Contents
- Esophagus pain
- Esophageal spasm
- Acid reflux
- Gastroesophageal acid reflux (GERD)
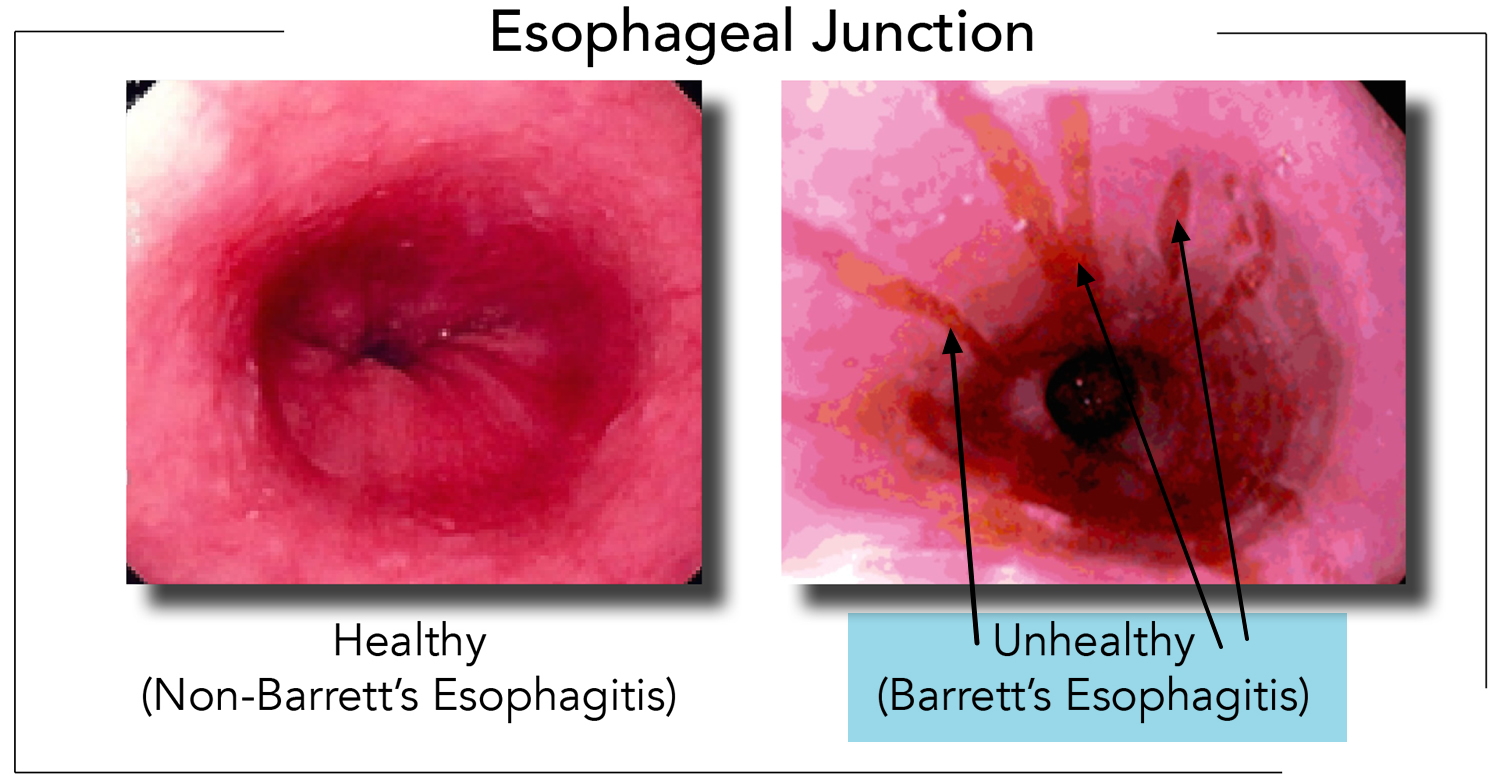
- Esophagitis
- Esophageal cancer
- Esophageal cancer causes
- Esophageal Cancer Risk Factors
- Esophageal Cancer Prevention
- Esophageal cancer signs and symptoms
- Esophageal cancer complications
- Esophageal cancer diagnosis
- Esophageal cancer treatment
Esophagus pain
Pain in the esophagus is non-specific sensation of discomfort or pain that you feel in your chest and can have many causes ranging from life-threatening medical emergency like a heart attack, pulmonary embolism (a sudden blockage in a lung artery due to a blood clot that breaks loose and travels through the bloodstream to the lungs) or angina (chest pain or discomfort that occurs when the heart’s blood flow is reduced) to digestive problems such as acid reflux or heartburn to esophagus disorders such as esophageal spasms, esophagitis (a condition in which the lining of the esophagus becomes swollen, inflamed, or irritated), gastroesophageal reflux disease (GERD) or esophageal cancer. Heartburn, acid reflux, esophageal spasm, angina and heart attack may feel very much alike. Don’t try to diagnose the cause yourself. Even experienced doctors can’t always tell the difference from your medical history and a physical exam. That’s why you must seek urgent medical attention. So if you are not sure seek medical attention immediately. If you have persistent chest pain, unexplained shortness of breath, and you aren’t sure it’s heartburn, call your local emergency number to ask for emergency medical help and an ambulance. Treatment depends on the cause of your chest pain.
The esophagus is a hollow muscular tube that carries food from your throat (pharynx) to your stomach. The esophagus lies behind the trachea (windpipe) and in front of the spine. In adults, the esophagus is usually between 10 and 13 inches (25 to 33 centimeters [cm]) long and is about ¾ of an inch (2cm) across at its smallest point 1. The esophagus starts with a special ring of muscle called the upper esophageal sphincter, formed in part by the cricopharyngeus muscle, and ends with the lower esophageal sphincter, surrounded by the crural diaphragm 2. When food enters your mouth, it mixes with saliva. The actions of salivary enzymes convert food into a mass called a food bolus. Once the food bolus reaches your throat (pharynx), swallowing starts, and relaxation of the upper esophageal sphincter ensues to allow passage of the food bolus into the esophagus 2. When you swallow, food and liquids travel through the inside of your esophagus called the lumen aided by peristaltic contractions of the esophageal muscles to reach your stomach. The lower part of your esophagus that connects to your stomach is called the gastroesophageal (GE) junction. A special ring of muscle near the gastroesophageal junction, called the lower esophageal sphincter (LES), controls the movement of food from the esophagus into the stomach. Between meals, it closes to keep the stomach’s acid and digestive juices out of the esophagus. When the food bolus finally reaches the distal end of the esophageal body, it triggers relaxation of the lower esophageal sphincter (LES), which in turn permits entry of the food bolus into your stomach.
What’s the best thing to do if you have chest pain and you’re not sure what’s causing it?
If you have persistent chest pain and you aren’t sure it’s heartburn, call your local emergency services number for emergency medical help.
See your doctor if you had an episode of unexplained chest pain that went away within a few hours and you did not seek medical attention. Both heartburn and a developing heart attack can cause symptoms that subside after a while. The pain doesn’t have to last a long time to be a warning sign.
Esophageal spasm
Esophageal spasm are painful abnormal painful contractions of the muscles in the esophagus (the muscular tube that carries food from your mouth to your stomach). Esophageal spasms do not move food effectively to your stomach. The cause of esophageal spasm is unknown. Very hot or very cold foods may trigger an episode of esophageal spasm in some people.
Esophageal spasm symptoms may include:
- Problems swallowing or pain with swallowing. Difficulty swallowing solids and liquids, sometimes related to swallowing specific substances. Red wine or extremely hot or cold liquids are more common culprits.
- Squeezing pain in your chest or upper abdomen that lasts from a few minutes to hours. The pain is often intense and might be mistaken for heart pain or heartburn.
- The feeling that an object is stuck in your throat.
- The return of food and liquids back up the esophagus also called regurgitation.
However, it can be hard to tell a esophageal spasm from angina pectoris, a chest pain or discomfort that occurs when your heart muscle doesn’t get enough oxygen-rich blood due to your heart’s arteries (coronary arteries) become partially or totally blocked. Angina is a common symptom of coronary artery disease (coronary heart disease) caused the lack of blood flow to your heart. A completely blocked coronary artery will cause a heart attack.
Esophageal spasms can feel like sudden, severe chest pain that lasts from a few minutes to hours. It can be hard to tell a esophageal spasm from angina (a symptom of heart disease) or a heart attack (myocardial infarction). A heart attack is a medical emergency. Call your local emergency number if you think you or someone else is having a heart attack.
Common heart attack symptoms include:
- Chest pain that may feel like pressure, tightness, fullness, squeezing, aching or pain. It is often in center or left side of the chest. It may go away and come back.
- Pain or discomfort that spreads to your shoulders, one or both arms, back, neck, jaw, teeth or sometimes your upper belly.
- It also can feel like heartburn or indigestion.
- Cold sweats.
- Fatigue.
- Heartburn.
- Nausea.
- Shortness of breath. Sometimes this is your only symptom. You may get it before or during the chest discomfort. It can happen when you are resting or doing a little bit of physical activity.
- Lightheadedness or sudden dizziness.
Chest pain is usually the most common symptom of heart attack. But for some people, such as women, the elderly and those with diabetes, symptoms may seem unrelated to a heart attack. For example, they may have nausea or a very brief pain in the neck or back. Some people having a heart attack don’t notice symptoms.
Coronary artery disease (coronary heart disease) symptoms may include:
- Chest pain called angina. You may feel squeezing, pressure, heaviness, tightness or pain in the chest. It may feel like somebody is standing on your chest. The chest pain usually affects the middle or left side of the chest. Activity or strong emotions can trigger angina. There are different types of angina. The type depends on the cause and whether rest or medicine makes symptoms better. In some people, especially women, the pain may be brief or sharp and felt in the neck, arm or back.
- Shortness of breath. You may feel like you can’t catch your breath.
- Fatigue. If your heart can’t pump enough blood to meet your body’s needs, you may feel unusually tired.
Symptoms of coronary artery disease may not be noticed at first. Sometimes symptoms only happen when the heart is beating hard, such as during exercise. As the coronary arteries continue to narrow, symptoms can get more severe or frequent.
Esophageal spasms may come and go (intermittent) or last for a long time (chronic). But sometimes the spasms are frequent and can prevent food and liquids from traveling through the esophagus. If esophageal spasms interfere with your ability to eat or drink, medicine can help relieve symptoms.
Nitroglycerin given under the tongue (sublingual) may help a sudden episode of esophageal spasm 3. Long-acting nitroglycerin and calcium channel blockers are also used for the problem 3.
Long-term (chronic) esophageal spasm cases are sometimes treated with low-dose antidepressants such as trazodone or nortriptyline to reduce symptoms 3.
Rarely, severe esophageal spasm cases may need dilation (widening) of the esophagus or surgery to control symptoms.
The squeezing chest pain associated with esophageal spasms can also be caused by a heart attack. If you experience squeezing chest pain, seek immediate medical care.
If you think you’re having a heart attack, immediately call your local emergency number for an ambulance and medical care. You should call, even if you are not sure that it is a heart attack. If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only as a last option.
The average person waits 3 hours before seeking help for symptoms of a heart attack. Sadly, many people with heart attack die before they reach a hospital. The sooner the person gets to the emergency room, the better the chance of survival. Prompt medical treatment reduces the amount of heart damage.
Are you having Esophageal spasm or Heart attack?
Each year almost 800,000 Americans have a heart attack. Every 40 seconds, someone in the United States has a heart attack 4. A heart attack happens when the flow of oxygen-rich blood to a section of heart muscle suddenly becomes blocked and the heart can’t get oxygen. If blood flow isn’t restored quickly, the section of heart muscle begins to die 5. But if you do get quick treatment, you may be able to prevent or limit damage to your heart muscle. That’s why it’s important to know the symptoms of a heart attack and call your local emergency services number if you or someone else is having a heart attack. You should call, even if you are not sure that it is a heart attack.
The most common warning symptoms of a heart attack for both men and women are:
- Chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest. The discomfort usually lasts for more than a few minutes or goes away and comes back. It can feel like pressure, squeezing, fullness, or pain. It also can feel like heartburn or indigestion. The feeling can be mild or severe.
- Upper body discomfort. You may feel pain or discomfort in one or both arms, the back, shoulders, neck, jaw, or upper part of the stomach (above the belly button).
- Shortness of breath. This may be your only symptom, or it may occur before or along with chest pain or discomfort. It can occur when you are resting or doing a little bit of physical activity.
Not everyone having a heart attack has typical symptoms. If you’ve already had a heart attack, your symptoms may not be the same for another one. However, some people may have a pattern of symptoms that recur.
Many people aren’t sure what’s wrong when they are having symptoms of a heart attack.
Not all heart attacks begin with the sudden, crushing chest pain that often is shown on TV or in the movies. In one study, for example, one-third of the patients who had heart attacks had no chest pain 6. These patients were more likely to be older, female, or diabetic.
The symptoms of a heart attack can vary from person to person. Some people can have few symptoms and are surprised to learn they’ve had a heart attack. If you’ve already had a heart attack, your symptoms may not be the same for another one. It is important for you to know the most common symptoms of a heart attack and also remember these facts:
- Heart attacks can start slowly and cause only mild pain or discomfort. Symptoms can be mild or more intense and sudden. Symptoms also may come and go over several hours.
- People who have high blood sugar (diabetes) may have no symptoms or very mild ones.
- The most common symptom, in both men and women, is chest pain or discomfort.
- Women are somewhat more likely to have shortness of breath, nausea and vomiting, unusual tiredness (sometimes for days), and pain in the back, shoulders, and jaw.
The more signs and symptoms you have, the more likely it is that you’re having a heart attack.
Other Common Signs and Symptoms include:
- Breaking out in a cold sweat
- Feeling unusually tired for no reason, sometimes for days (especially if you are a woman)
- Nausea (feeling sick to the stomach) and vomiting
- Light-headedness or sudden dizziness
- Any sudden, new symptom or a change in the pattern of symptoms you already have (for example, if your symptoms become stronger or last longer than usual)
The symptoms of angina can be similar to the symptoms of a heart attack. Angina is chest pain that occurs in people who have coronary heart disease, usually when they’re active. Angina pain usually lasts for only a few minutes and goes away with rest.
Chest pain or discomfort that doesn’t go away or changes from its usual pattern (for example, occurs more often or while you’re resting) can be a sign of a heart attack.
- All chest pain should be checked by a doctor.
The signs and symptoms of a heart attack can develop suddenly. However, they also can develop slowly—sometimes within hours, days, or weeks of a heart attack.
Any time you think you might be having heart attack symptoms or a heart attack, don’t ignore it or feel embarrassed to call for help. Call your local emergency number for emergency medical care, even if you are not sure whether you’re having a heart attack. Here’s why:
- Acting fast can save your life.
- An ambulance is the best and safest way to get to the hospital. Emergency medical services personnel can check how you are doing and start life-saving medicines and other treatments right away. People who arrive by ambulance often receive faster treatment at the hospital.
- The emergency phone operator or EMS technician can give you advice. You might be told to crush or chew an aspirin if you’re not allergic, unless there is a medical reason for you not to take one. Aspirin taken during a heart attack can limit the damage to your heart and save your life.
Every minute matters. Never delay calling your local emergency number in order to take aspirin or do anything else you think might help.
Heart attack treatment works best when it’s given right after symptoms occur.
- Don’t Wait–Get Help Quickly
- Quick Action Can Save Your Life
- If you think you or someone else is having a heart attack, even if you’re not sure, don’t feel embarrassed to call your local emergency number right away !
- Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. Take a nitroglycerin pill if your doctor has prescribed this type of treatment.
Other Names for a Heart Attack
- Myocardial infarction (MI)
- Acute myocardial infarction (AMI)
- Acute coronary syndrome
- Coronary thrombosis
- Coronary occlusion
Every year, about 790,000 Americans have a heart attack. Of these cases
- 580,000 are a first heart attack.
- 210,000 happen to people who have already had a first heart attack 4.
- About 15% of people who have a heart attack will die from it 4.
- Almost half of sudden cardiac deaths happen outside a hospital 7.
- One of 5 heart attacks is silent—the damage is done, but the person is not aware of it 4.
Heart attacks most often occur as a result of coronary heart disease (CHD), also called coronary artery disease. Coronary heart disease is a condition in which a waxy substance called plaque (cholesterol plaque) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart.
When plaque builds up in the arteries, the condition is called atherosclerosis. The buildup of plaque occurs over many years.
Eventually, an area of plaque can rupture (break open) inside of an artery. This causes a blood clot to form on the plaque’s surface. If the clot becomes large enough, it can mostly or completely block blood flow through a coronary artery.
If the blockage isn’t treated quickly, the portion of heart muscle fed by the artery begins to die. Healthy heart tissue is replaced with scar tissue. This heart damage may not be obvious, or it may cause severe or long-lasting problems.
Figure 2. Heart With Muscle Damage and a Blocked Artery
A less common cause of heart attack is a severe spasm (tightening) of a coronary artery. The spasm cuts off blood flow through the artery. Spasms can occur in coronary arteries that aren’t affected by atherosclerosis.
Heart attacks can be associated with or lead to severe health problems, such as heart failure and life-threatening arrhythmias.
Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. Arrhythmias are irregular heartbeats. Ventricular fibrillation is a life-threatening arrhythmia that can cause death if not treated right away.
Esophageal spasm causes
It’s not clear what causes esophageal spasms. However, they appear to be related to abnormal functioning of nerves that control the muscles you use when you swallow.
A healthy esophagus normally moves food into your stomach through a series of coordinated muscle contractions. Esophageal spasms make it difficult for the muscles in the walls of your lower esophagus to coordinate in order to move food to your stomach.
There are two types of esophageal spasms 8:
- Occasional contractions (diffuse esophageal spasms) also called corkscrew esophagus. This type of spasm may be painful and is often accompanied by regurgitation of food or liquids.
- Painfully strong contractions (nutcracker esophagus) also called jackhammer esophagus. Although painful, this type of spasm may not cause regurgitation of food or liquids.
Diffuse esophageal spasm
Diffuse esophageal spasm also called corkscrew esophagus is a rare motility disorder of the esophagus characterized by abnormal simultaneous, uncoordinated, or rapidly propagated contractions that are of normal amplitude leading to curling of the esophagus and accompanied by difficulty swallowing (dysphagia) 9, 10, 11, 12. Diffuse esophageal spasm is defined manometrically as simultaneous contractions in the smooth muscle of the esophagus alternating with normal peristalsis in over 20% of wet swallows with amplitude contractions of greater than 30 mmHg 12. However, after the introduction of high-resolution manometry (HRM) and esophageal pressure topography (EPT), the defining criteria for diffuse esophageal spasm has been changed, and is the presence of at least two premature contractions with a distal latency of under 4.5 seconds in a context of normal esophagogastric junction relaxation 13, 14. On barium swallow, diffuse esophageal spasm may appear as a corkscrew esophagus, but this is uncommon 15, 16.
Diffuse esophageal spasm is an unusual cause of 2% non-cardiac chest pain or 4% difficulty swallowing (dysphagia) 16. Diffuse esophageal spasm occurs most commonly in white, elderly, females and in people over 50 years old but can occur at any age.
Diffuse esophageal spasm occurs due to defective propagation of peristaltic waves through the esophageal wall 12. Several segments of the esophagus contract independently of each other simultaneously, therefore causing improper propagation of the food bolus in diffuse esophageal spasm 12. Diffuse esophageal spasm is thus characterized by quick wave progression through the esophageal wall and distinguished as a non-peristaltic wave during swallowing. However, many cases are thought to be caused by uncontrolled brain signals running to nerve endings 12.
The cause of diffuse esophageal spasm is unknown 12. There are various theories proposed. There is a disruption of coordination in peristalsis, which is probably due to an imbalance between the inhibitory and excitatory postganglionic pathways 12. Muscular hypertrophy or hyperplasia is present in the distal part of the esophagus, comprising almost two-thirds of the esophagus in diffuse esophageal spasm. Although the triggering event is unknown, the Increased release of acetylcholine might be a factor. Other theories include nitric oxide-mediated impairment of inhibitory ganglion neuronal function, gastric reflux, or a primary nerve or motor disorder as likely mechanisms of the peristaltic abnormalities seen in diffuse esophageal spasm 14. Exposure to acid can also result in esophageal spasms, whereas heartburn can lead to esophageal contractions 17, 18.
There have also been suggestions that total cholesterol and body mass index (BMI) are factors that have a high predictive value for esophageal contractility; at the same time, blood glucose and BMI are factors predictive for the function of the lower esophageal sphincter 19.
Figure 2. Diffuse esophageal spasm
Footnote: There is uncoordinated peristalsis in the thoracic esophagus with simultaneous contraction of the esophagus at multiple points also known as corkscrew esophagus or rosary bead esophagus.
[Source 20 ]Jackhammer esophagus
Jackhammer esophagus also called nutcracker esophagus is a rare hypercontractile disorder of the esophagus 21. Jackhammer esophagus is primarily diagnosed with high-resolution manometry (HRM) with high intra-esophageal pressure and normal peristalsis (involuntary muscle contractions that move food through the esophagus). The diagnostic criteria for Jackhammer esophagus (nutcracker esophagus) are at least 20% of swallows with a distal contractile integral (DCI) of > 8000 mmHg.s.cm (Figure 3). Studies showed that distal contractile integral (DCI) values of > 8000 mmHg.s.cm are rarely encountered in control healthy subjects and are usually associated with symptoms, such as difficulty swallowing and chest pain 22, 21, 23, 24. In Jackhammer esophagus or nutcracker esophagus, peristalsis is preserved and the distal contractile latency is normal, which differentiates it from achalasia and distal esophageal spasm, respectively 21. Jackhammer esophagus can be diagnosed even if the lower esophageal sphincter (LES) relaxation is impaired, when the median integrated relaxation pressure (IRP) is above the upper limit of normal range, as long as peristalsis is intact 22. Most patients will have a normal barium swallow x-ray (esophagram).
Jackhammer esophagus or nutcracker esophagus occurs in 10% of patients with non-cardiac chest pain 25. It was reported that about 70% of patients with Jackhammer esophagus presented with difficulty swallowing 23, 26, 27. The mean age of patients with Jackhammer esophagus was 62 years 22, 23.
The pathophysiology of Jackhammer esophagus remains uncertain, even though some observational studies suggested an association with esophagogastric outflow obstruction, gastroesophageal reflux disease (GERD) and eosinophilic esophagitis 23, 28, 29, 24. In a study, Jackhammer esophagus was observed in one patient with eosinophilic infiltration of the muscularis propria, in conjunction with elevated peripheral IgE levels but normal peripheral blood eosinophil levels 30. Endoscopic ultrasonography showed circumferential hypertrophy of the muscle layer. This entity has been referred to “eosinophilic esophageal myositis” 31. Some cases of Jackhammer esophagus are thought to be idiopathic, in the context of a primary motility disorder 28. It has been observed that the esophageal muscle thickness was increased on ultrasound in some patients with Jackhammer esophagus and that the circular and longitudinal layers showed asynchrony (absence or lack of concurrence in time) 21. A hypothesis to explain this is an abnormal cholinergic activity within the esophageal muscle innervation. Regardless of the cause of Jackhammer esophagus, the extreme hypercontractility is mainly located in the third contractile segment of the esophagus 21.
The natural course of Jackhammer esophagus is not well understood 30. One study reported a possible progression from Jackhammer esophagus to type III achalasia 22. The manometric predictor of this progression was an impaired esophagogastric junction (EGJ) relaxation (elevated median integrated relaxation pressure [IRP]) at the time of the initial high-resolution manometry (HRM) that diagnosed Jackhammer esophagus 22. The esophagogastric junction (EGJ) outflow obstruction is thought to cause motility “after load” against which the esophageal body has to contract more vigorously 22.
Jack hammer esophagus is a relatively rare disease and there is no definitive and dramatic treatment options. including medication, endoscopic treatments or surgical treatments 32. The therapeutic options for Jackhammer esophagus are drugs such as nitrates, phosphodiesterase 5 inhibitors, low-dose antidepressants, proton pump inhibitors, and endoscopic botulinum toxin injection into the esophageal body 32. However, the efficacy of these methods is not satisfactory 33, 34, 35, 36, 37. Per-oral endoscopic myotomy (POEM) has been used as an alternative treatment to overcome the limitations of the above therapies. However, there are still concerns regarding post-POEM complications, such as passage disturbance and sigmoid esophagus 38, 39, 40, 41.
Figure 3. Jackhammer esophagus
Footnotes: High resolution manometry (HRM) with pressure topography of a patient with Jackhammer esophagus. This hypercontractile swallow has normal integrated relaxation pressure (IRP) and distal latency (DL), with a distal contractile integral (DCI) superior to 8000 mmHg.s.cm.
