Contents
- What is Vancomycin
- Vancomycin mechanism of action
- What is vancomycin used for?
- Vancomycin contraindications
- Vancomycin special precautions
- Vancomycin administration
- Vancomycin dose
- Vancomycin oral dose
- Vancomycin IV dose
- Adult dose for Bacterial Infection
- Adult dose for Endocarditis
- Adult dose for Pneumonia
- Adult dose for Nosocomial Pneumonia
- Adult dose for Osteomyelitis
- Adult dose for Sepsis
- Adult dose for Skin or Soft Tissue Infection
- Adult dose for Bacteremia
- Adult dose for Meningitis
- Adult dose for CNS Infection
- Adult dose for Febrile Neutropenia
- Adult dose for Intraabdominal Infection
- Adult dose for Peritonitis
- Adult dose for Prevention of Perinatal Group B Streptococcal Disease
- Adult dose for Shunt Infection
- Adult dose for Surgical Prophylaxis
- Adult dose for Head Injury
- Pediatric dose for Bacteremia
- Pediatric dose for Osteomyelitis
- Pediatric dose for Bacterial Infection
- Pediatric dose for Sepsis
- Pediatric dose for Endocarditis
- Pediatric dose for Skin or Soft Tissue Infection
- Pediatric dose for Pneumonia
- Pediatric dose for Intraabdominal Infection
- Pediatric dose for Peritonitis
- Pediatric dose for Surgical Prophylaxis
- Pediatric dose for Meningitis
- Pediatric dose for CNS Infection
- Pediatric dose for Shunt Infection
- Pediatric dose for Head Injury
- Renal dose Adjustments
- Liver Dose Adjustments
- What should I do if I forget a dose?
- Vancomycin side effects
- Vancomycin toxicity
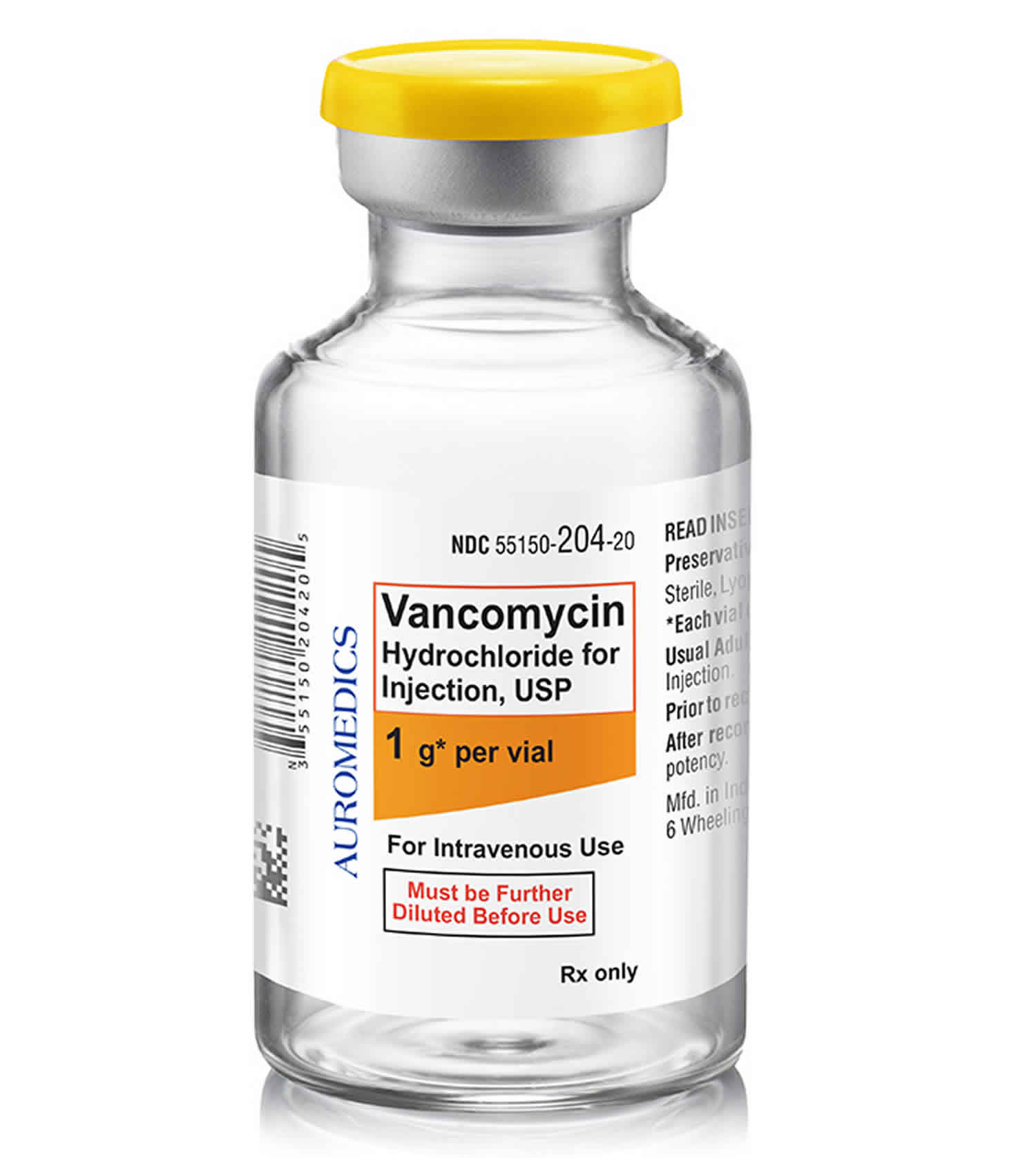
What is Vancomycin
Vancomycin is a broad spectrum tricyclic glycopeptide antibiotic that has activity against methicillin-resistant Staphylococcus aureus (MRSA) and is generally reserved for serious drug resistant gram-positive bacteria infections. Vancomycin antibiotic is originally derived from the organism Streptococcus orientalis with primary activity against gram positive bacteria 1. Vancomycin is also utilized for streptococci, enterococci, and methicillin-susceptible Staphylococcus aureus (MSSA) infections. Vancomycin has numerous FDA-approved and off-label clinical uses 2. Vancomycin was first approved for use in the United States in 1958 and it continues to be widely used, particularly with the recent rise in incidence of serious methicillin-resistant Staphylococcus aureus (MRSA) infections.
Vancomycin has a large, complex and unusual structure and is believed to act by inhibition of bacterial cell wall synthesis via binding to the cell wall precursor molecules. Vancomycin is active against, and its major use is in therapy of, infections due to methicillin-resistant Staphylococcus aureus (MRSA), including antibiotic-induced pseudomembranous colitis, staphylococcal enterocolitis, bacterial endocarditis, and sepsis. For systemic infections, vancomycin is given intravenously. For localized or nonsystemic infections, other routes of administration are used, including oral, rectal, topical, inhalational, intrathecal, intraperitoneal, and intraventricular.
The recommended vancomycin parenteral dosage in adults is 500 mg iv every 6 hours or 1000 mg every 12 hours, with modification to achieve a therapeutic range as needed. The recommended oral dosage in the treatment of antibiotic induced pseudomembranous enterocolitis is 125 to 500 mg every 6 hours for 7 to 10 days. Vancomycin is available generically and under several commercial names including Vancoled, Vancor, Lyphocin, and Vancocin in 125 and 250 mg pulvules and as power for injection or oral administration.
Vancomycin is largely well tolerated; common side effects include diarrhea, nausea, nephrotoxicity and neutropenia.
