Contents
- What is heart disease
- Heart Disease in Men
- Heart Disease in Women
What is heart disease
The term “heart disease” refers to several types of heart conditions or one of several cardiovascular diseases 1. The most common type of heart disease in the United States is coronary artery disease, which affects the blood flow to the heart. A heart attack happens when an coronary artery becomes blocked, preventing oxygen and nutrients from getting to the heart. Other heart disease or cardiovascular diseases include stroke, high blood pressure, angina (chest pain), and rheumatic heart disease.
One reason some women aren’t too concerned about heart disease is that they think it’s men’s problem and heart disease can be “cured” with surgery or medication 2. This is a myth. Heart disease is a lifelong condition—once you get it, you’ll always have it. True, procedures such as bypass surgery and percutaneous coronary intervention can help blood and oxygen flow to the heart more easily. But the arteries remain damaged, which means you are more likely to have a heart attack. What’s more, the condition of your blood vessels will steadily worsen unless you make changes in your daily habits. Many women die of complications from heart disease, or become permanently disabled. That’s why it is so vital to take action to prevent and control this disease.
Heart Disease Facts
- Heart disease is the leading cause of death for both men and women. More than half of the deaths due to heart disease in 2015 were in men 3.
- About 630,000 Americans die from heart disease each year—that’s 1 in every 4 deaths 3.
- Coronary heart disease is the most common type of heart disease, killing about 366,000 people in 2015 3.
- In the United States, someone has a heart attack every 40 seconds. Each minute, more than one person in the United States dies from a heart disease-related event 4.
- Heart disease is the leading cause of death for people of most racial/ethnic groups in the United States, including African Americans, Hispanics, and whites. For Asian Americans or Pacific Islanders and American Indians or Alaska Natives, heart disease is second only to cancer 5.
- Heart disease costs the United States about $200 billion each year 3. This total includes the cost of health care services, medications, and lost productivity.
Heart Disease Risk Factors
Several health conditions, your lifestyle, and your age and family history can increase your risk for heart disease. These are called risk factors. About half of all Americans (47%) have at least one of the three key risk factors for heart disease: high blood pressure, high cholesterol, and smoking 6.
Some of the risk factors for heart disease cannot be controlled, such as your age or family history. But you can take steps to lower your risk by changing the factors you can control.
Conditions that Increase Risk for Heart Disease
Several medical conditions can increase your risk for heart disease. If you have one of these conditions, you can take steps to control it and lower your risk.
- High Blood Pressure
High blood pressure is a major risk factor for heart disease. It is a medical condition that occurs when the pressure of the blood in your arteries and other blood vessels is too high. The high pressure, if not controlled, can affect your heart and other major organs of your body, including your kidneys and brain.
High blood pressure is often called a “silent killer” because many people do not notice symptoms to signal high blood pressure. Lowering blood pressure by changes in lifestyle or by medication can reduce your risk for heart disease and heart attack.
- High Cholesterol
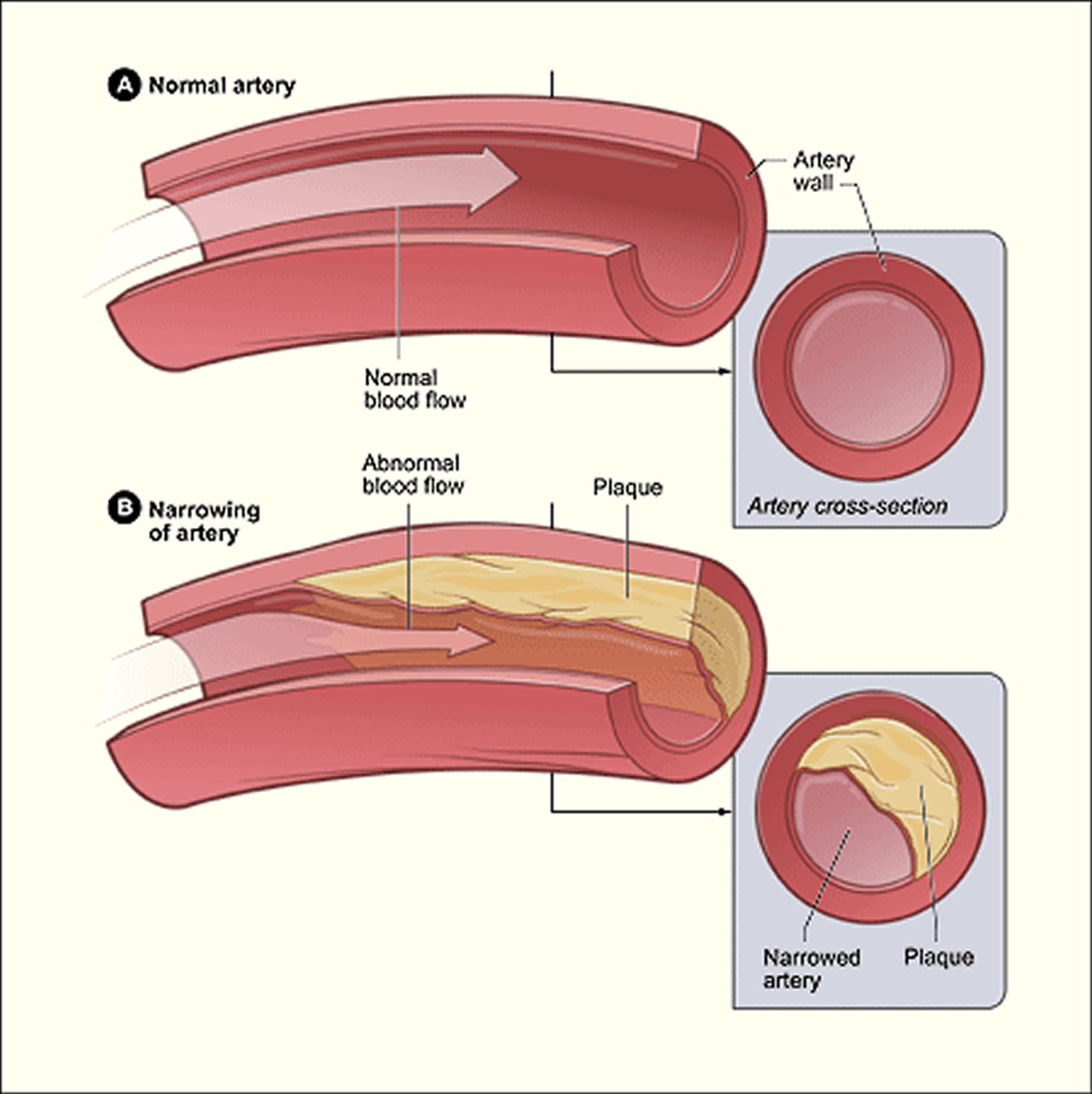
Cholesterol is a waxy, fat-like substance made by the liver or found in certain foods. Your liver makes enough for your body’s needs, but we often get more cholesterol from the foods we eat. If we take in more cholesterol than the body can use, the extra cholesterol can build up in the walls of the arteries, including those of the heart. This leads to narrowing of the arteries and can decrease the blood flow to the heart, brain, kidneys, and other parts of the body.
Some cholesterol is “good,” and some is “bad.” High cholesterol is the term used for high levels of low-density lipoprotein, or LDL, which are considered “bad” because they can lead to heart disease. A higher level of high-density lipoprotein cholesterol, or HDL, is considered “good” because it provides some protection against heart disease.
A blood test can detect the amount of cholesterol and triglycerides (a related kind of fat) in your blood.
- Diabetes
Diabetes mellitus also increases the risk for heart disease. Your body needs glucose (sugar) for energy. Insulin is a hormone made in the pancreas that helps move glucose from the food you eat to your body’s cells. If you have diabetes, your body doesn’t make enough insulin, can’t use its own insulin as well as it should, or both.
Diabetes causes sugars to build up in the blood. The risk of death from heart disease for adults with diabetes is two to four times higher than adults who do not have diabetes 7. Talk to your doctor about ways to manage diabetes and control other risk factors.
Behaviors That Increase Your Risk for Heart Disease
Your lifestyle choices can increase your risk for heart disease and heart attack. To reduce your risk, your doctor may recommend changes to your lifestyle. The good news is that healthy behaviors can lower your risk for heart disease.
Unhealthy Diet
Diets high in saturated fats, trans fat, and cholesterol have been linked to heart disease and related conditions, such as atherosclerosis. Also, too much salt (sodium) in the diet can raise blood pressure levels.
Physical Inactivity
Not getting enough physical activity can lead to heart disease. It also can increase the chances of having other medical conditions that are risk factors, including obesity, high blood pressure, high cholesterol, and diabetes. Regular physical activity can lower your risk for heart disease.
Obesity
Obesity is excess body fat. Obesity is linked to higher “bad” cholesterol and triglyceride levels and to lower “good” cholesterol levels. In addition to heart disease, obesity can also lead to high blood pressure and diabetes. Talk to your health care team about a plan to reduce your weight to a healthy level.
Too Much Alcohol
Drinking too much alcohol can raise blood pressure levels and the risk for heart disease. It also increases levels of triglycerides, a form of cholesterol, which can harden your arteries.
- Women should have no more than 1 drink a day.
- Men should have no more than 2 drinks a day.
Tobacco Use
Tobacco use increases the risk for heart disease and heart attack. Cigarette smoking can damage the heart and blood vessels, which increases your risk for heart conditions such as atherosclerosis and heart attack. Also, nicotine raises blood pressure, and carbon monoxide reduces the amount of oxygen that your blood can carry. Exposure to other people’s secondhand smoke can increase the risk for heart disease even for nonsmokers.
Family History and Other Characteristics That Increase Risk for Heart Disease
Family members share genes, behaviors, lifestyles, and environments that can influence their health and their risk for disease. Heart disease can run in a family, and your risk for heart disease can increase based on your age, and your race, or ethnicity.
Genetics and Family History
When members of a family pass traits from one generation to another through genes, that process is called heredity.
Genetic factors likely play some role in high blood pressure, heart disease, and other related conditions. However, it is also likely that people with a family history of heart disease share common environments and other potential factors that increase their risk.
The risk for heart disease can increase even more when heredity combines with unhealthy lifestyle choices, such as smoking cigarettes and eating an unhealthy diet.
Other Characteristics
Both men and women can have heart disease. Some other characteristics that you cannot control, like your age, sex, and race or ethnicity, can affect your risk for heart disease.
- Age. Your risk for heart disease increases as you get older.
- Sex. Heart disease was the number one killer of both men and women in 2013 8.
- Race or ethnicity. In 2013 heart disease was the leading cause of death in the United States for non-Hispanic whites, non-Hispanic blacks, and American Indians. For Hispanics, and Asian Americans and Pacific Islanders, heart disease is second only to cancer as a cause of death 8.
- Stress.
What Causes Heart Disease ?
Research suggests that coronary heart disease begins with damage to the lining and inner layers of the coronary (heart) arteries. Several factors contribute to this damage. They include:
- Smoking, including secondhand smoke
- High amounts of certain fats and cholesterol in the blood
- High blood pressure
- High amounts of sugar in the blood due to insulin resistance or diabetes
- Blood vessel inflammation
Plaque may begin to build up where the arteries are damaged. The buildup of plaque in the coronary arteries may start in childhood.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause chest pain or discomfort called angina.
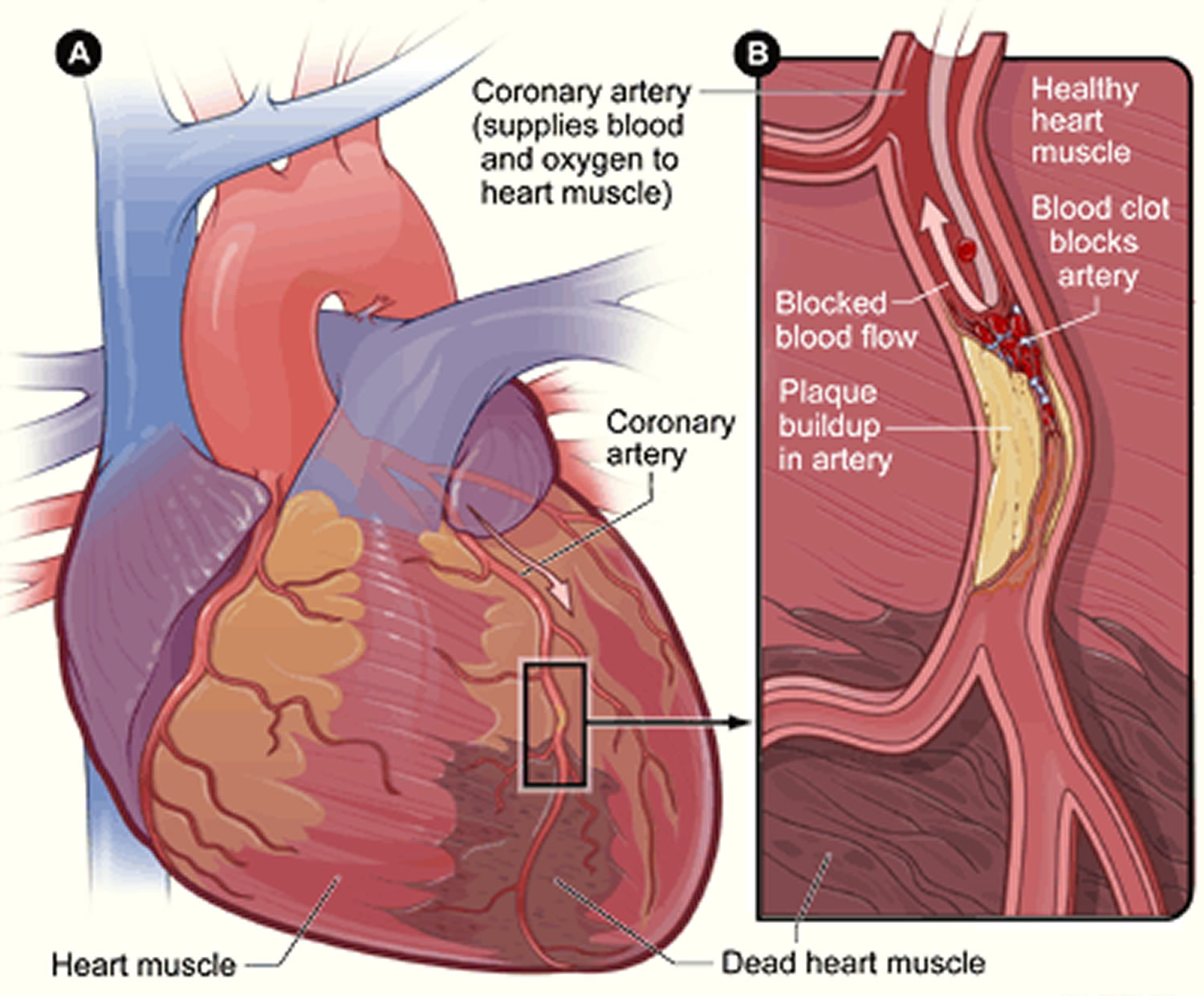
If the plaque ruptures, blood cell fragments called platelets stick to the site of the injury. They may clump together to form blood clots.
