Contents
- What is testicular cancer
- The Testes
- Types of testicular cancer
- Testicular cancer survival rate
- Testicular cancer causes
- Testicular cancer signs and symptoms
- Non-cancer causes of testicular or scrotal symptoms
- Testicular cancer prevention
- Testicular cancer diagnosis
- Testicular Cancer Stages
- Testicular cancer treatment
- Testicular cancer Treatment Options by Stage
- Treatment of Stage 0 (Testicular Intraepithelial Neoplasia)
- Stage 1 seminomas
- Stage 1S seminomas
- Stage 2A seminomas
- Stage 2B seminomas
- Stage 2C seminomas
- Stage 1 non-seminomas
- Stage 1S non-seminoma
- Stage 2 non-seminomas
- Stage 2A non-seminomas
- Stage 2B non-seminomas
- Stage 3 seminomas and non-seminomas
- Recurrent testicular cancer
- Sertoli cell and Leydig cell tumors
- Testicular cancer prognosis
What is testicular cancer
Cancer that starts in the testicles (testes) is called testicular cancer, which are located inside the scrotum, a loose bag of skin underneath the penis 1, 2, 3, 4. The testicles are part of the male reproductive system. The testicles produce male sex hormones and sperm for reproduction.
The testicles are made up of several types of cells, each of which can develop into one or more types of cancer. It is important to distinguish these types of cancers from one another because they differ in how they are treated and in their prognosis (outlook).
Compared with other types of cancer, testicular cancer is rare. But testicular cancer is the most common cancer in American males between the ages of 15 and 45. The average age at the time of diagnosis of testicular cancer is about 33. This is largely a disease of young and middle-aged men, but about 6% of cases occur in children and teens, and about 8% occur in men over the age of 55 5.
Testicular cancer facts 6
- Males of any age can develop testicular cancer, including infants and elderly men.
- About half of all cases of testicular cancer are in men between the ages of 20 and 34.
- Testicular cancer is not common; a man’s lifetime chance of getting it is about 1 in 263. The risk of dying from this cancer is about 1 in 5,000.
- Testicular cancer can be treated and usually cured, especially when it’s found early – when it’s small and hasn’t spread.
The American Cancer Society’s estimates for testicular cancer in the United States for 2025 are 5, 7:
- About 9,720 new cases of testicular cancer diagnosed
- About 600 deaths from testicular cancer
- Rate of new testicular cancer cases and deaths per 100,000: The rate of new cases of testicular cancer was 5.9 per 100,000 men per year. The death rate was 0.3 per 100,000 men per year. These rates are age-adjusted and based on 2017–2021 cases and 2018–2022 deaths.
- Lifetime risk of developing testicular cancer: Approximately 0.4 percent of men will be diagnosed with testicular cancer at some point during their lifetime, based on 2018–2021 data.
- Prevalence of testicular cancer: In 2021, there were an estimated 299,845 men living with testicular cancer in the United States.
The incidence rate of testicular cancer has been increasing in the United States and many other countries for several decades. The increase is mostly in seminomas. Experts have not been able to find reasons for this increase. Lately, the rate of increase has slowed.
Testicular cancer is not common; about 1 of every 250 males will develop testicular cancer at some point during their lifetime.
Because testicular cancer usually can be treated successfully, a man’s lifetime risk of dying from testicular cancer is very low: about 1 in 5,000 5. Testicular cancer 5-Year Relative Survival for a specific stage of testicular cancer is 95%, it means that men who have that cancer are, on average, about 95% as likely as men who don’t have that cancer to live for at least 5 years after being diagnosed 7.
Testicular cancer is highly treatable, even when cancer has spread beyond the testicle. Your treatment plan depends on your stage and type of testicular cancer. Usually you have surgery. You might have chemotherapy or radiotherapy after surgery or a combination.
What are germ cell tumors?
Germ cell tumors develop in germ cells. Germ cells are cells in your body that develop into sperms in males and eggs in females. Germ cell tumors most often develop in the ovary or testicle because this is where most germ cells are. However, germ cells can sometimes be left behind in other parts of your body from when you developed in the womb. So germ cell tumors can develop anywhere in your body where there are germ cells.
Doctors use different names to describe the different types of germ cell tumors (GCTs). The name describes:
- whereabouts in the body it started – such as ovarian or testicular
- what the tumor looks like under the microscope
Some tumors are non cancerous (benign). And some are cancerous (malignant):
- Benign germ cell tumors include mature teratomas.
- Malignant germ cell tumors are split into 2 main groups:
- Seminoma germ cell tumors (in females these are called dysgerminomas). Seminomas are sometimes called pure seminomas. They only contain one type of cell. Some germ cell tumor contain both seminoma cells and non seminoma cells. Doctors usually class and treat these as non seminoma tumors.
- Non-seminoma germ cell tumors (in females these are called non dysgerminomas). Some non-seminomas develop from just one type of cell. And some develop from a mixture of cell types. So, for example, a tumor can contain a mix of some teratoma cells and some embryonal carcinoma cells.
- Malignant non-seminoma tumors include:
- immature teratomas
- yolk sac tumors
- choriocarcinomas
- embryonal carcinomas
- Malignant non-seminoma tumors include:
Germ cell tumors (GCTs) can start in the:
- testicles
- ovaries
- chest (mediastinal germ cell tumors)
- back of the tummy (retroperitoneal germ cell tumor)
- brain (pineal region tumor)
- lower spine (sacrococcygeal germ cell tumor)
Germ cell tumors that grow outside the ovary or testicle are called extragonadal germ cell tumors (EGGCTs) and they are very rare. “Extragonadal” means outside of the gonads (sex organs). Extragonadal germ cell tumors (EGGCTs) may begin to grow anywhere in your body but usually begin in organs such as the pineal gland in your brain, in the mediastinum (area between the lungs), or in the retroperitoneum (the back wall of the abdomen). Extragonadal germ cell tumors (EGGCTs) can be benign (noncancer) or malignant (cancer). Benign extragonadal germ cell tumors are called benign teratomas. These are more common than malignant extragonadal germ cell tumors and often are very large.
Malignant extragonadal germ cell tumors are divided into two types, nonseminoma and seminoma. Nonseminomas tend to grow and spread more quickly than seminomas. They usually are large and cause signs and symptoms. If untreated, malignant extragonadal germ cell tumors may spread to the lungs, lymph nodes, bones, liver, or other parts of the body.
The main treatments are surgery and chemotherapy. Your treatment depends on your type of germ cell tumor and whereabouts it is in your body.
The Testes
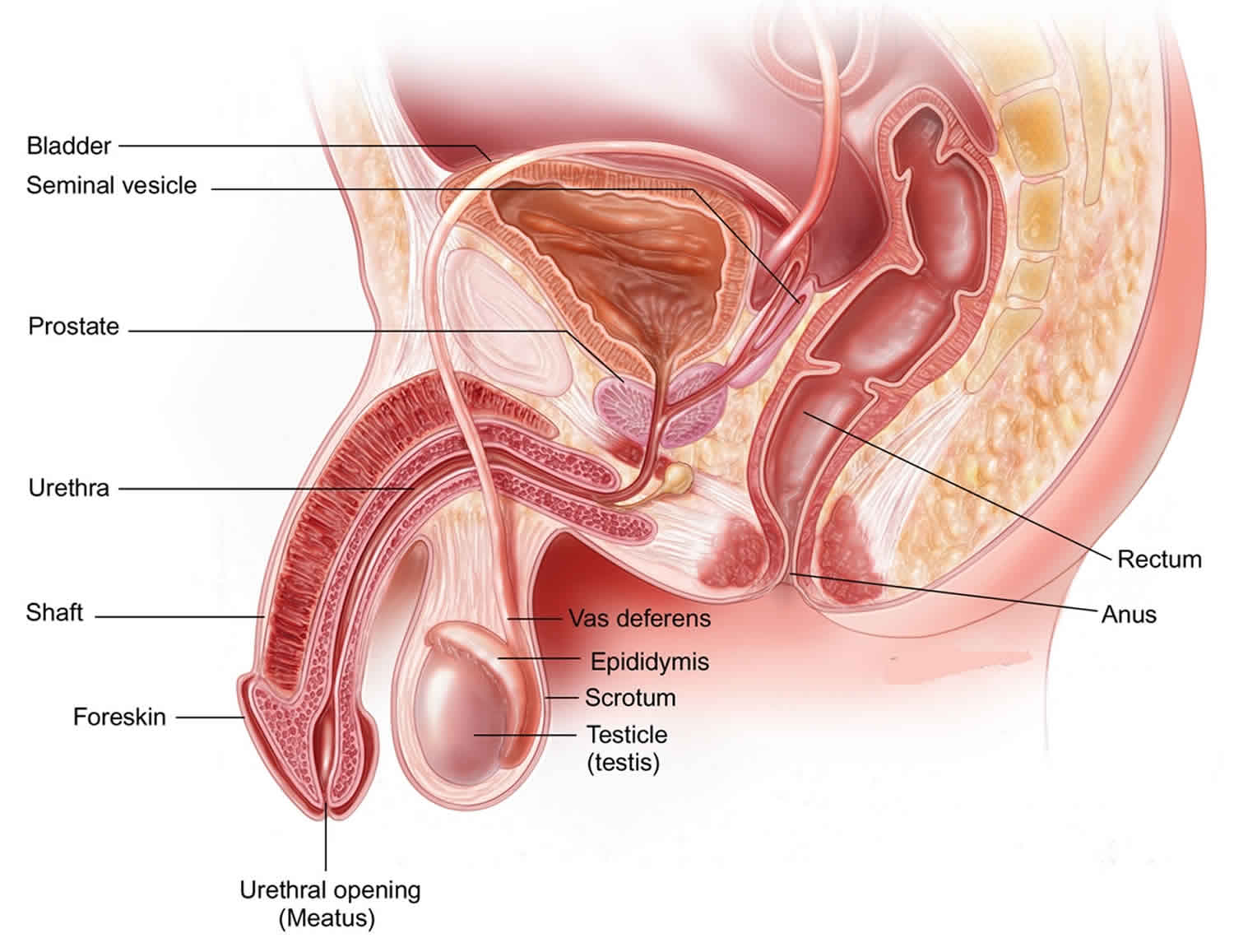
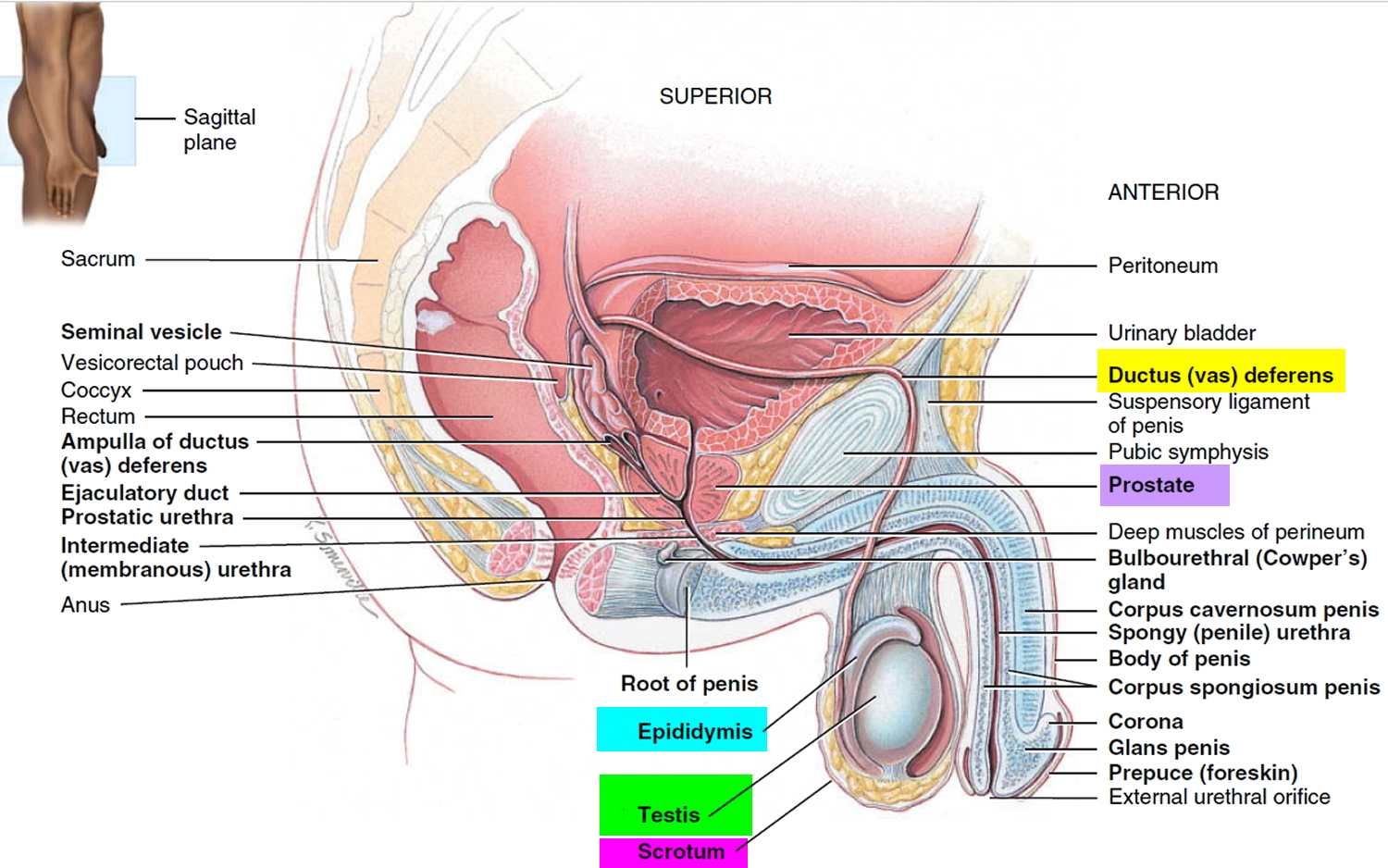
The testes or testicles (a single testicle is called a testis), are paired oval glands in the scrotum measuring about 5 cm (2 inch) long and 2.5 cm (1 inch) in diameter. Testicles are part of the male reproductive system. Each testis (singular) has a mass of 10–15 grams. The 2 oval glands are each normally a little smaller than a golf ball in adult males. They’re held within a sac of skin called the scrotum. The scrotum hangs under the base of the penis.
Testicles have 2 main functions:
- They make male hormones (androgens) such as testosterone.
- They make sperm, the male cells needed to fertilize a female egg cell to start a pregnancy.
The testes develop near the kidneys, in the posterior portion of the abdomen and they usually begin their descent into the scrotum through the inguinal canals (passageways in the lower anterior abdominal wall) during the latter half of the seventh month of fetal development.
