Contents
- Infective endocarditis
- What is endocarditis?
- Infective endocarditis causes
- Table 1. Infective Endocarditis Clinical Features According to Causative Organism
- Risk factors for infective endocarditis
- Native valve endocarditis
- Prosthetic valve endocarditis
- Opioid use disorder infective endocarditis
- Healthcare-associated infective endocarditis
- Fungal endocarditis
- Culture-Negative Endocarditis
- Infective endocarditis pathophysiology
- Infective endocarditis prevention
- Infective endocarditis signs and symptoms
- Infective endocarditis complications
- Infective endocarditis diagnosis
- Infective endocarditis treatment
- Infective endocarditis prognosis
Infective endocarditis
Infective endocarditis also called endocarditis, bacterial endocarditis or septic endocarditis is a rare life-threatening inflammation of the inner lining of the heart’s chambers and valves called the endocardium 1, 2. There are three forms of infective endocarditis 3:
- Acute infective endocarditis also called acute bacterial endocarditis develops suddenly and may become life threatening within days. Cases of acute bacterial endocarditis present with far more aggressive symptoms, including the following 4:
- Sepsis
- Congestive heart failure
- Kidney failure
- Stroke
- Septic emboli
- Subacute infective endocarditis also called subacute bacterial endocarditis or chronic infective endocarditis develops slowly over a period of weeks to several months. Fever, often low-grade and intermittent, is present in up to 90% of cases of subacute infective endocarditis. Heart murmurs are documented in approximately 85% of patients 4. 50% of patients may exhibit 1 or more classic signs and symptoms of subacute infective endocarditis. Signs and symptoms of subacute bacterial endocarditis include the following 4:
- Petechiae. Conjunctival petechiae (tiny purple, red or brown round spots on the skin [petechiae], in the whites of the eyes or inside the mouth).
- Splinter hemorrhages: Dark red, linear lesions in the nail beds
- Janeway lesions (painless red, purple or brown flat spots on the soles bottom of the feet or the palms of the hands).
- Osler’s nodes (painful red or purple bumps or patches of darkened skin [hyperpigmented] on the tips of the fingers or toes).
- Roth spots: Retinal hemorrhages with small, clear centers (rare)
- Signs of neurologic disease include the following 5, 6, 7, 8, 9.:
- Embolic stroke with focal neurologic deficits (the most common neurologic sign)
- Intracerebral hemorrhage
- Multiple microabscesses
- Prosthetic valvular infective endocarditis develops within a year after heart valve replacement.
The different types of infective endocarditis have varying causes and involve different pathogens. Infective endocarditis is primarily an inflammation of the endocardium caused by Gram-positive Streptococci, Staphylococci, and Enterococci bacteria 1. Together, these three groups of bacteria account for 80% to 90% of all infective endocarditis cases, with Staphylococcus aureus specifically responsible for around 30% of cases, while coagulase-negative Staphylococci accounting for ∼11% of cases in the developed world 10, 11, 12. Streptococci, primarily viridans group Streptococci, cause ∼30% of cases, with Streptococcus gallolyticus (a Streptococcus bovis group member) being involved in ∼20% to ∼50% of streptococcal cases 11, 12. Enterococci, especially Enterococcus faecalis, account for ∼10% of cases 11, 12. In addition to various Streptococci, Staphylococci, and Enterococci bacteria, other common colonizers of the oropharynx, such as the Haemophilus, Aggregatibacter (formerly Actinobacillus), Cardiobacterium, Eikenella, and Kingella species (HACEK organisms) can less frequently be the culprit bacteria 1. Less commonly, non-HACEK Gram-negative bacilli, such as the Enterobacteriaceae and nonfermenting Gram-negative bacilli have been previously identified as well but comprise only about 6% of total cases 13. Fungi are rare endocarditis causes, with Candida and Aspergillus infection in people with weakened immune system (immunocompromised patients) 1. A number of uncultivable or challenging to cultivate organisms cause endocarditis, the most common of which are Coxiella burnetii, Bartonella species, and Tropheryma whipplei 13.
In the United States, the incidence of infective endocarditis is approximately 12.7 cases per 100,000 persons per year 14. The most significant risk factor for infective endocarditis is residual heart valvular damage caused by a previous attack of endocarditis. Infective endocarditis most often involves the aortic or mitral valves, with tricuspid valve involvement accounting for fewer than 10% of cases often in association with injection drug use 11, 15, 16. Endocarditis associated with artificial heart valves or cardiovascular implantable electronic devices accounts for approximately one-third of cases and is most commonly caused by staphylococci 11, 16. Coagulase-negative Staphylococci are more frequent causes of prosthetic versus native valve endocarditis, while viridans group Streptococci more commonly cause native than prosthetic valve endocarditis 13. Although the majority of endocarditis cases are community acquired, health care-associated endocarditis is increasing and now accounts for approximately one-third of endocarditis cases in North America 11. Staphylococcus aureus, coagulase-negative Staphylococcus species, and Enterococci are most frequently detected in health care-associated cases 13. Organisms acquired in health care settings are notable for being increasingly resistant to antibacterial agents; methicillin-resistant Staphylococcus aureus (MRSA), for example, is more frequently associated with health care-acquired than community-acquired endocarditis, and most cases of endocarditis caused by non-HACEK Gram-negative bacilli are health care associated 17.
Infective endocarditis is a rare condition with an estimated yearly incidence of 3 to 10 cases per 100,000 people 18, 19, 20, 21. Endocarditis rarely happens in people whose hearts are healthy. According to the American Heart Association, about 47,000 people in the United States get an endocarditis diagnosis each year. Historically, infective endocarditis has a tendency for males, with a male to female ratio of nearly 2 to 1 1. The average age of infectious endocarditis patients is now greater than 65 years old 1. This tendency for the elderly likely corresponds to the increased prevalence of risk factors such as prosthetic valves, indwelling cardiac devices, acquired valvular disease, hemodialysis, and diabetes within this age group 22. Although previously a major risk factor, rheumatic heart disease now only affects less than 5% of all cases in the modern antibiotic era 1.
Recreational intravenous drug use (intravenous users of heroin, cocaine or amphetamine) represents a growing risk factor that now accounts for about 10% of all infectious endocarditis cases 23. One large single-center study demonstrated an increased incidence of infective endocarditis caused by intravenous drug use from 14.8% in 2004 to 26.1% in 2012–2014 24. They are mostly young people 25. For this reason, the incidence of infective endocarditis has been increasing, and intravenous drug users mortality ranges from 5% to 10% 26.
Infective endocarditis causes growths (vegetations) on the heart valves and these growths (vegetations) produce toxins and enzymes that kill and break down the heart tissue to cause holes in the heart valve, and spreads outside your heart and blood vessels. The resulting complications are:
- Embolism of material from the vegetation can get in the way of blood flow.
- Leaky valve.
- Heart block.
- Abnormal heart rhythm.
- Abscesses around the valve.
- Heart failure.
- Sepsis.
The symptoms of acute infective endocarditis usually begin with fever, chills, fast heart rate, fatigue, night sweats, aching joints and muscles, persistent cough or swelling in the feet, legs or abdomen. The symptoms of chronic infective endocarditis may include fatigue, mild fever, a moderately fast heart rate, weight loss, sweating and a low red blood cell count (anemia).
Infective endocarditis signs and symptoms include:
- Fever above 100°F (38.4°C).
- Sweats or chills, particularly night sweats.
- Skin rash.
- Pain, tenderness, redness or swelling.
- Wound or cut that won’t heal.
- Red, warm or draining sore.
- Sore throat, scratchy throat or pain when swallowing.
- Sinus drainage, nasal congestion, headaches or tenderness along your upper cheekbones.
- Persistent dry or a moist cough that lasts more than two days.
- White patches in your mouth or on your tongue.
- Nausea, vomiting or diarrhea.
- Emboli (small blood clots), hemorrhages (internal bleeding) or stroke.
- Shortness of breath.
- Poor appetite or weight loss.
- Muscle and joint aches.
Traditional infective endocarditis examination findings 27:
- Fever (~80% sensitive).
- Signs of local infection at the site of a pacemaker or indwelling catheter.
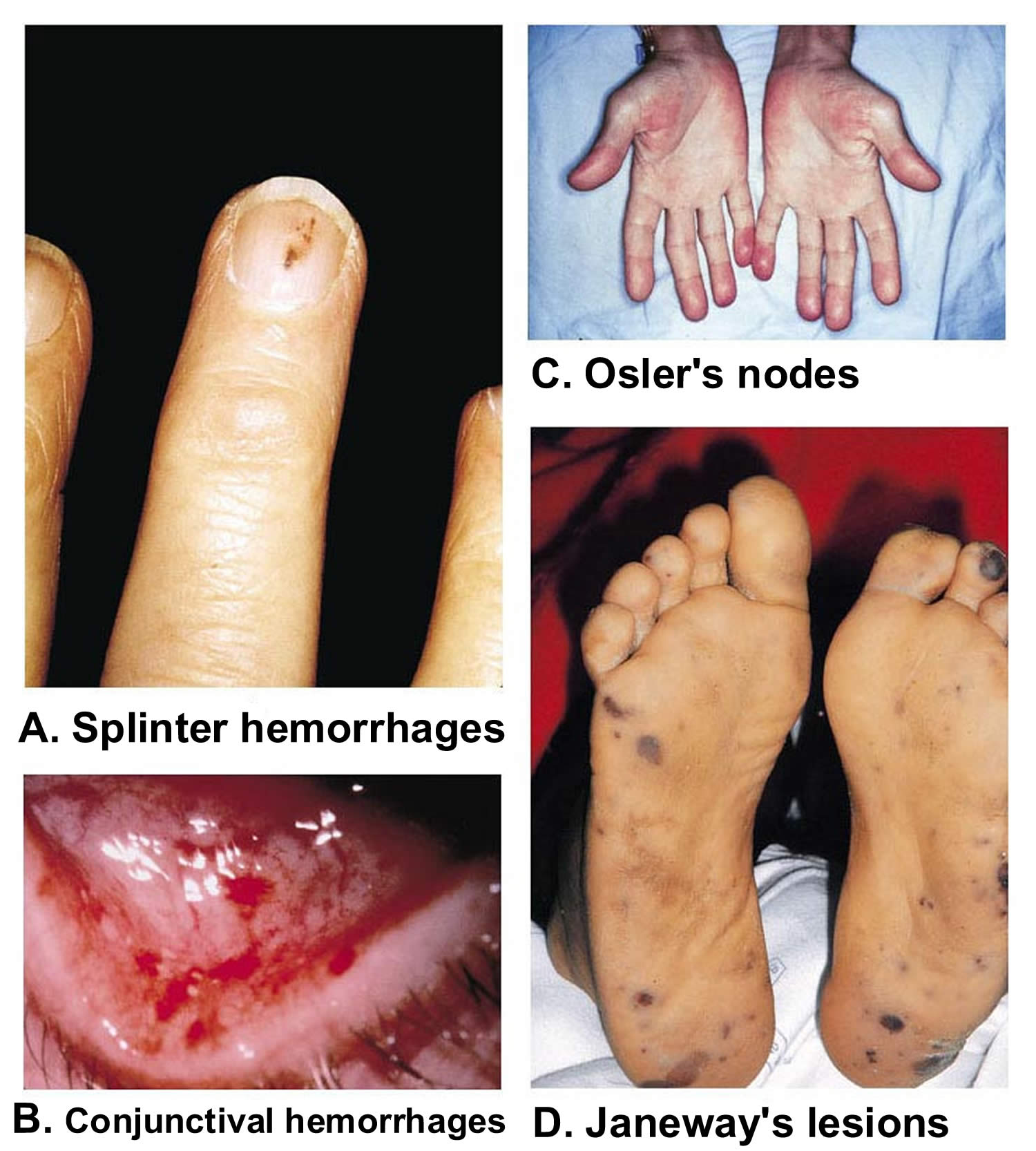
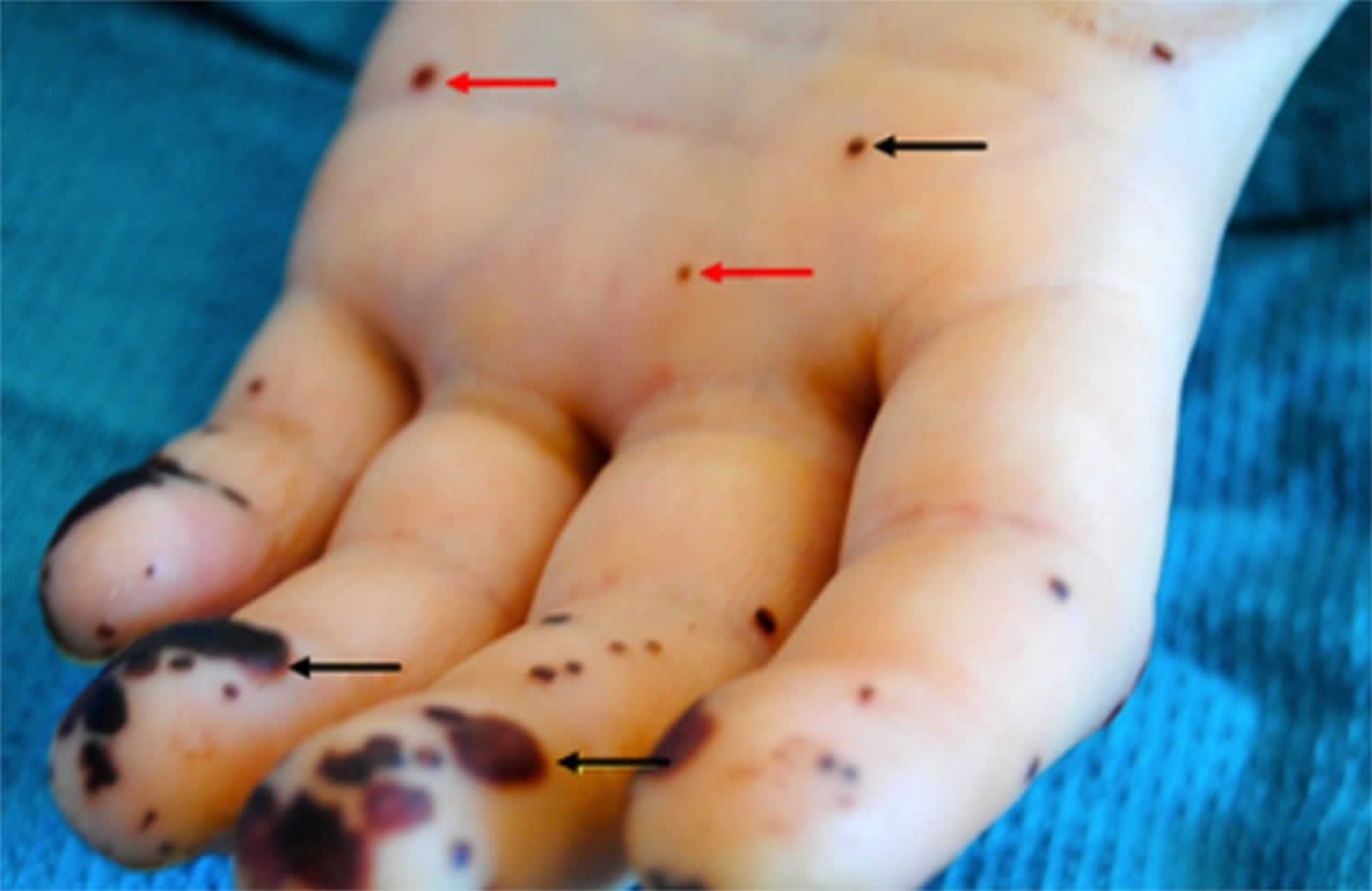
- Classic findings for endocarditis (<5% sensitive, mostly seen in subacute endocarditis) (see Figure 5 below):
- Splinter hemorrhages. Dark red, linear lesions in the nail beds
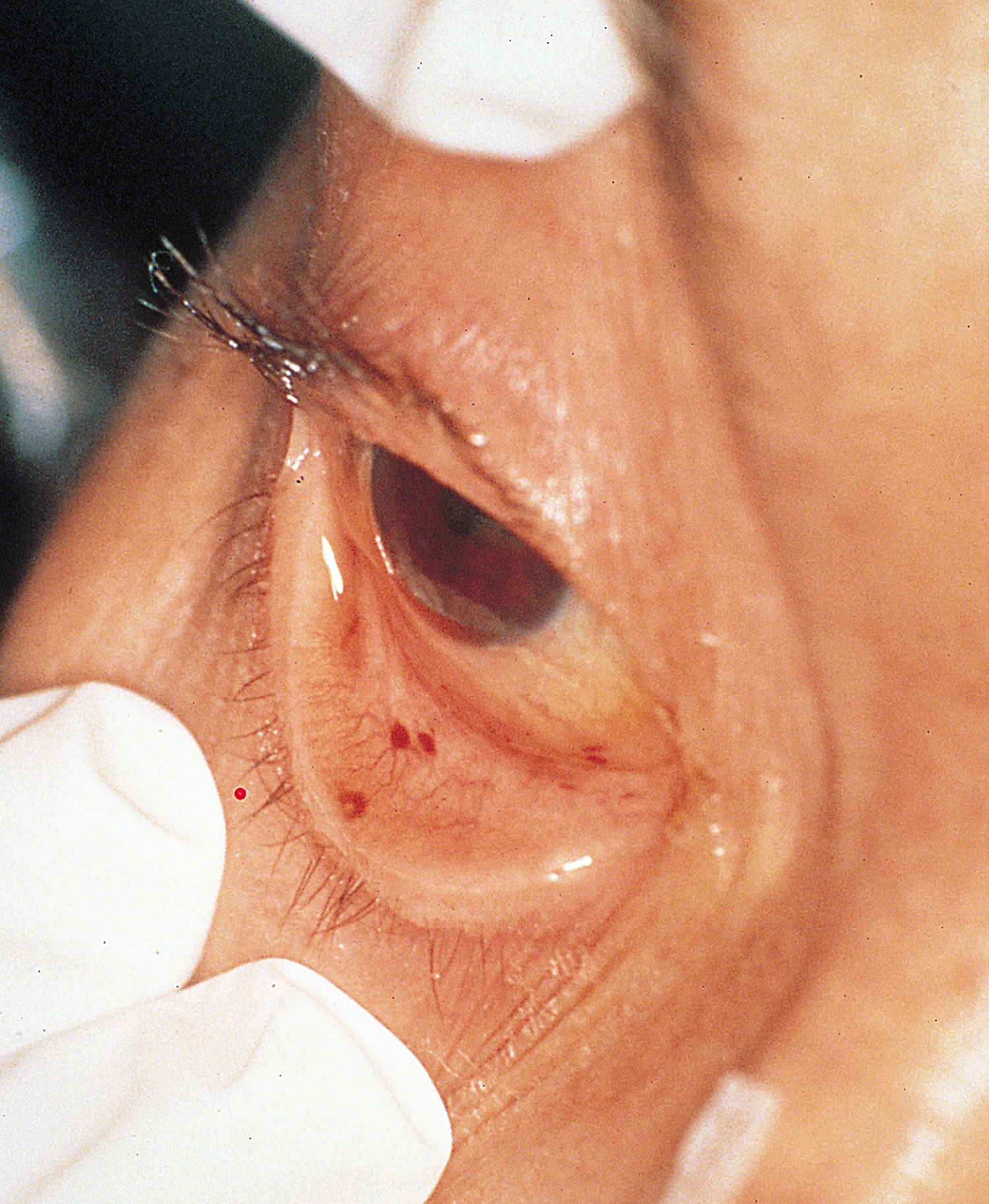
- Conjunctival petechiae (tiny purple, red or brown round spots on the skin [petechiae], in the whites of the eyes or inside the mouth).
- Janeway lesions (painless red, purple or brown flat spots on the soles bottom of the feet or the palms of the hands).
- Osler’s nodes (painful red or purple bumps or patches of darkened skin [hyperpigmented] on the tips of the fingers or toes).
Infective endocarditis diagnostic tests include:
- Blood cultures that show bacteria or microorganisms. Blood cultures — blood tests taken over time — allow a laboratory to isolate the specific bacteria that are causing your infection. To secure a diagnosis, the lab must take blood cultures before you start taking antibiotics.
- Complete blood count, which can tell your doctor if you have an unusually high number of white blood cells. This can mean you may have an infection.
- Blood tests for substances like C-reactive protein (CRP) can show you have inflammation.
- Echocardiogram (ultrasound of the heart), which may show growths (vegetations on your valve), abscesses (holes), new regurgitation (leaking) or stenosis (narrowing), or an artificial heart valve that has begun to pull away from your heart tissue. Sometimes providers insert an ultrasound probe into your esophagus or “food pipe” (transesophageal echo) to get a closer, more detailed look at your heart.
- Bopsy of heart valve tissue to find out which kind of microbe you have.
- Positron emission tomography (PET) or nuclear medicine scans to create images using radioactive material that can show an infection’s location.
The diagnosis of infective endocarditis requires the integration of clinical, laboratory, and echocardiographic data. Nonspecific laboratory abnormalities may be present, including anemia, leukocytosis, abnormal urinalysis results, and an elevated erythrocyte sedimentation rate and C-reactive protein level.
