Contents
What is trigger finger
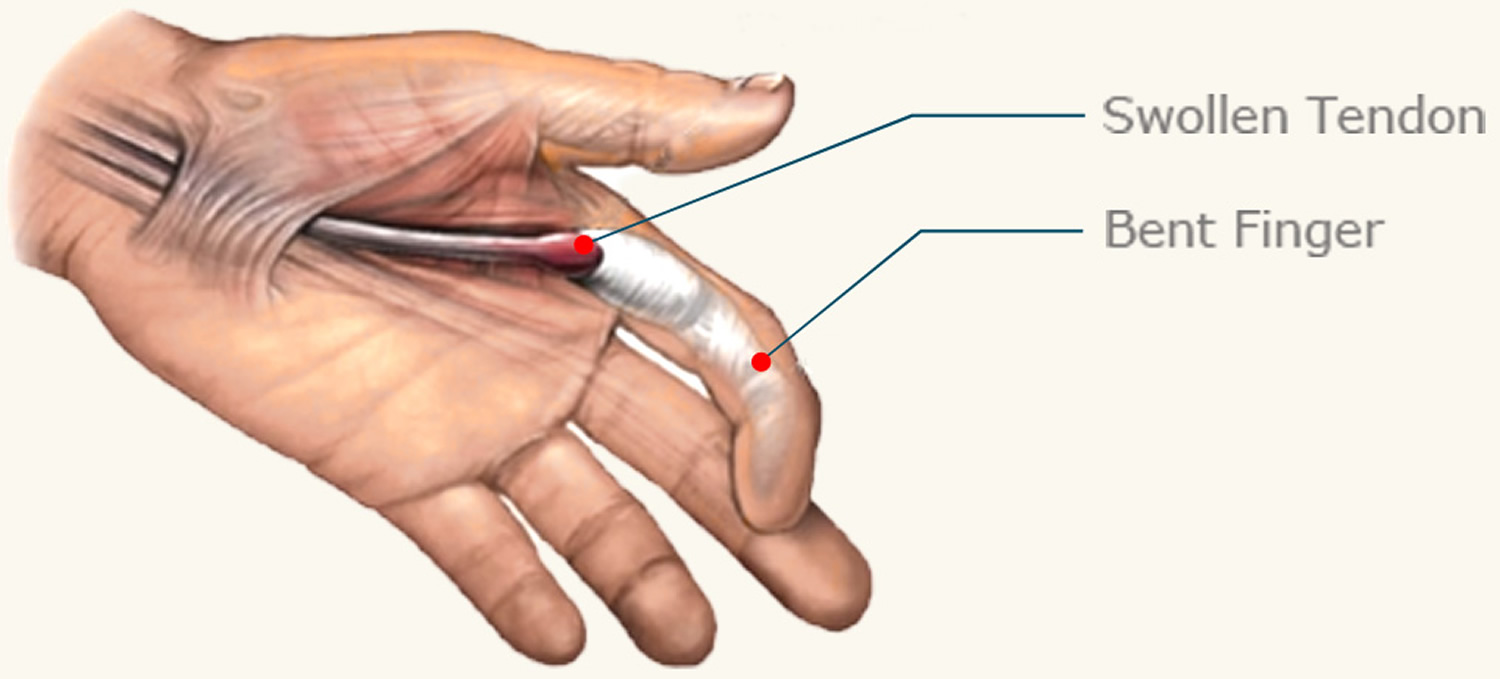
Trigger finger is a painful condition that affects one or more of the hand’s tendons, making it difficult to bend the affected finger or thumb. Trigger finger is usually caused by swelling of one of the tendons that run along your fingers and thumbs (see Figures 1 and 2), although the exact reason why this occurs isn’t fully understood.
If the tendon becomes swollen and inflamed it can ‘catch’ in the tunnel it runs through (the tendon sheath). This can make it difficult to move the affected finger or thumb causing the pain and stiffness associated with a clicking sensation.
The swelling can cause a section of the tendon to become bunched into a small lump (nodule) at the base of the affected finger or thumb.
If a nodule forms, the tendon can get trapped in the tendon sheath, causing the affected finger or thumb to become temporarily stuck in a bent position. The affected tendon may then suddenly break free, releasing your finger like the release of a trigger.
