Contents
- Early menopause
- What is perimenopause?
- When does perimenopause usually start?
- How will I know if I am in perimenopause?
- How long does perimenopause last?
- Should I continue using birth control during perimenopause?
- What is menopause?
- What is the earliest age for menopause?
- Can menopause start at 35?
- What is the difference between early and premature menopause?
- How common are premature menopause and early menopause?
- What is the difference between early menopause and premature ovarian failure?
- How do I know if I am going through early or premature menopause?
- Can you reverse early menopause?
- How can I reduce my risk of early menopause?
- If I have early menopause, can I still have children?
- Can my menstrual periods return if they’ve stopped after having chemotherapy or radiation therapy?
- How do you know if you are starting early menopause?
- Early menopause causes
- Early menopause signs and symptoms
- Early menopause complications
- Early menopause diagnosis
- Early menopause treatment
Early menopause
Early menopause is menopause that happens between the age of 40 and 45 1, 2, 3, 4, 5. Premature menopause is menopause before the age of 40 years 6, 5. In the Western world, the average age of menopause is between 46 and 55 years (the average age for menopause in the United States is 51) 7. About 10% of women naturally go through early menopause 8, 9, 6. Smoking, alcohol (alcohol 5-7 days/week), lack of physical activity, low body mass index (BMI < 18.5 kg/m²), obesity (BMI ≥ 35 kg/m²), a short period of oral contraceptives use (less than 1 year), lower number of pregnancies (less than 2 pregnancies), high intake of polyunsaturated fat and certain medicines or treatments can cause menopause to come earlier than usual 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25.
Early menopause can happen on its own for no clear reason or it can happen because of certain surgeries, medicines, or health conditions. Early menopause can be spontaneous such as primary ovarian insufficiency (premature ovarian failure) or induced due to cancer treatments including chemotherapy and radiation or surgical procedures such as surgery to remove the uterus (hysterectomy) or surgical removal of both ovaries (bilateral oophorectomy) 6, 26, 27, 28. Primary ovarian insufficiency occurs from a premature loss of ovarian follicles, resulting in lower levels of female reproductive hormones. Regardless of cause, women who go through early menopause at an age well before the age of natural menopause may face emotional challenges and struggles with infertility. In general, the onset of menopause brings about an increase in certain risk factors such as osteoporosis, psychosexual dysfunction, heart and blood vessel disease (cardiovascular disease), cognitive impairment, dementia, decreased quality of life and increased all-cause mortality 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 6.
According to the World Health Organization (WHO), natural menopause is defined as “permanent cessation of menstruation resulting from the loss of ovarian follicular activity”, which is normally recognized as 12 months in a row without a period (amenorrhea) 40. Hormonally, early menopause resembles natural menopause. Your ovaries produce very little or no estrogen. Ovulation completely or almost completely stops. And depending on the underlying cause of your early menopause, sometimes your ovaries may start functioning again for a short time and can release an egg, making pregnancy possible. The ovaries still contain thousands of eggs. Early menopause does not imply that a woman is aging prematurely. Early menopause means only that your ovaries are no longer functioning normally.
Early menopause has many causes 41:
- Primary ovarian insufficiency also called premature ovarian failure is a condition in which younger women skip many periods in a row or have no periods at all. In most cases, the exact cause of primary ovarian insufficiency is unknown 42, 43, 44.
- Genetic abnormalities: Chromosomes, including the sex chromosomes, may be abnormal. Sex chromosome abnormalities include Turner syndrome, disorders that result in having a Y chromosome (which normally occurs only in males), and Fragile X syndrome.
- Autoimmune disorder: Autoimmune disorder such as thyroiditis, vitiligo, myasthenia gravis, Addison disease (adrenal insufficiency) and rheumatoid arthritis. Although rare, the body’s immune system, which normally fights off diseases, may mistakenly attack the ovaries and keep them from making hormones.
- Metabolic disorders such as enzyme deficiencies
- Chemotherapy or radiation therapy for cancer
- Surgical removal of both ovaries (bilateral oophorectomy): Surgery to remove both ovaries (bilateral oophorectomy) ends menstrual periods and causes menopause.
- Surgical removal of the uterus (hysterectomy): Surgery to remove the uterus (hysterectomy) ends menstrual periods but does not cause most of the other symptoms of menopause as long as the ovaries are functioning.
- Women with mumps, chickenpox, malaria, shigella, and tuberculosis (TB) can destroy healthy ovarian tissue and substantially decrease the amount of functioning tissue that remains 43, 45, 46, 44.
- Toxins. Cigarette smoke, chemicals, nicotine, phthalates, polychlorinated biphenyls (PCBs), per- and polyfluoroalkyl substance (PFAS), bisphenol-A (BPA), dimethylbenzanthracene and pesticides can speed up ovarian follicle depletion.
- Viruse infections have been shown to affect follicle function 46, 43.
- HIV and AIDS. Women with HIV whose infection is not well controlled with medicine may experience early menopause 47. Women with HIV may also have more severe hot flashes than women without HIV 48.
Sometimes there’s no cause of early menopause. This is the case in up to 50% of women.
In early menopause, earlier loss of bone may lead to an earlier risk of bone fractures related to osteoporosis. Early menopause also may increase your risk of heart disease later in life. Because menopause appears to influence cognitive function (mental processes involved in the acquisition of knowledge, manipulation of information, and reasoning), this is an important consideration for women who experience menopause at a younger age. Estrogen has been shown to have protective effects on the brain. In addition, many of the same lifestyle habits used for heart health have been shown to be beneficial to memory and help protect the brain against dementia.
Just as important as the physical aspects of early menopause are the emotional ones. Early menopause can cause distress to a woman’s sense of self. For women who still want to have children, the effects may be particularly damaging. Early menopause may increase concerns about body image, sexuality, fertility, and the perception of growing old prematurely. For women with primary ovarian insufficiency (premature ovarian failure), a diagnosis may be delayed, which can be frustrating. Women going through early menopause also may need to cope with or continue treatment for the underlying condition that caused menopause to occur.
For women with induced menopause, especially when it results from treatment for a serious illness, a number of other fears and concerns may compound the challenges of early menopause:
- Pain and discomfort related to the disease or treatment
- Anxiety over additional treatments
- A sense of loss of control related to illness, treatments, hospitalizations, and adverse events
- Confusion over lack of information or a feeling of information overload
- Frustration over a lack of support
- Reduced self-esteem because of changes from surgery
- Embarrassment related to hair or skin changes caused by chemotherapy or radiation
- Feelings of resentment or guilt
- Apprehension about relationships, including sexual activity and intimacy
- A feeling of uncertainty or hopelessness
- Fear of not being cured or of death
- Fear of the disease coming back (recurrence)
If you believe you are going through early menopause and have concerns, see your doctor. Your doctor may order a blood test to check your hormone levels. Your doctor will check for estrogen as well as a follicle-stimulating hormone (FSH), luteinizing hormone (LH) and thyroid-stimulating hormone (TSH).
Symptoms of early menopause such as hot flashes, mood irritability, night sweats, sleep disturbance, vaginal dryness/irritation, and dyspareunia can be a nuisance for women. However, they are not life-threatening and can be improved by hormone replacement therapy (HRT) or birth control pills or a patch that contains both estrogen and progestin (combination oral contraceptives) 49. Hormone replacement therapy (HRT) comes in two main types: estrogen-only and estrogen plus progestin. Estrogen therapy helps relieve symptoms and helps prevent other effects of menopause (such as vaginal dryness, and mood swings). It also helps maintain bone density (to prevent osteoporosis). Because taking estrogen alone increases the risk of cancer of the uterine lining (endometrial cancer), most women should also take a progestin or progesterone with the estrogen to help protect against this cancer. Women who have had a hysterectomy (removal of the uterus) do not need to take a progestin or progesterone. These treatments are typically taken until about age 51 (the average age for menopause). Then, doctors decide whether to continue the treatments based on a woman’s individual circumstances.
If you are interested in taking hormone replacement therapy (HRT), your doctor should discuss the benefits and risks with you before you start the treatment. This discussion should cover both the short-term (over the next 5 years) and the longer term (beyond the next 5 years) benefits and risks for you. You should also be informed about available alternatives to hormone replacement therapy (HRT) along with their benefits and risks.
Hormone replacement therapy (HRT) is delivered either systemically (meaning it is released into the bloodstream) or locally (only to the affected area). If used systemically, it can be delivered via pills, skin patches, gels, injections, and sprays; if used locally (for example, for women experiencing only vaginal dryness), it may be applied directly to the affected area by vaginal ring, cream, or tablet.
The delivery methods may have estrogen and progestin together, or progestin may be taken separately. Depending on the type of hormone replacement therapy (HRT), it may be taken daily or on certain days of the month. Systemic hormone therapy is usually not recommended for women who have had endometrial cancer, stroke, a heart attack, blood clots, or liver disease or for those who are pregnant.
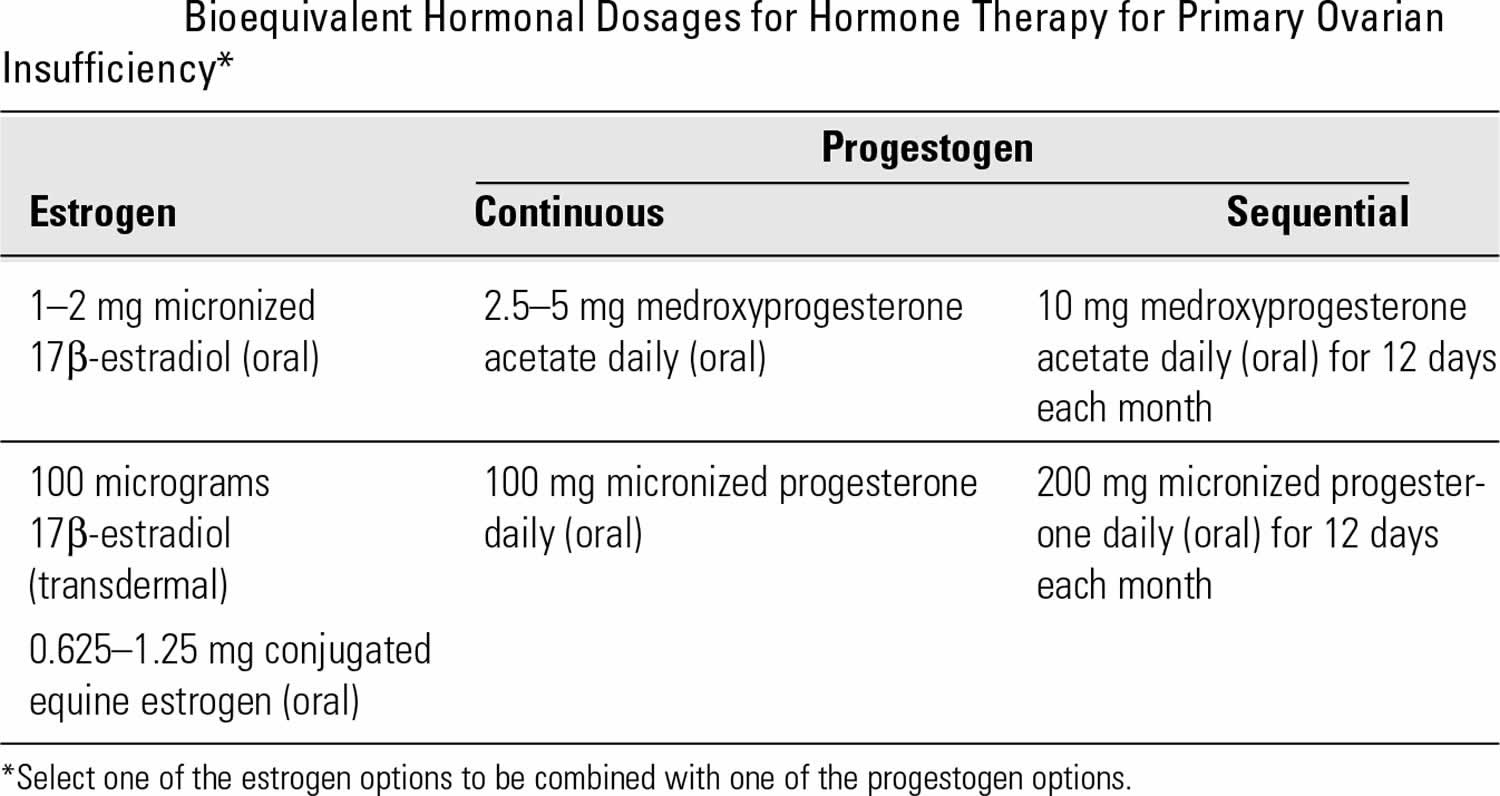
A common post-pubertal hormone replacement therapy (HRT) regimen is 100 mcg of daily transdermal estradiol or 0.625 mg of daily oral conjugated estrogens, adding 200 mg of micronized oral progesterone daily for 12 days each month 50, 51, 52. Transdermal estrogen may be associated with lower blood clot (venous thromboembolism) risk than oral formulations 53. It is also reasonable to recommend 1,200 mg of calcium daily and 1,000 IU of vitamin D daily with regular weight-bearing exercises to maintain bone mineral density in accordance with guidelines for postmenopausal women 54, 43.
