Contents
- What is scoliosis
- Types of scoliosis
- Scoliosis symptoms
- What causes scoliosis
- Screening for scoliosis
- Diagnosis of scoliosis
- Red Flags of Scoliosis
- Risk Factors for Scoliosis Progression
- Treatment of scoliosis
- Scoliosis in adults
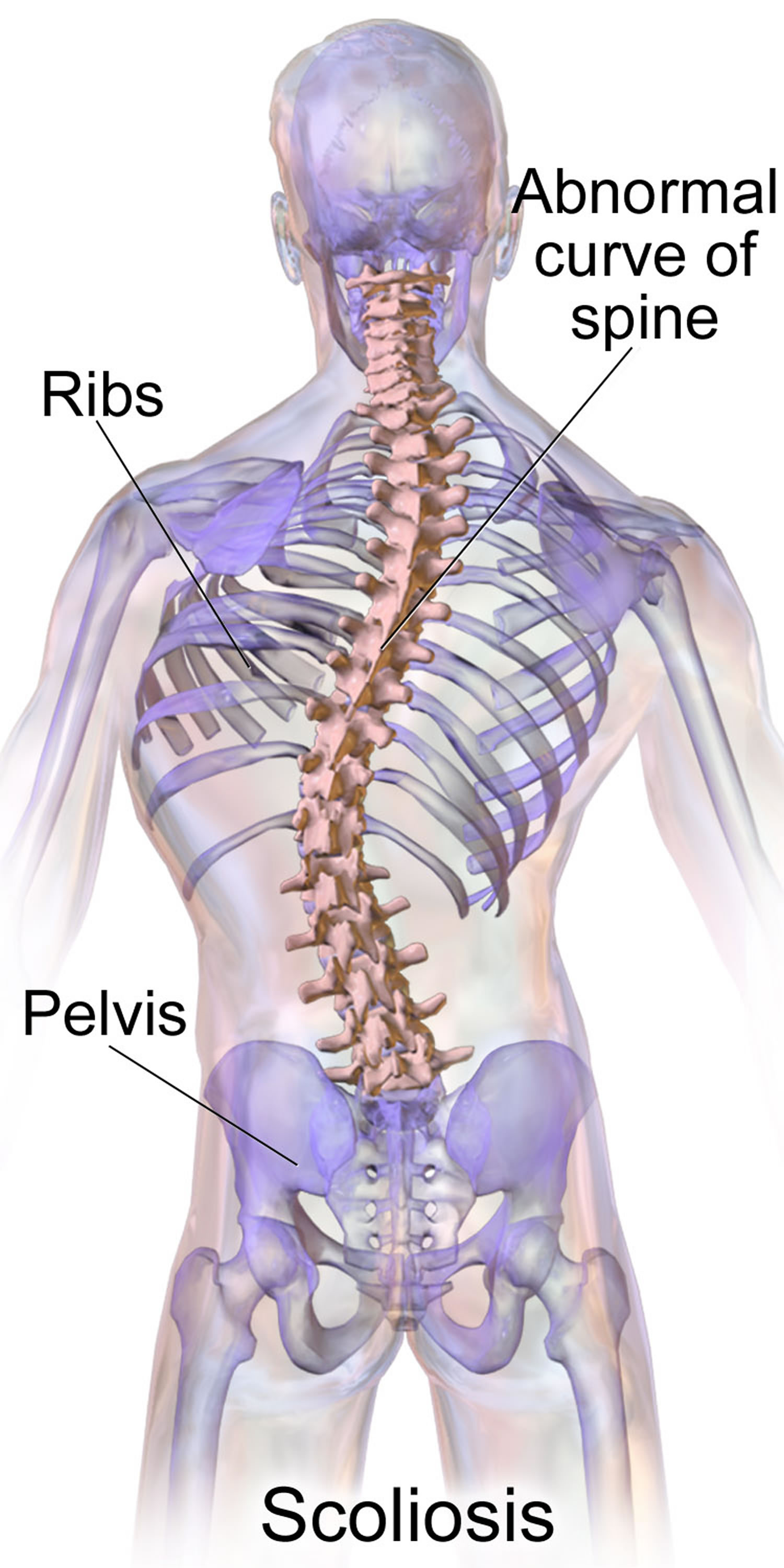
What is scoliosis
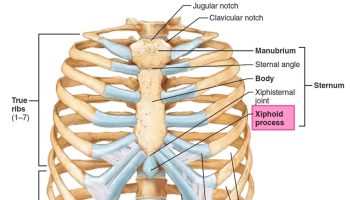
Scoliosis is a sideways curve in the spine commonly seen in children and adolescents 1. Scoliosis is defined as a lateral curve to the spine that is greater than 10 degrees with vertebral rotation 2.
There are several different types of scoliosis. By far, the most common type is “idiopathic,” which means the exact cause is not known. Idiopathic scoliosis can occur in toddlers and young children, but the majority of cases occur from age 10 to the time a child is fully grown. Children with true adolescent idiopathic scoliosis may have been born with the genetic markers that cause scoliosis. The genes that these markers are on are not known exactly, and researchers are working on finding them.
These curves are often S- or C-shaped. Scoliosis is most common in late childhood and the early teens, when children grow fast. It can run in families. Symptoms include leaning to one side and having uneven shoulders and hips. Sometimes it is easy to notice, but not always.
Adolescent idiopathic scoliosis is the most common form of scoliosis, affecting approximately 2% to 4% of (one out of every 25 children) adolescents. The incidence of scoliosis is about the same in males and females; however, females have up to a 10-fold greater risk of curve progression to more severe disease, possibly needing treatment 3. Adolescent idiopathic scoliosis is the most common form 4. Scoliosis usually does not cause problems, but sometimes leads to visible deformity, emotional distress, and respiratory impairment from rib deformity 5.
Children who have mild scoliosis are monitored closely, usually with X-rays, to see if the curve is getting worse. In many cases, no treatment is necessary. Some children will need to wear a brace to stop the curve from worsening. Others may need surgery to keep the scoliosis from worsening and to straighten severe cases of scoliosis.
Although physical therapy exercises can’t stop scoliosis (there is no evidence for or against exercises) 6, general exercise or participating in sports may have the benefit of improving overall health and well-being. Moreover, the use of exercise for the treatment of adolescent idiopathic scoliosis is controversial. Whilst it is currently routinely used in France, Germany, Italy, and a number of other countries in continental Europe, most centres in the UK and USA do not advocate its use. Until a high quality randomized clinical trial is conducted, we will not know for certain whether scoliosis-specific exercises are effective or not. In a recent International Scientific Society on Scoliosis Orthopaedic and Rehabilitation Treatment study 7 involving 24 young adolescents (5 males and 19 females, mean age 12.3 ± 1.4 years) showed there is evidence to suggest that Schroth scoliosis-specific exercises can slow progression in mild scoliosis 7. In the exercise group, spinal deformity improved in 17% of patients (Cobb angle improvement of ≥ 6°), worsened in 21% (Cobb angle increases of ≥ 6°), and remained stable in 62%. In the control group, 4% improved, 50% worsened, and 46% remained stable. In the subgroup analysis, 31% of patients who were compliant (13 cases) improved, 69% remained static, and none had worsened, while in the non-compliant group (11 cases), none had improved, 46% worsened, and 46% remained stable. Analysis of the secondary outcomes showed improvement of the truncal shift, angle of trunk rotation, the Scoliosis Research Society function domain, and total scores in favor of the exercise group 7. The Schroth method is the most widely studied and used physiotherapy scoliosis-specific exercises approach. It consists of three-dimensional principles of correction, namely auto-elongation, deflection, derotation, rotational breathing, and stabilization 8. It uses specific rotational angular breathing for vertebral and rib cage derotation, with muscle activation and mobilization. It emphasizes postural corrections throughout the day to change habitual postures and improve alignment, pain, and progression. The Schroth method exercises are curve pattern specific and can be applied in ordinary daily activity, thereby allowing the patients to spend more time in leisure activities and to live a normal life 9. See below under treatment for Schroth method scoliosis-specific exercises.
Children may get screening for scoliosis at school or during a checkup. If it looks like there is a problem, your doctor will use your medical and family history, a physical exam, and imaging tests to make a diagnosis. Treatment depends on your age, how much more you’re likely to grow, how much curving there is, and whether the curve is temporary or permanent.
When to see a doctor
Go to your doctor if you notice signs or symptoms of scoliosis in your child. Mild curves, however, can develop without the parent or child knowing it because they appear gradually and usually don’t cause pain. Occasionally, teachers, friends and sports teammates are the first to notice a child’s scoliosis.
How serious is adolescent scoliosis ?
Adolescent scoliosis is not life threatening, and most curves do not cause serious problems. Children with scoliosis can have normal active lives, including sports participation.
If the curve gets really large, it can cause heart and lung problems. A very severe curve can also compress nerves or the spinal cord, which can result in paralysis. This is extremely rare. Proper treatment will prevent the curve from progressing to such a severe degree.
Does scoliosis cause back pain ?
Adolescent scoliosis does not usually cause back pain, although larger curves may cause occasional discomfort.
If the back pain is severe or is associated with weakness of the limbs or numbness, call your doctor. This may require investigations to rule out other sources of pain.
Can scoliosis curves get better on their own ?
Some very small idiopathic scoliosis curves may improve without treatment but this is the exception rather than the rule. Many children have slight curves that do not need treatment. In these cases, the children grow up to lead normal lives — but their small curves remain.
If larger curves are not treated, the best you can hope for is that they will not get worse. This depends on how much growing your child has left to do. Curves in children who are almost fully grown may stop getting worse. If your child’s spine is still growing, it is more likely that the curves will worsen.
Will you be able to live a normal life ?
Yes. People who have curves that do not require surgery are able to participate in the same activities and sports as people without scoliosis. There are rarely restrictions on any of their activities.
The same usually applies to people who have had surgery for scoliosis. They can have the same jobs as people who have not had scoliosis surgery. They can usually do the same sports as before surgery. They should, however, contact their doctors before starting new activities (jobs or sports) to make sure they have no specific restrictions.
