Contents
- What is heart surgery
- Surgical Approaches
- Open-Heart Surgery
- Off-Pump Heart Surgery
- Minimally Invasive Heart Surgery
- Heart bypass surgery
- Heart stent surgery
- Heart ablation surgery
- Transmyocardial laser revascularization
- Heart Valve Repair or Replacement Surgery
- Arrhythmia Treatment
- Aneurysm Repair
- Heart Transplant
- Surgery To Place Ventricular Assist Devices or Total Artificial Hearts
What is heart surgery
Heart surgery can correct problems with the heart if other treatments haven’t worked or can’t be used 1. The first American open-heart surgery was performed in 1893 by an African-American, Dr. Daniel Hale Williams. Dr. Daniel Williams completed the operation on a young man named James Cornish. He had been rushed to Provident Hospital in Chicago–with a stab wound. Williams repaired the wound with the use of sutures.
Now many heart surgeries are done each year in the United States for various heart problems. Heart surgery is done in a hospital with a team of experts. Cardiothoracic surgeons perform the surgery with other doctors and nurses who help.
How long the surgery takes will depend on the type of surgery you’re having. Coronary artery bypass grafting (CABG), the most common type of heart surgery, takes about 3–6 hours.
Heart surgery is used for both children and adults. This article discusses heart surgery for adults. For more information about heart surgery for children, go to the articles about congenital heart disease.
There are many types of heart surgery. One person’s experience before surgery can be very different from another’s.
Some people carefully plan their surgeries with their doctors. They know exactly when and how their surgeries will happen. Other people need emergency heart surgery. For example, they might be diagnosed with blocked coronary arteries and admitted to the hospital right away for surgery.
If you’re having a planned surgery, your doctors and others on your health care team will meet with you to explain what will happen. They’ll tell you how to prepare for the surgery. You might be admitted to the hospital the afternoon or morning before your surgery.
You may have some tests before the surgery, such as an EKG (electrocardiogram), chest x ray, or blood tests. An intravenous (IV) line will be placed into a blood vessel in your arm or chest to give you fluids and medicines.
A member of your health care team may shave the area where your surgeon will make the incision (cut). Also, your skin might be washed with special soap to reduce the risk of infection.
Just before the surgery, you’ll be moved to the operating room. You’ll be given medicine so that you fall asleep and don’t feel pain during the surgery.
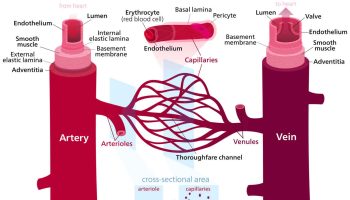
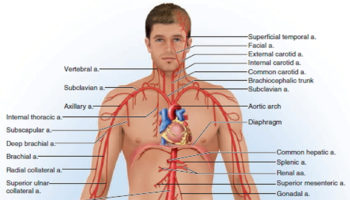
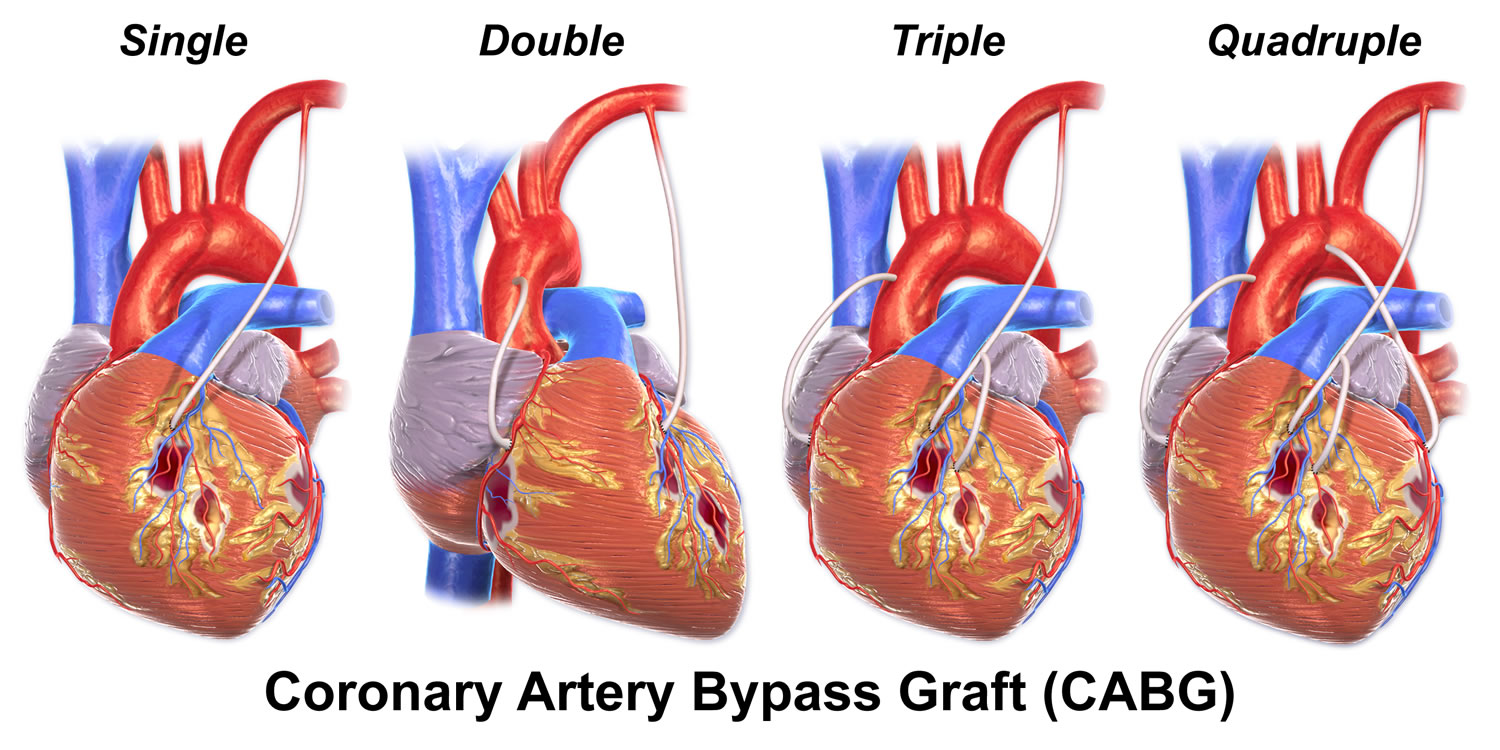
The most common type of heart surgery for adults is coronary artery bypass grafting (CABG). During coronary artery bypass grafting, a healthy artery or vein from the body is connected, or grafted, to a blocked coronary (heart) artery.
The grafted artery or vein bypasses (that is, goes around) the blocked portion of the coronary artery. This creates a new path for oxygen-rich blood to flow to the heart muscle. Coronary artery bypass grafting can relieve chest pain and may lower your risk of having a heart attack.
Doctors also use heart surgery to:
- Treat heart failure and coronary heart disease (coronary artery disease)
- Repair or replace heart valves that don’t work well, which control blood flow through the heart
- Repair abnormal or damaged structures in the heart
- Implant medical devices that help control the heartbeat or control abnormal heart rhythms and support heart function and blood flow
- Replace a damaged heart with a healthy heart from a donor (heart transplant)
Traditional heart surgery, often called open-heart surgery, is done by opening the chest wall to operate on the heart. The surgeon cuts through the patient’s breastbone (or just the upper part of it) to open the chest 2.
Once the heart is exposed, the patient is connected to a heart-lung bypass machine. The machine takes over the heart’s pumping action and moves blood away from the heart. This allows the surgeon to operate on a heart that isn’t beating and that doesn’t have blood flowing through it.
Another type of heart surgery is called off-pump, or beating heart, surgery. It’s like traditional open-heart surgery because the chest bone is opened to access the heart. However, the heart isn’t stopped, and a heart-lung bypass machine isn’t used. Off-pump heart surgery is limited to coronary artery bypass grafting.
Surgeons can now make small incisions (cuts) between the ribs to do some types of heart surgery. The breastbone is not opened to reach the heart. This is called minimally invasive heart surgery. This type of heart surgery may or may not use a heart-lung bypass machine.
Newer methods of heart surgery (such as off-pump and minimally invasive) may reduce risks and speed up recovery time. Studies are under way to compare these types of heart surgery with traditional open-heart surgery.
The results of these studies will help doctors decide the best surgery to use for each patient.
Outlook for heart surgery
The results of heart surgery in adults often are excellent 2. Heart surgery can reduce symptoms, improve quality of life, and improve the chances of survival.
What are the Risks of Heart Surgery ?
Heart surgery has risks, even though its results often are excellent. Risks include 3:
- Bleeding.
- Infection, fever, swelling, and other signs of inflammation.
- A reaction to the medicine used to make you sleep during the surgery.
- Arrhythmias (irregular heartbeats).
- Damage to tissues in the heart, kidneys, liver, and lungs.
- Stroke, which may cause short-term or permanent damage.
- Death. (Heart surgery is more likely to be life threatening in people who are very sick before the surgery.)
Memory loss and other issues, such as problems concentrating or thinking clearly, may occur in some people.
These problems are more likely to affect older patients and women. These issues often improve within 6–12 months of surgery.
In general, the risk of complications is higher if heart surgery is done in an emergency situation (for example, during a heart attack) 3. The risk also is higher if you have other diseases or conditions, such as diabetes, kidney disease, lung disease, or peripheral artery disease 3.
Heart surgery recovery
Recovery in the Hospital
You may spend a day or more in the hospital’s intensive care unit (ICU), depending on the type of heart surgery you have 4. An intravenous (IV) needle might be inserted in a blood vessel in your arm or chest to give you fluids until you’re ready to drink on your own.
Your health care team may give you extra oxygen through a face mask or nasal prongs that fit just inside your nose. They will remove the mask or prongs when you no longer need them.
When you leave the intensive care unit (ICU), you’ll be moved to another part of the hospital for several days before you go home. While you’re in the hospital, doctors and nurses will closely watch your heart rate, blood pressure, breathing, and incision site(s).