Duke criteria for diagnosing infective endocarditis 28:
Major criteria
- Blood culture typical of infective endocarditis, single positive culture for C. burnetti, or immunoglobulin G antiphase 1 level of ≥1/800. Major blood culture criteria for infective endocarditis include the following:
- 2 blood cultures positive for organisms typically found in patients with infective endocarditis
- Blood cultures persistently positive for 1 of these organisms, from cultures drawn more than 12 hours apart
- Three or more separate blood cultures drawn at least 1 hour apart
- Echocardiogram positive for infective endocarditis. Major echocardiographic criteria include the following:
- Echocardiogram positive for infective endocarditis, documented by an oscillating intracardiac mass on a valve or on supporting structures, in the path of regurgitant jets, or on implanted material, in the absence of an alternative anatomic explanation
- Myocardial abscess
- Development of partial dehiscence of a prosthetic valve
- New-onset valvular regurgitation
Minor criteria
- Predisposing heart condition or injection drug use
- Fever (temperature of >100.4°F [>38°C])
- Vascular phenomena, including major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage, or Janeway lesions
- Immunologic phenomena such as glomerulonephritis, Osler nodes, Roth spots, or rheumatoid factor
- Positive blood culture results not meeting major criteria or serologic evidence of active infection with an organism consistent with infective endocarditis
- Echocardiogram results consistent with infective endocarditis but not meeting major echocardiographic criteria
Definite endocarditis
- (i) 2 major clinical criteria OR
- (ii) 1 major clinical criterion and 3 minor clinical criteria OR
- (iii) 5 minor clinical criteria
Possible endocarditis
- (i) 1 major clinical criterion and 1 minor clinical criterion OR
- (ii) 3 minor clinical criteria
Rejected endocarditis
- (i) Firm alternative diagnosis is made explaining evidence of infective endocarditis;
- (ii) Resolution of infective endocarditis syndrome with antibiotic therapy for ≤4 days ;
- (iii) No pathologic evidence of infective endocarditis at surgery or autopsy, with antibiotic therapy for ≤4 days;
- (iv) Fail to meet criteria for for possible or definite infective endocarditis
Infective endocarditis can be life-threatening if left untreated. Once you get endocarditis, you’ll need quick treatment to prevent damage to your heart valves and more serious complications. After taking your blood cultures, your doctor will start you on intravenous (IV) antibiotic therapy. They’ll use a broad-spectrum antibiotic to cover as many suspected bacterial species as possible. As soon as they know which specific type of organism you have, they’ll adjust your antibiotics to target it. Usually, you’ll receive IV antibiotics for as long as six weeks to cure your infection. Your doctor will monitor your symptoms throughout your therapy to see if your treatment is effective. They’ll also repeat your blood cultures.
If endocarditis damages your heart valve and any other part of your heart, you may need surgery to fix your heart valve and improve your heart function.
After you complete your treatment, your doctor will determine the sources of bacteria in your blood (for example, dental infections) and treat them. In the future, you should take preventive or prophylactic antibiotics according to the national guidelines.
However, despite recent advances in diagnostic and treatment strategies for infective endocarditis, 1 year mortality has not improved and remains at 30%, which is worse than for many cancers 21, 29, 30.
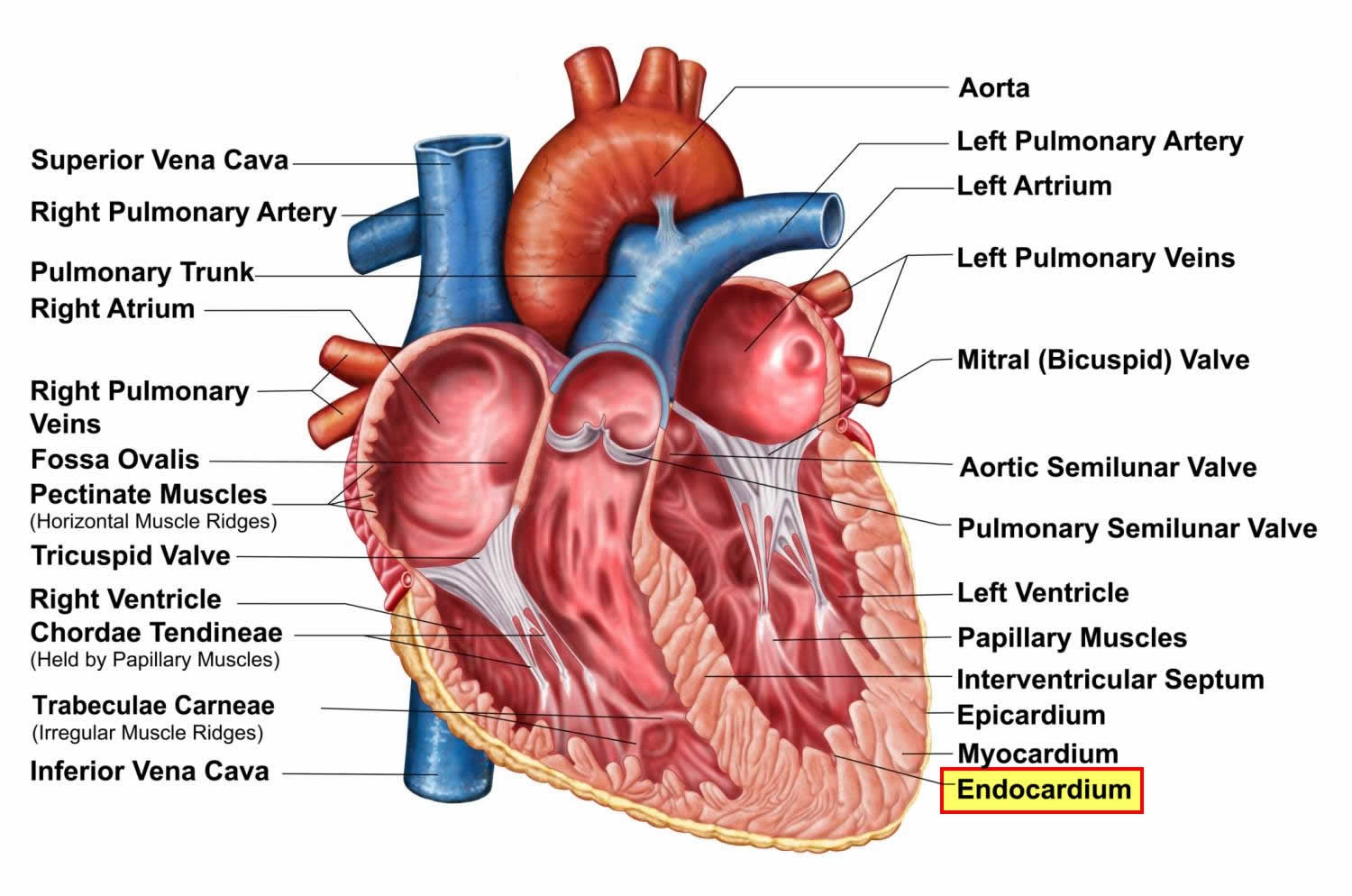
Figure 1. Heart anatomy
Footnote: A typical heart has 2 upper and 2 lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
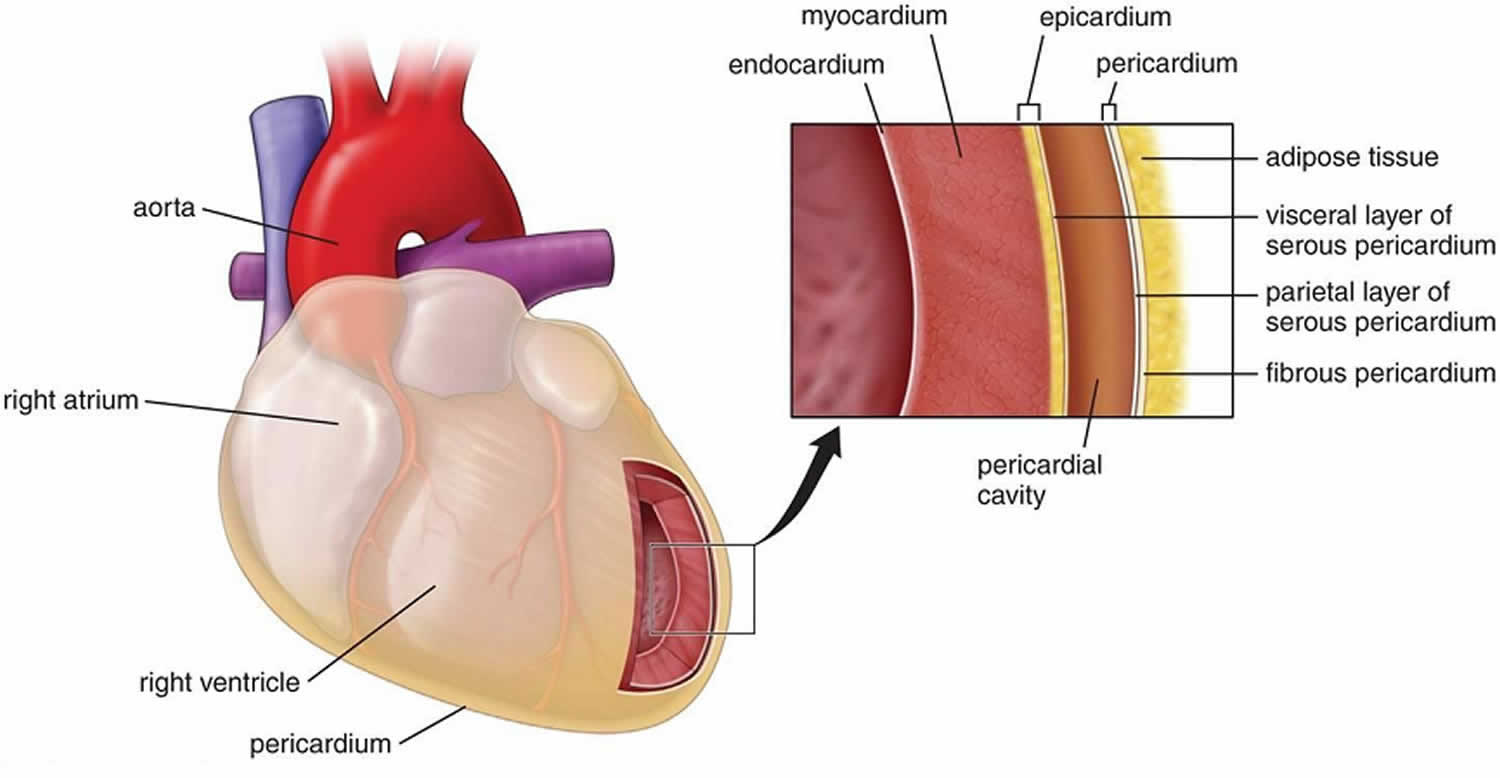
Figure 2. Endocardium
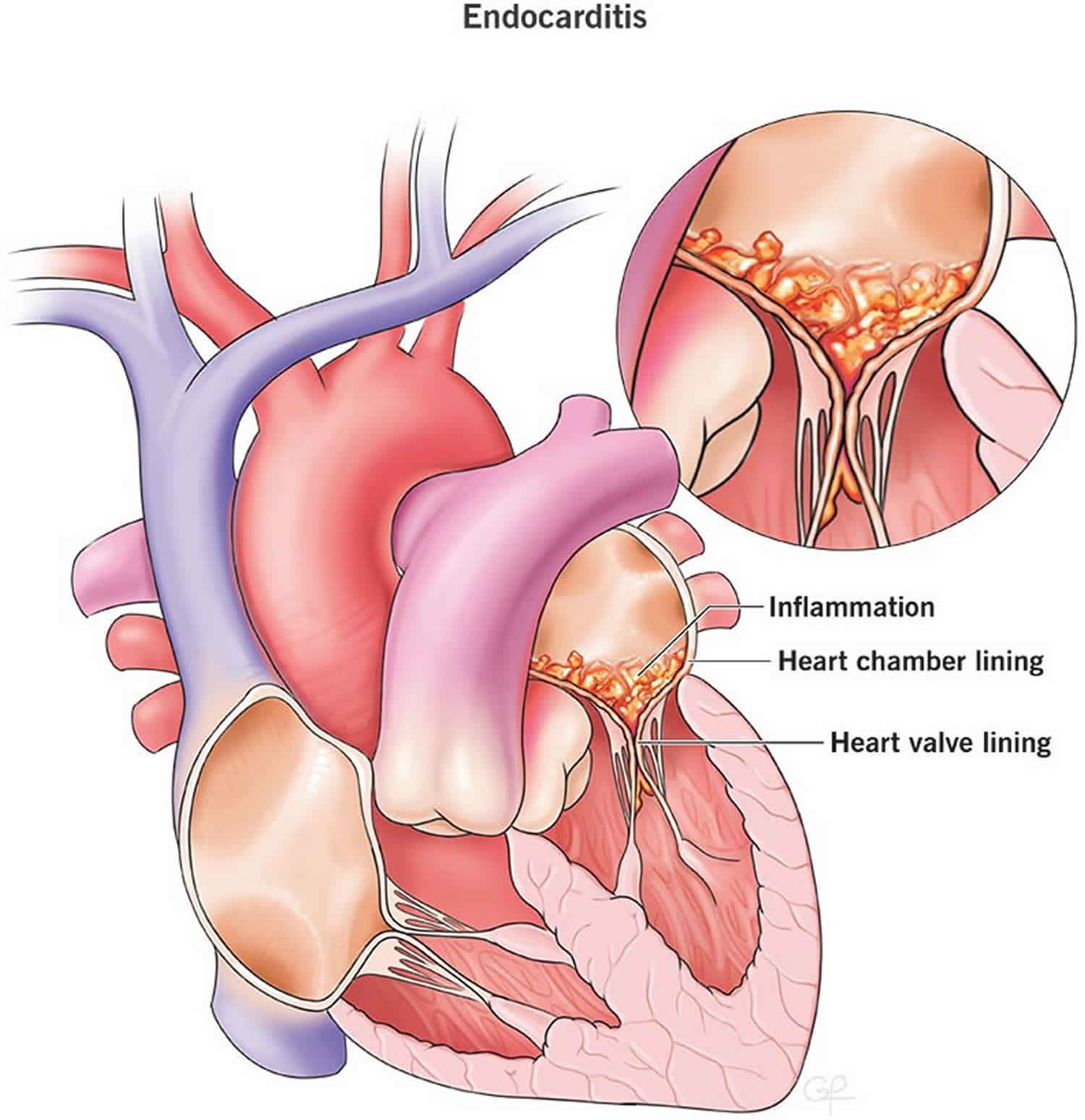
Figure 3. Infective endocarditis
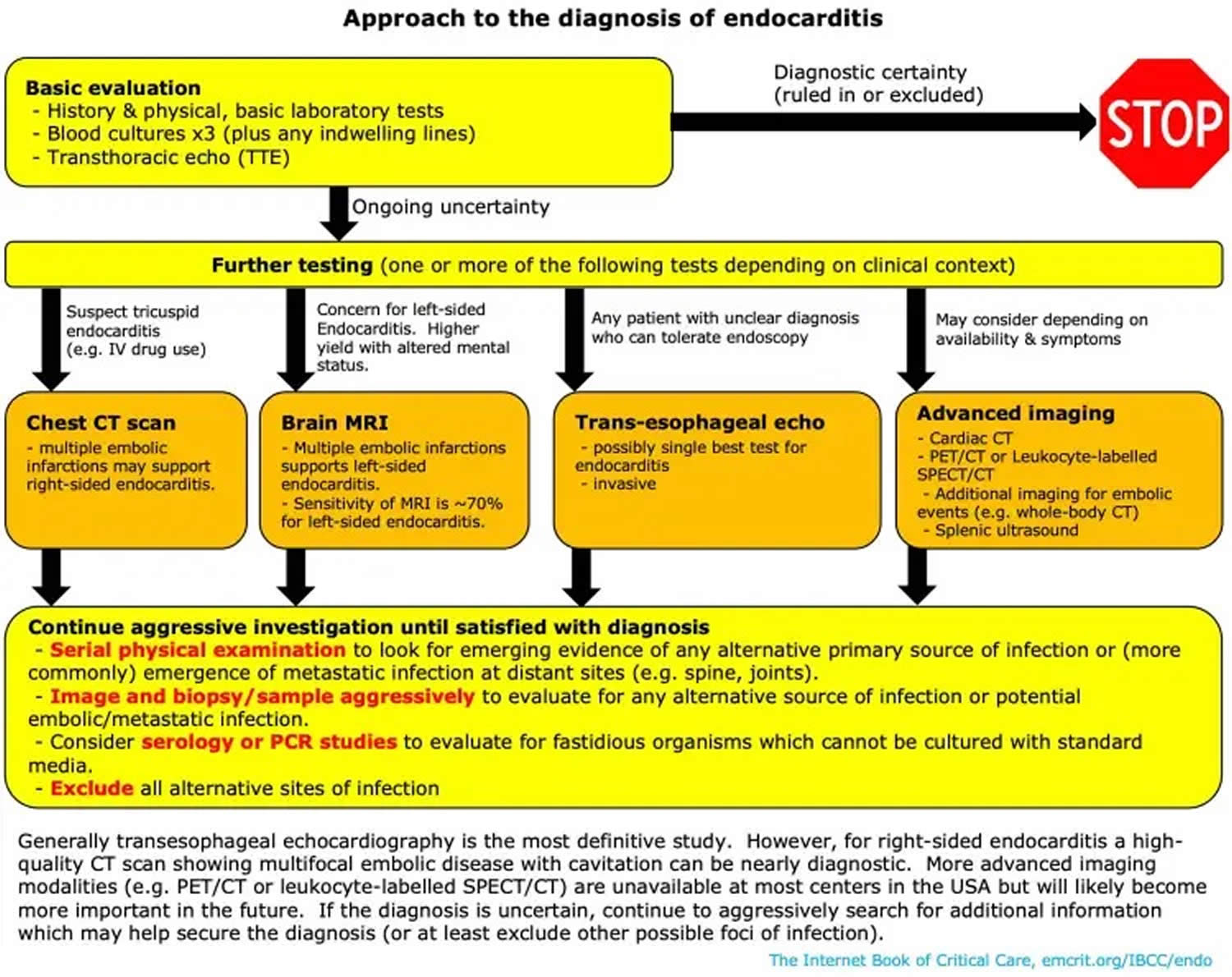
Footnotes: Diagnostic testing for identification of the microbiological origin of infective endocarditis. Peripheral blood cultures is the single most important test to order for suspected infective endocarditis. Cultures must be obtained prior to starting antibiotics in suspected endocarditis, even if this causes a short treatment delay. This diagnostic algorithm is intended for use in patients with clinical and/or echocardiographic findings suggestive of infective endocarditis based on the modified Duke criteria 31. Strong recommendations appear in boldface, with other diagnostic testing considerations shown in standard typeface. (1) Details on blood culture collection. (2) Coxiella burnetii anti-phase I IgG antibody titer of ≥1:800 is considered positive. (3) The sensitivity of Tropheryma whipplei PCR from blood in endocarditis is unknown; a negative result should not be used to rule out Tropheryma whipplei endocarditis. (4) If surgery is not performed, consider testing for noninfectious etiologies. (5) Histologic evaluation is used to evaluate for infectious and noninfectious etiologies and for correlation with microbiology test results. (6) Ideally, a representative sample of valvular tissue should be specifically collected for molecular testing in a sterile fashion in the operating room. (7) If sufficient valvular tissue is available after sampling for histopathological and molecular (microorganism-specific and broad-range) testing, consider culture and microbiology Gram stain. Due to the low sensitivity and specificity of culture, molecular testing should be prioritized over culture. (8) PAS-D, periodic acid-Schiff with diastase. Macrophages infected with Tropheryma whipplei will stain PAS positive following diastase digestion. (9) Examples include Mycoplasma hominis and Cutibacterium (formerly Propionibacterium) acnes PCR.
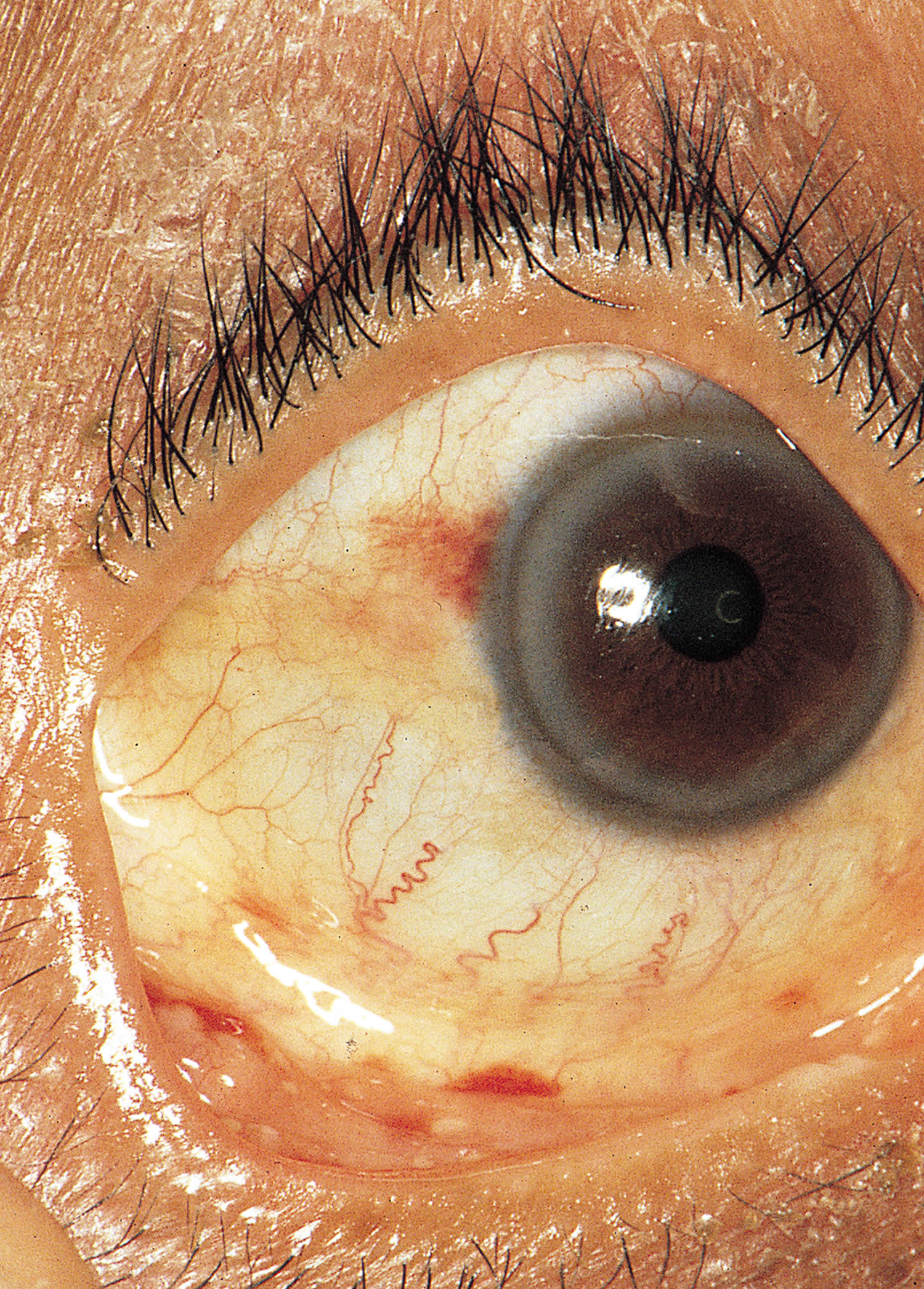
[Sources 32, 13 ]Figure 5. Infective endocarditis signs and symptoms
Footnotes: (A) Splinter hemorrhages are normally seen under the fingernails or toenails. They are usually linear and red for the first two to three days and brownish thereafter. (B) Shows conjunctival hemorrhages (petechiae). (C) Osler’s nodes are tender, subcutaneous nodules, often in the pulp of the digits or the thenar eminence. (D) Janeway’s lesions are nontender erythematous, hemorrhagic, or pustular lesions, often on the palms or soles.