Blood clots can further narrow the coronary arteries and worsen angina. If a clot becomes large enough, it can mostly or completely block a coronary artery and cause a heart attack.
In addition to the factors above, low estrogen levels before or after menopause may play a role in causing coronary microvascular disease. Coronary microvascular disease is heart disease that affects the heart’s tiny arteries.
The cause of broken heart syndrome isn’t yet known. However, a sudden release of stress hormones may play a role in causing the disorder. Most cases of broken heart syndrome occur in women who have gone through menopause.
Preventing Heart Disease: What You Can Do
You can help prevent heart disease by making healthy choices and managing any health conditions you may have.
- Practice healthy living habits.
- Prevent or treat medical conditions.
Healthy Living Habits
By living a healthy lifestyle, you can help keep your blood pressure, cholesterol, and sugar normal and lower your risk for heart disease and heart attack. A healthy lifestyle includes the following:
- Eating a healthy diet.
- Maintaining a healthy weight.
- Getting enough physical activity.
- Not smoking or using other forms of tobacco.
- Limiting alcohol use.
Healthy Diet
Choosing healthful meal and snack options can help you avoid heart disease and its complications. Be sure to eat plenty of fresh fruits and vegetables and fewer processed foods.
Eating foods low in saturated fats, trans fat, and cholesterol and high in fiber can help prevent high cholesterol. Limiting salt (sodium) in your diet also can lower your blood pressure. Limiting sugar in your diet can lower you blood sugar level to prevent or help control diabetes.
Healthy Weight
Being overweight or obese increases your risk for heart disease. To determine if your weight is in a healthy range, doctors often calculate your body mass index (BMI). If you know your weight and height, you can calculate your BMI.
You can calculate your BMI by dividing your weight in kilograms by your height in meters squared (kg/m2). You can also use an online BMI calculator or BMI table.
To find out about your body mass index (BMI), you can use a FREE online BMI calculators from the Centers for Disease Control and Prevention (CDC) :
- Adults 9
For children and adolescents (younger than 20 years of age), overweight and obesity are based on the Centers for Disease Control and Prevention’s (CDC’s) BMI-for-age growth charts, which are available at 10.
The CDC has a BMI percentile calculator for children and teens at 11.
- Children 12
Body Mass Index for Men and Women Adults
The body mass index is an attempt to quantify the amount of tissue mass (muscle, fat, and bone) in an individual, and then categorize that person as underweight, normal weight, overweight, or obese based on that value. Commonly accepted body mass index ranges are:
A) Underweight: under 18.5 kg/m2,
B) Normal (Healthy BMI) weight: 18.5 to 25 kg/m2,
C) Overweight: 25 to 30 kg/m2,
D) Obese: over 30 to 39.9 kg/m2.
E) Severely Obese: over 40 kg/m2.
Waist size matters, too. In people who are not overweight, waist size may be an even more telling warning sign of increased health risks than BMI 13. An expert panel convened by the National Institutes of Health identified these useful benchmarks: Men should aim for a waist size below 40 inches (102 cm) and women should aim for a waist size below 35 inches (88 cm) 14.
Physical Activity
Physical activity can help you maintain a healthy weight and lower your blood pressure, cholesterol, and sugar levels. For adults, the Surgeon General recommends 2 hours and 30 minutes of moderate-intensity exercise, like brisk walking or bicycling, every week. Children and adolescents should get 1 hour of physical activity every day.
No Smoking
Cigarette smoking greatly increases your risk for heart disease. If you don’t smoke, don’t start. If you do smoke, quitting will lower your risk for heart disease. Your doctor can suggest ways to help you quit.
Limited Alcohol
Avoid drinking too much alcohol, which can raise your blood pressure. Men should have no more than 2 drinks per day, and women only 1.
Other Medical Conditions
If you have high cholesterol, high blood pressure, or diabetes, you can take steps to lower your risk for heart disease.
Check Cholesterol
Your health care provider should test your blood levels of cholesterol at least once every 5 years. If you have already been diagnosed with high cholesterol or have a family history of the condition, you may have your cholesterol checked more frequently. Talk with your health care team about this simple blood test. If you have high cholesterol, medications and lifestyle changes can help reduce your risk for heart disease.
Control Blood Pressure
High blood pressure usually has no symptoms, so be sure to have it checked on a regular basis. Your health care team should measure your blood pressure at least once every 2 years if you have never had high blood pressure or other risk factors for heart disease. If you have been diagnosed with high blood pressure, also called hypertension, your health care team will measure your blood pressure more frequently to ensure you have the condition under control. Talk to your health care team about how often you should check your blood pressure. You can check it at a doctor’s office, at a pharmacy, or at home.
If you have high blood pressure, your health care team might recommend some changes in your lifestyle or advise you to lower the sodium in your diet; your doctor may also prescribe medication when necessary to help lower your blood pressure. There are many strategies to help monitor and improve blood pressure control and medication adherence to improve health outcomes for patients with hypertension.
Manage Diabetes
If your health care provider thinks you have symptoms of diabetes, he or she may recommend that you get tested. If you have diabetes, monitor your blood sugar levels carefully 15. Talk with your health care team about treatment options. Your doctor may recommend certain lifestyle changes to help keep your blood sugar under good control—those actions will help reduce your risk for heart disease.
Take Your Medicine
If you take medication to treat high cholesterol, high blood pressure, or diabetes, follow your doctor’s instructions carefully. Always ask questions if you don’t understand something. Never stop taking your medication without talking to your doctor, nurse, or pharmacist.
Talk with Your Health Care Team
You and your health care team can work together to prevent or treat the medical conditions that lead to heart disease. Discuss your treatment plan regularly, and bring a list of questions to your appointments.
If you’ve already had a heart attack, your health care team will work with you to prevent another heart attack. Your treatment plan may include medications or surgery and lifestyle changes to reduce your risk. Be sure to take your medications as directed and follow your doctor’s instructions.
Signs of Heart Disease
Early heart disease often doesn’t have symptoms, or the symptoms may be barely noticeable. This is especially true in older adults. That’s why regular checkups with your doctor are important.
Contact your doctor right away if you feel any chest pain. However, as you get older, chest pain is a less common sign of heart disease, so be aware of other symptoms. Tell your doctor if you feel:
- Pain in the shoulders, arms, neck, jaw, or back
- Shortness of breath when active or at rest
- Chest pain during physical activity that gets better when you rest
- Lightheaded
- Dizzy
- Confusion
- Headaches
- Cold sweats
- Nausea/vomiting
- Easily tired or fatigued
- Swelling in the ankles, feet, legs, stomach, and/or neck
- Less able to exercise or be physically active
- Problems doing your normal activities
Problems with a rapid or irregular heartbeat are much more common in older adults than younger people and need to be treated. See a doctor if you feel a fluttering in your chest or have the feeling that your heart is skipping a beat or beating too hard, especially if you are weaker than usual, dizzy, or tired.
If you have any signs of heart disease, your doctor may send you to see a cardiologist, a doctor who specializes in the heart.
Other Conditions Related to Heart Disease
Coronary artery disease is the most common type of heart disease, but there are many other conditions that affect the heart.
Acute coronary syndrome is a term that includes heart attack and unstable angina.
Angina, a symptom of coronary artery disease, is chest pain or discomfort that occurs when the heart muscle is not getting enough blood. Angina may feel like pressure or a squeezing pain in the chest. The pain also may occur in the shoulders, arms, neck, jaw, or back. It may feel like indigestion.
There are two forms of angina—stable or unstable:
- Stable angina happens during physical activity or under mental or emotional stress.
- Unstable angina is chest pain that occurs even while at rest, without apparent reason. This type of angina is a medical emergency.
Aortic aneurysm and dissection are conditions that can affect the aorta, the major artery that carries blood from the heart to the body. An aneurysm is an enlargement in the aorta that can rupture or burst. A dissection is a tear in the aorta. Both of these conditions are medical emergencies. Learn more from the aortic aneurysm fact sheet.
Arrhythmias are irregular or unusually fast or slow heartbeats. Arrhythmias can be serious. One example is called ventricular fibrillation. This type of arrhythmia causes an abnormal heart rhythm that leads to death unless treated right away with an electrical shock to the heart (called defibrillation). Other arrhythmias are less severe but can develop into more serious conditions, such as atrial fibrillation, which can cause a stroke.
Atherosclerosis occurs when plaque builds up in the arteries that supply blood to the heart (called coronary arteries). Plaque is made up of cholesterol deposits. Plaque buildup causes arteries to narrow over time.
Atrial fibrillation is a type of arrhythmia that can cause rapid, irregular beating of the heart’s upper chambers. Blood may pool and clot inside the heart, increasing the risk for heart attack and stroke. For more information, see our atrial fibrillation fact sheet.
Cardiomyopathy occurs when the heart muscle becomes enlarged or stiff. This can lead to inadequate heart pumping (or weak heart pump) or other problems. Cardiomyopathy has many causes, including family history of the disease, prior heart attacks, uncontrolled high blood pressure, and viral or bacterial infections. For more information, see the cardiomyopathy fact sheet.
Congenital heart defects are problems with the heart that are present at birth. They are the most common type of major birth defect. Examples include abnormal heart valves or holes in the heart’s walls that divide the heart’s chambers. Congenital heart defects range from minor to severe. For more information, see What is congenital heart disease article.
Heart failure is often called congestive heart failure because of fluid buildup in the lungs, liver, gastrointestinal tract, and the arms and legs. Heart failure is a serious condition that occurs when the heart can’t pump enough blood to meet the body’s needs. It does not mean that the heart has stopped but that muscle is too weak to pump enough blood. The majority of heart failure cases are chronic, or long-term heart failures.
The only cure for heart failure is a heart transplant. However, heart failure can be managed with medications or medical procedures. Learn more from our heart failure fact sheet.
Peripheral arterial disease occurs when the arteries that supply blood to the arms and legs (the periphery) become narrow or stiff. Peripheral arterial disease usually results from atherosclerosis, the buildup of plaque and narrowing of the arteries. With this condition, blood flow and oxygen to the arm and leg muscles are low or even fully blocked. Signs and symptoms include leg pain, numbness, and swelling in the ankles and feet.
Rheumatic heart disease is damage to the heart valves caused by a bacterial (streptococcal) infection called rheumatic fever.
Sudden Cardiac Arrest
Sudden cardiac arrest is a condition in which the heart suddenly and unexpectedly stops beating. If this happens, blood stops flowing to the brain and other vital organs. Sudden cardiac arrest usually causes death if it’s not treated within minutes 16.
Most people who have sudden cardiac arrest die from it—often within minutes. Rapid treatment of sudden cardiac arrest with a defibrillator can be lifesaving. A defibrillator is a device that sends an electric shock to the heart to try to restore its normal rhythm.
Automated external defibrillators can be used by bystanders to save the lives of people who are having sudden cardiac arrest. These portable devices often are found in public places, such as shopping malls, golf courses, businesses, airports, airplanes, casinos, convention centers, hotels, sports venues, and schools.
Sudden cardiac arrest is not the same as a heart attack. A heart attack occurs if blood flow to part of the heart muscle is blocked. During a heart attack, the heart usually doesn’t suddenly stop beating. Sudden cardiac arrest, however, may happen after or during recovery from a heart attack.
People who have heart disease are at higher risk for sudden cardiac arrest. However, sudden cardiac arrest can happen in people who appear healthy and have no known heart disease or other risk factors for sudden cardiac arrest.
What Causes Sudden Cardiac Arrest ?
Ventricular fibrillation causes most sudden cardiac arrests. Ventricular fibrillation is a type of arrhythmia.
During ventricular fibrillation, the ventricles (the heart’s lower chambers) don’t beat normally. Instead, they quiver very rapidly and irregularly. When this happens, the heart pumps little or no blood to the body. Ventricular fibrillation is fatal if not treated within a few minutes.
Other problems with the heart’s electrical system also can cause sudden cardiac arrest. For example, sudden cardiac arrest can occur if the rate of the heart’s electrical signals becomes very slow and stops. Sudden cardiac arrest also can occur if the heart muscle doesn’t respond to the heart’s electrical signals.
Certain diseases and conditions can cause the electrical problems that lead to sudden cardiac arrest. Examples include coronary heart disease, also called coronary artery disease; severe physical stress; certain inherited disorders; and structural changes in the heart.
Several research studies are under way to try to find the exact causes of sudden cardiac arrest and how to prevent them.
Coronary Heart Disease
Coronary Heart Disease is a disease in which a waxy substance called plaque builds up in the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
Plaque narrows the arteries and reduces blood flow to your heart muscle. Eventually, an area of plaque can rupture (break open). This may cause a blood clot to form on the plaque’s surface.
A blood clot can partly or fully block the flow of oxygen-rich blood to the portion of heart muscle fed by the artery. This causes a heart attack.
During a heart attack, some heart muscle cells die and are replaced with scar tissue. The scar tissue damages the heart’s electrical system. As a result, electrical signals may spread abnormally throughout the heart. These changes to the heart increase the risk of dangerous arrhythmias and sudden cardiac arrest.
Coronary heart disease seems to cause most cases of sudden cardiac arrest in adults. Many of these adults, however, have no signs or symptoms of coronary heart disease before having sudden cardiac arrest.
Physical Stress
Certain types of physical stress can cause your heart’s electrical system to fail. Examples include:
- Intense physical activity. The hormone adrenaline is released during intense physical activity. This hormone can trigger sudden cardiac arrest in people who have heart problems.
- Very low blood levels of potassium or magnesium. These minerals play an important role in your heart’s electrical signaling.
- Major blood loss.
- Severe lack of oxygen.
Inherited Disorders
A tendency to have arrhythmias runs in some families. This tendency is inherited, which means it’s passed from parents to children through the genes. Members of these families may be at higher risk for sudden cardiac arrest.
An example of an inherited disorder that makes you more likely to have arrhythmias is long QT syndrome. Long QT syndrome is a disorder of the heart’s electrical activity. Problems with tiny pores on the surface of heart muscle cells cause the disorder. Long QT syndrome can cause sudden, uncontrollable, dangerous heart rhythms.
People who inherit structural heart problems also may be at higher risk for sudden cardiac arrest. These types of problems often are the cause of sudden cardiac arrest in children.