Recovery at Home
People respond differently to heart surgery. Your recovery at home will depend on what kind of heart problem and surgery you had. Your doctor will tell you how to:
- Care for your healing incision(s)
- Recognize signs of infection or other complications
- Cope with the after-effects of surgery
You also will get information about followup appointments, medicines, and situations when you should call your doctor right away.
After-effects of heart surgery are normal. They may include muscle pain, chest pain, or swelling (especially if you have an incision in your leg from coronary artery bypass grafting, or coronary artery bypass grafting).
Other after-effects may include loss of appetite, problems sleeping, constipation, and mood swings and depression. After-effects usually go away over time.
Recovery time after heart surgery depends on the type of surgery you had, your overall health before the surgery, and any complications from the surgery.
Your doctor will let you know when you can go back to your daily routine, such as working, driving, and physical activity.
Ongoing Care
Ongoing care after your surgery will include checkups with your doctor. During these visits, you may have blood tests, an EKG (electrocardiogram), echocardiography, or a stress test. These tests will show how your heart is working after the surgery.
After some types of heart surgery, you’ll need to take a blood-thinning medicine. Your doctor will do routine tests to make sure you’re getting the right amount of medicine.
Your doctor also may recommend lifestyle changes and medicines to help you stay healthy. Lifestyle changes may include quitting smoking, changing your diet, being physically active, and reducing and managing stress.
Your doctor also may refer you to cardiac rehabilitation (rehab). Cardiac rehab is a medically supervised program that helps improve the health and well-being of people who have heart problems.
Cardiac rehab includes exercise training, education on heart healthy living, and counseling to reduce stress and help you recover. Your doctor can tell you where to find a cardiac rehab program near your home.
Surgical Approaches
Surgeons can use different approaches to operate on the heart, including open-heart surgery, off-pump heart surgery, and minimally invasive heart surgery.
The surgical approach will depend on the patient’s heart problem, general health, and other factors.
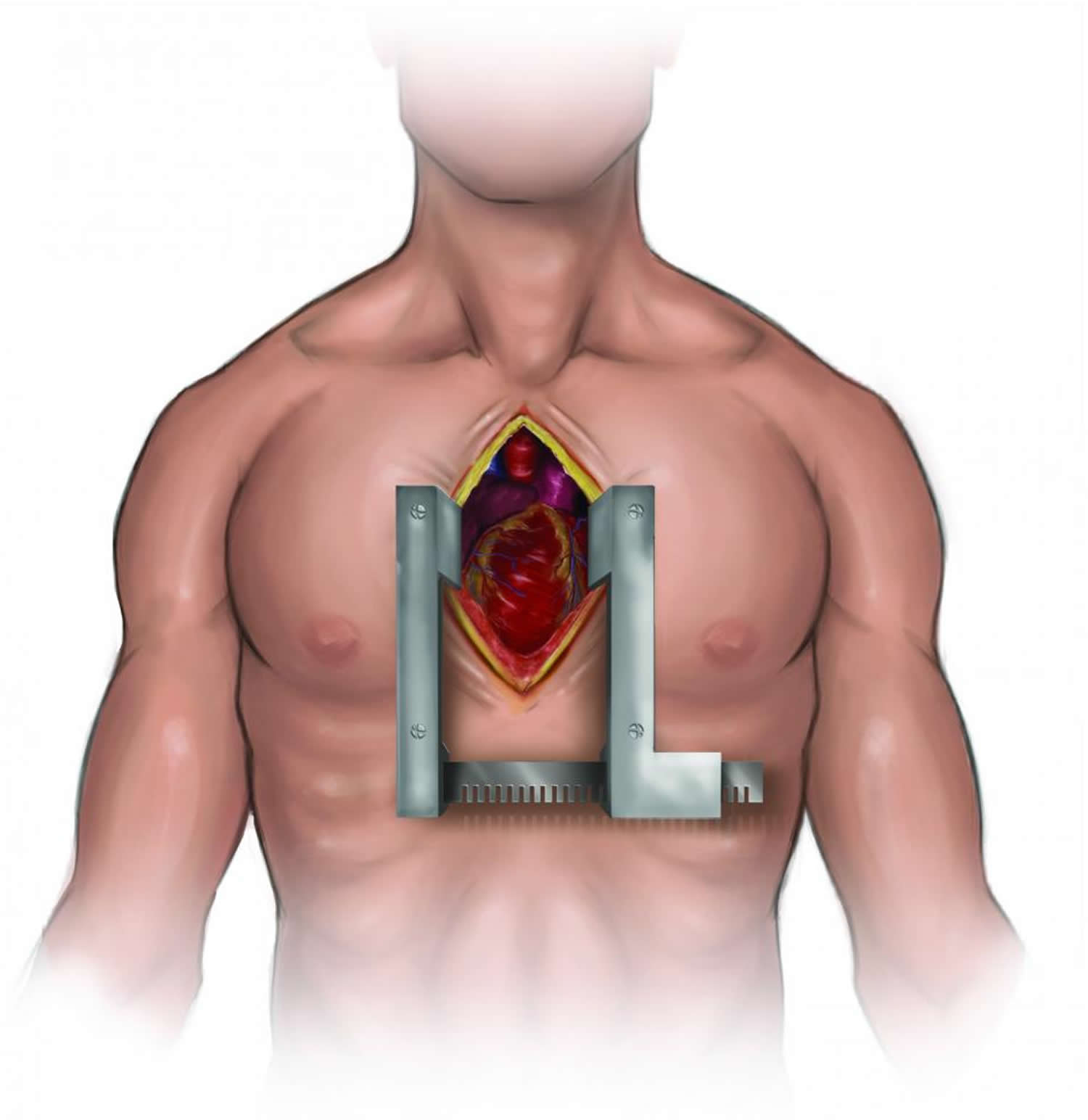
Open-Heart Surgery
Open-heart surgery is any kind of surgery in which a surgeon makes a large incision (cut) in the chest to open the rib cage and operate on the heart. “Open” refers to the chest, not the heart. Depending on the type of surgery, the surgeon also may open the heart.
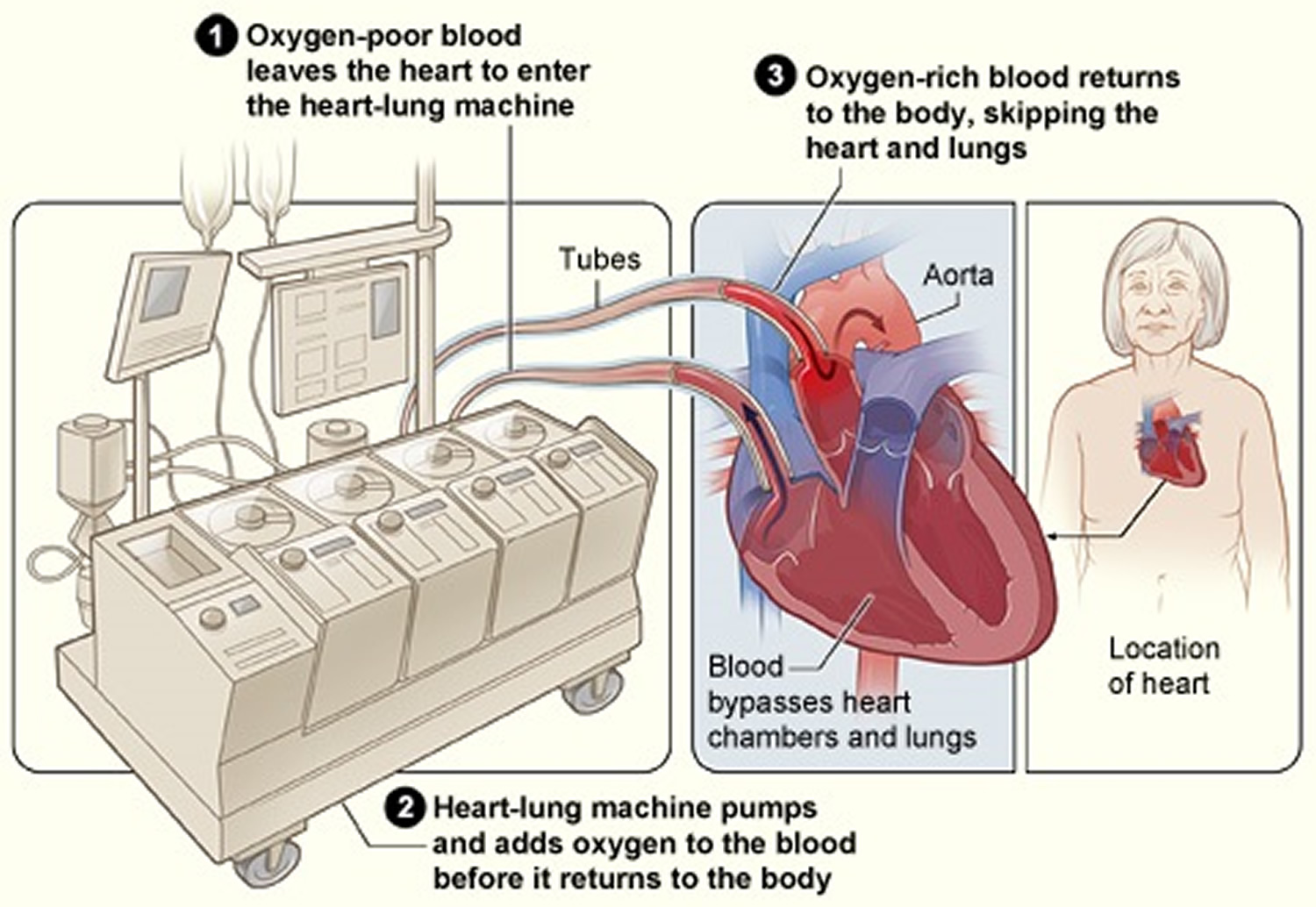
Once the heart is exposed, the patient is connected to a heart-lung bypass machine. The machine takes over the heart’s pumping action and moves blood away from the heart. This allows the surgeon to operate on a heart that isn’t beating and that doesn’t have blood flowing through it.
Open-heart surgery is used to do coronary artery bypass grafting, repair or replace heart valves, treat atrial fibrillation, do heart transplants, and place ventricular assist devices and total artificial hearts.