[Source 30 ]Risk factors for esophageal spasm
Esophageal spasms are a rare condition. They tend to occur in people between the ages of 60 and 80, and may be associated with gastroesophageal reflux disease (GERD). Women are more likely to have esophageal spasms than men.
Other factors that can increase the risk of esophageal spasms include:
- High blood pressure
- Anxiety or depression
- Drinking red wine or consuming very hot or very cold foods or drinks.
Esophageal spasm prevention
Avoid very hot or very cold foods if you get esophageal spasms.
Esophageal spasm symptoms
Esophageal spasm signs and symptoms may include:
- Squeezing pain in your chest. The pain is often intense, and you might mistake it for heart pain (angina).
- Difficulty swallowing, sometimes related to swallowing specific substances, such as red wine or extremely hot or cold liquids.
- The feeling that an object is stuck in your throat.
- The return of food and liquids back up your esophagus (regurgitation).
Esophageal spasm diagnosis
To diagnose esophageal spasms, your doctor may recommend:
- Upper endoscopy called esophagogastroduodenoscopy (EGD). A flexible tube (endoscope) with a tiny camera on the end that is passed down your throat allows your doctor to see the inside of your esophagus. Your doctor may remove a tissue sample (biopsy) for testing to rule out other esophageal diseases.
- X-rays of the upper digestive system called an esophagram (barium swallow x-ray). Images of your esophagus are taken after you drink a contrast chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows a specialist doctor to see a silhouette of the esophagus, stomach and upper intestine. Some people may experience loose stools for 1 to 2 days after this test.
- Esophageal manometry. High-resolution manometry (HRM) is the gold standard for the diagnosis of esophageal motility disorders 42. Esophageal manometry test measures the rhythmic muscle contractions in the esophagus when you swallow water; the coordination and force exerted by the esophagus muscles; and how well the lower esophageal sphincter relaxes or opens during a swallow. During esophageal manometry, a thin, pressure-sensitive tube is passed through your nose, down the esophagus, and into your stomach. Esophageal manometry is done in a hospital or outpatient center by a specially trained doctor called a gastroenterologist. Before the procedure, you receive numbing medicine inside the nose. This helps make the insertion of the tube less uncomfortable. After the tube is in the stomach, the tube is pulled slowly back into your esophagus. At this time, you are asked to swallow. The pressure of the muscle contractions is measured along several sections of your esophagus. While the tube is in place, other studies of your esophagus may be done. The tube is removed after the tests are completed. The test takes about 1 hour.
- Esophageal pH monitoring. This test can determine if stomach acid is flowing back into your esophagus (acid reflux).
Esophageal spasm treatment
Treatment depends on the frequency and severity of your esophageal spasms. If your esophageal spasms are occasional, your doctor might recommend avoiding trigger foods or situations to see if that relieves symptoms.
If your esophageal spasms make it difficult to eat or drink, your doctor might recommend:
Managing any underlying conditions
Esophageal spasms are sometimes associated with conditions such as heartburn, gastroesophageal reflux disease (GERD), anxiety or depression. Your doctor might recommend a proton pump inhibitor such as lansoprazole to treat GERD. Sometimes an antidepressant, such as trazodone or imipramine (Tofranil), may be prescribed. Antidepressants may help reduce the sensation of pain in your esophagus.
Patients with diffuse esophageal spasm and other esophageal motility disorders who suffer from psychiatric illnesses like anxiety and depression as well can receive tricyclic antidepressant therapy. Tricyclic antidepressants improve esophageal as well as psychological symptoms, leading to better outcomes 12.
Esophageal spasm medication to relax your swallowing muscles
Nitroglycerin given under the tongue (sublingual) may help a sudden episode of esophageal spasm. Long-acting nitroglycerin and calcium channel blockers are also used for the problem.
Long-term (chronic) cases are sometimes treated with low-dose antidepressants such as trazodone or nortriptyline to reduce symptoms.
Sildenafil (Revatio, Viagra), onabotulinumtoxinA (Botox) injections into the esophagus or calcium channel blockers, such as diltiazem (Cardizem CD, Tiazac, others), can also reduce the severity of esophageal spasms.
Botulinum toxin (Botox) injection is also considered an effective and low-risk procedure for short-term symptom relief. OnabotulinumtoxinA (Botox) is usually only an option for medically high-risk patients 43.
Surgery (myotomy)
If medication doesn’t work, your doctor might recommend a procedure that involves cutting the muscle at the lower end of the esophagus, to weaken esophageal contractions 44. Myotomy should involve the entire length of the affected segment (determined preoperatively with manometry) and extend several centimeters superior to the proximal border of the spastic region to prevent remnants of spasticity 45. It should also extend through the lower esophageal sphincter (LES) to prevent difficulty swallowing by preventing outlet obstruction postoperatively. An antireflux procedure like a partial wrap or a Nissen fundoplication can be performed at the same time. Most patients with difficulty swallowing as the primary symptom improve after a myotomy 46.
However, long-term studies of this approach aren’t available, so myotomy generally isn’t recommended for esophageal spasms. It might be considered if other treatments don’t work. Heller myotomy combined with fundoplication is a rare alternative for the refractory patient 12.
Peroral endoscopic myotomy (POEM)
Peroral endoscopic myotomy (POEM) is a safe and effective treatment for patients, especially those who are refractory to medical therapy 47, 48, 49, 50. In this new minimally invasive technique, an endoscope inserted through your mouth and down your throat allows an incision (cut) in the inside lining of your esophagus. Then, as in myotomy, the surgeon cuts the muscle at the lower end of the esophagus. Like myotomy, POEM is usually considered only if other treatments don’t work.
Esophageal spasm diet
To help you cope with occasional esophageal spasms, try to 51:
- Avoid your triggers. Make a list of foods and beverages that cause your esophageal spasms.
- Choose food that is warm or cool. Let foods and drinks that are very hot or very cold sit for a bit before eating or drinking them.
- Find ways to control stress. Esophageal spasms may be more common or more severe when you’re stressed.
- Suck a peppermint lozenge. Peppermint oil is a smooth-muscle relaxant and might help ease esophageal spasms. Place the peppermint lozenge under your tongue.
Acid reflux
Acid reflux also called heartburn, acid indigestion, acid regurgitation or gastroesophageal reflux (GER) is a painful burning feeling in your chest or throat that occurs when stomach acid backs up into the tube called the esophagus that carries food from your mouth to your stomach 52, 53, 54. Typically, when food is swallowed, a band of muscle around the bottom of your esophagus called the lower esophageal sphincter (LES) relaxes to allow food and liquid to flow down into your stomach. Then the lower esophageal sphincter muscle tightens again. If the lower esophageal sphincter (LES) isn’t working as it should, stomach acid can flow back up into your esophagus (acid reflux) and you might feel a burning sensation in your chest, commonly called heartburn. The acid backup may be worse when you’re bent over, lying down, after eating a big meal or drinking coffee or alcohol. Pregnancy, certain foods, and some medications can bring on heartburn. Treating heartburn is important because over time as acid reflux can damage your esophagus.
Many people experience heartburn and reflux at some point in their lives. In a survey of more than 70,000 people living in the United States, nearly a third had experienced heartburn and reflux in the past week 55.
Typical signs and symptoms of heartburn include:
- A burning sensation in the chest that may also involve the upper abdomen
- Usually occurs after eating or while lying down or bending over
- May awaken you from sleep, especially if you have eaten within two hours of going to bed
- Is usually relieved by antacids
- May be accompanied by a sour taste in your mouth — especially when you’re lying down
- May be accompanied by a small amount of stomach contents rising up into the back of your throat (regurgitation)
Sometimes acid reflux progresses to gastroesophageal reflux disease (GERD), a more severe form of acid reflux 56, 57, 58, 59, 60. If you have heartburn more than twice a week, you may have gastroesophageal reflux disease (GERD). But you can have gastroesophageal reflux disease (GERD) without having heartburn. Gastroesophageal reflux disease (GERD) can present as non-erosive reflux disease or erosive esophagitis. Gastroesophageal reflux disease (GERD) can seriously damage your esophagus or lead to precancerous changes in the esophagus called Barrett’s esophagus. Gastroesophageal reflux disease (GERD) can occur at any age, even in babies. Many times, you or your doctor can determine the triggers for your reflux. Gastroesophageal reflux disease (GERD) treatment may require prescription medications and, occasionally, surgery or other procedures.
There are many lifestyle changes you can make to reduce or eliminate acid reflux, including:
- Not drinking alcohol
- Don’t smoke or use tobacco. Smoking decreases the lower esophageal sphincter’s ability to function properly.
- Don’t eat within 3 or 4 hours before bed. Wait at least three hours after eating before lying down or going to bed.
- Lose weight if you’re overweight. Excess weight put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your esophagus.
- Avoid tight-fitting clothing that are tight around your waist or abdomen. Clothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
- Avoid foods or drinks that trigger your heartburn, such as chocolate, caffeine, peppermints, fried or fatty foods, spicy, and acidic foods
- Eating smaller meals or avoiding overeating
- Eat food slowly and chew thoroughly. Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Try to find ways to relax.
Don’t stop taking any prescribed medicine without speaking to a doctor first
Many nonprescription medications can help relieve heartburn. The options include:
- Antacids, such as Alka-Seltzer, Maalox, Mylanta, Rolaids, and Riopan, which help neutralize stomach acid, are usually the first drugs recommended to relieve symptoms of heartburn. Antacids may provide quick relief. But they can’t heal an esophagus damaged by stomach acid. Many brands on the market use different combinations of three basic salts—magnesium, calcium, and aluminum—with hydroxide or bicarbonate ions to neutralize the acid in the stomach. Antacids, however, can have side effects. Magnesium salt can lead to diarrhea, and aluminum salt may cause constipation. Aluminum and magnesium salts are often combined in a single product to balance these effects. Calcium carbonate antacids, such as Tums, Titralac, and Alka-2, can also be a supplemental source of calcium, though they may cause constipation.
- H2-receptor blockers (Histamine Type-2 Receptor Antagonists) include ranitidine (Zantac), cimetidine (Tagamet HB), famotidine (Pepcid AC), and nizatidine (Axid AR) and are available both by prescription and over-the-counter. H2-receptor blockers treat symptoms of indigestion by reducing the amount of stomach acid released into your digestive tract, which relieves ulcer pain and encourages healing. Stronger versions of these medicines also are available by prescription. They work longer than but not as quickly as antacids. Side effects of H2-receptor blockers may include headache, nausea, vomiting, constipation, diarrhea, and unusual bleeding or bruising.
- Proton pump inhibitors (PPIs) reduce stomach acid by blocking the action of the parts of cells that produce acid. Proton pump inhibitors (PPIs), which are stronger than H2-receptor blockers, also treat indigestion symptoms by reducing stomach acid. Proton pump inhibitors (PPIs) are most effective in treating symptoms of indigestion in people who also have GERD. Proton pump inhibitors (PPIs) include the prescription and over-the-counter medications omeprazole (Prilosec, Zegerid), lansoprazole (Prevacid), rabeprazole (Aciphex), esomeprazole (Nexium), dexlansoprazole (Dexilant) and pantoprazole (Protonix). There are very few medical differences between these drugs. However, long-term use of proton pump inhibitors (PPIs), particularly at high doses, may increase your risk of hip, wrist and spine fracture. Ask your doctor whether a calcium supplement may reduce this risk. In patients whose symptoms improve with proton pump inhibitors (PPIs), PPI (proton pump inhibitor) therapy should be discontinued every 6 to 12 months to reduce the long-term risk of therapy. Side effects of PPIs may include back pain, aching, cough, headache, dizziness, abdominal pain, gas, nausea, vomiting, constipation, and diarrhea. The standard dosages of orally administered proton pump inhibitors are as follows:
- Lansoprazole 30 mg daily
- Omeprazole 20 mg daily
- Pantoprazole 40 mg daily
- Rabeprazole 20 mg daily
- Esomeprazole 20 mg daily
- Proton pump inhibitors (PPIs) require a meal to activate them. You should eat a meal within 30 minutes to 1 hour after taking this medication for the acid suppression therapy to work most effectively. Waiting later than this time can decrease the positive effect of this medication. This might delay healing or even result in the failure of the ulcer to heal.
The World Gastroenterology Organization’s guidelines for treating frequent heartburn (heartburn symptoms two or more days/week) recommend a two-week course of treatment with an over-the-counter PPI (proton pump inhibitor) along with lifestyle and dietary modifications 61. In the US, over-the-counter esomeprazole 20 mg is approved for 14 days of treatment for frequent heartburn, a treatment course that can be repeated once every four months; however, if symptoms persist or recur within this time frame the individual should consult a physician 61, 62.
If nonprescription treatments don’t work or you rely on them often, see your doctor. You may need prescription medication and further testing. Additional tests might include:
- pH test. This test checks for acid in the esophagus.
- Upper endoscopy or gastroscopy. This procedure checks for other conditions. During it, your doctor looks into your stomach through a long, thin tube that is inserted down your esophagus. You are sedated for this procedure, so you don’t feel it. Your doctor may also check for Helicobacter pylori, bacteria that can cause ulcers.
How can I tell the difference between a acid reflux and heart attack?
Heartburn, angina and heart attack may feel very much alike. Even experienced doctors can’t always tell the difference from your medical history and a physical exam. That’s why, if you go to the emergency room because of chest pain, you’ll immediately have tests to rule out a heart attack.
The “textbook” heart attack involves sudden, crushing chest pain and difficulty breathing, often brought on by exertion. Many heart attacks don’t happen that way, though. The signs and symptoms of a heart attack vary greatly from person to person. Heartburn itself can accompany other symptoms of heart attack.
Typical heart attack signs and symptoms include:
- Pressure, tightness, pain, or a squeezing or aching sensation in your chest or arms that may spread to your neck, jaw or back
- Nausea, indigestion, heartburn or abdominal pain
- Shortness of breath
- Cold sweat
- Fatigue
- Lightheadedness or sudden dizziness
The most common symptom of heart attack for both men and women is chest pain or discomfort. But women are more likely than men to experience some of the other symptoms, such as jaw or back pain, shortness of breath, and nausea or vomiting. Heart problems are more common among people who have high blood pressure, diabetes or high cholesterol. Smoking and being overweight are other risk factors.
Is acid reflux the same as gastroesophageal reflux disease (GERD)?
Acid reflux and gastroesophageal reflux disease (GERD) are closely related, but the terms don’t necessarily mean the same thing.
Gastroesophageal reflux disease (GERD) is defined as “a condition that develops when the reflux of stomach contents into the esophagus causes troublesome symptoms and/or complications” 63. The Montreal Definition of gastroesophageal reflux disease (GERD) encapsulates most complications from patients with reflux esophagitis with or without symptoms (the latter actually accounting for close to 40% of such patients in Western populations, and possibly a much higher proportion in Asian populations) to those with symptoms but no other findings 64, 65. The most common symptom of gastroesophageal reflux disease (GERD) is frequent heartburn — two or more times a week. Other symptoms can include regurgitation of food or sour liquid, difficulty swallowing, coughing, wheezing, and chest pain — especially while lying down at night.
Acid reflux also known as gastroesophageal reflux (GER) is the backward flow of stomach acid into the tube that connects your throat to your stomach called the esophagus. During an episode of acid reflux, you might feel a burning sensation in your chest, commonly called heartburn. This can happen after eating a big meal or drinking coffee or alcohol.
Sometimes acid reflux progresses to gastroesophageal reflux disease (GERD), a more severe form of acid reflux.
Acid reflux causes
Acid reflux occurs when stomach acid backs up into the tube (esophagus) that carries food from your mouth to your stomach. Typically, when food is swallowed, a band of muscle around the bottom of the esophagus called lower esophageal sphincter (LES) relaxes to allow food and liquid to flow down into your stomach. Then the muscle tightens again. If the lower esophageal sphincter (LES) isn’t working as it should, stomach acid can flow back up into the esophagus (acid reflux) and cause heartburn. The acid backup may be worse when you’re bent over or lying down.
Hiatus hernia, a condition in which part of your stomach is pushed up through the diaphragm (the muscle wall between the stomach and chest) and into your chest, can also compromise lower esophageal sphincter (LES) function and cause heartburn
Risk factors for acid reflux
Certain foods and drinks can trigger heartburn in some people, including:
- Spicy foods
- Onions
- Citrus products
- Tomato products, such as ketchup
- Fatty or fried foods
- Peppermint
- Chocolate
- Alcohol, carbonated beverages, coffee or other caffeinated beverages
- Large or fatty meals
Being overweight or pregnant also can increase your risk of experiencing heartburn.
Acid reflux during pregnancy
Acid reflux is one of the most common gastrointestinal symptoms in pregnant women 66, 67. Acid reflux can occur in all trimesters of pregnancy and occurs in approximately two-thirds of all pregnancies reaching 80% in some populations 68, 69, 70, 71, 68, 72. Most women begin their symptoms late in the first trimester or in the second trimester and these symptoms become more frequent and severe in the final months of pregnancy 73, 67. The symptoms of heartburn in pregnancy may be frequent, severe and distressing, but serious complications are rare, symptoms are generally limited to the pregnancy period without long-term effects 73, 74.
Pregnancy hormones appear to weaken the lower esophageal sphincter (LES) muscle and your uterus pressing up against your stomach as your baby grows encourages acid reflux. You’re more likely to get heartburn during pregnancy if you’ve had a baby before or if you get heartburn when you’re not pregnant 67. Generally, if there has not been too much weight gain during the pregnancy, a woman’s heartburn improves after delivery.
The diagnosis of heartburn is based on clinical history. Upper endoscopy and other diagnostic tests are infrequently performed 75, 67, 76.
What might help for acid reflux during pregnancy:
- Eat several small meals instead of three large meals — eat slowly.
- Drink fluids between meals — not with meals.
- Don’t eat greasy and fried foods.
- Avoid citrus fruits or juices and spicy foods.
- Do not eat or drink within a few hours of bedtime.
- Do not lie down right after meals.
See your doctor if symptoms don’t improve after trying these suggestions. Ask your doctor about using an antacid.
If your heartburn doesn’t improve by changing how you eat, your doctor may suggest that you take medicine for it. Antacids are the first type of medicine to try. They can relieve your symptoms quickly. Antacids are safe in pregnancy as long as you don’t take more than the recommended dose. There are many different types — talk to your pharmacist to find one that’s most suitable for you.
If antacids don’t control your symptoms, speak to your doctor about other medicines you can take.
Figure 4. Acid reflux during pregnancy treatment algorithm
Footnote: Step-up approach towards management of gastroesophageal reflux disease (GERD) during pregnancy.
Abbreviations: GERD = gastroesophageal reflux disease, H2RA = histamine-2 receptor antagonist, PPI = proton pump inhibitor.
[Source 66 ]If your heartburn symptoms don’t go away with medicine, it’s important to see your doctor. A serious pregnancy condition called pre-eclampsia can cause pain under your ribs and a feeling of heartburn.
You should also see your doctor immediately if:
- you are vomiting up blood
- you are losing weight
- swallowing is painful or difficult
Can acid reflux during pregnancy hurt my baby?
Acid reflux during pregnancy usually won’t cause any problems for your baby, but it’s uncomfortable for you.
A healthy diet is important for both your and your baby’s health. If heartburn is making it hard to eat healthy food, it’s best to treat it.
Acid reflux during pregnancy causes
The cause of heartburn during pregnancy is multifactorial, involving both hormonal and mechanical factors. Pregnancy hormones called estrogen and progesterone, can relax the the lower esophageal sphincter (LES) muscle that usually holds your esophagus closed where it meets your stomach 72, 77, 78. The lowest lower esophageal sphincter pressure occurs at 36 weeks gestation 78. This allows food and acid from your stomach to go back up your esophagus. Pregnancy hormones also slow down the muscles of your digestive tract. So food tends to move more slowly and digestion is sluggish. This causes many pregnant women to feel bloated.
Other factors that may also play a part in heartburn during pregnancy are increased intragastric pressure secondary to the enlarging uterus and changes in gastrointestinal motility through ineffective esophageal motility, with prolonged clearance time 72, 79.
Abnormal gastric emptying or delayed small bowel transit might also contribute to heartburn in pregnancy 67.
Heartburn becomes more common as your pregnancy progresses. This can happen when your uterus (womb) pushes up against your stomach as your baby grows. This also pushes the contents of your stomach up into your esophagus.
Risk factors for heartburn in pregnancy include advancing gestational age, heartburn symptom before getting pregnant and women who have previously had one or more babies 67.
Heartburn can also be triggered by what you eat and drink, such as:
- a big meal
- high-fat foods
- spicy foods
- chocolate
- citrus fruit juices
- drinks containing caffeine, including coffee, tea and cola
- alcohol (which is not recommended in pregnancy)
Other things that may trigger heartburn include:
- doing exercise soon after eating
- lying down after eating
- feeling anxious
Because mothers are different, it’s a good idea to take note of the particular foods, drinks or activities that give you heartburn while you are pregnant.
Acid reflux during pregnancy prevention
If your symptoms are mild, changing how you eat may help prevent heartburn. You could try:
- eating smaller meals more often and eating slowly
- avoiding eating for 2 or 3 hours before exercise or going to bed
- avoiding foods and drinks that give you heartburn
- avoiding eating and drinking at the same time, which can make your stomach more full
- sitting up straight while eating and not lying down after a meal
- raising the head of your bed or sleeping on at least 2 pillows
- sleeping on your left side
You might find it helpful to chew gum, which makes you produce more saliva to help neutralize the acid from your stomach. Drinking milk can also help neutralize acid.
Acid reflux during pregnancy treatment
If your heartburn doesn’t improve by changing how you eat, your doctor may suggest that you take medicine for it. Antacids are the first type of medicine to try. They can relieve your symptoms quickly. Antacids are safe in pregnancy as long as you don’t take more than the recommended dose. There are many different types — talk to your pharmacist to find one that’s most suitable for you.
If antacids don’t control your symptoms, speak to your doctor about other medicines you can take.
The common drugs used for the treatment of heartburn in pregnancy include antacids, sucralfate, H2 receptor blockers (histamine-2 receptor antagonists), prokinetic drugs (drugs that stimulate the muscles of the gastrointestinal tract to prevent acids from staying in the stomach too long), proton pump inhibitors (PPIs), and alginate-based reflux suppressants such as Liquid Gaviscon and Gaviscon Advance 80, 81, 67. Traditional Chinese Medicine such as acupuncture has been used in treatment of heartburn in pregnancy in one study 82. There are insufficient data to assess acupuncture versus no treatment 83. More research is needed on acupuncture and other complimentary therapies as treatments for heartburn in pregnancy 83.
Acid reflux prevention
There are ways to prevent gastroesophageal reflux disease and acid reflux. To start, you need to know your body and how it reacts to different food and drinks. Spicy and acidic foods and carbonated drinks can trigger acid reflux. Try to avoid those things when possible. Eat smaller meals throughout the day, and don’t eat too late at night. Don’t lie down too soon after eating. Limit the use of alcohol. If you use tobacco, try to quit. Stress and lack of sleep also can worsen symptoms.
There are many dietary and lifestyle changes you can make to reduce or eliminate acid reflux, including:
- Not drinking alcohol
- Not smoking
- Avoid these foods and drinks that are commonly known to be heartburn triggers
- Fried foods
- Fast foods
- Pizzas
- Potato chips and other processed snacks
- Chili powder and pepper (white, black, cayenne)
- Fatty meats such as bacon and sausage
- Cheese
- Alcohol
- Carbonated beverages
- Caffeine
- Acidic foods
- Peppermints
- Not eating too close to bedtime
- Losing weight
- Not wearing tight clothing
- Eating smaller meals or avoiding overeating
Foods that help prevent acid reflux
Ginger is one of the best digestive aids because of its medicinal properties. Ginger is alkaline in nature and anti-inflammatory, which eases irritation in the digestive tract. Try sipping ginger tea when you feel heartburn coming on.
High-fiber foods
Fibrous foods make you feel full so you’re less likely to overeat, which may contribute to heartburn. So, load up on healthy fiber from these foods:
- Whole grains such as oatmeal, couscous and brown rice.
- Root vegetables such as sweet potatoes, carrots and beets.
- Green vegetables such as asparagus, broccoli and green beans.
Alkaline foods
Foods that have a low pH are acidic and more likely to cause reflux. Those with higher pH are alkaline and can help offset strong stomach acid. Alkaline foods include:
- Bananas
- Melons
- Cauliflower
- Fennel
- Nuts
Watery foods
Eating foods that contain a lot of water can dilute and weaken stomach acid. Choose foods such as:
- Celery
- Cucumber
- Lettuce
- Watermelon
- Broth-based soups
- Herbal tea
Acid reflux symptoms
Symptoms of acid reflux include:
- A burning pain in your chest that usually occurs after eating and may occur at night
- Pain that worsens when lying down or bending over
- A bitter or acidic taste in your mouth
Symptoms are often worse after eating, when lying down or when bending over.
