Contents
- What is mixed hyperlipidemia
- What is cholesterol?
- What are Cholesterol levels?
- Mixed hyperlipidemia cause
- Mixed hyperlipidemia prevention
- Mixed hyperlipidemia symptoms
- Mixed hyperlipidemia complications
- Mixed hyperlipidemia diagnosis
- Mixed hyperlipidemia treatment
- Foods for mixed hyperlipidemia
- Oatmeal, oat bran, barley and other whole grains and high-fiber foods
- Fish and omega-3 fatty acids
- Almonds and other nuts
- Apples, grapes, strawberries, citrus fruits
- Eggplant and okra
- Avocados
- Olive oil
- Vegetable oils
- Foods with added plant sterols or stanols
- Whey protein
- Soy
- Beans
- Fiber supplements
- Limiting saturated fats and trans fats
- Foods to avoid with high cholesterol
- Mixed hyperlipidemia prognosis
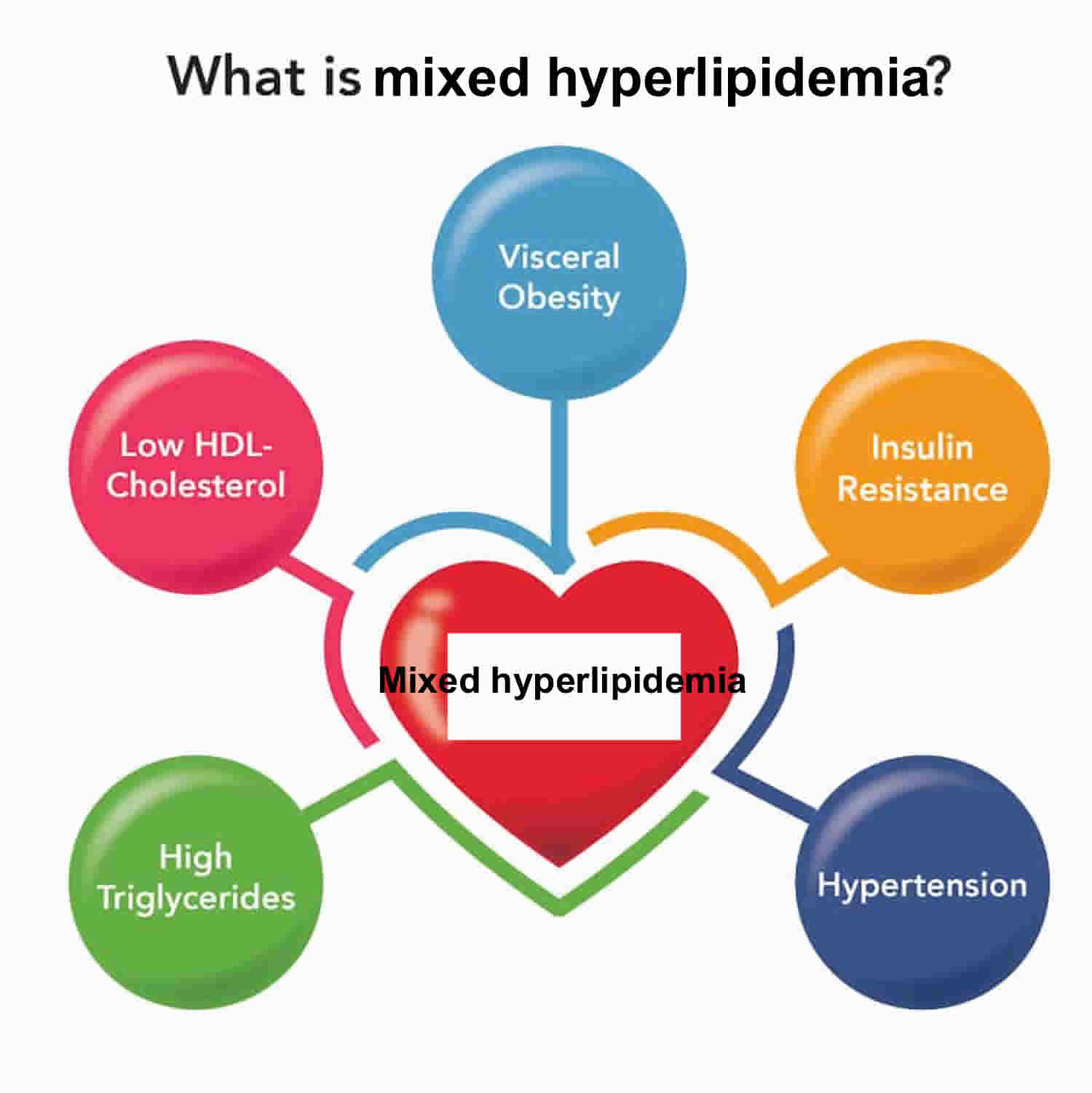
What is mixed hyperlipidemia
Mixed hyperlipidemia also called mixed hyperlipidaemia, mixed dyslipidemia, diabetic dyslipidemia, mixed hypercholesterolemia, type V hyperlipidemia, type V lipidemia or type V hyperlipoproteinemia is a lipid disorder characterized by elevated levels of total cholesterol (TC), elevated levels of “bad” low-density lipoprotein (LDL) cholesterol and elevated levels of triglycerides (hypertriglyceridemia), and reduced levels of “good” high-density lipoprotein (HDL) cholesterol 1, 2, 3, 4, 5, 6. Both genetic and environmental factors contribute to cause mixed hyperlipidema (e.g., insulin resistance) 7. Mixed hyperlipidemia is the most frequent lipid disorder found in patients with type 2 diabetes 8, 9. Mixed hyperlipidemia is typically linked with an increase of small, dense LDL particles, and an elevated apolipoprotein B (APOB). All these changes predispose to an increased risk of cardiovascular disease 10. Mixed hyperlipidemia represents a subgroup of familial combined hyperlipidemia, the most common inherited lipid metabolic disorder identified in young survivors of heart attack 6.
Mixed hyperlipidemia is caused by complex interactions between your genes and environmental factors such as an unhealthy diet, medications (amiodarone, glucocorticoids), underactive thyroid (hypothyroidism), uncontrolled diabetes, obesity, chronic kidney disease and/or a sedentary lifestyle 11.
An unhealthy lifestyle is the most common cause of high “bad” LDL cholesterol or low “good” HDL cholesterol. However, genes that you inherit from your parents, other medical conditions, and some medicines may also raise LDL cholesterol levels or lower “good” HDL cholesterol levels.
Any of the following conditions may cause hyperlipidemia or increase your risk of hyperlipidemia:
- Unhealthy eating habits or unhealthy diet, such as eating lots of bad fats. Eating a diet high in saturated fats and cholesterol. saturated fat, is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods. Eating a lot of foods high in saturated fats raises “bad” LDL cholesterol levels. Another type, trans fat, is in some fried and processed foods. Eating these fats can raise your “bad” LDL cholesterol. No more than 10% of your daily calories should come from saturated fats.
- Genetics – your genetic makeup might make it more difficult for your body to remove “bad” LDL cholesterol from your blood or break it down in the liver.
- Taking certain medications, hormonal or glucocorticoids. Some medicines that you take for other health problems can raise your level of “bad” LDL cholesterol or lower your level of “good” HDL cholesterol, including:
- Arrhythmia medicines, such as amiodarone
- Beta-blockers for relieving angina chest pain or treating high blood pressure
- Chemotherapy medicines used to treat cancer
- Diuretics, such as thiazide, to treat high blood pressure
- Immunosuppressive medicines, such as cyclosporine, to treat inflammatory diseases or to prevent rejection after organ transplant
- Retinoids to treat acne
- Steroids, such as prednisone, to treat inflammatory diseases such as lupus, rheumatoid arthritis, and psoriasis
- Medical conditions (diabetes, hypothyroidism, chronic kidney disease, HIV/AIDS, lupus, polycystic ovary syndrome)
- Living a sedentary lifestyle or lack of physical activity, with lots of sitting and little exercise. This lowers your “good” HDL cholesterol.
- Pregnancy
- Excessive alcohol consumption. Drinking more than two drinks a day for men or one drink a day for women can raise your total cholesterol level.
- Smoking or exposure to tobacco smoke, which lowers “good” HDL cholesterol, especially in women. It also raises your “bad” LDL cholesterol.
- Being overweight or obese.
- Stress may raise levels of certain hormones, such as corticosteroids. These can cause your body to make more cholesterol.
- Getting little or low-quality sleep has been linked to lower cardiovascular health.
- Age. Unhealthy levels of cholesterol can affect people of all ages, even young children. However, high cholesterol is most commonly diagnosed in people between ages 40 and 59. As you get older, your body’s metabolism changes. Your liver does not remove “bad” LDL cholesterol as well as it did when you were young. These normal changes may increase your risk for developing high blood cholesterol as you age.
- Race or ethnicity. Your race or ethnicity may affect your risk of high blood cholesterol:
- Overall, non-Hispanic White people are more likely than other groups to have high levels of total cholesterol.
- Asian Americans, including those of Indian, Filipino, Japanese, and Vietnamese descent, are more likely to have high levels of “bad” LDL cholesterol than other groups.
- Hispanic Americans are more likely to have lower levels of “good” HDL cholesterol than other groups.
- African Americans are more likely than other groups to have high levels of “good” HDL cholesterol.
- Gender or sex. Between ages 20 and 39, men have a greater risk for high total cholesterol than women. A woman’s risk goes up after menopause. Menopause lowers levels of female hormones that may protect against high blood cholesterol. After menopause, women’s levels of total and “bad” LDL cholesterol usually go up, while their levels of “good” HDL cholesterol go down.
High levels of “bad” low-density lipoprotein (LDL) cholesterol usually do not cause symptoms, although very high triglyceride levels can cause sensation of tingling, burning, pricking or prickling (paresthesias), shortness of breath (dyspnea) and confusion 12. Mixed hyperlipidemia is often a hidden risk factor which means it can happen without you knowing until it’s too late. Undiagnosed or untreated mixed hyperlipidemia can lead to serious problems, such as heart attack, stroke and acute pancreatitis (high triglyceride levels > 500 mg/dL [> 5.65 mmol/L]). That is why it’s so important to get your cholesterol level checked. Talk to your doctor about your risk and steps you can take to keep your cholesterol levels in a healthy range.
If you have familial hypercholesterolemia, you may have visible signs of high cholesterol. These include:
- Tendon xanthomata – swellings made from cholesterol on the knuckles of your hands, your knees or the Achilles tendon at the back of your ankle.
- Xanthelasmas – small, yellow lumps of cholesterol near the inner corner of your eye.
- Corneal arcus – this is a pale white ring around the colored part of your eye, your iris.
If you’re diagnosed with mixed hyperlipidemia, your overall health and other risks such as smoking, diabetes or high blood pressure will help guide treatment. Treatment options depend on the specific lipid abnormality you have, although different lipid abnormalities often coexist in mixed hyperlipidemia. The main treatments for mixed hyperlipidemia are lifestyle changes and medicines. Treatment should always include treatment of hypertension and diabetes and metabolic syndrome.
If you have high LDL or total cholesterol, you can lower your risk of heart disease by 13, 14, 15:
- Choosing heart-healthy foods. The DASH eating plans can help you lower your “bad” LDL cholesterol. These plans encourage:
- Limiting saturated fats found in fatty cuts of meats, dairy products, and desserts
- Eating whole grains, fruits, and vegetables rather than refined carbohydrates such as sweets and other high-sugar foods
- Eating a variety of nuts
- Preparing foods with little or no salt
- Getting regular physical activity. Studies have shown that physical activity can lower LDL “bad” cholesterol and triglycerides and raise your “good” HDL cholesterol. For example, resistance training among postmenopausal women may decrease total cholesterol, LDL cholesterol, and triglycerides. Aim for at least 30 minutes of exercise on most days. It’s recommended that you do at least 150 minutes of moderate intensity exercise per week. Moderate exercise is when you feel warm and comfortably breathless like when walking or pushing a lawn mower. Intense exercise is when you breathe hard and fast like when running, swimming or cycling. The recommended types of exercise for improving heart health are:
- Aerobic exercise – when you’re moving your body in a way that makes you warm and slightly out of breath like when walking, cycling, doing housework or gardening. Over time, this type of exercise helps your heart and circulatory system to work better by helping to lower your blood pressure and resting heart rate, improving cholesterol levels and helping you maintain a healthy weight
- Balance and flexibility exercise – exercise like yoga, tai chi and Pilates where we hold our bodies in less stable positions. These exercises make sure our muscles don’t get too tight and keep us flexible, helping avoid pain or injury and reduce the risk of having falls
- Resistance exercise – resistance training like lifting weights or using resistance bands and cables to strengthen your muscles. The stronger your muscles are, the harder they can work which takes the strain off your heart making it easier to do everyday tasks. Check in with your doctor before you start any resistance training as it may not be suitable for some people with heart conditions.
- Aiming for a healthy weight. Research has shown that adults with overweight and obesity can lower “bad” LDL cholesterol and raise “good” HDL cholesterol by losing only 3% to 5% of their weight.
- Managing stress. Research has shown that chronic stress can sometimes increase LDL cholesterol levels and decrease HDL cholesterol levels.
- Quitting smoking. If you smoke, quit. Smoking can raise your risk of heart disease and heart attack and worsen other heart disease risk factors. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
- Getting enough good quality sleep. Getting 7 to 9 hours of sleep a day lowers your risk for high “bad” cholesterol (LDL) and total cholesterol.
- Limiting alcohol. Visit the National Institute on Alcohol Abuse and Alcoholism for resources on support and treatment to stop drinking.
If you’ve made these important lifestyle changes and your cholesterol levels remain high, your doctor might recommend medication.
- Statins. Statins are the most common medicine used to treat high blood cholesterol. Statins reduce the amount of cholesterol made in your liver. Studies have shown that statins lower the risk of heart attack and stroke in people with high LDL cholesterol. Statins usually don’t cause side effects, but they may raise the risk of diabetes. However, this mainly happens in people already at high risk of diabetes, such as those who have prediabetes, overweight or obesity, or metabolic syndrome. Statins may also cause abnormal results on liver enzymes tests, but actual liver damage is extremely rare. Other rare side effects include muscle damage and cognitive impairment.
- Cholesterol absorption inhibitors. Your small intestine absorbs the cholesterol from your diet and releases it into your bloodstream. The drug ezetimibe (Zetia) helps reduce blood cholesterol by limiting the absorption of dietary cholesterol. Ezetimibe can be used with a statin drug.
- Bempedoic acid. This newer drug works in much the same way as statins but is less likely to cause muscle pain. Adding bempedoic acid (Nexletol) to a maximum statin dosage can help lower LDL significantly. A combination pill containing both bempedoic acid and ezetimibe (Nexlizet) also is available.
- Bile-acid-binding resins. Your liver uses cholesterol to make bile acids, a substance needed for digestion. The medications cholestyramine (Prevalite), colesevelam (Welchol) and colestipol (Colestid) lower cholesterol indirectly by binding to bile acids. This prompts your liver to use excess cholesterol to make more bile acids, which reduces the level of cholesterol in your blood.
