Trochlear nerve
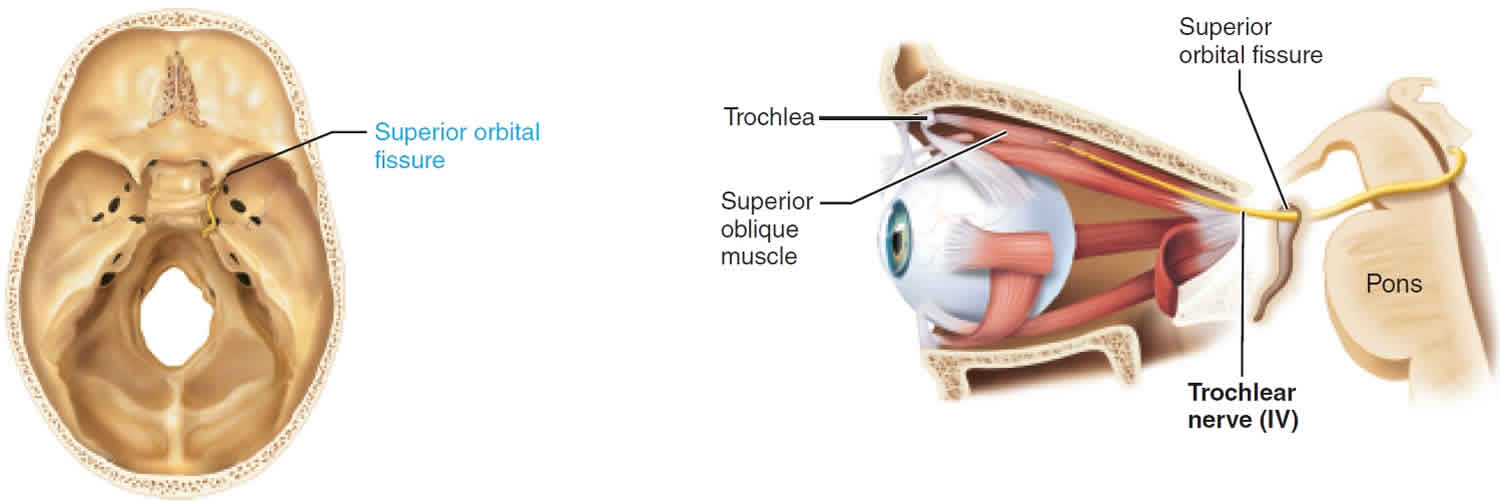
Trochlear nerve is a fourth cranial nerve (CN IV) that carries motor fibers to innervate the superior oblique muscle, an extra-ocular muscle in the orbit 1, that controls abduction and intorsion of the eye 2. Trochlear nerve damage results diplopia (double vision) with inability to look inferiorly when the eye is adducted (down and in). Trochlear nerve originates in the symmetrical trochlear nuclei within the midbrain and is the only cranial nerve to exit from the posterior surface of the brainstem (Figure 1). The left and right trochlear nerves then travel dorsally surrounding the periaqueductal gray matter, decussating before exiting the dorsal midbrain below the inferior colliculus. After curving around the midbrain, it enters the inferior surface of the free edge of the tentorium cerebelli, continues in an anterior direction in the lateral wall of the cavernous sinus where it runs anteriorly/ventrally above the abducens nerve and ophthalmic branch of the trigeminal nerve and enters the orbit through the superior orbital fissure above the origin of the levator palpebra muscle and continues to extend anteriorly to the superior oblique muscle 3. In the cavernous sinus, a few sympathetic fibers join the trochlear nerve with the possibility of some sensory fibers from the trigeminal nerve.
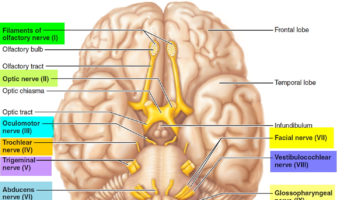
Figure 1. Trochlear nerve
What does the trochlear nerve do?
