Contents
- What is thyroid cancer
- Thyroid gland
- Benign thyroid enlargement and nodules
- Types of thyroid cancer
- How common is thyroid cancer?
- Thyroid cancer causes
- Thyroid cancer prevention
- Thyroid cancer signs and symptoms
- Thyroid cancer diagnosis
- Thyroid cancer stages
- Thyroid cancer survival rate
- Thyroid cancer treatment
- Surgery
- Radioactive Iodine (Radioiodine) Therapy for Thyroid Cancer
- Thyroid Hormone Therapy
- External Beam Radiation Therapy for Thyroid Cancer
- Injecting alcohol into thyroid cancers
- Targeted Therapy for Thyroid Cancer
- Treatment of Thyroid Cancer, by Type and Stage
- Follicular and Hürthle cell cancers
- Medullary thyroid carcinoma
- Anaplastic carcinoma
- If Thyroid Cancer Treatments Are No Longer Working
What is thyroid cancer
Thyroid cancer occurs in the cells of the thyroid gland — a butterfly-shaped gland located at the base of your neck, just below your Adam’s apple. Your thyroid produces hormones that regulate your heart rate, blood pressure, body temperature and weight.
Although thyroid cancer isn’t common in the United States, rates seem to be increasing. Doctors think this is because new technology is allowing them to find small thyroid cancers that may not have been found in the past.
Most cases of thyroid cancer can be cured with treatment. But advanced cancers can be hard to treat, especially if they do not respond to radioactive iodine therapy. Doctors and researchers are looking for new ways to treat thyroid cancer that are more effective and lead to fewer side effects.
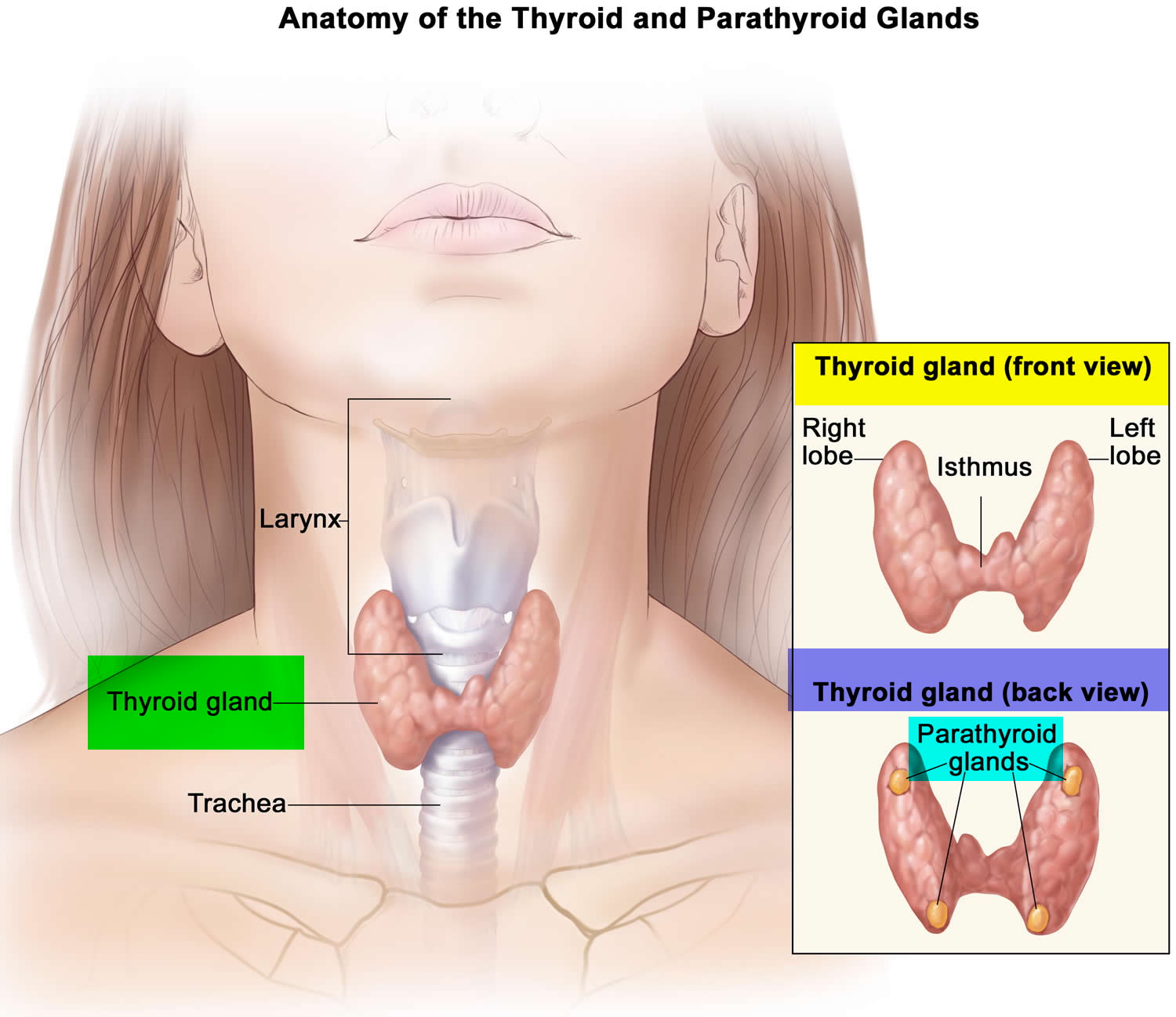
Thyroid gland
The thyroid gland has 2 main types of cells:
- Follicular cells use iodine from the blood to make thyroid hormones, which help regulate a person’s metabolism. Having too much thyroid hormone (a condition called hyperthyroidism) can cause a rapid or irregular heartbeat, trouble sleeping, nervousness, hunger, weight loss, and a feeling of being too warm. Having too little hormone (called hypothyroidism) causes a person to slow down, feel tired, and gain weight. The amount of thyroid hormone released by the thyroid is regulated by the pituitary gland at the base of the brain, which makes a substance called thyroid-stimulating hormone (TSH).
- C cells (also called parafollicular cells) make calcitonin, a hormone that helps control how the body uses calcium.
Other, less common cells in the thyroid gland include immune system cells (lymphocytes) and supportive (stromal) cells.
Different cancers develop from each kind of cell. The differences are important because they affect how serious the cancer is and what type of treatment is needed.
Many types of growths and tumors can develop in the thyroid gland. Most of these are benign (non-cancerous) but others are malignant (cancerous), which means they can spread into nearby tissues and to other parts of the body.
Formation, Storage, and Release of Thyroid Hormones
The thyroid gland is the only endocrine gland that stores its secretory product in large quantities—normally about a 100-day supply. Synthesis and secretion of triiodothyronine (T3) and tetraiodothyronine (T4) occurs as follows:
- Iodide trapping. Thyroid follicular cells trap iodide ions (I −) by actively transporting them from the blood into the cytosol. As a result, the thyroid gland normally contains most of the iodide in the body.
- Synthesis of thyroglobulin. While the follicular cells are trapping I −, they are also synthesizing thyroglobulin (TGB), a large glycoprotein that is produced in the rough endoplasmic reticulum, modified in the Golgi complex, and packaged into secretory vesicles. The vesicles then undergo exocytosis, which releases thyroglobulin into the lumen of the follicle.
- Oxidation of iodide. Some of the amino acids in thyroglobulin are tyrosines that will become iodinated. However, negatively charged iodide (I −) ions cannot bind to tyrosine until they undergo oxidation (removal of electrons) to iodine: I −→ I. As the iodide ions are being oxidized, they pass through the membrane into the lumen of the follicle.
- Iodination of tyrosine. As iodine atoms (I) form, they react with tyrosines that are part of thyroglobulin molecules. Binding of one iodine atom yields monoiodotyrosine (T1), and a second iodination produces diiodotyrosine (T2). The thyroglobulin with attached iodine atoms, a sticky material that accumulates and is stored in the lumen of the thyroid follicle, is termed colloid.
- Coupling of monoiodotyrosine (T1) and diiodotyrosine (T2). During the last step in the synthesis of thyroid hormone, two diiodotyrosine (T2) molecules join to form tetraiodothyronine (T4) or one T1 and one T2 join to form triiodothyronine (T3).
- Pinocytosis and digestion of colloid. Droplets of colloid reenter follicular cells by pinocytosis and merge with lysosomes. Digestive enzymes in the lysosomes break down thyroglobulin, cleaving off molecules of T3 and T4.
- Secretion of thyroid hormones. Because T3 and T4 are lipid soluble, they diffuse through the plasma membrane into interstitial fluid and then into the blood. T4 normally is secreted in greater quantity than T3, but T3 is several times more potent. Moreover, after T4 enters a body cell, most of it is converted to T3 by removal of one iodine.
- Transport in the blood. More than 99% of both the T3 and the T4 combine with transport proteins in the blood, mainly thyroxine binding globulin (TBG).
Figure 1. Thyroid gland location
Benign thyroid enlargement and nodules
Changes in the thyroid gland’s size and shape can often be felt or even seen by patients or by their doctor.
The medical term for an abnormally large thyroid gland is goiter. Some goiters are diffuse, meaning that the whole gland is large. Other goiters are nodular, meaning that the gland is large and has one or more nodules (bumps) in it. There are many reasons the thyroid gland might be larger than usual, and most of the time it is not cancer. Both diffuse and nodular goiters are usually caused by an imbalance in certain hormones. For example, not getting enough iodine in the diet can cause changes in hormone levels and lead to a goiter.
Lumps or bumps in the thyroid gland are called thyroid nodules. Most thyroid nodules are benign, but about 2 or 3 in 20 are cancerous. Sometimes these nodules make too much thyroid hormone and cause hyperthyroidism. Nodules that produce increased thyroid hormone are almost always benign.
People can develop thyroid nodules at any age, but they occur most commonly in older adults. Fewer than 1 in 10 adults have thyroid nodules that can be felt by a doctor. But when the thyroid is looked at with ultrasound, many more people are found to have nodules that are too small to feel. Most evidence suggests that they are benign.
