Contents
Continuous positive airway pressure
CPAP is a abbreviated term for continuous positive airway pressure, a treatment for sleep apnea especially obstructive sleep apnea (OSA) 1, 2, 3, 4. CPAP may also be used in the neonatal intensive care unit (NICU) to treat preterm infants whose lungs have not yet fully developed and who may have respiratory distress syndrome from surfactant deficiency 5, 6, 7. Pediatricians (medical specialists who diagnose, treat and provide medical care for babies and children) may also use CPAP to treat hypoxia and decrease the work of breathing in infants with acute infectious processes such as bronchiolitis and pneumonia or for those with collapsible airways such as in tracheomalacia. CPAP therapy utilizes machines specifically designed to deliver a flow of constant pressure 8. CPAP therapy keeps your airway open by gently providing air through a mask you wear while you sleep and eliminating the breathing pauses caused by sleep apnea. With continuous positive airway pressure (CPAP), the air pressure is somewhat greater than that of the surrounding air and is just enough to keep your upper airway passages open, preventing apnea and snoring.
A CPAP machine includes:
- A mask or other device that fits over your nose or your nose and mouth
- Straps to position the mask
- A tube (hose) that connects the mask to the machine’s motor
- A small air compressor that blows air into the tube
CPAP is applied via face mask, nasal mask, nasopharyngeal tube or nasal prongs, using a conventional ventilator, bubble circuit or CPAP driver. The hose connects the CPAP machine to your mask. The tubing is long enough to allow you to move around or turn over in your bed. Most machines are about the size of a tissue box, lightweight and relatively quiet. You can keep the CPAP machine on your nightstand or at the side of your bed. When you sleep with a CPAP machine, you will no longer snore or make choking noises in your sleep. You will be able to sleep through the night without your body waking up from a lack of oxygen.
The CPAP mask may cover only your nose or both your nose and mouth. Another option is to use nasal pillows, which fit in your nostrils. Some other masks fit snugly under your nose. No matter what type of mask you use, it is important that it fits well and is comfortable. The mask must make a seal in order to keep your airway open through the night. A good mask seal will prevent air leaks and maintain the right level of air pressure.
Your sleep doctor will determine the amount of air pressure needed for CPAP to treat your sleep apnea. The doctor may recommend a CPAP titration study to calibrate your air pressure setting. Most CPAP units also come with a timed pressure “ramp” setting. This starts the airflow at a very low level, so you can fall asleep comfortably. The machine slowly raises the pressure while you sleep until it reaches the right level to treat your sleep apnea.
CPAP is a lifestyle change. It works best when used all night, every night. You also should use CPAP when you are napping. Just one night without treatment can have a negative impact on your blood pressure. Your body will feel better the more you use CPAP.
After using CPAP regularly, you may notice:
- Better concentration and memory
- Feeling more alert and less sleepy during the day
- Improved sleep for your bed partner
- Being more productive at work
- Less anxiety and depression and a better mood
- Normal sleep patterns
- Lower blood pressure (in people with high blood pressure)
Long-term benefits of CPAP may include 9:
- Helping to prevent or control high blood pressure
- Lowering your risk for stroke
- Improving memory and other cognitive function
Benefits of starting CPAP treatment include better sleep quality, reduction or elimination of snoring, and less daytime sleepiness. Your memory, concentration, cognitive function and mood may also improve. The quality of your sleep will improve, which, for some people, means you will feel more rested and alert during the daytime. Your partner might even sleep better because you will stop snoring. CPAP can also improve pulmonary hypertension and lower blood pressure. CPAP can be used safely safe for all ages, including children.
CPAP helps in achieving better V/Q matching and ensures maintenance of functional residual capacity. CPAP is not associated with adverse effects of invasive mechanical ventilation like excessive use of sedation and side effects of positive pressure ventilation (volutrauma and barotrauma). In the inpatient setting, it should be monitored very closely with vital signs, blood gases, and clinical profile. If there is any sign of deterioration mechanical ventilation should be considered.
CPAP is only a temporary treatment for obstructive sleep apnea and does not decrease the risk of cardiac complications. While using CPAP you should also lose excess body weight, eat healthy, discontinue smoking and participate in regular exercise 10.