Structural Changes in the Heart
Changes in the heart’s normal size or structure may affect its electrical system. Examples of such changes include an enlarged heart due to high blood pressure or advanced heart disease. Heart infections also may cause structural changes in the heart.
Who is at Risk for Sudden Cardiac Arrest ?
The risk of sudden cardiac arrest increases 17:
- With age
- If you are a man. Men are more likely than women to have sudden cardiac arrest.
- Some studies show that blacks—particularly those with underlying conditions such as diabetes, high blood pressure, heart failure, and chronic kidney disease or certain cardiac findings on tests such as an electrocardiogram—have a higher risk for sudden cardiac arrest.
Major Risk Factor
The major risk factor for sudden cardiac arrest is coronary heart disease. Most people who have sudden cardiac arrest have some degree of coronary heart disease; however, many people may not know that they have coronary heart disease until sudden cardiac arrest occurs. Usually their coronary heart disease is “silent”—that is, it has no signs or symptoms. Because of this, doctors and nurses have not detected it.
Many people who have sudden cardiac arrest also have silent, or undiagnosed, heart attacks before sudden cardiac arrest happens. These people have no clear signs of heart attack, and they don’t even realize that they’ve had one. Read more about coronary heart disease risk factors.
Other Risk Factors
Other risk factors for sudden cardiac arrest include:
- A personal history of arrhythmias
- A personal or family history of sudden cardiac arrest or inherited disorders that make you prone to arrhythmias
- Drug or alcohol abuse
- Heart attack
- Heart failure
Signs and Symptoms of Sudden Cardiac Arrest
Usually, the first sign of sudden cardiac arrest is loss of consciousness (fainting). At the same time, no heartbeat (or pulse) can be felt 18.
Some people may have a racing heartbeat or feel dizzy or light-headed just before they faint. Within an hour before sudden cardiac arrest, some people have chest pain, shortness of breath, nausea (feeling sick to the stomach), or vomiting.
How is Sudden Cardiac Arrest Diagnosed ?
Sudden cardiac arrest happens without warning and requires emergency treatment 19. Doctors rarely diagnose sudden cardiac arrest with medical tests as it’s happening. Instead, sudden cardiac arrest often is diagnosed after it happens. Doctors do this by ruling out other causes of a person’s sudden collapse.
Specialists Involved
If you’re at high risk for sudden cardiac arrest, your doctor may refer you to a cardiologist. This is a doctor who specializes in diagnosing and treating heart diseases and conditions. Your cardiologist will work with you to decide whether you need treatment to prevent sudden cardiac arrest.
Some cardiologists specialize in problems with the heart’s electrical system. These specialists are called cardiac electrophysiologists.
Diagnostic Tests and Procedures
Doctors use several tests to help detect the factors that put people at risk for sudden cardiac arrest.
- EKG (Electrocardiogram)
An EKG is a simple, painless test that detects and records the heart’s electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
An EKG can show evidence of heart damage due to coronary heart disease. The test also can show signs of a previous or current heart attack.
- Echocardiography
Echocardiography, or echo, is a painless test that uses sound waves to create pictures of your heart. The test shows the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren’t contracting normally, and previous injury to the heart muscle caused by poor blood flow.
There are several types of echo, including stress echo. This test is done both before and after a cardiac stress test. During this test, you exercise (or are given medicine if you’re unable to exercise) to make your heart work hard and beat fast.
Stress echo shows whether you have decreased blood flow to your heart (a sign of coronary heart disease).
- MUGA Test or Cardiac MRI
A MUGA (multiple gated acquisition) test shows how well your heart is pumping blood. For this test, a small amount of radioactive substance is injected into a vein and travels to your heart.
The substance releases energy, which special cameras outside of your body can detect. The cameras use the energy to create pictures of many parts of your heart.
Cardiac MRI (magnetic resonance imaging) is a safe procedure that uses radio waves and magnets to create detailed pictures of your heart. The test creates still and moving pictures of your heart and major blood vessels.
Doctors use cardiac MRI to get pictures of the beating heart and to look at the structure and function of the heart.
- Cardiac Catheterization
Cardiac catheterization is a procedure used to diagnose and treat certain heart conditions. A long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart. Through the catheter, your doctor can do diagnostic tests and treatments on your heart.
Sometimes dye is put into the catheter. The dye will flow through your bloodstream to your heart. The dye makes your coronary (heart) arteries visible on x-ray pictures. The dye can show whether plaque has narrowed or blocked any of your coronary arteries.
- Electrophysiology Study
For an electrophysiology study, doctors use cardiac catheterization to record how your heart’s electrical system responds to certain medicines and electrical stimulation. This helps your doctor find where the heart’s electrical system is damaged.
- Blood Tests
Your doctor may recommend blood tests to check the levels of potassium, magnesium, and other chemicals in your blood. These chemicals play an important role in your heart’s electrical signaling.
How Is Sudden Cardiac Arrest Treated ?
Emergency Treatment
Sudden cardiac arrest is an emergency. A person having sudden cardiac arrest needs to be treated with a defibrillator right away 20. This device sends an electric shock to the heart. The electric shock can restore a normal rhythm to a heart that’s stopped beating.
To work well, defibrillation must be done within minutes of sudden cardiac arrest. With every minute that passes, the chances of surviving sudden cardiac arrest drop rapidly.
Police, emergency medical technicians, and other first responders usually are trained and equipped to use a defibrillator. Call your local emergency number right away if someone has signs or symptoms of sudden cardiac arrest. The sooner you call for help, the sooner lifesaving treatment can begin.
Automated External Defibrillators
Automated external defibrillators are special defibrillators that untrained bystanders can use. These portable devices often are found in public places, such as shopping malls, golf courses, businesses, airports, airplanes, casinos, convention centers, hotels, sports venues, and schools.
Automated external defibrillators are programmed to give an electric shock if they detect a dangerous arrhythmia, such as ventricular fibrillation. This prevents giving a shock to someone who may have fainted but isn’t having sudden cardiac arrest.
You should give cardiopulmonary resuscitation (CPR) to a person having sudden cardiac arrest until defibrillation can be done.
People who are at risk for sudden cardiac arrest may want to consider having an automated external defibrillator at home. A 2008 study by the National Heart, Lung, and Blood Institute and the National Institutes of Health found that automated external defibrillators in the home are safe and effective.
Some people feel that placing these devices in homes will save many lives because many sudden cardiac arrests occur at home. Others note that no evidence supports the idea that home-use automated external defibrillators save more lives. These people fear that people who have automated external defibrillators in their homes will delay calling for help during an emergency. They’re also concerned that people who have home-use automated external defibrillators will not properly maintain the devices or forget where they are.
When considering a home-use automated external defibrillator, talk with your doctor. He or she can help you decide whether having an automated external defibrillator in your home will benefit you.
Treatment in a Hospital
If you survive sudden cardiac arrest, you’ll likely be admitted to a hospital for ongoing care and treatment. In the hospital, your medical team will closely watch your heart. They may give you medicines to try to reduce the risk of another sudden cardiac arrest.
While in the hospital, your medical team will try to find out what caused your sudden cardiac arrest. If you’re diagnosed with coronary heart disease, you may have percutaneous coronary intervention, also known as coronary angioplasty, or coronary artery bypass grafting. These procedures help restore blood flow through narrowed or blocked coronary arteries.
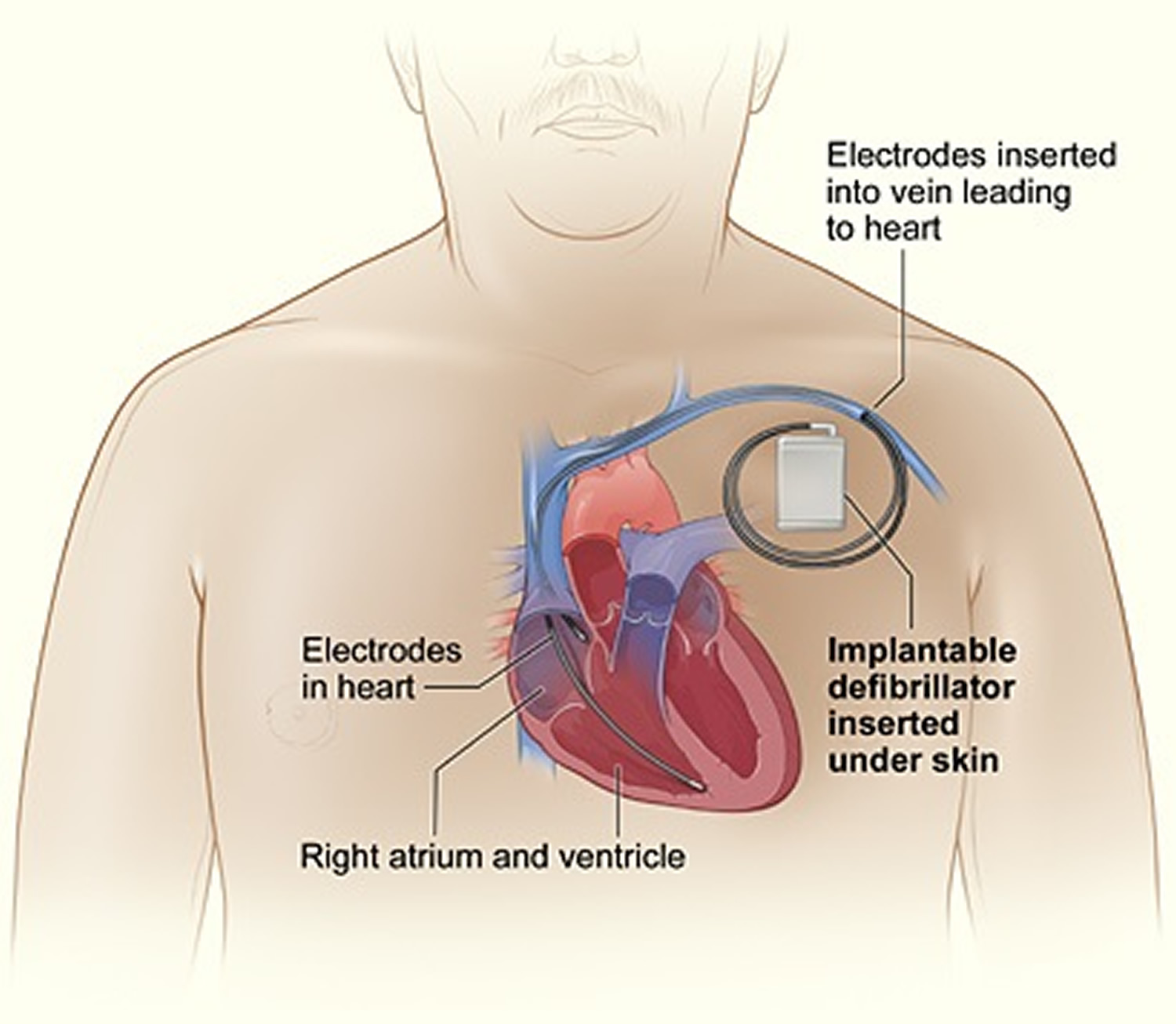
Often, people who have sudden cardiac arrest get a device called an implantable cardioverter defibrillator. This small device is surgically placed under the skin in your chest or abdomen. An implantable cardioverter defibrillator uses electric pulses or shocks to help control dangerous arrhythmias.
How Can Death Due to Sudden Cardiac Arrest Be Prevented ?
Ways to prevent death due to sudden cardiac arrest differ depending on whether 21:
- You’ve already had sudden cardiac arrest
- You’ve never had sudden cardiac arrest but are at high risk for the condition
- You’ve never had sudden cardiac arrest and have no known risk factors for the condition
For People Who Have Survived Sudden Cardiac Arrest
If you’ve already had sudden cardiac arrest, you’re at high risk of having it again. Research shows that an implantable cardioverter defibrillator reduces the chances of dying from a second sudden cardiac arrest. An implantable cardioverter defibrillator is surgically placed under the skin in your chest or abdomen. The device has wires with electrodes on the ends that connect to your heart’s chambers. The implantable cardioverter defibrillator monitors your heartbeat.
If the implantable cardioverter defibrillator detects a dangerous heart rhythm, it gives an electric shock to restore the heart’s normal rhythm. Your doctor may give you medicine to limit irregular heartbeats that can trigger the implantable cardioverter defibrillator.
Figure 1. Implantable cardioverter defibrillator
[Source 21]An implantable cardioverter defibrillator isn’t the same as a pacemaker. The devices are similar, but they have some differences. Pacemakers give off low-energy electrical pulses. They’re often used to treat less dangerous heart rhythms, such as those that occur in the upper chambers of the heart. Most new implantable cardioverter defibrillators work as both pacemakers and implantable cardioverter defibrillators.
For People at High Risk for a First Sudden Cardiac Arrest
If you have severe coronary heart disease, you’re at increased risk for sudden cardiac arrest. This is especially true if you’ve recently had a heart attack.
Your doctor may prescribe a type of medicine called a beta blocker to help lower your risk for sudden cardiac arrest. Your doctor also may discuss beginning statin treatment if you have an elevated risk for developing heart disease or having a stroke. Doctors usually prescribe statins for people who have:
- Diabetes
- Heart disease or had a prior stroke
- High LDL cholesterol levels
Your doctor also may prescribe other medications to:
- Decrease your chance of having a heart attack or dying suddenly.
- Lower blood pressure.
- Prevent blood clots, which can lead to heart attack or stroke.
- Prevent or delay the need for a procedure or surgery, such as angioplasty or coronary artery bypass grafting.
- Reduce your heart’s workload and relieve coronary heart disease symptoms.
Take all medicines regularly, as your doctor prescribes. Don’t change the amount of your medicine or skip a dose unless your doctor tells you to. You should still follow a heart-healthy lifestyle, even if you take medicines to treat your coronary heart disease.
Other treatments for coronary heart disease—such as percutaneous coronary intervention, also known as coronary angioplasty, or coronary artery bypass grafting—also may lower your risk for sudden cardiac arrest. Your doctor also may recommend an implantable cardioverter defibrillator if you’re at high risk for sudden cardiac arrest.
For People Who Have No Known Risk Factors for Sudden Cardiac Arrest
Coronary heart disease seems to be the cause of most sudden cardiac arrests in adults. Coronary heart disease also is a major risk factor for angina (chest pain or discomfort) and heart attack, and it contributes to other heart problems.
Following a heart-healthy lifestyle can help you lower your risk for coronary heart disease, sudden cardiac arrest, and other heart problems. A heart-healthy lifestyle includes:
- Heart-healthy eating
- Aiming for a healthy weight
- Managing stress
- Physical activity
- Quitting smoking.
Heart Disease in Men
- Heart disease is the leading cause of death for men in the United States, killing 321,000 men in 2013—that’s 1 in every 4 male deaths 22.