- PCSK9 inhibitors are injected under the skin every few weeks and are expensive. Your liver makes the protein, PCSK9. PCSK9 destroys parts of cells in the liver that allow LDL cholesterol to be absorbed. By stopping the PCSK9 protein, these inhibitors can reduce LDL cholesterol levels. These drugs can help the liver absorb more LDL cholesterol, which lowers the amount of cholesterol circulating in your blood. Alirocumab (Praluent) and evolocumab (Repatha) might be used for people who have a genetic condition that causes very high levels of LDL or in people with a history of coronary disease who have intolerance to statins or other cholesterol medications. Your cardiologist may prescribe a PCSK9 inhibitor and a statin if you are at high risk of complications like heart attack or stroke, or if you have familial hypercholesterolemia. In 2021, the United States Food and Drug Administration (FDA) approved the PCSK9 inhibitor, inclisiran (Leqvio) joining the already approved alirocumab (Praluent), for patients with familial hypercholesterolemia 16. The most common side effects are itching, pain, or swelling at the place where you injected it.
If you also have high triglycerides, your doctor might prescribe:
- Fibrates. The medications fenofibrate (Tricor, Fenoglide, others) and gemfibrozil (Lopid) reduce your liver’s production of very-low-density lipoprotein (VLDL) cholesterol and speed the removal of triglycerides from your blood. VLDL cholesterol contains mostly triglycerides. Using fibrates with a statin can increase the risk of statin side effects.
- Niacin. Niacin limits your liver’s ability to produce LDL and VLDL cholesterol. But niacin doesn’t provide additional benefits over statins. Niacin has also been linked to liver damage and strokes, so most doctors now recommend it only for people who can’t take statins.
- Omega-3 fatty acid supplements. Omega-3 fatty acid supplements can help lower your triglycerides. They are available by prescription or over-the-counter. If you choose to take over-the-counter supplements, get your doctor’s OK. Omega-3 fatty acid supplements could affect other medications you’re taking.
- Apo CIII inhibitor (an antisense inhibitor of apo CIII), volanesorsen, is available in some countries. It lowers triglyceride levels in patients with severely elevated triglyceride levels, including people with lipoprotein lipase deficiency. It is given as a weekly injection.
If your doctor or cardiologist prescribes medicines as part of your treatment plan, be sure to continue your healthy lifestyle changes. The combination of the medicines and heart-healthy lifestyle changes can help lower and control your blood cholesterol levels.
Some people with familial hypercholesterolemia (FH) may receive a treatment called lipoprotein apheresis. This treatment uses a filtering machine to remove LDL cholesterol from the blood. Then the machine returns the rest of the blood back to the person.
What is cholesterol?
Cholesterol is a waxy, fat-like substance that’s found in all the cells in your body. Cholesterol is produced by your liver, adrenal glands, intestines, and in gonads and 20 to 25% of cholesterol comes from your diet (foods you eat) 17. Cholesterol is an essential component of all cell membranes – it helps to maintain structural integrity and fluidity of cell membranes, allowing your cells to change shapes easily without cell walls 18. More than 90% of cellular cholesterol is located at the plasma membrane 19. Your body needs some cholesterol to make hormones such as testosterone and estrogen, vitamin D and the biosynthesis of bile acids in your liver that help you digest foods 20, 21, 22.
Cholesterol comes from two sources. Your liver makes all of the cholesterol your body needs to form cell membranes and to make certain hormones. Cholesterol is also found in foods from animal sources, such as egg yolks, meat, and cheese, which is called dietary cholesterol. Although we often blame the cholesterol found in foods that we eat for raising blood cholesterol, the main culprit is actually saturated fat. Foods rich in saturated fat include butter fat in milk products, fat from red meat, and tropical oils such as coconut oil.
Cholesterol travels through your blood on proteins called lipoproteins. One type, LDL (low-density lipoprotein), is sometimes called the “bad” cholesterol. A high LDL level leads to a buildup of cholesterol in your arteries. Another type, HDL (high-density lipoprotein), is sometimes called the “good” cholesterol. HDL carries cholesterol from other parts of your body back to your liver. Then your liver removes the cholesterol from your body.
Types of cholesterol:
- HDL stands for high-density lipoprotein or HDL-C (high-density lipoprotein cholesterol). HDL is sometimes called “good cholesterol” because it carries harmful cholesterol from other parts of your body including your arteries back to your liver. Your liver then removes the cholesterol from your body and helps protect you from heart attack and stroke. A healthy HDL-cholesterol level may protect against heart attack and stroke. If you have low HDL levels, you have a greater heart disease risk, even if your total cholesterol is below 200 mg/dL. Your doctor will evaluate your HDL and other cholesterol levels and other factors to assess your risk for heart attack or stroke. People with high blood triglycerides usually also have lower levels of HDL. Genetic factors, Type 2 diabetes, smoking, being overweight and being sedentary can all lower HDL cholesterol. Women tend to have higher levels of HDL cholesterol than men do, because the female hormone estrogen raises HDL, but this can change after menopause.
- LDL stands for low-density lipoprotein or LDL-C (low-density lipoprotein cholesterol). LDL is sometimes called “bad cholesterol” because a high LDL level leads to the buildup of plaque in your arteries. LDL is the most important lipid for predicting your heart disease risk. Low-density lipoprotein (LDL or ‘bad’) cholesterol can join with fats and other substances to build up (also known as plaque) in the inner walls of your arteries, which starts a disease process called atherosclerosis. The arteries can become clogged and narrow, and blood flow is reduced. When plaque builds up in your coronary arteries that supply blood to your heart, you are at greater risk of having a heart attack. Since LDL is the bad kind of cholesterol, a low LDL level is considered good for your heart health. A diet high in saturated and trans fat is unhealthy because it tends to raise LDL cholesterol levels. Your LDL levels may be high if you eat a diet with a lot of saturated fat, cholesterol, or both. Sometimes, an under-active thyroid called hypothyroidism may also increase LDL levels.
- VLDL stands for very low-density lipoprotein or VLDL-C (very low-density lipoprotein cholesterol). Some people also call VLDL a “bad cholesterol” because it too contributes to the buildup of plaque in your arteries. But VLDL and LDL are different; VLDL mainly carries triglycerides and LDL mainly carries cholesterol. VLDL particles are released into the blood by the liver and circulate in the bloodstream, ultimately being converted into LDL as they lose triglyceride, having carried it to other parts of the body. According to the National Heart, Lung and Blood Institute’s National Cholesterol Education Program Guidelines ATP III, there is growing evidence that VLDL plays an important role in atherogenesis, in which plaques form on the interior walls of arteries, narrowing these passageways and restricting blood flow, which can lead to heart disease and increase the risk of stroke. Currently, direct measurement of VLDL cholesterol requires specialized testing. However, since VLDL-C contains most of the circulating triglyceride (if a person is fasting) and since the composition of the different particles is relatively constant, it is possible to estimate the amount of VLDL-C based on the triglyceride value. To estimate VLDL-C, divide the triglyceride value by 5 if the value is in mg/dL or divide by 2.2 if the value is in mmol/L. In most cases, this formula provides a good estimate of VLDL-C. However, this formula becomes less accurate with increased triglyceride levels when, for example, a person has not fasted before having blood drawn. The calculation is not valid when the triglyceride level is greater than 400 mg/dl (4.5 mmol/L) because other lipoproteins are usually present. In this situation, VLDL-C may be measured directly using specialized testing.
- Triglycerides. Triglycerides are the most common type of fat in your blood. Triglycerides come from food, and your body also makes them. When you eat, your body converts calories it doesn’t need into triglycerides, which are stored in fat cells. Triglycerides are fats that provide energy for your muscles. If you eat foods with a lot of saturated fat or carbohydrates, you will raise your triglyceride levels. High triglyceride levels are associated with several factors, including being overweight, eating too many sweets or drinking too much alcohol, smoking, being sedentary, or having diabetes with elevated blood sugar levels. Elevated triglycerides levels are thought to lead to a greater risk of heart disease, but scientists do not agree that high triglycerides alone are a risk factor for heart disease. Normal triglyceride levels vary by age and sex. People with high triglycerides often have a high total cholesterol level, including a high LDL (bad) cholesterol level and a low HDL (good) cholesterol level. Many people with metabolic syndrome or diabetes also have high triglyceride levels. Extremely high triglyceride levels (more than 1000 mg/dL) can lead to abdominal pain and a life-threatening disorder of the pancreas called pancreatitis. Factors that can contribute to elevated triglyceride levels:
- Overweight or obesity
- Insulin resistance or metabolic syndrome
- Diabetes mellitus, especially with poor glucose control
- Alcohol consumption, especially in excess
- Excess sugar intake, especially from processed foods
- High saturated fat intake
- Hypothyroidism
- Chronic kidney disease
- Physical inactivity
- Pregnancy (especially in the third trimester)
- Inflammatory diseases (such as rheumatoid arthritis, systemic lupus erythematosus
- Some medications may also increase triglycerides.
Your body naturally produces all the LDL (bad) cholesterol it needs. However, the genes you inherit and your lifestyle habits play a major role in your cholesterol levels. The most common cause of high cholesterol is an unhealthy lifestyle. An unhealthy lifestyle makes your body produce more LDL cholesterol than it needs. This can include:
- Unhealthy eating habits or unhealthy diet, such as eating lots of bad fats. One type, saturated fat, is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods. Eating a lot of foods high in saturated fats raises “bad” LDL cholesterol levels. Another type, trans fat, is in some fried and processed foods. Eating these fats can raise your LDL (bad) cholesterol. No more than 10% of your daily calories should come from saturated fats.
- Lack of physical activity, with lots of sitting and little exercise. This lowers your HDL (good) cholesterol.
- Smoking or exposure to tobacco smoke, which lowers HDL cholesterol, especially in women. It also raises your LDL cholesterol.
- Being overweight or obese.
- Stress may raise levels of certain hormones, such as corticosteroids. These can cause your body to make more cholesterol.
- Drinking too much alcohol (more than two drinks a day for men or one drink a day for women) can raise your total cholesterol level.
- Getting little or low-quality sleep has been linked to lower cardiovascular health.
Genetics may also cause people to have high cholesterol. For example, some people inherit genes from their mother, father or even grandparents that cause them to have too much cholesterol. This is called familial hypercholesterolemia (FH). The severity of familial hypercholesterolemia is related to the duration and degree of LDL cholesterol in the blood. Familial hypercholesterolemia is dangerous because it can cause premature atherosclerotic heart disease. If you have a family history of familial hypercholesterolemia or problems related to high cholesterol, get your cholesterol levels checked.
High cholesterol usually causes no signs or symptoms. Cholesterol travels through your blood silently. And it turns into atherosclerotic plaque (hardened deposits) silently. Plaque buildup is like someone tip-toeing on carpet. You might not see or notice its presence for a long time. You may have no symptoms until you have a heart attack or stroke. At that point, the plaque is like high heels on a hardwood floor. And it’s already caused serious damage to your body.
You can live for many years with high cholesterol and not even know it. That’s why it’s essential to get your cholesterol levels checked on a regular basis. If your cholesterol levels are too high (hyperlipidemia), that’s a red flag for you and your doctor. High cholesterol is a major risk factor for heart disease. But catching it early gives you a chance to make changes and get your cholesterol to a healthy level.
You can find out your cholesterol level with a cholesterol or lipid profile blood test. If you are concerned about your cholesterol level, talk to your doctor. You will need to stop eating for 10 to 12 hours before a cholesterol or lipid profile blood test, and the only liquid you may drink is water.
Lifestyle changes such as regular physical activity, losing excess weight, quitting if you smoke and healthy eating are the first line of defense against high cholesterol. Eating lots of fruit and vegetables, whole grains (especially oats), and beans and lentils can help lower your cholesterol. You can also help by losing weight, avoiding foods that are high in saturated fat, quitting smoking and being active. But, if you’ve made these important lifestyle changes and your cholesterol levels remain high, your doctor might recommend medication.
To reduce your risk with high cholesterol, it’s important to:
- Quit cigarette smoking.
- Do regular aerobic exercise.
- Identify and treat high blood pressure.
- Maintain a healthy weight.
- Diagnose and treat diabetes.
- Have a healthy diet.
High cholesterol is one of the major controllable risk factors for coronary heart disease, heart attack and stroke. If you have other risk factors such as smoking, high blood pressure or diabetes, your risk increases even more. The more risk factors you have and the more severe they are, the higher your overall risk.
Remember, making even modest changes now can help to prevent significant medical issues later. Do all you can to reduce your risk for the serious effects of heart attack and stroke.
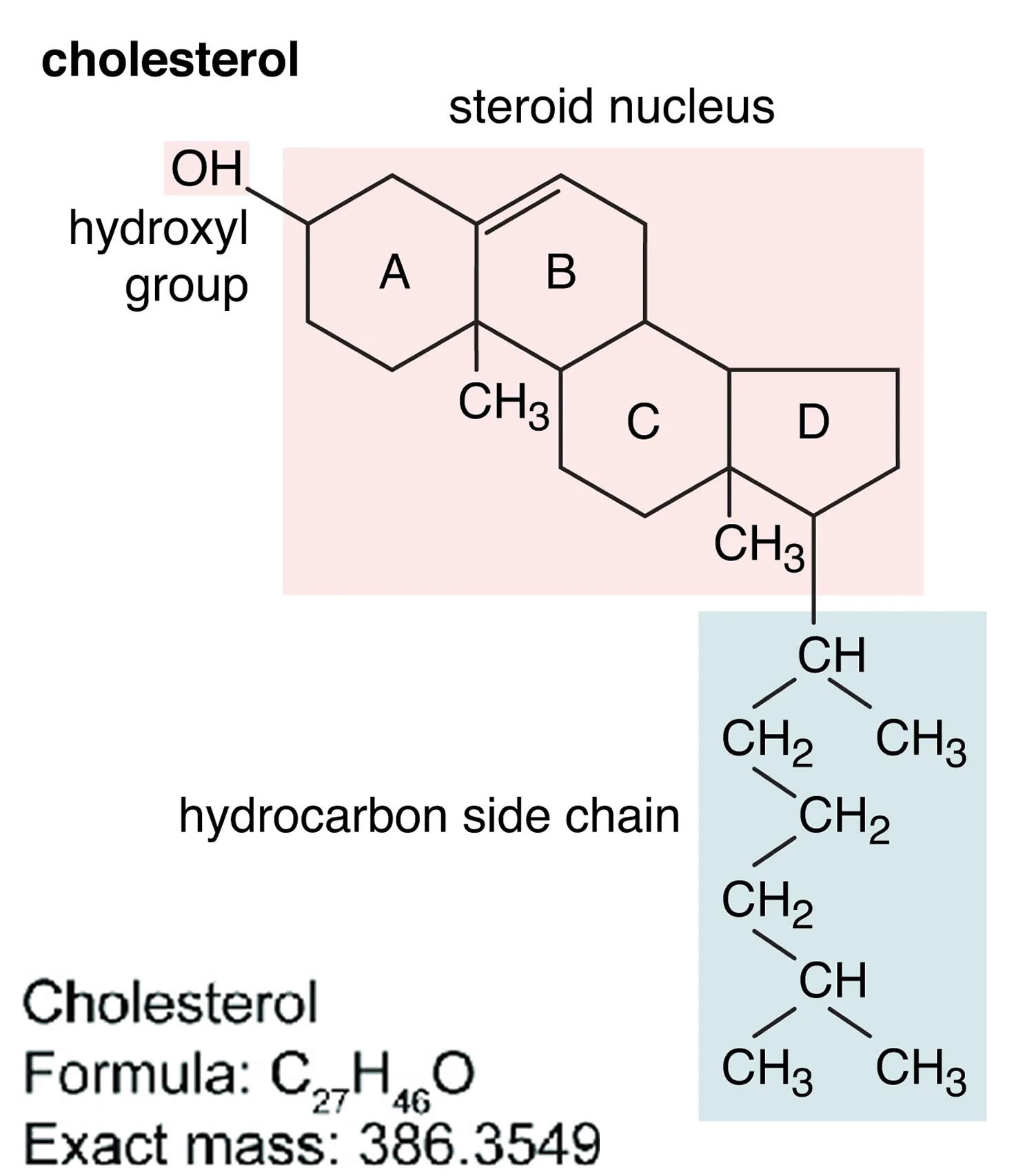
Figure 1. Cholesterol molecular structure
Footnotes: A cholesterol molecule contains three major parts: 1) tetracyclic carbon ring (A, B, C and D) as the core of steroids, 2) polar hydroxyl (OH) group attached to ring A, and 3) short non-polar carbon chain attached to ring D 23, 24. All four rings (A, B, C and D) of the sterol group are in a trans conformation, making cholesterol a planner molecule. The double bond between C5 and C6 helps to keep the rigidity of cholesterol.