What is perimenopause?
Perimenopause also called the “menopausal transition” or “around menopause” is the time leading up to your last period or the transitional time to menopause 55. Perimenopause is the gradual transition between your reproductive years and menopause (the cessation of menstrual periods). Menopause is when your periods stop permanently and you can no longer get pregnant. You have reached menopause only after it has been a full 12 months in a row since you have your last period. This means you have not had any bleeding, including spotting, for 12 months in a row. Perimenopause is a natural process when your ovaries gradually stop working. As your body transitions to menopause, your hormone levels may change randomly, causing menopause symptoms unexpectedly. During perimenopause, your ovaries make different amounts of the hormones estrogen and progesterone than usual. Your ovulation may become erratic and then stop. A common sign of perimenopause is a change in your menstrual cycle. Your menstrual cycle lengthens and flow may become irregular before your final period. Irregular periods happen during this time because you may not ovulate every month. Your periods may be longer or shorter than usual. You might skip periods a few months or have unusually long or short menstrual cycles. Your period may be heavier or lighter than before. Many women also have hot flashes and other menopause symptoms during perimenopause.
Perimenopause is generally a transition that is many years long and can be associated with shorter menstrual intervals, irregular periods, night sweats, and other symptoms. In some women, these symptoms are troublesome enough to need medical intervention.
Women start perimenopause at different ages. You may notice signs of progression toward menopause, such as menstrual irregularity, sometime in your 40s 56. But some women notice changes as early as their mid-30s 57.
- However, the perimenopause transition phase most often begins between ages 45 and 55 and may last for 4 to 8 years (usually lasts about 7 years), but can last as long as 14 years.
- Perimenopause begins with changes in the length of time between periods and ends 1 year after the final menstrual period. Once you’ve gone through 12 consecutive months without a menstrual period, you’ve officially reached menopause, and the perimenopause period is over.
The level of estrogen — the main female hormone — in your body rises and falls unevenly during perimenopause. Your menstrual cycles may lengthen or shorten, and you may begin having menstrual cycles in which your ovaries don’t release an egg (ovulate). You may also experience menopause-like symptoms, such as hot flashes, sleep problems and vaginal dryness.
No two women will experience perimenopause in the same way. Some women do not have any symptoms of perimenopause or have only a few mild symptoms. Others have many symptoms that can be severe.
These are the most common perimenopause symptoms 58:
- Hot flashes. A hot flash is a sudden feeling of heat that rushes to your upper body and face. A hot flash may last from a few seconds to several minutes or longer. Some women have hot flashes a few times a month. Others have them several times a day. Hot flashes that happen at night (night sweats) may wake you up and cause you to feel tired and sluggish during the day.
- Sleep problems. You may have insomnia (trouble falling asleep), or you may wake up long before your usual time. Night sweats may disrupt your sleep.
- Vaginal and urinary tract changes. As your estrogen levels decrease, the lining of your vagina may become thinner, dryer, and less elastic. Vaginal dryness may cause pain during sex. Vaginal infections also may occur more often. The urethra can become dry, inflamed, or irritated. This can cause more frequent urination and increase the risk of urinary tract infections.
Other perimenopause symptoms include:
- Irregular periods. Your menstrual periods may not come as regularly as before. They also might last longer or be shorter. You might skip some months. Periods might stop for a few months and then start up again.
- Your periods might be heavier or lighter than before.
- You might experience mood swings or be irritable.
- Changes in sexual desire (libido). You may have less interest in sex. It may take longer for you to get aroused.
- Trouble concentrating or with memory
- Headaches
- Joint and muscle aches
- Heavy sweating
- Having to pee often
- Premenstrual syndrome (PMS)-like symptoms
Other possible changes are not as noticeable. For example, you might begin to lose bone density because you have less estrogen. This can lead to osteoporosis, a condition that causes bones to become weak and break easily. Changing estrogen levels can also increase your cholesterol levels and increase your risk for heart disease and stroke.
The symptoms of perimenopause may look like other health conditions. Always talk with your family doctor for a diagnosis.
Sometimes it’s hard to tell if you are having symptoms of perimenopause. Your symptoms, health history, age, and a physical exam may help your doctor with the diagnosis. You may also have blood tests to measure your hormone levels.
Perimenopause doesn’t need to be treated unless your symptoms are bothering you. Treatments are available to help ease perimenopause symptoms.
Perimenopause treatments may include:
- Find what triggers your hot flashes by keeping a record. For example, alcohol, coffee, or tea may be a trigger.
- Hormone therapy using estrogen or estrogen and progestins to level out hormone levels.
- Selective estrogen receptor modulators (SERMs)
- Antidepressants
- Gabapentin
- Clonidine
- Cognitive behavioral therapy (CBT)
- Plant-based therapies
Your family doctor may suggest healthy lifestyle changes:
- Eat a healthy diet with fruits and vegetables and whole grains.
- Get at least 1,000 mg to 1,200 mg of calcium each day through your diet or supplements.
- Exercise regularly.
Discuss other treatments for easing symptoms with your family doctor.
You may hear about herbal supplements that claim to help manage hot flashes. It’s important to remember that the FDA does not regulate these supplements. They are not tested like traditional medicines to prove that they work and are safe to take. Talk with your family doctor before using any herbal supplements.
When does perimenopause usually start?
Perimenopause, the transition to menopause, usually starts in a woman’s mid- to late 40s 56. On average, women are in perimenopause for four years before their periods stop.
How will I know if I am in perimenopause?
Sometimes it can be hard for you and your doctor to tell whether you are in perimenopause, the transition to menopause:
- Symptoms: Tell your doctor about your symptoms such as hot flashes or trouble sleeping.
- Irregular periods: Track your periods. Irregular periods may be your first sign of menopause.
- Hormone levels: Your doctor may test the amount of hormones in your blood if your periods stopped at an early age (before 40). Doctors don’t usually recommend this test unless there is a medical reason to do so. This is because for most women hormone levels go up and down in an unpredictable way during perimenopause. So it is difficult to tell for sure whether you have gone through menopause or are getting close to it based on this blood test alone.
How long does perimenopause last?
Perimenopause can last between two and eight years before your periods stop permanently 59. For most women, perimenopause lasts about 4 years. You will know you have reached menopause only after it has been a full 12 months in a row since your last period. This means you have not had any bleeding, including spotting, for 12 months in a row.
Should I continue using birth control during perimenopause?
Yes. You can still get pregnant during perimenopause even if you miss your period for a month or a few months 59. During perimenopause you may still ovulate, or release an egg, on some months. But it is impossible to know for sure when you will ovulate 59. If you don’t want to get pregnant, you should continue to use birth control until one full year after your last period. Talk to your doctor about your birth control needs.
What is menopause?
Menopause is when your periods stop permanently and you can no longer get pregnant. Menopause happens when you have gone 12 months in a row without a period. This means you have not had any bleeding, including spotting, for 12 months in a row. After menopause your ovaries make very little of the hormones estrogen and progesterone. These low hormone levels can raise your risk for certain health problems.
The average age of menopause in the United States is 51. The range for women is usually between 45 and 58. One way to tell when you might go through menopause is the age your mother went through it 60.
Menopause may happen earlier if you:
- Never had children. Pregnancy, especially more than one pregnancy, may delay menopause 61.
- Smoke. Studies show smoking can cause you to start menopause up to two years earlier than women who don’t smoke 62.
Certain health problems can also cause you to start menopause earlier. Menopause usually happens on its own. However, you may enter menopause earlier than you normally would if you have had chemotherapy or surgery to remove both ovaries.
What is the earliest age for menopause?
Menopause can happen when a person is in their 20s, 30s or 40s. Premature menopause describes menopause that occurs any time before age 40. It’s rare for menopause to happen before age 30.
Can menopause start at 35?
Yes, starting menopause around age 35 is premature menopause.
What is the difference between early and premature menopause?
Early or premature menopause happens when ovaries stop making hormones and periods stop at a younger age than usual. This can happen naturally or for a medical reason, such as when both ovaries are removed in a hysterectomy.
Early and premature menopause can have the same causes. The only difference is the age at which it happens. Menopause that happens between the age of 40 and 45 is called early menopause. Menopause that happens before age 40 is called premature menopause.
Women who have gone through early or premature menopause cannot get pregnant.
How common are premature menopause and early menopause?
Early menopause (menopause between the age of 40 and 45) occurs in about 10% of women. Premature menopause (menopause before the age 40) happens in about 1% of women. It’s rare to experience menopause in your 20s. This happens in about 0.1% of women.
What is the difference between early menopause and premature ovarian failure?
Early menopause is not the same as premature ovarian failure, although some people use the terms interchangeably. Doctors now refer to premature ovarian failure as primary ovarian insufficiency (POI).
How do I know if I am going through early or premature menopause?
You know you have gone through menopause when you have not had your period for 12 months in a row. If you think you may be reaching menopause early, talk to your doctor.
- Your doctor will ask you about your symptoms, such as hot flashes, irregular periods, sleep problems, and vaginal dryness.
- Your doctor may give you a blood test to measure estrogen and related hormones, like follicle-stimulating hormone (FSH). You may choose to get tested if you want to know whether you can still get pregnant. Your doctor will test your hormone levels in the first few days of your menstrual cycle (when bleeding begins).
Can you reverse early menopause?
You can’t reverse menopause or make your ovaries function normally again. However, your doctor can help reduce the symptoms and side effects of menopause. In the case of primary ovarian insufficiency (POI), there’s a small possibility you’ll regain ovarian function.
How can I reduce my risk of early menopause?
Most causes of early menopause are beyond your control (see Early menopause causes). Smoking cigarettes is the only lifestyle factor that may cause early menopause. You can reduce your risk of menopause by quitting smoking. The other causes of menopause like health conditions, surgeries or treatment for cancer are unpreventable in most cases.
If I have early menopause, can I still have children?
Women with primary ovarian insufficiency (premature ovarian failure) do sometimes ovulate, and pregnancy can occur naturally, which is why contraception is still recommended for those who do not desire pregnancy. However, the chance of a natural pregnancy is low, occurring in less than 10% of women with primary ovarian insufficiency (premature ovarian failure). For women with primary ovarian insufficiency (premature ovarian failure) who desire children, there is increasing information and testing available about the number of remaining healthy eggs a woman has (her ovarian reserve) and how this relates to her chance of getting pregnant. A referral to a fertility specialist or a reproductive endocrinologist may be beneficial.
It’s possible to get pregnant through in vitro fertilization (IVF) after menopause. You can use eggs from a donor or your own eggs (if you froze your eggs prior to menopause). Any eggs that are left after menopause typically aren’t viable. Surrogacy and adoption are also options.
Can my menstrual periods return if they’ve stopped after having chemotherapy or radiation therapy?
It is possible that your periods may return after your ovaries have had time to recover after one of these therapies. However, the more time that passes without having a period, the less likely you are to have one again.
How do you know if you are starting early menopause?
You may start having irregular menstrual cycles for a few years prior to your last menstrual period. Longer or shorter menstrual cycles, spotting between periods or changes in vaginal bleeding are often some of the first signs of menopause. If you experience irregular periods, speak with a doctor to look into possible causes.
The other signs of premature and early menopause include many of the typical menopause symptoms. You may experience:
- Hot flashes (sudden warmth that spreads over your body).
- Night sweats.
- Vaginal dryness and discomfort during sex.
- Frequent urge to pee.
- More frequent urinary tract infections (UTIs).
- Difficulty sleeping (insomnia).
- Emotional changes (irritability, mood swings, depression or anxiety).
- Dry skin, dry eyes or dry mouth.
- Breast tenderness.
- Racing heart.
- Headaches.
- Joint and muscle aches and pains.
- Changes in your sex drive (libido).
- Difficulty concentrating or being more forgetful.
- Weight gain or weight loss.
- Hair loss or thinning.
Early menopause causes
Many of the causes of premature menopause can also be causes of early menopause. Some causes of early menopause include cancer treatment, surgery or certain health conditions. But, sometimes, the cause is unknown. Anything that damages your ovaries or stops your body from making estrogen can cause menopause.
There are two types of early menopause, primary and secondary. Primary early menopause means that your ovaries do not function normally. This may be because they have been removed by surgery, or it may be caused by some cancer treatments and certain diseases or genetic conditions. In secondary early menopause, the ovaries are normal but there is a problem getting hormone signals to them from your brain. This is usually caused by diseases of the pituitary gland or hypothalamus. Some women with early menopause sometimes have menstrual periods and may be able to have children.