Figure 1. Scoliosis
Types of scoliosis
Idiopathic scoliosis
The term “idiopathic” means unknown cause. Although doctors do not know for sure what causes the majority of scoliosis cases (80% to 85%), doctors do know it tends to run in families 10. Scoliosis is not a disease that is caught from someone else, like a cold. There is nothing you could have done to prevent it.
Idiopathic scoliosis can be further classified by age of onset 11:
- Infantile (birth to two years),
- Juvenile (three to nine years), and
- Adolescent (10 years and older). Adolescent idiopathic scoliosis is the most common form. Scoliosis usually does not cause problems, but sometimes leads to visible deformity, emotional distress, and respiratory impairment from rib deformity.
Congenital scoliosis
The term “congenital” means that you are born with the condition. Congenital scoliosis starts as the spine forms before birth. Part of one vertebra (or more) does not form completely or the vertebrae do not separate properly. Some types of congenital scoliosis can change quickly with growth while others remain unchanged. This type of scoliosis can be associated with other health issues, such as heart and kidney problems.
Neuromuscular scoliosis
Any medical condition that affects the nerves and muscles can lead to scoliosis. This is most commonly due to muscle imbalance and/or weakness. Common neuromuscular conditions that can lead to scoliosis include cerebral palsy, muscular dystrophy, and spinal cord injury.
Scoliosis symptoms
People with scoliosis might have:
- shoulders that are uneven
- waist creases that are uneven
- one shoulder blade that sticks out more than the other
- one hip higher than the other
- an obvious exaggerated curve of the spine
- back pain or discomfort.
Some people with scoliosis have a posture that is unusual or uneven.
If a scoliosis curve gets worse, the spine will also rotate or twist, in addition to curving side to side. This causes the ribs on one side of the body to stick out farther than on the other side.
If you are concerned that your child may have scoliosis, see your doctor. Early diagnosis and treatment is important.
What causes scoliosis
Doctors don’t know what causes the most common type of scoliosis — although it appears to involve hereditary factors, because the disorder tends to run in families 12. If both parents have idiopathic scoliosis, their children are 50 times more likely to require scoliosis treatment compared with the general population 2. Scoliosis is believed to be a polygenic disorder with multiple inheritance patterns 12. Saliva-based genetic markers could be a useful adjunct in predicting which patients are at risk of scoliosis progression 12. However, further studies are needed, and genetic testing is not recommended at this time.
Less common types of scoliosis may be caused by:
- Neuromuscular conditions, such as cerebral palsy or muscular dystrophy
- Birth defects affecting the development of the bones of the spine
- Injuries to or infections of the spine
Sometimes it is congenital, meaning it is present at birth. It is sometimes caused by problems with the nerves and muscles, such as with cerebral palsy.
Risk factors of scoliosis
Risk factors for developing the most common type of scoliosis include:
- Age. Signs and symptoms typically begin during the growth spurt that occurs just prior to puberty.
- Sex. Although both boys and girls develop mild scoliosis at about the same rate, girls have a much higher risk of the curve worsening and requiring treatment.
- Family history. Scoliosis can run in families, but most children with scoliosis don’t have a family history of the disease.
Complications of scoliosis
While most people with scoliosis have a mild form of the disorder, scoliosis may sometimes cause complications, including:
- Lung and heart damage. In severe scoliosis, the rib cage may press against the lungs and heart, making it more difficult to breathe and harder for the heart to pump.
- Back problems. Adults who had scoliosis as children are more likely to have chronic back pain than are people in the general population.
- Appearance. As scoliosis worsens, it can cause more noticeable changes — including unlevel shoulders, prominent ribs, uneven hips, and a shift of the waist and trunk to the side. Individuals with scoliosis often become self-conscious about their appearance.
Screening for scoliosis
For decades, scoliosis screenings were a routine part of school physical examinations in adolescents 13. The screening itself carries little cost and negligible risk to the patient, but radiographs and referrals in youths who may be at low risk of disease progression can lead to significant expense and risk of harm to patients 14.
The U.S. Preventive Services Task Force 14 did not find good evidence that screening in asymptomatic adolescents detects idiopathic scoliosis at an earlier stage than no screening.
Here is the U.S. Preventive Services Task Force 14 conclusion:
“We found no direct evidence for a benefit of universal adolescent-idiopathic-scoliosis screening of adolescents on long-term health outcomes. There is evidence that demonstrates that AIS can be identified with the most commonly used screening test for adolescent-idiopathic-scoliosis (FBT with scoliometer, followed by referral for diagnostic imaging), although estimates of predictive value and sensitivity are variable, and the majority of individuals identified through screening will never require treatment. Theoretical harms of universal screening have been proposed, but high-quality evidence is lacking. A growing body of evidence suggests that brace treatment can interrupt or slow progression of scoliosis curves before skeletal maturity; and limited evidence suggests that curves of smaller magnitude may respond similarly to physiotherapeutic scoliosis-specific exercise treatment. Surgical treatment remains the standard of care for curves that progress to greater than 40–50 degrees; however, there are no controlled studies of surgical versus non-surgical treatment in individuals with lower degrees of curvature at adolescent-idiopathic-scoliosis detection, which would represent a likely screening population. Although long-term observational studies suggest that continued curve progression in adulthood is less likely if the magnitude of the curve at skeletal maturity is smaller, and that very high degrees of curvature may be associated with pathology in later adulthood, direct evidence on the association between magnitude of curve at skeletal maturity and adult quality of life outcomes is lacking.”
The accuracy of the most common screening test, the Adam’s forward bend test, with or without a scoliometer, is variable. The U.S. Preventive Services Task Force 14 found that most cases detected through screening do not progress to clinically significant scoliosis, and scoliosis requiring surgery is likely to be detected without screening.
In a prospective study in the Netherlands that followed more than 30,000 students 10 to 14 years of age for up to three years, annual scoliosis screening in addition to the usual biennial health checkup detected no cases of idiopathic scoliosis requiring surgery, and the authors concluded that additional annual scoliosis screening was not needed. Based on these findings, in 2004 the U.S. Preventive Services Task Force 14 concluded that the harms of screening asymptomatic adolescents for idiopathic scoliosis exceeded the potential benefits. The American Academy of Family Physicians concurs in recommending against routine screening 15.
The Scoliosis Research Society, American Academy of Orthopaedic Surgeons, American Academy of Pediatrics, and Pediatric Orthopaedic Society of North America convened a task force in 2007 supporting scoliosis screening, while also recognizing the need for greater care in deciding which patients with positive screening results need further evaluation 16. These groups argue that the cost of scoliosis screening is relatively low, and that the radiation exposure with current radiographic techniques is significantly less than in the past. They list prevention of deformity progression with brace treatment and earlier recognition of severe deformities requiring surgery as potential benefits of screening.
The 14 suggests that most patients who need treatment will be detected without screening, when presenting with visible curvature or possibly incidentally during another type of examination.
Diagnosis of scoliosis
The doctor will initially take a detailed medical history and may ask questions about recent growth. During the physical exam, your doctor may have your child stand and then bend forward from the waist, with arms hanging loosely, to see if one side of the rib cage is more prominent than the other.
Your doctor may also perform a neurological exam to check for:
- Muscle weakness
- Numbness
- Abnormal reflexes
Physical Examination
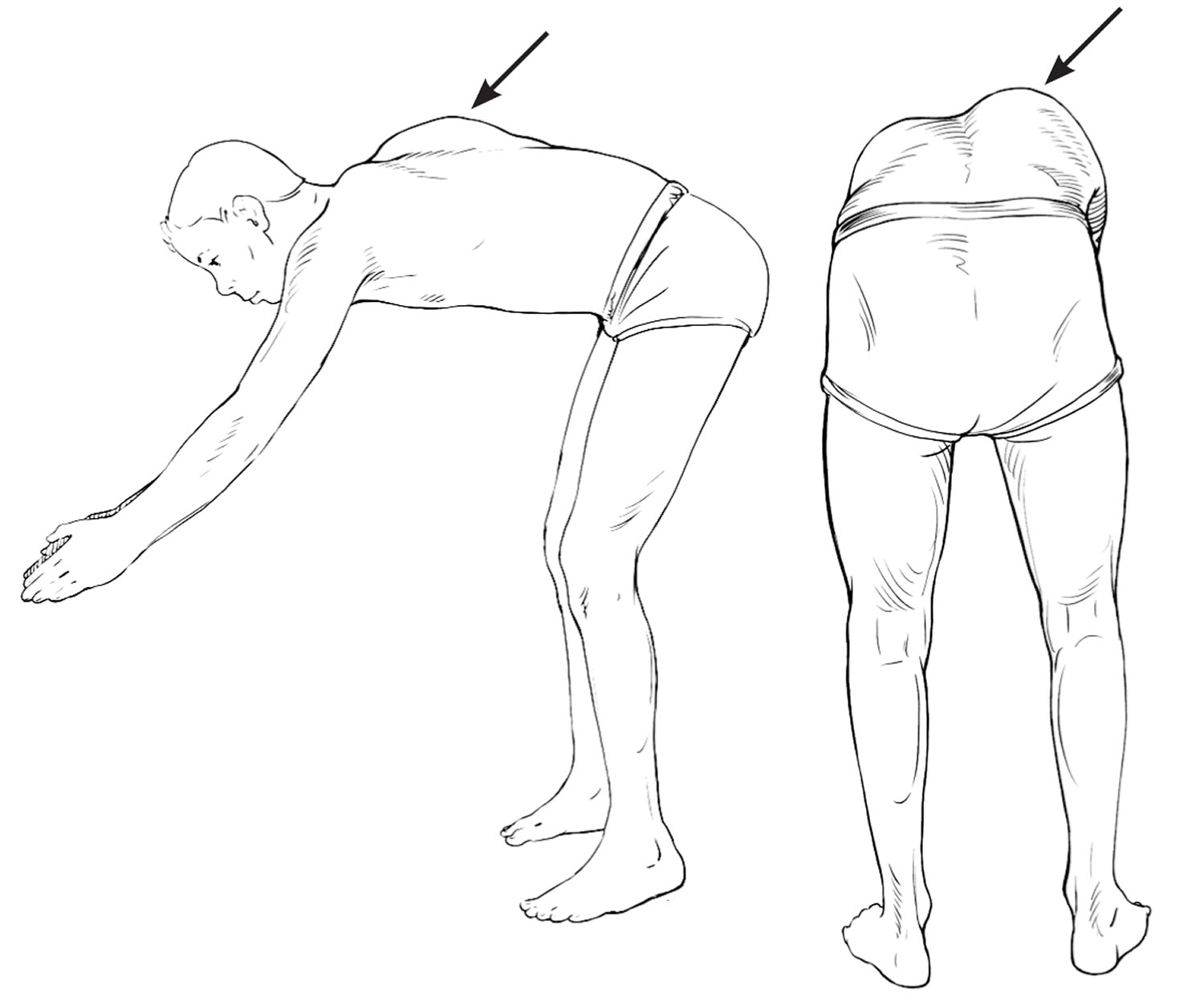
Physical examination for scoliosis mainly consists of the Adam’s forward bend test (Figure 2) 11. The patient stands and bends forward at the waist, with the examiner assessing for symmetry of the back from behind and beside the patient 17. Patients with possible scoliosis will have a lateral bending of the spine, but the curve will cause spinal rotation and eventually a rib hump, which is visible on examination 18.