Trigger finger is also known as stenosing tenosynovitis or stenosing tenovaginosis. Tenosynovitis is an inflammation of the tendons, tendon sheaths and synovial membranes surrounding certain joints. Trigger finger usually affects the thumb, ring finger or little finger. One or more fingers can be affected, and the problem may develop in both hands. It’s more common in the right hand, which may be because most people are right-handed.
Trigger finger is generally less common in children than in adults, but sometimes young children aged between six months and two years develop it. It can affect the child’s ability to straighten their thumb, but it’s rarely painful and usually gets better without treatment.
Trigger Finger Anatomy
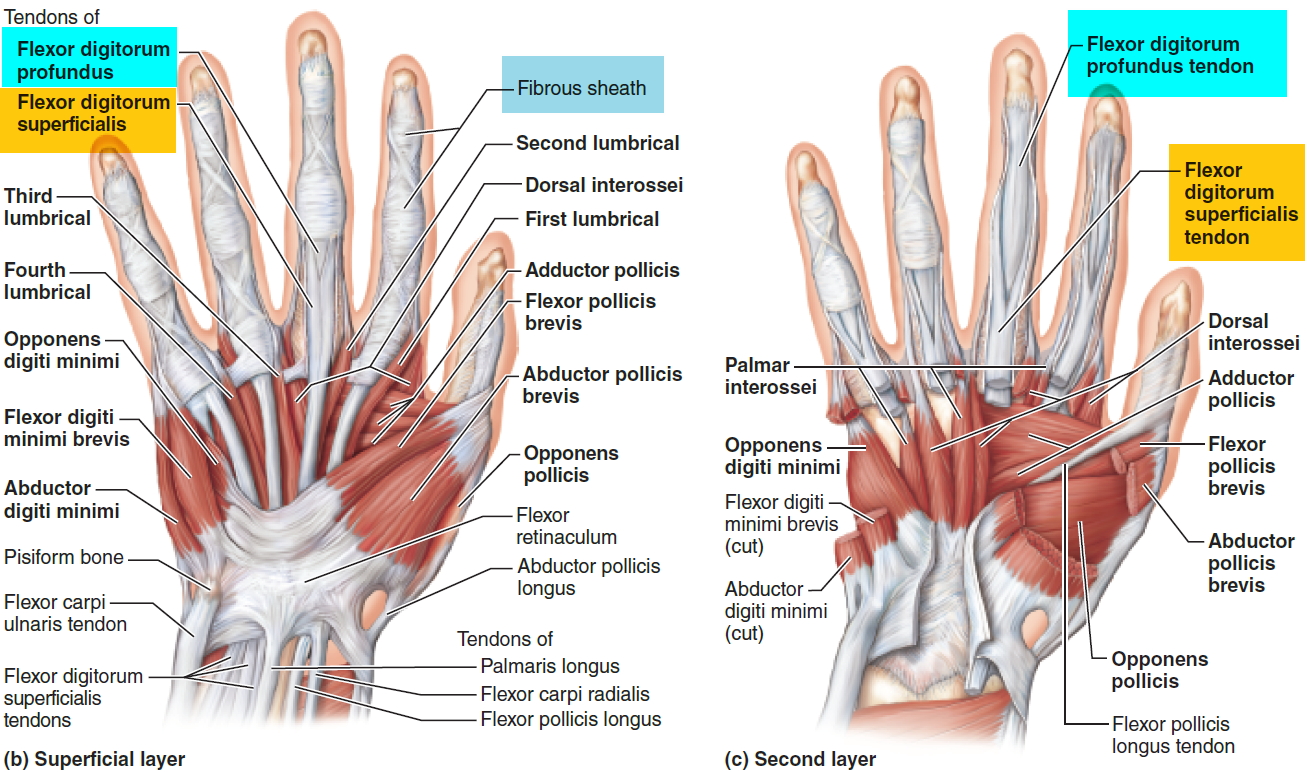
Tendons are tissues that connect muscles to bone. When muscles contract, tendons pull on bones. This is what causes some parts of the body to move.
The muscles that move the fingers and thumb are located in the forearm, above the wrist. Long tendons — called the flexor tendons — extend from the muscles through the wrist and attach to the small bones of the fingers and thumb.