For this type of surgery, you’ll be given medicine to help you fall asleep. A doctor will check your heartbeat, blood pressure, oxygen levels, and breathing during the surgery.
A breathing tube will be placed in your lungs through your throat. The tube will connect to a ventilator (a machine that supports breathing).
Your surgeon will make a 6- to 8-inch incision (cut) down the center of your chest wall. Then, he or she will cut your breastbone and open your rib cage to reach your heart.
During the surgery, you’ll receive medicine to thin your blood and keep it from clotting. A heart-lung bypass machine will be connected to your heart. The machine will take over your heart’s pumping action and move blood away from your heart.
A specialist will oversee the heart-lung bypass machine. The machine will allow the surgeon to operate on a heart that isn’t beating and that doesn’t have blood flowing through it.
Figure 1. Open-Heart Surgery
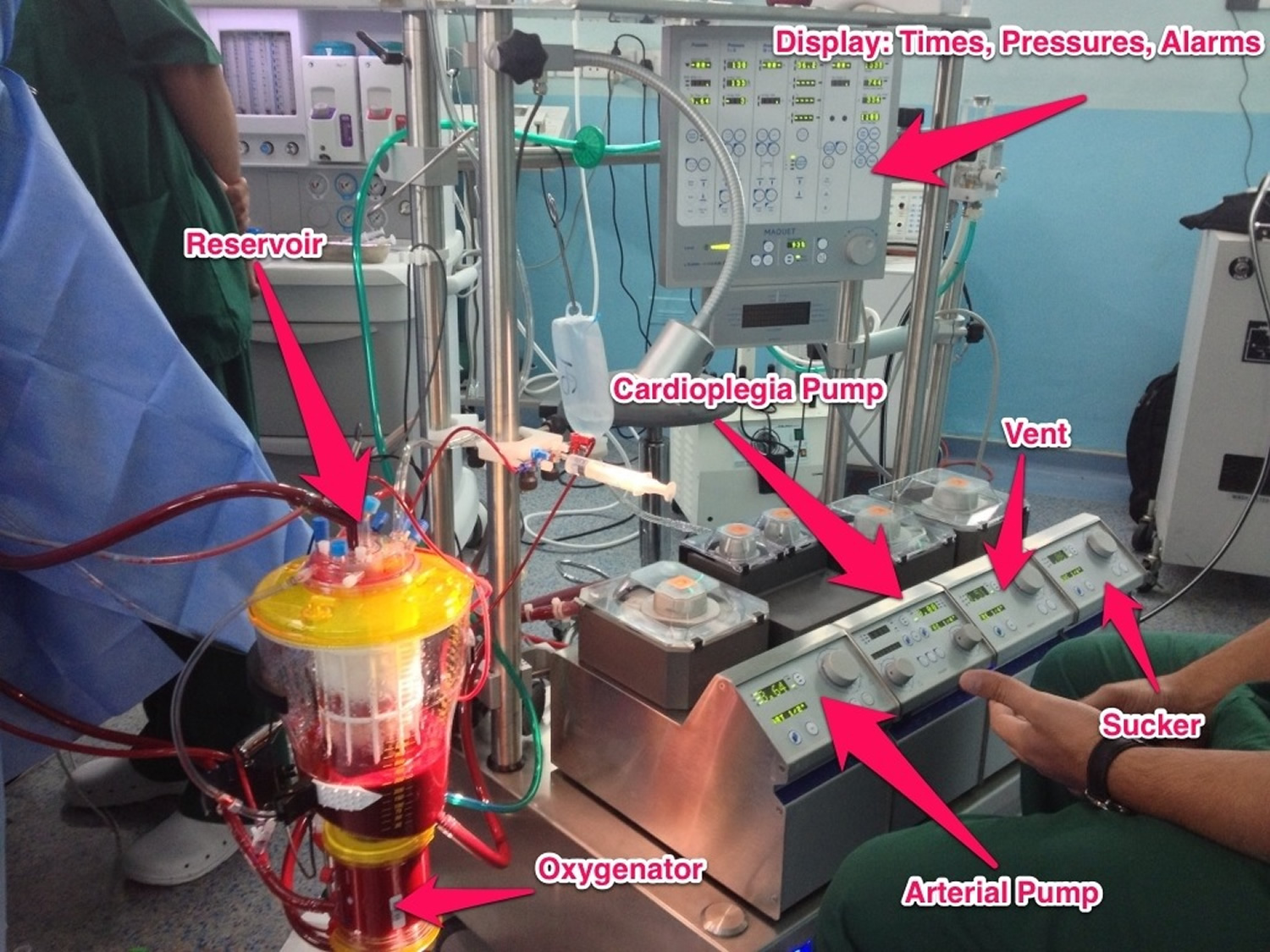
Heart-Lung Bypass Machine
You’ll be given medicine to stop your heartbeat once you’re connected to the heart-lung bypass machine. A tube will be placed in your heart to drain blood to the machine.
The machine will remove carbon dioxide (a waste product) from your blood, add oxygen to your blood, and then pump the blood back into your body. Your surgeon will insert tubes into your chest to drain fluid.
Once the bypass machine starts to work, the surgeon will repair your heart problem. After the surgery is done, he or she will restore blood flow to your heart. Usually, your heart will start beating again on its own. Sometimes mild electric shocks are used to restart the heart.
Once your heart has started beating again, your surgeon will remove the tubes and stop the heart-lung bypass machine. You’ll be given medicine to allow your blood to clot again.
The surgeon will use wires to close your breastbone. The wires will stay in your body permanently. After your breastbone heals, it will be as strong as it was before the surgery.
Stitches or staples will be used to close the skin incision. Your breathing tube will be removed when you’re able to breathe without it.
Figure 2. Heart-Lung Bypass Machine
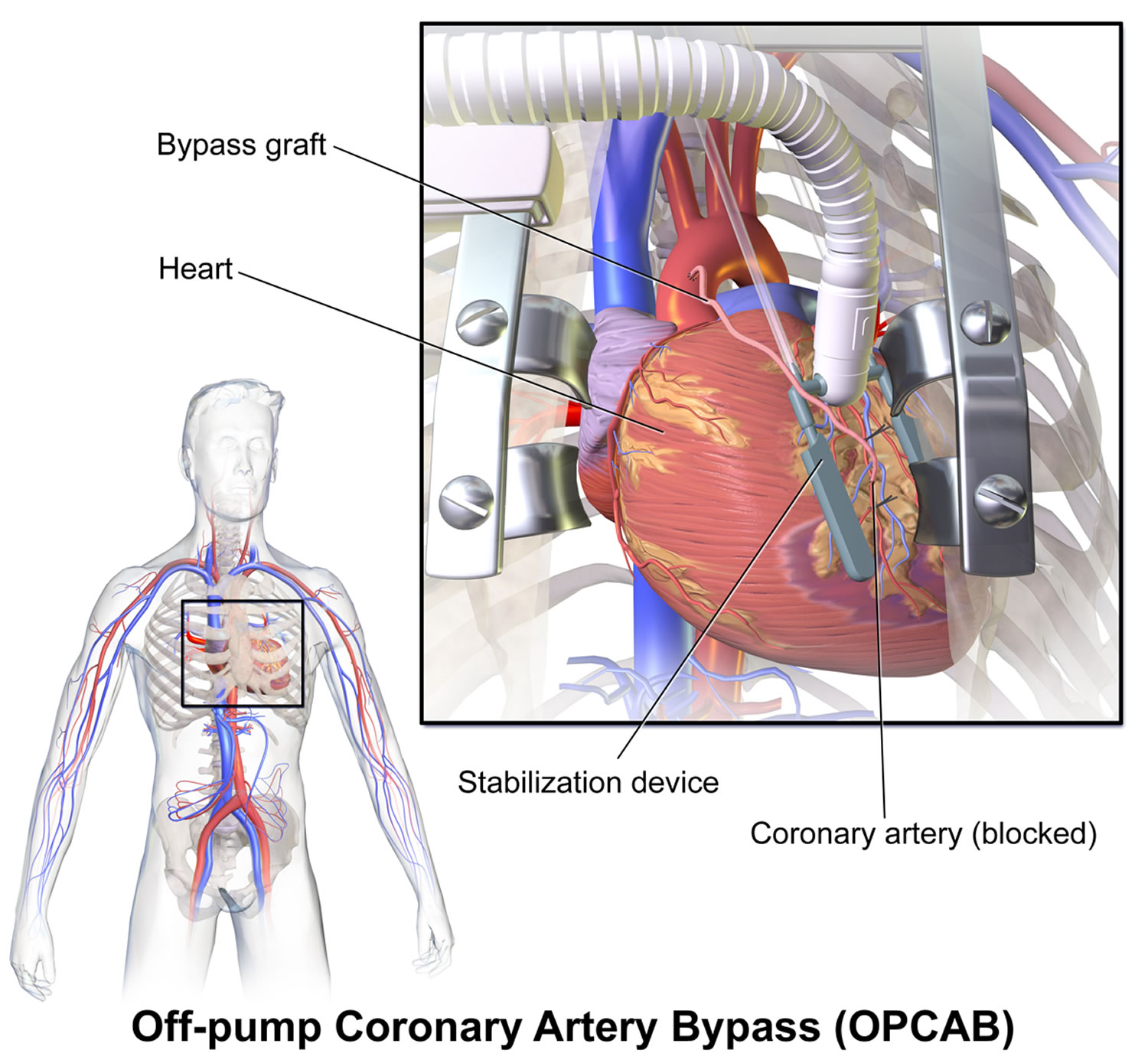
Off-Pump Heart Surgery
Surgeons also use off-pump, or beating heart, surgery to do coronary artery bypass grafting. This approach is like traditional open-heart surgery because the chest bone is opened to access the heart. However, the heart isn’t stopped, and a heart-lung bypass machine isn’t used 5. Instead, your surgeon will steady your heart with a mechanical device so he or she can work on it. Your heart will continue to pump blood to your body.
Off-pump heart surgery isn’t right for all patients. Work with your doctor to decide whether this type of surgery is an option for you. Your doctor will carefully consider your heart problem, age, overall health, and other factors that may affect the surgery.