[Source 27 ]What is endocarditis?
Endocarditis is sometimes also called infective endocarditis, is a rare life-threatening inflammation or infection of the lining inside your heart’s chambers and valves (the endocardium). Endocarditis is usually caused by bacteria, fungi or other germs from another part of your body, such as your mouth that get into your bloodstream and travel to your heart and lodge on abnormal heart valves or damaged heart tissue. Once germs get inside your heart, the germs can attach to the lining or get trapped in the valves (the endocardium). They start to grow, causing an infection. Abnormal growths (vegetations) that contain collections of bacteria may form in your heart at the site of the infection and damage the heart valves, which can cause them to leak. If not treated quickly, the infection can cause damage to the heart and lead to serious health problems.
Bacterial endocarditis is an infection of the lining of the heart (the endocardium) caused by various bacteria. The responsible bacteria include various species of staphylococcus, streptococcus, pseudomonas, bartonella and several other organisms. Streptococci (viridans-group streptococci) and staphylococci (Staphylococcus aureus) have collectively accounted for approximately 80% of infective endocarditis cases 33.
Infective endocarditis causes
Endocarditis is usually caused by an infection with bacteria, fungi or other germs. Most of the time, infective endocarditis can be caused by bacteria introduced into the blood stream and travel to the heart. In the heart, they attach to damaged heart valves or damaged heart tissue. Infection can result from many sources, including poor dental hygiene, tooth brushing that causes minor injury to the lining of the mouth or gums, dental procedures, endoscopic examinations, implanted cardiovascular medical devices, chronic skin disorders and infections, burns, infectious diseases, intravenous drug use and more. These bacteria can lodge on heart valves and cause infection of the endocardium. The bacteria rapidly form colonies, grow vegetation and produce enzymes, destroying the surrounding tissue and opening the path for invasion.
Normal heart valves are very resistant to infection. However, bacteria can attach to defects on the surface of diseased heart valves. Replacement heart valves are more prone to infection than normal valves. Bacteria can grow on the heart valves and it is difficult to fight this infection, whether through the body’s own immune system or through medications that rely on the blood system for delivery. This results in complications such as embolization or valve destruction.
Infective endocarditis is primarily an inflammation of the endocardium caused by Gram-positive Streptococci, Staphylococci, and Enterococci bacteria 1. Together, these three groups of bacteria account for 80% to 90% of all infective endocarditis cases, with Staphylococcus aureus specifically responsible for around 30% of cases, while coagulase-negative Staphylococci accounting for ∼11% of cases in the developed world 10, 11, 12. Streptococci, primarily viridans group Streptococci, cause ∼30% of cases, with Streptococcus gallolyticus (a Streptococcus bovis group member) being involved in ∼20% to ∼50% of streptococcal cases 11, 12. Enterococci, especially Enterococcus faecalis, account for ∼10% of cases 11, 12. In addition to various Streptococci, Staphylococci, and Enterococci bacteria, other common colonizers of the oropharynx, such as the Haemophilus aphrophilus, Aggregatibacter actinomycetemcomitans (formerly Actinobacillus actinomycetemcomitans), Cardiobacterium hominis, Eikenella corrodens, Kingella kingae (HACEK organisms) can less frequently be the culprit bacteria 1. Less commonly, non-HACEK Gram-negative bacilli, such as the Enterobacteriaceae and nonfermenting Gram-negative bacilli have been previously identified as well but comprise only about 6% of total cases 13. Fungi are rare endocarditis causes, with Candida and Aspergillus infection in people with weakened immune system (immunocompromised patients) 1. A number of uncultivable or challenging to cultivate organisms cause endocarditis, the most common of which are Coxiella burnetii, Bartonella species, and Tropheryma whipplei 13.
Infective endocarditis most often involves the aortic or mitral valves, with tricuspid valve involvement accounting for fewer than 10% of cases often in association with injection drug use 11, 15, 16. Endocarditis associated with artificial heart valves or cardiovascular implantable electronic devices accounts for approximately one-third of cases and is most commonly caused by staphylococci 11, 16. Coagulase-negative Staphylococci are more frequent causes of prosthetic versus native valve endocarditis, while viridans group Streptococci more commonly cause native than prosthetic valve endocarditis 13. Although the majority of endocarditis cases are community acquired, health care-associated endocarditis is increasing and now accounts for approximately one-third of endocarditis cases in North America 11. Staphylococcus aureus, coagulase-negative Staphylococcus species, and Enterococci are most frequently detected in health care-associated cases 13. Organisms acquired in health care settings are notable for being increasingly resistant to antibacterial agents; methicillin-resistant Staphylococcus aureus (MRSA), for example, is more frequently associated with health care-acquired than community-acquired endocarditis, and most cases of endocarditis caused by non-HACEK Gram-negative bacilli are health care associated 17.
Table 1. Infective Endocarditis Clinical Features According to Causative Organism
| Causative Organism(s) | Clinical Features of infective endocarditis |
|---|---|
| Staphylococcus aureus | Overall, Staphylococcus aureus infection is the most common cause of infective endocarditis, including prosthetic valve endocarditis, acute infective endocarditis, and intravenous drug abuser infective endocarditis. Approximately 35-60.5% of Staphylococcal bacteremias are complicated by infective endocarditis. More than half of cases are not associated with underlying valvular disease. The mortality rate for Staphylococcus aureus infective endocarditis is 40-50%. Staphylococcus aureus infection is the second most common cause of nosocomial bloodstream infections, second only to coagulase-negative staphylococci infection. The incidence of MRSA infections, both the hospital- and community-acquired varieties, has dramatically increased (50% of isolates). Sixty percent of individuals are intermittent carriers of MRSA or MSSA . The primary risk factor for Staphylococcus aureus bloodstream infection is the presence of intravascular lines. Other risk factors include cancer, diabetes, corticosteroid use, intravenous drug abuser, alcoholism, and renal failure. The realization that approximately 50% of hospital- and community-acquired staphylococcal bacteremias arise from infected vascular catheters has led to the reclassification of staphylococcal bloodstream infections. Bloodstream infections are carried not only in the hospital but also in any type of healthcare facility (eg, nursing home, dialysis center). Of Staphylococcus aureus bacteremia cases in the United States, 7.8% (200,000) per year are associated with intravascular catheters. |
| Streptococcus viridans | This organism accounts for approximately 50-60% of cases of subacute disease. Most clinical signs and symptoms are mediated immunologically. Streptococcus gordonii has migrated from Norway to the United States over the last 15 years. It characteristically is associated with a sterile inflammatory response manifest after the bacterial component has been successfully treated. |
| Streptococcus intermedius group | These infections may be acute or subacute. Streptococcus intermedius infection accounts for 15% of streptococcal infective endocarditis cases. Members of the Streptococcus intermedius group, especially Streptococcus anginosus, are unique among the streptococci in that they can actively invade tissue and form abscesses, often in the central nervous system (CNS). |
| Abiotrophia | Approximately 5% of subacute cases of infective endocarditis are due to infection with Abiotrophia species. They require metabolically active forms of vitamin B6 for growth. This type of infective endocarditis is associated with large vegetations that lead to embolization and a high rate of posttreatment relapse. |
| Group D streptococci | Most cases are subacute. The source is the gastrointestinal or genitourinary tract. It is the third most common cause of infective endocarditis. They pose major resistance problems for antibiotics. |
| Nonenterococcal group D | The clinical course is subacute. Infection often reflects underlying abnormalities of the large bowel (eg, ulcerative colitis, polyps, cancer). The organisms are sensitive to penicillin. |
| Group B streptococci | Acute disease develops in pregnant patients and older patients with underlying diseases (eg, cancer, diabetes, alcoholism). The mortality rate is 40%. Complications include metastatic infection, arterial thrombi, and congestive heart failure. It often requires valve replacement for cure. |
| Group A, C, and G streptococci | Acute disease resembles that of S aureus infective endocarditis (30-70% mortality rate), with suppurative complications. Group A organisms respond to penicillin alone. Group C and G organisms require a combination of synergistic antibiotics (as with enterococci). |
| Coagulase-negative S aureus | This causes subacute disease. It behaves similarly to S viridans infection. It accounts for approximately 30% of prosthetic valve endocarditis cases and less than 5% of native valve endocarditis cases. |
| Staphylococcus lugdunensis | Staphylococcus lugdunensis is another coagulase-negative Staphylococcus species but is extremely aggressive compared to coagulase-positive Staphylococcus aureus. Staphylococcus lugdunensis frequently causes infective endocarditis. |
| Pseudomonas aeruginosa | This is usually acute, except when it involves the right side of the heart in intravenous drug abuser infective endocarditis. Surgery is commonly required for cure. |
| HACEK (ie, Haemophilus aphrophilus, Aggregatibacter actinomycetemcomitans (formerly Actinobacillus actinomycetemcomitans), Cardiobacterium hominis, Eikenella corrodens, Kingella kingae) | These organisms usually cause subacute disease. They account for approximately 5% of infective endocarditis cases. They are the most common gram-negative organisms isolated from patients with infective endocarditis. Complications may include massive arterial emboli and congestive heart failure. Cure requires ampicillin, gentamicin, and surgery. |
| Fungal | These usually cause subacute disease. The most common organism of both fungal native valve endocarditis and fungal prosthetic valve endocarditis is Candida albicans. Fungal intravenous drug abuser infective endocarditis is usually caused by Candida parapsilosis or Candida tropicalis. Aspergillus species are observed in fungal prosthetic valve endocarditis and native valve infective endocarditis. Candida auris is progressively contaminating all types of healthcare facilities worldwide |
| Bartonella | The most involved species is Bartonella quintana. Infective endocarditis typically develops in homeless males who have extremely substandard hygiene. Bartonella must be considered in cases of culture-negative endocarditis among homeless individuals. |
| Multiple pathogens (polymicrobial | Pseudomonas and enterococci are the most common combination of organisms . It is observed in cases of intravenous drug abuser infective endocarditis The cardiac surgery mortality rate is twice that associated with single-agent infective endocarditis. |
Risk factors for infective endocarditis
Endocarditis rarely happens in people whose hearts are healthy. Having a faulty, diseased or damaged heart valve increases the risk of endocarditis. However, endocarditis may occur in those without heart valve problems. According to the American Heart Association, about 47,000 people in the United States get an endocarditis diagnosis each year. Historically, infective endocarditis has a tendency for males, with a male to female ratio of nearly 2 to 1 1. The average age of infectious endocarditis patients is now greater than 65 years old 1. This tendency for the elderly likely corresponds to the increased prevalence of risk factors such as prosthetic valves, indwelling cardiac devices, acquired valvular disease, hemodialysis, and diabetes within this age group 22. Although previously a major risk factor, rheumatic heart disease now only affects less than 5% of all cases in the modern antibiotic era 1. Recreational intravenous drug use represents a growing risk factor that now accounts for about 10% of all infectious endocarditis cases 23.
People most at risk of developing bacterial endocarditis include those who have:
- Acquired heart valve disease (for example, rheumatic heart disease) including mitral valve prolapse with valve regurgitation (leaking) and/or thickened valve leaflets.
- An artificial (prosthetic) heart valve, including bioprosthetic and homograft valves. Germs are more likely to attach to an artificial (prosthetic) heart valve than to a regular heart valve.
- Transcatheter aortic valve replacement (TAVR).
- Previous bacterial endocarditis. A history of endocarditis increases the risk of infection.
- Certain congenital (present at birth) heart defects. Being born with certain types of heart defects, such as an irregular heart or damaged heart valves, raises the risk of heart infections.
- Implanted heart device such as a pacemaker or implantable cardioverter-defibrillator (ICD), PICC line or subcutaneous port (e.g., used for chemotherapy) and left ventricular assist device (LVAD). Bacteria can attach to an implanted device, such as a pacemaker, causing an infection of the heart’s lining.
- A suppressed immune system.
- Illegal intravenous drug abuse habit. Using dirty needles can lead to infections such as endocarditis. Contaminated needles and syringes are a special concern for people who use illegal drugs, such as heroin or cocaine.
- Aortic stenosis.
- Hypertrophic cardiomyopathy (HCM).
- Hemodialysis (17 fold increase in endocarditis risk)
- Older age. Endocarditis occurs most often in adults over age 60.
- Recent hospitalization.
- Long-term catheter use. A catheter is a thin tube that’s used to do some medical procedures. Having a catheter in place for a long period of time (indwelling catheter) increases the risk of endocarditis.
- Poor care of the teeth and gums. A healthy mouth and healthy gums are essential for good health. If you don’t brush and floss regularly, bacteria can grow inside your mouth and may enter your bloodstream through a cut on your gums. Some dental procedures that can cut the gums also may allow bacteria to get in the bloodstream.
Native valve endocarditis
The following are the main underlying causes of native valve endocarditis:
- Rheumatic valvular disease (30% of native valve endocarditis) – Primarily involves the mitral valve
- Congenital heart disease (15% of native valve endocarditis) – Underlying causes include a patent ductus arteriosus, ventricular septal defect, tetralogy of Fallot, or any native or surgical high-flow lesion
- Mitral valve prolapse with an associated murmur (20% of native valve endocarditis)
- Degenerative heart disease – Including calcific aortic stenosis resulting from a bicuspid valve, Marfan syndrome, or syphilitic disease
Approximately 70% of infections in native valve endocarditis are caused by Streptococcus species, including Streptococcus viridans, Streptococcus bovis, and enterococci. Staphylococcus species cause 25% of cases and generally demonstrate a more aggressive acute course.
Prosthetic valve endocarditis
Early prosthetic valve endocarditis (PVE), which presents shortly after surgery, has a different bacteriology and prognosis than late prosthetic valve endocarditis, which presents in a subacute fashion similar to native valve endocarditis. Early prosthetic valve endocarditis may be caused by a variety of pathogens, including Staphylococcus aureus and Staphylococcus epidermidis. These hospital-acquired organisms often are methicillin-resistant Staphylococcus aureus (eg, MRSA) 35. Late disease most commonly is caused by Streptococci. Overall, coagulase-negative Staphylococci are the most frequent cause of prosthetic valve endocarditis (30%).
Staphylococcus aureus causes 17% of early prosthetic valve endocarditis and 12% of late prosthetic valve endocarditis.
Corynebacterium, nonenterococcal streptococci, fungi (eg, Candida albicans, Candida stellatoidea, Aspergillus species), Legionella, and the HACEK (ie, Haemophilus aphrophilus, Aggregatibacter actinomycetemcomitans (formerly Actinobacillus actinomycetemcomitans), Cardiobacterium hominis, Eikenella corrodens, Kingella kingae) organisms cause the remaining cases.
Infection associated with aortic valve prostheses is particularly associated with local abscess and fistula formation, and valvular dehiscence. This may lead to shock, heart failure, heart block, shunting of blood to the right atrium, pericardial tamponade, and peripheral emboli to the central nervous system and elsewhere.
Opioid use disorder infective endocarditis
Diagnosis of endocarditis in those who abuse IV drugs can be difficult and requires a high index of suspicion. Two thirds of patients have no previous history of heart disease or murmur on admission. A murmur may be absent in those with tricuspid disease, owing to the relatively small pressure gradient across this valve. Pulmonary manifestations may be prominent in patients with tricuspid infection: one third have pleuritic chest pain, and three quarters demonstrate chest radiographic abnormalities
Staphylococcus aureus is the most common (< 50% of cases) etiologic organism in patients with intravenous drug abuser infective endocarditis. MRSA accounts for an increasing portion of S aureus infections and has been associated with previous hospitalizations, long-term addiction, and nonprescribed antibiotic use. Groups A, C, and G streptococci and enterococci also are recovered from patients with intravenous drug abuser infective endocarditis.
Gram-negative organisms are involved infrequently. Pseudomonas aeruginosa and the HACEK family (Haemophilus aphrophilus, Aggregatibacter actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, Kingella kingae) are the most common examples 36.
Healthcare-associated infective endocarditis
Endocarditis may be associated with therapeutic modalities involving intravascular devices such as central or peripheral intravenous catheters, rhythm control devices such as pacemakers and defibrillators, hemodialysis shunts and catheters, and chemotherapeutic and hyperalimentation lines. These patients tend to have significant comorbidities, more advanced age, and predominant infection with Staphylococcus aureus. The mortality rate is high in this group.
The gram-positive cocci (ie, Staphylococcus aureus, coagulase-negative staphylococci, enterococci, nonenterococcal streptococci) are the most common pathogens of non-nosocomial healthcare-associated infective endocarditis (HCIE). Non-nosocomial healthcare-associated infective endocarditis (HCIE) occurs when patients acquire the infection outside the hospital but following contact with the healthcare system.
Fungal endocarditis
Fungal endocarditis is found in IV drug users and intensive care unit patients who receive broad-spectrum antibiotics 5. Blood cultures may be negative. Microscopic examination of large emboli may detect the organism.
Candida auris is particularly concerning since most infections are recognized in healthcare facilities and can rapidly spread throughout a given facility and between that facility and previously uninfected sites. There were at least 8200 cases in the United States in 2022. Cleaning or disinfecting infected surfaces, including patient’s skin, is ineffective. Candida auris typically is resistant to many antifungals 37, 38.
Culture-Negative Endocarditis
Many cases of culture-negative endocarditis are due to inappropriate institution antibiotics prior to obtaining adequately drawn blood cultures 39. Blood cultures are negative in 2% to 40% of cases of endocarditis, with some studies reporting blood culture-negative rates up to 71% 11, 12, 40, 41. The causes of so-called “culture-negative endocarditis” fall into two categories: negative blood cultures due to concomitant or antecedent antibacterial therapy or the presence of an organism that does not grow in routine blood cultures, with concomitant or antecedent antibacterial therapy being more common 13. Even if considered necessary, antibacterial agents should not be started in patients with suspected endocarditis until after blood cultures have been collected 13. For cases in which antibiotics have been administered prior to blood culture collection, consideration may be given to stopping antibiotics if possible, with recollection of blood cultures after an antibiotic-free period 13. While 7 to 10 days off antimicrobial therapy has been recommended, the ideal length of time needed off therapy is unknown and may vary depending on the infecting organism, antibiotics used, and duration of therapy administered 42. Nevertheless, many patients with bacterial endocarditis receive antibiotics without blood cultures having been appropriately collected, obscuring subsequent microbiologic diagnosis of endocarditis 13.
In patients who have not received antibiotics, the most common causes of culture-negative endocarditis are Coxiella burnetii and Bartonella species, with the former accounting for 28% to 37% and the latter accounting for 12% to 28% of cases 16, 43. Tropheryma whipplei causes up to 6% of cases of culture-negative endocarditis 16, 43, 44. Cutibacterium acnes, a rare cause of endocarditis, may cause culture-negative endocarditis due to the requirement for prolonged blood culture incubation for growth of some strains 45; in addition, some strains may not grow in blood cultures. Mycoplasmal endocarditis, while rare, is primarily caused by Mycoplasma hominis and is usually diagnosed using molecular methods. Traditionally, Mycoplasma pneumoniae has been considered an important cause of culture-negative endocarditis, but reported cases have relied primarily on serologic testing, rendering these historical diagnoses questionable. The incidence of extremely rare causes of endocarditis, such as those caused by Legionella species, Chlamydia/Chlamydophila species, and Mycoplasma species other than M. hominis, is unclear and requires further study, especially in light of evolving diagnostics.
A number of microbiologic tools have been developed to facilitate identification of an infectious agent in patients with suspected endocarditis and negative blood cultures. These technologies should be incorporated into a multimodal strategy to optimize detection of the etiological agent in culture-negative endocarditis.
Infective endocarditis pathophysiology
The intact, healthy endocardium is typically resistant to bacterial seeding and subsequent infection. The development of infectious endocarditis requires previous endocardial injury followed by a period of the presence of bacteria in the blood or bacteremia 1. The preliminary endocardial disruption may emerge secondary to turbulent blood flow around diseased heart valves or from the direct mechanical trauma caused by catheter or electrode insertion 1. In the setting of intravenous drug use, repetitive valvular barrage by co-injected particulate matter generates the necessary injury 21. As evidenced by the preference for growths (vegetations) to form on the ventricular surface of the aortic valve and the atrial surface of the mitral valve, hemodynamics plays an important role in the pathogenesis 1. The growths (vegetations) are localized immediately downstream from regurgitant flow, leading to the hypothesis that hypoperfusion of the intima predisposes these areas to endocardial injury 1. Furthermore, infectious endocarditis is more common with high turbulence lesions such as a small ventricular septal defect with a jet lesion or stenotic valves; presumably, the high-pressure flow creates more local damage than defects associated with large surface areas or low flow 46. The damaged endocardium serves as a source for platelet aggregation and activation of the coagulation cascade, which fosters the formation of a sterile, non-bacterial thrombotic vegetation 47.
