Contents
What are seasonal allergies
Seasonal allergies also called hay fever or seasonal allergic rhinitis. Seasonal allergies (seasonal allergic rhinitis), commonly referred to as hay fever, are caused by allergens like molds, pollen, dust mites, insects and animal dander. Seasonal allergies affects millions of people worldwide. Symptoms include sneezing, stuffiness, a runny nose and itchiness in your nose, the roof of your mouth, throat, eyes or ears. These allergic reactions are most commonly caused by pollen and mold spores in the air, which start a chain reaction in your immune system.
Your immune system controls how your body defends itself. For instance, if you have an allergy to pollen, your immune system identifies pollen as an invader or allergen. Your immune system overreacts by producing antibodies called Immunoglobulin E (IgE) 1. These antibodies travel to mast cells that release histamine and other chemicals, causing an allergic reaction with symptoms such as sneezing, stuffiness, a runny nose, itching and post-nasal drip.
Millions of people suffer from seasonal allergies triggered by airborne pollen—not just in spring but in summer and fall, too—and now evidence suggests their numbers will rise in a changing climate. Pollen seasons can last for several months and exposure is difficult to avoid. However, some people have symptoms year-round due to indoor allergens from pets, mold, dust mites and cockroach residue. This is called perennial allergic rhinitis. You can suffer from either seasonal or perennial allergic rhinitis, or a combination of both. According to the U.S. Department of Agriculture (USDA), the intensity of an allergic reaction depends on three interrelated factors: how much pollen a given species emits into the air, the duration of exposure, and the allergenicity of the pollen. In ragweed these factors coalesce in a perfect storm of allergic misery. What’s unique about ragweed is that it produces so much pollen—roughly a billion grains per plant. And the Amb a 1 protein [contained in the ragweed pollen coat] is also highly reactive with the immune system.
People with allergic rhinitis are also prone to itchy, watery eyes (from allergic conjunctivitis or eye allergies), and they may be more sensitive to irritants such as smoke, perfume or cold, dry air. Rhinitis can contribute to other problems such as asthma, sinus or ear conditions, or trouble sleeping.
What is pollen?
The word pollen is derived from the Greek word meaning ‘fine flour’. Pollen is the male fertilizing agent (male gametes or sperm cells) of flowering plants, trees, grasses and weeds and the role of the pollen grain is to fertilize the female flower to reproduce plant species. Pollen is also a major allergen that causes symptoms of seasonal allergic rhinitis (hay fever).
Pollen from plants with colorful flowers, like roses, usually do not cause allergies. These plants large, waxy pollen are carried from plant to plant by bees and other insects for fertilization. On the other hand, many trees, grasses and low-growing weeds have small, light, dry powdery pollen that are easily spread by wind. These are the pollen that trigger allergy symptoms.
Each plant has a period of pollination that does not vary much from year to year. However, weather conditions affect pollen levels. For instance, wind and humidity may affect pollen counts. Because pollen are small, light and dry, they can be easily spread by wind, which keeps pollen airborne and carries it over long distances. When the air is humid, such as during or after it rains, pollen becomes damp and heavy with moisture, keeping it still and on the ground. Seasonal allergic rhinitis is often caused by tree pollen in the early spring. During the late spring and early summer, grass pollen often cause symptoms. Late summer and fall hay fever is caused by weed pollen. In warmer places, pollination can be year-round.
Allergy symptoms are often minimal on days that are rainy, cloudy or windless, because pollen does not move about during these conditions. Hot, dry and windy weather signals greater pollen and mold distribution and therefore, increased allergy symptoms.
Pollen grains can be spread by birds, bees or wind:
- Some plants (such as flowering plants, including wattle trees) produce small amounts of pollen which are distributed by birds and bees from one plant to another.
- Other plants (such as pasture grasses and weeds) rely on the wind to spread their pollen. These pollen are produced in vast quantities, blow long distances and cause allergies in people, even if they live a long way from the source.
Most of the pollen that cause seasonal allergies is produced by airborne pollen from grasses, trees and weeds:
- Improved pasture grasses are more allergenic than native grasses.
- Pollen from exotic trees, which are planted for their autumn colors, is more allergenic than pollen from native trees.
How long do seasonal allergies last
Pollen seasons can last for several months. For more information you may want to visit the American Academy of Allergy, Asthma & Immunology’s National Allergy Bureau (NAB™) to find information on the current pollen and mold spore levels in your area: http://www.aaaai.org/global/nab-pollen-counts
The National Allergy Bureau currently provides the most accurate and reliable pollen and mold levels from approximately 84 counting stations throughout the United States, one counting station in Canada, and six counting stations in Argentina. The stations use air sampling equipment to collect airborne pollen and spores which are then examined microscopically. This information is also used for research to aid in the diagnosis, treatment and management of allergic diseases.