Figure 2. Adam’s forward bend test for scoliosis screening
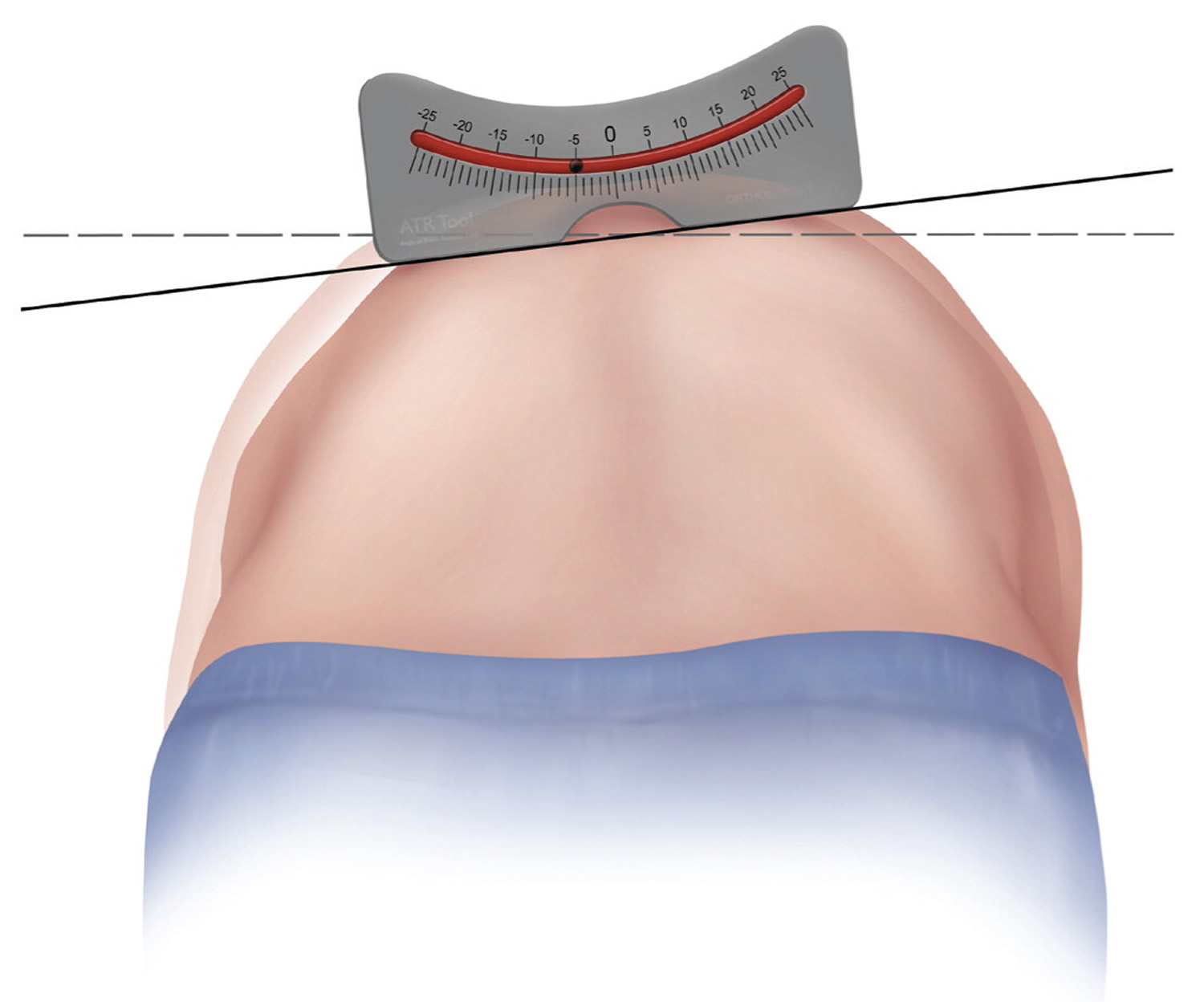
The examiner may then attempt to quantify the spinal curve and rotation with a scoliometer, or inclinometer (Figure 3) 3. The inclination angle measured by a scoliometer will help determine which patients may need radiography. The estimated magnitude of the spinal curve can be used to determine the angle of trunk rotation. This can help avoid imaging in patients with clearly insignificant curves; however, a Cobb angle measurement using radiography is needed for the official diagnosis of scoliosis. Generally, an angle of trunk rotation that is less than 5 degrees is insignificant and may not require follow-up. A measurement of 5 to 9 degrees at least warrants reexamination in six months. A measurement of 10 degrees or greater requires radiologic evaluation for Cobb angle measurement (see Figure 4).
Figure 3. Scoliometer measurement for scoliosis
Imaging tests
Plain X-rays can confirm the diagnosis of scoliosis and reveal the severity of the spinal curvature. If a doctor suspects that an underlying condition — such as a tumor — is causing the scoliosis, he or she may recommend additional imaging tests, such as an MRI.
Figure 4. Cobb angle
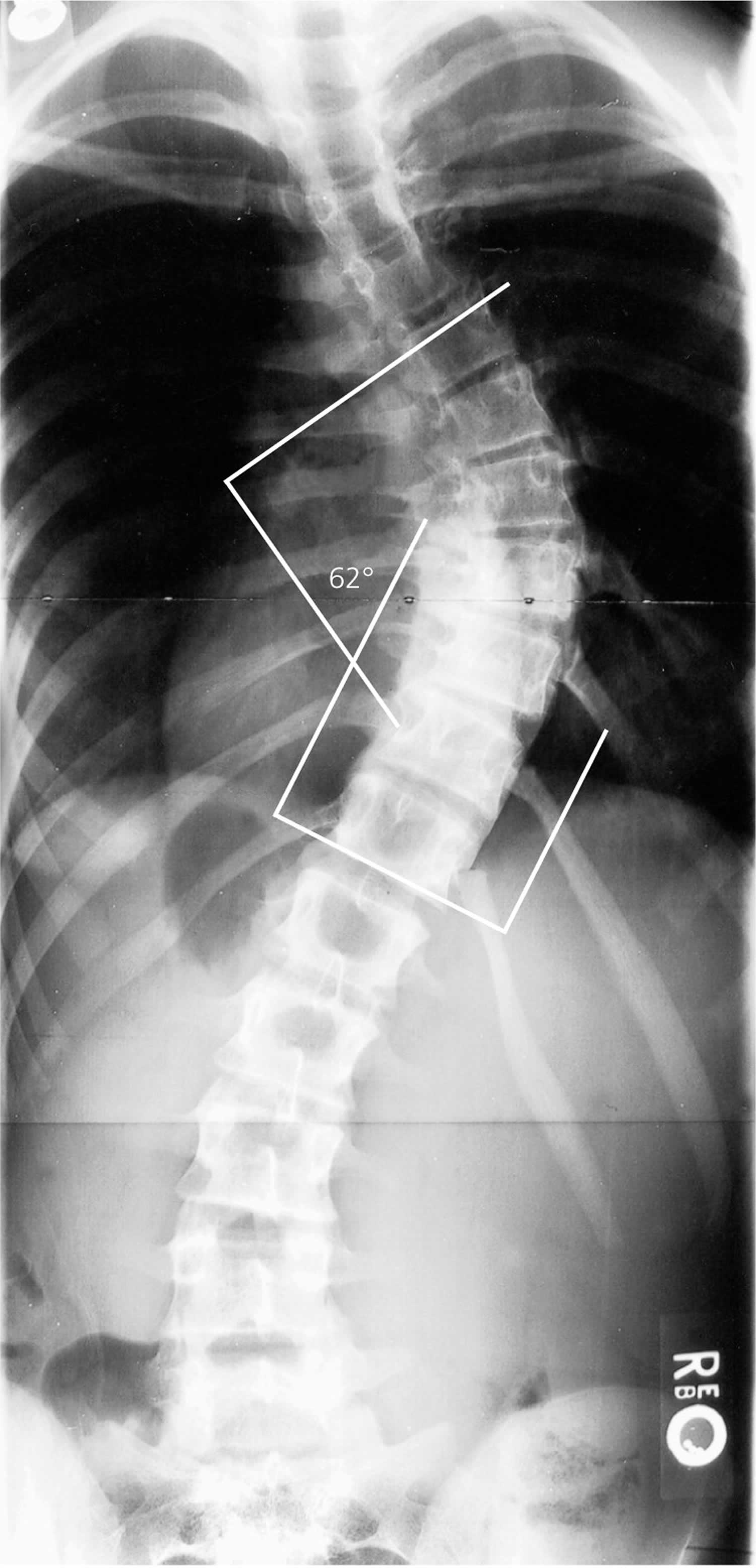
Note: Tangential lines are drawn from the superior end plate of the superior vertebra and the inferior end plate of the inferior vertebra. The angle formed at the intersection of these two lines is the Cobb angle (62 degrees in this image). A Cobb angle of at least 10 degrees is necessary for diagnosing scoliosis.
Red Flags of Scoliosis
Although scoliosis is usually benign and rarely requires treatment, there are several characteristics that suggest more serious problems and a diagnosis of nonidiopathic scoliosis. Approximately 85% to 90% of adolescent idiopathic scoliosis cases involve a right thoracic curve (the spinal curve is convex to the right) 4. A left thoracic curve (convex to the left) is more likely to be associated with additional pathology, including spinal cord tumors, neuromuscular disorders, Arnold-Chiari malformations, or occult syrinx 10.