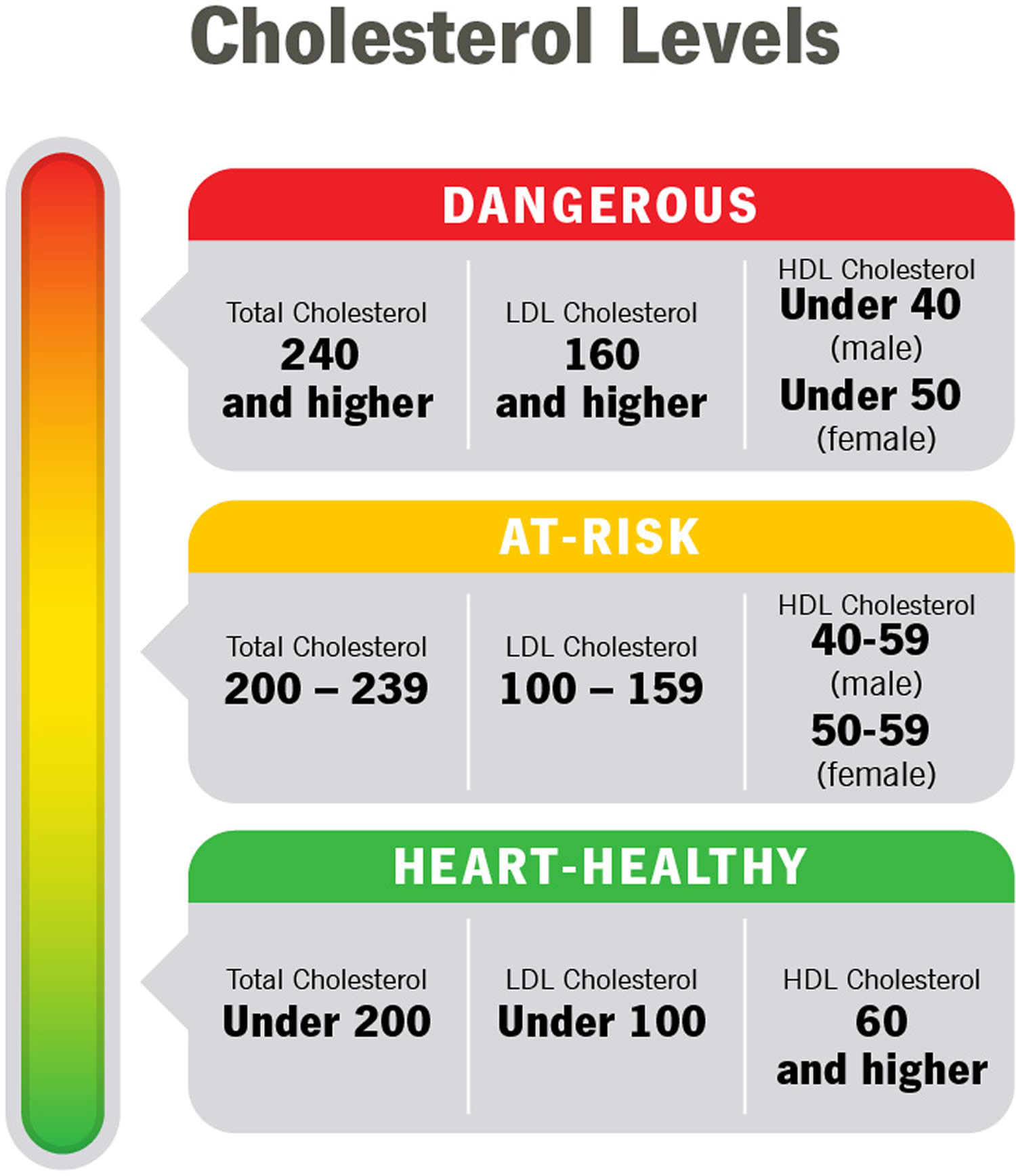
[Source 25 ]What are Cholesterol levels?
Your cholesterol levels show how much cholesterol is circulating in your blood. Your blood cholesterol levels tell you how much lipid or fat is in your blood and your cholesterol levels are expressed in milligrams per deciliter (mg/dL). High cholesterol usually has no symptoms. You can find out your blood cholesterol levels with a cholesterol or lipid profile blood test. You will need to stop eating for 10 to 12 hours before a cholesterol or lipid profile blood test, and the only liquid you may drink is water.
Total blood or serum cholesterol is a composite of different measurements. Your “total blood cholesterol” is calculated by adding your HDL (“good” cholesterol) and LDL (“bad” cholesterol) cholesterol levels, plus 20% of your triglyceride level. Here’s the formula for calculating your “total blood cholesterol”:
Total cholesterol = HDL + LDL + 20% triglycerides.
- “Total cholesterol” is the total amount of cholesterol that’s circulating in your blood. Your “Total cholesterol” should be below 200 milligrams per deciliter of blood (less than 200 mg/dL) or 5.18 mmol/L.
- Your HDL “good” cholesterol is the one number you want to be high, ideally above 60 mg/dL (1.55 mmol/L) or higher.
- Your LDL “bad” cholesterol should be below 100 mg/dL (less than 2.59 mmol/L).
- Your triglycerides should be below 150 mg/dL (less than 1.70 mmol/L). Triglycerides are the most common type of fat in your blood. Triglycerides come from food, and your body also makes them. When you eat, your body converts calories it doesn’t need into triglycerides, which are stored in fat cells. High triglyceride levels are associated with several factors, including being overweight, eating too many sweets or drinking too much alcohol, smoking, being sedentary, or having diabetes with elevated blood sugar levels.
- According to the American Heart Association, more than 43% of American adults have cholesterol levels of 200 milligrams (mg) per deciliter (dL) or higher. Talk with your doctor about what your results mean for you and how to manage your cholesterol.
“Normal cholesterol levels” are less important than your overall cardiovascular risk. Like HDL and LDL cholesterol levels, your total blood cholesterol level should be considered in context with your other known risk factors. To determine your cardiovascular risk, your doctor will consider your cholesterol test results in context with your age, sex and family history. Other risk factors, such as smoking, diabetes and high blood pressure, will be considered as well. If your risk remains uncertain, and treatment options are unclear, your doctor may consider other factors and/or request a coronary artery calcium measurement to provide greater insight into your risk and help in decision-making.
In general, you want to have a total cholesterol level below 200 mg/dL or 5.18 mmol/L. Between 200 mg/dL and 239 mg/dL, your cholesterol level is elevated or borderline-high and should be lowered if you can. With a total cholesterol level of 240 mg/dL or above, your cholesterol level is high, and there is a need for action. For example, changing your diet, beginning an exercise program, and taking statins or other cholesterol-lowering medicines are all ways to lower your cholesterol level.
Factors that can increase your risk of bad cholesterol include:
- Poor diet. Eating saturated fat, found in animal products, and trans fats, found in some commercially baked cookies and crackers and microwave popcorn, can raise your cholesterol level. Foods that are high in cholesterol, such as red meat and full-fat dairy products, will also increase your cholesterol.
- Age. Your cholesterol levels tend to rise as you get older. For instance, as you age, your liver becomes less able to remove LDL cholesterol. Even though it is less common, younger people, including children and teens, can also have high cholesterol.
- Sex. Between ages 20 and 39, men have a greater risk for high total cholesterol than women. A woman’s risk goes up after menopause. Menopause lowers levels of female hormones that may protect against high blood cholesterol. After menopause, women’s levels of total and “bad” LDL cholesterol usually go up, while their levels of “good” HDL cholesterol go down.
- Heredity. High blood cholesterol can run in families.
- Weight. Being overweight or having obesity raises your cholesterol level. Having a body mass index (BMI) of 30 or greater puts you at risk of high cholesterol.
- Race. Certain races may have an increased risk of high cholesterol.
- Overall, non-Hispanic White people are more likely than other groups to have high levels of total cholesterol.
- Asian Americans, including those of Indian, Filipino, Japanese, and Vietnamese descent, are more likely to have high levels of “bad” LDL cholesterol than other groups.
- Hispanic Americans are more likely to have lower levels of “good” HDL cholesterol than other groups.
- African Americans are more likely than other groups to have high levels of “good” HDL cholesterol.
- Lack of exercise. Being physically inactive contributes to overweight and can raise LDL and lower HDL. Exercise helps boost your body’s HDL, or “good,” cholesterol while increasing the size of the particles that make up your LDL, or “bad,” cholesterol, which makes it less harmful.
- Smoking. Cigarette smoking damages the walls of your blood vessels, making them more prone to accumulate fatty deposits. Smoking might also lower your level of HDL, or “good,” cholesterol.
- Diabetes. High blood sugar contributes to higher levels of a dangerous cholesterol called very-low-density lipoprotein (VLDL) and lower HDL cholesterol. High blood sugar also damages the lining of your arteries.
The following foods can lower your bad cholesterol.
- Vegetables such as leafy greens (spinach, collard greens, kale, cabbage), broccoli, and carrots
- Fruits such as apples, bananas, oranges, pears, grapes, and prunes
- Whole grains such as plain oatmeal, brown rice, and whole-grain bread or tortillas
- Fat-free or low-fat dairy foods such as milk, cheese, or yogurt
- Protein-rich foods:
- Fish high in omega-3 fatty acids (salmon, tuna, and trout)
- Lean meats such as 95% lean ground beef or pork tenderloin or skinless chicken or turkey
- Eggs
- Nuts, seeds, and soy products (tofu)
- Legumes such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
- Oils and foods high in monounsaturated and polyunsaturated fats:
- Canola, corn, olive, safflower, sesame, sunflower, and soybean oils (not coconut or palm oil)
- Nuts such as walnuts, almonds, and pine nuts
- Nut and seed butters
- Salmon and trout
- Seeds (sesame, sunflower, pumpkin, or flax)
- Avocados
- Tofu
There are usually no signs or symptoms that you have high cholesterol. A blood test is the only way to detect if you have it. The American Heart Association recommends all adults age 20 or older with no other risk factors for heart disease should have their cholesterol (and other traditional risk factors) checked every four to six years. If certain factors put you at high risk, or if you already have heart disease, your doctor may ask you to check it more often. Work with your doctor to determine your risk for cardiovascular disease and stroke and create a plan to reduce your risk.
If you have risk factors or if previous testing showed that you had a high cholesterol level, more frequent testing with a full lipid panel is recommended.
Examples of risk factors other than high LDL include:
- Cigarette smoking
- Being overweight or obese
- Unhealthy diet
- Being physically inactive—not getting enough exercise
- Age (if you are a male 45 years or older or a female 50-55 years or older)
- Hypertension (blood pressure of 140/90 or higher or taking high blood pressure medications)
- Family history of premature heart disease (heart disease in a first-degree male relative under age 55 or a first-degree female relative under age 65)
- Pre-existing heart disease or already having had a heart attack
- Diabetes or prediabetes
For people who are age 20 or older:
- Younger adults should have the test every 5 years
- Men ages 45 to 65 and women ages 55 to 65 should have it every 1 to 2 years.
Children, teens, and young adults (ages 2 to 24 years old) with no risk factors should have a lipid panel once between the ages of 9 and 11 and again between 17 and 21, according to the American Academy of Pediatrics.
For people who are age 19 or younger:
- The first test should be between ages 9 to 11
- Children should have the test again every 5 years
- Some children may have this test starting at age 2 if there is a family history of high blood cholesterol, heart attack, or stroke.
Children, teens, and young adults with an increased risk of developing heart disease as adults should have earlier and more frequent screening with lipid panels. Some of the risk factors are similar to those in adults and include a family history of heart disease or health problems such as diabetes, high blood pressure, or being overweight. High-risk children should be tested between 2 and 8 years old with a fasting lipid panel, according to the American Academy of Pediatrics.
Children younger than 2 years old are too young to be tested.
Figure 2. Cholesterol levels
Table 1. Normal Cholesterol Levels
| Age | Total cholesterol | Non-HDL cholesterol | LDL (“bad” cholesterol) | HDL (“good” cholesterol) |
|---|---|---|---|---|
| 19 and younger | Below 170 milligrams per deciliter of blood (mg/dL) | Below 120 mg/dL | Below 110 mg/dL | Above 45 mg/dL |
| 20 and older Male | 125 to 200 milligrams per deciliter of blood (mg/dL) | Below 130 mg/dL | Below 100 mg/dL | 40 mg/dL or higher |
| 20 and older Female | 125 to 200 milligrams per deciliter of blood (mg/dL) | Below 130 mg/dL | Below 100 mg/dL | 50 mg/dL or higher |
Footnotes: As you review your results, remember that you want your LDL to be low and your HDL to be high. Ideally, your HDL should be above 60 mg/dL (1.55 mmol/L). It’s the helpful cholesterol. An HDL above 60 mg/dL (greater than 1.55 mmol/L) offers you protection against heart disease.
Table 2. High Cholesterol Levels
| Age | Total cholesterol | Non-HDL cholesterol | LDL (“bad” cholesterol) |
|---|---|---|---|
| 19 and younger | Borderline high: 170-199 mg/dL High: 200 mg/dL or higher | Borderline high: 120-144 mg/dL High: 145 mg/dL or higher | Borderline high: 110-129 mg/dL High: 130 mg/dL or higher |
| 20 and older | Borderline high: 200-239 mg/dL High: 240 mg/dL or higher | High: 130 mg/dL or higher | Near-optimal: 100-129 mg/dL Borderline high: 130-159 mg/dL High: 160-189 mg/dL Very high: 190 mg/dL or higher |
Footnotes: High cholesterol generally means your total cholesterol is 200 mg/dL (greater than 5.18 mmol/L) or higher. But doctors use additional categories like “borderline high” and “near optimal” to break down your results. If your numbers are close to normal levels, they may be easier to manage through lifestyle and dietary changes.
