Contents
- What is Barrett’s esophagus
What is Barrett’s esophagus
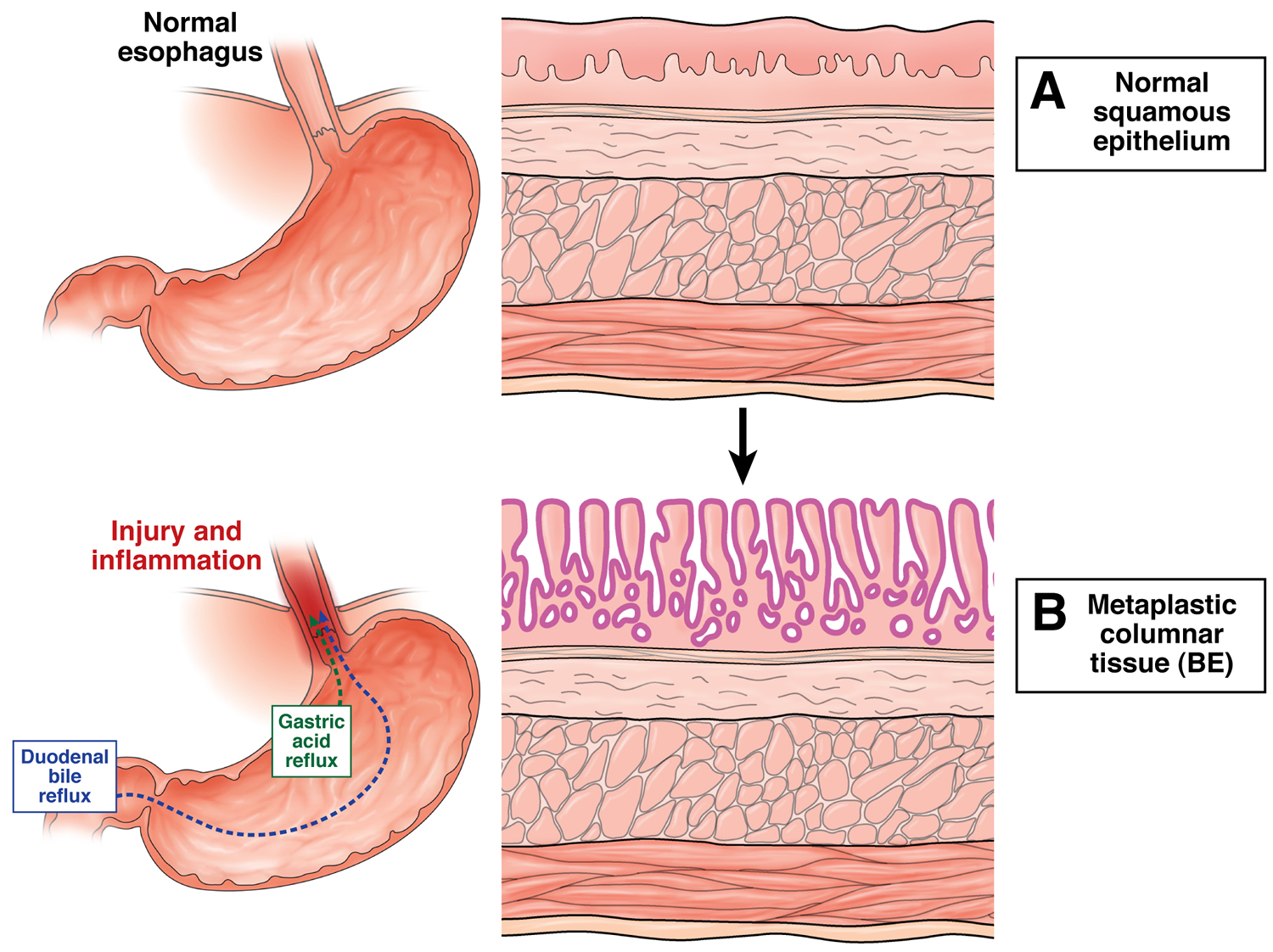
Barrett’s esophagus (BE) is a disorder in which the lining of the esophagus is damaged by stomach acid 1. The esophagus is also called the food pipe or swallowing tube.
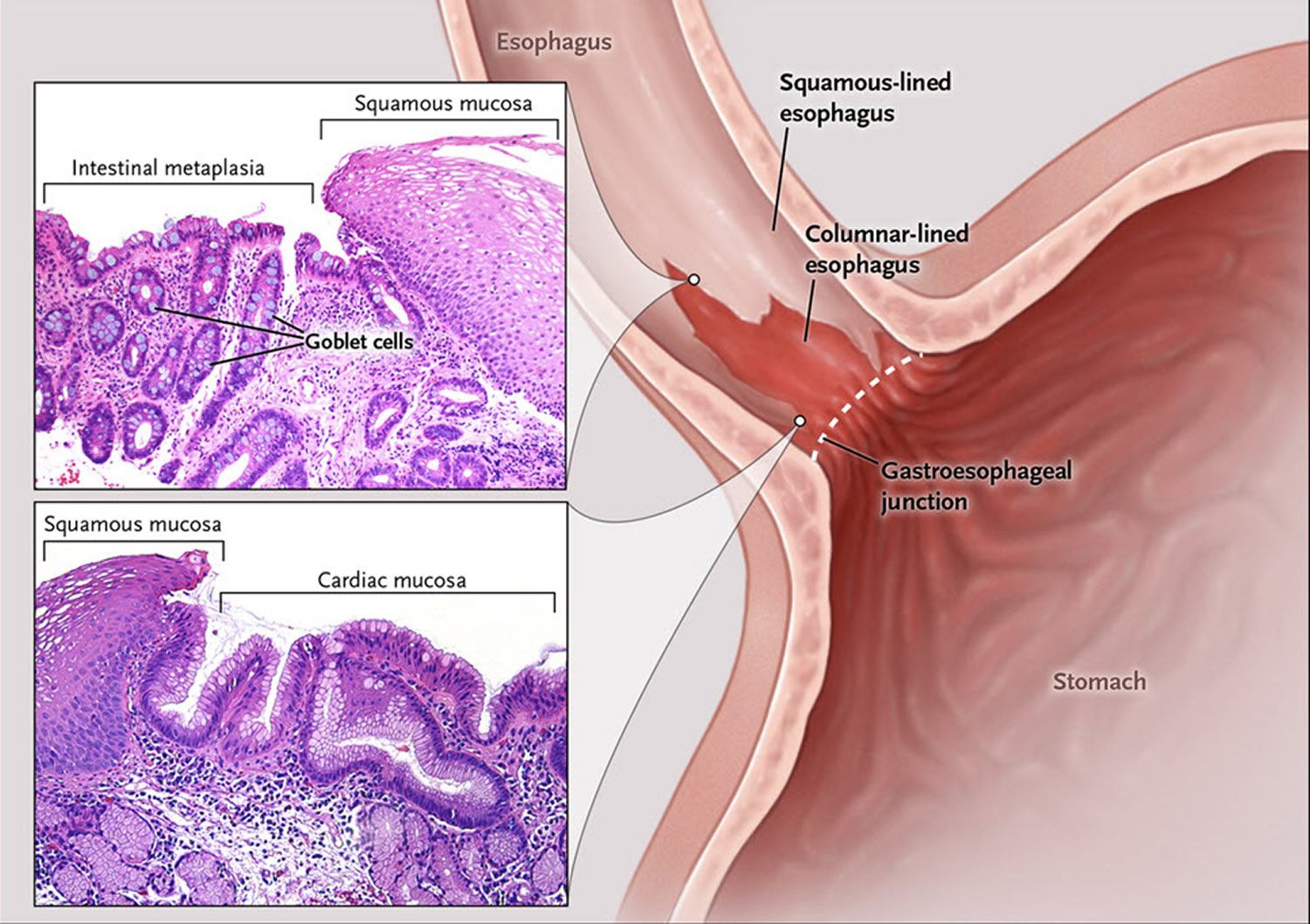
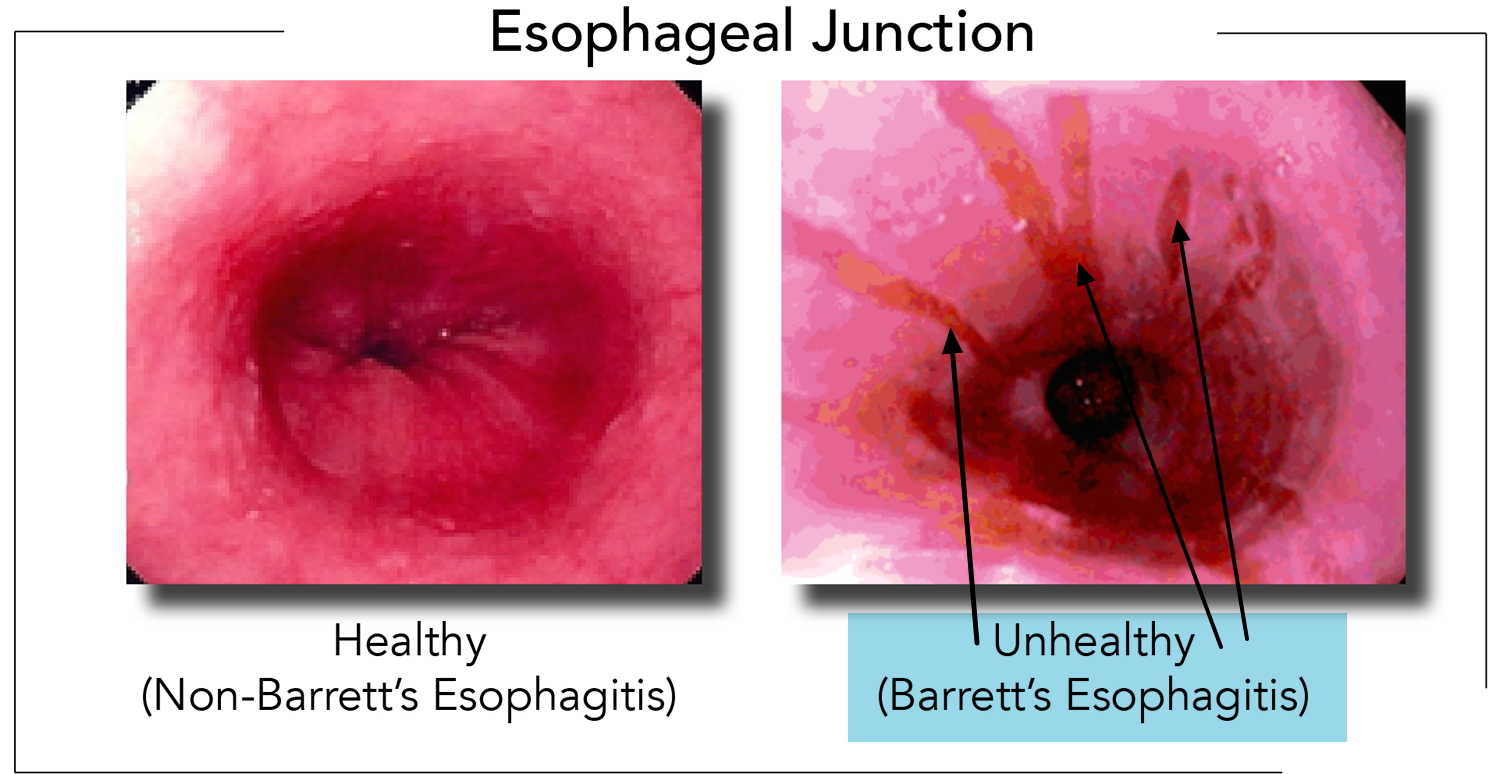
In order to understand Barrett’s esophagus, it is useful to understand the normal appearance of the esophagus. In the normal esophagus, the tissue lining appears pale pink and smooth 2. These flat square cells, called “squamous” (Latin for square) cells, make up the normal lining of the esophagus. See Figures 2 and 3.
In contrast, Barrett’s esophagus is a salmon-colored lining in the esophagus (see Figures 3 and 4), made up of cells that are similar to cells found in the small intestine and are called “specialized intestinal metaplasia.”