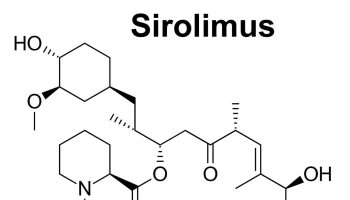
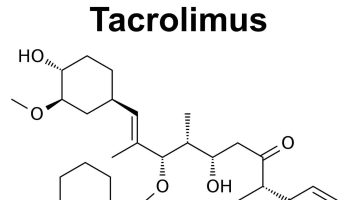
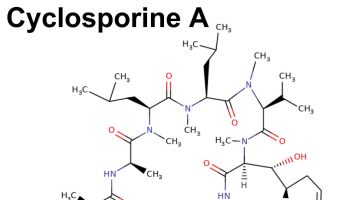
Vancomycin mechanism of action
Vancomycin is a glycopeptide antibiotic that exerts its bactericidal effect by inhibiting the polymerization of peptidoglycans in the bacterial cell wall. The bacterial cell wall contains a rigid peptidoglycan layer that has a highly cross-linked structure composed of long polymers of N-acetylmuramic acid (NAM) and N-acetylglucosamine (NAG). Vancomycin binds to D-alanyl D-alanine which inhibits glucosyltransferase (peptidylglycan synthase) and the P-phospholipid carrier, thereby preventing the synthesis and polymerization of N-acetylmuramic acid and N-acetylglucosamine within in the peptidoglycan layer. This inhibition weakens bacterial cell walls and ultimately causes leakage of intracellular components, resulting in bacterial cell death. Vancomycin is only active against gram-positive bacteria 3.
What is vancomycin used for?
Vancomycin injection is used alone or in combination with other medications to treat certain serious infections such as endocarditis (infection of the heart lining and valves), peritonitis (inflammation of the lining of the abdomen), and infections of the lungs, skin, blood, and bones. Vancomycin injection is in a class of medications called glycopeptide antibiotics. It works by killing bacteria that cause infections.
Antibiotics such as vancomycin injection will not work for colds, flu, or other viral infections. Taking or using antibiotics when they are not needed increases your risk of getting an infection later that resists antibiotic treatment.
FDA-approved clinical uses of Vancomycin 1:
- Clostridium difficile-associated diarrhea (oral administration)
- Staphylococcus enterocolitis
- Pseudomembranous colitis
- Endocarditis: Diphtheroid, Enterococcal, Staphylococcal, and Streptococcal species.
- Staphylococcal infections: septicemia, skin and soft tissue infections, bone infections, lower respiratory tract infections, etc.
Off-Label clinical uses of Vancomycin include 1:
- Catheter-related infections
- Community-acquired bacterial pneumonia
- Clostridium difficile infection
- Neonatal prophylaxis for Group B streptococcus
- Intra-abdominal infections due to MRSA or ampicillin-resistant enterococci
- Bacterial meningitis
- Bacterial endophthalmitis (systemic or intravitreal administration)
- Native vertebral osteomyelitis
- Peritonitis
- Prosthetic joint infection
- Necrotizing skin and soft tissue infections
- Surgical prophylaxis
- Surgical-site infections
Vancomycin contraindications
Vancomycin is contraindicated in patients with a known hypersensitivity reaction to the drug or any component within the formulation 4.
Although vancomycin does not have many contraindications, there are some important clinical considerations to keep in mind during patient care.
Vancomycin special precautions
Before using vancomycin injection:
- tell your doctor and pharmacist if you are allergic to vancomycin, any other medications, or any of the ingredients in vancomycin injection. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: amikacin, amphotericin (Abelcet, Ambisome, Amphotec), bacitracin (Baciim); cisplatin, colistin, kanamycin, neomycin (Neo-Fradin), paromomycin, polymyxin B, streptomycin, and tobramycin. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had hearing problems or kidney disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while using vancomycin injection, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are receiving vancomycin injection.
Vancomycin may cause a rare but serious type of an allergic reaction called an infusion reaction. This can be life-threatening and require immediate medical attention. Tell your doctor right away if you or your child starts to have cough, difficulty with swallowing, dizziness, fast heartbeat, trouble with breathing, chest tightness, swelling in your face or hands, fever, chills, itching or hives, or lightheadedness or faintness while you are receiving vancomycin.
Tell your doctor right away if you or your child have confusion, dizziness, headache, decrease in how much or how often you urinate, rapid weight gain, swelling of your hands, ankles, or feet after receiving vancomycin. This may be symptom of a serious kidney problem.
Hearing loss may occur while you are receiving vancomycin. Tell your doctor if you or your child have ringing or buzzing in the ears, dizziness, feeling of fullness in the ears, or loss of balance after receiving vancomycin.
Vancomycin may cause diarrhea, and in some cases it can be severe. It may occur 2 months or more after you stop using vancomycin. Do not take any medicine to treat diarrhea without first checking with your doctor. If you have any questions or if mild diarrhea continues or gets worse, check with your doctor.
Vancomycin can temporarily lower the number of white blood cells in your blood, increasing the chance of getting an infection. If you can, avoid people with infections. Check with your doctor immediately if you think you are getting an infection or if you get a fever or chills, cough or hoarseness, lower back or side pain, or painful or difficult urination.
Vancomycin may cause severe tenderness and pain at the injection site. Contact your doctor right away if you notice any of these side effects at the injection site: bleeding, blistering, burning, coldness, discoloration of the skin, feeling of pressure, hives, infection, inflammation, itching, lumps, numbness, pain, rash, redness, scarring, soreness, stinging, swelling, tenderness, tingling, ulceration, or warmth.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Geriatric
Elderly patients are more prone to vancomycin toxicity with IV administration due to age-related changes in renal function, the volume of distribution, and accumulation. These patients need to be carefully monitored and may require a more conservative dosage regimen.
Vancomycin in Pregnancy
Oral vancomycin capsules are currently listed as a category B drug for use in pregnancy whereas the intravenous vancomycin injection is listed as category C. Vancomycin should not be used during pregnancy unless the benefits outweigh the risks of the medication. If treatment with vancomycin is necessary, close monitoring of maternal blood is recommended to reduce the risk of ototoxicity and nephrotoxicity in the fetus. Animal studies have not yet determined any evidence of fetal harm from maternal vancomycin use. However, vancomycin crosses the placenta and has been detected in fetal serum, amniotic fluid, and cord blood. Patients who become pregnant while taking vancomycin should contact their healthcare provider immediately. Moreover, it is important to note that pregnant patients may require higher doses of vancomycin to achieve therapeutic concentrations due to alterations in pharmacokinetics, such as an increased volume of distribution and total plasma clearance.
Vancomycin in Breastfeeding
Vancomycin is excreted in breast milk following intravenous administration. In comparison, oral vancomycin has minimal systemic absorption, and therefore, limited excretion through breast milk. Breastfeeding mothers who receive intravenous vancomycin should be advised to consult with their provider before continuing as it may affect the health of their baby. Nevertheless, vancomycin is recommended for the treatment of Clostridium difficile infections in breastfeeding women. Careful assessment regarding the discontinuation of breastfeeding is recommended before initiating vancomycin therapy in nursing mothers.
Renal Impairment
The reduced renal function can cause vancomycin to accumulate in the body, thereby increasing the risk of adverse effects. Dosing adjustments are necessary for renal impairment. Close monitoring of vancomycin trough concentrations is necessary for all patients with renal impairment. Patients should be advised to contact their provider if they experience symptoms of reduced kidney function, such as decreased urine output, swelling, and abdominal pain as vancomycin may exacerbate renal impairment.
Bacterial Resistance
Similar to other antimicrobials, prolonged or inappropriate treatment with vancomycin can lead to bacterial resistance such as Vancomycin-resistant enterococci (VRE). Providers need to be aware of increased antimicrobial resistance patterns and practice appropriate antimicrobial stewardship. Moreover, patients should be counseled on the importance of medication adherence to prevent the development of multidrug-resistant infections.
Vancomycin Drug Interactions
Co-administration of other medications along with vancomycin may increase the risk of adverse effects and toxicity. Therefore dosing adjustments, additional monitoring, and consideration of alternative treatment should be considered when combining vancomycin with certain medications. Caution is advised when administering vancomycin with other nephrotoxic agents such as aminoglycosides, amphotericin products, and IV contrast.
Using vancomycin with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amikacin
- Cholera Vaccine, Live
- Gentamicin
- Piperacillin
- Tobramycin
Using vancomycin with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Succinylcholine
- Warfarin
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of vancomycin. Make sure you tell your doctor if you have any other medical problems, especially:
Allergy to corn or corn products—Should not be used in patients with this condition.
- Congestive heart failure or
- Hearing loss or
- Kidney disease—Use with caution. May cause side effects to become worse.