Pollen counts from the National Allergy Bureau stations are based on actual counts, which reflect the real day to day weather events. Predicted counts reported on many websites may be based on pollen data from previous years and general weather forecasts.
Ragweed Pollen
Ragweed and other weeds such as curly dock, lambs quarters, pigweed, plantain, sheep sorrel and sagebrush are some of the most prolific producers of pollen allergens .
Although the ragweed pollen season runs from August to November, ragweed pollen levels usually peak in mid-September in many areas in the country.
In addition, pollen counts are highest between 5:00 a.m. – 10:00 a.m. and on dry, hot and windy days.
Preventive Strategies
- Avoid the outdoors between 5:00 a.m. – 10:00 a.m. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Grass Pollen
As with tree pollen, grass pollen is regional as well as seasonal. In addition, grass pollen levels can be affected by temperature, time of day and rain.
Of the 1,200 species of grass that grow in North America, only a small percentage of these cause allergies. The most common grasses that can cause allergies are:
- Bermuda grass
- Johnson grass
- Kentucky bluegrass
- Orchard grass
- Sweet vernal grass
- Timothy grass
Preventive Strategies:
- If you have a grass lawn, have someone else do the mowing. If you must mow the lawn yourself, wear a mask.
- Keep grass cut short.
- Choose ground covers that don’t produce much pollen, such as Irish moss, bunch, and dichondra.
- Avoid the outdoors between 5:00 a.m. – 10:00 a.m. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Tree Pollen
Trees can aggravate your allergy whether or not they are on your property, since trees release large amounts of pollen that can be distributed miles away from the original source.
Trees are the earliest pollen producers, releasing their pollen as early as January in the Southern states and as late as May or June in the Northern states.
Most allergies are specific to one type of tree such as:
- catalpa
- elm
- hickory
- olive
- pecan
- sycamore
- walnut
or to the male cultivar of certain trees. The female of these species are totally pollen-free:
- ash
- box elder
- cottonwood
- date palm
- maple (red)
- maple (silver)
- Phoenix palm
- poplar
- willow
Some people, though, do show cross-reactivity among trees in the alder, beech, birch and oak family, and the juniper and cedar family.
Preventive Strategies
- If you buy trees for your yard, look for species that do not aggravate allergies such as crape myrtle, dogwood, fig, fir, palm, pear, plum, redbud and redwood trees or the female cultivars of ash, box elder, cottonwood, maple, palm, poplar or willow trees.
- Avoid the outdoors between 5:00 a.m. – 10:00 a.m. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Seasonal Allergic Rhinitis Triggers
Seasonal allergic rhinitis, commonly known as hay fever, is triggered by outdoor allergens such as pollen and mold spores. Some people have symptoms year-round due to indoor allergens from pets, mold, dust mites and cockroach residue. This is called perennial allergic rhinitis. You can suffer from either seasonal or perennial allergic rhinitis, or a combination of both.
Risk factors for seasonal allergic rhinitis
The following can increase your risk of developing hay fever:
- Having other allergies or asthma
- Having atopic dermatitis (eczema)
- Having a blood relative (such as a parent or sibling) with allergies or asthma
- Living or working in an environment that constantly exposes you to allergens — such as animal dander
- Having a mother who smoked during your first year of life
Complications of seasonal allergic rhinitis
Problems that may be associated with hay fever include:
- Reduced quality of life. Hay fever can interfere with your enjoyment of activities and cause you to be less productive. For many people, hay fever symptoms lead to absences from work or school.
- Poor sleep. Hay fever symptoms can keep you awake or make it hard to stay asleep, which can lead to fatigue and a general feeling of being unwell (malaise).
- Worsening asthma. Hay fever can worsen signs and symptoms of asthma, such as coughing and wheezing.
- Sinusitis. Prolonged sinus congestion due to hay fever may increase your susceptibility to sinusitis — an infection or inflammation of the membrane that lines the sinuses.
- Ear infection. In children, hay fever often is a factor in middle ear infection (otitis media).
Prevention of seasonal allergic rhinitis
There’s no way to avoid getting hay fever. If you have hay fever, the best thing to do is to lessen your exposure to the allergens that cause your symptoms. Take allergy medications before you’re exposed to allergens, as directed by your doctor.
Diagnosis of Seasonal Allergic Rhinitis
An allergist/immunologist, often referred to as an allergist, has specialized training and experience to determine which allergens, if any, are causing your symptoms. Your allergist will take a detailed health history, perform a physical exam and then most likely test you for allergies. Skin tests show the results within 20 minutes. These results, as well as how frequent and bad your symptoms are, will be considered when developing a treatment plan. Steps to manage your symptoms may include avoiding the allergens you are allergic to, medications or allergy immunotherapy (allergy shots or tablets).
- Skin prick test. You’re watched for an allergic reaction after small amounts of material that can trigger allergies are pricked into the skin of your arm or upper back. If you’re allergic, you develop a raised bump (hive) at the site of that allergen. Allergy specialists usually are best equipped to perform allergy skin tests.