Scoliosis rarely causes significant pain; therefore, severe pain should prompt evaluation for other possible etiologies. Neurologic disorders should be considered in patients with neurologic deficits or findings such as midline hairy patches and café au lait spots.
Risk Factors for Scoliosis Progression
Three major factors that determine whether scoliosis will progress are patient sex, magnitude of curve on presentation, and growth potential. One study followed 186 skeletally immature patients with idiopathic scoliosis, diagnosed through school screening, until skeletal maturity. The initial Cobb angle magnitude was the most important predictor of long-term curve progression and behavior past skeletal maturity, whereas initial age, sex, age of menarche, and pubertal status were less important prognostic factors. The authors suggested an initial Cobb angle of 25 degrees as an important threshold magnitude for long-term curve progression 19.
The examiner may estimate growth potential based on age and Tanner stage; however, for more precise determination of growth potential, radiographs may be needed to measure the Risser grade. The Risser grade measures bony fusion of the iliac apophysis (Figure 5), with higher Risser grades indicating greater skeletal ossification, hence less potential for growth and curve progression 20. The time of greatest curve change is in early adolescence (curve acceleration phase). Progression of scoliosis curve averages 0.2 degrees per month before the curve acceleration phase, although curves could change 1 to 2 degrees per month at the start of this phase 21.
Figure 5. Risser grade
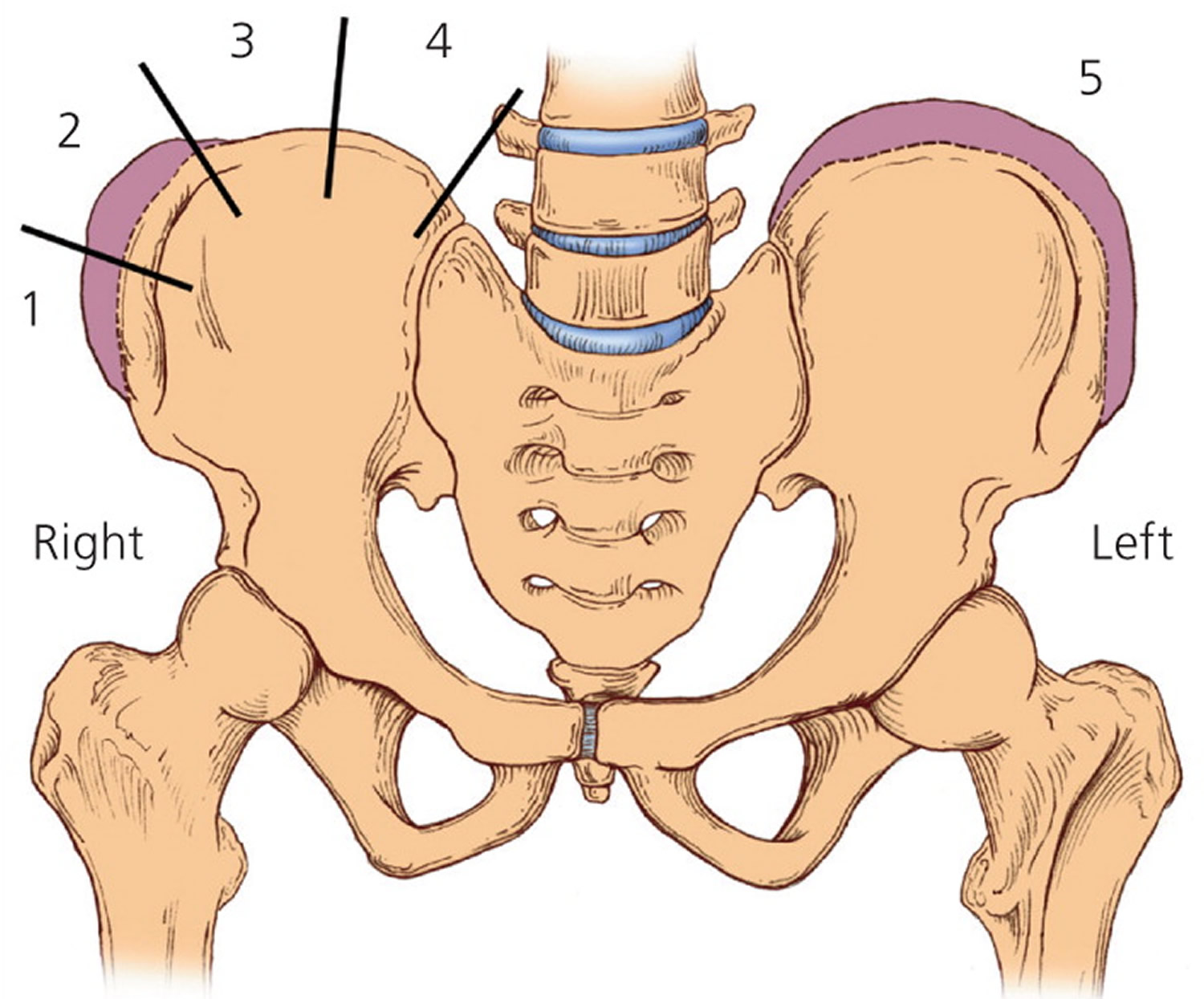
Note: The Risser grade is used to measure ossification of the iliac apophysis. Grade 1 is 25% ossification, grade 2 is 50% ossification, grade 3 is 75% ossification, grade 4 is 100% ossification, and grade 5 is fusion of ossified epiphysis to the iliac wing.
The Tanner-Whitehouse 3 assessments, which assess skeletal maturity based on radiographic evaluation of the epiphyses of the distal radius, distal ulna, and small hand bones, were simplified and used to create a skeletal scoring system to estimate scoliosis behavior 22. The researchers eliminated the radial and ulnar radiographic scores to produce a digital skeletal age score, which correlates with the curve acceleration phase. Table 1 shows predictions of scoliosis progressing to a 50-degree curve, with its potential for surgical treatment, based on digital skeletal age staging and curvature at the time of the measurement. The simplified Tanner-Whitehouse 3 skeletal maturity assessment goes up to stage 8, which corresponds to Risser grade 5. Many patients could be stage 5 on the simplified Tanner-Whitehouse 3 scale, but be a Risser grade 0. Therefore, the prediction of scoliosis activity may be stronger with the simplified Tanner-Whitehouse 3 scale than with the Risser grade 22.
The Cobb angle and Risser grade or digital skeletal age can be compared to predict the likelihood of curve progression (Tables 1 and 2). This information can help guide decisions about referral and treatment.
Table 1. Incidence of Progression as Related to the Magnitude of the Curve and the Risser Sign
| Risser sign | Percentage of curves that progressed | |
|---|---|---|
| 5- to 19-degree curves | 20- to 29-degree curves | |
Grade 0 or 1 | 22 | 68 |
2, 3, or 4 | 1.6 | 23 |
Table 2. Treatment and Referral Guidelines for Patients with Scoliosis
| Cobb angle (degrees) | Risser grade | Radiography/referral | Treatment |
|---|---|---|---|
10 to 19 | 0 to 1 | Radiography every six months, no referral | Observe |
10 to 19 | 2 to 4 | Radiography every six months, no referral | Observe |
20 to 29 | 0 to 1 | Radiography every six months, referral | Brace after 25 degrees |
20 to 29 | 2 to 4 | Radiography every six months, referral | Observe or brace* |
29 to 40 | 0 to 1 | Referral | Brace |
29 to 40 | 2 to 4 | Referral | Brace |
> 40 | 0 to 4 | Referral | Surgery† |
*—Risser grade 4 probably warrants only observation.
†—Surgery can be delayed with Risser grade 4.
Treatment of scoliosis
Treatment usually aims to straighten the spine to improve the person’s appearance. What treatment to use depends on how severe the scoliosis is and the age of the person affected.
If the condition is mild, regular check-ups are all that is needed.
If it is more severe, the treatment may involve wearing a brace, which can help prevent the curvature getting worse.
For some people, the curvature is so severe that surgery is suggested. That might involve the insertion of metal rods to straighten the spine, or surgery to fuse some of the bones together.
Exercise and physiotherapy can help ease pain.
Most children with scoliosis have mild curves and probably won’t need treatment with a brace or surgery. Children who have mild scoliosis may need checkups every four to six months to see if there have been changes in the curvature of their spines.
While there are guidelines for mild, moderate and severe curves, the decision to begin treatment is always made on an individual basis. Factors to be considered include:
- Sex. Girls have a much higher risk of progression than do boys.
- Severity of curve. Larger curves are more likely to worsen with time.
- Curve pattern. Double curves, also known as S-shaped curves, tend to worsen more often than do C-shaped curves.
- Location of curve. Curves located in the center (thoracic) section of the spine worsen more often than do curves in the upper or lower sections of the spine.
- Maturity. If a child’s bones have stopped growing, the risk of curve progression is low. That also means that braces have the most effect in children whose bones are still growing.
Scoliosis braces
If your child’s bones are still growing and he or she has moderate scoliosis, your doctor may recommend a brace. Wearing a brace won’t cure scoliosis or reverse the curve, but it usually prevents further progression of the curve.
The most common type of brace is made of plastic and is contoured to conform to the body. This close-fitting brace is almost invisible under the clothes, as it fits under the arms and around the rib cage, lower back and hips.
Most braces are worn day and night. A brace’s effectiveness increases with the number of hours a day it’s worn. Children who wear braces can usually participate in most activities and have few restrictions. If necessary, kids can take off the brace to participate in sports or other physical activities.
