Contents
- What is perimenopause
- When does perimenopause usually start?
- How will I know if I am in perimenopause?
- How do I know if my period is abnormal?
- How long does perimenopause last?
- Should I continue using birth control during perimenopause?
- What other health problems increase during perimenopause?
- What is menopause?
- When does menopause usually happen?
- What happens after menopause?
- Perimenopause symptoms
- Perimenopause causes
- Perimenopause complications
- Perimenopause diagnosis
- Perimenopause treatment
What is perimenopause
Perimenopause also called the “menopausal transition” or “around menopause” is the time leading up to your last period or the transitional time to menopause 1, 2. Perimenopause is the gradual transition between your reproductive years and menopause (the cessation of menstrual periods). Menopause is when your periods stop permanently and you can no longer get pregnant. You have reached menopause only after it has been a full 12 months in a row since you have your last period. This means you have not had any bleeding, including spotting, for 12 months in a row. Perimenopause is a natural process when your ovaries gradually stop working. As your body transitions to menopause, your hormone levels may change randomly, causing menopause symptoms unexpectedly. During perimenopause, your ovaries make different amounts of the hormones estrogen and progesterone than usual. Your ovulation may become erratic and then stop. Some months, the ovaries may release an egg (ovulate). Other months, they do not release an egg. A common sign of perimenopause is a change in your menstrual cycle. Your menstrual cycle lengthens and flow may become irregular before your final period. Irregular periods happen during this time because you may not ovulate every month. Your periods may be longer or shorter than usual. You might skip periods a few months or have unusually long or short menstrual cycles. Your period may be heavier or lighter than before. Many women also have hot flashes and other menopause symptoms during perimenopause.
Perimenopause is generally a transition that is many years long and can be associated with shorter menstrual intervals, irregular periods, night sweats, and other symptoms. In some women, these symptoms are troublesome enough to need medical intervention.
Women start perimenopause at different ages. You may notice signs of progression toward menopause, such as menstrual irregularity, sometime in your 40s 3. But some women notice changes as early as their mid-30s 4.
- However, the perimenopause transition phase most often begins between ages 45 and 55 and may last for 4 to 8 years (usually lasts about 7 years), but can last as long as 14 years.
- Perimenopause begins with changes in the length of time between periods and ends 1 year after the final menstrual period. Once you’ve gone through 12 consecutive months without a menstrual period, you’ve officially reached menopause, and the perimenopause period is over.
The level of estrogen — the main female hormone — in your body rises and falls unevenly during perimenopause. Your menstrual cycles may lengthen or shorten, and you may begin having menstrual cycles in which your ovaries don’t release an egg (ovulate). You may also experience menopause-like symptoms, such as hot flashes, sleep problems and vaginal dryness.
No two women will experience perimenopause in the same way. Some women do not have any symptoms of perimenopause or have only a few mild symptoms. Others have many symptoms that can be severe.
These are the most common perimenopause symptoms 5:
- Hot flashes. A hot flash is a sudden feeling of heat that rushes to your upper body and face. A hot flash may last from a few seconds to several minutes or longer. Some women have hot flashes a few times a month. Others have them several times a day. Hot flashes that happen at night (night sweats) may wake you up and cause you to feel tired and sluggish during the day.
- Sleep problems. You may have insomnia (trouble falling asleep), or you may wake up long before your usual time. Night sweats may disrupt your sleep.
- Vaginal and urinary tract changes. As your estrogen levels decrease, the lining of your vagina may become thinner, dryer, and less elastic. Vaginal dryness may cause pain during sex. Vaginal infections also may occur more often. The urethra can become dry, inflamed, or irritated. This can cause more frequent urination and increase the risk of urinary tract infections.
Other perimenopause symptoms include:
- Irregular periods. Your menstrual periods may not come as regularly as before. They also might last longer or be shorter. You might skip some months. Periods might stop for a few months and then start up again.
- Your periods might be heavier or lighter than before.
- You might experience mood swings or be irritable.
- Changes in sexual desire (libido). You may have less interest in sex. It may take longer for you to get aroused.
- Trouble concentrating or with memory
- Headaches
- Joint and muscle aches
- Heavy sweating
- Having to pee often
- Premenstrual syndrome (PMS)-like symptoms
Other possible changes are not as noticeable. For example, you might begin to lose bone density because you have less estrogen. This can lead to osteoporosis, a condition that causes bones to become weak and break easily. Changing estrogen levels can also increase your cholesterol levels and increase your risk for heart disease and stroke.
The symptoms of perimenopause may look like other health conditions. Always talk with your family doctor for a diagnosis.
Sometimes it’s hard to tell if you are having symptoms of perimenopause. Your symptoms, health history, age, and a physical exam may help your doctor with the diagnosis. You may also have blood tests to measure your hormone levels.
Perimenopause doesn’t need to be treated unless your symptoms are bothering you. Treatments are available to help ease perimenopause symptoms.
Perimenopause treatments may include:
- Find what triggers your hot flashes by keeping a record. For example, alcohol, coffee, or tea may be a trigger.
- Menopausal hormonal therapy (MHT) also called hormone replacement therapy (HRT) using estrogen or estrogen and progestins to level out hormone levels. Many menopausal symptoms, such as hot flushes and night sweats, are due to low oestrogen levels. Systemic estrogen therapy (with or without progestin [man made progesterone]) has been shown to be the best treatment for the relief of hot flashes and night sweats. Estrogen can be given in several forms. Systemic forms include pills, skin patches, and gels and sprays that are applied to the skin. If progestin (synthetic progesterone) is prescribed, it can be given separately or combined with estrogen in the same pill or in a patch. With systemic therapy, estrogen is released into the bloodstream and travels to the organs and tissues where it is needed. Women who only have vaginal dryness may be prescribed “local” estrogen therapy in the form of a vaginal ring, tablet, or cream. These forms release small doses of estrogen into the vaginal tissue. Both systemic and local types of estrogen therapy relieve vaginal dryness. Systemic estrogen protects against the bone loss that occurs early in menopause and helps prevent hip and spine fractures. Combined estrogen and progestin therapy may reduce the risk of colon cancer. In some cases, testosterone therapy is also used. However, hormone therapy may increase your risk of certain types of cancer and other conditions:
- Estrogen-only therapy causes the lining of the uterus to grow and can increase the risk of endometrial cancer.
- Combined hormone therapy is associated with a small increased risk of heart attack. This risk may be related to age, existing medical conditions, and when a woman starts taking hormone therapy.
- Combined hormone therapy and estrogen-only therapy are associated with a small increased risk of stroke and deep vein thrombosis (DVT). Forms of therapy not taken by mouth (patches, sprays, rings, and others) may have less risk of causing deep vein thrombosis (DVT) than those taken by mouth. Combined hormone therapy is associated with a small increased risk of breast cancer.
- There is a small increased risk of gallbladder disease associated with estrogen therapy with or without progestin. The risk is greatest with oral forms of therapy.
- Selective estrogen receptor modulators (SERMs). Selective estrogen receptor modulators (SERMs) are drugs that act on tissues that respond to estrogen. SERMs are available for the relief of hot flashes and pain during intercourse caused by vaginal dryness.
- Antidepressants (drugs that are used to treat depression). Several antidepressants are available for the treatment of hot flashes.
- Gabapentin (an epilepsy medicine). Gabapentin, an antiseizure medication, is prescription drug that can be prescribed to reduce hot flashes and ease sleep problems associated with menopause.