- Heart disease is the leading cause of death for men of most racial/ethnic groups in the United States, including African Americans, American Indians or Alaska Natives, Hispanics, and whites. For Asian American or Pacific Islander men, heart disease is second only to cancer 23.
- About 8.5% of all white men, 7.9% of black men, and 6.3% of Mexican American men have coronary heart disease 24.
- Half of the men who die suddenly of coronary heart disease have no previous symptoms 24. Even if you have no symptoms, you may still be at risk for heart disease.
- Between 70% and 89% of sudden cardiac events occur in men 24.
Risk Factors for Heart Disease in Men
High blood pressure, high LDL cholesterol, and smoking are key heart disease risk factors for heart disease. About half of Americans (49%) have at least one of these three risk factors 25.
Several other medical conditions and lifestyle choices can also put people at a higher risk for heart disease, including:
- Diabetes
- Overweight and obesity
- Poor diet
- Physical inactivity
- Excessive alcohol use
Heart Disease in Women
In the United States, 1 in 4 women dies from heart disease. In fact, coronary heart disease—the most common type of heart disease—is the #1 killer of both men and women in the United States 26.
Other types of heart disease, such as coronary microvascular disease and broken heart syndrome, also pose a risk for women 26. These disorders, which mainly affect women, are not as well understood as coronary heart disease. However, research is ongoing to learn more about coronary microvascular disease and broken heart syndrome.
- Heart disease is the leading cause of death for women in the United States, killing 289,758 women in 2013—that’s about 1 in every 4 female deaths 27.
- Although heart disease is sometimes thought of as a “man’s disease,” around the same number of women and men die each year of heart disease in the United States. Despite increases in awareness over the past decade, only 54% of women recognize that heart disease is their number 1 killer 28.
- Heart disease is the leading cause of death for African American and white women in the United States. Among Hispanic women, heart disease and cancer cause roughly the same number of deaths each year. For American Indian or Alaska Native and Asian or Pacific Islander women, heart disease is second only to cancer 23.
- About 5.8% of all white women, 7.6% of black women, and 5.6% of Mexican American women have coronary heart disease 24.
- Almost two-thirds (64%) of women who die suddenly of coronary heart disease have no previous symptoms 24. Even if you have no symptoms, you may still be at risk for heart disease.
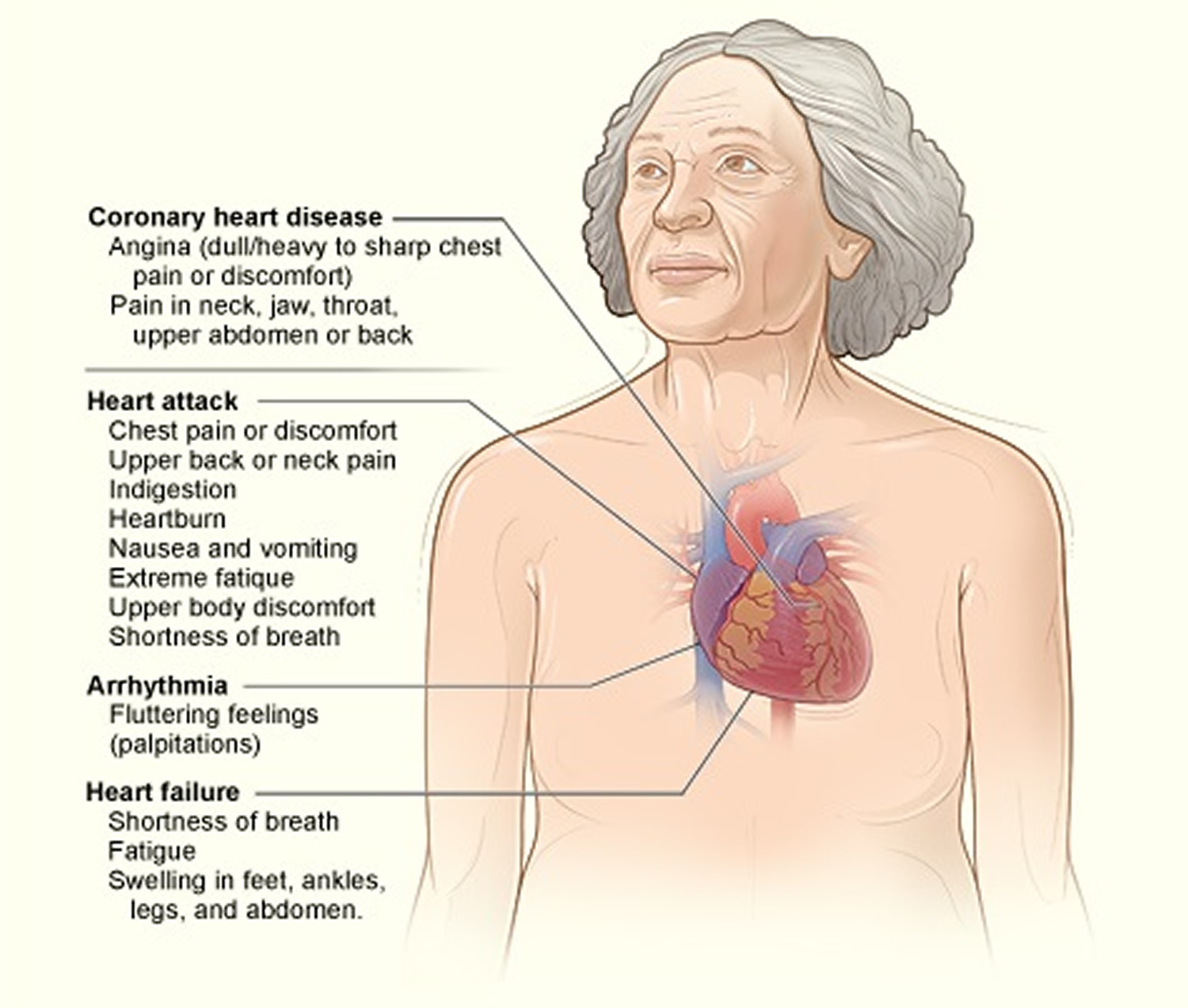
Symptoms of heart disease in women
The signs and symptoms of coronary heart disease may differ between women and men. Some women who have coronary heart disease have no signs or symptoms. This is called silent coronary heart disease 29.
Silent coronary heart disease may not be diagnosed until a woman has signs and symptoms of a heart attack, heart failure, or an arrhythmia (irregular heartbeat).
Other women who have coronary heart disease will have signs and symptoms of the disease – others experience angina (dull, heavy to sharp chest pain or discomfort), pain in the neck/jaw/throat or pain in the upper abdomen or back. These may occur during rest, begin during physical activity, or be triggered by mental stress 29.
In women who have coronary microvascular disease, angina often occurs during routine daily activities, such as shopping or cooking, rather than while exercising. Mental stress also is more likely to trigger angina pain in women than in men 29.
The severity of angina varies. The pain may get worse or occur more often as the buildup of plaque continues to narrow the coronary (heart) arteries.
Women are more likely to describe chest pain that is sharp, burning and more frequently have pain in the neck, jaw, throat, abdomen or back 29.
Sometimes heart disease may be silent and not diagnosed until a woman experiences signs or symptoms of a heart attack, heart failure, an arrhythmia, or stroke 29.
Figure 2. Heart Disease Signs and Symptoms in Women
[Source 29]These symptoms may include
- Heart Attack: Chest pain or discomfort, upper back pain, indigestion, heartburn, nausea/vomiting, extreme fatigue, upper body discomfort, and shortness of breath.
- Arrhythmia: Fluttering feelings in the chest (palpitations) 29.
- Heart Failure: Shortness of breath, fatigue, swelling of the feet/ankles/legs/abdomen.
- Stroke: Sudden weakness, paralysis (inability to move) or numbness of the face/arms/legs, especially on one side of the body.
- Other symptoms may include: confusion, trouble speaking or understanding speech, difficulty seeing in one or both eyes, shortness of breath, dizziness, loss of balance or coordination, loss of consciousness, or sudden and severe headache 30.
Who is at Risk for Heart Disease in Women
Certain traits, conditions, or habits may raise your risk for coronary heart disease. These conditions are known as risk factors. Risk factors also increase the chance that existing coronary heart disease will worsen.
Women generally have the same coronary heart disease risk factors as men. However, some risk factors may affect women differently than men. For example, diabetes raises the risk of coronary heart disease more in women. Also, some risk factors, such as birth control pills and menopause, only affect women 31.
There are many known coronary heart disease risk factors. Your risk for coronary heart disease and heart attack rises with the number of risk factors you have and their severity. Risk factors tend to “gang up” and worsen each other’s effects.
Having just one risk factor doubles your risk for coronary heart disease. Having two risk factors increases your risk for coronary heart disease fourfold. Having three or more risk factors increases your risk for coronary heart disease more than tenfold.
Also, some risk factors, such as smoking and diabetes, put you at greater risk for coronary heart disease and heart attack than others.
More than 75 percent of women aged 40 to 60 have one or more risk factors for coronary heart disease. Many risk factors start during childhood; some even develop within the first 10 years of life. You can control most risk factors, but some you can’t.
For more information about coronary heart disease risk factors, go to the What is coronary heart disease article. To find out whether you’re at risk for coronary heart disease, talk with your doctor or health care provider.
Risk Factors You Can Control
Smoking
Smoking is the most powerful risk factor that women can control. Smoking tobacco or long-term exposure to secondhand smoke raises your risk for coronary heart disease and heart attack.
Smoking exposes you to carbon monoxide. This chemical robs your blood of oxygen and triggers a buildup of plaque in your arteries.
Smoking also increases the risk of blood clots forming in your arteries. Blood clots can block plaque-narrowed arteries and cause a heart attack. The more you smoke, the greater your risk for a heart attack.
Even women who smoke fewer than two cigarettes a day are at increased risk for coronary heart disease.
High Blood Cholesterol and High Triglyceride Levels
Cholesterol travels in the bloodstream in small packages called lipoproteins The two major kinds of lipoproteins are low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol.
LDL cholesterol is sometimes called “bad” cholesterol. This is because it carries cholesterol to tissues, including your heart arteries. HDL cholesterol is sometimes called “good” cholesterol. This is because it helps remove cholesterol from your arteries.
A blood test called a lipoprotein panel is used to measure cholesterol levels. This test gives information about your total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides (a type of fat found in the blood).
Cholesterol levels are measured in milligrams (mg) of cholesterol per deciliter (dL) of blood. A woman’s risk for coronary heart disease increases if she has a total cholesterol level greater than 200 mg/dL, an LDL cholesterol level greater than 100 mg/dL, or an HDL cholesterol level less than 50 mg/dL.
A triglyceride level greater than 150 mg/dL also increases a woman’s risk for coronary heart disease. A woman’s HDL cholesterol and triglyceride levels predict her risk for CHD better than her total cholesterol or LDL cholesterol levels.
High Blood Pressure
Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps blood. If this pressure rises and stays high over time, it can damage the body in many ways.
Women who have blood pressure greater than 120/80 mmHg are at increased risk for coronary heart disease. The mmHg is millimeters of mercury—the units used to measure blood pressure.
High blood pressure is defined differently for people who have diabetes or chronic kidney disease. If you have one of these diseases, work with your doctor to set a healthy blood pressure goal.
Diabetes and Prediabetes
Diabetes is a disease in which the body’s blood sugar level is too high. This is because the body doesn’t make enough insulin or doesn’t use its insulin properly.
Insulin is a hormone that helps move blood sugar into cells, where it’s used for energy. Over time, a high blood sugar level can lead to increased plaque buildup in your arteries.
Prediabetes is a condition in which your blood sugar level is higher than normal, but not as high as it is in diabetes. Prediabetes puts you at higher risk for both diabetes and coronary heart disease.
Diabetes and prediabetes raise the risk of coronary heart disease more in women than in men. In fact, having diabetes doubles a woman’s risk of developing coronary heart disease.
Before menopause, estrogen provides women some protection against coronary heart disease. However, in women who have diabetes, the disease counters the protective effects of estrogen.
Overweight and Obesity
The terms “overweight” and “obesity” refer to body weight that’s greater than what is considered healthy for a certain height.
The most useful measure of overweight and obesity is body mass index (BMI). BMI is calculated from your height and weight. In adults, a BMI of 18.5 to 24.9 is considered normal. A BMI of 25 to 29.9 is considered overweight. A BMI of 30 or more is considered obese.
You can calculate your BMI by dividing your weight in kilograms by your height in meters squared (kg/m2). You can also use an online BMI calculator or BMI table.
To find out about your body mass index (BMI), you can use a FREE online BMI calculators from the Centers for Disease Control and Prevention (CDC) :
- Adults 9
For children and adolescents (younger than 20 years of age), overweight and obesity are based on the Centers for Disease Control and Prevention’s (CDC’s) BMI-for-age growth charts, which are available at 10.
The CDC has a BMI percentile calculator for children and teens at 11.
- Children 12
Body Mass Index for Men and Women Adults
The body mass index is an attempt to quantify the amount of tissue mass (muscle, fat, and bone) in an individual, and then categorize that person as underweight, normal weight, overweight, or obese based on that value. Commonly accepted body mass index ranges are:
A) Underweight: under 18.5 kg/m2,
B) Normal (Healthy BMI) weight: 18.5 to 25 kg/m2,
C) Overweight: 25 to 30 kg/m2,
D) Obese: over 30 to 39.9 kg/m2.
E) Severely Obese: over 40 kg/m2.
Waist size matters, too. In people who are not overweight, waist size may be an even more telling warning sign of increased health risks than BMI 13. An expert panel convened by the National Institutes of Health identified these useful benchmarks: Men should aim for a waist size below 40 inches (102 cm) and women should aim for a waist size below 35 inches (88 cm) 14.
Studies suggest that where extra weight occurs on the body may predict coronary heart disease risk better than BMI. Women who carry much of their fat around the waist are at greatest risk for coronary heart disease. These women have “apple-shaped” figures.
Women who carry most of their fat on their hips and thighs—that is, those who have “pear-shaped” figures—are at lower risk for coronary heart disease.
To fully know how excess weight affects your coronary heart disease risk, you should know your BMI and waist measurement. If you have a BMI greater than 24.9 and a waist measurement greater than 35 inches, you’re at increased risk for coronary heart disease.
If your waist measurement divided by your hip measurement is greater than 0.9, you’re also at increased risk for coronary heart disease.
Studies also suggest that women whose weight goes up and down dramatically (typically due to unhealthy dieting) are at increased risk for coronary heart disease. These swings in weight can lower HDL cholesterol levels.