Braces are discontinued after the bones stop growing. This typically occurs:
- About two years after girls begin to menstruate
- When boys need to shave daily
- When there are no further changes in height
Figure 6. Scoliosis brace
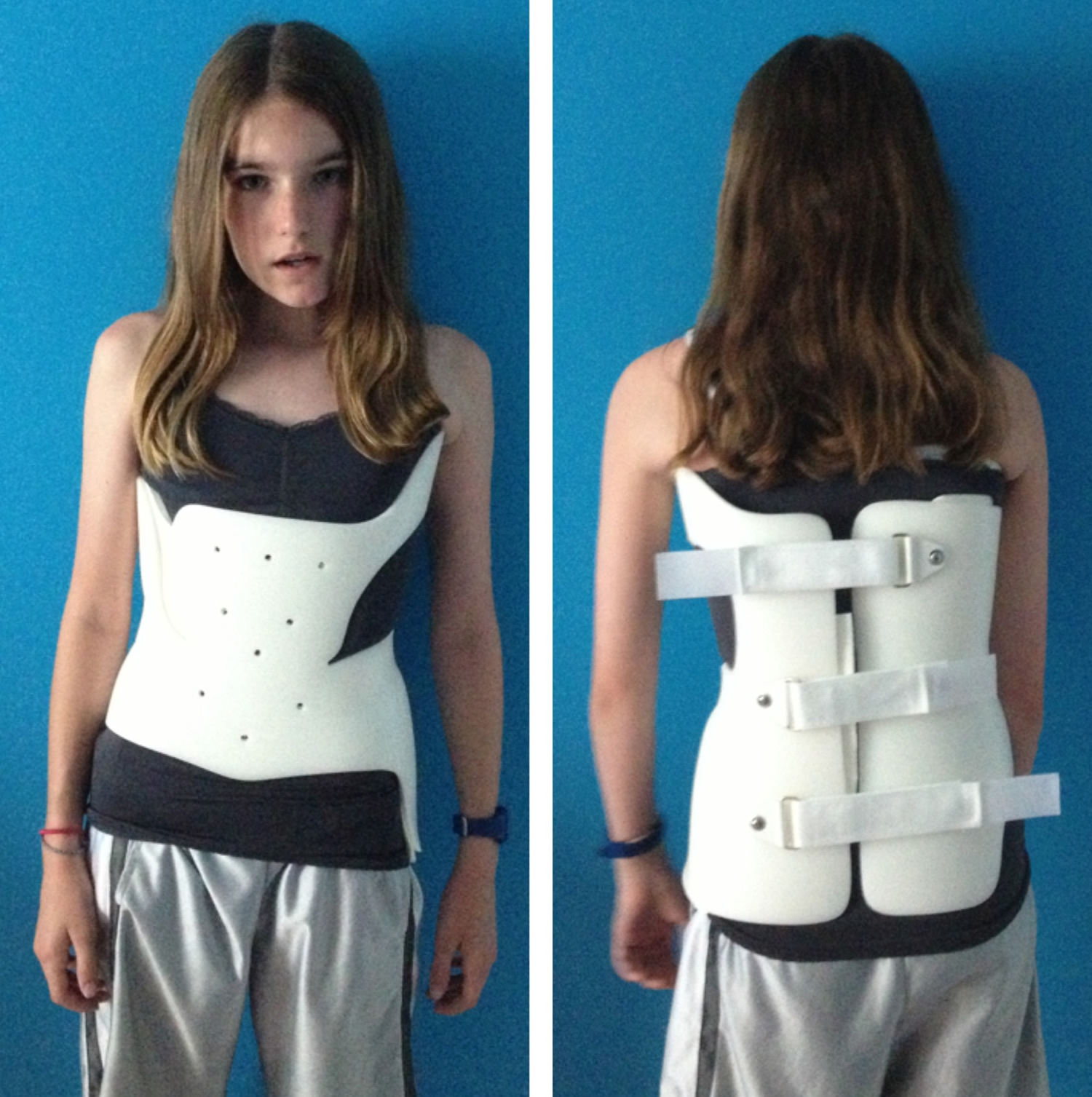
Note: This low-profile brace is made of plastic materials and is contoured to conform to the body.
Schroth method physiotherapy scoliosis-specific exercises
Based upon typical physiotherapeutic principles, the Schroth method was developed by Katharina Schroth in 1920, and continuously refined through the treatment of approximately 3,000 scoliosis cases per year. The Asklepios Katharina Schroth Spinal Deformities Rehabilitation Centre in Germany offers a scoliosis-specific intensive inpatient rehabilitation program. In addition to the treatment offered at the Centre, 2,500 trained and certified Schroth therapists treat patients through the center’s residential outpatient treatment program.
The Schroth Classification system
The Schroth system of classification 25 is derived from the Schroth principle of dividing the body into ‘Body Blocks’. This symbolic description helps to explain the scoliotic alterations as compensatory adaptations. The Body Blocks depict the trunk deformation as a change in their geometric form from a rectangle to a trapezium shape. Side-shift and rotation as well as compression on the concave side and expansion on the convex side are clearly visible. In the standing static position the body blocks should be aligned perpendicularly with their center of gravity integrated in the central sacral line as seen in Figure 7. The scoliotic trunk asymmetry is a loss of symmetry and shows the blocks skewed and off-center (Figure 7).
Figure 7. Schroth Body Blocks
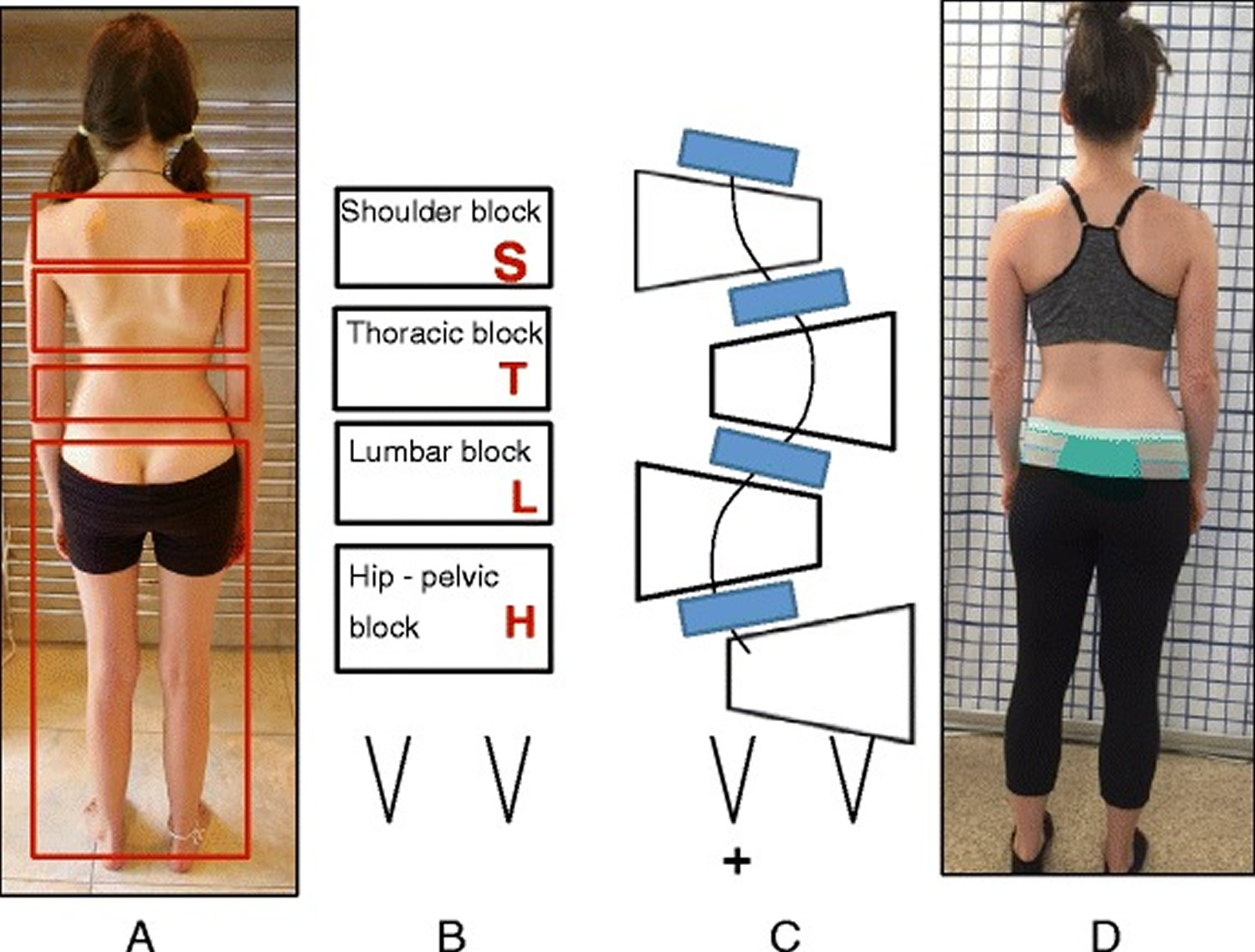
Note: (a, b, c, d): Schroth Body Blocks. The Schroth system of scoliosis curve classification is derived from the Schroth principle of dividing the body into “body blocks” as pictured anatomically (a) and schematically (b). Scoliosis causes the body blocks to become deformed, changing their geometric shape from a rectangle (b) to a trapezium (c). A patient with a major lumbar scoliosis left convex curve has a lumbar block shifted to the left and a hip-pelvic block shifted to the right (d)
The Schroth classification system gives the direction of the side deviation and rotation of the main important body blocks (major curves) and a clear orientation for the standardized therapy plan which includes the therapy diagram, exercise-program with home-exercises, and necessary mobilizing technique.
According to the Schroth classification system, the different scoliosis types always start with the major curve and are followed by relevant secondary curves.
The uppercase letters represent the body blocks and the lowercase letters describe the direction of the lateral deviation and rotation: right = ri, left = le.
Schroth body blocks:
H – Hip-pelvic block including the lower limbs reaching the lower end vertebra (LEV) of the lumbar curve.
L – Lumbar block enclosed by upper end vertebra (UEV) and LEV of the lumbar curve or thoracolumbar curve respectively.
T – Thoracic block between UEV and LEV of the thoracic curve.
S – Shoulder block represents the cervical thoracic (proximal thoracic) curve located between UEV of the thoracic curve and UEV of the proximal thoracic curve.
The following is an overview of the classifications:
Thoracic scoliosis (means that the major curve is located in the thoracic spine, and the curve can be to the right or to the left).
- Thoracic only.
- Thoracic with lumbar to opposite side with hips in center.
- Thoracic with lumbar and hips protruding to the opposite side of the thoracic curve (along with the lumbar).
