Contents
- What is ovarian cancer
- Female reproductive system
- Ovarian cancer types
- Ovarian cancer signs and symptoms
- Can ovarian cancer be found early?
- Ovarian cancer causes
- Ovarian cancer risk factors
- Getting older
- Being overweight or obese
- Having children later or never having a full-term pregnancy
- Using fertility treatment
- Taking hormone therapy after menopause
- Having a family history of ovarian cancer, breast cancer, or colorectal cancer
- Having a family cancer syndrome
- Having had breast cancer
- Endometriosis or diabetes
- Smoking and alcohol use
- Asbestos
- Factors with unclear effects on ovarian cancer risk
- Factors that can lower risk of ovarian cancer
- Ovarian cancer prevention
- Ovarian cancer diagnosis
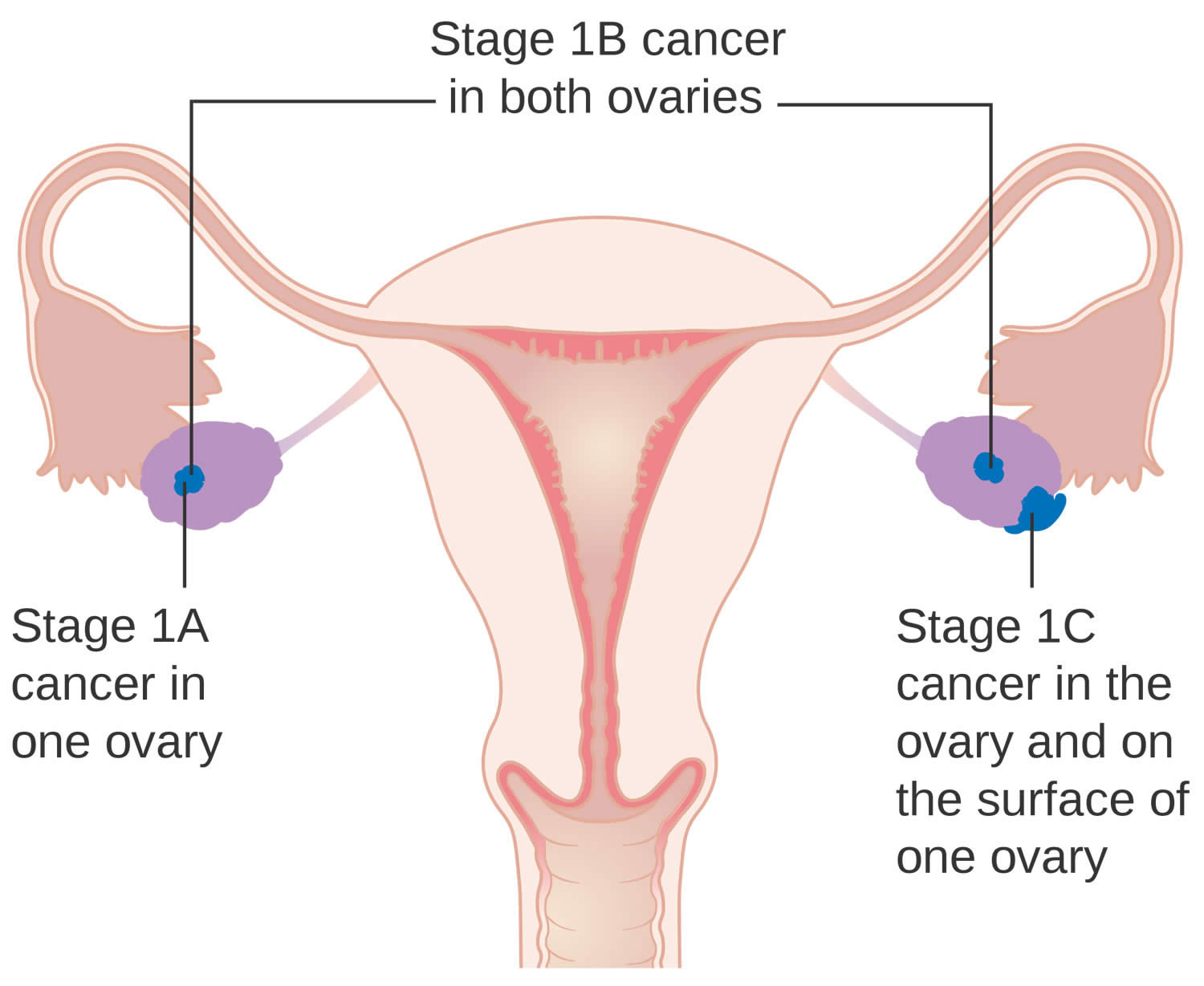
- Ovarian cancer stages
- Ovarian cancer treatment
- Surgery
- Chemotherapy
- Targeted Drug Therapy for Ovarian Cancer
- Radiotherapy
- Hormone therapy
- Immunotherapy
- Supportive (palliative) care
- Ovarian cancer treatment and fertility
- Stage 1 ovarian cancer treatment
- Stage 2 ovarian cancer treatment
- Stage 3 ovarian cancer treatment
- Stage 4 ovarian cancer treatment
- Coping and support
- Ovarian cancer prognosis
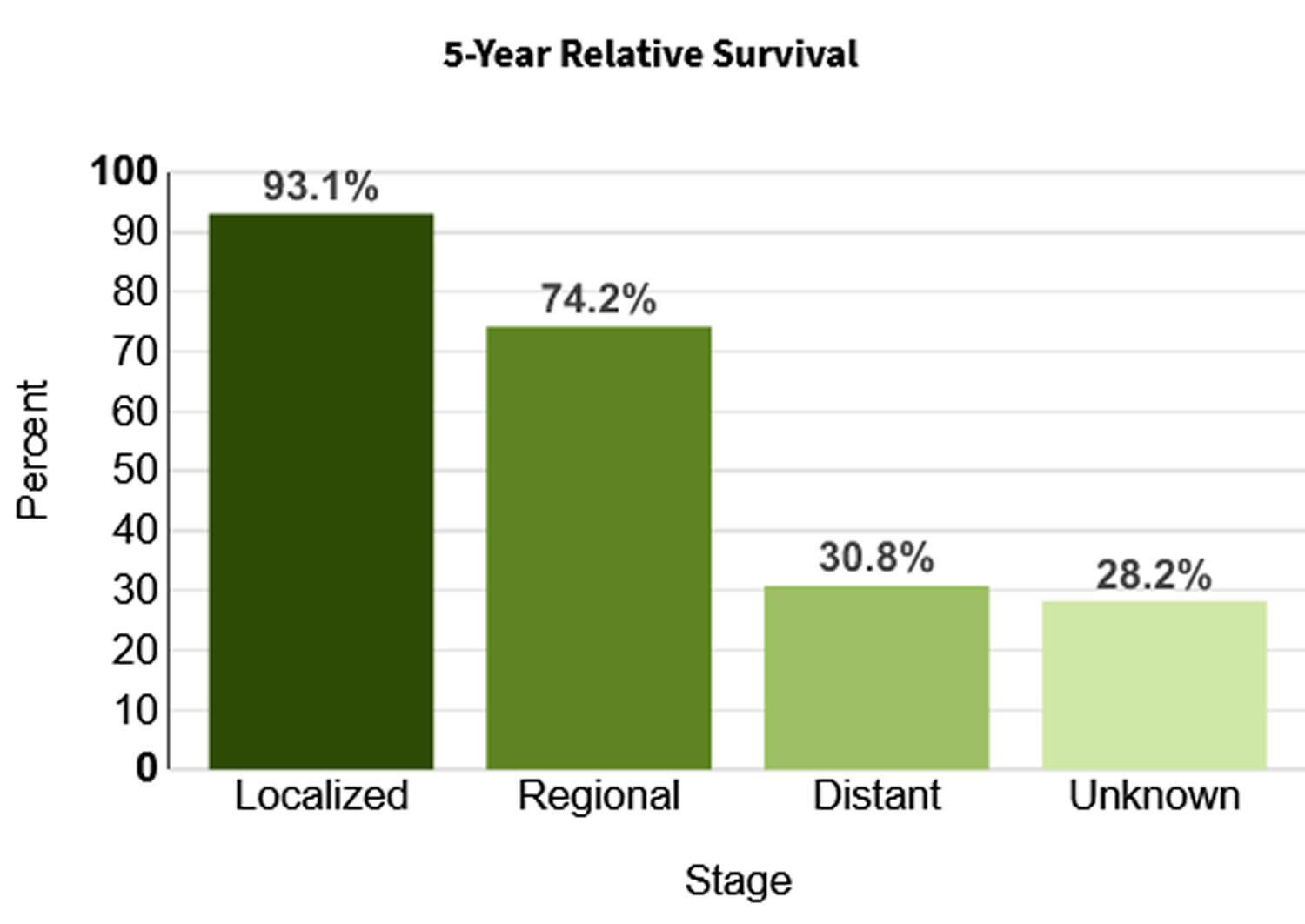
- Ovarian cancer survival rate
What is ovarian cancer
Ovarian cancer is cancer that forms in tissues of the ovary (one of a pair of female reproductive glands in which the eggs or ova, are formed). The ovaries are a pair of small organs in the female reproductive system that contain and release an egg once a month in women of menstruating age. This is known as ovulation. Ovarian cancers were previously believed to begin only in the ovaries, but recent evidence suggests that many ovarian cancers may actually start in the cells in the far (distal) end of the fallopian tubes.
Most ovarian cancers are either ovarian epithelial cancers (cancer that begins in the cells on the surface of the ovary) or malignant germ cell tumors (cancer that begins in egg cells). Fallopian tube cancer and primary peritoneal cancer are similar to ovarian epithelial cancer and are staged and treated the same way.
In general, cancer begins when a cell develops errors (mutations) in its DNA. The mutations tell the cell to grow and multiply quickly, creating a mass (tumor) of abnormal cells. The abnormal cells continue living when healthy cells would die. They can invade nearby tissues and break off from an initial tumor to spread elsewhere in the body (metastasize).
There are several types of ovarian cancer. They include:
- Epithelial ovarian cancer, which affects the outer surface layers of the ovary; it is by far the most common type. About 90 percent of ovarian cancers are epithelial tumors.
- Germ cell ovarian cancer, which originate in the cells that make the eggs. These rare ovarian cancers tend to occur in younger women.
- Stromal tumors, which develop within the cells that release female hormones. Stromal tumors are usually diagnosed at an earlier stage than other ovarian cancers. About 7 percent of ovarian tumors are stromal.
It is also possible to have borderline epithelial tumors which are not as aggressive as other epithelial tumors. These are sometimes called ‘low malignant potential’ or LMP tumors.
Ovarian cancer mainly develops in older women who have experienced menopause (usually over the age of 50), but it can affect women of any age. About half of the women who are diagnosed with ovarian cancer are 63 years or older. It is more common in white women than African-American women 1.
Ovarian cancer can spread to other parts of the reproductive system and the surrounding areas, including the womb (uterus), vagina and abdomen.
The symptoms of ovarian cancer can be difficult to recognize, particularly in the early stages of the disease. They are often the same as the symptoms of other, less serious, conditions, such as irritable bowel syndrome (IBS) or premenstrual syndrome (PMS). The symptoms of ovarian cancer can be similar to other conditions making them difficult to recognize. However, there are early symptoms to look out for such as pain in the pelvis and lower stomach, persistent bloating and difficulty eating. Consult your doctor if you are experiencing any of these symptoms.
The most common symptoms of ovarian cancer are:
- Pain. You might have pain or discomfort in:
- your belly (abdomen)
- the area between your hip bones (pelvis)
- your back – although this is less common
- Swollen belly. Feeling bloated or an increase in the size of your abdomen that doesn’t go away can be a symptom of ovarian cancer.
- Loss of appetite. You might feel full quickly when you eat. Or you may not feel like eating.
- Urinary changes. You may need to pee more often, or have to go more urgently.
You may also have some other symptoms including:
- Tiredness. You might feel extremely tired for no obvious reason if you have ovarian cancer.
- Bowel changes. You might have loose poop or need to poop more often (diarrhea). Or you may go less often or have hard poop (constipation).
- Weight loss and feeling sick. You might lose weight even if you aren’t trying to. This might be due to feeling sick.
- Indigestion. Indigestion causes heartburn, bloating and sickness. It is a common problem in the general population, and for most people it isn’t a sign of cancer.
- Vaginal bleeding. You might notice bleeding in between your periods. Or you could have bleeding from your vagina after your menopause.
Ovarian cancer often goes undetected until it has spread within the pelvis and abdomen. At this late stage, ovarian cancer is more difficult to treat and is frequently fatal. Early-stage ovarian cancer, in which the disease is confined to the ovary, is more likely to be treated successfully.
Surgery and chemotherapy are generally used to treat ovarian cancer. The amount and type of surgery you have depends on how far your cancer has spread and on your general health. For women of childbearing age who have certain kinds of tumors and whose cancer is in the earliest stage, it may be possible to treat the disease without removing both ovaries and the uterus.