Subsequent bacteremia then allows for colonization of the vegetation. The necessary bacteremia can stem from an established, distant source of infection or emerge transiently secondary to intermittent blood inoculation of oral flora from dental or gum manipulation 1. Although the minimum bacterial burden remains unknown, experimental models have precipitated cases of infectious endocarditis with slow 1 mL infusions of 106 colony-forming units (CFU) of bacteria 48. Even in the setting of endocardial injury and bacteremia, pathogenesis still requires a virulent organism capable of binding to and facilitating platelet-fibrin deposits 1. For example, 3 Staphylococcus aureus proteins (clumping factors A, B, and serine-aspartate repeat protein) have been found to independently mediate platelet aggregation 48. In theory, expanding the originally sterile platelet-fibrin deposits protects pathogens from the host’s immune response and allows the vegetation to grow 49.
Mature vegetations consist of an amalgamation of inflammatory cells, fibrin, platelets, and erythrocyte debris 1. The initial platelet-fibrin clot provides a source for bacterial adherence and further platelet aggregation. Confocal laser scanning microscopic analysis of infected valve tissue demonstrates bacterial biofilms embedded with platelet collections. In a self-revolving fashion, platelets facilitate bacterial colonization, which in turn propagates further bacterial aggregation through the binding of surface proteins 50. In the acute setting, vegetations remain avascular; however, once healing commences, neovascularization, fibroblasts, and fibrosis may start to emerge in the affected valve 1.
Both the gross and histologic appearance of valvular tissue will vary based on the infecting organism 1. Virulent pathogens such as Staphylococcus aureus characteristically generate an inflammatory milieu predominated by neutrophils and large bacterial colonies. A macroscopic evaluation may demonstrate friable tissue with frank destruction. The inflammation associated with less virulent organisms such as viridans group streptococci involves more mononuclear cell infiltration 13.
In regard to prosthetic valve endocarditis, one study found that the associated inflammatory cells remain relegated to the vegetation on the surface of the valve cusp. Compared to the inflammatory response that characterizes degenerative valve calcification, prosthetic valve endocarditis primarily involves neutrophilic infiltrates rather than macrophages and lymphocytes 51.
Infective endocarditis prevention
You can take the following steps to help prevent endocarditis:
- Know the signs and symptoms of endocarditis. See your doctor immediately if you develop any symptoms of infection — especially a fever that won’t go away, unexplained fatigue, any type of skin infection, or open cuts or sores that don’t heal properly.
- Take care of your teeth and gums. Brush and floss your teeth and gums often. Get regular dental checkups. Good dental hygiene is an important part of maintaining your overall health.
- Don’t use illegal drugs. Dirty needles can send bacteria into the bloodstream, increasing the risk of endocarditis.
Preventive antibiotics
Certain dental and medical procedures may allow bacteria to enter your bloodstream. If you’re at high risk of endocarditis, the American Heart Association recommends taking antibiotics an hour before having any dental work done 52, 53.
Heart conditions that identify individuals at high-, moderate- or low-risk of developing infective endocarditis 53, 52, 54, 55:
You’re at high risk of endocarditis and need antibiotics before dental work if you have:
- Previous history of infective endocarditis
- Prosthetic cardiac valve including transcatheter valves
- Prosthetic material used for valve repair (including annuloplasty and transcatheter valve procedures using prosthetic material)
- A heart transplant, in some cases
- Unrepaired cyanotic congenital heart disease
- Congenital heart disease surgery in the last six months using palliative shunts or conduits
- Completely repaired congenital heart defect with prosthetic material or device (whether placed by surgical or transcatheter techniques)
- Ventricular assist devices
Antibiotic prophylaxis may be considered in heart transplant recipients
Moderate Risk also known as intermediate risk:
- Rheumatic heart disease
- Non-rheumatic valve disease (including mitral valve prolapse)
- Congenital valve anomalies (including aortic stenosis)
- Patients with cardiac implantable electronic devices (CIED) e.g. pacemaker or defibrillatorb
- Hypertrophic cardiomyopathy
Low risk
- Patients with none of the above high- or moderate-risk conditions
People with the highest risk for bacterial endocarditis need antibiotics before dental visits or certain medical or surgical procedures. You may want to request an endocarditis wallet card from the American Heart Association (https://www.heart.org/-/media/files/health-topics/infective-endocarditis/infective-endocarditis-wallet-card.pdf?la=en). Ask your doctor if you’re part of the highest risk group. If so, let all your healthcare providers know about your risk.
If you’re at high risk of endocarditis, the American Heart Association recommends taking antibiotics an hour before having any dental work done (https://www.heart.org/-/media/files/health-topics/infective-endocarditis/infective-endocarditis-wallet-card.pdf?la=en).
Antibiotic prophylaxis is reasonable before dental procedures that involve manipulation of the gingival tissue, manipulation of the periapical region of teeth, or perforation of the oral mucosa in patients with valvular heart disease who have any of the following (https://www.heart.org/-/media/files/health-topics/infective-endocarditis/infective-endocarditis-wallet-card.pdf?la=en):
- Prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts
- Prosthetic material used for cardiac valve repair, such as annuloplasty rings, chords or clips
- Previous bacterial endocarditis
- Unrepaired cyanotic congenital heart defect (CHD) or repaired congenital heart defect, with residual shunts or valvular regurgitation at the site of or adjacent to the site of a prosthetic patch or prosthetic device*
- A heart transplant with valve regurgitation due to a structurally abnormal valve
*Except for the conditions listed above, antibiotic prophylaxis before dental procedures is not recommended for any other types of congenital heart defect.
So if you have endocarditis or any type of congenital heart disease, talk to your dentist and cardiologist about your risks and whether you need preventive antibiotics before having invasive dental procedures.
It is important to remember that the American Heart Association recommendations are not standards but guidelines, and thus they may be modified in particular circumstances 53. The American Heart Association guidelines remain unproven by randomized controlled clinical trials with many examples of failure of these recommendations have been noted, even when they are applied appropriately 56, 57, 58, 59, 60, 61, 62, 63, 64.
The United Kingdom’s National Institute for Health and Care Excellence (NICE) guidelines on prophylaxis against infective endocarditis differ from the American Heart Association recommendations 65, 52. The NICE guidelines do not recommend antibiotic prophylaxis for infective endocarditis in patients undergoing dental procedures; however, they agree with the American Heart Association guidelines in not recommending prophylaxis for those undergoing procedures in the upper and lower gastrointestinal tracts, the genitourinary tract, or the upper and lower respiratory tracts 65. However, the authors of this Lancet article 53 shows that antibiotic prophylaxis is both safe and effective in reducing the infective endocarditis-risk following invasive dental procedures in those at high-risk. Data also show that antibiotic prophylaxis is cost-effective and would result in significant cost savings and health benefits if re-introduced into the UK’s National Health Service for high-risk patients 53.
In 2023, the European Society of Cardiology (ESC) updated its infective endocarditis guidelines strongly endorsing antibiotic prophylaxis before invasive dental procedures for high-risk patient 66. The American Heart Association is aligned with this view and reaffirmed the need for antibiotic prophylaxis to prevent infective endocarditis in those at high-risk in its 2021 guidelines 52.
Antibiotic Regimens
An antibiotic for prophylaxis should be administered in a single dose before the procedure. If the dosage of antibiotic is inadvertently not administered before the procedure, the dosage may be administered up to 2 hours after the procedure. However, administration of the dosage after the procedure should be considered only when the patient did not receive the pre-procedure dose. Some patients who are scheduled for an invasive procedure may have a coincidental endocarditis. The presence of fever or other manifestations of systemic infection should alert the provider to the possibility of infective endocarditis. In these circumstances, it is important to obtain blood cultures and other relevant tests before administration of antibiotics intended to prevent infective endocarditis. Failure to do so may result in delay in diagnosis or treatment of a concomitant case of infective endocarditis.
Table 2. Antibiotic Regimens for a Dental Procedure
| Situation | Agent | Regimen: Single Dose 30 to 60 min Before Procedure | |
|---|---|---|---|
| Adults | Children | ||
| Oral | Amoxicillin | 2 g | 50 mg/kg |
| Unable to take oral medication | Ampicillin OR Cefazolin or ceftriaxone | 2 g IM or IV | 50 mg/kg IM or IV |
| 1 g IM or IV | 50 mg/kg IM or IV | ||
| Allergic to penicillins or ampicillin—oral | Cephalexin*† OR Clindamycin OR Azithromycin or clarithromycin | 2 g | 50 mg/kg |
| 600 mg | 20 mg/kg | ||
| 500 mg | 15 mg/kg | ||
| Allergic to penicillins or ampicillin and unable to take oral medication | Cefazolin or ceftriaxone† OR Clindamycin | 1 g IM or IV | 50 mg/kg IM or IV |
| 600 mg IM or IV | 20 mg/kg IM or IV | ||
Footnotes:
* Other first- or second-generation oral cephalosporin in equivalent adult or pediatric dosage.
† Cephalosporins should not be used in an individual with a history of anaphylaxis, angioedema, or urticaria with penicillins or ampicillin.
Abbreviations: IM = intramuscular; IV = intravenous.
[Source 67 ]Infective endocarditis signs and symptoms
Symptoms of endocarditis can vary from person to person. Infective endocarditis may develop slowly or suddenly. It depends on the type of germs causing the infection and whether there are other heart problems. The symptoms of acute infective endocarditis usually begin with fever, chills, fast heart rate, fatigue, night sweats, aching joints and muscles, persistent cough or swelling in the feet, legs or abdomen. The symptoms of chronic infective endocarditis may include fatigue, mild fever, a moderately fast heart rate, weight loss, sweating and a low red blood cell count (anemia).
Common symptoms of infective endocarditis include:
- Fever above 100°F (38.4°C).
- Aching joints and muscles
- Chest pain when you breathe
- Fatigue
- Flu-like symptoms, such as fever and chills
- Sweats or chills, particularly night sweats.
- Shortness of breath
- Swelling in the feet, legs or belly
- A new or changed whooshing sound in your heart (heart murmur)
Less common endocarditis symptoms can include:
- Poor appetite or unexplained weight loss
- Blood in the urine
- Tenderness under the left rib cage (spleen)
- Painless red, purple or brown flat spots on the soles bottom of the feet or the palms of the hands (Janeway lesions)
- Painful red or purple bumps or patches of darkened skin (hyperpigmented) on the tips of the fingers or toes (Osler nodes)
- Tiny purple, red or brown round spots on the skin (petechiae), in the whites of the eyes or inside the mouth.
- Wound or cut that won’t heal.
- Red, warm or draining sore.
- Sore throat, scratchy throat or pain when swallowing.
- Sinus drainage, nasal congestion, headaches or tenderness along your upper cheekbones.
- Persistent dry or a moist cough that lasts more than two days.
- White patches in your mouth or on your tongue.
- Nausea, vomiting or diarrhea.
- Emboli (small blood clots), hemorrhages (internal bleeding) or stroke.
Classic findings for endocarditis (<5% sensitive, mostly seen in subacute endocarditis) (Figure 5) 27:
- Splinter hemorrhages.
- Conjunctival petechiae.
- Janeway lesions (painless red/blue macules on palms and soles).
- Osler’s nodes (painful swelling in pulp of fingers).
Left-sided endocarditis signs and symptoms 32:
- Fever above 100°F (38.4°C) (~80% sensitivity)
- Fever plus IV drug use indicates ~15% risk of endocarditis.
- Flu-like, nonspecific illness (e.g., chills, night sweats, headache).
- Heart failure from valve regurgitation (~25%).
- Septic shock (e.g., Staph aureus causing acute bacterial endocarditis).
- Systemic emboli (e.g., ischemic stroke, kidney infarction; 25%):
- Stroke in a young patient is a classic endocarditis presentation.
- Delirium due to multifocal emboli (with no clinically obvious focal neurologic lesion).
Right-sided endocarditis signs and symptoms 32:
- Fever above 100°F (38.4°C).
- Septic pulmonary emboli:
- Will often initially mimic pneumonia (with a constellation of respiratory failure, pulmonary infiltrates, and fever) or pulmonary embolism.
- May eventually lead to hemoptysis, pneumothorax, or empyema.
- The key radiologic finding is multiple pulmonary nodules that eventually cavitate.
Signs of infective endocarditis
There are four peripheral signs of infective endocarditis: Roth spots, Osler nodes, Janeway lesions, and splinter hemorrhages 68. Sandre and Shafran 69 reported the incidence of peripheral signs of endocarditis as follows: 39% for splinter hemorrhages, 6.7% for Osler nodes, 2.2% for Janeway lesions, and 3% for Roth spots. Patients with dermatological manifestations of infective endocarditis have significantly higher complication rates 70.
Osler nodes
Osler nodes also called Osler’s node are red-purple, slightly raised, tender or painful lumps, often with a pale center typically found on the tip of the fingers and/or toes 71, 72, 73. Pain often precedes the development of the visible lesion by up to 24 hours. Osler’s nodes can occur at any time during the course of bacterial endocarditis, usually subacute and last from hours to several days. Osler’s node was first described by William Osler 73.
Figure 6. Osler’s nodes (tender red spots or nodules under the skin of the toes)
Figure 7. Osler nodes and Janeway lesions
Footnote: Osler nodes (black arrow) seen in the palm of the left hand, and Janeway lesions (red arrow) seen on the finger pulp and palm of the left hand.
[Source 74 ]Janeway lesions
Janeway lesions are painless (non-tender) often hemorrhagic (bleeding into the skin) slightly nodular lesions that occur mostly on palms and soles on the thenar and hypothenar eminences (at the base of the thumb and little finger respectively) 75. Janeway lesions tend to last days to weeks before healing totally 76. Janeway lesions are more commonly seen in acute form of bacterial endocarditis, when bacteria such as Staphylococcus aureus may be cultured from them 76. The histology is usually consistent with microabscesses in the dermis (i.e. bacteria may be found within the blood in the capillaries with neutrophil infiltration) with thrombosis of small vessels, without evidence of vasculitis 77, 78, 79. Janeway lesions are associated with embolic events other than cerebral emboli 80.
Figure 8. Janeway lesions (A, Nontender, small purpuric spots on all toes. B, Linear reddish-brown streaks on the distal portions of the nail plates of all fingers)
Figure 9. Janeway lesions (non-tender hemorrhagic macules and papules over the palms and volar aspect of the fingers)
Figure 10. Conjunctival Petechiae
Figure 11. Conjunctival Hemorrhage
Splinter hemorrhages
Splinter hemorrhage in the proximal nail plate is also a sign of bacterial endocarditis. Splinter hemorrhages are small areas of longitudinal bleeding (hemorrhage) under the fingernails or toenails and look like a wood splinter. Seen end-on, splinter hemorrhage is in the lower part of the nail plate or underneath it. Splinter hemorrhages in nails are formed by the hemorrhage of blood from the rupture of the longitudinally oriented blood vessels of the nail bed. Splinter hemorrhages look like thin, red to reddish-brown lines of blood under the nails. Splinter hemorrhages run in the direction of nail growth. The underlying blood will attach to the nail plate and seems to move up as the nail grows. Splinter hemorrhages can be single or multiple.
Figure 12. Splinter hemorrhage with bacterial endocarditis
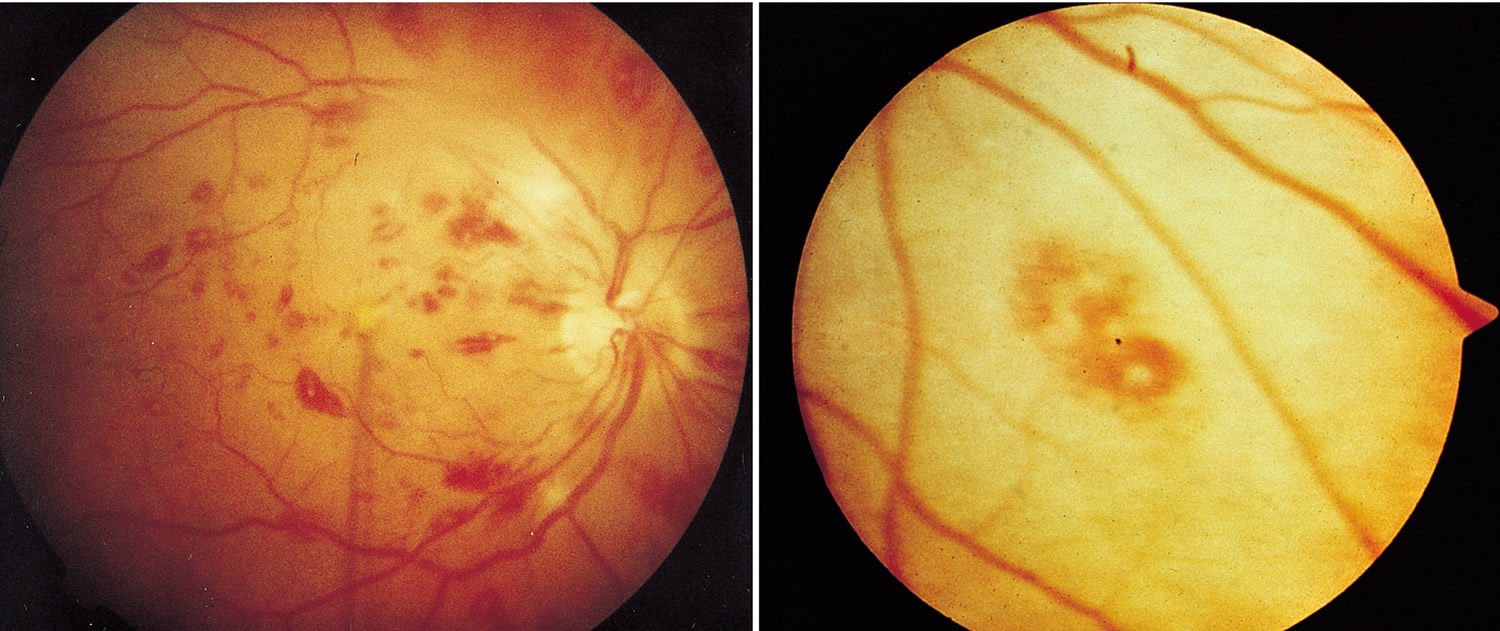
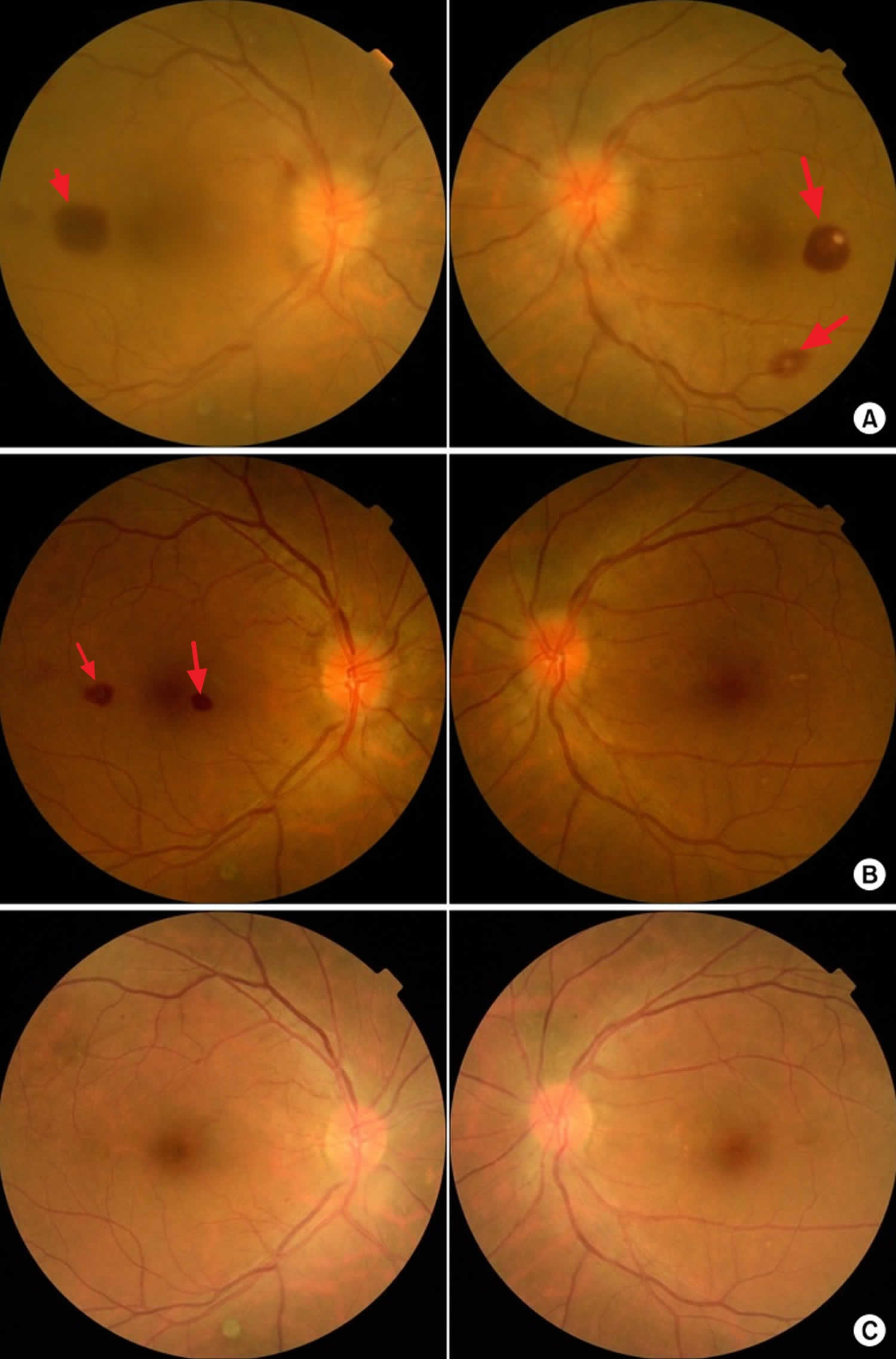
Roth spots
Roth spots appear as white-centered retinal hemorrhages on a fundoscopic examination 81, 82, 82. The white center of a Roth spot is thought to be a platelet-fibrin plug 83, 84, 84. These platelet-fibrin plugs presumably form in response to vascular leaks brought about by elevated intravascular pressure, ischemia, increased capillary fragility, or combinations thereof 84. In most cases, emboli appear to play no role 85. Although Roth spots are a classic peripheral sign of endocarditis, they are also present in other conditions, including hematologic malignancies, connective tissue diseases, vasculitis, anemia, hypertension, diabetes mellitus, human immunodeficiency virus infections, and intracranial hemorrhages 85.