You may also have:
- Non-burning chest pain, which is usually located in the middle of the chest and radiates to the back
- Difficulty swallowing (dysphagia)
- Atypical reflux symptoms relating to the throat, larynx or lungs:
- Sore throat
- Coughing or hiccups that keep coming back
- Increased salivation
- Shortness of breath
- A hoarse voice
- Bad breath
- Bloating and feeling sick
Acid reflux complications
Acid reflux that occurs frequently and interferes with your routine is considered gastroesophageal reflux disease (GERD). Gastroesophageal reflux disease (GERD) can seriously damage your esophagus or lead to precancerous changes in the esophagus called Barrett’s esophagus.
Gastroesophageal reflux disease (GERD) can sometimes lead to the following complications:
- Swelling of the vocal cords, also known as reflux laryngitis
- Inflammation of the tissue in the esophagus (esophagitis). Stomach acid can break down tissue in the esophagus, causing inflammation, bleeding, and sometimes an open sore (ulcer). Esophagitis can cause pain and make swallowing difficult.
- Narrowing of the esophagus (esophageal stricture), caused by scar tissues that develop due to repeated ulcerations. Damage to the lower esophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing. American College of Gastroenterology guidelines recommend esophageal dilation and continue proton pump inhibitor (PPI) therapy to prevent the need for repeated dilations 84.
- Barrett’s esophagus, a precancerous changes to the esophagus tissue caused by long-lasting gastroesophageal reflux disease which increases the risk of esophageal cancer. Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s esophagus 85.
- Lung damage which may include pulmonary fibrosis and bronchiectasis
- Ulcers in the esophagus, caused by burning from stomach acid.
Acid reflux diagnosis
To determine if your acid reflux is a symptom of gastroesophageal reflux disease (GERD) starts with a thorough medical history during which you describe your signs and symptoms and physical examination. If the typical symptoms of acid reflux disease are present, including heartburn and regurgitation, your doctor may begin treatment without performing specific diagnostic tests.
However, tests may be performed if:
- Your symptoms are atypical
- The severity of acid reflux raises concerns about esophageal damage
- Symptoms do not respond to initial treatment
- Your doctor is considering anti-reflux surgery
To confirm a diagnosis of gastroesophageal reflux disease (GERD) or to check for complications, your doctor might recommend:
- Upper endoscopy or gastroscopy. Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat. The endoscope helps your provider see inside your esophagus and stomach. Test results may not show problems when reflux is present, but an endoscopy may detect inflammation of the esophagus (esophagitis) or other complications. An endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications such as Barrett esophagus. In some instances, if a narrowing is seen in the esophagus, it can be stretched or dilated during this procedure. This is done to improve trouble swallowing (dysphagia).
- Transnasal esophagoscopy. This test is done to look for any damage in your esophagus. A thin, flexible tube with a video camera is put through your nose and moved down your throat into the esophagus. The camera sends pictures to a video screen.
- Reflux testing (wireless pH/pH impedance). Ambulatory acid (pH) probe is placed in your esophagus to identify when, and for how long, stomach acid regurgitates there. The monitor connects to a small computer that you wear around your waist or with a strap over your shoulder. The monitor might be a thin, flexible tube (catheter) that’s threaded through your nose into your esophagus. Or it might be a clip that’s placed in your esophagus during an endoscopy. The clip passes into your stool after about two days.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- Your doctor performs an endoscopy and places a small chip in your lower esophagus
- The chip records the acid level in your esophagus for 48 hours.
- The chip transmits your acid level to a wireless recording device that you wear around your belt.
- The data from the recording device can gauge your reflux severity.
- 24-Hour pH Impedance. Your doctor may order this procedure to evaluate your reflux. This procedure monitors your pH level (level of acidity) for a prolonged period. During pH impedance:
- Your doctor places a thin, flexible catheter with an acid-sensitive tip through your nose into your esophagus. The catheter is placed in separate recording spots to evaluate the flow of liquid from your stomach into your esophagus.
- The catheter stays in your nose for a period of 24 hours.
- Your doctor is able to evaluate whether you have GERD, the severity of your reflux, the presence of non-acid reflux and the correlation between your reflux and symptoms. This procedure helps in the design of a course of treatment for you.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- X-ray of the upper digestive system. X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus and stomach. This is particularly useful for people who are having trouble swallowing. You may also be asked to swallow a barium pill that can help diagnose a narrowing of the esophagus that may interfere with swallowing.
- Esophageal manometry also known as esophageal motility (movement) studies. This test measures the rhythmic muscle contractions in your esophagus when you swallow. Esophageal manometry also measures the coordination and force exerted by the muscles of your esophagus. This is typically done in people who have trouble swallowing. An esophageal manometry is an essential part of the assessment process prior to anti-reflux surgery.
- During an esophageal manometry your doctor places a pressure-sensitive catheter into the esophagus. This may be performed right before esophageal pH impedance studies, as it determines where your doctor should place the catheter. The catheter evaluates the strength and coordination of your muscle contractions. It also tests the strength and relaxation function of the lower esophageal sphincter.
- Barium esophagram also called barium swallow, is an imaging test that checks for problems in your upper gastrointestinal tract. Your upper gastrointestinal tract includes your mouth, back of the throat, esophagus, stomach, and first part of your small intestine. The test uses a special type of x-ray called fluoroscopy. Fluoroscopy is a kind of X-ray “movie.” A barium esophagram also evaluates the coordination of your esophageal motor function. While it does not test for the presence of reflux, it is useful for evaluating injury to your esophagus.
- During barium contrast radiography:
- You swallow a contrast solution called barium.
- The barium coats your esophagus and gastrointestinal tract, making it easier for the doctor to detect abnormalities.
- An X-ray is taken.
- During the X-ray, your doctor looks for a narrowing in the esophagus called a stricture.
- During barium contrast radiography:
Acid reflux treatment
If your symptoms are mild, treatment may not be necessary. Your doctor is likely to recommend that you first try lifestyle changes and nonprescription medications. If you don’t experience relief within a few weeks, your doctor might recommend prescription medication and additional testing.
Over-the-counter medicine is effective for treating mild cases of acid reflux. These medicines include:
- Antacids: This is a quick-acting medicine that reduces stomach acid. Unfortunately, antacids alone won’t heal the damage stomach acid causes in your esophagus. Sometimes, overusing antacids can cause diarrhea or constipation.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists): These medicines reduce acid production. They don’t work as quickly as antacids. However, they provide longer relief (up to 12 hours). Stronger versions of these medications are available by prescription from your doctor.
- Proton pump inhibitors (PPIs): These medicines block acid production and heal the damage in your throat. They are stronger than H2-receptor blockers.
If these medicines are not providing relief after a few weeks, contact your doctor. Your doctor may give you a prescription version of H2 receptor blockers or proton pump inhibitors. Additionally, your doctor may prescribe medicine to strengthen the lower esophageal sphincter. The medicine may decrease the number of times your muscle relaxes. It is often used for severe reflux. Side effects include fatigue or confusion. Another medicine your doctor may prescribe helps your stomach empty faster. This will cause the food to move along the digestive tract and not back up into your throat. Your doctor may combine more than one medicine, depending upon the severity of your reflux.
In some cases, surgery may be required to treat acid reflux. This is when medicine doesn’t help, or if you want a long-term solution. Types of surgery may include:
- Nissen fundoplication: This surgery reinforces the lower muscle in the esophagus. A surgeon will wrap the very top of the stomach around the outside of the lower esophagus. This reduces reflux by putting pressure on your esophagus. This is a laparoscopic surgery. This means the surgeon makes three or four small cuts in the abdomen (stomach region). He or she will insert instruments, including a flexible tube with a tiny camera, through the cuts.
- Linx surgery: This surgery strengthens the muscle in the esophagus. The Linx device is a ring of tiny beads made of titanium. The surgery wraps the ring around the area between the stomach and esophagus. The magnetic attraction of the beads keeps the opening between the two closed. This helps keep acid from backing up into your throat. However, it’s weak enough to allow food to pass. The surgery is minimally invasive.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Home remedies for acid reflux
You can ease, stop or reduce heartburn and acid reflux yourself by doing the following:
- Eat smaller, more frequent meals.
- Eat food slowly and chew thoroughly. Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Lose weight if you’re overweight. Excess weight put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your esophagus.
- Try to find ways to relax
- Avoid foods or drinks that trigger your heartburn — such as alcohol, fried or fatty foods, chocolate, and peppermint.
- Don’t eat within 3 or 4 hours before bed. Wait at least three hours after eating before lying down or going to bed.
- Avoid tight-fitting clothing that are tight around your waist or abdomen. Clothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
- Don’t smoke or use tobacco. Smoking decreases the lower esophageal sphincter’s ability to function properly.
- Don’t drink alcohol
- Don’t stop taking any prescribed medicine without speaking to a doctor first
Elevate the head of your bed. You may find that using wood, bricks or books under the feet at the head end of your bed to raise the head of your bed by around 10 to 20 cm, so your chest and head are above your waist, helps relieve symptoms. This can help stop stomach acid traveling up towards your throat. If you can’t elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows isn’t effective as this can increase pressure on your abdomen and make your symptoms worse. When you go to bed, start by lying on your left side to help make it less likely that you will have reflux.
Alternative medicine
Some complementary and alternative therapies, such as ginger, chamomile and slippery elm, may be recommended to treat gastroesophageal reflux disease. However, none have been proved to treat gastroesophageal reflux disease or reverse damage to the esophagus. Talk to your doctor if you’re considering taking alternative therapies to treat GERD.
Nonprescription medications
If necessary, occasional acid reflux can be treated with nonprescription medication, options include:
- Antacids that neutralize stomach. Antacids containing calcium carbonate such as Mylanta, Rolaids and Tums, may provide quick relief. But antacids alone won’t heal an inflamed esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or sometimes kidney problems.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists) to reduce acid production, such as cimetidine (Tagamet HB), famotidine (Pepcid AC) or nizatidine (Axid AR). H-2 blockers don’t act as quickly as antacids, but they provide longer relief and may decrease acid production from the stomach for up to 12 hours. Stronger versions are available by prescription.
- Proton pump inhibitors (PPIs) block acid production and heal the esophagus. Proton pump inhibitors are stronger acid blockers than H-2 blockers and allow time for damaged esophageal tissue to heal. Nonprescription proton pump inhibitors include lansoprazole (Prevacid 24 HR), omeprazole (Prilosec OTC) and esomeprazole (Nexium 24 HR).
If you suspect that you have gastroesophageal reflux disease (GERD), your symptoms worsen, or you have nausea, vomiting or difficulty swallowing, talk to your doctor. Prescription medications might help. In a few cases, gastroesophageal reflux disease (GERD) might be treated with surgery or other procedures.
Prescription medications
Prescription-strength treatments for gastroesophageal reflux disease (GERD) include:
- Prescription-strength proton pump inhibitors. Prescription-strength proton pump inhibitors include esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix), rabeprazole (Aciphex) and dexlansoprazole (Dexilant). Although generally well tolerated, prescription-strength proton pump inhibitors might cause diarrhea, headaches, nausea, or in rare instances, low vitamin B-12 or magnesium levels.
- Prescription-strength H-2 blockers. Prescription-strength H-2 blockers include prescription-strength famotidine and nizatidine. Side effects from these medications are generally mild and well tolerated.
Multiple studies have demonstrated that proton-pump inhibitors (PPIs) provide superior therapeutic efficacy in the management of GERD than other antireflux medications such as H-2 receptor antagonists 86. Overall, proton-pump inhibitors (PPIs) demonstrate an unsurpassed rates of symptomatic relief and healing of esophageal inflammation as well as significant improvement in health-related quality of life in patients with erosive esophagitis 87, 88.
Surgery and other procedures
Gastroesophageal reflux disease (GERD) can usually be controlled with medication. But if medications don’t help or you wish to avoid long-term medication use, your doctor might recommend:
- Fundoplication. The surgeon wraps the top of your stomach around the lower esophageal sphincter, to tighten the muscle and prevent reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. The wrapping of the top part of the stomach can be complete (Nissen fundoplication) or partial. The most common partial procedure is the Toupet fundoplication. Your surgeon will recommend the type that is best for you.
- LINX device. A ring of tiny magnetic beads is wrapped around the junction of the stomach and esophagus. The magnetic attraction between the beads is strong enough to keep the junction closed to refluxing acid, but weak enough to allow food to pass through. The LINX device can be implanted using minimally invasive surgery. The magnetic beads do not have an effect on airport security or magnetic resonance imaging.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Because obesity can be a risk factor for gastroesophageal reflux disease (GERD), your doctor may suggest weight-loss surgery as an option for treatment. Talk with your doctor to find out if you’re a candidate for weight-loss surgery.
Acid reflux diet
Diet plays a major role in controlling acid reflux symptoms and is the first line of therapy used for people with gastroesophageal reflux disease (GERD).
Foods that help prevent acid reflux
Ginger is one of the best digestive aids because of its medicinal properties. Ginger is alkaline in nature and anti-inflammatory, which eases irritation in the digestive tract. Try sipping ginger tea when you feel heartburn coming on.
High-fiber foods
Fibrous foods make you feel full so you’re less likely to overeat, which may contribute to heartburn. So, load up on healthy fiber from these foods:
- Whole grains such as oatmeal, couscous and brown rice.
- Root vegetables such as sweet potatoes, carrots and beets.
- Green vegetables such as asparagus, broccoli and green beans.
Alkaline foods
Foods that have a low pH are acidic and more likely to cause reflux. Those with higher pH are alkaline and can help offset strong stomach acid. Alkaline foods include:
- Bananas
- Melons
- Cauliflower
- Fennel
- Nuts
Watery foods
Eating foods that contain a lot of water can dilute and weaken stomach acid. Choose foods such as:
- Celery
- Cucumber
- Lettuce
- Watermelon
- Broth-based soups
- Herbal tea.
Gastroesophageal acid reflux (GERD)
Gastroesophageal reflux disease also called GERD, gastro-oesophageal reflux disease (GORD), acid reflux or heartburn, is a condition that develops when there is a backward flow or reflux of stomach contents (acid from the food and liquid in your stomach) back up into your throat and esophagus causing troublesome symptoms and/or complications 56, 57, 58, 59, 60. Gastroesophageal reflux disease can present as non-erosive reflux disease or erosive esophagitis. It can occur at any age, even in babies. Many times, you or your doctor can determine the triggers for your reflux.
The main symptoms of gastroesophageal reflux disease (GERD) are:
- Heartburn – a burning sensation in the middle of your chest, usually after eating, which might be worse after eating, when lying down or when bending over.
- An unpleasant sour taste in your mouth, caused by stomach acid
You may also have:
- Cough or hiccups that keep coming back
- Hoarse voice
- Bad breath
- Bloating and feeling sick
If you have nighttime acid reflux, you might also experience:
- An ongoing cough
- Inflammation of the vocal cords (laryngitis)
- New or worsening asthma
Gastroesophageal reflux disease is caused by a weakened muscle at the end of your esophagus where it connects to your stomach called the lower esophageal sphincter (LES). The lower esophageal sphincter (LES) muscle doesn’t close properly, which allows acid to back up into your throat. Typically, when food is swallowed, the lower esophageal sphincter (a band of muscle around the bottom of the esophagus) relaxes to allow food and liquid to flow down into the stomach. Then the muscle tightens again. If the lower esophageal sphincter isn’t working as it should, stomach acid can flow back up into the esophagus (acid reflux) and cause heartburn. The acid backup may be worse when you’re bent over or lying down.
Sometimes gastroesophageal reflux disease is caused or made worse by:
- certain food and drink – such as coffee, tomatoes, alcohol, chocolate and fatty or spicy foods
- being overweight
- smoking
- pregnancy
- stress and anxiety
- an increase in some types of hormones, such as progesterone and estrogen
- taking certain medicines such as anti-inflammatory painkillers like ibuprofen
- a hiatus hernia – when part of your stomach moves up into your chest
- a stomach ulcer
- a bacterial infection in your stomach
In the United States, 20% of the population experience gastroesophageal reflux disease-related symptoms weekly and 7% daily 89, 90. The prevalence of gastroesophageal reflux disease is slightly higher in men compared to women 91. Several studies have demonstrated that patients with gastroesophageal reflux disease (GERD) have reduced health-related quality of life and work productivity 92.
The danger of untreated gastroesophageal reflux disease (GERD) is that it can cause health problems such as inflammation of the esophagus (esophagitis), which is a risk factor for esophageal cancer. Gastroesophageal reflux disease (GERD) also may lead to breathing problems such as asthma, fluid in the lungs, chest congestion, as well as damaging teeth.
Not everyone who has an episode of acid reflux has gastroesophageal reflux disease (GERD). Your doctor may have you undergo testing to see if you have gastroesophageal reflux disease (GERD). Such tests could include:
- Ambulatory acid (pH) probe test: This test measures the acid in your stomach for 24 hours. Your doctor will insert a small, thin tube into your nose and down into your throat. The tube is connected to a small computer you strap around your waist. Another version of this involves a small probe placed in your throat. The probe transmits a signal for a period of time. After 2 days, the probe falls off and is passed in your stool.
- X-ray of the upper digestive system: The X-ray will look at the inside your upper digestive system (throat, stomach, and upper intestine). For this test, you will you be given a chalky liquid to swallow. This liquid coats your digestive tract to provide better views of the inside.
- Endoscopy or gastroscopy: This is where a thin tube with a camera inside it is passed down your throat and into your stomach. This allows your doctor to look inside your upper digestive tract. He or she may also take a sample of the tissue inside your tract for further testing, for example, tests to check for bacteria that can cause heartburn
- Esophageal motility test (manometry): This test measures the movement and pressure of your esophagus. It involves inserting small, thin tube through your nose and down your throat.
Based on endoscopic and histopathologic appearance, gastroesophageal reflux disease (GERD) is classified into three different types 93:
- Non-erosive reflux disease (NERD). Non-erosive reflux disease (NERD) is a subcategory of gastroesophageal reflux disease (GERD). It is characterized by troublesome reflux symptoms with abnormally increased gastroesophageal reflux observed on 24-hour ambulatory pH-impedance monitoring in the absence of esophageal mucosal injury confirmed on endoscopy.
- Erosive esophagitis. Erosive esophagitis is characterized by erosions or ulcers of the esophageal mucosa 94. Patients may be asymptomatic or can present with worsening symptoms of gastroesophageal reflux disease (GERD). The degree of esophagitis is endoscopically graded using the Los Angeles esophagitis classification system, which employs the A, B, C, D grading system based on variables that include length, location, and circumferential severity of mucosal breaks in the esophagus 95.
- Barrett’s esophagus. Barrett’s esophagus occurs as a result of chronic pathological acid exposure to the distal esophageal mucosa. It leads to a histopathological change of the distal esophageal mucosa, which is normally lined by stratified squamous epithelium to metaplastic columnar epithelium. Barrett’s esophagus is more commonly seen in Caucasian males above 50 years, obesity, and history of smoking and predisposes to the development of esophageal adenocarcinoma 94. Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s esophagus 85.
Non-erosive reflux disease (NERD) is the most prevalent type seen in 60-70% of patients followed by erosive esophagitis and Barrett’s esophagus seen in 30% and 6-12% of patients with gastroesophageal reflux disease (GERD), respectively 93, 92, 96.
If you have acid reflux, your doctor may prescribe a medicine called a proton pump inhibitor (PPI) or H-2 receptor blockers (Histamine-2 Receptor Antagonists) that reduces how much acid your stomach makes. You’ll usually need to take this type of medicine for 4 or 8 weeks, depending on how serious your acid reflux is.
Go back to your doctor if your symptoms return after stopping your medicine. You may need a long-term prescription.
In some cases, surgery may be required to treat acid reflux. This is when medicine doesn’t help, or if you want a long-term solution. Types of surgery may include:
- Nissen fundoplication: This surgery reinforces the lower muscle in the esophagus. A surgeon will wrap the very top of the stomach around the outside of the lower esophagus. This reduces reflux by putting pressure on your esophagus. This is a laparoscopic surgery. This means the surgeon makes three or four small cuts in the abdomen (stomach region). He or she will insert instruments, including a flexible tube with a tiny camera, through the cuts.
- Linx surgery: This surgery strengthens the muscle in the esophagus. The Linx device is a ring of tiny beads made of titanium. The surgery wraps the ring around the area between the stomach and esophagus. The magnetic attraction of the beads keeps the opening between the two closed. This helps keep acid from backing up into your throat. However, it’s weak enough to allow food to pass. The surgery is minimally invasive.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Figure 5. Gastroesophageal reflux disease (GERD)
Figure 6. Gastroesophageal reflux disease diagnostic algorithm
[Source 52 ]Chest pain may be a symptom of a heart attack. Seek immediate medical care if you have severe chest pain or pressure, especially when combined with pain in the arm or jaw or difficulty breathing. These may be signs and symptoms of a heart attack.
Make an appointment with your doctor if:
- Heartburn occurs more than twice a week
- Symptoms persist despite use of nonprescription medications
- Take over-the-counter medications for heartburn more than twice a week
- Experience severe or frequent acid reflux symptoms
- You have difficulty swallowing
- You have persistent nausea or vomiting
- You have weight loss because of poor appetite or difficulty eating
Contact your doctor right away if pain is severe or accompanied by:
- If you are 55 or over
- Unintentional weight loss or loss of appetite
- Difficulty swallowing (dysphagia)
- Repeated vomiting or vomiting with blood
- Black, tarry stools
- Trouble swallowing that gets progressively worse
- Fatigue or weakness, which may indicate anemia
Seek immediate medical attention if you have:
- Shortness of breath, sweating or chest pain radiating to the jaw, neck or arm
- Chest pain on exertion or with stress
These symptoms can be a sign of something more serious.
IMPORTANT: Sometimes a heart attack can masquerade as heartburn. Seek medical attention right away if your heartburn is accompanied by sweating, shortness of breath or a tight, clenching feeling in your upper abdominal area.
Gastroesophageal reflux disease causes
Currently, there is no known cause to explain the development of gastroesophageal reflux disease 60. Over the years, several risk factors have been identified and implicated in the pathogenesis of gastroesophageal reflux disease 97. Gastroesophageal reflux disease is caused by frequent acid reflux or reflux of nonacidic content from the stomach. When you swallow, a circular band of muscle around the bottom of your esophagus called the lower esophageal sphincter relaxes to allow food and liquid to flow into your stomach. Then the sphincter closes again. If the lower esophageal sphincter does not relax as it should or it weakens, stomach acid can flow back into your esophagus. This constant backwash of acid irritates the lining of your esophagus, often causing it to become inflamed.
A meta-analysis by Hampel H et al. 98 concluded that obesity was associated with an increased risk of developing gastroesophageal reflux disease (GERD) symptoms, erosive esophagitis, and esophageal cancer. The study by Malfertheiner et al. 99 evaluated the predictive factors for erosive reflux disease in more than 6000 patients with GERD and noted that the odds ratio for the erosive disease increased with the body mass index (BMI). Several other risk factors have been independently associated with the development of GERD symptoms that include age ≥50 years, low socioeconomic status, tobacco use, consumption of excess alcohol, connective tissue disorders, pregnancy, postprandial supination, and different classes of drugs which include anticholinergic drugs, benzodiazepines, NSAID or aspirin use, nitroglycerin, albuterol, calcium channel blockers, antidepressants, and glucagon 100, 101, 59.
Risk factors for gastroesophageal reflux disease
The following factors can lead to the onset of gastroesophageal reflux disease or aggravate acid reflux:
- Certain diseases, such as Zollinger-Ellison syndrome or scleroderma.
- Increased abdominal pressure due to obesity or pregnancy.
- Increased production of gastrin, a hormone that regulates the release of stomach acid.
- Hiatal hernia, a condition where the upper part of the stomach moves up into the chest through an opening in the diaphragm. This condition lowers the pressure in the esophageal sphincter.
- Certain medications, including asthma medicine, calcium channel blockers, antihistamines, painkillers, sedatives, and antidepressants.
- Certain foods and beverages, such as fried, spicy, or fatty foods, chocolate, peppermint, coffee, or alcoholic beverages.
- Smoking or inhaling second-hand smoke.
- Delayed stomach emptying.
Factors that can aggravate acid reflux include:
- Smoking
- Eating large meals or eating late at night
- Eating certain foods (triggers) such as fatty or fried foods
- Drinking certain beverages, such as alcohol or coffee
- Taking certain medications, such as aspirin, ibuprofen and naproxen.