- Clonidine. Clonidine is a blood pressure medication called a vasodilator (dilate blood vessels). Clonidine is mainly used to treat hot flushes or sweats that may happen during the menopause.
- Fezolinetant (Veozah). Fezolinetant (Veozah) is a hormone-free option for treating menopause hot flashes. It works by blocking a pathway in the brain that helps regulate body temperature.
- Cognitive behavioral therapy (CBT). Cognitive behavioral therapy (CBT) is a talking therapy which can help with low mood and anxiety caused by menopause and perimenopause. Cognitive behavioral therapy (CBT) is also used to manage some physical symptoms like hot flushes and joint pain.
- Plant-based therapies. You may hear about herbal supplements that claim to help manage hot flashes. Plants and herbs that have been used for relief of menopause symptoms include soy, black cohosh, Red clover and Chinese herbal remedies. It’s important to remember that the U.S. Food and Drug Administration (FDA) does not regulate these supplements. Only a few of these substances have been studied for safety and effectiveness. Ask your doctor or pharmacist for advice if you’re thinking about using any herbal supplements.
- Over-the-counter (OTC) products can be used to help with vaginal dryness and painful sexual intercourse that may occur during menopause. They do not contain hormones, so they do not have an effect on the vagina’s thickness or elasticity. Vaginal moisturizers can be used every 2–3 days as needed. Lubricants can be used each time you have sexual intercourse. DO NOT use petroleum jelly. DO NOT use mineral oils or other oils if you use condoms, as these may damage latex condoms or diaphragms.
Discuss other treatments for easing symptoms with your family doctor.
A healthy lifestyle can help you make the best of the years after menopause. Your family doctor may suggest healthy lifestyle changes:
- Eat a healthy diet with fruits and vegetables and whole grains. Eating a balanced diet will help you stay healthy before, during, and after menopause. Be sure to include enough calcium and vitamin D in your diet to help maintain strong bones.
- Get at least 1,000 mg to 1,200 mg of calcium each day through your diet or supplements.
- Exercise regularly. Regular exercise slows down bone loss and improves your overall health. Weight-bearing exercise, such as walking, can help keep bones strong. Strength training strengthens your muscles and bones by resisting against weight, such as your own body, an exercise band, or handheld weights. Balance training, such as yoga and tai chi, may help you avoid falls, which could lead to broken bones.
- Get enough sleep. Try to create the best environment possible for comfortable sleep:
- Go to bed and wake up at the same time every day.
- Avoid your computer, phone, TV, and other screens in the hour before bedtime.
- Avoid heavy meals close to bedtime.
- Skip coffee, soda, or tea in the afternoon—caffeine can affect you up to 8 hours after drinking it.
- Keep your bedroom quiet, cool, and dark. Use a fan if that makes you more comfortable.
- Quit smoking if you smoke. With each puff of a cigarette, your body is exposed to more than 7,000 chemicals. Hundreds of these chemicals are toxic. About 70 are carcinogens. The chemicals in cigarette smoke move from your lungs to your blood. Smoking is a leading cause of death in women. Lung cancer causes more deaths in women than any other type of cancer, including breast cancer and ovarian cancer. Another smoking-related disease, heart disease, is currently the number one killer of women in the United States. Death occurs earlier in women who smoke. On average, female smokers die 12 years earlier than female nonsmokers.
- Practice stress reduction techniques. Practiced regularly, stress-reduction techniques, such as meditation or yoga, can promote relaxation and good health throughout your lifetime, but they may be particularly helpful during the menopausal transition.
- Visit your doctor once a year to have regular exams and tests. During perimenopause, see your obstetrician–gynecologist (ob-gyn) regularly and discuss how you are feeling. Ob-gyns, mental health professionals, and other members of your health care team can help you through this phase of life. Dental checkups and eye exams are important, too. Routine health care visits, even if you are not sick, can help detect problems early.
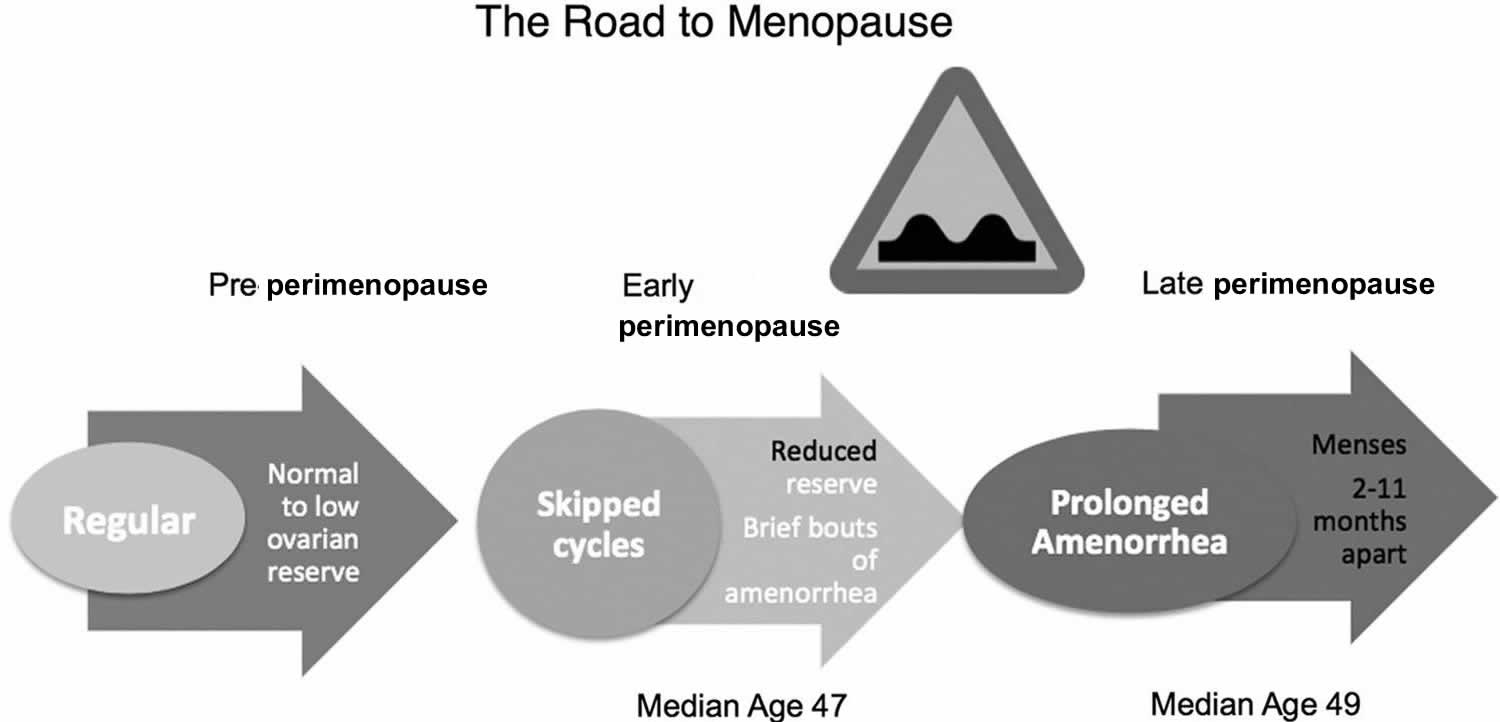
Figure 1. Stages and ages that precede menopause
[Source 6 ]Some women seek medical attention for their perimenopausal symptoms. But others either tolerate the changes or simply don’t experience symptoms severe enough to need attention. Because symptoms may be subtle and come on gradually, you may not realize at first that they’re all connected to the same thing — rising and falling levels of estrogen and progesterone, another key female hormone.