Some women with ovarian cancer might have:
- Targeted cancer drugs
- Hormone therapy
- Radiotherapy (radiation therapy)
The American Cancer Society estimates for ovarian cancer in the United States for 2025 are 1, 2:
- New cases: About 20,890 women will receive a new diagnosis of ovarian cancer. The rate at which women are diagnosed with ovarian cancer has been slowly falling over the past 20 years. The incidence rate declined by 1% to 2% per year from 1990 to the mid-2010s and by almost 2% per year from 2012 to 2021. This trend is likely due at least in part to increased oral contraceptive use in the latter half of the past century and decreased menopausal hormone therapy use during the 2000s, both of which can lower risk.
- Deaths: About 12,730 women will die from ovarian cancer. Ovarian cancer ranks fifth in cancer deaths among women, accounting for more deaths than any other cancer of the female reproductive system. Ovarian cancer mortality has declined from 2% annually during the 2000s and early 2010s to more than 3% annually from 2016 to 2020, reflecting both decreased incidence and improved treatment.
- 5-Year Relative Survival: 50.9%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Ovarian cancer deaths as a percentage of All Cancer Deaths: 2.1%.
- Rate of New Cases and Deaths per 100,000: The rate of new cases of ovarian cancer was 10.2 per 100,000 women per year. The death rate was 6.0 per 100,000 women per year. These rates are age-adjusted and based on 2017–2021 cases and 2018–2022 deaths.
- Lifetime Risk of Developing Ovarian Cancer: Approximately 1.1 percent of women will be diagnosed with ovarian cancer at some point during their lifetime, based on 2018–2021 data.
- In 2021, there were an estimated 238,484 women living with ovarian cancer in the United States.
A woman’s risk of getting ovarian cancer during her lifetime is about 1 in 91. Her lifetime chance of dying from ovarian cancer is about 1 in 143. These statistics don’t count low malignant potential ovarian tumors.
Known risk factors for ovarian cancer include:
- Getting older: women who are over 50 are more likely to develop ovarian cancer than younger women. The risk of ovarian cancer increases steeply from around 45 years. And is greatest in those aged between 75 and 79 years.
- Inheriting a faulty gene called a gene mutation that increases the risk of ovarian cancer. Between 5 and 15 out of 100 ovarian cancers (5 to 15%) are caused by an inherited faulty gene. Mutations in the breast cancer susceptibility genes 1 and 2 (BRCA1 and BRCA2), and those associated with Lynch syndrome, raise ovarian cancer risk.
- Having a strong family history of ovarian cancer, breast cancer, or some other cancers, including colorectal cancer and endometrial cancer
- Having had breast cancer in the past. The risk is higher in women diagnosed with breast cancer at a younger age. And those with estrogen receptor negative (ER negative) breast cancer.
Only around 5-15% of all ovarian cancers are due to inherited factors.
Research suggests that the risk of ovarian cancer is slightly higher for women who:
- have medical conditions such as endometriosis and diabetes. Studies have shown that women with endometriosis or diabetes have an increased risk of ovarian cancer. In diabetics, the increase in risk might be higher in those that use insulin.
- use long-term hormone replacement therapy (HRT). Using HRT (hormone replacement therapy) after the menopause increases the risk of ovarian cancer.
- had early puberty (menstruating before 12) or late menopause (onset after 50)
- smoke cigarettes. Smoking can increase your risk of certain types of ovarian cancer such as mucinous ovarian cancer. The longer you have smoked, the greater the risk.
- are overweight or obese. Having excess body fat is linked to an increase in risk of ovarian cancer.
Women have a lower risk of developing ovarian cancer if:
- they had a baby before the age of 26
- they used oral contraceptives (the pill) for at least 3 months
- they have had a hysterectomy (removal of the uterus) and tubal ligation (tubes tied)
Make an appointment with your doctor if you have any signs or symptoms that worry you.
If you have a family history of ovarian cancer or breast cancer, talk to your doctor about your risk of ovarian cancer. Your doctor may refer you to a genetic counselor to discuss testing for certain gene mutations that increase your risk of breast and ovarian cancers.
Female reproductive system
The female reproductive system includes parts of the female body that are involved in sexual activity, fertility, pregnancy and childbirth. The female reproductive system is made up of female body parts that include the following:
- Ovaries — There are 2 ovaries, which are about the size and shape of almonds, 1 ovary on each side of the uterus where female hormones (estrogen and progesterone) are produced, and eggs (ova) are stored to mature. Every month, an egg (ovum) is released. This is called ovulation. All the other female reproductive organs are there to transport, nurture and otherwise meet the needs of the egg or developing fetus.
- Fallopian tubes are 2 thin tubes that connect your ovaries to your uterus (womb), allowing the egg (ovum) to travel to your uterus (womb).
- The fallopian tubes are about 10 cm long and begin as funnel-shaped passages next to the ovary. They have a number of finger-like projections known as fimbriae on the end near the ovary. When an egg is released by the ovary it is ‘caught’ by one of the fimbriae and transported along the fallopian tube to the uterus. The egg is moved along the fallopian tube by the wafting action of cilia — hairy projections on the surfaces of cells at the entrance of the fallopian tube — and the contractions made by the tube. It takes the egg about 5 days to reach the uterus and it is on this journey down the fallopian tube that fertilisation may occur if a sperm penetrates and fuses with the egg. The egg, however, is usually viable for only 24 hours after ovulation, so fertilization usually occurs in the top one-third of the fallopian tube.
- Uterus (the womb) — Your uterus also known as the womb is a hollow muscular organ about the size of a pear (in women who have never been pregnant) that exists to house a developing fertilized egg (zygote). The main part of the uterus which sits in the pelvic cavity is called the body of the uterus, while the rounded region above the entrance of the fallopian tubes is the fundus and its narrow outlet, which protrudes into the vagina, is the cervix. The thick wall of your uterus is composed of 3 layers. The inner layer is known as the endometrium. The inner lining of your uterus (endometrium) thickens with blood and other substances every month. If an egg (ovum) has been fertilized (zygote), pregnancy occurs, the fertilized egg (zygote) will burrow into the endometrium in your uterus, where it will stay for the rest of its growth, growing into a fetus and then a baby. Your uterus (womb) will expand during a pregnancy to make room for the growing fetus. A part of the wall of the fertilized egg (zygote), which has burrowed into the endometrium, develops into the placenta. If an egg has not been fertilized, the endometrial lining is shed at the end of each menstrual cycle, this lining flows out of your body. This is known as menstruation or your period.
- The myometrium is the large middle layer of your uterus, which is made up of interlocking groups of muscle. It plays an important role during the birth of a baby, contracting rhythmically to move the baby out of the body via the birth canal (vagina).
- Cervix is the lower part of your uterus, that connects your uterus to your vagina.
- Vagina is a muscular tube connecting your cervix to the outside of your body (the vestibule of the vulva). Your vagina receives the penis and semen during sexual intercourse and also provides a passageway for menstrual blood flow to leave the body.
The female reproductive system also plays an important part in pregnancy and birth.
Figure 1. Female reproductive system (normal female reproductive system anatomy)
Figure 2. Female reproductive system
What are the ovaries?
Ovaries are female reproductive glands found only in females (women). The 2 ovaries (one ovary is on each side of your uterus or womb) produce female hormones (estrogen and progesterone) and eggs (ova) for reproduction. The eggs travel from your ovaries through the fallopian tubes into your uterus (womb) where the fertilized egg settles in and develops into a fetus (unborn baby).
Your ovaries are held in place by various ligaments which anchor them to your uterus and the pelvis. The ovary contains ovarian follicles, in which eggs develop. Once a follicle is mature, it ruptures and the developing egg is ejected from the ovary into the fallopian tubes. This is called ovulation. Ovulation occurs in the middle of the menstrual cycle and usually takes place every 28 days or so in a mature female. It takes place from either the right or left ovary at random.
Your ovaries are mainly made up of 3 kinds of cells. Each type of cell can develop into a different type of tumor:
- Epithelial tumors start from the cells that cover the outer surface of the ovary. Most ovarian tumors are epithelial cell tumors.
- Germ cell tumors start from the cells that produce the eggs (ova).
- Stromal tumors start from structural tissue cells that hold the ovary together and produce the female hormones estrogen and progesterone.
Some of these tumors are benign (non-cancerous) and never spread beyond the ovary. Malignant (cancerous) or borderline (low malignant potential) ovarian tumors can spread (metastasize) to other parts of the body and can be fatal.
Figure 3. The ovaries lie in shallow depressions in the lateral wall of the pelvic cavity
Figure 4. Ovary blood supply
Figure 5. Ovary anatomy
Ovarian cancer types
Your ovaries are made up of different types of cells. The type of ovarian cancer you have depends on the type of cell it starts in.
The main types of ovarian cancer are 3:
- Epithelial ovarian cancers which start in the surface layer which covers the ovary, fallopian tube or peritoneum.
- Germ cell ovarian cancer which begins in the cells that develop into eggs.
- Sex cord stromal cancers which begin in the tissues that support your ovaries and produce hormones.
Knowing which type of ovarian cancer you have helps your doctors decide what treatment you need.
Epithelial ovarian tumors
Epithelial ovarian tumors start in the outer surface of the ovaries. These tumors can be benign (not cancer), borderline (low malignant potential), or malignant (cancer).
Benign epithelial ovarian tumors
Epithelial ovarian tumors that are benign don’t spread and usually don’t lead to serious illness. There are several types of benign epithelial tumors including serous cystadenomas, mucinous cystadenomas, and Brenner tumors.
Borderline epithelial tumors
When looked at in the lab, some ovarian epithelial tumors don’t clearly appear to be cancerous and are known as borderline epithelial ovarian cancer. Around 15 out of 100 ovarian tumors (15%) are borderline tumors. They are sometimes called atypical proliferative tumors or tumors of low malignant potential.
Borderline epithelial ovarian tumors are different to ovarian cancer because they don’t grow into the supportive tissue of the ovary (the stroma). They usually grow slowly and in a more controlled way than cancer cells.
Borderline epithelial ovarian tumors usually affect women aged between 20 and 40. They are usually diagnosed at an early stage. This means the abnormal cells are still within the ovary.
Sometimes abnormal cells break away from the tumor and settle elsewhere in the body. This is usually in the belly (abdomen). Very rarely, these cells start to grow into the underlying tissue.
There are different types of borderline ovarian tumors. The two most common types are atypical proliferative serous carcinoma and atypical proliferative mucinous carcinoma. These tumors were previously called tumors of low malignant potential (LMP tumors). These are different from typical ovarian cancers because they don’t grow into the supporting tissue of the ovary called the ovarian stroma. If they do spread outside the ovary, for example, into the abdominal cavity (belly), they might grow on the lining of the abdomen but not into it.
These tumors grow slowly and are less life-threatening than most ovarian cancers.
Malignant epithelial ovarian tumors
Cancerous epithelial tumors are called carcinomas. About 85% to 90% of malignant ovarian cancers are epithelial ovarian carcinomas. These tumor cells have several features (when looked at in the lab) that can be used to classify epithelial ovarian carcinomas into different types. The serous type is by far the most common, and can include high grade and low grade tumors. The other main types include mucinous, endometrioid, and clear cell.
- Serous carcinomas (52%)
- High grade serous carcinoma is the most common type of epithelial ovarian cancer. It can affect the ovaries, fallopian tubes or the peritoneum. Doctors think that most high grade serous carcinomas start in the cells at the end of the fallopian tube (fimbriae). These early cancer cells then spread to the ovary and grow. So they might sometimes be called fallopian tube cancer or tubo ovarian cancer.
- Low grade serous ovarian cancers are rare. They are usually diagnosed in younger people and are slow growing. Chemotherapy doesn’t tend to work as well as it does for other types of epithelial ovarian cancer.
- Endometroid carcinoma (10%)
- Endometrioid ovarian cancer is the 2nd most common type of epithelial ovarian cancer. It can be linked to endometriosis. Most cases of endometrioid ovarian cancer are diagnosed at an early stage and are low grade. Some women have endometroid ovarian cancer at the same time as a separate womb (endometrial) cancer.
- Clear cell carcinoma (6%)
- Clear cell ovarian cancer can also be linked to endometriosis. The treatment is the same as for high grade serous ovarian cancer. But chemotherapy doesn’t tend to work as well as it does for other types of epithelial ovarian cancer.
- Mucinous carcinoma (6%)
- Mucinous ovarian cancer is rare. It can be difficult to diagnose. The doctor does tests to check if the cancer started to grow in the ovary. Or if it spread there from somewhere else in your digestive system. Chemotherapy doesn’t tend to work as well for mucinous ovarian cancer. Mucinous tumors can be one of the following:
- non-cancerous (benign)
- borderline (contain abnormal cells but are not a cancer)
- cancerous (malignant)
- Mucinous ovarian cancer is rare. It can be difficult to diagnose. The doctor does tests to check if the cancer started to grow in the ovary. Or if it spread there from somewhere else in your digestive system. Chemotherapy doesn’t tend to work as well for mucinous ovarian cancer. Mucinous tumors can be one of the following:
- Undifferentiated or unclassifiable
- Some epithelial ovarian cancers are undifferentiated or unclassifiable. These cancers have cells that are very undeveloped. So it is not possible to tell which type of cell the cancer started from.