Metabolic Syndrome
Metabolic syndrome is the name for a group of risk factors that raises your risk for coronary heart disease and other health problems, such as diabetes and stroke. A diagnosis of metabolic syndrome is made if you have at least three of the following risk factors:
- A large waistline. Having extra fat in the waist area is a greater risk factor for coronary heart disease than having extra fat in other parts of the body, such as on the hips.
- A higher than normal triglyceride level (or you’re on medicine to treat high triglycerides).
- A lower than normal HDL cholesterol level (or you’re on medicine to treat low HDL cholesterol).
- Higher than normal blood pressure (or you’re on medicine to treat high blood pressure).
- Higher than normal fasting blood sugar (or you’re on medicine to treat diabetes)
Metabolic syndrome is more common in African American women and Mexican American women than in men of the same racial groups. The condition affects White women and men about equally.
Birth Control Pills
Women who smoke and take birth control pills are at very high risk for coronary heart disease, especially if they’re older than 35. For women who take birth control pills but don’t smoke, the risk of coronary heart disease isn’t fully known.
Lack of Physical Activity
Inactive people are nearly twice as likely to develop coronary heart disease as those who are physically active. A lack of physical activity can worsen other coronary heart disease risk factors, such as high blood cholesterol and triglyceride levels, high blood pressure, diabetes and prediabetes, and overweight and obesity.
Unhealthy Diet
An unhealthy diet can raise your risk for coronary heart disease. For example, foods that are high in saturated and trans fats and cholesterol raise your LDL cholesterol level. A high-sodium (salt) diet can raise your risk for high blood pressure.
Foods with added sugars will give you extra calories without nutrients, such as vitamins and minerals. This can cause you to gain weight, which raises your risk for coronary heart disease.
Too much alcohol also can cause you to gain weight, and it will raise your blood pressure.
Stress or Depression
Stress may play a role in causing coronary heart disease. Stress can trigger your arteries to narrow. This can raise your blood pressure and your risk for a heart attack.
Getting upset or angry also can trigger a heart attack. Stress also may indirectly raise your risk for coronary heart disease if it makes you more likely to smoke or overeat foods high in fat and sugar.
People who are depressed are two to three times more likely to develop coronary heart disease than people who are not. Depression is twice as common in women as in men.
Anemia
Anemia is a condition in which your blood has a lower than normal number of red blood cells.
The condition also can occur if your red blood cells don’t contain enough hemoglobin. Hemoglobin is an iron-rich protein that carries oxygen from your lungs to the rest of your organs.
If you have anemia, your organs don’t get enough oxygen-rich blood. This causes your heart to work harder, which may raise your risk for coronary heart disease.
Sleep Apnea
Sleep apnea is a common disorder that causes pauses in breathing or shallow breaths while you sleep. Breathing pauses can last from a few seconds to minutes. They often occur 5 to 30 times or more an hour.
Typically, normal breathing starts again after the pause, sometimes with a loud snort or choking sound. Major signs of sleep apnea are snoring and daytime sleepiness.
When you stop breathing, the lack of oxygen triggers your body’s stress hormones. This causes blood pressure to rise and makes the blood more likely to clot.
Untreated sleep apnea can raise your risk for high blood pressure, diabetes, and even a heart attack or stroke.
Women are more likely to develop sleep apnea after menopause.
Risk Factors You Can’t Control
Age and Menopause
As you get older, your risk for coronary heart disease and heart attack rises. This is due in part to the slow buildup of plaque inside your heart arteries, which can start during childhood.
Before age 55, women have a lower risk for coronary heart disease than men. Estrogen provides women with some protection against coronary heart disease before menopause. After age 55, however, the risk of coronary heart disease increases in both women and men.
You may have gone through early menopause, either naturally or because you had your ovaries removed. If so, you’re twice as likely to develop coronary heart disease as women of the same age who aren’t yet menopausal.
Another reason why women are at increased risk for coronary heart disease after age 55 is that middle age is when you tend to develop other coronary heart disease risk factors.
Women who have gone through menopause also are at increased risk for broken heart syndrome.
Family History
Family history plays a role in coronary heart disease risk. Your risk increases if your father or a brother was diagnosed with coronary heart disease before 55 years of age, or if your mother or a sister was diagnosed with coronary heart disease before 65 years of age.
Also, a family history of stroke—especially a mother’s stroke history—can help predict the risk of heart attack in women.
Having a family history of coronary heart disease or stroke doesn’t mean that you’ll develop heart disease. This is especially true if your affected family member smoked or had other risk factors that were not well treated.
Making lifestyle changes and taking medicines to treat risk factors often can lessen genetic influences and prevent or delay heart problems.
Preeclampsia
Preeclampsia is a condition that develops during pregnancy. The two main signs of preeclampsia are a rise in blood pressure and excess protein in the urine.
These signs usually occur during the second half of pregnancy and go away after delivery. However, your risk of developing high blood pressure later in life increases after having preeclampsia.
Preeclampsia also is linked to an increased lifetime risk of heart disease, including coronary heart disease, heart attack, and heart failure. Likewise, having heart disease risk factors, such as diabetes or obesity, increases your risk for preeclampsia.
If you had preeclampsia during pregnancy, you’re twice as likely to develop heart disease as women who haven’t had the condition. You’re also more likely to develop heart disease earlier in life.
Preeclampsia is a heart disease risk factor that you can’t control. However, if you’ve had the condition, you should take extra care to try and control other heart disease risk factors.
The more severe your preeclampsia was, the greater your risk for heart disease. Let your doctor know that you had preeclampsia so he or she can assess your heart disease risk and how to reduce it.
Emerging Risk Factors
Research suggests that inflammation plays a role in causing coronary heart disease. Inflammation is the body’s response to injury or infection. Damage to the arteries’ inner walls seems to trigger inflammation and help plaque grow.
High blood levels of a protein called C-reactive protein (CRP) are a sign of inflammation in the body. Research suggests that women who have high blood levels of CRP are at increased risk for heart attack.
Also, some inflammatory diseases, such as lupus and rheumatoid arthritis, may increase the risk for coronary heart disease.
Some studies suggest that women who have migraine headaches may be at greater risk for coronary heart disease. This is especially true for women who have migraines with auras (visual disturbances), such as flashes of light or zig-zag lines.
Low bone density and low intake of folate and vitamin B6 also may raise a woman’s risk for coronary heart disease.
More research is needed to find out whether calcium supplements with or without vitamin D affect coronary heart disease risk. You may want to talk with your doctor to find out whether these types of supplements are right for you.
Researchers are just starting to learn about broken heart syndrome risk factors. Most women who have this disorder are White and have gone through menopause.
Many of these women have other heart disease risk factors, such as high blood pressure, high blood cholesterol, diabetes, and smoking. However, these risk factors tend to be less common in women who have broken heart syndrome than in women who have coronary heart disease.
Risk Factors of heart disease in women
High blood pressure, high LDL cholesterol, and smoking are key risk factors for heart disease. About half of Americans (49%) have at least one of these three risk factors 32.
Several other medical conditions and lifestyle choices can also put people at a higher risk for heart disease, including:
- Smoking, including secondhand smoke
- Diabetes
- Overweight and obesity
- Poor diet
- Physical inactivity
- Excessive alcohol use
Screening of heart disease in women 33
To reduce your chances of getting heart disease it’s important to:
- Know your blood pressure. Having uncontrolled blood pressure can result in heart disease. High blood pressure has no symptoms so it’s important to have your blood pressure checked regularly.
- Talk to your healthcare provider about whether you should be tested for diabetes. Having uncontrolled diabetes raises your chances of heart disease.
- Quit smoking.
- Discuss checking your cholesterol and triglycerides with your healthcare provider.
- Make healthy food choices. Being overweight and obese raises your risk of heart disease.
- Limit alcohol intake to one drink a day.
- Lower your stress level and find healthy ways to cope with stress.
Coronary Heart Disease
Coronary heart disease is a common term for the buildup of plaque in the heart’s arteries that could lead to heart attack 34. But what about coronary artery disease ? Is there a difference ? The answer is often no — health professionals frequently use the terms interchangeably. Coronary heart disease is actually a result of coronary artery disease.
Other names for Coronary Heart Disease 35
- Atherosclerosis
- Coronary artery disease
- Hardening of the arteries
- Heart disease
- Ischemic heart disease
- Narrowing of the arteries
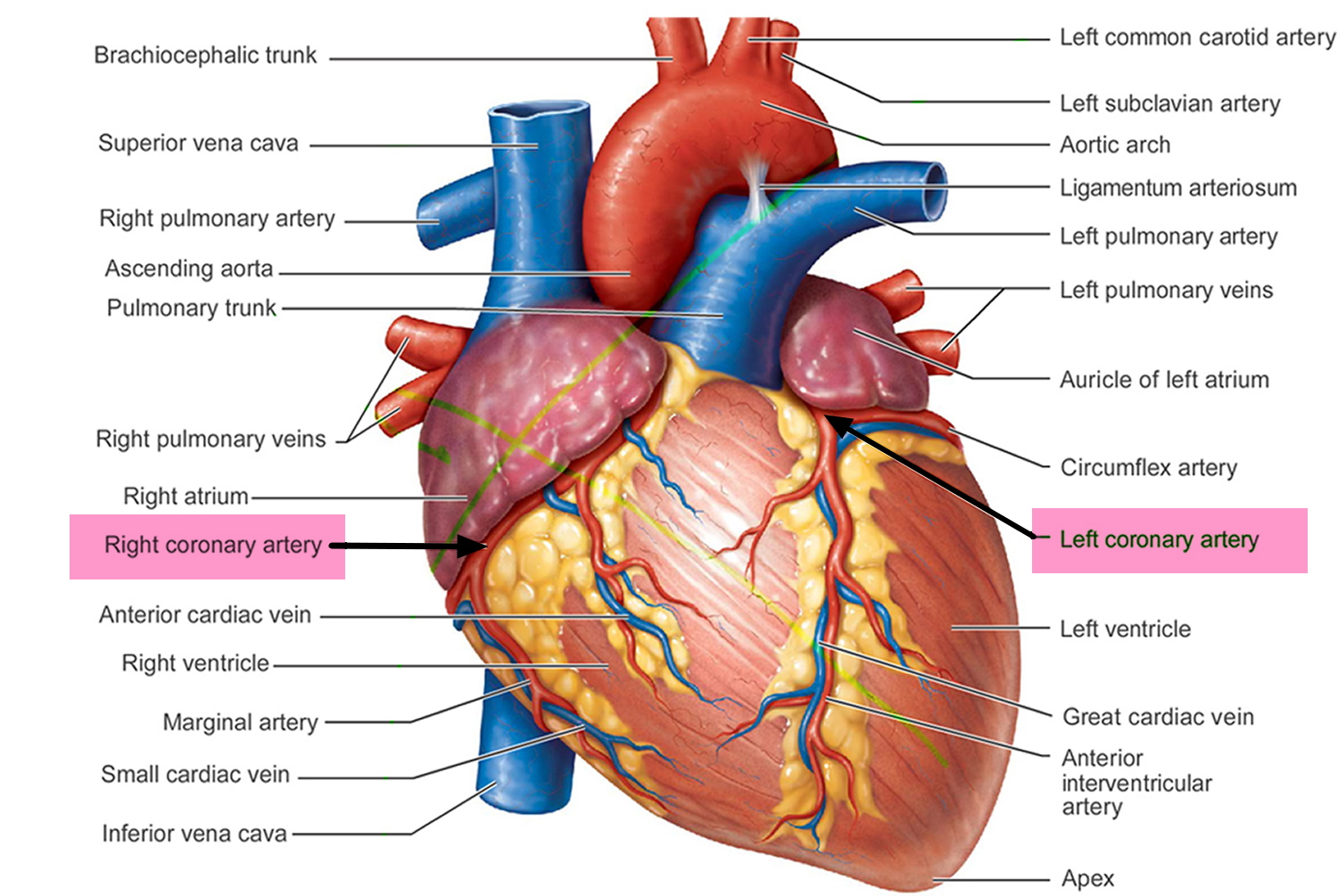
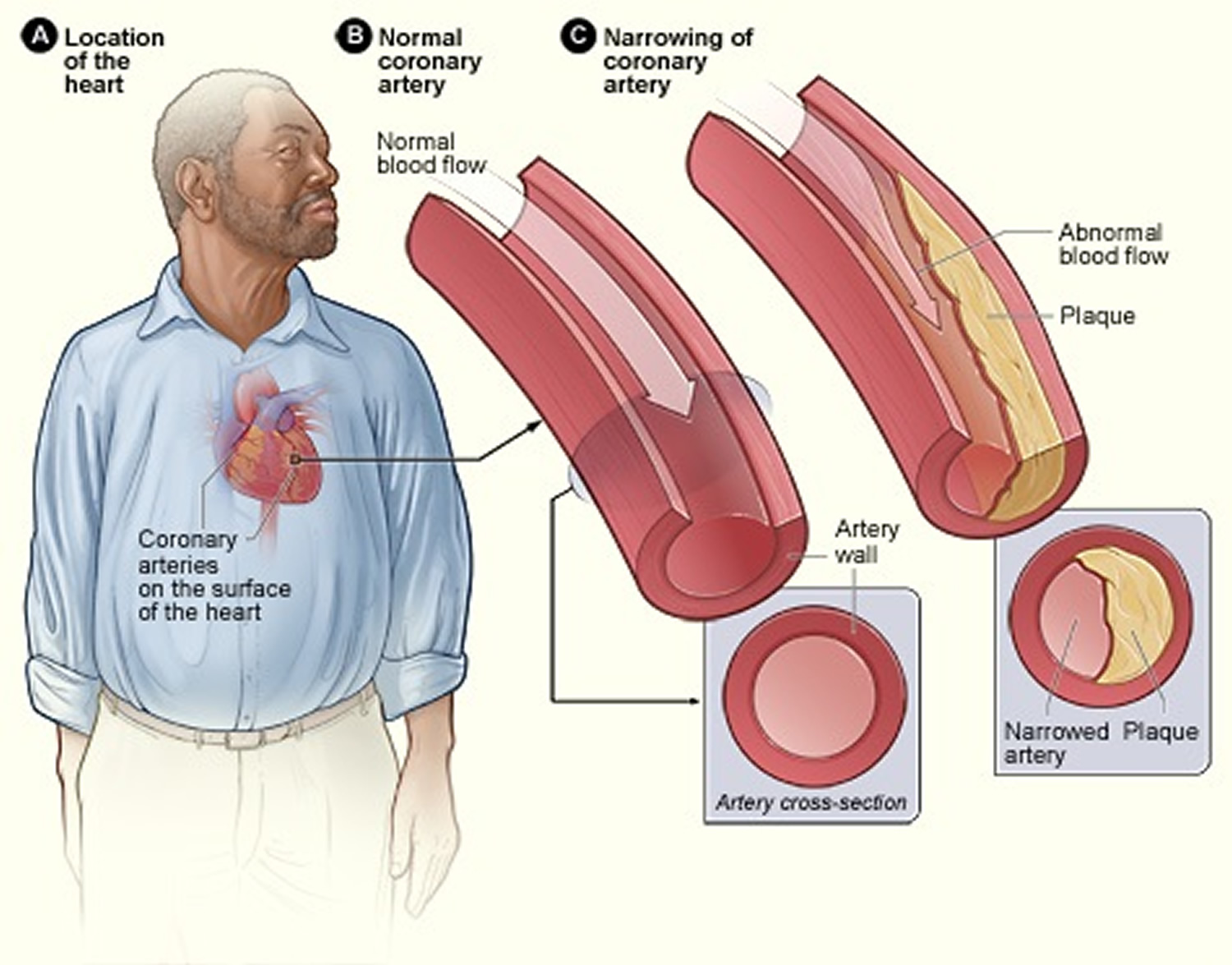
Coronary artery disease develops when the major blood vessels (coronary arteries) that supply your heart with blood, oxygen and nutrients become damaged or diseased. The coronary arteries supply oxygen-rich blood to your heart muscle.