Figure 3. Off-pump coronary artery bypass heart surgery
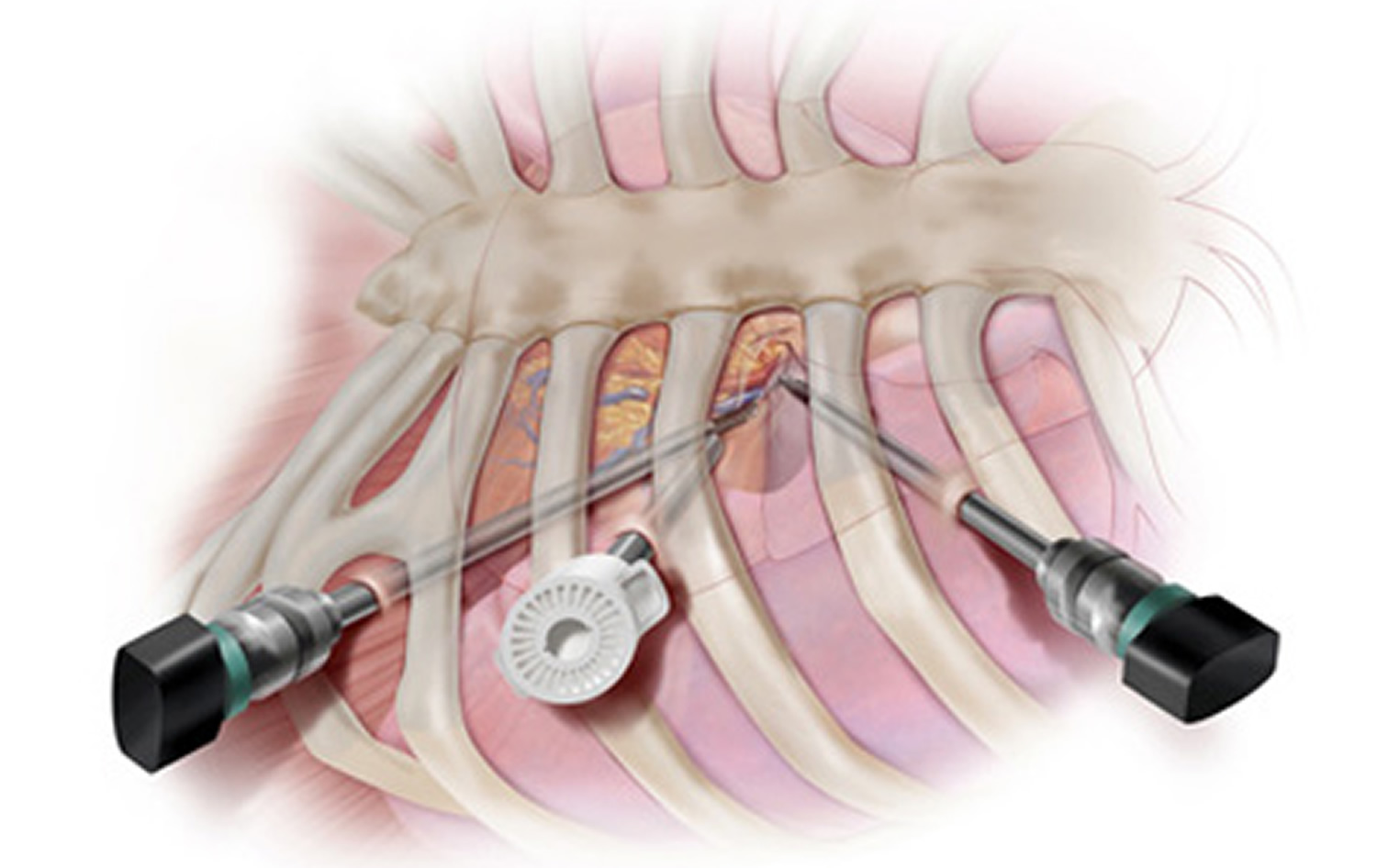
Minimally Invasive Heart Surgery
For minimally invasive heart surgery, a surgeon makes small incisions (2–3 inches) in the side of the chest between the ribs. This type of surgery may or may not use a heart-lung bypass machine.
Minimally invasive heart surgery is used to do some bypass and maze surgeries. It’s also used to repair or replace heart valves, insert pacemakers or implantable cardioverter defibrillators, or take a vein or artery from the body to use as a bypass graft for coronary artery bypass grafting.
One type of minimally invasive heart surgery that is becoming more common is robotic-assisted surgery. For this surgery, a surgeon uses a computer to control surgical tools on thin robotic arms.
The tools are inserted through small incisions in the chest. This allows the surgeon to do complex and highly precise surgery. The surgeon always is in total control of the robotic arms; they don’t move on their own.
Figure 4. Minimally Invasive Heart Surgery
Heart bypass surgery
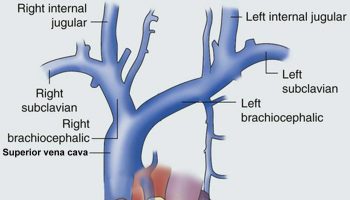
Coronary artery bypass grafting or heart bypass surgery is the most common type of heart surgery 5. Coronary artery bypass grafting improves blood flow to the heart. Surgeons use coronary artery bypass grafting to treat people who have severe coronary heart disease (coronary artery disease).
Coronary heart disease is a disease in which a waxy substance called plaque builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause chest pain or discomfort called angina.
If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. This is the most common cause of a heart attack. Over time, ruptured plaque also hardens and narrows the coronary arteries.
During coronary artery bypass grafting, a healthy artery or vein from the body is connected, or grafted, to the blocked coronary artery. The grafted artery or vein bypasses (that is, goes around) the blocked portion of the coronary artery. This creates a new path for oxygen-rich blood to flow to the heart muscle.
Surgeons can bypass multiple blocked coronary arteries during one surgery.
Figure 5. Coronary artery bypass grafting
Coronary artery bypass grafting isn’t the only treatment for coronary artery disease. A nonsurgical procedure that opens blocked or narrow coronary arteries is percutaneous coronary intervention (PCI), also known as coronary angioplasty or heart stent surgery.
Heart stent surgery
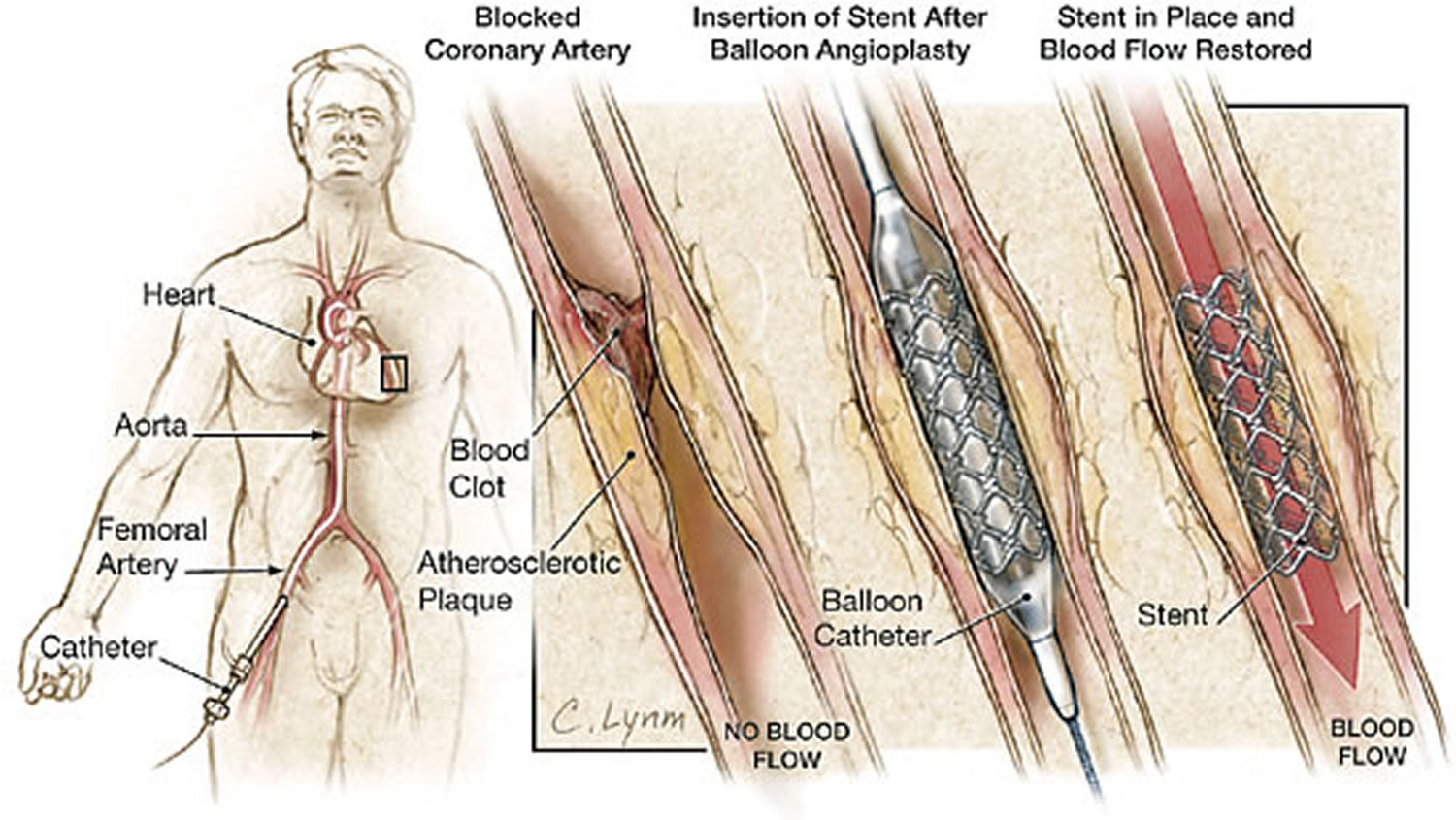
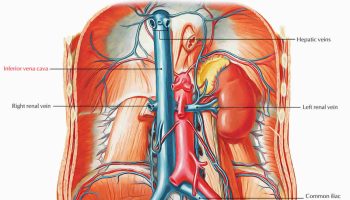
During percutaneous coronary intervention or heart stent surgery, a thin, flexible tube with a balloon at its tip is threaded through a blood vessel to the narrow or blocked coronary artery. Once in place, the balloon is inflated to push the plaque against the artery wall. This restores blood flow through the artery.