Most nodules are cysts filled with fluid or with a stored form of thyroid hormone called colloid. Solid nodules have little fluid or colloid. These nodules are more likely to be cancerous than are fluid-filled nodules. Still, most solid nodules are not cancer. Some types of solid nodules, such as hyperplastic nodules and adenomas, have too many cells, but the cells are not cancer cells.
Benign thyroid nodules sometimes can be left alone (not treated) as long as they’re not growing or causing symptoms. Others may require some form of treatment.
Types of thyroid cancer
The main types of thyroid cancer are:
- Differentiated (including papillary, follicular and Hṻrthle cell)
- Medullary thyroid cancer
- Anaplastic (an aggressive undifferentiated tumor)
Differentiated thyroid cancers
Most thyroid cancers are differentiated cancers. The cells in these cancers look a lot like normal thyroid tissue when seen with a microscope. These cancers develop from thyroid follicular cells. These are described below.
Papillary thyroid cancer
About 8 out of 10 thyroid cancers are papillary cancers (also called papillary carcinomas or papillary adenocarcinomas). Papillary cancers tend to grow very slowly and usually develop in only one lobe of the thyroid gland. Even though they grow slowly, papillary cancers often spread to the lymph nodes in the neck. Still, these cancers that have spread to the lymph nodes can often be treated successfully and are rarely fatal. Papillary thyroid cancer can occur at any age, but most often it affects people ages 30 to 50.
There are several subtypes of papillary cancers. Of these, the follicular subtype (also called mixed papillary-follicular variant) occurs most often. The usual form of papillary cancer and the follicular subtype have the same good outlook (prognosis) when found early, and they are treated the same way. Other subtypes of papillary carcinoma (columnar, tall cell, insular, and diffuse sclerosing) are not as common and tend to grow and spread more quickly.
Follicular thyroid cancer
Follicular cancer, also called follicular carcinoma or follicular adenocarcinoma, is the next most common type, making up about 1 out of 10 thyroid cancers. It is more common in countries where people don’t get enough iodine in their diet. These cancers usually do not spread to lymph nodes, but they can spread to other parts of the body, such as the lungs or bones. The outlook (prognosis) for follicular cancer is not quite as good as that of papillary cancer, although it is still very good in most cases.
Hṻrthle (Hurthle) cell thyroid cancer
This type is also known as oxyphil cell carcinoma. About 3% of thyroid cancers are this type. It is harder to find and to treat.
Medullary thyroid cancer
Medullary thyroid cancer accounts for about 4% of thyroid cancers. It develops from the C cells of the thyroid gland, which normally make calcitonin, a hormone that helps control the amount of calcium in blood. Sometimes this cancer can spread to lymph nodes, the lungs, or liver even before a thyroid nodule is discovered.
This type of thyroid cancer is more difficult to find and treat, There are 2 types of medullary thyroid cancer:
- Sporadic medullary thyroid cancer, which accounts for about 8 out of 10 cases of medullary thyroid cancer, is not inherited (meaning it does not run in families). It occurs mostly in older adults and affects only one thyroid lobe.
- Familial medullary thyroid cancer is inherited and 20% to 25% can occur in each generation of a family. These cancers often develop during childhood or early adulthood and can spread early. Patients usually have cancer in several areas of both lobes. Familial MTC is often linked with an increased risk of other types of tumors. This is described in more detail in Thyroid Cancer Risk Factors.
Anaplastic (undifferentiated) thyroid cancer
Anaplastic carcinoma (also called undifferentiated carcinoma) is a rare form of thyroid cancer, making up about 2% of all thyroid cancers. It is thought to sometimes develop from an existing papillary or follicular cancer. This cancer is called undifferentiated because the cancer cells do not look very much like normal thyroid cells under the microscope. This cancer often spreads quickly into the neck and to other parts of the body, and is very hard to treat.
Less Common Thyroid Cancers
Less than 4% of cancers found in the thyroid are thyroid lymphomas, thyroid sarcomas, or other rare tumors.
Parathyroid cancer
Behind, but attached to, the thyroid gland are 4 tiny glands called the parathyroids. The parathyroid glands help regulate the body’s calcium levels. Cancers of the parathyroid glands are very rare — there are probably fewer than 100 cases each year in the United States.
Parathyroid cancers are often found because they cause high blood calcium levels. This makes a person tired, weak, and drowsy. It can also make you urinate (pee) a lot, causing dehydration, which can make the weakness and drowsiness worse. Other symptoms include bone pain and fractures, pain from kidney stones, depression, and constipation.
Larger parathyroid cancers may also be found as a nodule near the thyroid. No matter how large the nodule is, the only treatment is to remove it surgically. Parathyroid cancer is much harder to cure than thyroid cancer.
Complications of Thyroid cancer
Thyroid cancer that comes back
Despite treatment, thyroid cancer can return, even if you’ve had your thyroid removed. This could happen if microscopic cancer cells spread beyond the thyroid before it’s removed.
Thyroid cancer may recur in:
- Lymph nodes in the neck
- Small pieces of thyroid tissue left behind during surgery
- Other areas of the body
Thyroid cancer that recurs can be treated. Your doctor may recommend periodic blood tests or thyroid scans to check for signs of a thyroid cancer recurrence.
How common is thyroid cancer?
The American Cancer Society’s most recent estimates for thyroid cancer in the United States for 2017 are 1:
- About 56,870 new cases of thyroid cancer (42,470 in women, and 14,400 in men)
- About 2,010 deaths from thyroid cancer (1,090 women and 920 men)
The death rate from thyroid cancer has been fairly steady for many years, and remains very low compared with most other cancers.
Lifetime risk of thyroid cancer
Thyroid cancer is commonly diagnosed at a younger age than most other adult cancers. Nearly 3 out of 4 cases are found in women. About 2% of thyroid cancers occur in children and teens.
The chance of being diagnosed with thyroid cancer has risen in recent years and is the most rapidly increasing cancer in the US tripling in the past three decades. Much of this rise appears to be the result of the increased use of thyroid ultrasound, which can detect small thyroid nodules that might not otherwise have been found in the past.
Thyroid cancer causes
Thyroid cancer is linked with a number of inherited conditions (see thyroid cancer risk factors below), but the exact cause of most thyroid cancers is not yet known.
Certain changes in a person’s DNA can cause thyroid cells to become cancerous. DNA is the chemical in each of our cells that makes up our genes – the instructions for how our cells function. We usually look like our parents because they are the source of our DNA. But DNA affects more than just how we look. It also can influence our risk for developing certain diseases, including some kinds of cancer.
Some genes contain instructions for controlling when our cells grow and divide into new cells. Certain genes that help cells grow and divide or make them live longer than they should are called oncogenes. Other genes that slow down cell division or make cells die at the right time are called tumor suppressor genes. Cancers can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes.
People inherit 2 copies of each gene – one from each parent. You can inherit damaged DNA from one or both parents. Most cancers, though, are not caused by inherited gene changes. In these cases, the genes change during a person’s life. They may occur when a cell’s DNA is damaged by something in the environment, like radiation, or they may just be random events that sometimes happen inside a cell, without an outside cause.
Papillary thyroid cancer
Several DNA mutations (changes) have been found in papillary thyroid cancer. Many of these cancers have changes in specific parts of the RET gene. The altered form of this gene, known as the PTC oncogene, is found in about 10% to 30% of papillary thyroid cancers overall, and in a larger percentage of these cancers in children and/or linked with radiation exposure. These RET mutations usually are acquired during a person’s lifetime rather than being inherited. They are found only in cancer cells and are not passed on to the patient’s children.
Many papillary thyroid cancers have a mutated BRAF gene. The BRAF mutation is less common in thyroid cancers in children and in those thought to develop from exposure to radiation. Cancers with BRAF changes tend to grow and spread to other parts of the body more quickly.
Both BRAF and RET/PTC changes are thought to make cells grow and divide. It is extremely rare for papillary cancers to have changes in both the BRAF and RET/PTC genes. Some doctors now advise testing thyroid biopsy samples for these gene mutations, as they can help diagnose cancer and may also affect the patient’s outlook.
Changes in other genes have also been linked to papillary thyroid cancer, including those in the NTRK1 gene and the MET gene.
Follicular thyroid cancer
Acquired changes in the RAS oncogene as well as changes in the PAX8–PPAR-γ rearrangement have a role in causing some follicular thyroid cancers.
Anaplastic thyroid cancer
These cancers tend to have some of the mutations described above and often have changes in the TP53 tumor suppressor gene and the CTNNB1 oncogene as well.
Medullary thyroid cancer
People who have medullary thyroid cancer have mutations in different parts of the RET gene compared with papillary carcinoma patients. Nearly all patients with the inherited form of medullary thyroid cancer and about 1 of every 10 with the sporadic (non-inherited) form of medullary thyroid cancer have a mutation in the RET gene. Most patients with sporadic medullary thyroid cancer have gene mutations only in their cancer cells. Those with familial medullary thyroid cancer and multiple endocrine neoplasia type 2 (MEN 2) inherit the RET mutation from a parent. These mutations are in every cell of the patient’s body and can be detected by testing the DNA of blood cells.
In people with inherited mutations of RET, one RET gene is usually normal and one is mutated. Because every person has 2 RET genes but passes only one of them to a child (the child’s other RET gene comes from the other parent), the odds that a person with familial medullary thyroid cancer will pass a mutated gene on to a child are 1 in 2 (or 50%).
Thyroid Cancer Risk Factors
A risk factor is anything that affects a person’s chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed.
But risk factors don’t tell us everything. Having a risk factor, or even several risk factors, does not mean that you will get the disease. And many people who get the disease may have few or no known risk factors. Even if a person with thyroid cancer has a risk factor, it is very hard to know how much that risk factor may have contributed to the cancer.
Scientists have found a few risk factors that make a person more likely to develop thyroid cancer.