Vancomycin administration
Vancomycin is FDA-approved for administration by either intravenous injection or oral route. Rectal administration is an off-label use of vancomycin that can be used to treat Clostridium difficile infection. Administration is dependent on the type and location of the infection. Vancomycin has poor oral bioavailability; therefore, it must be administered intravenously in order to treat most infections 5.
Intravenous vancomycin injection can be used to treat MRSA infections as well as other susceptible gram-positive organisms. The dose of vancomycin required is dependent on the type and severity of infection, the patient’s overall clinical presentation, renal function, and body weight. The desired intravenous dose should be administered slowly over at least 60 minutes. The frequency of administration ranges from every 8 to 24 hours and should be adjusted based on renal function, age, and serum trough concentrations. Serum trough concentrations should be closely monitored in all patients.
Oral vancomycin has low systemic absorption and is only effective for treating intestinal infections. Therefore, it is only indicated for treatment of Clostridium difficile-associated diarrhea, pseudomembranous colitis, and Staphylococcal enterocolitis. Oral vancomycin is not an appropriate treatment option for systemic infections affecting other organs or parts of the body. Oral vancomycin is currently available as capsules and an oral solution. It is typically administered four times a day for a period of 7 to 10 days. However, the exact dose and length of therapy are determined by multiple factors, including indication, assessment of the patient’s clinical presentation, and the severity of an infection. Oral vancomycin does not require dosage adjustment for renal impairment due to its low systemic absorption. Moreover, routine serum trough monitoring is not recommended for patients who are only receiving oral vancomycin 6.
Pharmacodynamics/Kinetics:
- Route of administration: Intravenous, oral, rectal administration (off-label)
- Inhibition of bacterial growth: Slowly bactericidal
- PK/PD parameter: AUC:MIC
- Absorption: Oral vancomycin has a bioavailability of less than 10%.
- Onset of action: Vancomycin has a rapid onset of action with a serum peak concentration immediately following the completion of the intravenous infusion. The onset of action of oral vancomycin is currently unknown.
- Distribution: Large volume of distribution (0.4 L/kg to 1.0 L/kg) in body tissues and fluids, excluding cerebrospinal fluid (CSF) with non-inflammed meninges
- Protein Binding: approximately 55%
- Metabolism: No evident metabolism (excreted unchanged)
- Clearance: 0.71 mL/minute/kg to 1.31 mL/minute/kg in adults with normal renal function
- Half-life: Vancomycin has a bi-phasic elimination half-life with its initial half-life being relatively quick and terminal half-life of 4 to 6 hours in healthy adults with normal renal function. The elimination half-life is significantly prolonged in patients with renal dysfunction. Close monitoring is required in these patients.
- Excretion: Intravenous vancomycin injection is primarily eliminated by glomerular filtration in the kidney (75% via urine). Oral vancomycin is predominantly excreted in feces.
- Therapeutic drug monitoring/range: 10 to 20 mcg/mL (trough)
- AAP Recommendations:
- Invasive MRSA infections: At least a 400 mghr/L 24-hour AUC to MIC ratio is recommended.
- Neonates with a MIC 1 mg/L: 10 to 12 mg/L (trough)
Vancomycin dose
Vancomycin oral dose
The dose of vancomycin will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of vancomycin. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage forms (capsules or oral liquid):
For treatment of C. difficile-associated diarrhea:
- Adults—125 milligrams (mg) 4 times a day for 10 days.
- Children—Dose is based on body weight and must be determined by the doctor. The usual dose is 40 milligrams per kilogram (mg/kg) of body weight, divided into 3 or 4 doses, and taken for 7 to 10 days. However, the total daily dose is usually not more than 2000 mg per day.
For treatment of Staphylococcal enterocolitis:
- Adults—500 to 2000 milligrams (mg) divided into 3 or 4 doses for 7 to 10 days.
- Children—Dose is based on body weight and must be determined by the doctor. The usual dose is 40 milligrams per kilogram (mg/kg) of body weight, divided into 3 or 4 doses, and taken for 7 to 10 days. However, the total daily dose is usually not more than 2000 mg per day.
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Vancomycin IV dose
A nurse or other trained health professional will give you vancomycin IV in a hospital. Vancomycin is given through a needle placed in one of your veins.
Adult dose for Bacterial Infection
- 500 mg IV every 6 hours OR 1 g IV every 12 hours
Use: Empirical treatment of serious/severe staphylococcal infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
Comments:
- Vancomycin should be administered at a rate up to 10 mg/min or over 1 hour, whichever is longer.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Infectious Diseases Society of America (IDSA) Recommendations:
- 15 mg/kg IV every 12 hours
Uses:
- Preferred treatment for IV catheter-related bloodstream infections caused by methicillin-resistant Staphylococcus aureus (MRSA)/coagulase-negative staphylococci, ampicillin-resistant, vancomycin-sensitive E faecalis/E faecium, Corynebacterium jeikeium (Group JK)
- Alternative treatment for IV catheter-related bloodstream infections caused by methicillin-susceptible Staphylococcus aureus (MSSA)/coagulase-negative staphylococci, ampicillin-susceptible E faecalis/E faecium
Comments:
- Treatment plus an aminoglycoside should be used for ampicillin-resistant, vancomycin-sensitive Enterococcus faecalis/Enterococcus faecium.
Adult dose for Endocarditis
- 500 mg IV every 6 hours OR 1 g IV every 12 hours
Uses:
- Empirical treatment of staphylococcal endocarditis caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment (with an aminoglycoside) of endocarditis caused by enterococci, Streptococcus bovis, or Streptococcus viridans
- Empirical treatment (with an aminoglycoside and/or rifampin) of early-onset prosthetic valve endocarditis caused by Staphylococcus epidermidis or diphtheroids
Comments:
- Vancomycin should be administered at a rate up to 10 mg/min or over 1 hour, whichever is longer.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
- Successful treatment of diphtheroid endocarditis has been reported.
American Heart Association (AHA) and IDSA Recommendations:
- 15 to 20 mg/kg per day IV every 8 to 12 hours
- Maximum dose: 2 g/dose
Duration of treatment:
- Native Valve Endocarditis: At least 4 weeks
- Prosthetic Valve Endocarditis: At least 6 weeks
Uses:
- Treatment of endocarditis caused by highly penicillin-susceptible and relatively resistant to penicillin viridians group streptococci (VGS) and Streptococcus gallolyticus (bovis) in patients who cannot tolerate penicillin or ceftriaxone
- Treatment of endocarditis involving a prosthetic value/other prosthetic material caused by VGS and S gallolyticus (bovis)
- Alternative treatment of endocarditis caused by oxacillin-resistant staphylococci in patients with immediate-type hypersensitivity to beta-lactam antibiotics
- Treatment of penicillin-resistant endocarditis caused by enterococci in patients unable to tolerate beta-lactam antibiotics
Comments:
- Patients may not require the addition of gentamicin or rifampin.
- Patients with native valve endocarditis caused by oxacillin-resistant staphylococci may require at least 6 weeks of treatment.