- Allergy blood test. A blood sample is sent to a lab to measure your immune system’s response to a specific allergen. Also called the radioallergosorbent test (RAST), this test measures the amount of allergy-causing antibodies in your bloodstream, known as immunoglobulin E (IgE) antibodies.
Seasonal allergies treatments
The first step to manage this condition is to avoid allergens that cause symptoms. For instance, if you are allergic to dust mites, it is important to take steps to prevent exposure to dust mites, such as frequently washing bed linens in hot water. The same is true for outdoor allergens. Limiting your exposure during times of high pollen and mold counts may help reduce symptoms 2.
Nasal saline irrigation alone or combined with traditional treatments for allergic rhinitis has been shown to improve symptoms and quality of life while decreasing overall allergy medication use. Additional studies are needed to determine the optimal method and frequency of nasal irrigation and the preferred type of saline solution 3.
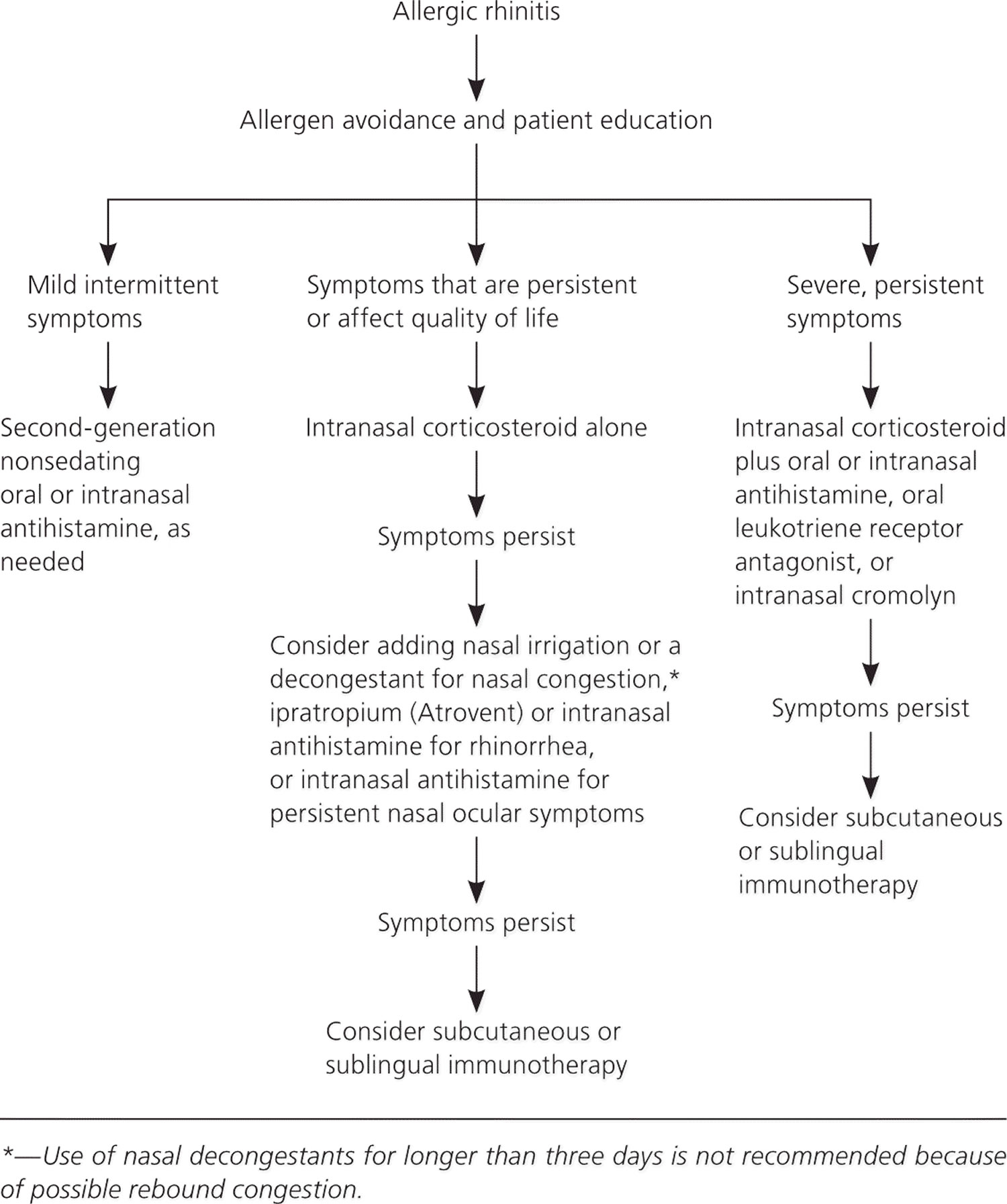
Figure 1. Treatment of Allergic Rhinitis
[Source 4]Sometimes taking steps to avoid allergens isn’t possible or it isn’t enough to control allergic rhinitis symptoms. That is when your allergist may suggest allergy immunotherapy or recommend medications to control inflammation and prevent symptoms.