Each ovarian cancer is given a grade, based on how much the tumor cells look like normal tissue:
- Grade 1 epithelial ovarian carcinomas look more like normal tissue and tend to have a better prognosis (outlook).
- Grade 3 epithelial ovarian carcinomas look less like normal tissue and usually have a worse outlook.
Other traits are also taken into account, such as how fast the cancer cells grow and how well they respond to chemotherapy, to come up with the tumor’s type:
- Type 1 tumors tend to grow slowly and cause fewer symptoms. These tumors also seem not to respond well to chemotherapy. Low grade (grade 1) serous carcinoma, clear cell carcinoma, mucinous carcinoma and endometroid carcinoma are examples of type 1 tumors.
- Type 2 tumors grow fast and tend to spread sooner. These tumors tend to respond better to chemotherapy. High grade (grade 3) serous carcinoma is an example of a type 2 tumor.
Other cancers that are similar to epithelial ovarian cancer
Primary peritoneal carcinoma
Primary peritoneal carcinoma is a rare cancer closely related to epithelial ovarian cancer. At surgery, it looks the same as an epithelial ovarian cancer that has spread through the abdomen. In the lab, primary peritoneal carcinoma also looks just like epithelial ovarian cancer. Other names for this cancer include extra-ovarian (meaning outside the ovary) primary peritoneal carcinoma and serous surface papillary carcinoma.
Primary peritoneal carcinoma appears to start in the cells lining the inside of the fallopian tubes.
Like ovarian cancer, primary peritoneal carcinoma tends to spread along the surfaces of the pelvis and abdomen, so it is often difficult to tell exactly where the cancer first started. This type of cancer can occur in women who still have their ovaries, but it is of more concern for women who have had their ovaries removed to prevent ovarian cancer. This cancer does rarely occur in men.
Symptoms of primary peritoneal carcinoma are similar to those of ovarian cancer, including abdominal pain or bloating, nausea, vomiting, indigestion, and a change in bowel habits. Also, like ovarian cancer, primary peritoneal carcinoma may elevate the blood level of a tumor marker called CA-125.
Women with primary peritoneal carcinoma usually get the same treatment as those with widespread ovarian cancer. This could include surgery to remove as much of the cancer as possible (a process called debulking that is discussed in the section about surgery), followed by chemotherapy like that given for ovarian cancer. Its outlook is likely to be similar to widespread ovarian cancer.
Fallopian tube cancer
This is another rare cancer that is similar to epithelial ovarian cancer. It begins in the tube that carries an egg from the ovary to the uterus (the fallopian tube). Like primary peritoneal carcinoma, fallopian tube cancer and ovarian cancer have similar symptoms. The treatment for fallopian tube cancer is much like that for ovarian cancer, but the outlook (prognosis) is slightly better.
Ovarian germ cell tumors
Germ cells usually form the ova or eggs in females and the sperm in males. Germ cell ovarian tumors begin in the ovarian cells that develop into eggs (germ cells). They are rare and usually affect people up to their early 30s. Less than 2% of ovarian cancers are germ cell tumors. Most ovarian germ cell tumors are benign, but some are cancerous and may be life threatening. Overall, they have a good outlook, with more than 9 out of 10 patients surviving at least 5 years after diagnosis. You usually have surgery to remove the tumor. You might have chemotherapy if your tumor is cancerous. Treatment usually works well and most women are cured.
There are several subtypes of germ cell tumors. They can be non cancerous (benign) or cancerous (malignant).
Benign germ cell ovarian tumors
- Mature teratomas also called ovarian dermoid cysts are the most common type of ovarian germ cell tumor. They are non cancerous (benign). They are most common in women during their teens to their forties.
Malignant germ cell ovarian tumors
- These tumors contain cancer cells. There are different types including:
- immature teratomas
- dysgerminoma
- yolk sac tumor
- non gestational choriocarcinoma
- embryonal carcinoma
The most common germ cell tumors are teratomas, dysgerminomas, endodermal sinus tumors, and choriocarcinomas. Germ cell tumors can also be a mix of more than a single subtype.
Teratoma
Teratomas are germ cell tumors with areas that, when seen under the microscope, look like each of the 3 layers of a developing embryo: the endoderm (innermost layer), mesoderm (middle layer), and ectoderm (outer layer). This germ cell tumor has a benign form called mature teratoma and a cancerous form called immature teratoma.
The mature teratoma is by far the most common ovarian germ cell tumor. It is a benign tumor that usually affects women of reproductive age (teens through forties). It is often called a dermoid cyst because its lining is made up of tissue similar to skin (dermis). These tumors or cysts can contain different kinds of benign tissues including, bone, hair, and teeth. The patient is cured by surgical removal of the cyst, but sometimes a new cyst develops later in the other ovary.
Immature teratomas are a type of cancer. They occur in girls and young women, usually younger than 18. These are rare cancers that contain cells that look like those from embryonic or fetal tissues such as connective tissue, respiratory passages, and brain. Tumors that are relatively more mature (called grade 1 immature teratoma) and haven’t spread beyond the ovary are treated by surgical removal of the ovary. When they have spread beyond the ovary and/or much of the tumor has a very immature appearance (grade 2 or 3 immature teratomas), chemotherapy is recommended in addition to surgery.
Dysgerminoma
This type of cancer is rare, but it is the most common ovarian germ cell cancer. It usually affects women in their teens and twenties. Dysgerminomas are considered malignant (cancerous), but most don’t grow or spread very rapidly. When they are limited to the ovary, more than 75% of patients are cured by surgically removing the ovary, without any further treatment. Even when the tumor has spread further (or if it comes back later), surgery, radiation therapy, and/or chemotherapy are effective in controlling or curing the disease in about 90% of patients.
Endodermal sinus tumor (yolk sac tumor) and choriocarcinoma
These very rare tumors typically affect girls and young women. They tend to grow and spread rapidly but are usually very sensitive to chemotherapy. Choriocarcinoma that starts in the placenta (during pregnancy) is more common than the kind that starts in the ovary. Placental choriocarcinomas usually respond better to chemotherapy than ovarian choriocarcinomas do.
Ovarian stromal tumors
About 1% of ovarian cancers are ovarian stromal cell tumors. More than half of stromal tumors are found in women older than 50, but about 5% of stromal tumors occur in young girls.
The most common symptom of these tumors is abnormal vaginal bleeding. This happens because many of these tumors produce female hormones (estrogen). These hormones can cause vaginal bleeding (like a period) to start again after menopause. In young girls, these tumors can also cause menstrual periods and breast development to occur before puberty.
Less often, stromal tumors make male hormones (like testosterone). If male hormones are produced, the tumors can cause normal menstrual periods to stop. They can also make facial and body hair grow. If the stromal tumor starts to bleed, it can cause sudden, severe abdominal pain.
Types of malignant (cancerous) stromal tumors include granulosa cell tumors (the most common type), granulosa-theca tumors, and Sertoli-Leydig cell tumors, which are usually considered low-grade cancers. Thecomas and fibromas are benign stromal tumors. Cancerous stromal tumors are often found at an early stage and have a good outlook, with more than 75% of patients surviving long-term.
Ovarian cysts
An ovarian cyst is a collection of fluid inside an ovary. Most ovarian cysts occur as a normal part of the process of ovulation (egg release) — these are called functional cysts. These cysts usually go away within a few months without any treatment. If you develop a cyst, your doctor may want to check it again after your next menstrual cycle (period) to see if it has gotten smaller.
An ovarian cyst can be more concerning in a female who isn’t ovulating (like a woman after menopause or a girl who hasn’t started her periods), and the doctor may want to do more tests. The doctor may also order other tests if the cyst is large or if it does not go away in a few months. Even though most of these cysts are benign (not cancer), a small number of them could be cancer. Sometimes the only way to know for sure if the cyst is cancer is to take it out with surgery. Cysts that appear to be benign (based on how they look on imaging tests) can be observed (with repeated physical exams and imaging tests), or removed with surgery.
Ovarian cancer signs and symptoms
Early-stage ovarian cancer rarely causes any symptoms. Advanced-stage ovarian cancer may cause few and nonspecific symptoms that are often mistaken for more common benign conditions.
Signs and symptoms of ovarian cancer may include:
- Abdominal bloating or swelling
- Quickly feeling full when eating
- Weight loss
- Discomfort in the pelvis area
- Changes in bowel habits, such as constipation
- A frequent need to urinate
These symptoms are also commonly caused by benign (non-cancerous) diseases and by cancers of other organs. When they are caused by ovarian cancer, they tend to be persistent and a change from normal − for example, they occur more often or are more severe. These symptoms are more likely to be caused by other conditions, and most of them occur just about as often in women who don’t have ovarian cancer. But if you have these symptoms more than 12 times a month, see your doctor so the problem can be found and treated if necessary.
Others symptoms of ovarian cancer can include:
- Fatigue (extreme tiredness)
- Upset stomach
- Back pain
- Pain during sex
- Constipation
- Changes in a woman’s period, such as heavier bleeding than normal or irregular bleeding
- Abdominal (belly) swelling with weight loss
Early symptoms of ovarian cancer
The symptoms of ovarian cancer can be difficult to recognize, particularly in the early stages of the disease. They are often the same as the symptoms of other, less serious, conditions, such as irritable bowel syndrome (IBS) or premenstrual syndrome (PMS). However, the most common symptoms that may indicate ovarian cancer are:
- abdominal bloating or feeling full
- abdominal or back pain
- appetite loss or feeling full quickly
- changes in toilet habits
- needing to urinate more often
- unexplained weight loss or weight gain
- indigestion or heartburn
- fatigue
- bleeding in-between periods or after menopause
- indigestion or nausea
- pain during intercourse
If any of these symptoms are unusual for you, and they persist, it’s important to see your doctor. Many of these symptoms may be the result of other conditions in the pelvic area.
If you have any of these symptoms, keep a symptom diary to see how many of these symptoms you have over a longer period. Bear in mind that ovarian cancer is rare in women under 40 years of age. If you regularly have any of these symptoms, talk to your doctor. It’s unlikely that they are being caused by a serious problem, but it’s best to be checked.
If you’ve already seen your doctor and the symptoms continue or get worse, it is important to go back and explain this, as you know your body better than anyone.
Can ovarian cancer be found early?
Only about 20% of ovarian cancers are found at an early stage. When ovarian cancer is found early, about 94% of patients live longer than 5 years after diagnosis.
The National Institute for Health and Care Excellence recommends that if you (especially if 50 or over) have the following symptoms on a persistent or frequent basis – particularly more than 12 times per month, your doctor should arrange tests – especially if you’re are over 50 4:
- persistent swollen tummy (abdomen) or bloating
- feeling full (early satiety) and/or loss of appetite
- pelvic or abdominal pain
- increased urinary urgency and/or frequency.
First tests:
- Measure serum cancer antigen 125 (CA125) in primary care in women with symptoms that suggest ovarian cancer
- If serum CA125 is 35 IU/ml or greater, arrange an ultrasound scan of the abdomen and pelvis.
- For any woman who has normal serum CA125 (less than 35 IU/ml), or CA125 of 35 IU/ml or greater but a normal ultrasound:
- assess her carefully for other clinical causes of her symptoms and investigate if appropriate
- if no other clinical cause is apparent, advise her to return to her doctor if her symptoms become more frequent and/or persistent.
Ways to find ovarian cancer early
Regular women’s health exams
During a pelvic exam, the health care professional feels the ovaries and uterus for size, shape, and consistency. A pelvic exam can be useful because it can find some female cancers at an early stage, but most early ovarian tumors are difficult or impossible to feel. Pelvic exams may, however, help find other cancers or female conditions. Women should discuss the need for these exams with their doctor.
The Pap test is effective in early detection of cervical cancer, but it isn’t a test for ovarian cancer. Rarely, ovarian cancers are found through Pap tests, but usually they are at an advanced stage.
See a doctor if you have symptoms
Early cancers of the ovaries often cause no symptoms. Symptoms of ovarian cancer can also be caused by other, less serious conditions. By the time ovarian cancer is considered as a possible cause of these symptoms, it usually has already spread. Also, some types of ovarian cancer can rapidly spread to nearby organs. Prompt attention to symptoms may improve the odds of early diagnosis and successful treatment. If you have symptoms similar to those of ovarian cancer almost daily for more than a few weeks, report them right away to your health care professional.
Screening tests for ovarian cancer
Screening tests and exams are used to detect a disease, like cancer, in people who don’t have any symptoms. (For example, a mammogram can often detect breast cancer in its earliest stage, even before a doctor can feel the cancer.)
There has been a lot of research to develop a screening test for ovarian cancer, but there hasn’t been much success so far. The 2 tests used most often (in addition to a complete pelvic exam) to screen for ovarian cancer are transvaginal ultrasound (TVUS) and the CA-125 blood test.