Gastroesophageal reflux disease prevention
There are ways to prevent gastroesophageal reflux disease and acid reflux. To start, you need to know your body and how it reacts to different food and drinks. Spicy and acidic foods and carbonated drinks can trigger acid reflux. Try to avoid those things when possible. Eat smaller meals throughout the day, and don’t eat too late at night. Don’t lie down too soon after eating. Limit the use of alcohol. If you use tobacco, try to quit. Stress and lack of sleep also can worsen symptoms.
There are many dietary and lifestyle changes you can make to reduce or eliminate acid reflux, including:
- Not drinking alcohol
- Not smoking
- Avoid these foods and drinks that are commonly known to be heartburn triggers
- Fried foods
- Fast foods
- Pizzas
- Potato chips and other processed snacks
- Chili powder and pepper (white, black, cayenne)
- Fatty meats such as bacon and sausage
- Cheese
- Alcohol
- Carbonated beverages
- Caffeine
- Acidic foods
- Peppermints
- Not eating too close to bedtime
- Losing weight
- Not wearing tight clothing
- Eating smaller meals or avoiding overeating
Foods that help prevent acid reflux
Ginger is one of the best digestive aids because of its medicinal properties. Ginger is alkaline in nature and anti-inflammatory, which eases irritation in the digestive tract. Try sipping ginger tea when you feel heartburn coming on.
High-fiber foods
Fibrous foods make you feel full so you’re less likely to overeat, which may contribute to heartburn. So, load up on healthy fiber from these foods:
- Whole grains such as oatmeal, couscous and brown rice.
- Root vegetables such as sweet potatoes, carrots and beets.
- Green vegetables such as asparagus, broccoli and green beans.
Alkaline foods
Foods that have a low pH are acidic and more likely to cause reflux. Those with higher pH are alkaline and can help offset strong stomach acid. Alkaline foods include:
- Bananas
- Melons
- Cauliflower
- Fennel
- Nuts
Watery foods
Eating foods that contain a lot of water can dilute and weaken stomach acid. Choose foods such as:
- Celery
- Cucumber
- Lettuce
- Watermelon
- Broth-based soups
- Herbal tea
Gastroesophageal reflux disease symptoms
The main symptom of gastroesophageal reflux disease (GERD) is heartburn, often described as a burning feeling in the back of your throat, in the middle of your chest, or behind the sternum (breastbone), and regurgitating sour or bitter liquid to the throat or mouth 60, 94. The combination of heartburn and regurgitation is such a common characteristic of gastroesophageal reflux disease (GERD) that formal testing may be unnecessary 102.
Other symptoms of gastroesophageal reflux disease include 103, 104, 63:
- An acid taste in your mouth.
- A dry cough, asthma, and difficulty swallowing (these may occur without the burning sensation)
- Excessive saliva and a sore throat that doesn’t go away
You may also have:
- Non-burning chest pain, which is usually located in the middle of the chest and radiates to the back
- Difficulty swallowing (dysphagia)
- Atypical reflux symptoms relating to the throat, larynx or lungs:
- Sore throat
- Coughing or hiccups that keep coming back
- Increased salivation
- Shortness of breath
- A hoarse voice
- Bad breath
- Bloating and feeling sick
Symptoms are often worse after eating, when lying down or when bending over.
Gastroesophageal reflux disease complications
Gastroesophageal reflux disease can sometimes lead to the following complications:
- Swelling of the vocal cords, also known as reflux laryngitis
- Inflammation of the tissue in the esophagus (esophagitis). Stomach acid can break down tissue in the esophagus, causing inflammation, bleeding, and sometimes an open sore (ulcer). Esophagitis can cause pain and make swallowing difficult.
- Narrowing of the esophagus (esophageal stricture), caused by scar tissues that develop due to repeated ulcerations. Damage to the lower esophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing. American College of Gastroenterology guidelines recommend esophageal dilation and continue proton pump inhibitor (PPI) therapy to prevent the need for repeated dilations 84.
- Barrett’s esophagus, a precancerous changes to the esophagus tissue caused by long-lasting gastroesophageal reflux disease which increases the risk of esophageal cancer. Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s esophagus 85.
- Lung damage which may include pulmonary fibrosis and bronchiectasis
- Ulcers in the esophagus, caused by burning from stomach acid.
Gastroesophageal reflux disease diagnosis
A diagnosis of gastroesophageal reflux disease (GERD) starts with a thorough medical history during which you describe your signs and symptoms and physical examination. If the typical symptoms of acid reflux disease are present, including heartburn and regurgitation, your doctor may begin treatment without performing specific diagnostic tests.
However, tests may be performed if:
- Your symptoms are atypical
- The severity of acid reflux raises concerns about esophageal damage
- Symptoms do not respond to initial treatment
- Your doctor is considering anti-reflux surgery
To confirm a diagnosis of gastroesophageal reflux disease (GERD) or to check for complications, your doctor might recommend:
- Upper endoscopy or gastroscopy. Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat. The endoscope helps your provider see inside your esophagus and stomach. Test results may not show problems when reflux is present, but an endoscopy may detect inflammation of the esophagus (esophagitis) or other complications. An endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications such as Barrett esophagus. In some instances, if a narrowing is seen in the esophagus, it can be stretched or dilated during this procedure. This is done to improve trouble swallowing (dysphagia).
- Transnasal esophagoscopy. This test is done to look for any damage in your esophagus. A thin, flexible tube with a video camera is put through your nose and moved down your throat into the esophagus. The camera sends pictures to a video screen.
- Reflux testing (wireless pH/pH impedance). Ambulatory acid (pH) probe is placed in your esophagus to identify when, and for how long, stomach acid regurgitates there. The monitor connects to a small computer that you wear around your waist or with a strap over your shoulder. The monitor might be a thin, flexible tube (catheter) that’s threaded through your nose into your esophagus. Or it might be a clip that’s placed in your esophagus during an endoscopy. The clip passes into your stool after about two days.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- Your doctor performs an endoscopy and places a small chip in your lower esophagus
- The chip records the acid level in your esophagus for 48 hours.
- The chip transmits your acid level to a wireless recording device that you wear around your belt.
- The data from the recording device can gauge your reflux severity.
- 24-Hour pH Impedance. Your doctor may order this procedure to evaluate your reflux. This procedure monitors your pH level (level of acidity) for a prolonged period. During pH impedance:
- Your doctor places a thin, flexible catheter with an acid-sensitive tip through your nose into your esophagus. The catheter is placed in separate recording spots to evaluate the flow of liquid from your stomach into your esophagus.
- The catheter stays in your nose for a period of 24 hours.
- Your doctor is able to evaluate whether you have GERD, the severity of your reflux, the presence of non-acid reflux and the correlation between your reflux and symptoms. This procedure helps in the design of a course of treatment for you.
- Wireless pH Testing. Wireless pH testing allows your doctor to evaluate your reflux activity over a 48-hour period while you continue your normal activities. To perform wireless pH testing:
- X-ray of the upper digestive system. X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your esophagus and stomach. This is particularly useful for people who are having trouble swallowing. You may also be asked to swallow a barium pill that can help diagnose a narrowing of the esophagus that may interfere with swallowing.
- Esophageal manometry also known as esophageal motility (movement) studies. This test measures the rhythmic muscle contractions in your esophagus when you swallow. Esophageal manometry also measures the coordination and force exerted by the muscles of your esophagus. This is typically done in people who have trouble swallowing. An esophageal manometry is an essential part of the assessment process prior to anti-reflux surgery.
- During an esophageal manometry your doctor places a pressure-sensitive catheter into the esophagus. This may be performed right before esophageal pH impedance studies, as it determines where your doctor should place the catheter. The catheter evaluates the strength and coordination of your muscle contractions. It also tests the strength and relaxation function of the lower esophageal sphincter.
- Barium esophagram also called barium swallow, is an imaging test that checks for problems in your upper gastrointestinal tract. Your upper gastrointestinal tract includes your mouth, back of the throat, esophagus, stomach, and first part of your small intestine. The test uses a special type of x-ray called fluoroscopy. Fluoroscopy is a kind of X-ray “movie.” A barium esophagram also evaluates the coordination of your esophageal motor function. While it does not test for the presence of reflux, it is useful for evaluating injury to your esophagus.
- During barium contrast radiography:
- You swallow a contrast solution called barium.
- The barium coats your esophagus and gastrointestinal tract, making it easier for the doctor to detect abnormalities.
- An X-ray is taken.
- During the X-ray, your doctor looks for a narrowing in the esophagus called a stricture.
- During barium contrast radiography:
Gastroesophageal reflux disease treatments
If your symptoms are mild, treatment may not be necessary. Your doctor is likely to recommend that you first try lifestyle changes and nonprescription medications. If you don’t experience relief within a few weeks, your doctor might recommend prescription medication and additional testing.
Over-the-counter medicine is effective for treating mild cases of acid reflux. These medicines include:
- Antacids: This is a quick-acting medicine that reduces stomach acid. Unfortunately, antacids alone won’t heal the damage stomach acid causes in your esophagus. Sometimes, overusing antacids can cause diarrhea or constipation.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists): These medicines reduce acid production. They don’t work as quickly as antacids. However, they provide longer relief (up to 12 hours). Stronger versions of these medications are available by prescription from your doctor.
- Proton pump inhibitors (PPIs): These medicines block acid production and heal the damage in your throat. They are stronger than H2-receptor blockers.
If these medicines are not providing relief after a few weeks, contact your doctor. Your doctor may give you a prescription version of H2 receptor blockers or proton pump inhibitors. Additionally, your doctor may prescribe medicine to strengthen the lower esophageal sphincter. The medicine may decrease the number of times your muscle relaxes. It is often used for severe reflux. Side effects include fatigue or confusion. Another medicine your doctor may prescribe helps your stomach empty faster. This will cause the food to move along the digestive tract and not back up into your throat. Your doctor may combine more than one medicine, depending upon the severity of your reflux.
In some cases, surgery may be required to treat acid reflux. This is when medicine doesn’t help, or if you want a long-term solution. Types of surgery may include:
- Nissen fundoplication: This surgery reinforces the lower muscle in the esophagus. A surgeon will wrap the very top of the stomach around the outside of the lower esophagus. This reduces reflux by putting pressure on your esophagus. This is a laparoscopic surgery. This means the surgeon makes three or four small cuts in the abdomen (stomach region). He or she will insert instruments, including a flexible tube with a tiny camera, through the cuts.
- Linx surgery: This surgery strengthens the muscle in the esophagus. The Linx device is a ring of tiny beads made of titanium. The surgery wraps the ring around the area between the stomach and esophagus. The magnetic attraction of the beads keeps the opening between the two closed. This helps keep acid from backing up into your throat. However, it’s weak enough to allow food to pass. The surgery is minimally invasive.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Lifestyle and home remedies for acid reflux
You can ease, stop or reduce heartburn and acid reflux yourself by doing the following:
- Eat smaller, more frequent meals.
- Eat food slowly and chew thoroughly. Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Lose weight if you’re overweight. Excess weight put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your esophagus.
- Try to find ways to relax
- Avoid foods or drinks that trigger your heartburn — such as alcohol, fried or fatty foods, chocolate, and peppermint.
- Don’t eat within 3 or 4 hours before bed. Wait at least three hours after eating before lying down or going to bed.
- Avoid tight-fitting clothing that are tight around your waist or abdomen. Clothes that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
- Don’t smoke or use tobacco. Smoking decreases the lower esophageal sphincter’s ability to function properly.
- Don’t drink alcohol
- Don’t stop taking any prescribed medicine without speaking to a doctor first
Elevate the head of your bed. You may find that using wood, bricks or books under the feet at the head end of your bed to raise the head of your bed by around 10 to 20 cm, so your chest and head are above your waist, helps relieve symptoms. This can help stop stomach acid traveling up towards your throat. If you can’t elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows isn’t effective as this can increase pressure on your abdomen and make your symptoms worse. When you go to bed, start by lying on your left side to help make it less likely that you will have reflux.
Alternative medicine
Some complementary and alternative therapies, such as ginger, chamomile and slippery elm, may be recommended to treat gastroesophageal reflux disease. However, none have been proved to treat gastroesophageal reflux disease or reverse damage to the esophagus. Talk to your doctor if you’re considering taking alternative therapies to treat GERD.
Nonprescription medications
If necessary, occasional acid reflux can be treated with nonprescription medication, options include:
- Antacids that neutralize stomach. Antacids containing calcium carbonate such as Mylanta, Rolaids and Tums, may provide quick relief. But antacids alone won’t heal an inflamed esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or sometimes kidney problems.
- H-2 receptor blockers (Histamine-2 Receptor Antagonists) to reduce acid production, such as cimetidine (Tagamet HB), famotidine (Pepcid AC) or nizatidine (Axid AR). H-2 blockers don’t act as quickly as antacids, but they provide longer relief and may decrease acid production from the stomach for up to 12 hours. Stronger versions are available by prescription.
- Proton pump inhibitors (PPIs) block acid production and heal the esophagus. Proton pump inhibitors are stronger acid blockers than H-2 blockers and allow time for damaged esophageal tissue to heal. Nonprescription proton pump inhibitors include lansoprazole (Prevacid 24 HR), omeprazole (Prilosec OTC) and esomeprazole (Nexium 24 HR).
If you suspect that you have gastroesophageal reflux disease (GERD), your symptoms worsen, or you have nausea, vomiting or difficulty swallowing, talk to your doctor. Prescription medications might help. In a few cases, gastroesophageal reflux disease (GERD) might be treated with surgery or other procedures.
Prescription medications
Prescription-strength treatments for gastroesophageal reflux disease (GERD) include:
- Prescription-strength proton pump inhibitors. Prescription-strength proton pump inhibitors include esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix), rabeprazole (Aciphex) and dexlansoprazole (Dexilant). Although generally well tolerated, prescription-strength proton pump inhibitors might cause diarrhea, headaches, nausea, or in rare instances, low vitamin B-12 or magnesium levels.
- Prescription-strength H-2 blockers. Prescription-strength H-2 blockers include prescription-strength famotidine and nizatidine. Side effects from these medications are generally mild and well tolerated.
Multiple studies have demonstrated that proton-pump inhibitors (PPIs) provide superior therapeutic efficacy in the management of GERD than other antireflux medications such as H-2 receptor antagonists 86. Overall, proton-pump inhibitors (PPIs) demonstrate an unsurpassed rates of symptomatic relief and healing of esophageal inflammation as well as significant improvement in health-related quality of life in patients with erosive esophagitis 87, 88.
Surgery and other procedures
Gastroesophageal reflux disease (GERD) can usually be controlled with medication. But if medications don’t help or you wish to avoid long-term medication use, your doctor might recommend:
- Fundoplication. The surgeon wraps the top of your stomach around the lower esophageal sphincter, to tighten the muscle and prevent reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. The wrapping of the top part of the stomach can be complete (Nissen fundoplication) or partial. The most common partial procedure is the Toupet fundoplication. Your surgeon will recommend the type that is best for you.
- LINX device. A ring of tiny magnetic beads is wrapped around the junction of the stomach and esophagus. The magnetic attraction between the beads is strong enough to keep the junction closed to refluxing acid, but weak enough to allow food to pass through. The LINX device can be implanted using minimally invasive surgery. The magnetic beads do not have an effect on airport security or magnetic resonance imaging.
- Transoral incisionless fundoplication (TIF). This new procedure involves tightening the lower esophageal sphincter by creating a partial wrap around the lower esophagus using polypropylene fasteners. Transoral incisionless fundoplication (TIF) is performed through the mouth by using an endoscope and requires no surgical incision. Its advantages include quick recovery time and high tolerance. If you have a large hiatal hernia, transoral incisionless fundoplication (TIF) alone is not an option. However, transoral incisionless fundoplication (TIF) may be possible if it is combined with laparoscopic hiatal hernia repair.
Because obesity can be a risk factor for gastroesophageal reflux disease (GERD), your doctor may suggest weight-loss surgery as an option for treatment. Talk with your doctor to find out if you’re a candidate for weight-loss surgery.
Esophagitis
Esophagitis is present when the lining of the esophagus becomes swollen, inflamed, or irritated 105. Esophagitis is also called erosive esophagitis or ulcerative esophagitis. Esophagitis can cause painful, difficult swallowing. Esophagitis can also lead to chest pain. Various things can cause esophagitis. Some common causes include stomach acids backing up into the esophagus, infection, medicines taken by mouth and allergies. Chronic acid reflux (GERD) is a common cause of esophagitis.
Esophagitis may feel like:
- A sore throat.
- Heartburn.
- Difficulty swallowing.
- Chest pain.
The pain may be mild to severe and may be constant or come and go.
Depending on the cause and the severity of esophagitis, you might also notice:
- Acid reflux.
- Regurgitations.
- Food getting stuck in your throat.
- Indigestion.
- Feeding difficulties in children.
- Nausea and vomiting.
- Blood in your vomit.
- Mouth sores.
Treatment for esophagitis depends on its exact cause and how badly the tissue that lines the esophagus is damaged. Without treatment, esophagitis can damage this lining. The esophagus may start to have trouble moving food and liquid from the mouth to the stomach. Esophagitis also can lead to other serious health issues. These include scarring or narrowing of the esophagus, unhealthy weight loss, and dehydration.
Most symptoms of esophagitis can be caused by a few different conditions that affect your digestive system.
See your doctor if your symptoms:
- Last more than a few days.
- Don’t get better after using medicines called antacids that are available without a prescription.
- Are bad enough to make it hard for you to eat or cause you to lose weight.
- Happen along with flu symptoms such as headache, fever and muscle aches.
Get emergency care if you:
- Have pain in your chest that lasts more than a few minutes.
- Think you have food stuck in your esophagus.
- Have a history of heart disease and feel chest pain.
- Feel pain in your mouth or throat when you eat.
- Have shortness of breath or chest pain that happens soon after eating.
- Vomit large amounts, often have forceful vomiting or have trouble breathing after vomiting.
- Notice that your vomit is yellow or green, looks like coffee grounds, or has blood in it.
Esophagitis causes
Esophagitis is often caused by stomach fluid that flows back into the food pipe. The fluid contains acid, which irritates the tissue. This problem is called gastroesophageal reflux (GER). An autoimmune disorder called eosinophilic esophagitis can also causes esophagitis.
The following increase your risk of esophagitis:
- Alcohol use
- Cigarette smoking
- Surgery or radiation to the chest (for example, treatment for lung cancer)
- Taking certain medicines without drinking plenty of water. These medicines include alendronate, doxycycline, ibandronate, risedronate, tetracycline, potassium tablets, and vitamin C
- Vomiting
People who have a weakened immune system may develop infections. Infections may lead to swelling of the food pipe. Infection may be due to:
- Fungi or yeast (most often Candida)
- Viruses, such as herpes or cytomegalovirus.
Reflux esophagitis
A valve called the lower esophageal sphincter (LES) usually keeps stomach acid out of your esophagus. But sometimes the lower esophageal sphincter (LES) doesn’t close properly. Or it opens when it shouldn’t. In some people, the upper part of the stomach bulges through the large muscle that separates the stomach and the chest. This is known as a hiatal hernia. It also can cause stomach acid to back up into the esophagus.
Gastroesophageal reflux disease (GERD) is a condition in which this backflow of acid is a frequent or ongoing problem. GERD can lead to ongoing swelling and tissue damage in the esophagus.
Eosinophilic esophagitis
Eosinophils are white blood cells that play a key role in allergic reactions. Eosinophilic esophagitis can happen if lots of these white blood cells build up in your esophagus. This most likely happens in response to a substance that causes an allergy, acid reflux or both.
Certain foods may trigger eosinophilic esophagitis, including:
- Milk.
- Eggs.
- Wheat.
- Soy.
- Peanuts.
- Seafood.
Typical allergy testing often is not able to spot these foods as being triggers.
People with eosinophilic esophagitis may have other allergies that aren’t caused by food. For example, sometimes allergens in the air, such as pollen, may be the cause. One common symptom of eosinophilic esophagitis is food getting stuck in the esophagus after swallowing. This is called food impaction. Another common symptom is trouble swallowing, also called dysphagia.
Lymphocytic esophagitis
Lymphocytic esophagitis is a rare condition of the esophagus. With lymphocytic esophagitis, a higher than typical number of white blood cells called lymphocytes build up in the lining of the esophagus. Lymphocytic esophagitis may be related to eosinophilic esophagitis or to gastroesophageal reflux disease (GERD).
Medicine-induced esophagitis
Medicine-induced esophagitis also called drug-induced esophagitis, happens when some medicines taken by mouth cause tissue damage in your esophagus. The damage happens if the medicines stay in contact with the lining of the esophagus for too long. For example, you might swallow a pill with little or no water. If you do that, the pill itself or residue from the pill may stay in the esophagus.
Medicines that have been linked to esophagitis include:
- Pain-relieving medicines such as aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
- Antibiotics such as tetracycline and doxycycline.
- Medicine called potassium chloride that is used to treat low levels of the mineral potassium.
- Medicines called bisphosphonates that treat bone conditions such as osteoporosis. These medicines include alendronate (Binosto, Fosamax).
- A treatment for heart conditions called quinidine.
Infectious esophagitis
An infection in tissues of the esophagus may cause esophagitis. The infection could be due to bacteria, viruses or funguses. Infectious esophagitis is fairly rare. It happens most often in people with weakened immune systems, such as people with HIV/AIDS or cancer.
A fungus usually present in the mouth called Candida albicans is a common cause of infectious esophagitis. This type of fungal infection often is linked with a weakened immune system, diabetes, cancer, or use of steroid or antibiotic medicines.
Risk factors for esophagitis
Risk factors for esophagitis vary depending on the cause of the esophagitis.
Reflux esophagitis
Factors that raise the risk of gastroesophageal reflux disease (GERD) also are factors in reflux esophagitis. These risk factors include the following:
- Eating right before going to bed.
- Eating meals that are too large and fatty.
- Smoking.
- Gaining extra weight, including from pregnancy.
Foods that can make symptoms of GERD or reflux esophagitis worse include:
- Caffeine.
- Alcohol.
- Fatty foods.
- Chocolate.
- Peppermint.
Eosinophilic esophagitis
Risk factors for this allergy-related esophagitis may include:
- A history of certain allergic reactions. These include asthma, atopic dermatitis and allergic rhinitis, also known as hay fever.
- A family history of eosinophilic esophagitis.
Medicine-induced esophagitis
Risk factors for medicine-induced esophagitis are often linked with issues that prevent quick and complete passage of a pill into your stomach. These factors include:
- Swallowing a pill with little or no water.
- Taking medicines while lying down.
- Taking medicines right before sleep. This risk factor likely is due in part to less saliva being made and less swallowing happening during sleep.
- Being older in age. This may be a factor because of age-related changes to the muscles of the esophagus or to glands making less saliva.
- Taking large or oddly shaped pills.
Infectious esophagitis
Risk factors for infectious esophagitis often relate to medicines such as steroids or antibiotics. People with diabetes also have a higher risk of esophagitis caused by a fungal candida infection in particular.
Other causes of infectious esophagitis may relate to poor immune system function. This may be due to an immune system condition, such as HIV/AIDS, or certain cancers. Also, certain cancer treatments may raise the risk of infectious esophagitis. So might medicines called immunosuppressants that block immune system reactions to transplanted organs.
Esophagitis symptoms
The infection or irritation may cause the food pipe to become inflamed. Sores called ulcers may form.
Common symptoms of esophagitis include:
- Cough
- Stomach acid that backs up into the esophagus, also called acid reflux.
- Difficulty swallowing
- Painful swallowing
- Swallowed food becoming stuck in the esophagus, also known as food impaction.
- Heartburn (acid reflux). It’s common to feel heartburn behind the breastbone while eating.
- Hoarseness
- Sore throat.
Babies and some children with esophagitis are too young to explain their discomfort or pain. Their symptoms can include:
- Feeding troubles, such as getting easily upset, arching of the back and not wanting to eat.
- Failure to thrive.
- Chest or belly pain in older children.
Esophagitis complications
If not treated, esophagitis may cause severe discomfort. Scarring (stricture) of the food pipe may develop. This can cause swallowing problems.
A condition called Barrett esophagus can develop after years of gastroesophageal reflux (GERD). Rarely, Barrett esophagus may lead to cancer of the food pipe.
Without treatment, esophagitis can lead to complications that include:
- Scarring or narrowing of the esophagus, known as a stricture.
- Tearing of the lining of the esophagus. This can be due to retching or to healthcare professionals passing medical tools through an inflamed esophagus during endoscopy. Endoscopy is a way for your doctor to check your digestive system.
- A condition called Barrett esophagus in which the cells lining the esophagus are damaged from acid reflux. This raises the risk of cancer that starts in the esophagus, also called esophageal cancer.