These flexor tendons control the movements of the fingers and thumb. When you bend or straighten your finger, the flexor tendon slides through a snug tunnel, called the tendon sheath, that keeps the tendon in place next to the bones.
The flexor tendon can become irritated as it slides through the tendon sheath tunnel. As it becomes more and more irritated, the tendon may thicken and nodules may form, making its passage through the tunnel more difficult.
The tendon sheath may also thicken, causing the opening of the tunnel to become smaller.
If you have trigger finger, the tendon becomes momentarily stuck at the mouth of the tendon sheath tunnel when you try to straighten your finger. You might feel a pop as the tendon slips through the tight area and your finger will suddenly shoot straight out.
Figure 1. Finger tendons and tendon sheaths
Figure 2. Trigger finger
Symptoms of trigger finger can include pain at the base of the affected finger or thumb when you move it or press on it, and stiffness or clicking when you move the affected finger or thumb, particularly first thing in the morning.
If the condition gets worse, your finger may get stuck in a bent position and then suddenly pop straight. Eventually, it may not fully bend or straighten.
See your doctor if you think you may have trigger finger. They’ll examine your hand and advise you about appropriate treatments.
Trigger finger causes
Tendons are tough cords that join bone to muscle. They move the bone when the muscle contracts. In the hand, tendons run along the front and back of the bones in the fingers and are attached to the muscles in the forearm.
The tendons on the palm side of the hand (flexor tendons) are held in place by strong bands of tissue, known as ligaments, which are shaped in arches over the tendon. The tendons are covered by a protective sheath which produces a small amount of fluid to keep the tendons lubricated. This allows them to move freely and smoothly within the sheath when the fingers are bent and straightened (see Figure 1).
Trigger finger occurs if there’s a problem with the tendon or sheath, such as inflammation and swelling (tenosynovitis). The tendon can no longer slide easily through the sheath and can bunch up to form a small lump (nodule). This makes bending the affected finger or thumb difficult. If the tendon gets caught in the sheath, the finger can click painfully as it’s straightened.
The exact reason why these problems occur isn’t known, but several factors may increase the likelihood of trigger finger developing. For example, it’s more common in women, people over 40 years of age, and those with certain medical conditions.
There are factors that put people at greater risk for developing trigger finger.
- Trigger fingers are more common in women than men.
- They occur most frequently in people who are between the ages of 40 and 60 years of age.
- Trigger fingers are more common in people with certain medical problems, such as diabetes and rheumatoid arthritis.
- Trigger fingers may occur after activities that strain the hand.
Another hand-related condition called Dupuytren’s contracture can also increase your risk of developing trigger finger. In Dupuytren’s contracture, the connective tissue in the palm of the hand thickens, causing one or more fingers to bend into the palm of the hand.
Long-term conditions, such as diabetes and rheumatoid arthritis, are also sometimes associated with trigger finger.
Risk factors for developing trigger finger
The exact cause of trigger finger isn’t fully understood. However, you’re more at risk of developing trigger finger if:
- you’re female (trigger finger is more common in women than men)
- you’re aged in your 40s or 50s (trigger finger is more common in these age groups)
- you’ve had a previous hand injury – trigger finger may be more likely to develop after injuring the base of your finger or palm
Other health conditions
You may also be more likely to develop trigger finger if you have any of the following conditions:
- Diabetes – a lifelong condition that causes a person’s blood sugar level to become too high
- Rheumatoid arthritis – a long-term condition caused by a problem with your immune system (the body’s natural defence system), resulting in pain and stiffness in your joints
- Gout – a type of arthritis where crystals of sodium urate form inside and around joints causing them to become inflamed (swollen)
- Amyloidosis – a condition where an abnormal protein called amyloid builds up in organs, such as your liver
- Underactive thyroid (hypothyroidism) – where your body doesn’t produce enough of certain hormones
- Carpal tunnel syndrome – a condition that affects the nerves in your wrist, causing pain and tingling
- Dupuytren’s contracture – a condition that causes one or more fingers to bend into the palm of your hand
- De Quervain’s disease – a condition that affects the tendons in your thumb, causing pain in your wrist.