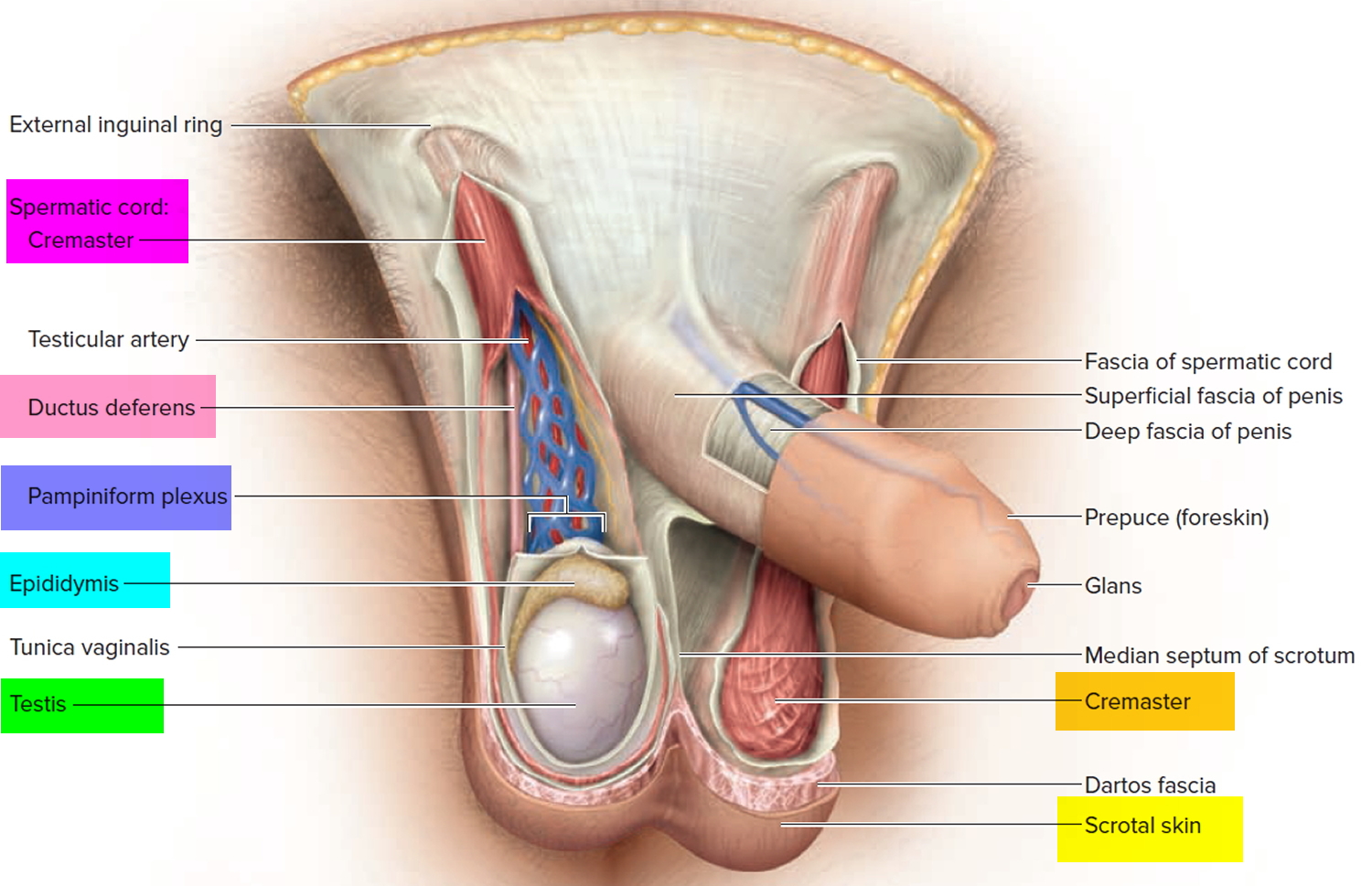
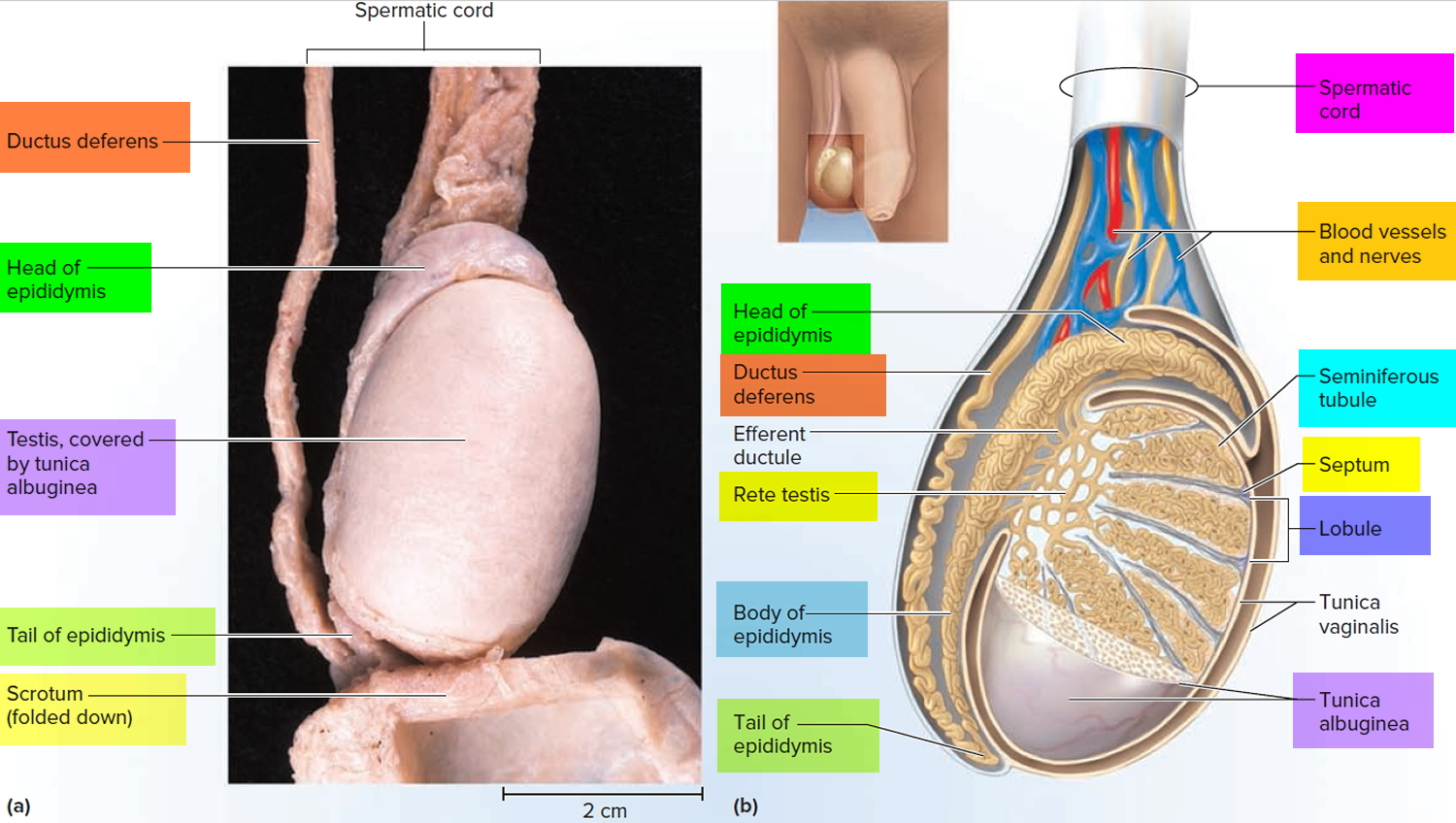
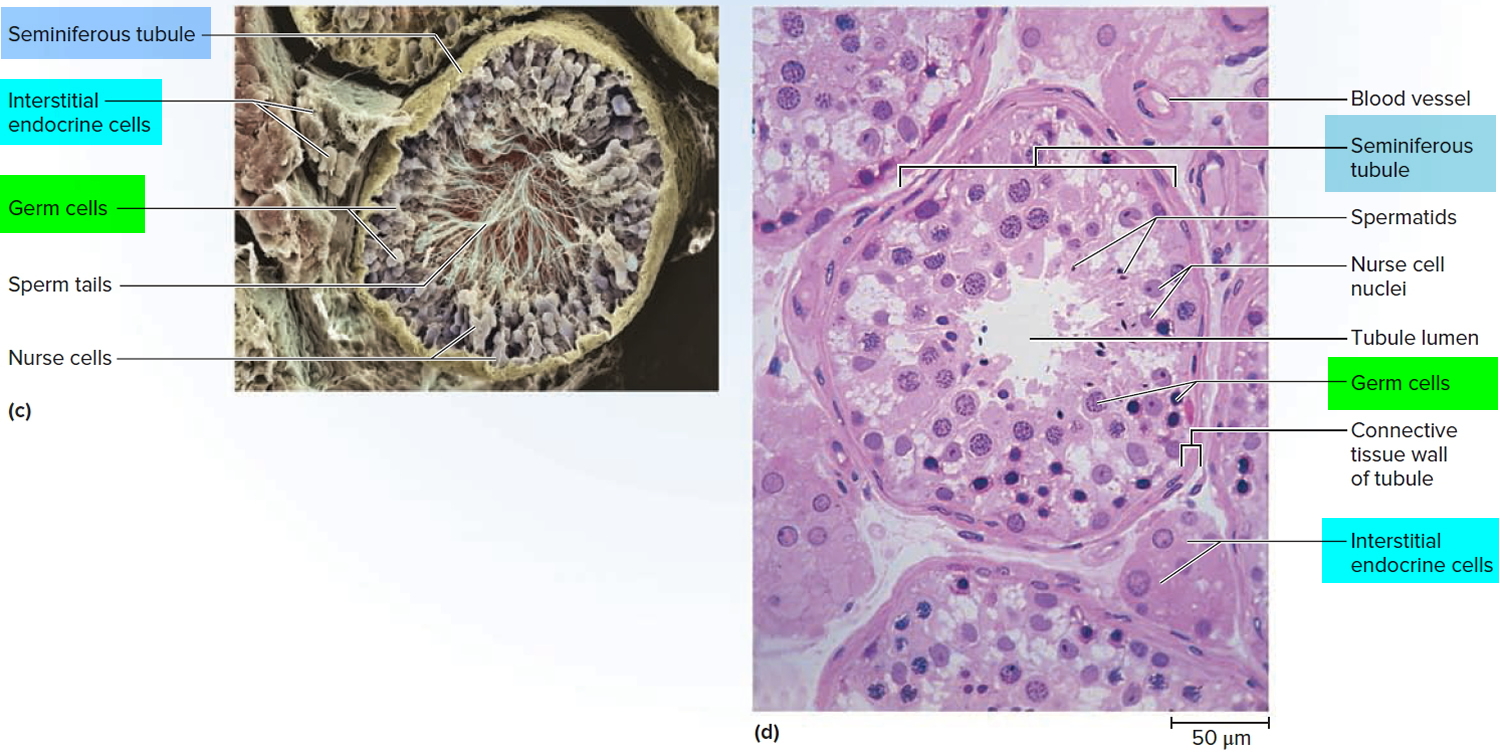
A serous membrane called the tunica vaginalis, which is derived from the peritoneum and forms during the descent of the testes, partially covers the testes. A collection of serous fluid in the tunica vaginalis is called a hydrocele. It may be caused by injury to the testes or inflammation of the epididymis. Usually, no treatment is required. Internal to the tunica vaginalis the testis is surrounded by a white fibrous capsule composed of dense irregular connective tissue, the tunica albuginea; it extends inward, forming septa that divide the testis into a series of internal compartments called lobules. Each of the 200–300 lobules contains one to three tightly coiled tubules, the seminiferous tubules, where sperm are produced. The process by which the seminiferous tubules of the testes produce sperm is called spermatogenesis.
The seminiferous tubules contain two types of cells: spermatogenic cells, the sperm-forming cells, and sustentacular cells or Sertoli cells, which have several functions in supporting spermatogenesis. Stem cells called spermatogonia develop from primordial germ cells that arise from the yolk sac and enter the testes during the fifth week of development. In the embryonic testes, the primordial germ cells differentiate into spermatogonia, which remain dormant during childhood and actively begin producing sperm at puberty. Toward the lumen of the seminiferous tubule are layers of progressively more mature cells. In order of advancing maturity, these are primary spermatocytes, secondary spermatocytes, spermatids, and sperm cells. After a sperm cell, or spermatozoon, has formed, it is released into the lumen of the seminiferous tubule. Sperm cells are then stored in a small coiled tube behind each testicle called the epididymis. This is where they mature.
During ejaculation, sperm cells are carried from the epididymis through the vas deferens to seminal vesicles, where they mix with fluids made by the vesicles, prostate gland, and other glands to form semen. This fluid then enters the urethra, the tube in the center of the penis through which both urine and semen leave the body.
Embedded among the spermatogenic cells in the seminiferous tubules are large sustentacular cells or Sertoli cells, which extend from the basement membrane to the lumen of the tubule. Internal to the basement membrane and spermatogonia, tight junctions join neighboring sustentacular cells to one another. These junctions form an obstruction known as the blood–testis barrier because substances must first pass through the sustentacular cells before they can reach the developing sperm. By isolating the developing gametes from the blood, the blood–testis barrier prevents an immune response against the spermatogenic cell’s surface antigens, which are recognized as “foreign” by the immune system. The blood–testis barrier does not include spermatogonia.
Sustentacular cells (Sertoli cells) support and protect developing spermatogenic cells in several ways. They nourish spermatocytes, spermatids, and sperm; phagocytize excess spermatid cytoplasm as development proceeds; and control movements of spermatogenic cells and the release of sperm into the lumen of the seminiferous tubule. They also produce fluid for sperm transport, secrete the hormone inhibin, and regulate the effects of testosterone and FSH (follicle-stimulating hormone).
In the spaces between adjacent seminiferous tubules are clusters of cells called interstitial cells or Leydig cells. These cells secrete testosterone, the most prevalent androgen. An androgen is a hormone that promotes the development of masculine characteristics. Testosterone also promotes a man’s libido (sexual drive).