Esophagitis diagnosis
Your doctor may perform the following tests:
- Esophagogastroduodenoscopy (EGD) and removing a piece of tissue from the food pipe for examination (biopsy). Endoscopy is a test that’s used to check the digestive system. A healthcare professional guides a long, thin tube equipped with a tiny camera down the throat and into the esophagus. This tool is called an endoscope. Your healthcare professional can use an endoscope to see if the esophagus looks different than usual. Small tissue samples may be taken for testing. This is called a biopsy. The esophagus may look different depending on the cause of the swelling, such as medicine-induced or reflux esophagitis. Before this test, you receive medicine that helps you relax.
- Esophageal capsule. Esophageal capsule test can be done in your doctor’s office. It involves swallowing a capsule attached to a string. The capsule dissolves in the stomach and releases a sponge. Your doctor pulls the sponge out of your mouth with the string. As the sponge is pulled out, it samples the tissues of the esophagus. This may help your doctor figure out how inflamed your esophagus is without doing an endoscopy.
- Upper GI series (barium swallow x-ray). Barium X-ray involves drinking a solution or taking a pill that contains a compound called barium. Barium coats the lining of the esophagus and the stomach so that they show up on images taken. The images can help healthcare professionals find narrowing of the esophagus and other changes in structure. The images also can help spot a hiatal hernia, tumors or other conditions that may be causing symptoms.
- Esophageal manometry
- Biopsy. Small tissue samples removed during an endoscopic exam are sent to the lab for testing. Depending on the suspected cause of the condition, tests may be used to:
- Diagnose an infection caused by a bacterium, a virus or a fungus.
- Find out if allergy-related white blood cells called eosinophils have built up in the esophagus.
- Spot cells that aren’t regular. Such cells may be clues of esophageal cancer or changes that raise the risk of cancer.
Esophagitis treatment
Treatment depends on the cause. Treatments for esophagitis are intended to lessen symptoms, manage complications and treat the causes of the condition.
Common treatment options for esophagitis are:
- Medicines that reduce stomach acid in case of reflux disease
- Antibiotics to treat infections
- Medicines and diet changes to treat eosinophilic esophagitis
- Medicines to coat the lining of the food pipe to treat damage related to pills.
Esophagitis home remedies
Depending on the type of esophagitis you have, you may lessen symptoms or stop recurring problems by following these steps:
- Do not eat foods that may make reflux worse. Consuming large amounts of certain foods or drinks may make symptoms of acid reflux worse. These can include alcohol, drinks with caffeine, chocolate and mint-flavored foods.
- Use proper pill-taking habits. Take a pill with plenty of water and before eating a meal. Don’t lie down for at least 30 minutes after taking a pill.
- Lose extra weight. Talk with your doctor or dietitian about a diet and exercise routine to help you lose weight and stay at a healthy weight.
- If you smoke, quit. You can ask your doctor to help you end a smoking habit.
- Try not to stoop or bend, especially soon after eating.
- Do not lie down after eating. Wait at least three hours after eating to lie down or go to bed.
- Raise the head of your bed. Place wooden blocks under your bed to raise the head. Aim to raise it 6 to 8 inches (15 to 20 centimeters). If it’s not possible to elevate your bed, place a wedge between your mattress and box spring. This raises your body from the waist up. Raising your head by using only pillows doesn’t work.
Reflux esophagitis treatment
Treatment for reflux esophagitis may include:
- Medicines available without a prescription. These include antacids (Maalox, Mylanta, others); medicines called H-2-receptor blockers that lower stomach acid, such as cimetidine (Tagamet HB); and medicines called proton pump inhibitors that block stomach acid and heal the esophagus, such as lansoprazole (Prevacid 24 HR) and omeprazole (Prilosec OTC), among others.
- Prescription medicines. These include prescription-strength H-2-receptor blockers and proton pump inhibitors.
- Surgery. A type of surgery called fundoplication may improve the condition of the esophagus if other treatments don’t work. The surgeon wraps a portion of the stomach around the lower esophageal sphincter that separates the esophagus and stomach. This surgery can strengthen the sphincter and prevent acid from backing up into the esophagus.
Eosinophilic esophagitis treatment
Treatment for eosinophilic esophagitis involves staying away from the allergen that trigger symptoms. Treatment also involves easing the allergic reaction with medicines. Medicines may include:
- Proton pump inhibitors. Your doctor likely will first prescribe a proton pump inhibitor. You might take one such as esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec) or pantoprazole (Protonix).
- Steroids. Some studies show that swallowed steroids may act on the surface tissue of the esophagus to treat eosinophilic esophagitis. One steroid called budesonide (Eohilia) comes in a liquid form. Another steroid called fluticasone is sprayed into the mouth and then swallowed. Your doctor can tell you how to swallow the steroid solution so that it coats your esophagus. Swallowing a steroid solution is much less likely to cause serious side effects compared with taking steroid pills by mouth.
- Elimination and elemental diets. A reaction to a food allergen is likely the cause of eosinophilic esophagitis. So it may help to stop eating the food that seems to cause the allergy. Standard allergy tests can’t tell you for sure if you’re allergic to a certain food. For that reason, your healthcare professional may recommend that you remove common food allergens from your diet. Then you can slowly add foods back into your diet and note when symptoms come back. This is known as an elimination diet. It needs to be done with guidance from your allergy specialist. A more restrictive method is to remove all food from your diet for a time. Your allergy specialist replaces food with an amino acid-based formula. Over time, you slowly get back to eating food. This is called an elemental diet. It also must be done under the watch of a allergy specialist and dietitian.
- Monoclonal antibodies. This type of medicine works to block the action of certain proteins in the body that cause inflammation. A monoclonal antibody called dupilumab (Dupixent) may be a treatment option for people age 12 and older with eosinophilic esophagitis. Dupilumab is given as an injection every week or every two weeks depending on your weight.
Medicine-induced esophagitis treatment
Treatment for medicine-induced esophagitis involves not using the problem medicine when possible. It also involves lowering the risk of this condition with proper pill-taking habits.
Your doctor may recommend:
- Taking a different medicine that is less likely to cause medicine-induced esophagitis.
- Taking a liquid version of a medicine if possible.
- Sitting or standing for at least 30 minutes after taking a pill.
- Drinking an entire glass of water with a pill. But this option isn’t right for everyone. For instance, some people need to drink less fluid because of another condition, such as kidney disease.
Infectious esophagitis treatment
Your doctor may prescribe medicine to treat an infection that causes infectious esophagitis. Medicines can help clear up infections from viruses, bacteria or fungi.
Treating common complications
A doctor called a gastroenterologist who treats digestive conditions may use medical tools to expand the esophagus. This treatment is called esophageal dilation. It tends to be used only if the esophagus becomes very narrow or if food becomes stuck in the esophagus.
During esophageal dilation, your doctor guides small narrow tubes through the esophagus. Versions of these devices may be equipped with:
- A tapered tip that starts with a rounded point that gradually widens.
- A balloon that can be expanded after it’s placed in the esophagus.
Outlook (Prognosis) for Esophagitis
Most of the time, the disorders that cause swelling of the food pipe, respond to treatment.
Esophageal cancer
Esophageal cancer is cancer that occurs in the esophagus. Esophageal cancer usually begins in the cells that line the inside of the esophagus. Esophageal cancer can occur anywhere along the esophagus. More men than women get esophageal cancer.
Esophageal cancer makes up about 1% of all cancers diagnosed in the United States, but it is much more common in some other parts of the world, such as Iran, northern China, India, and southern Africa.
Esophageal cancer is the sixth most common cause of cancer deaths worldwide. Incidence rates vary within different geographic locations. In some regions, higher rates of esophageal cancer cases may be attributed to tobacco and alcohol use or particular nutritional habits and obesity.
The American Cancer Society’s estimates for esophageal cancer in the United States for 2024 are 106, 107:
- New cases: About 22,370 new esophageal cancer cases diagnosed (17,690 in men and 4,680 in women)
- Deaths: About 16,130 deaths from esophageal cancer (12,880 in men and 3,250 in women)
- 5-Year Relative Survival: 21.6%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their esophageal cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Esophageal cancer deaths as a percentage of All Cancer Deaths: 2.6%.
- Rate of New Cases and Deaths per 100,000: The rate of new cases of esophageal cancer was 4.2 per 100,000 men and women per year. The death rate was 3.7 per 100,000 men and women per year. These rates are age-adjusted and based on 2017–2021 cases and 2018–2022 deaths.
- Lifetime Risk of Developing Cancer: Approximately 0.5 percent of men and women will be diagnosed with esophageal cancer at some point during their lifetime, based on 2018–2021 data.
- In 2021, there were an estimated 51,185 people living with esophageal cancer in the United States.
Esophageal cancer is more common in men than women, and it is associated with older age, heavy alcohol use and tobacco use 107. The rate of new cases of esophageal cancer was 4.2 per 100,000 men and women per year based on 2017–2021 cases, age-adjusted 107. The lifetime risk of esophageal cancer in the United States is about 1 in 127 in men and about 1 in 434 in women 106. Esophageal cancer is the eleventh leading cause of cancer death in the United States. The death rate was 3.7 per 100,000 men and women per year based on 2018–2022 deaths, age-adjusted.
Overall, the rates of esophageal cancer in the United States have been fairly stable for many years, but over the past decade they have been decreasing slightly 106. Esophageal cancer is most common in whites, but is now almost equally as common in African Americans. American Indian, Alaska Natives, and Hispanics have lower rates of esophageal cancer, followed by Asians and Pacific Islanders.
Adenocarcinoma is the most common type of cancer of the esophagus among whites, while squamous cell carcinomais more common in African Americans.
Esophageal cancer makes up about 1.1% of all cancers diagnosed in the United States, but it is much more common in other parts of the world, such as Iran, northern China, India, and southern Africa.
Many people with esophageal cancer do not have signs or symptoms when the cancer first starts. Later, when the tumor gets larger, symptoms can include:
- Difficulty swallowing (dysphagia)
- Weight loss for no known reason
- Chest pain, pressure or burning
- Worsening indigestion or heartburn
- Hiccups
- Throwing up with streaks of blood
- Coughing or hoarseness
- Streaks of blood in mucus coughed up from the lungs
Although many people with esophageal cancer will go on to die from this cancer, treatment has improved and survival rates are getting better. During the 1960s and 1970s, only about 5% of patients survived at least 5 years after being diagnosed. Now, about 21.6% of patients survive at least 5 years after diagnosis 107. This number includes patients with all stages of esophageal cancer. Survival rates for people with early stage cancer are higher.
Make an appointment with your doctor if you have any persistent signs and symptoms that worry you.
You should see your doctor if you have:
- difficulty swallowing
- symptoms that are unusual for you
- symptoms that don’t go away
Your symptoms are unlikely to be cancer but it is important to get them checked by a doctor.
If you’ve been diagnosed with Barrett’s esophagus, a precancerous condition caused by chronic acid reflux, your risk of esophageal cancer is higher. Ask your doctor what signs and symptoms to watch for that may signal that your condition is worsening.
If you’ve had trouble with heartburn, regurgitation and acid reflux for more than five years, then you should ask your doctor about your risk of Barrett’s esophagus.
Screening for esophageal cancer may be an option for people with Barrett’s esophagus. If you have Barrett’s esophagus, discuss the pros and cons of screening with your doctor.
Seek immediate help if you:
- Have chest pain, which may be a symptom of a heart attack
- Have difficulty swallowing
- Are vomiting red blood or blood that looks like coffee grounds
- Are passing black, tarry or bloody stools
- Are unintentionally losing weight
Esophageal cancer causes
It’s not exactly clear what causes esophageal cancer. However, there are certain risk factors that make getting esophageal cancer more likely.
Factors that cause irritation in the cells of your esophagus and increase your risk of esophageal cancer include:
- Having gastroesophageal reflux disease (GERD)
- Smoking
- Having precancerous changes in the cells of the esophagus (Barrett’s esophagus)
- Being obese
- Drinking alcohol
- Having bile reflux
- Having difficulty swallowing because of an esophageal sphincter that won’t relax (achalasia)
- Having a steady habit of drinking very hot liquids
- Not eating enough fruits and vegetables
- Undergoing radiation treatment to the chest or upper abdomen
Scientists believe that some risk factors, such as the use of tobacco or alcohol, may cause esophageal cancer by damaging the DNA in cells that line the inside of the esophagus. Long-term irritation of the lining of the esophagus, as happens with reflux, Barrett’s esophagus, achalasia, Plummer-Vinson syndrome, or scarring from swallowing lye, may also lead to DNA damage.
DNA is the chemical in each of our cells that makes up your genes – the instructions for how your cells function. You usually look like your parents because they are the source of your DNA. However, DNA affects more than how you look. Some genes control when cells grow, divide into new cells, and die. Genes that help cells grow, divide, and stay alive are called oncogenes. Genes that slow down cell division or make cells die at the right time are called tumor suppressor genes. Cancers can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes.
The DNA of esophageal cancer cells often shows changes in many different genes. However, it’s not clear if there are specific gene changes that can be found in all (or most) esophageal cancers.
Some people inherit DNA changes (mutations) from their parents that increase their risk for developing certain cancers. These are called inherited mutations. But esophageal cancer does not seem to run in families, and inherited gene mutations are not thought to be a major cause of this disease. For example:
- Tylosis with esophageal cancer (sometimes called Howel-Evans syndrome) is caused by inherited changes in the RHBDF2 gene. People with changes in this gene are more at risk of developing the squamous cell type of esophageal cancer.
- Bloom syndrome is caused by changes in the BLM gene. The BLM gene is important in making a protein that stabilizes DNA as a cell divides. Without this protein, the DNA can become damaged, which can lead to cancer. People with Bloom syndrome are at a higher risk of developing squamous cell esophageal cancer, as well as AML, ALL, and other cancers involving the lymph system. For this syndrome, an abnormal gene is usually inherited from both parents, not just one.
- Fanconi anemia is a rare syndrome that involves abnormal genes that cannot repair damaged DNA. Mutations (changes) in certain FANC genes can lead to a higher risk of many cancers including AML and squamous cell cancer of the esophagus.
- Familial Barrett’s Esophagus is a syndrome that includes families with Barrett’s esophagus and adenocarcinoma of the esophagus and gastroesophageal (GE) junction. The exact genes associated with this are still being studied.
Special genetic tests can find some of the gene mutations linked to these inherited syndromes. If you have a family history of esophageal cancer or other symptoms linked to these syndromes, you may want to ask your doctor about genetic counseling and genetic testing. The American Cancer Society recommends discussing genetic testing with a qualified cancer genetics professional before any genetic testing is done.
Esophageal Cancer Risk Factors
A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed.
Scientists have found several factors that can affect your risk of esophageal cancer. Some are more likely to increase the risk for adenocarcinoma of the esophagus and others for squamous cell carcinoma of the esophagus.
But having a risk factor, or even many, does not mean that you will get esophageal cancer. And some people who get the disease may not have any known risk factors.
Age
The chance of getting esophageal cancer increases with age. Less than 15% of cases are found in people younger than age 55.
Gender
Men are more likely than women to get esophageal cancer.
Gastroesophageal reflux disease (GERD)
The stomach normally makes strong acid and enzymes to help digest food. In some people, acid can escape from the stomach up into the lower part of the esophagus. The medical term for this is gastroesophageal reflux disease (GERD), or just reflux. In many people, reflux causes symptoms such as heartburn or pain that seem to come from the middle of the chest. In some, though, reflux doesn’t cause any symptoms at all.
People with GERD have a slightly higher risk of getting adenocarcinoma of the esophagus. This risk seems to be higher in people who have more frequent symptoms. But GERD is very common, and most of the people who have it do not go on to develop esophageal cancer. GERD can also cause Barrett’s esophagus (discussed below), which is linked to an even higher risk.
If reflux of stomach acid into the lower esophagus goes on for a long time, it can damage the inner lining of the esophagus. This causes the squamous cells that normally line the esophagus to be replaced with gland cells. These gland cells usually look like the cells that line the stomach and the small intestine, and are more resistant to stomach acid. This condition is known as Barrett’s (or Barrett) esophagus.
The longer someone has reflux, the more likely it is that they will develop Barrett’s esophagus. Most people with Barrett’s esophagus have had symptoms of heartburn, but many have no symptoms at all, a condition often called “silent reflux.”
GERD is an extremely common condition with prevalence rates ranging from 8-40% worldwide. Barrett’s esophagus is found in 1.3 to 1.6% of the general population and 5 to 15% of symptomatic GERD patients undergoing endoscopy 108.
Barrett’s esophagus
Barrett’s esophagus is a condition in which tissue that is similar to the lining of your intestine replaces the tissue lining your esophagus. Doctors call this process intestinal metaplasia. People with Barrett’s esophagus are more likely to develop a rare type of esophageal cancer called esophageal adenocarcinoma 109.
Barrett’s esophagus is defined as the presence of a specialized columnar epithelium with intestinal metaplasia with goblet cells 110. According to the American College of Gastroenterology (ACG) guidelines, Barrett’s esophagus is diagnosed by the presence of intestinal metaplasia on biopsy in addition to the presence of columnar epithelium of at least 1 cm in the esophagus, generally described as “salmon-pink” colored mucosa extending more than 1 cm proximal to the gastroesophageal junction 111. However, the British Society of Gastroenterology 112, as well as the GERD Society Study Committee in Japan 113, do not require the presence of goblet cells to diagnose Barrett’s esophagus and base the diagnosis solely on the presence of columnar metaplasia. Due to the controversy over the significance of goblet cells, another alternative classification has been proposed, which allows the pathologist to state that there is columnar metaplasia and then further specify whether goblet cells are present or are not present. To maximize the possibility of finding Barrett’s esophagus, dysplasia, and/or carcinoma, a minimum of 8 biopsies is recommended by the American College of Gastroenterology. The Prague C & M criteria are recommended for endoscopic grading of Barrett’s esophagus, with the most proximal extent of circumferential columnar mucosa from the gastroesophageal (GE) junction being the C value, and the maximal extent of non-circumferential columnar mucosa above the gastroesophageal (GE) junction being the M value 114.
The development of Barrett’s esophagus is thought to be related to the reflux of gastric acid and bile into the esophagus and the presence of mucosal damage associated with reflux esophagitis 115. In fact, studies using esophageal pH monitoring have reported that acid exposure time in the esophagus is associated with the presence and length of Barrett’s esophagus 116. Furthermore, bilirubin exposure time in the esophagus is associated with the presence and length of Barrett’s esophagus 117. It has also been shown that the combination of gastric and bile acids further increases the risk of developing Barrett’s esophagus 118. However, why Barrett’s esophagus develops in some patients with GERD and not in others remains unclear 108.
In order to understand Barrett’s esophagus, it is useful to understand the normal appearance of the esophagus. In the normal esophagus, the tissue lining appears pale pink and smooth 119. These flat square cells, called “squamous” (Latin for square) cells, make up the normal lining of the esophagus.
In contrast, Barrett’s esophagus is a salmon-colored lining in the esophagus, made up of cells that are similar to cells found in the small intestine and are called “specialized intestinal metaplasia.”
The reason Barrett’s esophagus is important is because people who have it have a small increased risk of developing esophageal cancer 119. Barrett’s esophagus and heartburn symptoms are associated with a specific type of esophageal cancer called “esophageal adenocarcinoma.” However, cancer is not common 109.
More than 95% of patients with Barrett’s esophagus do not develop cancer. Between 1 and 5 people out of 100 (1–5%) with Barrett’s esophagus will develop esophageal cancer 120. People with Barrett’s esophagus are at a much higher risk than people without this condition to develop adenocarcinoma of the esophagus. Still, most people with Barrett’s esophagus do not get esophageal cancer.
Factors that increase your risk of Barrett’s esophagus include:
- Family history. Your odds of having Barrett’s esophagus increase if you have a family history of Barrett’s esophagus or esophageal cancer.
- Being male. Men are far more likely to develop Barrett’s esophagus.
- Being white. White people have a greater risk of the disease than do people of other races.
- Age. Barrett’s esophagus can occur at any age but is more common in adults over 50.
- Chronic heartburn and acid reflux. Having gastroesophageal reflux disease (GERD) that doesn’t get better when taking medications known as proton pump inhibitors or having GERD that requires regular medication can increase the risk of Barrett’s esophagus.
- Current or past smoking.
- Being overweight. Body fat around your abdomen further increases your risk.
The development of Barrett’s esophagus is most often attributed to long-standing gastroesophageal reflux disease (GERD), which may include these signs and symptoms:
- Frequent heartburn and regurgitation of stomach contents
- Difficulty swallowing food
- Less commonly, chest pain
Curiously, approximately half of the people diagnosed with Barrett’s esophagus report little if any symptoms of acid reflux. So, you should discuss your digestive health with your doctor regarding the possibility of Barrett’s esophagus.
Typically, before esophageal adenocarcinoma develops, precancerous cells appear in the Barrett’s tissue. Doctors call this pre-cancerous condition dysplasia and classify the dysplasia as low grade or high grade. Dysplasia is graded by how abnormal the cells look under the microscope. Low-grade dysplasia looks more like normal cells, while high-grade dysplasia is more abnormal. High-grade dysplasia is linked to the highest risk of cancer.
Studies indicate the absolute annual risk of esophageal adenocarcinoma in nondysplastic Barrett’s esophagus is 0.1 to 0.5% per year, a highly variable 1 to 43% per year for low-grade dysplasia, and 23-60% per year for high-grade dysplasia. A greater extent of dysplasia has a significantly higher risk of cancer as well as the presence of an endoscopic abnormality 121, 122.
In January 2016, the American College of Gastroenterology (ACG) published its new clinical guideline for the diagnosis and management of Barrett’s esophagus 110. The American College of Gastroenterology now recommends screening for Barrett’s esophagus in men with at least five years of chronic GERD symptoms who also have at least two additional risk factors including greater than 50 years of age, history of smoking, white ethnicity, central obesity, or a confirmed family history of Barrett’s esophagus. The current recommendation for surveillance is four-quadrant biopsies every 2 cm (or 1 cm in known or suspected dysplasia) followed by biopsy of mucosal irregularity (nodules, ulcers, or other visible lesions) performed at 3- to 5-year intervals. Due to the extremely low prevalence of esophageal adenocarcinoma in women, this population has no indications for screening except for the presence of multiple risk factors 123, 124.
Figure 7. Barrett’s esophagus microscopic view showing changes in the lining of the esophagus
Figure 8. Barrett’s esophagus endoscopic view (as seen by your gut specialist)
Tobacco and alcohol
The use of tobacco products, including cigarettes, cigars, pipes, and chewing tobacco, is a major risk factor for esophageal cancer. The more a person uses tobacco and the longer it is used, the higher the cancer risk. Someone who smokes a pack of cigarettes a day or more has at least twice the chance of getting adenocarcinoma of the esophagus than a nonsmoker, and the risk does not go away if tobacco use stops. The link to squamous cell esophageal cancer is even stronger, but this risk does go down for people who quit tobacco. .
Drinking alcohol also increases the risk of esophageal cancer. The more alcohol someone drinks, the higher their chance of getting esophageal cancer. Alcohol affects the risk of the squamous cell type more than the risk of adenocarcinoma.
Combining smoking and drinking alcohol raises the risk of esophageal cancer much more than using either alone.
Obesity
People who are overweight or obese (very overweight) – obesity means being very overweight with a body mass index (BMI) of 30 or higher — have a higher chance of getting adenocarcinoma of the esophagus. Being overweight or obese is linked to more than 1 in 4 esophageal cancers in men and more than 1 in 10 in women. The more overweight you are the higher the risk. This is in part explained by the fact that people who are obese are more likely to have gastroesophageal reflux.
Diet
Certain substances in the diet may increase esophageal cancer risk. For example, there have been suggestions, as yet not well proven, that a diet high in processed meat may increase the chance of developing esophageal cancer. This may help explain the high rate of this cancer in certain parts of the world.
On the other hand, a diet high in fruits and vegetables is linked to a lower risk of esophageal cancer. The exact reasons for this are not clear, but fruits and vegetables have a number of vitamins and minerals that may help prevent cancer.
Frequently drinking very hot liquids (temperatures of 149° F or 65° C – much hotter than a typical cup of coffee) may increase the risk for the squamous cell type of esophageal cancer. This might be the result of long-term damage to the cells lining the esophagus from the hot liquids.
Achalasia
In this condition, the muscle at the lower end of the esophagus (the lower esophageal sphincter) does not relax properly. Food and liquid that are swallowed have trouble passing into the stomach and tend to collect in the lower esophagus, which becomes stretched out (dilated) over time. The cells lining the esophagus in that area can become irritated from being exposed to foods for longer than normal amounts of time.
People with achalasia have a risk of esophageal cancer that is many times normal. On average, the cancers are found about 15 to 20 years after the achalasia began.