Seasonal allergy medicine
Medicine for the treatment of allergic rhinitis include intranasal corticosteroids, oral and intranasal antihistamines, decongestants, intranasal cromolyn, intranasal anticholinergics, and leukotriene receptor antagonists 5. Decongestants and intranasal cromolyn are not recommended for children 6.
The International Primary Care Respiratory Group; British Society for Allergy and Clinical Immunology; and American Academy of Allergy, Asthma, and Immunology recommend intranasal corticosteroids alone for the initial treatment of persistent symptoms affecting quality of life and second-generation nonsedating antihistamines for mild intermittent disease 2. People with more severe disease not responding to intranasal corticosteroids with or without second-line therapies should be referred for consideration of immunotherapy 7. Table 1 lists treatments based on symptom type 8. Table 2 summarizes the treatment options 8.
Table 1. Symptom-Based Treatments for Allergic Rhinitis
| Treatment | Symptoms | |||
|---|---|---|---|---|
| Ocular | Nasopharyngeal itching | Sneezing | Rhinorrhea | |
Intranasal corticosteroids | ✓ | ✓ | ✓ | ✓ |
Oral and intranasal antihistamines | ✓ | ✓ | ✓ | |
Combination intranasal corticosteroid and antihistamine | ✓ | ✓ | ✓ | ✓ |
Oral and intranasal decongestants | ✓ | |||
Intranasal cromolyn | ✓ | ✓ | ✓ | |
Intranasal anticholinergics | ✓ | |||
Leukotriene receptor antagonists | ✓ | ✓ | ✓ | |
Immunotherapy | ✓ | ✓ | ✓ | ✓ |
note: Treatments are listed in approximate order of preference.
Table 2. Summary of Treatments for Allergic Rhinitis
| Type of therapy | FDA pregnancy category | Minimum age for use | Mechanism/onset of action | Adverse effects |
| Intranasal corticosteroids | Decrease the influx of inflammatory cells and inhibit the release of cytokines; onset of action is less than 30 minutes | Bitter aftertaste, burning, epistaxis, headache, nasal dryness; possible systemic absorption, rhinitis medicamentosa, stinging, throat irritation | ||
| Beclomethasone | C | 4 years | ||
| Budesonide (Rhinocort Aqua) | B | 6 years | ||
| Ciclesonide (Omnaris) | C | 6 years | ||
| Flunisolide | C | 6 years | ||
| Fluticasone furoate (Veramyst) | C | 2 years | ||
| Fluticasone propionate (Flonase) | C | 4 years | ||
| Mometasone (Nasonex) | C | 2 years | ||
| Triamcinolone acetonide | C | 2 years | ||
| Oral antihistamines | Block histamine H1 receptors; onset of action is 15 to 30 minutes | Dry mouth, sedation at higher than recommended doses | ||
| Cetirizine (Zyrtec) | B | 6 months | ||
| Desloratadine (Clarinex) | C | 6 months | ||
| Fexofenadine (Allegra) | C | 2 years (allergic rhinitis) | ||
| Loratadine (Claritin) | B | 2 years | ||
| Combination intranasal corticosteroid and antihistamine | See intranasal corticosteroids and intranasal antihistamines | See intranasal corticosteroids and intranasal antihistamines | ||
| Azelastine/fluticasone (Dymista) | C | 6 years | ||
| Intranasal antihistamines | ||||
| Azelastine (Astelin) | C | 5 years | Block H1 receptors; onset of action is 15 minutes | Bitter aftertaste, epistaxis, headache, nasal irritation, sedation |
| Oral decongestants | ||||
| Pseudoephedrine | C | 2 years (usually not started until 4 years) | Vasoconstriction; onset of action is 15 to 30 minutes | Headache, elevated blood pressure and intraocular pressure, tremor, urinary retention, dizziness, tachycardia, and insomnia |
| Intranasal cromolyns | ||||
| Cromolyn | B | 2 years | Inhibits histamine release | Epistaxis, nasal irritation, sneezing |
| Intranasal anticholinergics | ||||
| Ipratropium (Atrovent) | B | 5 years | Block acetylcholine receptors; onset of action is 15 minutes | Epistaxis, headache, nasal dryness |
| Leukotriene receptor antagonists | ||||
| Montelukast (Singulair) | B | 6 months | Block leukotriene receptors; onset of action is 2 hours | Elevated levels of alanine transaminase, aspartate transaminase, and bilirubin |
| Immunotherapy | Not well understood, believed to shift immune response from immunoglobulin E mediated to immunoglobulin G mediated | Minor local mouth irritation, diarrhea, vomiting; rare anaphylaxis | ||
| Sublingual Grastek (timothy grass pollen extract, cross reactive with 6 other grass pollens) | B | 5 years | ||
| Sublingual Oralair (5-grass pollen extract) | B | 10 years | ||
| Sublingual Ragwitek (short ragweed pollen extract) | C | 18 years | ||
| Subcutaneous allergen extracts: several tree, grass, weed pollens; cat and dog dander; dust mites; certain molds; and cockroaches; administered by a physician | Should not be initiated during pregnancy; maintenance therapy is considered safe | Has not been established; usually 5 years so that the child is old enough to cooperate | Local injection site reactions and, less commonly, systemic allergic reactions |
Note: Treatments are listed in approximate order of preference.