Reasons for early menopause can include:
- Family history. Women with a family history of early or premature menopause are more likely to have early or premature menopause.
- Smoking. Women who smoke may reach menopause as much as two years before nonsmokers. They may also get more severe menopause symptoms 62. Research suggests that women who have early or premature menopause and smoke die about two years earlier than nonsmoking women 63.
- Chemotherapy or pelvic radiation treatments for cancer. These treatments can damage your ovaries and cause your periods to stop forever or just for a while. You also may have trouble getting pregnant or not be able to get pregnant again. However, not all women who have chemotherapy or radiation will go through menopause. The younger a woman is at the time of chemotherapy or radiation, the less likely she is to go through menopause.
- Surgery to remove the ovaries. Surgical removal of both ovaries, called a bilateral oophorectomy, may cause menopausal symptoms right away. Your periods will stop after this surgery, and your hormone levels will drop quickly. You may have strong menopausal symptoms, like hot flashes and less sexual desire.
- Surgery to remove the uterus. Some women who have a hysterectomy, which removes the uterus, can keep their ovaries. If this happens, you will no longer have periods, and you cannot get pregnant. But you will probably not go through menopause right away because your ovaries will continue to make hormones. Later on, you might have natural menopause a year or two earlier than expected.
- Certain health conditions:
- Autoimmune diseases. Autoimmune disorder such as thyroiditis, vitiligo, myasthenia gravis, Addison disease (adrenal insufficiency) and rheumatoid arthritis. Although rare, the body’s immune system, which normally fights off diseases, may mistakenly attack the ovaries and keep them from making hormones.
- HIV and AIDS. Women with HIV whose infection is not well controlled with medicine may experience early menopause 47. Women with HIV may also have more severe hot flashes than women without HIV 48.
- Missing chromosomes. Women born with missing chromosomes or problems with chromosomes can go through menopause early. For example, women with the condition called Turner’s syndrome are born without all or part of one X chromosome, so their ovaries do not form normally at birth and their menstrual cycles, including the time around menopause, may not be normal.
- Chronic fatigue syndrome. Women with myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS) have extreme tiredness, weakness, muscle and joint pain, memory loss, headache, unrefreshing sleep, and other symptoms. Research has found that women with myalgic encephalomyelitis / chronic fatigue syndrome are more likely to have early or early menopause 64.
Induced early menopause
Induced menopause occurs when a medical treatment, such as surgery, chemotherapy, or radiation, removes or seriously damages both ovaries. The reason for the medical treatment may affect whether hormone therapy will be recommended.
- Surgery that removes both ovaries called bilateral oophorectomy: Your ovaries make hormones, including estrogen and progesterone, that control your menstrual cycle. When both ovaries are surgically removed, menopause results. Cancer is a common reason for this surgery. Removing both ovaries may be done to treat ovarian cancer or to help prevent breast and ovarian cancer in women who are considered to be at high risk. You’re likely to have hot flashes and other menopausal symptoms. Symptoms can be severe because the surgery causes hormones to drop all at once rather than slowly over several years.
- Chemotherapy: Chemotherapy is a powerful drug therapy to treat various types of cancer. Chemotherapy may be used along with surgery, radiation therapy, or both. Periods sometimes return after chemotherapy. Then you can still get pregnant. So you might want to keep using birth control.
- Radiation therapy: Radiation therapy uses high-energy particles or waves to damage cancer cells and reduce their size or keep them from growing. Radiation therapy aimed at the pelvis, belly and lower spine can cause menopause. Radiation to the whole body for stem cell transplant also can cause menopause. Radiation therapy to other parts of the body, such as breast tissue or the head and neck, likely won’t affect menopause.
Primary ovarian insufficiency
Primary ovarian insufficiency also called premature ovarian failure is a condition in which younger women skip many periods in a row or have no periods at all. In most cases, the exact cause of primary ovarian insufficiency is unknown 42, 43, 44. Approximately 90% of all diagnosed cases of spontaneous primary ovarian insufficiency do not have a determined underlying cause 49. Research shows that primary ovarian insufficiency is related to problems with the ovarian follicles, the small sacs in the ovaries in which eggs grow and mature 44. Ovarian follicles start out as microscopic seeds called primordial follicles. These seeds are not yet follicles, but they can grow into them. Normally, a woman is born with approximately 2 million primordial follicles 46, typically enough to last until she goes through natural menopause, usually around age 50 43.
For a woman with primary ovarian insufficiency there are problems with the ovarian follicles 65:
- Follicle depletion. A woman with follicle depletion runs out of working follicles earlier than normal or expected. In the case of primary ovarian insufficiency, the woman runs out of working follicles before natural menopause occurs around age 50. Presently there is no safe way for scientists today to make primordial follicles.
- Follicle dysfunction. A woman with follicle dysfunction has follicles remaining in her ovaries, but the follicles are not working properly. Scientists do not have a safe and effective way to make follicles start working normally again 44.
Although the exact cause of primary ovarian insufficiency is unknown in a majority of cases, some causes of follicle depletion and dysfunction have been identified:
- Genetic and chromosomal disorders.
- Starting at the level of the ovary, rare mutations in the genes for follicle-stimulating hormone (FSH) and luteinizing hormone (LH) receptors can alter the ovaries’ response to these circulating gonadotropins leading to nonfunctional ovarian tissue 45, 46, 44.
- Chromosomal abnormalities such as Fragile X syndrome and Turner syndrome can cause accelerated egg (oocyte) depletion early in life 44, 46, 66.
- Genetic mutations and autosomal recessive diseases such as galactosemia (reduction of galactose-1-phosphate), ataxia-telangiectasia (ATM gene), and blepharophimosis-ptosis-epicanthus-inversus syndrome (known as BPES, a mutation in FOXL2) have undefined effects on primary ovarian insufficiency 44, 46, 66.
- Low number of follicles. Some women are born with fewer primordial follicles, so they have a smaller pool of follicles to use throughout their lives. Even though only one mature follicle releases an egg each month, less mature follicles usually develop along with that mature follicle and egg. Scientists don’t understand exactly why this happens, but these “supporting” follicles seem to help the mature follicle function normally. If these extra follicles are missing, the main follicle will not mature and release an egg properly.
- Autoimmune diseases. Typically, the body’s immune cells protect the body from invading bacteria and viruses. However, in autoimmune diseases, immune cells turn on healthy tissue. In the case of primary ovarian insufficiency, the immune system may damage developing follicles in the ovaries. It could also damage the glands that make the hormones needed for the ovaries and follicles to work properly. Several studies suggest that about one-fifth of with primary ovarian insufficiency have an autoimmune disease 43, 67.
- Thyroiditis such as Hashimoto thyroiditis is the autoimmune disorder most commonly associated with primary ovarian insufficiency 67. It is an inflammation of the thyroid gland, which makes hormones that control metabolism, or the pace of body processes.
- Addison’s disease (adrenal insufficiency) is also associated with primary ovarian insufficiency. Addison’s disease affects the adrenal glands, which produce hormones that help the body respond to physical stress, such as illness and injury; the hormones also affect ovary function 68. A small percentage of women with primary ovarian insufficiency have Addison’s disease.
- Rheumatoid arthritis, systemic lupus erythematosus (SLE), type 1 diabetes, nontypical congenital adrenal hyperplasia, myasthenia gravis, and inflammatory bowel disease (Crohn’s disease and ulcerative colitis) have also been associated with primary ovarian insufficiency 44, 45.
- Chemotherapy or radiation therapy. These strong treatments for cancer may damage the genetic material in cells, including follicle cells 42, 44.
- Metabolic disorders. Metabolic disorders affect the body’s ability to create, store, and use the energy it needs. For example, galactosemia affects how your body processes galactose, a type of sugar. A majority of women with galactosemia also have primary ovarian insufficiency 67.
- Women with mumps, chickenpox, malaria, shigella, and tuberculosis (TB) can destroy healthy ovarian tissue and substantially decrease the amount of functioning tissue that remains 43, 45, 46, 44.
- Toxins. Cigarette smoke, chemicals, nicotine, phthalates, polychlorinated biphenyls (PCBs), per- and polyfluoroalkyl substance (PFAS), bisphenol-A (BPA), dimethylbenzanthracene and pesticides can speed up ovarian follicle depletion.
- Viruses have been shown to affect follicle function 46, 43.
A blood test may report a high follicle-stimulating hormone (FSH) level, which can be a sign of menopause and of few eggs left in the ovaries. However, the release of an egg from an ovary (ovulation) may still occur on occasion, which means that pregnancy is still possible.
Some women with primary ovarian insufficiency experience typical menopause symptoms, whereas others do not. If they do experience symptoms, they may be intermittent. Some women resume normal periods at some point, and others do not. There are several known causes of primary ovarian insufficiency, including certain genetic and autoimmune disorders. Unfortunately, much is still unknown about this condition, which makes it difficult to predict what will happen. Women aged younger than 40 years who have missed three or more menstrual periods are advised to see a healthcare professional to determine whether this is caused by primary ovarian insufficiency or whether another reason for absent or irregular menstruation is at play.
Risk factors for early menopause
The main risk factor for early menopause include:
- Surgery to remove both ovaries.
- Certain cancer treatments e.g., chemotherapy, radiation therapy.
- Smoking. Women who smoked at age 16 had 51% higher odds of early menopause, compared to those who did not smoke at this age
- Genetic abnormality (e.g. Turner syndrome or Fragile X syndrome)
- Metabolic disorders
- Viral infection (e.g. mumps).
- Autoimmune diseases such as Addison’s disease, thyroid disease, type 1 diabetes, Crohns’ disease and coeliac disease
Early menopause signs and symptoms
Women who go through menopause early may have symptoms or health problems similar to those of regular menopause. Different people have different menopause symptoms. Some women may have no symptoms, except that menstrual periods become lighter or irregular, or stop (amenorrhea). Women who haven’t had a menstrual period for 12 straight months, and aren’t on any medication that could stop menstruation, may have reached menopause. Other women have infertility or develop the same symptoms that are associated with normal menopause (which occurs at about age 51), such as hot flashes, night sweats, or mood swings.
Most people who go through menopause experience some symptoms include the following:
- Irregular periods. This is one of the first signs of nearing menopause. You may skip periods, or they may occur closer together. Your flow may be lighter or heavier than usual.
- Hot flashes. Hot flashes are the most common symptom of menopause. When you have a hot flash, you’ll feel warm from your chest to your head. These often happen in wave-like sensations. Your skin may turn red, and you may sweat. You may feel sick to your stomach and dizzy. You may also have a headache and feel like your heart is beating very fast and hard.
- Vaginal dryness. During and after menopause, the skin of your vagina and vulva (the area around your vagina) becomes thinner. Your vagina also loses its ability to produce as much lubrication (wetness) during sexual arousal. These changes can lead to pain during sex. You may need to help supplement vaginal moisture to make having sex less painful. You can use an over-the-counter water-based sexual lubricant (such as K-Y Jelly). Or you can use moisturizers for the vaginal area (such as Vagisil). You can also talk to your doctor about the benefits and risks of using prescription estrogen cream for vaginal changes. Topical estrogens are absorbed into the bloodstream and cause many of the same side effects as when they are taken by mouth. Estrogens used vaginally at very low doses will not protect against osteoporosis or stop the hot flashes caused by menopause. They can interact with other medicines and conditions.
- Urinary tract problems. You’re more likely to have bladder and urinary tract infections during and after menopause. Talk to your doctor if you have to go to the bathroom more often or feel an urgent need to urinate. Also let your doctor know if you feel a burning sensation when urinating or are not able to urinate.
- Headaches, night sweats, trouble sleeping, and tiredness. As you’re going through menopause, you may have trouble falling asleep or staying asleep. Night sweats may wake you up. You may not get enough rapid eye movement (REM) sleep (the stage of sleep during which you dream). A lack of REM sleep may make you feel tired, moody, and stressed out.
- Mood swings or be irritable. Many people experience emotional symptoms during menopause. These symptoms may include sadness, anxiety, and mood swings. For some people, symptoms can be severe. If you find that you’re having emotional problems, talk to your family doctor.
- Trouble finding words and remembering, often called brain fog.
- Weight gain. Many people gain weight (an average of 5 pounds) during menopause. A healthy diet and exercising most, if not all, days of the week will help keep you fit.
Women may have symptoms of the disorder that caused early menopause. For example, if Turner syndrome is the cause, they may have physical or cognitive abnormalities.
If early menopause is caused by an autoimmune process, women may also have other autoimmune disorders such as thyroiditis, vitiligo, myasthenia gravis, and Addison disease (adrenal insufficiency). Addison disease can be life threatening (Addisonian crisis).
The lack of estrogen may lead to thinning and drying of the lining of the vagina (vaginal atrophy). The risk of other conditions such as depression, anxiety, Parkinson disease, dementia, and coronary artery disease, may be increased.