If you have symptoms that interfere with your life or well-being, such as hot flashes, mood swings or changes in sexual function that concern you, see your doctor.
When does perimenopause usually start?
Perimenopause, the transition to menopause, usually starts in a woman’s mid- to late 40s 3. On average, women are in perimenopause for four years before their periods stop.
How will I know if I am in perimenopause?
Sometimes it can be hard for you and your doctor to tell whether you are in perimenopause, the transition to menopause:
- Symptoms: Tell your doctor about your symptoms such as hot flashes or trouble sleeping. If you’re getting too little or poor-quality sleep, you may have trouble making decisions, solving problems, controlling your emotions and behavior, and coping with change. Not getting enough sleep has also been linked to depression, risk-taking behavior, and suicide.
- Irregular periods: Track your periods. Irregular periods may be your first sign of menopause.
- Hormone levels: Your doctor may test the amount of hormones in your blood if your periods stopped at an early age (before 40). Doctors don’t usually recommend this test unless there is a medical reason to do so. This is because for most women hormone levels go up and down in an unpredictable way during perimenopause. So it is difficult to tell for sure whether you have gone through menopause or are getting close to it based on this blood test alone.
How do I know if my period is abnormal?
It is NOT normal to have:
- Bleeding or spotting between periods
- Bleeding or spotting after sex
- Heavy bleeding during your period
- Bleeding that is heavier or lasts for more days than usual
- Bleeding after menopause
You should always see your doctor about any bleeding changes. Abnormal bleeding sometimes can be a sign of health problems. It’s especially important to tell your doctor if you have bleeding after menopause.
Many things can cause abnormal bleeding, including:
- Polyps. Polyps are noncancerous (benign) growths that attach to the wall of the uterus. They also may develop on the endometrium (lining of the uterus). These growths may cause irregular or heavy bleeding. Polyps also can grow on the cervix or inside the cervical canal. Polyps on the cervix may cause bleeding after sex.
- Endometrial atrophy. After menopause, the uterine lining may become too thin. This can happen when a woman has low levels of estrogen. The condition is called endometrial atrophy. As the lining thins, a woman may have abnormal bleeding.
- Endometrial hyperplasia is a condition that causes the lining of the uterus to get too thick. The condition is not cancer, but in some cases, it can lead to cancer. Endometrial hyperplasia most often is caused when a woman has too much estrogen and not enough progesterone. Early treatment may reduce the risk of endometrial cancer developing.Endometrial hyperplasia.
- Endometrial cancer. Endometrial cancer is cancer of the lining of the uterus. It is the most common type of cancer of the female reproductive system. Bleeding is the most common sign of endometrial cancer in postmenopausal women. When diagnosed early, most cases of endometrial cancer can be treated successfully.
- Other types of cancer.
How long does perimenopause last?
Perimenopause can last between two and eight years before your periods stop permanently 7. For most women, perimenopause lasts about 4 years. You will know you have reached menopause only after it has been a full 12 months in a row since your last period. This means you have not had any bleeding, including spotting, for 12 months in a row.
Should I continue using birth control during perimenopause?
Yes. You can still get pregnant during perimenopause even if you miss your period for a month or a few months 7. During perimenopause you may still ovulate, or release an egg, on some months. But it is impossible to know for sure when you will ovulate 7. A missing period may mean you are pregnant. It’s important to take a pregnancy test if you miss a period. If you don’t want to get pregnant, you should continue to use birth control until one full year after your last period. Talk to your doctor about your birth control needs.
What other health problems increase during perimenopause?
The estrogen produced by women’s ovaries before menopause protects against heart attacks and stroke. When less estrogen is made during perimenopause and after menopause, women lose much of this protection. Midlife also is the time when risk factors for heart disease, such as high cholesterol levels, high blood pressure, and being physically inactive, are more common. All of these combined factors increase the risk of heart attack and stroke in menopausal women.
What is menopause?
Menopause is when your periods stop permanently and you can no longer get pregnant. Menopause happens when you have gone 12 months in a row without a period. This means you have not had any bleeding, including spotting, for 12 months in a row. After menopause your ovaries make very little of the hormones estrogen and progesterone. These low hormone levels can raise your risk for certain health problems.
The average age of menopause in the United States is 51. The range for women is usually between 45 and 58. One way to tell when you might go through menopause is the age your mother went through it 8.
When does menopause usually happen?
Menopause happens when you have gone 12 months in a row without a period. The average age of menopause in the United States is 51. The range for women is usually between 45 and 58 3. One way to tell when you might go through menopause is the age your mother went through it 8.
Menopause may happen earlier if you:
- Never had children. Pregnancy, especially more than one pregnancy, may delay menopause 9.
- Smoke. Studies show smoking can cause you to start menopause up to two years earlier than women who don’t smoke 10.
Certain health problems can also cause you to start menopause earlier. Menopause usually happens on its own. However, you may enter menopause earlier than you normally would if you have had chemotherapy or surgery to remove both ovaries.
What happens after menopause?
After menopause you will no longer be able to get pregnant and you will no longer get a period. If you have any type of vaginal bleeding after menopause, you should see a doctor as soon as possible. Vaginal bleeding after menopause is not normal and can mean that you have a serious health problem.
You may experience any of the following after menopause:
- Low hormone levels. With menopause, your ovaries make very little of the hormones estrogen and progesterone. Because of changing hormone levels, you may develop certain health risks, including osteoporosis, heart disease, and stroke.
- Menopause symptoms instead of period problems. After menopause, most women get relief from period problems or menopause symptoms. However, you may still experience symptoms such as hot flashes because of changing estrogen levels. One recent study found that hot flashes can continue for up to 14 years after menopause 11, 12.
- Vaginal dryness. Vaginal dryness may be more common post-menopause.
Perimenopause symptoms
The signs and symptoms that many women experience during perimenopause are caused by gradually decreasing levels of estrogen. Each woman’s perimenopause experience is different. Many women who undergo natural menopause report no physical changes at all during the perimenopausal years except irregular menstrual periods that eventually stop when they reach menopause. Other changes may include hot flashes, difficulty sleeping, memory problems, mood disturbances, vaginal dryness, and weight gain. Not all these changes are hormone-related, and some, such as hot flashes and memory problems, tend to resolve after menopause. Maintaining a healthy lifestyle during this time of transition is essential for your health and can even prevent or blunt some of these changes.
You may have only a few symptoms, or you may have many. Symptoms may be mild, or they may be severe.
Changes in Your Menstrual Cycle
A common sign of perimenopause is a change in your menstrual cycle. Cycles may become longer than usual for you, or they may become shorter. You may begin to skip periods. The amount of flow may become lighter or heavier. Although changes in menstrual bleeding are normal as you approach menopause, you still should report them to your doctor.
Irregular periods. As ovulation becomes more unpredictable, the length of time between periods may be longer or shorter, your flow may be light to heavy, and you may skip some periods. If you have a persistent change of seven days or more in the length of your menstrual cycle, you may be in early perimenopause. If you have a space of 60 days or more between periods, you’re likely in late perimenopause.
Abnormal bleeding may be a sign of other problem. Talk to your doctor if you have any of the following:
- Bleeding between periods
- Bleeding after sex
- Spotting at anytime in the menstrual cycle
- Bleeding that is heavier or lasts for more days than usual
- Any bleeding after menopause
Many things can cause abnormal bleeding, including:
- Polyps. Polyps are noncancerous (benign) growths that attach to the wall of the uterus. They also may develop on the endometrium (lining of the uterus). These growths may cause irregular or heavy bleeding. Polyps also can grow on the cervix or inside the cervical canal. Polyps on the cervix may cause bleeding after sex.