Although continuous positive airway pressure (CPAP) is the most common and reliable method of treating sleep apnea, some people find it cumbersome or uncomfortable. Some people give up on the CPAP machine. But with practice, most people learn to adjust the tension of the straps on the mask to obtain a comfortable and secure fit.
You might need to try more than one type of mask to find one that’s comfortable. Don’t stop using the CPAP machine if you have problems. Check with your doctor to see what changes can be made to increase your comfort.
Additionally, contact your doctor if you’re still snoring or begin snoring again despite CPAP treatment. If your weight changes, the pressure settings of the CPAP machine might need to be adjusted.
Side effects of CPAP treatment may include nasal congestion, runny nose, dry mouth, or nosebleeds; humidification can often help with these symptoms 1. Masks may cause irritation or redness of the skin, and use of the right size mask and padding can minimize pressure sores from tight contact with skin. The mask and tube must be kept clean, regularly inspected and should be replaced every 3 to 6 months 1. Abdominal distension or a sensation of bloating might occur which rarely can lead to nausea, vomiting and subsequently aspiration this can be minimized by decreasing the CPAP pressure or gastric decompression through a tube in hospitalized patients 1.
There may arise rare instances of respiratory distress where a hospitalized patient would greatly benefit from CPAP but does not tolerate the mask or is not complaint due to delirium, agitation or factors such as very young age in children or the elderly. In such scenarios, mild sedation with low dose fentanyl or dexmedetomidine can be used to improve compliance, until the therapy is no longer indicated. As the use of any sedative or anxiolytic agent can lead to decrease in consciousness and decrease in respiratory drive these patients should be monitored very closely. If adequate minute ventilation and or oxygenation cannot be achieved, then management should include escalation to bilevel positive airway pressure (BiPAP) or intubation with mechanical ventilation following the code status and goals of care.
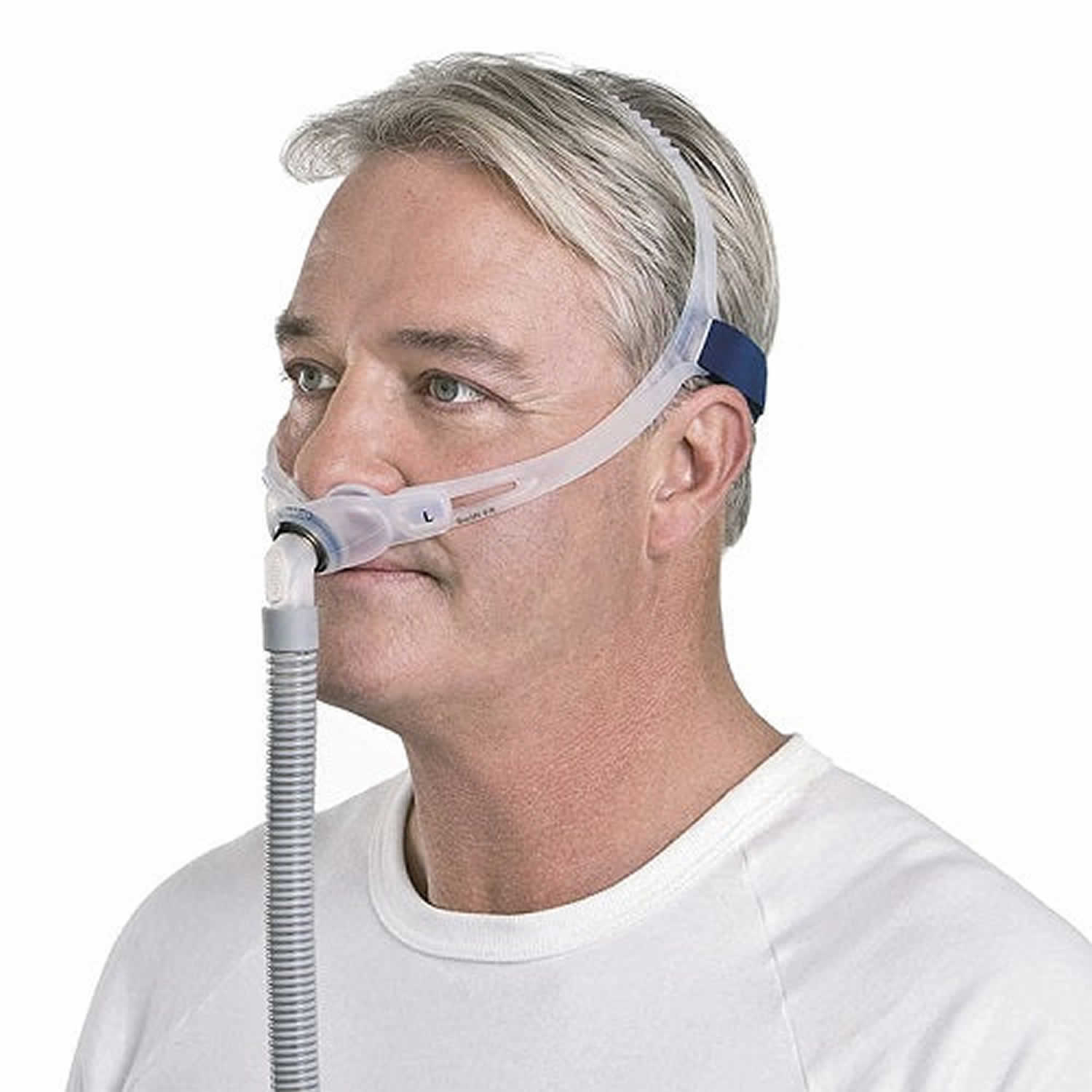
Figure 1. CPAP machine
Positive airway pressure therapy types
There are several forms of positive airway pressure (PAP) therapy other than CPAP. All forms of positive airway pressure (PAP) therapy keep your airway open as you sleep by providing a stream of air through a mask that you wear.
Autotitrating positive airway pressure (APAP)
Autotitrating positive airway pressure (APAP) therapy automatically raises or lowers your air pressure as needed during the night.
Bilevel positive airway pressure (BPAP)
Bilevel positive airway pressure (BPAP) devices have two alternating levels of pressure. There is a certain pressure when you inhale that drops when you exhale. If you have a problem using CPAP or autotitrating positive airway pressure (APAP), your sleep doctor may recommend BPAP. Your doctor also may recommend using BPAP if you have sleep apnea along with another breathing disorder.