Figure 3. Coronary Arteries supplying blood, oxygen & nutrients to your heart
Coronary heart disease or coronary artery disease is a condition in which a waxy substance called plaque builds up inside of the coronary arteries 36.
Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque hardens and narrows your arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body.
When plaque builds up in the arteries, the condition is called atherosclerosis. Atherosclerosis can lead to serious problems, including heart attack, stroke, or even death.
Atherosclerosis is a disease in which plaque builds up inside your arteries. The buildup of plaque occurs over many years.
Atherosclerosis plaque narrows the coronary arteries and reduces blood flow to your heart muscle. Plaque narrows and stiffens the coronary arteries. This reduces the flow of oxygen-rich blood to the heart muscle, causing chest pain.
Plaque buildup also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow, which can cause a heart attack.
- If blood flow to your heart muscle is reduced or blocked, you may have angina (chest pain or discomfort) or a heart attack.
Plaque also can form in the heart’s smallest arteries. This disease is called coronary microvascular disease. In coronary microvascular disease, plaque doesn’t cause blockages in the arteries as it does in coronary heart disease.
Coronary artery disease can lead to:
- Chest pain (angina). When your coronary arteries narrow, your heart may not receive enough blood when demand is greatest — particularly during physical activity. This can cause chest pain (angina) or shortness of breath.
- Heart attack. If a cholesterol plaque ruptures and a blood clot forms, complete blockage of your heart artery may trigger a heart attack. The lack of blood flow to your heart may damage your heart muscle. The amount of damage depends in part on how quickly you receive treatment.
- Heart failure. If some areas of your heart are chronically deprived of oxygen and nutrients because of reduced blood flow, or if your heart has been damaged by a heart attack, your heart may become too weak to pump enough blood to meet your body’s needs. This condition is known as heart failure.
- Abnormal heart rhythm (arrhythmia). Inadequate blood supply to the heart or damage to heart tissue can interfere with your heart’s electrical impulses, causing abnormal heart rhythms.
Figure 4. Atherosclerosis plaque
[Source 37]Figure 5. Atherosclerosis blocking the coronary artery in your heart
[Source 37]Figure 6. Heart With Muscle Damage and a Blocked Left Coronary Artery
[Source 38]When plaque builds up in the arteries, the condition is called atherosclerosis. Because coronary artery disease often develops over decades, you might not notice a problem until you have a significant blockage or a heart attack.
Eventually, an area of plaque can rupture (break open) inside of an artery. This causes a blood clot to form on the plaque’s surface. If the clot becomes large enough, it can mostly or completely block blood flow through a coronary artery.
If the blockage isn’t treated quickly, the portion of heart muscle fed by the artery begins to die. Healthy heart tissue is replaced with scar tissue. This heart damage may not be obvious, or it may cause severe or long-lasting problems.
A heart attack happens if the flow of oxygen-rich blood to a section of heart muscle suddenly becomes blocked and the heart can’t get oxygen. Most heart attacks occur as a result of coronary heart disease 36.
Over time, coronary heart disease can weaken the heart muscle and lead to heart failure and heart arrhythmias. Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Heart arrhythmias are problems with the rate or rhythm of the heartbeat.
Coronary artery disease begins in childhood, so that by the teenage years, there is evidence that plaques that will stay with us for life are formed in most people 34. But there’s plenty you can do to prevent and treat coronary artery disease. A healthy lifestyle can make a big impact. The traditional risk factors for coronary artery disease are high LDL cholesterol, low HDL cholesterol, high blood pressure, family history, diabetes, smoking, being post-menopausal for women and being older than 45 for men. Obesity may also be a risk factor.
Women tend to have coronary heart disease about 10 years later than men. However, coronary heart disease remains the #1 killer of women in the United States.
The good news is that you can control many coronary heart disease risk factors. Coronary heart disease risk factors are conditions or habits that raise your risk for coronary heart disease and heart attack. These risk factors also can increase the chance that existing coronary heart disease will worsen.
Lifestyle changes, medicines, and medical or surgical procedures can help women lower their risk for coronary heart disease. Thus, early and ongoing coronary heart disease prevention is important.
Signs and Symptoms Coronary Heart Disease Complications
Heart Attack
The most common heart attack symptom in men and women is chest pain or discomfort. However, only half of women who have heart attacks have chest pain.
Women are more likely than men to report back or neck pain, indigestion, heartburn, nausea (feeling sick to the stomach), vomiting, extreme fatigue (tiredness), or problems breathing.
Heart attacks also can cause upper body discomfort in one or both arms, the back, neck, jaw, or upper part of the stomach. Other heart attack symptoms are light-headedness and dizziness, which occur more often in women than men.
Men are more likely than women to break out in a cold sweat and to report pain in the left arm during a heart attack.
Heart Failure
Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Heart failure doesn’t mean that your heart has stopped or is about to stop working. It means that your heart can’t cope with the demands of everyday activities.
Heart failure causes shortness of breath and fatigue that tends to increase with physical exertion. Heart failure also can cause swelling in the feet, ankles, legs, abdomen, and veins in the neck.
Heart Arrhythmia
An arrhythmia is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
Some people describe arrhythmias as fluttering or thumping feelings or skipped beats in their chests. These feelings are called palpitations.
Some arrhythmias can cause your heart to suddenly stop beating. This condition is called sudden cardiac arrest (SCA). SCA causes loss of consciousness and death if it’s not treated right away.
Broken Heart Syndrome
Women are also more likely than men to have a condition called broken heart syndrome. In this recently recognized heart problem, extreme emotional stress can lead to severe (but often short-term) heart muscle failure 26.
Broken heart syndrome is also called stress-induced cardiomyopathy or takotsubo cardiomyopathy 26 is characterized by severe but potentially reversible regional left ventricular wall motion abnormalities, ie, akinesia, in the absence of explanatory angiographic evidence of a coronary occlusion..
Doctors may misdiagnose broken heart syndrome as a heart attack because it has similar symptoms and test results. However, there’s no evidence of blocked heart arteries in broken heart syndrome, and most people have a full and quick recovery.
Researchers are just starting to explore what causes this disorder and how to diagnose and treat it. Often, patients who have broken heart syndrome have previously been healthy.
Signs and Symptoms of Broken Heart Syndrome
Women are also more likely than men to have a condition called broken heart syndrome. In this recently recognized heart problem, extreme emotional stress can lead to severe (but often short-term) heart muscle failure 26.
Broken heart syndrome is also called stress-induced cardiomyopathy or Takotsubo cardiomyopathy is characterized by severe but potentially reversible regional left ventricular wall motion abnormalities, i.e, akinesia, in the absence of explanatory angiographic evidence of a coronary occlusion 39.
Stress-induced cardiomyopathy or broken heart syndrome, ampulla cardiomyopathy, and apical ballooning syndrome, was first recognized in Japan almost twenty years ago. Since then, more than 1500 reports on the subject have been published, and an increasing amount of articles are published each year 40.
Approximately 90% of reported stress-induced cardiomyopathy patients were women 41. As the name of this syndrome implies, a preceding somatic and/or emotional stressor can be identified in a majority of the patients.
Table 1. Preceding somatic or emotional stressors in the development of broken heart syndrome
| Somatic stressors | Emotional stressors |
|---|---|
| Vigorous exercise | Grief (eg, death or illness of a loved one) |
| Pheochromocytoma | Receiving bad news (eg, being diagnosed with major illness, learning of a daughter’s divorce) |
| Subarachnoid hemorrhage | Fear |
| Seizure | Relationship conflicts |
| Postoperative pain | Public speaking |
| Hyperthyroidism | Financial problems |
| Alcohol/opiate withdrawal | Being bullied |
| Invasive medical procedures | Surprise party |
| Exacerbation of underlying noncardiac disease | Changing residence |
| Involvement in accident | |
| Sexual intercourse | |
| Administration of sympathomimetics |
The typical pattern is that of an akinetic apex with preserved contractions in the base, but other variants are also common, including basal or midmyocardial akinesia with preserved apical function 42. Stress-induced cardiomyopathy is associated with electrocardiogram (EKG) changes indicative of ischemia and elevated plasma levels of cardiac proteins. Although several attempts have been made to distinguish between stress-induced cardiomyopathy and acute myocardial infarction, based on noninvasive diagnostic criteria, as of yet, these two conditions can only reliably be distinguished by invasive procedures, i.e, absence of explanatory coronary lesions on the angiogram 43, 44. The etiology, epidemiology, and pathophysiology of stress-induced cardiomyopathy remain largely unknown, but catecholamines are believed to play a pivotal role 39. Among the evidence suggesting an important role of catecholamines in the pathophysiology of stress-induced cardiomyopathy is the observation that plasma catecholamine levels are severely elevated in these patients, and stress-induced cardiomyopathy is common in patients with pheochromocytoma 45, 46. In addition, iatrogenically administered beta-adrenoceptor agonists have been documented to trigger episodes 47. Last but not least, others have provoked stress-induced cardiomyopathy-like cardiac dysfunction in rats by exogenous administration of catecholamines 48, 49.
The short- and long-term prognoses of stress-induced cardiomyopathy patients were initially believed to be excellent, but recent reports indicate that stress-induced cardiomyopathy may be associated with significant mortality 50, 51, 52, 53. Data from Sahlgrenska University Hospital indicate a significant mortality in patients with stress-induced cardiomyopathy 53.
Figure 7. Connection between stress-induced cardiomyopathy and neuropsychiatry
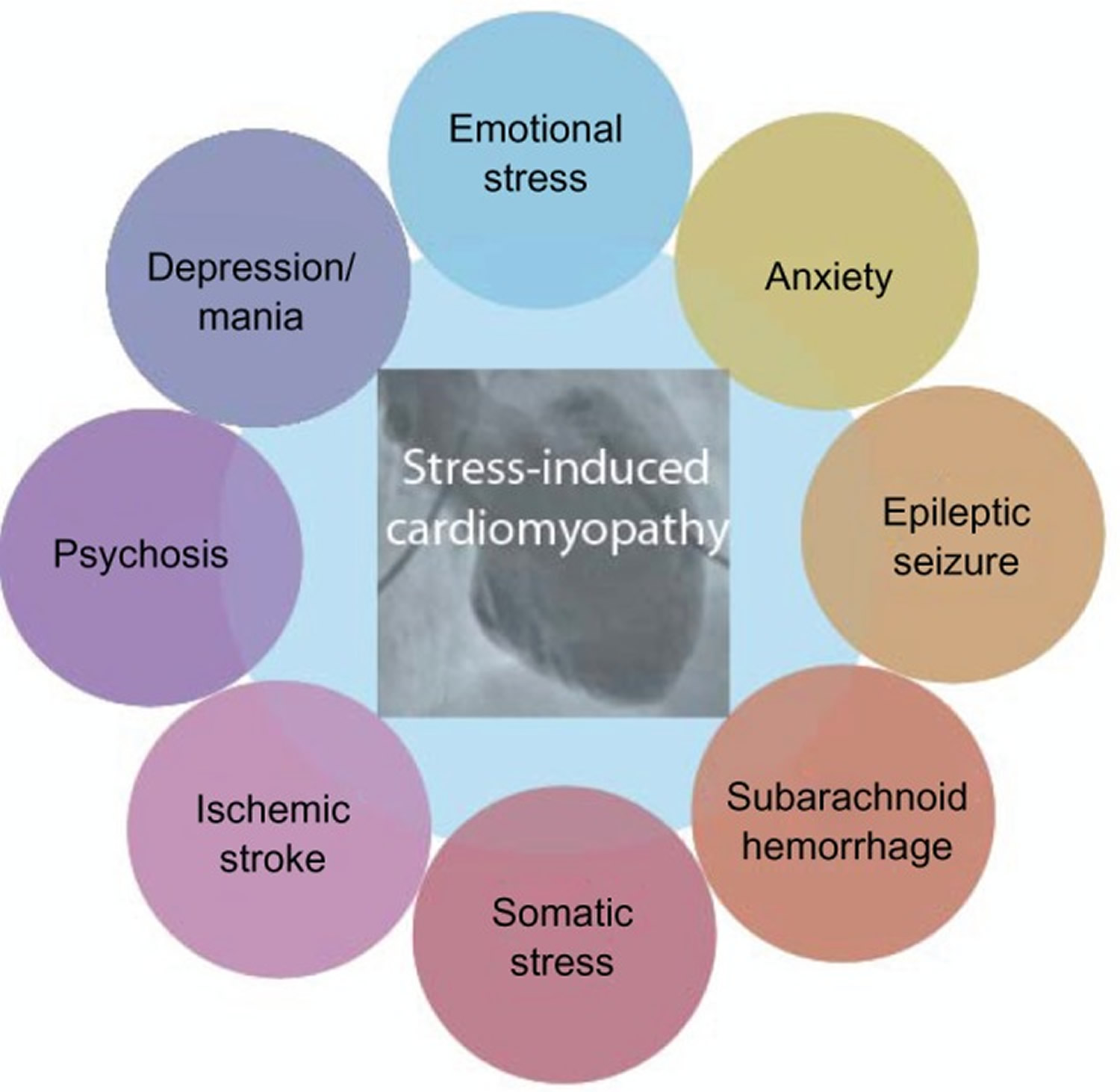
Note: A somatic and/or emotional stressor can be identified in most stress-induced cardiomyopathy patients. Although these stressors are often categorized as either emotional or somatic, they could also be viewed as elements of a continuous spectrum of stressors able to induce stress-induced cardiomyopathy.