Figure 13. Infective Endocarditis – Retinal Roth Spots (retinal hemorrhages) – image on the right is a close up image of a Roth spot showing a central clearing
Figure 14. Roth spots
Footnote: Fundoscopic findings of Roth spots. (A) Preoperative findings. (B) 2 weeks postoperatively. (C) 6 weeks postoperatively.
[Source 83 ]Infective endocarditis complications
In endocarditis, irregular growths made of germs and cell pieces form a mass in the heart called vegetations can break loose and travel to your brain, lungs, kidneys and other organs. They can also travel to the arms and legs.
Most common complications of infective endocarditis may include:
- Heart failure
- Heart valve damage
- Ischemic stroke
- Pockets of collected pus (abscesses) that develop in the heart, brain, lungs and other organs
- Blood clot in a lung artery (pulmonary embolism)
- Kidney damage and failure
- Enlarged spleen
- Interstitial bleeding
- Septic shock
Infective endocarditis diagnosis
To diagnose endocarditis, your doctor will asks questions about your medical history and symptoms and do a physical exam. Tests are also done to help confirm or rule out endocarditis.
Tests used to help diagnose endocarditis include:
- Blood culture test. This test helps identify germs in the bloodstream. Results from this test help determine the antibiotic or combination of antibiotics to use for treatment.
- Complete blood count. This test can determine if there’s a lot of white blood cells, which can be a sign of infection. A complete blood count can also help diagnose low levels of healthy red blood cells (anemia), which can be a sign of endocarditis. Other blood tests also may be done.
- Echocardiogram. Sound waves are used to create images of the beating heart. This test shows how well the heart’s chambers and valves pump blood. It can also show the heart’s structure. Your provider may use two different types of echocardiograms to help diagnose endocarditis.
- In a standard (transthoracic) echocardiogram (TTE), a wandlike device (transducer) is moved over the chest area. The device directs sound waves at the heart and records them as they bounce back.
- In a transesophageal echocardiogram (TEE), a flexible tube containing a transducer is guided down the throat and into the tube connecting the mouth to the stomach (esophagus). A transesophageal echocardiogram provides much more detailed pictures of the heart than is possible with a standard echocardiogram.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. During an electrocardiogram (ECG), sensors (electrodes) are attached to the chest and sometimes to the arms or legs. It isn’t specifically used to diagnose endocarditis, but it can show if something is affecting the heart’s electrical activity.
- Chest X-ray. A chest X-ray shows the condition of the lungs and heart. It can help determine if endocarditis has caused heart swelling or if any infection has spread to the lungs.
- Computerized tomography (CT) scan or magnetic resonance imaging (MRI). You may need scans of your brain, chest or other parts of your body if your provider thinks that infection has spread to these areas.
Duke Criteria for daignosing endocarditis
The Duke criteria are used to rule in or rule out endocarditis. In 1994, a group at Duke University proposed standardized criteria for assessing patients with suspected infective endocarditis 86. The Duke criteria combine the clinical, microbiologic, pathologic, and echocardiographic findings of a specific case 86. The usefulness of Duke criteria in assessing patients with potential infective endocarditis has been validated in several subsequent studies 28, 87, 88, 89, 90, 91, 92, 93, 94, 95. The specificity of the initially proposed Duke criteria (the ability to reject the diagnosis correctly) was high 95 and the negative predictive value was greater than 92 percent 96. Also, a retrospective study of 410 patients with diagnosed endocarditis found that the Duke criteria had good (72 to 90 percent) agreement with clinical assessment by infectious-disease experts 93. Most discrepancies occurred when the experts rejected cases categorized as possible endocarditis according to the Duke criteria. Misclassification of culture-negative cases, the increasing role of transesophageal echocardiography, the relative risk of endocarditis in Staph. aureus bacteremia, and the overly broad categorization of cases as “possible” were problems with the original criteria. A modified version of the Duke criteria has recently been proposed 97.
Duke criteria for diagnosing infective endocarditis 28:
Major criteria
- Blood culture typical of infective endocarditis, single positive culture for C. burnetti, or immunoglobulin G antiphase 1 level of ≥1/800. Major blood culture criteria for infective endocarditis include the following:
- 2 blood cultures positive for organisms typically found in patients with infective endocarditis
- Blood cultures persistently positive for 1 of these organisms, from cultures drawn more than 12 hours apart
- Three or more separate blood cultures drawn at least 1 hour apart
- Echocardiogram positive for infective endocarditis. Major echocardiographic criteria include the following:
- Echocardiogram positive for infective endocarditis, documented by an oscillating intracardiac mass on a valve or on supporting structures, in the path of regurgitant jets, or on implanted material, in the absence of an alternative anatomic explanation
- Myocardial abscess
- Development of partial dehiscence of a prosthetic valve
- New-onset valvular regurgitation
Minor criteria
- Predisposing heart condition or injection drug use
- Fever (temperature of >100.4°F [>38°C])
- Vascular phenomena, including major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage, or Janeway lesions
- Immunologic phenomena such as glomerulonephritis, Osler nodes, Roth spots, or rheumatoid factor
- Positive blood culture results not meeting major criteria or serologic evidence of active infection with an organism consistent with infective endocarditis
- Echocardiogram results consistent with infective endocarditis but not meeting major echocardiographic criteria
Definite endocarditis
- (i) 2 major clinical criteria OR
- (ii) 1 major clinical criterion and 3 minor clinical criteria OR
- (iii) 5 minor clinical criteria
Possible endocarditis
- (i) 1 major clinical criterion and 1 minor clinical criterion OR
- (ii) 3 minor clinical criteria
Rejected endocarditis
- (i) Firm alternative diagnosis is made explaining evidence of infective endocarditis;
- (ii) Resolution of infective endocarditis syndrome with antibiotic therapy for ≤4 days ;
- (iii) No pathologic evidence of infective endocarditis at surgery or autopsy, with antibiotic therapy for ≤4 days;
- (iv) Fail to meet criteria for for possible or definite infective endocarditis
Peripheral blood cultures
Since endocarditis is associated with the persistent presence of infecting microorganisms in your blood, for this reason, blood cultures is the single most important test to order for suspected endocarditis to find the germs in the bloodstream that is causing infective endocarditis. Cultures must be obtained prior to starting antibiotics in suspected endocarditis, even if this causes a short treatment delay.
Routine blood cultures incubated on modern automated, continuous-monitoring blood culture systems allow recovery of almost all easily cultivable agents of endocarditis without additional specialized testing, such as prolonged incubation or terminal subculture. Recommendations regarding the number and timing of blood cultures differ by guideline set.
- The American Heart Association and the European Society of Cardiology recommend at least 3 sets of blood cultures collected from different venipuncture sites, with at least 1 hour between the first and last draw 29, 15.
- The British Society for Antimicrobial Chemotherapy (BSAC) recommends collection of 2 sets of blood cultures within 1 hour of each other in patients with suspected endocarditis and acute sepsis and 3 sets of blood cultures spaced ≥6 hours apart in cases of suspected subacute or chronic endocarditis 42.
3 sets of blood cultures, with each set including one aerobic and one anaerobic bottle, are collected. Alternatively, 2 sets may be collected, with 2 aerobic and 1 anaerobic bottle per set (i.e., a total of six blood culture bottles) 98. Yield of blood cultures is directly related to volume of blood cultured, with properly filled blood culture bottles (i.e., 10 ml of blood per Bactec or BacT/Alert bottle) being essential. Most, if not all, blood cultures from patients with endocarditis caused by microorganisms able to grow in blood culture systems should be positive, provided that blood cultures are appropriately collected and drawn prior to the administration of antimicrobial therapy; a single positive blood culture does not typically represent an endocarditis pathogen. Although the concept of spacing blood culture draws to detect continuous bacteremia is promulgated in the above-referenced guidelines, separation of blood culture draws over time is not the norm for routine blood culture draws. We are not aware of evidence supporting the value of spaced blood culture draws for etiologic diagnosis of endocarditis; for these reasons, we do not recommend routinely spacing blood culture draws in cases of suspected endocarditis.
Standard blood culture incubation times of 5 days are adequate for recovery of almost all cultivable causes of endocarditis, including Candida species. The Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, and Kingella species (HACEK organisms) were classically considered challenging to detect in blood cultures due to their fastidious nature; accordantly, in the past, prolonged incubation times were advised. With current blood culture systems, extended incubation (and terminal blind subculture) is unnecessary for recovery of these organisms, as they are easily grown and detected within the standard 5-day incubation period 99, 100. Current blood culture systems also contain sufficient supplements to support growth of Abiotrophia and Granulicatella species (nutritionally variant streptococci). Brucella species are infrequent causes of endocarditis in the United States, and detection in routine blood cultures is typically achieved within the standard 5-day incubation period 101; serologic testing may be helpful if exposures are suggestive of Brucella endocarditis. Cutibacterium (formerly Propionibacterium) acnes deserves special consideration, however, as some strains of this species may require prolonged blood culture incubation (e.g., 14 days) 45. The Clinical and Laboratory Standards Institute (CLSI) guidelines recommend terminal subculture to chocolate agar if blood cultures are negative at 5 days and an endocarditis diagnosis is under consideration 102. However, current evidence fails to support the usefulness of blind subculture, and this practice is not recommended in the British Society for Antimicrobial Chemotherapy (BSAC) guidelines 42, 103. Fungal endocarditis is most commonly caused by Candida species, which should grow in routine blood cultures. Noncandidal fungal causes of endocarditis (e.g., Histoplasma capsulatum, Aspergillus species) are rare, require specialized testing (e.g., antigen detection, specialized fungal blood cultures), and should only be considered in patients with specific risks for these types of endocarditis (e.g., malignancy, injection drug use, prolonged health care exposure, presence of a prosthetic heart valve) after more common causes have been excluded 13.
Number of cultures:
- One “set” of cultures = two bottles (anaerobic & aerobic) drawn from a single location.
- Ideally three sets should be obtained from three different locations (two sets are OK if this isn’t possible).
Location of cultures:
- Ideally cultures should be obtained from a fresh peripheral stick.
- If this isn’t feasible, obtain blood wherever you can get it. For example, obtaining blood from a freshly placed central line is OK.
Timing
- In endocarditis, bacteremia is generally constant, so there is little rationale to space cultures out over time.
- Don’t worry about the timing of cultures – the key thing is to get a lot of cultures and fill the culture bottles fully. (Get a lot of blood; more blood removed = higher likelihood of capturing a causative pathogen).
Serologic testing
For organisms that do not grow in routine bacterial cultures (e.g., Coxiella burnetii) or are especially fastidious (e.g., Bartonella species), serologic evaluation may aid in diagnosis. In one study, when evaluated in conjunction with blood cultures, systematic serologic testing established an etiological diagnosis in an additional 8% (34/425) of patients 12. In a separate investigation focused on culture-negative endocarditis, serology provided a diagnosis in 77% (268/348) of cases 43. Organisms for which serologic tests have been shown to aid in the diagnosis of endocarditis include Coxiella burnetii and Bartonella species and, in areas where Brucella endocarditis occurs, Brucella species. Generally, these pathogens cause subacute endocarditis resulting in elevated IgG titers. Serology for Coxiella burnetii is the best established serologic test for the diagnosis of endocarditis and is included as a major criterion in the modified Duke criteria 29, 31. In chronic Q fever with endocarditis, anti-phase I IgG Coxiella burnetii titers of ≥1:800 are diagnostic. Aside from that for Coxiella burnetii, specific serological criteria for the diagnosis of endocarditis have not been incorporated into the modified Duke criteria, although Bartonella endocarditis is often diagnosed by serologic testing. Dependence on antibody detection for etiological diagnosis of endocarditis may be complicated by serologic cross-reactivity; most notably, Chlamydia or Chlamydophila serologic assays demonstrate high level cross-reactivity with Bartonella species, possibly leading to erroneous diagnoses of chlamydial endocarditis 104. Low-level cross-reactivity has also been demonstrated between Bartonella and Coxiella, although in cases of endocarditis, antibody titers against the “true” agent are typically more elevated than those against the cross-reacting organism. Seroreactivity resulting from prior exposure to organisms unrelated to the episode of endocarditis under evaluation may confound interpretation. Serologic testing for extremely rare causes of endocarditis (e.g., Legionella species, Chlamydia/Chlamydophila species) is not recommended due to challenges with falsely positive results 13.
Other lab tests
- Urinalysis consistent with glomerulonephritis is seen in ~60% of patients (proteinuria, microscopic hematuria).
- Rheumatoid factor (may help satisfy the diagnostic criteria for endocarditis).
- Acute-phase reactants (C-reactive protein):
- More than 95% sensitive for endocarditis.
- May be useful for subsequent follow-up, to help determine if the infection is responding to therapy.
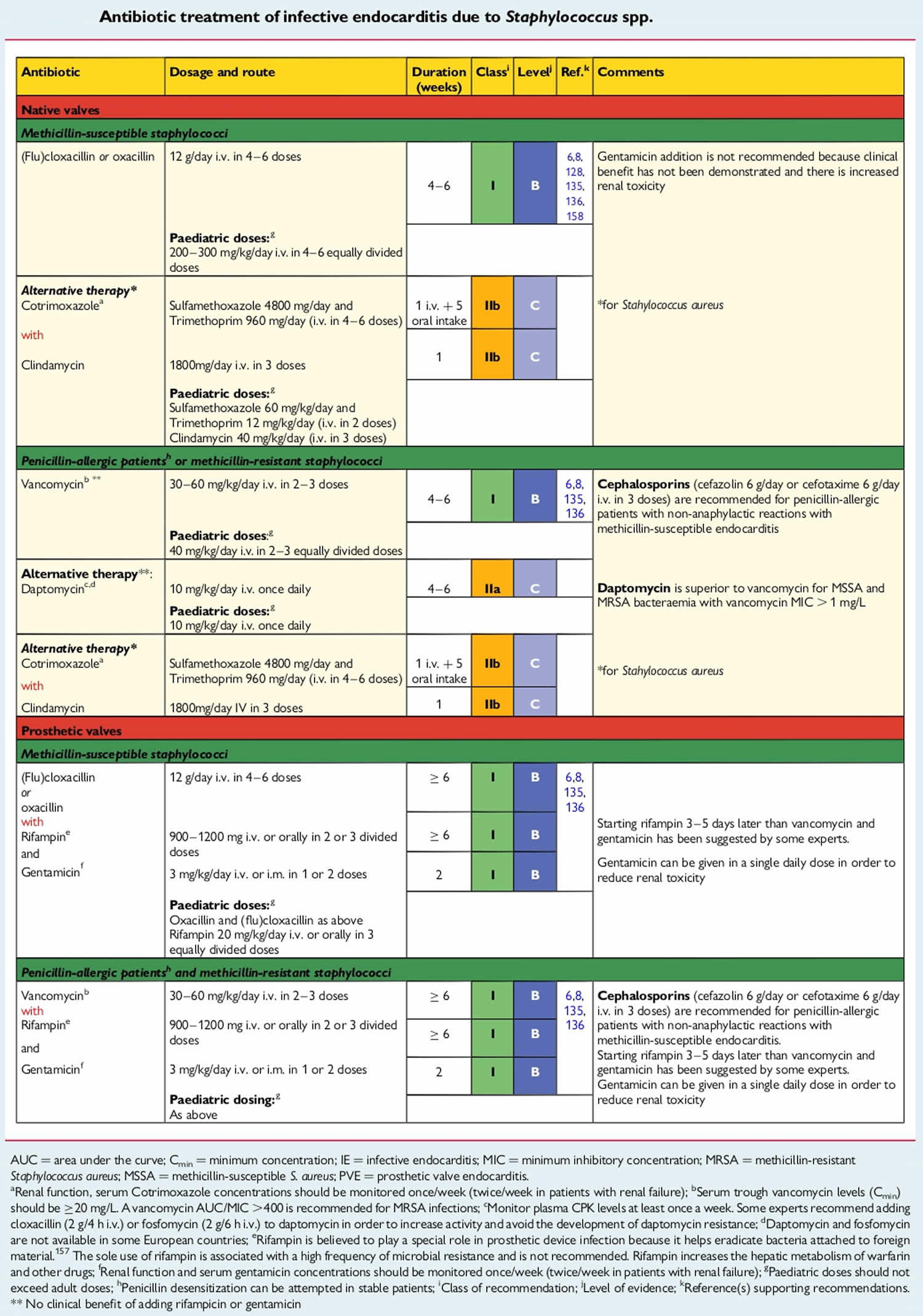
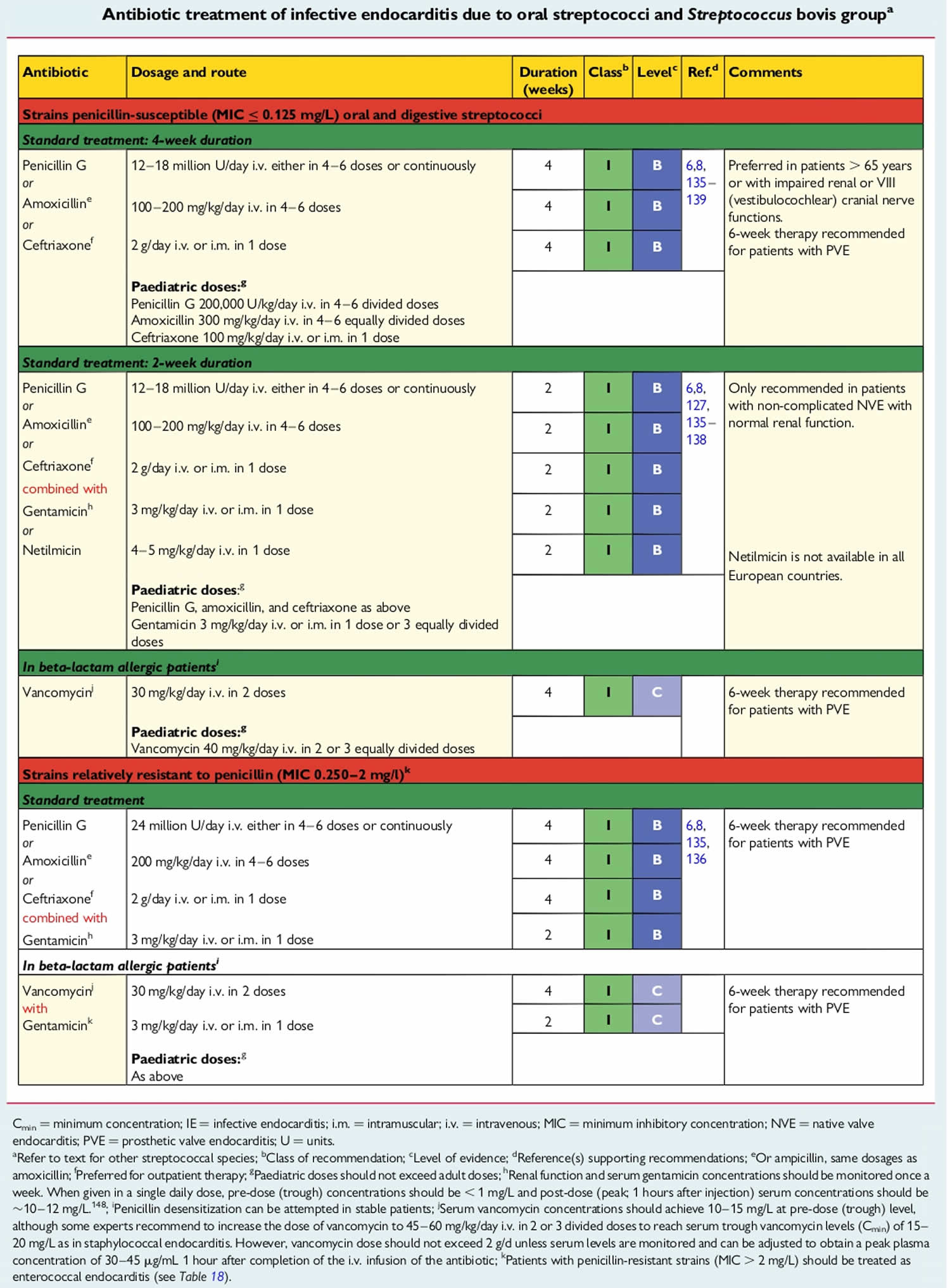
Infective endocarditis treatment
Infective endocarditis treatment usually consists of IV antibiotics. The choice of antibiotic and the length of treatment is based on the type of germs causing your endocarditis. Sometimes, surgery may be needed to fix or replace damaged heart valves and clean up any remaining signs of the infection.
Infective endocarditis medications
The type of medication you receive depends on what’s causing your endocarditis. High doses of antibiotics are used to treat endocarditis caused by bacteria. If you receive antibiotics, you’ll generally spend a week or more in the hospital so that care providers can determine if the treatment is working.
Once your fever and any severe symptoms have gone away, you might be able to leave the hospital. Some people continue antibiotics with visits to a provider’s office or at home with home care. Antibiotics are usually taken for several weeks.