- Endometrial atrophy. After menopause, the uterine lining may become too thin. This can happen when a woman has low levels of estrogen. The condition is called endometrial atrophy. As the lining thins, a woman may have abnormal bleeding.
- Endometrial hyperplasia is a condition that causes the lining of the uterus to get too thick. The condition is not cancer, but in some cases, it can lead to cancer. Endometrial hyperplasia most often is caused when a woman has too much estrogen and not enough progesterone. Early treatment may reduce the risk of endometrial cancer developing.Endometrial hyperplasia.
- Endometrial cancer. Endometrial cancer is cancer of the lining of the uterus. It is the most common type of cancer of the female reproductive system. Bleeding is the most common sign of endometrial cancer in postmenopausal women. When diagnosed early, most cases of endometrial cancer can be treated successfully.
- Other types of cancer.
Although the removal of the uterus (a hysterectomy) ends menstrual periods, it does not cause menopause unless the ovaries also are removed. This type of surgery is called an oophorectomy. An oophorectomy causes immediate menopause signs and symptoms if it is done before a woman reaches menopause.
Hot Flashes
Hot flashes and night sweats also called vasomotor symptoms are one of the most common symptoms of perimenopause and menopause and can significantly affect women’s quality of life 11, 13, 14, 15.
- A hot flash is a sudden feeling of heat that spreads over the face and body. The skin may redden like a blush. You also may break out in a sweat. A hot flash may last from a few seconds to several minutes or longer. Hot flashes are not harmful, but they sometimes are embarrassing and may interfere with daily life. Some women have hot flashes a few times a month. Others have them several times a day. Hot flashes that happen at night (night sweats) may wake you up and cause you to feel tired and sluggish during the day. The intensity, length and frequency vary. Although their exact cause still isn’t fully understood, hot flashes are thought to be the result of changes in the hypothalamus, the part of the brain that regulates the body’s temperature. If the hypothalamus mistakenly senses that a woman is too warm, it starts a chain of events to cool her down. Blood vessels near the surface of the skin begin to dilate (enlarge), increasing blood flow to the surface in an attempt to dissipate body heat. This produces a red, flushed look to the face and neck in light-skinned women. It may also make a woman perspire to cool the body down. The heart may beat faster, and women may sense that rapid heartbeat. A cold chill often follows a hot flash. A few women experience only the chill.
- Most women experience hot flashes for 6 months to 2 years, although some reports suggest that they last considerably longer—as long as 10 years, depending on when they began. For a small proportion of women, they may never go away. It is not uncommon for women to experience a recurrence of hot flashes more than 10 years after menopause, even into their 70s or beyond. There is no reliable way of predicting when they will start—or stop.
Night sweats
If you wake up with your pyjamas and sheets soaked with perspiration, even when it’s not hot or you don’t have too many blankets on the bed, you may be having night sweats. Anyone can have night sweats, no matter your gender or age.
The most common causes of night sweats are related to hormonal changes in women, such as occur with:
- Menopause or perimenopause
- Premenstrual syndrome (PMS)
- Pregnancy
For menopause-related night sweats, your doctor may recommend hormone replacement therapy (HRT). Ask your doctor if hormone therapy is suitable for you, as it isn’t recommended for everyone.
Other causes include:
- anxiety and being stressed
- sleep disorders such as sleep apnoea
- some infections, including flu (influenza), and tuberculosis
- some kinds of cancer, such as non-Hodgkins lymphoma or leukaemia
- stroke
- thyroid disease
- idiopathic hyperhidrosis — a condition in which the body continually produces too much sweat for no clear reason
Some medicines can also cause night sweats, including:
- medicines used to reduce fever, such as paracetamol and aspirin
- antidepressants
- diabetes medicines
- medicines used to treat high blood pressure
- steroid medicines, such as prednisolone
- some cancer treatments
- methadone (used to treat opioid dependence)
Sleep problems
Sleep problems are often due to hot flashes or night sweats, but sometimes sleep becomes unpredictable even without them. However, there are many reasons for sleep disturbances besides menopausal night sweats (simply, hot flashes at night). Your sleep disturbances may be caused by factors that affect many women beginning at midlife, such as sleep-disordered breathing (known as sleep apnea), restless legs syndrome, stress, anxiety, depression, painful chronic illnesses, and even some medications. Any treatment should first focus on improving your sleep routine—use regular hours to sleep each night, avoid getting too warm while sleeping, avoid stimulants such as caffeine and dark chocolate. When lifestyle changes fail to alleviate sleep disturbances, your clinician may want to refer you to a sleep center to rule out sleep-related disorders before initiating prescription treatment. If your sleep disturbance is related solely to hot flashes, hormone therapy is likely to help.
Mood changes
Mood swings and irritability that are similar to premenstrual syndrome (PMS) may happen during perimenopause. You might feel irritable, have low energy, feel tearful and moody, or have a hard time concentrating. Unlike PMS (premenstrual syndrome), these symptoms may come at times unrelated to your menstrual cycle. Symptoms may occur for years with no pattern. This type of mood change is known as perimenopausal mood instability. About 4 in 10 women have mood symptoms during perimenopause. The cause of these symptoms may be sleep disruption associated with hot flashes. Mood changes may also be caused by factors not related to the hormonal changes of perimenopause. Most women make the transition into menopause without experiencing depression, but many women report symptoms of moodiness, depressed mood, anxiety, stress, and a decreased sense of well-being during perimenopause. Women with a history of clinical depression or a history of premenstrual syndrome (PMS) or postpartum depression seem to be particularly vulnerable to recurrent depression during perimenopause, as are women who report significant stress, sexual dysfunction, physical inactivity, or hot flashes.
Most studies showed that the risk of depression increases during perimenopause. Symptoms of depression include crying a lot, feeling hopeless or worthless, feeling numb, and losing interest in your normal activities.
The idea of growing older may be difficult or depressing for some women. Sometimes menopause just comes at a bad time in a woman’s life. She may have other challenges to deal with at midlife, and menopause gives her one more problem on her list. It has been suggested that mood symptoms may be related to erratic fluctuations in estrogen levels, but limited data exist on why this occurs. Antidepressants are the primary pharmacologic treatment for menopause-associated depression. Menopause hormone therapy and hormone contraceptives can be used as off-label therapies, especially in women with concurrent hot flashes.
Anxiety
There are few studies about anxiety and perimenopause, but some women report symptoms of anxiety during this time. Anxiety involves constant worrying that gets in the way of your day-to-day life. You may feel muscle tension, sweating, or nausea. Both depression and anxiety can make it hard to concentrate, sleep, and take care of yourself.
Vaginal and Urinary Tract Changes
As estrogen levels decrease, changes take place in the vagina. Over time, the vaginal lining gets thinner, dryer, and less elastic. Vaginal dryness may cause pain during sexual intercourse. Vaginal infections also may occur more often.
The urinary tract also changes with age. The urethra can become dry, inflamed, or irritated. Some women may need to urinate more often. Women may have an increased risk of urinary tract infections after menopause.
Vaginal and bladder problems. When estrogen levels diminish, your vaginal tissues may lose lubrication and elasticity, making intercourse painful. Low estrogen may also leave you more vulnerable to urinary or vaginal infections. Loss of tissue tone may contribute to urinary incontinence.