- TVUS (transvaginal ultrasound) is a test that uses sound waves to look at the uterus, fallopian tubes, and ovaries by putting an ultrasound wand into the vagina. It can help find a mass (tumor) in the ovary, but it can’t actually tell if a mass is cancer or benign. When it is used for screening, most of the masses found are not cancer.
- CA-125 blood test measures the amount of a protein called CA-125 in your blood. Many women with ovarian cancer have high levels of CA-125. This test can be useful as a tumor marker to help guide treatment in women known to have ovarian cancer, because a high level often goes down if treatment is working. But checking CA-125 levels has not been found to be as useful as a screening test for ovarian cancer. The problem with using this test for ovarian cancer screening is that high levels of CA-125 is more often caused by common conditions such as endometriosis and pelvic inflammatory disease. Also, not everyone who has ovarian cancer has a high CA-125 level. When someone who is not known to have ovarian cancer has an abnormal CA-125 level, the doctor might repeat the test (to make sure the result is correct) and may consider ordering a transvaginal ultrasound test.
Better ways to screen for ovarian cancer are being researched but currently there are no reliable screening tests. Hopefully, improvements in screening tests will eventually lead to fewer deaths from ovarian cancer.
If you’re at average risk
There are no recommended screening tests for ovarian cancer for women who do not have symptoms and are not at high risk of developing ovarian cancer. In studies of women at average risk of ovarian cancer, using transvaginal ultrasound (TVUS) and CA-125 for screening led to more testing and sometimes more surgeries, but did not lower the number of deaths caused by ovarian cancer. For that reason, no major medical or professional organization recommends the routine use of transvaginal ultrasound (TVUS) or the CA-125 blood test to screen for ovarian cancer in women at average risk.
If you’re at high risk
Some organizations state that transvaginal ultrasound (TVUS) and CA-125 may be offered to screen women who have a high risk of ovarian cancer due to an inherited genetic syndrome such as Lynch syndrome, BRCA gene mutations or a strong family history of breast and ovarian cancer. Still, even in these women, it has not been proven that using these tests for screening lowers their chances of dying from ovarian cancer.
Screening tests for germ cell tumors/stromal tumors
There are no recommended screening tests for germ cell tumors or stromal tumors. Some germ cell cancers release certain protein markers such as human chorionic gonadotropin (hCG) and alpha-fetoprotein (AFP) into the blood. After these tumors have been treated by surgery and chemotherapy, blood tests for these markers can be used to see if treatment is working and to determine if the cancer is coming back.
Ovarian cancer causes
Scientists don’t yet know exactly what causes most ovarian cancers. Scientists do know some risk factors that make a woman more likely to develop epithelial ovarian cancer. Much less is known about risk factors for germ cell and stromal tumors of the ovaries.
The most recent and important finding about the cause of ovarian cancer is that it starts in cells at the tail ends of the fallopian tubes and not necessarily in the ovary itself. This new information may open more research studies looking at preventing and screening for this type of cancer.
There are many theories about the causes of ovarian cancer. Some of them came from looking at the things that change the risk of ovarian cancer. For example, pregnancy and taking birth control pills both lower the risk of ovarian cancer. Since both of these things reduce the number of times the ovary releases an egg (ovulation), some researchers think that there may be some relationship between ovulation and the risk of developing ovarian cancer.
Also, experts know that tubal ligation and hysterectomy lower the risk of ovarian cancer. One theory to explain this is that some cancer-causing substances may enter the body through the vagina and pass through the uterus and fallopian tubes to reach the ovaries. This would explain how removing the uterus or blocking the fallopian tubes affects ovarian cancer risk.
Another theory is that male hormones (androgens) can cause ovarian cancer.
Researchers have made great progress in understanding how certain mutations (changes) in DNA can cause normal cells to become cancerous. DNA is the chemical that carries the instructions for nearly everything your cells do. You usually look like your parents because they are the source of your DNA. However, DNA affects more than the way you look. Some genes (parts of your DNA) contain instructions for controlling when our cells grow and divide. Mutations in these genes can lead to the development of cancer.
Inherited genetic mutations
Between 5 and 15 out of 100 ovarian cancers (5 to 15%) are caused by an inherited faulty gene. Inherited genes that increase the risk of ovarian cancer include faulty versions of BRCA1 and BRCA2 genes. Faults in BRCA1 and BRCA2 genes also increase the risk of breast cancer.
Other inherited faulty genes such as PTEN (PTEN tumor hamartoma syndrome), STK11 (Peutz-Jeghers syndrome), MUTYH (MUTYH-asociated polyposis, and the many genes that can cause hereditary nonpolyposis colon cancer (MLH1, MLH3, MSH2, MSH6, TGFBR2, PMS1, and PMS2) are related to other family cancer syndromes and linked to an increased risk of ovarian cancer.
Besides the gene mutations mentioned above, there are other genes linked to ovarian cancer. These include ATM, BRIP1, RAD51C, RAD51D, and PALB2. Some of these genes are also associated with cancers such as breast and pancreas.
Having relatives with ovarian cancer does not necessarily mean that you have a faulty inherited gene in the family. The cancers could have happened by chance. But women with a mother or sister diagnosed with ovarian cancer have around 3 times the risk of ovarian cancer. This is compared to women without a family history.
Genetic tests can detect mutations associated with these inherited syndromes. If you have a family history of cancers linked to these syndromes, such as breast and ovarian cancers, thyroid and ovarian cancer, and/or colorectal and endometrial (uterine) cancer, you might want to ask your doctor about genetic counseling and testing. The American Cancer Society recommends discussing genetic testing with a qualified cancer genetics professional before any genetic testing is done.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://findageneticcounselor.nsgc.org) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://abgc.learningbuilder.com/Search/Public/MemberRole/Verification) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (https://www.acmg.net/ACMG/Directories.aspx) has a searchable database of medical genetics clinic services in the United States.
Acquired genetic changes
Most mutations related to ovarian cancer are not inherited but instead occur during a woman’s life and are called acquired mutations. In some cancers, these types of mutations leading to the development of cancer may result from radiation or cancer-causing chemicals, but there is no evidence for this in ovarian cancer. So far, studies haven’t been able to specifically link any single chemical in the environment or in our diets to mutations that cause ovarian cancer. The cause of most acquired mutations remains unknown.
Most ovarian cancers have several acquired mutations. Research has suggested that tests to identify acquired mutations in ovarian cancers, like the TP53 tumor suppressor gene or the HER2 oncogene, can help predict a woman’s prognosis. The role of these tests is still not certain, and more research is needed.
Ovarian cancer risk factors
A risk factor is anything that increases your chance of getting a disease like cancer. Generally, it’s not possible to say what causes ovarian cancer in an individual woman. However, some features are more common among women who have developed ovarian cancer. These features are called risk factors. Having certain risk factors increases a woman’s chance of developing ovarian cancer.
Having one or more risk factors for ovarian cancer doesn’t mean a woman will definitely develop ovarian cancer. In fact, many women with ovarian cancer have no obvious risk factors.
Factors that increase your risk of ovarian cancers
Getting older
The risk of developing ovarian cancer gets higher with age. Ovarian cancer is rare in women younger than 40. The risk of ovarian cancer increases steeply from around 45 years. Most ovarian cancers develop after menopause. And is greatest in those aged between 75 and 79 years. Half of all ovarian cancers are found in women 63 years of age or older.
Being overweight or obese
Obesity has been linked to a higher risk of developing many cancers. The current information available for ovarian cancer risk and obesity is not clear. Obese women (those with a body mass index [BMI] of at least 30) may have a higher risk of developing ovarian cancer, but not necessarily the most aggressive types, such as high grade serous cancers. Obesity may also affect the overall survival of a woman with ovarian cancer.
Having children later or never having a full-term pregnancy
Women who have their first full-term pregnancy after age 35 or who never carried a pregnancy to term have a higher risk of ovarian cancer.
Using fertility treatment
Fertility treatment with in vitro fertilization (IVF) seems to increase the risk of the type of ovarian tumors known as “borderline” or “low malignant potential” (LMP tumors). Other studies, however, have not shown an increased risk of invasive ovarian cancer with fertility drugs. If you are taking fertility drugs, you should discuss the potential risks with your doctor.
Taking hormone therapy after menopause
Women using estrogens after menopause have an increased risk of developing ovarian cancer. The risk seems to be higher in women taking estrogen alone (without progesterone) for many years (at least 5 or 10). The increased risk is less certain for women taking both estrogen and progesterone.
Having a family history of ovarian cancer, breast cancer, or colorectal cancer
Ovarian cancer can run in families. Your ovarian cancer risk is increased if your mother, sister, or daughter has (or has had) ovarian cancer. The risk also gets higher the more relatives you have with ovarian cancer. Increased risk for ovarian cancer can also come from your father’s side.
A family history of some other types of cancer such as colorectal and breast cancer is linked to an increased risk of ovarian cancer. This is because these cancers can be caused by an inherited mutation (change) in certain genes that cause a family cancer syndrome that increases the risk of ovarian cancer.
Having a family cancer syndrome
About 5 to 10% of ovarian cancers are a part of family cancer syndromes resulting from inherited changes (mutations) in certain genes.
Hereditary breast and ovarian cancer syndrome
This syndrome is caused by inherited mutations in the genes BRCA1 and BRCA2, as well as possibly some other genes that have not yet been found. This syndrome is linked to a high risk of breast cancer as well as ovarian, fallopian tube, and primary peritoneal cancers. The risk of some other cancers, such as pancreatic cancer and prostate cancer, are also increased.
Mutations in BRCA1 and BRCA2 are also responsible for most inherited ovarian cancers. Mutations in BRCA1 and BRCA2 are about 10 times more common in those who are Ashkenazi Jewish than those in the general U.S. population.
The lifetime ovarian cancer risk for women with a BRCA1 mutation is estimated to be between 35% and 70%. This means that if 100 women had a BRCA1 mutation, between 35 and 70 of them would get ovarian cancer. For women with BRCA2 mutations the risk has been estimated to be between 10% and 30% by age 70. These mutations also increase the risks for primary peritoneal carcinoma and fallopian tube carcinoma.
In comparison, the ovarian cancer lifetime risk for the women in the general population is less than 2%.
PTEN tumor hamartoma syndrome
In this syndrome, also known as Cowden disease, people are primarily affected with thyroid problems, thyroid cancer, and breast cancer. Women also have an increased risk of endometrial and ovarian cancer. It is caused by inherited mutations in the PTEN gene.
Hereditary nonpolyposis colon cancer
Women with this syndrome have a very high risk of colon cancer and also have an increased risk of developing cancer of the uterus (endometrial cancer) and ovarian cancer. Many different genes can cause this syndrome. They include MLH1, MLH3, MSH2, MSH6, TGFBR2, PMS1, and PMS2. The lifetime risk of ovarian cancer in women with hereditary nonpolyposis colon cancer (Lynch syndrome) is about 10%. Up to 1% of all ovarian epithelial cancers occur in women with hereditary nonpolyposis colon cancer (Lynch syndrome).
Peutz-Jeghers syndrome
People with this rare genetic syndrome develop polyps in the stomach and intestine while they are teenagers. They also have a high risk of cancer, particularly cancers of the digestive tract (esophagus, stomach, small intestine, colon). Women with this syndrome have an increased risk of ovarian cancer, including both epithelial ovarian cancer and a type of stromal tumor called sex cord tumor with annular tubules (SCTAT). This syndrome is caused by mutations in the gene STK11.
MUTYH-associated polyposis
People with this syndrome develop polyps in the colon and small intestine and have a high risk of colon cancer. They are also more likely to develop other cancers, including cancers of the ovary and bladder. This syndrome is caused by mutations in the gene MUTYH.
Having had breast cancer
If you have had breast cancer, you might also have an increased risk of developing ovarian cancer. There are several reasons for this. Some of the reproductive risk factors for ovarian cancer may also affect breast cancer risk. The risk of ovarian cancer after breast cancer is highest in those women with a family history of breast cancer. A strong family history of breast cancer may be caused by an inherited mutation in the BRCA1 or BRCA2 genes and hereditary breast and ovarian cancer syndrome, which is linked to an increased risk of ovarian cancer.
Endometriosis or diabetes
Studies have shown that women with endometriosis or diabetes have an increased risk of ovarian cancer. In diabetics, the increase in risk might be higher in those that use insulin.
Smoking and alcohol use
Smoking doesn’t increase the risk of ovarian cancer overall, but it is linked to an increased risk for the mucinous ovarian cancer. The longer you have smoked, the greater your risk.
Drinking alcohol is not linked to ovarian cancer risk.
Asbestos
Asbestos is an insulating material that’s heat and fire resistant. The International Agency for Research on Cancer (IARC) classify asbestos as a cause of ovarian cancer. The use of asbestos was banned in the late 1990s in the US. Asbestos was widely used in:
- building industry
- shipbuilding
- manufacturing of household appliances
- motor industry
- power stations
- telephone exchanges
There are 3 main types of asbestos – blue, brown and white.
Asbestos is made up of tiny fibers. You can breathe these fibers in when you come into contact with asbestos.