If endocarditis is caused by a fungal infection, antifungal medication is given. Some people need lifelong antifungal pills to prevent endocarditis from returning.
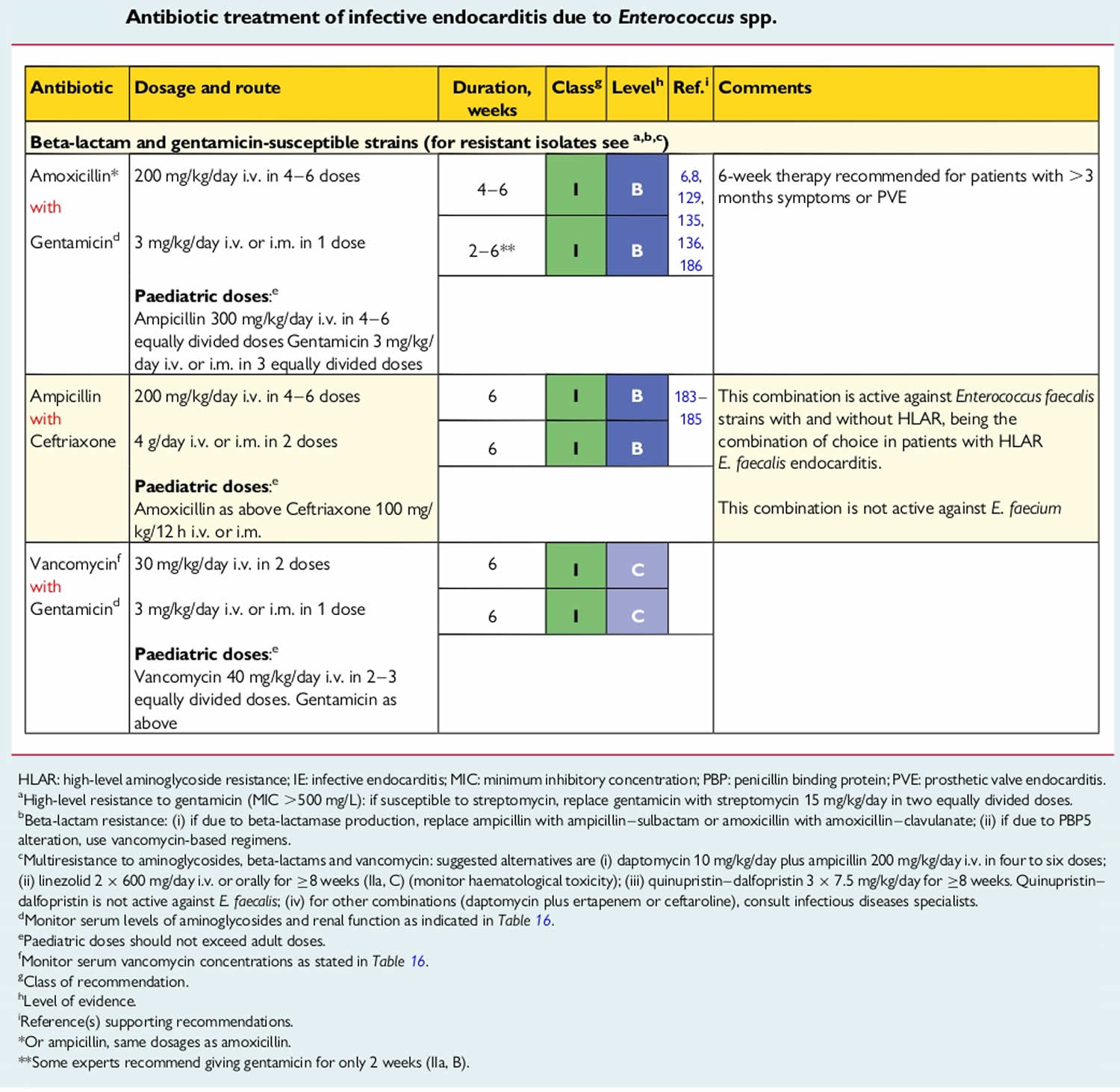
Figure 6. Staphylococcus endocarditis antibiotics
[Source 105 ]Figure 7. Streptococcus endocarditis antibiotics
[Source 105 ]Figure 8. Enterococcus endocarditis antibiotics
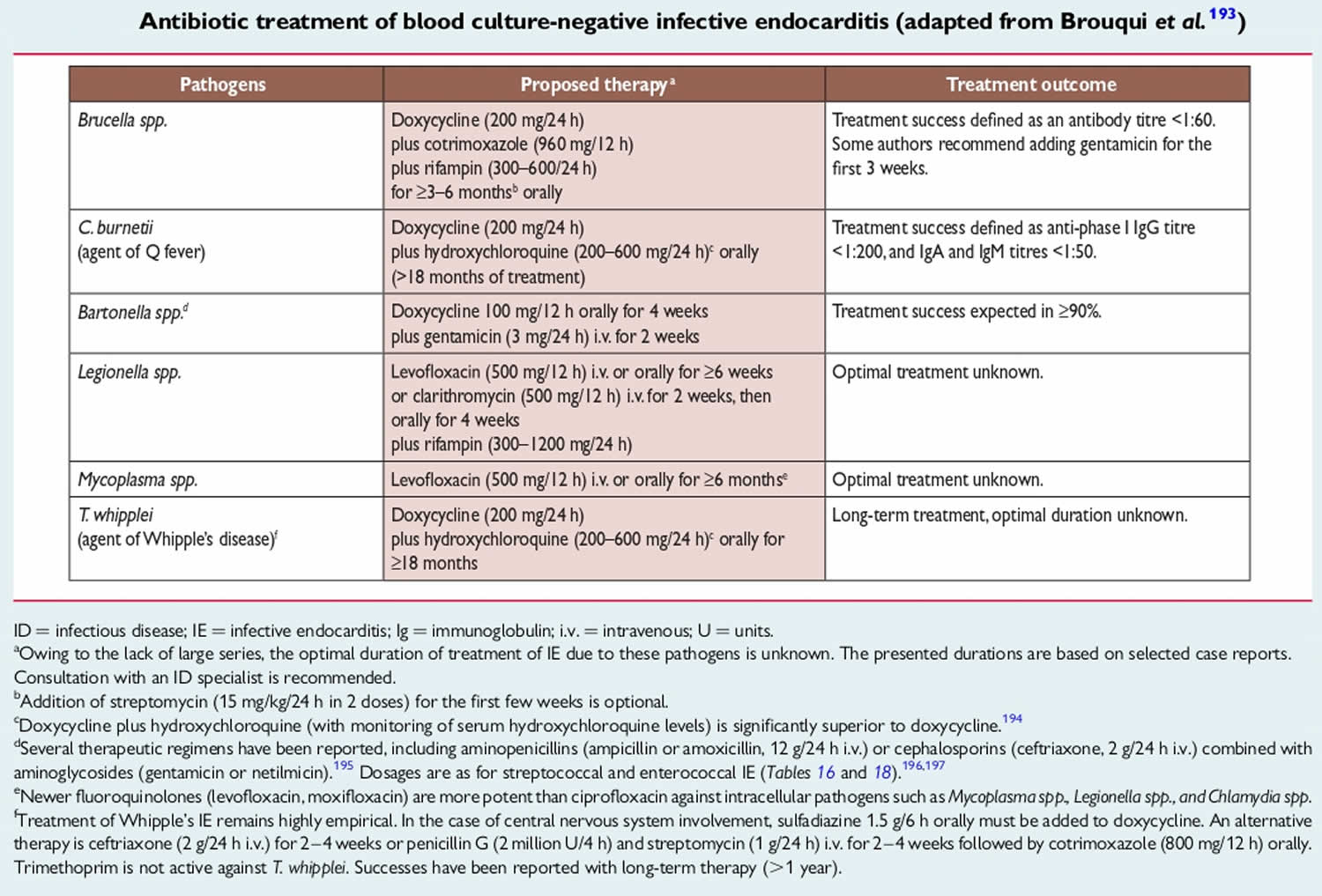
[Source 105 ]Figure 9. Culture-negative infective endocarditis antibiotics
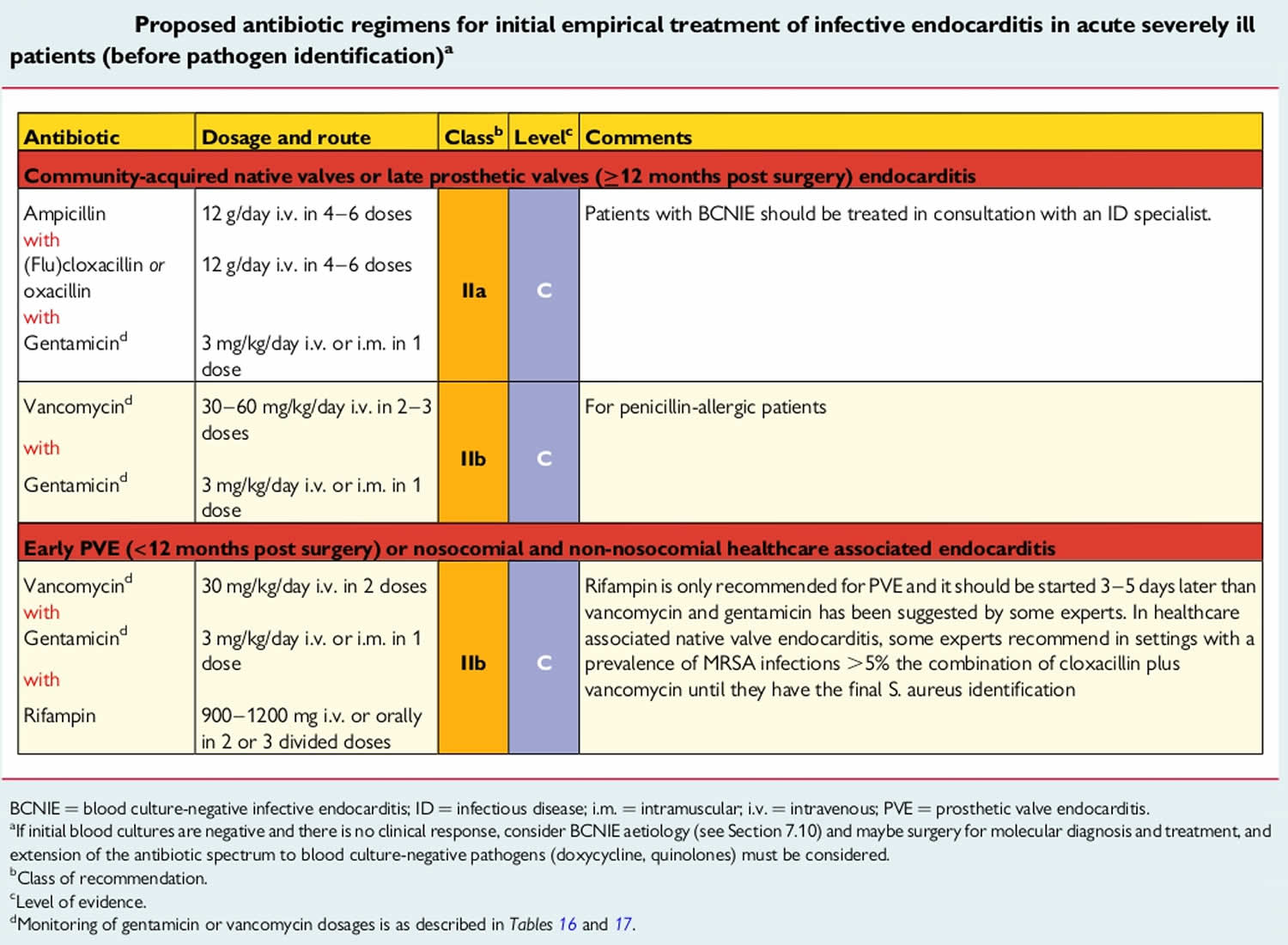
[Source 105 ]Figure 10. Infective endocarditis in acute severely ill patients antibiotic regimens before pathogen identification of pathogen
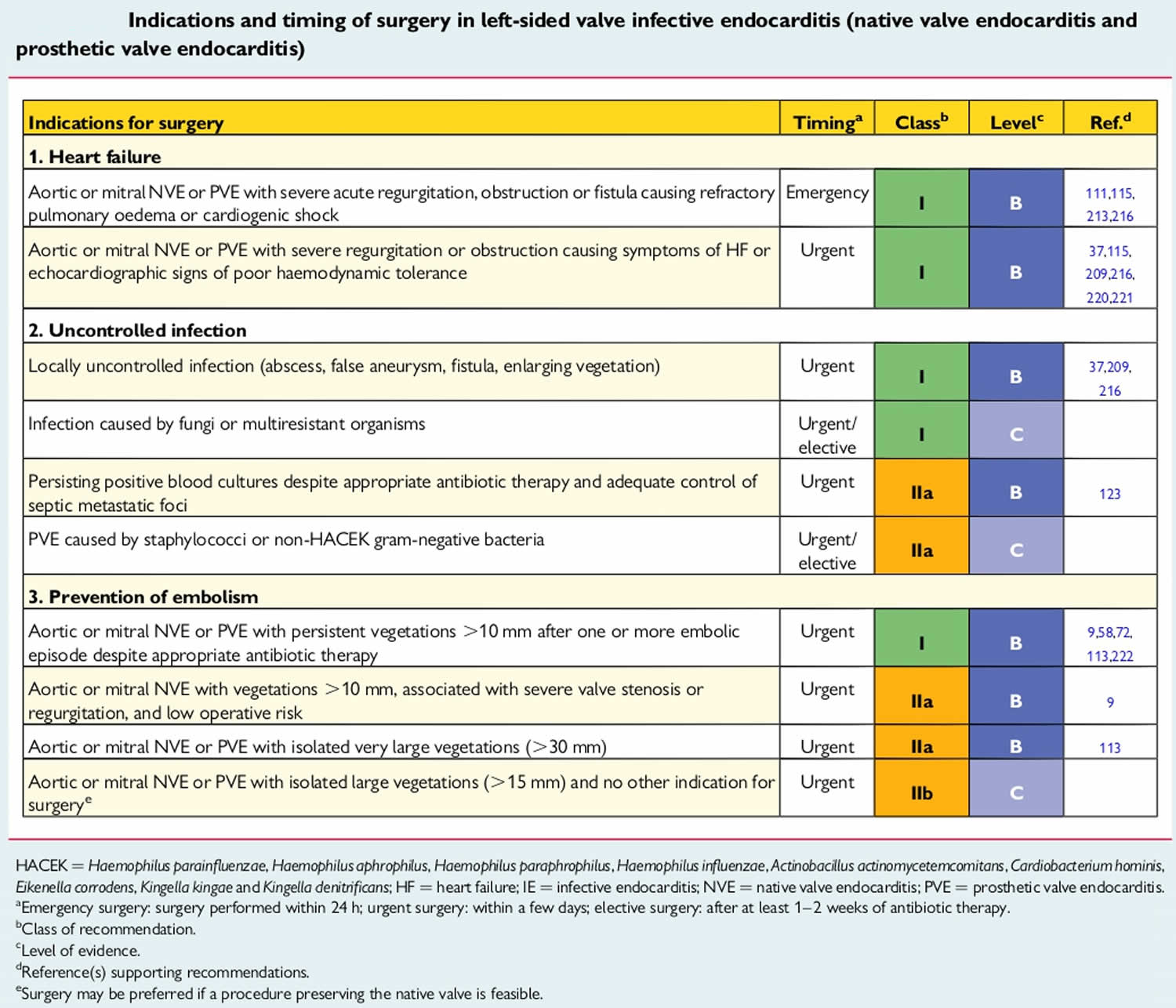
[Source 105 ]Infective endocarditis surgery or other procedures
Heart valve surgery may be needed to treat persistent endocarditis infections or to replace a damaged valve. Surgery is sometimes needed to treat endocarditis that’s caused by a fungal infection.
Depending on your condition, your doctor may recommend either repairing your damaged valve or replacing it with an artificial valve made of cow, pig or human heart tissue (biological tissue valve) or man-made materials (mechanical valve).
The three main surgical procedures that are used to treat endocarditis are:
- Repair of the damaged heart valve
- Replacement of the damaged heart valves with prosthetic ones
- Draining of any abscesses and the repair of any fistulas that may have developed in the heart muscle
Surgery for endocarditis can be very challenging, not least because a person who needs surgery will usually be very ill to begin with. Despite the best efforts of their surgical teams, approximately one in 10 people will die during or shortly after surgery for endocarditis.
The principal consensus indications for valve surgery are heart failure, uncontrolled infection and prevention of embolic events in patients at high risk 106. Uncontrolled infection may be related to paravalvular complications, such as abscess, an enlarging vegetation or dehiscence of a prosthetic valve. In addition, uncontrolled infection may be manifested by ongoing systemic illness with persistent fevers and positive blood cultures despite appropriate antibiotic therapy. As larger left-sided vegetations are more likely to lead to embolic events, infective endocarditis with a vegetation of >10 mm in length is a relative indication for surgical intervention.
The timing of cardiac surgery for patients with infective endocarditis and neurovascular complications remains controversial. A large prospective cohort study of 857 patients with infective endocarditis complicated by ischemic stroke without hemorrhagic conversion found that no patient benefit was gained from delaying surgery 107. By contrast, patients with embolic stroke complicated by hemorrhagic conversion sustained higher mortality when surgery was performed within 4 weeks of the hemorrhagic event compared with later surgery (75% versus 40%, respectively) 108. On the basis of these observational data, the American Heart Association 109 currently recommends that valve surgery may be considered in patients with infective endocarditis who also have stroke or subclinical cerebral emboli without delay if intracranial hemorrhage has been excluded by imaging studies and neurological damage is not severe (such as coma). In patients with major ischemic stroke or intracranial haemorrhage, American Heart Association guidelines currently state that delaying valve surgery for at least 4 weeks is reasonable 109.
Valve surgery was traditionally recommended for difficult-to-treat pathogens such as Pseudomonas aeruginosa, fungal organisms and β-lactam resistant staphylococci. However, these pathogen-specific recommendations for surgery have been recently called into question in favor of an individualized decision-making approach based upon hemodynamic and structural indications 110.
Figure 11. Indications and timing of surgery in left-sided valve infective endocarditis (native valve endocarditis and prosthetic valve endocarditis)
[Source 105 ]Other add-on therapies
Anticoagulation
Patients with prosthetic valve infective endocarditis who are receiving oral anticoagulants may be at an increased risk of death from cerebral hemorrhage 111. Antiplatelet therapies are not currently recommended for infective endocarditis. A single randomized trial examined the role of 325 mg of aspirin daily for patients with infective endocarditis. The incidence of embolic events was similar in between aspirin- and placebo-treated patients, and there was a non-significant increase in the rate of cerebral bleeding episodes 112. There are several limitations to this study, however, that include dose of aspirin used and delayed initiation of aspirin. For patients with another indication for antiplatelet therapy, it may be reasonable to continue the antiplatelet agent unless bleeding complications develop. Similarly, it is not recommended to initiate anticoagulant therapy such as warfarin for the purpose of treating infective endocarditis. In patients with infective endocarditis who have another indication for anticoagulation therapy, such as a mechanical valve, data are contradictory on whether to continue anticoagulation during acute therapy 111 and bridging therapy with heparin products has not been studied.
Management of metastatic foci
Metastatic foci of infection frequently complicate infective endocarditis. As with any infection, recognition of these foci of infection is important so that targeted interventions, such as drainage of abscesses or removal of infected prosthetic material, may be undertaken. This is of critical importance in patients who require valve surgery because a persistent source of infection may serve as a source from which a recently placed prosthetic valve or annuloplasty ring becomes infected 109. Some metastatic foci, such as vertebral osteomyelitis, may require additional antibiotic therapy beyond what is typically indicated for infective endocarditis 113. There is currently insufficient evidence to recommend specific imaging strategies to look for metastatic foci in all patients with infective endocarditis.
Neurological complications of infective endocarditis treatment
Symptomatic neurological complications occur in 15–30% of patients with infective endocarditis and are mainly the consequence of embolism from vegetations 114, 115, 116. Neurological manifestations occur before or at infective endocarditis diagnosis in a majority of cases, but new or recurrent events can also take place later in the course of infective endocarditis. Clinical presentation is variable and may
include multiple symptoms or signs in the same patient, but focal signs predominate and ischemic strokes are most commonly diagnosed. Transient ischemic attack, intracerebral or subarachnoidal hemorrhage, brain abscess, meningitis and toxic encephalopathy are also seen, and firm evidence supports that additional clinically silent cerebral embolisms occur in 35–60% of infective endocarditis patients 117, 118, 119.
Staphylococcus aureus infective endocarditis is more frequently associated with neurological complications compared with infective endocarditis caused by other bacteria. Vegetation length and mobility also correlate with embolic tendency 120, 121. Neurological complications are associated with an excess mortality, as well as complications, particularly in the case of stroke 115, 116. Rapid diagnosis and initiation of appropriate antibiotics are of major importance to prevent a first or recurrent neurological complication 122. Early surgery in high-risk patients is the second mainstay of embolism prevention, while antithrombotic drugs have no role.
Figure 12. Neurological complications of infective endocarditis treatment
[Source 105 ]Infective endocarditis prognosis
Without treatment, infective endocarditis is a fatal disease. Early detection and appropriate treatment of this endocarditis can be lifesaving. However, despite recent advances in diagnostic and treatment strategies for infective endocarditis, 1 year mortality has not improved and remains at 30%, which is worse than for many cancers 21, 29, 30. Infective endocarditis prognosis largely depends on whether you develop any complications 123. Increased mortality rates are associated with older age, infection involving the aortic valve, development of congestive heart failure, central nervous system complications, and underlying disease such as diabetes mellitus. Catastrophic neurological events of all types resulting from infective endocarditis are highly predictive of morbidity and mortality.