Risk factors that can’t be changed
Gender and age
For unclear reasons thyroid cancers (like almost all diseases of the thyroid) occur about 3 times more often in women than in men.
Thyroid cancer can occur at any age, but the risk peaks earlier for women (who are most often in their 40s or 50s when diagnosed) than for men (who are usually in their 60s or 70s).
Hereditary conditions
Several inherited conditions have been linked to different types of thyroid cancer, as has family history. Still, most people who develop thyroid cancer do not have an inherited condition or a family history of the disease.
Medullary thyroid cancer: About 2 out of 10 medullary thyroid carcinomas result from inheriting an abnormal gene. These cases are known as familial medullary thyroid carcinoma. Familial medullary thyroid carcinoma can occur alone, or it can be seen along with other tumors.
The combination of familial medullary thyroid carcinoma and tumors of other endocrine glands is called multiple endocrine neoplasia type 2 (MEN 2). There are 2 subtypes, MEN 2a and MEN 2b, both of which are caused by mutations (defects) in a gene called RET.
- In MEN 2a, medullary thyroid carcinoma occurs along with pheochromocytomas (tumors that make adrenaline) and with parathyroid gland tumors.
- In MEN 2b, medullary thyroid carcinoma is associated with pheochromocytomas and with benign growths of nerve tissue on the tongue and elsewhere called neuromas. This subtype is much less common than MEN 2a.
In these inherited forms of medullary thyroid carcinoma, the cancers often develop during childhood or early adulthood and can spread early. Medullary thyroid carcinoma is most aggressive in the MEN 2b syndrome. If MEN 2a, MEN 2b, or isolated familial medullary thyroid carcinoma runs in your family, you may be at very high risk of developing medullary thyroid carcinoma. Ask your doctor about having regular blood tests or ultrasound exams to look for problems and the possibility of genetic testing.
Other thyroid cancers: People with certain inherited medical conditions have a higher risk of more common forms of thyroid cancer. Higher rates of thyroid cancer occur among people with uncommon genetic conditions such as:
Familial adenomatous polyposis: People with this syndrome develop many colon polyps and have a very high risk of colon cancer. They also have an increased risk of some other cancers, including papillary thyroid cancer. Gardner syndrome is a subtype of familial adenomatous polyposis in which patients also get certain benign tumors. Both Gardner syndrome and familial adenomatous polyposis are caused by defects in the gene APC.
Cowden disease: People with this syndrome have an increased risk of thyroid problems and certain benign growths (including some called hamartomas). They also have an increased risk of cancers of the thyroid, uterus, breast, as well as some others. The thyroid cancers tend to be either the papillary or follicular type. This syndrome is most often caused by defects in the gene PTEN. It is also known as Multiple Hamartoma Syndrome and PTEN Hamartoma Tumor Syndrome
Carney complex, type I: People with this syndrome may develop a number of benign tumors and hormone problems. They also have an increased risk of papillary and follicular thyroid cancers. This syndrome is caused by defects in the gene PRKAR1A.
Familial nonmedullary thyroid carcinoma: Thyroid cancer occurs more often in some families, and is often seen at an earlier age. The papillary type of thyroid cancer most often runs in families. Genes on chromosome 19 and chromosome 1 are suspected of causing these familial cancers.
If you suspect you might have a familial condition, talk with your doctor, who might recommend genetic counseling if your medical history warrants it.
Family history
Having a first-degree relative (parent, brother, sister, or child) with thyroid cancer, even without a known inherited syndrome in the family, increases your risk of thyroid cancer. The genetic basis for these cancers is not totally clear.
Risk factors that can be changed
A diet low in iodine
Follicular thyroid cancers are more common in areas of the world where people’s diets are low in iodine. In the United States, most people get enough iodine in their diet because it is added to table salt and other foods. A diet low in iodine may also increase the risk of papillary cancer if the person also is exposed to radioactivity.
Radiation
Radiation exposure is a proven risk factor for thyroid cancer. Sources of such radiation include certain medical treatments and radiation fallout from power plant accidents or nuclear weapons.
Having had head or neck radiation treatments in childhood is a risk factor for thyroid cancer. Risk depends on how much radiation is given and the age of the child. In general, the risk increases with larger doses and with younger age at treatment.
Before the 1960s, children were sometimes treated with low doses of radiation for things we wouldn’t use radiation for now, like acne, fungus infections of the scalp (ringworm), or enlarged tonsils or adenoids. Years later, the people who had these treatments were found to have a higher risk of thyroid cancer. Radiation therapy in childhood for some cancers such as lymphoma, Wilms tumor, and neuroblastoma also increases risk. Thyroid cancers that develop after radiation therapy are not more serious than other thyroid cancers.
Imaging tests such as x-rays and CT scans also expose children to radiation, but at much lower doses, so it’s not clear how much they might raise the risk of thyroid cancer (or other cancers). If there is an increased risk it is likely to be small, but to be safe, children should not have these tests unless they are absolutely needed. When they are needed, they should be done using the lowest dose of radiation that still provides a clear picture.
Several studies have pointed to an increased risk of thyroid cancer in children because of radioactive fallout from nuclear weapons or power plant accidents. For instance, thyroid cancer was many times more common than normal in children who lived near Chernobyl, the site of a 1986 nuclear plant accident that exposed millions of people to radioactivity. Adults involved with the cleanup after the accident and those who lived near the plant have also had higher rates of thyroid cancer. Children who had more iodine in their diet appeared to have a lower risk.
Some radioactive fallout occurred over certain regions of the United States after nuclear weapons were tested in western states during the 1950s. This exposure was much, much lower than that around Chernobyl. A higher risk of thyroid cancer has not been proven at these low exposure levels. If you are concerned about possible exposure to radioactive fallout, discuss this with your doctor.
Being exposed to radiation when you are an adult carries much less risk of thyroid cancer.
Thyroid cancer prevention
Most people with thyroid cancer have no known risk factors, so it is not possible to prevent most cases of this disease.
Radiation exposure, especially in childhood, is a known thyroid cancer risk factor. Because of this, doctors no longer use radiation to treat less serious diseases. Imaging tests such as x-rays and CT scans also expose children to radiation, but at much lower doses, so it’s not clear how much they might raise the risk of thyroid cancer (or other cancers). If there is an increased risk it is likely to be small, but to be safe, children should not have these tests unless they are absolutely needed. When they are needed, they should be done using the lowest dose of radiation that still provides a clear picture.
Blood tests can be done to look for the gene mutations found in familial medullary thyroid cancer. Because of this, most of the familial cases of medullary thyroid cancer can be prevented or treated early by removing the thyroid gland. Once the disease is discovered in a family, the rest of the family members can be tested for the mutated gene.
If you have a family history of medullary thyroid cancer, it is important that you see a doctor who is familiar with the latest advances in genetic counseling and genetic testing for this disease. Removing the thyroid gland in children who carry the abnormal gene will probably prevent a cancer that might otherwise be fatal.
Prevention for people near nuclear power plants
Fallout from an accident at a nuclear power plant could cause thyroid problems in people living nearby. If you live within 10 miles of a nuclear power plant in the United States, you may be eligible to receive a medication (potassium iodide) that blocks the effects of radiation on the thyroid. If an emergency were to occur, you and your family could take the potassium iodide tablets to help prevent thyroid problems. Contact your state or local emergency management department for more information.
Thyroid cancer signs and symptoms
Thyroid cancer typically doesn’t cause any signs or symptoms early in the disease. As thyroid cancer grows, it may cause:
- A lump that can be felt through the skin on your neck, sometimes growing quickly
- Swelling in the neck
- Changes to your voice, including increasing hoarseness
- Difficulty swallowing
- Pain in the front of the neck and throat, sometimes going up to the ears
- Swollen lymph nodes in your neck
- Hoarseness or other voice changes that do not go away
- Trouble breathing
- A constant cough that is not due to a cold
If you have any of these signs or symptoms, talk to your doctor right away. Many of these symptoms can also be caused by non-cancerous conditions or even other cancers of the neck area. Lumps in the thyroid are common and are usually benign. Still, if you have any of these symptoms, it’s important to see your doctor right away so the cause can be found and treated, if needed.
Thyroid cancer diagnosis
Many cases of thyroid cancer can be found early. In fact, most thyroid cancers are now found much earlier than in the past and can be treated successfully.
Most early thyroid cancers are found when patients see their doctors because of neck lumps or nodules they noticed. If you have unusual symptoms such as a lump or swelling in your neck, you should see your doctor right away.
Other cancers are found by health care professionals during a routine checkup. There is no recommended screening test to find thyroid cancer early. Some doctors also recommend that people examine their necks twice a year to look and feel for any growths or lumps.
Early thyroid cancers are also sometimes found when people have ultrasound tests for other health problems, such as narrowing of carotid arteries (which pass through the neck to supply blood to the brain) or for enlarged or overactive parathyroid glands.
Blood tests or thyroid ultrasound can often find changes in the thyroid, but these tests are not recommended as screening tests for thyroid cancer unless a person is at increased risk, such as because of a family history of thyroid cancer.
People with a family history of medullary thyroid cancer, with or without type 2 multiple endocrine neoplasia (MEN 2), might have a very high risk for developing this cancer. Most doctors recommend genetic testing for these people when they are young to see if they carry the gene changes linked to medullary thyroid cancer. For those who may be at risk but don’t get genetic testing, blood tests can help find medullary thyroid cancer at an early stage, when it may still be curable. Thyroid ultrasounds may also be done in high-risk people.
Tests for Thyroid Cancer
Thyroid cancer may be diagnosed after a person goes to a doctor because of symptoms, or it might be found during a routine physical exam or other tests. If there is a reason to suspect you might have thyroid cancer, your doctor will use one or more tests to find out. Signs and symptoms might suggest you have thyroid cancer, but you will need tests to confirm the diagnosis.
Medical history and physical exam
If you have any signs or symptoms that suggest you might have thyroid cancer, your health care professional will want to know your complete medical history. You will be asked questions about your possible risk factors, symptoms, and any other health problems or concerns. If someone in your family has had thyroid cancer (especially medullary thyroid cancer) or tumors called pheochromocytomas, it is important to tell your doctor, as you might be at high risk for this disease.