Table 3. Desirable Cholesterol Levels
| Desirable Cholesterol Levels | |
|---|---|
| Total cholesterol | Less than 200 milligrams per deciliter of blood (mg/dL) or 5.18 mmol/L |
| LDL (“bad” cholesterol) | Less than 100 mg/dL (2.59 mmol/L) |
| HDL (“good” cholesterol) | 60 mg/dL (1.55 mmol/L) or higher |
| Triglycerides | Less than 150 mg/dL (1.70 mmol/L) |
Mixed hyperlipidemia cause
Mixed hyperlipidemia is caused by complex interactions between your genes and environmental factors such as an unhealthy diet, medications (amiodarone, glucocorticoids), underactive thyroid (hypothyroidism), uncontrolled diabetes, obesity, chronic kidney disease and/or a sedentary lifestyle 11.
An unhealthy lifestyle is the most common cause of high “bad” LDL cholesterol or low “good” HDL cholesterol. However, genes that you inherit from your parents, other medical conditions, and some medicines may also raise LDL cholesterol levels or lower “good” HDL cholesterol levels.
Any of the following conditions may cause hyperlipidemia or increase your risk of hyperlipidemia:
- Unhealthy eating habits or unhealthy diet, such as eating lots of bad fats. Eating a diet high in saturated fats and cholesterol. saturated fat, is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods. Eating a lot of foods high in saturated fats raises “bad” LDL cholesterol levels. Another type, trans fat, is in some fried and processed foods. Eating these fats can raise your “bad” LDL cholesterol. No more than 10% of your daily calories should come from saturated fats.
- Genetics – your genetic makeup might make it more difficult for your body to remove “bad” LDL cholesterol from your blood or break it down in the liver.
- Taking certain medications, hormonal or glucocorticoids. Some medicines that you take for other health problems can raise your level of “bad” LDL cholesterol or lower your level of “good” HDL cholesterol, including:
- Arrhythmia medicines, such as amiodarone
- Beta-blockers for relieving angina chest pain or treating high blood pressure
- Chemotherapy medicines used to treat cancer
- Diuretics, such as thiazide, to treat high blood pressure
- Immunosuppressive medicines, such as cyclosporine, to treat inflammatory diseases or to prevent rejection after organ transplant
- Retinoids to treat acne
- Steroids, such as prednisone, to treat inflammatory diseases such as lupus, rheumatoid arthritis, and psoriasis
- Medical conditions (diabetes, hypothyroidism, chronic kidney disease, HIV/AIDS, lupus, polycystic ovary syndrome)
- Living a sedentary lifestyle or lack of physical activity, with lots of sitting and little exercise. This lowers your “good” HDL cholesterol.
- Pregnancy
- Excessive alcohol consumption. Drinking more than two drinks a day for men or one drink a day for women can raise your total cholesterol level.
- Smoking or exposure to tobacco smoke, which lowers “good” HDL cholesterol, especially in women. It also raises your “bad” LDL cholesterol.
- Being overweight or obese.
- Stress may raise levels of certain hormones, such as corticosteroids. These can cause your body to make more cholesterol.
- Getting little or low-quality sleep has been linked to lower cardiovascular health.
- Age. Unhealthy levels of cholesterol can affect people of all ages, even young children. However, high cholesterol is most commonly diagnosed in people between ages 40 and 59. As you get older, your body’s metabolism changes. Your liver does not remove “bad” LDL cholesterol as well as it did when you were young. These normal changes may increase your risk for developing high blood cholesterol as you age.
- Race or ethnicity. Your race or ethnicity may affect your risk of high blood cholesterol:
- Overall, non-Hispanic White people are more likely than other groups to have high levels of total cholesterol.
- Asian Americans, including those of Indian, Filipino, Japanese, and Vietnamese descent, are more likely to have high levels of “bad” LDL cholesterol than other groups.
- Hispanic Americans are more likely to have lower levels of “good” HDL cholesterol than other groups.
- African Americans are more likely than other groups to have high levels of “good” HDL cholesterol.
- Gender or sex. Between ages 20 and 39, men have a greater risk for high total cholesterol than women. A woman’s risk goes up after menopause. Menopause lowers levels of female hormones that may protect against high blood cholesterol. After menopause, women’s levels of total and “bad” LDL cholesterol usually go up, while their levels of “good” HDL cholesterol go down.
Risk factors for developing mixed hyperlipidemia
Factors that can increase your risk of mixed hyperlipidemia include:
- Poor diet. Eating too much saturated fat or trans fats can result in unhealthy cholesterol levels. Saturated fats are found in fatty cuts of meat and full-fat dairy products. Trans fats are often found in packaged snacks or desserts.
- Obesity. Having a body mass index (BMI) of 30 or greater puts you at risk of high cholesterol.
- Lack of exercise. Exercise helps boost your body’s HDL, the “good,” cholesterol.
- Smoking. Cigarette smoking may lower your level of HDL, the “good,” cholesterol.
- Alcohol. Drinking too much alcohol can increase your total cholesterol level.
- Age. Even young children can have unhealthy cholesterol, but it’s much more common in people over 40. As you age, your liver becomes less able to remove LDL cholesterol.
Mixed hyperlipidemia prevention
The same heart-healthy lifestyle changes that can lower your cholesterol can help prevent you from having mixed hyperlipidemia in the first place. To help prevent mixed hyperlipidemia, you can 13, 14:
- Eat a low-salt diet that emphasizes fruits, vegetables and whole grains
- Limit the amount of animal fats and use good fats in moderation
- Lose extra pounds and maintain a healthy weight
- Quit smoking
- Exercise on most days of the week for at least 30 minutes. Aim to walk quickly or do something else that will get you a little out of breath for 30 minutes, on at least five days of the week. If you’re short of time, do it in three 10-minute slots.
- Drink alcohol in moderation, if at all
- Manage stress
Looking after your weight and being more active makes it easier for your body to manage your blood sugar levels and help prevent insulin resistance, which can lead to type 2 diabetes. Half of people at risk of type 2 diabetes can reduce their risk or delay the condition developing by eating healthily as well as keeping to a healthy weight and waist size.
Mixed hyperlipidemia symptoms
There are usually no symptoms of mixed dyslipidemia, although very high triglyceride levels can cause sensation of tingling, burning, pricking or prickling (paresthesias), shortness of breath (dyspnea) and confusion 12. But if left untreated, mixed hyperlipidemia can lead to heart attack, stroke and acute pancreatitis (high triglyceride levels > 500 mg/dL [> 5.65 mmol/L]).
Mixed hyperlipidemia is often a hidden risk factor which means it can happen without us knowing until it’s too late. Undiagnosed or untreated mixed hyperlipidemia can lead to serious problems, such as heart attack and stroke. That is why it’s so important to get your cholesterol level checked. Talk to your doctor about your risk and steps you can take to keep your cholesterol levels in a healthy range.
According to the National Heart, Lung and Blood Institute, a person’s first cholesterol screening should occur between the ages of 9 and 11 and then be repeated every five years after that 27. The National Heart, Lung and Blood Institute recommends that cholesterol screenings occur every 1 to 2 years for men ages 45 to 65 and for women ages 55 to 65. People over 65 should receive cholesterol tests annually 27. More-frequent cholesterol testing might be needed if your initial cholesterol test results were abnormal or if you already have coronary artery disease, you’re taking cholesterol-lowering medications or you’re at higher risk of coronary artery disease because you:
- Have a family history of high cholesterol or heart attacks
- Are overweight
- Are physically inactive
- Have diabetes
- Eat an unhealthy diet
- Smoke cigarettes
People undergoing treatment for high cholesterol require regular cholesterol testing to monitor the effectiveness of their treatments.
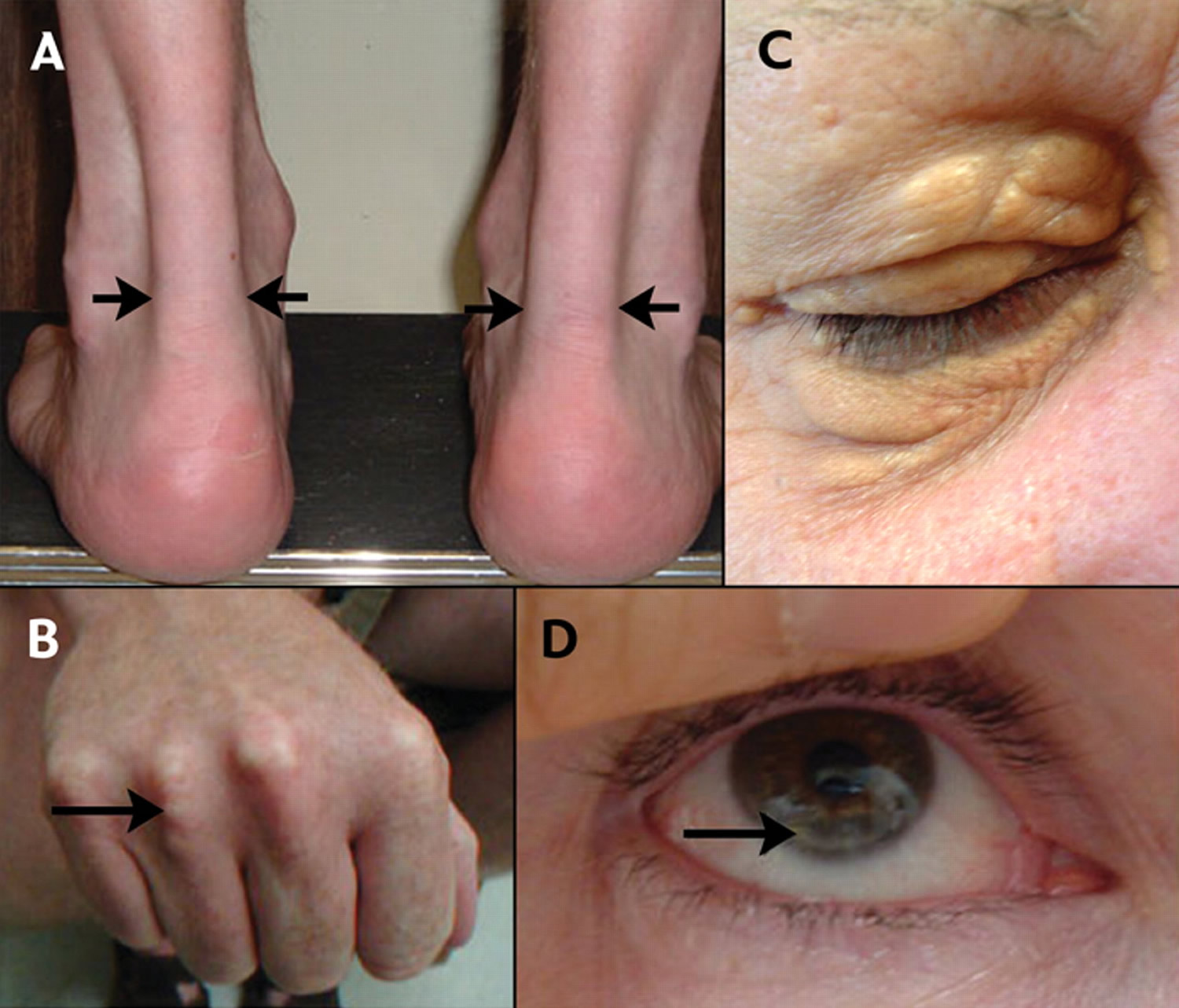
If you have familial hypercholesterolemia, you may have visible signs of high cholesterol. These include:
- Tendon xanthomata – swellings made from cholesterol on the knuckles of your hands, your knees or the Achilles tendon at the back of your ankle.
- Xanthelasmas – small, yellow lumps of cholesterol near the inner corner of your eye.
- Corneal arcus – this is a pale white ring around the colored part of your eye, your iris.
Figure 3. Familial hypercholesterolemia – Physical signs of heterozygous familial hypercholesterolemia, as a result of cholesterol deposition within macrophages in specific sites.
Footnotes: (A) Lateral borders of thickened Achilles’ tendons are shown with arrows. (B) Tendinous xanthomas can also occur in the extensor tendons of the hands (shown), feet, elbows and knees. (C) Xanthelasmas are cholesterol deposits in the eyelids. (D) Arcus cornealis (corneal arcus) is a greyish-white ring of cholesterol infiltration around the corneal rim (arrow). A corneal arcus at a young age can mean that the child has homozygous familial hypercholesterolemia.
Figure 4. Eruptive xanthomas associated with hypertriglyceridemia and new-onset type 2 diabetes
Footnote: Eruptive xanthomas associated with hypertriglyceridemia and new-onset type 2 diabetes. (Panels A and B) A previously healthy, 38-year-old man with a family history of early cerebrovascular accidents presented with a sudden eruption of pink papules with creamy-colored centers on his arms and upper torso. He was otherwise asymptomatic and had no abdominal pain. The results of laboratory tests performed while the patient was fasting included a total cholesterol level of 1268 mg per deciliter (32.8 mmol per liter), a total triglyceride level of 8869 mg per deciliter (100.1 mmol per liter), a glucose level of 241 mg per deciliter (13.4 mmol per liter), and a glycosylated hemoglobin value of 13.4 percent. Triglyceride-lowering therapy with gemfibrozil was initiated to enhance lipoprotein lipase activity, and insulin therapy was initiated to treat the hyperglycemia. Twenty-four hours later, his total triglyceride level was 6466 mg per deciliter (73.0 mmol per liter). At follow-up visits three and five months later, the patient’s eruptive xanthomas had decreased in size and number. After eight months of treatment with gemfibrozil, glyburide, and glucophage, his total cholesterol level was 218 mg per deciliter (5.6 mmol per liter), his total triglyceride level was 302 mg per deciliter (3.4 mmol per liter), and his glycosylated hemoglobin value was 8.3 percent; the eruptive xanthomas had completely resolved.
[Source 28 ]Mixed hyperlipidemia complications
Mixed hyperlipidemia can cause a dangerous accumulation of cholesterol and other deposits on the walls of your arteries (atherosclerosis). These deposits (plaques) can reduce blood flow through your arteries, which can cause complications, such as:
- Chest pain. If the arteries that supply your heart with blood (coronary arteries) are affected, you might have chest pain (angina) and other symptoms of coronary artery disease.
- Heart attack. If plaques tear or rupture, a blood clot can form at the plaque-rupture site — blocking the flow of blood or breaking free and plugging an artery downstream. If blood flow to part of your heart stops, you’ll have a heart attack.
- Stroke. Similar to a heart attack, a stroke occurs when a blood clot blocks blood flow to part of your brain.
- Hypertriglyceridemia is responsible for a mild amount of acute pancreatitis. There is a direct correlation with increased risk of pancreatitis as triglyceride levels rise above 500 mg/dL. When values rise above 1000 mg/dL, there is a described 5% risk of pancreatitis that then doubles when values reach more than 2000 mg/dL.