Factors with unclear effects on ovarian cancer risk
Androgens
Androgens, such as testosterone, are male hormones. There appears to be a link between certain androgens and specific types of ovarian cancer, but further studies of the role of androgens in ovarian cancer are needed.
Talcum powder
It has been suggested that talcum powder might cause cancer in the ovaries if the powder particles (applied to the genital area or on sanitary napkins, diaphragms, or condoms) were to travel through the vagina, uterus, and fallopian tubes to the ovary.
Many studies in women have looked at the possible link between talcum powder and cancer of the ovary. Findings have been mixed, with some studies reporting a slightly increased risk and some reporting no increase. Many case-control studies have found a small increase in risk. But these types of studies can be biased because they often rely on a person’s memory of talc use many years earlier. One prospective cohort study, which would not have the same type of potential bias, has not found an increased risk. A second found a modest increase in risk of one type of ovarian cancer.
For any individual woman, if there is an increased risk, the overall increase is likely to very be small. Still, talc is widely used in many products, so it is important to determine if the increased risk is real. Research in this area continues.
Diet
Some studies have shown a reduced rate of ovarian cancer in women who ate a diet high in vegetables or a low fat diet, but other studies disagree. The American Cancer Society recommends eating a variety of healthful foods, with an emphasis on plant sources. Eat at least 2 ½ cups of fruits and vegetables every day, as well as several servings of whole grain foods from plant sources such as breads, cereals, grain products, rice, pasta, or beans. Limit the amount of red meat and processed meats you eat. Even though the effect of these dietary recommendations on ovarian cancer risk remains uncertain, following them can help prevent several other diseases, including some other types of cancer.
Factors that can lower risk of ovarian cancer
Pregnancy and breastfeeding
Women who have been pregnant and carried it to term before age 26 have a lower risk of ovarian cancer than women who have not. The risk goes down with each full-term pregnancy. Breastfeeding may lower the risk even further.
Birth control
Women who have used oral contraceptives also known as birth control pills or the pill have a lower risk of ovarian cancer. The risk is lower the longer the pills are used. This lower risk continues for many years after the pill is stopped. Other forms of birth control such as tubal ligation (having fallopian tubes tied) and short use of IUDs (intrauterine devices) have also been associated with a lower risk of ovarian cancer.
Having a hysterectomy or having your tubes tied
Having your tubes tied because you don’t want any more pregnancies is called sterilization. Studies have found that having your fallopian tubes tied reduces your risk of ovarian cancer.
Until recently, most research has shown that having your womb removed (hysterectomy) may also reduce your risk of ovarian cancer. But this has become less clear in recent years. It might depend on several factors including your age when you had the operation. Any reduction in risk may be greater for younger women. Researchers continue to study this area.
A hysterectomy (removing the uterus without removing the ovaries) also seems to reduce the risk of getting ovarian cancer by about one-third.
Ovarian cancer prevention
Most women have one or more risk factors for ovarian cancer. But most of the common factors only slightly increase your risk, so they only partly explain the frequency of the disease. So far, what is known about risk factors has not translated into practical ways to prevent most cases of ovarian cancer.
There are several ways you can reduce your risk of developing the most common type of ovarian cancer, epithelial ovarian cancer. Much less is known about ways to lower the risk of developing germ cell and stromal tumors of the ovaries, so this information does not apply to those types. It is important to realize that some of these strategies lower your risk only slightly, while others lower it much more. Some strategies are easily followed, and others require surgery. If you are concerned about your risk of ovarian cancer, talk to your health care professionals. They can help you consider these ideas as they apply to your own situation.
Avoiding certain risk factors
Some risk factors for ovarian cancer, like getting older or having a family history, cannot be changed. But women might be able to lower their risk slightly by avoiding other risk factors, for example, by staying at a healthy weight, or not taking hormone replacement therapy after menopause.
Oral contraceptives
Using oral contraceptives (birth control pills) decreases the risk of developing ovarian cancer for average risk women and BRCA mutation carriers , especially among women who use them for several years. Women who used oral contraceptives for 5 or more years have about a 50% lower risk of developing ovarian cancer compared with women who never used oral contraceptives. Still, birth control pills do have some serious risks and side effects such as slightly increasing breast cancer risk. Women considering taking these drugs for any reason should first discuss the possible risks and benefits with their doctor.
Gynecologic surgery
Both tubal ligation and hysterectomy may reduce the chance of developing certain types of ovarian cancer, but experts agree that these operations should only be done for valid medical reasons — not for their effect on ovarian cancer risk.
If you are going to have a hysterectomy for a valid medical reason and you have a strong family history of ovarian or breast cancer, you may want to consider having both ovaries and fallopian tubes removed called a bilateral salpingo-oophorectomy as part of that procedure.
Even if you don’t have an increased risk of ovarian cancer, some doctors recommend that the ovaries be removed with the uterus if a woman has already gone through menopause or is close to menopause. If you are older than 40 and you are going to have a hysterectomy, you should discuss the potential risks and benefits of having your ovaries removed with your doctor.
Another option for average risk women who do not wish to have their ovaries removed because they don’t want to lose ovarian function (and go through menopause early) is to have just the fallopian tubes removed (a bilateral salpingectomy) along with the uterus (a hysterectomy). They may choose to have their ovaries removed later. This has not been studied as well as removing both the ovaries and fallopian tubes at the same time, but there is enough information that it may be considered an option to reduce ovarian cancer risk in average risk women.
Prevention strategies for women with a family history of ovarian cancer or BRCA mutation
If your family history suggests that you (or a close relative) might have a syndrome linked with a high risk of ovarian cancer, you might want to consider genetic counseling and testing. During genetic counseling (by a genetic counselor or other health care professional with training in genetic risk evaluation), your personal medical and family history is reviewed. This can help predict whether you are likely to have one of the gene mutations associated with an increased ovarian cancer risk.
The counselor will also discuss the benefits and potential drawbacks of genetic testing with you. Genetic testing can help determine if you or members of your family carry certain gene mutations that cause a high risk of ovarian cancer. Still, the results are not always clear, and a genetic counselor can help you sort out what the results mean to you.
For some women with a strong family history of ovarian cancer, knowing they do not have a mutation that increases their ovarian cancer risk can be a great relief for them and their children. Knowing that you do have such a mutation can be stressful, but many women find this information very helpful in making important decisions about certain prevention strategies for them and their children.
Using oral contraceptives is one way that high risk women (women with BRCA1 and BRCA2 mutations) can reduce their risk of developing ovarian cancer. But birth control pills can increase breast cancer risk in women with or without these mutations. This increased risk appears highest while women are actively taking birth control pills but can continue even after stopping them. Research is continuing to find out more about the risks and benefits of oral contraceptives for women at high ovarian and breast cancer risk.
Tubal ligation may also effectively reduce the risk of ovarian cancer in women who have BRCA1 or BRCA2 mutations. Usually this type of surgery is not done alone and is typically done for reasons other than ovarian cancer prevention.
Sometimes a woman may want to consider having both ovaries and fallopian tubes removed (called a bilateral salpingo-oophorectomy) to reduce her risk of ovarian cancer before cancer is even suspected. If the ovaries are removed to prevent ovarian cancer, the surgery is called risk-reducing or prophylactic. Generally, salpingo-oophorectomy may be recommended for high-risk women after they have finished having children. This operation lowers ovarian cancer risk a great deal but does not entirely eliminate it. That’s because some women who have a high risk of ovarian cancer already have a cancer at the time of surgery. These cancers can be so small that they are only found when the ovaries and fallopian tubes are looked at in the lab after they are removed. Also, women with BRCA1 or BRCA2 gene mutations have an increased risk of primary peritoneal carcinoma. Although the risk is low, this cancer can still develop after the ovaries and fallopian tubes are removed.
The risk of fallopian tube cancer is also increased in women with mutations in BRCA1 or BRCA2. Sometimes early fallopian tube cancers are found unexpectedly when the fallopian tubes are removed as a part of a risk-reducing surgery. In fact, some cancers that were thought to be ovarian or primary peritoneal cancers may have actually started in the fallopian tubes. That is why experts recommend that women at high risk of ovarian cancer who are having their ovaries removed should have their fallopian tubes completely removed as well (salpingo-oophorectomy).
Research has shown that premenopausal women who have BRCA gene mutations and have had their ovaries removed reduce their risk of breast cancer as well as their risk of ovarian cancer. The risk of ovarian cancer is reduced by 85% to 95%, and the risk of breast cancer cut by 50% or more.
Some women who have a high risk of ovarian cancer due to BRCA gene mutations feel that having their ovaries and fallopian tubes removed is not right for them. Often doctors recommend that those women have screening tests to try to find ovarian cancer early.
Ovarian cancer diagnosis
If your doctor finds something suspicious during a pelvic exam, or if you have symptoms that might be due to ovarian cancer, your doctor, will recommend exams and tests to find the cause.
Medical history and physical exam
Your doctor will ask about your medical history to learn about possible risk factors, including your family history. You will also be asked if you’re having any symptoms, when they started, and how long you’ve had them. Your doctor will likely do a pelvic exam to check for an enlarged ovary or signs of fluid in the abdomen (which is called ascites). During a pelvic exam, your doctor inserts gloved fingers into your vagina and simultaneously presses a hand on your abdomen in order to feel (palpate) your pelvic organs. The doctor also visually examines your external genitalia, vagina and cervix.
If there is reason to suspect you have ovarian cancer based on your symptoms and/or physical exam, your doctor will order some tests to check further.
Surgery
Sometimes your doctor can’t be certain of your diagnosis until you undergo surgery to remove an ovary and have it tested for signs of cancer.
Consultation with a specialist
If the results of your pelvic exam or other tests suggest that you have ovarian cancer, you will need a doctor or surgeon who specializes in treating women with this type of cancer. A gynecologic oncologist is an obstetrician/gynecologist who is specially trained in treating cancers of the female reproductive system. Treatment by a gynecologic oncologist helps ensure that you get the best kind of surgery for your cancer. It has also has been shown to help patients with ovarian cancer live longer. Anyone suspected of having ovarian cancer should see this type of specialist before having surgery.
Ovarian cancer tests
Imaging tests
Doctors use imaging tests to take pictures of the inside of your body. Imaging tests can show whether a pelvic mass is present, but they cannot confirm that the mass is a cancer. These tests are also useful if your doctor is looking to see if ovarian cancer has spread (metastasized) to other tissues and organs.
Ultrasound
Ultrasound (ultrasonography) uses sound waves to create an image on a video screen. Sound waves are released from a small probe placed in the woman’s vagina and a small microphone-like instrument called a transducer gives off sound waves and picks up the echoes as they bounce off organs. A computer turns these echoes into an image on the screen.
Ultrasound is often the first test done if a problem with the ovaries is suspected. It can be used to find an ovarian tumor and to check if it is a solid mass (tumor) or a fluid-filled cyst. It can also be used to get a better look at the ovary to see how big it is and how it looks inside. This helps the doctor decide which masses or cysts are more worrisome.
Computed tomography (CT) scans
The CT scan is an x-ray test that makes detailed cross-sectional images of your body. The test can help tell if ovarian cancer has spread to other organs.
CT scans do not show small ovarian tumors well, but they can see larger tumors, and may be able to see if the tumor is growing into nearby structures. A CT scan may also find enlarged lymph nodes, signs of cancer spread to liver or other organs, or signs that an ovarian tumor is affecting your kidneys or bladder.
CT scans are not usually used to biopsy an ovarian tumor (see biopsy in the section “Other tests”), but they can be used to biopsy a suspected metastasis (area of spread). For this procedure, called a CT-guided needle biopsy, the patient stays on the CT scanning table, while a radiologist moves a biopsy needle toward the mass. CT scans are repeated until the doctors are confident that the needle is in the mass. A fine needle biopsy sample (tiny fragment of tissue) or a core needle biopsy sample (a thin cylinder of tissue about ½ inch long and less than 1/8 inch in diameter) is removed and examined in the lab.
Barium enema x-ray
A barium enema is a test to see if the cancer has invaded the colon (large intestine) or rectum. This test is rarely used for women with ovarian cancer. Colonoscopy may be done instead.
Magnetic resonance imaging (MRI) scans
MRI scans also create cross-section pictures of your insides. But MRI uses strong magnets to make the images – not x-rays. A contrast material called gadolinium may be injected into a vein before the scan to see details better.
MRI scans are not used often to look for ovarian cancer, but they are particularly helpful to examine the brain and spinal cord where cancer could spread.
Chest x-ray
An x-ray might be done to determine whether ovarian cancer has spread (metastasized) to the lungs. This spread may cause one or more tumors in the lungs and more often causes fluid to collect around the lungs. This fluid, called a pleural effusion, can be seen with chest x-rays as well as other types of scans.
Positron emission tomography (PET) scan
For a PET scan, radioactive glucose (sugar) is given to look for the cancer. PET scans can help find cancer when it has spread, but are not used often to look for ovarian cancer. Body cells take in different amounts of the sugar, depending on how fast they are growing. Cancer cells, which grow quickly, are more likely to take up larger amounts of the sugar than normal cells. A special camera is used to create a picture of areas of radioactivity in the body.