Adult dose for Pneumonia
- 500 mg IV every 6 hours OR 1 g IV every 12 hours
Use:
- Empirical treatment of lower respiratory tract infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
Comments:
- Vancomycin should be administered at a rate up to 10 mg/min or over 1 hour, whichever is longer.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
IDSA Recommendations:
- 15 mg/kg IV every 8 to 12 hours
- Some experts recommend a loading dose of 25 to 30 mg/kg IV ONCE (severe illness)
Uses:
- Empiric treatment of clinically suspected ventilator-associated pneumonia where MRSA coverage is appropriate
- Add-on empiric treatment of hospital-acquired pneumonia in patients not at high risk of mortality but with MRSA risk factors
- Add-on empiric treatment of hospital-acquired pneumonia in patients at high risk of mortality or with receipt of IV antibiotics within the previous 90 days
Adult dose for Nosocomial Pneumonia
- 500 mg IV every 6 hours OR 1 g IV every 12 hours
Use:
- Empirical treatment of lower respiratory tract infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
Comments:
- Vancomycin should be administered at a rate up to 10 mg/min or over 1 hour, whichever is longer.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
IDSA Recommendations:
- 15 mg/kg IV every 8 to 12 hours
- Some experts recommend a loading dose of 25 to 30 mg/kg IV ONCE (severe illness)
Uses:
- Empiric treatment of clinically suspected ventilator-associated pneumonia where MRSA coverage is appropriate
- Add-on empiric treatment of hospital-acquired pneumonia in patients not at high risk of mortality but with MRSA risk factors
- Add-on empiric treatment of hospital-acquired pneumonia in patients at high risk of mortality or with receipt of IV antibiotics within the previous 90 days
Adult dose for Osteomyelitis
- 500 mg IV every 6 hours OR 1 g IV every 12 hours
Use:
- Empirical treatment of bone infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
Comments:
- Vancomycin should be administered at a rate up to 10 mg/min or over 1 hour, whichever is longer.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
IDSA Recommendations:
- 15 to 20 mg/kg IV every 12 hours
- Duration of therapy: 4 to 6 weeks
Uses:
- First choice treatment for native vertebral osteomyelitis caused by oxacillin-resistant staphylococci, penicillin-resistant Enterococcus species
- Alternative treatment for native vertebral osteomyelitis caused by oxacillin-susceptible staphylococci
- Alternative treatment for native vertebral osteomyelitis caused by penicillin-susceptible Enterococcus species, Enterobacteriaceae, beta-hemolytic streptococci, or Propionibacterium acnes in patients allergic to penicillin
Adult dose for Sepsis
- 500 mg IV every 6 hours OR 1 g IV every 12 hours
Use:
- Empirical treatment of septicemia caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
Comments:
- Vancomycin should be administered at a rate up to 10 mg/min or over 1 hour, whichever is longer.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Adult dose for Skin or Soft Tissue Infection
- 500 mg IV every 6 hours OR 1 g IV every 12 hours
Use:
- Empirical treatment of skin and skin structure infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
Comments:
- Vancomycin should be administered at a rate up to 10 mg/min or over 1 hour, whichever is longer.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
IDSA Recommendations:
- 15 mg/kg IV every 6 to 12 hours
Comment: Multidrug resistant organisms may require daily doses up to 60 mg/kg.
Uses:
- First-line treatment of treatment of skin and soft tissue infections (SSTIs) caused by MRSA in patients who require parenteral treatment
- Alternative treatment of SSTIs in patients with penicillin allergies
- Treatment of incisional surgical site infections of the lower trunk or extremity away from the axilla/perineum
- First-line treatment of necrotizing infections of the skin, fascia, and muscle caused by mixed infections
Adult dose for Bacteremia
IDSA Recommendations:
- 15 to 20 mg/kg IV every 8 to 12 hours
- Duration of treatment: Up to 6 weeks, depending on the severity of infection
Use: Treatment of bacteremia
Adult dose for Meningitis
IDSA, American Academy of Neurology (AAN), American Association of Neurological Surgeons (AANS), and Neurocritical Care Society (NCS) Recommendations:
- 30 to 60 mg/kg IV per day, given in divided doses every 8 to 12 hours
- Some experts recommend: 15 mg/kg IV once, followed by 60 mg/kg per day continuous infusion
- Maximum dose: 2 g/dose
- Duration of treatment: At least 2 weeks
Comment: Surgical evaluation is recommended for patients with septic thromboses, empyema, and/or abscesses.
Uses:
- Treatment of patients with healthcare-associated ventriculitis and meningitis caused by methicillin-resistant staphylococci
- In combination with a third-generation cephalosporin, treatment of patients with healthcare-associated ventriculitis and meningitis caused by Streptococcus pneumoniae
- Alternative treatment of patients with healthcare-associated ventriculitis and meningitis caused by methicillin-sensitive staphylococci or P acnes
- Treatment of patients with brain abscess, subdural empyema, and/or spinal epidural abscess
- Treatment of patients with septic thrombosis of cavernous/dural venous sinus
Adult dose for CNS Infection
IDSA, American Academy of Neurology (AAN), American Association of Neurological Surgeons (AANS), and Neurocritical Care Society (NCS) Recommendations:
- 30 to 60 mg/kg IV per day, given in divided doses every 8 to 12 hours
- Some experts recommend: 15 mg/kg IV once, followed by 60 mg/kg per day continuous infusion
- Maximum dose: 2 g/dose
- Duration of treatment: At least 2 weeks
Comment: Surgical evaluation is recommended for patients with septic thromboses, empyema, and/or abscesses.
Uses:
- Treatment of patients with healthcare-associated ventriculitis and meningitis caused by methicillin-resistant staphylococci
- In combination with a third-generation cephalosporin, treatment of patients with healthcare-associated ventriculitis and meningitis caused by Streptococcus pneumoniae
- Alternative treatment of patients with healthcare-associated ventriculitis and meningitis caused by methicillin-sensitive staphylococci or P acnes
- Treatment of patients with brain abscess, subdural empyema, and/or spinal epidural abscess
- Treatment of patients with septic thrombosis of cavernous/dural venous sinus
Adult dose for Febrile Neutropenia
National Comprehensive Cancer Network (NCCN) Recommendations:
- 15 mg/kg IV every 12 hours
Use:
- Empiric prophylaxis in patients at high-risk for febrile neutropenia caused by serious gram-positive infections
Comments:
- Vancomycin should not be used as routine therapy for febrile neutropenia.
- Empiric therapy should be reassessed within 2 to 3 days of initiation. If gram-positive organisms are not found, discontinuation of treatment should be considered.
- Patients with resolved fever and neutrophil counts of at least 500 cells/mcL may discontinue therapy.
Adult dose for Intraabdominal Infection
Surgical Infection Society (SIS) and IDSA Recommendations:
- 15 to 20 mg/kg IV every 8 to 12 hours
Uses:
- Empiric treatment of complicated intra-abdominal infections
- Treatment of peritonitis caused by enterococci species or MRSA
Comment: Initial doses should be determined by total body weight.
International Society for Peritoneal Dialysis (ISPD) Recommendations:
- Intermittent: 15 to 30 mg/kg intraperitoneally every 5 to 7 days
Duration of therapy:
- Enterococcal peritonitis: 3 weeks
- Culture-negative peritonitis: 2 weeks
Use: Treatment of bacterial peritonitis
Adult dose for Peritonitis
Surgical Infection Society (SIS) and IDSA Recommendations:
- 15 to 20 mg/kg IV every 8 to 12 hours
Comment: Initial doses should be determined by total body weight.
Uses:
- Empiric treatment of complicated intra-abdominal infections
- Treatment of peritonitis caused by enterococci species or MRSA
International Society for Peritoneal Dialysis (ISPD) Recommendations:
- Intermittent: 15 to 30 mg/kg intraperitoneally every 5 to 7 days
Duration of therapy:
- Enterococcal peritonitis: 3 weeks
- Culture-negative peritonitis: 2 weeks
Use: Treatment of bacterial peritonitis
Adult dose for Prevention of Perinatal Group B Streptococcal Disease
US Centers for Disease Control and Prevention (US CDC) Recommendations:
- 1 g IV every 12 hours until delivery
Use:
- Prevention of early-onset Group B streptococcal disease in patients with penicillin hypersensitivity and susceptibility is unknown/not possible or the isolates are resistant to erythromycin or clindamycin
Adult dose for Shunt Infection
IDSA, AAN, AANS, and NCS Recommendations:
- Patients with slit ventricles: 5 mg via intraventricular route (plus gentamicin)
- Patients with normal-sized ventricles: 10 mg via intraventricular route (plus gentamicin)
- Patients with enlarged ventricles: 15 to 20 mg via intraventricular route (plus gentamicin)
Frequency of dosing:
- External drain output less than 50 mL/day: Every 3 days
- External drain output 50 to 100 mL/day: Every 2 days
- External drain output 100 to 150 mL/day: Once a day
- External drain output 150 to 200 mL/day: Increase the dose by 5 mg (plus gentamicin) and give once a day
- External drain output 200 to 250 mL/day: Increase the dose by 10 mg (plus gentamicin) and give once a day
Use: Treatment of healthcare-associated ventriculitis and meningitis in patients who respond poorly to systemic antibiotics
Adult dose for Surgical Prophylaxis
American Society of Health-System Pharmacists (ASHP), IDSA, SHEA, and SIS Recommendations:
- 15 mg/kg IV once, within 120 minutes before surgery
Uses:
Alternative agent for surgical prophylaxis in patients who have a beta-lactam allergy and are undergoing:
- Cardiac procedures (e.g., coronary artery bypass, cardiac device insertion, ventricular assist devices)
- Neurosurgery (e.g., elective craniotomy and cerebrospinal fluid-shunting procedures, implantation of intrathecal pumps)
- Thoracic procedures (e.g., lobectomy, pneumonectomy, lung resection, thoracotomy, or video-assisted thorascopic surgery)
- Some orthopedic procedures (e.g., spinal procedures without instrumentation, hip fracture repair)
- Some urologic procedures (e.g., clean surgery without entry into urinary tract)
- Heart, lung, and heart-lung transplantation procedures (e.g., heart transplantation, lung and heart-lung transplantation)
- Clean-contaminated or clean plastic surgery procedures with risk factors
Alternative agent (in combination with an aminoglycoside, aztreonam, or fluoroquinolone) for surgical prophylaxis in patients who have a beta-lactam allergy and are undergoing:
- Gastroduodenal procedures (e.g., procedures involving entry in to the lumen of the gastrointestinal tract or procedures not entering the GI tract in high-risk patients)
- Some urologic procedures (e.g., clean surgery involving implanted prosthesis)
Adult dose for Head Injury
Armed Forces Infectious Disease Society (AFIDS), SIS, and IDSA Recommendations:
- 1 g IV every 12 hours plus ciprofloxacin
- Duration of therapy: 5 days OR until cerebrospinal fluid leak is closed, whichever is longer
Use: Antimicrobial prophylaxis for patients with penicillin allergies who have a penetrating brain or spinal cord injury
Pediatric dose for Bacteremia
Neonates:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose:
- First week of life: 10 mg/kg IV every 12 hours
- After first week of life: 10 mg/kg IV every 8 hours
Pediatric patients: 10 mg/kg IV every 6 hours
Comments:
- Vancomycin should be infused over 1 hour.