Is CPAP covered by insurance?
If your doctor (sleep specialist) prescribes CPAP for your sleep apnea, your insurance will work with a medical device company to provide you with a CPAP machine and the mask and tube.
Your doctor will set up your machine with certain pressure settings. After using your machine for a while, your doctor and possibly your insurance company will want to check the data card from your machine to confirm that you are using your CPAP device and to see if the machine and its pressure settings are working to reduce or eliminate apnea events while you sleep.
How does CPAP work?
When using a CPAP setup:
- You wear a mask over your nose or nose and mouth while you sleep.
- The mask is connected by a hose to a small machine that sits at the side of your bed.
- The machine pumps air under pressure through the hose and mask and into your airway while you sleep. This helps keep your airway open.
You may start to use CPAP while you are in a sleep center for the night. At first CPAP patients should be monitored in a sleep lab where the optimal CPAP pressure is often determined by a technologist manually titrating settings to minimize apnea. A sleep doctor or pulmonologist can help find the most comfortable mask, trial a humidifier chamber in the machine, or use a different CPAP machine that allows multiple or auto-adjusting pressure settings. Auto-titrating CPAP machines use computer algorithms and pressure transducer sensors to determine the ideal pressure to eliminate apneic events. Some newer machines (self-adjusting or auto-PAP), may be set up for you and then just given to you to sleep with at home, without the need for a test to adjust the pressures.
- Your sleep specialist or pulmonologist will help choose the mask that fits you best.
- They will adjust the settings on the machine while you are asleep.
- The settings will be adjusted based on the severity of your sleep apnea.
It can take time to get used to using the CPAP setup. The first few nights are often the hardest and you may not sleep well. If you are having problems, you may be tempted not to use the CPAP machine for the whole night. But you will get used to it more quickly if you use the CPAP machine for the entire night.
When using the CPAP setup for the first time, you may have:
- A feeling of being closed in (claustrophobia)
- Chest muscle discomfort, which often goes away after awhile
- Eye irritation
- Redness and sores over the bridge of your nose
- Runny or stuffed-up nose
- Sore or dry mouth
- Nosebleeds
- Upper respiratory infections
Many of these problems can be helped or prevented.
- Ask your sleep specialist about using a mask that is lightweight and cushioned. Some masks are used only around or inside the nostrils.
- Make sure the mask fits correctly so that it does not leak air. It should not be too tight or too loose.