Some women with early menopause may also have:
- Higher risk of serious health problems. For example, you might begin to lose bone density because you have less estrogen. This can lead to osteoporosis, a condition that causes bones to become weak and break easily. Changing estrogen levels can also raise your cholesterol levels and increase your risk for heart disease and stroke. Talk to your doctor about steps to lower your risk for these health problems.
- More severe menopause symptoms. Talk to your doctor about treatments to help with symptoms if they affect your daily life.
- Sadness or depression over the early loss of fertility or the change in their bodies. Talk to your doctor if you have symptoms of depression, including less energy or a lack of interest in things you once enjoyed that lasts longer than a few weeks. Your doctor can recommend specialists who can help you deal with your feelings. Your doctor can also discuss options, such as adoption or donor egg programs, if you want to have children.
Early menopause complications
Unless women with early menopause receive estrogen therapy until about age 51 (the average age for menopause), the risk of osteoporosis, dementia, Parkinson disease, depression, and coronary artery disease is increased 69, 32, 32, 70, 71, 72, 73, 74.
- Heart and blood vessel disease. This also is called cardiovascular disease. When your estrogen levels fall, your risk of cardiovascular disease increases. Heart disease is the leading cause of death in both women and men.
- Weakened bones called osteoporosis. This condition causes bones to become brittle and weak, leading to a greater risk of breaking bones. During the first few years after menopause, you may lose bone density quickly. This ups your risk of osteoporosis. Bones often broken after menopause include the spine, hips and wrists.
- Loss of bladder control called urinary incontinence. As the tissues of your vagina and urethra change, you may have sudden, strong urges to urinate often. Then you might lose urine, called urge incontinence. Or you might lose urine with coughing, laughing or lifting, called stress incontinence. You may have urinary tract infections more often.
- Sex problems. Menopause causes the vagina to get drier and lose its stretch. This can cause discomfort and slight bleeding during sexual intercourse. Also, less feeling in the area may lessen your desire for sex, called libido.
- Weight gain. Many women gain weight during and after menopause because calorie burning, called metabolism, slows.
If early menopause is caused by an autoimmune disorder, women are at risk of potentially life-threatening primary adrenal insufficiency (Addison disease).
Bone loss and fracture
Women with primary ovarian insufficiency-related estrogen deficiency are at risk of osteopenia, osteoporosis, and fracture, especially if estrogen deficiency (hypoestrogenism) occurs early in life and before accrual of peak bone mass 75, 76, 29, 77. A number of large, well-designed prospective studies have provided strong evidence that early age at menopause, especially when occurring at 45 years or younger, is associated with a risk of fracture that is 1.5 to 3 fold higher than the risk for women who experience menopause after age 50 years 29, 78, 79, 80, 81. In a study of more than 1,000 patients, the incidence of hip fracture in women starting menopause at age 40 years was 9.4% compared with 3.3% in those starting menopause at age 48 years 78. In the Rotterdam study, a prospective population-based cohort study that evaluated risk factors for incident fractures among 3,000 men and women, vertebral fracture was 2.5 times more likely to occur in women who experienced menopause before age 45 years compared with those who experienced menopause after age 50 years 81. In studies that have evaluated the role of hormone replacement therapy (HRT) in women at increased risk of fracture based on menopausal age, significant reductions in fracture risk have been described 29, 80, 81.
Other risk factors for low bone mass in women with primary ovarian insufficiency include delay in primary ovarian insufficiency diagnosis of 1 year or more, vitamin D deficiency, nonadherence to prescribed hormone replacement therapy (HRT), sedentary lifestyle, and lack of calcium supplementation 77. Dual-energy X-ray absorptiometry (DEXA scan) has been recommended for the evaluation of bone mineral density in women diagnosed with primary ovarian insufficiency, but consensus regarding the frequency of interval surveillance is lacking, especially in adolescent girls 43, 75, 82. In contrast to the treatment of postmenopausal osteopenia or osteoporosis, which focuses on bisphosphonates as first-line therapy, low bone mass in women with primary ovarian insufficiency is managed most appropriately with hormone replacement therapy (HRT) 83. Given the extremely long half-life of bisphosphonates, there is concern regarding the safety of this class of drugs in young women with primary ovarian insufficiency, who could spontaneously become pregnant or pursue donor egg in vitro fertilization (IVF) to achieve a pregnancy 84. To date, long-term use of bisphosphonates is not recommended in the adolescent girl population because of uncertain adverse effects and safety profiles 75.
Cardiovascular disease
Postmenopausal women have less favorable lipid profiles compared with premenopausal women and the risk of metabolic syndrome has been shown to increase after menopausal transition 85, 86. Women who develop primary ovarian insufficiency are also at increased risk of cardiovascular events and cardiovascular mortality compared with women who do not experience early menopause 87, 88, 89. In a 20-year follow-up of a 12,000-woman cohort study conducted in the Netherlands, cardiovascular mortality decreased by 2% for every year that menopause was delayed after age 39 years 89. In a subsequent prospective cohort study that monitored more than 6,000 U.S. women for 12 years, patients who reported experiencing menopause between the ages of 35 years and 40 years at study entry had a 50% greater subsequent risk of ischemic heart disease-related death (risk adjusted for diabetes, hypertension, parity, age at first birth, and physical activity) compared with those who experienced menopause between the ages of 49 years and 51 years 87. The association between primary ovarian insufficiency and cardiovascular disease risk may be explained in part by metabolic and endothelial changes that occur with estrogen deprivation. A cohort study observed significant endothelial dysfunction in women with primary ovarian insufficiency compared with age- and body mass index-matched women, demonstrated by diminished flow-mediated brachial artery diameter. After 6 months of hormone replacement therapy (HRT), the brachial artery diameters of women with primary ovarian insufficiency were comparable with those of the control group 90. In this study and others, hormone replacement therapy (HRT) has been shown to improve endothelial dysfunction and reduce intima media thickness 91, blood pressure, plasma angiotensin, and creatinine 92. Primary ovarian insufficiency also may be related to cardiovascular disease risk and death as an indicator of overall aging and age-related illness 93, 94.
Epidemiologic evidence supporting the use of hormone replacement therapy (HRT) to prevent cardiovascular events in women with primary ovarian insufficiency is currently lacking. However, there also are no data that indicate that women with primary ovarian insufficiency who are treated with hormone replacement therapy (HRT) experience an increased risk of cardiovascular adverse effects compared with unaffected women using hormone replacement therapy (HRT) or combination hormonal contraceptives (daily combined estrogen–progestin in the form of combination oral birth control pills, the contraceptive ring, or transdermal patches) 75, 67.
Vasomotor symptoms
Women with primary ovarian insufficiency may experience hot flushes, night sweats, vaginal dryness, dyspareunia, and disordered sleep; some symptoms may develop before cycle irregularity 43. These symptoms routinely respond well to hormone replacement therapy (HRT) as indicated. Some women may be asymptomatic; younger women in particular may not exhibit symptoms.
Evidence regarding cognitive decline in women with primary ovarian insufficiency is limited and mixed. A cohort study reported that young (defined as younger than 43 years) surgically menopausal women who were not receiving hormone replacement therapy (HRT) demonstrated signs of cognitive impairment compared with controls 95. These findings contrast with other reports that suggest preserved cognitive function in women with primary ovarian insufficiency who have intact ovaries 96.
Primary ovarian insufficiency has been referred to as “the silent grief” because of the negative self-image and isolation that can develop once a diagnosis is confirmed 97. Women with primary ovarian insufficiency who were surveyed about their diagnosis report significant levels of grief, diminished self-esteem, sadness, and limited access to psychological support to address these feelings 97, 75, 98, 99, 100, 101. Poor psychosocial functioning is explained, in small part, by vasomotor symptoms in this population 102. The emotional response to a diagnosis of primary ovarian insufficiency may be more complex and challenging in the adolescent population than for adults. Support from family or mental health professionals is important to facilitate the understanding and acceptance of the diagnosis 102, 43, 75.
Emotional wellbeing
Women who experience early menopause can be at greater risk of depression, anxiety and mood changes. If you experience menopause in your 20s or 30s, it can be very upsetting. It’s normal to feel a sense of loss, sadness and grief. You may also have mixed feelings about your body image, fertility, femininity and sexuality.
There are lots of things you can do to look after yourself during this difficult time. If you feel very emotional, anxious or depressed after your diagnosis, it’s important to talk to someone. You can do counselling or join a support group. Your doctor can help with symptom relief and refer you to a psychologist if needed.
Sex and relationships
After a diagnosis of early menopause, physical and emotional changes may reduce your desire to be intimate with your partner. It can be distressing to have hot flushes and sweats at a young age. You might also feel conscious of physical changes, like vaginal dryness, which can cause pain during sex and result in a reduced sex drive (libido).
Depending on your stage of life and family plans, this diagnosis may change your plans and affect your relationship.
It’s important to seek support from people close to you. If you have a partner, they might not know about menopause symptoms or what you are going through. You can suggest going to your gynaecologist or doctor’s appointments together or seek counselling if required.
Early menopause diagnosis
If you believe you are going through early menopause and have concerns, see your doctor. Doctors suspect early menopause when a woman younger than 45 of years of age has menopausal symptoms, or few or no periods, or cannot become pregnant (infertile). Your doctor may order a blood test to check your hormone levels.
If a woman is younger than age 40 and begins having irregular periods or stops having periods for 4 months or longer, her doctor may take these steps to diagnose the problem 103, 104, 105:
- Do a physical exam. During the physical exam, your doctor looks for signs of other disorders. In some cases, the presence of these other disorders will rule out primary ovarian insufficiency. Or, if the other disorders are associated with primary ovarian insufficiency, such as Addison’s disease. If on the physical exam there is evidence of high levels of androgens (male sex hormones e.g., testosterone, androsterone and androstenedione in women), such as hirsutism, acne, enlarged clitoris (clitoromegaly), or male pattern baldness, then it would be appropriate to evaluate the levels of 17-hydroxyprogesterone (21-hydroxylase antibodies), testosterone, and DHEA-S 106. The aforementioned laboratory work would help to include or exclude the diagnosis of thyroid dysfunction (hypo- or hyperthyroidism) versus prolactinoma versus polycystic ovarian syndrome (PCOS) versus nontypical congenital adrenal hyperplasia that could be the cause of the patient’s secondary amenorrhea.
- Do a pregnancy test. This test will rule out an unexpected pregnancy as the reason for missed periods.
- Measurement of hormone levels
- Follicle-stimulating hormone (FSH) and estrogen (estradiol). Follicle-stimulating hormone (FSH) signals the ovaries to make estrogen, sometimes called the “female hormone” because women need high levels of it for fertility and overall health. If your ovaries are not working properly, as is the case in early menopause, the level of follicle-stimulating hormone (FSH) in your blood increases and estrogen goes down. Your doctor may do two FSH tests, at least a month apart. If the FSH level in both tests is as high as it is in women who have gone through menopause, then early menopause is likely.
- Luteinizing hormone (LH). Luteinizing hormone (LH) signals a mature follicle to release an egg. Women with primary ovarian insufficiency have high luteinizing hormone (LH) levels, more evidence that the follicles are not functioning normally 65.
- Thyroid-stimulating hormone (TSH). Overactive thyroid, called hyperthyroidism, can cause symptoms like those of menopause.
- Antimullerian hormone (AMH) can be obtained and is used as a marker for ovarian reserve, but is not part of the diagnostic criteria for primary ovarian insufficiency 45. A blood test for antimüllerian hormone (AMH) can be done to evaluate how well the ovaries are functioning and to estimate the chances that a woman will be able to become pregnant after treatment with fertility medications. Normal antimüllerian hormone (AMH) levels are between 1.5 and 4.0 ng/mL. Most women diagnosed with primary ovarian insufficiency have antimüllerian hormone (AMH) levels less than 1 ng/mL 106. A very low antimüllerian hormone (AMH) level suggests decreased ovarian reserve. Reproductive endocrinologists use antimüllerian hormone (AMH) levels to help predict which women may respond poorly to fertility medications and generally which couples are less likely to be successful with fertility treatment. Antimüllerian hormone (AMH) can be drawn at any time during the menstrual cycle. Newer, more sensitive antimüllerian hormone tests may help clinicians diagnose early menopause.
- Genetic counseling and testing for the FMR1 premutation (Fragile X mutation) are indicated if women have a family history of primary ovarian insufficiency or have intellectual disability, tremor, or loss of balance (ataxia) or have a close relative with early menopause or if they are younger than 35.
- Karyotype test. This test looks at all 46 of your chromosomes to check for abnormalities. The karyotype test could reveal genetic changes in the structure of chromosomes that might be associated with primary ovarian insufficiency and other health problems 43, 65.
- Pelvic ultrasound. In this test, your doctor uses a sound wave (sonogram) machine to create and view pictures of the inside of a woman’s pelvic area. A sonogram can show whether or not the ovaries are enlarged or have multiple follicles 42, 43.