The scrotum (bag), the supporting structure for the testes, consists of loose skin and underlying subcutaneous layer that hangs from the root (attached portion) of the penis. Externally, the scrotum looks like a single pouch of skin separated into lateral portions by a median ridge called the raphe. Internally, the scrotal septum divides the scrotum into two compartments, each containing a single testis. The location of the scrotum and the contraction of its muscle fibers regulate the temperature of the testes. Normal sperm production requires a temperature about 2–3°C below core body temperature. This lowered temperature is maintained within the scrotum because it is outside the pelvic cavity. In response to cold temperatures, the cremaster and dartos muscles contract. Contraction of the cremaster muscles moves the testes closer to the body, where they can absorb body heat. Contraction of the dartos muscle causes the scrotum to become tight (wrinkled in appearance), which reduces heat loss. Exposure to warmth reverses these actions.
Figure 1. Male reproductive system
Figure 2. Testis
Figure 3. Testicle anatomy
Figure 4. Testis and scrotum (cross section view)
Figure 5. Scanning electron micrograph of the seminiferous tubules
Types of testicular cancer
Your testicles are made up of many types of cells, each of which can develop into one or more types of cancer. It’s important to know the type of cell the cancer started in and what kind of cancer it is because they differ in how they’re treated and in their prognosis (outlook). Doctors can tell what type of testicular cancer you have by looking at the cells under a microscope.
Germ cell tumors
More than 90% of cancers of the testicle develop in special cells known as germ cells. These are the cells that make sperm. They are also called germ cell tumors. The 2 main types of germ cell tumors in men are:
- Seminomas: Slow-growing cancer that primarily affects people in their 40s or 50s.
- Non-seminomas: Non-seminoma testicular cancer grows more rapidly than seminomas. Non-seminoma testicular cancer mainly affects males in their late teens, 20s and early 30s. There are four types of non-seminoma tumors. Each is named after the type of germ cell that makes up the tumor. Non-seminoma tumors include embryonal carcinoma, yolk sac carcinoma, choriocarcinoma and teratoma.
Doctors can tell what type of testicular cancer you have by looking at the cells under a microscope.
These 2 types of testicular cancer occur about equally. Many testicular cancers contain both seminoma and non-seminoma cells. These mixed germ cell tumors are treated as non-seminomas because they grow and spread like non-seminomas.
Seminomas
- Classical seminoma: More than 95% of seminomas are classical. These usually occur in men between 25 and 45.
- Spermatocytic seminoma: This rare type of seminoma tends to occur in older men. The average age of men diagnosed with spermatocytic seminoma is about 65. Spermatocytic tumors tend to grow more slowly and are less likely to spread to other parts of the body than classical seminomas.
Some seminomas can increase blood levels of a protein called human chorionic gonadotropin (HCG). Human chorionic gonadotropin (HCG) can be detected by a simple blood test and is considered a tumor marker for certain types of testicular cancer. It can be used for diagnosis and to check how the patient is responding to treatment.
Non-seminomas
These types of germ cell tumors usually occur in men between their late teens and early 30s. The 4 main types of non-seminoma tumors are:
Most tumors are a mix of different types sometimes with a seminoma component as well, but this doesn’t change the general approach to treatment of most non-seminoma cancers. These mixed germ cell tumors are treated as non-seminomas because they grow and spread like non-seminomas.
- 1) Embryonal carcinoma: This type of non-seminoma is present to some degree in about 40% of testicular tumors, but pure embryonal carcinomas occur only 3% to 4% of the time. When seen under a microscope, these tumors can look like tissues of very early embryos (fetus). This type of non-seminoma tends to grow rapidly and spread outside the testicle. Embryonal carcinoma can increase blood levels of a tumor marker protein called alpha-fetoprotein (AFP), as well as human chorionic gonadotropin (HCG).
- 2) Yolk sac carcinoma: These tumors are so named because their cells look like the yolk sac of an early human embryo. Other names for this cancer include yolk sac tumor, endodermal sinus tumor, infantile embryonal carcinoma, or orchidoblastoma. Yolk sac carcinoma is the most common form of testicular cancer in children especially in infants, but pure yolk sac carcinomas (tumors that do not have other types of non-seminoma cells) are rare in adults. When they occur in children, yolk sac carcinomas usually are treated successfully. But they are of more concern when they occur in adults, especially if they are pure. Yolk sac carcinomas respond very well to chemotherapy, even if they have spread. Yolk sac carcinoma almost always increases blood levels of AFP (alpha-fetoprotein).
- 3) Choriocarcinoma: This is a very rare and aggressive type of testicular cancer in adults. Pure choriocarcinoma is likely to spread rapidly to distant organs of the body, including the lungs, bones, and brain. More often, choriocarcinoma cells are present with other types of non-seminoma cells in a mixed germ cell tumor. These mixed tumors tend to have a somewhat better outlook than pure choriocarcinomas, although the presence of choriocarcinoma is always a worrisome finding. Choriocarcinoma increases blood levels of HCG (human chorionic gonadotropin).
- 4) Teratoma: Teratomas are germ cell tumors with areas that, under a microscope, look like each of the 3 layers of a developing embryo: the endoderm (innermost layer), mesoderm (middle layer), and ectoderm (outer layer). Pure teratomas of the testicles are rare and do not increase AFP (alpha-fetoprotein) or HCG (human chorionic gonadotropin) levels. More often, teratomas are seen as parts of mixed germ cell tumors. There are 3 main types of teratomas:
- Mature teratomas are tumors formed by cells similar to cells of adult tissues. They rarely spread to nearby tissues and distant parts of the body. They can usually be cured with surgery, but some come back (recur) after treatment.
- Immature teratomas are less well-developed cancers with cells that look like those of an early embryo. This type is more likely than a mature teratoma to grow into (invade) surrounding tissues, to spread (metastasize) outside the testicle, and to come back (recur) years after treatment.
- Teratomas with somatic type malignancy are very rare cancers. These cancers have some areas that look like mature teratomas but have other areas where the cells have become a type of cancer that normally develops outside the testicle (such as a sarcoma, adenocarcinoma, or even leukemia).
Carcinoma in situ of the testicle
Testicular germ cell cancers can begin as a non-invasive form of the disease called carcinoma in situ (CIS) or intratubular germ cell neoplasia. In testicular carcinoma in situ, the cells look abnormal under the microscope, but they have not yet spread outside the walls of the seminiferous tubules (where sperm cells are formed). Carcinoma in situ doesn’t always progress to invasive cancer.
It is hard to find carcinoma in situ before it does become an invasive cancer because it generally does not cause symptoms and often does not form a lump that you or the doctor can feel. The only way to diagnose testicular carcinoma in situ is to have a biopsy (a procedure that removes a tissue sample and looks at it under a microscope). Some cases are found incidentally (by accident) when a testicular biopsy is done for another reason, such as infertility.
Experts don’t agree about the best treatment for carcinoma in situ. Since carcinoma in situ doesn’t always become an invasive cancer, many doctors in the United States consider observation (watchful waiting) to be the best treatment option.
When carcinoma in situ of the testicle becomes invasive, its cells are no longer just in the seminiferous tubules but have grown into other structures of the testicle. These cancer cells can then spread either to the lymph nodes (small, bean-shaped collections of white blood cells) through lymphatic channels (fluid-filled vessels that connect the lymph nodes), or through the blood to other parts of the body.
Stromal tumors
Tumors can also develop in the supportive and hormone-producing tissues, or stroma, of the testicles. These tumors are known as gonadal stromal tumors. They make up less than 5% of adult testicular tumors but up to 20% of childhood testicular tumors. The 2 main types are Leydig cell tumors and Sertoli cell tumors.
Leydig cell tumors
These tumors develop from the Leydig cells in the testicle that normally make male sex hormones (androgens like testosterone). Leydig cell tumors can develop in both adults and children. These tumors often make androgens (male hormones) but sometimes produce estrogens (female sex hormones).
Most Leydig cell tumors are benign. They usually do not spread beyond the testicle and are cured with surgery. But a small portion of Leydig cell tumors spread to other parts of the body and tend to have a poor outlook because they usually do not respond well to chemotherapy or radiation therapy.
Sertoli cell tumors
These tumors develop from normal Sertoli cells, which support and nourish the sperm-making germ cells. Like the Leydig cell tumors, these tumors are usually benign. But if they spread, they usually don’t respond well to chemotherapy and radiation therapy.
Secondary testicular cancers
Cancers that start in another organ and then spread to the testicle are called secondary testicular cancers. These are not true testicular cancers – they are named and treated based on where they started.
Lymphoma is the most common secondary testicular cancer. Testicular lymphoma occurs more often than primary testicular tumors in men older than 50. The outlook depends on the type and stage of lymphoma. The usual treatment is surgical removal, followed by radiation and/or chemotherapy.
In boys with acute leukemia, the leukemia cells can sometimes form a tumor in the testicle. Along with chemotherapy to treat the leukemia, this might require treatment with radiation or surgery to remove the testicle.
Cancers of the prostate, lung, skin (melanoma), kidney, and other organs also can spread to the testicles. The prognosis for these cancers tends to be poor because these cancers have usually spread widely to other organs as well. Treatment depends on the specific type of cancer.
Testicular cancer survival rate
The 5-year survival rate refers to the percentage of patients who live at least 5 years after their cancer is diagnosed. Of course, many people live much longer than 5 years (and many are cured).
Five-year relative survival rates assume that some people will die of other causes and compare the observed survival with that expected for people without the cancer. This is a better way to see the impact of the cancer on survival.
In order to get 5-year survival rates, doctors have to look at people who were treated at least 5 years ago. Improvements in treatment since then may result in a more favorable outlook for people now being diagnosed with testicular cancer.
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they cannot predict what will happen in any particular person’s case. Many other factors may affect a person’s outlook, such as your age and how well the cancer responds to treatment. Your doctor can tell you how the numbers below may apply to you, as he or she is familiar with your particular situation.
Testicular cancer survival rates, by stage
The survival statistics below come from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database, and are based on patients who were diagnosed with testicular cancer (of any type) between 2003 and 2009.
The SEER database does not divide survival rates by the American Joint Committee on Cancer (AJCC) TNM stage. Instead, it divides cancers into summary stages: localized, regional, and distant:
- Localized means that the cancer is still only in the testicle. This includes most AJCC stage 1 tumors (stage 0 cancers are not included in these statistics).
- Regional means that the cancer has spread to nearby lymph nodes or tissues. This includes T4 tumors and cancers with lymph node spread (all stage 2 cancers and some stage 3B and 3C cancers).
- Distant means that the cancer has spread to organs or lymph nodes away from the tumor, such as all M1 cancers (which can be stage 3A, 3B, or 3C).
| Stage | 5-Year Relative Survival Rate |
| Localized | 99% |
| Regional | 96% |
| Distant | 73% |
Footnotes: These numbers apply only to the stage of the cancer when it is first diagnosed. They do not apply later on if the cancer grows, spreads, or comes back after treatment. These numbers don’t take everything into account. These survival rates are grouped based on how far the cancer has spread. But other factors, including your age and overall health, the type of testicular cancer, and how well the cancer responds to treatment can also affect your outlook. Ask your doctor to explain how these or other factors might be important for you. People now being diagnosed with testicular cancer may have a better outlook than these numbers show. Treatments improve over time, and these numbers are based on people who were diagnosed and treated at least five years earlier.
Other prognostic factors
As can be seen in the table above, how far the cancer has spread at the time it’s diagnosed can affect your chances of long-term survival. But in general, the outlook for testicular cancers is very good, and most of these cancers can be cured, even if they have spread.
Some other factors can also affect outlook, such as:
- The type of testicular cancer
- Levels of tumor markers after the testicular tumor has been removed
Ask your doctor how these or other prognostic factors might affect your outlook.
Testicular cancer causes
It’s not clear what causes testicular cancer in most cases.
Doctors know that testicular cancer occurs when healthy cells in a testicle become altered. Healthy cells grow and divide in an orderly way to keep your body functioning normally. But sometimes some cells develop abnormalities, causing this growth to get out of control — these cancer cells continue dividing even when new cells aren’t needed. The accumulating cells form a mass in the testicle.
Nearly all testicular cancers begin in the germ cells — the cells in the testicles that produce immature sperm. What causes germ cells to become abnormal and develop into cancer isn’t known.
Scientists have found that the disease is linked with a number of other conditions, which are described in the section the risk factors for testicular cancer. A great deal of research is being done to learn more about the causes.
Researchers are learning how certain changes in a cell’s DNA can cause the cell to become cancerous. DNA is the chemical in each of our cells that makes up our genes. Genes tell our cells how to function. They are packaged in chromosomes, which are long strands of DNA in each cell. Most cells in the body have 2 sets of 23 chromosomes (one set of chromosomes comes from each parent), but each sperm or egg cell has only 23 chromosomes. When the sperm and egg combine, the resulting embryo has a normal number of chromosomes in each cell, half of which are from each parent. We usually look like our parents because they are the source of our DNA. But DNA affects more than how we look.
Some genes control when our cells grow, divide into new cells, and die. Certain genes that help cells grow and divide are called oncogenes. Others that slow down cell division or make cells die at the right time are called tumor suppressor genes. Cancers can be caused by changes in chromosomes that turn on oncogenes or turn off tumor suppressor genes.
Most testicular cancer cells have extra copies of a part of chromosome 12 (called isochromosome 12p or i12p). Some testicular cancers have changes in other chromosomes as well, or even abnormal numbers of chromosomes (often too many). Scientists are studying these DNA and chromosome changes to learn more about which genes are affected and how this might lead to testicular cancer.
Risk factors for testicular cancer
Factors that may increase your risk of testicular cancer include:
- An undescended testicle (cryptorchidism). The testes form in the abdominal area during fetal development and usually descend into the scrotum before birth. Normally, the testicles develop inside the abdomen of the fetus and they go down (descend) into the scrotum before birth. In about 3% of boys, however, the testicles do not make it all the way down before the child is born. Sometimes the testicle remains in the abdomen. In other cases, the testicle starts to descend but remains stuck in the groin area. Men who have a testicle that never descended are at greater risk of testicular cancer than are men whose testicles descended normally. The risk remains elevated even if the testicle has been surgically relocated to the scrotum. Still, the majority of men who develop testicular cancer don’t have a history of undescended testicles. About 1 out of 4 cases of testicular cancer occur in the normally descended testicle. Because of this, some doctors conclude that cryptorchidism doesn’t actually cause testicular cancer but that there is something else that leads to both testicular cancer and abnormal positioning of one or both testicles.
- Abnormal testicle development. Conditions that cause testicles to develop abnormally, such as Klinefelter syndrome, may increase your risk of testicular cancer.
- Family history. If family members especially in a father or brother have had testicular cancer, you may have an increased risk. But only a small number of testicular cancers occur in families. Most men with testicular cancer do not have a family history of the disease.
- Age. Testicular cancer affects teens and younger men, particularly those between ages 15 and 35. However, it can occur at any age, including infants and elderly men.
- Race. Testicular cancer is more common in white men than in black men.