- Premature infants may require longer dosing intervals.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Uses:
- Empirical treatment of serious/severe staphylococcal infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of septicemia caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of bone infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
American Academy of Pediatrics (AAP) Recommendations:
- Empiric treatment:
- Life-threatening infections: 15 mg/kg IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IV every 6 to 8 hours
Bacterial Infection:
- Neonates (Up to 28 postnatal days):
- Loading dose: 20 mg/kg IV ONCE
- Gestational age 28 weeks or less:
- Serum creatinine less than 0.5 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.5 to 0.7 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 0.8 to 1 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.1 to 1.4 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.4 mg/dL: 15 mg/kg IV every 48 hours
- Gestational age greater than 28 weeks:
- Serum creatinine less than 0.7 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.7 to 0.9 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 1 to 1.2 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.3 to 1.6 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.6 mg/dL: 15 mg/kg IV every 48 hours
Pediatric patients greater than 28 days: 45 to 60 mg/kg IV per day, given in 3 to 4 divided doses
Nonmeningeal pneumococcal infections:
- Infants and Children: 40 to 45 mg/kg IV per day, given in divided doses every 6 to 8 hours
Comment: Serum concentrations should be used to guide ongoing treatment.
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia, central nervous system [CNS] infections)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis (e.g., skin infection, cellulitis, osteomyelitis, pyarthrosis) when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin minimum inhibitory concentrations (MICs) of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of vancomycin-intermediately susceptible Staphylococcus aureus (VISA) infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Treatment of invasive pneumococcal infections
IDSA Recommendations:
Bacteremia:
- 15 mg/kg IV every 6 hours
- Duration of therapy: 2 to 6 weeks, depending on the severity of infection
Bacterial Infection:
- 7 days or less and less than 1200 g: 15 mg/kg IV every 24 hours
- 7 days or less than 1200 to 2000 g: 10 to 15 mg/kg IV every 12 to 18 hours
- 7 days or less than greater than 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and less than 1200 g: 15 mg/kg IV every 24 hours
- 8 to 30 days and 1200 to 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and greater than 2000 g: 15 to 20 mg/kg IV every 8 hours
- 1 month to 18 years: 10 to 13.33 mg/kg IV every 6 to 8 hours
Maximum dose: 40 mg/kg/day
Uses:
- Preferred treatment for IV catheter-related bloodstream infections caused by MRSA/coagulase-negative staphylococci, ampicillin-resistant, vancomycin-sensitive E faecalis/E faecium, C jeikeium (Group JK)
- Alternative treatment for IV catheter-related bloodstream infections caused by MSSA/coagulase-negative staphylococci, ampicillin susceptible E faecalis/E faecium
- Treatment of bacteremia
Pediatric dose for Osteomyelitis
Neonates:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose:
- First week of life: 10 mg/kg IV every 12 hours
- After first week of life: 10 mg/kg IV every 8 hours
Pediatric patients: 10 mg/kg IV every 6 hours
Comments:
- Vancomycin should be infused over 1 hour.
- Premature infants may require longer dosing intervals.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Uses:
- Empirical treatment of serious/severe staphylococcal infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of septicemia caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of bone infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
American Academy of Pediatrics (AAP) Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IV every 6 to 8 hours
Bacterial Infection:
Neonates (Up to 28 postnatal days):
- Loading dose: 20 mg/kg IV ONCE
Gestational age 28 weeks or less:
- Serum creatinine less than 0.5 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.5 to 0.7 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 0.8 to 1 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.1 to 1.4 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.4 mg/dL: 15 mg/kg IV every 48 hours
Gestational age greater than 28 weeks:
- Serum creatinine less than 0.7 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.7 to 0.9 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 1 to 1.2 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.3 to 1.6 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.6 mg/dL: 15 mg/kg IV every 48 hours
Pediatric patients greater than 28 days: 45 to 60 mg/kg IV per day, given in 3 to 4 divided doses
Nonmeningeal pneumococcal infections:
- Infants and Children: 40 to 45 mg/kg IV per day, given in divided doses every 6 to 8 hours
Comment: Serum concentrations should be used to guide ongoing treatment.
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia, central nervous system [CNS] infections)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis (e.g., skin infection, cellulitis, osteomyelitis, pyarthrosis) when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin minimum inhibitory concentrations (MICs) of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of vancomycin-intermediately susceptible Staphylococcus aureus (VISA) infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Treatment of invasive pneumococcal infections
IDSA Recommendations:
Bacteremia:
- 15 mg/kg IV every 6 hours
- Duration of therapy: 2 to 6 weeks, depending on the severity of infection
Bacterial Infection:
- 7 days or less and less than 1200 g: 15 mg/kg IV every 24 hours
- 7 days or less than 1200 to 2000 g: 10 to 15 mg/kg IV every 12 to 18 hours
- 7 days or less than greater than 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and less than 1200 g: 15 mg/kg IV every 24 hours
- 8 to 30 days and 1200 to 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and greater than 2000 g: 15 to 20 mg/kg IV every 8 hours
- 1 month to 18 years: 10 to 13.33 mg/kg IV every 6 to 8 hours
Maximum dose: 40 mg/kg/day
Uses:
- Preferred treatment for IV catheter-related bloodstream infections caused by MRSA/coagulase-negative staphylococci, ampicillin-resistant, vancomycin-sensitive E faecalis/E faecium, C jeikeium (Group JK)
- Alternative treatment for IV catheter-related bloodstream infections caused by MSSA/coagulase-negative staphylococci, ampicillin susceptible E faecalis/E faecium
- Treatment of bacteremia
Pediatric dose for Bacterial Infection
Neonates:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose:
- First week of life: 10 mg/kg IV every 12 hours
- After first week of life: 10 mg/kg IV every 8 hours
Pediatric patients: 10 mg/kg IV every 6 hours
Comments:
- This drug should be infused over 1 hour.