Mixed hyperlipidemia diagnosis
There are usually no signs or symptoms that you have high cholesterol. A blood test is the only way to detect if you have it. Lipid profile or lipid panel is a blood test that will give you results for your HDL (good) cholesterol, LDL (bad) cholesterol, triglycerides and total blood (or serum) cholesterol. When and how often you should get this test depends on your age, risk factors, and family history. The general recommendations are:
The American Heart Association recommends all adults age 20 or older with no other risk factors for heart disease should have their cholesterol (and other traditional risk factors) checked every four to six years. If certain factors put you at high risk, or if you already have heart disease, your doctor may ask you to check it more often. Work with your doctor to determine your risk for cardiovascular disease and stroke and create a plan to reduce your risk.
If you have risk factors or if previous testing showed that you had a high cholesterol level, more frequent testing with a full lipid panel is recommended.
Examples of risk factors other than high LDL include:
- Cigarette smoking
- Being overweight or obese
- Unhealthy diet
- Being physically inactive—not getting enough exercise
- Age (if you are a male 45 years or older or a female 50-55 years or older)
- Hypertension (blood pressure of 140/90 or higher or taking high blood pressure medications)
- Family history of premature heart disease (heart disease in a first-degree male relative under age 55 or a first-degree female relative under age 65)
- Pre-existing heart disease or already having had a heart attack
- Diabetes or prediabetes
For people who are age 20 or older:
- Younger adults should have the test every 5 years
- Men ages 45 to 65 and women ages 55 to 65 should have it every 1 to 2 years.
Children, teens, and young adults (ages 2 to 24 years old) with no risk factors should have a lipid panel once between the ages of 9 and 11 and again between 17 and 21, according to the American Academy of Pediatrics.
For people who are age 19 or younger:
- The first test should be between ages 9 to 11
- Children should have the test again every 5 years
- Some children may have this test starting at age 2 if there is a family history of high blood cholesterol, heart attack, or stroke.
Children, teens, and young adults with an increased risk of developing heart disease as adults should have earlier and more frequent screening with lipid panels. Some of the risk factors are similar to those in adults and include a family history of heart disease or health problems such as diabetes, high blood pressure, or being overweight. High-risk children should be tested between 2 and 8 years old with a fasting lipid panel, according to the American Academy of Pediatrics.
Children younger than 2 years old are too young to be tested.
Table 4. Cholesterol test general recommendations
| Age Group | Risk Factors | Screening Frequency |
|---|---|---|
| Children | No risk factors | Once between ages 9 to 11; again between 17 to 21 years old |
| Children | One or more | Every 1 to 3 years starting when the risk factor is identified |
| Adolescents and adults of any age | One or more | At least every 5 years; often more frequently based on specific risk factors |
| Males ages 20 to 45 years Females ages 20 to 55 years | No risk factors | Every 4 to 6 years |
| Males ages 45 to 65 years Females ages 55 to 65 years | No risk factors | Every 1 to 2 years |
| People over 65 years | With or without risk factors | Annually |
Footnotes: Having your cholesterol levels checked at regular intervals gives doctors a chance to notice any changes that could become harmful to your health. High or increasing cholesterol levels are a risk factor for heart disease, diabetes, or stroke, among other conditions. Doctors may want to test your cholesterol levels more regularly if you or your family have a history of heart disease, smoking, high blood pressure, type 2 diabetes, obesity, a sedentary lifestyle, or a diet high in saturated fat.
Can I test my cholesterol at home?
At-home cholesterol testing is available to measure total cholesterol. You prick your finger and put blood on a piece of paper that will change color based on your cholesterol level or use your blood and a small device to do the same thing. There are also kits available that have you collect a blood sample at home and then mail it to a reference laboratory, which will then perform a lipid panel and send the results back to you.
There are two types of at-home LDL tests that use a fingerstick blood sample:
- Self-tests: In this kind of test, the analysis of your blood happens at home. This can be done by applying a drop of blood on paper that is then placed into a small device that determines the cholesterol levels. Another type of self-test uses chemically treated paper that indicates the levels of cholesterol in your blood.
- Self-collection: For this kind of test, your blood sample is taken at home but is then sent to a laboratory for analysis.
For help deciding whether an at-home cholesterol test kit is right for you, it may be helpful to talk to your doctor or cardiologist. It is common to have a follow-up cholesterol test performed by a doctor if an at-home cholesterol test kit finds abnormal results.
Your doctor can best help you understand what your specific test results mean for your health. Some doctors may set a specific target level when prescribing medication to lower cholesterol. Factors like diet, age, smoking, physical activity, weight, sex, genetics, medicines, and other medical conditions can all affect your LDL cholesterol level.
How much does at-home cholesterol test cost?
The price may depend on the type of cholesterol test, your insurance coverage, and where the test is performed. You may find it helpful to talk with your doctor about the costs of cholesterol testing.
Blood testing is typically covered by insurance when prescribed by a doctor, but you may be responsible for out-of-pocket costs on copays, deductibles, or technician fees.
Other tests
In some patients, additional tests for secondary causes of mixed hyperlipidemia should be done in most patients with newly diagnosed dyslipidemia and repeated when a component of the lipid profile has inexplicably changed for the worse.
- Lipoprotein-A or Lp(a) levels and C-reactive protein (CRP) levels should be measured in patients with premature atherosclerotic cardiovascular disease, cardiovascular disease (even if they have lower risk lipid levels), or high LDL cholesterol levels refractory to drug therapy. Lipoprotein-A or Lp(a) levels may also be directly measured in patients with borderline-high LDL cholesterol levels to determine whether drug therapy is warranted.
- Measurements of LDL particle number or apoprotein B-100 (apo B) is useful in patients with elevated triglycerides and the metabolic syndrome. Apo B provides similar information to LDL particle number because there is one apo B molecule for each LDL particle. Apo B measurement includes all atherogenic particles, including remnants and Lp(a). Apo B value reflects all non-HDL cholesterol (VLDL, IDL, and LDL) and is more predictive of coronary artery disease risk than LDL cholesterol. Non-HDL cholesterol (Total Cholesterol − HDL cholesterol) is also more predictive of coronary artery disease risk than LDL cholesterol, especially in patients with hypertriglyceridemia.
- Creatinine
- Fasting glucose and/or glycosylated hemoglobin (HbA1C)
- Liver enzymes
- Thyroid-stimulating hormone (TSH)
- Urinary protein
Mixed hyperlipidemia treatment
If you’re diagnosed with mixed hyperlipidemia, your overall health and other risks such as smoking, diabetes or high blood pressure will help guide treatment. The main goal for mixed dyslipidemia treatment is prevention of atherosclerotic cardiovascular disease (ASCVD), including acute coronary syndromes, stroke, transient ischemic attack (TIA), or peripheral arterial disease presumed caused by atherosclerosis.
Initial treatment options for mixed hyperlipidemia include lifestyle changes and statin drug therapy 29, 30, 31. The addition of fibrates to statin therapy is more effective in controlling atherogenic hyperlipidemia in patients with mixed hyperlipidemia than the administration of either drug alone with several short-term studies in various patient populations supporting this hypothesis 32, 33, 34, 35, 36.
If you have high LDL or total cholesterol, you can lower your risk of heart disease by 13, 14, 15:
- Choosing heart-healthy foods. The DASH eating plans can help you lower your “bad” LDL cholesterol. These plans encourage:
- Limiting saturated fats found in fatty cuts of meats, dairy products, and desserts
- Eating whole grains, fruits, and vegetables rather than refined carbohydrates such as sweets and other high-sugar foods
- Eating a variety of nuts
- Preparing foods with little or no salt
- Getting regular physical activity. Studies have shown that physical activity can lower LDL “bad” cholesterol and triglycerides and raise your “good” HDL cholesterol. For example, resistance training among postmenopausal women may decrease total cholesterol, LDL cholesterol, and triglycerides. Aim for at least 30 minutes of exercise on most days. It’s recommended that you do at least 150 minutes of moderate intensity exercise per week. Moderate exercise is when you feel warm and comfortably breathless like when walking or pushing a lawn mower. Intense exercise is when you breathe hard and fast like when running, swimming or cycling. The recommended types of exercise for improving heart health are:
- Aerobic exercise – when you’re moving your body in a way that makes you warm and slightly out of breath like when walking, cycling, doing housework or gardening. Over time, this type of exercise helps your heart and circulatory system to work better by helping to lower your blood pressure and resting heart rate, improving cholesterol levels and helping you maintain a healthy weight
- Balance and flexibility exercise – exercise like yoga, tai chi and Pilates where we hold our bodies in less stable positions. These exercises make sure our muscles don’t get too tight and keep us flexible, helping avoid pain or injury and reduce the risk of having falls
- Resistance exercise – resistance training like lifting weights or using resistance bands and cables to strengthen your muscles. The stronger your muscles are, the harder they can work which takes the strain off your heart making it easier to do everyday tasks. Check in with your doctor before you start any resistance training as it may not be suitable for some people with heart conditions.
- Aiming for a healthy weight. Research has shown that adults with overweight and obesity can lower “bad” LDL cholesterol and raise “good” HDL cholesterol by losing only 3% to 5% of their weight.
- Managing stress. Research has shown that chronic stress can sometimes increase LDL cholesterol levels and decrease HDL cholesterol levels.
- Quitting smoking. If you smoke, quit. Smoking can raise your risk of heart disease and heart attack and worsen other heart disease risk factors. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
- Getting enough good quality sleep. Getting 7 to 9 hours of sleep a day lowers your risk for high “bad” cholesterol (LDL) and total cholesterol.
- Limiting alcohol. Visit the National Institute on Alcohol Abuse and Alcoholism for resources on support and treatment to stop drinking.
If you’ve made these important lifestyle changes and your cholesterol levels remain high, your doctor might recommend medication.
- Statins. Statins are the most common medicine used to treat high blood cholesterol. Statins reduce the amount of cholesterol made in your liver. Studies have shown that statins lower the risk of heart attack and stroke in people with high LDL cholesterol. Statins usually don’t cause side effects, but they may raise the risk of diabetes. However, this mainly happens in people already at high risk of diabetes, such as those who have prediabetes, overweight or obesity, or metabolic syndrome. Statins may also cause abnormal results on liver enzymes tests, but actual liver damage is extremely rare. Other rare side effects include muscle damage and cognitive impairment.
- Cholesterol absorption inhibitors. Your small intestine absorbs the cholesterol from your diet and releases it into your bloodstream. The drug ezetimibe (Zetia) helps reduce blood cholesterol by limiting the absorption of dietary cholesterol. Ezetimibe can be used with a statin drug.
- Bempedoic acid. This newer drug works in much the same way as statins but is less likely to cause muscle pain. Adding bempedoic acid (Nexletol) to a maximum statin dosage can help lower LDL significantly. A combination pill containing both bempedoic acid and ezetimibe (Nexlizet) also is available.
- Bile-acid-binding resins. Your liver uses cholesterol to make bile acids, a substance needed for digestion. The medications cholestyramine (Prevalite), colesevelam (Welchol) and colestipol (Colestid) lower cholesterol indirectly by binding to bile acids. This prompts your liver to use excess cholesterol to make more bile acids, which reduces the level of cholesterol in your blood.
- PCSK9 inhibitors are injected under the skin every few weeks and are expensive. Your liver makes the protein, PCSK9. PCSK9 destroys parts of cells in the liver that allow LDL cholesterol to be absorbed. By stopping the PCSK9 protein, these inhibitors can reduce LDL cholesterol levels. These drugs can help the liver absorb more LDL cholesterol, which lowers the amount of cholesterol circulating in your blood. Alirocumab (Praluent) and evolocumab (Repatha) might be used for people who have a genetic condition that causes very high levels of LDL or in people with a history of coronary disease who have intolerance to statins or other cholesterol medications. Your cardiologist may prescribe a PCSK9 inhibitor and a statin if you are at high risk of complications like heart attack or stroke, or if you have familial hypercholesterolemia. In 2021, the United States Food and Drug Administration (FDA) approved the PCSK9 inhibitor, inclisiran (Leqvio) joining the already approved alirocumab (Praluent), for patients with familial hypercholesterolemia 16. The most common side effects are itching, pain, or swelling at the place where you injected it.
If you also have high triglycerides, your doctor might prescribe:
- Fibrates. The medications fenofibrate (Tricor, Fenoglide, others) and gemfibrozil (Lopid) reduce your liver’s production of very-low-density lipoprotein (VLDL) cholesterol and speed the removal of triglycerides from your blood. VLDL cholesterol contains mostly triglycerides. Using fibrates with a statin can increase the risk of statin side effects.
- Niacin. Niacin limits your liver’s ability to produce LDL and VLDL cholesterol. But niacin doesn’t provide additional benefits over statins. Niacin has also been linked to liver damage and strokes, so most doctors now recommend it only for people who can’t take statins.
- Omega-3 fatty acid supplements. Omega-3 fatty acid supplements can help lower your triglycerides. They are available by prescription or over-the-counter. If you choose to take over-the-counter supplements, get your doctor’s OK. Omega-3 fatty acid supplements could affect other medications you’re taking.
- Apo CIII inhibitor (an antisense inhibitor of apo CIII), volanesorsen, is available in some countries. It lowers triglyceride levels in patients with severely elevated triglyceride levels, including people with lipoprotein lipase deficiency. It is given as a weekly injection.
If your doctor or cardiologist prescribes medicines as part of your treatment plan, be sure to continue your healthy lifestyle changes. The combination of the medicines and heart-healthy lifestyle changes can help lower and control your blood cholesterol levels.
Some people with familial hypercholesterolemia (FH) may receive a treatment called lipoprotein apheresis. This treatment uses a filtering machine to remove LDL cholesterol from the blood. Then the machine returns the rest of the blood back to the person.
Lifestyle changes
Lifestyle changes include:
- Eating a heart-healthy diet
- Becoming more physically active
- Quitting smoking
- Losing weight
- Manage stress
Eating a heart-healthy diet
Some foods are also high in saturated and trans fats. These fats cause your liver to make more cholesterol than it otherwise would. For some people, this added production means they go from a normal cholesterol level to one that’s unhealthy. Some tropical oils – such as palm oil, palm kernel oil and coconut oil – contain saturated fat that can increase bad cholesterol. These oils are often found in baked goods.
From a dietary standpoint, the best way to lower your cholesterol is reduce your intake of saturated fat, trans fat and cholesterol. The American Heart Association recommends limiting saturated fat to less than 6% of daily calories and minimizing the amount of trans fat you eat.
Reducing these fats means limiting your intake of red meat and dairy products made with whole milk. Choose skim milk, low-fat or fat-free dairy products instead. It also means limiting fried food and cooking with healthy oils, such as vegetable oil.
A heart-healthy diet emphasizes fruits, vegetables, whole grains, poultry, fish, nuts and nontropical vegetable oils, while limiting red and processed meats, sodium and sugar-sweetened foods and beverages.
Many diets fit this general description. For example, the DASH (Dietary Approaches to Stop Hypertension) eating plan promoted by the National Heart, Lung, and Blood Institute as well as diets suggested by the U.S. Department of Agriculture and the American Heart Association are heart-healthy approaches. Such diets can be adapted based on your cultural and food preferences.