Trigger finger symptoms
Symptoms of trigger finger usually start without any injury, although they may follow a period of heavy hand use. Trigger finger may start with discomfort felt at the base of the finger or thumb, where the finger joins the palm. This area is often sensitive to pressure. You might feel a lump there.
Symptoms may include:
- A tender lump in your palm
- Swelling
- Limited finger movement
- Catching or popping sensation in your finger or thumb joints
- Pain when bending or straightening your finger
Stiffness and catching tend to be worse after inactivity, such as when you wake in the morning. Your fingers will often loosen up as you move them.
Sometimes, when the tendon breaks free, it may feel like your finger joint is dislocating. In severe cases of trigger finger, the finger cannot be straightened, even with help. Sometimes, one or more fingers are affected.
Trigger finger diagnosis
Your doctor can diagnose the problem by talking with you and examining your hand. No other testing or x-rays are usually needed to diagnose trigger finger.
Trigger finger treatment
The treatment for trigger finger depends on the severity of your symptoms and how long you’ve had them.
In some people, trigger finger may get better without treatment, so your doctor may recommend avoiding activities that cause the pain to see if this helps relieve your symptoms. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may also be helpful in relieving any pain.
However, if it isn’t treated, there’s a chance the affected finger or thumb could become permanently bent, which will make performing everyday tasks difficult.
If treatment is necessary, several options are available, including:
- Rest and medication – If symptoms are mild, resting the finger may be enough to resolve the problem. Avoiding certain activities and taking non-steroidal anti-inflammatory drugs (NSAIDs) may help relieve pain.
- Splinting, where the affected finger is strapped to a plastic splint to keep your finger in a neutral, resting position and reduce movement.
- Corticosteroid injections (steroids are medicines that can reduce swelling).
- Surgery on the affected sheath – surgery involves releasing the affected sheath to allow the tendon to move freely again. It’s usually used when other treatments have failed. It can be up to 100% effective, although you may need to take two to four weeks off work to fully recover.
Treating children with trigger finger
Trigger finger in children will often improve without treatment as the child gets older, although splinting and simple hand stretches may help.
Steroid injections aren’t usually used in children, but surgery under general anesthetic can be carried out if necessary.
Trigger finger splint
Strapping your affected finger or thumb to a plastic splint can ease your symptoms by stopping your finger moving. If your finger is particularly stiff in the morning, it may help to use a splint overnight. Your doctor can advise you about how long you need to wear the splint for.
Using a splint can be helpful for some people, but it’s generally less effective than the treatments described below, particularly in the long-term.
Figure 3. Trigger finger splint
Trigger finger injection
Corticosteroid injections: Corticosteroids are medicines that can be used to reduce swelling. In cases of trigger finger, liquid corticosteroids are injected into the tendon sheath (the membrane that the tendon slides through), at the base of the affected finger or thumb.
Corticosteroids are thought to work by reducing swelling of the tendon, allowing the tendon to move freely again. This can sometimes happen within a few days of having the injection, but it usually takes a few weeks.
It’s estimated that corticosteroid injections are an effective treatment for 50–80% of people with trigger finger. However, they’re generally less effective in people with certain underlying health conditions, such as diabetes and rheumatoid arthritis.
A corticosteroid injection can permanently improve trigger finger but, in some cases, the problem can return after treatment. You can have a second injection if the effect wears off, but it’s often less effective than the first injection.
The risks of corticosteroid injections for trigger finger are small. Very occasionally, it causes some thinning or color change in the skin at the site of injection. There’s also a very small risk of infection.
Trigger finger surgery
Surgery may be recommended if the above treatments don’t work or are unsuitable. The surgeon will cut through the affected section of the tendon sheath so that your tendon can move freely again.
Whether surgery is recommended will depend on considerations such as the amount of pain you’re in, whether it’s associated with other medical problems, such as rheumatoid arthritis, and how much it’s affecting your life.
In most cases, trigger finger is a nuisance rather than a serious condition. However, if it isn’t treated, the affected finger or thumb may become permanently stuck in a bent position or, less commonly, in a straightened position. This can make carrying out everyday tasks difficult.
Surgery for trigger finger is effective and it’s rare for the problem to return in the treated finger or thumb. However, you may need to take some time off work and there’s a risk of complications (see below).
The operation takes around 20 minutes, and you won’t need to stay in hospital overnight. The procedure is usually carried out under local anesthetic, so you’ll be awake but unable to feel any pain in your hand.