Autoimmune disorders such as systemic lupus erythematosus (SLE), rheumatoid arthritis, myasthenia gravis, Hashimoto thyroiditis (thyroid peroxidase autoantibodies and antithyroglobulin antibodies), and diabetes mellitus should also be considered 45. If doctors suspect a woman also has Hashimoto thyroiditis (an autoimmune disorder), they measure thyroid hormone levels in the blood such as thyroid-stimulating hormone (TSH), thyroxine (T4), and antithyroid–peroxidase and antithyroglobulin antibodies. If adrenal insufficiency is suspected, measurement of a morning cortisol level or an adrenocorticotropic hormone (ACTH) stimulation test can confirm the diagnosis.
Other tests for an autoimmune dysfunction should be done; they include a complete blood count with differential, erythrocyte sedimentation rate (ESR), and measurement of antinuclear antibody and rheumatoid factor.
Bone density may be measured to check for osteoporosis if women have symptoms or signs of estrogen deficiency.
Early menopause treatment
If a woman with early menopause does not wish to become pregnant, she is given one of the following:
- Birth control pills or a patch that contains estrogen and a progestin (combination oral contraceptives)
- Menopausal hormone therapy (MHT) also called hormone replacement therapy (HRT) that contains both estrogen and a progestin (a synthetic form of the female hormone progesterone) or progesterone. In women with primary ovarian insufficiency, systemic hormone replacement therapy (HRT) is an effective approach to treat the symptoms of hypoestrogenism and reduce long-term health risks if there are no contraindications to treatment. Hormone replacement therapy (HRT) is indicated to reduce the risk of osteoporosis, cardiovascular disease, and urogenital atrophy and to improve the quality of life of women with primary ovarian insufficiency. The results from the Women’s Health Initiative trials related to menopause therapy are not applicable to young women with primary ovarian insufficiency whose exposure to physiologic estrogen has been withdrawn prematurely. When hormone replacement therapy (HRT) is withheld from women with primary ovarian insufficiency because of extrapolation of good epidemiologic evidence from the wrong population, those women may experience many negative health consequences.
These treatments are typically taken until about age 51 (the average age for menopause). Then, doctors decide whether to continue the treatments based on a woman’s individual circumstances.
Estrogen therapy helps relieve symptoms and helps prevent other effects of menopause (such as vaginal dryness, and mood swings). It also helps maintain bone density (to prevent osteoporosis). Because taking estrogen alone increases the risk of cancer of the uterine lining (endometrial cancer), most women should also take a progestin or progesterone with the estrogen to help protect against this cancer. Women who have had a hysterectomy (removal of the uterus) do not need to take a progestin or progesterone.
If a woman with early menopause wishes to become pregnant, doctors may recommend in vitro fertilization (IVF) using another woman’s eggs (donor eggs). These eggs are implanted in the uterus after they have been fertilized in the laboratory. This technique gives women with early menopause about a 50% chance (sometimes even higher) of becoming pregnant. Otherwise about 5 to 10% of women with primary ovarian insufficiency eventually become pregnant on their own, without fertility treatments. No treatment has been proved to increase the ovulation rate or restore fertility in women with primary ovarian insufficiency.
Other options for women who desire pregnancy include cryopreservation of ovarian tissue, oocytes, or embryos and embryo donation. These techniques may be used before or during ovarian failure, especially in cancer patients. Neonatal and adult ovaries possess a small number of oogonial stem cells that can stably proliferate for months and produce mature oocytes in vitro; these cells may be used to develop infertility treatments in the future. Ovarian tissue transplantation has been successful and, in the future, may become an option for women who are no longer fertile 107.
Unless contraindicated, hormonal therapy or estrogen/progestin contraceptives are recommended rather than other bone-specific treatments (eg, bisphosphonates) to prevent bone loss in women with premature ovarian insufficiency; these treatments are given until women reach the average age for menopause (about age 51), when treatment may be reassessed.
To help prevent osteoporosis, women with primary ovarian insufficiency should consume an adequate amount of calcium and vitamin D (in the diet and/or as supplements).
Women with a Y chromosome require bilateral oophorectomy via laparotomy or laparoscopy because risk of ovarian germ cell cancer is increased 105.
Hormone replacement therapy (HRT)
Hormone replacement therapy (HRT) is the most common form of prescribed treatment for menopausal symptoms. Hormone replacement therapy (HRT) helps to replace the hormone estrogen in your body, which decreases around your menopause. You may sometimes also need other hormones such as progesterone and testosterone that your body is no longer producing. Hormone replacement therapy (HRT) may reduce associated menopause symptoms, bone mineral density loss, and cardiovascular risk and should be continued until the age of natural menopause (50 to 51 years) 50, 108, 109, 51, 52, 110. If you are interested in taking hormone replacement therapy (HRT), your doctor should discuss the benefits and risks with you before you start the treatment. This discussion should cover both the short-term (over the next 5 years) and the longer term (beyond the next 5 years) benefits and risks for you. You should also be informed about available alternatives to hormone replacement therapy (HRT) along with their benefits and risks.
Unopposed estrogen replacement therapy is an important risk factor for endometrial hyperplasia (10–50% incidence per year) and endometrial cancer (up to a 10-fold increase in absolute risk) and, therefore, is not recommended 111, 112, 113, 114, 115, 116. The addition of progesterone therapy to estrogen replacement significantly reduces the risk; current combined hormone replacement therapy (HRT) regimens are not associated with an increased risk of endometrial hyperplasia or cancer 111, 117, 118. The current hormone replacement therapy (HRT) regimens add continuous or sequential progestogen therapy to estrogen replacement 119, 120.
Professional organizations including the North American Menopause Society, the British Menopause Society, and the International Menopause Society recommend estrogen replacement therapy for women with early menopause or premature ovarian failure 121, 122, 123. There is some evidence, although not from randomized controlled clinical trials, that restoring pathologically low estrogen levels will reduce the later development of cardiovascular disease, osteoporosis, and possibly dementia. This leads to the general recommendation that estrogen be continued in women who experience premature menopause or early menopause until at least around the median age of natural menopause (approximately age 51 years) 6.
Data are insufficient to evaluate the association between hormone replacement therapy (HRT) or combined hormonal birth control pills administered to women with primary ovarian insufficiency and the risk of developing breast cancer 83. Although a number of epidemiologic studies have examined the association between hormone replacement therapy (HRT) in women who are naturally menopausal at midlife and breast cancer risk, demonstrating a 20–30% increased risk of breast cancer in these postmenopausal hormone replacement therapy (HRT) users 111, 124, these data are not generalizable to women with primary ovarian insufficiency 83. Women with primary ovarian insufficiency are much younger at the time of hormone replacement therapy (HRT) initiation and their baseline risk of breast cancer is significantly lower compared with women to whom hormone replacement therapy (HRT) is administered after natural menopause 83. Short-term exposure to hormone replacement therapy (HRT) in BRCA1 and BRCA2 gene carriers following risk-reducing bilateral salpingo-oophorectomy has not been associated with an increased risk of developing breast cancer 125. Like women with primary ovarian insufficiency, these women are young and require physiologic replacement of hormones. Although reassuring, these data are not a substitute for epidemiologic studies that specifically evaluate the risk of breast cancer in women with primary ovarian insufficiency who are treated with long-term hormone replacement therapy (HRT) 83.
Multiple epidemiologic studies have tested the association between combined hormonal birth control pills use in the general population and risk of breast cancer. Overall, the evidence suggests that women who use or have a history of using combined hormonal contraceptives are not at increased risk of breast cancer 126, 127, 128, 129, 130, 131, 132, 133, 134, 135. Although this is reassuring, an even more important question for women with primary ovarian insufficiency is whether long-term use of combined hormonal birth control pills beginning at a relatively young age is associated with breast cancer risk 83. Data regarding risk of breast cancer for long-term users are mixed 83. In a systemic review of 15 publications addressing this question, five demonstrated an association between oral birth control pill use of at least 5–10 years and breast cancer, whereas the remaining 10 demonstrated no such association 126. Meta-analyses have demonstrated no association between long-term oral birth control pill use and breast cancer risk when pooling estimates of multiple studies 127, 128. More specifically, studies on the association between long-term combined hormonal birth control pill use initiated by nulliparous women younger than 30–45 years and breast cancer risk have yielded mixed results 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139; some of the highest-quality population-based case-control studies showed no association 131, 132. Data specifically evaluating the use of combined hormonal contraceptives in women with primary ovarian insufficiency are lacking, so care should be individualized to the needs of each patient 83. Women and gynecologists and other health care providers should engage in shared decision making to make the best treatment decision after a discussion of risks and benefits of combined hormonal birth control pill use 83.
A common post-pubertal hormone replacement therapy (HRT) regimen is 100 mcg of daily transdermal estradiol or 0.625 mg of daily oral conjugated estrogens, adding 200 mg of micronized oral progesterone daily for 12 days each month 50, 51, 52. Transdermal estrogen may be associated with lower blood clot (venous thromboembolism) risk than oral formulations 53. It is also reasonable to recommend 1,200 mg of calcium daily and 1,000 IU of vitamin D daily with regular weight-bearing exercises to maintain bone mineral density in accordance with guidelines for postmenopausal women 54, 43.
Hormone replacement therapy (HRT) options
Although exogenous estrogen replacement is recommended for women with primary ovarian insufficiency, data comparing various hormonal regimens for disease prevention, symptom reduction, and safety are lacking in this population 83. As a first-line approach, hormone replacement therapy (HRT) either orally or transdermally that achieves replacement levels of estrogen is recommended 119, 43, 75. However, serum estradiol level testing is not recommended to monitor the effects of treatment 83. Estrogen replacement can be achieved with the following estradiol preparations: 1–2 mg oral 17β-estradiol daily, 100 micrograms transdermal 17β-estradiol daily, or conjugated equine estrogens 0.625–1.25 mg daily (see Table 1 below) 43, 119, 140. The choice of estrogen therapy should be combined with appropriately dosed progestogen therapy (administered continuously or sequentially) to prevent endometrial hyperplasia and cancer. In contrast with continuous progestogen therapy, cyclic administration allows for earlier recognition of a pregnancy. Women with primary ovarian insufficiency may spontaneously ovulate on an infrequent basis, and the absence of a withdrawal bleed should prompt the patient to test for pregnancy 83.
Another common approach is the use of combined hormonal birth control pills, which may allow for ease of administration and less patient stigma compared with a hormone replacement therapy (HRT) regimen 83. However, the dose of estrogen and progestin in combined hormonal birth control pills is not replacement dosage; these hormonal preparations are significantly more potent than the hormone replacement therapy (HRT) options 119. To date, no well-powered randomized trials exist comparing hormone replacement therapy (HRT) with combined hormonal birth control pills in women with primary ovarian insufficiency to determine cardiovascular risk (either coronary artery disease prevention or risk of venous thromboembolism), quality-of-life measures (eg, vasomotor symptoms, bleeding profile, sexual dysfunction, patient satisfaction), or bone health 83. Because the replacement doses of estrogen provided in hormone replacement therapy (HRT) are less potent than the estrogen in combined hormonal birth control pills, hormone replacement therapy (HRT) may have a lower risk of blood clot (venous thromboembolism). To further reduce the risk of venous thromboembolism with hormone replacement therapy (HRT), some experts recommend treatment by the transdermal route, eliminating the “first-pass” effect on the liver 53, 141.
Combined hormonal birth control pills prevent ovulation and pregnancy more reliably than hormone replacement therapy (HRT); despite only modest odds of spontaneous pregnancy in women with primary ovarian insufficiency, this is a critical consideration for those who deem pregnancy prevention a priority 83. For a woman who prefers noncontraceptive estrogen replacement and wants highly effective contraception, insertion of a levonorgestrel intrauterine device (IUD) is preferable to oral progestin therapy 116, 142. Barrier methods of contraception also may be used. Treatment for all women with primary ovarian insufficiency should continue until the average age of natural menopause is reached (age 50–51 years) 46. Treatment may continue past age 50–51 years if a woman has clinical symptoms or indications 83. Regardless of age, the decision to continue hormone replacement therapy (HRT) should be individualized and based on a woman’s symptoms and the risk–benefit ratio 83.