Tylosis
This is a rare, inherited disease that causes excess growth of the top layer of skin on the palms of the hands and soles of the feet. People with this condition also develop small growths (papillomas) in the esophagus and have a very high risk of getting squamous cell cancer of the esophagus.
People with tylosis need to be watched closely to try to find esophageal cancer early. Often this requires regular monitoring with an upper endoscopy.
Plummer-Vinson syndrome
People with this rare syndrome (also called Paterson-Kelly syndrome) have webs in the upper part of the esophagus, typically along with anemia (low red blood cell counts) due to low iron levels, tongue irritation (glossitis), brittle fingernails, and sometimes a large thyroid gland or spleen.
A web is a thin membrane extending out from the inner lining of the esophagus that causes an area of narrowing. Most esophageal webs do not cause any problems, but larger ones can cause food to get stuck in the esophagus, which can lead to problems swallowing and chronic irritation in that area from the trapped food.
About 1 in 10 people with this syndrome eventually develop squamous cell cancer of the esophagus or cancer in the lower part of the throat (hypopharynx).
Workplace exposures
Exposure to chemical fumes in certain workplaces may lead to an increased risk of esophageal cancer. For example, exposure to some of the solvents used for dry cleaning might lead to a greater risk of esophageal cancer. Some studies have found that dry cleaning workers may have a higher rate of esophageal cancer, but not all studies have found this link.
Injury to the esophagus
Lye is a chemical found in strong industrial and household cleaners such as drain cleaners. Lye is a corrosive agent that can burn and destroy cells. Accidentally drinking from a lye-based cleaner bottle can cause a severe chemical burn in the esophagus. As the injury heals, the scar tissue can cause an area of the esophagus to become very narrow (called a stricture). People with these strictures have an increased risk of squamous cell esophageal cancer, which often occurs many years (even decades) later.
History of certain other cancers
People who have had certain other cancers, such as lung cancer, mouth cancer, and throat cancer have a high risk of getting squamous cell carcinoma of the esophagus as well. This may be because these cancers can also be caused by smoking.
Human papilloma virus (HPV) infection
HPV is a group of more than 100 related viruses. They are called papilloma viruses because some of them cause a type of growth called a papilloma (or wart). Infection with certain types of HPV is linked to a number of cancers, including throat cancer, anal cancer, and cervical cancer.
Signs of HPV infection have been found in up to one-third of esophagus cancers from patients in parts of Asia and South Africa. But signs of HPV infection have not been found in esophagus cancers from patients in the other areas, including the US.
Radiotherapy
Radiotherapy for other cancers slightly increases your risk of esophageal cancer, including
- breast cancer
- lung cancer
- oropharynx cancer
- larynx cancer
- Hodgkin lymphoma
Your risk of getting esophageal cancer is still small. You would be at a higher risk from your existing cancer if you didn’t have the radiotherapy your doctor recommends.
Esophageal Cancer Prevention
Not all esophageal cancers can be prevented, but the risk of developing this disease can be greatly reduced by avoiding certain risk factors.
Avoiding tobacco and alcohol
In the United States, the most important lifestyle risk factors for cancer of the esophagus are the use of tobacco and alcohol. Each of these factors alone increases the risk of esophageal cancer many times, and the risk is even greater if they are combined. Avoiding tobacco and alcohol is one of the best ways of limiting your risk of esophageal cancer.
If you smoke, talk to your doctor about strategies for quitting. Medications and counseling are available to help you quit. If you don’t use tobacco, don’t start.
Watching your diet and body weight
Eating a healthy diet and staying at a healthy weight are also important. A diet rich in fruits and vegetables may help protect against esophageal cancer. Obesity has been linked with esophageal cancer, particularly the adenocarcinoma type, so staying at a healthy weight may also help limit the risk of this disease.
Getting treated for gastroesophageal reflux or Barrett’s esophagus
Treating people with reflux may help prevent Barrett’s esophagus and esophageal cancer. Often, reflux is treated using drugs called proton pump inhibitors (PPIs), such as omeprazole (Prilosec®), lansoprazole (Prevacid®), or esomeprazole (Nexium®). Surgery might also be an option for treating reflux if the reflux is not controlled with medical therapy alone.
People at a higher risk for esophageal cancer, such as those with Barrett’s esophagus, are often watched closely by their doctors to look for signs that the cells lining the esophagus have become more abnormal. If dysplasia (a pre-cancerous condition) is found, the doctor may recommend treatments to keep it from developing into esophageal cancer.
For those who have Barrett’s esophagus, daily treatment with a proton pump inhibitor might lower the risk of developing cell changes (dysplasia) that can turn into cancer. If you have chronic heartburn (or reflux), tell your doctor. Treatment can often improve symptoms and might prevent future problems.
Some studies have found that the risk of cancer of the esophagus is lower in people with Barrett’s esophagus who take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen. However, taking these drugs every day can lead to problems, such as kidney damage and bleeding in the stomach. For this reason, most doctors don’t advise that people take NSAIDs to try to prevent cancer. If you are thinking of taking an NSAID regularly, discuss the potential benefits and risks with your doctor first.
Some studies have also found a lower risk of esophageal cancer in people with Barrett’s esophagus who take drugs called statins, which are used to treat high cholesterol. Examples include atorvastatin (Lipitor®) and rosuvastatin (Crestor®). While taking one of these drugs might help some patients lower esophageal cancer risk, doctors don’t advise taking them just to prevent cancer because they can have serious side effects.
Esophageal cancer signs and symptoms
Early esophageal cancer typically causes no signs or symptoms. Cancers of the esophagus are usually found because of the symptoms they cause. Diagnosis in people without symptoms is rare and usually accidental (because of tests done for other medical problems). Unfortunately, most esophageal cancers do not cause symptoms until they have reached an advanced stage, when they are harder to treat.
The most common symptoms of esophageal cancer are:
- Difficulty swallowing (dysphagia)
- Weight loss without trying
- Chest pain, pressure or burning
- Worsening indigestion or heartburn
- Coughing or hoarseness
- Chronic cough
- Vomiting
- Bone pain (if cancer has spread to the bone)
- Bleeding into the esophagus. This blood then passes through the digestive tract, which may turn the stool black. Over time, this blood loss can lead to anemia (low red blood cell levels), which can make a person feel tired.
Having one or more symptoms does not mean you have esophageal cancer. In fact, many of these symptoms are more likely to be caused by other conditions. Still, if you have any of these symptoms, especially trouble swallowing, it’s important to have them checked by a doctor so that the cause can be found and treated, if needed.
Patients commonly experience difficulty swallowing as the tumor gets larger and the width of the esophagus becomes narrowed. At first, most have trouble swallowing solid foods such as meats, breads or raw vegetables. As the tumor grows, the esophagus becomes more narrowed causing difficulty in swallowing even liquids. Cancer of the esophagus can also cause symptoms of indigestion, heartburn, vomiting and choking. Patients may also have coughing and hoarseness of the voice. Involuntary weight loss is also common.
Trouble swallowing (dysphagia)
The most common symptom of esophageal cancer is a problem swallowing, with a feeling like the food is stuck in the throat or chest, or even choking on food. The medical term for trouble swallowing is dysphagia. This is often mild when it starts, and then gets worse over time as the opening inside the esophagus gets smaller.
When swallowing becomes harder, people often change their diet and eating habits without realizing it. They take smaller bites and chew their food more carefully and slowly. As the cancer grows larger, the problem can get worse. People then might start eating softer foods that can pass through the esophagus more easily. They might avoid bread and meat, since these foods typically get stuck. The swallowing problem may even get bad enough that some people stop eating solid food completely and switch to a liquid diet. If the cancer keeps growing, at some point even liquids might be hard to swallow.
To help pass food through the esophagus, the body makes more saliva. This causes some people to complain of bringing up lots of thick mucus or saliva.
A harmless narrowing of the esophagus called a stricture can also make it difficult for you to swallow. It is important to get this symptom checked by your doctor.
Food coming back up
You may regurgitate food – this is when food comes back up soon after you swallow it. It usually starts with food like meat and bread. You may start to bring up soft foods such as mashed potato, drinks and saliva if you don’t have treatment.
Chest pain
Sometimes, people have pain or discomfort in the middle part of their chest. Some people get a feeling of pressure or burning in the chest. These symptoms are more often caused by problems other than cancer, such as heartburn, so they are rarely seen as a signal that a person might have cancer.
You can get indigestion when acid from the stomach goes back up (refluxes) into the esophagus or if the stomach is inflamed or irritated.
The valve between the stomach and esophagus normally stops this from happening. The valve is called the cardiac sphincter. A tumor that develops here can stop the valve working, causing indigestion.
Remember that indigestion is common and it’s not usually caused by cancer. It can be very painful, even when there’s nothing seriously wrong.
See your doctor if you’ve had heartburn most days for 3 weeks or more, even if you’re taking medicine and it seems to help. Heartburn is burning chest pain or discomfort that happens after eating.
Swallowing may become painful if the cancer is large enough to limit the passage of food through the esophagus. Pain may be felt a few seconds after swallowing, as food or liquid reaches the tumor and has trouble getting past it.
Weight loss
About half of people with esophageal cancer lose weight (without trying to). This happens because their swallowing problems keep them from eating enough to maintain their weight. Other factors include a decreased appetite and an increase in metabolism from the cancer.
Other symptoms
Other possible symptoms of cancer of the esophagus can include:
- Hoarseness
- Chronic cough
- Vomiting
- Hiccups
- Bone pain
- Bleeding into the esophagus. This blood then passes through the digestive tract, which may turn the stool black. Over time, this blood loss can lead to anemia (low red blood cell levels), which can make a person feel tired.
Having one or more of the symptoms above does not mean you have esophageal cancer. In fact, many of these symptoms are more likely to be caused by other conditions. Still, if you have any of these symptoms, especially trouble swallowing, it’s important to have them checked by a doctor so that the cause can be found and treated, if needed.
Esophageal cancer complications
As esophageal cancer advances, it can cause complications, such as:
- Obstruction of the esophagus. Cancer may make it difficult or impossible for food and liquid to pass through your esophagus.
- Pain. Advanced esophageal cancer can cause pain.
- Bleeding in the esophagus. Esophageal cancer can cause bleeding. Though bleeding is usually gradual, it can be sudden and severe at times.
Esophageal cancer diagnosis
Esophagus cancers are usually found because of signs or symptoms a person is having. If esophagus cancer is suspected, exams and tests will be needed to confirm the diagnosis. If cancer is found, further tests will be done to help determine the extent (stage) of the cancer.
Medical history and physical exam
If you have symptoms that might be caused by esophageal cancer, the doctor will ask about your medical history to check for possible risk factors and to learn more about your symptoms.
Your doctor will also examine you to look for possible signs of esophageal cancer and other health problems. He or she will probably pay special attention to your neck and chest areas.
If the results of the exam are abnormal, your doctor will probably order tests to help find the problem. You may also be referred to a gastroenterologist (a doctor specializing in digestive system diseases) for further tests and treatment.
Imaging tests to look for esophagus cancer
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. Imaging tests might be done for many reasons, such as:
- To help find a suspicious area that might be cancer
- To learn if and how far cancer has spread
- To help determine if the treatment is working
- To look for possible signs of cancer coming back after treatment
Barium swallow
In this test, a thick, chalky liquid called barium is swallowed to coat the walls of the esophagus. When x-rays are then taken, the barium clearly outlines the esophagus. This test can be done by itself, or as a part of a series of x-rays that includes the stomach and part of the intestine, called an upper gastrointestinal (GI) series. A barium swallow test can show any abnormal areas in the normally smooth surface of the inner lining of the esophagus, but it can’t be used to determine how far a cancer may have spread outside of the esophagus.
This is sometimes the first test done to see what is causing a problem with swallowing. Even small, early cancers can often be seen using this test. Early cancers can look like small round bumps or flat, raised areas (called plaques), while advanced cancers look like large irregular areas and can cause narrowing of the inside of the esophagus.
This test can also be used to diagnose one of the more serious complications of esophageal cancer called a tracheo-esophageal fistula. This occurs when the tumor destroys the tissue between the esophagus and the trachea (windpipe) and creates a hole connecting them. Anything that is swallowed can then pass from the esophagus into the windpipe and lungs. This can lead to frequent coughing, gagging, or even pneumonia. This problem can be helped with surgery or an endoscopy procedure.
Computed tomography (CT or CAT) scan
A CT scan uses x-rays to produce detailed cross-sectional images of your body. This test can help tell if esophageal cancer has spread to nearby organs and lymph nodes (bean-sized collections of immune cells to which cancers often spread first) or to distant parts of the body.
Before the test, you may be asked to drink 1 to 2 pints of a liquid called oral contrast. This helps outline the esophagus and intestines. If you are having any trouble swallowing, you need to tell your doctor before the scan.
Magnetic resonance imaging (MRI) scan
Like CT scans, MRI scans provide detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. A contrast material called gadolinium may be injected into a vein before the scan to see details better. MRI can be used to look at abnormal areas in the brain and spinal cord that might be due to cancer spread.
Positron emission tomography (PET) scan
PET scans usually use a form of radioactive sugar (known as fluorodeoxyglucose or FDG) that is injected into the blood. Normal cells use different amounts of the sugar, depending on how fast they are growing. Cancer cells, which grow quickly, are more likely to absorb larger amounts of the radioactive sugar than normal cells. These areas of radioactivity can be seen on a PET scan using a special camera.
The picture from a PET scan is not as detailed as a CT or MRI scan, but it provides helpful information about whether abnormal areas seen on these other tests are likely to be cancer or not.
If you have already been diagnosed with cancer, your doctor may use this test to see if the cancer has spread to lymph nodes or other parts of the body. A PET scan can also be useful if your doctor thinks the cancer may have spread but doesn’t know where.
PET/CT scan: Some machines can do both a PET and CT scan at the same time. This lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed picture of that area on the CT scan.
Endoscopy
An endoscope is a flexible, narrow tube with a tiny video camera and light on the end that is used to look inside the body. Tests that use endoscopes can help diagnose esophageal cancer or determine the extent of its spread.
Upper endoscopy
This is an important test for diagnosing esophageal cancer. During an upper endoscopy, you are sedated (made sleepy) and then the doctor passes an endoscope down yourthroat and into the esophagus and stomach. The camera is connected to a monitor, which lets the doctor see any abnormal areas in the wall of the esophagus clearly.
The doctor can use special instruments through the scope to remove (biopsy) samples from any abnormal areas. These samples are sent to the lab to see if they contain cancer.
If the esophageal cancer is blocking the opening (called the lumen) of the esophagus, certain instruments can be used to help enlarge the opening to help food and liquid pass.
Upper endoscopy can give the doctor important information about the size and spread of the tumor, which can be used to help determine if the tumor can be removed with surgery.
Endoscopic ultrasound
This test is usually done at the same time as the upper endoscopy. For an endoscopic ultrasound, a probe that gives off sound waves is at the end of an endoscope. This allows the probe to get very close to tumors in the esophagus. This test is very useful in determining the size of an esophageal cancer and how far it has grown into nearby areas. It can also help show if nearby lymph nodes might be affected by the cancer. If enlarged lymph nodes are seen on the ultrasound, the doctor can pass a thin, hollow needle through the endoscope to get biopsy samples of them. This helps the doctor decide if the tumor can be removed with surgery.
Bronchoscopy
This exam may be done for cancer in the upper part of the esophagus to see if it has spread to the windpipe (trachea) or the tubes leading from the windpipe into the lungs (bronchi).
Thoracoscopy and laparoscopy
These exams let the doctor see lymph nodes and other organs near the esophagus inside the chest (by thoracoscopy) or the abdomen (by laparoscopy) through a hollow lighted tube.
These procedures are done in an operating room while you are under general anesthesia (in a deep sleep). A small incision (cut) is made in the side of the chest wall (for thoracoscopy) or the abdomen (for laparoscopy). Sometimes more than one cut is made. The doctor then inserts a thin, lighted tube with a small video camera on the end through the incision to view the space around the esophagus. The surgeon can pass thin tools into the space to remove lymph nodes and biopsy samples to see if the cancer has spread. This information is often important in deciding whether a person is likely to benefit from surgery.
Lab tests of biopsy samples
Usually if a suspected esophageal cancer is found on endoscopy or an imaging test, it is biopsied. In a biopsy, the doctor removes a small piece of tissue with a special instrument passed through the scope.
HER2 testing
If esophageal cancer is found but is too advanced for surgery, your biopsy samples may be tested for the HER2 gene or protein. Some people with esophageal cancer have too much of the HER2 protein on the surface of their cancer cells, which helps the cells grow. A drug that targets the HER2 protein called trastuzumab (Herceptin®) may help treat these cancers when used along with chemotherapy. Only cancers that have too much of the HER2 gene or protein are likely to be affected by this drug, which is why doctors may test tumor samples for it.
PD-L1 testing
An esophageal cancer that cannot be treated with surgery or has spread to distant sites may be tested to see if it makes a checkpoint protein called PD-L1. This protein is found in 35% to 45% of esophageal cancers. Tumors that make this protein might be treated with the immunotherapy drug pembrolizumab.
MMR and MSI testing
Esophageal cancer cells might be tested to see if they show high levels of gene changes called microsatellite instability (MSI), or if they have changes in any of the mismatch repair (MMR) genes (MLH1, MSH2, MSH6, and PMS2).
Esophageal cancers that test positive for mismatch repair (MMR) or high microsatellite instability (MSI) and cannot be treated with surgery, have come back after initial treatment, or have spread to other parts of the body might benefit from immunotherapy with the drug pembrolizumab.
Blood tests
Your doctor might order certain blood tests to help determine if you have esophageal cancer.
Complete blood count (CBC): This test measures the different types of cells in your blood. It can show if you have anemia (too few red blood cells). Some people with esophageal cancer become anemic because the tumor has been bleeding.
Liver enzymes: You may also have a blood test to check your liver function, because esophageal cancer can spread to the liver.
Blood tests
Your doctor might order certain blood tests to help determine if you have esophageal cancer.
Complete blood count (CBC): This test measures the different types of cells in your blood. It can show if you have anemia (too few red blood cells). Some people with esophageal cancer become anemic because the tumor has been bleeding.
Liver enzymes: You may also have a blood test to check your liver function, because esophageal cancer can spread to the liver.
Esophageal cancer treatment
What treatments you receive for esophageal cancer are based on the type of cells involved in your cancer, your cancer’s stage, your overall health and your preferences for treatment.
If you’ve been diagnosed with esophageal cancer, your cancer care team will discuss your treatment options with you. It’s important that you think carefully about each of your choices. You will want to weigh the benefits of each treatment option against the possible risks and side effects.
Which treatments are used for esophageal cancer?
There are several ways to treat esophageal cancer, depending on its type and stage.
Local treatments: Some treatments are called local therapies, meaning they treat the tumor in a specific location, without affecting the rest of the body. Types of local therapy used for esophageal cancer include:
- Surgery
- Radiation therapy
- Endoscopic treatments
These treatments are more likely to be useful for earlier stage (less advanced) cancers, although they might also be used in some other situations.
Systemic treatments: Esophageal cancer can also be treated using drugs, which can be given by mouth or directly into the bloodstream. These are called systemic therapies because they travel through your whole system, allowing them to reach cancer cells almost anywhere in the body. Depending on the type of esophageal cancer, several different types of drugs might be used, including:
- Chemotherapy
- Combined chemotherapy and radiation is called chemoradiotherapy or chemoradiation. You might have chemoradiotherapy before surgery. Or you might have it on its own as your main treatment.
- Targeted drug therapy
- Immunotherapy
Depending on the stage of the cancer and other factors, different types of treatment may be combined at the same time or used after one another.
Esophageal cancer surgery
For some earlier stage cancers, surgery can be used to try to remove the cancer and some of the normal surrounding tissue. In some cases, it might be combined with other treatments, such as chemotherapy and/or radiation therapy.
Surgery used to treat esophageal cancer include:
- an esophagectomy – your surgeon removes the part of the esophagus containing the cancer
- a total esophagectomy – your surgeon removes your whole esophagus
- an esophago-gastrectomy – your surgeon removes the top of your stomach and the part of the esophagus containing cancer
Your surgeon also removes some of the nearby lymph nodes. This is called a lymphadenectomy or lymph node dissection. It helps to reduce the risk of cancer coming back.
Surgery for palliative care
Sometimes minor types of surgery are used to help prevent or relieve problems caused by the cancer, instead of trying to cure it. For example, minor surgery can be used to place a feeding tube directly into the stomach or small intestine in people who need help getting enough nutrition.
Endoscopic Treatments for Esophageal Cancer
Several types of treatment for esophageal cancer can be done by passing an endoscope (a long, flexible tube) down the throat and into the esophagus. Some of these treatments may be used to try to cure very early stage cancers, or even to prevent them from developing by treating Barrett’s esophagus or dysplasia. Other treatments are used mainly to help relieve symptoms from more advanced esophageal cancers that can’t be removed.
Endoscopic mucosal resection
Endoscopic mucosal resection (EMR) can be used for dysplasia (pre-cancer) and some small, very early-stage cancers of the esophagus.
In this technique, a piece of the inner lining of the esophagus is removed with instruments passed down the endoscope. After the abnormal tissue is removed, patients take drugs called proton pump inhibitors to suppress acid production in the stomach. This can help keep the disease from returning.
The most common side effect of endoscopic mucosal resection is bleeding in the esophagus, which is usually not serious. Less common but more serious side effects can include esophageal strictures (areas of narrowing) that might need to be treated by with dilation, and puncture (perforation) of the wall of the esophagus.
Photodynamic therapy
Photodynamic therapy (PDT) can be used to treat Barrett’s esophagus, esophageal pre-cancers (dysplasia), and some very early stage esophageal cancers. It is also often used to treat large cancers that are blocking the esophagus. In this situation, photodynamic therapy is not meant to destroy all the cancer, but to kill enough of the cancer to improve a person’s ability to swallow.
For this technique, a light-activated drug called porfimer sodium (Photofrin®) is injected into a vein. Over the next couple of days, the drug is more likely to collect in cancer cells than in normal cells. A special type of laser light is then focused on the cancer through an endoscope. This light changes the drug into a new chemical that can kill the cancer cells. The dead cells may then be removed a few days later during an upper endoscopy. This process can be repeated if needed.
The advantage of photodynamic therapy is that it can kill cancer cells with very little harm to normal cells. But because the chemical must be activated by light, it can only kill cancer cells near the inner surface of the esophagus – those that can be reached by the light. This light cannot reach cancers that have spread deeper into the esophagus or to other organs.
Photodynamic therapy can cause swelling in the esophagus for a few days, which may lead to some problems swallowing. Strictures (areas of extreme narrowing) can also happen. These often need to be treated by with dilation. Other possible side effects include bleeding or holes in the esophagus.
Some of this drug also collects in normal cells in the body, such as skin and eye cells. This can make you very sensitive to sunlight or strong indoor lights. Too much exposure can cause serious skin reactions, which is why doctors recommend staying out of any strong light for 4 to 6 weeks after the injection.
This treatment can cure some very early esophageal cancers that have not spread to deeper tissues. But this procedure destroys the tissue, so it can be hard to be certain that the cancer hasn’t spread into deeper layers of the esophagus. Since the light used in photodynamic therapy can only reach those cancer cells near the surface of the esophagus, cells of deeper cancers could be left behind, and grow into a new tumor. People getting this treatment need to have follow-up endoscopies to make sure the cancer hasn’t grown back. They also need to stay on a drug called a proton pump inhibitor to stop stomach acid production.
Radiofrequency ablation (RFA)
Radiofrequency ablation (RFA) can be used to treat dysplasia in areas of Barrett’s esophagus. It may lower the chance of cancer developing in that area.
A balloon containing many small electrodes is passed into an area of Barrett’s esophagus through an endoscope. The balloon is then inflated so that the electrodes are in contact with the inner lining of the esophagus. Then an electrical current is passed through it, which kills the cells in the lining by heating them.
Over time, normal cells will grow in to replace the Barrett’s cells. People getting this treatment need to stay on drugs to block stomach acid production after the procedure. Endoscopy (with biopsies) is then done periodically to watch for any further changes in the lining of the esophagus. Rarely, radiofrequency ablation (RFA) can cause strictures (narrowing) or bleeding in the esophagus.
Treatments to help keep the esophagus open
Laser ablation
This technique can be used to help open the esophagus when it is blocked by an advanced cancer. This can help improve problems swallowing.
A laser beam is aimed at the cancer through the tip of an endoscope to destroy the cancerous tissue. The laser is called a neodymium: yttrium-aluminum-garnet (Nd:YAG) laser. Laser endoscopy can be helpful, but the cancer often grows back, so the procedure may need to be repeated every month or two.