Your doctor will examine you to get more information about possible signs of thyroid cancer and other health problems. During the exam, the doctor will pay special attention to the size and firmness of your thyroid and any enlarged lymph nodes in your neck.
Biopsy
The actual diagnosis of thyroid cancer is made with a biopsy, in which cells from the suspicious area are removed and looked at under a microscope. However, this might not be the first test done if you have a suspicious lump in your neck. The doctor might order other tests first, such as blood tests, an ultrasound exam, or a radioiodine scan to get a better sense of whether you might have thyroid cancer. These tests are described below.
If your doctor thinks a biopsy is needed, the simplest way to find out if a thyroid lump or nodule is cancerous is with a fine needle aspiration (FNA) of the thyroid nodule. This type of biopsy can usually be done in your doctor’s office or clinic.
Before the biopsy, local anesthesia (numbing medicine) may be injected into the skin over the nodule, but in most cases an anesthetic is not needed. Your doctor will place a thin, hollow needle directly into the nodule to aspirate (take out) some cells and a few drops of fluid into a syringe. The doctor usually repeats this 2 or 3 more times, taking samples from several areas of the nodule. The biopsy samples are then sent to a lab, where they are looked at under a microscope to see if the cells look cancerous or benign.
Bleeding at the biopsy site is very rare except in people with bleeding disorders. Be sure to tell your doctor if you have problems with bleeding or are taking medicines that could affect bleeding, such as aspirin or blood thinners.
This test is generally done on all thyroid nodules that are big enough to be felt. This means that they are larger than about 1 centimeter (about 1/2 inch) across. Doctors often use ultrasound to see the thyroid during the biopsy, which helps make sure they are getting samples from the right areas. This is especially helpful for smaller nodules. Fine needle aspiration biopsies can also be used to get samples of swollen lymph nodes in the neck to see if they contain cancer.
Sometimes a fine needle aspiration biopsy will need to be repeated because the samples didn’t contain enough cells. Most fine needle aspiration biopsies will show that the thyroid nodule is benign. Rarely, the biopsy may come back as benign even though cancer is present. Cancer is clearly diagnosed in only about 1 of every 20 fine needle aspiration biopsies.
Sometimes the test results first come back as “suspicious” or “of undetermined significance” if fine needle aspiration findings don’t show for sure if the nodule is either benign or malignant. If this happens, the doctor may order tests on the sample to see if the BRAF or RET/PTC genes are mutated. Finding these changes makes thyroid cancer much more likely, and may also play a role in determining the best treatment for the cancer.
If the diagnosis is not clear after a fine needle aspiration biopsy, you might need a more involved biopsy to get a better sample, particularly if the doctor has reason to think the nodule may be cancerous. This might include a core biopsy using a larger needle, a surgical “open” biopsy to remove the nodule, or a lobectomy (removal of half of the thyroid gland). Surgical biopsies and lobectomies are done in an operating room while you are under general anesthesia (in a deep sleep). A lobectomy can also be the main treatment for some early cancers, although for many cancers the rest of the thyroid will need to be removed as well (during an operation called a completion thyroidectomy).
Imaging tests
Imaging tests may be done for a number of reasons, including helping find suspicious areas that might be cancer, to learn how far cancer may have spread, and to help determine if treatment is working.
People who have or may have thyroid cancer will get one or more of these tests.
Ultrasound
Ultrasound uses sound waves to create images of parts of your body. For this test, a small, wand-like instrument called a transducer is placed on the skin in front of your thyroid gland. It gives off sound waves and picks up the echoes as they bounce off the thyroid. The echoes are converted by a computer into a black and white image on a computer screen. You are not exposed to radiation during this test.
This test can help determine if a thyroid nodule is solid or filled with fluid. (Solid nodules are more likely to be cancerous.) It can also be used to check the number and size of thyroid nodules. How a nodule looks on ultrasound can sometimes suggest if it is likely to be a cancer, but ultrasound can’t tell for sure.
For thyroid nodules that are too small to feel, this test can be used to guide a biopsy needle into the nodule to obtain a sample. Even when a nodule is large enough to feel, most doctors prefer to use ultrasound to guide the needle.
Ultrasound can also help determine if any nearby lymph nodes are enlarged because the thyroid cancer has spread. Many thyroid specialists recommend ultrasound for all patients with thyroid nodules large enough to be felt.
Radioiodine scan
Radioiodine scans can be used to help determine if someone with a lump in the neck might have thyroid cancer. They are also often used in people who have already been diagnosed with differentiated (papillary, follicular, or Hürthle cell) thyroid cancer to help show if it has spread. Because medullary thyroid cancer cells do not absorb iodine, radioiodine scans are not used for this cancer.
For this test, a small amount of radioactive iodine (called I-131) is swallowed (usually as a pill) or injected into a vein. Over time, the iodine is absorbed by the thyroid gland (or thyroid cells anywhere in the body). A special camera is used several hours later to see where the radioactivity is.
For a thyroid scan, the camera is placed in front of your neck to measure the amount of radiation in the gland. Abnormal areas of the thyroid that have less radioactivity than the surrounding tissue are called cold nodules, and areas that take up more radiation are called hot nodules. Hot nodules usually are not cancerous, but cold nodules can be benign or cancerous. Because both benign and cancerous nodules can appear cold, this test by itself can’t diagnose thyroid cancer.
After surgery for thyroid cancer, whole-body radioiodine scans are useful to look for possible spread throughout the body. These scans become even more sensitive if the entire thyroid gland has been removed by surgery because more of the radioactive iodine is picked up by any remaining thyroid cancer cells.
Radioiodine scans work best if patients have high blood levels of thyroid-stimulating hormone (TSH, or thyrotropin). For people whose thyroid has been removed, TSH levels can be increased by stopping thyroid hormone pills for a few weeks before the test. This leads to low thyroid hormone levels (hypothyroidism) and causes the pituitary gland to release more TSH, which in turn stimulates any thyroid cancer cells to take up the radioactive iodine. A downside of this is that it can cause the symptoms of hypothyroidism, including tiredness, depression, weight gain, sleepiness, constipation, muscle aches, and reduced concentration. One way to raise TSH levels without withholding thyroid hormone is to give an injectable form of thyrotropin (Thyrogen®) before the scan.
Because any iodine already in the body can affect this test, people are usually told not to ingest foods or medicines that contain iodine in the days before the scan.
Radioactive iodine can also be used to treat differentiated thyroid cancer, but it is given in much higher doses.
Chest x-ray
If you have been diagnosed with thyroid cancer (especially follicular thyroid cancer), a plain x-ray of your chest may be done to see if cancer has spread to your lungs.
Computed tomography (CT) scan
The CT scan is an x-ray test that produces detailed cross-sectional images of your body. It can help determine the location and size of thyroid cancers and whether they have spread to nearby areas, although ultrasound is usually the test of choice. A CT scan can also be used to look for spread into distant organs such as the lungs.
One problem using CT scans is that the CT contrast dye contains iodine, which interferes with radioiodine scans. For this reason, many doctors prefer MRI scans for differentiated thyroid cancer.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans can be used to look for cancer in the thyroid, or cancer that has spread to nearby or distant parts of the body. But ultrasound is usually the first choice for looking at the thyroid. MRI can provide very detailed images of soft tissues such as the thyroid gland. MRI scans are also very helpful in looking at the brain and spinal cord.
Positron emission tomography (PET) scan
This test can be very useful if your thyroid cancer is one that doesn’t take up radioactive iodine. In this situation, the PET scan may be able to tell whether the cancer has spread.
Blood tests
Blood tests are not used to find thyroid cancer. But they can help show if your thyroid is working normally, which may help the doctor decide what other tests may be needed. They can also be used to monitor certain cancers.
Thyroid-stimulating hormone (TSH)
Tests of blood levels of thyroid-stimulating hormone (TSH or thyrotropin) may be used to check the overall activity of your thyroid gland. Levels of TSH, which is made by the pituitary gland, may be high if the thyroid is not making enough hormones. This information can be used to help choose which imaging tests (such as ultrasound or radioiodine scans) to use to look at a thyroid nodule. The TSH level is usually normal in thyroid cancer.
T3 and T4 (thyroid hormones)
These are the main hormones made by the thyroid gland. Levels of these hormones may also be measured to get a sense of thyroid gland function. The T3 and T4 levels are usually normal in thyroid cancer.
Thyroglobulin
Thyroglobulin is a protein made by the thyroid gland. Measuring the thyroglobulin level in the blood can’t be used to diagnose thyroid cancer, but it can be helpful after treatment. A common way to treat thyroid cancer is to remove most of the thyroid by surgery and then use radioactive iodine to destroy any remaining thyroid cells. These treatments should lead to a very low level of thyroglobulin in the blood within several weeks. If it is not low, this might mean that there are still thyroid cancer cells in the body. If the level rises again after being low, it is a sign that the cancer could be coming back.
Calcitonin
Calcitonin is a hormone that helps control how the body uses calcium. It is made by C cells in the thyroid, the cells that can develop into medullary thyroid cancer. If medullary thyroid cancer is suspected or if you have a family history of the disease, blood tests of calcitonin levels can help look for medullary thyroid cancer. This test is also used to look for the possible recurrence of medullary thyroid cancer after treatment. Because calcitonin can affect blood calcium levels, these may be checked as well.
Carcinoembryonic antigen (CEA)
People with medullary thyroid cancer often have high blood levels of a protein called carcinoembryonic antigen (CEA). Tests for CEA can help monitor this cancer.
Other blood tests
You might have other blood tests as well. For example, if you are scheduled for surgery, tests will be done to check your blood cell counts, to look for bleeding disorders, and to check your liver and kidney function.