The picture from a PET scan is not as detailed as a CT or MRI scan, but it provides helpful information about whether abnormal areas seen on these other tests are likely to be cancer or not.
If you have already been diagnosed with cancer, your doctor may use this test to see if the cancer has spread to lymph nodes or other parts of the body. A PET scan can also be useful if your doctor thinks the cancer may have spread but doesn’t know where.
PET/CT scan: Some machines can do both a PET and CT scan at the same time. This lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed picture of that area on the CT scan.
Other tests
Laparoscopy
This procedure uses a thin, lighted tube through which a doctor can look at the ovaries and other pelvic organs and tissues in the area. The tube is inserted through a small incision (cut) in the lower abdomen and sends the images of the pelvis or abdomen to a video monitor. Laparoscopy provides a view of organs that can help plan surgery or other treatments and can help doctors confirm the stage (how far the tumor has spread) of the cancer. Also, doctors can manipulate small instruments through the laparoscopic incision(s) to perform biopsies.
Colonoscopy
A colonoscopy is a way to examine the inside of the large intestine (colon). The doctor looks at the entire length of the colon and rectum with a colonoscope, a thin, flexible, lighted tube with a small video camera on the end. It is inserted through the anus and into the rectum and the colon. Any abnormal areas seen can by biopsied. This procedure is more commonly used to look for colorectal cancer.
Biopsy
The only way to determine for certain if a growth is cancer is to remove a piece of it and examine it in the lab. This procedure is called a biopsy. For ovarian cancer, the biopsy is most commonly done by removing the tumor during surgery.
In rare cases, a suspected ovarian cancer may be biopsied during a laparoscopy procedure or with a needle placed directly into the tumor through the skin of the abdomen. Usually the needle will be guided by either ultrasound or CT scan. This is only done if you cannot have surgery because of advanced cancer or some other serious medical condition, because there is concern that a biopsy could spread the cancer.
If you have ascites (fluid buildup inside the abdomen), samples of the fluid can also be used to diagnose the cancer. In this procedure, called paracentesis, the skin of the abdomen is numbed and a needle attached to a syringe is passed through the abdominal wall into the fluid in the abdominal cavity. Ultrasound may be used to guide the needle. The fluid is taken up into the syringe and then sent for analysis to see if it contains cancer cells.
In all these procedures, the tissue or fluid obtained is sent to the lab. There it is examined by a pathologist, a doctor who specialize in diagnosing and classifying diseases by examining cells under a microscope and using other lab tests.
Blood tests
Your doctor will order blood count tests to make sure you have enough red blood cells, white blood cells and platelets (cells that help stop bleeding). There will also be tests to measure your kidney and liver function as well as your general health. The doctor will also order a CA-125 test. Women who have a high CA-125 level are often referred to a gynecologic oncologist, but any woman with suspected ovarian cancer should see a gynecologic oncologist, as well.
Some germ cell cancers can cause elevated blood levels of the tumor markers human chorionic gonadotropin (HCG), alpha-fetoprotein (AFP), and/or lactate dehydrogenase (LDH). These may be checked if your doctor suspects that your ovarian tumor could be a germ cell tumor.
Some ovarian stromal tumors cause the blood levels of a substance called inhibin and hormones such as estrogen and testosterone to go up. These levels may be checked if your doctor suspects that you have this type of tumor.
Lab tests for gene or protein changes
In some ovarian cancers, doctors might look for specific gene or protein changes in the cancer cells that could mean certain targeted or immunotherapy drugs might help treat the cancer. These tests can be done on a piece of the cancer taken during a biopsy or surgery for ovarian cancer.
- BRCA1 and BRCA2 gene mutations: BRCA genes are normally involved in DNA repair, and mutations in these genes can cause cells to grow out of control and turn into cancer. Ovarian cancers with BRCA gene mutations are more likely to be helped by treatment with targeted drugs called PARP inhibitors.
- Folate receptor-alpha (FR-alpha) testing: In many ovarian cancers, the cells have high levels of the FR-alpha protein on their surfaces. Testing for FR-alpha levels can show if the cancer is more likely to respond to treatment with a targeted drug such as mirvetuximab soravtansine (Elahere).
- NTRK gene mutations: Some ovarian cancers might be tested for changes in one of the NTRK genes. Cells with these gene changes can lead to abnormal cell growth and cancer. Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek) are targeted drugs that stop the proteins made by the abnormal NTRK genes. The number of ovarian cancers that have this mutation is very small, but this may be an option for some women.
- MSI and MMR gene testing: Women who have clear cell, endometrioid, or mucinous ovarian cancer might have their tumor tested to see if it shows high levels of gene changes called microsatellite instability (MSI). Testing might also be done to see if the cancer cells have changes in any of the mismatch repair (MMR) genes (MLH1, MSH2, MSH6, and PMS2). Changes in MSI or in MMR genes (or both) are often seen in people with Lynch syndrome (HNPCC). Up to 10% of all ovarian epithelial cancers have changes in these genes.
There are 2 possible reasons to test ovarian cancers for MSI or for MMR gene changes:
- To identify patients who should be tested for Lynch syndrome. A diagnosis of Lynch syndrome can help determine if a person should have screenings for other types of cancer, such as endometrial or colon cancer. If a person does have Lynch syndrome, their relatives could also have it, and may want to be tested for it.
- To determine treatment options for ovarian cancer. Ovarian cancers that have certain MSI or MMR gene changes might be treated with certain immunotherapy drugs known as checkpoint inhibitors.
Genetic counseling and testing if you have ovarian cancer
If you have been diagnosed with an epithelial ovarian cancer, your doctor will likely recommend that you get genetic counseling to help you decide if you should be tested for certain inherited gene changes, such as a mutation in the BRCA1 or BRCA2 gene. Some ovarian cancers are linked to mutations in these or other genes.
Genetic testing to look for inherited mutations can be helpful in several ways:
- If you are found to have a gene mutation, you might be more likely to get other types of cancer as well, so you might benefit from doing what you can to lower your risk of these cancers, as well as having tests to find them early.
- If you have a gene mutation, your family members (blood relatives) might also have it, so they can decide if they want to be tested to learn more about their cancer risk.
- If you have a BRCA1 or BRCA2 mutation, at some point you might benefit from treatment with targeted drugs called PARP inhibitors.
You may have heard about some home-based genetic tests. There is a concern that these tests are promoted by companies without giving full information. For example, a test for a small number of BRCA1 and BRCA2 gene mutations has been approved by the FDA. However, there are more than 1,000 known BRCA mutations, and the ones included in the approved test are not the most common ones. This means there are many BRCA mutations that would not be detected by this test.
A genetic counselor or other qualified medical professional can help you understand the pros, cons, and possible limits of what genetic testing can tell you. This can help you decide if testing is right for you, and which testing is best.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://findageneticcounselor.nsgc.org) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://abgc.learningbuilder.com/Search/Public/MemberRole/Verification) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (https://www.acmg.net/ACMG/Directories.aspx) has a searchable database of medical genetics clinic services in the United States.
Ovarian cancer stages
After a woman is diagnosed with ovarian cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
Ovarian cancer stages range from stage I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV (4), means cancer has spread to distant areas of the body. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
One of the goals of surgery for ovarian cancer is to take tissue samples for diagnosis and staging. To stage the cancer, samples of tissues are taken from different parts of the pelvis and abdomen and examined in the lab.
How is ovarian cancer stage determined?
The 2 systems used for staging ovarian cancer, the FIGO (International Federation of Gynecology and Obstetrics) system and the AJCC (American Joint Committee on Cancer) TNM staging system are basically the same.
They both use 3 factors to stage (classify) ovarian cancer:
- The extent (size) of the tumor (T): Has the cancer spread outside the ovary or fallopian tube? Has the cancer reached nearby pelvic organs like the uterus or bladder?
- The spread to nearby lymph nodes (N): Has the cancer spread to the lymph nodes in the pelvis or around the aorta (the main artery that runs from the heart down along the back of the abdomen and pelvis)? Also called para-aortic lymph nodes.
- The spread (metastasis) to distant sites (M): Has the cancer spread to fluid around the lungs (malignant pleural effusion) or to distant organs such as the liver or bones?
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
The staging system in the table below uses the pathologic stage (also called the surgical stage). It is determined by examining tissue removed during an operation. This is also known as surgical staging. Sometimes, if surgery is not possible right away, the cancer will be given a clinical stage instead. This is based on the results of a physical exam, biopsy, and imaging tests done before surgery.
The system described below is the most recent American Joint Committee on Cancer (AJCC) system effective January 2018. It is the staging system for ovarian cancer, fallopian tube cancer, and primary peritoneal cancer.
Cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
Table 1. Ovarian cancer stages
| AJCC Stage | Stage grouping | FIGO Stage | Stage description* |
|---|---|---|---|
| 1 | T1 N0 M0 | 1 | The cancer is only in the ovary (or ovaries) or fallopian tube(s) (T1). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 1A | T1a N0 M0 | 1A | The cancer is in one ovary, and the tumor is confined to the inside of the ovary; or the cancer is in in one fallopian tube, and is only inside the fallopian tube. There is no cancer on the outer surfaces of the ovary or fallopian tube. No cancer cells are found in the fluid (ascites) or washings from the abdomen and pelvis (T1a). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 1B | T1b N0 M0 | 1B | The cancer is in both ovaries or fallopian tubes but not on their outer surfaces. No cancer cells are found in the fluid (ascites) or washings from the abdomen and pelvis (T1b). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 1C | T1c N0 M0 | 1C | The cancer is in one or both ovaries or fallopian tubes and any of the following are present:
It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 2
| T2 N0 M0 | 2 | The cancer is in one or both ovaries or fallopian tubes and has spread to other organs (such as the uterus, bladder, the sigmoid colon, or the rectum) within the pelvis or there is primary peritoneal cancer (T2). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 2A | T2a N0 M0 | 2A | The cancer has spread to or has invaded (grown into) the uterus or the fallopian tubes, or the ovaries. (T2a). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 2B | T2b N0 M0 | 2B | The cancer is on the outer surface of or has grown into other nearby pelvic organs such as the bladder, the sigmoid colon, or the rectum (T2b). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 3A1 | T1 or T2 N1 M0 | 3A1 | The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer (T1) and it may have spread or grown into nearby organs in the pelvis (T2). It has spread to the retroperitoneal (pelvic and/or para-aortic) lymph nodes only. It has not spread to distant sites (M0). |
| 3A2 | T3a N0 or N1 M0 | 3A2 | The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer and it has spread or grown into organs outside the pelvis. During surgery, no cancer is visible in the abdomen (outside of the pelvis) to the naked eye, but tiny deposits of cancer are found in the lining of the abdomen when it is examined in the lab (T3a). The cancer might or might not have spread to retroperitoneal lymph nodes (N0 or N1), but it has not spread to distant sites (M0). |
| 3B | T3b N0 or N1 M0 | 3B | There is cancer in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer and it has spread or grown into organs outside the pelvis. The deposits of cancer are large enough for the surgeon to see, but are no bigger than 2 cm (about 3/4 inch) across. (T3b). It may or may not have spread to the retroperitoneal lymph nodes (N0 or N1), but it has not spread to the inside of the liver or spleen or to distant sites (M0). |
| 3C | T3c N0 or N1 M0 | 3C | The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer and it has spread or grown into organs outside the pelvis. The deposits of cancer are larger than 2 cm (about 3/4 inch) across and may be on the outside (the capsule) of the liver or spleen (T3c). It may or may not have spread to the retroperitoneal lymph nodes (N0 or N1), but it has not spread to the inside of the liver or spleen or to distant sites (M0). |
| 4A | Any T Any N M1a | 4A | Cancer cells are found in the fluid around the lungs (called a malignant pleural effusion) with no other areas of cancer spread such as the liver, spleen, intestine, or lymph nodes outside the abdomen (M1a). |
| 4B | Any T Any N M1b | 4B | The cancer has spread to the inside of the spleen or liver, to lymph nodes other than the retroperitoneal lymph nodes, and/or to other organs or tissues outside the peritoneal cavity such as the lungs and bones (M1b). |
Footnotes:
* The following additional categories are not described in the table above:
- TX: Main tumor cannot be assessed due to lack of information
- T0: No evidence of a primary tumor.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Grades of ovarian cancer
The grade of a cancer tells you how much the cancer cells look like normal cells. It gives your doctor an idea of how the cancer might behave. As a normal cell grows and matures, it becomes specialized for its role and place in the body. This is called differentiation. Cancer cells can look like normal cells. They are described as well differentiated or low grade. These cancers are more likely to grow slowly. Cancer cells can also look underdeveloped and nothing like a normal cell. They are known as undifferentiated or high grade. These cancers tend to grow and spread more quickly than low grade cancers.
Doctors use different systems to grade ovarian cancer. It depends on your type of ovarian cancer.
- Doctors describe serous epithelial ovarian cancer as either high grade or low grade. This depends on how much the tumor cells look like normal tissue.