Predictors of poor outcome in patients with infective endocarditis 105:
- Patient characteristics
- Older age
- Prosthetic valve endocarditis
- Diabetes mellitus
- Comorbidity (e.g., frailty, immunosuppression, kidney or lung disease)
- Clinical complications of endocarditis
- Heart failure
- Kidney failure
- Moderate area of ischemic stroke
- Brain hemorrhage
- Septic shock
- What type of organism made you sick
- Staphylococcus aureus
- Fungi
- Non-HACEK Gram-negative bacilli
- Echocardiographic findings
- Periannular complications
- Severe left-sided valve regurgitation
- Low left ventricular ejection fraction
- Pulmonary hypertension
- Large vegetations
- Severe prosthetic valve dysfunction
- Premature mitral valve closure and other signs of elevated diastolic pressures.
Cure rates for appropriately managed (including both medical and surgical therapies) native valve endocarditis are as follows 123:
- For Streptococcus viridans and Streptococcus bovis infection, the rate is 98%.
- For enterococci and Staphylococcus aureus infection in individuals who abuse intravenous drugs, the rate is 90%.
- For community-acquired Staphylococcus aureus infection in individuals who do not abuse intravenous drugs, the rate is 60-70%.
- For infection with aerobic gram-negative organisms, the rate is 40-60%.
- For infection with fungal organisms, the rate is lower than 50%.
For prosthetic valve endocarditis, the cure rates are as follows 123:
- Rates are 10-15% lower for each of the above categories, for both early and late prosthetic valve endocarditis.
- Surgery is required far more frequently.
- Approximately 60% of early coagulase-negative Staphylococci prosthetic valve endocarditis cases and 70% of late coagulase-negative Staphylococci prosthetic valve endocarditis cases are curable.
The overall mortality rate has remained stable at 14.5% and there has been no overall improvement in outcomes of infective endocarditis of congenital heart disease 123. The in-hospital mortality rate hovers around 18%, with one-year mortality reaching up to 40% 124. Mortality rates in native valve endocarditis range from 16-27%, and mortality rates in patients with prosthetic valve endocarditis are higher. More than 50% of these infections occur within 2 months after surgery. The fatality rate of pacemaker infective endocarditis ranges up to 34% 121, 125, 126, 127, 128.
In general, cases of artificial (prosthetic) valve endocarditis occurring within the first 60 days of surgery demonstrate the highest in-hospital mortality rates of about 30%. A large, Japanese prospective cohort study found a Staphylococcal infection and heart failure to be the greatest predictors of in-hospital mortality 129. Although nearly 50% of infectious endocarditis cases now undergo surgical intervention, in of itself, the surgical intervention does not appear to elevate the in-hospital mortality risk 11. The largest study to date indicates that in cases of infective endocarditis complicated by heart failure, valvular surgery reduces the 1-year mortality rate. More recent studies document that early surgery in patients, especially those with large vegetations, significantly reduces the risk for death from any cause 130, 131, 132, 133.
Mortality rates also vary with the infecting organism. Acute endocarditis caused by Staphylococcus aureus is associated with a high mortality rate (30-40%), except when it is associated with IV drug use 134, whereas infective endocarditis resulting from Streptococci has a mortality rate of approximately 10% 135.
- Yallowitz AW, Decker LC. Infectious Endocarditis. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557641[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Que, YA., Moreillon, P. Infective endocarditis. Nat Rev Cardiol 8, 322–336 (2011). https://doi.org/10.1038/nrcardio.2011.43[↩]
- Heart Valves and Infective Endocarditis. https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/heart-valves-and-infective-endocarditis[↩]
- Infective Endocarditis. https://emedicine.medscape.com/article/216650-overview[↩][↩][↩]
- Guzek A, Braksator W, Gąsior Z, Kuśmierczyk M, Różański J, Rybicki Z. Infective endocarditis – can we treat it more effectively? Kardiochir Torakochirurgia Pol. 2020 Mar;17(1):8-14. doi: 10.5114/kitp.2020.94184[↩][↩]
- Hackett AJ, Stuart J. Infective endocarditis: identification and management in the emergency department. Emerg Med Pract. 2020 Sep;22(9):1-24. https://www.ebmedicine.net/topics/cardiovascular/infective-endocarditis[↩]
- Fowler VG, Durak DT, Selton-Suty C, et al. The 2023 Duke-ISCVID Criteria for Infective Endocarditis: Updating the Modified Duke Criteria. CID. May 2023. 200.[↩]
- Brusch JL. Infective endocarditis and its mimics in the critical care unit. Cunha BA, ed. Infectious Diseases in Critical Care. 2nd ed. New York, NY: Informa Healthcare; 2007. 261-2.[↩]
- Popovich KJ, Weinstein RA. Questioning Old Staphylococcus aureus Beliefs With New Technology. J Infect Dis. 2023 Apr 26;227(9):1028-1030. doi: 10.1093/infdis/jiac439[↩]
- Barnett R. Infective endocarditis. Lancet. 2016 Sep 17;388(10050):1148. https://doi.org/10.1016/S0140-6736(16)31602-6[↩][↩]
- Murdoch DR, Corey GR, Hoen B, Miro JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falco V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF, Utili R, Wang A, Woods CW, Cabell CH. 2009. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort study. Arch Intern Med 169:463–473. doi: 10.1001/archinternmed.2008.603[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Raoult D, Casalta JP, Richet H, Khan M, Bernit E, Rovery C, Branger S, Gouriet F, Imbert G, Bothello E, Collart F, Habib G. 2005. Contribution of systematic serological testing in diagnosis of infective endocarditis. J Clin Microbiol 43:5238–5242. doi: 10.1128/JCM.43.10.5238-5242.2005[↩][↩][↩][↩][↩][↩][↩][↩]
- Liesman RM, Pritt BS, Maleszewski JJ, Patel R. Laboratory Diagnosis of Infective Endocarditis. J Clin Microbiol. 2017 Sep;55(9):2599-2608. doi: 10.1128/JCM.00635-17[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Bor DH, Woolhandler S, Nardin R, Brusch J, Himmelstein DU. Infective endocarditis in the U.S., 1998-2009: a nationwide study. PLoS One. 2013;8(3):e60033. doi: 10.1371/journal.pone.0060033[↩]
- Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015 Nov 21;36(44):3075-3128. doi: 10.1093/eurheartj/ehv319[↩][↩][↩]
- Fournier PE, Thuny F, Richet H, Lepidi H, Casalta JP, Arzouni JP, Maurin M, Celard M, Mainardi JL, Caus T, Collart F, Habib G, Raoult D. 2010. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clin Infect Dis 51:131–140. doi: 10.1086/653675[↩][↩][↩][↩][↩][↩]
- Morpeth S, Murdoch D, Cabell CH, Karchmer AW, Pappas P, Levine D, Nacinovich F, Tattevin P, Fernandez-Hidalgo N, Dickerman S, Bouza E, del Rio A, Lejko-Zupanc T, de Oliveira Ramos A, Iarussi D, Klein J, Chirouze C, Bedimo R, Corey GR, Fowler VG Jr. 2007. Non-HACEK gram-negative bacillus endocarditis. Ann Intern Med 147:829–835. doi: 10.7326/0003-4819-147-12-200712180-00002[↩][↩]
- Slipczuk L, Codolosa JN, Davila CD, Romero-Corral A, Yun J, Pressman GS, Figueredo VM. Infective endocarditis epidemiology over five decades: a systematic review. PLoS One. 2013 Dec 9;8(12):e82665. doi: 10.1371/journal.pone.0082665. Erratum in: PLoS One. 2014;9(10):e111564[↩]
- Pant S, Patel NJ, Deshmukh A, Golwala H, Patel N, Badheka A, Hirsch GA, Mehta JL. Trends in infective endocarditis incidence, microbiology, and valve replacement in the United States from 2000 to 2011. J Am Coll Cardiol. 2015 May 19;65(19):2070-6. doi: 10.1016/j.jacc.2015.03.518[↩]
- Bustamante-Munguira J, Mestres CA, Alvarez P, Figuerola-Tejerina A, Eiros Bachiller R, Gómez-Sánchez E, Alvarez FJ, Resino S, Castrodeza J, Tamayo E. Surgery for acute infective endocarditis: epidemiological data from a Spanish nationwide hospital-based registry. Interact Cardiovasc Thorac Surg. 2018 Oct 1;27(4):498-504. doi: 10.1093/icvts/ivy127[↩]
- Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016 Feb 27;387(10021):882-93. https://doi.org/10.1016/S0140-6736(15)00067-7[↩][↩][↩][↩]
- Correa de Sa DD, Tleyjeh IM, Anavekar NS, Schultz JC, Thomas JM, Lahr BD, Bachuwar A, Pazdernik M, Steckelberg JM, Wilson WR, Baddour LM. Epidemiological trends of infective endocarditis: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 2010 May;85(5):422-6. doi: 10.4065/mcp.2009.0585. Erratum in: Mayo Clin Proc. 2010 Aug;85(8):772.[↩][↩]
- Murdoch DR, Corey GR, Hoen B, Miró JM, et al. International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) Investigators. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009 Mar 9;169(5):463-73. doi: 10.1001/archinternmed.2008.603[↩][↩]
- Shetty N, Nagpal D, Koivu S, Mrkobrada M. Surgical and Medical Management of Isolated Tricuspid Valve Infective Endocarditis in Intravenous Drug Users. J Card Surg. 2016 Feb;31(2):83-8. doi: 10.1111/jocs.12682[↩]
- Yanagawa B, Bahji A, Lamba W, Tan DH, Cheema A, Syed I, Verma S. Endocarditis in the setting of IDU: multidisciplinary management. Curr Opin Cardiol. 2018 Mar;33(2):140-147. doi: 10.1097/HCO.0000000000000493[↩]
- Miró JM, del Río A, Mestres CA. Infective endocarditis and cardiac surgery in intravenous drug abusers and HIV-1 infected patients. Cardiol Clin. 2003 May;21(2):167-84, v-vi. doi: 10.1016/s0733-8651(03)00025-0[↩]
- Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001 Nov 1;345(18):1318-30. doi: 10.1056/NEJMra010082[↩][↩][↩]
- Raoult D, Casalta JP, Richet H, Khan M, Bernit E, Rovery C, Branger S, Gouriet F, Imbert G, Bothello E, Collart F, Habib G. Contribution of systematic serological testing in diagnosis of infective endocarditis. J Clin Microbiol. 2005 Oct;43(10):5238-42. doi: 10.1128/JCM.43.10.5238-5242.2005[↩][↩][↩]
- Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Tleyjeh IM, Rybak MJ, Barsic B, Lockhart PB, Gewitz MH, Levison ME, Bolger AF, Steckelberg JM, Baltimore RS, Fink AM, O’Gara P, Taubert KA. 2015. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 132:1435–1486. doi: 10.1161/CIR.0000000000000296[↩][↩][↩][↩]
- Thuny F, Grisoli D, Collart F, Habib G, Raoult D. 2012. Management of infective endocarditis: challenges and perspectives. Lancet 379:965–975. doi: 10.1016/S0140-6736(11)60755-1[↩][↩]
- Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR. 2000. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633–638. doi: 10.1086/313753[↩][↩]
- Endocarditis. https://emcrit.org/ibcc/endo/[↩][↩][↩]
- Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Federspiel JJ, Stearns SC, Peppercorn AF, Chu VH, Fowler VG Jr. Arch Intern Med. 2012 Feb 27; 172(4):363-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3314241/[↩]
- Infective Endocarditis. https://emedicine.medscape.com/article/216650-overview#a4[↩]
- Reyes MP, Ali A, Mendes RE, Biedenbach DJ. Resurgence of Pseudomonas endocarditis in Detroit, 2006-2008. Medicine (Baltimore). 2009 Sep;88(5):294-301. doi: 10.1097/MD.0b013e3181b8bedc[↩]
- Wang A, Athan E, Pappas PA, Fowler VG Jr, Olaison L, Paré C, Almirante B, Muñoz P, Rizzi M, Naber C, Logar M, Tattevin P, Iarussi DL, Selton-Suty C, Jones SB, Casabé J, Morris A, Corey GR, Cabell CH; International Collaboration on Endocarditis-Prospective Cohort Study Investigators. Contemporary clinical profile and outcome of prosthetic valve endocarditis. JAMA. 2007 Mar 28;297(12):1354-61. doi: 10.1001/jama.297.12.1354[↩]
- Alvarez-Moreno CA, Morales-López S, Rodriguez GJ, Rodriguez JY, Robert E, Picot C, Ceballos-Garzon A, Parra-Giraldo CM, Le Pape P. The Mortality Attributable to Candidemia in C. auris Is Higher than That in Other Candida Species: Myth or Reality? J Fungi (Basel). 2023 Mar 31;9(4):430. doi: 10.3390/jof9040430[↩]
- Fuller R, Jacobs SE. Candida Infectious Endocarditis and Implantable Cardiac Device Infections. Mycopathologia. 2023 Dec;188(6):893-905. doi: 10.1007/s11046-023-00745-x[↩]
- Lin KP, Yeh TK, Chuang YC, Wang LA, Fu YC, Liu PY. Blood Culture Negative Endocarditis: A Review of Laboratory Diagnostic Approaches. Int J Gen Med. 2023 Jan 24;16:317-327. doi: 10.2147/IJGM.S393329[↩]
- Morris AJ, Drinkovic D, Pottumarthy S, Strickett MG, MacCulloch D, Lambie N, Kerr AR. 2003. Gram stain, culture, and histopathological examination findings for heart valves removed because of infective endocarditis. Clin Infect Dis 36:697–704. doi: 10.1086/367842[↩]
- Topan A, Carstina D, Slavcovici A, Rancea R, Capalneanu R, Lupse M. 2015. Assesment of the Duke criteria for the diagnosis of infective endocarditis after twenty-years. An analysis of 241 cases. Clujul Med 88:321–326. doi: 10.15386/cjmed-469[↩]
- Gould FK, Denning DW, Elliott TS, Foweraker J, Perry JD, Prendergast BD, Sandoe JA, Spry MJ, Watkin RW, Working Party of the British Society for Antimicrobial Chemotherapy. 2012. Guidelines for the diagnosis and antibiotic treatment of endocarditis in adults: a report of the Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 67:269–289. doi: 10.1093/jac/dkr450[↩][↩][↩]
- Houpikian P, Raoult D. 2005. Blood culture-negative endocarditis in a reference center: etiologic diagnosis of 348 cases. Medicine (Baltimore) 84:162–173. doi: 10.1097/01.md.0000165658.82869.17[↩][↩][↩]
- Geissdorfer W, Moos V, Moter A, Loddenkemper C, Jansen A, Tandler R, Morguet AJ, Fenollar F, Raoult D, Bogdan C, Schneider T. 2012. High frequency of Tropheryma whipplei in culture-negative endocarditis. J Clin Microbiol 50:216–222. doi: 10.1128/JCM.05531-11[↩]
- Sohail MR, Gray AL, Baddour LM, Tleyjeh IM, Virk A. 2009. Infective endocarditis due to Propionibacterium species. Clin Microbiol Infect 15:387–394. doi: 10.1111/j.1469-0691.2009.02703.x[↩][↩]
- RODBARD S. HEMODYNAMIC CONSIDERATIONS IN ENDOCARDITIS. Med Sci. 1964 Jan;15:43-9.[↩]
- Durack DT, Beeson PB, Petersdorf RG. Experimental bacterial endocarditis. 3. Production and progress of the disease in rabbits. Br J Exp Pathol. 1973 Apr;54(2):142-51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2072580/pdf/brjexppathol00410-0029.pdf[↩]
- Veloso TR, Chaouch A, Roger T, Giddey M, Vouillamoz J, Majcherczyk P, Que YA, Rousson V, Moreillon P, Entenza JM. Use of a human-like low-grade bacteremia model of experimental endocarditis to study the role of Staphylococcus aureus adhesins and platelet aggregation in early endocarditis. Infect Immun. 2013 Mar;81(3):697-703. doi: 10.1128/IAI.01030-12[↩][↩]
- O’Brien L, Kerrigan SW, Kaw G, Hogan M, Penadés J, Litt D, Fitzgerald DJ, Foster TJ, Cox D. Multiple mechanisms for the activation of human platelet aggregation by Staphylococcus aureus: roles for the clumping factors ClfA and ClfB, the serine-aspartate repeat protein SdrE and protein A. Mol Microbiol. 2002 May;44(4):1033-44. doi: 10.1046/j.1365-2958.2002.02935.x[↩]
- Jung CJ, Yeh CY, Shun CT, Hsu RB, Cheng HW, Lin CS, Chia JS. Platelets enhance biofilm formation and resistance of endocarditis-inducing streptococci on the injured heart valve. J Infect Dis. 2012 Apr 1;205(7):1066-75. doi: 10.1093/infdis/jis021[↩]
- Hubert Lepidi, Jean-Paul Casalta, Pierre-Edouard Fournier, Gilbert Habib, Frédéric Collart, Didier Raoult, Quantitative Histological Examination of Bioprosthetic Heart Valves, Clinical Infectious Diseases, Volume 42, Issue 5, 1 March 2006, Pages 590–596, https://doi.org/10.1086/500135[↩]
- Wilson WR, Gewitz M, Lockhart PB, Bolger AF, DeSimone DC, Kazi DS, Couper DJ, Beaton A, Kilmartin C, Miro JM, Sable C, Jackson MA, Baddour LM; American Heart Association Young Hearts Rheumatic Fever, Endocarditis and Kawasaki Disease Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young; Council on Cardiovascular and Stroke Nursing; and the Council on Quality of Care and Outcomes Research. Prevention of Viridans Group Streptococcal Infective Endocarditis: A Scientific Statement From the American Heart Association. Circulation. 2021 May 18;143(20):e963-e978. doi: 10.1161/CIR.0000000000000969. Epub 2021 Apr 15. Erratum in: Circulation. 2021 Aug 31;144(9):e192. doi: 10.1161/CIR.0000000000001012. Erratum in: Circulation. 2022 Apr 26;145(17):e868. doi: 10.1161/CIR.0000000000001066[↩][↩][↩][↩]
- Thornhill M, Prendergast B, Dayer M, Frisby A, Baddour LM. Endocarditis prevention: time for a review of NICE guidance. Lancet Reg Health Eur. 2024 Mar 5;39:100876. doi: 10.1016/j.lanepe.2024.100876[↩][↩][↩][↩][↩]
- Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, de Jesus Antunes M, Thilen U, Lekakis J, Lengyel M, Müller L, Naber CK, Nihoyannopoulos P, Moritz A, Zamorano JL; ESC Committee for Practice Guidelines. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J. 2009 Oct;30(19):2369-413. doi: 10.1093/eurheartj/ehp285[↩]
- Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Surgery and Anesthesia; Quality of Care and Outcomes Research Interdisciplinary Working Group. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007 Oct 9;116(15):1736-54. doi: 10.1161/CIRCULATIONAHA.106.183095. Epub 2007 Apr 19. Erratum in: Circulation. 2007 Oct 9;116(15):e376-7.[↩]
- Baddour LM, Cha YM, Wilson WR. Clinical practice. Infections of cardiovascular implantable electronic devices. N Engl J Med. 2012 Aug 30;367(9):842-9. doi: 10.1056/NEJMcp1107675. Erratum in: N Engl J Med. 2012 Oct 11;367(15):1474. Erratum in: N Engl J Med. 2012 Sep 27;367(13):1272.[↩]
- Buchan BW, Windham S, Balada-Llasat JM, Leber A, Harrington A, Relich R, Murphy C, Dien Bard J, Naccache S, Ronen S, Hopp A, Mahmutoglu D, Faron ML, Ledeboer NA, Carroll A, Stone H, Akerele O, Everhart K, Bonwit A, Kwong C, Buckner R, Warren D, Fowler R, Chandrasekaran S, Huse H, Campeau S, Humphries R, Graue C, Huang A. Practical Comparison of the BioFire FilmArray Pneumonia Panel to Routine Diagnostic Methods and Potential Impact on Antimicrobial Stewardship in Adult Hospitalized Patients with Lower Respiratory Tract Infections. J Clin Microbiol. 2020 Jun 24;58(7):e00135-20. doi: 10.1128/JCM.00135-20[↩]
- Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, Douglas PS, Faxon DP, Gillam LD, Kimball TR, Kussmaul WG, Pearlman AS, Philbrick JT, Rakowski H, Thys DM, Antman EM, Smith SC Jr, Alpert JS, Gregoratos G, Anderson JL, Hiratzka LF, Hunt SA, Fuster V, Jacobs AK, Gibbons RJ, Russell RO; American College of Cardiology; American Heart Association; American Society of Echocardiography. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003 Sep 2;108(9):1146-62. doi: 10.1161/01.CIR.0000073597.57414.A9[↩]
- Jassal DS, Picard MH. Echocardiography. Brusch JL, ed. Infective Endocarditis: Management in the Era of Intravascular Devices. New York, NY: Informa Healthcare; 2007. 255-72.[↩]
- Roe MT, Abramson MA, Li J, Heinle SK, Kisslo J, Corey GR, Sexton DJ. Clinical information determines the impact of transesophageal echocardiography on the diagnosis of infective endocarditis by the duke criteria. Am Heart J. 2000 Jun;139(6):945-51. doi: 10.1067/mhj.2000.104762[↩]