Medullary thyroid carcinoma can be caused by a genetic syndrome that also causes a tumor called pheochromocytoma. Pheochromcytomas can cause problems during surgery if the patient is under anesthesia. This is why patients with MTC who will have surgery are often tested to see if they have a pheochromocytoma, as well. This can mean blood tests for epinephrine (adrenaline) and a related hormone called norepinephrine, and/or urine tests for their breakdown products (called metanephrines).
Other tests
Vocal cord exam (laryngoscopy)
Thyroid tumors can sometimes affect the vocal cords. If you are going to have surgery to treat thyroid cancer, a procedure called a laryngoscopy will probably be done first to see if the vocal cords are moving normally. For this exam, the doctor looks down the throat at the larynx (voice box) with special mirrors or with a laryngoscope, a thin tube with a light and a lens on the end for viewing.
Thyroid cancer stages
Staging is the process of finding out if and how far a cancer has spread. The stage of a cancer is one of the most important factors in choosing treatment options and predicting your chance for cure.
Staging is based on the results of the physical exam, biopsy, and imaging tests (ultrasound, radioiodine scan, CT scan, MRI, chest x-ray, and/or PET scans), which are described in Tests for thyroid cancer.
The American Joint Committee on Cancer TNM staging system
A staging system is a standard way to sum up how large a cancer is and how far it has spread.
The most common system used to describe the stages of thyroid cancer is the American Joint Committee on Cancer TNM system. The TNM system is based on 3 key pieces of information:
- T indicates the size of the main (primary) tumor and whether it has grown into nearby areas.
- N describes the extent of spread to nearby (regional) lymph nodes. Lymph nodes are bean-shaped collections of immune system cells to which cancers often spread first. Cells from thyroid cancers can travel to lymph nodes in the neck and chest areas.
- M indicates whether the cancer has spread (metastasized) to other organs of the body. (The most common sites of spread of thyroid cancer are the lungs, the liver, and bones.)
Numbers or letters appear after T, N, and M to provide more details about each of these factors. Higher numbers mean the cancer is more advanced. The letter X means a category can’t be assessed because the information is not available.
T categories for thyroid cancer (other than anaplastic thyroid cancer)
TX: Primary tumor cannot be assessed.
T0: No evidence of primary tumor.
T1: The tumor is 2 cm (slightly less than an inch) across or smaller and has not grown out of the thyroid.
T1a: The tumor is 1 cm (less than half an inch) across or smaller and has not grown outside the thyroid.
T1b: The tumor is larger than 1 cm but not larger than 2 cm across and has not grown outside of the thyroid.
T2: The tumor is more than 2 cm but not larger than 4 cm (slightly less than 2 inches) across and has not grown out of the thyroid.
T3: The tumor is larger than 4 cm across, or it has just begun to grow into nearby tissues outside the thyroid.
T4a: The tumor is any size and has grown extensively beyond the thyroid gland into nearby tissues of the neck, such as the larynx (voice box), trachea (windpipe), esophagus (tube connecting the throat to the stomach), or the nerve to the larynx. This is also called moderately advanced disease.
T4b: The tumor is any size and has grown either back toward the spine or into nearby large blood vessels. This is also called very advanced disease.
T categories for anaplastic thyroid cancer
All anaplastic thyroid cancers are considered T4 tumors at the time of diagnosis.
T4a: The tumor is still within the thyroid.
T4b: The tumor has grown outside the thyroid.
N categories for thyroid cancer
NX: Regional (nearby) lymph nodes cannot be assessed.
N0: The cancer has not spread to nearby lymph nodes.
N1: The cancer has spread to nearby lymph nodes.
N1a: The cancer has spread to lymph nodes around the thyroid in the neck (called pretracheal, paratracheal, and prelaryngeal lymph nodes).
N1b: The cancer has spread to other lymph nodes in the neck (called cervical) or to lymph nodes behind the throat (retropharyngeal) or in the upper chest (superior mediastinal).
M categories for thyroid cancer
MX: Distant metastasis cannot be assessed.
M0: There is no distant metastasis.
M1: The cancer has spread to other parts of the body, such as distant lymph nodes, internal organs, bones, etc.
Stage grouping
Once the values for T, N, and M are determined, they are combined into stages, expressed as a Roman numeral from I through IV. Sometimes letters are used to further divide a stage. Unlike most other cancers, thyroid cancers are grouped into stages in a way that also considers the subtype of cancer and the patient’s age.
Papillary or follicular (differentiated) thyroid cancer in patients younger than 45
Younger people have a low likelihood of dying from differentiated (papillary or follicular) thyroid cancer. The TNM stage groupings for these cancers take this fact into account. So, all people younger than 45 years with these cancers are stage I if they have no distant spread and stage II if they have distant spread.
Stage I (Any T, Any N, M0): The tumor can be any size (any T) and may or may not have spread to nearby lymph nodes (any N). It has not spread to distant sites (M0).
Stage II (Any T, Any N, M1): The tumor can be any size (any T) and may or may not have spread to nearby lymph nodes (any N). It has spread to distant sites (M1).
Papillary or follicular (differentiated) thyroid cancer in patients 45 years and older
Stage I (T1, N0, M0): The tumor is 2 cm or less across and has not grown outside the thyroid (T1). It has not spread to nearby lymph nodes (N0) or distant sites (M0).
Stage II (T2, N0, M0): The tumor is more than 2 cm but not larger than 4 cm across and has not grown outside the thyroid (T2). It has not spread to nearby lymph nodes (N0) or distant sites (M0).
Stage III: One of the following applies:
T3, N0, M0: The tumor is larger than 4 cm across or has grown slightly outside the thyroid (T3), but it has not spread to nearby lymph nodes (N0) or distant sites (M0).
T1 to T3, N1a, M0: The tumor is any size and may have grown slightly outside the thyroid (T1 to T3). It has spread to lymph nodes around the thyroid in the neck (N1a) but not to other lymph nodes or to distant sites (M0).
Stage IVA: One of the following applies:
- T4a, any N, M0: The tumor is any size and has grown beyond the thyroid gland and into nearby tissues of the neck (T4a). It might or might not have spread to nearby lymph nodes (any N). It has not spread to distant sites (M0).
- T1 to T3, N1b, M0: The tumor is any size and might have grown slightly outside the thyroid gland (T1 to T3). It has spread to certain lymph nodes in the neck (cervical nodes) or to lymph nodes in the upper chest (superior mediastinal nodes) or behind the throat (retropharyngeal nodes) (N1b), but it has not spread to distant sites (M0).
Stage IVB (T4b, Any N, M0): The tumor is any size and has grown either back toward the spine or into nearby large blood vessels (T4b). It might or might not have spread to nearby lymph nodes (any N), but it has not spread to distant sites (M0).
Stage IVC (Any T, Any N, M1): The tumor is any size and might or might not have grown outside the thyroid (any T). It might or might not have spread to nearby lymph nodes (any N). It has spread to distant sites (M1).
Medullary thyroid cancer
Age is not a factor in the stage of medullary thyroid cancer.
Stage I (T1, N0, M0): The tumor is 2 cm or less across and has not grown outside the thyroid (T1). It has not spread to nearby lymph nodes (N0) or distant sites (M0).
Stage II: One of the following applies:
- T2, N0, M0: The tumor is more than 2 cm but is not larger than 4 cm across and has not grown outside the thyroid (T2). It has not spread to nearby lymph nodes (N0) or distant sites (M0).
- T3, N0, M0: The tumor is larger than 4 cm or has grown slightly outside the thyroid (T3), but it has not spread to nearby lymph nodes (N0) or distant sites (M0).
Stage III (T1 to T3, N1a, M0): The tumor is any size and might have grown slightly outside the thyroid (T1 to T3). It has spread to lymph nodes around the thyroid in the neck (N1a) but not to other lymph nodes or to distant sites (M0).
Stage IVA: One of the following applies:
- T4a, any N, M0: The tumor is any size and has grown beyond the thyroid gland and into nearby tissues of the neck (T4a). It might or might not have spread to nearby lymph nodes (any N). It has not spread to distant sites (M0).
- T1 to T3, N1b, M0: The tumor is any size and might have grown slightly outside the thyroid gland (T1 to T3). It has spread to certain lymph nodes in the neck (cervical nodes) or to lymph nodes in the upper chest (superior mediastinal nodes) or behind the throat (retropharyngeal nodes) (N1b), but it has not spread to distant sites (M0).
Stage IVB (T4b, Any N, M0): The tumor is any size and has grown either back toward the spine or into nearby large blood vessels (T4b). It might or might not have spread to nearby lymph nodes (any N), but it has not spread to distant sites (M0).
Stage IVC (Any T, Any N, M1): The tumor is any size and might or might not have grown outside the thyroid (any T). It might or might not have spread to nearby lymph nodes (any N). It has spread to distant sites (M1).
Anaplastic (undifferentiated) thyroid cancer
All anaplastic thyroid cancers are considered stage IV, reflecting the poor prognosis of this type of cancer.
Stage IVA (T4a, Any N, M0): The tumor is still within the thyroid (T4a). It might or might not have spread to nearby lymph nodes (any N), but it has not spread to distant sites (M0).
Stage IVB (T4b, Any N, M0): The tumor has grown outside the thyroid (T4b). It might or might not have spread to nearby lymph nodes (any N), but it has not spread to distant sites (M0).
Stage IVC (Any T, Any N, M1): The tumor might or might not have grown outside of the thyroid (any T). It might or might not have spread to nearby lymph nodes (any N). It has spread to distant sites (M1).
Recurrent thyroid cancer
This is not an actual stage in the TNM system. Cancer that comes back after treatment is called recurrent (or relapsed). If thyroid cancer returns it is usually in the neck, but it may come back in another part of the body (for example, lymph nodes, lungs, or bones). Doctors may assign a new stage based on how far the cancer has spread, but this is not usually as formal a process as the original staging. The presence of recurrent disease does not change the original, formal staging.
If you have any questions about the stage of your cancer or how it affects your treatment options, be sure to ask your doctor.