Lumbar scoliosis (means that the major curve is located in the lumbar spine, and the curve can be to the right or to the left).
- Lumbar only with hips protruding to the opposite side of the curve.
- Lumbar curve with thoracic and hips protruding to the opposite side of the lumbar curve.
- Lumbar and thoracic curves with hips in center.
- Sagittal plane deformities including increased thoracic kyphosis (round back), decreased thoracic kyphosis (flat back) and increased lumbar kyphosis or loss of the normal anatomical lordosis (curve) of the lumbar spine.
Age specifics
The Schroth method is primarily used for idiopathic scoliosis, including Adolescent Idiopathic Scoliosis and late juvenile idiopathic scoliosis. People with early onset scoliosis and adults, are treated with modified principles. Sagittal plane deformities such as hyper-kyphosis (Scheuermann’s kyphosis) and lordosis (inverted back) can also be treated with Schroth exercises. Treatment of juvenile idiopathic scoliosis involves a less intense and modified Schroth method as well. Treatment of Adolescent Idiopathic Scoliosis using strict Schroth principles is aimed at preventing curve progression before the end of growth. Treatment of adult onset scoliosis implements a modified Schroth method based on the severity of pain and the degree and rigidity of the spinal deformity.
3D principles of correction
In the Schroth method there are five pelvic corrections that are assumed prior to the execution of the main principles of correction. These five pelvic corrections ensure that the pelvis is best aligned with the trunk prior to the major corrections.
The five principles of the Schroth method are: 1) Auto-elongation (detorsion); 2) Deflection; 3) Derotation; 4) Rotational breathing; and 5) Stabilization. During the application of these principals, the patient is taught how to de-collapse the concaved areas of the trunk and how to reduce the prominences.
Description of Schroth method exercises
Four of the most commonly used exercises in the Schroth method are the “50 x Pezziball” exercise, Prone exercise, Sail exercise, and the Muscle-cylinder exercise. All of these exercises can be used for all curve types. The “50 x Pezziball” exercise works on auto-self-elongation and activation of muscles in the trunk that force the convexities in the trunk “forward and inward” and the concavities “outward and backward” (Figure 9).
Figure 8. Schroth method lumbar mobilization (a) and curve flexibility (b) exercises
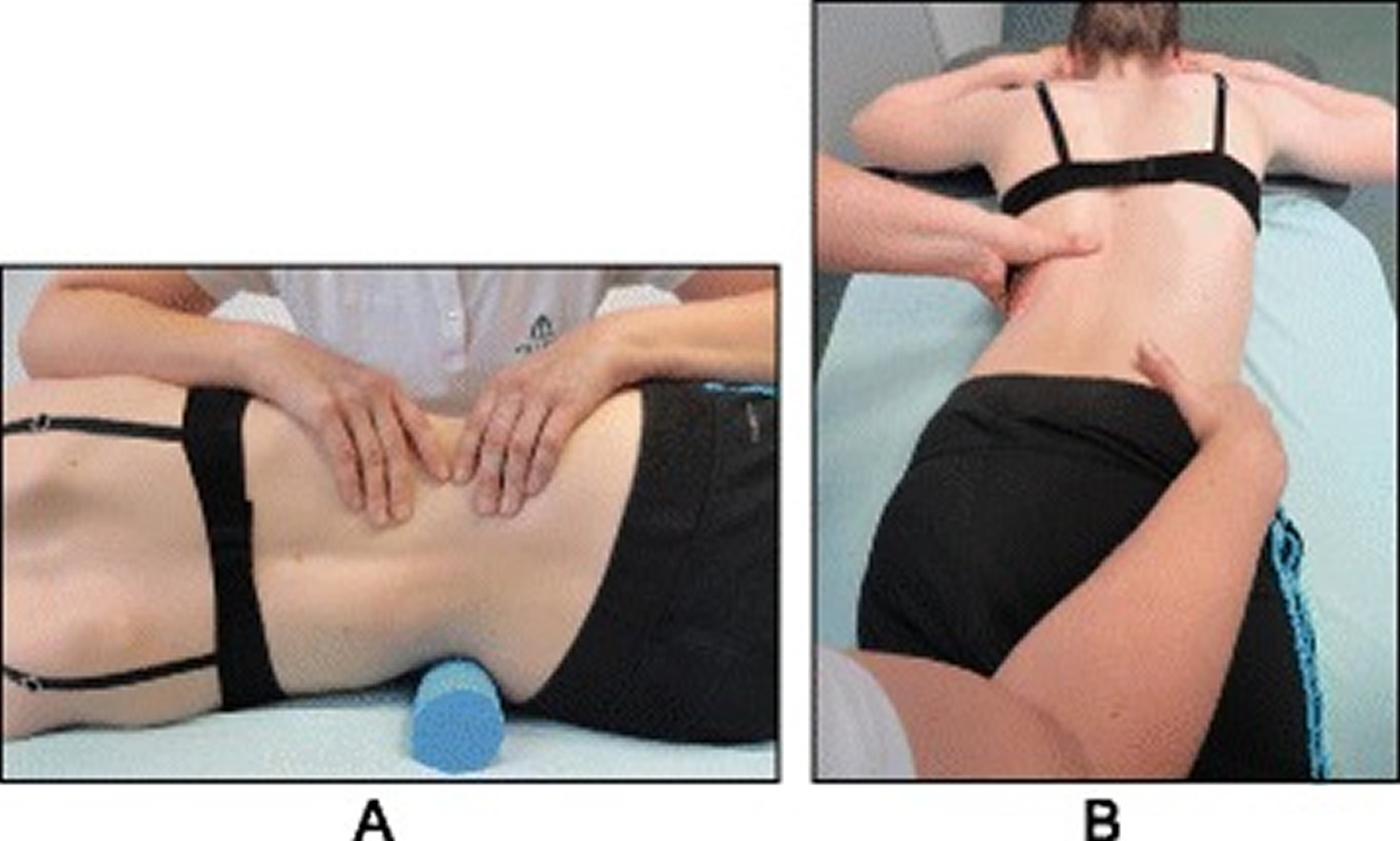
Figure 9. Schroth 50 x Pezziball exercise
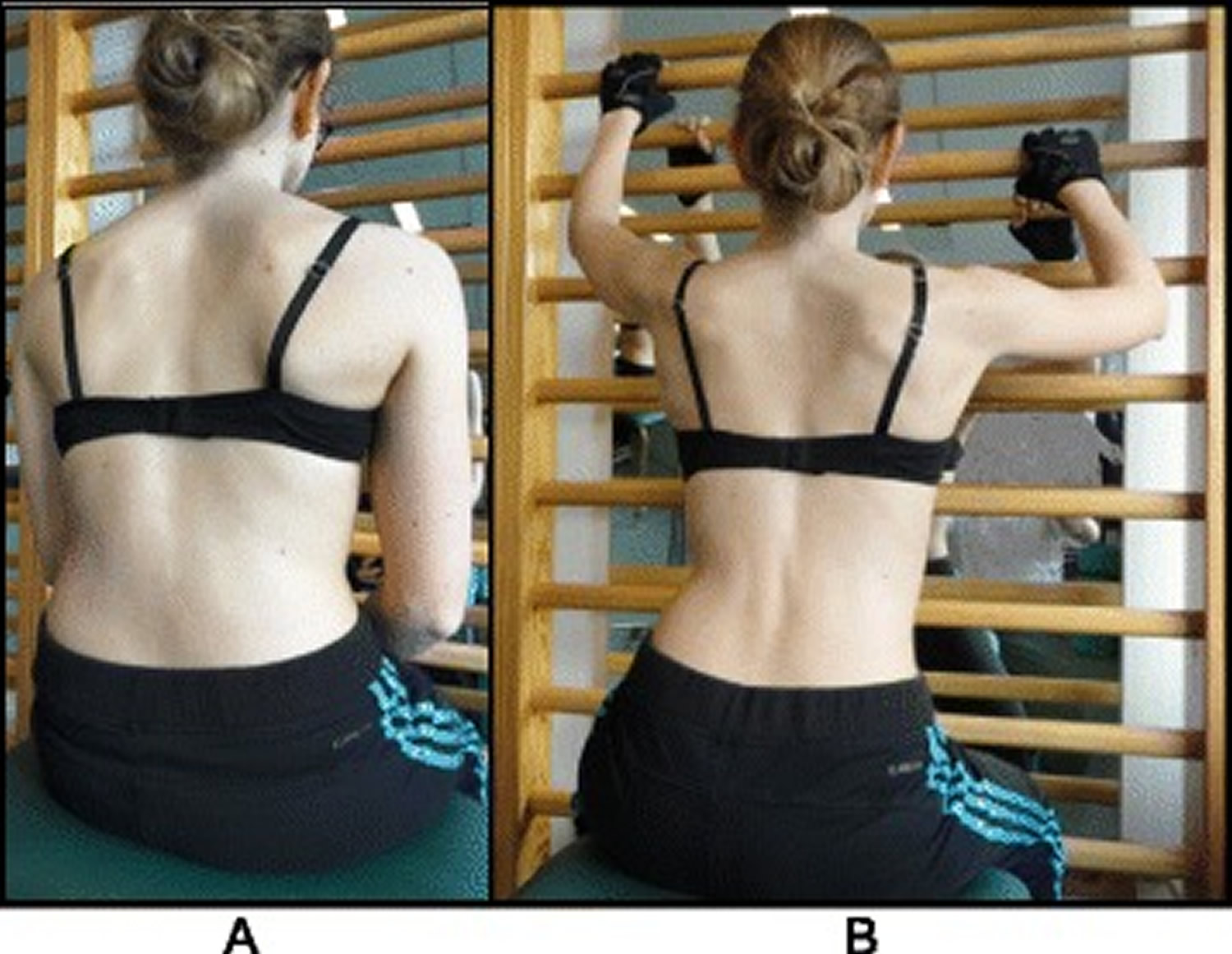
Note: The Schroth “50 x Pezziball” exercise where the patient sits on a Swiss-ball in front of a mirror (a) and performs active 3D auto self-correction using the wall bar (b)
The Prone exercise corrects the thoracic curve using shoulder traction and shoulder counter-traction and the lumbar curve via activation of the iliopsoas muscle (Figure 10). The Sail exercise is a very effective stretching exercise, which helps elongate the thoracic concavity (Figure 11). The Muscle-cylinder engages the quadratus lumborum muscle to correct the lumbar curve against gravity (Figure 12). Other exercises related to the Schroth method involve postural correction during activities of daily living. These exercises focus on correcting posture while resting, sitting, or standing.