- Try nasal salt water sprays for a stuffy nose.
- Use a humidifier to help with dry skin or nasal passages.
- Keep your equipment clean.
- Place your machine underneath your bed to limit noise.
- Most machines are quiet, but if you notice sounds that make it hard to sleep, tell your provider.
Your sleep specialist can lower the pressure on the machine and then increase it again at a slow pace. Some new machines can automatically adjust to the right pressure.
If your symptoms don’t improve after you’re on CPAP treatment, the settings on the machine may need to be changed. Your sleep specialist may teach you how to adjust the settings at home. Or, you may need to go to the sleep center to have it adjusted.
CPAP uses
CPAP (continuous positive airway pressure) prevents episodes of airway collapse that block the breathing in people with obstructive sleep apnea (OSA) and other breathing problems 1. However, if you only have mild sleep apnea and do not feel very sleepy during the day, you may not need CPAP.
A noticeable sign of obstructive sleep apnea is snoring. You might also snort, choke or gasp. This pattern can repeat itself 5 to 30 times or more each hour, all night. This makes it hard to reach the deep, restful phases of sleep.
In North America, the prevalence of obstructive sleep apnea (OSA) is between 15 and 30 percent in males and 10 to 15 percent in females 11, 12. The prevalence of obstructive sleep apnea (OSA) varies by race, and in the United States is more prevalent in African Americans than in other groups, independent of body weight 13, 14.
The prevalence of obstructive sleep apnea (OSA) also appears to be increasing, which is thought to be related to a combination of increasing rates of obesity as well as increased diagnosis and detection 15. In a study by Peppard et al. 12, it was estimated that the prevalence of obstructive sleep apnea (OSA) increased from 11 to 14 percent from 1990 to 2010 among adult American males.
The major predisposing factor for obstructive sleep apnea (OSA) is excess body weight (obesity), male sex, and advancing age (maximum prevalence in the middle age group 40 to 64 year) 16, 17. Obesity is a major risk factor for obstructive sleep apnea as 60 to 70 percent of individuals with obstructive sleep apnea (OSA) have obesity. It is thought that excess fatty tissue in the head and neck constricts airways and abdominal fat may prevent the chest and lungs from fully expanding and relaxing. Other risk factors for obstructive sleep apnea include alcohol use; frequent nasal congestion; and blockages of the airways, such as by enlarged tonsils and adenoids 18. CPAP is only a temporary treatment for obstructive sleep apnea and does not decrease the risk of cardiac complications. While using CPAP you should also lose excess body weight, eat healthy, discontinue smoking and participate in regular exercise 10.
CPAP may also be used in the neonatal intensive care unit (NICU) to treat preterm infants whose lungs have not yet fully developed and who may have respiratory distress syndrome from surfactant deficiency 6, 7. Pediatricians (medical specialists who diagnose, treat and provide medical care for babies and children) may also use CPAP to treat hypoxia and decrease the work of breathing in infants with acute infectious processes such as bronchiolitis and pneumonia or for those with collapsible airways such as in tracheomalacia.
CPAP is also used in hypoxic respiratory failure associated with congestive heart failure in which it augments the cardiac output and improves V/Q matching 1. The application of CPAP maintains positive end-expiratory pressure (PEEP), can decrease atelectasis, increases the surface area of the alveolus, improves V/Q matching, and hence, improves oxygenation.
CPAP can aid oxygenation via positive end-expiratory pressure (PEEP) prior to placement of an artificial airway during endotracheal intubation. Positive end-expiratory pressure (PEEP) is the pressure in the alveoli above atmospheric pressure at the end of expiration.
CPAP is used to successfully extubate patients that might still benefit from positive pressure but who may not need invasive ventilation, such as obese patients with obstructive sleep apnea (OSA) or patients with congestive heart failure 1.
CPAP monitoring
Your doctor should monitor and follow up with you closely especially during initiation of CPAP therapy to ensure long-term success 19. Your must tell your doctor any adverse effects of using CPAP therapy which must then be addressed by your doctor. Patients also need long-term follow up with an annual office visit to check equipment, titrate settings as needed, and to ensure ongoing mask and interface fit.
CPAP Contraindications
CPAP cannot be used in individuals who are not spontaneously breathing 1. Patients with poor respiratory drive need invasive ventilation or non-invasive ventilation with CPAP plus additional pressure support and a backup rate (BiPAP) 1.