The reason Barrett’s esophagus is important is because people who have it have a small increased risk of developing esophageal cancer 2. Barrett’s esophagus and heartburn symptoms are associated with a specific type of esophageal cancer called “esophageal adenocarcinoma.” However, cancer is not common 1.
The risk of esophageal adenocarcinoma in people with Barrett’s esophagus is about 0.5 percent per year 3. Typically, before this cancer develops, precancerous cells appear in the Barrett’s tissue. Doctors call this condition dysplasia and classify the dysplasia as low grade or high grade (see Figures 6 and 7 below).
How Common is Barrett’s Esophagus ?
Barrett’s esophagus is more commonly seen in people who have frequent, persistent heartburn or gastroesophageal reflux disease (GERD). Gastroesophageal reflux disease (GERD) symptoms include heartburn (burning under your breast bone) that may wake you up at night, occur after meals or in between, and may temporarily improve with antacids. Acid regurgitation, or the experience of sour or bitter-tasting fluid coming back up into your mouth, is also a gastroesophageal reflux disease (GERD) symptom. Some people do not have any of these symptoms and are still at risk of developing Barrett’s esophagus.
What are the Risk Factors for Barrett’s Esophagus ?
- Age (age 50 or over),
- Male sex,
- Caucasian ethnicity and
- Heartburn symptoms of longer than 10 years’ duration are risk factors for Barrett’s esophagus.
- Heartburn, tobacco smoking, and obesity are risk factors for developing esophageal carcinoma.
Tobacco use (especially chewing tobacco) and alcohol consumption are much stronger risk factors for a different type of cancer: squamous cell cancer of the esophagus. Tobacco slightly increases a person’s chance of developing esophageal adenocarcinoma.
Most people with Barrett’s esophagus are in their 60’s at the time of diagnosis 2. It is thought that most people who are diagnosed with Barrett’s have had it for 10 to 20 years before diagnosis.
Men are 3 to 4 times more likely to have Barrett’s esophagus compared to women. Caucasians are about 10 times more likely to have Barrett’s esophagus than persons of African American ethnic background.
Although people who experience weekly heartburn or acid regurgitation are 64 times more likely to get esophageal adenocarcinoma than people who have never experienced these symptoms, 40% of people with esophageal adenocarcinoma deny ever experiencing heartburn. Why these people developed esophageal adenocarcinoma remains a mystery 2.
Prevention of Barrett’s Esophagus
Diagnosis and treatment of gastroesophageal reflux (GERD) may prevent Barrett esophagus.
The risk factors for gastroesophageal reflux (GERD) include:
- Use of alcohol (possibly)
- Hiatal hernia (a condition in which part of the stomach moves above the diaphragm, which is the muscle that separates the chest and abdominal cavities)
- Obesity
- Pregnancy
- Scleroderma
- Smoking
Heartburn and gastroesophageal reflux can be brought on or made worse by pregnancy.
Symptoms can also be caused by certain medicines, such as:
- Anticholinergics (for example, seasickness medicine)
- Bronchodilators for asthma
- Calcium channel blockers for high blood pressure
- Dopamine-active drugs for Parkinson disease
- Progestin for abnormal menstrual bleeding or birth control
- Sedatives for insomnia or anxiety
- Tricyclic antidepressants
Talk to your health care provider if you think one of your medicines may be causing heartburn. Never change or stop taking a medicine without first talking to your provider.
Barrett’s esophagus diet
Can your diet help prevent Barrett’s esophagus ?
Researchers have not found that diet and nutrition play an important role in causing or preventing Barrett’s esophagus 4.
If you have gastroesophageal reflux or gastroesophageal reflux disease (GERD), you can prevent or relieve your symptoms by changing your diet. Dietary changes that can help reduce your symptoms include:
- decreasing fatty foods
- eating small, frequent meals instead of three large meals
Avoid eating or drinking the following items that may make gastroesophageal reflux or gastroesophageal reflux disease (GERD) worse:
- chocolate
- coffee
- peppermint
- greasy or spicy foods
- tomatoes and tomato products
- citrus juices
- alcoholic drinks
- smoking
Figure 1. Esophagus
Figure 2. Barrett’s esophagus
Figure 3. Barrett’s esophagus microscopic view showing changes in the lining of the esophagus
Figure 4. Barrett’s esophagus endoscopic view (as seen by your gut specialist)
Causes of Barrett’s esophagus
When you eat, food passes from your throat to your stomach through the esophagus. The esophagus is also called the food pipe or swallowing tube. A ring of muscle fibers in the lower esophagus keeps stomach contents from moving backward.
If these muscles do not close tightly, harsh stomach acid can leak into the esophagus. This is called reflux or gastroesophageal reflux (GERD). It may cause tissue damage over time. The lining becomes similar to that of the stomach.
Barrett’s esophagus occurs more often in men than women. People who have had gastroesophageal reflux (GERD) for a long time are more likely to have this condition.
What is the Risk of Getting Esophageal Cancer ?
Doctors now know why patients with Barrett’s esophagus have a low risk of esophageal cancer. A person with Barrett’s esophagus has less than a 1 in 200 chance per year of developing esophageal adenocarcinoma 2. The overall risk of cancer may increase as the years go by, but more than 90% of people with Barrett’s esophagus WILL NOT develop cancer 2. Therefore, Barrett’s esophagus is a condition that you need to know about and take care of if you have it. However, the vast majority of patients with Barrett’s esophagus will never get cancer.
When Should You See a Doctor about Barrett’s Esophagus ?
You should ask a doctor about Barrett’s esophagus if you have the risk factors listed earlier (male sex, age 50 or over, Caucasian ethnic group, gastroesophageal reflux (GERD) symptoms of longer than 10 years’ duration). If you have alarm symptoms such as trouble swallowing, losing weight without trying, blood in your stool, vomiting, persistent symptoms despite medical therapy, or new chest pain, you should discuss your symptoms with your doctor and have an endoscopic examination.
Barrett’s esophagus symptoms
Barrett’s esophagus itself does not cause symptoms. The acid reflux that causes Barrett’s esophagus often leads to symptoms of heartburn. Many people with this condition do not have any symptoms.