Becoming more physically active
A sedentary lifestyle lowers HDL cholesterol. Less HDL means there’s less good cholesterol to remove bad cholesterol from your arteries.
Physical activity is important. At least 150 minutes of moderate-intensity aerobic exercise a week is enough to lower both cholesterol and high blood pressure. And you have lots of options: brisk walking, swimming, bicycling or even yard work can fit the bill.
Quitting smoking
Smoking and vaping lowers HDL cholesterol.
Worse still, when a person with unhealthy cholesterol levels also smokes, risk of coronary heart disease increases more than it otherwise would. Smoking also compounds the risk from other risk factors for heart disease, such as high blood pressure and diabetes.
By quitting, smokers can lower their LDL cholesterol and increase their HDL cholesterol levels. It can also help protect their arteries. Nonsmokers should avoid exposure to secondhand smoke.
Losing weight
Being overweight or obese tends to raise bad cholesterol and lower good cholesterol. But a weight loss of as little as 5% to 10% can help improve cholesterol numbers. Losing even 5 to 10 pounds can help lower cholesterol levels.
Managing stress
Research has shown that chronic stress can sometimes raise your LDL cholesterol and lower your HDL cholesterol. Try to reduce your stress. You can do that by deep breathing and relaxation techniques. Examples include meditation and gentle exercise (such as walking or yoga). Also talking with a friend, family member, or health care professional may be helpful.
Medications for high cholesterol
Your doctor might suggest medication to help keep your cholesterol in the healthy range. The choice of medication or combination of medications depends on various factors, including your personal risk factors, your age, your health and possible drug side effects. Common choices include:
- Statins. Statins block a substance your liver needs to make cholesterol. This causes your liver to remove cholesterol from your blood. Statins can also help your body reabsorb cholesterol from built-up deposits on your artery walls, potentially reversing coronary artery disease. Choices include atorvastatin (Lipitor), fluvastatin (Lescol XL), lovastatin (Altoprev), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor). The common side effects of statins are muscle pains and muscle damage, reversible memory loss and confusion, and elevated blood sugar.
- Bile-acid-binding resins. Your liver uses cholesterol to make bile acids, a substance needed for digestion. The medications cholestyramine (Prevalite), colesevelam (Welchol) and colestipol (Colestid) lower cholesterol indirectly by binding to bile acids. This prompts your liver to use excess cholesterol to make more bile acids, which reduces the level of cholesterol in your blood.
- Cholesterol absorption inhibitors. Your small intestine absorbs the cholesterol from your diet and releases it into your bloodstream. The drug ezetimibe (Zetia) helps reduce blood cholesterol by limiting the absorption of dietary cholesterol. Ezetimibe can be used with a statin drug.
- Bempedoic acid. This newer drug works in much the same way as statins but is less likely to cause muscle pain. Adding bempedoic acid (Nexletol) to a maximum statin dosage can help lower LDL significantly. A combination pill containing both bempedoic acid and ezetimibe (Nexlizet) also is available.
- Bile-acid-binding resins. Your liver uses cholesterol to make bile acids, a substance needed for digestion. The medications cholestyramine (Prevalite), colesevelam (Welchol) and colestipol (Colestid) lower cholesterol indirectly by binding to bile acids. This prompts your liver to use excess cholesterol to make more bile acids, which reduces the level of cholesterol in your blood.
- Injectable medications. A newer class of drugs, known as PCSK9 inhibitors, can help the liver absorb more LDL cholesterol — which lowers the amount of cholesterol circulating in your blood. Alirocumab (Praluent) and evolocumab (Repatha) might be used for people who have a genetic condition that causes very high levels of LDL or in people with a history of coronary disease who have intolerance to statins or other cholesterol medications. PCSK9 inhibitors are injected under the skin every few weeks and are expensive.
If you also have high triglycerides (hypertriglyceridemia), your doctor might prescribe:
- Fibrates. Fibrates mostly lower triglycerides and, to a lesser degree, raise HDL levels. Fibrates are less effective in lowering LDL levels. The medications fenofibrate (Tricor, Fenoglide, others) and gemfibrozil (Lopid) reduce your liver’s production of very-low-density lipoprotein (VLDL) cholesterol and speed the removal of triglycerides from your blood. VLDL cholesterol contains mostly triglycerides. Using fibrates with a statin can increase the risk of statin side effects.
- Nicotinic acid also called niacin or vitamin B3. Niacin is the generic name for nicotinic acid (pyridine-3-carboxylic acid), nicotinamide (niacinamide or pyridine-3-carboxamide), and related derivatives, such as nicotinamide riboside 37. Niacin is a water-soluble B3 vitamin that should be taken only under physician supervision. Niacin limits your liver’s ability to produce LDL and VLDL cholesterol. It improves all lipoproteins—total cholesterol, LDL, triglycerides, and HDL—when taken in doses well abovethe vitamin requirement. But niacin doesn’t provide additional benefits over statins. Niacin has also been linked to liver damage and strokes, so most doctors now recommend it only for people who can’t take statins.
- Omega-3 fatty acid supplements. Omega-3 fatty acid supplements can help lower your triglycerides. They are available by prescription or over-the-counter. If you choose to take over-the-counter supplements, get your doctor’s OK. Omega-3 fatty acid supplements could affect other medications you’re taking.
Currently available triglyceride-lowering therapies include fibrates, omega-3 fatty acids and niacin can reduce triglycerides levels up to 45% 38. Primary cholesterol lowering therapies such as statins, ezetimibe, and PCSK9 inhibitors also modestly improve triglyceride levels (averaging 5-25%) 38.
If you are on such medication, you might need regular cholesterol tests to check that they are working well and that you are taking the right dose. If you decide to take cholesterol medication, your doctor might recommend liver function tests to monitor the medication’s effect on your liver.
Experts from the National Cholesterol Education Program (NCEP) say that more aggressive cholesterol treatment is needed for people at high risk of dying from a heart attack or cardiovascular disease. The basic message of the group’s recommendations is the lower the better when it comes to levels of low-density lipoprotein (LDL) or “bad cholesterol”. The updated recommendations say that almost all high-risk patients with LDL cholesterol levels of 100 mg/dL or higher should begin taking cholesterol-lowering medicine.
Table 5. Hypertriglyceridemia medications
| Fibrates | Omega 3 fish oil |
|---|---|
| Gemfibrozil Doses: 300 mg, 600 mg taken twice daily | Omega -3 fatty acids (Epanova) 850 mg polyunsaturated fatty acids, including eicosapentanoic acid (EPA) and docosahexanoic acid (DHA) |
| Fenofibrate Micronizeda 43, 130 mg or 67, 134, 200 mg | Omega 3 ethyl esters (Lovaza, Omacor) 375 mg DHA and 465 mg EPA |
| Bezafibrate (not available in the United States) 200 mg twice daily or 400 mg extended release once daily | Icosapent ethyl (Vascepa) EPA only—0.5 or 1 g |
Lipoprotein apheresis
Some people with familial hypercholesterolemia may benefit from lipoprotein apheresis to lower their blood cholesterol levels. Lipoprotein apheresis uses a filtering machine to remove unwanted substances from the body. The machine removes “bad” LDL cholesterol from the blood, then returns the remainder of the blood to your body.
Treatment in patients with other medical conditions
Treatment of diabetic dyslipidemia should always involve lifestyle changes and statins to reduce LDL cholesterol. To decrease the risk of pancreatitis, fibrates can be used to decrease triglycerides when levels are > 500 mg/dL (> 5.65 mmol/L). Metformin lowers triglycerides, which may be a reason to choose it over other oral antihyperglycemic drugs when treating diabetes. Some Thiazolidinediones (e.g., rosiglitazone and pioglitazone) that help insulin work better at the cell site can increase both HDL cholesterol and LDL cholesterol. Some thiazolidinediones also decrease triglycerides. These antihyperglycemic drugs should not be chosen over lipid-lowering drugs to treat lipid abnormalities in patients with diabetes but may be useful add-ons. Patients with very high triglyceride levels and less than optimally controlled diabetes may have a better response to insulin than to oral antihyperglycemic drugs.
Treatment of dyslipidemia in patients with hypothyroidism, chronic kidney disease, liver disease, or a combination of these disorders involves treating the underlying disorders primarily and lipid abnormalities secondarily. Abnormal lipid levels in patients with low-normal thyroid function (high-normal TSH levels) improve with hormone replacement. Reducing the dosage of or stopping drugs that cause lipid abnormalities should be considered.
Alternative medicine
Few natural products have been proved to reduce cholesterol, but some might be helpful. With your doctor’s OK, consider these cholesterol-lowering supplements and products:
- Barley
- Plant sterols and stanols, found in oral supplements, some fortified orange juices and some margarines, such as Promise Activ
- Blond psyllium, found in seed husk and products such as Metamucil
- Oat bran, found in oatmeal and whole oats
Another popular cholesterol-lowering supplement is red yeast rice. There is evidence that red yeast rice can help lower your LDL cholesterol. Some red yeast rice products contain substances called monacolins, which are produced by the yeast. However, the U.S. Food and Drug Administration (FDA) has said that red yeast rice products that contain monacolin K, a naturally occurring form of the prescription cholesterol-lowering drug lovastatin and can cause the same types of side effects and drug interactions as lovastatin, cannot be sold legally as dietary supplements in the United States. Other red yeast rice products contain little or no monacolin K, and it is not known whether these products have any effect on cholesterol levels. Unfortunately, there is no way to know how much monacolin K is present in most red yeast rice products.
If you buy red yeast rice supplements in the United States, there’s no way to know whether you’re getting enough monacolin K to lower your LDL cholesterol. In other countries, lovastatin in red yeast rice products is potentially dangerous because there’s no way to know how much might be in a particular product or what the quality of the lovastatin is.
- Flaxseed. Studies of flaxseed preparations to lower cholesterol levels report mixed results. A 2009 review of the scientific research of flaxseed for lowering cholesterol found modest improvements in cholesterol, seen more often in postmenopausal women and in people with high initial cholesterol concentrations.
- Garlic. Some evidence indicates that taking garlic supplements can slightly lower blood cholesterol levels. A recent review of the research on garlic supplements concluded that they can lower cholesterol if taken for more than 2 months, but their effect is modest in comparison with the effects of cholesterol-lowering drugs. However, a National Center for Complementary and Integrative Health-funded study on the safety and effectiveness of three garlic preparations (fresh garlic, dried powdered garlic tablets, and aged garlic extract tablets) for lowering blood cholesterol levels found no effect. Although garlic supplements appear to be safe for most adults, they can thin the blood in a manner similar to aspirin, so use caution if you are planning to have surgery or dental work. Garlic supplements have also been found to interfere with the effectiveness of saquinavir, a drug used to treat HIV infection.
- Some soy products can have a small cholesterol-lowering effect. An analysis of data from 35 studies indicated that soy foods were more effective in lowering cholesterol than soy protein supplements and that isoflavones (substances in soy that have a weak estrogenic effect) did not lower cholesterol. The effect of soy is much smaller than that of cholesterol-lowering drugs.
- Limited evidence indicates that green tea may have a cholesterol-lowering effect. The evidence on black tea is less consistent.
- Chromium, vitamin C, artichoke extract, the herb Hibiscus sabdariffa, coenzyme Q10, and selenium have been studied for cholesterol but have not been found to be effective. Research findings don’t show clear evidence regarding the cholesterol-lowering effects of policosanol (derived from sugar cane) and guggulipid (from the mukul mirth tree in western India).
Even if you take cholesterol-lowering supplements, remember the importance of a healthy lifestyle, and take medication to reduce your cholesterol as directed. Tell your doctor which supplements you take.
Monitoring treatment
Lipid levels should be monitored periodically after starting treatment. No data support specific monitoring intervals, but measuring lipid levels 2 to 3 months after starting or changing therapies and once or twice yearly after lipid levels are stabilized is common practice.
Liver and severe muscle toxicity with statin use occurs in 0.5 to 2% of all users. Routine monitoring of liver enzyme levels is not necessary, and routine measurement of creatine kinase (CK) is not useful to predict the onset of rhabdomyolysis. Muscle enzyme levels need not be checked regularly unless patients develop myalgias or other muscle symptoms. If statin-induced muscle damage is suspected, statin use is stopped and creatine kinase (CK) may be measured. When muscle symptoms subside, a lower dose or a different statin can be tried. If symptoms do not subside within 1 to 2 weeks of stopping the statin, another cause should be sought for the muscle symptoms (eg, polymyalgia rheumatica).
Foods for mixed hyperlipidemia
Changing what foods you eat can lower your cholesterol and improve the amount and type of fats floating through your bloodstream. The way that you prepare all of your foods has a huge effect on your health. It’s better to boil, steam or grill them. Different foods lower cholesterol in various ways. Some deliver soluble fiber, which binds cholesterol and its precursors in the digestive system and drags them out of the body before they get into circulation. Some give you polyunsaturated fats, which directly lower the low-density lipoprotein (LDL), the “bad” cholesterol. And some contain plant sterols and stanols, which block the body from absorbing cholesterol.
A major 2012 analysis of several controlled trials involving hundreds of men and women found that dietary changes reduced LDL and total cholesterol and adding aerobic exercise did enhance the lipid-lowering effects of a heart-healthy diet.
A largely vegetarian “dietary portfolio of cholesterol-lowering foods” substantially lowered LDL, triglycerides, and blood pressure. The key dietary components are plenty of fruits and vegetables, whole grains instead of highly refined ones, and protein mostly from plants. Add margarine enriched with plant sterols; oats, barley, psyllium, okra, and eggplant, all rich in soluble fiber; soy protein; and whole almonds.
The American Heart Association recommends a dietary pattern that emphasizes poultry and limits red meat. The amount of saturated fat in meats can vary widely, depending on the cut and how it’s prepared.
Here are some ways to reduce the saturated fat in meat:
- Select lean cuts of meat with minimal visible fat. Lean beef cuts include the round, chuck, sirloin or loin. Lean pork cuts include the tenderloin or loin chop. Lean lamb cuts come from the leg, arm and loin.
- Buy “choice” or “select” grades rather than “prime.” Select lean or extra lean ground beef.
- Trim all visible fat from meat before cooking.
- Broil rather than pan-fry meats such as hamburger, lamb chops, pork chops and steak.
- Use a rack to drain off fat when broiling, roasting or baking. Instead of basting with drippings, keep meat moist with wine, fruit juices or an acceptable oil-based marinade.
- Cook a day ahead of time. Stews, boiled meat, soup stock or other dishes in which fat cooks into the liquid can be refrigerated. Then, remove the hardened fat from the top.
- When a recipe calls for browning the meat first, try browning it under the broiler instead of in a pan.
- Eat chicken and turkey rather than duck and goose, which are higher in fat. Choose white meat most often when eating poultry.
- Remove the skin from chicken or turkey before cooking. If your poultry dries out too much, first try basting with wine, fruit juices or an acceptable oil-based marinade. Or leave the skin on for cooking and remove it before eating.
- Limit processed meats such as sausage, bologna, salami and hot dogs. Many processed meats — even those with “reduced fat” labels — are high in calories and saturated fat. Often they’re high in sodium, too. Read labels carefully and choose processed meats only occasionally.