The only muscle the trochlear nerve innervates, the superior oblique muscle, is the longest and thinnest muscle among the extraocular muscles. The muscle belly originates from the back of the roof of the orbit, and the tendon extends between the roof and medial wall to the pulley (known as the trochlea). The tendon then reaches backward and downward passing the superior rectus muscle to the upper back of the eye. The trochlea of the superior oblique is a U-shaped cartilage attached to the upper front of the orbit.
Because of the unusual shape and direction of the superior oblique muscle afforded by the trochlea, the muscle can depress, abduct, and intorts the eye. Because of the muscle’s placement at the upper back of the eye, the muscle elevates the posterior of the eye, causing the front of the eye to become depressed. The muscle also causes abduction of the eye, moving the pupil away from the nose, and intorsion, rotating the eye such that the top of the eye moves toward the nose.
The superior oblique muscle is the only extraocular muscle that can lower the pupil with the eye adducted. Thus, to isolate the function of the superior oblique muscle from the other extraocular muscles, the muscle can be tested by requesting the patient to adduct the eye and then ask to depress the eye. Failure to depress the eye during adduction indicates a problem with the superior oblique muscle or the trochlear nerve 4.
Trochlear nerve lesion
The trochlear nerve because of its fragility and its extensive intracranial course is especially vulnerable to trauma compared to most cranial nerves. Thus, the most common cause of an acquired defect of the trochlear nerve is head trauma. Traumatic trochlear nerve palsies are associated with motor vehicle accidents and boxing, as they involve rapid deceleration of the head. Because the trochlear nerve is so fragile, this can occur in minor head injuries that do not involve loss of consciousness or skull fracture.
Other significant causes are microvascular, congenital, and idiopathic. Microvascular trochlear nerve palsy usually occurs in the setting of diabetes in patients who are 50 years of age and older. The nerve, however, is less affected compared to the other ocular motor nerves (CN III and CN VI). These nerve injuries are relatively transient with symptom resolution in a few months without treatment.
Congenital trochlear nerve palsies are almost always unilateral. These nerve palsies in children can be initially mistaken for torticollis because of the head tilt many of these children display. Diplopia is not usually present in these patients, and in fact, these patients may compensate for the nerve palsy until adulthood, when diplopia and/or blurry vision may result in a supposed new onset of nerve palsy 5.
Other more minor causes of the trochlear nerve palsy include Lyme disease, Meningioma, Guillain-Barre Syndrome, Herpes zoster, and Cavernous Sinus Syndrome.
Most trochlear nerve palsies are unilateral. However, because the decussation of the trochlear nerve pair happens when the nerve pair is near each other, a single lesion at the dorsal midbrain can cause bilateral trochlear nerve palsy 5.
Lesions of the trochlear nerve can either involve the nucleus or the nerve, but both virtually present with similar symptoms. The only difference is that a unilateral trochlear nuclear lesion affects the contralateral nerve and superior oblique muscle, while a fascicular lesion affects the ipsilateral nerve and muscle.
If other ocular motor nerves are involved in the patients’ symptoms, a lesion in the cavernous sinus or midbrain is most likely, as these nerves are relatively near each other in this space.