- Premature infants may require longer dosing intervals.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Uses:
- Empirical treatment of serious/severe staphylococcal infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of septicemia caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of bone infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
American Academy of Pediatrics (AAP) Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IV every 6 to 8 hours
Bacterial Infection:
Neonates (Up to 28 postnatal days):
- Loading dose: 20 mg/kg IV ONCE
Gestational age 28 weeks or less:
- Serum creatinine less than 0.5 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.5 to 0.7 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 0.8 to 1 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.1 to 1.4 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.4 mg/dL: 15 mg/kg IV every 48 hours
Gestational age greater than 28 weeks:
- Serum creatinine less than 0.7 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.7 to 0.9 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 1 to 1.2 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.3 to 1.6 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.6 mg/dL: 15 mg/kg IV every 48 hours
Pediatric patients greater than 28 days: 45 to 60 mg/kg IV per day, given in 3 to 4 divided doses
Nonmeningeal pneumococcal infections:
- Infants and Children: 40 to 45 mg/kg IV per day, given in divided doses every 6 to 8 hours
Comment: Serum concentrations should be used to guide ongoing treatment.
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia, central nervous system [CNS] infections)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis (e.g., skin infection, cellulitis, osteomyelitis, pyarthrosis) when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin minimum inhibitory concentrations (MICs) of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of vancomycin-intermediately susceptible Staphylococcus aureus (VISA) infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Treatment of invasive pneumococcal infections
IDSA Recommendations:
Bacteremia:
- 15 mg/kg IV every 6 hours
- Duration of therapy: 2 to 6 weeks, depending on the severity of infection
Bacterial Infection:
- 7 days or less and less than 1200 g: 15 mg/kg IV every 24 hours
- 7 days or less than 1200 to 2000 g: 10 to 15 mg/kg IV every 12 to 18 hours
- 7 days or less than greater than 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and less than 1200 g: 15 mg/kg IV every 24 hours
- 8 to 30 days and 1200 to 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and greater than 2000 g: 15 to 20 mg/kg IV every 8 hours
- 1 month to 18 years: 10 to 13.33 mg/kg IV every 6 to 8 hours
Maximum dose: 40 mg/kg/day
Uses:
- Preferred treatment for IV catheter-related bloodstream infections caused by MRSA/coagulase-negative staphylococci, ampicillin-resistant, vancomycin-sensitive E faecalis/E faecium, C jeikeium (Group JK)
- Alternative treatment for IV catheter-related bloodstream infections caused by MSSA/coagulase-negative staphylococci, ampicillin susceptible E faecalis/E faecium
- Treatment of bacteremia
Pediatric dose for Sepsis
Neonates:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose:
- First week of life: 10 mg/kg IV every 12 hours
- After first week of life: 10 mg/kg IV every 8 hours
Pediatric patients: 10 mg/kg IV every 6 hours
Comments:
- This drug should be infused over 1 hour.
- Premature infants may require longer dosing intervals.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Uses:
- Empirical treatment of serious/severe staphylococcal infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of septicemia caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment of bone infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
American Academy of Pediatrics (AAP) Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IV every 6 to 8 hours
Bacterial Infection:
Neonates (Up to 28 postnatal days):
- Loading dose: 20 mg/kg IV ONCE
Gestational age 28 weeks or less:
- Serum creatinine less than 0.5 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.5 to 0.7 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 0.8 to 1 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.1 to 1.4 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.4 mg/dL: 15 mg/kg IV every 48 hours
Gestational age greater than 28 weeks:
- Serum creatinine less than 0.7 mg/dL: 15 mg/kg IV every 12 hours
- Serum creatinine 0.7 to 0.9 mg/dL: 20 mg/kg IV every 24 hours
- Serum creatinine 1 to 1.2 mg/dL: 15 mg/kg IV every 24 hours
- Serum creatinine 1.3 to 1.6 mg/dL: 10 mg/kg IV every 24 hours
- Serum creatinine greater than 1.6 mg/dL: 15 mg/kg IV every 48 hours
Pediatric patients greater than 28 days: 45 to 60 mg/kg IV per day, given in 3 to 4 divided doses
Nonmeningeal pneumococcal infections:
- Infants and Children: 40 to 45 mg/kg IV per day, given in divided doses every 6 to 8 hours
Comment: Serum concentrations should be used to guide ongoing treatment.
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia, central nervous system [CNS] infections)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis (e.g., skin infection, cellulitis, osteomyelitis, pyarthrosis) when rates of MRSA colonization and infection in the community are substantial.
-Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy - Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin minimum inhibitory concentrations (MICs) of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of vancomycin-intermediately susceptible Staphylococcus aureus (VISA) infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Treatment of invasive pneumococcal infections
IDSA Recommendations:
Bacteremia:
- 15 mg/kg IV every 6 hours
- Duration of therapy: 2 to 6 weeks, depending on the severity of infection
Bacterial Infection:
- 7 days or less and less than 1200 g: 15 mg/kg IV every 24 hours
- 7 days or less than 1200 to 2000 g: 10 to 15 mg/kg IV every 12 to 18 hours
- 7 days or less than greater than 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and less than 1200 g: 15 mg/kg IV every 24 hours
- 8 to 30 days and 1200 to 2000 g: 10 to 15 mg/kg IV every 8 to 12 hours
- 8 to 30 days and greater than 2000 g: 15 to 20 mg/kg IV every 8 hours
- 1 month to 18 years: 10 to 13.33 mg/kg IV every 6 to 8 hours
Maximum dose: 40 mg/kg/day
Uses:
- Preferred treatment for IV catheter-related bloodstream infections caused by MRSA/coagulase-negative staphylococci, ampicillin-resistant, vancomycin-sensitive E faecalis/E faecium, C jeikeium (Group JK)
- Alternative treatment for IV catheter-related bloodstream infections caused by MSSA/coagulase-negative staphylococci, ampicillin susceptible E faecalis/E faecium
- Treatment of bacteremia
Pediatric dose for Endocarditis
Neonates:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose:
- First week of life: 10 mg/kg IV every 12 hours
- After first week of life: 10 mg/kg IV every 8 hours
Pediatric patients: 10 mg/kg IV every 6 hours
Comments:
- This drug should be infused over 1 hour.
- Premature infants may require longer dosing intervals.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
- Successful treatment of diphtheroid endocarditis has been reported.
Use:
- Empirical treatment of staphylococcal endocarditis caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
- Empirical treatment (with an aminoglycoside) of endocarditis caused by enterococci, S bovis, or S viridans
- Empirical treatment (with an aminoglycoside and/or rifampin) of early-onset prosthetic valve endocarditis caused by S epidermidis or diphtheroids
AAP Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IV every 6 to 8 hours
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., endocarditis)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
AHA Recommendations:
- 40 to 60 mg/kg IV per day, given in divided doses every 6 to 12 hours
- Maximum dose: 2 g/day
Duration of therapy:
- Empirical treatment: 4 to 6 weeks
- Staphylococci infection: 6 weeks
Comment: Gentamycin should be added to patients with enterococci infections.
Uses:
- Treatment of native valve and prosthetic valve infective endocarditis
- Empirical alternative treatment (with gentamicin) of community-acquired native valve or late prosthetic valve (over 1 year after surgery) endocarditis
- Empirical treatment of nosocomial endocarditis associated with vascular cannulae or early prosthetic valve endocarditis (1 year or less after surgery)
- Alternative treatment for streptococcal infections highly susceptible to penicillin G (e.g., Groups A, B, C, G nonenterococcal, Group D streptococci) and streptococci relatively resistant to penicillin (e.g., enterococci, less-susceptible S viridians)
- Alternative treatment for endocarditis caused by S aureus or coagulase-negative staphylococci susceptible or resistant to penicillin G and/or oxacillin in patients highly allergic to beta-lactam antibiotics
Pediatric dose for Skin or Soft Tissue Infection
Neonates:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose:
- First week of life: 10 mg/kg IV every 12 hours
- After first week of life: 10 mg/kg IV every 8 hours
Pediatric patients: 10 mg/kg IV every 6 hours
Comments:
- This drug should be infused over 1 hour.
- Premature infants may require longer dosing intervals.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Use:
- Empirical treatment of skin and skin structure infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
AAP Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IM or IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IM or IV every 6 to 8 hours
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis (e.g., skin infection, cellulitis) when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
IDSA Recommendations:
- 10 to 15 mg/kg IV 3 to 4 times a day
Comments:
- Patients with necrotizing infections may require up to a 13 mg/kg dose given IV every 8 hours plus piperacillin.
- Patients with necrotizing infections caused by resistant S aureus may require 15 mg/kg given IV every 6 hours.