FDA = U.S. Food and Drug Administration; NA = not available.
[Source 4]Intranasal Corticosteroids
Intranasal corticosteroids are the mainstay of treatment for allergic rhinitis. They act by decreasing the influx of inflammatory cells and inhibiting the release of cytokines, thereby reducing inflammation of the nasal mucosa 9. Their onset of action can be less than 30 minutes, although peak effect may take several hours to days, with maximum effectiveness usually noted after two to four weeks of use 10. Many studies have demonstrated that intranasal corticosteroids are more effective than oral and intranasal antihistamines in the treatment of persistent or more severe allergic rhinitis 7.
There is no evidence that one intranasal corticosteroid is superior. However, many of the products have different age indications from the U.S. Food and Drug Administration (FDA), only budesonide (Rhinocort Aqua) has an FDA pregnancy category B safety rating, and only fluticasone furoate (Flonase) and triamcinolone acetonide are available over the counter.
The most common adverse effects of intranasal corticosteroids are throat irritation, epistaxis, stinging, burning, and nasal dryness 7. Although there has been concern about potential systemic adverse effects, including the suppression of the hypothalamic-pituitary axis, these effects have not been shown with currently available intranasal corticosteroids 11. The studies that specifically looked at the effects of the drugs on skeletal growth and adrenal activity did not demonstrate a decrease in growth of children over the course of one to three years 12. Despite these data, all intranasal corticosteroids carry a warning that long-term use may restrict growth in children.
Oral Antihistamines
Histamine is the most studied mediator in early allergic response. It causes smooth muscle constriction, mucus secretion, vascular permeability, and sensory nerve stimulation, resulting in the symptoms of allergic rhinitis.
First-generation antihistamines, including brompheniramine, chlorpheniramine, clemastine, and diphenhydramine (Benadryl), may cause sedation, fatigue, and impaired mental status. These adverse effects occur because the older antihistamines are more lipid soluble and more readily cross the blood-brain barrier than second-generation antihistamines. The use of first-generation sedating antihistamines has been associated with poor school performance, impaired driving, and increased automobile collisions and work injuries 13.
Compared with first-generation antihistamines, second-generation drugs have a better adverse effect profile and cause less sedation, with the exception of cetirizine (Zyrtec).27 Second-generation nonsedating oral antihistamines include loratadine (Claritin), desloratadine (Clarinex), levocetirizine (Xyzal), and fexofenadine (Allegra). Second-generation antihistamines have more complex chemical structures that decrease their movement across the blood-brain barrier, reducing central nervous system adverse effects such as sedation. Although cetirizine is generally classified as a second-generation antihistamine and a more potent histamine antagonist, it does not have the benefit of decreased sedation.
In general, oral antihistamines have been shown to effectively relieve the histamine-mediated symptoms associated with allergic rhinitis (e.g., sneezing, pruritus, rhinorrhea), but they are less effective than intranasal corticosteroids at treating nasal congestion and ocular symptoms. Because their onset of action is typically within 15 to 30 minutes and they are considered safe for children older than two years, second-generation antihistamines are useful for many patients with mild symptoms requiring as-needed treatment.
Intranasal Antihistamines
Compared with oral antihistamines, intranasal antihistamines have the advantage of delivering a higher concentration of medication to a targeted area, resulting in fewer adverse effects and an onset of action within 15 minutes 7. Intranasal antihistamines FDA-approved for the treatment of allergic rhinitis are azelastine (Astelin; for patients five years and older) and olopatadine (Patanol; for patients six years and older). They have been shown to be similar or superior to oral antihistamines in treating symptoms of conjunctivitis and rhinitis, and may improve congestion 14. Adverse effects include a bitter aftertaste, headache, nasal irritation, epistaxis, and sedation. Although intranasal antihistamines are an option if symptoms do not improve with nonsedating oral antihistamines, their use as first- or second-line therapy is limited by adverse effects, twice daily dosing, cost, and decreased effectiveness compared with intranasal corticosteroids 14.