The fact that acute severe emotional stress can trigger stress-induced cardiomyopathy has been known since the syndrome was first described, and this observation led to the coining of the terms “stress-induced cardiomyopathy” and “broken heart syndrome.” Two recent extensive overviews of American stress-induced cardiomyopathy cohorts found that anxiety and chronic stress were both associated with significantly higher odds of developing stress-induced cardiomyopathy 54, 55. Also, depression was associated with near-significantly increased odds of developing stress-induced cardiomyopathy 54. This is consistent with a previous report that found an increased prevalence of premorbid psychiatric diagnoses, particularly anxiety disorders, in stress-induced cardiomyopathy patients 56. These findings are intriguing, as they imply that chronic stress and impaired well-being may predispose an individual to develop stress-induced cardiomyopathy. If this is indeed the case, it adds to the evidence that stress-induced cardiomyopathy spans the domains of psychiatric as well as somatic medicine, highlighting the inherent link between the two. One survey found that almost 16% of postmenopausal women reported significant depressive symptoms and that depressive symptoms were associated with cardiovascular events 57. Again, this is the typical stress-induced cardiomyopathy patient category. Indeed, chronic stress and depression have both been shown to cause structural changes to the cerebrum, including decreased volume of the hippocampus and loss of grey matter in the prefrontal and cingulate cortices. Furthermore, these structural changes have been linked to alterations in the hypothalamic-pituitary-adrenal axis response to stress 58. Researchers believe that stress-induced cardiomyopathy may occur acutely in biologically predisposed individuals in response to an acute stressor and that this biological predisposition may, in turn, be caused by chronic stress or impaired well-being.
Psychiatric conditions may not only predispose an individual to develop stress-induced cardiomyopathy in response to a strong emotional and/or somatic stressor, there have been published reports describing exacerbations of psychiatric illnesses that have, in themselves, acutely triggered stress-induced cardiomyopathy 59.
It is propose that stress-induced cardiomyopathy be viewed as a cardiocirculatory syndrome that is intimately linked to other organs, perhaps most importantly the brain. Because stress-induced cardiomyopathy is a potential complication of, among others, neurological and psychiatric conditions, researchers believe that increased awareness of the syndrome is desirable, not only among cardiologists but also among other specialists. Although the treatment of stress-induced cardiomyopathy is the task of the cardiologist, successful prevention, and to some extent, early detection, may sometimes lie in the hands of other physicians.
The most common signs and symptoms of broken heart syndrome are chest pain and shortness of breath. In this disorder, these symptoms tend to occur suddenly in people who have no history of heart disease.
Arrhythmias or cardiogenic shock also may occur. Cardiogenic shock is a condition in which a suddenly weakened heart isn’t able to pump enough blood to meet the body’s needs.
Some of the signs and symptoms of broken heart syndrome differ from those of heart attack. For example, in people who have broken heart syndrome:
- Symptoms occur suddenly after having extreme emotional or physical stress.
- EKG (electrocardiogram) results don’t look the same as the EKG results for a person having a heart attack. (An EKG is a test that records the heart’s electrical activity.)
- Blood tests show no signs or mild signs of heart damage.
- Tests show no signs of blockages in the coronary arteries.
- Tests show ballooning and unusual movement of the lower left heart chamber (left ventricle).
- Recovery time is quick, usually within days or weeks (compared with the recovery time of a month or more for a heart attack).
Coronary Microvascular Disease
Coronary Microvascular Disease is heart disease that affects the heart’s tiny arteries. This disease is also called cardiac syndrome X or nonobstructive coronary heart disease. In coronary microvascular disease, the walls of the heart’s tiny arteries are damaged or diseased 26.
Figure 8. Coronary Microvascular Disease
[Source 26]Note: Figure A shows the small coronary artery network (microvasculature), containing a normal artery and an artery with coronary microvascular disease. Figure B shows a large coronary artery with plaque buildup.
Women are more likely than men to have coronary microvascular disease. Many researchers think that a drop in estrogen levels during menopause combined with other heart disease risk factors causes coronary microvascular disease.
Although death rates from heart disease have dropped in the last 30 years, they haven’t dropped as much in women as in men. This may be the result of coronary microvascular disease.
Standard tests for coronary heart disease are not designed to detect coronary microvascular disease. Thus, test results for women who have coronary microvascular disease may show that they are at low risk for heart disease.
Research is ongoing to learn more about coronary microvascular disease and its causes.
How Is Heart Disease Diagnosed in Women
Your doctor will diagnose coronary heart disease based on your medical and family histories, your risk factors, a physical exam, and the results from tests and procedures.
No single test can diagnose coronary heart disease. If your doctor thinks you have coronary heart disease, he or she may recommend one or more of the following tests.
EKG (Electrocardiogram)
An EKG is a simple, painless test that detects and records the heart’s electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart.
An EKG can show signs of heart damage due to coronary heart disease and signs of a previous or current heart attack.
Stress Testing
During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can’t exercise, you may be given medicines to increase your heart rate.
When your heart is working hard and beating fast, it needs more blood and oxygen. Plaque-narrowed coronary (heart) arteries can’t supply enough oxygen-rich blood to meet your heart’s needs.
A stress test can show possible signs and symptoms of coronary heart disease, such as:
- Abnormal changes in your heart rate or blood pressure
- Shortness of breath or chest pain
- Abnormal changes in your heart rhythm or your heart’s electrical activity
If you can’t exercise for as long as what is considered normal for someone your age, your heart may not be getting enough oxygen-rich blood. However, other factors also can prevent you from exercising long enough (for example, lung diseases, anemia, or poor general fitness).
As part of some stress tests, pictures are taken of your heart while you exercise and while you rest. These imaging stress tests can show how well blood is flowing in your heart and how well your heart pumps blood when it beats.
Echocardiography
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test provides information about the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can show areas of poor blood flow to the heart, areas of heart muscle that aren’t contracting normally, and previous injury to the heart muscle caused by poor blood flow.
Chest X Ray
A chest x ray creates pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels.
A chest x ray can reveal signs of heart failure, as well as lung disorders and other causes of symptoms not related to coronary heart disease.
Blood Tests
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels may be a sign that you’re at risk for coronary heart disease. Blood tests also help detect anemia, a risk factor for coronary heart disease.
During a heart attack, heart muscle cells die and release proteins into the bloodstream. Blood tests can measure the amount of these proteins in the bloodstream. High levels of these proteins are a sign of a recent heart attack.
Coronary Angiography and Cardiac Catheterization
Your doctor may recommend coronary angiography if other tests or factors suggest you have coronary heart disease. This test uses dye and special x rays to look inside your coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization.
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is threaded into your coronary arteries, and the dye is released into your bloodstream.
Special x rays are taken while the dye is flowing through your coronary arteries. The dye lets your doctor study the flow of blood through your heart and blood vessels.
Coronary angiography detects blockages in the large coronary arteries. However, the test doesn’t detect coronary microvascular disease. This is because coronary microvascular disease doesn’t cause blockages in the large coronary arteries.
Even if the results of your coronary angiography are normal, you may still have chest pain or other coronary heart disease symptoms. If so, talk with your doctor about whether you might have coronary microvascular disease.
Your doctor may ask you to fill out a questionnaire called the Duke Activity Status Index. This questionnaire measures how easily you can do routine tasks. It gives your doctor information about how well blood is flowing through your coronary arteries.
Your doctor also may recommend other tests that measure blood flow in the heart, such as a cardiac MRI (magnetic resonance imaging) stress test.
Cardiac MRI uses radio waves, magnets, and a computer to create pictures of your heart as it beats. The test produces both still and moving pictures of your heart and major blood vessels.
Other tests done during cardiac catheterization can check blood flow in the heart’s small arteries and the thickness of the artery walls.
Tests Used To Diagnose Broken Heart Syndrome
If your doctor thinks you have broken heart syndrome, he or she may recommend coronary angiography. Other tests are also used to diagnose this disorder, including blood tests, EKG, echo, and cardiac MRI.
How Is Heart Disease Treated in Women
Treatment for coronary heart disease usually is the same for both women and men. Treatment may include lifestyle changes, medicines, medical and surgical procedures, and cardiac rehabilitation (rehab).
The goals of treatment are to:
- Relieve symptoms.
- Reduce risk factors in an effort to slow, stop, or reverse the buildup of plaque.
- Lower the risk of blood clots forming. (Blood clots can cause a heart attack.)
- Widen or bypass plaque-clogged coronary (heart) arteries.
- Prevent coronary heart disease complications.
Lifestyle Changes
Making lifestyle changes can help prevent or treat coronary heart disease. These changes may be the only treatment that some people need.
Quit Smoking
If you smoke or use tobacco, try to quit. Smoking can raise your risk for coronary heart disease and heart attack and worsen other coronary heart disease risk factors. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
If you find it hard to quit smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
Follow a Healthy Diet
A healthy diet is an important part of a healthy lifestyle. A healthy diet includes a variety of vegetables and fruits. These foods can be fresh, canned, frozen, or dried. A good rule is to try to fill half of your plate with vegetables and fruits.
A healthy diet also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
Choose and prepare foods with little sodium (salt). Too much salt can raise your risk for high blood pressure. Studies show that following the Dietary Approaches to Stop Hypertension (DASH) eating plan can lower blood pressure.
Try to avoid foods and drinks that are high in added sugars. For example, drink water instead of sugary drinks, like soda.
Also, try to limit the amount of solid fats and refined grains that you eat. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
If you drink alcohol, do so in moderation. Research suggests that regularly drinking small to moderate amounts of alcohol may lower the risk of coronary heart disease. Women should have no more than one alcoholic drink a day.
One drink a day can lower your coronary heart disease risk by raising your HDL cholesterol level. One drink is a glass of wine, beer, or a small amount of hard liquor.
If you don’t drink, this isn’t a recommendation to start using alcohol. Also, you shouldn’t drink if you’re pregnant, if you’re planning to become pregnant, or if you have another health condition that could make alcohol use harmful.
Too much alcohol can cause you to gain weight and raise your blood pressure and triglyceride level. In women, even one drink a day may raise the risk of certain types of cancer.
Be Physically Active
Regular physical activity can lower many coronary heart disease risk factors, including high LDL cholesterol, high blood pressure, and excess weight.
Physical activity also can lower your risk for diabetes and raise your HDL cholesterol level. (HDL cholesterol helps remove cholesterol from your arteries.)
Talk with your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. Walking is an excellent heart healthy exercise. The more active you are, the more you will benefit.
Maintain a Healthy Weight
Overweight and obesity are risk factors for CHD. If you’re overweight or obese, try to lose weight. Cut back your calorie intake and do more physical activity. Eat smaller portions and choose lower calorie foods. Your health care provider may refer you to a dietitian to help you manage your weight.
A BMI of less than 25 and a waist circumference of 35 inches or less is the goal for preventing and treating coronary heart disease. BMI measures your weight in relation to your height and gives an estimate of your total body fat.
To measure your waist, stand and place a tape measure around your middle, just above your hipbones. Measure your waist just after you breathe out. Make sure the tape is snug but doesn’t squeeze the flesh. See Waist Hip Ratio on how to measure your waist and hip ratio.
Stress and Depression
Research shows that getting upset or angry can trigger a heart attack. Also, some of the ways people cope with stress—such as drinking, smoking, or overeating—aren’t heart healthy.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health.
Having supportive people in your life with whom you can share your feelings or concerns can help relieve stress. Physical activity, yoga, and relaxation therapy also can help relieve stress. You may want to consider taking part in a stress management program.
Depression can double or triple your risk for coronary heart disease. Depression also makes it hard to maintain a heart healthy lifestyle.
Talk with your doctor if you have symptoms of depression, such as feeling hopeless or not taking interest in daily activities. He or she may recommend counseling or prescribe medicines to help you manage the condition.
Medicines
You may need medicines to treat coronary heart disease if lifestyle changes aren’t enough. Medicines can help:
- Reduce your heart’s workload and relieve coronary heart disease symptoms
- Decrease your chance of having a heart attack or dying suddenly
- Lower your LDL cholesterol, blood pressure, and other coronary heart disease risk factors
- Prevent blood clots
- Prevent or delay the need for a procedure or surgery, such as angioplasty or coronary artery bypass grafting (CABG)
Women who have coronary microvascular disease and anemia may benefit from taking medicine to treat the anemia.
Women who have broken heart syndrome also may need medicines. Doctors may prescribe medicines to relieve fluid buildup, treat blood pressure problems, prevent blood clots, and manage stress hormones. Most people who have broken heart syndrome make a full recovery within weeks.
Take all of your medicines as prescribed. If you have side effects or other problems related to your medicines, tell your doctor. He or she may be able to provide other options.
Menopausal Hormone Therapy
Recent studies have shown that menopausal hormone therapy doesn’t prevent coronary heart disease. Some studies have even shown that menopausal hormone therapy increases women’s risk for coronary heart disease, stroke, and breast cancer.
However, these studies tested menopausal hormone therapy on women who had been postmenopausal for at least several years. During that time, they could have already developed coronary heart disease.
Research is ongoing to see whether menopausal hormone therapy helps prevent coronary heart disease when taken right when menopause starts. While questions remain, current findings suggest menopausal hormone therapy shouldn’t routinely be used to prevent or treat coronary heart disease.
Ask your doctor about other ways to prevent or treat coronary heart disease, including lifestyle changes and medicines.
Procedures and Surgery
You may need a procedure or surgery to treat coronary heart disease. Both angioplasty and CABG are used as treatments. You and your doctor can discuss which treatment is right for you.
- Percutaneous Coronary Intervention
Percutaneous coronary intervention, commonly known as angioplasty, is a nonsurgical procedure that opens blocked or narrowed coronary arteries.
A thin, flexible tube with a balloon or other device on the end is threaded through a blood vessel to the narrowed or blocked coronary artery. Once in place, the balloon is inflated to compress the plaque against the wall of the artery. This restores blood flow through the artery.
Percutaneous coronary intervention can improve blood flow to your heart and relieve chest pain. A small mesh tube called a stent usually is placed in the artery to help keep it open after the procedure.
- Coronary Artery Bypass Grafting
CABG is a type of surgery. During CABG, a surgeon removes arteries or veins from other areas in your body and uses them to bypass (that is, go around) narrowed or blocked coronary arteries.
CABG can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
Cardiac Rehabilitation
Your doctor may prescribe cardiac rehab for angina or after angioplasty, CABG, or a heart attack. Almost everyone who has coronary heart disease can benefit from cardiac rehab.
Cardiac rehab is a medically supervised program that can improve the health and well-being of people who have heart problems.
The cardiac rehab team may include doctors, nurses, exercise specialists, physical and occupational therapists, dietitians or nutritionists, and psychologists or other mental health specialists.
Cardiac rehab has two parts:
- Exercise training. This part of rehab helps you learn how to exercise safely, strengthen your muscles, and improve your stamina. Your exercise plan will be based on your personal abilities, needs, and interests.