The following are relative contraindications for CPAP 1:
- Uncooperative or extremely anxious patient
- Reduced consciousness and inability to protect their airway
- Unstable cardiorespiratory status or respiratory arrest
- Trauma or burns involving the face
- Facial, esophageal, or gastric surgery
- Air leak syndrome (pneumothorax with bronchopleural fistula)
- Copious respiratory secretions
- Severe nausea with vomiting
- Severe air trapping diseases with hypercarbia asthma or chronic obstructive pulmonary disease (COPD)
CPAP machine
CPAP machine is a small air compressor that work by pressurizing air that is delivered through a hose and mask into your airway during sleep. The steady flow of air keeps your upper airway open, improving respiration and sleep quality 1. Some CPAP machines have other features as well, such as heated humidifiers. A CPAP machine also includes straps to position the mask, a hose or tube that connects the mask to the machine’s motor, a motor that blows air into the tube, and an air filter to purify the air entering the nose.
CPAP can be administered in several ways based on the mask interface used:
- Nasal CPAP: Nasal prongs that fit directly into the nostrils or a small mask that fits over the nose
- Nasopharyngeal (NP) CPAP: Administered via a nasopharyngeal tube- an airway placed through the nose whose tip terminates in the nasopharynx. This has the advantage of bypassing the nasal cavity, and CPAP is delivered more distally.
- CPAP via face mask: A full face mask is placed over the nose and mouth with a good seal. It can be used for those that are mouth breathers, or for pre-oxygenation in spontaneously breathing patients prior to intubation.
Bubble CPAP is a mode of delivering CPAP used in neonates and infants where the pressure in the circuit is maintained by immersing the distal end of the expiratory tubing in water 20. The depth of the tubing in water determines the pressure CPAP generated. Blended and humidified oxygen is delivered via nasal prongs or nasal masks and as the gas flows through the system, it “bubbles” out the expiratory tubing into the water, giving a characteristic sound. Pressures used are typically between 5 to 10 cm H2O. It requires skilled nurses and respiratory therapists to maintain effective and safe use of the bubble CPAP system.
For patients using CPAP in the outpatient setting at home, it is important to wear it regularly while asleep overnight and during daytime naps. Some CPAP units also come with a timed pressure “ramp” setting that starts the airflow at a low level and slowly raises the pressure to the set level that may make it more comfortable and easier to which to become accustomed.
How to setup and use a CPAP machine
- Find a good space to put the CPAP machine. A first step is deciding where you’re going to put the CPAP. For most people, the optimal spot is on a nightstand or small table next to their bed. A good space for your device meets these characteristics:
- Provides stable support to the base of the CPAP
- Allows the hose to reach the head of the bed
- Close enough to an outlet so that you can easily plug in the machine
- Permits unobstructed ability to turn on the device, open the filter compartment, and add water to the humidifier
- Check the filter. The CPAP machine comes with a replaceable filter, but the exact type of filter depends on your device. There is usually a small compartment in which the filter fits snugly. Written instructions or instructions from your sleep technician should provide specific details about the filter in your CPAP machine.
- Attach the hose to the CPAP machine. The machine has a special connector for the hose. The hose should attach and stay in place without exerting considerable force or effort.
- Attach the hose to the CPAP mask. The other end of the hose plugs into the CPAP mask and should create a tight connection, sometimes by clicking into place.
- Set up the humidifier (when applicable). Many CPAP machines have an attached humidifier to moisturize the air so that it’s less likely to dry out your mouth and throat over the course of the night. If your CPAP has a humidifier, fill it with distilled water only. Using distilled water prevents mineral buildup or any impurity issues that can come from using tap water. The humidifier reservoir should have a clear “MAX” fill line. Be careful not to exceed that level, which can cause water to enter the hose.
- Plug in the CPAP machine into an electrical outlet.
- Put on and adjust the mask. There are several types of masks that can be used with a CPAP. Full-face masks go over your nose and mouth. Other masks go over the nose or just underneath it. Your doctor or sleep specialist will recommend a mask based on several factors including how you breathe, the pressure you need, and your sleeping position. Regardless of the type of mask you use, it will be held in place using one or more straps that go around the top and/or back of your head. Start by positioning the mask on your face, and then attach or pull the straps to secure it. The mask should form a seal against your face, but it should not pinch or press deeply into your skin. Adjust the length of the straps to find a comfortable fit.