Trochlear nerve palsy can present in patients as diplopia, but can also present as blurry vision or a minor vision problem when looking down like reading a book or going down the stairs. The diplopia presented in trochlear nerve palsy is either vertical or diagonal and is worse with downward gaze. Compensation for the nerve palsy usually includes a head tilt to the opposing side and tucking in the chin, so the affected eye’s pupil can move up and extort, instead of downwards and intort. During clinical examination, the eyes will display hypertropia with the affected eye being slightly elevated relative to the other normal eye. Under cover, the affected eye will show an upward drift relative to the other eye 6. There is no established treatment for superior oblique myokymia due to two main reasons: a lack of sufficient patient populations to perform a randomized controlled clinical trial, and the unpredictability and variable time course of superior oblique myokymia, making it difficult to evaluate the efficacy of existing medical therapies 7. Variable success has been seen with topical beta blockers, carbamazepine, phenytoin, baclofen, gabapentin, clonazepam, mirtazapine, memantine, and surgery 7. Botulinum toxin injections have variable success rates and could potentially only provide temporary relief due to difficulty in isolating the superior oblique muscle from the other extraocular muscles [2]. In many cases, continuous medical therapy at dosages on a case-by-case basis has been correlated with favorable prognosis in superior oblique myokymia patients 7. However, unfavorable side effects of these drugs make treatment more difficult, and gabapentin is often used as a favorable first-line of treatment due to the relatively few side effects 8.
Beta blockers such as propranolol, timolol, and betaxolol have recently been reported as successful treatment alternatives due to their ability to reduce blood pressure amplitude. This would mitigate symptoms caused by vascular compression of the trochlear nerve 7.
When medical management is unsuccessful, surgical intervention may be used 9. The procedures most commonly used for superior oblique myokymia are superior oblique tenotomy along with inferior oblique myectomy, or microvascular decompression of the trochlear nerve 7. The latter may only be used when vascular compression is identified as the cause of superior oblique myokymia by MRI. In some cases, patients with superior oblique myokymia see spontaneous improvement or recovery 10. In most patients, however, chronic episodes of superior oblique myokymia occur and symptoms can attempt to be controlled using various medical treatments or surgical interventions 10.
- Kim SY, Naqvi IA. Neuroanatomy, Cranial Nerve 4 (Trochlear) [Updated 2018 Dec 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537244[↩]
- Laine FJ. Cranial nerves III, IV, and VI. Top Magn Reson Imaging. 1996 Apr;8(2):111-30.[↩]
- Park HK, Rha HK, Lee KJ, Chough CK, Joo W. Microsurgical Anatomy of the Oculomotor Nerve. Clin Anat. 2017 Jan;30(1):21-31[↩]
- Demer JL. Compartmentalization of extraocular muscle function. Eye (Lond). 2015 Feb;29(2):157-62[↩]
- Adamec I, Habek M. Superior oblique myokymia. Pract Neurol. 2018 Oct;18(5):415-416.[↩][↩]
- Brazis PW. Isolated palsies of cranial nerves III, IV, and VI. Semin Neurol. 2009 Feb;29(1):14-28 ).
Treatment of trochlear nerve palsies includes surgical procedures, the most common one being the weakening of the inferior oblique muscle. Diabetic nerve palsies virtually do not need additional treatment as they resolve spontaneously.
Another condition that involves the trochlear nerve is superior oblique myokymia which causes spasms of the superior oblique muscle. Symptoms include transient vertical diplopia. The cause is not known but may be related to other conditions that cause microtremors. Rarely this can cause superior oblique muscle weakness ((Adamec I, Habek M. Superior oblique myokymia. Pract Neurol. 2018 Oct;18(5):415-416.[↩]
- Zhang M, Gilbert A, Hunter DG. Superior oblique myokymia. Survey of Ophthalmology. 2018;63(4):507-517. doi:10.1016/j.survophthal.2017.10.005.[↩][↩][↩][↩][↩]
- Jain S, Farooq SJ, Gottlob I. Resolution of superior oblique myokymia with memantine. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2008;12(1):87-88. doi:10.1016/j.jaapos.2007.07.007[↩]
- Williams PE, Purvin VA, Kawasaki A. Superior oblique myokymia: Efficacy of medical treatment. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2007;11(3):254-257. doi:10.1016/j.jaapos.2006.10.019.[↩]
- Brazis PW. The Natural History and Results of Treatment of Superior Oblique Myokymia. Archives of Ophthalmology. 1994;112(8):1063-1067. doi:10.1001/archopht.1994.01090200069025[↩][↩]