During percutaneous coronary intervention, a stent might be placed in the coronary artery to help keep it open. A stent is a small mesh tube that supports the inner artery wall.
Both coronary artery bypass grafting and percutaneous coronary intervention are options, your doctor can help you decide which treatment is right for you.
Figure 6. Heart stent surgery (percutaneous coronary intervention)
Heart ablation surgery
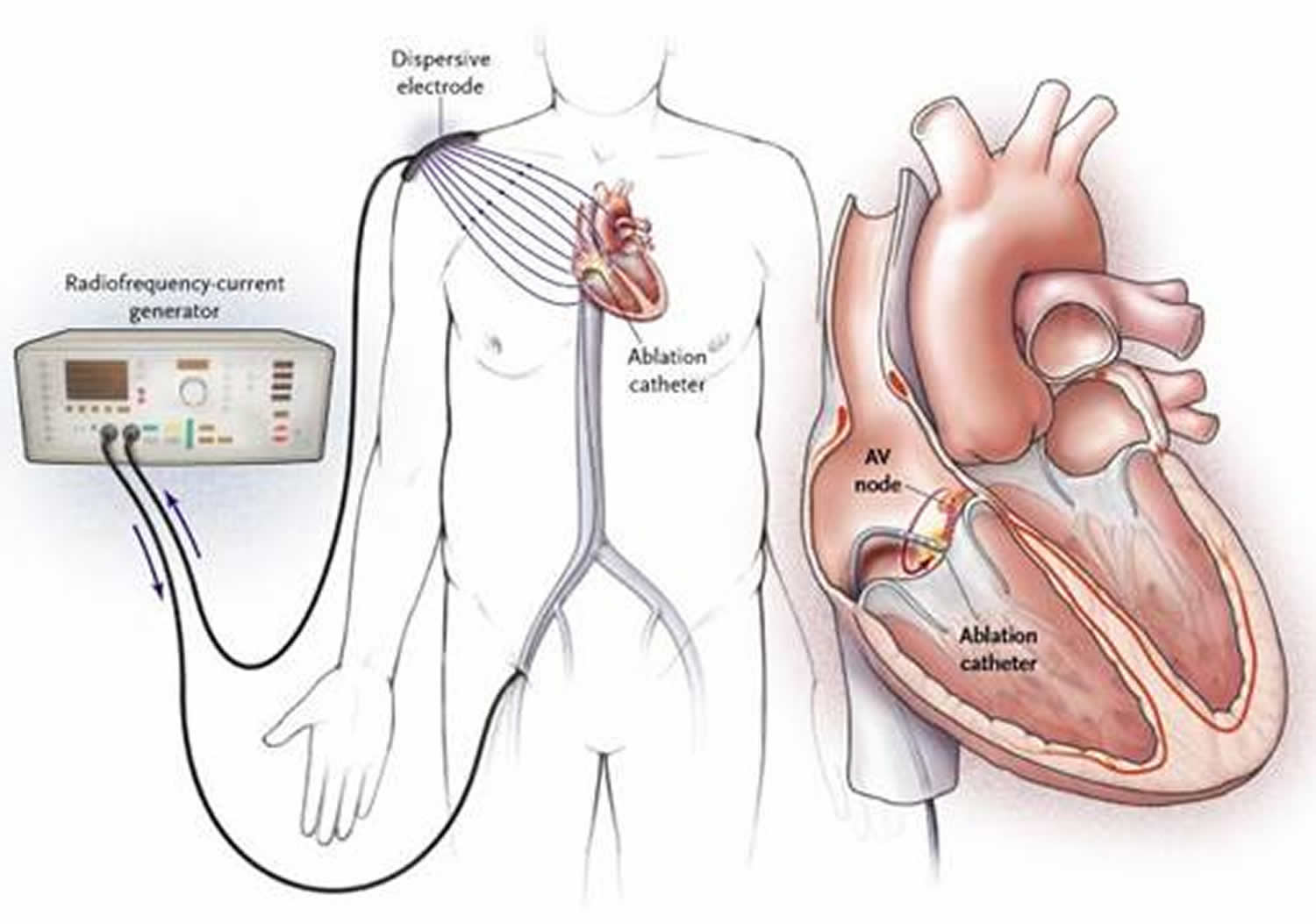
Heart ablation surgery also known as catheter ablation, is a procedure that uses radiofrequency energy (similar to microwave heat) to destroy a small area of heart tissue that is causing rapid and irregular heartbeats 6. Destroying this tissue helps restore your heart’s regular rhythm. The procedure is also called radiofrequency ablation.
A catheter with an electrode at its tip is guided through the veins to the heart muscle with real-time, moving X-rays (fluoroscopy) displayed on a video screen. The catheter is placed at the exact site inside the heart where cells give off the electrical signals that stimulate the abnormal heart rhythm. Then a mild, painless radiofrequency energy (similar to microwave heat) is transmitted to the pathway. This destroys carefully selected heart muscle cells in a very small area (about 1/5 of an inch). This procedure takes place in a special hospital room called an electrophysiology lab or a cardiac catheterization lab. It takes 2 to 4 hours 6.
Radiofrequency ablation is the preferred treatment for many types of rapid heartbeats (arrhythmias) especially supraventricular tachyarrhythmias.
Why do people have catheter ablation ?
Special cells in your heart create electrical signals that travel along pathways to the chambers of your heart. These signals make the heart’s upper and lower chambers beat in the proper sequence. Abnormal cells may create disorganized electrical signals that cause irregular or rapid heartbeats called arrhythmias. When this happens, your heart may not pump blood effectively and you may feel faint, short of breath and weak. You may also feel your heart pounding.
Medicines to treat rapid and irregular heartbeats work very well for most people. But they don’t work for everyone, and they may cause side effects in some people. In these cases, doctors may suggest catheter ablation. The procedure is used most often to treat a condition called supraventricular tachycardia (SVT), which occurs because of abnormal conduction fibers in the heart. Catheter ablation is also used to help control other heart rhythm problems such as atrial flutter and atrial fibrillation. Catheter ablation destroys the abnormal tissue without damaging the rest of the heart.
What are the risks of catheter ablation ?
There are few risks. The most common problems result from the use of the catheters – long, thin tubes doctors insert into your arteries or veins. Inserting the tubes can occasionally damage your blood vessel or cause bleeding or infection. These problems are rare.
Figure 7. Radiofrequency ablation of the heart
NOTE: During radiofrequency catheter ablation procedure, the tip of a catheter is guided to the area of heart tissue that is producing abnormal electrical signals. Then the catheter emits a pulse of painless radiofrequency energy that destroys the abnormal tissue and corrects the irregular heartbeat.
What happens during catheter ablation ?
A doctor with special training performs the procedure along with a team of nurses and technicians. The procedure is done in a hospital electrophysiology lab or a cardiac catheterization lab.
- A nurse will put an IV (intravenous line) into a vein in your arm so you can get medicine (anesthesia) to prevent pain. You may also get a medicine (sedative) to help you relax but you will be awake throughout the procedure.
- The nurse will clean and shave the area where the doctor will be working. This is usually in your groin.
- The nurse will give you a shot — a local anesthetic — to numb the needle puncture site.
- The doctor will make a needle puncture through your skin and into the blood vessel (typically a vein, but sometimes an artery) in your groin. A small straw-sized tube (called a sheath) will be inserted into the blood vessel. The doctor will gently guide a catheter (a long, thin tube) into your vessel through the sheath. A video screen will show the position of the catheter. You may feel some pressure in your groin, but you shouldn’t feel any pain.
- The doctor inserts several long, thin tubes with wires, called electrode catheters, through the sheath and feeds these tubes into your heart.
- To locate the abnormal tissue causing arrhythmia, the doctor sends a small electrical impulse through the electrode catheter. This activates the abnormal tissue that is causing your arrhythmia. Other catheters record the heart’s electrical signals to locate the abnormal sites.
- The doctor places the catheter at the exact site inside your heart where the abnormal cells are. Then, a mild, painless, radiofrequency energy (similar to microwave heat) is sent to the tissue. This destroys heart muscle cells in a very small area (about 1/5 of an inch) that are responsible for the extra impulses that caused your rapid heartbeats.
- Catheter ablation usually takes 2 to 4 hours. If you have more than one area of abnormal tissue, the procedure will take longer. You can usually go home the same day, or you may have to stay overnight.
What happens after catheter ablation ?
You’ll be moved to a recovery room. The sheath usually stays in your leg for several hours after catheter ablation. During this time, you have to lie flat.
After the doctor or nurse removes the sheath:
- A nurse will put pressure on the puncture site to stop the bleeding.
- You should keep your leg straight for 6 to 8 hours after the doctor or nurse removes the sheath. The nurse will tell you when you can get out of bed.
- The nurse will watch you carefully and check your heartbeat and vital signs (pulse and blood pressure).
- Tell your doctor or nurse right away if you notice any swelling, pain or bleeding at the puncture site, or if you have chest pain.
- Before you leave the hospital, the nurse will give you written instructions about what to do at home.
- Aspirin is often prescribed for 2 to 4 weeks to minimize risk of clot formation at ablation sites.
What happens after you get home ?
Follow the instructions your nurse or doctor gave you. Most people can return to their normal activities on the day after they leave the hospital.
- Don’t drive for 24 hours after you leave the hospital.
- Don’t drink alcohol for 24 hours after you leave the hospital.
- Avoid heavy physical activity for three days. Ask your doctor when you can return to strenuous exercise.
- A small bruise at the puncture site is normal. If the site starts to bleed, lie flat and press firmly on top of it. Have someone call the doctor or hospital.
Call your local emergency number if you notice:
- The puncture site swells up very fast.
- Bleeding from the puncture site does not slow down when you press on it firmly.