Decongestants
Oral and intranasal decongestants improve nasal congestion associated with allergic rhinitis by acting on adrenergic receptors, which causes vasoconstriction in the nasal mucosa, decreasing inflammation 5. The most common decongestants are phenylephrine, oxymetazoline (Afrin), and pseudoephedrine. The abuse potential for pseudoephedrine should be weighed against its benefits.
Common adverse effects of intranasal decongestants are sneezing and nasal dryness. Use for more than three to five days is usually not recommended because patients may develop rhinitis medicamentosa, or may have rebound or recurring congestion 2. Oral decongestants may cause headache, elevated blood pressure and intraocular pressure, tremor, urinary retention, dizziness, tachycardia, and insomnia; therefore, these medications should be used with caution in patients with underlying cardiovascular conditions, glaucoma, or hyperthyroidism 7. Decongestants may be considered for short-term use in patients without improvement in congestion with intranasal corticosteroids 2.
Intranasal cromolyn
Intranasal cromolyn is available over the counter and is thought to inhibit the degranulation of mast cells.1 Although safe for general use, it is not considered first-line therapy for allergic rhinitis because it is less effective than antihistamines and intranasal corticosteroids and is given three or four times daily 7.
Intranasal Anticholinergics
Although evidence supports the use of intranasal ipratropium (Atrovent) for severe rhinorrhea, one study showed that it may also improve congestion and sneezing in children, but to a lesser extent than intranasal corticosteroids 15. Adverse effects include dryness of the nasal mucosa, epistaxis, and headache, and the recommended administration is two to three times daily 1.
Leukotriene Receptor Antagonists
The leukotriene D4 receptor antagonist montelukast (Singulair) is comparable to oral antihistamines but is less effective than intranasal corticosteroids 7. It may be particularly useful in patients with coexistent asthma because it reduces bronchospasm and attenuates the inflammatory response.
Combination Therapy
Although most patients should be treated with just one medication at a time, combination therapy is an option for patients with severe or persistent symptoms. Many studies have looked at the combination of an intranasal corticosteroid and an oral antihistamine or leukotriene receptor antagonist, but most have concluded that combination therapy is no more effective than an intranasal corticosteroid alone 2. However, recent studies have found the combination of azelastine/fluticasone (Dymista) to be superior (better effectiveness and faster symptom relief) to either treatment alone in patients with more severe allergic rhinitis 16.
Immunotherapy
Immunotherapy should be considered for moderate or severe persistent allergic rhinitis that is not responsive to usual treatments, in patients who cannot tolerate standard therapies or who want to avoid long-term medication use, and in patients with allergic asthma 17. Targeted immunotherapy, the only treatment that changes the natural course of allergic rhinitis, consists of administering a small amount of allergen extract subcutaneously or sublingually 18.
Subcutaneous injections are administered in the physician’s office at regular intervals, typically three times per week during a buildup phase, then every two to four weeks during a maintenance phase. The first dose of sublingual immunotherapy is administered in the physician’s office so that the patient can be observed for adverse effects, and then it is administered at home daily. The optimal length of therapy has not been determined, but three to five years is thought to be the best duration 2. The effects of immunotherapy can last up to seven to 12 years after the treatment is discontinued 19.
Subcutaneous immunotherapy has been proven effective in the treatment of adults and children with allergic rhinitis from exposure to dust mites, birch, Parietaria, ragweed, grass pollen, dog and cat dander, certain molds, and cockroaches.46 Sublingual immunotherapy is available only for allergy to five-grass, timothy grass, and short ragweed pollens. Although studies show subcutaneous immunotherapy may be slightly superior to sublingual immunotherapy for the reduction of allergic rhinitis and conjunctivitis, sublingual immunotherapy has a better safety profile, including lower risk of anaphylaxis, higher compliance, and possible prevention of new asthma in patients with allergic rhinitis 2. Sublingual therapy is limited in the United States because of high cost.
Omalizumab (Xolair), an anti-immunoglobulin E antibody approved for use in asthma treatment, has been shown to be effective in reducing nasal symptoms and improving quality-of-life scores in patients with allergic rhinitis 20. The main limitations of its use are high cost (approximately $900 per 150 mg, with dosing typically 300 mg every three to four weeks up to eight weeks) and lack of FDA approval for use in the treatment of allergic rhinitis.
Other Therapies
Many randomized controlled trials looking at acupuncture as a treatment for allergic rhinitis in adults and children have not shown sufficient evidence to support or refute its use 21. The safety and effectiveness of probiotics and herb and plant extract compounds have not been established 22.
Home remedies for seasonal allergies
Reduce your exposure to allergy triggers
To reduce your exposure to the things that trigger your allergy signs and symptoms (allergens):
- Stay indoors on dry, windy days. The best time to go outside is after a good rain, which helps clear pollen from the air.
- Delegate lawn mowing, weed pulling and other gardening chores that stir up allergens.
- Remove clothes you’ve worn outside and shower to rinse pollen from your skin and hair.