Figure 10. Schroth prone exercise

Note: The Schroth prone exercise with activation of the iliopsoas muscle (right hip flexion). Blue arrows represent trunk elongation with caudal and cranial forces. Red arrows represent areas of muscle activation around the convexities towards the midline. Green half-moons represent areas of expansion of the concavities. Red circles represent additional corrective forces: red circles around the right lower extremity and the right upper extremity represent iliopsoas activation and shoulder traction/counter-traction, respectively, resulting in correction of the lumbar and thoracic curves
Figure 11. Schroth Sail exercise

Note: The Schroth “Sail” exercise where the patient stands on a half foam-roll with two poles and performs active stabilization. The red circle represents the concavity (weak side according to Schroth). During active stabilization, the patient is consciously expanding the left rib cage with right directional breathing, opening the collapsed left lung, while maintaining 3D postural correction
Figure 12. Schroth Side-lying exercise
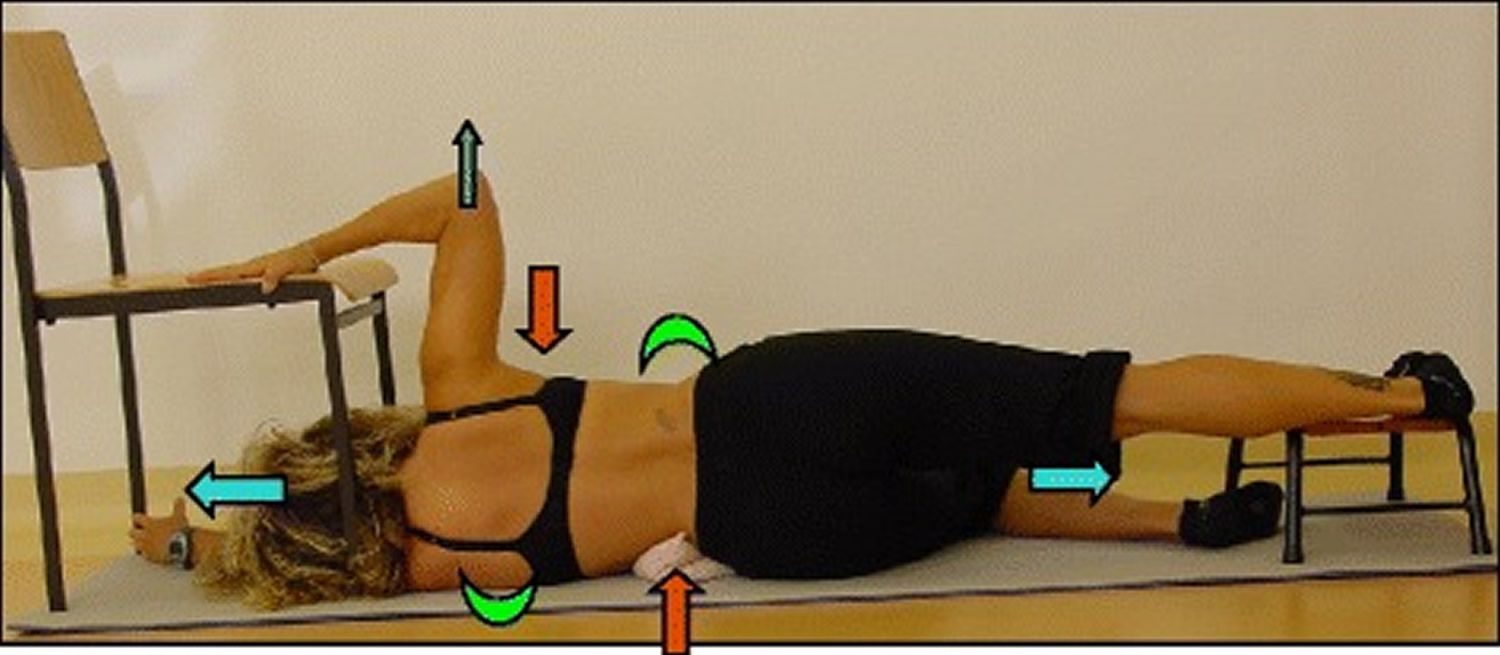
Note: The “Muscle-cylinder” exercise (also known as the “Side-lying” exercise), focusing mainly on the correction of the lumbar scoliosis curve. During this exercise, the patient lies on the lumbar convex side. The lumbar convexity is supported by a rice bag to help align the spine in the horizontal plane. The patient’s right leg is supported by a stool (in case of 4C/major lumbar scoliosis) and the patient’s right arm is supported on a chair during the exercise. Light blue arrows represent trunk elongation with cranial and caudal forces. Green half-moons represent areas of expansion of the concavities. Red arrows represent areas of muscle activation, approximating the convexities towards midline, and the direction of the correction. The dark blue arrow pointing upwards from the right elbow represents the shoulder traction, which is an isometric tension from the shoulder in a lateral/outward direction with a fixed scapula as a continuation of the transversal expansion in the proximal thoracic region
Activities of daily living
The Schroth method emphasizes teaching postural corrections throughout the day in order to change habitual default postures and improve alignment, pain and progression (Figure 13). The main advantage of this program lies in its application to ordinary daily activity for the purpose of changing the asymmetrical loading on the body in order to decrease progression and pain. This also reduces the amount of time needed to practice the highly demanding exercises and allows patients to spend more time in leisure activities and to live a normal life.
Figure 13. Schroth 3D postural corrections

Note: Patients performing Schroth 3D postural corrections in sitting and standing positions. These postural corrections are practiced during activities of daily living in order to change habitual default postures and improve alignment, pain, and curve progression.
What can you do to prevent my scoliosis from getting worse ?
The only treatments that have been shown to effect idiopathic scoliosis are bracing and surgery. There is no evidence in the current medical literature that physical therapy, electrical stimulation, chiropractic care, or other options have any long term impact on scoliosis curves. Scoliosis Specific Exercises (SSE) may be useful together with bracing and are currently being studied.
Is it safe for you to exercise and participate in sports ?
Children with idiopathic scoliosis can participate in any sport up to their own level of tolerance. It is always a good idea for children to stay physically fit with exercise.
Surgery for scoliosis
Severe scoliosis typically progresses with time, so your doctor might suggest scoliosis surgery to reduce the severity of the spinal curve and to prevent it from getting worse. The most common type of scoliosis surgery is called spinal fusion.
In spinal fusion, surgeons connect two or more of the bones in the spine (vertebrae) together, so they can’t move independently. Pieces of bone or a bone-like material are placed between the vertebrae. Metal rods, hooks, screws or wires typically hold that part of the spine straight and still while the old and new bone material fuses together.
If the scoliosis is progressing rapidly at a young age, surgeons can install a rod that can adjust in length as the child grows. This growing rod is attached to the top and bottom sections of the spinal curvature, and is usually lengthened every six months.
Complications of spinal surgery may include bleeding, infection, pain or nerve damage. Rarely, the bone fails to heal and another surgery may be needed.
Alternative medicine
Studies indicate that the following treatments for scoliosis are ineffective:
- Chiropractic manipulation
- Electrical stimulation of muscles
- Dietary supplements
Scoliosis in adults
Everyone’s spine has subtle natural curves. But some people have different curves, side-to-side spinal curves that also twist the spine. This condition is called “scoliosis”. On an x-ray with a front or rear view of the body, the spine of a person with scoliosis looks more like an “S” or a “C” than a straight line. These curves can make a person’s shoulders or waist appear uneven. These curves can’t be corrected simply by learning to stand up straight. You can’t cause scoliosis; it does not come from carrying heavy backpacks, participating vigorously in sports, or poor posture.
Types of Adult Scoliosis
In addition to the two types of adult scoliosis discussed in this section—Adult Idiopathic Scoliosis and Adult Degenerative Scoliosis—types of scoliosis that develops early in life or that results from a separate syndrome also effect adults.
Adult Idiopathic Scoliosis
Adult idiopathic scoliosis is, in essence, a continuation of adolescent idiopathic scoliosis 26. Sometimes a spine curvature of an idiopathic (cause not known) nature that began during teenage years may progress during adult life. Curves may increase in size 0.5° to 2° per year. Adolescent curves less than 30° are unlikely to progress significantly into adulthood, while those over 50° are likely to get bigger, which is why adult scoliosis specialists should monitor the curves over time.
Locations of adult scoliosis
Occurs in the thoracic (upper) and lumbar (lower) spine, with the same basic appearance as that in teenagers, such as shoulder asymmetry, a rib hump, or a prominence of the lower back on the side of the curvature. Curves can worsen in the older patient due to disc degeneration and/or sagittal imbalance. Additionally, arthritis commonly affects joints of the spine and leads to the formation of bone spurs.
Symptoms of adult scoliosis
Adults with idiopathic scoliosis have more symptoms than teens because of degeneration in discs and joints leading to narrowing of the openings for the spinal sac and nerves (spinal stenosis). Some patients may lean forward to try and open up space for their nerves. Others may lean forward because of loss of their natural curve (lordosis, sway back) in their lumbar spine (low back). The imbalance causes the patients to compensate by bending their hips and knees to try and maintain an upright posture. Adult patients may have a variety of symptoms, which can lead to gradual loss of function:
- Low back pain and stiffness are the 2 most common symptoms
- Numbness, cramping, and shooting pain in the legs due to pinched nerves
- Fatigue results from strain on the muscles of the lower back and legs
Imaging Evaluation of adult scoliosis
Scoliosis defined with radiographs that can include the following:
- Standing x-ray of the entire spine looking both from the back as well as from the side so your physician can measure the radiographs to determine curve magnitude, measured in degrees using the Cobb method.
- Magnetic resonance imaging (MRI) study of the spine is rarely used for patients experiencing minimal symptoms with adult idiopathic scoliosis. An MRI is usually ordered if you have leg pain, your physician finds some subtle neurologic abnormalities on physical examination, or if you have significant pain or an “atypical” curve pattern.