Transmyocardial laser revascularization
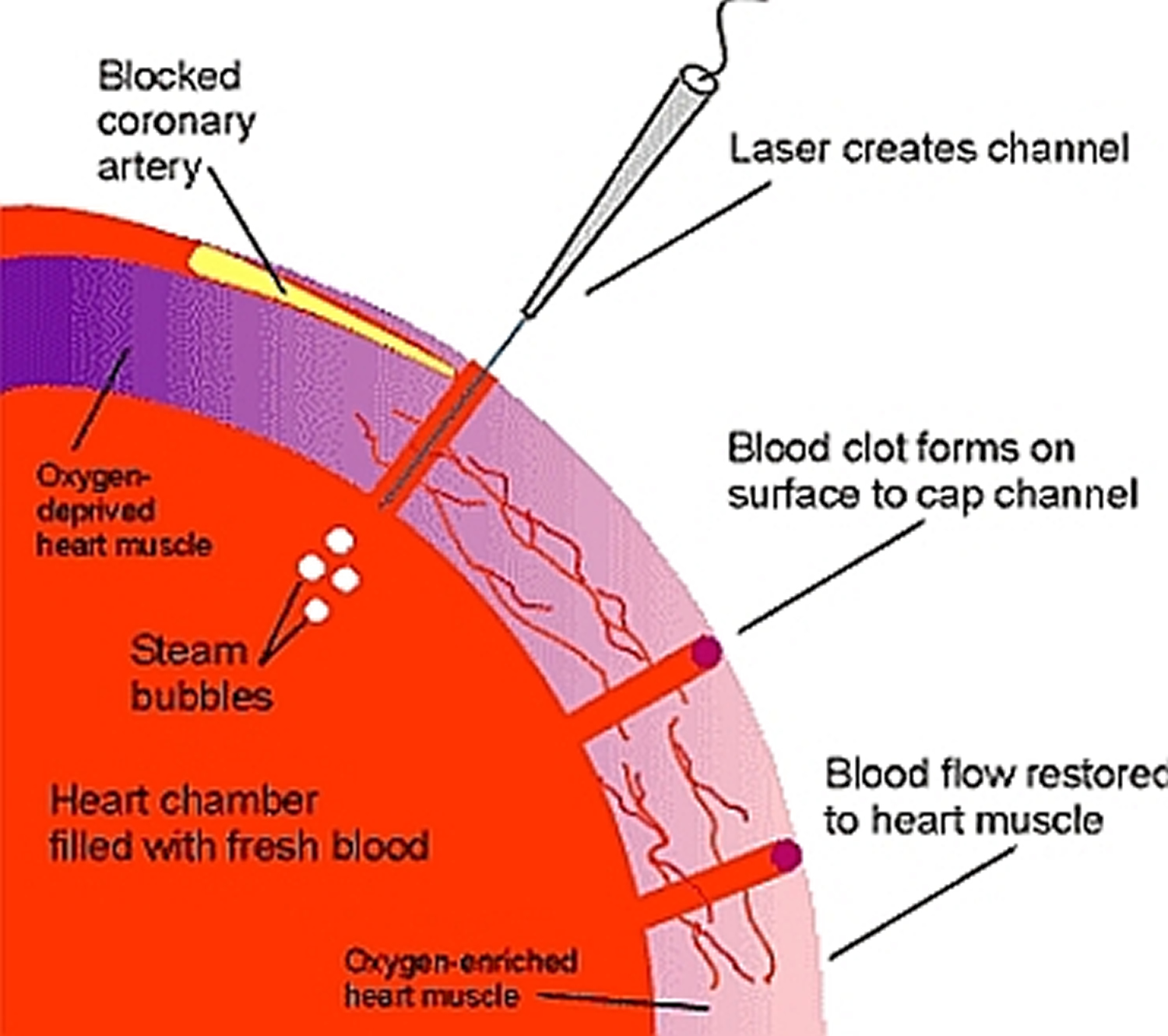
Transmyocardial laser revascularization is surgery used to treat angina 5.
Transmyocardial laser revascularization is most often used when no other treatments work. For example, if you’ve already had one coronary artery bypass grafting procedure and can’t have another one, transmyocardial laser revascularization might be an option. For some people, transmyocardial laser revascularization is combined with coronary artery bypass grafting.
If transmyocardial laser revascularization is done alone, an incision is made on the left breast to expose the heart. Then, a laser is used to drill a series of holes from the outside of the heart into the heart’s pumping chamber.
During transmyocardial laser revascularization, a surgeon uses lasers to make small channels through the heart muscle and into the heart’s lower left chamber (the left ventricle).
It isn’t fully known how transmyocardial laser revascularization relieves angina. The surgery may help the heart grow tiny new blood vessels. Oxygen-rich blood may flow through these vessels into the heart muscle, which could relieve angina.
Figure 8. Transmyocardial laser revascularization
Heart Valve Repair or Replacement Surgery
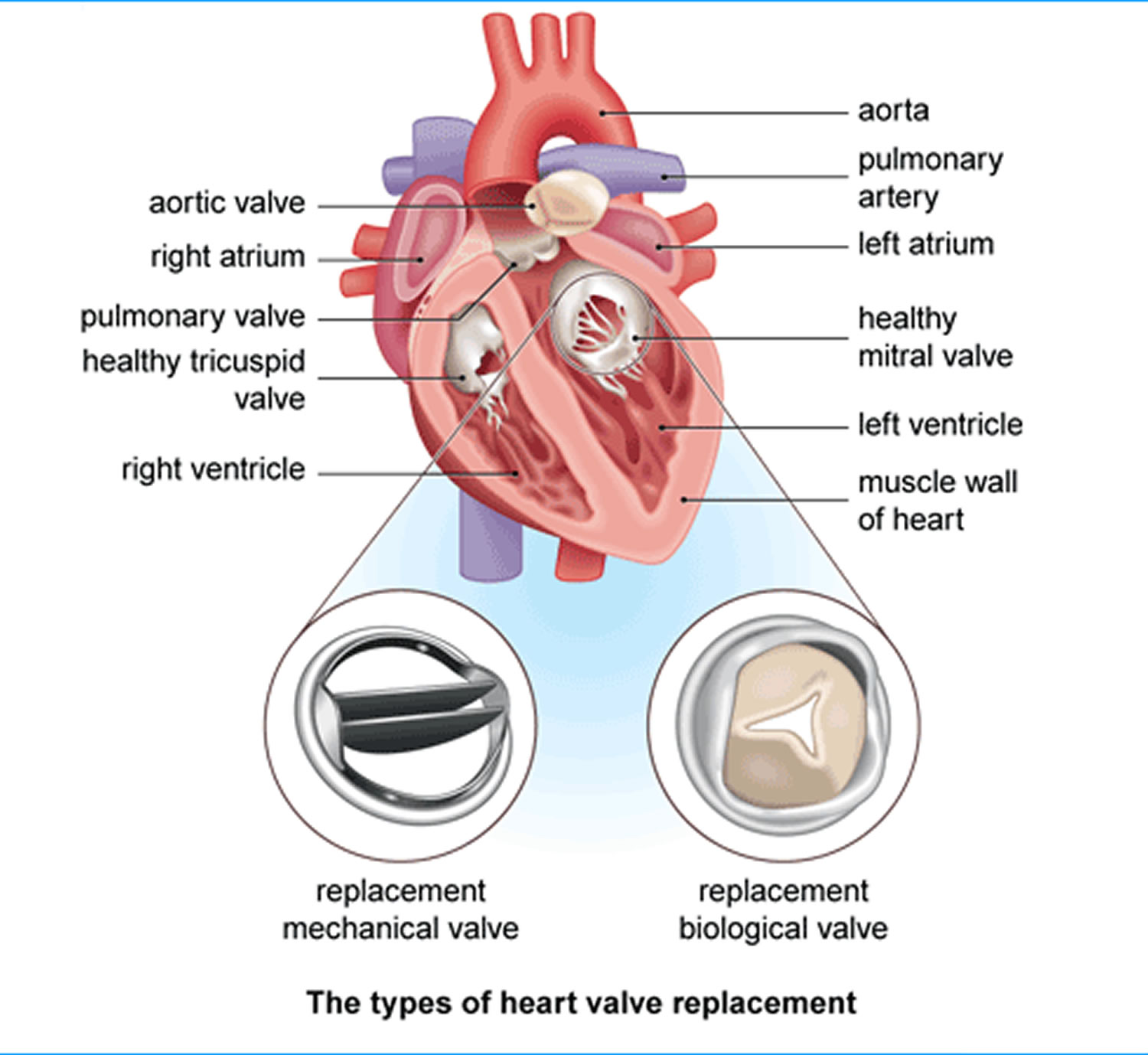
For the heart to work well, blood must flow in only one direction. The heart’s valves make this possible. Healthy valves open and close in a precise way as the heart pumps blood.
Each valve has a set of flaps called leaflets. The leaflets open to allow blood to pass from one heart chamber into another or into the arteries. Then the leaflets close tightly to stop blood from flowing backward.
Heart surgery is used to fix leaflets that don’t open as wide as they should. This can happen if they become thick or stiff or fuse together. As a result, not enough blood flows through the valve.
Heart surgery also is used to fix leaflets that don’t close tightly. This problem can cause blood to leak back into the heart chambers, rather than only moving forward into the arteries as it should.
To fix these problems, surgeons either repair the valve or replace it with a man-made or biological valve 5. Biological valves are made from pig, cow, or human heart tissue and may have man-made parts as well.
To repair a mitral or pulmonary valve that’s too narrow, a cardiologist (heart specialist) will insert a catheter (a thin, flexible tube) through a large blood vessel and guide it to the heart.
The cardiologist will place the end of the catheter inside the narrow valve. He or she will inflate and deflate a small balloon at the tip of the catheter. This widens the valve, allowing more blood to flow through it. This approach is less invasive than open-heart surgery.
Researchers also are testing new ways to use catheters in other types of valve surgeries. For example, catheters might be used to place clips on the mitral valve leaflets to hold them in place.
Catheters also might be used to replace faulty aortic valves. For this procedure, the catheter usually is inserted into an artery in the groin (upper thigh) and threaded to the heart.