Table 1. HRT for premature ovarian failure
Table 2. HRT contraindications
| CONTRAINDICATIONS | |
|---|---|
| Absolute | Relative |
| Hormone-related cancer or active liver disease | Chronic liver disease |
| History of hormone-induced thromboembolism | Severe hypertriglyceridemia |
| History of pulmonary embolism not caused by trauma | Endometriosis |
| Vaginal bleeding of unknown etiology | History of endometrial cancer |
| Pregnancy | History of breast cancer Proven coronary heart disease or recent event |
- Gold EB, et al. Factors related to age at natural menopause: Longitudinal analyses from SWAN. Am. J. Epidemiol. 2013;178:70–83. doi: 10.1093/aje/kws421[↩]
- Pelosi E, Simonsick E, Forabosco A, Garcia-Ortiz JE, Schlessinger D. Dynamics of the ovarian reserve and impact of genetic and epidemiological factors on age of menopause. Biol Reprod. 2015 May;92(5):130. doi: 10.1095/biolreprod.114.127381[↩]
- Vogel B, et al. The Lancet women and cardiovascular disease commission: Reducing the global burden by 2030. Lancet. 2021;397(10292):2385–2438. doi: 10.1016/S0140-6736(21)00684-X[↩]
- Crandall CJ, Barrett-Connor E. Endogenous sex steroid levels and cardiovascular disease in relation to the menopause: A systematic review. Endocrinol. Metab. Clin. North Am. 2013;42:227–253. doi: 10.1016/j.ecl.2013.02.003[↩]
- North American Menopause Society. Menopause Practice: A Clinician’s Guide. 3rd ed. Cleveland, OH: North American Menopause Society; 2007.[↩][↩]
- Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. Premature menopause or early menopause: long-term health consequences. Maturitas. 2010 Feb;65(2):161-6. doi: 10.1016/j.maturitas.2009.08.003[↩][↩][↩][↩][↩]
- Warren MP, Shu AR, Dominguez JE. Menopause and Hormone Replacement. [Updated 2015 Feb 25]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279050[↩]
- Jacobsen BK, Heuch I, Kvåle G. Age at natural menopause and all-cause mortality: a 37-year follow-up of 19,731 Norwegian women. Am J Epidemiol. 2003 May 15;157(10):923-9. doi: 10.1093/aje/kwg066[↩]
- Broekmans FJ, Soules MR, Fauser BC. Ovarian aging: mechanisms and clinical consequences. Endocr Rev. 2009 Aug;30(5):465-93. doi: 10.1210/er.2009-0006[↩]
- Aydin ZD, Erbas B, Karakus N, Aydin O, K-Ozkan S. Sun exposure and age at natural menopause: a cross-sectional study in Turkish women. Maturitas. 2005 Nov-Dec;52(3-4):235-48. doi: 10.1016/j.maturitas.2005.02.023[↩]
- Ortega-Ceballos PA, Morán C, Blanco-Muñoz J, Yunes-Díaz E, Castañeda-Iñiguez MS, Salmerón J. Reproductive and lifestyle factors associated with early menopause in Mexican women. Salud Publica Mex. 2006 Jul-Aug;48(4):300-7. doi: 10.1590/s0036-36342006000400004[↩]
- Gold EB, Crawford SL, Avis NE, Crandall CJ, Matthews KA, Waetjen LE, Lee JS, Thurston R, Vuga M, Harlow SD. Factors related to age at natural menopause: longitudinal analyses from SWAN. Am J Epidemiol. 2013 Jul 1;178(1):70-83. doi: 10.1093/aje/kws421[↩]
- Greendale GA, Hogan P, Kritz-Silverstein D, et al. Age at menopause in women participating in the Postmenopausal Estrogen/Progestins Interventions (PEPI) trial: an example of bias introduced by selection criteria. Menopause. 1995;2(1):27–34.[↩]
- Torgerson DJ, Avenell A, Russell IT, Reid DM. Factors associated with onset of menopause in women aged 45-49. Maturitas. 1994 Aug;19(2):83-92. doi: 10.1016/0378-5122(94)90057-4[↩]
- Reynolds RF, Obermeyer CM. Age at natural menopause in Spain and the United States: results from the DAMES project. Am J Hum Biol. 2005 May-Jun;17(3):331-40. doi: 10.1002/ajhb.20121[↩]
- Kinney A, Kline J, Levin B. Alcohol, caffeine and smoking in relation to age at menopause. Maturitas. 2006 Apr 20;54(1):27-38. doi: 10.1016/j.maturitas.2005.10.001[↩]
- Emaus A, Dieli-Conwright C, Xu X, Lacey JV Jr, Ingles SA, Reynolds P, Bernstein L, Henderson KD. Increased long-term recreational physical activity is associated with older age at natural menopause among heavy smokers: the California Teachers Study. Menopause. 2013 Mar;20(3):282-90. doi: 10.1097/GME.0b013e31826ce3d4[↩]
- Nagata C, Wada K, Nakamura K, Tamai Y, Tsuji M, Shimizu H. Associations of physical activity and diet with the onset of menopause in Japanese women. Menopause. 2012 Jan;19(1):75-81. doi: 10.1097/gme.0b013e3182243737[↩]
- Dorjgochoo T, Kallianpur A, Gao YT, Cai H, Yang G, Li H, Zheng W, Shu XO. Dietary and lifestyle predictors of age at natural menopause and reproductive span in the Shanghai Women’s Health Study. Menopause. 2008 Sep-Oct;15(5):924-33. doi: 10.1097/gme.0b013e3181786adc[↩]
- Nagata C, Takatsuka N, Inaba S, Kawakami N, Shimizu H. Association of diet and other lifestyle with onset of menopause in Japanese women. Maturitas. 1998 Jun 3;29(2):105-13. doi: 10.1016/s0378-5122(98)00012-7[↩]
- Parazzini F; Progetto Menopausa Italia Study Group. Determinants of age at menopause in women attending menopause clinics in Italy. Maturitas. 2007 Mar 20;56(3):280-7. doi: 10.1016/j.maturitas.2006.09.003[↩]
- van Noord PA, Dubas JS, Dorland M, Boersma H, te Velde E. Age at natural menopause in a population-based screening cohort: the role of menarche, fecundity, and lifestyle factors. Fertil Steril. 1997 Jul;68(1):95-102. doi: 10.1016/s0015-0282(97)81482-3[↩]
- Evans EM, Racette SB. Menopause and risk for obesity: how important is physical activity? J Womens Health (Larchmt). 2006 Mar;15(2):211-3. doi: 10.1089/jwh.2006.15.211[↩]
- Dratva J, Zemp E, Staedele P, Schindler C, Constanza MC, Gerbase M, Probst-Hensch N, Rochat T, Ackermann-Liebrich U; SAPALDIA-Team. Variability of reproductive history across the Swiss SAPALDIA cohort–patterns and main determinants. Ann Hum Biol. 2007 Jul-Aug;34(4):437-53. doi: 10.1080/03014460701365821. Erratum in: Ann Hum Biol. 2008 Mar-Apr;35(2):256-7. Constanza, Michael [corrected to Constanza, Michael C].[↩]
- Szegda KL, Whitcomb BW, Purdue-Smithe AC, Boutot ME, Manson JE, Hankinson SE, Rosner BA, Bertone-Johnson ER. Adult adiposity and risk of early menopause. Hum Reprod. 2017 Dec 1;32(12):2522-2531. doi: 10.1093/humrep/dex304[↩]
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483-91. doi: 10.3109/13697137.2015.1020484[↩]
- Lepine LA, Hillis SD, Marchbanks PA, Koonin LM, Morrow B, Kieke BA, Wilcox LS. Hysterectomy surveillance–United States, 1980-1993. MMWR CDC Surveill Summ. 1997 Aug 8;46(4):1-15. https://www.cdc.gov/mmwr/preview/mmwrhtml/00048898.htm[↩]
- Minton SE, Munster PN. Chemotherapy-induced amenorrhea and fertility in women undergoing adjuvant treatment for breast cancer. Cancer Control. 2002 Nov-Dec;9(6):466-72. doi: 10.1177/107327480200900603[↩]
- Gallagher JC. Effect of early menopause on bone mineral density and fractures. Menopause. 2007 May-Jun;14(3 Pt 2):567-71. doi: 10.1097/gme.0b013e31804c793d[↩][↩][↩][↩]
- Chen WY, Manson JE. Premature ovarian failure in cancer survivors: new insights, looming concerns. J Natl Cancer Inst. 2006 Jul 5;98(13):880-1. doi: 10.1093/jnci/djj276[↩]
- Ganz PA. Breast cancer, menopause, and long-term survivorship: critical issues for the 21st century. Am J Med. 2005 Dec 19;118 Suppl 12B:136-41. doi: 10.1016/j.amjmed.2005.09.047[↩]
- Wellons M, Ouyang P, Schreiner PJ, Herrington DM, Vaidya D. Early menopause predicts future coronary heart disease and stroke: the Multi-Ethnic Study of Atherosclerosis. Menopause. 2012 Oct;19(10):1081-7. doi: 10.1097/gme.0b013e3182517bd0[↩][↩][↩]
- Honigberg MC, Zekavat SM, Niroula A, Griffin GK, Bick AG, Pirruccello JP, Nakao T, Whitsel EA, Farland LV, Laurie C, Kooperberg C, Manson JE, Gabriel S, Libby P, Reiner AP, Ebert BL; NHLBI Trans-Omics for Precision Medicine Program; Natarajan P. Premature Menopause, Clonal Hematopoiesis, and Coronary Artery Disease in Postmenopausal Women. Circulation. 2021 Feb 2;143(5):410-423. doi: 10.1161/CIRCULATIONAHA.120.051775[↩]
- Buijs C, de Vries EG, Mourits MJ, Willemse PH. The influence of endocrine treatments for breast cancer on health-related quality of life. Cancer Treat Rev. 2008 Nov;34(7):640-55. doi: 10.1016/j.ctrv.2008.04.001[↩]
- Rocca WA, Grossardt BR, de Andrade M, Malkasian GD, Melton LJ 3rd. Survival patterns after oophorectomy in premenopausal women: a population-based cohort study. Lancet Oncol. 2006 Oct;7(10):821-8. doi: 10.1016/S1470-2045(06)70869-5[↩]
- Rivera CM, Grossardt BR, Rhodes DJ, Brown RD Jr, Roger VL, Melton LJ 3rd, Rocca WA. Increased cardiovascular mortality after early bilateral oophorectomy. Menopause. 2009 Jan-Feb;16(1):15-23. doi: 10.1097/gme.0b013e31818888f7[↩]
- Rocca WA, Shuster LT, Grossardt BR, Maraganore DM, Gostout BS, Geda YE, Melton LJ 3rd. Long-term effects of bilateral oophorectomy on brain aging: unanswered questions from the Mayo Clinic Cohort Study of Oophorectomy and Aging. Womens Health (Lond). 2009 Jan;5(1):39-48. doi: 10.2217/17455057.5.1.39[↩]
- Farrag AK, Khedr EM, Abdel-Aleem H, Rageh TA. Effect of surgical menopause on cognitive functions. Dement Geriatr Cogn Disord. 2002;13(3):193-8. doi: 10.1159/000048652[↩]
- Nappi RE, Sinforiani E, Mauri M, Bono G, Polatti F, Nappi G. Memory functioning at menopause: impact of age in ovariectomized women. Gynecol Obstet Invest. 1999;47(1):29-36. doi: 10.1159/000010058[↩]
- Research on the menopause in the 1990s. Report of a WHO Scientific Group. World Health Organ Tech Rep Ser. 1996;866:1-107.[↩]
- Premature Menopause. https://www.msdmanuals.com/en-au/home/women-s-health-issues/menstrual-disorders-and-abnormal-vaginal-bleeding/premature-menopause[↩]
- Kodaman PH. Early menopause: primary ovarian insufficiency and surgical menopause. Semin Reprod Med. 2010 Sep;28(5):360-9. doi: 10.1055/s-0030-1262895[↩][↩][↩][↩]
- Nelson LM. Clinical practice. Primary ovarian insufficiency. N Engl J Med. 2009 Feb 5;360(6):606-14. doi: 10.1056/NEJMcp0808697[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- De Vos M, Devroey P, Fauser BC. Primary ovarian insufficiency. Lancet. 2010 Sep 11;376(9744):911-21. doi: 10.1016/S0140-6736(10)60355-8[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Lambrinoudaki I, Paschou SA, Lumsden MA, Faubion S, Makrakis E, Kalantaridou S, Panay N. Premature ovarian insufficiency: A toolkit for the primary care physician. Maturitas. 2021 May;147:53-63. doi: 10.1016/j.maturitas.2020.11.004[↩][↩][↩][↩][↩][↩]
- Welt CK. Primary ovarian insufficiency: a more accurate term for premature ovarian failure. Clin Endocrinol (Oxf). 2008 Apr;68(4):499-509. doi: 10.1111/j.1365-2265.2007.03073.x[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Imai, Kentaro, Sutton, Madeline Y., Mdodo, Rennatus, del Rio, Carlos, HIV and Menopause: A Systematic Review of the Effects of HIV Infection on Age at Menopause and the Effects of Menopause on Response to Antiretroviral Therapy, Obstetrics and Gynecology International, 2013, 340309, 11 pages, 2013. https://doi.org/10.1155/2013/340309[↩][↩]
