.nlm.nih.gov/pubmed/19574172[↩]
- Rocha Filho EA, Lima JC, Pinho Neto JS, Montarroyos U. Essential fatty acids for premenstrual syndrome and their effect on prolactin and total cholesterol levels: a randomized, double blind, placebo-controlled study. Reproductive Health. 2011;8:2. doi:10.1186/1742-4755-8-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3033240/[↩]
- Girman, A., Lee, R., Kligler, B. (2003). An integrative medicine approach to premenstrual syndrome. American Journal of Obstetrics and Gynecology, 188 (5), S56–S65. https://www.ncbi.nlm.nih.gov/pubmed/12748452[↩]
- Dietz, B. M., Hajirahimkhan, A., Dunlap, T. L., Bolton, J. L. (2016). Botanicals and their bioactive phytochemicals for women’s health. Pharmacological Reviews, 68(4): 1026-1073. doi: https://doi.org/10.1124/pr.115.010843[↩]
- Johnson, T. L., Fahey, J. W. (2012). Black cohosh: coming full circle? Journal of Ethnopharmacolgy, 141(3): 775-9. doi: 10.1016/j.jep.2012.03.050. https://www.ncbi.nlm.nih.gov/pubmed/22504147[↩]
- Dietz, B. M., Hajirahimkhan, A., Dunlap, T. L., Bolton, J. L. (2016). Botanicals and their bioactive phytochemicals for women’s health. Pharmacological Reviews, 68(4): 1026-1073. doi: https://doi.org/10.1124/pr.115.010843 http://pharmrev.aspetjournals.org/content/68/4/1026.[↩]
- Hsiao MC, Liu CY. Effective open-label treatment of premenstrual dysphoric disorder with venlafaxine. Psychiatry Clin Neurosci. 2003;57(3):317–321.[↩][↩]
- Jackson C, Pearson B, Girdler S, et al. Double-blind, placebo-controlled pilot study of adjunctive quetiapine SR in the treatment of PMS/PMDD. Hum Psychopharmacol. 2015;30(6):425–434[↩][↩][↩]
- Freeman EW, Halbreich U, Grubb GS, et al. An overview of four studies of a continuous oral contraceptive (levonorgestrel 90 mcg/ethinyl estradiol 20 mcg) on premenstrual dysphoric disorder and premenstrual syndrome. Contraception. 2012;85(5):437–445.[↩][↩]
- Halbreich U, Freeman EW, Rapkin AJ, et al. Continuous oral levonorgestrel/ethinyl estradiol for treating premenstrual dysphoric disorder. Contraception. 2012;85(1):19–27.[↩]
- Lopez LM, Kaptein AA, Helmerhorst FM. Oral contraceptives containing drospirenone for premenstrual syndrome. Cochrane Database Syst Rev. 2012;(2):CD006586.[↩][↩][↩]
- Thys-Jacobs S, Starkey P, Bernstein D, Tian J; Premenstrual Syndrome Study Group. Calcium carbonate and the premenstrual syndrome: effects on premenstrual and menstrual symptoms. Am J Obstet Gynecol. 1998;179(2):444–452.[↩][↩]
- Ghanbari Z, Haghollahi F, Shariat M, Foroshani AR, Ashrafi M. Effects of calcium supplement therapy in women with premenstrual syndrome. Taiwan J Obstet Gynecol. 2009;48(2):124–129.[↩]
- Bertone-Johnson ER, Chocano-Bedoya PO, Zagarins SE, Micka AE, Ronnenberg AG. Dietary vitamin D intake, 25-hydroxyvitamin D3 levels and premenstrual syndrome in a college-aged population. J Steroid Biochem Mol Biol. 2010;121(1–2):434–437.[↩][↩]
- Bertone-Johnson ER, Hankinson SE, Forger NG, et al. Plasma 25-hydroxy-vitamin D and risk of premenstrual syndrome in a prospective cohort study. BMC Womens Health. 2014;14:56.[↩][↩]
- Kashanian M, Mazinani R, Jalalmanesh S. Pyridoxine (vitamin B6) therapy for premenstrual syndrome. Int J Gynaecol Obstet. 2007;96(1):43–44.[↩]
- Nevatte T, O’Brien PM, Bäckström T, et al.; Consensus Group of the International Society for Premenstrual Disorders. ISPMD consensus on the management of premenstrual disorders. Arch Womens Ment Health. 2013;16(4):279–291.[↩][↩]
- Imai A, Ichigo S, Matsunami K, Takagi H. Premenstrual syndrome: management and pathophysiology. Clin Exp Obstet Gynecol. 2015;42(2):123–128.[↩]
- Jang SH, Kim DI, Choi MS. Effects and treatment methods of acupuncture and herbal medicine for premenstrual syndrome/premenstrual dysphoric disorder: systematic review. BMC Complement Altern Med. 2014;14:11.[↩][↩][↩]
- Jing Z, Yang X, Ismail KM, Chen X, Wu T. Chinese herbal medicine for premenstrual syndrome. Cochrane Database Syst Rev. 2009;(1):CD006414.[↩]
- Lustyk MK, Gerrish WG, Shaver S, Keys SL. Cognitive-behavioral therapy for premenstrual syndrome and premenstrual dysphoric disorder: a systematic review. Arch Womens Ment Health. 2009;12(2):85–96.[↩]