Eat more fish
Fish can be fatty or lean, but it’s still low in saturated fat. Choose oily fish such as salmon, trout and herring, which are high in omega-3 fatty acids. Prepare fish baked, broiled, grilled or boiled rather than breaded and fried, and without added salt, saturated fat and trans fat. Shrimp and crawfish have more cholesterol than most other types of seafood, but they’re lower in total fat and saturated fat than most meats and poultry.
Eat more fruit and vegetables
Evidence shows that eating fruit and vegetables lowers risk of cardiovascular disease. They are low in saturated fat (many contain no fat at all), high in fiber and low in calories to help you manage your weight. Also, their phytochemicals (natural plant substances), vitamins, minerals and antioxidants help you maintain good health.
Eat more soluble fiber
Wholegrains, peas, beans, lentils, broccoli, apples, berries, prunes and sweet potato contain good amounts of soluble fiber. This helps to regulate cholesterol.
Eat Less meat
Try meatless meals featuring vegetables or beans. For example, think eggplant lasagna, a big grilled portobello mushroom on a bun instead of a burger, or beans-n-weenies without the weenies and salt. Or think of meat as a condiment in casseroles, stews, low-sodium soups and spaghetti — use it sparingly and just for flavor rather than as a main ingredient.
Cook fresh vegetables the heart-healthy way
Try cooking vegetables in a tiny bit of vegetable oil and add a little water during cooking if needed, or use a vegetable oil spray. Just 1 to 2 teaspoons of oil is enough for a package of plain frozen vegetables without sauce or seasonings that serves four. Place in a skillet with tight cover, season and cook over a very low heat until the vegetables are done.
Add herbs and spices to make vegetables even tastier. For example, these combinations add new and subtle flavors:
- Rosemary with peas, cauliflower and squash
- Oregano with zucchini
- Dill with green beans
- Marjoram with Brussels sprouts, carrots and spinach
- Basil with tomatoes
Start with a small quantity (1/8 to 1/2 teaspoon to a package of frozen vegetables), then let your own and your family’s taste be your guide. Chopped parsley and chives, sprinkled on just before serving, also enhance the flavor of many vegetables.
Use liquid vegetable oils in place of solid fats
Liquid vegetable oils such as canola, safflower, sunflower, soybean and olive can often be used instead of solid fats such as butter, lard or shortening. If you must use margarine, try the soft or liquid kind. Use a little liquid oil to:
- Pan-fry fish and poultry.
- Saute vegetables.
- Make cream sauces and soups using low-fat or fat-free milk.
- Add to whipped or scalloped potatoes using low-fat or fat-free milk.
- Brown rice for Spanish, curried or stir-fried rice.
- Cook dehydrated potatoes and other prepared foods that call for fat to be added.
- Make pancakes or waffles.
Puree fruits and veggies for baking
You can replace the oil in muffin, cookie, cake and snack bar recipes with pureed fruits or veggies to give your treats an extra healthy boost. For many recipes, use the specified amount of puree instead of oil. Check the mix’s package or your cookbook’s substitutions page for other conversions. You can:
- Use applesauce in spice muffins or oatmeal cookies.
- Include bananas in breads and muffins.
- Try zucchini in brownies.
Lower dairy fats
Low-fat (1%) or fat-free (skim) milk can be used in many recipes in place of whole milk or half-and-half. Some dishes like puddings may result in a softer set. You can also use low-fat, low-sodium cottage cheese, part-skim milk mozzarella or ricotta and other low-fat, low-sodium cheeses with little or no change in consistency.
Sauces and gravies
Let your cooking liquid cool, then remove the hardened fat before making gravy. Or use a fat separator to pour off the good liquid from cooking stock, leaving the fat behind.
Increase fiber and whole grains (Dietary Fiber at least 14-28 grams per day)
Foods high in fiber can help reduce your risk of heart disease. It’s also good for your digestive tract and for overall health. Further, eating foods rich in fiber can help you feel full on fewer calories, which makes it a good food choice if you need to lose weight.
- Toast and crush or cube fiber-rich whole-grain bread to make breadcrumbs, stuffing or croutons.
- Replace the breadcrumbs in your meatloaf with uncooked oatmeal.
- Serve whole fruit at breakfast in place of juice.
- Use brown rice instead of white rice and try whole grain pasta.
- Add lots of colorful veggies to your salad — carrots, broccoli and cauliflower are high in fiber and give your salad a delicious crunch
Doing this requires a two-pronged strategy:
- Add foods that lower the low-density lipoprotein (LDL), the “bad” cholesterol, the harmful cholesterol-carrying particle that contributes to artery-clogging atherosclerosis.
- At the same time, cut back on foods that boost LDL.
Adding several foods to lower cholesterol in different ways should work better than focusing on one or two. Remember to count your calories
Just as important, a diet that is heavy on fruits, vegetables, beans, and nuts is good for the body in ways beyond lowering cholesterol. It keeps blood pressure in check. It helps arteries stay flexible and responsive. It’s good for bones and digestive health, for vision and mental health.
Eat Nuts
Studies show that eating nuts (e.g., walnuts, almonds and cashews) more regularly can lower cholesterol, as well as your overall cardiovascular disease risk. This is partly because, as well as unsaturated fats, nuts contain plant sterols and stanols, and are high in fibre. Opt for unsalted nuts.
Oatmeal, oat bran, barley and other whole grains and high-fiber foods
Oatmeal and oat bran, barley and other whole grains can help lower the risk of heart disease, mainly via the soluble fiber they deliver. Oatmeal contains soluble fiber called beta-glucan, which forms a gel that binds cholesterol in the body, preventing it from being absorbed into the bloodstream, thus reducing your low-density lipoprotein (LDL) cholesterol, the “bad” cholesterol. Soluble fiber is also found in such foods as kidney beans, apples, pears, barley and prunes. One serving of a breakfast cereal with oatmeal or oat bran provides 3 to 4 grams of fiber.
Soluble fiber can reduce the absorption of cholesterol into your bloodstream. Five to 10 grams or more of soluble fiber a day decreases your total and LDL cholesterol. Eating 1 1/2 cups of cooked oatmeal provides 6 grams of fiber. At least three 1-ounce servings a day. If you add fruit, such as bananas, you’ll add about 4 more grams of fiber. To mix it up a little, try steel-cut oatmeal or cold cereal made with oatmeal or oat bran.
Fish and omega-3 fatty acids
Eating fatty fish can be heart healthy because of its high levels of omega-3 fatty acids, which can reduce your blood pressure and risk of developing blood clots. Fatty fish has high levels of omega-3 fatty acids, which can reduce your triglycerides — a type of fat found in blood — as well as reduce your blood pressure and risk of developing blood clots. In people who have already had heart attacks, omega-3 fatty acids may reduce the risk of sudden death.
Omega-3 fatty acids don’t affect LDL cholesterol levels. But because of omega-3 fatty acids’ other heart benefits, the American Heart Association recommends eating at least two servings of fish a week (at least two 3.5-ounce servings a week). People with diabetes are recommended to also eat two portions of fish a week (at least two 3.5-ounce servings a week). Baking or grilling the fish avoids adding unhealthy fats.
The highest levels of omega-3 fatty acids are in:
- Mackerel
- Lake trout
- Herring
- Sardines
- Albacore tuna
- Salmon
- Halibut
You should bake or grill the fish to avoid adding unhealthy fats. If you don’t like fish, you can also get small amounts of omega-3 fatty acids from foods such as ground flaxseed or canola oil.
Foods such as walnuts, flaxseed and canola oil also have small amounts of omega-3 fatty acids.
Omega-3 and fish oil supplements are available. You can take an omega-3 or fish oil supplement to get some of the benefits, but you won’t get other nutrients in fish, such as selenium. If you decide to take a supplement, talk to your doctor about how much you should take.
Almonds and other nuts
Almonds, peanuts and other tree nuts can improve blood cholesterol. Walnuts are especially high in omega-3 fatty acids, the same heart-healthy fat found in oily fish, but are a lot easier to stash in your pocket or purse. A recent study concluded that a diet supplemented with walnuts can lower the risk of heart complications in people with history of a heart attack. Eating about a handful (1.5 ounces, or 42.5 grams) a day of most nuts, such as almonds, hazelnuts, peanuts, pecans, some pine nuts, pistachio nuts and walnuts, may reduce your risk of heart disease. Make sure the nuts you eat aren’t salted or coated with sugar.
Eating 2 ounces of nuts a day can slightly lower LDL, on the order of 5%. Nuts have additional nutrients that protect the heart in other ways.
All nuts are high in calories, so a handful added to a salad or eaten as a snack will do. To avoid eating too many nuts and gaining weight, replace foods high in saturated fat with nuts. For example, instead of using cheese, meat or croutons in your salad, add a handful of walnuts or almonds.
All nuts will go bad (rancid) in time so keep them in the fridge. The same goes for nut oils and nut butters in jars after you’ve opened them. Rancid nuts have an unpleasant smell and bitter taste.
Apples, grapes, strawberries, citrus fruits
Pears and apples have a lot of pectin, which is a type of fiber that can lower cholesterol. So do citrus fruits like oranges and lemons. Berries are also high in fiber.
Eggplant and okra
These two low-calorie vegetables are good sources of soluble fiber.
Avocados
Avocados are a potent source of nutrients as well as monounsaturated fatty acids (MUFAs). Research suggests that adding an avocado a day to a heart-healthy diet can help improve LDL cholesterol levels in people who are overweight or obese.
People tend to be most familiar with avocados in guacamole, which usually is eaten with high-fat corn chips. Try adding avocado slices to salads and sandwiches or eating them as a side dish. Also try guacamole with raw cut vegetables, such as cucumber slices.
Replacing saturated fats, such as those found in meats, with monounsaturated fatty acids (MUFAs) are part of what makes the Mediterranean diet heart healthy.
Olive oil
Another good source of monounsaturated fatty acids (MUFAs) is olive oil. Try using about 2 tablespoons (23 grams) of olive oil a day in place of other fats in your diet to get its heart-healthy benefits. To add olive oil to your diet, you can saute vegetables in it, add it to a marinade or mix it with vinegar as a salad dressing. You can also use olive oil as a substitute for butter when basting meat or as a dip for bread.
Vegetable oils
Using liquid vegetable oils such as canola, sunflower, safflower, and others in place of butter, lard, or shortening when cooking or at the table helps lower LDL cholesterol.
Foods with added plant sterols or stanols
There is evidence that foods that contain certain added ingredients, such as plant sterols and stanols, can reduce levels of cholesterol in the blood. Sterols and stanols are substances found in plants that help block the absorption of cholesterol. Plant sterols and stanols are found in nuts, seeds and legumes, vegetable oils, breads and cereals, and fruits and vegetables. You need to eat 2 to 3 grams a day of plant sterols and stanols to assist in reducing high cholesterol. To work well, they need to be eaten regularly at meal times. Eating more is not harmful, but you won’t get any additional benefits. Sterols and stanols are also safe to use alongside medications such as statins or fibrates.
Foods that have been fortified with sterols or stanols are available.
Margarines, low-fat milks, low-fat yogurts and breakfast cereals, lower fat cheese, processed cheese and orange juice with added plant sterols can help reduce LDL cholesterol. Adding 2 grams of sterol to your diet every day can lower your LDL cholesterol by 5 to 15 percent. The amount of daily plant sterols needed for results is at least 2 grams — which equals about two 8-ounce (237-milliliter) servings of plant sterol-fortified orange juice a day. People who do not have high cholesterol should not eat these products regularly, particularly children and pregnant or breastfeeding women.
If you do eat foods that are designed to lower cholesterol, read the label carefully to avoid eating too much.
You should not eat foods fortified with plant sterols as a substitute for medication. You can use plant sterol-enriched foods while taking cholesterol medication, but check with your doctor first.
However, it’s not clear whether food with plant sterols or stanols reduces your risk of heart attack or stroke — although experts assume that foods that reduce cholesterol do reduce the risk. Plant sterols or stanols don’t appear to affect levels of triglycerides or of high-density lipoprotein (HDL) cholesterol, the “good” cholesterol.
Whey protein
Whey protein, which is one of two proteins in dairy products — the other is casein — may account for many of the health benefits attributed to dairy. Studies have shown that whey protein given as a supplement lowers both LDL and total cholesterol as well as blood pressure. You can find whey protein powders in health food stores and some grocery stores. Follow the package directions for how to use them.
Soy
Eating soybeans and foods made from them, like tofu and soy milk, was once touted as a powerful way to lower cholesterol. Analyses show that the effect is more modest — consuming 25 grams of soy protein a day (10 ounces of tofu or 2 1/2 cups of soy milk) can lower LDL by 5% to 6%.
Beans
Black beans, kidney beans, lentils. All are rich in soluble fiber, which binds to cholesterol in the blood and moves it out of the body. Recent studies show eating 4.5 ounces of beans a day can reduce LDL levels by 5 percent. Try black bean burritos, or dip some veggies in hummus, which is made with chickpeas, for an afternoon snack.
Fiber supplements
Supplements offer the least appealing way to get soluble fiber. Two teaspoons a day of psyllium, which is found in Metamucil and other bulk-forming laxatives, provide about 4 grams of soluble fiber.
Limiting saturated fats and trans fats
Getting the full benefit of these foods requires other changes to your diet and lifestyle. One of the most beneficial changes is limiting the saturated and trans fats you eat.
- Saturated fats — such as those in meat, butter, cheese and other full-fat dairy products — raise your total cholesterol. Decreasing your consumption of saturated fats to less than 7 percent of your total daily calorie intake can reduce your LDL cholesterol by 8 to 10 percent.
- Trans fats, sometimes listed on food labels as “partially hydrogenated vegetable oil,” are often used in margarines and store-bought cookies, crackers and cakes. Trans fats raise overall cholesterol levels. The Food and Drug Administration (FDA) has banned the use of partially hydrogenated vegetable oils by 1 January 2021.
Foods To Avoid or Consume in Moderation
- Animal products high in saturated fat (beef, lamb, veal, pork, duck, goose, cream, cheese, butter, egg yolk)
- Fried foods
- High-fat processed meats, such as hot dogs and sausages
- Simple sugars (found in soft drinks, candy, cakes, cookies and other baked goods)
- Saturated oils, such as coconut and palm oil
- Shortening, partially hydrogenated margarine and lard
Although some fats are healthy, you need to limit the saturated and trans fats you eat. Saturated fats, like those in meat, butter, cheese and other full-fat dairy products, and some oils, raise your total cholesterol. Trans fats, often used in margarines and store-bought cookies, crackers and cakes, are particularly bad for your cholesterol levels. Trans fats raise LDL cholesterol, and lower high-density lipoprotein (HDL), the “good” cholesterol.
Food labels report the content of trans fats, but, unfortunately, only in foods that contain at least one gram per serving. That means you could be getting some trans fats in a number of foods, which could add up to enough trans fats in a day to be unhealthy and increase cholesterol. If a food label lists “partially hydrogenated oil,” it has trans fat, and it’s best to avoid it.
In addition to changing your diet, making other heart-healthy lifestyle changes is key to improving your cholesterol. Exercising, quitting smoking and maintaining a healthy weight will help keep your cholesterol at a healthy level.