In some cases, surgeons might make a small cut in the chest and left ventricle (the lower left heart chamber). They will thread the catheter into the heart through the small opening.
The catheter has a deflated balloon at its tip with a folded replacement valve around it. The balloon is used to expand the new valve so it fits securely within the old valve.
Currently, surgery to replace the valve is the traditional treatment for reasonably healthy people. However, catheter procedures might be a safer option for patients who have conditions that make open-heart surgery very risky.
Figure 9. Heart Valve Repair / Replacement Surgery
Arrhythmia Treatment
An arrhythmia is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm.
Many arrhythmias are harmless, but some can be serious or even life threatening. If the heart rate is abnormal, the heart may not be able to pump enough blood to the body. Lack of blood flow can damage the brain, heart, and other organs.
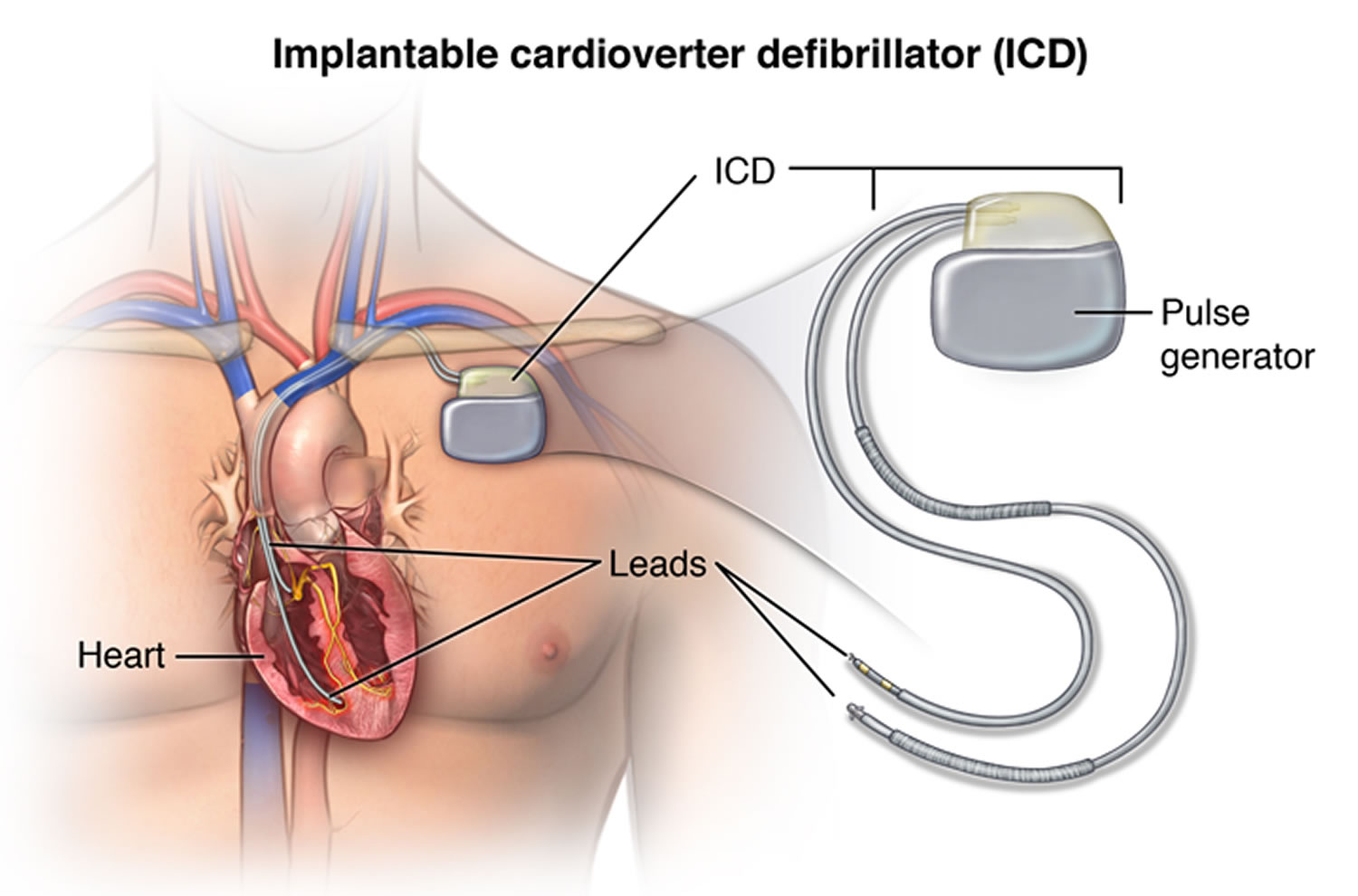
Medicine usually is the first line of treatment for arrhythmias. If medicine doesn’t work well, your doctor may recommend surgery. For example, surgery may be used to implant a pacemaker or an implantable cardioverter defibrillator.
A pacemaker is a small device that’s placed under the skin of your chest or abdomen. Wires connect the pacemaker to your heart chambers. The device uses low-energy electrical pulses to control your heart rhythm. Most pacemakers have a sensor that starts the device only if your heart rhythm is abnormal.
An implantable cardioverter defibrillator is another small device that’s placed under the skin of your chest or abdomen. This device also is connected to your heart with wires. An implantable cardioverter defibrillator checks your heartbeat for dangerous arrhythmias. If the device senses one, it sends an electric shock to your heart to restore a normal heart rhythm.
Another arrhythmia treatment is called maze surgery. For this surgery, the surgeon makes new paths for the heart’s electrical signals to travel through. This type of surgery is used to treat atrial fibrillation, the most common type of serious arrhythmia.
Simpler, less invasive procedures also are used to treat atrial fibrillation. These procedures use high heat or intense cold to prevent abnormal electrical signals from moving through the heart.
Figure 10. Implantable cardioverter defibrillator and/or pacemaker
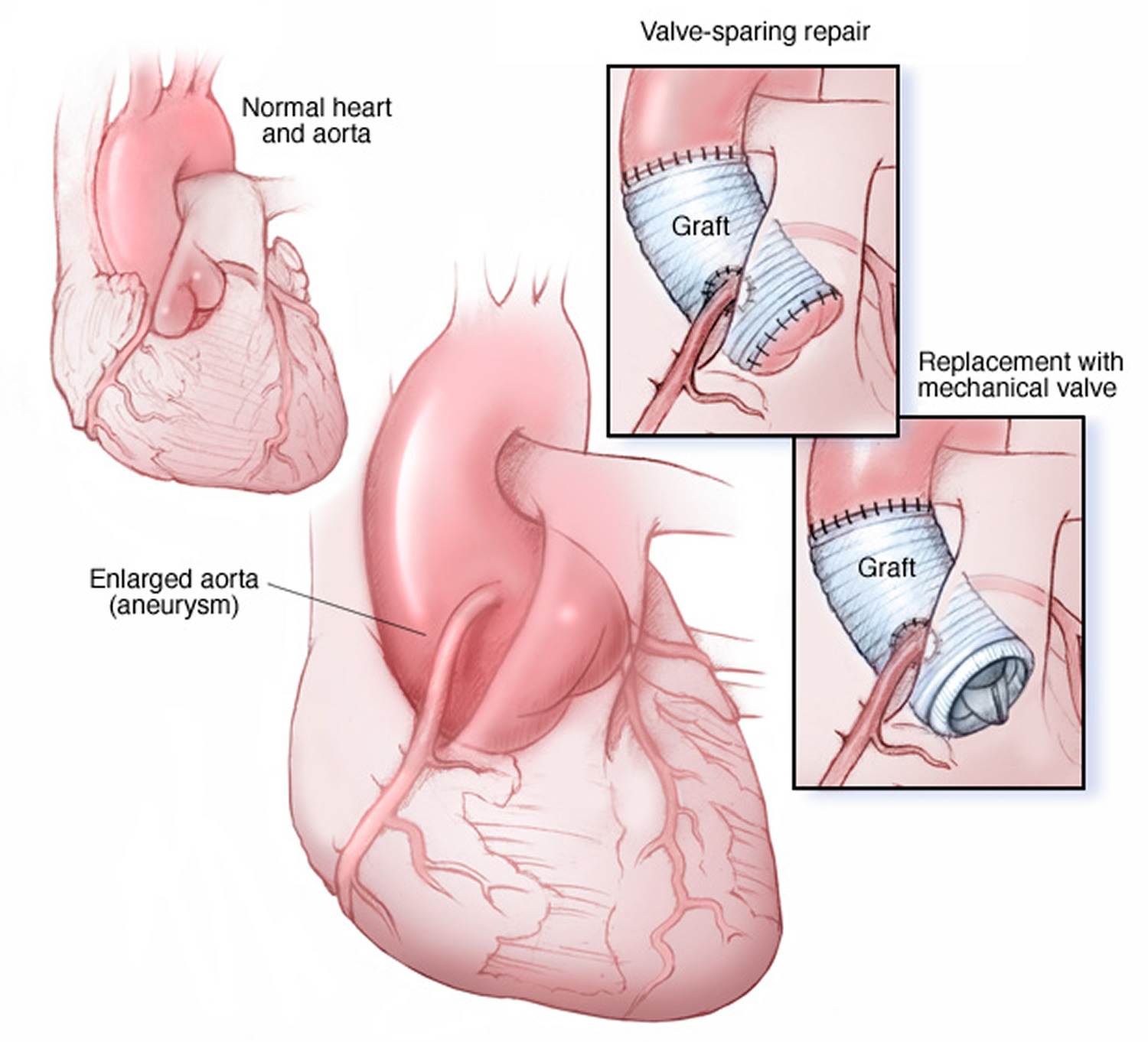
Aneurysm Repair
An aneurysm is a balloon-like bulge in the wall of an artery or the heart muscle. This bulge can occur if the artery wall weakens. Pressure from blood moving through the artery or heart causes the weak area to bulge.
Over time, an aneurysm can grow and burst, causing dangerous, often fatal bleeding inside the body. Aneurysms also can develop a split in one or more layers of the artery wall. The split causes bleeding into and along the layers of the artery wall.