- Don’t hang laundry outside — pollen can stick to sheets and towels.
- Wear a pollen mask if you do outside chores.
Take extra steps when pollen counts are high
Seasonal allergy signs and symptoms can flare up when there’s a lot of pollen in the air. These steps can help you reduce your exposure:
- Check your local TV or radio station, your local newspaper, or the Internet for pollen forecasts and current pollen levels.
- If high pollen counts are forecasted, start taking allergy medications before your symptoms start.
- Close doors and windows at night or any other time when pollen counts are high.
- Avoid outdoor activity in the early morning when pollen counts are highest.
Pollen or molds
- Close doors and windows during pollen season.
- Don’t hang laundry outside — pollen can stick to sheets and towels.
- Use air conditioning in your house and car.
- Use an allergy-grade filter in your home ventilation system and change it regularly.
- Avoid outdoor activity in the early morning, when pollen counts are highest.
- Stay indoors on dry, windy days.
- Use a dehumidifier to reduce indoor humidity.
- Use a high-efficiency particulate air (HEPA) filter in your bedroom and other rooms where you spend a lot of time.
- Avoid mowing the lawn or raking leaves.
- Wear a dust mask when cleaning house or gardening.
Dust mites
- Use allergy-proof covers on mattresses, box springs and pillows.
- Wash sheets and blankets in water heated to at least 130 F (54 C).
- Use a dehumidifier or air conditioner to reduce indoor humidity.
- Vacuum carpets weekly with a vacuum cleaner equipped with a small-particle or HEPA filter.
- Spray insecticide designed to kill dust mites (acaricides) and approved for indoor use on carpets, furniture and bedding.
- Consider removing carpeting, especially where you sleep, if you’re highly sensitive to dust mites.
Cockroaches
- Block cracks and crevices where roaches can enter.
- Fix leaky faucets and pipes.
- Wash dishes and empty garbage daily.
- Sweep food crumbs from counters and floors.
- Store food, including pet food, in sealed containers.
- Consider professional pest extermination.
Pet dander
- Keep pets out of your home, if possible.
- Bathe dogs twice a week, if possible. The benefit of bathing cats hasn’t been proven.
- Keep pets out of the bedroom and off furniture.
Keep indoor air clean
There’s no miracle product that can eliminate all allergens from the air in your home, but these suggestions may help:
- Use the air conditioning in your house and car.
- If you have forced air heating or air conditioning in your house, use high-efficiency filters and follow regular maintenance schedules.
- Keep indoor air dry with a dehumidifier.
- Use a portable high-efficiency particulate air (HEPA) filter in your bedroom.
- Clean floors often with a vacuum cleaner that has a HEPA filter.
Try an over-the-counter remedy
Several types of nonprescription medications can help ease allergy symptoms. They include:
- Oral antihistamines. Antihistamines can help relieve sneezing, itching, a runny nose and watery eyes. Examples of oral antihistamines include loratadine (Claritin, Alavert), cetirizine (Zyrtec Allergy) and fexofenadine (Allegra Allergy).
- Decongestants. Oral decongestants such as pseudoephedrine (Sudafed, Afrinol, others) can provide temporary relief from nasal stuffiness. Decongestants also come in nasal sprays, such as oxymetazoline (Afrin) and phenylephrine (Neo-Synephrine). Only use nasal decongestants for a few days in a row. Longer-term use of decongestant nasal sprays can actually worsen symptoms (rebound congestion).
- Nasal spray. Cromolyn sodium nasal spray can ease allergy symptoms and doesn’t have serious side effects, though it’s most effective when you begin using it before your symptoms start.
- Combination medications. Some allergy medications combine an antihistamine with a decongestant. Examples include loratadine-pseudoephedrine (Claritin-D) and fexofenadine-pseudoephedrine (Allegra-D).
Rinse your sinuses
Rinsing your nasal passages with saline solution (nasal irrigation) is a quick, inexpensive and effective way to relieve nasal congestion. Rinsing directly flushes out mucus and allergens from your nose.
Look for a squeeze bottle or a neti pot — a small container with a spout designed for nasal rinsing — at your pharmacy or health food store. Use water that’s distilled, sterile, previously boiled and cooled, or filtered using a filter with an absolute pore size of 1 micron or smaller to make up the saline irrigation solution. Also be sure to rinse the irrigation device after each use with similarly distilled, sterile, previously boiled and cooled, or filtered water and leave open to air-dry.
When home remedies aren’t enough, see your doctor
For many people, avoiding allergens and taking over-the-counter medications is enough to ease symptoms. But if your seasonal allergies are still bothersome, don’t give up. A number of other treatments are available.
If you have bad seasonal allergies, your doctor may recommend that you have skin tests or blood tests to find out exactly what allergens trigger your symptoms. Testing can help determine what steps you need to take to avoid your specific triggers and identify which treatments are likely to work best for you.