Argon plasma coagulation
This technique is like laser ablation, but it uses argon gas and a high-voltage spark delivered through the tip of an endoscope. The spark causes the gas to reach very high temperatures, which can then be aimed at the tumor. This approach is used to help unblock the esophagus for people who have trouble swallowing.
Electrocoagulation (electrofulguration)
For this treatment, a probe is passed down into the esophagus through an endoscope to burn the tumor off with electric current. In some cases, this treatment can help relieve esophageal blockage.
Esophageal stent
A stent is a device that, once in place, self-expands (opens up) to become a tube that helps hold the esophagus open. Stents are made of mesh material. Most often stents are made of metal, but they can also be made of plastic. Using endoscopy, a stent can be placed into the esophagus across the length of the tumor.
How well the stent works depends on the type that is used and where it is placed. Stents will relieve trouble swallowing for most people. They are often used after other endoscopic treatments to help keep the esophagus open.
Chemotherapy
Chemotherapy is drug treatment that uses chemicals to kill cancer cells. Chemotherapy drugs are typically used before (neoadjuvant chemotherapy) or after (adjuvant chemotherapy ) surgery in people with esophageal cancer. Chemotherapy can also be combined with radiation therapy. In people with advanced cancer that has spread beyond the esophagus, chemotherapy may be used alone to help relieve signs and symptoms caused by the cancer.
The chemotherapy side effects that you experience depend on which chemotherapy drugs you receive.
Some common drugs and drug combinations used to treat esophageal cancer include those below which can be given along with radiation or without:
- Carboplatin and paclitaxel (Taxol)
- Oxaliplatin and either 5-FU or capecitabine
- Cisplatin and either 5-fluorouracil (5-FU) or capecitabine
- Cisplatin and Irinotecan (Camptosar)
- Paclitaxel (Taxol) and either 5-FU or capecitabine
Other common drugs and drug combinations that can be used to treat esophageal cancer but are usually not given with radiation include:
- ECF: epirubicin (Ellence), cisplatin, and 5-FU (especially for gastroesophageal junction tumors)
- DCF: docetaxel (Taxotere), cisplatin, and 5-FU
- Trifluridine and tipiracil (Lonsurf), a combination drug in pill form
For some esophageal cancers, chemo may be used along with the targeted drug trastuzumab (Herceptin) or ramucirumab (Cyramza).
Chemo drugs for esophageal cancer are typically given into a vein (IV), either as an injection over a few minutes or as an infusion over a longer period of time. Some drugs you take by mouth. All of these drugs enter your bloodstream and reach most areas of your body. These drugs can be given in a doctor’s office, infusion center, or in a hospital.
Often, a slightly larger and sturdier IV called a central venus catheter (CVC) is needed to administer chemo. It might also be called a central venous access device (CVAD), or central line. Once put in place, a CVC can stay in as long as you’re getting treatment so you won’t need to be stuck with a needle in the arms or hands each time to put in an IV catheter. It can be used to put medicines, blood products, nutrients, or fluids right into your blood. It can also be used to take out blood for testing. There are many different kinds of CVCs. The most common types are the port and the PICC line.
Chemo is given in cycles, followed by a rest period to give you time to recover from the effects of the drugs. Cycles are most often 2 or 3 weeks long. The schedule varies depending on the drugs used. For example, with some drugs, the chemo is given only on the first day of the cycle. With others, it is given for a few days in a row, or once a week. Then, at the end of the cycle, the chemo schedule repeats to start the next cycle.
Adjuvant or neoadjuvant chemo is often given for a total of 3 to 6 months, depending on the drugs used. The length of treatment for advanced esophageal cancer depends on how well it is working and what side effects you might have.
Chemotherapy side effects
Chemo drugs can cause side effects. These depend on the type and dose of drugs given, and the length of treatment. Some of the most common side effects of chemo include:
- Nausea and vomiting
- Loss of appetite
- Hair loss
- Mouth sores
- Diarrhea or constipation
Chemo can also affect the blood-forming cells of the bone marrow, which can lead to:
- Increased chance of infection (from having too few white blood cells)
- Easy bleeding or bruising (from having too few blood platelets)
- Fatigue (from having too few red blood cells and other reasons)
Other side effects are also possible. Some of these are more common with certain chemo drugs. For example:
- Hand-foot syndrome. During treatment with capecitabine or 5-FU (when given as an infusion), this can start out as redness in the hands and feet, and then progress to pain and sensitivity in the palms and soles. If it worsens, blistering or skin peeling can occur, sometimes leading to painful sores. It’s important to tell your doctor right away about any early symptoms, such as redness or sensitivity, so that steps can be taken to keep things from getting worse.
- Neuropathy (nerve damage). This is a common side effect of oxaliplatin, cisplatin, docetaxel, and paclitaxel. Symptoms include numbness, tingling, and even pain in the hands and feet. Oxaliplatin can also cause intense sensitivity to cold in the throat and esophagus (the tube connecting the throat to the stomach) and the palms of the hands. This can cause problems swallowing liquids or holding a cold glass. If you will be getting oxaliplatin, talk with your doctor about side effects, and let them know right away if you develop numbness and tingling or other side effects.
- Allergic or sensitivity reactions. Some people can have reactions while getting the drug oxaliplatin. Symptoms can include skin rash, chest tightness and trouble breathing, back pain, or feeling dizzy, lightheaded, or weak. Be sure to tell your nurse right away if you notice any of these symptoms while you are getting chemo.
- Diarrhea. This is a common side effect with many of these drugs, but can be particularly bad with irinotecan. It needs to be treated right away — at the first loose stool — to prevent severe dehydration. This often means taking drugs like loperamide (Imodium). If you are on a chemo drug that is likely to cause diarrhea, your doctor will give you instructions on what drugs to take and how often to take them to control this symptom.
- Weight loss. People with esophageal cancer often have already lost weight before the cancer was found. Treatments such as chemo, radiation, or both can make it hard to eat well enough to get good nutrition, making weight loss worse. Depending on your situation, the cancer care team might recommend placement of a feeding tube to keep up your nutrition and weight during treatment. This feeding tube may be used short-term (during treatment and a bit afterwards) or it may be permanent depending on your cancer.
Most of these side effects tend to go away after treatment is finished. Some, such as hand and foot numbness, may last for a long time. There are often ways to lessen these side effects. For example, you can be given drugs to help prevent or reduce nausea and vomiting.
Be sure to discuss any questions about side effects with your cancer care team. Report any side effects or changes you notice while getting chemo right away so that they can be treated promptly. In some cases, the doses of the chemo drugs may need to be reduced or treatment may need to be delayed or stopped to prevent the effects from getting worse.
Radiation therapy
Radiation therapy uses high-powered X-ray beams to kill cancer cells. Radiation typically will come from a machine outside your body that aims the beams at your cancer (external-beam radiation therapy [EBRT]). Or, less commonly, radiation can be placed inside your body near the cancer (brachytherapy).
Radiation therapy may be used:
- As part of the main treatment of esophageal cancer in some patients, typically along with chemo (chemoradiation). This is often used for people who can’t have surgery due to poor health or for people who don’t want surgery.
- Before surgery (and along with chemo when possible), to try to shrink the cancer and make it easier to remove. This is called neoadjuvant therapy.
- After surgery (and along with chemo when possible), to try to kill any cancer cells that may have been left behind but are too small to see. This is known as adjuvant therapy.
- To ease the symptoms of advanced esophageal cancer such as pain, bleeding, or trouble swallowing. This is called palliative therapy.
Radiation therapy is most often combined with chemotherapy in people with esophageal cancer. It’s typically used before surgery (neoadjuvant therapy) or occasionally after surgery (adjuvant therapy). Radiation therapy is also used to relieve complications of advanced esophageal cancer, such as when a tumor grows large enough to stop food from passing to your stomach. Treatment can last from two to six weeks of daily radiation treatments.
If you are going to get radiation therapy, it’s important to ask your doctor beforehand about the possible side effects so you know what to expect.
Possible Side effects of external radiation therapy can include:
- Skin changes in areas getting radiation, such as redness, blistering and peeling
- Nausea and vomiting
- Diarrhea
- Fatigue
- Painful sores in the mouth and throat
- Dry mouth or thick saliva (spit)
- Pain with swallowing
These side effects are often worse if chemotherapy is given at the same time as radiation.
Most side effects of radiation are temporary, but some less common side effects can be permanent. For example, in some cases radiation can cause a stricture (narrowing) in the esophagus, which might require more treatment. Radiation to the chest can cause lung damage, which may lead to problems breathing and shortness of breath.
If you notice any side effects, talk to your doctor right away so steps can be taken to lessen them.
Combined chemotherapy and radiation
Combining chemotherapy and radiation therapy may enhance the effectiveness of each treatment. Combined chemotherapy and radiation may be the only treatment you receive, or combined therapy can be used before surgery. But combining chemotherapy and radiation treatments increases the likelihood and severity of side effects.
- Chemoradiotherapy as your main treatment. You might have chemoradiotherapy instead of surgery if you have a squamous cell esophageal cancer that hasn’t spread. The doctors keep a close eye on you after the treatment. This is called active surveillance.
- Chemoradiotherapy before surgery also called neoadjuvant chemoradiotherapy. You might have chemoradiotherapy before surgery if you have adenocarcinoma or squamous cell esophageal cancer which hasn’t spread to other parts of your body. It shrinks the cancer and makes it easier to remove.
- Chemoradiotherapy instead of surgery. You might have other health conditions that mean you’re not well enough to have surgery. Or you might not be able to have surgery because the cancer has grown into nearby tissues. The doctor might offer you chemoradiotherapy instead.
Targeted drug therapy
Cancer cells are different to normal cells. These differences help them to grow and survive. There are medicines that can target those changes. These drugs are called targeted cancer drugs.
Targeted drugs work differently from standard chemotherapy drugs. They sometimes work when standard chemo drugs don’t, and they often have different side effects. They can be used either along with chemo or by themselves.
Drugs that target HER2
Some esophagus cancers have too much of the HER2 protein on the surface of their cells, which can help cancer cells grow. Having too much of this protein is caused by having too many copies of the HER2 gene. Cancers with increased levels of HER2 are called HER2-positive. Drugs that target the HER2 protein can often be helpful in treating HER2-positive cancers.
Trastuzumab (Herceptin, others)
Trastuzumab is a monoclonal antibody, a man-made version of an immune system protein, which targets HER2. It can be used to help treat some HER2-positive cancers of the gastroesophageal (GE) junction (the place where the esophagus and stomach meet).
If you have a gastroesophageal (GE) junction cancer and can’t have surgery, your doctor may have your tumor tested for the HER2 protein or gene. People whose cancers have normal amounts of HER2 are very unlikely to be helped by this drug.
Trastuzumab is given into a vein (IV), typically once every 3 weeks, along with chemo.
Herceptin was the original brand name for trastuzumab, but several similar versions (called biosimilars) are now available as well, including Ogivri, Herzuma, Ontruzant, Trazimera, and Kanjinti.
Possible side effects of trastuzumab
Most of the side effects of trastuzumab are relatively mild and can include fever and chills, cough, and headache. These occur less often after the first dose.
Trastuzumab can also sometimes cause heart damage, leading to the heart muscle becoming weak. Trastuzumab is not given with certain chemo drugs called anthracyclines, such as epirubicin (Ellence) or doxorubicin (Adriamycin), because it can further increase the risk of heart damage if they are given together. Before starting treatment with trastuzumab, your doctor may test your heart function with an echocardiogram or a MUGA scan.
Fam-trastuzumab deruxtecan (Enhertu)
This is an antibody-drug conjugate, which is a monoclonal antibody linked to a chemotherapy drug. In this case, the anti-HER2 antibody acts like a homing signal by attaching to the HER2 protein on cancer cells, bringing the chemo directly to them.
This antibody-drug conjugate can be used by itself to treat advanced HER2-positive GE junction cancers, typically after treatment with trastuzumab has been tried.
Fam-trastuzumab deruxtecan (Enhertu) is infused into a vein (IV). It is typically given once every 3 weeks.
Side effects of fam-trastuzumab deruxtecan
- Fam-trastuzumab deruxtecan (Enhertu) can cause low blood cell counts, which can increase a person’s risk of infections and bleeding. Other common side effects can include nausea, vomiting, diarrhea or constipation, loss of appetite, fever, feeling tired, and hair loss.
- Fam-trastuzumab deruxtecan (Enhertu) can cause serious lung disease in some people, which might even be life threatening. It’s very important to let your doctor or nurse know right away if you’re having symptoms such as coughing, wheezing, trouble breathing, or fever.
- Fam-trastuzumab deruxtecan (Enhertu) can also rarely cause heart damage. Before starting treatment with this drug, your doctor may test your heart function with an echocardiogram or a MUGA scan.
Ramucirumab
For cancers to grow and spread, they need to make new blood vessels so that the tumors get blood and nutrients. One of the proteins that tells the body to make new blood vessels is called vascular endothelial growth factor (VEGF). To start this process, VEGF attaches to other proteins on the outside of the cancer cell called receptors.
Ramucirumab (Cyramza) is a monoclonal antibody that blocks the process of making new blood vessels. Ramucirumab joins to the VEGF receptor, which blocks VEGF and stops the signal to the body to make more blood vessels. This can help slow or stop the growth of the cancer.
Ramucirumab is used to treat cancers that start at the gastroesophageal (GE) junction when they are advanced. It is most often used after another drug stops working. It can be used alone or in combination with the chemo drug paclitaxel.
Ramucirumab is given as infusion into a vein (IV) every 2 weeks.
Possible side effects of ramucirumab
The most common side effects of this drug are high blood pressure, swelling of the arms or legs, protein in the urine, and fatigue. Rare but possibly serious side effects include blood clots, severe bleeding, holes forming in the stomach or intestines (called perforations), and problems with wound healing. If a hole forms in the stomach or intestine it can lead to severe infection and may require surgery to correct.
Entrectinib and larotrectinib
In some cancers, the cells have genes that join together. The fusion of one of these genes, called NTRK, with another gene can lead to abnormal cell growth.
Drugs that target cells with this abnormal gene fusion, called TRK inhibitors, include entrectinib (Rozlytrek) and larotrectinib (Vitrakvi). One of these drugs might be used to treat esophageal cancer with an NTRK gene fusion if the cancer cannot be removed with surgery or has spread to other parts of the body, and if it has grown despite other treatments.
Entrectinib and larotrectinib are given as pills daily.
Possible side effects of entrectinib and larotrectinib
The most common side effects are fatigue, nausea, vomiting, dizziness, cough, diarrhea, and constipation. Other more serious, but less common, side effects include liver problems and confusion.
Immunotherapy
Immunotherapy is the use of medicines that help a person’s own immune system find and destroy cancer cells more effectively. It can be used to treat some people with esophagus cancer.
An important part of the immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses “checkpoint” proteins on immune cells, which act like switches that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system.
Drugs called immune checkpoint inhibitors target these checkpoint proteins, which can help restore the immune response against esophagus cancer cells.
Possible side effects of immune checkpoint inhibitors
Common side effects of these drugs can include fatigue, cough, nausea, skin rash, poor appetite, constipation, muscle or joint pain, itching, fever, and diarrhea.
Other, more serious side effects happen less often. These can include:
- Infusion reactions: Some people might have an infusion reaction while getting one of these drugs. This is like an allergic reaction, and can include fever, chills, flushing of the face, rash, itchy skin, feeling dizzy, wheezing, and trouble breathing. It’s important to tell your doctor or nurse right away if you have any of these symptoms while getting one of these drugs.
- Autoimmune reactions: These drugs work by basically removing one of the safeguards on the body’s immune system. Sometimes the immune system starts attacking other parts of the body, which can cause serious or even life-threatening problems in the lungs, intestines, liver, hormone-making glands, kidneys, skin, or other organs.
It’s very important to report any new side effects to your health care team promptly. If serious side effects do occur, treatment may need to be stopped and you may get high doses of corticosteroids to suppress your immune system.
PD-1 inhibitors
Pembrolizumab (Keytruda) and nivolumab (Opdivo) are drugs that target PD-1, a protein on T cells (a type of immune system cell). The PD-1 protein normally helps keep T cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth.
Pembrolizumab can be used to treat some advanced cancers of the esophagus or gastroesophageal junction (GEJ), typically when treatments such as surgery and chemoradiation (chemotherapy plus radiation therapy) can’t be done. Pembrolizumab might be given by itself or along with chemotherapy, depending on the situation.
In certain cases when no other treatment options are available, this drug can be used for people whose cancer has tested positive for specific gene changes, such as a high level of microsatellite instability (MSI-H), or changes in one of the mismatch repair (MMR) genes.
Pembrolizumab can also be used with chemotherapy, and the targeted drug, trastuzumab, as the first treatment in people with advanced GEJ cancers that test positive for HER2.
Pembrolizumab is given as an intravenous (IV) infusion, typically every 3 or 6 weeks.
Nivolumab (Opdivo) can be used in different situations:
- Nivolumab can be used in people with cancer of the esophagus or gastroesophageal junction (GEJ) who got chemotherapy and radiation (chemoradiation) before surgery, if lab tests after surgery show that some cancer may have been left behind.
- Nivolumab can be used by itself in people with advanced squamous cell cancer of the esophagus, typically after chemotherapy has been tried.
- Nivolumab can be used along with chemotherapy as a first treatment in people with advanced squamous cell cancer of the esophagus. When given this way, it can help some people live longer.
- Nivolumab can be used along with ipilimumab as a first treatment in people with advanced squamous cell cancer of the esophagus. When given this way, it can help some people live longer.
- Nivolumab can be used along with chemo in people with advanced adenocarcinoma of the esophagus or with advanced cancer of the gastroesophageal junction (GEJ).
Nivolumab is given as an intravenous (IV) infusion, usually once every 2, 3, or 4 weeks.
CTLA-4 inhibitor
Ipilimumab (Yervoy) is another drug that boosts the immune response, but it has a different target. It blocks CTLA-4, another protein on T cells that normally helps keep them in check.
It can be used along with nivolumab as the first option to treat advanced squamous cell cancer of the esophagus that can’t be removed by surgery or that has spread to other parts of the body.
Ipilimumab (Yervoy) is given as an intravenous (IV) infusion, usually once every 6 weeks when given in combination with nivolumab.
Treatments for complications
Treatments for esophageal obstruction and difficulty swallowing (dysphagia) can include:
- Relieving esophageal obstruction. If your esophageal cancer has narrowed your esophagus, a surgeon may do esophageal dilation to stretch out an area of the esophagus that is narrowed or blocked to allow better swallowing. A small balloon-like device or a device shaped like a pipe is passed down the throat and pushed through the narrowed area to stretch it out. This can be repeated if needed. Before the procedure, your doctor may give you a sedative to help you relax and may numb your throat by spraying it with a local anesthetic. There is a small risk of bleeding or tearing a hole in the esophagus (called a perforation) with this procedure, which could require surgery or other treatments to fix. The esophagus typically stays open only a few weeks after dilation, so this is often followed by other treatments (such as placing an expandable stent) to help keep the esophagus open. Other endoscopic procedures that can be used to help keep the esophagus open in people who are having trouble swallowing include:
- Esophageal stent placement
- Photodynamic therapy
- Electrocoagulation
- Laser ablation
- Argon plasma coagulation
- Providing nutrition. Your doctor may recommend a feeding tube if you’re having trouble swallowing or if you’re having esophagus surgery. A feeding tube allows nutrition to be delivered directly to your stomach or small intestine, giving your esophagus time to heal after cancer treatment. Some people with esophageal cancer may need to have a feeding tube, usually called a jejunostomy tube (or J-tube), put in place before treatment. This is done through a small hole in the skin over the abdomen during a minor operation. A J-tube lets liquid nutrition be put directly into the small intestine to prevent further weight loss and improve nutrition. This can make treatment easier to tolerate. Less often, the tube is placed into the stomach instead. This is known as a gastrostomy tube (G-tube). A feeding tube can easily be removed when it’s no longer needed.