Use:
- First-line treatment of treatment of SSTIs caused by MRSA in patients who require parenteral treatment
- Alternative treatment of SSTIs in patients with penicillin allergies
- First-line treatment of necrotizing infections of the skin, fascia, and muscle caused by mixed infections
Pediatric dose for Pneumonia
Neonates:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose:
- First week of life: 10 mg/kg IV every 12 hours
- After first week of life: 10 mg/kg IV every 8 hours
Pediatric patients: 10 mg/kg IV every 6 hours
Comments:
- This drug should be infused over 1 hour.
- Premature infants may require longer dosing intervals.
- Doses should be determined by patient-specific factors (e.g., obesity, age).
Use: Empirical treatment of lower respiratory tract infections caused by susceptible strains of methicillin-resistant staphylococci in patients who are allergic to penicillin, failed to respond/cannot receive other drugs (e.g., penicillins, cephalosporins), and/or to treat organisms that are resistant to other drugs
Pediatric Infectious Diseases Society (PIDS) and IDSA Recommendations:
- 10 to 20 mg/kg every 6 to 8 hours
Uses:
- Alternative treatment of community acquired pneumonia caused by S pneumoniae with penicillin MICs of less than or equal to 2 mcg/mL, S pneumoniae resistant to penicillin (MICs at least 4 mcg/mL), Group A Streptococcus, or MSSA
- Preferred treatment of community acquired pneumonia caused by MRSA (with/without susceptibility to clindamycin)
Pediatric dose for Intraabdominal Infection
AAP Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IM or IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IM or IV every 6 to 8 hours
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis (e.g., skin infection, cellulitis) when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
SIS and IDSA Recommendations:
- 40 mg/kg IV per day, divided and given every 6 to 8 hours
Comment: This drug should be given as a 1-hour infusion.
Uses:
- Treatment of complicated intra-abdominal infections
- Treatment of peritonitis caused by Enterococci species or MRSA
ISPD Recommendations:
Prophylaxis: 25 mg/L intraperitoneally once
Treatment: 30 mg/kg intraperitoneally once, then 15 mg/kg intraperitoneally every 3 to 5 days
Uses:
- Prophylaxis against peritonitis in patients with known MRSA colonization at risk of touch contamination during instillation of peritoneal dialysis fluid after system disconnection OR disconnection during peritoneal dialysis
- Treatment of bacterial peritonitis
Pediatric dose for Peritonitis
AAP Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IM or IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IM or IV every 6 to 8 hours
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis (e.g., skin infection, cellulitis) when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
SIS and IDSA Recommendations:
- 40 mg/kg IV per day, divided and given every 6 to 8 hours
Comment: This drug should be given as a 1-hour infusion.
Uses:
- Treatment of complicated intra-abdominal infections
- Treatment of peritonitis caused by Enterococci species or MRSA
ISPD Recommendations:
Prophylaxis: 25 mg/L intraperitoneally once
Treatment: 30 mg/kg intraperitoneally once, then 15 mg/kg intraperitoneally every 3 to 5 days
Uses:
- Prophylaxis against peritonitis in patients with known MRSA colonization at risk of touch contamination during instillation of peritoneal dialysis fluid after system disconnection OR disconnection during peritoneal dialysis
- Treatment of bacterial peritonitis
Pediatric dose for Surgical Prophylaxis
AAP Recommendations:
Neonates (72 hours) or older: 15 mg/kg IV ONCE
Uses:
Alternative agent for surgical prophylaxis in patients undergoing:
- Cardiac surgical procedures (e.g., prosthetic valve/pacemaker, ventricular assist devices) where Staphylococcus epidermidis (including methicillin-resistant Staphylococcus epidermidis [MRSE]), Staphylococcus aureus (including MRSA), Corynebacterium species, and/or enteric gram-negative bacilli are likely
- Neurosurgery (e.g., craniotomy, intrathecal baclofen shunt/ventricular shunt placement) where S epidermidis (including MRSE) or S aureus (including MRSA) are likely
- Orthopedic (e.g., internal fixation of fractures, implantation of materials including prosthetic joint and spinal procedures with/without instrumentation) where S epidermidis (including MRSE) or S aureus (including MRSA) are likely
- Thoracic (noncardiac) where S epidermidis S aureus (including MRSA), streptococci, or gram-negative enteric bacilli are likely
ASHP, IDSA, SHEA, and SIS Recommendations:
- 15 mg/kg IV once, within 120 minutes before surgery
Uses:
Alternative agent for surgical prophylaxis in patients who have a beta-lactam allergy and are undergoing:
- Cardiac procedures (e.g., coronary artery bypass, cardiac device insertion, ventricular assist devices)
- Neurosurgery (e.g., elective craniotomy and cerebrospinal fluid-shunting procedures, implantation of intrathecal pumps)
- Thoracic procedures (e.g., lobectomy, pneumonectomy, lung resection, thoracotomy, or video-assisted thorascopic surgery)
- Some orthopedic procedures (e.g., spinal procedures without instrumentation, hip fracture repair)
- Some urologic procedures (e.g., clean surgery without entry into urinary tract)
- Heart, lung, and heart-lung transplantation procedures (e.g., heart transplantation, lung and heart-lung transplantation)
- Clean-contaminated or clean plastic surgery procedures with risk factors
Alternative agent (in combination with an aminoglycoside, aztreonam, or fluoroquinolone) for surgical prophylaxis in patients who have a beta-lactam allergy and are undergoing:
- Gastroduodenal procedures (e.g., procedures involving entry in to the lumen of the gastrointestinal tract or procedures not entering the GI tract in high-risk patients)
- Some urologic procedures (e.g., clean surgery involving implanted prosthesis)
Pediatric dose for Meningitis
AAP Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IV every 6 to 8 hours
Infants and Children:
- Meningitis: 60 mg/kg IV per day, given in divided doses every 6 hours
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia, CNS infections)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Treatment of invasive pneumococcal meningitis
IDSA, AAN, AANS, and NCS Recommendations:
- 60 mg/kg IV per day, given in divided doses every 6 hours
- Duration of therapy: 2 weeks
Use: Treatment of patients with healthcare-associated ventriculitis and meningitis
Pediatric dose for CNS Infection
AAP Recommendations:
Empiric treatment:
- Life-threatening infections: 15 mg/kg IV every 6 hours PLUS nafcillin OR oxacillin
- Non-life-threatening infections without signs of sepsis: 15 mg/kg IV every 6 to 8 hours
Infants and Children:
- Meningitis: 60 mg/kg IV per day, given in divided doses every 6 hours
Uses:
- Drug of choice for the treatment of life-threatening infections (e.g., septicemia, CNS infections)
- Drug of choice for the treatment of non-life-threatening infection without signs/symptoms of sepsis when rates of MRSA colonization and infection in the community are substantial.
- Alternative treatment of MSSA in patients with serious penicillin and cephalosporin allergy
- Drug of choice (with gentamicin) for the treatment of healthcare-associated, multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Drug of choice (with gentamicin) for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug for the treatment of community-associated, not multi-drug resistant MRSA infections and oxacillin MICs of 4 mcg/mL or greater
- Alternative drug (with linezolid with/without gentamicin) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Alternative drug (with sulfamethoxazole-trimethoprim) for the treatment of VISA infections with MICs of 4 to 16 mcg/mL
- Treatment of invasive pneumococcal meningitis
IDSA, AAN, AANS, and NCS Recommendations:
- 60 mg/kg IV per day, given in divided doses every 6 hours
- Duration of therapy: 2 weeks
Use: Treatment of patients with healthcare-associated ventriculitis and meningitis
Pediatric dose for Shunt Infection
IDSA, AAN, AANS, and NCS Recommendations:
- Patients with slit ventricles: 5 mg via intraventricular route (plus gentamicin)
- Patients with normal-sized ventricles: 10 mg via intraventricular route (plus gentamicin)
- Patients with enlarged ventricles: 15 to 20 mg via intraventricular route (plus gentamicin)
Frequency of dosing:
- External drain output less than 50 mL/day: Every 3 days
- External drain output 50 to 100 mL/day: Every 2 days
- External drain output 100 to 150 mL/day: Once a day
- External drain output 150 to 200 mL/day: Increase the dose by 5 mg (plus gentamicin) and give once a day
- External drain output 200 to 250 mL/day: Increase the dose by 10 mg (plus gentamicin) and give once a day
Comment: Some experts recommend decreasing the dose by 60% when treating infants to account for lower cerebrospinal fluid volume (compared to adults).