Decreasing fertility
As ovulation becomes irregular, your ability to conceive decreases. However, as long as you’re having periods, pregnancy is still possible. If you wish to avoid pregnancy, use birth control until you’ve had no periods for 12 months.
Changes in sexual function
During perimenopause, sexual arousal and desire may change. But if you had satisfactory sexual intimacy before menopause, this will likely continue through perimenopause and beyond.
Sexual desire decreases with age in both sexes, and low desire is common in women in their 40s and 50s, but not universal. Some women have increased interest, while others notice no change at all. There is no major drop in testosterone at menopause. If lack of interest is related to discomfort with intercourse, estrogen may help. What’s important to remember is that there is a full range of psychological, cultural, personal, interpersonal and biological factors that can contribute to declining sexual interest, so if the decline in desire is bothering you, tell your healthcare provider. A clinical evaluation can identify any underlying medical or psychological causes of low sexual desire, which then can be treated as appropriate.
Bone Changes and Osteoporosis
Bones are constantly changing throughout life. Old bone is removed in a process called resorption. New bone is built in a process called formation. During the teen years, bone is formed faster than it is broken down. The amount of bone in the body (sometimes called the “bone mass”) reaches its peak during the late teen years. In midlife, the process begins to reverse: Bone is broken down faster than it is made. A small amount of bone loss after age 35 years is normal for men and women. But during the first 4–8 years after menopause, women lose bone more rapidly. This rapid loss occurs because of the decreased levels of estrogen. If too much bone is lost, it can increase your risk of osteoporosis (a disease that causes fragile bones). Osteoporosis increases the risk of bone fracture. The bones of the hip, wrist, and spine are affected most often.
Changing cholesterol levels
Declining estrogen levels may lead to unfavorable changes in your blood cholesterol levels, including an increase in low-density lipoprotein (LDL) cholesterol — the “bad” cholesterol — which contributes to an increased risk of heart disease. At the same time, high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — decreases in many women as they age, which also increases the risk of heart disease.
Headaches
Studies suggest that hormones may play a role in headaches. Women at increased risk for hormonal headaches during perimenopause are those who have already had headaches influenced by hormones, such as those with a history of headaches around their menstrual periods (so-called menstrual migraines) or when taking oral contraceptives. Hormonal headaches typically stop when menopause is reached and hormone levels are consistently low. Most headaches do not require treatment or can be treated with nonprescription pain medications. Some headaches, however, can be serious. More serious headaches, including migraines, may require prescription drugs; however, care should be taken to monitor the use of these drugs. If a headache is unusually painful or different from those you have had before, seek medical help promptly.
Memory changes
Your memory and other cognitive abilities change throughout life. Difficulty concentrating and remembering are common complaints during perimenopause and the years right after menopause. Some data imply that even though there is a trend for memory to be worse during the menopause transition, memory after the transition is as good as it was before. Memory problems may be more related to normal cognitive aging, mood, and other factors than to menopause or the menopause transition. Maintaining an extensive social network, remaining physically and mentally active, consuming a healthy diet, not smoking, and consuming alcohol in moderation may all help prevent memory loss. Atherosclerosis (hardening of the arteries) may also contribute to mental decline. Aim for normal cholesterol, normal weight, and normal blood pressure to help protect your brain. Women who are concerned about declining cognitive performance are advised to consult with their healthcare providers.
Perimenopause causes
Perimenopause takes place as your ovaries start to run out of eggs. As you go through perimenopause, your body’s production of estrogen and progesterone rises and falls. Changes in your hormone levels can cause perimenopausal symptoms like hot flushes. Many of the changes you experience during perimenopause are a result of decreasing estrogen.
Some people experience sudden menopause because of surgery or cancer treatment.
Risk factors of perimenopause
Menopause is a normal phase in life. But it may occur earlier in some women than in others. Although not always conclusive, some evidence suggests that certain factors may make it more likely that you start perimenopause at an earlier age, including:
- Smoking. The onset of menopause occurs one to two years earlier in women who smoke than in women who don’t smoke.
- Family history. Women with a family history of early menopause may experience early menopause themselves.
- Cancer treatment. Treatment for cancer with chemotherapy or pelvic radiation therapy has been linked to early menopause.
- Hysterectomy. A hysterectomy is surgery that removes your uterus, but not your ovaries, usually doesn’t cause menopause. Although you no longer have periods, your ovaries still produce estrogen. But such surgery may cause menopause to occur earlier than average. Also, if you have one ovary removed, the remaining ovary might stop working sooner than expected.
Perimenopause complications
Irregular periods are a hallmark of perimenopause. Most of the time this is normal and nothing to be concerned about. However, see your doctor if:
- Bleeding is extremely heavy — you’re changing tampons or pads every hour or two for two or more hours
- Bleeding lasts longer than seven days
- Bleeding occurs between periods
- Periods regularly occur less than 21 days apart
Signs such as these may mean there’s a problem with your reproductive system that requires diagnosis and treatment.
Perimenopause diagnosis
Perimenopause is a process — a gradual transition to menopause. No one test or sign is enough to determine if you’ve entered perimenopause. Your doctor takes many things into consideration, including your age, menstrual history, family history and what symptoms or body changes you’re experiencing. In around 75% of women, symptoms of perimenopause begin during the expected age range and doctors can diagnose menopause without laboratory testing. Menopause is confirmed after a woman has had no menstrual period for 12 months.
However, menopause testing is often ordered when the cause of your symptoms is not clear. For example, menopause testing may be used for women who have had a hysterectomy (surgery to remove the uterus), women who begin to have symptoms of menopause several years before age 50, or when a woman experiences abnormal symptoms suggestive of menopause.
Some doctors may order tests to check your hormone levels. But other than checking thyroid function, which can affect hormone levels, hormone testing is rarely necessary or useful to evaluate perimenopause.
Perimenopause test
As women age, the ovaries become less responsive to follicle-stimulating hormone (FSH) and luteinizing hormone (LH), two hormones important for ovulation and regulating menstrual periods. In response, the ovaries stop producing estrogen and progesterone, causing estrogen levels in the body to decrease and follicle-stimulating hormone (FSH) levels to increase.
When testing for menopause is warranted, doctors may order an follicle-stimulating hormone (FSH) test to detect elevated levels of FSH in the blood. Measuring FSH can help determine if a woman is perimenopausal or has already gone through menopause.
Because FSH levels naturally fluctuate each month to stimulate ovulation, results of FSH testing should be interpreted with caution and may be misleading. Rather than interpreting a single FSH test result, consistently elevated levels over time are used to confirm menopause.
Additional hormone tests that may be ordered to help a doctor diagnose menopause include:
- Estrogens. Level of estradiol in the blood to diagnose menstrual problems
- Luteinizing hormone (LH). Luteinizing hormone (LH) that can confirm the start of perimenopause
- Anti-Müllerian Hormone (AMH). Anti-Müllerian Hormone (AMH) can predict the start of menopause or determine the reason for early menopause
Perimenopause test at home
At-home perimenopause test kits are available that can analyze hormones that may be relevant to menopause, such as the following:
- At-home follicle-stimulating hormone (FSH) testing: At-home FSH tests detect elevated levels of FSH in a urine sample. However, this test cannot definitely diagnose menopause. At-home kits may be less accurate than a laboratory test for FSH.
- At-home estrogen testing: At-home estrogen testing measures the levels of three types of estrogens in a saliva sample: estrone, estradiol, and estriol. Estradiol levels may be used to help determine menopausal status but must be interpreted with the help of a doctor.