- Turn on CPAP machine. Once you have the mask in place, you can turn on your CPAP machine. The pressure settings will have already been set by your health care team, so you should be able to plug-and-play. When the machine is on, you will notice pressurized air coming through the mask. If you hear air escaping from the mask, it’s a sign that you need to adjust it for a tighter seal. Some CPAP machines have a function to test whether the mask has a good seal. When the device is turned on, you can decide whether to use the Ramp function. This starts with lower pressure that gradually increases before reaching your prescribed pressure for the night. Some people like to ease into their sleep with the Ramp function while others like to have full pressure from the start.
- Find a comfortable sleeping position. Test out a few sleeping positions to find those that are comfortable for your body, don’t interfere with your ability to wear the mask, and don’t pinch or block the hose.
What’s the Best CPAP Machine?
Choosing the right CPAP machine is an important and complex decision whether you’re buying for the first time or shopping for a replacement. You want to find a machine that works best for your needs, and things like cost, size, noise, portability, and features vary widely between manufacturers. The ResMed AirSense 11 AutoSet checks all of the important boxes when it comes to comfortable CPAP therapy. Highlights include automatic pressure adjustments based on your breathing, a heated humidifier, up to an hour of ramp-up time. Another important feature is MyAir, a digital assistant that helps first-time users navigate the device.
ResMed AirSense 11 AutoSet Pros
- Automatic pressure adjustments may increase therapy comfort. An auto-ramp feature also allows you to ease into your therapy with pressure that gradually builds to your prescribed levels. This can be set to increase pressure for up to 1 hour after turning on the machine.
- Heated humidifier limits dryness and irritation. The built-in humidifier is heated to minimize condensation in your connective hose.
- Compatible with the myAir (a digital assistant that provides voice-guided video instructions the first few times you use the machine) mobile app. For the first month of therapy, you’ll receive check-ins and CPAP coaching based on your medical history.
ResMed AirSense 11 AutoSet Cons
- Slightly more expensive than the average CPAP machine ($1,499)
- Advanced features are appealing but may not be necessary for all users
CPAP masks
Continuous positive airway pressure (CPAP) masks and headgear come in many styles and sizes to comfortably treat your sleep apnea. Everyone has different needs, preferences and face shapes, and sometimes you will need to try different mask styles before you find the one that works the best for you.
Sizes may vary across different CPAP mask styles and brands. You may need to try on several styles and sizes to find the best combination of comfort and efficiency.
For example, if you take a small in one type it does not necessarily mean you will need a small in a different brand. Proper sizing is very important to comfort and performance of CPAP masks.
Work with your doctor and CPAP mask supplier to make sure you have a mask that suits your needs and fits you properly.
Nasal pillow CPAP mask
Nasal pillow CPAP mask fits at the nostrils to supply air pressure. Nasal pillow CPAP masks might be good if:
- You feel claustrophobic in masks that cover more of your face.
- You want a full field of vision for reading or watching TV.
- You want to wear your glasses.
- You have facial hair that interferes with other masks.
Figure 2. Nasal pillow CPAP mask
Nasal CPAP masks
Nasal CPAP masks cover your nose to supply air pressure. Nasal CPAP masks might be good if:
- Your doctor has prescribed a high air pressure setting.
- You move around a lot in your sleep.
Figure 3. Nasal CPAP masks
Full-face CPAP masks
Full-face CPAP masks also called oronasal CPAP masks cover your nose and mouth to supply air pressure. Full-face CPAP masks might be a good choice if:
- You have nasal blockage or congestion that makes it hard to breathe through your nose.
- You breathe through your mouth at night despite a month of trying a nasal mask or nasal pillow. A nasal mask or nasal pillow are typically combined with a heated humidity feature, a chin strap or both to keep your mouth closed.
Figure 4. Full-face CPAP masks
Oral CPAP masks
Oral CPAP masks also known as a hybrid CPAP masks deliver air pressure through your mouth. Oral CPAP masks might be right for you if:
- You breathe through your mouth.
- You wear eyeglasses.