How is Barrett’s Esophagus Diagnosed
Endoscopy is the test of choice for Barrett’s esophagus. During endoscopy, a thin tube with a light and camera on the end are run through your mouth, down your throat and into your stomach. During the endoscopy, your health care provider may take biopsies (tissue samples) from different parts of the food pipe. Biopsies, meaning small pieces of tissue can be collected to look at under the microscope. In Barrett’s esophagus, tissue is the issue. Tissue, showing a certain abnormal cell type, is necessary to make the diagnosis of Barrett’s esophagus, and is one of the keys to management of Barrett’s. Biopsies also help look for changes that could lead to cancer.
During endoscopy, your doctor will get multiple biopsies every 1 to 2 cm (one half to one inch) along the length of your Barrett’s esophagus segment. How the biopsies look on a microscope slide influences your management.
Your provider may recommend a follow-up endoscopy to look for cell changes that indicate cancer. People with Barrett esophagus are recommended to have follow-up endoscopy every 3 to 5 years, or more if abnormal cells are found.
An upper gastrointestinal barium study can be helpful in finding strictures (areas of narrowing), usually causing trouble swallowing. Barium studies are not useful for diagnosing Barrett’s esophagus, because it is a diagnosis that requires biopsies of the tissues to make.
Barrett’s esophagus treatment
What are the Treatment Options for Barrett’s Esophagus ?
Generally, doctors treat the symptoms of gastroesophageal reflux (GERD), not Barrett’s esophagus specifically. Barrett’s esophagus is an acquired disorder, meaning it develops over time and is not present at birth. It is usually diagnosed around age 60, although we estimate that half of people with Barrett’s esophagus have it by age 40.
Treatment for gastroesophageal reflux (GERD) are listed in the “what is esophagitis” article of our website. Generally, this will include antacids, histamine receptor antagonists and proton pump inhibitors. Surgery is also an option. The large majority of patients with Barrett’s esophagus will be treated with a proton pump inhibitor.
Treatment should improve acid reflux symptoms, and may keep Barrett’s esophagus from getting worse. Treatment may involve lifestyle changes and medicines.
Lifestyle Modification
In order to decrease the amount of gastric contents that reach the lower esophagus, certain simple guidelines should be followed:
- Raise the Head of the Bed. The simplest method is to use a 4″ x 4″ piece of wood to which two jar caps have been nailed an appropriate distance apart to receive the legs or casters at the upper end of the bed. Failure to use the jar caps inevitably results in the patient being jolted from sleep as the upper end of the bed rolls off the 4″ x 4″.
- Alternatively, one may use an under-mattress foam wedge to elevate the head about 6-10 inches. Pillows are not an effective alternative for elevating the head in preventing reflux.
- Change Eating and Sleeping Habits. Avoid lying down for two hours after eating. Do not eat for at least two hours before bedtime. This decreases the amount of stomach acid available for reflux.
- Avoid Tight Clothing. Reduce your weight if obesity contributes to the problem.
- Avoid foods and beverages that contribute to heartburn: chocolate, fats, coffee, peppermint, greasy or spicy foods, citrus juice, tomato products, peppers and alcoholic beverages.
- Avoid drugs such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve, Naprosyn). Take acetaminophen (Tylenol) to relieve pain.
- Stop smoking. Tobacco inhibits saliva, which is the body’s major buffer. Tobacco may also stimulate stomach acid production and relax the muscle between the esophagus and the stomach, permitting acid reflux to occur.
- Reduce weight if too heavy. Obesity is linked to GERD, so maintaining a healthy body weight may help prevent the condition.
- Do not eat 2-3 hours before sleep.
- For infrequent episodes of heartburn, take an over-the-counter antacid or an H2 blocker, some of which are now available without a prescription.
Medications:
- Antacids after meals and at bedtime
- Histamine H2 receptor blockers
- Proton pump inhibitors (PPIs)
- Avoiding tobacco use
The proton pump inhibitors (PPIs) include: esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix), rabeprazole (Aciphex), omeprazole powder (Zegerid), and dexlansoprazole (Dexilant). With regard to the optimal way to take a proton pump inhibitor, for most brands it is suggested that you take your medication half an hour before a meal. Most other pills can be taken along with PPI’s, except for antacids, Carafate, and Questran. Antacids, Carafate and Questran bind almost everything they come in contact with, so if you are on these medicines, you should not be taking them at the same time as other medicines in the first place.
Proton pump inhibitors (PPIs) work by turning off the pumps in the lining of your stomach that pump acid into the stomach. Eating food 20 to 60 minutes after taking your pill on an empty stomach activates millions of these acid pumps which are then turned off by the medication. This is the key for the best dosing of a proton pump inhibitors (PPIs).
All of these medicines are available by prescription. Omeprazole and lansoprazole are also available in over-the-counter strength.
Your doctor may consider anti-reflux surgery if you have GERD symptoms and don’t respond to medicines. However, research has not shown that medicines or surgery for GERD and Barrett’s esophagus lower your chances of developing dysplasia or esophageal adenocarcinoma.
- Endoscopic biopsy can show changes in the cell that may be cancer. You provider may advise surgery or other procedures to treat that.
Some of the following procedures remove the harmful tissue in your esophagus:
- Photodynamic therapy (PDT) uses a special laser device, called an esophageal balloon, along with a drug called Photofrin.
- Other procedures use different types of high energy to destroy the precancerous tissue.
- Surgery to remove the abnormal lining.
Endoscopic ablative therapies
Endoscopic ablative therapies use different techniques to destroy the dysplasia in your esophagus. After the therapies, your body should begin making normal esophageal cells.
A doctor, usually a gastroenterologist or surgeon, performs these procedures at certain hospitals and outpatient centers. You will receive local anesthesia and a sedative. The most common procedures are the following:
Photodynamic therapy
Photodynamic therapy uses a light-activated chemical called porfimer (Photofrin), an endoscope, and a laser to kill precancerous cells in your esophagus. A doctor injects porfimer into a vein in your arm, and you return 24 to 72 hours later to complete the procedure.