- HIV infection. Some evidence has shown that men infected with the human immunodeficiency virus (HIV), particularly those with AIDS, are at increased risk. No other infections have been shown to increase testicular cancer risk.
- Carcinoma in situ of the testicle. This condition often doesn’t cause a lump in the testicles or any other symptoms. It isn’t clear how often carcinoma in situ (CIS) in the testicles progresses to cancer. In some cases, CIS is found in men who have a testicular biopsy to evaluate infertility or have a testicle removed because of cryptorchidism. Doctors in Europe are more likely than the doctors in this country to look for CIS. This may be why the numbers for diagnosis and progression of CIS to cancer are lower in the United States than in parts of Europe. Since doctors don’t know how often CIS becomes true (invasive) cancer, it isn’t clear if treating CIS is a good idea. Some experts think that it may be better to wait and see if the disease gets worse or becomes a true cancer. This could allow many men with CIS to avoid the risks and side effects of treatment. When CIS is treated, radiation or surgery (to remove the testicle) is used.
- Having had testicular cancer before. A personal history of testicular cancer is another risk factor. About 3% or 4% of men who have been cured of cancer in one testicle will eventually develop cancer in the other testicle.
- Body size. Several studies have found that tall men have a somewhat higher risk of testicular cancer, but some other studies have not. Most studies have not found a link between testicular cancer and body weight.
Unproven or controversial risk factors
Prior injury or trauma to the testicles and recurrent actions such as horseback riding do not appear to be related to the development of testicular cancer.
Most studies have not found that strenuous physical activity increases testicular cancer risk. Being physically active has been linked with a lower risk of several other forms of cancer as well as a lower risk of many other health problems.
Testicular cancer signs and symptoms
If you have any of these signs or symptoms, see your doctor without delay. Many of these symptoms are more likely to be caused by something other than testicular cancer.
Symptoms of testicular cancer
You can’t be sure you have testicular cancer from just symptoms, so it’s important to see a doctor about any testicular symptoms that concern you. Don’t wait.
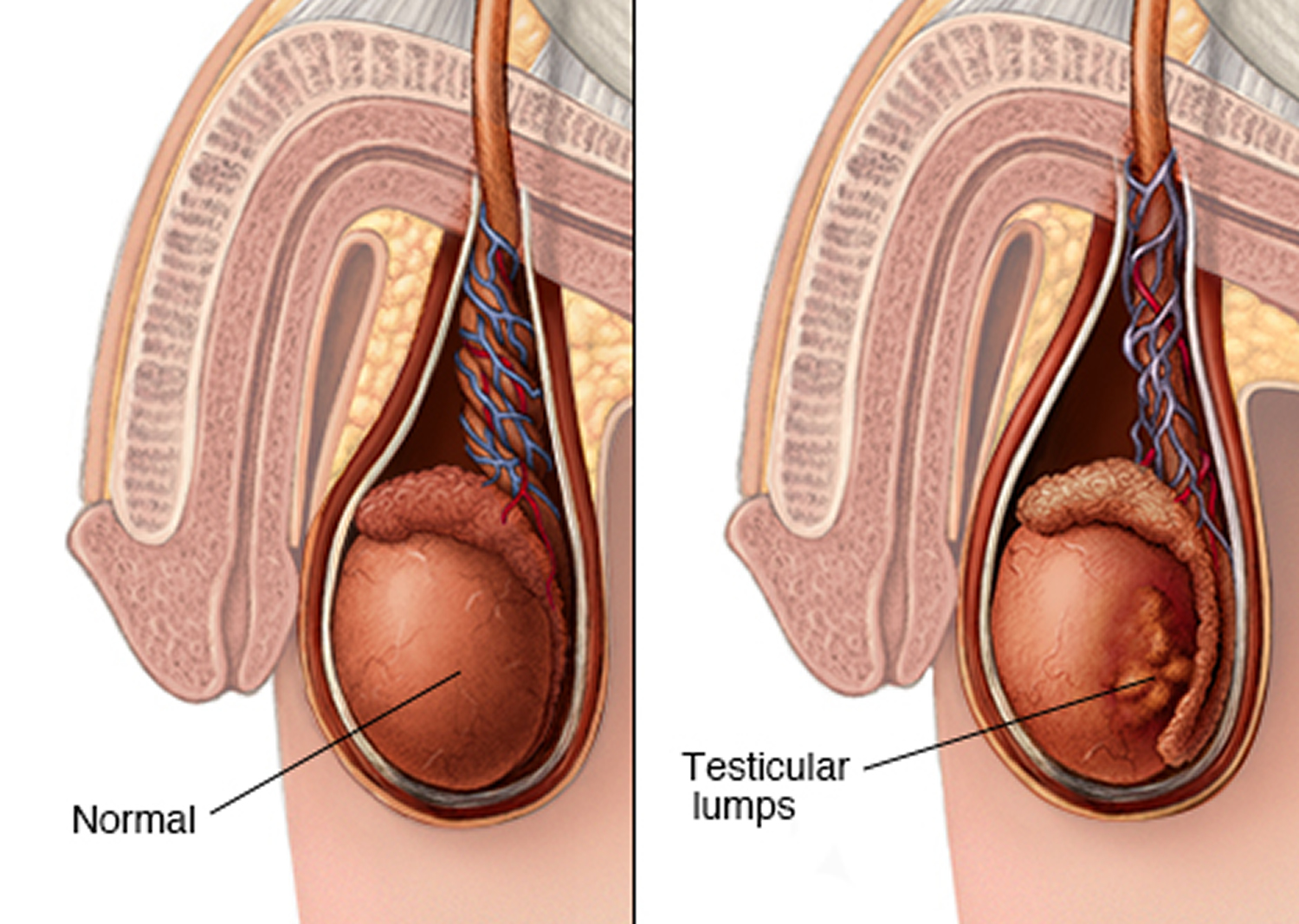
- The most common symptom of testicular cancer is a painless lump on or in a testicle.
- Sometimes the testicle may become swollen or larger, without a lump. (It’s normal for one testicle to be slightly larger than the other, and for one to hang lower than the other.)
- Some testicular tumors might cause pain, but most of the time they don’t. Men with testicular cancer may also have a heavy or aching feeling in the lower belly or scrotum.
- Breast growth or soreness: Rarely, testicular cancers can cause men’s breasts to grow or become sore. This is because certain types of testicular cancer can make high levels of hormones that affect the breasts. Some men might also notice a loss of sexual desire.
- Signs of early puberty in boys: Some testicular cancers make male sex hormones. This may not cause any specific symptoms in men, but in boys it can cause signs of puberty, such as a deepening of the voice and the growth of facial and body hair, at an early age.
Lump or swelling in the testicle
Most often, the first symptom of testicular cancer is a lump on the testicle, or the testicle becomes swollen or larger. It’s normal for one testicle to be slightly larger than the other, and for one to hang lower than the other. Some testicular tumors might cause pain, but most of the time they do not. Men with testicular cancer can also have a feeling of heaviness or aching in the lower abdomen or scrotum.
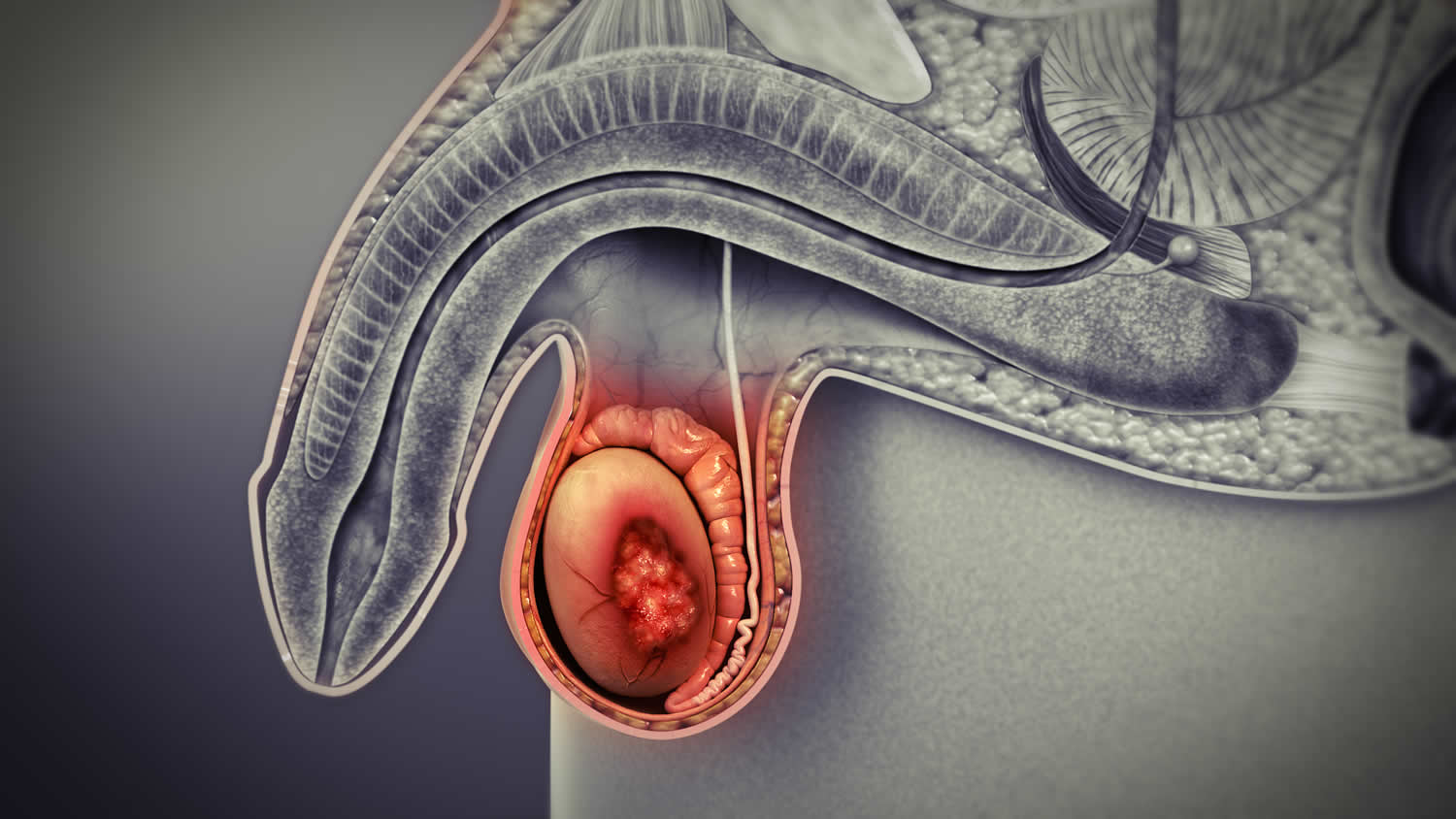
Figure 6. Testicular cancer lump
Note: Pain, swelling or lumps in your testicle or groin area may be a sign or symptom of testicular cancer or other medical conditions requiring treatment.
Breast growth or soreness
In rare cases, germ cell tumors can make breasts grow or become sore. This occurs because certain types of germ cell tumors secrete high levels of a hormone called human chorionic gonadotropin (HCG), which stimulates breast development.
Some Leydig cell tumors can make estrogens (female sex hormones), which can cause breast growth or loss of sexual desire.
Early puberty in boys
Some Leydig cell tumors can make androgens (male sex hormones). Androgen-producing tumors may not cause any specific symptoms in men, but in boys they can cause signs of puberty at an abnormally early age, such as a deepening voice and the growth of facial and body hair.
Symptoms of testicular cancer that has spread
If testicular cancer is not found early, it can spread to other parts of the body. Even when testicular cancer has spread, there may still be no symptoms. But some men might have some of the following:
- Low back pain from cancer that has spread to the lymph nodes in back of the belly. (Lymph nodes are bean-sized collections of immune cells.)
- Shortness of breath, chest pain, or a cough (even coughing up blood) from cancer spread in the lungs.
- Belly pain, either from enlarged lymph nodes, or because the cancer has spread to the liver.
- Headaches or confusion from cancer spread to the brain.
A number of non-cancerous conditions, such as testicle injury or inflammation, can cause symptoms similar to those of testicular cancer. Inflammation of the testicle (known as orchitis) and inflammation of the epididymis (epididymitis) can cause swelling and pain of the testicle. Both of these also can be caused by viral or bacterial infections.
Signs of testicular cancer
Some men with testicular cancer have no symptoms at all, and their cancer is found during medical testing for other conditions. Sometimes imaging tests done to find the cause of infertility can uncover a small testicular cancer.
Non-cancer causes of testicular or scrotal symptoms
Problems other than cancer can also cause symptoms. Because it’s hard to figure out the cause based on symptoms alone, it’s important to have any testicular or scrotal change checked by a doctor.
Some of the conditions that can cause a testicle lump, swelling, and/or pain include:
- Torsion of the testicle
- Injury
- Infection
- Hydrocele
- Varicocele
- Epididymal cyst/spermatocele
- Inguinal hernia
- Kidney stones
Torsion of the testicle
In testicular torsion, one of the testicles gets twisted inside the scrotum. This cuts off the blood supply to the testicle, epididymis, and other structures, leading to sudden, severe pain in the scrotum along with swelling and redness. It can also cause belly pain or nausea and vomiting.
Testicular torsion occurs most often in teen boys, but may occur later in life. It’s often diagnosed using ultrasound of the testicle/scrotum. Torsion is a medical emergency that needs to be treated right away. Surgery is needed to untwist the testicle, which restores the blood supply. If the torsion isn’t treated within several hours, the testicle can die and will have to be removed.
Injury
Physical injury to the scrotum or testicle can cause pain right way, or it may cause slowly worsening pain and swelling later on as the scrotum fills with blood. This is known as a hematocele. Sometimes treatment may be needed to stop the bleeding, but the problem may get better on its own.
A testicular injury can be very painful, but it does not cause cancer.
Infection
Infections in the scrotal area are usually caused by bacteria or viruses.
Epididymitis is inflammation of the epididymis, the coiled tube next to each testicle that stores sperm. This can be caused by a sexually transmitted infection, but it can also be caused by other types of infection.
Epididymitis can cause:
- Pain and swelling on one side of the scrotum. The pain tends to come on slowly, and it may spread to the side or back.
- Pain when passing urine
- Fever
- Milky discharge from the penis
If the infection is caused by bacteria, antibiotics often will make the symptoms go away completely. But if these problems continue after you’ve taken antibiotics, you need to go back to the doctor.
Orchitis happens when the testicle(s) becomes inflamed. It can cause painful swelling in one or both testicles. It also can impair fertility (make it harder to get a woman pregnant).