- Looby SE, Shifren J, Corless I, Rope A, Pedersen MC, Joffe H, Grinspoon S. Increased hot flash severity and related interference in perimenopausal human immunodeficiency virus-infected women. Menopause. 2014 Apr;21(4):403-9. doi: 10.1097/GME.0b013e31829d4c4c[↩][↩]
- Sullivan SD, Sarrel PM, Nelson LM. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause. Fertil Steril. 2016 Dec;106(7):1588-1599. doi: 10.1016/j.fertnstert.2016.09.046[↩][↩]
- Klein DA, Poth MA. Amenorrhea: an approach to diagnosis and management. Am Fam Physician. 2013 Jun 1;87(11):781-8. https://www.aafp.org/pubs/afp/issues/2013/0601/p781.html[↩][↩][↩]
- Popat VB, Calis KA, Kalantaridou SN, Vanderhoof VH, Koziol D, Troendle JF, Reynolds JC, Nelson LM. Bone mineral density in young women with primary ovarian insufficiency: results of a three-year randomized controlled trial of physiological transdermal estradiol and testosterone replacement. J Clin Endocrinol Metab. 2014 Sep;99(9):3418-26. doi: 10.1210/jc.2013-4145[↩][↩][↩]
- Committee Opinion No. 698: Hormone Therapy in Primary Ovarian Insufficiency. Obstet Gynecol. 2017 May;129(5):e134-e141. doi: 10.1097/AOG.0000000000002044[↩][↩][↩]
- Canonico M, Oger E, Plu-Bureau G, Conard J, Meyer G, Lévesque H, Trillot N, Barrellier MT, Wahl D, Emmerich J, Scarabin PY; Estrogen and Thromboembolism Risk (ESTHER) Study Group. Hormone therapy and venous thromboembolism among postmenopausal women: impact of the route of estrogen administration and progestogens: the ESTHER study. Circulation. 2007 Feb 20;115(7):840-5. doi: 10.1161/CIRCULATIONAHA.106.642280[↩][↩][↩]
- Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists and American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis – 2016. Endocr Pract. 2016;22(suppl 4):1-42. Endocr Pract. 2016 Sep 2;22(Suppl 4):1-42. doi: 10.4158/EP161435.GL[↩][↩]
- Perimenopause & Premature Menopause FAQS. http://www.menopause.org/for-women/expert-answers-to-frequently-asked-questions-about-menopause/perimenopause-premature-menopause-faqs[↩]
- Shifren JL, Gass ML; NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014 Oct;21(10):1038-62. doi: 10.1097/GME.0000000000000319[↩][↩]
- Perimenopause. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666[↩]
- The Menopause Years. https://www.acog.org/womens-health/faqs/the-menopause-years[↩]
- Menopause basics. https://www.womenshealth.gov/menopause/menopause-basics[↩][↩][↩]
- Mishra GD, Cooper R, Tom SE, Kuh D. Early life circumstances and their impact on menarche and menopause. Womens Health (Lond). 2009 Mar;5(2):175-90. doi: 10.2217/17455057.5.2.175[↩]
- A longitudinal analysis of women’s attitudes toward the menopause: results from the Massachusetts Women’s Health Study. Avis, N.E. et al. Maturitas, Volume 13, Issue 1, 65 – 79. https://www.maturitas.org/article/0378-5122(91)90286-Y/abstract[↩]
- Smoking’s Impact on Women’s Health. https://women.smokefree.gov/quit-smoking-women/what-women-should-know/smokings-impact-on-women[↩][↩]
- Bellavia A, Wolk A, Orsini N. Differences in age at death according to smoking and age at menopause. Menopause. 2016 Jan;23(1):108-10. doi: 10.1097/GME.0000000000000501[↩]
- Boneva RS, Lin JM, Unger ER. Early menopause and other gynecologic risk indicators for chronic fatigue syndrome in women. Menopause. 2015 Aug;22(8):826-34. doi: 10.1097/GME.0000000000000411[↩]
- Primary Ovarian Insufficiency in Adolescents and Young Women. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2014/07/primary-ovarian-insufficiency-in-adolescents-and-young-women[↩][↩][↩]
- Cordts EB, Christofolini DM, Dos Santos AA, Bianco B, Barbosa CP. Genetic aspects of premature ovarian failure: a literature review. Arch Gynecol Obstet. 2011 Mar;283(3):635-43. doi: 10.1007/s00404-010-1815-4[↩][↩]
- Rebar RW. Premature ovarian failure. Obstet Gynecol. 2009 Jun;113(6):1355-1363. doi: 10.1097/AOG.0b013e3181a66843[↩][↩][↩][↩]
- Addison Disease. https://medlineplus.gov/addisondisease.html[↩]
- van Der Voort DJ, van Der Weijer PH, Barentsen R. Early menopause: increased fracture risk at older age. Osteoporos Int. 2003 Jul;14(6):525-30. doi: 10.1007/s00198-003-1408-1[↩]
- Bleil ME, Gregorich SE, McConnell D, Rosen MP, Cedars MI. Does accelerated reproductive aging underlie premenopausal risk for cardiovascular disease? Menopause. 2013 Nov;20(11):1139-46. doi: 10.1097/GME.0b013e31828950fa[↩]
- Torrealday S, Pal L. Premature Menopause. Endocrinol Metab Clin North Am. 2015 Sep;44(3):543-57. doi: 10.1016/j.ecl.2015.05.004[↩]
- Rocca WA, Grossardt BR, Miller VM, Shuster LT, Brown RD., Jr Premature menopause or early menopause and risk of ischemic stroke. Menopause. 2012;19:272–277. doi: 10.1097/gme.0b013e31822a9937[↩]
- Jacobsen BK, Heuch I, Kvåle G. Age at natural menopause and all-cause mortality: A 37-year follow-up of 19,731 Norwegian women. Am. J. Epidemiol. 2003;157:923–929. doi: 10.1093/aje/kwg066[↩]
- van der Schouw YT, van der Graaf Y, Steyerberg EW, Eijkemans JC, Banga JD. Age at menopause as a risk factor for cardiovascular mortality. Lancet. 1996;347:714–718. doi: 10.1016/s0140-6736(96)90075-6[↩]
- Committee opinion no. 605: primary ovarian insufficiency in adolescents and young women. Obstet Gynecol. 2014 Jul;124(1):193-197. doi: 10.1097/01.AOG.0000451757.51964.98[↩][↩][↩][↩][↩][↩][↩]
- Anasti JN, Kalantaridou SN, Kimzey LM, Defensor RA, Nelson LM. Bone loss in young women with karyotypically normal spontaneous premature ovarian failure. Obstet Gynecol. 1998 Jan;91(1):12-5. doi: 10.1016/s0029-7844(97)00583-8[↩]
- Popat VB, Calis KA, Vanderhoof VH, Cizza G, Reynolds JC, Sebring N, Troendle JF, Nelson LM. Bone mineral density in estrogen-deficient young women. J Clin Endocrinol Metab. 2009 Jul;94(7):2277-83. doi: 10.1210/jc.2008-1878[↩][↩]
- Vega EM, Egea MA, Mautalen CA. Influence of the menopausal age on the severity of osteoporosis in women with vertebral fractures. Maturitas. 1994 Aug;19(2):117-24. doi: 10.1016/0378-5122(94)90061-2[↩][↩]
- Gärdsell P, Johnell O, Nilsson BE. The predictive value of bone loss for fragility fractures in women: a longitudinal study over 15 years. Calcif Tissue Int. 1991 Aug;49(2):90-4. doi: 10.1007/BF02565127[↩]
- Tuppurainen M, Kröger H, Honkanen R, Puntila E, Huopio J, Saarikoski S, Alhava E. Risks of perimenopausal fractures–a prospective population-based study. Acta Obstet Gynecol Scand. 1995 Sep;74(8):624-8. doi: 10.3109/00016349509013475[↩][↩]
- van der Klift M, de Laet CE, McCloskey EV, Johnell O, Kanis JA, Hofman A, Pols HA. Risk factors for incident vertebral fractures in men and women: the Rotterdam Study. J Bone Miner Res. 2004 Jul;19(7):1172-80. doi: 10.1359/JBMR.040215[↩][↩][↩]
- Leite-Silva P, Bedone A, Pinto-Neto AM, Costa JV, Costa-Paiva L. Factors associated with bone density in young women with karyotypically normal spontaneous premature ovarian failure. Arch Gynecol Obstet. 2009 Aug;280(2):177-81. doi: 10.1007/s00404-008-0881-3[↩]
- Hormone Therapy in Primary Ovarian Insufficiency. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/05/hormone-therapy-in-primary-ovarian-insufficiency[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc. 2008 Sep;83(9):1032-45. doi: 10.4065/83.9.1032[↩]
- Campos H, McNamara JR, Wilson PW, Ordovas JM, Schaefer EJ. Differences in low density lipoprotein subfractions and apolipoproteins in premenopausal and postmenopausal women. J Clin Endocrinol Metab. 1988 Jul;67(1):30-5. doi: 10.1210/jcem-67-1-30[↩]
- Jensen J, Nilas L, Christiansen C. Influence of menopause on serum lipids and lipoproteins. Maturitas. 1990 Nov;12(4):321-31. doi: 10.1016/0378-5122(90)90012-u[↩]
- Jacobsen BK, Knutsen SF, Fraser GE. Age at natural menopause and total mortality and mortality from ischemic heart disease: the Adventist Health Study. J Clin Epidemiol. 1999 Apr;52(4):303-7. doi: 10.1016/s0895-4356(98)00170-x[↩][↩]
- de Kleijn MJ, van der Schouw YT, Verbeek AL, Peeters PH, Banga JD, van der Graaf Y. Endogenous estrogen exposure and cardiovascular mortality risk in postmenopausal women. Am J Epidemiol. 2002 Feb 15;155(4):339-45. doi: 10.1093/aje/155.4.339[↩]
- van der Schouw YT, van der Graaf Y, Steyerberg EW, Eijkemans JC, Banga JD. Age at menopause as a risk factor for cardiovascular mortality. Lancet. 1996 Mar 16;347(9003):714-8. doi: 10.1016/s0140-6736(96)90075-6[↩][↩]
- Kalantaridou SN, Naka KK, Papanikolaou E, Kazakos N, Kravariti M, Calis KA, Paraskevaidis EA, Sideris DA, Tsatsoulis A, Chrousos GP, Michalis LK. Impaired endothelial function in young women with premature ovarian failure: normalization with hormone therapy. J Clin Endocrinol Metab. 2004 Aug;89(8):3907-13. doi: 10.1210/jc.2004-0015[↩]
- Ostberg JE, Storry C, Donald AE, Attar MJ, Halcox JP, Conway GS. A dose-response study of hormone replacement in young hypogonadal women: effects on intima media thickness and metabolism. Clin Endocrinol (Oxf). 2007 Apr;66(4):557-64. doi: 10.1111/j.1365-2265.2007.02772.x[↩]
- Langrish JP, Mills NL, Bath LE, Warner P, Webb DJ, Kelnar CJ, Critchley HO, Newby DE, Wallace WH. Cardiovascular effects of physiological and standard sex steroid replacement regimens in premature ovarian failure. Hypertension. 2009 May;53(5):805-11. doi: 10.1161/HYPERTENSIONAHA.108.126516[↩]
- Snowdon DA, Kane RL, Beeson WL, Burke GL, Sprafka JM, Potter J, Iso H, Jacobs DR Jr, Phillips RL. Is early natural menopause a biologic marker of health and aging? Am J Public Health. 1989 Jun;79(6):709-14. doi: 10.2105/ajph.79.6.709[↩]
- Butts S, Riethman H, Ratcliffe S, Shaunik A, Coutifaris C, Barnhart K. Correlation of telomere length and telomerase activity with occult ovarian insufficiency. J Clin Endocrinol Metab. 2009 Dec;94(12):4835-43. doi: 10.1210/jc.2008-2269[↩]
- Rocca WA, Bower JH, Maraganore DM, Ahlskog JE, Grossardt BR, de Andrade M, Melton LJ 3rd. Increased risk of cognitive impairment or dementia in women who underwent oophorectomy before menopause. Neurology. 2007 Sep 11;69(11):1074-83. doi: 10.1212/01.wnl.0000276984.19542.e6[↩]
- Ross JL, Stefanatos GA, Kushner H, Bondy C, Nelson L, Zinn A, Roeltgen D. The effect of genetic differences and ovarian failure: intact cognitive function in adult women with premature ovarian failure versus turner syndrome. J Clin Endocrinol Metab. 2004 Apr;89(4):1817-22. doi: 10.1210/jc.2003-031463[↩]