Complications of photodynamic therapy may include:
- sensitivity of your skin and eyes to light for about 6 weeks after the procedure
- burns, swelling, pain, and scarring in nearby healthy tissue
- coughing, trouble swallowing, stomach pain, painful breathing, and shortness of breath.
Radiofrequency ablation
Radiofrequency ablation uses radio waves to kill precancerous and cancerous cells in the Barrett’s tissue. An electrode mounted on a balloon or an endoscope creates heat to destroy the Barrett’s tissue and precancerous and cancerous cells.
Complications of radiation ablation may include:
- chest pain
- cuts in the lining of your esophagus
- strictures
Clinical trials have shown that complications are less common with radiofrequency ablation compared with photodynamic therapy.
Endoscopic mucosal resection
In endoscopic mucosal resection, your doctor lifts the Barrett’s tissue, injects a solution underneath or applies suction to the tissue, and then cuts the tissue off. The doctor then removes the tissue with an endoscope. Gastroenterologists perform this procedure at certain hospitals and outpatient centers. You will receive local anesthesia to numb your throat and a sedative to help you relax and stay comfortable.
Before performing an endoscopic mucosal resection for cancer, your doctor will do an endoscopic ultrasound.
Complications can include bleeding or tearing of your esophagus. Doctors sometimes combine endoscopic mucosal resection with photodynamic therapy.
Surgery
Surgery called esophagectomy is an alternative to endoscopic therapies. Many doctors prefer endoscopic therapies because these procedures have fewer complications.
Esophagectomy is the surgical removal of the affected sections of your esophagus. After removing sections of your esophagus, a surgeon rebuilds your esophagus from part of your stomach or large intestine. The surgery is performed at a hospital. You’ll receive general anesthesia, and you’ll stay in the hospital for 7 to 14 days after the surgery to recover.
Surgery may not be an option if you have other medical problems. Your doctor may consider the less-invasive endoscopic treatments or continued frequent surveillance instead.
Management of Barrett’s esophagus
The key to the management of Barrett’s esophagus is the level of dysplasia that the biopsies show. “Dysplasia” is how much precancerous changes the cells have. “No Dysplasia” means that the Barrett’s cells show no precancerous changes. Low-grade dysplasia means that the cells show some of the early characteristics of cancer. High-grade dysplasia means that the cells show more advanced changes of cancer. The worse the dysplasia, the higher the risk that the Barrett’s will go on to cancer.
All of our cells are programmed to die. We are constantly making new cells while old cells slough off. For example, dandruff is old dead scalp cells that have dried up and flaked off. Just like your skin on the outside of your body, the lining of the esophagus is skin on the inside of your body. Cells keep their DNA in their nucleus. Cancer is DNA that has lost control of how fast the cells divide, or how quickly they die. In cancer, cells grow and grow without dying.
When cells are changing from normal to cancer, they go through the steps of dysplasia outlined above.
No Dysplasia
If a diagnosis of Barrett’s esophagus is made, ideally there should be NO dysplasia.
Figure 5. Barrett’s esophagus “NO dysplasia”
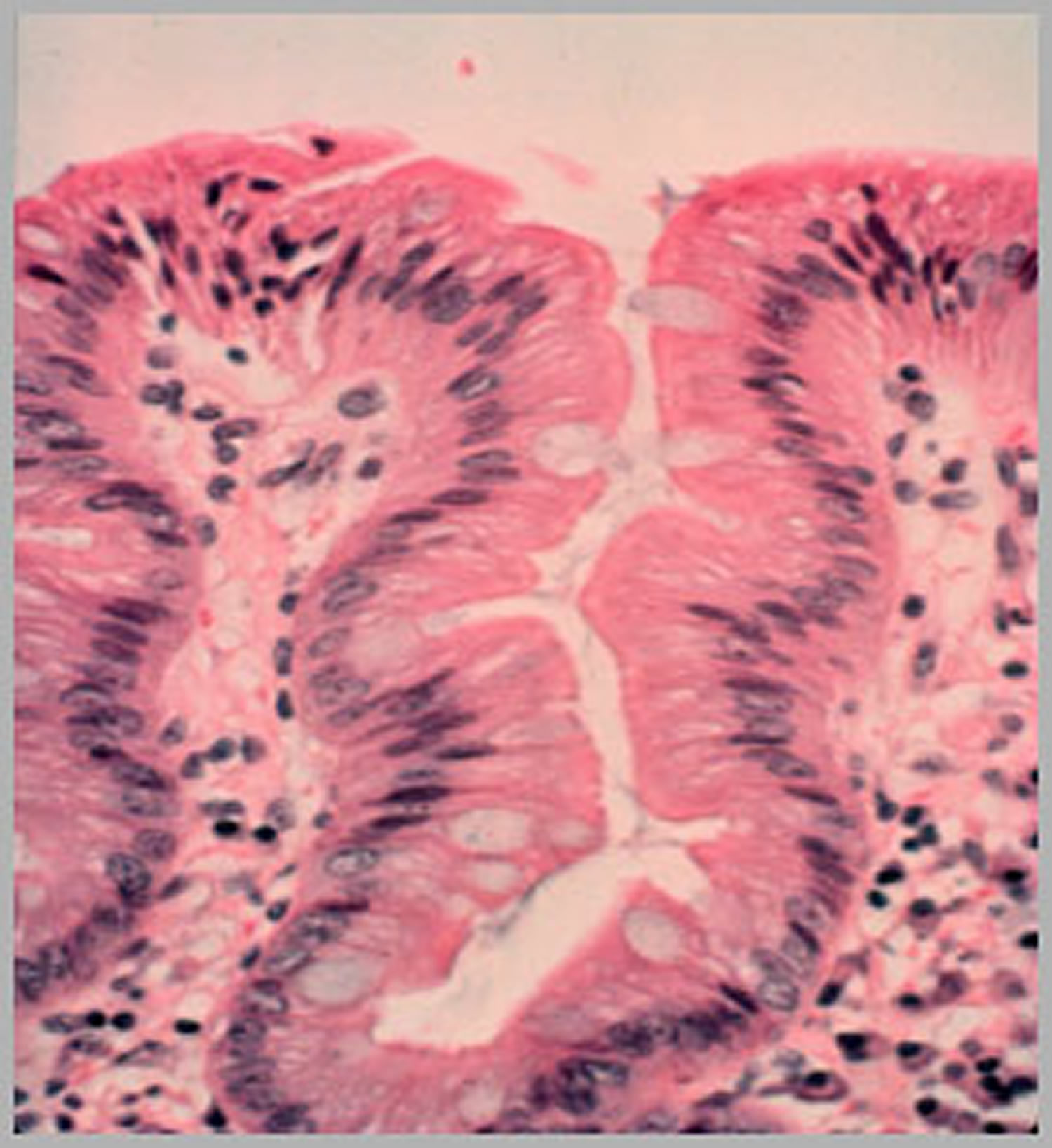
Note: In biopsies with no dysplasia, the nuclei are small, organized and located at the base (bottom) of the Barrett’s cell.