Orchitis can be caused by bacteria, including those that cause sexually transmitted infections and epididymitis. In fact, epididymitis and orchitis can happen at the same time. The mumps virus can also cause orchitis.
Hydrocele
Sometimes a testicle can feel enlarged because fluid has collected around it. This is called a hydrocele. It’s usually painless unless it grows too large. Sometimes the pain can spread to the lower belly or back. Hydroceles can have many causes. They’re usually harmless and rarely need to be treated. Hydroceles are often diagnosed with an ultrasound exam of the testicle and scrotum.
Varicocele
In varicocele, the veins within the scrotum get very large (dilate). This can cause swelling and lumpiness around the testicle. It has been described as the scrotum feeling like a “bag of worms.” It’s usually painless, but it may cause a feeling of heaviness in the scrotum. Varicoceles can be diagnosed by a physical exam or with an ultrasound exam of the testicle and scrotum. They do not usually need to be treated.
Epididymal cyst/spermatocele
An epididymal cyst may also be called a spermatocele. It’s a fluid-filled sac much like a hydrocele, but the fluid inside contains sperm cells. It’s usually a small, painless lump in the scrotum that’s not connected to the testicle. These cysts are very common, and rarely need to be treated. They are often diagnosed with an ultrasound exam of the testicle and scrotum.
Inguinal hernia
An inguinal hernia is in the groin. These hernias are caused by defects or weak spots in the muscles of the lower belly (the abdominal wall), which allow structures in the belly, such as fatty tissues and/or a loop of intestine, to go into the scrotum. There may be a slight lump or bulge in the groin or scrotum. The lump may be easier to see or feel when standing up. It’s sometimes painful, especially when bending over, lifting something heavy, coughing, or straining to pass urine or have a bowel movement.
Most of the time a hernia isn’t dangerous, but your doctor might recommend surgery to repair it, especially if it causes pain or is getting larger. Surgery can help prevent a problem called strangulation. This is when a part of the intestine gets trapped in the groin, cutting off its blood supply. This causes severe pain, nausea, and vomiting, and needs to be treated right away because it can be life threatening.
Kidney stones
Kidney stones are small crystals that form in the kidneys and can get stuck in the tubes leading to the bladder (the ureters). The stones can cause severe pain, most often in the back or belly. This pain can extend down to the scrotum. Many men also have nausea and vomiting. Blood is often found in the urine, but it might not be seen with the naked eye. Large stones may need to be removed using surgery or other procedures.
Testicular cancer prevention
There’s no way to prevent testicular cancer.
Some doctors recommend regular testicle self-examinations to identify testicular cancer at its earliest stage. But not all doctors agree. Discuss testicular self-examination with your doctor if you’re unsure about whether it’s right for you.
Testicular self-exam
Most doctors agree that checking a man’s testicles should be part of a routine physical exam. And some doctors recommend that all men examine their testicles monthly after puberty.
How to do a testicular self-exam
The best time to do the self-exam is during or after a bath or shower, when the skin of the scrotum is relaxed.
- Hold your penis out of the way and check one testicle at a time.
- Hold the testicle between your thumbs and fingers of both hands and roll it gently between your fingers.
- Look and feel for any hard lumps or smooth rounded bumps or any change in the size, shape, or consistency of the testicles.
It’s normal for one testicle to be slightly larger than the other, and for one to hang lower than the other. You should also know that each normal testicle has a small, coiled tube (epididymis) that can feel like a small bump on the upper or middle outer side of the testicle. Normal testicles also have blood vessels, supporting tissues, and tubes that carry sperm. Some men may confuse these with abnormal lumps at first. If you have any concerns, ask your doctor.
If you check your testicles regularly, in time you will learn what’s normal for you and will be able to tell when something is different.
What if you find something different?
If you find something unusual or something you’re not sure about, either during a self-exam or at any other time, see a doctor right away.
Your doctor will ask if you’re having any symptoms (such as pain) and how long you’ve had them. During a physical exam, your doctor will feel your testicles for swelling or tenderness and for the size and location of any lumps. Your doctor might also examine your abdomen (belly), groin area, and other parts of your body, looking for any possible signs of cancer spread.
If anything abnormal is found, an ultrasound may be done to look at the scrotum and testicles. This is an easy and painless way of finding out whether there’s a tumor or another problem. Other tests might be done as well.
Testicular cancer diagnosis
Testicular cancer is usually found as a result of symptoms that a person is having. It can also be found as a result of tests for another condition. Often the next step is an exam by a doctor.
The doctor will feel the testicles for swelling or tenderness and for the size and location of any lumps. The doctor will also examine your abdomen, lymph nodes, and other parts of your body carefully, looking for any possible signs of cancer spread. Often the results of the exam are normal aside from the testicles. If a lump or other sign of testicular cancer is found, testing is needed to look for the cause.
Ultrasound of the testicles
An ultrasound is often the first test done if the doctor thinks you might have testicular cancer.
This test uses sound waves to produce images of internal organs. A transducer (wand-like instrument) gives off sound waves and picks up the echoes as they bounce off the organs. A computer creates an image on a monitor from the pattern of the echoes.
The pattern of echoes can be used to distinguish certain benign conditions (like hydrocele or varicocele), from a solid tumor that could be a cancer. If the lump is solid, then it’s more likely to be a cancer, so the doctor will recommend further tests or even surgery to remove the testicle.
Ultrasound is an easy test to have and it uses no radiation. You are on your back on a table as the technician moves the transducer along the skin of the scrotum. Usually, the skin is first lubricated with gel.
Blood tests for tumor markers
Some blood tests can help diagnose testicular tumors. Many testicular cancers make high levels of certain proteins called tumor markers, such as alpha-fetoprotein (AFP) and human chorionic gonadotropin (HCG or beta-HCG). When these tumor markers are in the blood, it suggests that there is a testicular tumor.
- Alpha fetoprotein (AFP) is absent in the serum of normal adults but is detectable in patients with nonseminomatous germ cell tumors and hepatocellular carcinoma. Elevation of serum alpha-fetoprotein (AFP) is seen in 40% to 60% of men with nonseminomas. Alpha fetoprotein (AFP) is not elevated in patients with pure seminomas 8. Men who have an elevated serum AFP have a mixed germ cell tumor (i.e., nonseminomatous germ cell tumors [NSGCT]) even if the pathology shows a pure seminoma—unless there is a more persuasive explanation for the elevated AFP, such as liver disease 9.
- Beta human chorionic gonadotropin (β-HCG) is produced by embryonal carcinoma and choriocarcinoma and is the most commonly elevated tumor marker in patients with nonseminomatous germ cell tumors. Beta-hCG is also elevated in 15% to 25% of patients with seminomas 8. Elevation of beta-hCG is found in approximately 14% of patients with stage 1 pure seminomas before orchiectomy and in about one-half of patients with metastatic seminomas 10, 11, 12. Approximately 40% to 60% of men with nonseminomas have an elevated serum beta human chorionic gonadotropin (β-HCG) 9.
- Lactate dehydrogenase (LDH) is a less sensitive and less specific tumor marker than beta-hCG or AFP for men with nonseminomatous germ cell tumors (NSGCTs) but is elevated in 40% to 60% of men with testicular germ cell tumors 8. Seminomas and nonseminomas alike may result in elevated lactate dehydrogenase (LDH) but such values are of unclear prognostic significance because lactate dehydrogenase (LDH) may be elevated in many conditions unrelated to cancer. A study evaluated the use of lactate dehydrogenase (LDH) in 499 patients with a testicular germ cell tumor who were undergoing surveillance after orchiectomy or treatment of stage 2 or 3 disease. It found that 7.7% of patients had elevated lactate dehydrogenase (LDH) unrelated to cancer, while only 1.4% of patients had cancer-related increases in lactate dehydrogenase (LDH) 13. Among 15 patients with relapsed disease, LDH was elevated in six patients and was the first sign of relapse in one patient. Over 9% of the men had a persistent false-positive increase in LDH. The positive predictive value for an elevated LDH was 12.8%. A second study reported that among 494 patients with stage I germ cell tumors who subsequently had a relapse, 125 had an elevated LDH at the time of relapse. Of these 125 patients, all had other evidence of relapse: 112 had a concurrent rise in AFP and/or beta-hCG, one had computed tomography (CT) evidence of relapse before the elevation in LDH, one had palpable disease on examination, and one complained of back pain that led to imaging that revealed retroperitoneal relapse 14. On one hand, measuring LDH appears to have little value for predicting relapse during surveillance of germ cell tumors. On the other hand, for patients with metastatic nonseminomatous germ cell tumors (NSGCTs), large studies of prognostic models have found the LDH level to be a significant independent predictor of survival 15, 16.
Rises in AFP or HCG can also help doctors tell which type of testicular cancer it might be. Non-seminomas often raise alpha-fetoprotein (AFP) and/or human chorionic gonadotropin (HCG) levels. Pure seminomas occasionally raise human chorionic gonadotropin (HCG) levels but never AFP levels, so any increase in AFP means that the tumor has a non-seminoma component. (Tumors can be mixed and have areas of seminoma and non-seminoma.) Sertoli and Leydig cell tumors do not make these substances. Some cancers are too small to elevate levels of these tumor markers.
A testicular tumor might also increase the levels of an enzyme called lactate dehydrogenase (LDH). LDH levels can also be increased in conditions other than cancer. A high LDH level often (but not always) indicates widespread disease.
Tumor marker tests sometimes are also used for other reasons, such as to help estimate how much cancer is present, to follow the patient’s response to treatment, or to look for signs the tumor might have returned.
Significant and unambiguously rising levels of AFP and/or beta-hCG signal relapsed germ cell tumor in most cases and are an indication for treatment even in the absence of radiological evidence of metastatic disease. Nonetheless, tumor marker elevations need to be interpreted with caution. For example, false-positive beta-hCG levels can result from cross reactivity of the assay with luteinizing hormone in which case an intramuscular injection of testosterone should result in normalization of beta-hCG values. There are also clinical reports of marijuana use resulting in elevations of serum beta-hCG and some experts recommend querying patients about drug use and retesting beta-hCG levels after a period of abstinence from marijuana use. Similarly, AFP is chronically mildly elevated in some individuals for unclear reasons and can be substantially elevated by liver disease.
Surgery to diagnose testicular cancer
Most types of cancer are diagnosed by removing a small piece of the tumor and looking at it under a microscope for cancer cells. This is known as a biopsy. But a biopsy is rarely done for a testicular tumor because it might risk spreading the cancer. The doctor can often get a good idea of whether it is testicular cancer based on the ultrasound and blood tumor marker tests, so instead of a biopsy the doctor will very likely recommend surgery to remove the tumor as soon as possible.
The operation to remove a testicular tumor or cancer is called a radical inguinal orchiectomy. In this procedure, the surgeon makes a cut (incision) just above the pubic area and then removes the entire tumor along with the testicle and spermatic cord. The spermatic cord contains part of the vas deferens, as well as blood and lymph vessels that could act as pathways for testicular cancer to spread to the rest of the body. To lessen the chance that cancer cells will spread, these vessels are tied off early in the operation.
The entire specimen is sent to the lab, where a pathologist (a doctor specializing in laboratory diagnosis of diseases) looks at pieces of the tumor under a microscope. If cancer cells are found, the pathologist sends back a report describing the type and extent of the cancer.
In rare cases, when a diagnosis of testicular cancer is uncertain, the doctor may biopsy the testicle before removing it. This is done in the operating room. The surgeon makes a cut above the pubic area, withdraws the testicle from the scrotum, and examines it without cutting the spermatic cord. If a suspicious area is seen, a portion of it is removed and looked at right away by the pathologist. If cancer is found, the testicle and spermatic cord are then removed. If the tissue is not cancerous, the testicle can often be returned to the scrotum, and treatment will be surgery to remove only the tumor or the use of appropriate medicines.
If testicular cancer is found, your doctor will order imaging tests of other parts of your body to check for spread outside the testicle. These tests may also be ordered before the diagnosis is confirmed by surgery.
Abdominal lymph node dissection
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
A surgical procedure in which lymph nodes in your abdomen are removed and a sample of tissue is checked under a microscope for signs of cancer. This procedure is also called lymphadenectomy. For patients with nonseminoma, removing the lymph nodes may help stop the spread of disease. Cancer cells in the lymph nodes of seminoma patients can be treated with radiation therapy.
Imaging tests
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. Ultrasound of the testicles, described above, is a type of imaging test. Other imaging tests may be done for a number of reasons after a testicular cancer diagnosis, including:
- To learn how far cancer might have spread
- To help determine if treatment has been effective
- To look for possible signs of cancer coming back after treatment
Computed tomography (CT) scan
CT scans can be used to help determine the stage (extent) of the cancer by showing if it has spread to the lymph nodes, lungs, liver, or other organs.
The CT scan uses x-rays to produce detailed cross-sectional images of your body. Instead of taking one picture, like a standard x-ray, a CT scanner takes many pictures of the part of your body being studied as it rotates around you. A computer then combines these pictures into an image of a slice of your body. Before the test, you might be asked to drink a contrast solution and/or get an intravenous (IV) injection of a contrast dye that helps better outline structures in the body. You may need an IV line to inject the contrast dye. The injection can cause some flushing (redness and a warm feeling that often lasts seconds). Some people are allergic to the dye and get hives. Rarely, more serious reactions like trouble breathing and low blood pressure can occur. Medicine can be given to prevent and treat allergic reactions. Be sure to tell the doctor if you have any allergies or if you have ever reacted to any contrast material used for x-rays.
A CT scanner has been described as a large donut, with a narrow table that slides in and out of the middle opening. You need to lie still on the table while the scan is being done. CT scans take longer that regular x-rays, and you might feel a bit confined by the ring you have to lie in while the pictures are being taken.
CT guided needle biopsy: CT scans are sometimes used to guide a biopsy needle precisely into a suspected area of cancer spread. For this procedure, you stay on the CT scanning table while a doctor advances a biopsy needle through the skin toward the mass. CT scans are repeated until the doctor can see that the needle is within the mass. A fine needle biopsy sample (tiny fragment of tissue) or a core needle biopsy sample (a thin cylinder of tissue) is then removed and examined under a microscope.
Magnetic resonance imaging (MRI) scan
MRI scans are particularly helpful in looking at the brain and spinal cord. They are only done in patients with testicular cancer if the doctor has reason to think the cancer might have spread to those areas.
Like CT scans, MRI scans provide detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. The energy from the radio waves is absorbed and then released in a pattern formed by the type of body tissue and by certain diseases. A computer translates the pattern into a very detailed image of parts of the body. A contrast material might be injected just as with CT scans. MRI scans take longer than CT scans – often up to an hour – and are a little more uncomfortable. You lie on a table that slides inside a narrow tube, which is confining and can upset people with a fear of enclosed spaces. Special, more open MRI machines can help with this if needed, but the images may not be as sharp in some cases. The MRI machine makes buzzing and clicking noises, so some places will provide earplugs to help block this out.