- At-home luteinizing hormone (LH) test: At-home luteinizing hormone tests measure levels of luteinizing hormone (LH) in a urine sample. This home test may be used to detect ovulation, but is not commonly used to detect menopause.
Tests to rule out other conditions
Other conditions can cause irregular menstruation or can stop it completely. In some cases, doctors will perform testing to determine whether something other than menopause is affecting menstruation.
Pregnancy test (Human Chorionic Gonadotropin Test)
A pregnancy test measures a hormone in the body called human chorionic gonadotropin (hCG), produced during pregnancy by the placenta and found in the blood and urine. Testing for hCG can be done as soon as 10 days after conception to help determine if you are pregnant. Measuring hCG can also help identify complications during pregnancy. Both urine and blood tests for hCG can be used for this purpose. Very early in a pregnancy, tests that measure the amount of hCG may also help assess the age of a fetus.
A pregnancy test is most commonly done when you believe you may be pregnant. Testing may detect a pregnancy as soon as 10 days after conception. The accuracy of pregnancy tests usually increases if taken at least one to two weeks after a missed menstrual period.
It may also be done when there are signs and symptoms that suggest an ectopic pregnancy or a pregnancy that is failing.
Signs of an ectopic pregnancy may include:
- Abnormal vaginal bleeding
- Low back pain
- Pain in the lower abdomen or pelvic area
- Cramping on one side of the pelvis
There are 2 different ways hCG results are reported:
- Qualitative hCG: Qualitative hCG tests give a positive or negative result depending on the presence or absence of hCG in the sample. Qualitative tests can be done using either a blood or urine sample. This type of testing is done most often to confirm a pregnancy.
- Quantitative hCG: Quantitative hCG testing measures the amount of hCG present in the blood. These tests frequently use a blood sample, but some urine tests can provide a degree of quantitative measurement. Along with confirming a pregnancy, quantitative hCG tests can also be used as part of the diagnostic process for abnormal pregnancies.
Thyroid function test
The thyroid function test is used to see how well your thyroid gland is functioning. The thyroid gland is responsible for producing hormones important for many bodily processes. Abnormal thyroid function, such as underactive thyroid (hypothyroidism) or overactive thyroid (hyperthyroidism), can lead to many symptoms. By measuring levels of thyroid hormones in the blood, the thyroid function test can help diagnose thyroid disorders and disrupted thyroid function. Another reason to get a thyroid test is if you are currently undergoing thyroid treatment and your doctor wants to determine whether it is effective or if your thyroid feels enlarged.
Three hormones are part of a standard thyroid function test:
- Thyroid-stimulating Hormone (TSH)
- Free T4 (thyroxine)
- Triiodothyronine (T3)
Prolactin blood test
Prolactin (PRL) is a hormone produced by the pituitary gland. Prolactin (PRL) is an anterior pituitary gland hormone for initiating and maintaining lactation. A prolactin test measures the amount of prolactin in your blood. Prolactin is often detected in high levels in people who are pregnant or just after childbirth. People who are not pregnant usually have low levels of prolactin in the blood.
Increased prolactin (PRL) level is seen in:
- Breast stimulation.
- Pregnancy.
- Breastfeeding.
- Stress.
- Exercise.
- A tumor in the pituitary gland called a prolactinoma that produce prolactin.
Moderate level increase in prolactin (PRL) is seen in the following:
- Secondary amenorrhea.
- Galactorrhea.
- Primary hypothyroidism.
- Polycystic ovary syndrome (PCOS).
- Anorexia.
Elevated prolactin (PRL) can interfere with the function of the ovaries and testes, which may cause the following symptoms:
- Infertility
- A change in sex drive
- Breast milk production that is not related to pregnancy or childbirth
- Erectile dysfunction
- Irregular menstrual cycles.
Perimenopause treatment
Medications are often used to treat perimenopausal symptoms.
- Hormone therapy also called menopausal hormonal therapy (MHT) or hormone replacement therapy (HRT). Systemic estrogen therapy — which comes in pill, skin patch, gel or cream form — remains the most effective treatment option for relieving perimenopausal and menopausal hot flashes and night sweats. About 1 in 4 women have symptoms that need treatment with these hormone medicines. There are benefits and risks to menopausal hormonal therapy (MHT), so it is important to talk to your doctor if you are considering starting or stopping it. Depending on your personal and family medical history, your doctor may recommend estrogen in the lowest dose needed to provide symptom relief for you. If you still have your uterus, you’ll need progestin in addition to estrogen. Systemic estrogen can help prevent bone loss. In some cases, testosterone therapy is also used.
- Selective estrogen receptor modulators (SERMs). Selective estrogen receptor modulators (SERMs) are drugs that act on tissues that respond to estrogen. SERMs are available for the relief of hot flashes and pain during intercourse caused by vaginal dryness.
- Vaginal estrogen. To relieve vaginal dryness, estrogen can be administered directly to the vagina using a vaginal tablet, ring or cream. This treatment releases just a small amount of estrogen, which is absorbed by the vaginal tissue. It can help relieve vaginal dryness, discomfort with intercourse and some urinary symptoms.
- Antidepressants. Certain antidepressants related to the class of drugs called selective serotonin reuptake inhibitors (SSRIs) may reduce menopausal hot flashes. An antidepressant for management of hot flashes may be useful for women who can’t take estrogen for health reasons or for women who need an antidepressant for a mood disorder.
- Gabapentin (Neurontin). Gabapentin is approved to treat seizures, but it has also been shown to help reduce hot flashes. Gabapentin is useful in women who can’t use estrogen therapy for health reasons and in those who also have migraines.
- Clonidine. Clonidine is a blood pressure medication called a vasodilator (dilate blood vessels). Clonidine helps to relax and widen blood vessels in the heart so blood can pass through them more easily. Clonidine is mainly used to treat hot flushes or sweats that may happen during the menopause.
- Fezolinetant (Veozah). Fezolinetant (Veozah) is a hormone-free option for treating menopause hot flashes. It works by blocking a pathway in the brain that helps regulate body temperature.
Before deciding on any form of treatment, talk with your doctor about your options and the risks and benefits involved with each. Review your options yearly, as your needs and treatment options may change.
Hormone therapy for perimenopause
Menopausal hormonal therapy (MHT) or hormone replacement therapy (HRT) for perimenopause include the following:
- Estrogen plus progestogen (natural or synthetic forms of progesterone) — for women who still have their uterus. Combined oestrogen and progestogen HRT is suitable for women who still have their uterus. Taking estrogen on its own would increase the risk of cancer of the lining of the uterus (endometrial cancer), but the progestogen helps protect against this. With this type of HRT, the estrogen is taken continuously, but the progestogen may be either continuous or cyclical (taken 10-14 days of each cycle).
- Estrogen only — for women who have had a surgery to remove the uterus (hysterectomy). Estrogen-only HRT is suitable for women who have had their uterus removed (hysterectomy).
- Tibolone. Tibolone is a synthetic estrogen used for treatment of symptoms of menopause and prevention of osteoporosis. Tibolone is approved in several European countries, but not in United States. Tibolone acts as a combined hormone therapy, with some effects of oestrogen, progesterone and testosterone. It is a synthetic steroid which is taken as a tablet. Tibolone can help with hot flushes and prevent bone loss after menopause. It can also help improve sexual function. It is not suitable for women who have had breast cancer.