[Source 2]Most people with Barrett’s esophagus and no dysplasia will need to undergo future endoscopies to assure there is no progression of the condition. When the next endoscopy occurs is usually based on recommendations by groups of experts whose opinion is endorsed The American College of Gastroenterology. Follow up endoscopy for Barrett’s without dysplasia is usually recommended at 3-5 years, but your doctor will help decide what is most appropriate for you.
Low Grade Dysplasia
If biopsies are found to have low-grade dysplasia (Figure 6), where the nuclei are still small but somewhat disorganized, several things should happen: First, the doctor should have a second pathologist also look at your biopsies, because low-grade dysplasia can be a hard diagnosis for a pathologist to make correctly, and sometimes there is disagreement among pathologists that might require yet another opinion to resolve.
Figure 6. Barrett’s esophagus “Low grade dysplasia”
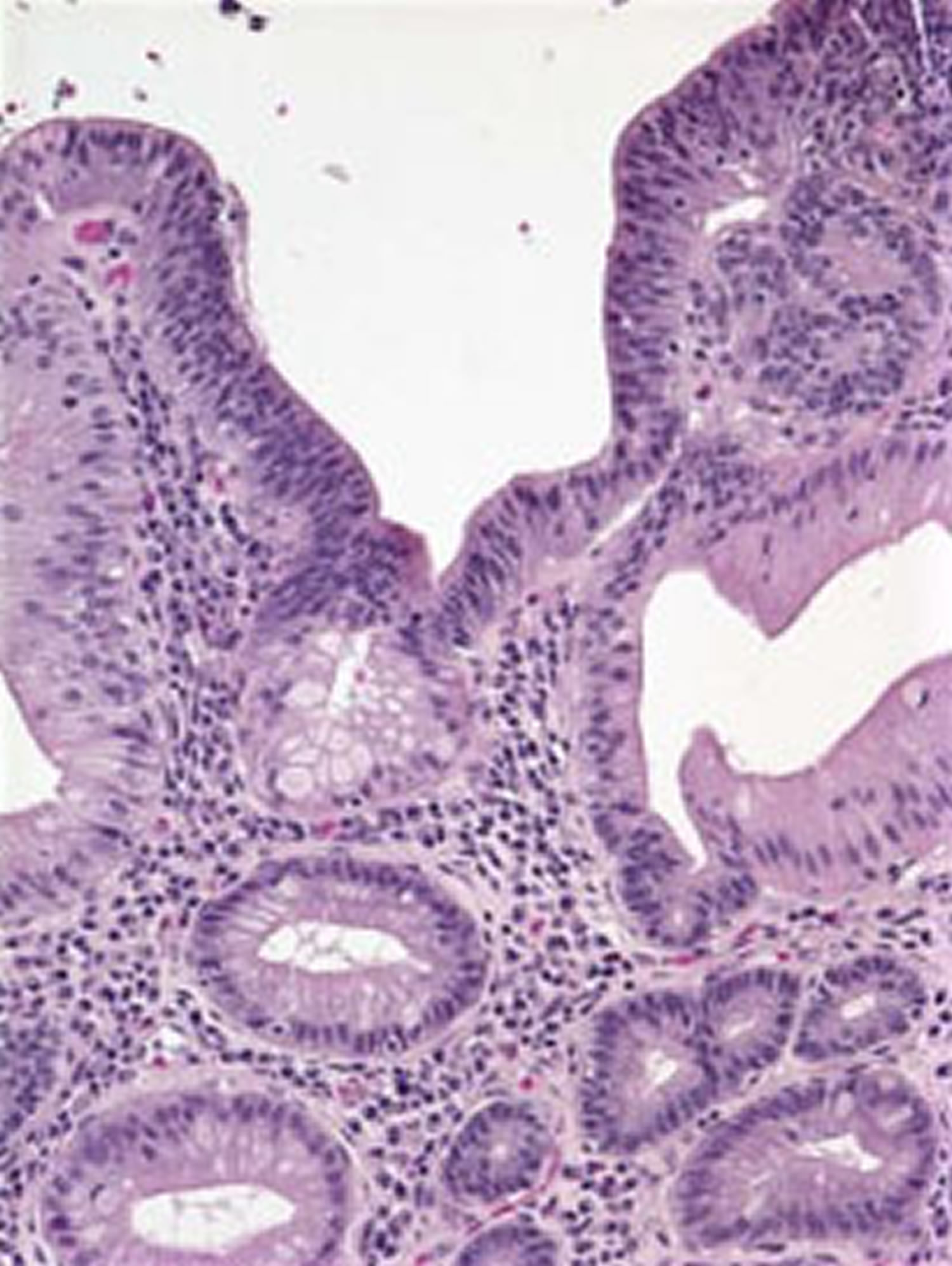
If the diagnosis of low-grade dysplasia is confirmed, it is recommended that otherwise healthy people consider getting endoscopic treatment to get rid of their Barrett’s esophagus. The most common way of doing this is a process called radiofrequency ablation. In radiofrequency ablation treatments, heat is applied to the precancerous tissue to kill those cells so that normal healthy cells can grow there instead. Studies demonstrate that these treatments can lower the patient’s chance of ever getting cancer. Another acceptable option if low-grade dysplasia is found is to continue to perform endoscopies to monitor the condition, without doing any ablation treatments. If this option is selected, the repeat endoscopy is usually performed 1 year after the first one.