For some people, allergy shots (allergen immunotherapy) can be a good option. Also known as desensitization, this treatment involves regular injections containing tiny amounts of the substances that cause your allergies. Over time, these injections reduce the immune system reaction that causes symptoms. For some allergies, treatment can be given as tablets under the tongue.
- Nelson HS, Rachelefsky GS, Bernick J. The Allergy Report. Milwaukee, Wis.: American Academy of Allergy, Asthma, and Immunology; 2000.[↩][↩]
- Seidman MD, Gurgel RK, Lin SY, et al. Clinical practice guideline: allergic rhinitis executive summary. Otolaryngol Head Neck Surg. 2015;152(2):197–206.[↩][↩][↩][↩][↩][↩][↩]
- Hermelingmeier KE, Weber RK, Hellmich M, Heubach CP, Mösges R. Nasal irrigation as an adjunctive treatment in allergic rhinitis: a systematic review and meta-analysis. Am J Rhinol Allergy. 2012;26(5):e119–e125.[↩]
- Treatment of Allergic Rhinitis. Am Fam Physician. 2015 Dec 1;92(11):985-992. https://www.aafp.org/afp/2015/1201/p985.html[↩][↩]
- Scadding GK, Durham SR, Mirakian R, et al.; British Society for Allergy and Clinical Immunology. BSACI guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy. 2008;38(1):19–42.[↩][↩]
- Barr JG, Al-Reefy H, Fox AT, Hopkins C. Allergic rhinitis in children [published correction appears in BMJ. 2014;349:4923]. BMJ. 2014;349:g4153.[↩]
- Brozek JL, Bousquet J, Baena-Cagnani CE, et al.; Global Allergy and Asthma European Network; Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic rhinitis and its impact on asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126(3):466–476.[↩][↩][↩][↩][↩][↩][↩]
- Sur DK, Scandale S. Treatment of allergic rhinitis. Am Fam Physician. 2010;81(12):1440–1446.[↩][↩][↩]
- Brozek JL, Bousquet J, Baena-Cagnani CE, et al.; Global Allergy and Asthma European Network; Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic rhinitis and its impact on asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126(3):466–476[↩]
- Derendorf H, Meltzer EO. Molecular and clinical pharmacology of intranasal corticosteroids: clinical and therapeutic implications. Allergy. 2008;63(10):1292–1300.[↩]
- Sastre J, Mosges R. Local and systemic safety of intranasal corticosteroids. J Investig Allergol Clin Immunol. 2012;22(1):1–12.[↩]
- Mansfield LE, Mendoza CP. Medium and long-term growth in children receiving intranasal beclomethasone dipropionate: a clinical experience. South Med J. 2002;95(3):334–340.[↩]
- Robb G, Sultana S, Ameratunga S, Jackson R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj Prev. 2008;14(1):51–58.[↩]
- Tran NP, Vickery J, Blaiss MS. Management of rhinitis: allergic and non-allergic. Allergy Asthma Immunol Res. 2011;3(3):148–156.[↩][↩]
- Milgrom H, Biondi R, Georgitis JW, et al. Comparison of ipratropium bromide 0.03% with beclomethasone dipropionate in the treatment of perennial rhinitis in children. Ann Allergy Asthma Immunol. 1999;83(2):105–111.[↩]
- Price D, Shah S, Bhatia S, et al. A new therapy (MP29-02) is effective for the long-term treatment of chronic rhinitis. J Investig Allergol Clin Immunol. 2013;23(7):495–503.[↩]
- Solelhac G, Charpin D. Management of allergic rhinitis. F1000Prime Rep. 2014;6:94.[↩]
- Durham SR, Yang WH, Pedersen MR, Johansen N, Rak S. Sublingual immunotherapy with once-daily grass allergen tablets: a randomized controlled trial in seasonal allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2006;117(4):802–809.[↩]
- Burks AW, Calderon MA, Casale T, et al. Update on allergy immunotherapy: American Academy of Allergy, Asthma & Immunology/European Academy of Allergy and Clinical Immunology/PRACTALL consensus report. J Allergy Clin Immunol. 2013;131(5):1288–96.e3.[↩]
- Casale TB, Condemi J, LaForce C, et al.; Omalizumab Seasonal Allergic Rhinitis Trial Group. Effect of omalizumab on symptoms of seasonal allergic rhinitis: a randomized controlled trial. JAMA. 2001;286(23):2956–2967.[↩]
- Brinkhaus B, Witt CM, Jena S, Liecker B, Wegscheider K, Willich SN. Acupuncture in patients with allergic rhinitis: a pragmatic randomized trial. Ann Allergy Asthma Immunol. 2008;101(5):535–543.[↩]
- Schapowal A; Petasites Study Group. Randomised controlled trial of butterbur and cetirizine for treating seasonal allergic rhinitis. BMJ. 2002;324(7330):144–146.[↩]