Aneurysms in the heart most often occur in the heart’s lower left chamber (the left ventricle). Repairing an aneurysm involves surgery to replace the weak section of the artery or heart wall with a patch or graft.
Figure 11. Aortic aneurysm repair
Heart Transplant
A heart transplant is surgery to remove a person’s diseased heart and replace it with a healthy heart from a deceased donor. Most heart transplants are done on patients who have end-stage heart failure.
Heart failure is a condition in which the heart is damaged or weak. As a result, it can’t pump enough blood to meet the body’s needs. “End-stage” means the condition is so severe that all treatments, other than heart transplant, have failed.
Patients on the waiting list for a donor heart receive ongoing treatment for heart failure and other medical conditions. Ventricular assist devices or total artificial hearts might be used to treat these patients.
Surgery To Place Ventricular Assist Devices or Total Artificial Hearts
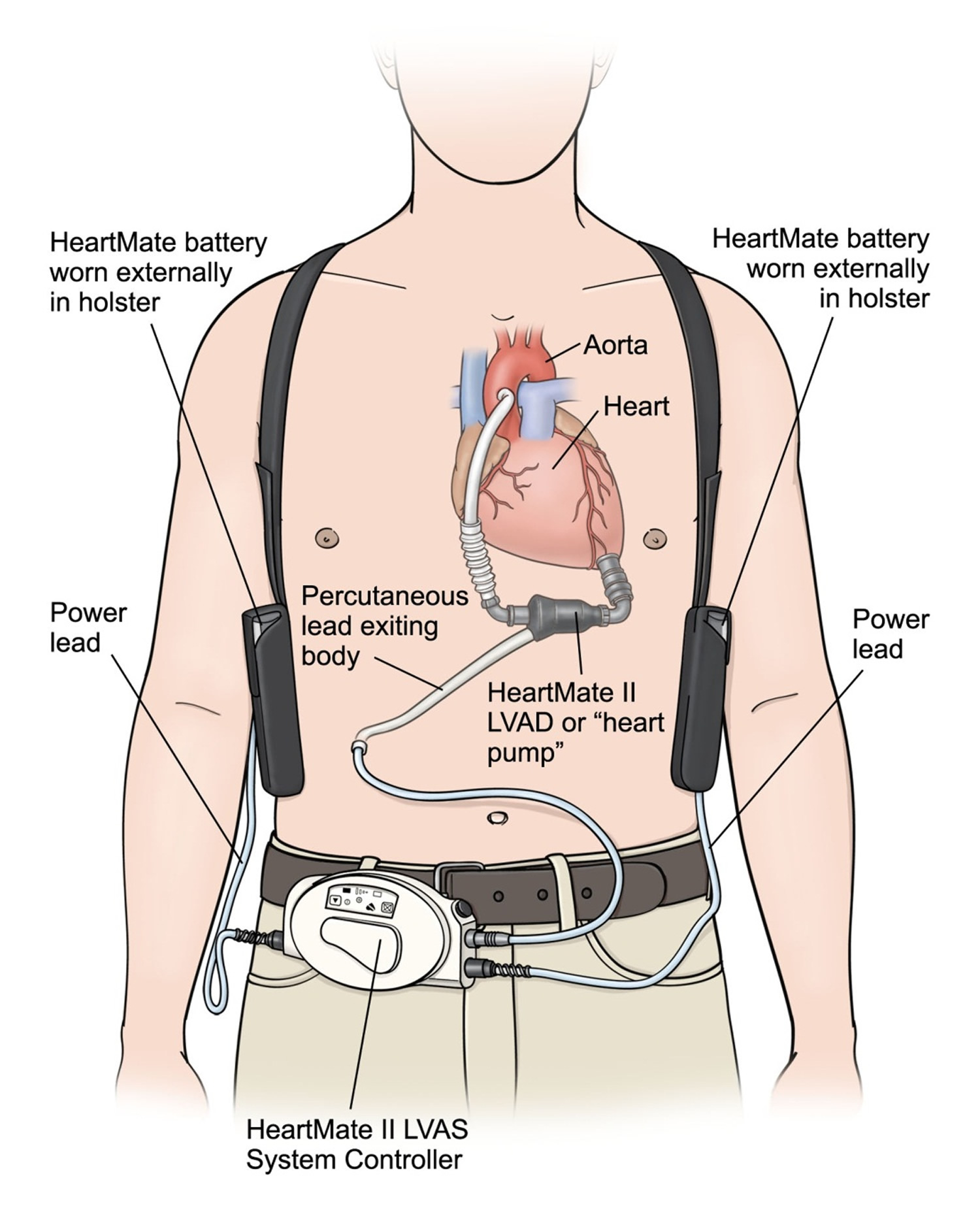
A ventricular assist device is a mechanical pump that is used to support heart function and blood flow in people who have weak hearts.
Your doctor may recommend a ventricular assist device if you have heart failure that isn’t responding to treatment or if you’re waiting for a heart transplant. You can use a ventricular assist device for a short time or for months or years, depending on your situation.
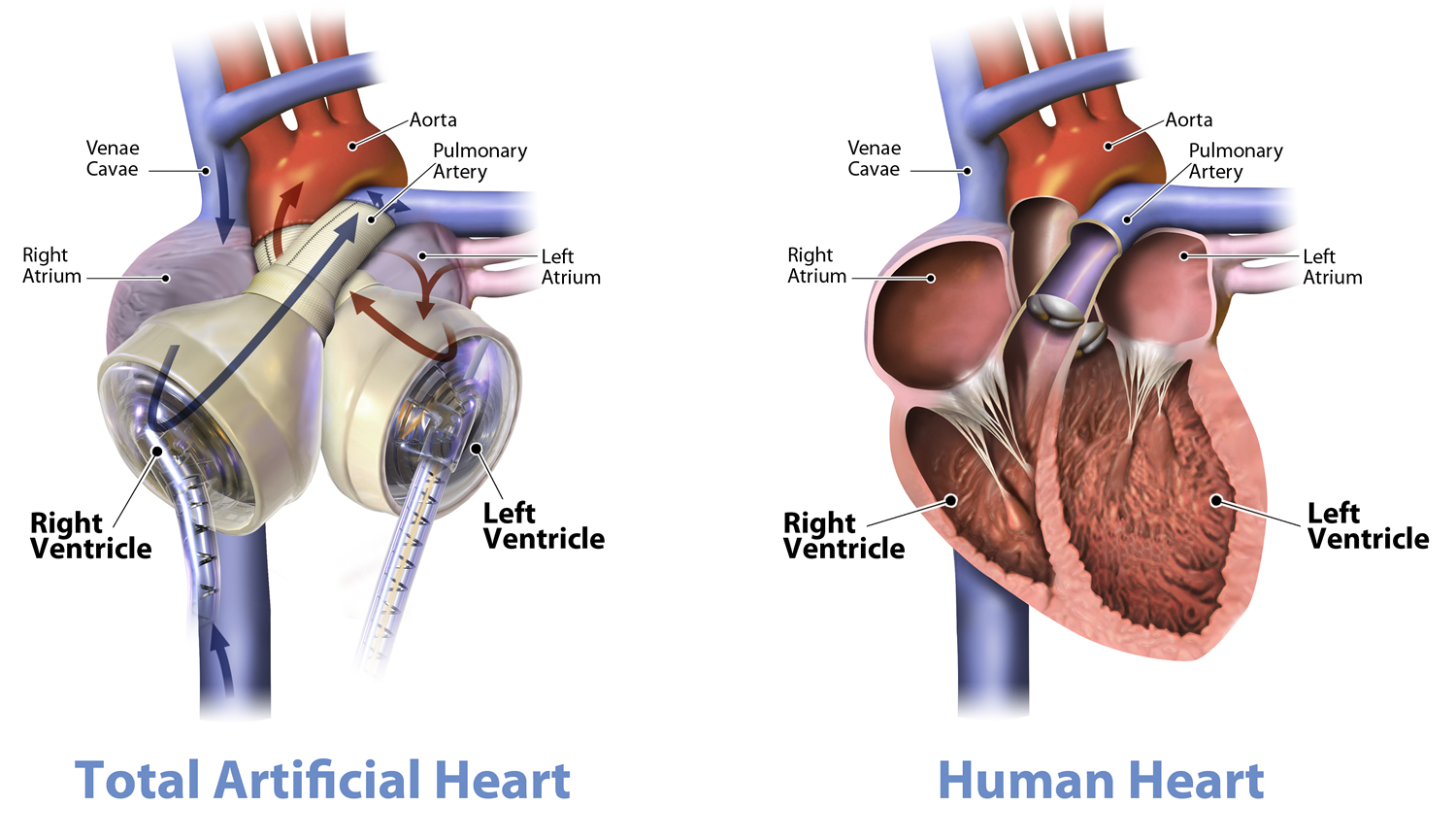
A total artificial heart is a device that replaces the two lower chambers of the heart (the ventricles). You may benefit from a TAH if both of your ventricles don’t work well due to end-stage heart failure.
Placing either device requires open-heart surgery.
Figure 12. Ventricular assist device
Figure 13. Total artificial heart
- Heart Surgery. Medline Plus, U.S. National Library of Medicine. https://medlineplus.gov/heartsurgery.html[↩]
- Heart Surgery. National Heart, Lung and Blood Institute, Department of Health and Human Services. https://www.nhlbi.nih.gov/health/health-topics/topics/hs/[↩][↩]
- What Are the Risks of Heart Surgery ? National Heart, Lung and Blood Institute, Department of Health and Human Services. https://www.nhlbi.nih.gov/health/health-topics/topics/hs/risks[↩][↩][↩]
- What To Expect After Heart Surgery. National Heart, Lung and Blood Institute, Department of Health and Human Services. https://www.nhlbi.nih.gov/health/health-topics/topics/hs/after[↩]
- Types of Heart Surgery. National Heart, Lung and Blood Institute, Department of Health and Human Services. https://www.nhlbi.nih.gov/health/health-topics/topics/hs/types[↩][↩][↩][↩]
- Ablation for Arrhythmias. American Heart Association. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/PreventionTreatmentofArrhythmia/Ablation-for-Arrhythmias_UCM_301991_Article.jsp[↩][↩]