Foods to avoid with high cholesterol
You can lower cholesterol over time by eating fewer of the foods that cause high cholesterol and more of the foods that lower cholesterol.
Saturated fats are found in all animal foods and some plant sources. You can reduce the amount of saturated fat in your food and have a healthy diet.
The following foods may be high in saturated fats. Many of them are also low in nutrients and have extra calories from sugar:
- Baked goods (cake, doughnuts, Danish)
- Fried foods (fried chicken, fried seafood, French fries)
- Fatty cuts of meat or processed meats (bacon, sausage, chicken with skin, cheeseburger, steak)
- Whole-fat dairy products (butter, ice cream, pudding, cheese, whole milk)
- Solid fats such as coconut oil, palm, and palm kernel oils (found in packaged foods)
Here are some examples of popular food items with the saturated fat content in a typical serving:
- 12 ounces (oz) or 340 g, steak — 20 g
- Cheeseburger — 10 g
- Vanilla shake — 8 g
- 1 tbsp (15 mL) butter — 7 g
It is fine to treat yourself to these types of foods once in a while. But, it is best to limit how often you eat them and limit portion sizes when you do.
You can cut how much saturated fat you eat by substituting healthier foods for less healthy options. Replace foods high in saturated fats with foods that have polyunsaturated and monounsaturated fats. Here is how to get started:
- Replace red meats with skinless chicken or fish a few days a week.
- Use canola or olive oil instead of butter and other solid fats.
- Replace whole-fat dairy with low-fat or nonfat milk, yogurt, and cheese.
- Eat more fruits, vegetables, whole grains, and other foods with low or no saturated fat.
Trans fats are made when food makers turn liquid oils into solid fats, like shortening or margarine. Trans fats can be found in many fried, “fast” packaged, or processed foods, including:
- Anything fried and battered
- Shortening and stick margarine
- Cakes, cake mixes, pies, pie crust, and doughnuts
Animal foods, such as red meats and dairy, have small amounts of trans fats. But most trans fats come from processed foods.
Trans fats are found in many processed and packaged foods. Note that these foods are often low in nutrients and have extra calories from sugar:
- Cookies, pies, cakes, biscuits, sweet rolls, and donuts
- Breads and crackers
- Frozen foods, such as frozen dinners, pizza, ice cream, frozen yogurt, milk shakes, and pudding
- Snack foods
- Fast food
- Solid fats, such as shortening and margarine
- Nondairy creamer
Not all packaged foods have trans fats. It depends on the ingredients that were used. That is why it is important to read labels.
While it is fine to treat yourself to sweets and other high-fat foods once in a while, it is best to avoid food with trans fats completely.
You can cut how much trans fat you eat by substituting healthier foods for less healthy options. Replace foods high in trans and saturated fats with foods that have polyunsaturated and monounsaturated fats. Here is how to get started:
- Use safflower or olive oil instead of butter, shortening, and other solid fats.
- Switch from solid margarine to soft margarine.
- Ask what type of fats foods are cooked in when you eat out at restaurants.
- Avoid fried, packaged, and processed foods.
- Replace meats with skinless chicken or fish a few days a week.
- Replace whole-fat diary with low-fat or nonfat milk, yogurt, and cheese.
Mixed hyperlipidemia prognosis
Mixed hyperlipidemia can lead to hardening of your arteries or atherosclerosis. This occurs when fat, cholesterol, and other substances build up in the walls of arteries and form hard structures called plaques. The biggest risk of high cholesterol is Atherosclerotic Cardiovascular Disease (ASCVD) is caused by plaque buildup in arterial walls and refers to conditions that include:
- Coronary heart disease (coronary artery disease), such as heart attack (myocardial infarction), angina, and coronary artery stenosis.
- Cerebrovascular disease, such as a transient ischemic attack, ischemic stroke, and carotid artery stenosis.
- Peripheral artery disease (PAD), such as claudication.
- Aortic atherosclerotic disease, such as abdominal aortic aneurysm and descending thoracic aneurysm.
People with insulin resistance or type 2 diabetes are more likely to develop and die from cardiovascular diseases, such as heart attacks, strokes and heart failure. People with diabetes may avoid or delay heart and blood vessel disease by managing their risk factors.
If your lifestyle is altered, then there is a significant improvement in body weight, hypertension, and diabetes. Cessation of smoking is also very important in improving outcomes. Countless studies have shown that when high cholesterol is appropriately managed, the outcomes are good 39, 40.
Furthermore, since the introduction of the cholesterol lowering drug called statins, the mortality associated with high cholesterol has significantly decreased in many trials 41. Today, cholesterol-lowering is a useful strategy for the primary prevention of heart disease.
- Miller M, Dolinar C, Cromwell W, Otvos JD. Effectiveness of high doses of simvastatin as monotherapy in mixed hyperlipidemia. Am J Cardiol. 2001 Jan 15;87(2):232-4, A9. https://doi.org/10.1016/S0002-9149(00)01327-8[↩]
- Lewis B. Classification of lipoproteins and lipoprotein disorders. J Clin Pathol Suppl (Assoc Clin Pathol). 1973;5:26-31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1436097/pdf/jcpsuppasso00009-0031.pdf[↩]
- Miller M. Managing mixed dyslipidemia in special populations. Prev Cardiol. 2010 Spring;13(2):78-83. doi: 10.1111/j.1751-7141.2009.00057.x[↩]
- Rehman HU. The work-up for mixed hyperlipidemia: a case study. J Fam Pract. 2012 Mar;61(3):133-6. https://www.mdedge.com/familymedicine/article/64659/cardiology/work-mixed-hyperlipidemia-case-study[↩]
- Wu L, Parhofer KG. Diabetic dyslipidemia. Metabolism. 2014 Dec;63(12):1469-79. https://doi.org/10.1016/j.metabol.2014.08.010[↩]
- Goldstein JL, Schrott HG, Hazzard WR, Bierman EL, Motulsky AG. Hyperlipidemia in coronary heart disease. II. Genetic analysis of lipid levels in 176 families and delineation of a new inherited disorder, combined hyperlipidemia. J Clin Invest. 1973 Jul;52(7):1544-68. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC302426/pdf/jcinvest00183-0022.pdf[↩][↩]
- de Graaf J, Stalenhoef AF. Defects of lipoprotein metabolism in familial combined hyperlipidaemia. Curr Opin Lipidol. 1998 Jun;9(3):189-96. doi: 10.1097/00041433-199806000-00002[↩]
- Szapary PO, Rader DJ. The triglyceride-high-density lipoprotein axis: an important target of therapy? Am Heart J. 2004 Aug;148(2):211-21. doi: 10.1016/j.ahj.2004.03.037[↩]
- Farnier M, Picard S. Diabetes: statins, fibrates, or both? Curr Atheroscler Rep. 2001 Jan;3(1):19-28. doi: 10.1007/s11883-001-0006-y[↩]
- Best JD, O’Neal DN. Diabetic dyslipidaemia: current treatment recommendations. Drugs. 2000 May;59(5):1101-11. doi: 10.2165/00003495-200059050-00006[↩]
- Ballantyne CM, Grundy SM, Oberman A, Kreisberg RA, Havel RJ, Frost PH, Haffner SM. Hyperlipidemia: diagnostic and therapeutic perspectives. J Clin Endocrinol Metab. 2000 Jun;85(6):2089-112. doi: 10.1210/jcem.85.6.6642-1[↩][↩]
- Dyslipidemia. https://www.msdmanuals.com/professional/endocrine-and-metabolic-disorders/lipid-disorders/dyslipidemia[↩][↩]
- Khera A. The New 2018 Cholesterol Guidelines. Circulation. 2019 Jun 18;139(25):2805-2808. doi: 10.1161/CIRCULATIONAHA.118.038629[↩][↩][↩]
- Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Sep 10;140(11):e596-e646. doi: 10.1161/CIR.0000000000000678. Epub 2019 Mar 17. Erratum in: Circulation. 2019 Sep 10;140(11):e649-e650. doi: 10.1161/CIR.0000000000000725. Erratum in: Circulation. 2020 Jan 28;141(4):e60. doi: 10.1161/CIR.0000000000000755. Erratum in: Circulation. 2020 Apr 21;141(16):e774. doi: 10.1161/CIR.0000000000000771[↩][↩][↩]
- Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Sep 10;140(11):e563-e595. doi: 10.1161/CIR.0000000000000677. Epub 2019 Mar 17. Erratum in: Circulation. 2019 Sep 10;140(11):e647-e648. doi: 10.1161/CIR.0000000000000724. Erratum in: Circulation. 2020 Jan 28;141(4):e59. doi: 10.1161/CIR.0000000000000754. Erratum in: Circulation. 2020 Apr 21;141(16):e773. doi: 10.1161/CIR.0000000000000770[↩][↩]
- FDA approves add-on therapy to lower cholesterol among certain high-risk adults. https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-add-therapy-lower-cholesterol-among-certain-high-risk-adults[↩][↩]
- Norum KR, Berg T, Helgerud P, Drevon CA. Transport of cholesterol. Physiol Rev. 1983 Oct;63(4):1343-419. https://doi.org/10.1152/physrev.1983.63.4.1343[↩]
- Maekawa M, Fairn GD. Complementary probes reveal that phosphatidylserine is required for the proper transbilayer distribution of cholesterol. J Cell Sci. 2015;128:1422–33. doi: 10.1242/jcs.164715[↩]
- Goluszko P, Nowicki B. Membrane cholesterol: a crucial molecule affecting interactions of microbial pathogens with mammalian cells. Infect Immun. 2005;73:7791–6. doi: 10.1128/IAI.73.12.7791-7796.2005[↩]
- Mauvais-Jarvis F, editor. Sex and gender factors affecting metabolic homeostasis, diabetes and obesity. Vol. 1043. Cham: Springer International Publishing; 2017.[↩]
- Faridi KF, Lupton JR, Martin SS, Banach M, Quispe R, Kulkarni K, et al. Vitamin D deficiency and non-lipid biomarkers of cardiovascular risk. Arch Med Sci. 2017;13:732–7. doi: 10.5114/aoms.2017.68237[↩]
- Boyer JL. Bile formation and secretion. Compr Physiol. 2013 Jul;3(3):1035-78. doi: 10.1002/cphy.c120027[↩]
- Zhou Y, Briand V, Sharma N, Ahn S, Kasi R. Polymers comprising cholesterol: synthesis, self-assembly, and applications. Materials (Basel) 2009;2:636–60. doi: 10.3390/ma2020636[↩]
- Song Y, Kenworthy AK, Sanders CR. Cholesterol as a co-solvent and a ligand for membrane proteins. Protein Sci. 2014;23:1–22. doi: 10.1002/pro.2385[↩]
- Li LH, Dutkiewicz EP, Huang YC, Zhou HB, Hsu CC. Analytical methods for cholesterol quantification. J Food Drug Anal. 2019 Apr;27(2):375-386. doi: 10.1016/j.jfda.2018.09.001[↩]
- National Cholesterol Education Program. Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. https://www.nhlbi.nih.gov/files/docs/guidelines/atp3xsum.pdf[↩]
- Blood Cholesterol Diagnosis. https://www.nhlbi.nih.gov/health/blood-cholesterol/diagnosis[↩][↩]
- Nayak KR, Daly RG. Images in clinical medicine. Eruptive xanthomas associated with hypertriglyceridemia and new-onset diabetes mellitus. N Engl J Med. 2004 Mar 18;350(12):1235. doi: 10.1056/NEJMicm030676[↩]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002 Dec 17;106(25):3143-421.[↩]
- Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, Kastelein JJ, Bittner V, Fruchart JC; Treating to New Targets Investigators. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007 Sep 27;357(13):1301-10. doi: 10.1056/NEJMoa064278[↩]
- Miller M, Cannon CP, Murphy SA, Qin J, Ray KK, Braunwald E; PROVE IT-TIMI 22 Investigators. Impact of triglyceride levels beyond low-density lipoprotein cholesterol after acute coronary syndrome in the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2008 Feb 19;51(7):724-30. doi: 10.1016/j.jacc.2007.10.038[↩]
- Vasilios G. Athyros, Athanasios A. Papageorgiou, Valasia V. Athyrou, Dimokritos S. Demitriadis, Athanasios G. Kontopoulos; Atorvastatin and Micronized Fenofibrate Alone and in Combination in Type 2 Diabetes With Combined Hyperlipidemia. Diabetes Care 1 July 2002; 25 (7): 1198–1202. https://doi.org/10.2337/diacare.25.7.1198[↩]
- Grundy SM, Vega GL, Yuan Z, Battisti WP, Brady WE, Palmisano J. Effectiveness and tolerability of simvastatin plus fenofibrate for combined hyperlipidemia (the SAFARI trial). Am J Cardiol. 2005 Feb 15;95(4):462-8. doi: 10.1016/j.amjcard.2004.10.012. Erratum in: Am J Cardiol. 2006 Aug 1;98(3):427-8.[↩]
- Koh KK, Quon MJ, Han SH, Chung WJ, Ahn JY, Seo YH, Choi IS, Shin EK. Additive beneficial effects of fenofibrate combined with atorvastatin in the treatment of combined hyperlipidemia. J Am Coll Cardiol. 2005 May 17;45(10):1649-53. https://doi.org/10.1016/j.jacc.2005.02.052[↩]
- Durrington PN, Tuomilehto J, Hamann A, Kallend D, Smith K. Rosuvastatin and fenofibrate alone and in combination in type 2 diabetes patients with combined hyperlipidaemia. Diabetes Res Clin Pract. 2004 May;64(2):137-51. doi: 10.1016/j.diabres.2003.11.012[↩]
- Vega GL, Ma PT, Cater NB, Filipchuk N, Meguro S, Garcia-Garcia AB, Grundy SM. Effects of adding fenofibrate (200 mg/day) to simvastatin (10 mg/day) in patients with combined hyperlipidemia and metabolic syndrome. Am J Cardiol. 2003 Apr 15;91(8):956-60. doi: 10.1016/s0002-9149(03)00111-5[↩]
- Kirkland JB. Niacin. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease, 11th ed. Baltimore, MD: Williams & Wilkins; 2014:331-40.[↩]
- Savitha Subramanian, Approach to the Patient With Moderate Hypertriglyceridemia, The Journal of Clinical Endocrinology & Metabolism, Volume 107, Issue 6, June 2022, Pages 1686–1697, https://doi.org/10.1210/clinem/dgac085[↩][↩][↩]
- Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson AM, Zethelius B, Miftaraj M, McGuire DK, Rosengren A, Gudbjörnsdottir S. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2018 Aug 16;379(7):633-644. doi: 10.1056/NEJMoa1800256[↩]
- Gorina M, Limonero JT, Álvarez M. Effectiveness of primary healthcare educational interventions undertaken by nurses to improve chronic disease management in patients with diabetes mellitus, hypertension and hypercholesterolemia: A systematic review. Int J Nurs Stud. 2018 Oct;86:139-150. doi: 10.1016/j.ijnurstu.2018.06.016[↩]
- Ibrahim MA, Asuka E, Jialal I. Hypercholesterolemia. [Updated 2023 Apr 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459188[↩]