Positron emission tomography (PET) scan
A PET scan can help spot small collections of cancer cells in the body. It is sometimes useful to see if lymph nodes that are still enlarged after chemotherapy contain cancer or are just scar tissue. PET scans are often more useful for seminomas than for non-seminomas, so they are less often used in patients with non-seminoma.
For this test, a form of radioactive sugar (known as fluorodeoxyglucose or FDG) is injected into a vein (IV). (The amount of radioactivity is very low and will pass out of the body over the next day or so.) Because of the way cancer cells in the body grow rapidly, they often take up and use more of the radioactive sugar. After about an hour, you will be moved onto a table in the PET scanner. You lie on the table for about 30 minutes while a special camera creates a picture of areas of radioactivity in the body. The picture is not finely detailed like a CT or MRI scan, but it can provide helpful information about your whole body.
Many centers have special machines that can do both a PET and CT scan at the same time (PET/CT scan). This lets the doctor compare areas of higher radioactivity on the PET with the more detailed appearance of that area on the CT.
Bone scan
A bone scan can help show if a cancer has spread to the bones. It might be done if there is reason to think the cancer might have spread to the bones (because of symptoms such as bone pain) and if other test results aren’t clear.
For this test, a small amount of low-level radioactive material is injected into a vein (IV). The substance settles in areas of bone changes throughout the entire skeleton over the course of a couple of hours. Then, you lie on a table for about 30 minutes while a special camera detects the radioactivity and creates a picture of your skeleton.
Areas of active bone changes attract the radioactivity and show up as “hot spots.” These areas may suggest metastatic cancer, but arthritis or other bone diseases can also cause the same pattern. To distinguish among these conditions, your cancer care team may use other imaging tests such as plain x-rays or MRI scans to get a better look at the areas that light up, or they may even take biopsy samples of the bone.
Testicular Cancer Stages
After someone is diagnosed with testicular cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Cancer stage is the best predictor of your prognosis (outlook) how likely your cancer is to be cured. Doctors also use a cancer’s stage when talking about survival statistics.
The earliest stage of testicular cancer is stage 0 (zero) also called germ cell neoplasia in situ (GCNIS) 17. The other main stages range from I (1) through III (3). There is no stage IV (4) testicular cancer 17. Some stages are split further, using capital letters (A, B, etc.) 17.
As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage 3 (III), means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
How is the stage determined?
The staging system most often used for testicular cancer is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 4 key pieces of information 17:
- The size and extent of the main tumor (T): How large is the tumor? Has it grown into nearby structures or organs?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes? How large are they, and how many are affected?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant parts of the body? The most common sites of spread for testicular cancer are distant lymph nodes, the bones, the liver, and the lungs.
- The serum (blood) levels of tumor markers (S): Are any tumor marker levels higher than normal? This includes alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG) and lactate dehydrogenase (LDH).
Numbers or letters after T, N, M, and S provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, M, and S categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
The system described below is the most recent AJCC system, effective as of January 2018. It’s used for germ cell tumors (seminomas and non-seminomas) that occur after puberty, and for sex cord stromal tumors (Leydig cell tumors and Sertoli cell tumors) 17.
Testicular cancer might be given a clinical T category (written as cT) based on the results of a physical exam, biopsy, and imaging tests. Once surgery is done, the pathologic T category (written as pT) is determined by examining tissue removed during the operation.
Testicular cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
Table 1. Stages of testicular cancer
| American Joint Committee on Cancer (AJCC) Stage | Stage grouping | Stage description* |
|---|---|---|
| 0 | pTis N0 M0 S0 | The cancer is only in the seminiferous tubules (small tubes inside each testicle). It has not grown into other parts of the testicle (pTis). It hasn’t spread to nearby lymph nodes (N0) or to distant parts of the body (M0). All tumor marker levels are within normal limits (S0). |
| 1 | pT1-pT4 N0 M0 SX | The tumor has grown beyond the seminiferous tubules, and might have grown outside the testicle and into nearby structures (pT1-pT4). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). Tumor marker test results aren’t available, or the tests haven’t been done (SX). |
| 1A | pT1 N0 M0 S0 | The tumor has grown beyond the seminiferous tubules, but is still within the testicle, and it hasn’t grown into nearby blood vessels or lymph nodes (pT1). The cancer hasn’t spread to nearby lymph nodes (N0) or to distant parts of the body (M0). All tumor marker levels are within normal limits (S0). |
| 1B | pT2-pT4 N0 M0 S0 | The tumor has grown outside of the testicle and into nearby structures (pT2-pT4). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). All tumor marker levels are within normal limits (S0). |
| 1S | Any pT (or TX) N0 M0 S1-S3 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer has not spread to nearby lymph nodes (N0) or to distant parts of the body (M0). At least one tumor marker level is higher than normal (S1-S3). |
| 2 | Any pT (or TX) N1-N3 M0 SX | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer has spread to 1 or more nearby lymph nodes (N1-N3), but it hasn’t spread to distant parts of the body (M0). Tumor marker test results aren’t available, or the tests haven’t been done (SX). |
| 2A | Any pT (or TX) N1 M0 S0 or S1 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer has spread to at least 1 nearby lymph node (but no more than 5, if checked by surgery), and none of the lymph nodes are larger than 2 centimeters (cm) across (N1). The cancer has not spread to distant parts of the body (M0). All tumor marker levels are within normal limits (S0), or at least 1 tumor marker level is slightly higher than normal (S1). |
| 2B | Any pT (or TX) N2 M0 S0 or S1 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer has spread to at least 1 nearby lymph node that’s larger than 2 cm but no larger than 5 cm across, OR it has grown outside of a lymph node, OR more than 5 nodes contain cancer (found during surgery) (N2). The cancer has not spread to distant parts of the body (M0). All tumor marker levels are within normal limits (S0), or at least 1 tumor marker level is slightly higher than normal (S1). |
| 2C | Any pT (or TX) N3 M0 S0 or S1 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer has spread to at least 1 nearby lymph node that’s larger than 5 cm across (N3). The cancer has not spread to distant parts of the body (M0). All tumor marker levels are within normal limits (S0), or at least 1 tumor marker level is slightly higher than normal (S1). |
| 3 | Any pT (or TX) Any N M1 SX | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer might or might not have spread to nearby lymph nodes (any N). It has spread to distant parts of the body (M1). Tumor marker test results aren’t available, or the tests haven’t been done (SX). |
| 3A | Any pT (or TX) Any N M1a S0 or S1 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer might or might not have spread to nearby lymph nodes (any N). It has spread to distant lymph nodes or to the lungs (M1a). All tumor marker levels are within normal limits (S0), or at least 1 tumor marker level is slightly higher than normal (S1). |
| 3B | Any pT (or TX) N1-N3 M0 S2 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer has spread to 1 or more nearby lymph nodes (N1-N3), but it hasn’t spread to distant parts of the body (M0). At least 1 tumor marker level is much higher than normal (S2). |
| OR | ||
| Any pT (or TX) Any N M1a S2 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer might or might not have spread to nearby lymph nodes (any N). It has spread to distant lymph nodes or to the lungs (M1a). At least 1 tumor marker level is much higher than normal (S2). | |
| 3C | Any pT (or TX) N1-N3 M0 S3 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer has spread to 1 or more nearby lymph nodes (N1-N3), but it hasn’t spread to distant parts of the body (M0). At least 1 tumor marker level is very high (S3). |
| OR | ||
| Any pT (or TX) Any N M1a S3 | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer might or might not have spread to nearby lymph nodes (any N). It has spread to distant lymph nodes or to the lungs (M1a). At least 1 tumor marker level is very high (S3). | |
| OR | ||
| Any pT (or TX) Any N M1b Any S | The tumor might or might not have grown outside the testicle (any pT), or the extent of the tumor can’t be assessed for some reason (TX). The cancer might or might not have spread to nearby lymph nodes (any N). It has spread to distant parts of the body other than the lymph nodes or to the lungs (M1b). Tumor marker levels might or might not be higher than normal (any S). | |
Footnotes: * The following additional category is not listed on the table above; NX = Nearby lymph nodes cannot be assessed due to lack of information.
[Source 17 ]Stage 0 testicular cancer
In stage 0 (zero) testicular cancer, abnormal cells are found in the tiny tubules where the sperm cells begin to develop. These abnormal cells may become cancer and spread into nearby normal tissue. All tumor marker levels are normal. Stage 0 is also called germ cell neoplasia in situ.
Stage 1 testicular cancer
In stage 1 testicular cancer, cancer has formed. Stage 1 testicular cancer is divided into stages 1A, 1B, and 1S.
- Stage 1A testicular cancer, cancer is found in the testicle, including the rete testis, but has not spread to the blood vessels or lymph vessels in the testicle. All tumor marker levels are normal.
- Stage 1B testicular cancer, cancer:
- is found in the testicle, including the rete testis, and has spread to the blood vessels or lymph vessels in the testicle; or
- has spread into the hilar soft tissue (tissue made of fibers and fat with blood vessels and lymph vessels), the epididymis, or the outer membranes around the testicle; or
- has spread to the spermatic cord; or
- has spread to the scrotum.
- All tumor marker levels are normal.
- Stage 1S testicular cancer, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Tumor marker levels range from slightly above normal to high.
Stage 2 testicular cancer
Stage 2 is divided into stages 2A, 2B, and 2C.
- Stage 2A testicular cancer, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread to 1 to 5 nearby lymph nodes and the lymph nodes are 2 centimeters or smaller. All tumor marker levels are normal or slightly above normal.
- Stage 2B testicular cancer, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread to:
- 1 nearby lymph node and the lymph node is larger than 2 centimeters but not larger than 5 centimeters; or
- more than 5 nearby lymph nodes and the lymph nodes are not larger than 5 centimeters; or
- a nearby lymph node and the cancer has spread outside the lymph node.
- All tumor marker levels are normal or slightly above normal.
- Stage 2C testicular cancer, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread to a nearby lymph node and the lymph node is larger than 5 centimeters. All tumor marker levels are normal or slightly above normal.
Stage 3 testicular cancer
Stage 3 is divided into stages 3A, 3B, and 3C.
- Stage 3A testicular cancer, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer may have spread to one or more nearby lymph nodes. Cancer has spread to distant lymph nodes or to the lungs. All tumor marker levels are normal or slightly above normal.
- Stage 3B testicular cancer, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread:
- to one or more nearby lymph nodes and has not spread to other parts of the body; or
- to one or more nearby lymph nodes. Cancer has spread to distant lymph nodes or to the lungs.
- The level of one or more tumor markers is moderately above normal.
- Stage 3C testicular cancer, cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has spread:
- to one or more nearby lymph nodes and has not spread to other parts of the body; or
- to one or more nearby lymph nodes. Cancer has spread to distant lymph nodes or to the lungs.
- The level of one or more tumor markers is high.
- OR
- Cancer is found anywhere in the testicle and may have spread into the spermatic cord or scrotum. Cancer has not spread to distant lymph nodes or the lung, but has spread to other parts of the body, such as the liver or bone. Tumor marker levels may range from normal to high.
Testicular cancer treatment
After testicular cancer is diagnosed and staged, your cancer care team will discuss treatment options with you. Treatment for testicular cancer is based mainly on the type and stage of the cancer. Among the different stages of germ cell tumors, pure seminomas tend to be treated one way, and non-seminomas and mixed germ cell tumors are treated another way.
Depending on the type and stage of testicular cancer and other factors, treatment options for testicular cancer can include:
- Surgery
- Radiation therapy
- Chemotherapy (chemo)
- High-dose chemotherapy and stem cell transplant
In some cases, more than one of type of treatment might be used.
Your treatment depends on:
- how far your cancer has grown or spread and the level of particular proteins (markers) in your blood (the stage)
- the type of cancer (for example, seminoma or non seminoma)
- the risk of the cancer coming back
- your general health and level of fitness
Factors that might affect the risk of your cancer coming back include:
- whether the cancer has spread into lymph vessels or blood vessels around the cancer – this is called lympho vascular invasion
- whether the cancer has spread into the network of small tubes in your testicle (rete testis)
- the size of your cancer
Your doctor will discuss your risk of the cancer coming back. They usually discuss further treatment you might need, and will explain the benefits and the possible side effects.
Testicular cancer is broadly divided into seminomas and nonseminomas for treatment planning. Seminomatous types of testicular cancer are more sensitive to radiation therapy and chemotherapy and are less prone to distant metastases than nonseminomatous types 9. Nonseminomas may include teratomatous elements, which tend to be resistant to chemotherapy and often require surgery for cure 9. By definition, pure seminomas do not contain elements of teratoma. Therefore, surgery plays a larger role in the management of nonseminomas than in the management of seminomas 9.
You may have different types of doctors on your treatment team, depending on the stage of your cancer and your treatment options. These doctors may include:
- A urologist: a surgeon who specializes in treating diseases of the urinary system and male reproductive system
- A radiation oncologist: a doctor who treats cancer with radiation therapy
- A medical oncologist: a doctor who treats cancer with medicines such as chemotherapy
Many other specialists might be involved in your care as well, including physician assistants, nurse practitioners, nurses, physical therapists, social workers, and other health professionals.
Surgery
Operations used to treat testicular cancer include:
- Surgery to remove your testicle (radical inguinal orchiectomy) is the primary treatment for nearly all stages and types of testicular cancer. To remove your testicle, your surgeon makes an incision in your groin and extracts the entire testicle through the opening. A prosthetic, saline-filled testicle can be inserted if you choose. In cases of early-stage testicular cancer, surgical removal of the testicle may be the only treatment needed.
- Surgery to remove nearby lymph nodes (retroperitoneal lymph node dissection [RPLND]). Testicular cancer can spread to the lymph nodes in the back of your abdomen. These are called the retroperitoneal lymph nodes. You might need to have an operation to remove these lymph nodes. The operation is called a retroperitoneal lymph node dissection (RPLND). This is a large operation. You have the surgery in a specialist center. Retroperitoneal lymph node dissection (RPLND) is performed through an incision in your abdomen. Your surgeon takes care to avoid damaging nerves surrounding the lymph nodes, but in some cases harm to the nerves may be unavoidable. Damaged nerves can cause difficulty with ejaculation, but won’t prevent you from having an erection.
If surgery is your only treatment for testicular cancer, your doctor will recommend a schedule of follow-up appointments. At these appointments — typically every few months for the first few years and then less frequently after that — you’ll undergo blood tests, CT scans and other procedures to check for signs that your cancer has returned.