- Education, counseling, and training. This part of rehab helps you understand your heart condition and find ways to lower your risk for future heart problems. The rehab team will help you learn how to cope with the stress of adjusting to a new lifestyle and with your fears about the future.
Living With Heart Disease
If you have coronary heart disease, you can take steps to control its risk factors and prevent complications. Lifestyle changes and ongoing care can help you manage the disease.
Having coronary heart disease raises your risk for a heart attack. Thus, knowing the warning signs of a heart attack is important. If you think you’re having a heart attack, call your local emergency number right away. For more detailed information about heart attack warning signs, go to the section on warning signs below.
Lifestyle Changes
Adopting a heart healthy lifestyle can help you control coronary heart disease risk factors. However, making lifestyle changes can be a challenge.
Try to take things one step at a time. Learn about the benefits of lifestyle changes, and make a plan with specific, realistic goals. Reward yourself for your progress.
The good news is that many lifestyle changes help control several coronary heart disease risk factors at the same time. For example, physical activity lowers your blood pressure and LDL cholesterol level, helps control diabetes and prediabetes, reduces stress, and helps control your weight.
Ongoing Care
Your coronary heart disease risk factors can change over time, so having ongoing care is important. Your doctor will track your blood pressure, blood cholesterol, and blood sugar levels with routine tests. These tests will show whether your doctor needs to adjust your treatment.
Ask your doctor how often you should schedule followup visits and blood tests. Between visits, call your doctor if you have any new symptoms or if your symptoms worsen.
You may feel depressed or anxious if you’ve been diagnosed with coronary heart disease. You may worry about heart problems or making lifestyle changes.
Your doctor may recommend medicine, professional counseling, or relaxation therapy if you have depression or anxiety. It’s important to treat these conditions because they raise your risk for coronary heart disease and heart attack. Depression and anxiety also can make it harder for you to make lifestyle changes.
Heart Attack Warning Signs
If you have coronary heart disease, learn the warning signs of a heart attack. Heart attack signs and symptoms include:
- Chest pain or discomfort. This involves uncomfortable pressure, squeezing, fullness, or pain in the center or left side of the chest that can be mild or strong.
- This pain or discomfort often lasts more than a few minutes or goes away and comes back.
- Upper body discomfort in one or both arms, the back, neck, jaw, or upper part of the stomach.
- Shortness of breath, which may occur with or before chest discomfort.
- Nausea (feeling sick to your stomach), vomiting, light-headedness or fainting, or breaking out in a cold sweat.
- Sleep problems, fatigue (tiredness), and lack of energy.
If you think you’re having a heart attack, call your local emergency number at once. Early treatment can prevent or limit damage to your heart muscle.
If you think you’re having a heart attack, do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room.
Let the people you see regularly know you’re at risk for a heart attack. They can seek emergency care if you suddenly faint, collapse, or have other severe symptoms.
Living With Broken Heart Syndrome
Most people who have broken heart syndrome make a full recovery within weeks. The risk is low for a repeat episode of this disorder.
To check your heart health, your doctor may recommend echocardiography about a month after you’re diagnosed with the syndrome. Talk with your doctor about how often you should schedule followup visits.
- Centers for Disease Control and Prevention. About Heart Disease. https://www.cdc.gov/heartdisease/about.htm[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. The Heart Truth » Lower Heart Disease Risk. https://www.nhlbi.nih.gov/health/educational/hearttruth/lower-risk/what-is-heart-disease.htm[↩]
- Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple Cause of Death 1999-2015 on CDC WONDER Online Database, released December 2016. Data are from the Multiple Cause of Death Files, 1999-2015, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. https://wonder.cdc.gov/mcd-icd10.html[↩][↩][↩][↩]
- Heron M. Deaths: Leading causes for 2014. National vital statistics reports. 2016;65(5). https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_05.pdf[↩]
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. Circulation. 2017;135:e1–e458. DOI: 10.1161/CIR.0000000000000485.[↩]
- Fryar CD, Chen T, Li X. Prevalence of Uncontrolled Risk Factors for Cardiovascular Disease: United States, 1999–2010. NCHS Data Brief, No. 103. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2012.[↩]
- CDC. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Preventions, 2011. https://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf[↩]
- Kochanek KD, Xu JQ, Murphy SL, Miniño AM, Kung HC. Deaths: final data for 2009. Nat Vital Stat Rep. 2011;60(3). https://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_03.pdf[↩][↩]
- BMI Calculator Adults. https://www.cdc.gov/healthyweight/assessing/bmi/adult_BMI/english_bmi_calculator/bmi_calculator.html[↩][↩]
- Centers for Disease Control and Prevention. CDC Clinical Growth Charts. https://www.cdc.gov/growthcharts/clinical_charts.htm[↩][↩]
- Centers for Disease Control and Prevention. BMI Percentile Calculator for Child and Teen. https://nccd.cdc.gov/dnpabmi/Calculator.aspx[↩][↩]
- BMI Calculator Children. https://nccd.cdc.gov/dnpabmi/Calculator.aspx[↩][↩]
- Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117:1658-67. http://circ.ahajournals.org/content/117/13/1658.long[↩][↩]
- National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bethesda, MD; 1998. https://www.nhlbi.nih.gov/health/health-topics/topics/obe[↩][↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Take Charge of Your DIABETES. https://www.cdc.gov/diabetes/pubs/pdf/tcyd.pdf[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Sudden Cardiac Arrest. https://www.nhlbi.nih.gov/health/health-topics/topics/scda[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Who Is at Risk for Sudden Cardiac Arrest ? https://www.nhlbi.nih.gov/health/health-topics/topics/scda/atrisk[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Are the Signs and Symptoms of Sudden Cardiac Arrest ? https://www.nhlbi.nih.gov/health/health-topics/topics/scda/signs[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. How Is Sudden Cardiac Arrest Diagnosed ? https://www.nhlbi.nih.gov/health/health-topics/topics/scda/diagnosis[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. How Is Sudden Cardiac Arrest Treated ? https://www.nhlbi.nih.gov/health/health-topics/topics/scda/treatment[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. How Can Death Due to Sudden Cardiac Arrest Be Prevented ? https://www.nhlbi.nih.gov/health/health-topics/topics/scda/prevention[↩][↩]
- Xu, JQ, Murphy, SL., Kochanek, KD, Bastian, BA. Deaths: Final data for 2013. National Vital Statistics Report. 2016:64(2).[↩]
- Heron M. Deaths: Leading causes for 2008. National vital statistics reports. 2012;60(6). https://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_06.pdf[↩][↩]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–220. http://circ.ahajournals.org/content/125/1/e2.long[↩][↩][↩][↩][↩]
- CDC. Million Hearts™: strategies to reduce the prevalence of leading cardiovascular disease risk factors. United States, 2011. MMWR 2011;60(36):1248–51. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6036a4.htm?s_cid=mm6036a4_w[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Disease in Women. https://www.nhlbi.nih.gov/health/health-topics/topics/hdw[↩][↩][↩][↩][↩][↩][↩]
- Xu, JQ, Murphy, SL., Kochanek, KD, Bastian, BA. Deaths: Final data for 2013. National Vital Statistics Report. 2016:64(2). https://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_02.pdf[↩]
- Mosca L, Mochari-Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circulation: Cardiovascular Quality Outcomes. 2010;3:120-7.[↩]
- National Heart, Lung and Blood Institute. What Are the Signs and Symptoms of Heart Disease? https://www.nhlbi.nih.gov/health/health-topics/topics/hdw/signs[↩][↩][↩][↩][↩][↩][↩]
- National Heart Lung and Blood Institute. What are the Signs and Symptoms of a Stroke ? https://www.nhlbi.nih.gov/health/health-topics/topics/stroke/signs[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Who Is at Risk for Heart Disease ? https://www.nhlbi.nih.gov/health/health-topics/topics/hdw/atrisk[↩]
- CDC. Million Hearts: strategies to reduce the prevalence of leading cardiovascular disease risk factors. United States, 2011. MMWR 2011;60(36):1248–51. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6036a4.htm?s_cid=mm6036a4_w[↩]
- U.S. Department of Health and Human Services, Office on Women’s Health. Heart Disease. Heart Disease and Stroke. https://www.womenshealth.gov/heart-disease-and-stroke[↩]
- American Heart Association. Coronary Artery Disease – Coronary Heart Disease. http://www.heart.org/HEARTORG/Conditions/More/MyHeartandStrokeNews/Coronary-Artery-Disease—The-ABCs-of-CAD_UCM_436416_Article.jsp[↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Other Names for Coronary Heart Disease. https://www.nhlbi.nih.gov/health/health-topics/topics/cad/names[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Causes a Heart Attack ? https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack/causes[↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Coronary Heart Disease. https://www.nhlbi.nih.gov/health/health-topics/topics/cad[↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Attack. https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack[↩]
- Redfors B, Shao Y, Omerovic E. Stress-induced cardiomyopathy (Takotsubo) – broken heart and mind? Vascular Health and Risk Management. 2013;9:149-154. doi:10.2147/VHRM.S40163. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3632585/[↩][↩][↩][↩]
- Trends in publications on stress-induced cardiomyopathy. Shao Y, Redfors B, Lyon AR, Rosengren A, Swedberg K, Omerovic E. Int J Cardiol. 2012 Jun 14; 157(3):435-6. https://www.ncbi.nlm.nih.gov/pubmed/22521379/[↩]
- Prevalence of Takotsubo cardiomyopathy in the United States. Deshmukh A, Kumar G, Pant S, Rihal C, Murugiah K, Mehta JL. Am Heart J. 2012 Jul; 164(1):66-71.e1. https://www.ncbi.nlm.nih.gov/pubmed/22795284/[↩]
- Shao Y, Redfors B, Lyon AR, Rosengren A, Swedberg K, Omerovic E. Trends in publications on stress-induced cardiomyopathy. Int J Cardiol. 2012;157(3):435–436. https://www.ncbi.nlm.nih.gov/pubmed/22521379[↩]
- Johnson NP, Chavez JF, Mosley WJ, 2nd, Flaherty JD, Fox JM. Performance of electrocardiographic criteria to differentiate Takotsubo cardiomyopathy from acute anterior ST elevation myocardial infarction. Int J Cardiol. 2011 Jul 28; Epub. https://www.ncbi.nlm.nih.gov/pubmed/21802749[↩]
- Ahmed KA, Madhavan M, Prasad A. Brain natriuretic peptide in apical ballooning syndrome (Takotsubo/stress cardiomyopathy): comparison with acute myocardial infarction. Coron Artery Dis. 2012;23(4):259–264. https://www.ncbi.nlm.nih.gov/pubmed/22395239[↩]
- Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352(6):539–548. https://www.ncbi.nlm.nih.gov/pubmed/15703419[↩]
- Park JH, Kim KS, Sul JY, et al. Prevalence and patterns of left ventricular dysfunction in patients with pheochromocytoma. J Cardiovasc Ultrasound. 2011;19(2):76–82. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3150700/[↩]
- Abraham J, Mudd JO, Kapur NK, Klein K, Champion HC, Wittstein IS. Stress cardiomyopathy after intravenous administration of catecholamines (neurotransmitters and hormones that include epinephrine, norepinephrine, and dopamine) and beta-receptor agonists. J Am Coll Cardiol. 2009;53(15):1320–1325. https://www.ncbi.nlm.nih.gov/pubmed/19358948[↩]
- Shao Y, Redfors B, Scharin Täng M, et al. Novel rat model reveals important roles of β-adrenoreceptors in stress-induced cardiomyopathy. Int J Cardiol. 2013 Jan 25; Epub. https://www.ncbi.nlm.nih.gov/pubmed/23357048[↩]
- Paur H, Wright PT, Sikkel MB, et al. High levels of circulating epinephrine trigger apical cardiodepression in a β2-adrenergic receptor/Gi-dependent manner: a new model of Takotsubo cardiomyopathy. Circulation. 2012;126(6):697–706. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4890655/[↩]
- Sharkey SW, Windenburg DC, Lesser JR. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55(4):333–341. https://www.ncbi.nlm.nih.gov/pubmed/20117439[↩]
- Lee PH, Song JK, Sun BJ. Outcomes of patients with stress-induced cardiomyopathy diagnosed by echocardiography in a tertiary referral hospital. J Am Soc Echocardiogr. 2010;23(7):766–771. https://www.ncbi.nlm.nih.gov/pubmed/20620862[↩]
- Burgdorf C, Kurowski V, Bonnemeier H, Schunkert H, Radke PW. Long-term prognosis of the transient left ventricular dysfunction syndrome (Tako-Tsubo cardiomyopathy): focus on malignancies. Eur J Heart Fail. 2008;10(10):1015–1019. https://www.ncbi.nlm.nih.gov/pubmed/18692439[↩]
- Schultz T, Shao Y, Redfors B, et al. Stress-induced cardiomyopathy in Sweden: evidence for different ethnic predisposition and altered cardio-circulatory status. Cardiology. 2012;122(3):180–186. https://www.ncbi.nlm.nih.gov/pubmed/22846788[↩][↩]
- Deshmukh A, Kumar G, Pant S, Rihal C, Murugiah K, Mehta JL. Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J. 2012;164(1):66–71. https://www.ncbi.nlm.nih.gov/pubmed/22795284[↩][↩]
- El-Sayed AM, Brinjikji W, Salka S. Demographic and co-morbid predictors of stress (takotsubo) cardiomyopathy. Am J Cardiol. 2012;110(9):1368–1372. https://www.ncbi.nlm.nih.gov/pubmed/22819424[↩]
- Summers MR, Lennon RJ, Prasad A. Pre-morbid psychiatric and cardiovascular diseases in apical ballooning syndrome (tako-tsubo/stress-induced cardiomyopathy): potential pre-disposing factors? J Am Coll Cardiol. 2010;55(7):700–701. https://www.ncbi.nlm.nih.gov/pubmed/20170799[↩]
- Wassertheil-Smoller S, Shumaker S, Ockene J, et al. Depression and cardiovascular sequelae in postmenopausal women. The Women’s Health Initiative (WHI) Arch Intern Med. 2004;164(3):289–298. https://www.ncbi.nlm.nih.gov/pubmed/14769624[↩]
- Gianaros PJ, Jennings JR, Sheu LK, Greer PJ, Kuller LH, Matthews KA. Prospective reports of chronic life stress predict decreased grey matter volume in the hippocampus. Neuroimage. 2007;35(2):795–803. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1868546/[↩]
- Corrigan FE, 3rd, Kimmel MC, Jayaram G. Four cases of takotsubo cardiomyopathy linked with exacerbations of psychiatric illness. Innov Clin Neurosci. 2011;8(7):50–53. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3159544/[↩]