- Estrogen plus SERM (selective oestrogen receptor modulator). Estrogen plus selective estrogen receptor modulator (SERM) is a newer treatment for menopause. It is a combination therapy containing an estrogen with a SERM (selective oestrogen receptor modulator) called bazedoxifene. It is taken as a tablet and can improve menopausal symptoms of hot flushes and night sweats, and to prevent osteoporosis. It is less effective than combined estrogen plus progestogen HRT, but has fewer side effects of breast tenderness and vaginal bleeding. It is only suitable for females with a uterus.
Menopausal hormonal therapy (MHT) can be helpful if you have problems with hot flushes and night sweats. You may also find that your sleep, mood, sex drive, joint aches and vaginal dryness gets better.
Hormone replacement therapy (HRT) may have some benefits in reducing your risk of osteoporosis, heart disease, fractures, type 2 diabetes and some types of cancers. If you don’t have hot flushes or night sweats, your doctor probably wouldn’t recommend you start HRT to try and prevent these conditions.
What are the risks of hormone replacement therapy (HRT)?
Some studies have shown that hormone replacement therapy (HRT) can lead to a slightly increased risk of developing breast cancer, while other studies suggest that some specific types of hormone replacement therapy (HRT) can lower your risk of breast cancer. Because these risks are based on specific health factors, it’s best to have a discussion with your doctor before you decide if you want to start or stop taking hormone replacement therapy (HRT).
Some forms of oestrogen in hormone replacement therapy (HRT) can increase your risk of blood clots (e.g., deep vein thrombosis), but using a cream is unlikely to increase the risk.
Current international recommendations say that the benefits of hormone replacement therapy (HRT) outweigh the risks for females with significant menopausal symptoms, and that hormone replacement therapy (HRT) is effective and safe for most healthy females.
Hormone replacement therapy (HRT) side effects may include:
- Nausea
- Headache
- Breast tenderness
- Fluid retention
- Bloating
- Irregular bleeding
These side effects often go away within a few months.
Hormone replacement therapy (HRT) is NOT suitable for you if you have or have had:
- breast cancer, endometrial cancer or other cancers that are dependent on hormones
- vaginal bleeding without a known cause
- a blood clot in a vein, such as those in the legs or lungs
- heart disease or stroke
- liver disease
- untreated high blood pressure
The risks of hormone replacement therapy (HRT) depend on many factors including:
- your age
- the type and dose of hormone therapy you take
- how long you take it for
- your medical history
If you can’t take hormone replacement therapy (HRT), your doctor may suggest other non-medical options and treatments that may be helpful.
Perimenopause hot flashes treatments
Although the available treatments for hot flashes do not cure hot flashes, they do offer relief. Hot flashes usually fade away eventually without treatment, and no treatment is necessary unless hot flashes are bothersome. A few women have an occasional hot flash forever. There are a number of low-risk coping strategies and lifestyle changes that may be helpful for managing hot flashes, but if hot flashes remain very disruptive, prescription therapy may be considered.
Prescription hormone therapy sometimes called menopausal hormone therapy (MHT) or hormone replacement therapy (HRT) approved by the US Food and Drug Administration (FDA) and by Health Canada include systemic estrogen therapy and estrogen-progestogen therapy (for women with a uterus)—are the standard treatment. Another FDA-approved hormone product, for women with a uterus, combines estrogen with bazedoxifene instead of a progestogen. Bazedoxifene is an estrogen agonist/antagonist, which means that it works like estrogen in some tissues while inhibiting estrogen activity in others. In this case, it helps to protect the uterus from cancer.
There are risks associated with taking hormones, including increased risk of heart attack, stroke, blood clots, breast cancer, gallbladder disease, and dementia. Women are encouraged to discuss the risks with their doctor. The risks vary by a woman’s age and whether she has had a hysterectomy. Women who still have a uterus would take estrogen combined with progesterone or another therapy to protect the uterus. Progesterone is added to estrogen to protect the uterus against cancer, but it also seems to increase the risk of blood clots and stroke.
For women who prefer not to take hormones or cannot hormones, nonhormone drugs approved to treat depression, called selective serotonin-reuptake inhibitors (SSRIs), have been found to be effective in treating hot flashes in women who don’t have depression. The only SSRI FDA has approved thus far for treating hot flashes is paroxetine 7.5 mg.
Researchers are studying other antidepressants, which doctors may prescribe for off-label use.
Women who use an antidepressant to help manage hot flashes generally take a lower dose than people who use the medication to treat depression. As with any medication, talk with your doctor about whether this is the right medication for you and how you might manage any possible side effects.
Lifestyle changes to improve hot flashes
Before considering medication, first try making changes to your lifestyle. If hot flashes keep you up at night, lower the temperature in your bedroom and try drinking small amounts of cold water before bed. Layer your bedding so it can be adjusted as needed and turn on a fan. Here are some other lifestyle changes you can make:
- Dress in layers that can be removed at the start of a hot flash.
- Carry a portable fan to use when a hot flash strikes.
- Avoid alcohol, spicy foods, and caffeine. These can make menopausal symptoms worse.
- If you smoke, try to quit, not only for hot flashes, but for your overall health.
- Try to maintain a healthy weight. Women who are overweight or obese may experience more frequent and severe hot flashes.
- Explore mind-body practices. Some early-stage research has shown that hypnotherapy and mindfulness meditation could help with management of hot flashes.
Perimenopause birth control: What are your options?
If you don’t intend to have any children in the future, one option is permanent sterilization for either you or your partner. Otherwise, if you’re generally in good health, and you don’t have any medical conditions that might preclude their use, hormonal forms of birth control may be an option, too.
For a woman during perimenopause, birth control options include:
- A combination estrogen-progestin pill or ring, if you don’t have a medical reason not to take contraceptive-strength doses of estrogen.
- A progestin-only contraceptive, such as the levonorgestrel intrauterine system (Mirena, Skyla), the etonogestrel subdermal implant (Nexplanon), or the progestin-only minipill, which also provide protection from cancer of the endometrium — the tissue that lines your uterus.
- An estrogen-progestin skin patch, if you’re not at risk of blood clots or other bleeding disorder. However, caution is needed when using this form of birth control. A patch that contains both estrogen and progestin, such as the skin path containing norelgestromin and ethinyl estradiol (Ortho Evra), increases blood clot risk compared with other forms of estrogen-progestin contraception, such as a pill or vaginal ring.
- A sterilization procedure, such as vasectomy or tubal ligation, which provides a permanent form of birth control.
Whichever method you choose, doctors generally recommend that you continue birth control during perimenopause and for about 12 months after your menstrual periods naturally stop.
Lifestyle and home remedies for perimenopause
Making these healthy lifestyle choices may help ease some symptoms of perimenopause and promote good health as you age:
- Ease vaginal discomfort. Use over-the-counter, water-based vaginal lubricants (Astroglide, K-Y jelly, others) or moisturizers (Replens, Vagisil, others). Choose products that don’t contain glycerin, which can cause burning or irritation in women who are sensitive to that chemical. Staying sexually active also helps by increasing blood flow to the vagina. DO NOT use petroleum jelly. DO NOT use mineral oils or other oils if you use condoms, as these may damage latex condoms or diaphragms.
- Eat healthy. Because your risk of osteoporosis and heart disease increases at this time, a healthy diet is more important than ever. Adopt a low-fat, high-fiber diet that’s rich in fruits, vegetables and whole grains. Add calcium-rich foods. Ask your doctor if you should also take a calcium supplement and if so, what type and how much — also ask if you need more vitamin D, which helps your body absorb calcium. Avoid alcohol and caffeine if they seem to trigger hot flashes.