Sometimes testicular cancer can spread to other parts of your body. For example, testicular cancer can spread to your lungs or brain. You might have surgery to remove the cancer. Your surgeon will give you more information if you need to have this specialized surgery.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. During external radiation therapy, you’re positioned on a table and a large machine moves around you, aiming the energy beams at precise points on your body.
Radiation therapy is a treatment option that’s sometimes used in people who have the seminoma type of testicular cancer. Radiation therapy may be recommended after surgery to remove your testicle.
Side effects may include nausea and fatigue, as well as skin redness and irritation in your abdominal and groin areas. Radiation therapy is also likely to temporarily reduce sperm counts and may impact fertility in some men. Talk to your doctor about your options for preserving your sperm before beginning radiation therapy.
Side effects of radiotherapy for testicular cancer
Side effects tend to start a few days after the radiotherapy begins. They gradually get worse during the treatment. They can continue to get worse after your treatment ends. But they usually begin to improve after 1 or 2 weeks.
Everyone is different and the side effects vary from person to person. You might not have all of the side effects mentioned.
Your doctor and radiographers will let you know what to expect but do let them know if you have any side effects, They can help you manage them.
Feeling tired and generally weak
Tiredness often starts during your treatment and can continue for a few weeks after your treatment has finished. You might also feel weak and lack energy. Some research has shown that taking gentle exercise can give you more energy. It is important to balance exercise with resting.
Sore skin and skin changes
A skin reaction can make your skin red or look darker in darker skinned people. It can also be sore, itchy, or look like sunburn, and it might peel and blister. Skin reactions don’t develop straight away but gradually throughout your course of radiotherapy. Your radiographer looks out for these reactions. But you should also let them know if you feel any soreness. They can let you know what you can use to treat the soreness. Skin reactions usually settle down 2 to 4 weeks after your treatment ends.
Feeling sick or being sick
You usually have radiotherapy to your abdomen if you are having treatment for testicular cancer which can cause sickness. Sickness can usually be well controlled with medicines. Your radiotherapy doctor can prescribe anti sickness tablets for you to take. Some people find that it helps to take an anti sickness tablet about 20 to 60 minutes before having treatment.
Other people find they manage better by taking anti sickness tablets regularly throughout the day. They do this during the course of their treatment. You can discuss which would be best for you with your radiotherapy team.
Diarrhea
You might have diarrhea during or after radiotherapy to your abdomen. You might also have stomach cramps and wind. It is unpleasant to have diarrhea and it can also make you feel weak and tired, so rest if you need to. It is important to let your radiographers and doctors know if you have diarrhea.
There are several things that can help you, such as:
- anti diarrhea drugs, which your healthcare team can give you
- anti spasm medicines from your healthcare team
- drinking plenty – this is important as you can easily get dehydrated
Effects on your fertility
If you have radiotherapy for testicular cancer, you usually have treatment to the lymph nodes in the abdomen. The radiographer directs the beams:
- at an area down the middle of the stomach or abdomen
- sometimes at the groin
A shield protects your testicle from the radiotherapy beams. But there is a small risk that your remaining testicle could get a dose of radiation.
Doctors advise that you use contraception during treatment and for about a year afterwards. Your doctor will give you more information and explain the precautions you should take and how long you need to take them. Your doctor will also speak to you about sperm banking.
Possible late side effects
Some side effects can start years after the end of treatment. For testicular cancer, there is a:
- risk of heart problems
- small increased risk of developing a second cancer
Your radiotherapy doctor will tell you more about this.
Chemotherapy
Chemotherapy treatment uses drugs to kill cancer cells. Chemotherapy drugs travel throughout your body to kill cancer cells that may have migrated from the original tumor.
You usually have a combination of drugs to treat testicular cancer. Or you might have a drug called carboplatin on its own.
U.S. Food and Drug Administration (FDA) Drugs Approved for Testicular Cancer 18:
- Bleomycin Sulfate
- Cisplatin
- Cosmegen (Dactinomycin)
- Dactinomycin
- Etopophos (Etoposide Phosphate)
- Etoposide
- Etoposide Phosphate
- Ifex (Ifosfamide)
- Ifosfamide
- Vinblastine Sulfate
Chemotherapy combination drugs include:
- bleomycin, etoposide and cisplatin (BEP)
- carboplatin, etoposide and bleomycin (JEB)
- cisplatin (Platinol), etoposide and bleomycin (PEB)
- vinblastine sulfate (Velban), ifosfamide and cisplatin (VeIP)
- etoposide (VP-16), ifosfamide and cisplatin (VIP)
- etoposide and cisplatin (EP)
- vinblastine, ifosfamide, cisplatin (VeIP)
- paclitaxel (Taxol), ifosfamide, cisplatin (TIP)
- gemcitabine, ifosfamide and cisplatin (GIP)
Chemotherapy may be your only treatment, or it may be recommended before or after lymph node removal surgery.
You usually have several types of chemotherapy drugs together. You have them into your bloodstream (intravenously). You have treatment through a thin short tube (a cannula) that goes into a vein in your arm each time you have treatment.
You usually have chemotherapy as a course of several cycles of treatment. A cycle of treatment is the time between 1 round of treatment and the start of another. Usually each treatment cycle lasts 3 weeks (21 days).
You have chemotherapy on set days of each cycle.
The number of cycles you have depends on:
- whether your cancer has spread
- where it has spread to
- your tumor marker blood test results
- how well your cancer responds to the drugs
Side effects of chemotherapy depend on the specific drugs being used. Ask your doctor what to expect. Common side effects include fatigue, nausea, hair loss and an increased risk of infection. There are medications and treatments available that reduce some of the side effects of chemotherapy.
Other side effects of chemotherapy for testicular cancer that can start after the end of treatment include:
- heart problems
- developing a second cancer
Chemotherapy may also lead to infertility in some men, which can be permanent in some cases. Talk to your doctor about your options for preserving your sperm before beginning chemotherapy.
High-Dose Chemotherapy and Stem Cell Transplant for Testicular Cancer
In general, testicular cancers respond well to chemotherapy (chemo), but not all cancers are cured. Even though higher doses of chemo might be more effective, they are not given because they could severely damage the bone marrow, which is where new blood cells are formed. This could lead to life-threatening infections, bleeding, and other problems because of low blood cell counts.
A stem cell transplant allows doctors to use higher doses of chemo. Blood-forming stem cells are collected from the bloodstream in the weeks before treatment using a special machine. In the past the stem cells were taken from the bone marrow, but this is done less often now. The stem cells are frozen, and then the patient receives high-doses of chemo.
After the chemo the patient gets his stem cells back again. This is called a transplant, but it doesn’t involve surgery – the cells are infused into a vein much like a blood transfusion. The stem cells settle in the bone marrow and start making new blood cells over the next few weeks.
For testicular cancer, stem cell transplant is most often used to treat cancers that have come back after treatment with chemo. Current studies are exploring whether a stem cell transplant may be valuable in treating some patients with advanced germ cell cancers as part of their first treatment.
A stem cell transplant is a complex treatment that can cause life-threatening side effects because of the high doses of chemotherapy used. Be sure you understand the possible benefits and risks. If the doctors think you might benefit from a transplant, it should be done at a hospital where the staff has experience with the procedure and with managing the recovery phase.
Stem cell transplants often require a long hospital stay and can be very expensive. Even if the transplant is covered by your insurance, your co-pays or other costs could add up to a lot of money. It is important to find out what your insurer will cover before deciding on a transplant to get an idea of what you might have to pay.
Coping and support
Each man comes to terms with his testicular cancer and deals with the ensuing emotions in his own way. You may feel scared and unsure of your future after your diagnosis. While feelings of anxiety may never go away, you can create a plan to help manage your emotions. Try to:
- Learn enough about testicular cancer to feel comfortable making decisions about your care. Write down questions and ask them at your next doctor’s appointment. Ask your doctor or other members of your health care team to recommend reputable sources of further information. Good places to start include the National Cancer Institute 19 and the American Cancer Society 20.
- Take care of yourself. Make healthy choices in your everyday life to prepare for cancer treatment. Eat a healthy diet with a variety of fruits and vegetables.
- Get plenty of rest so that you wake each morning feeling refreshed. Eliminate unnecessary stress so that you can concentrate on getting well. Try to exercise most days of the week. If you smoke, stop. Talk to your doctor about medications and other strategies to help you stop smoking.
- Connect with other cancer survivors. Find other testicular cancer survivors in your community or online. Contact the American Cancer Society for support groups in your area.
- Stay connected with loved ones. Your family and friends are just as concerned for your health as you are. They want to help, so don’t turn down their offers to assist with transportation to appointments or with errands. Close friends and family will listen when you need someone to talk to or provide a distraction when you’re feeling down.
Testicular cancer Treatment Options by Stage
Treatment of Stage 0 (Testicular Intraepithelial Neoplasia)
In this stage, the cancer has not spread outside the testicle, and tumor marker levels like HCG and AFP are not elevated.
If carcinoma in situ (CIS) is diagnosed after surgery removes the testicle, no other treatment is needed. If carcinoma in situ (CIS) is found after a testicular biopsy (such as for fertility problems), the doctor may recommend that it not be treated right away. Instead, it may be watched closely with repeat physical exams, ultrasound of the testicle, and blood tests of tumor marker levels. Treatment may not be needed as long as there are no signs that the CIS is growing or turning into an invasive cancer. If carcinoma in situ (CIS) is treated, it’s typically surgery to remove the testicle or radiation therapy to the testicle.
If tumor marker levels are high, the cancer isn’t really stage 0 – even when only carcinoma in situ (CIS) is found in the testicle and there are no signs of cancer spread. In this case, the treatment used is for stage 1S cancers.
Stage 1 seminomas
These cancers can be cured in nearly all patients. Surgery is done first to remove the testicle and spermatic cord (called a radical inguinal orchiectomy). After surgery, there are often several treatment choices:
- Careful observation (surveillance): If the cancer has not spread beyond the testicle, the plan most experts prefer is close monitoring for up to 10 years. This means getting physical exams and blood tests every 3 to 6 months for the first year, and less often after that. Imaging tests (CT scans and sometimes chest x-rays) are done every 3 months for 6 months, and then once or twice a year. If these tests do not find any signs that cancer has spread beyond the testicle, no other treatment is needed. If the cancer has spread, treatments like radiation or chemo may be used. The cancer will come back in about 15% to 20% of patients, most often as spread to lymph nodes, but if it does, radiation or chemo can still usually cure the cancer.
- Radiation therapy: Radiation aimed at para-aortic lymph nodes is another option. These nodes are in the back of the abdomen (belly), around the large blood vessel called the aorta. Because seminoma cells are very sensitive to radiation, low doses can be used. About 10 to 15 treatments are given over 2 to 3 weeks.
- Chemotherapy: An option that works as well as radiation is 1 or 2 cycles of chemo with the drug carboplatin after surgery. Many experts prefer chemo over radiation because it seems to be easier to tolerate.
Stage 1S seminomas
In this stage, one or more tumor marker levels is still high after the testicle containing the seminoma has been removed. This is very rare, and it can be treated with chemotherapy.
Stage 2A seminomas
- Radiation: After surgery to remove the testicle (radical inguinal orchiectomy), one treatment option is radiation to the retroperitoneal lymph nodes. These are the lymph nodes at the back of the abdomen (belly). Usually stage 2 seminomas are given higher doses of radiation than stage 1 seminomas.
- Chemotherapy: Another option is chemo, with either 4 cycles of EP (etoposide and cisplatin) or 3 cycles of BEP (bleomycin, etoposide, and cisplatin). The doctor will then watch closely (every 3 to 6 months) for any signs that the cancer has come back.
Stage 2B seminomas
These seminomas have spread to cause larger lymph nodes or have spread to many different lymph nodes.
- Chemotherapy: This is typically the preferred treatment. It is usually either 4 cycles of EP (etoposide and cisplatin) or 3 cycles of BEP (bleomycin, etoposide, and cisplatin).
- Radiation: This may be an option instead of chemo if the lymph nodes aren’t enlarged from cancer spread.
Stage 2C seminomas
Treatment is typically chemotherapy with 4 cycles of EP (etoposide and cisplatin) or 3 or 4 cycles of BEP (bleomycin, etoposide, and cisplatin). Another option might be VIP (etoposide, ifosfamide, and cisplatin) for 4 cycles. Radiation therapy is generally not used for stage 2C seminoma.
Treatment of Stage 0 (Testicular Intraepithelial Neoplasia)
Stage 1 non-seminomas
Nearly all of these cancers can be cured, but the treatment is different from that of seminomas. As with seminomas, the initial treatment is surgery to remove the testicle and tumor called radical inguinal orchiectomy. The other treatment choices will depend on the stage.
Choices for stage 1A (T1)
- Careful observation (surveillance): Surveillance is preferred by most experts, but it requires a lot of doctor visits and tests. A typical schedule might include visits every 2 months for the first year, with CT scans every 4 to 6 months; then every 3 months for the second year, with scans every 6 to 12 months. As time goes on and you have no problems, the time between visits and tests gets longer. If the cancer does come back (relapse), it’s usually within the first year or two. Relapses are generally treated with chemo. Even though more patients will have a relapse with surveillance than with lymph node dissection, the cure rates are much the same because the relapses are usually found early.
- Retroperitoneal lymph node dissection (RPLND): Having the lymph nodes at the back of the abdomen (belly) removed has the advantage of a high initial cure rate, but the disadvantages of major surgery with its possible complications, including losing the ability to ejaculate normally. After retroperitoneal lymph node dissection (RPLND), if cancer is found in the nodes, chemo may be recommended.
- Chemotherapy: Instead of surgery, the doctor may suggest 1 cycle of the BEP regimen (bleomycin, etoposide, and cisplatin). This helps reduce the risk of relapse.
Choices for stage 1B (T2, T3, or T4)
- Retroperitoneal lymph node dissection (RPLND): This is surgery to remove the lymph nodes at the back of the abdomen (belly). If cancer is found in the lymph nodes, chemo is often recommended depending on the number of nodes with cancer in them.
- Chemotherapy: Instead of surgery, the doctor may recommend 1 cycle of the BEP regimen (bleomycin, etoposide, and cisplatin). This can help reduce the risk that the cancer will come back. If cancer was found in the lymph nodes after surgery, 2 to 4 cycles of BEP or EP (etoposide and cisplatin) may be given, depending on how many nodes had cancer in them. This has a high cure rate, but it can have side effects (which are mostly short-term).
- Careful observation (surveillance): This requires frequent doctor visits and tests for several years. This may be an option for some T2 tumors that haven’t reached blood vessels.
Stage 1S non-seminoma
If your tumor marker levels (like AFP or HCG) are still high even after the cancer has been removed, but the CT scan doesn’t show a tumor, chemo is typically recommended. This may be either 3 cycles of BEP (bleomycin, etoposide, and cisplatin) or 4 cycles of EP (etoposide and cisplatin).