Thyroid cancer survival rate
Survival rates tell you what portion of people with the same type and stage of cancer are still alive a certain amount of time ( usually 5 years) after their cancer is diagnosed. These numbers can’t tell you how long you will live, but they may help give you a better understanding about how likely it is that your treatment will be successful. Some people will want to know the survival rates for their cancer type and stage, and some people won’t. If you don’t want to know, you don’t have to.
What is a 5-year survival rate?
Statistics on the outlook for a certain type and stage of cancer are often given as 5-year survival rates, but many people live longer – often much longer – than 5 years. The 5-year survival rate is the percentage of people who live at least 5 years after being diagnosed with cancer. For example, a 5-year survival rate of 50% means that an estimated 50 out of 100 people who have that cancer are still alive 5 years after being diagnosed. Keep in mind, however, that many of these people live much longer than 5 years after diagnosis.
Relative survival rates are a more accurate way to estimate the effect of cancer on survival. These rates compare people with cancer to people in the overall population. For example, if the 5-year relative survival rate for a specific type and stage of cancer is 50%, it means that people who have that cancer are, on average, about 50% as likely as people who don’t have that cancer to live for at least 5 years after being diagnosed.
But remember, survival rates are estimates – your outlook can vary based on a number of factors specific to you.
Survival rates don’t tell the whole story
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they can’t predict what will happen in any particular person’s case. Your doctor can tell you how the numbers below may apply to you, as he or she is familiar with the aspects of your particular situation.
The following survival statistics were published in 2010 in the 7th edition of the AJCC Cancer Staging Manual. They are based on the stage of the cancer when the person is first diagnosed.
Papillary thyroid cancer*
| Stage | 5-Year Relative Survival Rate |
| I | near 100% |
| II | near 100% |
| III | 93% |
| IV | 51% |
*Based on patients diagnosed 1998 to 1999
Follicular thyroid cancer*
| Stage | 5-Year Relative Survival Rate |
| I | near 100% |
| II | near 100% |
| III | 71% |
| IV | 50% |
*Based on patients diagnosed 1998 to 1999
Medullary thyroid cancer**
| Stage | 5-Year Relative Survival Rate |
| I | near 100% |
| II | 98% |
| III | 81% |
| IV | 28% |
**Based on patients diagnosed between 1985 and 1991
Anaplastic thyroid cancer
The 5-year relative survival rate for anaplastic (undifferentiated) carcinomas, all of which are considered stage IV, is around 7% (based on patients diagnosed between 1985 and 1991).
Thyroid cancer treatment
After thyroid cancer is found and staged, your cancer care team will discuss your treatment options with you. It is important to take the time to consider each of your options. In choosing a treatment plan, factors to consider include the type and stage of the cancer and your general health. The treatment options for thyroid cancer might include:
- Surgery
- Radioactive iodine treatment
- Thyroid hormone therapy
- External beam radiation therapy
- Chemotherapy
- Targeted therapy
Often 2 or more of these options are combined.
Most thyroid cancers can be cured, especially if they have not spread to distant parts of the body. If the cancer can’t be cured, the goal of treatment may be to remove or destroy as much of the cancer as possible and to keep it from growing, spreading, or returning for as long as possible. Sometimes treatment is aimed at palliating (relieving) symptoms such as pain or problems with breathing and swallowing.
If you have any concerns about your treatment plan, if time permits it is often a good idea to get a second opinion. In fact, many doctors encourage this. A second opinion can provide more information and help you feel confident about the treatment plan you choose.
Some treatments for thyroid cancer might affect your ability to have children later in life. If this might be a concern for you, talk to your doctor about it before you decide on treatment.
Surgery
Most people with thyroid cancer undergo surgery to remove all or most of the thyroid.
Thyroid surgery carries a risk of bleeding and infection. Damage can also occur to your parathyroid glands during surgery, which can lead to low calcium levels in your body. There’s also a risk of accidental damage to the nerves connected to your vocal cords, which can cause vocal cord paralysis, hoarseness, soft voice or difficulty breathing. There is also the risk of excessive bleeding or formation of a major blood clot in the neck (called a hematoma) and wound infection.
Operations used to treat thyroid cancer include:
Removing all or most of the thyroid (thyroidectomy)
In most cases, doctors recommend removing the entire thyroid in order to treat thyroid cancer. Your surgeon makes an incision at the base of your neck to access your thyroid.
This is the most common surgery for thyroid cancer. If the entire thyroid gland is removed, it is called a total thyroidectomy. Sometimes the surgeon may not be able to remove the entire thyroid. If nearly all of the gland is removed, it is called a near-total thyroidectomy. If most of the gland is removed, it is called a subtotal thyroidectomy.
After a thyroidectomy (and possibly radioactive iodine [radioiodine] therapy), you will need to take daily thyroid hormone (levothyroxine) pills. But one advantage of this surgery over lobectomy is that your doctor can most often watch you for disease recurrence afterward using radioiodine scans and thyroglobulin blood tests.
Removing a portion of the thyroid (thyroid lobectomy)
This operation is sometimes used to treat differentiated (papillary or follicular) thyroid cancers that are small and show no signs of spread beyond the thyroid gland. It is also sometimes used to diagnose thyroid cancer if an fine needle aspiration biopsy result doesn’t provide a clear diagnosis.
First, the surgeon makes an incision (cut) a few inches long across the front of the neck and exposes the thyroid. The lobe containing the cancer is then removed, usually along with the isthmus (the small piece of the gland that acts as a bridge between the left and right lobes).
An advantage of this surgery, is that some patients might not need to take thyroid hormone pills afterward because it leaves part of the gland behind. But having some thyroid left can interfere with some tests that look for cancer recurrence after treatment, such as radioiodine scans and thyroglobulin blood tests.
Removing lymph nodes in the neck
If cancer has spread to nearby lymph nodes in the neck, these will be removed at the same time surgery is done on the thyroid. This is especially important for treatment of medullary thyroid cancer and for anaplastic cancer (when surgery is an option).
For papillary or follicular cancer where only 1 or 2 enlarged lymph nodes are thought to contain cancer, the enlarged nodes may be removed and any small deposits of cancer cells that may be left are then treated with radioactive iodine (see the section about radioactive iodine [radioiodine] therapy). More often, several lymph nodes near the thyroid are removed in an operation called a central compartment neck dissection. Removal of even more lymph nodes, including those on the side of the neck, is called a modified radical neck dissection.
Radioactive Iodine (Radioiodine) Therapy for Thyroid Cancer
Your thyroid gland absorbs nearly all of the iodine in your body. When radioactive iodine (RAI), also known as I-131, is taken into the body in liquid or capsule form, it concentrates in thyroid cells. The radiation can destroy the thyroid gland and any other thyroid cells (including cancer cells) that take up iodine, with little effect on the rest of your body. The radiation dose used here is much stronger than the one used in radioiodine scans.
This treatment can be used to ablate (destroy) any thyroid tissue not removed by surgery or to treat some types of thyroid cancer that have spread to lymph nodes and other parts of the body.
Radioactive iodine therapy improves the survival rate of patients with papillary or follicular thyroid cancer (differentiated thyroid cancer) that has spread to the neck or other body parts, and this treatment is now standard practice in such cases. But the benefits of RAI therapy are less clear for patients with small cancers of the thyroid gland that do not seem to have spread, which can often be removed completely with surgery. Discuss your risks and benefits of RAI therapy with your doctor. Radioactive iodine therapy cannot be used to treat anaplastic (undifferentiated) and medullary thyroid carcinomas because these types of cancer do not take up iodine.
For RAI therapy to be most effective, patients must have high levels of thyroid-stimulating hormone (TSH or thyrotropin) in the blood. This substance stimulates thyroid tissue (and cancer cells) to take up radioactive iodine. If the thyroid has been removed, one way to raise TSH levels is to not take thyroid hormone pills for several weeks. This causes very low thyroid hormone levels (a condition known as hypothyroidism), which in turn causes the pituitary gland to release more TSH. This intentional hypothyroidism is temporary, but it often causes symptoms like tiredness, depression, weight gain, constipation, muscle aches, and reduced concentration. Another way to raise TSH levels before RAI therapy is to give an injectable form of thyrotropin (Thyrogen), which can make withholding thyroid hormone for a long period of time unnecessary. This drug is given daily for 2 days, with RAI given on the 3rd day.
Most doctors also recommend that the patient follow a low iodine diet for 1 or 2 weeks before treatment. This means avoiding foods that contain iodized salt and red dye #3, as well as dairy products, eggs, seafood, and soy.
Risks and side effects
Your body will give off radiation for some time after you get RAI therapy. Depending on the dose of radioiodine used and where you are being treated, you might need to be in the hospital for a few days after treatment, staying in a special isolation room to prevent others from being exposed to radiation. Some people may not need to be hospitalized. Once you are allowed to go home after treatment, you will be given instructions on how to protect others from radiation exposure and how long you need to take these precautions. These instructions may vary slightly by treatment center. Be sure you understand the instructions before you leave the hospital.
Short-term side effects of RAI treatment may include:
- Neck tenderness and swelling
- Nausea and vomiting
- Swelling and tenderness of the salivary glands
- Dry mouth
- Taste changes
Chewing gum or sucking on hard candy may help with salivary gland problems.
Radioiodine treatment also reduces tear formation in some people, leading to dry eyes. If you wear contact lenses, ask your doctor how long you should keep them out.
Men who receive large total doses because of many treatments with RAI may have lower sperm counts or, rarely, become infertile. Radioactive iodine may also affect a woman’s ovaries, and some women may have irregular periods for up to a year after treatment. Many doctors recommend that women avoid becoming pregnant for 6 months to a year after treatment. No ill effects have been noted in the children born to parents who received radioactive iodine in the past.
Both men and women who have had RAI therapy may have a slightly increased risk of developing leukemia in the future. Doctors disagree on exactly how much this risk is increased, but most of the largest studies have found that this is an extremely rare complication. Some research even suggests the risk of leukemia may not be significantly increased.
Talk to your health care team if you have any questions about the possible risks and benefits of your treatment.
Thyroid Hormone Therapy
Taking daily pills of thyroid hormone (thyroid hormone therapy) can serve 2 purposes:
- It can help maintain the body’s normal metabolism (by replacing missing thyroid hormone after surgery).