Figure 5. Oral CPAP mask
CPAP side effects
Side effects of continuous positive airway pressure (CPAP) treatment may include:
- Nasal congestion
- Dry eyes
- Dry mouth
- Nosebleeds
- Runny nose
- Dry mouth
- Respiratory infections
- Skin irritation from the mask or straps
- Chest discomfort
If you experience stomach discomfort or bloating, you should stop using your CPAP machine and contact your doctor. Depending on the type of sleep apnea you have, you may need another type of breathing device, such as an auto-adjusting positive airway pressure (APAP) machine or a bilevel positive airway pressure (BPAP) machine. It’s recommended that you discuss the most appropriate breathing device for you with your sleep specialist.
- Pinto VL, Sharma S. Continuous Positive Airway Pressure. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482178[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2019 Feb 15;15(2):335-343. doi: 10.5664/jcsm.7640[↩]
- Tingting X, Danming Y, Xin C. Non-surgical treatment of obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2018 Feb;275(2):335-346. doi: 10.1007/s00405-017-4818-y[↩]
- How to Use a CPAP Machine for Better Sleep. https://www.sleepfoundation.org/cpap/how-to-use-cpap-machine[↩]
- Ho JJ, Subramaniam P, Davis PG. Continuous positive airway pressure (CPAP) for respiratory distress in preterm infants. Cochrane Database Syst Rev. 2020 Oct 15;10(10):CD002271. doi: 10.1002/14651858.CD002271.pub3[↩]
- Gupta S, Donn SM. Continuous Positive Airway Pressure: To Bubble or Not to Bubble? Clin Perinatol. 2016 Dec;43(4):647-659. doi: 10.1016/j.clp.2016.07.003[↩][↩]
- Polin RA, Sahni R. Newer experience with CPAP. Semin Neonatol. 2002 Oct;7(5):379-89. doi: 10.1053/siny.2002.0132[↩][↩]
- Brown LK, Javaheri S. Positive Airway Pressure Device Technology Past and Present: What’s in the “Black Box”? Sleep Med Clin. 2017 Dec;12(4):501-515. doi: 10.1016/j.jsmc.2017.07.001[↩]
- CPAP. https://www.nhlbi.nih.gov/health/cpap[↩]
- Johnson BP, Shipper AG, Westlake KP. Systematic Review Investigating the Effects of Nonpharmacological Interventions During Sleep to Enhance Physical Rehabilitation Outcomes in People With Neurological Diagnoses. Neurorehabil Neural Repair. 2019 May;33(5):345-354. doi: 10.1177/1545968319840288[↩][↩]
- Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ. 2009 Aug;108(5):246-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2858234[↩]
- Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013 May 1;177(9):1006-14. doi: 10.1093/aje/kws342[↩][↩]
- Redline S, Tishler PV, Hans MG, Tosteson TD, Strohl KP, Spry K. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997 Jan;155(1):186-92. doi: 10.1164/ajrccm.155.1.9001310. Erratum in: Am J Respir Crit Care Med 1997 May;155(5):1820.[↩]
- Ancoli-Israel S, Klauber MR, Stepnowsky C, Estline E, Chinn A, Fell R. Sleep-disordered breathing in African-American elderly. Am J Respir Crit Care Med. 1995 Dec;152(6 Pt 1):1946-9. doi: 10.1164/ajrccm.152.6.8520760[↩]
- Cumpston E, Chen P. Sleep Apnea Syndrome. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564431[↩]
- Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010 May;11(5):441-6. doi: 10.1016/j.sleep.2009.10.005[↩]
- Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998 Jan;157(1):144-8. doi: 10.1164/ajrccm.157.1.9706079[↩]
- Brockbank JC. Update on pathophysiology and treatment of childhood obstructive sleep apnea syndrome. Paediatr Respir Rev. 2017 Sep;24:21-23. doi: 10.1016/j.prrv.2017.06.003[↩]
- Schwab RJ, Badr SM, Epstein LJ, Gay PC, Gozal D, Kohler M, Lévy P, Malhotra A, Phillips BA, Rosen IM, Strohl KP, Strollo PJ, Weaver EM, Weaver TE; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013 Sep 1;188(5):613-20. doi: 10.1164/rccm.201307-1282ST[↩]
- Casey JL, Newberry D, Jnah A. Early Bubble Continuous Positive Airway Pressure: Investigating Interprofessional Best Practices for the NICU Team. Neonatal Netw. 2016;35(3):125-34. doi: 10.1891/0730-0832.35.3.125[↩]