Stage 2 non-seminomas
Surgery is done first to remove the testicle and spermatic cord (called a radical inguinal orchiectomy). After surgery, treatment choices depend on the details of the cancer.
Stage 2A non-seminomas
Treatment depends on tumor marker levels after surgery and the extent of spread to the retroperitoneal lymph nodes. These are the lymph nodes at the back of the abdomen (belly).
If tumor marker levels are normal, there are 2 main options:
- Retroperitoneal lymph node dissection (RPLND): This is surgery to remove the lymph nodes at the back of the abdomen. If the lymph nodes that were removed contain cancer, chemo (typically for 2 cycles) might be given. If there’s no cancer in the nodes, the doctor will watch closely for signs that the cancer has come back.
- Chemotherapy: This would include either 4 cycles of EP (etoposide and cisplatin) or 3 cycles of BEP (bleomycin, etoposide, and cisplatin). Surgery might be done after this if there are signs there might still be cancer present.
If tumor markers are still higher than normal after the initial surgery, treatment is typically with chemo as listed above (EP or BEP)..
Stage 2B non-seminomas
Treatment depends on tumor marker levels after surgery and the extent of spread to the lymph nodes at the back of the abdomen (belly). These are called the retroperitoneal lymph nodes.
If tumor marker levels are normal, the options are:
- Chemotherapy: Either 4 cycles of EP (etoposide and cisplatin) or 3 cycles of BEP (bleomycin, etoposide, and cisplatin) may be used. Surgery may then be done to take out all enlarged nodes if the tumor marker return to normal.
- Retroperitoneal lymph node dissection (RPLND): In few select cases, where the cancer has spread only to these lymph nodes, surgery may be done to take them out. Chemo may then be given after surgery.
If tumor markers are still higher than normal after the initial surgery, treatment is typically with chemo as listed above (EP or BEP).
Stage 3 seminomas and non-seminomas
Even though stage 3 cancers have spread by the time they are found, most of them can still be cured.
Both stage 3 seminomas and non-seminomas are treated with radical inguinal orchiectomy, followed by chemo. Depending on the risk group the cancer falls into, this might be with:
- EP (etoposide and cisplatin) for 4 cycles
- BEP (bleomycin, etoposide, and cisplatin) for 3 or 4 cycles
- VIP (etoposide, ifosfamide, and cisplatin) for 4 cycles
If there’s a high suspicion that the cancer might be a testicular choriocarcinoma, chemo may be started without a biopsy or surgery to remove the testicle.
If the cancer has spread to the brain, surgery (if there are only 1 or 2 tumors in the brain), radiation therapy aimed at the brain, or both may also be used. If the tumors in the brain are not bleeding or causing symptoms, some doctors may choose to start the chemo first.
Once chemo is complete, the doctor looks for any cancer that’s left. If scans and tumor marker levels are normal, no further treatment may be needed.
Sometimes a few tumors might be left after treatment. These are most often in the lung or in the retroperitoneal lymph nodes. Further treatment at this point depends on the type of cancer:
- Stage 3 seminoma that’s still there after chemo or doesn’t “light up” on a PET scan, will be watched with CT scans to see if it grows. If it does, more treatment is needed. If the tumors do light up on a PET scan, they could be cancer, and treatment is needed. Treatment may be surgery (such as a retroperitoneal lymph node dissection) or chemo (using a different combination of drugs).
- Stage 3 non-seminoma tumor that remains after treatment is usually removed surgically, which may result in a cure. If cancer is found in the tumors removed, you might need more chemo, maybe with different drugs. After this, surgery might be done to take out any tumors that remain.
If the cancer is resistant to chemo or has spread to many organs, the usual doses of chemo may not always be enough. The doctor might recommend high-dose chemo followed by a stem cell transplant. Enrolling in a clinical trial of a newer chemo regimen might be another good option.
Recurrent testicular cancer
If the cancer goes away with treatment and then comes back, it’s said to have recurred or relapsed. Testicular cancer can recur (come back) after it has been treated. The cancer may come back many years after the initial cancer, in the other testicle or in other parts of the body. If this happens, it’s usually within the first 2 years after treatment. In general, if the cancer recurs, it’s probably best to get a second opinion from a center with extensive experience in treating relapsed testicular cancer before starting treatment.
Treatment of recurrent germ cell tumors depends on the initial treatment and where the cancer recurs. Cancer that comes back in the retroperitoneal lymph nodes can be treated by surgery to remove the nodes (RPLND) if the recurrence is small and if the only surgical treatment given before was orchiectomy. Depending on the results of the surgery, chemo may be recommended as well.
If it looks as if cancer has recurred in a lot of the retroperitoneal lymph nodes or if the cancer has returned elsewhere, chemo is usually recommended. This may be followed by surgery.
If a man’s cancer recurs after chemo or if treatment is no longer working, he will be treated with different chemo, which typically includes ifosfamide, cisplatin, and either etoposide, paclitaxel, or vinblastine.
The treatment of testicular cancer that has come back after chemo is not always as effective as doctors would like, so some doctors may advise high-dose chemo followed by a stem cell transplant. This may be a better option for some men with recurrent disease, rather than standard chemo. Clinical trials of newer treatments may also be good options.
Sertoli cell and Leydig cell tumors
Typically, radical inguinal orchiectomy is the treatment for Sertoli cell and Leydig cell tumors. Radiation therapy and chemo generally don’t work for these rare types of testicular tumors. If the doctor suspects the tumor has spread beyond the testicle, the retroperitoneal lymph nodes may be surgically removed.
Testicular cancer prognosis
An international germ cell tumor prognostic (IGCC) classification has been developed based on a retrospective analysis of 5,202 patients with metastatic nonseminomatous and 660 patients with metastatic seminomatous germ cell tumors 15. All patients received treatment with cisplatin- or carboplatin-containing therapy as their first chemotherapy course. The prognostic classification, shown below, was agreed on in 1997 by all major clinical trial groups worldwide 15. It is used for reporting clinical trial results of patients with germ cell tumors.
A meta-analysis of treatment outcomes for patients with advanced nonseminoma suggested that 5-year survival rates have improved for those patients with a poor prognosis during the period of 1989 to 2004 16. In addition to improved therapy, the improvement in survival rates could be the result of publication bias, changes in patient selection in reported clinical trials, or more sensitive staging methods that could migrate less-advanced stages to more-advanced stage categories (i.e., stage migration).
Good Prognosis
Nonseminoma
- Testis/retroperitoneal primary, and
- No nonpulmonary visceral metastases, and
- Good markers–all of:
- Alpha-fetoprotein (AFP) less than 1,000 ng/mL, and
- Beta-human chorionic gonadotropin (beta-hCG) less than 5,000 IU/mL (1,000 ng/mL), and
- Lactate dehydrogenase (LDH) less than 1.5 × the upper limit of normal
A total of 56% to 61% of nonseminomas are good prognosis. The 5-year progression-free survival rate is 89%; the 5-year survival rate is 92%–94%.
Seminoma
- Any primary site, and
- No nonpulmonary visceral metastases, and
- Normal alpha-fetoprotein (AFP), any beta-human chorionic gonadotropin (beta-hCG), any lactate dehydrogenase (LDH)
A total of 90% of seminomas are good prognosis. The 5-year progression-free survival rate is 82%; the 5-year survival rate is 86%.
Intermediate Prognosis
Nonseminoma
- Testis/retroperitoneal primary, and
- No nonpulmonary visceral metastases, and
- Intermediate markers–any of:
- Alpha-fetoprotein (AFP) 1,000 ng/mL or more and 10,000 ng/mL or less, or
- Beta-human chorionic gonadotropin (beta-hCG) 5,000 IU/L or more and 50,000 IU/L or less, or
- Lactate dehydrogenase (LDH) 1.5 or more × N* and less than 10 × N*
- *[Note: N indicates the upper limit of normal for the LDH assay.]
A total of 13% to 28% of nonseminomas are intermediate prognosis. The 5-year progression-free survival rate is 75%; the 5-year survival rate is 80%–83%.
Seminoma
- Any primary site, and
- Nonpulmonary visceral metastases, and
- Normal alpha-fetoprotein (AFP), any
- beta-human chorionic gonadotropin (beta-hCG), any lactate dehydrogenase (LDH)
A total of 10% of seminomas are intermediate prognosis. The 5-year progression-free survival rate is 67%; the 5-year survival rate is 72%.
Poor Prognosis
Nonseminoma
- Mediastinal primary, or
- Nonpulmonary visceral metastases, or
- For markers–any of:
- Alpha-fetoprotein (AFP) more than 10,000 ng/mL, or
- Beta-human chorionic gonadotropin (beta-hCG) more than 50,000 IU/mL (10,000 ng/mL), or
- Lactate dehydrogenase (LDH) more than 10 × the upper limit of normal
A total of 16% to 26% of nonseminomas are poor prognosis. The 5-year progression-free survival rate rate is 41%; the 5-year survival rate is 71%.
Seminoma
There is no poor prognosis grouping for seminoma testicular tumors. Seminoma is one of the treatable and curable cancers, with a survival rate above 95% if discovered in early stages 21, 22, 23, 24.
- Gaddam SJ, Bicer F, Chesnut GT. Testicular Cancer. [Updated 2023 May 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563159[↩]
- PDQ Adult Treatment Editorial Board. Testicular Cancer Treatment (PDQ®): Health Professional Version. 2024 Mar 15. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK65777[↩]
- PDQ Adult Treatment Editorial Board. Testicular Cancer Treatment (PDQ®): Patient Version. 2023 May 17. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK65847[↩]
- Rajpert-De Meyts E, Aksglaede L, Bandak M, et al. Testicular Cancer: Pathogenesis, Diagnosis and Management with Focus on Endocrine Aspects. [Updated 2023 Mar 29]. In: Feingold KR, Ahmed SF, Anawalt B, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278992[↩]
- Key Statistics for Testicular Cancer. https://www.cancer.org/cancer/types/testicular-cancer/about/key-statistics.html[↩][↩][↩]
- Do I Have Testicular Cancer? https://www.cancer.org/cancer/testicular-cancer/do-i-have-testicular-cancer.html[↩]
- Testicular Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/testis.html[↩][↩]
- Gilligan TD, Seidenfeld J, Basch EM, Einhorn LH, Fancher T, Smith DC, Stephenson AJ, Vaughn DJ, Cosby R, Hayes DF; American Society of Clinical Oncology. American Society of Clinical Oncology Clinical Practice Guideline on uses of serum tumor markers in adult males with germ cell tumors. J Clin Oncol. 2010 Jul 10;28(20):3388-404. doi: 10.1200/JCO.2009.26.4481[↩][↩][↩]
- Testicular Cancer Treatment (PDQ®)–Health Professional Version. https://www.cancer.gov/types/testicular/hp/testicular-treatment-pdq[↩][↩][↩][↩][↩]
- Gholam D, Fizazi K, Terrier-Lacombe MJ, Jan P, Culine S, Theodore C. Advanced seminoma–treatment results and prognostic factors for survival after first-line, cisplatin-based chemotherapy and for patients with recurrent disease: a single-institution experience in 145 patients. Cancer. 2003 Aug 15;98(4):745-52. doi: 10.1002/cncr.11574[↩]
- Oliver RT, Mason MD, Mead GM, von der Maase H, Rustin GJ, Joffe JK, de Wit R, Aass N, Graham JD, Coleman R, Kirk SJ, Stenning SP; MRC TE19 collaborators and the EORTC 30982 collaborators. Radiotherapy versus single-dose carboplatin in adjuvant treatment of stage I seminoma: a randomised trial. Lancet. 2005 Jul 23-29;366(9482):293-300. doi: 10.1016/S0140-6736(05)66984-X[↩]
- Weissbach L, Bussar-Maatz R, Mann K. The value of tumor markers in testicular seminomas. Results of a prospective multicenter study. Eur Urol. 1997;32(1):16-22.[↩]
- Venkitaraman R, Johnson B, Huddart RA, Parker CC, Horwich A, Dearnaley DP. The utility of lactate dehydrogenase in the follow-up of testicular germ cell tumours. BJU Int. 2007 Jul;100(1):30-2. doi: 10.1111/j.1464-410X.2007.06905.x [↩]
- Ackers C, Rustin GJ. Lactate dehydrogenase is not a useful marker for relapse in patients on surveillance for stage I germ cell tumours. Br J Cancer. 2006 May 8;94(9):1231-2. doi: 10.1038/sj.bjc.6603087[↩]
- International Germ Cell Consensus Classification: a prognostic factor-based staging system for metastatic germ cell cancers. International Germ Cell Cancer Collaborative Group. J Clin Oncol. 1997 Feb;15(2):594-603. doi: 10.1200/JCO.1997.15.2.594[↩][↩][↩]
- van Dijk MR, Steyerberg EW, Habbema JD. Survival of non-seminomatous germ cell cancer patients according to the IGCC classification: An update based on meta-analysis. Eur J Cancer. 2006 May;42(7):820-6. doi: 10.1016/j.ejca.2005.08.043[↩][↩]
- Testicular Cancer Stages. https://www.cancer.org/cancer/types/testicular-cancer/detection-diagnosis-staging/staging.html[↩][↩][↩][↩][↩][↩]
- Drugs Approved for Testicular Cancer. https://www.cancer.gov/about-cancer/treatment/drugs/testicular[↩]
- National Cancer Institute. https://www.cancer.gov/[↩]
- American Cancer Society. https://www.cancer.org[↩]
- Bokemeyer C, Nichols CR, Droz JP, Schmoll HJ, Horwich A, Gerl A, Fossa SD, Beyer J, Pont J, Kanz L, Einhorn L, Hartmann JT. Extragonadal germ cell tumors of the mediastinum and retroperitoneum: results from an international analysis. J Clin Oncol. 2002 Apr 1;20(7):1864-73. doi: 10.1200/JCO.2002.07.062[↩]
- Dieckmann KP, Richter-Simonsen H, Kulejewski M, Ikogho R, Zecha H, Anheuser P, Pichlmeier U, Isbarn H. Testicular Germ-Cell Tumours: A Descriptive Analysis of Clinical Characteristics at First Presentation. Urol Int. 2018;100(4):409-419. doi: 10.1159/000488284[↩]
- Chung P, Warde P. Testicular cancer: seminoma. BMJ Clin Evid. 2011 Jan 25;2011:1807. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217763/[↩]
- Fung C, Dinh PC, Fossa SD, Travis LB. Testicular Cancer Survivorship. J Natl Compr Canc Netw. 2019 Dec;17(12):1557-1568. doi: 10.6004/jnccn.2019.7369[↩]