The two types of surgery for trigger finger are:
- open trigger finger release surgery
- percutaneous trigger finger release surgery
If you have rheumatoid arthritis, these types of surgery may not be recommended because they can cause your finger to drift sideways. Instead, a procedure known as a tenosynovectomy may be necessary. This involves removing part of the tendon sheath to allow the tendon to move again.
Open trigger finger release surgery
If you have open trigger finger release surgery, the surgeon will give you an injection of local anesthetic into the palm of your hand.
A small incision will be made in the palm of your hand along one of the natural creases, which may mean the scar will be less noticeable. The surgeon will carefully cut through the tendon sheath to make it wider. The wound will then be closed with stitches and covered with a light bandage.
Percutaneous trigger finger release surgery
Percutaneous means ‘through the skin’. As with open surgery, the surgeon will inject your hand with a local anesthetic. However, instead of making an incision in your palm, a needle will be inserted into the base of the affected finger and used to slice through the ligament to get to the tendon.
As percutaneous surgery doesn’t involve making an incision, you won’t have a wound or scar. However, the procedure is slightly more risky than open surgery and may be less effective at resolving the problem. Important nerves and arteries are very close to the tendon sheath and can easily be damaged. For this reason, open surgery is usually the preferred method.
Complications of surgery
Trigger finger release surgery is a safe procedure. However, as with any type of surgery, there are some risks. Complications are rare, but could include:
- Infection
- Stiffness or pain in the finger
- Incomplete extension — due to persistent tightness of the tendon sheath beyond the part that was released
- Persistent triggering — due to incomplete release of the first part of the sheath
- A tender scar
- Nerve damage (if a nerve is damaged during surgery, you may never recover the full sensation in the affected area)
- Tendon bowstringing, where the tendon is in the wrong position or due to excessive release of the sheath
- complex regional pain syndrome (CRPS), which causes pain and swelling in your hand after surgery – this usually resolves itself after a few months, but there can be permanent problems
Before your operation, ask your surgeon to discuss the possible complications and risks with you in more detail.
Recovering from surgery
After the procedure, you should be able to move your finger straight away. The dressings can usually be removed after a few days to make movement easier, and full movement should return within a week or two.
If you’ve had open surgery, your palm may feel sore immediately after the procedure, but any discomfort should pass within two weeks.
You can start driving again as soon as you feel it’s safe for you to drive, which is usually after three to five days. You may be able to write and use a computer immediately.
You can play sports after around two or three weeks, once your wound has healed and you can grip again.
When you can return to work will depend on your job. If you have a desk job or a role that involves light manual duties, you may not need any time off work. If your job involves manual labor, you may need up to four weeks off.
If you’ve had surgery on more than one finger, your recovery period may be longer.
If you’ve had percutaneous surgery rather than open trigger finger release surgery, your recovery period may be shorter because you won’t have a wound on your palm.
If your finger was quite stiff before surgery, physical therapy and finger exercises may help loosen it up.
Caring for your wound
If you’ve had open surgery, your surgeon should advise you about how to care for the wound in your palm. Washing it with mild soap and warm water is usually all that’s required.
If you have stitches, you’ll be told if you need to return to hospital to have them removed. Some stitches are dissolvable and will disappear on their own in around three weeks.
After your wound has healed, you may be left with a small scar running along your palm, where the incision was made. Read more about scars.
Trigger finger exercises
If your finger was quite stiff before surgery, you may need specialized hand therapy after your operation to loosen it. Discuss this with your surgeon before the operation. Your doctor may also suggest gentle stretching exercises to help maintain mobility in your finger.
- Start with your fingers straight
- Bend the tips of your fingers into a hook, whilst keeping the large knuckles up straight
- Make a tabletop by bending the large knuckles and keeping the rest of the joints straight
- Touch your palm keeping the end joints straight
- Make a full fist by bending all of the joints
Figure 4. Trigger finger exercises
The types of therapy you may need include:
- physiotherapy – where manipulation, massage and exercises are used to improve the movement and function of your hand
- occupational therapy – if you’re struggling with everyday tasks and activities, either at work or at home, an occupational therapist will be able to give you practical support to make those tasks easier.