High Grade Dysplasia
High-grade dysplasia (Figure 7) is thought to be the stage that occurs before esophageal cancer. However high-grade dysplasia can regress to low-grade dysplasia. If diagnosed with high-grade dysplasia the biopsies should be examined again by a pathologist who specializes in diseases of the esophagus.
Figure 7. Barrett’s esophagus “High grade dysplasia”
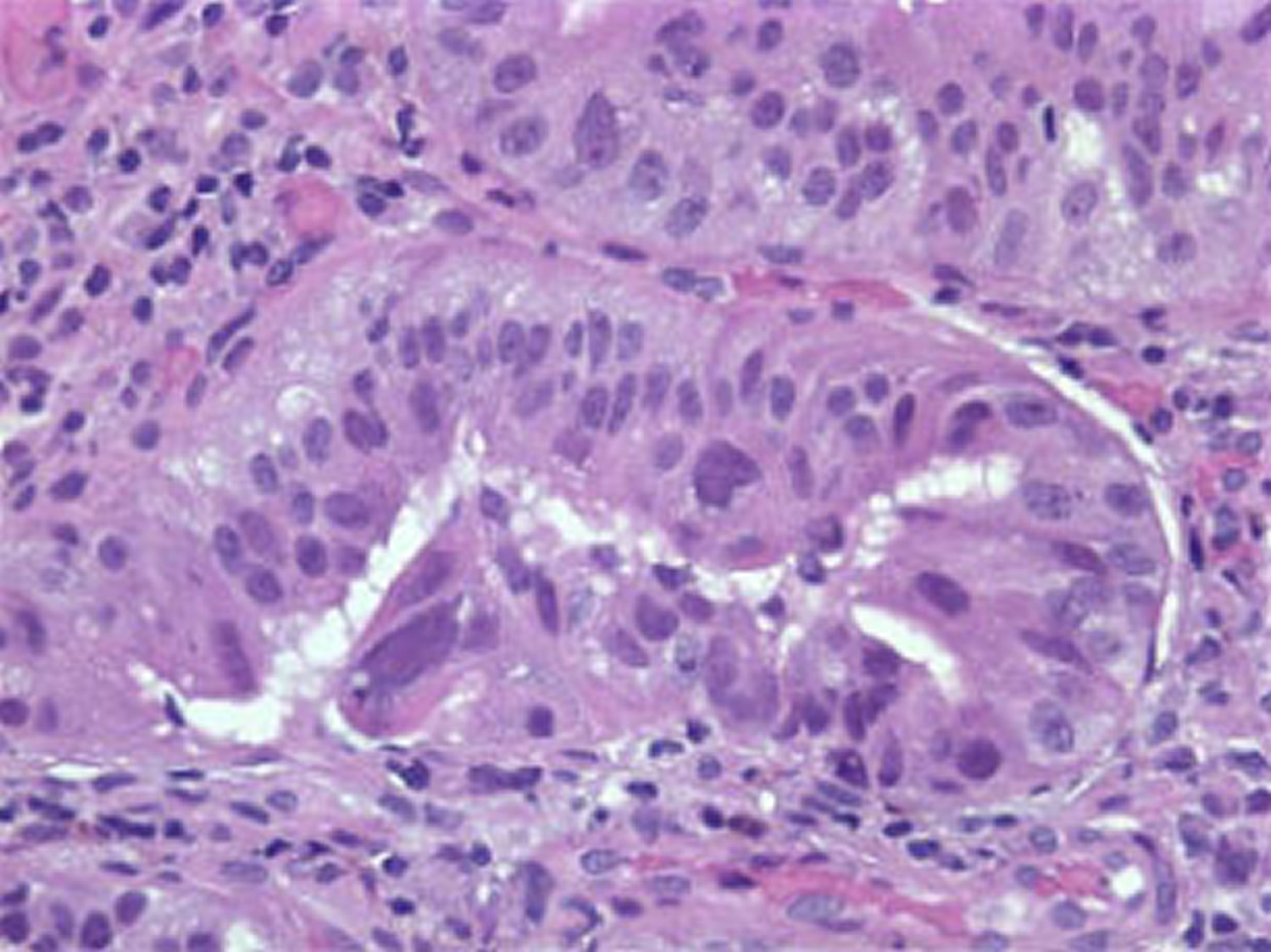
If a diagnosis of high-grade dysplasia is confirmed, it is recommended that the patient undergo endoscopic treatments to get rid of the Barrett’s esophagus. As above, the most commonly used treatment in high-grade dysplasia is radiofrequency ablation. Surgical removal of the esophagus can also be performed for high-grade dysplasia; however, this is done more rarely now that effective endoscopic treatments are available.
Barrett’s esophagus is best managed by doctors with an interest in this disease, including gastroenterologists, esophagus surgeons and gastroenterology pathologists.
Barrett’s esophagus cancer
Esophageal cancer is cancer that starts in the esophagus 5.
You’re at greater risk for getting esophageal cancer if you smoke, drink heavily, or have acid reflux. Your risk also goes up as you age.
Your doctor uses imaging tests and a biopsy to diagnose esophageal cancer. Treatments include surgery, radiation, and chemotherapy.
When the cancer has not spread outside the esophagus, surgery may improve the chance of survival.
When the cancer has spread to other areas of the body, a cure is generally not possible 5. Treatment is directed toward relieving symptoms. You might also need nutritional support, since the cancer or treatment may make it hard to swallow.
There are two main types of cancer that can occur in the esophagus 6:
- Squamous cell carcinoma occurs more commonly in the upper or middle part of the esophagus.
- Adenocarcinoma occurs in the lower part of the esophagus.
Squamous cell esophageal cancer is linked to smoking and drinking too much alcohol.
Adenocarcinoma is the more common type of esophageal cancer. Having Barrett esophagus increases the risk of this type of cancer. Acid reflux disease (gastroesophageal reflux disease or GERD) can develop into Barrett’s esophagus. Other risk factors include smoking, being male, or being obese.
Early esophageal cancer usually does not cause symptoms. Later, you may have symptoms such as:
- Painful or difficult swallowing
- Weight loss
- A hoarse voice or cough that doesn’t go away.