- Doctors describe other types of epithelial ovarian cancers as:
- Grade 1 or well differentiated
- Grade 2 or moderately differentiated
- Grade 3 or poorly differentiated (or undifferentiated)
Stage 1 ovarian cancer
Stage 1 ovarian cancer is only in the ovaries. Stage 1 ovarian cancer is divided into 3 groups:
- Stage 1A means the cancer is completely inside one ovary
- Stage 1B means the cancer is completely inside both ovaries
- Stage 1C is split in to 3 groups:
- Stage 1C1 means the cancer is in one or both ovaries and the ovary ruptures (bursts) during surgery
- Stage 1C2 means the cancer is in one or both ovaries and the ovary ruptures (bursts) before surgery or there is some cancer on the surface of an ovary
- Stage 1C3 means the cancer is in one or both ovaries and there are cancer cells in fluid taken from inside your abdomen during surgery
Figure 6. Stage 1 ovarian cancer
Stage 2 ovarian cancer
Stage 2 ovarian cancer means the cancer has grown outside the ovary or ovaries. And is growing within the area circled by your hip bones (the pelvis). There may also be cancer cells in the abdomen.
Stage 2 ovarian cancer is divided into 2 groups:
- Stage 2A means the cancer has grown into the fallopian tubes or the uterus
- Stage 2B means the cancer has grown into other tissues in the pelvis, for example the bladder or rectum
Figure 7. Stage 2 ovarian cancer
Stage 3 ovarian cancer
Stage 3 ovarian cancer means the cancer has spread outside the pelvis to the lining of your abdominal cavity (peritoneum). It can also spread to the lymph nodes in the back of your abdomen.
There are three groups of stage 3 ovarian cancer- 3A, 3B and 3C:
- Stage 3A has 2 groups:
- Stage 3A1 means the cancer has spread to the lymph nodes in the back of your abdomen
- Stage 3A2 means that the doctor finds cancer cells in tissue samples they take from the lining of your abdomen (peritoneum). And it might also be in your lymph nodes
- Stage 3B means there are cancer growths that are 2cm or smaller in size on the lining of your abdomen (peritoneum). And there might also be cancer in your lymph nodes.
- Stage 3C means there are cancer growths larger than 2cm on the lining of your abdomen (peritoneum). And there might also be cancer in your lymph nodes.
Figure 8. Stage 3 ovarian cancer
Stage 4 ovarian cancer
Stage 4 ovarian cancer means the cancer has spread to other body organs some distance away from the ovaries. Such as the liver or lungs.
Stage 4 ovarian cancer is divided into 2 groups:
- Stage 4A means the cancer has caused a build up of fluid in the lining of the lungs (called the pleura). This is called a pleural effusion.
- Stage 4B means the cancer has spread to:
- the inside of the liver or spleen
- lymph nodes outside the abdomen
- other organs such as the lungs
Figure 9. Stage 4 ovarian cancer
Ovarian cancer treatment
The main treatments for ovarian cancer are surgery and chemotherapy. Less often, treatment may include radiotherapy. Ovarian cancer treatment is usually managed by a gynecological oncologist as they specialize in treating cancers of the reproductive tract and have very specialized surgical skills. Ideally, they will be part of a multidisciplinary health care team – where each member of the team specializes in a different area of care and that care is co-ordinated between each member.
The type of treatment women receive depends on the type and stage of their ovarian cancer and their general health.
Almost all women with ovarian cancer will need surgery. The amount and type of surgery you have will depend on your stage and type of cancer.
For some women with very early stage ovarian cancer, surgery is the only treatment you need.
Most women with ovarian cancer are diagnosed with advanced disease and have a combination of both surgery and chemotherapy. You may have chemotherapy after surgery, or both before and after surgery.
Some women with ovarian cancer might have:
- Targeted cancer drugs
- Hormone therapy
- Radiotherapy (radiation therapy)
Surgery
Surgery to remove ovarian cancer include:
- Surgery to remove one ovary. For very early stage cancer that hasn’t spread beyond one ovary, surgery may involve removing the affected ovary and its fallopian tube. This procedure may preserve your ability to have children.
- Surgery to remove both ovaries. If cancer is present in both your ovaries, but there are no signs of additional cancer, your surgeon may remove both ovaries and both fallopian tubes. This procedure leaves your uterus intact, so you may still be able to become pregnant using your own frozen embryos or eggs or with eggs from a donor.
- Surgery to remove both ovaries and the uterus. If your cancer is more extensive or if you don’t wish to preserve your ability to have children, your surgeon will remove the ovaries, the fallopian tubes, the uterus, nearby lymph nodes and a fold of fatty abdominal tissue (omentum). This operation is called a total abdominal hysterectomy (TAH) and bilateral salpingo-oophorectomy (BSO). If the omentum is also removed (an omentectomy).
- Surgery for advanced cancer. If your cancer is advanced, your doctor may recommend chemotherapy followed by surgery to remove as much of the cancer as possible.
The first treatment for ovarian cancer is usually an operation called a ‘laparotomy’. This operation is also the main way that a diagnosis of ovarian cancer is confirmed.
During a laparotomy, a long vertical cut is made in your abdomen, which allows the surgeon to find and remove as much of the tumor as possible. In many cases, the surgeon will do a biopsy of the tumor at the beginning of the operation to confirm that it is cancer. This is called a ‘frozen section’. If the frozen section confirms that the tumor is cancer, the operation will continue.
To know where the ovarian cancer is in your body to remove it, the surgeon typically uses the imaging tests done before surgery as well as a bright light and feeling for the tumors during the operation. Still, some tumors that are not easily seen or felt by hand might be missed. To help find these tumors, intraoperative imaging might be used. This approach uses a special imaging system in the operating room during the surgery. A fluorescent drug called pafolacianine (Cytalux) will be injected into your blood a few hours before surgery. The drug travels through the body and attaches to a specific protein found on ovarian cancer cells. During surgery, the imaging system gives off near-infrared fluorescent light that will cause the drug to light up so the surgeon can see which areas need to be removed. The most common side effects from pafolacianine (Cytalux) are belly pain, heartburn, itching, chest pain, nausea, vomiting, and flushing. Your doctor will probably ask you to avoid taking any supplements that have folic acid in them for a few days before the procedure so they don’t disturb the test.
For most women, the operation will involve removal of the ovaries, fallopian tubes, the uterus, the omentum (the fat pad around the organs in your abdomen), the appendix and some of the lymph glands in the area. Sometimes it may be necessary to remove some of the bowel.
After your operation, samples of the tissue removed are sent to a laboratory for further examination. The results of these biopsies will provide more information about the type and extent of your cancer and enables the gynecological oncologist to make decisions about further treatment.
If you were still having menstrual periods before you were diagnosed with ovarian cancer and you have both your ovaries removed, this surgery will result in menopause and can affect your ability to have children. As well as learning that you have ovarian cancer, this surgically-induced menopause and infertility creates all kinds of extra challenges to live with. It’s important for women who have not yet completed their family to speak to a doctor about these issues before surgery.
Staging epithelial ovarian cancer
The first goal of ovarian cancer surgery is to stage your ovarian cancer − to see how far the cancer has spread from the ovary. Usually this means removing the uterus (this operation is called a hysterectomy), along with both ovaries and fallopian tubes (this is called a bilateral salpingo-oophorectomy or BSO). In addition, the omentum is also removed (an omentectomy). The omentum is a layer of fatty tissue that covers the abdominal contents like an apron, and ovarian cancer sometimes spreads to this area. Some lymph nodes in the pelvis and abdomen might also be biopsied (taken out to see if the cancer has spread from the ovary).
If there is fluid in the pelvis or abdominal cavity, it will be removed for testing. The surgeon may “wash” the abdominal cavity with salt water (saline) and send that fluid to the lab for testing. Biopsies may also be taken from different areas inside the abdomen and pelvis. All the tissue and fluid samples taken during the operation are sent to a lab to look for cancer cells. Staging is very important because ovarian cancers at different stages are treated differently. If the staging isn’t done correctly, the doctor may not be able to decide on the best treatment.
Intraoperative imaging
To know where the ovarian cancer is in your body to remove it, the surgeon typically uses the imaging tests done before surgery as well as a bright light and feeling for the tumors during the operation. Still, some tumors that are not easily seen or felt by hand might be missed. To help find these tumors, intraoperative imaging might be used.
This approach uses a special imaging system in the operating room during the surgery. A fluorescent drug called pafolacianine (Cytalux) will be injected into your blood a few hours before surgery. The drug travels through the body and attaches to a specific protein found on ovarian cancer cells. During surgery, the imaging system gives off near-infrared fluorescent light that will cause the drug to light up so the surgeon can see which areas need to be removed.
The most common side effects from pafolacianine (Cytalux) are belly pain, heartburn, itching, chest pain, nausea, vomiting, and flushing.
Your doctor will probably ask you to avoid taking any supplements that have folic acid in them for a few days before the procedure so they don’t disturb the test.
Debulking epithelial ovarian cancer
The other important goal of ovarian cancer surgery is to remove as much of the tumor as possible − this is called debulking. Debulking is very important when ovarian cancer has already spread throughout the abdomen (belly) at the time of surgery. The aim of debulking surgery is to leave behind no visible cancer or no tumors larger than 1 cm (less than 1/2 an inch). This is called optimally debulked. Patients whose tumors have been optimally debulked, have a better outlook (prognosis) than those left with larger tumors after surgery (called sub-optimally debulked).
In some cases, other organs might be affected by debulking:
- Sometimes the surgeon will need to remove a piece of colon to debulk the cancer properly. In some cases, a piece of colon is removed and then the 2 ends that remain are sewn back together. In other cases, though, the ends can’t be sewn back together right away. Instead, the top end of the colon is attached to an opening (stoma) in the skin of the abdomen to allow body wastes to get out. This is known as a colostomy. Most often, this is only temporary, and the ends of the colon can be reattached later in another operation.
- Sometimes, a part of the small intestine may need to be removed. Just like with the colon, the small intestine can either be reconnected (which is most common) or an ileostomy might be made. This is usually temporary, but will need special care, so ask your doctor if this is a possibility before having surgery.
- Debulking surgery might also mean removing a piece of the bladder. If this happens, a catheter (to empty the bladder) will be placed during surgery. This will be left in place until the bladder recovers enough to be able to empty on its own. Then, the catheter can be removed.
- Debulking might also require removing the spleen and/or the gallbladder, as well as part of the stomach, liver, and/or pancreas.
If both ovaries and/or the uterus are removed, you will not be able to become pregnant. It also means that you will go into menopause if you haven’t done so already. Most women will stay in the hospital for 3 to 7 days after the operation and can resume their usual activities within 4 to 6 weeks.
Surgery for ovarian germ cell tumors and ovarian stromal tumors
For germ cell tumors and stromal tumors, the main goal of surgery is to remove the cancer. Most ovarian germ cell tumors are treated with a hysterectomy and bilateral salpingo-oophorectomy (BSO). If the cancer is in only one ovary and you still want to be able to have children, only the ovary containing the cancer and the fallopian tube on the same side are removed (leaving behind the other ovary and fallopian tube and the uterus).
Ovarian stromal tumors are often confined to just one ovary, so surgery may just remove that ovary. If the cancer has spread, more tissue may need to be removed. This could mean a hysterectomy and bilateral salpingo-oophorectomy and even debulking surgery.
Sometimes, after child bearing is finished, surgery to remove the other ovary, the other fallopian tube, and the uterus may be recommended, for both germ cell and stromal ovarian tumors.
Chemotherapy
Chemotherapy also called chemo is a drug treatment that uses chemicals to kill fast-growing cells in the body, including cancer cells. Chemotherapy drugs can be injected into a vein or taken by mouth. Sometimes the drugs are injected directly into the abdomen (intraperitoneal chemotherapy).
Chemotherapy is often used after surgery to kill any cancer cells that might remain. It can also be used before surgery.
In certain situations, chemotherapy drugs may be heated and infused into the abdomen during surgery (hyperthermic intraperitoneal chemotherapy). The drugs are left in place for a certain amount of time before they’re drained. Then the operation is completed.
Chemo drugs can cause side effects. These depend on the type and dose of drugs given, and the length of treatment. Some of the most common possible side effects include:
- Nausea and vomiting
- Loss of appetite
- Loss of hair
- Hand and foot rashes
- Mouth sores
Chemotherapy can also affect the blood-forming cells of the bone marrow, which can lead to:
- Increased chance of infections (from low white blood cell counts, also called leukopenia)
- Easy bruising or bleeding (from low blood platelet counts. also called thrombocytopenia)
- Fatigue (from low red blood cell counts and other reasons, also called anemia)
These side effects usually go away after treatment is finished. While you are in treatment, tell your cancer care team about any side effects you are having. There are often ways to lessen these side effects. For example, drugs can be given to help prevent or reduce nausea and vomiting.
Some chemo drugs may have long-term or even permanent side effects:
- Cisplatin can cause kidney damage. To help prevent this, doctors give lots of IV fluid before and after this drug is given.