Use: Treatment of healthcare-associated ventriculitis and meningitis in patients who respond poorly to systemic antibiotics
Pediatric dose for Head Injury
AFIDS, SIS, and IDSA Recommendations:
- 60 mg/kg, divided and given every 6 to 8 hours
- Duration of therapy: 5 days OR until cerebrospinal fluid leak is closed, whichever is longer
Use: Antimicrobial prophylaxis for patients with penicillin allergies who have a penetrating brain or spinal cord injury
Renal dose Adjustments
Mild to moderate renal dysfunction:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose: The manufacturer product information should be consulted regarding dose adjustments in patients with this level of renal dysfunction.
Severe renal dysfunction and functionally anephric patients:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose: 1.9 mg/kg IV every 24 hours OR 250 to 1000 mg IV once every several days
Patients with anuria:
- Initial dose: 15 mg/kg IV ONCE
- Maintenance dose: 1000 mg IV once every 7 to 10 days
Liver Dose Adjustments
- Data not available
What should I do if I forget a dose?
Infuse the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not infuse a double dose to make up for a missed one.
Vancomycin side effects
Vancomycin adverse effects – Intravenous Vancomycin Injection
Common adverse effects of intravenous vancomycin injection include nephrotoxicity, hypotension, and hypersensitivity reactions. Anaphylaxis is a type of hypersensitivity reaction that can be seen with vancomycin 7.
Red man syndrome is an infusion-related reaction associated with rapid intravenous infusion of vancomycin. Symptoms include flushing, pruritus, and an erythematous rash on the face, neck, and upper torso. Signs of red man syndrome often appear 4 to 10 minutes after starting or shortly after the completion of an infusion. The incidence of red man syndrome varies between 3.7% and 47% in patients. However, there is a direct correlation between the increased incidence of red man syndrome with faster rates of vancomycin administration. Rapid infusion of vancomycin can lead to angioedema and hypotension, which accompany red man syndrome. Reports show the most severe forms of this reaction frequently occur in children and patients younger than the age of 40. Prolonging the infusion time is the primary management strategy used to mitigate red man syndrome. Nevertheless, premedication with antihistamines, such as diphenhydramine or hydroxyzine, can be used to prevent the occurrence of red man syndrome.
Less common adverse effects include local phlebitis, chills, drug fever, skin rash, eosinophilia, and reversible neutropenia.
In rare situations, patients have reported DRESS syndrome (drug rash with eosinophilia and systemic symptoms), ototoxicity, thrombocytopenia, vasculitis, and Stevens-Johnson syndrome.
Vancomycin injection may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- pain, redness, or swelling at the injection site
- fever
- nausea
- chills
Some side effects can be serious. If you experience any of these symptoms or those listed in the HOW section, call your doctor immediately or get emergency medical treatment:
- severe diarrhea with watery or bloody stools (up to 2 months after your treatment)
- stomach pain or cramps
- rash
- peeling or blistering of the skin
- swelling of the eyes, face, throat, tongue, or lips
- difficulty breathing or swallowing
- hoarseness
- hearing loss, roaring or ringing in the ears, or dizziness
Vancomycin injection may cause other side effects. Call your doctor if you have any unusual problems while receiving vancomycin injection.
Vancomycin adverse effects – Oral Vancomycin
Gastrointestinal adverse effects, such as abdominal pain and nausea, are commonly seen with oral vancomycin. Dysgeusia or distorted sense of taste is a common adverse effect unique to vancomycin oral solution. Patients should be told to seek medical attention if these adverse effects are severe and bothersome. Note that many of these adverse effects are temporary.
Less common adverse effects of oral vancomycin include peripheral edema, fatigue, headache, diarrhea, flatulence, vomiting, back pain, urinary tract infection, and fever.
Rare cases of increased serum creatinine, red man syndrome, interstitial nephritis, nephrotoxicity, ototoxicity, thrombocytopenia, and vasculitis have also been reported with the use of oral vancomycin.
Vancomycin oral may cause side effects. Tell your doctor if this symptom is severe or does not go away:
- upset stomach
Some side effects can be serious. The following symptoms are uncommon, but if you experience any of them, call your doctor immediately:
- sore throat, fever, chills, and other signs of infection
- hives
- skin rash
- itching
- difficulty breathing or swallowing
- redness of the skin above the waist
- pain and muscle tightness of the chest and back
- unusual bleeding or bruising
- fainting
- dizziness
- blurred vision
- ringing in the ears
Vancomycin toxicity
Nephrotoxicity and ototoxicity have been associated with the use of vancomycin 8. Although there are numerous case reports of acute renal failure attributed to vancomycin use, there is currently limited data suggesting a direct causal relationship. The proposed mechanism of nephrotoxicity is renal tubular ischemia due to the oxidative effect of vancomycin on cells of the proximal renal tubule. Common risk factors for nephrotoxicity include preexisting renal impairment, concurrent use of nephrotoxic medications, advanced age, and dehydration. Although vancomycin-induced nephrotoxicity is commonly reversible, it can be challenging to differentiate it from acute interstitial nephritis and worsening renal function due to an uncontrolled infection. Vancomycin-induced nephrotoxicity can be identified by increases in serum creatinine in the absence of a causative explanation. Dosing vancomycin based on estimated creatinine clearance is a commonly used technique to prevent nephrotoxicity. Patients who experience signs of acute renal failure precipitated by vancomycin use should promptly discontinue their therapy. It is also important to note that cases of nephrotoxicity have been reported with both oral and intravenous vancomycin use. Cases of nephrotoxicity associated with oral vancomycin have typically been reported in patients over 65 years of age.
Ototoxicity is a rare complication associated with vancomycin monotherapy. It is commonly reported in patients receiving excessive vancomycin doses, concurrent ototoxic medications (e.g., aminoglycosides, loop diuretics, antineoplastic agents), and those with underlying hearing loss conditions. Treatment should be discontinued if patients experience signs of ototoxicity such as tinnitus, loss of hearing, and unbalanced movements. It should be noted that vancomycin-induced ototoxicity may be irreversible in some cases. Auditory function testing may be beneficial to identify early symptoms.
- Patel S, Preuss CV, Bernice F. Vancomycin. [Updated 2019 May 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459263[↩][↩][↩]
- Ishii H, Hirai K, Sugiyama K, Nakatani E, Kimura M, Itoh K. Validation of a Nomogram for Achieving Target Trough Concentration of Vancomycin: Accuracy in Patients With Augmented Renal Function. Ther Drug Monit. 2018 Dec;40(6):693-698[↩]
- Lee T, Pang S, Abraham S, Coombs GW. Antimicrobial-resistant CC17 Enterococcus faecium: The past, the present and the future. J Glob Antimicrob Resist. 2019 Mar;16:36-47[↩]
- Cieslak PR, Strausbaugh LJ, Fleming DW, Ling JM. Vancomycin in Oregon: who’s using it and why. Infect Control Hosp Epidemiol. 1999 Aug;20(8):557-60[↩]
- Butler-Laporte G, De L’Étoile-Morel S, Cheng MP, McDonald EG, Lee TC. MRSA colonization status as a predictor of clinical infection: A systematic review and meta-analysis. J. Infect. 2018 Dec;77(6):489-495[↩]
- Gerding DN, Sambol SP, Johnson S. Non-toxigenic Clostridioides (Formerly Clostridium) difficile for Prevention of C. difficile Infection: From Bench to Bedside Back to Bench and Back to Bedside. Front Microbiol. 2018;9:1700[↩]
- Gerstein W, Colombo E, Harji F. Documented vancomycin-induced severe immune-mediated thrombocytopaenia. BMJ Case Rep. 2018 Aug 27;2018[↩]
- Monteiro JF, Hahn SR, Gonçalves J, Fresco P. Vancomycin therapeutic drug monitoring and population pharmacokinetic models in special patient subpopulations. Pharmacol Res Perspect. 2018 Jul;6(4):e00420.[↩]