- Singer D, Mann E, Hunter MS, Pitkin J, Panay N. The silent grief: psychosocial aspects of premature ovarian failure. Climacteric. 2011 Aug;14(4):428-37. doi: 10.3109/13697137.2011.571320[↩][↩]
- Benetti-Pinto CL, de Almeida DM, Makuch MY. Quality of life in women with premature ovarian failure. Gynecol Endocrinol. 2011 Sep;27(9):645-9. doi: 10.3109/09513590.2010.520374[↩]
- Orshan SA, Ventura JL, Covington SN, Vanderhoof VH, Troendle JF, Nelson LM. Women with spontaneous 46,XX primary ovarian insufficiency (hypergonadotropic hypogonadism) have lower perceived social support than control women. Fertil Steril. 2009 Aug;92(2):688-93. doi: 10.1016/j.fertnstert.2008.07.1718[↩]
- Groff AA, Covington SN, Halverson LR, Fitzgerald OR, Vanderhoof V, Calis K, Nelson LM. Assessing the emotional needs of women with spontaneous premature ovarian failure. Fertil Steril. 2005 Jun;83(6):1734-41. doi: 10.1016/j.fertnstert.2004.11.067[↩]
- Schmidt PJ, Cardoso GM, Ross JL, Haq N, Rubinow DR, Bondy CA. Shyness, social anxiety, and impaired self-esteem in Turner syndrome and premature ovarian failure. JAMA. 2006 Mar 22;295(12):1374-6. doi: 10.1001/jama.295.12.1374[↩]
- Mann E, Singer D, Pitkin J, Panay N, Hunter MS. Psychosocial adjustment in women with premature menopause: a cross-sectional survey. Climacteric. 2012 Oct;15(5):481-9. doi: 10.3109/13697137.2011.647841[↩][↩]
- Stuenkel CA, Gompel A, Davis SR, et al: Approach to the patient with new-onset secondary amenorrhea: Is this primary ovarian insufficiency? J Clin Endocrinol Metab 107 (3):825–835, 2022. doi: 10.1210/clinem/dgab766[↩]
- Novosad JA, Kalantaridou SN, Tong ZB, Nelson LM: Ovarian antibodies as detected by indirect immunofluorescence are unreliable in the diagnosis of autoimmune premature ovarian failure: A controlled evaluation. BMC Womens Health 3 (1):2, 2003. doi: 10.1186/1472-6874-3-2[↩]
- Primary Ovarian Insufficiency. https://www.msdmanuals.com/en-au/professional/gynecology-and-obstetrics/menstrual-abnormalities/primary-ovarian-insufficiency[↩][↩]
- Klein DA, Paradise SL, Reeder RM. Amenorrhea: A Systematic Approach to Diagnosis and Management. Am Fam Physician. 2019 Jul 1;100(1):39-48. https://www.aafp.org/pubs/afp/issues/2019/0701/p39.html[↩][↩]
- Sheshpari S, Shahnazi M, Mobarak H, Ahmadian S, Bedate AM, Nariman-Saleh-Fam Z, Nouri M, Rahbarghazi R, Mahdipour M. Ovarian function and reproductive outcome after ovarian tissue transplantation: a systematic review. J Transl Med. 2019 Nov 29;17(1):396. doi: 10.1186/s12967-019-02149-2[↩]
- Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO, Lin AE, Mauras N, Quigley CA, Rubin K, Sandberg DE, Sas TCJ, Silberbach M, Söderström-Anttila V, Stochholm K, van Alfen-van derVelden JA, Woelfle J, Backeljauw PF; International Turner Syndrome Consensus Group. Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur J Endocrinol. 2017 Sep;177(3):G1-G70. doi: 10.1530/EJE-17-0430[↩]
- Christ JP, Gunning MN, Palla G, Eijkemans MJC, Lambalk CB, Laven JSE, Fauser BCJM. Estrogen deprivation and cardiovascular disease risk in primary ovarian insufficiency. Fertil Steril. 2018 Apr;109(4):594-600.e1. doi: 10.1016/j.fertnstert.2017.11.035[↩]
- Burgos N, Cintron D, Latortue-Albino P, Serrano V, Rodriguez Gutierrez R, Faubion S, Spencer-Bonilla G, Erwin PJ, Murad MH. Estrogen-based hormone therapy in women with primary ovarian insufficiency: a systematic review. Endocrine. 2017 Dec;58(3):413-425. doi: 10.1007/s12020-017-1435-x. Epub 2017 Oct 16. Erratum in: Endocrine. 2018 Jan;59(1):235. doi: 10.1007/s12020-017-1491-2[↩]
- Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. The Writing Group for the PEPI Trial. JAMA. 1995 Jan 18;273(3):199-208. Erratum in: JAMA 1995 Dec 6;274(21):1676.[↩][↩][↩]
- Woodruff JD, Pickar JH. Incidence of endometrial hyperplasia in postmenopausal women taking conjugated estrogens (Premarin) with medroxyprogesterone acetate or conjugated estrogens alone. The Menopause Study Group. Am J Obstet Gynecol. 1994 May;170(5 Pt 1):1213-23. doi: 10.1016/s0002-9378(94)70129-6[↩]
- Schiff I, Sela HK, Cramer D, Tulchinsky D, Ryan KJ. Endometrial hyperplasia in women on cyclic or continuous estrogen regimens. Fertil Steril. 1982 Jan;37(1):79-82. doi: 10.1016/s0015-0282(16)45981-9[↩]
- Henderson BE. The cancer question: an overview of recent epidemiologic and retrospective data. Am J Obstet Gynecol. 1989 Dec;161(6 Pt 2):1859-64. doi: 10.1016/s0002-9378(89)80007-9[↩]
- Beral V, Bull D, Reeves G; Million Women Study Collaborators. Endometrial cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2005 Apr 30-May 6;365(9470):1543-51. doi: 10.1016/S0140-6736(05)66455-0[↩]
- Practice Bulletin No. 149: Endometrial cancer. Obstet Gynecol. 2015 Apr;125(4):1006-1026. doi: 10.1097/01.AOG.0000462977.61229.de[↩][↩]
- Voigt LF, Weiss NS, Chu J, Daling JR, McKnight B, van Belle G. Progestagen supplementation of exogenous oestrogens and risk of endometrial cancer. Lancet. 1991 Aug 3;338(8762):274-7. doi: 10.1016/0140-6736(91)90417-n[↩]
- Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J; Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002 Jul 17;288(3):321-33. doi: 10.1001/jama.288.3.321[↩]
- Fritz MA, Speroff L. Clinical and gynecologic endocrinology and infertility . 8th ed.Philadelphia (PA): Wolters Kluwer/Lippincott Williams & Wilkins; 2011.[↩][↩][↩][↩]
- ACOG Practice Bulletin No. 141: management of menopausal symptoms. Obstet Gynecol. 2014 Jan;123(1):202-216. doi: 10.1097/01.AOG.0000441353.20693.78. Erratum in: Obstet Gynecol. 2016 Jan;127(1):166. doi: 10.1097/AOG.0000000000001230. Erratum in: Obstet Gynecol. 2018 Mar;131(3):604. doi: 10.1097/AOG.0000000000002513[↩]
- Utian WH, Archer DF, Bachmann GA, Gallagher C, Grodstein Fn, Heiman JR, Henderson VW, Hodis HN, Karas RH, Lobo RA, Manson JE, Reid RL, Schmidt PJ, Stuenkel CA; North American Menopause Society. Estrogen and progestogen use in postmenopausal women: July 2008 position statement of The North American Menopause Society. Menopause. 2008 Jul-Aug;15(4 Pt 1):584-602. doi: 10.1097/gme.0b013e31817b076a[↩]
- Pitkin J, Rees MC, Gray S, Lumsden MA, Marsden J, Stevenson JC, Williamson J. Management of premature menopause. Menopause Int. 2007 Mar;13(1):44-5. doi: 10.1258/175404507780456719[↩]
- Board of the International Menopause Society; Pines A, Sturdee DW, Birkhäuser MH, Schneider HP, Gambacciani M, Panay N. IMS updated recommendations on postmenopausal hormone therapy. Climacteric. 2007 Jun;10(3):181-94. doi: 10.1080/13697130701361657[↩]
- Beral V; Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003 Aug 9;362(9382):419-27. doi: 10.1016/s0140-6736(03)14065-2. Erratum in: Lancet. 2003 Oct 4;362(9390):1160.[↩]
- Rebbeck TR, Friebel T, Wagner T, Lynch HT, Garber JE, Daly MB, Isaacs C, Olopade OI, Neuhausen SL, van ‘t Veer L, Eeles R, Evans DG, Tomlinson G, Matloff E, Narod SA, Eisen A, Domchek S, Armstrong K, Weber BL; PROSE Study Group. Effect of short-term hormone replacement therapy on breast cancer risk reduction after bilateral prophylactic oophorectomy in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol. 2005 Nov 1;23(31):7804-10. doi: 10.1200/JCO.2004.00.8151[↩]
- Malone KE, Daling JR, Weiss NS. Oral contraceptives in relation to breast cancer. Epidemiol Rev. 1993;15(1):80-97. doi: 10.1093/oxfordjournals.epirev.a036119[↩][↩]
- Romieu I, Berlin JA, Colditz G. Oral contraceptives and breast cancer. Review and meta-analysis. Cancer. 1990 Dec 1;66(11):2253-63. doi: 10.1002/1097-0142(19901201)66:11<2253::aid-cncr2820661102>3.0.co;2-g[↩][↩]
- Thomas DB. Oral contraceptives and breast cancer: review of the epidemiologic literature. Contraception. 1991 Jun;43(6):597-642. doi: 10.1016/0010-7824(91)90006-2[↩][↩]
- Rosenberg L, Miller DR, Kaufman DW, Helmrich SP, Stolley PD, Schottenfeld D, Shapiro S. Breast cancer and oral contraceptive use. Am J Epidemiol. 1984 Feb;119(2):167-76. doi: 10.1093/oxfordjournals.aje.a113735[↩][↩]
- Romieu I, Willett WC, Colditz GA, Stampfer MJ, Rosner B, Hennekens CH, Speizer FE. Prospective study of oral contraceptive use and risk of breast cancer in women. J Natl Cancer Inst. 1989 Sep 6;81(17):1313-21. doi: 10.1093/jnci/81.17.1313[↩][↩]
- Paul C, Skegg DC, Spears GF. Oral contraceptives and risk of breast cancer. Int J Cancer. 1990 Sep 15;46(3):366-73. doi: 10.1002/ijc.2910460305[↩][↩][↩]
- Oral contraceptive use and breast cancer risk in young women. UK National Case-Control Study Group. Lancet. 1989 May 6;1(8645):973-82.[↩][↩][↩]
- Shelton JD. Breast cancer and combined oral contraceptives. Br J Cancer. 1990 Sep;62(3):468-70. doi: 10.1038/bjc.1990.321[↩][↩]
- Vessey MP, McPherson K, Villard-Mackintosh L, Yeates D. Oral contraceptives and breast cancer: latest findings in a large cohort study. Br J Cancer. 1989 Apr;59(4):613-7. doi: 10.1038/bjc.1989.124[↩][↩]
- McPherson K, Vessey MP, Neil A, Doll R, Jones L, Roberts M. Early oral contraceptive use and breast cancer: results of another case-control study. Br J Cancer. 1987 Nov;56(5):653-60. doi: 10.1038/bjc.1987.261[↩][↩]
- Meirik O, Lund E, Adami HO, Bergström R, Christoffersen T, Bergsjö P. Oral contraceptive use and breast cancer in young women. A joint national case-control study in Sweden and Norway. Lancet. 1986 Sep 20;2(8508):650-4. doi: 10.1016/s0140-6736(86)90166-2[↩]
- Paffenbarger RS Jr, Kampert JB, Chang HG. Characteristics that predict risk of breast cancer before and after the menopause. Am J Epidemiol. 1980 Aug;112(2):258-68. doi: 10.1093/oxfordjournals.aje.a112992[↩]
- Jick SS, Walker AM, Stergachis A, Jick H. Oral contraceptives and breast cancer. Br J Cancer. 1989 Apr;59(4):618-21. doi: 10.1038/bjc.1989.125[↩]
- Miller DR, Rosenberg L, Kaufman DW, Schottenfeld D, Stolley PD, Shapiro S. Breast cancer risk in relation to early oral contraceptive use. Obstet Gynecol. 1986 Dec;68(6):863-8.[↩]
- Chetkowski RJ, Meldrum DR, Steingold KA, Randle D, Lu JK, Eggena P, Hershman JM, Alkjaersig NK, Fletcher AP, Judd HL. Biologic effects of transdermal estradiol. N Engl J Med. 1986 Jun 19;314(25):1615-20. doi: 10.1056/NEJM198606193142505[↩]
- ACOG committee opinion no. 556: Postmenopausal estrogen therapy: route of administration and risk of venous thromboembolism. Obstet Gynecol. 2013 Apr;121(4):887-890. doi: 10.1097/01.AOG.0000428645.90795.d9[↩]
- Jaakkola S, Lyytinen HK, Dyba T, Ylikorkala O, Pukkala E. Endometrial cancer associated with various forms of postmenopausal hormone therapy: a case control study. Int J Cancer. 2011 Apr 1;128(7):1644-51. doi: 10.1002/ijc.25762[↩]