- What Is Cancer of the Esophagus? https://www.cancer.org/cancer/types/esophagus-cancer/about/what-is-cancer-of-the-esophagus.html[↩]
- Bajwa SA, Toro F, Kasi A. Physiology, Esophagus. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519011[↩][↩]
- Esophageal spasm. https://medlineplus.gov/ency/article/000289.htm[↩][↩][↩]
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. 2017; 135:e1–e458. DOI: 10.1161/CIR.0000000000000485.[↩][↩][↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Attack. https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack[↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Are the Symptoms of a Heart Attack ? https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack/signs[↩]
- Zheng ZJ, Croft JB, Giles WH, Ayala CI, Greenlund KJ, Keenan NL, Neff L, Wattigney WA, Mensah GA. State Specific Mortality from Sudden Cardiac Death: United States, 1999. MMWR 2002;51(6):123–126. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5106a3.htm[↩]
- Oesophageal motility disorders. Richter, Joel E. The Lancet, Volume 358, Issue 9284, 823 – 828 https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(01)05973-6/abstract[↩]
- Allen MK, Frei W. Diffuse Esophageal Spasm: An Alternative Treatment Approach. Cureus. 2024 May 7;16(5):e59822. doi: 10.7759/cureus.59822[↩]
- Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021;33:e14058. doi: 10.1111/nmo.14053[↩]
- Patel DA, Vaezi MF. A Spiraling Case of Persistent Dysphagia. Diffuse Esophageal Spasm. Gastroenterology. 2015 Aug;149(2):298-9. doi: 10.1053/j.gastro.2015.04.049[↩]
- Goel S, Nookala V. Diffuse Esophageal Spasm. [Updated 2023 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541106[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Achem SR, Gerson LB. Distal esophageal spasm: an update. Curr Gastroenterol Rep. 2013 Sep;15(9):325. doi: 10.1007/s11894-013-0325-5[↩]
- Valdovinos MA, Zavala-Solares MR, Coss-Adame E. Esophageal hypomotility and spastic motor disorders: current diagnosis and treatment. Curr Gastroenterol Rep. 2014 Nov;16(11):421. doi: 10.1007/s11894-014-0421-1[↩][↩]
- Fonseca EK, Yamauchi FI, Tridente CF, Baroni RH. Corkscrew esophagus. Abdom Radiol (NY). 2017 Mar;42(3):985-986. doi: 10.1007/s00261-016-0965-7[↩]
- Diffuse esophageal spasm. https://radiopaedia.org/articles/diffuse-oesophageal-spasm?lang=us[↩][↩]
- Pehlivanov N, Liu J, Mittal RK. Sustained esophageal contraction: a motor correlate of heartburn symptom. Am J Physiol Gastrointest Liver Physiol. 2001 Sep;281(3):G743-51. doi: 10.1152/ajpgi.2001.281.3.G743[↩]
- Crozier RE, Glick ME, Gibb SP, Ellis FH Jr, Veerman JM. Acid-provoked esophageal spasm as a cause of noncardiac chest pain. Am J Gastroenterol. 1991 Nov;86(11):1576-80.[↩]
- Tanaka Y, Ihara E, Nakamura K, Muta K, Fukaura K, Mukai K, Bai X, Takayanagi R. Clinical characteristics associated with esophageal motility function. J Gastroenterol Hepatol. 2016 Jun;31(6):1133-40. doi: 10.1111/jgh.13262[↩]
- Diffuse esophageal spasm. https://radiopaedia.org/cases/diffuse-esophageal-spasm[↩]
- Roman S., Pandolfino J. E., Chen J., Boris L., Luger D., Kahrilas P. J. Phenotypes and clinical context of hypercontractility in high-resolution Esophageal Pressure Topography (EPT) American Journal of Gastroenterology. 2012;107(1):37–45. doi: 10.1038/ajg.2011.313[↩][↩][↩][↩][↩]
- Huang L., Pimentel M., Rezaie A. Do Jackhammer contractions lead to achalasia? A longitudinal study. Neurogastroenterology & Motility. 2017;29(3) doi: 10.1111/nmo.12953[↩][↩][↩][↩][↩][↩]
- Jia Y., Arenas J., Hejazi R. A., Elhanafi S., Saadi M., McCallum R. W. Frequency of jackhammer esophagus as the extreme phenotypes of esophageal hypercontractility based on the new chicago classification. Journal of Clinical Gastroenterology. 2016;50(8):615–618. doi: 10.1097/MCG.0000000000000496[↩][↩][↩][↩]
- García-Lledó J, Clemente-Sánchez A, Merino-Rodríguez B, Nogales-Rincón Ó, González-Asanza C, Menchén-Fernández-Pacheco P. Hypercontractile “jackhammer esophagus”. Rev Esp Enferm Dig. 2015 Apr;107(4):234.[↩][↩]
- Hypercontracting (nutcracker) esophagus. https://radiopaedia.org/articles/hypercontracting-nutcracker-oesophagus?lang=us[↩]
- Estremera-Arévalo F., Albéniz E., Rullán M., Areste I., Iglesias R., Vila J. Efficacy of peroral endoscopic myotomy compared with other invasive treatment options for the different esophageal motor disorders. Revista Española de Enfermedades Digestivas. 2017;109(8):578–586. doi: 10.17235/reed.2017.4773/2016[↩]
- Herregods T. V., Smout A. J., Ooi J. L., Sifrim D., Bredenoord A. J. Jackhammer esophagus: observations on a european cohort. Neurogastroenterology & Motility. 2017;29(4) doi: 10.1111/nmo.12975.e12975[↩]
- Tolone S., Savarino E., Docimo L. Radiofrequency catheter ablation for atrial fibrillation elicited “Jackhammer Esophagus”: a new complication due to vagal nerve stimulation? Journal of Neurogastroenterology and Motility. 2015;21(4):612–615. doi: 10.5056/jnm15034[↩][↩]
- Schlottmann F., Patti M. Primary esophageal motility disorders: beyond achalasia. International Journal of Molecular Sciences. 2017;18(7):p. 1399. doi: 10.3390/ijms1807139[↩]
- Clément M, Zhu WJ, Neshkova E, Bouin M. Jackhammer Esophagus: From Manometric Diagnosis to Clinical Presentation. Can J Gastroenterol Hepatol. 2019 Mar 3;2019:5036160. doi: 10.1155/2019/5036160[↩][↩][↩]
- Sato H., Takeuchi M., Takahashi K., et al. Nutcracker and jackhammer esophagus treatment: a three-case survey, including two novel cases of eosinophilic infiltration into the muscularis propria. Endoscopy. 2015;47(9):855–857. doi: 10.1055/s-0034-1391985[↩]
- Choi YI, Kim KO, Park DK, Chung JW, Kim YJ, Kwon KA. Clinical outcomes and safety of high-resolution manometry guided superficial partial circular muscle myotomy in per-oral endoscopic myotomy for Jackhammer esophagus: Two cases report. World J Clin Cases. 2019 Aug 26;7(16):2322-2329. doi: 10.12998/wjcc.v7.i16.2322[↩][↩]
- Kandulski A, Fuchs KH, Weigt J, Malfertheiner P. Jackhammer esophagus: high-resolution manometry and therapeutic approach using peroral endoscopic myotomy (POEM) Dis Esophagus. 2016;29:695–696. doi: 10.1111/dote.12182[↩]
- Herregods TV, Smout AJ, Ooi JL, Sifrim D, Bredenoord AJ. Jackhammer esophagus: Observations on a European cohort. Neurogastroenterol Motil. 2017:29. doi: 10.1111/nmo.12975[↩]
- Xiao Y, Carlson DA, Lin Z, Alhalel N, Pandolfino JE. Jackhammer esophagus: Assessing the balance between prepeak and postpeak contractile integral. Neurogastroenterol Motil. 2018;30:e13262. doi: 10.1111/nmo.13262[↩]
- Dawod E, Saumoy M, Xu MM, Kahaleh M. Peroral endoscopic myotomy (POEM) in jackhammer esophagus: a trick of the trade. Endoscopy. 2017;49:E254–E255. doi: 10.1055/s-0043-115887[↩]
- Khan MA, Kumbhari V, Ngamruengphong S, Ismail A, Chen YI, Chavez YH, Bukhari M, Nollan R, Ismail MK, Onimaru M, Balassone V, Sharata A, Swanstrom L, Inoue H, Repici A, Khashab MA. Is POEM the Answer for Management of Spastic Esophageal Disorders? A Systematic Review and Meta-Analysis. Dig Dis Sci. 2017;62:35–44. doi: 10.1007/s10620-016-4373-1[↩]
- Li C, Gong A, Zhang J, Duan Z, Ge L, Xia N, Leng J, Li M, Liu Y. Clinical Outcomes and Safety of Partial Full-Thickness Myotomy versus Circular Muscle Myotomy in Peroral Endoscopic Myotomy for Achalasia Patients. Gastroenterol Res Pract. 2017;2017:2676513. doi: 10.1155/2017/2676513[↩]
- Al-Qaisi MT, Siddiki HA, Crowell MD, Burdick GE, Fleischer DE, Ramirez FC, Vela MF. The clinical significance of hypercontractile peristalsis: comparison of high-resolution manometric features, demographics, symptom presentation, and response to therapy in patients with Jackhammer esophagus versus Nutcracker esophagus. Dis Esophagus. 2017;30:1–7. doi: 10.1093/dote/dox085[↩]
- Roman S, Kahrilas PJ. Management of spastic disorders of the esophagus. Gastroenterol Clin North Am. 2013;42:27–43. doi: 10.1016/j.gtc.2012.11.002[↩]
- Bechara R, Ikeda H, Inoue H. Peroral endoscopic myotomy for Jackhammer esophagus: to cut or not to cut the lower esophageal sphincter. Endosc Int Open. 2016;4:E585–E588. doi: 10.1055/s-0042-105204[↩]
- Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021 Jan;33(1):e14058. doi: 10.1111/nmo.14058. Erratum in: Neurogastroenterol Motil. 2024 Feb;36(2):e14179. doi: 10.1111/nmo.14179[↩]
- van Hoeij FB, Tack JF, Pandolfino JE, Sternbach JM, Roman S, Smout AJ, Bredenoord AJ. Complications of botulinum toxin injections for treatment of esophageal motility disorders†. Dis Esophagus. 2017 Feb 1;30(3):1-5. doi: 10.1111/dote.12491[↩]
- Diffuse esophageal spasm: the surgical approach. Salvador R, Costantini M, Rizzetto C, Zaninotto G. Dis Esophagus. 2012;25:311–318. doi: 10.1111/j.1442-2050.2010.01172.x[↩]
- Ponds FA, Smout AJPM, Fockens P, Bredenoord AJ. Challenges of peroral endoscopic myotomy in the treatment of distal esophageal spasm. Scand J Gastroenterol. 2018 Mar;53(3):252-255. doi: 10.1080/00365521.2018.1424933[↩]
- Schlottmann F, Shaheen NJ, Madanick RD, Patti MG. The role of Heller myotomy and POEM for nonachalasia motility disorders. Dis Esophagus. 2017 Apr 1;30(4):1-5. doi: 10.1093/dote/dox003[↩]
- Sugihara Y, Sakae H, Hamada K, Okada H. Peroral endoscopic myotomy is an effective treatment for diffuse esophageal spasm. Clin Case Rep. 2020 Feb 26;8(5):927-928. doi: 10.1002/ccr3.2755[↩]
- Khashab MA, Benias PC, Swanstrom LL. Endoscopic Myotomy for Foregut Motility Disorders. Gastroenterology. 2018 May;154(7):1901-1910. doi: 10.1053/j.gastro.2017.11.294[↩]
- Khan MA, Kumbhari V, Ngamruengphong S, Ismail A, Chen YI, Chavez YH, Bukhari M, Nollan R, Ismail MK, Onimaru M, Balassone V, Sharata A, Swanstrom L, Inoue H, Repici A, Khashab MA. Is POEM the Answer for Management of Spastic Esophageal Disorders? A Systematic Review and Meta-Analysis. Dig Dis Sci. 2017 Jan;62(1):35-44. doi: 10.1007/s10620-016-4373-1[↩]
- Khashab MA, Messallam AA, Onimaru M, Teitelbaum EN, Ujiki MB, Gitelis ME, Modayil RJ, Hungness ES, Stavropoulos SN, El Zein MH, Shiwaku H, Kunda R, Repici A, Minami H, Chiu PW, Ponsky J, Kumbhari V, Saxena P, Maydeo AP, Inoue H. International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc. 2015 May;81(5):1170-7. doi: 10.1016/j.gie.2014.10.011[↩]
- Esophageal spasms. https://www.mayoclinic.org/diseases-conditions/esophageal-spasms/diagnosis-treatment/drc-20372255[↩]
- Provenza D, Gillette C, Peacock B, Rejeski J. Managing heartburn and reflux in primary care. JAAPA. 2024 Mar 1;37(3):24-29. doi: 10.1097/01.JAA.0001005620.54669.f4[↩][↩]
- Peery AF, Crockett SD, Murphy CC, Jensen ET, Kim HP, Egberg MD, Lund JL, Moon AM, Pate V, Barnes EL, Schlusser CL, Baron TH, Shaheen NJ, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022 Feb;162(2):621-644. doi: 10.1053/j.gastro.2021.10.017[↩]
- Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022 Jan 1;117(1):27-56. doi: 10.14309/ajg.0000000000001538[↩]
- Delshad SD, Almario CV, Chey WD, Spiegel BMR. Prevalence of Gastroesophageal Reflux Disease and Proton Pump Inhibitor-Refractory Symptoms. Gastroenterology. 2020 Apr;158(5):1250-1261.e2. doi: 10.1053/j.gastro.2019.12.014[↩]
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x[↩][↩]
- Hungin APS, Molloy-Bland M, Scarpignato C. Revisiting Montreal: new insights into symptoms and their causes, and implications for the future of GERD. Am J Gastroenterol. 2019;114:414–421. doi: 10.1038/s41395-018-0287-1[↩][↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589[↩][↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018 Mar;67(3):430-440. doi: 10.1136/gutjnl-2016-313589[↩][↩][↩]
- Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441938[↩][↩][↩][↩]
- Hunt R, Quigley E, Abbas Z, Eliakim A, Emmanuel A, Goh KL, Guarner F, Katelaris P, Smout A, Umar M, Whorwell P, Johanson J, Saenz R, Besançon L, Ndjeuda E, Horn J, Hungin P, Jones R, Krabshuis J, LeMair A; World Gastroenterology Organisation. Coping with common gastrointestinal symptoms in the community: a global perspective on heartburn, constipation, bloating, and abdominal pain/discomfort May 2013. J Clin Gastroenterol. 2014 Aug;48(7):567-78. doi: 10.1097/MCG.0000000000000141[↩][↩]
- Nexium 24HR [product labeling]. Madison, NJ: Pfizer Consumer Healthcare; 2014.[↩]
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006 Aug;101(8):1900-20; quiz 1943. doi: 10.1111/j.1572-0241.2006.00630.x[↩][↩]
- Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Graffner H, Vieth M, Stolte M, Engstrand L, Talley NJ, Agréus L. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005 Mar;40(3):275-85. doi: 10.1080/00365520510011579[↩]
- Zou D, He J, Ma X, Chen J, Gong Y, Man X, Gao L, Wang R, Zhao Y, Yan X, Liu W, Wernersson B, Johansson S, Dent J, Sung JJ, Li Z. Epidemiology of symptom-defined gastroesophageal reflux disease and reflux esophagitis: the systematic investigation of gastrointestinal diseases in China (SILC). Scand J Gastroenterol. 2011 Feb;46(2):133-41. doi: 10.3109/00365521.2010.521888[↩]
- Altuwaijri M. Evidence-based treatment recommendations for gastroesophageal reflux disease during pregnancy: A review. Medicine (Baltimore). 2022 Sep 2;101(35):e30487. doi: 10.1097/MD.0000000000030487[↩][↩]
- Richter JE. Review article: the management of heartburn in pregnancy. Aliment Pharmacol Ther. 2005 Nov 1;22(9):749-57. doi: 10.1111/j.1365-2036.2005.02654.x[↩][↩][↩][↩][↩][↩][↩]
- Quartarone G. Gastroesophageal reflux in pregnancy: a systematic review on the benefit of raft forming agents. Minerva Ginecol. 2013 Oct;65(5):541-9.[↩][↩]
- Audu BM, Mustapha SK. Prevalence of gestrointestinal symptoms in pregnancy. Niger J Clin Pract. 2006 Jun;9(1):1-6.[↩]
- Ho KY, Kang JY, Viegas OA. Symptomatic gastro-oesophageal reflux in pregnancy: a prospective study among Singaporean women. J Gastroenterol Hepatol. 1998 Oct;13(10):1020-6. doi: 10.1111/j.1440-1746.1998.tb00564.x[↩]
- Law R, Maltepe C, Bozzo P, Einarson A. Treatment of heartburn and acid reflux associated with nausea and vomiting during pregnancy. Can Fam Physician. 2010 Feb;56(2):143-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2821234/[↩]
- Richter JE. Gastroesophageal reflux disease during pregnancy. Gastroenterol Clin North Am. 2003 Mar;32(1):235-61. doi: 10.1016/s0889-8553(02)00065-1[↩][↩][↩]
- Vazquez JC. Heartburn in pregnancy. BMJ Clin Evid. 2015 Sep 8;2015:1411 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4562453/[↩][↩]
- Dowswell T, Neilson JP. Interventions for heartburn in pregnancy. Cochrane Database Syst Rev. 2008 Oct 8;2008(4):CD007065. doi: 10.1002/14651858.CD007065.pub2[↩]
- Armstrong D, Marshall JK, Chiba N, Enns R, Fallone CA, Fass R, Hollingworth R, Hunt RH, Kahrilas PJ, Mayrand S, Moayyedi P, Paterson WG, Sadowski D, van Zanten SJ; Canadian Association of Gastroenterology GERD Consensus Group. Canadian Consensus Conference on the management of gastroesophageal reflux disease in adults – update 2004. Can J Gastroenterol. 2005 Jan;19(1):15-35. doi: 10.1155/2005/836030[↩]
- Baron TH, Ramirez B, Richter JE. Gastrointestinal motility disorders during pregnancy. Ann Intern Med. 1993 Mar 1;118(5):366-75. doi: 10.7326/0003-4819-118-5-199303010-00008[↩]
- Marrero JM, Goggin PM, de Caestecker JS, Pearce JM, Maxwell JD. Determinants of pregnancy heartburn. Br J Obstet Gynaecol. 1992 Sep;99(9):731-4. doi: 10.1111/j.1471-0528.1992.tb13873.x[↩]
- Van Thiel DH, Gavaler JS, Joshi SN, Sara RK, Stremple J. Heartburn of pregnancy. Gastroenterology. 1977 Apr;72(4 Pt 1):666-8.[↩][↩]
- Ho SC, Chang CS, Wu CY, Chen GH. Ineffective esophageal motility is a primary motility disorder in gastroesophageal reflux disease. Dig Dis Sci. 2002 Mar;47(3):652-6. doi: 10.1023/a:1017992808762[↩]
- Mandel KG, Daggy BP, Brodie DA, Jacoby HI. Review article: alginate-raft formulations in the treatment of heartburn and acid reflux. Aliment Pharmacol Ther. 2000 Jun;14(6):669-90. doi: 10.1046/j.1365-2036.2000.00759.x[↩]
- Strugala V, Bassin J, Swales VS, Lindow SW, Dettmar PW, Thomas EC. Assessment of the Safety and Efficacy of a Raft-Forming Alginate Reflux Suppressant (Liquid Gaviscon) for the Treatment of Heartburn during Pregnancy. ISRN Obstet Gynecol. 2012;2012:481870. doi: 10.5402/2012/481870[↩]
- da Silva JB, Nakamura MU, Cordeiro JA, Kulay L Jr, Saidah R. Acupuncture for dyspepsia in pregnancy: a prospective, randomised, controlled study. Acupunct Med. 2009 Jun;27(2):50-3. doi: 10.1136/aim.2009.000497[↩]
- Phupong V, Hanprasertpong T. Interventions for heartburn in pregnancy. Cochrane Database Syst Rev. 2015 Sep 19;2015(9):CD011379. doi: 10.1002/14651858.CD011379.pub2[↩][↩]
- Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013 Mar;108(3):308-28; quiz 329. doi: 10.1038/ajg.2012.444. Epub 2013 Feb 19. Erratum in: Am J Gastroenterol. 2013 Oct;108(10):1672.[↩][↩]
- Wang KK, Sampliner RE; Practice Parameters Committee of the American College of Gastroenterology. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett’s esophagus. Am J Gastroenterol. 2008 Mar;103(3):788-97. doi: 10.1111/j.1572-0241.2008.01835.x[↩][↩][↩]
- Chiba N, De Gara CJ, Wilkinson JM, Hunt RH. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology. 1997 Jun;112(6):1798-810. doi: 10.1053/gast.1997.v112.pm9178669[↩][↩]
- Hershcovici T, Fass R. Pharmacological management of GERD: where does it stand now? Trends Pharmacol Sci. 2011 Apr;32(4):258-64. doi: 10.1016/j.tips.2011.02.007[↩][↩]
- Fass R, Shapiro M, Dekel R, Sewell J. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease–where next? Aliment Pharmacol Ther. 2005 Jul 15;22(2):79-94. doi: 10.1111/j.1365-2036.2005.02531.x[↩][↩]
- Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997 May;112(5):1448-56. doi: 10.1016/s0016-5085(97)70025-8[↩]
- Nebel OT, Fornes MF, Castell DO. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis. 1976 Nov;21(11):953-6. doi: 10.1007/BF01071906[↩]
- Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Prevalence of gastro-oesophageal reflux symptoms and the influence of age and sex. Scand J Gastroenterol. 2004 Nov;39(11):1040-5. doi: 10.1080/00365520410003498[↩]
- Fass R, Frazier R. The role of dexlansoprazole modified-release in the management of gastroesophageal reflux disease. Therap Adv Gastroenterol. 2017 Feb;10(2):243-251. doi: 10.1177/1756283X16681701[↩][↩]
- Fass R, Ofman JJ. Gastroesophageal reflux disease–should we adopt a new conceptual framework? Am J Gastroenterol. 2002 Aug;97(8):1901-9. doi: 10.1111/j.1572-0241.2002.05912.x[↩][↩]
- Kellerman R, Kintanar T. Gastroesophageal Reflux Disease. Prim Care. 2017 Dec;44(4):561-573. doi: 10.1016/j.pop.2017.07.001[↩][↩][↩]
- Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ, Tytgat GN, Wallin L. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999 Aug;45(2):172-80. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1727604/pdf/v045p00172.pdf[↩]
- Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007 Feb;41(2):131-7. doi: 10.1097/01.mcg.0000225631.07039.6d[↩]
- Argyrou A, Legaki E, Koutserimpas C, Gazouli M, Papaconstantinou I, Gkiokas G, Karamanolis G. Risk factors for gastroesophageal reflux disease and analysis of genetic contributors. World J Clin Cases. 2018 Aug 16;6(8):176-182. doi: 10.12998/wjcc.v6.i8.176[↩]
- Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005 Aug 2;143(3):199-211. doi: 10.7326/0003-4819-143-3-200508020-00006[↩]
- Malfertheiner P, Nocon M, Vieth M, Stolte M, Jaspersen D, Koelz HR, Labenz J, Leodolter A, Lind T, Richter K, Willich SN. Evolution of gastro-oesophageal reflux disease over 5 years under routine medical care–the ProGERD study. Aliment Pharmacol Ther. 2012 Jan;35(1):154-64. doi: 10.1111/j.1365-2036.2011.04901.x[↩]
- El-Serag HB, Hashmi A, Garcia J, Richardson P, Alsarraj A, Fitzgerald S, Vela M, Shaib Y, Abraham NS, Velez M, Cole R, Rodriguez MB, Anand B, Graham DY, Kramer JR. Visceral abdominal obesity measured by CT scan is associated with an increased risk of Barrett’s oesophagus: a case-control study. Gut. 2014 Feb;63(2):220-9. doi: 10.1136/gutjnl-2012-304189[↩]
- Mohammed I, Nightingale P, Trudgill NJ. Risk factors for gastro-oesophageal reflux disease symptoms: a community study. Aliment Pharmacol Ther. 2005 Apr 1;21(7):821-7. doi: 10.1111/j.1365-2036.2005.02426.x[↩]
- Gastroesophageal Reflux Disease (GERD). https://www.hopkinsmedicine.org/health/conditions-and-diseases/gastroesophageal-reflux-disease-gerd[↩]
- Sandhu DS, Fass R. Current Trends in the Management of Gastroesophageal Reflux Disease. Gut Liver. 2018 Jan 15;12(1):7-16. doi: 10.5009/gnl16615[↩]
- Hom C, Vaezi MF. Extraesophageal manifestations of gastroesophageal reflux disease. Gastroenterol Clin North Am. 2013 Mar;42(1):71-91. doi: 10.1016/j.gtc.2012.11.004[↩]
- Esophagitis. Medline Plus. https://medlineplus.gov/ency/article/001153.htm[↩]
- Key Statistics for Esophageal Cancer. https://www.cancer.org/cancer/types/esophagus-cancer/about/key-statistics.html[↩][↩][↩]
- Esophageal Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/esoph.html[↩][↩][↩][↩]
- Khieu M, Mukherjee S. Barrett Esophagus. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430979[↩][↩]
- Barrett esophagus. Medline Plus. https://medlineplus.gov/ency/article/001143.htm[↩][↩]
- Clermont M, Falk GW. Clinical Guidelines Update on the Diagnosis and Management of Barrett’s Esophagus. Dig Dis Sci. 2018 Aug;63(8):2122-2128. doi: 10.1007/s10620-018-5070-z[↩][↩]
- Shaheen NJ, Falk GW, Iyer PG, Gerson LB; American College of Gastroenterology. ACG Clinical Guideline: Diagnosis and Management of Barrett’s Esophagus. Am J Gastroenterol. 2016 Jan;111(1):30-50; quiz 51. doi: 10.1038/ajg.2015.322. Epub 2015 Nov 3. Erratum in: Am J Gastroenterol. 2016 Jul;111(7):1077.[↩]
- Beg S, Ragunath K, Wyman A, Banks M, Trudgill N, Pritchard DM, Riley S, Anderson J, Griffiths H, Bhandari P, Kaye P, Veitch A. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut. 2017 Nov;66(11):1886-1899. doi: 10.1136/gutjnl-2017-314109. Epub 2017 Aug 18. Erratum in: Gut. 2017 Dec;66(12 ):2188.[↩]
- Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 11th Edition: part I. Esophagus. 2017;14(1):1-36. doi: 10.1007/s10388-016-0551-7[↩]
- Akın H, Aydın Y. How should we describe, diagnose and observe the Barrett’s esophagus? Turk J Gastroenterol. 2017 Dec;28(Suppl 1):S26-S30. doi: 10.5152/tjg.2017.08[↩]
- Koike T, Saito M, Ohara Y, Hatta W, Masamune A. Current status of surveillance for Barrett’s esophagus in Japan and the West. DEN Open. 2022 Feb 13;2(1):e94. doi: 10.1002/deo2.94[↩]
- Fass R, Hell RW, Garewal HS, Martinez P, Pulliam G, Wendel C, Sampliner RE. Correlation of oesophageal acid exposure with Barrett’s oesophagus length. Gut. 2001 Mar;48(3):310-3. doi: 10.1136/gut.48.3.310[↩]
- Koek GH, Sifrim D, Lerut T, Janssens J, Tack J. Multivariate analysis of the association of acid and duodeno-gastro-oesophageal reflux exposure with the presence of oesophagitis, the severity of oesophagitis and Barrett’s oesophagus. Gut. 2008 Aug;57(8):1056-64. doi: 10.1136/gut.2006.119206[↩]
- Champion G, Richter JE, Vaezi MF, Singh S, Alexander R. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett’s esophagus. Gastroenterology. 1994 Sep;107(3):747-54. doi: 10.1016/0016-5085(94)90123-6[↩]
- Barrett’s Esophagus. American College of Gastroenterology. http://patients.gi.org/topics/barretts-esophagus/[↩][↩]
- Desai TK, Krishnan K, Samala N, Singh J, Cluley J, Perla S, Howden CW. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut. 2012 Jul;61(7):970-6. doi: 10.1136/gutjnl-2011-300730[↩]
- Erőss B, Farkas N, Vincze Á, Tinusz B, Szapáry L, Garami A, Balaskó M, Sarlós P, Czopf L, Alizadeh H, Rakonczay Z Jr, Habon T, Hegyi P. Helicobacter pylori infection reduces the risk of Barrett’s esophagus: A meta-analysis and systematic review. Helicobacter. 2018 Aug;23(4):e12504. doi: 10.1111/hel.12504[↩]
- Thrift AP. Barrett’s Esophagus and Esophageal Adenocarcinoma: How Common Are They Really? Dig Dis Sci. 2018 Aug;63(8):1988-1996. doi: 10.1007/s10620-018-5068-6[↩]
- Michopoulos S. Critical appraisal of guidelines for screening and surveillance of Barrett’s esophagus. Ann Transl Med. 2018 Jul;6(13):259. doi: 10.21037/atm.2018.05.09[↩]
- Bellizzi AM, Hafezi-Bakhtiari S, Westerhoff M, Marginean EC, Riddell RH. Gastrointestinal pathologists’ perspective on managing risk in the distal esophagus: convergence on a pragmatic approach. Ann N Y Acad Sci. 2018 Dec;1434(1):35-45. doi: 10.1111/nyas.13680[↩]