Causes of Esophageal cancer
Studies show that esophageal cancer is more commonly diagnosed in people over the age of 55 years. Men are affected twice as commonly as women. Squamous cell esophageal cancer is more common in African Americans than Caucasians. On the other hand, adenocarcinoma appears to be more common in middle-aged Caucasian men.
The exact cause is unknown; however there are well-recognized risk factors. In the US, alcohol, smoking and obesity are the major risk factors. Stopping drinking and smoking may reduce the chance of getting esophageal cancer as well as other types of cancers. Sometimes adenocarcinoma of the esophagus runs in families.
The risk of cancer of the esophagus is also increased by irritation of the lining of the esophagus. In patients with acid reflux, where contents from the stomach back up into the esophagus, the cells that line the esophagus can change and begin to resemble the cells of the intestine. This condition is knows as Barrett’s esophagus. Those with Barrett’s esophagus have a higher risk of developing esophageal cancer.
Less common causes of irritation can also increase the chance of developing esophageal cancer. For example, people who have swallowed caustic substances like lye can have damage to the esophagus that increases the risk of developing esophageal cancer.
Prevention of esophageal cancer
To reduce your risk of cancer of the esophagus:
- DO NOT smoke.
- Limit or DO NOT drink alcoholic beverages.
- Get checked by your doctor if you have severe GERD.
- Get regular checkups if you have Barrett’s esophagus.
What are the symptoms of esophageal cancer ?
Very small tumors at an early stage do not generally cause symptoms.
Symptoms may include any of the following:
- Backward movement of food through the esophagus and possibly mouth (regurgitation)
- Chest pain not related to eating
- Difficulty swallowing solids or liquids
- Heartburn
- Vomiting blood
- Weight loss
Patients commonly experience difficulty swallowing as the tumor gets larger and the width of the esophagus becomes narrowed. At first, most have trouble swallowing solid foods such as meats, breads or raw vegetables. As the tumor grows, the esophagus becomes more narrowed causing difficulty in swallowing even liquids. Cancer of the esophagus can also cause symptoms of indigestion, heartburn, vomiting and choking. Patients may also have coughing and hoarseness of the voice. Involuntary weight loss is also common.
How is esophageal cancer diagnosed ?
Tests used to help diagnose esophageal cancer may include:
- Barium swallow
- Chest MRI or thoracic CT (usually used to help determine the stage of the disease)
- Endoscopic ultrasound (also sometimes used to determine the stage of disease)
- Esophagogastroduodenoscopy (EGD) and biopsy
- PET scan (sometimes useful for determining the stage of disease, and whether surgery is possible)
Stool testing may show small amounts of blood in the stool.
The doctor will generally start by taking a complete history and performing a physical examination. An esophagram, also called a barium swallow, is a series of x-rays of the esophagus. The patient is asked to drink a barium solution, which coats the inside of the esophagus. Multiple x-rays are then taken to look for changes in the shape of the esophagus.
Most patients undergo a test called endoscopy where a thin flexible lighted instrument with a camera at the end is passed through the mouth into the esophagus. This scope allows the doctor to see the inner layer of the esophagus. Biopsies can be taken during this procedure if needed and submitted to the pathologist for examination under a microscope to detect cancer cells.
A CT scan of the neck, chest and abdomen may help to identify if there is any spread of the cancer to other organs in the body so that the doctor can determine appropriate management.
Endoscopic ultrasound is a newer technique that can be used to provide detailed assessment of the depth of the tumor and involvement of adjacent lymph nodes. This instrument is similar to the endoscope above except there is ultrasound embedded at the tip of the scope.
What is the treatment for esophageal cancer ?
Upper endoscopy (EGD) will be used to obtain a tissue sample from the esophagus to diagnose cancer. Depending on the stage of esophageal cancer the patient may undergo surgery, radiation and/or chemotherapy. Other measures that may improve symptoms include stretching or dilation, tube prosthesis (stent) and radiation or laser treatment to reduce the size of the cancer.
Doctors are actively looking at new ways of combining various types of treatment to see if they may have a better effect on treating esophageal cancer. Many patients with esophageal cancer undergo some form of combination therapy with surgery, radiation and chemotherapy.
When the cancer is only in the esophagus and has not spread, surgery will be done. The cancer and part, or all, of the esophagus is removed. The surgery may be done using:
- Open surgery, during which one or two larger incisions are made.
- Minimally invasive surgery, during which a 2 to 4 small incisions are made in the belly. A laparoscope with a tiny camera is inserted into the belly through one of the incisions.
Radiation therapy may also be used instead of surgery in some cases when the cancer has not spread outside the esophagus.
Either chemotherapy, radiation, or both may be used to shrink the tumor and make surgery easier to perform.
If the person is too ill to have major surgery or the cancer has spread to other organs, chemotherapy or radiation may be used to help reduce symptoms. This is called palliative therapy. In such cases, the disease is usually not curable.
Beside a change in diet, other treatments that may be used to help the patient swallow include:
- Dilating (widening) the esophagus using an endoscope. Sometimes a stent is placed to keep the esophagus open.
- A feeding tube into the stomach.
- Photodynamic therapy, in which a special drug is injected into the tumor and is then exposed to light. The light activates the medicine that attacks the tumor.
- Barrett esophagus. Medline Plus. https://medlineplus.gov/ency/article/001143.htm[↩][↩]
- Barrett’s Esophagus. American College of Gastroenterology. http://patients.gi.org/topics/barretts-esophagus/[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Definition & Facts for Barrett’s Esophagus. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/barretts-esophagus/definition-facts[↩]
- Eating, Diet, & Nutrition for Barrett’s Esophagus. National Institute of Diabetes and Digestive and Kidney Disorders. https://www.niddk.nih.gov/health-information/digestive-diseases/barretts-esophagus/eating-diet-nutrition[↩]
- Esophageal cancer. Medline Plus. https://medlineplus.gov/ency/article/000283.htm[↩][↩]
- Esophageal Cancer. American College of Gastroenterology. http://patients.gi.org/topics/esophageal-cancer/[↩]