Treatment Options of adult scoliosis
Nonoperative treatment
The majority of adults with idiopathic scoliosis do not have disabling symptoms and can be managed with simple measures including the following:
- Periodic observation
- Over-the-counter pain relievers
- Exercises aimed at strengthening the core muscles of the abdomen and back and improving flexibility
- Braces, in short-term use for pain relief (long-term use in adults is discouraged because braces can weaken the core muscles)
- Epidurals or nerve block injections for temporary relief if the patient has persistent leg pain and other symptoms due to arthritis and pinched nerves.
- Patients should track their response to the various injections to help define their pain generators.
Stronger pain medications can also be habit-forming and must be used with caution. If narcotics are needed to control the pain, see a scoliosis surgeon to learn more about the possible causes of pain.
Operative treatment
Surgical treatment is reserved for patients who have:
- Failed all reasonable conservative (non-operative) measures.
- Disabling back and/or leg pain and spinal imbalance.
- Severely restricted functional activities and substantially reduced overall quality of life.
The goals of surgery are to restore spinal balance and reduce pain and discomfort by relieving nerve pressure (decompression) and maintaining corrected alignment by fusing and stabilizing the spinal segments. When patients are carefully chosen and mentally well-prepared for surgery, excellent functional outcomes can be achieved which can provide positive life-changing experience for a given individual patient. When larger surgeries—those greater than 8 hours—are necessary, surgery may be divided into 2 surgeries 5 to 7 days apart.
Surgical procedures include:
- Microdecompression relieves pressure on the nerves; A small incision is made and magnification loupes or a microscopic assists the surgeon in guiding tools to the operation site. This type of procedure is typically used only at one vertebra level, and carries a risk of causing the curve to worsen, especially in larger curves >30 degrees.
- Surgical stabilization involves anchoring hooks, wires or screws to the spinal segments and using metal rods to link the anchors together. They stabilize the spine and allow the spine to fuse in the corrected position.
- Fusion uses the patient’s own bone or using cadaver or synthetic bone substitutes to “fix” the spine into a straighter position
- Osteotomy is a procedure in which spinal segments are cut and realigned
- Vertebral column resection removes entire vertebral sections prior to realigning the spine and is used when an osteotomy and other operative measures cannot correct the scoliosis.
Adult Degenerative Scoliosis
Also known as de novo (new) scoliosis. This type of scoliosis begins in the adult patient due to degeneration of the discs, arthritis of the facet joints and collapse and wedging of the disc spaces 26.
Locations of Adult Degenerative Scoliosis
It is typically seen in the lumbar spine (lower back), and usually accompanied by straightening of the spine from the side view (loss of lumbar lordosis).
Symptoms of Adult Degenerative Scoliosis
Disc degeneration and spinal stenosis associated with adult degenerative scoliosis can cause the following symptoms:
- Back pain
- Numbness
- Shooting pain down the legs
Imaging Evaluation of Adult Degenerative Scoliosis
X-rays, front and standing, must include all segments of the spine as well as the pelvis and hips to measure alignment, curvatures, and balance. For the side x-rays, hips and knees must be straight. Focused x-rays of the cervical, thoracic, and lumbar spine may also be necessary.
Magnetic resonance imaging (MRI) or computerized tomography (CT), advanced imaging techniques to assess patients with lower extremity symptoms or other neurologic signs or symptoms.
Treatment Options for Adult Degenerative Scoliosis
Nonoperative treatment is appropriate for the majority of adults with degenerative scoliosis who don’t have disabling symptoms. Treatments include:
- Periodic observation
- Over-the-counter pain relievers
- Exercises aimed at strengthening the core muscles of the abdomen and back and improving flexibility
- Braces with short-term use of for pain relief (long-term use in adolescents is discouraged because braces can weaken the core muscles)
- Epidurals or nerve block injections for temporary relief of leg pain and other symptoms
Stronger pain medications can also be habit-forming and must be used with caution. If narcotics are needed to control the pain, see a scoliosis surgeon to learn more about the pain generators.
Operative treatment of Adult Degenerative Scoliosis
Surgical treatment is reserved for patients who have:
- Failed all reasonable conservative (non-operative) measures.
- Disabling back and/or leg pain and spinal imbalance.
- Severely restricted functional activities and substantially reduced overall quality of life.
The goals of surgery are to restore spinal balance and reduce pain and discomfort by relieving nerve pressure (decompression) and maintaining corrected alignment by fusing and stabilizing the spinal segments. When patients are carefully chosen and mentally well-prepared for surgery, excellent functional outcomes can be achieved which can provide positive life-changing experience for a given individual patient. When larger surgeries—those greater than 8 hours—are necessary, surgery may be divided into 2 surgeries 5 to 7 days apart.
Surgical procedures include:
- Decompression surgery removes the roof of the spinal canal (laminectomy) and enlarging the spaces where the nerve roots exit the canal (foraminotomy), resulting in decompressed nerve roots and pain relief. Typically only used at one or two vertebral levels in patients with leg pain from stenosis and smaller curves (< 30 degrees). In patients with more than two levels of stenosis and larger curves >30 degrees, a decompression without fusion has a risk of destabilizing the spine and causing the curve to worsen.
- Surgical stabilization involves anchoring hooks, wires or screws to the spinal segments and using metal rods to link the anchors together. They stabilize the spine and allow the spine to fuse in the corrected position, and is always performed with the addition of a fusion.
- Fusion uses the patient’s own bone or using cadaver or synthetic bone substitutes to “fix” the spine into a straighter position
- Osteotomy is a procedure in which spinal segments are cut and realigned
- Vertebral column resection removes entire vertebral sections prior to realigning the spine and is used when an osteotomy and other operative measures cannot correct the scoliosis.
- Scoliosis. Pediatric Orthopaedic Society of North America. http://orthoinfo.aaos.org/topic.cfm?topic=A00633[↩]
- Smith JR, Sciubba DM, Samdani AF. Scoliosis: a straightforward approach to diagnosis and management. JAAPA. 2008;21(11):40–45.[↩][↩]
- Bunnell WP. Selective screening for scoliosis. Clin Orthop Relat Res. 2005;(434):40–45.[↩][↩]
- O’Connor F. Pediatric Orthopedics for the Family Physician. Infant, Child & Adolescent Medicine. AAFP CME Program. 2007.[↩][↩]
- Glassman SD, Carreon LY, Shaffrey CI, et al. The costs and benefits of nonoperative management for adult scoliosis. Spine (Phila Pa 1976). 2010;35(5):578–582.[↩]
- Romano M, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Kotwicki T, Maier-Hennes A, Negrini S. Exercises for adolescent idiopathic scoliosis. Cochrane Database of Systematic Reviews 2012, Issue 8. Art. No.: CD007837. DOI: 10.1002/14651858.CD007837.pub2. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007837.pub2/full[↩]
- Effectiveness of Schroth exercises during bracing in adolescent idiopathic scoliosis: results from a preliminary study—SOSORT Award 2017 Winner. Published online 2017 Oct 16. doi: 10.1186/s13013-017-0139-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641990/[↩][↩][↩]
- [Schroth’s three dimensional treatment of scoliosis]. ZFA (Stuttgart). 1979 Dec 10;55(34):1969-76. https://www.ncbi.nlm.nih.gov/pubmed/547573/[↩]
- Physiotherapy scoliosis-specific exercises – a comprehensive review of seven major schools. Berdishevsky H, Lebel VA, Bettany-Saltikov J, Rigo M, Lebel A, Hennes A, Romano M, Białek M, M’hango A, Betts T, de Mauroy JC, Durmala J. Scoliosis Spinal Disord. 2016; 11():20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4973373/[↩]
- Neinstein LS, Chorley JN. Scoliosis and kyphosis. Adolescent Health Care: A Practical Guide. 4th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2002:345–355.[↩][↩]
- Reamy BV, Slakey JB. Adolescent idiopathic scoliosis: review and current concepts. Am Fam Physician. 2001;64(1):111–116.[↩][↩][↩]
- Ogilvie J. Adolescent idiopathic scoliosis and genetic testing. Curr Opin Pediatr. 2010;22(1):67–70.[↩][↩][↩]
- Linker B. A dangerous curve: the role of history in America’s scoliosis screening programs. Am J Public Health. 2012;102(4):606–616.[↩]
- U.S. Preventive Services Task Force. Screening for idiopathic scoliosis in adolescents. Recommendation statement. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryDraft/adolescent-idiopathic-scoliosis-screening1[↩][↩][↩][↩][↩][↩]
- American Academy of Family Physicians. Clinical recommendations. Scoliosis, idiopathic in adolescents. 2004. http://www.aafp.org/patient-care/clinical-recommendations/all/scoliosis.html[↩]
- Richards BS, Vitale M. SRS/AAOS position statement. School screening programs for the early detection of scoliosis. 2017. http://www.srs.org/patients-and-families/patient-brochures[↩]
- Greene WB, ed. Essentials of Musculoskeletal Care. 2nd ed. Rosemont, Ill.: American Academy of Orthopaedic Surgeons; 2001:696–699.[↩]
- Roach JW. Adolescent idiopathic scoliosis. Orthop Clin North Am. 1999;30(3):353–365, vii–viii.[↩]
- Tan KJ, Moe MM, Vaithinathan R, Wong HK. Curve progression in idiopathic scoliosis: follow-up study to skeletal maturity. Spine (Phila Pa 1976). 2009;34(7):697–700.[↩]
- Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66(7):1061–1071.[↩]
- Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90(3):540–553.[↩]
- Greiner KA. Adolescent idiopathic scoliosis: radiologic decision-making. Am Fam Physician. 2002;65(9):1817–1822.[↩][↩]
- Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66(7):1067.[↩]
- Adolescent Idiopathic Scoliosis: Diagnosis and Management. Am Fam Physician. 2014 Feb 1;89(3):193-198. http://www.aafp.org/afp/2014/0201/p193.html#afp20140201p193-b6[↩]
- Lenhert-Schroth C. Three diamentional treatment of scoloisis. 2007.[↩]
- Adults Scoliosis. Scoliosis Research Society. http://www.srs.org/patients-and-families/conditions-and-treatments/adults/scoliosis[↩][↩]