- Feuchtner GM, Stolzmann P, Dichtl W, Schertler T, Bonatti J, Scheffel H, Mueller S, Plass A, Mueller L, Bartel T, Wolf F, Alkadhi H. Multislice computed tomography in infective endocarditis: comparison with transesophageal echocardiography and intraoperative findings. J Am Coll Cardiol. 2009 Feb 3;53(5):436-44. doi: 10.1016/j.jacc.2008.01.077[↩]
- Cunha BA. Persistent S. aureus acute bacteremia: clinical pathway for diagnosis and treatment. Antibiot for Clin. 2006. 10:39-46.[↩]
- Pujol M, Miró JM, Shaw E, Aguado JM, et al. MRSA Bacteremia (BACSARM) Trial Investigators. Daptomycin Plus Fosfomycin Versus Daptomycin Alone for Methicillin-resistant Staphylococcus aureus Bacteremia and Endocarditis: A Randomized Clinical Trial. Clin Infect Dis. 2021 May 4;72(9):1517-1525. doi: 10.1093/cid/ciaa1081[↩]
- Jones T, Yeaman MR, Sakoulas G, Yang SJ, Proctor RA, Sahl HG, Schrenzel J, Xiong YQ, Bayer AS. Failures in clinical treatment of Staphylococcus aureus Infection with daptomycin are associated with alterations in surface charge, membrane phospholipid asymmetry, and drug binding. Antimicrob Agents Chemother. 2008 Jan;52(1):269-78. doi: 10.1128/AAC.00719-07[↩]
- Prophylaxis against infective endocarditis: antimicrobial prophylaxis against infective endocarditis in adults and children undergoing interventional procedures. https://www.nice.org.uk/guidance/cg64/resources/prophylaxis-against-infective-endocarditis-antimicrobial-prophylaxis-against-infective-endocarditis-in-adults-and-children-undergoing-interventional-procedures-pdf-975567956677[↩][↩]
- Delgado V, Ajmone Marsan N, de Waha S, et al. ESC Scientific Document Group. 2023 ESC Guidelines for the management of endocarditis. Eur Heart J. 2023 Oct 14;44(39):3948-4042. doi: 10.1093/eurheartj/ehad193. Erratum in: Eur Heart J. 2023 Dec 1;44(45):4780. doi: 10.1093/eurheartj/ehad625. Erratum in: Eur Heart J. 2024 Jan 1;45(1):56. doi: 10.1093/eurheartj/ehad776[↩]
- Prevention of Infective Endocarditis. Circulation. 2007;116:1736-1754 http://circ.ahajournals.org/content/116/15/1736[↩]
- Habib G, Lancellotti P, Iung B. 2015 ESC Guidelines on the management of infective endocarditis: a big step forward for an old disease. Heart. 2016 Jul 1;102(13):992-4. doi: 10.1136/heartjnl-2015-308791[↩]
- Sandre RM, Shafran SD. Infective endocarditis: review of 135 cases over 9 years. Clin Infect Dis. 1996;22:276–86. doi: 10.1093/clinids/22.2.276[↩]
- Servy A, Valeyrie-Allanore L, Alla F, Lechiche C, Nazeyrollas P, Chidiac C, Hoen B, Chosidow O, Duval X; Association Pour l’Etude et la Prévention de l’Endocardite Infectieuse Study Group. Prognostic value of skin manifestations of infective endocarditis. JAMA Dermatol. 2014 May;150(5):494-500. doi: 10.1001/jamadermatol.2013.8727[↩]
- Hirai T, Koster M. Osler’s nodes, Janeway lesions and splinter haemorrhages. Case Reports 2013;2013:bcr2013009759[↩]
- Marrie TJ. Osler’s nodes and Janeway lesions. Am J Med 2008;2013:105–6.[↩]
- Osler W. Chronic infectious endocarditis. Q J Med 1909;2:219–30.[↩][↩]
- Tikoo M, Bardia A, Gupta A, Pandey A. Dermatological Manifestations of Infective Endocarditis. J Gen Intern Med. 2015 Aug;30(8):1229-30. doi: 10.1007/s11606-015-3256-z[↩]
- Silverman ME, Upshaw CB., Jr Extracardiac manifestations of infective endocarditis and their historical descriptions. Am J Cardiol. 2007;100(12):1802–7. doi: 10.1016/j.amjcard.2007.07.034[↩]
- Beaulieu A, Rehman HU. Janeway lesions. CMAJ. 2010 Jul 13;182(10):1075. doi: 10.1503/cmaj.091528[↩][↩]
- Gunson, T.H. and Oliver, G.F. (2007), Osler’s nodes and Janeway lesions. Australasian Journal of Dermatology, 48: 251-255. https://doi.org/10.1111/j.1440-0960.2007.00397.x[↩]
- Sethi K, Buckley J, de Wolff J. Splinter haemorrhages, Osler’s nodes, Janeway lesions and Roth spots: the peripheral stigmata of endocarditis. Br J Hosp Med (Lond). 2013 Sep;74(9):C139-42.[↩]
- KERR, A., JR. and TAN, J.S. (1979), Biopsies of the Janeway Lesion of Infective Endocarditis. Journal of Cutaneous Pathology, 6: 124-129. https://doi.org/10.1111/j.1600-0560.1979.tb01113.x[↩]
- Misin A, Di Bella S, Priolo L, Luzzati R. Image of the month: ‘Diagnostic hands’: Janeway lesions. Clin Med (Lond). 2017 Jul;17(4):373-374. doi: 10.7861/clinmedicine.17-4-373[↩]
- Sapira JD. The art & science of bedside diagnosis. Baltimore: Urban & Schwarzenberg, Inc.; 1990. p. 197–8.[↩]
- Van Uitert RL, Solomon GE. White-centered retinal hemorrhages: a sign of intracranial hemorrhage. Neurology. 1979 Feb;29(2):236-9. doi: 10.1212/wnl.29.2.236[↩][↩]
- Chong Y, Han SJ, Rhee YJ, Kang SK, Yu JH, Na MH. Classic Peripheral Signs of Subacute Bacterial Endocarditis. Korean J Thorac Cardiovasc Surg. 2016 Oct;49(5):408-412. doi: 10.5090/kjtcs.2016.49.5.408[↩][↩]
- Duane TD, Osher RH, Green WR. White centered hemorrhages: their significance. Ophthalmology. 1980 Jan;87(1):66-9. doi: 10.1016/s0161-6420(80)35277-9[↩][↩][↩]
- Fred HL. Little black bags, ophthalmoscopy, and the Roth spot. Tex Heart Inst J. 2013;40(2):115-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3649782[↩][↩]
- Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994 Mar;96(3):200-9. https://doi.org/10.1016/0002-9343(94)90143-0[↩][↩]
- Hoen B, Béguinot I, Rabaud C, Jaussaud R, Selton-Suty C, May T, Canton P. The Duke criteria for diagnosing infective endocarditis are specific: analysis of 100 patients with acute fever or fever of unknown origin. Clin Infect Dis. 1996 Aug;23(2):298-302. doi: 10.1093/clinids/23.2.298[↩]
- Hoen B, Selton-Suty C, Danchin N, Weber M, Villemot JP, Mathieu P, Floquet J, Canton P. Evaluation of the Duke criteria versus the Beth Israel criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 1995 Oct;21(4):905-9. doi: 10.1093/clinids/21.4.905[↩]
- Millar B, Moore J, Mallon P, Xu J, Crowe M, Mcclurg R, Raoult D, Earle J, Hone R, Murphy P. Molecular diagnosis of infective endocarditis–a new Duke’s criterion. Scand J Infect Dis. 2001;33(9):673-80. doi: 10.1080/00365540110026764[↩]
- Bayer AS, Ward JI, Ginzton LE, Shapiro SM. Evaluation of new clinical criteria for the diagnosis of infective endocarditis. Am J Med. 1994 Mar;96(3):211-9. doi: 10.1016/0002-9343(94)90144-9[↩]
- Gagliardi JP, Nettles RE, McCarty DE, Sanders LL, Corey GR, Sexton DJ. Native valve infective endocarditis in elderly and younger adult patients: comparison of clinical features and outcomes with use of the Duke criteria and the Duke Endocarditis Database. Clin Infect Dis. 1998 May;26(5):1165-8. doi: 10.1086/520304[↩]
- Nettles RE, McCarty DE, Corey GR, Li J, Sexton DJ. An evaluation of the Duke criteria in 25 pathologically confirmed cases of prosthetic valve endocarditis. Clin Infect Dis. 1997 Dec;25(6):1401-3. doi: 10.1086/516145[↩]
- Sekeres MA, Abrutyn E, Berlin JA, Kaye D, Kinman JL, Korzeniowski OM, Levison ME, Feldman RS, Strom BL. An assessment of the usefulness of the Duke criteria for diagnosing active infective endocarditis. Clin Infect Dis. 1997 Jun;24(6):1185-90. doi: 10.1086/513657[↩][↩]
- Habib G, Derumeaux G, Avierinos JF, Casalta JP, Jamal F, Volot F, Garcia M, Lefevre J, Biou F, Maximovitch-Rodaminoff A, Fournier PE, Ambrosi P, Velut JG, Cribier A, Harle JR, Weiller PJ, Raoult D, Luccioni R. Value and limitations of the Duke criteria for the diagnosis of infective endocarditis. J Am Coll Cardiol. 1999 Jun;33(7):2023-9. doi: 10.1016/s0735-1097(99)00116-3[↩]
- Pérez-Vázquez A, Fariñas MC, García-Palomo JD, Bernal JM, Revuelta JM, González-Macías J. Evaluation of the Duke criteria in 93 episodes of prosthetic valve endocarditis: could sensitivity be improved? Arch Intern Med. 2000 Apr 24;160(8):1185-91. doi: 10.1001/archinte.160.8.1185[↩][↩]
- Dodds GA, Sexton DJ, Durack DT, Bashore TM, Corey GR, Kisslo J. Negative predictive value of the Duke criteria for infective endocarditis. Am J Cardiol. 1996 Feb 15;77(5):403-7. doi: 10.1016/s0002-9149(97)89372-1[↩]
- Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000 Apr;30(4):633-8. doi: 10.1086/313753[↩]
- Patel R, Vetter EA, Harmsen WS, Schleck CD, Fadel HJ, Cockerill FR III. 2011. Optimized pathogen detection with 30- compared to 20-milliliter blood culture draws. J Clin Microbiol 49:4047–4051. doi: 10.1128/JCM.01314-11[↩]
- Petti CA, Bhally HS, Weinstein MP, Joho K, Wakefield T, Reller LB, Carroll KC. 2006. Utility of extended blood culture incubation for isolation of Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella organisms: a retrospective multicenter evaluation. J Clin Microbiol 44:257–259. doi: 10.1128/JCM.44.1.257-259.2006[↩]
- Chambers ST, Murdoch D, Morris A, Holland D, Pappas P, Almela M, Fernandez-Hidalgo N, Almirante B, Bouza E, Forno D, del Rio A, Hannan MM, Harkness J, Kanafani ZA, Lalani T, Lang S, Raymond N, Read K, Vinogradova T, Woods CW, Wray D, Corey GR, Chu VH. 2013. HACEK infective endocarditis: characteristics and outcomes from a large, multi-national cohort. PLoS One 8:e63181. doi: 10.1371/journal.pone.0063181[↩]
- Sagi M, Nesher L, Yagupsky P. 2017. The Bactec FX blood culture system detects Brucella melitensis bacteremia in adult patients within the routine 1-week incubation period. J Clin Microbiol 55:942–946. doi: 10.1128/JCM.02320-16[↩]
- Clinical and Laboratory Standards Institute. 2007. Principles and procedures for blood cultures; approved standard—1st ed CLSI document M47-A. Clinical and Laboratory Standards Institute, Wayne, PA.[↩]
- Baron EJ, Scott JD, Tompkins LS. 2005. Prolonged incubation and extensive subculturing do not increase recovery of clinically significant microorganisms from standard automated blood cultures. Clin Infect Dis 41:1677–1680. doi: 10.1086/497595[↩]
- Maurin M, Eb F, Etienne J, Raoult D. Serological cross-reactions between Bartonella and Chlamydia species: implications for diagnosis. J Clin Microbiol. 1997 Sep;35(9):2283-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC229955/pdf/352283.pdf[↩]
- Habib G, Lancellotti P, Antunes MJ, et al. ESC Scientific Document Group. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015 Nov 21;36(44):3075-3128. https://orbi.uliege.be/bitstream/2268/191313/1/eur%20h%20j%202015%2036%203075.pdf[↩][↩][↩][↩][↩][↩][↩][↩]
- Holland TL, Baddour LM, Bayer AS, Hoen B, Miro JM, Fowler VG. Infective endocarditis. Nature reviews Disease primers. 2016;2:16059. doi:10.1038/nrdp.2016.59. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5240923/[↩]
- Barsic B, et al. Influence of the timing of cardiac surgery on the outcome of patients with infective endocarditis and stroke. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2013;56:209–217. This study of 857 patient patients with endocarditis complicated by ischemic stroke without haemorrhagic conversion found that no survival benefit was gained from delaying surgery. https://www.ncbi.nlm.nih.gov/pubmed/23074311[↩]
- Garcia-Cabrera E, et al. Neurological complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation. 2013;127:2272–2284. http://circ.ahajournals.org/content/127/23/2272.long[↩]
- Baddour LM, et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation. 2015;132:1435–1486. This guideline from the American Heart Association updates the previous 2005 guideline for diagnosis and management of infective endocarditis, including detailed antibiotic guidance. http://circ.ahajournals.org/content/132/15/1435.long[↩][↩][↩]
- Arnold CJ, et al. Candida infective endocarditis: an observational cohort study with a focus on therapy. Antimicrobial agents and chemotherapy. 2015;59:2365–2373. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4356766/[↩]
- Tornos P, et al. Infective endocarditis due to Staphylococcus aureus: deleterious effect of anticoagulant therapy. Archives of internal medicine. 1999;159:473–475 https://www.ncbi.nlm.nih.gov/pubmed/10074955[↩][↩]
- Chan KL, et al. Effect of long-term aspirin use on embolic events in infective endocarditis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;46:37–41. https://www.ncbi.nlm.nih.gov/pubmed/18171211[↩]
- Park KH, et al. Optimal Duration of Antibiotic Therapy in Patients With Hematogenous Vertebral Osteomyelitis at Low Risk and High Risk of Recurrence. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;62:1262–1269. https://www.ncbi.nlm.nih.gov/pubmed/26917813[↩]
- Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falcó V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF, Utili R, Wang A, Woods CW, Cabell CH; International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) Investigators. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009 Mar 9;169(5):463-73. doi: 10.1001/archinternmed.2008.603[↩]
- García-Cabrera E, Fernández-Hidalgo N, Almirante B, Ivanova-Georgieva R, Noureddine M, Plata A, Lomas JM, Gálvez-Acebal J, Hidalgo-Tenorio C, Ruíz-Morales J, Martínez-Marcos FJ, Reguera JM, de la Torre-Lima J, de Alarcón González A; Group for the Study of Cardiovascular Infections of the Andalusian Society of Infectious Diseases; Spanish Network for Research in Infectious Diseases. Neurological complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation. 2013 Jun 11;127(23):2272-84. doi: 10.1161/CIRCULATIONAHA.112.000813[↩][↩]
- Heiro M, Nikoskelainen J, Engblom E, Kotilainen E, Marttila R, Kotilainen P. Neurologic manifestations of infective endocarditis: a 17-year experience in a teaching hospital in Finland. Arch Intern Med. 2000 Oct 9;160(18):2781-7. doi: 10.1001/archinte.160.18.2781[↩][↩]
- Huang JS, Ho AS, Ahmed A, Bhalla S, Menias CO. Borne identity: CT imaging of vascular infections. Emerg Radiol. 2011 Aug;18(4):335-43. doi: 10.1007/s10140-011-0946-7[↩]
- Duval X, Iung B, Klein I, Brochet E, Thabut G, Arnoult F, Lepage L, Laissy JP, Wolff M, Leport C; IMAGE (Resonance Magnetic Imaging at the Acute Phase of Endocarditis) Study Group. Effect of early cerebral magnetic resonance imaging on clinical decisions in infective endocarditis: a prospective study. Ann Intern Med. 2010 Apr 20;152(8):497-504, W175. doi: 10.7326/0003-4819-152-8-201004200-00006[↩]
- Hess A, Klein I, Iung B, Lavallée P, Ilic-Habensus E, Dornic Q, Arnoult F, Mimoun L, Wolff M, Duval X, Laissy JP. Brain MRI findings in neurologically asymptomatic patients with infective endocarditis. AJNR Am J Neuroradiol. 2013 Aug;34(8):1579-84. doi: 10.3174/ajnr.A3582[↩]
- Iung B, Tubiana S, Klein I, Messika-Zeitoun D, Brochet E, Lepage L, Al-Attar N, Ruimy R, Leport C, Wolff M, Duval X; ECHO-IMAGE Study Group. Determinants of cerebral lesions in endocarditis on systematic cerebral magnetic resonance imaging: a prospective study. Stroke. 2013 Nov;44(11):3056-62. doi: 10.1161/STROKEAHA.113.001470[↩]
- Di Salvo G, Habib G, Pergola V, Avierinos JF, Philip E, Casalta JP, Vailloud JM, Derumeaux G, Gouvernet J, Ambrosi P, Lambert M, Ferracci A, Raoult D, Luccioni R. Echocardiography predicts embolic events in infective endocarditis. J Am Coll Cardiol. 2001 Mar 15;37(4):1069-76. doi: 10.1016/s0735-1097(00)01206-7[↩][↩]
- Dickerman SA, Abrutyn E, Barsic B, Bouza E, Cecchi E, Moreno A, Doco-Lecompte T, Eisen DP, Fortes CQ, Fowler VG Jr, Lerakis S, Miro JM, Pappas P, Peterson GE, Rubinstein E, Sexton DJ, Suter F, Tornos P, Verhagen DW, Cabell CH; ICE Investigators. The relationship between the initiation of antimicrobial therapy and the incidence of stroke in infective endocarditis: an analysis from the ICE Prospective Cohort Study (ICE-PCS). Am Heart J. 2007 Dec;154(6):1086-94. doi: 10.1016/j.ahj.2007.07.023[↩]
- Infective Endocarditis. https://emedicine.medscape.com/article/216650-overview#a6[↩][↩][↩][↩]
- Cabell CH, Jollis JG, Peterson GE, et al. Changing Patient Characteristics and the Effect on Mortality in Endocarditis. Arch Intern Med. 2002;162(1):90–94. doi:10.1001/archinte.162.1.9[↩]
- Ortiz-Bautista C, López J, García-Granja PE, Vilacosta I, Sevilla T, Sarriá C, Olmos C, Ferrera C, Sáez C, Puerto A, San Román JA. Right-sided infective endocarditis in cardiac device carriers: Clinical profile and prognosis. Med Clin (Barc). 2017 Dec 7;149(11):477-482. English, Spanish. doi: 10.1016/j.medcli.2017.03.055[↩]
- Özcan C, Raunsø J, Lamberts M, Køber L, Lindhardt TB, Bruun NE, Laursen ML, Torp-Pedersen C, Gislason GH, Hansen ML. Infective endocarditis and risk of death after cardiac implantable electronic device implantation: a nationwide cohort study. Europace. 2017 Jun 1;19(6):1007-1014. doi: 10.1093/europace/euw404[↩]
- Cresti A, Chiavarelli M, Scalese M, Nencioni C, Valentini S, Guerrini F, D’Aiello I, Picchi A, De Sensi F, Habib G. Epidemiological and mortality trends in infective endocarditis, a 17-year population-based prospective study. Cardiovasc Diagn Ther. 2017 Feb;7(1):27-35. doi: 10.21037/cdt.2016.08.09[↩]
- Janga KC, Sinha A, Greenberg S, Sharma K. Nephrologists Hate the Dialysis Catheters: A Systemic Review of Dialysis Catheter Associated Infective Endocarditis. Case Rep Nephrol. 2017;2017:9460671. doi: 10.1155/2017/9460671[↩]
- Ohara T, Nakatani S, Kokubo Y, Yamamoto H, Mitsutake K, Hanai S; CADRE investigators. Clinical predictors of in-hospital death and early surgery for infective endocarditis: results of CArdiac Disease REgistration (CADRE), a nation-wide survey in Japan. Int J Cardiol. 2013 Sep 10;167(6):2688-94. doi: 10.1016/j.ijcard.2012.06.117[↩]
- Baddley JW, Benjamin DK Jr, Patel M, Miró J, Athan E, Barsic B, Bouza E, Clara L, Elliott T, Kanafani Z, Klein J, Lerakis S, Levine D, Spelman D, Rubinstein E, Tornos P, Morris AJ, Pappas P, Fowler VG Jr, Chu VH, Cabell C; International Collaboration on Endocarditis-Prospective Cohort Study Group (ICE-PCS). Candida infective endocarditis. Eur J Clin Microbiol Infect Dis. 2008 Jul;27(7):519-29. doi: 10.1007/s10096-008-0466-x[↩]
- Hill EE, Herijgers P, Claus P, Vanderschueren S, Herregods MC, Peetermans WE. Infective endocarditis: changing epidemiology and predictors of 6-month mortality: a prospective cohort study. Eur Heart J. 2007 Jan;28(2):196-203. doi: 10.1093/eurheartj/ehl427[↩]
- Liu PY, Huang YF, Tang CW, Chen YY, Hsieh KS, Ger LP, Chen YS, Liu YC. Staphylococcus lugdunensis infective endocarditis: a literature review and analysis of risk factors. J Microbiol Immunol Infect. 2010 Dec;43(6):478-84. doi: 10.1016/S1684-1182(10)60074-6[↩]
- Wallace SM, Walton BI, Kharbanda RK, Hardy R, Wilson AP, Swanton RH. Mortality from infective endocarditis: clinical predictors of outcome. Heart. 2002 Jul;88(1):53-60. doi: 10.1136/heart.88.1.53[↩]
- Soong G, Chun J, Parker D, Prince A. Staphylococcus aureus activation of caspase 1/calpain signaling mediates invasion through human keratinocytes. J Infect Dis. 2012 May 15;205(10):1571-9. doi: 10.1093/infdis/jis244[↩]
- Hémar V, Camou F, Roubaud-Baudron C, Ternacle J, Pernot M, Greib C, Dijos M, Wirth G, Chaussade H, Peuchant O, Bonnet F, Issa N; MoISE Study Group. The Mortality of Infective endocarditis with and without Surgery in Elderly (MoISE) Study. Clin Infect Dis. 2023 Nov 17;77(10):1440-1448. doi: 10.1093/cid/ciad384[↩]