- Be active. Regular exercise and physical activity helps prevent weight gain, improves your sleep and elevates your mood. Try to exercise for 30 minutes or more on most days of the week, although not right before bedtime. Regular exercise has been shown to reduce hip fracture risk in older women and to strengthen bone density.
- Get enough sleep. Try to keep a consistent sleep schedule. Avoid caffeine, which can make it hard to get to sleep, and avoid drinking too much alcohol, which can interrupt sleep.
- Practice stress reduction techniques. Practiced regularly, stress-reduction techniques, such as meditation or yoga, can promote relaxation and good health throughout your lifetime, but they may be particularly helpful during the menopausal transition.
To help control hot flashes:
- Dress lightly and in layers. Try to keep your environment cool.
- Practice slow, deep breathing whenever a hot flash starts to come on. Try taking six breaths per minute.
- Try relaxation techniques such as yoga, tai chi, or meditation.
Watching what you eat or drink can improve your symptoms and help you sleep:
- Eat at regular times each day. Eat a healthy diet that is low in fat and includes lots of fruits and vegetables.
- Milk and other dairy products contain tryptophan, which may help induce sleep.
- If you can, avoid coffee, colas with caffeine, and energy drinks completely. If you cannot avoid them, try not to have any after the early part of the afternoon.
- Alcohol may make your symptoms worse and often leads to a more disrupted sleep.
Nicotine stimulates the body and will make it harder to fall asleep. This includes both cigarettes and smokeless tobacco. So if you smoke, consider quitting.
Perimenopause supplements
In addition to conventional therapies, many women transitioning toward menopause want to know more about complementary and alternative approaches to treating symptoms. Researchers are looking into these therapies to determine their safety and effectiveness, but evidence is still often lacking.
Some of perimenopause supplements include:
Black cohosh. This herb extract is used by some women to treat hot flashes and other menopausal symptoms. There’s not enough evidence to support its use. Experts also are unsure of what risks taking black cohosh poses. Past studies suggested that black cohosh was harmful to the liver, but a more recent review of studies found no evidence that this is true. Researchers also question whether the herb extract is safe for women with or at risk of breast cancer.
Phytoestrogens. These estrogens occur naturally in certain foods. Two main types of phytoestrogens are isoflavones and lignans. Isoflavones are found in soybeans, chickpeas and other legumes. Lignans occur in flaxseed, whole grains, and some fruits and vegetables. There are also plant-derived compounds that have estrogen-like properties. Studies on phytoestrogens — whether from food or supplements — conflict on whether they help reduce menopausal symptoms. Studies also conflict on what beneficial impact, if any, phytoestrogens may have on breast cancer risk.
Isoflavone supplements generally come from soy or red clover. Lignans come mainly from flaxseed.
Bioidentical hormones. The term “bioidentical” implies the hormones in the product are chemically identical to those your body produces. However, compounded bioidentical hormones aren’t regulated by the Food and Drug Administration (FDA), so quality and risks could vary. There’s also no evidence that compounded bioidentical hormones are safer or more effective than conventional hormone therapy.
Dehydroepiandrosterone (DHEA). This natural steroid produced by your adrenal gland is available as a dietary supplement and has been used by some to reduce pain during intercourse due to vaginal atrophy. But evidence on its effectiveness is mixed, and there are some concerns about possible harmful effects.
Low-risk complementary therapies, such as acupuncture, yoga and paced breathing may help reduce stress and improve psychological well-being. Research on acupuncture for decreasing hot flashes is inconclusive, but promising. Relaxation can help reduce stress, which may in turn help improve menopausal symptoms.
Talk with your doctor before taking any herbal or dietary supplements for perimenopausal or menopausal symptoms. The FDA does not regulate herbal products, and some can be dangerous or interact with other medications you take, putting your health at risk.
- Santoro N. Perimenopause: From research to practice. J. Women’s Health. 2016;25:332–339. doi: 10.1089/jwh.2015.5556[↩]
- Perimenopause & Premature Menopause FAQS. http://www.menopause.org/for-women/expert-answers-to-frequently-asked-questions-about-menopause/perimenopause-premature-menopause-faqs[↩]
- Shifren JL, Gass ML; NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014 Oct;21(10):1038-62. doi: 10.1097/GME.0000000000000319[↩][↩][↩]
- Perimenopause. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666[↩]
- The Menopause Years. https://www.acog.org/womens-health/faqs/the-menopause-years[↩]
- Santoro N. Perimenopause: From Research to Practice. J Womens Health (Larchmt). 2016 Apr;25(4):332-9. doi: 10.1089/jwh.2015.5556[↩]
- Menopause basics. https://www.womenshealth.gov/menopause/menopause-basics[↩][↩][↩]
- Mishra GD, Cooper R, Tom SE, Kuh D. Early life circumstances and their impact on menarche and menopause. Womens Health (Lond). 2009 Mar;5(2):175-90. doi: 10.2217/17455057.5.2.175[↩][↩]
- A longitudinal analysis of women’s attitudes toward the menopause: results from the Massachusetts Women’s Health Study. Avis, N.E. et al. Maturitas, Volume 13, Issue 1, 65 – 79. https://www.maturitas.org/article/0378-5122(91)90286-Y/abstract[↩]
- Smoking’s Impact on Women’s Health. https://women.smokefree.gov/quit-smoking-women/what-women-should-know/smokings-impact-on-women[↩]
- Avis NE, Crawford SL, Greendale G, Bromberger JT, Everson-Rose SA, Gold EB, Hess R, Joffe H, Kravitz HM, Tepper PG, Thurston RC; Study of Women’s Health Across the Nation. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015 Apr;175(4):531-9. doi: 10.1001/jamainternmed.2014.8063[↩][↩]
- Tepper PG, Brooks MM, Randolph JF Jr, Crawford SL, El Khoudary SR, Gold EB, Lasley BL, Jones B, Joffe H, Hess R, Avis NE, Harlow S, McConnell DS, Bromberger JT, Zheng H, Ruppert K, Thurston RC. Characterizing the trajectories of vasomotor symptoms across the menopausal transition. Menopause. 2016 Oct;23(10):1067-74. doi: 10.1097/GME.0000000000000676[↩]
- Avis NE, Ory M, Matthews KA, Schocken M, Bromberger J, Colvin A. Health-related quality of life in a multiethnic sample of middle-aged women: Study of Women’s Health Across the Nation (SWAN). Med Care. 2003 Nov;41(11):1262-76. doi: 10.1097/01.MLR.0000093479.39115.AF[↩]
- Blümel JE, Chedraui P, Baron G, Belzares E, Bencosme A, Calle A, Danckers L, Espinoza MT, Flores D, Gomez G, Hernandez-Bueno JA, Izaguirre H, Leon-Leon P, Lima S, Mezones-Holguin E, Monterrosa A, Mostajo D, Navarro D, Ojeda E, Onatra W, Royer M, Soto E, Tserotas K, Vallejo S; Collaborative Group for Research of the Climacteric in Latin America (REDLINC). A large multinational study of vasomotor symptom prevalence, duration, and impact on quality of life in middle-aged women. Menopause. 2011 Jul;18(7):778-85. doi: 10.1097/gme.0b013e318207851d[↩]
- Williams RE, Levine KB, Kalilani L, Lewis J, Clark RV. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas. 2009 Feb 20;62(2):153-9. doi: 10.1016/j.maturitas.2008.12.006[↩]