- It can help stop any remaining cancer cells from growing (by lowering TSH levels).
After a thyroidectomy, the body can no longer make the thyroid hormone it needs, so patients must take thyroid hormone (levothyroxine) pills to replace the loss of the natural hormone.
Taking thyroid hormone may also help prevent some thyroid cancers from returning. Normal thyroid function is regulated by the pituitary gland. The pituitary makes a hormone called TSH that causes the thyroid gland to make thyroid hormone for the body. TSH also promotes growth of the thyroid gland and probably of thyroid cancer cells. The level of TSH, in turn, is regulated by how much thyroid hormone is in the blood. If the level of thyroid hormone is low, the pituitary makes more TSH. If the level of thyroid hormone is high, not as much TSH is needed, so the pituitary makes less of it.
Doctors have learned that by giving higher than normal doses of thyroid hormone, TSH levels can be kept very low. This may slow the growth of any remaining cancer cells and lower the chance of some thyroid cancers (especially high-risk cancers) coming back.
Possible side effects
Taking higher than normal levels of thyroid hormone seems to have few short-term side effects, but some doctors have expressed concerns about taking them for long periods of time. High levels of thyroid hormone can lead to problems with a rapid or irregular heartbeat. Over the long run, high doses of thyroid hormone can lead to weak bones (osteoporosis). Because of this, high doses of thyroid hormone may be reserved for people with differentiated thyroid cancers who are at high risk of recurrence.
External Beam Radiation Therapy for Thyroid Cancer
External beam radiation therapy uses high-energy rays (or particles) to destroy cancer cells or slow their growth. A carefully focused beam of radiation is delivered from a machine outside the body. Generally, this type of radiation treatment is not used for cancers that take up iodine (that is, most differentiated thyroid cancers), which are better treated with radioiodine therapy. It is more often used as part of the treatment for medullary thyroid cancer and anaplastic thyroid cancer.
When a cancer that does not take up iodine has spread beyond the thyroid, external radiation treatment may help treat the cancer or reduce the chance of the disease coming back in the neck after surgery. If a cancer does not respond to radioiodine therapy, external radiation therapy may be used to treat local neck recurrence or distant metastases that are causing pain or other symptoms.
External beam radiation therapy is usually given 5 days a week for several weeks. Before your treatments start, the medical team will take careful measurements to find the correct angles for aiming the radiation beams and the proper dose of radiation. The treatment itself is painless and much like getting a regular x-ray. Each treatment lasts only a few minutes, although the setup time — getting you into place for treatment — usually takes longer.
Chemotherapy (chemo) uses anti-cancer drugs that are injected into a vein or muscle, or are taken by mouth. Chemotherapy is systemic therapy, which means that the drug enters the bloodstream and travels throughout the body to reach and destroy cancer cells.
Chemotherapy is seldom helpful for most types of thyroid cancer, but fortunately it is not needed in most cases. It is combined with external beam radiation therapy for anaplastic thyroid cancer and is sometimes used for other advanced cancers that no longer respond to other treatments.
Possible side effects
Chemo drugs attack cells that are dividing quickly, which is why they work against cancer cells. But other cells in the body, such as those in the bone marrow, the lining of the mouth and intestines, and the hair follicles, also divide quickly. These cells are also likely to be affected by chemotherapy, which can lead to side effects.
The side effects of chemotherapy depend on the type and dose of drugs given and the length of time they are taken. Common side effects of chemo include:
- Hair loss
- Mouth sores
- Loss of appetite
- Nausea and vomiting
- Diarrhea
- Increased chance of infections (from too few white blood cells)
- Easy bruising or bleeding (from too few low blood platelets)
- Fatigue (from too few low red blood cells)
These side effects are usually short-term and go away after treatment is finished. There are often ways to lessen these side effects. For example, drugs can be given to help prevent or reduce nausea and vomiting.
Some chemotherapy drugs may have other specific side effects that require monitoring. For example, doxorubicin (one of the most common chemo drugs used in thyroid cancer) can affect heart function. Therefore, a patient taking doxorubicin will get regular heart function tests like echocardiograms.
Injecting alcohol into thyroid cancers
Alcohol ablation involves injecting small thyroid cancers with alcohol using imaging such as ultrasound to ensure precise placement of the injection. This treatment is helpful for treating cancer that occurs in areas that aren’t easily accessible during surgery. Your doctor may recommend this treatment if you have recurrent thyroid cancer limited to small areas in your neck.
Targeted Therapy for Thyroid Cancer
Researchers have begun to develop newer drugs that specifically target the changes inside cells that cause them to become cancerous. Unlike standard chemotherapy drugs, which work by attacking rapidly growing cells in general (including cancer cells), these drugs attack one or more specific targets on cancer cells.
Targeted drugs for medullary thyroid cancer
Doctors have been especially interested in finding targeted drugs to treat medullary thyroid cancer because thyroid hormone-based treatments (including radioactive iodine therapy) are not effective against these cancers.
Vandetanib (Caprelsa®) is a targeted drug taken as a pill once a day. In patients with advanced medullary thyroid cancer, vandetanib stops cancers from growing for an average of about 6 months, although it is not yet clear if it can help people live longer.
Some common side effects of vandetanib include diarrhea, rash, nausea, high blood pressure, headache, fatigue, decreased appetite, and belly (abdominal) pain. Rarely, it can also cause serious problems with heart rhythm and infection that can lead to death. Because of its potential side effects, doctors must get special training before they are allowed to prescribe this drug.
Cabozantinib (Cometriq®) is another targeted drug used to treat medullary thyroid cancer. It is taken in pill form once a day. In medullary thyroid cancer patients, cabozantinib has been shown to help stop cancers from growing for about 7 months longer than a sugar pill. So far, though, it has not been shown to help patients live longer.
Common side effects include diarrhea, constipation, belly pain, mouth sores, decreased appetite, nausea, weight loss, fatigue, high blood pressure, loss of hair color, and hand-foot syndrome (redness, pain, and swelling of the hands and feet). Rarely, this drug can also cause serious side effects, such as severe bleeding and holes in the intestine.
Targeted drugs for papillary or follicular thyroid cancer
Fortunately, most of these cancers can be treated effectively with surgery and radioactive iodine therapy, so there is less need for other drugs to treat them. But for cancers in which these treatments aren’t effective, targeted drugs can be helpful.
Sorafenib (Nexavar®) and lenvatinib (Lenvima®) are both the type of targeted drug known as kinase inhibitors. They work in 2 ways. They help block tumors from forming new blood vessels, which the tumors need to grow. These drugs also target some of the proteins made by cancer cells that normally help them grow.
These drugs can help stop cancer growth for a time when given to patients with differentiated thyroid cancer (papillary, follicular, and poorly differentiated thyroid cancers) whose cancers no longer respond to treatment with radioactive iodine. It isn’t yet clear if these drugs help patients live longer.
Both of these drugs are taken by mouth.
Common side effects include fatigue, rash, loss of appetite, diarrhea, nausea, high blood pressure, and hand foot syndrome (redness, pain, swelling, or blisters on the palms of the hands or soles of the feet). Other side effects can also occur, some of which can be serious. Ask your doctor what you can expect.
Treatment of Thyroid Cancer, by Type and Stage
The type of treatment your doctor will recommend depends on the type and stage of the cancer and on your overall health. This section discusses the typical treatment options for each type and stage of thyroid cancer, but your doctor may have reasons for suggesting a different treatment plan. Don’t hesitate to ask him or her questions about your treatment options.
Papillary carcinoma and its variants
Most cancers are treated with removal of the thyroid gland (thyroidectomy), although small tumors that have not spread outside the thyroid gland may be treated by just removing the side of the thyroid containing the tumor (lobectomy). If lymph nodes are enlarged or show signs of cancer spread, they will be removed as well.
In addition, recent studies have suggested that patients with micro-papillary carcinomas (very small thyroid cancers) may safely choose to be managed by close observation with ongoing ultrasounds rather than have immediate surgery.
Even if the lymph nodes aren’t enlarged, some doctors recommend central compartment neck dissection (surgical removal of lymph nodes next to the thyroid) along with removal of the thyroid. Although this operation has not been shown to improve cancer survival, it might lower the risk of cancer coming back in the neck area. Because removing the lymph nodes allows them to be checked for cancer under the microscope, this surgery also makes it easier to accurately stage the cancer. If cancer has spread to other neck lymph nodes, a modified radical neck dissection (a more extensive removal of lymph nodes from the neck) is often done.
Treatment after surgery depends on the stage of the cancer.
Radioactive iodine (RAI) treatment is sometimes used after thyroidectomy for early stage cancers (T1 or T2, N0, M0), but the cure rate with surgery alone is excellent. If the cancer does come back, radioiodine treatment can still be given.
RAI therapy is often given for more advanced cancers such as T3 or T4 tumors, or cancers that have spread to lymph nodes or distant sites. The goal is to destroy any remaining thyroid tissue and to try to treat any cancer remaining in the body. Areas of distant spread that do not respond to RAI may need to be treated with external beam radiation therapy, targeted therapy, or chemotherapy.
People who have had a thyroidectomy will need to take daily thyroid hormone (levothyroxine) pills. If RAI treatment is planned, the start of thyroid hormone therapy may be delayed until the treatment is finished (usually about 6 weeks after surgery).
Recurrent cancer: Treatment of cancer that comes back after initial therapy depends mainly on where the cancer is, although other factors may be important as well. The recurrence may be found by either blood tests or imaging tests such as ultrasound or radioiodine scans.
If cancer comes back in the neck, an ultrasound-guided biopsy is done first to confirm that it is really cancer. Then, if the tumor appears to be resectable (removable), surgery is often used. If the cancer shows up on a radioiodine scan (meaning the cells are taking up iodine), radioactive iodine (RAI) therapy may be used, either alone or with surgery. If the cancer does not show up on the radioiodine scan but is found by other imaging tests such as an MRI or PET scan, external radiation may be used.
The targeted therapy drugs sorafenib (Nexavar®) and lenvatinib (Lenvima®) may be tried if the cancer has spread to several places and RAI and other treatments are not helpful, but doctors are still trying to find effective drugs for this disease. Because these cancers can be hard to treat, another option is taking part in a clinical trial of newer treatments.
Follicular and Hürthle cell cancers
Often, it isn’t clear that a tumor is a follicular cancer based on a FNA biopsy. If the biopsy results are unclear, they might list “follicular neoplasm” as a diagnosis. Only about 2 of every 10 follicular neoplasms will actually turn out to be cancer, so the next step is usually surgery to remove the half of the thyroid gland that has the tumor (a lobectomy).
If the tumor turns out to be a follicular cancer, a second operation to remove the rest of the thyroid is usually needed (this is called a completion thyroidectomy). If the patient is only willing to have one operation, the doctor may just remove the whole thyroid gland in the first place. Still, for most patients, this isn’t really needed.
If there are signs the cancer has spread before surgery, the tumor must be a cancer and so a thyroidectomy will be done.
Hürthle (Hurthle) cell carcinoma can also be hard to diagnose with certainty based on a FNA biopsy. Tumors suspected of being Hürthle cell carcinomas are often treated like follicular neoplasms. A lobectomy is usually done first. If the diagnosis is confirmed, a completion thyroidectomy is done. A thyroidectomy may be done as the first surgery if there are signs the cancer has spread or if the patient requests it to keep from having more surgery later.
As with papillary cancer, some lymph nodes usually are removed and examined. If cancer has spread to lymph nodes, a central compartment or modified neck dissection (surgical removal of lymph nodes from the neck) may be done. Because the thyroid is removed, patients will need to take thyroid hormone therapy as well, although it is often not started right away.
Radioiodine scanning is usually done after surgery to look for areas still taking up iodine. Spread to nearby lymph nodes and to distant sites that shows up on the scan can be treated by radioactive iodine (RAI). For cancers that don’t take up iodine, external beam radiation therapy may help treat the tumor or prevent it
from growing back in the neck.
Distant metastases may need to be treated with external beam radiation therapy, or targeted therapy with sorafenib (Nexavar®) or lenvatinib (Lenvima®) if they do not respond to RAI. Another option is taking part in a clinical trial of newer treatments or chemotherapy
Recurrent cancer: Treatment of cancer that comes back after initial therapy depends mainly on where the cancer is, although other factors may be important as well. The recurrence may be found by either blood tests or imaging tests such as ultrasound or radioiodine scans.
If cancer comes back in the neck, an ultrasound-guided biopsy is first done to confirm that it is really cancer. Then, if the tumor appears to be resectable (removable), surgery is often used. If the cancer shows up on a radioiodine scan (meaning the cells are taking up iodine), radioactive iodine (RAI) therapy may be used, either alone or with surgery. If the cancer does not show up on the radioiodine scan but is found by other imaging tests such as an MRI or PET scan, external radiation may be used.
Targeted therapy with sorafenib (Nexavar®) and lenvatinib (Lenvima®) is tried first if the cancer has spread to several places and RAI was not helpful. Because these cancers can be hard to treat, another option is taking part in a clinical trial of newer treatments. If a clinical trial is not available your doctor may recommend chemotherapy.
Medullary thyroid carcinoma
Most doctors advise that patients diagnosed with medullary thyroid carcinoma (MTC) be tested for other tumors that are typically seen in patients with the MEN 2 syndromes (see Thyroid Cancer Risk Factors), such as pheochromocytoma and parathyroid tumors.
Screening for pheochromocytoma is particularly important, since the unknown presence of this tumor can make anesthesia and surgery extremely dangerous. If surgeons and anesthesiologists know about such tumors ahead of time, they can treat the patient with medicines before and during surgery to make surgery safe.
Stages I and II: Total thyroidectomy is the main treatment for MTC and often cures patients with stage I or stage II MTC. Nearby lymph nodes are usually removed as well (central compartment or modified radical neck dissection). Because the thyroid gland is removed, thyroid hormone therapy is needed after surgery. For MTC, thyroid hormone therapy is meant to provide enough hormone to keep the patient healthy, but it does not reduce the risk that the cancer will come back.
Because MTC cells do not take up radioactive iodine, there is no role for radioactive iodine therapy in treating MTC. Still, some doctors give a dose of radioactive iodine to destroy any remaining normal thyroid tissue. If MTC cells are in or near the thyroid, this may affect them as well.
Stages III and IV: Surgery is the same as for stages I and II (usually after screening for MEN 2 syndrome and pheochromocytoma). Thyroid hormone therapy is given afterward. When the tumor is extensive and invades many nearby tissues or cannot be completely removed, external beam radiation therapy may be given after surgery to try to reduce the chance of recurrence in the neck.
For cancers that have spread to distant parts of the body, surgery, radiation therapy, or similar treatments may be used if possible. If these treatments can’t be used, vandetanib (Caprelsa), cabozantinib (Cometriq), or other targeted drugs may be tried. Chemotherapy may be another option. Because these cancers can be hard to treat, another option is taking part in a clinical trial of newer treatments.
Recurrent cancer: If the cancer recurs in the neck or elsewhere, surgery, external radiation therapy, targeted therapy (such as vandetanib or cabozantinib), or chemotherapy may be needed. Clinical trials of new treatments may be another option if standard treatments aren’t effective.
Genetic testing in medullary thyroid cancer: If you are told that you have MTC, even if you are the first one in the family to be diagnosed with this disease, ask your doctor about genetic counseling and testing. Genetic testing can find mutations in the RET gene, which is seen in cases of familial MTC and the MEN 2 syndromes.
If you have one of these mutations, it’s important that close family members (children, brothers, sisters, and parents) be tested as well. Because almost all children and adults with mutations in this gene will develop MTC at some time, most doctors agree anyone who has a RET gene mutation should have their thyroid removed to prevent MTC soon after getting the test results. This includes children, since some hereditary forms of MTC affect children and pre-teens. Total thyroidectomy can prevent this cancer in people with RET mutations who have not yet developed it. Of course, this means that lifelong thyroid hormone replacement will be needed.
Anaplastic carcinoma
Because this cancer is already widespread when it is diagnosed, surgery is often not helpful as treatment. If the cancer is confined to the area around the thyroid, which is rare, the entire thyroid and nearby lymph nodes may be removed. The goal of surgery is to remove as much cancer in the neck area as possible, ideally leaving no cancer tissue behind. Because of the way anaplastic carcinoma spreads, this is often difficult or impossible.
Radioactive iodine treatment does not work in this cancer and so is not used.
External beam radiation therapy may be used alone or combined with chemotherapy:
- To try to shrink the cancer before surgery to increase the chance of complete tumor removal
- After surgery to try to control any disease that remains in the neck
- When the tumor is too large or widespread to be treated by surgery
If the cancer is causing (or may eventually cause) trouble breathing, a hole may be placed surgically in the front of the neck and into the windpipe to bypass the tumor and allow the patient to breathe more comfortably. This hole is called a tracheostomy.
For cancers that have spread to distant sites, chemotherapy can be used, sometimes along with radiation therapy if the cancer is not too widespread. Because these cancers can be hard to treat, clinical trials of newer treatments are an option as well.
If Thyroid Cancer Treatments Are No Longer Working
If cancer keeps growing or comes back after one kind of treatment, it may be possible to try another treatment plan that might still cure the cancer, or at least shrink the tumors enough to help you live longer and feel better. But when a person has tried many different treatments and the cancer has not gotten any better, the cancer tends to become resistant to all treatment. If this happens, it’s important to weigh the possible limited benefits of a new treatment against the possible downsides, including treatment side effects. Everyone has their own way of looking at this.
This is likely to be the hardest part of your battle with cancer – when you have been through many medical treatments and nothing’s working anymore. Your doctor may offer you new options, but at some point you may need to consider that treatment is not likely to improve your health or change your outcome or survival.
If you want to continue to get treatment for as long as you can, you need to think about the odds of treatment having any benefit and how this compares to the possible risks and side effects. In many cases, your doctor can estimate how likely it is the cancer will respond to treatment you are considering. For instance, the doctor may say that more treatment might have about a 1 in 100 chance of working. Some people are still tempted to try this. But it is important to think about and understand your reasons for choosing this plan.
No matter what you decide to do, it is important that you feel as good as you can. Make sure you are asking for and getting treatment for any symptoms you might have, such as nausea or pain. This type of treatment is called palliative care.
Palliative care helps relieve symptoms, but is not expected to cure the disease. It can be given along with cancer treatment, or can even be cancer treatment. The difference is its purpose – the main goal is to improve the quality of your life, or help you feel as good as you can for as long as you can. Sometimes this means using drugs to help with symptoms like pain or nausea. Sometimes, though, the treatments used to control your symptoms are the same as those used to treat cancer. For instance, radiation might be used to help relieve bone pain caused by cancer that has spread to the bones. But this is not the same as treatment to try to cure the cancer.
At some point, you may benefit from hospice care. This is special care that treats the person rather than the disease; it focuses on quality rather than length of life. Most of the time, it is given at home. Your cancer may be causing problems that need to be managed, and hospice focuses on your comfort. You should know that while getting hospice care often means the end of treatments such as chemo and radiation, it doesn’t mean you can’t have treatment for the problems caused by your cancer or other health conditions. In hospice, the focus of your care is on living life as fully as possible and feeling as well as you can at this difficult time. You can learn more about hospice in our document called Hospice Care.
Staying hopeful is important, too. Your hope for a cure may not be as bright, but there is still hope for good times with family and friends – times that are filled with happiness and meaning. Pausing at this time in your cancer treatment gives you a chance to refocus on the most important things in your life. Now is the time to do some things you’ve always wanted to do and to stop doing the things you no longer want to do. Though the cancer may be beyond your control, there are still choices you can make.
- https://cancerstatisticscenter.cancer.org/#!/cancer-site/Thyroid[↩]