- Both cisplatin and the taxanes can cause nerve damage (called neuropathy). This can lead to problems with numbness, tingling, or even pain in the hands and feet.
- Cisplatin can also damage the nerves to the ear, which can lead to hearing loss (called ototoxicity).
- Chemo can also cause early menopause and infertility (being unable to become pregnant), which may be permanent. This is rarely an issue in the treatment of epithelial ovarian cancer, since most women have both ovaries removed as a part of treatment.
- Rarely, some chemo drugs can permanently damage bone marrow. This can later cause a bone marrow cancer such as myelodysplastic syndrome or even acute myeloid leukemia. This is called a second cancer. Your health care team knows which drugs can cause this problem and will discuss this possibility with you. Their positive effects against ovarian cancer offset the small chance that any of these drugs will cause another cancer.
- Ifosfamide can cause irritation and bleeding of the bladder lining (hemorrhagic cystitis). This can usually be prevented by giving the drug mesna with the ifosfamide.
Other drugs can have other side effects, so ask your doctor what side effects to expect from the drugs that you will receive. Most side effects improve once treatment is stopped, but some can last a long time and may never go away completely.
Chemotherapy for epithelial ovarian cancer
Chemo for ovarian cancer usually involves getting two different types of drugs together. Getting a combination of drugs instead of just one drug alone seems to work better as a first treatment for ovarian cancer. Usually, the combination includes a type of chemo drug called a platinum compound (usually cisplatin or carboplatin), and another type of chemo drug called a taxane, such as paclitaxel (Taxol®) or docetaxel (Taxotere®). These drugs are usually given as an IV (put into a vein) every 3 to 4 weeks.
The typical course of chemo for epithelial ovarian cancer involves 3 to 6 cycles of treatment, depending on the stage and type of ovarian cancer. A cycle is a schedule of regular doses of a drug, followed by a rest period. Different drugs have varying cycles; your doctor will let you know what schedule is planned for your chemo.
Epithelial ovarian cancer often shrinks or even seems to go away with chemo, but the cancer cells may eventually begin to grow again. If the first chemo seemed to work well and the cancer stayed away for at least 6 to 12 months, it can be treated with the same chemotherapy used the first time. In some cases, different drugs may be used.
Some of the other chemo drugs that are helpful in treating ovarian cancer include:
- Albumin bound paclitaxel (nab-paclitaxel, Abraxane®)
- Altretamine (Hexalen®)
- Capecitabine (Xeloda®)
- Cyclophosphamide (Cytoxan®)
- Etoposide (VP-16)
- Gemcitabine (Gemzar®)
- Ifosfamide (Ifex®)
- Irinotecan (CPT-11, Camptosar®)
- Liposomal doxorubicin (Doxil®)
- Melphalan
- Pemetrexed (Alimta®)
- Topotecan
- Vinorelbine (Navelbine®)
Intraperitoneal chemotherapy
For women who have stage 3 ovarian cancer (cancer that has not spread outside the abdomen) and whose cancers were optimally debulked (no tumors larger than 1 cm after surgery), intraperitoneal (IP) chemotherapy might be given in addition to systemic chemo (paclitaxel given in a vein).
In intraperitoneal (IP) chemotherapy, the drugs cisplatin and paclitaxel are injected into the abdominal cavity through a catheter (thin tube). The tube can be placed during the staging/debulking surgery, but sometimes it is placed later. If it is done later, it can be placed by a surgeon using laparoscopy, or by an interventional radiologist under x-ray guidance. The catheter is usually connected to a port, a half dollar-sized disk topped with a pliable diaphragm. The port is placed under the skin against a bony structure of the abdominal wall, such as a rib or pelvic bone. A needle can be placed through the skin and into the port to give chemo and other drugs. Over time, problems may occur with the catheter (for example, it might become plugged or infected), but this is rare.
Giving chemo this way gives the most concentrated dose of the drugs directly to the cancer cells in the abdominal cavity. This chemo also gets absorbed into the bloodstream and so can reach cancer cells outside the abdominal cavity. Intraperitoneal (IP) chemotherapy seems to help some women live longer than intravenous (IV) chemo alone, but the side effects are often more severe. Women getting intraperitoneal (IP) chemotherapy might have more abdominal pain, nausea, vomiting, and other side effects, which might make some women stop their treatment early. The risk of side effects also means a woman must have normal kidney function and be in good overall heath before starting intraperitoneal (IP) chemotherapy. Women also cannot have a lot of adhesions or scar tissue inside their abdomen (belly) because this can keep the chemo from reaching all the exposed cancer cells.
Chemotherapy for germ cell tumors
If you have a germ cell tumor, you will likely be treated with combination chemo (several different drugs at once). The combination used most often is called BEP, and includes the chemotherapy drugs bleomycin, etoposide and cisplatin (Platinol). If the cancer is a dysgerminoma, these are usually very sensitive to chemotherapy, and can sometimes be treated with the less toxic combination of carboplatin and etoposide. Other drug combinations may be used if the cancer isn’t responding to treatment or to treat cancer that has recurred (come back). These include:
- High dose chemotherapy (the exact drugs used can vary depending on what cancer center is giving the treatment)
- TIP (paclitaxel/Taxol, ifosfamide, and cisplatin/Platinol)
- VeIP (vinblastine, ifosfamide, and cisplatin/Platinol)
- VIP (etoposide/VP-16, ifosfamide, and cisplatin/Platinol)
- VAC (vincristine, dactinomycin, and cyclophosphamide)
Chemotherapy for stromal tumors
Ovarian stromal tumors are not often treated with chemotherapy, but when they are, the combination of carboplatin plus paclitaxel or PEB (cisplatin/Platinol, etoposide, and bleomycin) is used most often.
Targeted Drug Therapy for Ovarian Cancer
Targeted therapy is a type of cancer treatment that uses drugs that target the specific weaknesses present within your cancer cells. By attacking these weaknesses, targeted drug treatments can cause cancer cells to die. Each type of targeted therapy works differently, but they all change the way a cancer cell grows, divides, repairs itself, or interacts with other cells.
Targeted therapy drugs are usually reserved for treating ovarian cancer that returns after initial treatment or cancer that resists other treatments. Your doctor may test your cancer cells to determine which targeted therapy is most likely to have an effect on your cancer.
Targeted therapy is an active area of cancer research. Many clinical trials are testing new targeted therapies.
Bevacizumab
Bevacizumab (Avastin, other names) belongs to a class of drugs called angiogenesis inhibitors. For cancers to grow and spread, they need to make new blood vessels to nourish themselves (called angiogenesis). This drug attaches to a protein called VEGF (that signals new blood vessels to form) and slows or stops cancer growth. Bevacizumab is given as an infusion into the vein (IV) every 2 to 3 weeks.
Bevacizumab has been shown to shrink or slow the growth of advanced epithelial ovarian cancers. Bevacizumab appears to work even better when given along with chemotherapy having shown good results in terms of shrinking (or stopping the growth of) tumors. But it doesn’t seem to help women live longer.
Bevacizumab can also be given with olaparib as maintenance treatment in women whose cancers have a BRCA gene mutation or genomic instability (see below) and have shrunk quite a bit with chemotherapy containing carboplatin or cisplatin.
Side effects of bevacizumab
- Common side effects can include high blood pressure, tiredness, bleeding, low white blood cell counts, headaches, mouth sores, loss of appetite, and diarrhea.
- Rare but possibly serious side effects can include blood clots, severe bleeding, slow wound healing, holes forming in the colon (called perforations), and the formation of abnormal connections between the bowel and the skin or bladder (fistulas). If a perforation or fistula occurs it can lead to severe infection and may require surgery to correct.
PARP inhibitors
Olaparib (Lynparza), rucaparib (Rubraca), and niraparib (Zejula) are drugs known as a PARP (poly(ADP)-ribose polymerase) inhibitors. PARP enzymes normally help repair damaged DNA inside cells. The proteins made by the BRCA genes (BRCA1 and BRCA2) also normally help repair DNA, but in a different way. Mutations in BRCA genes can make it hard for a cell to repair its DNA. PARP inhibitors can make it even harder for tumor cells with an abnormal BRCA gene to repair damaged DNA, which often leads to the death of these cells. All of these drugs are taken daily by mouth, as pills or capsules.
If you are not known to have a BRCA mutation, your doctor might test your blood or saliva and your tumor to be sure you have one before starting treatment with one of these drugs.
PARP inhibitors have been shown to help shrink or slow the growth of some advanced ovarian cancers for a time. So far, though, it’s not clear if they can help women live longer.
Olaparib (Lynparza) is used to treat advanced ovarian cancer, typically after chemotherapy has been tried. This drug can be used in patients with or without mutations in one of the BRCA genes.
- In women with a BRCA mutation:
- Olaparib can be used as maintenance treatment for advanced ovarian cancer that has gotten smaller in response to first treatment with chemotherapy containing cisplatin or carboplatin.
- Olaparib can be used with bevacizumab (see above) as maintenance treatment in women whose cancers have shrunk quite a bit with chemotherapy containing carboplatin or cisplatin.
- In women without a BRCA mutation:
- If the tumor has a high genomic instability score (a test measuring the amount of abnormal genes in cancer cells), olaparib can be used with bevacizumab as maintenance treatment in women whose cancers have shrunk quite a bit with chemotherapy containing carboplatin or cisplatin.
- In women with or without a BRCA mutation:
- Olaparib can be used as maintenance treatment for advanced ovarian cancer that has come back after treatment, and then has shrunk in response to chemotherapy containing cisplatin or carboplatin.
Niraparib (Zejula) may be used in some situations to treat ovarian cancer.
- In women with or without a BRCA gene mutation:
- Niraparib might be used as maintenance treatment for advanced ovarian cancer, where the cancer has shrunk with first-line chemotherapy containing cisplatin or carboplatin.
- In women with a BRCA gene mutation:
- Niraparib might be used as maintenance treatment for advanced ovarian cancer that has come back after treatment, where the cancer has then shrunk with chemotherapy containing cisplatin or carboplatin.
Rucaparib (Rubraca) can be used in women with or without a BRCA mutation, as maintenance treatment for advanced ovarian cancer that has come back after treatment, and then has shrunk in response to chemotherapy containing cisplatin or carboplatin.
Side effects of PARP inhibitors
- Side effects of these drugs can include nausea, vomiting, diarrhea, fatigue, loss of appetite, taste changes, low red blood cell counts (anemia), belly pain, and muscle and joint pain.
- Rarely, some patients treated with these drugs have developed a blood cancer, such as myelodysplastic syndrome or acute myeloid leukemia.
Drugs that target folate receptor-alpha
In many ovarian cancers, the cells have high levels of the folate receptor-alpha (FR-alpha) protein on their surfaces. Drugs that target this protein might be an option to treat these cancers.
Mirvetuximab soravtansine (Elahere) is an antibody-drug conjugate (ADC), which is a lab-made antibody linked to a chemotherapy drug. Once it’s in the body, the antibody acts like a homing device by attaching to the folate receptor-alpha protein on cancer cells, which brings the chemo directly to them. Mirvetuximab soravtansine (Elahere) can be used to treat epithelial ovarian cancer that tests positive for folate receptor-alpha and that is no longer responding to platinum chemotherapy drugs such as cisplatin or carboplatin.
Mirvetuximab soravtansine is infused into a vein (through an IV line or central venous catheter), typically once every 3 weeks. Before each treatment, you’ll get medicines to help prevent infusion reactions, nausea, and vomiting.
Side effects of mirvetuximab soravtansine:
- Common side effects of this drug can include nausea and vomiting, diarrhea or constipation, feeling tired, belly pain, low blood cell counts, and changes in mineral levels in the blood.
- Mirvetuximab soravtansine can cause eye problems, which can sometimes be serious. Problems can include blurred vision, dry eyes, light sensitivity, eye pain, or vision changes. You’ll need an eye exam before being treated with this drug, and your doctor will prescribe eye drops for you to use before and during your treatment. Tell your doctor or nurse right away if you develop any eye problems.
- Mirvetuximab soravtansine can cause serious lung disease in some people, which might even be life threatening. It’s very important to let your doctor or nurse know right away if you’re having symptoms such as coughing, trouble breathing, or chest pain.
- Mirvetuximab soravtansine can also cause nerve damage (peripheral neuropathy), which can lead to numbness, tingling, or weakness in the hands or feet.
Drugs that target cells with NTRK gene changes
A very small number of ovarian cancers have changes in one of the NTRK genes. Cells with these gene changes can lead to abnormal cell growth and cancer. Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek) are targeted drugs that stop the proteins made by the abnormal NTRK genes. These drugs can be used in people with advanced ovarian cancer whose tumor has an NTRK gene change and is still growing despite other treatments. Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek) are taken as pills, once or twice a day.
Side effects of drugs that target NTRK gene changes:
- Common side effects can include dizziness, fatigue, nausea, vomiting, constipation, weight gain, and diarrhea.
- Less common but serious side effects can include abnormal liver tests, heart problems, and confusion.
Radiotherapy
Radiotherapy is occasionally used as a treatment option for ovarian cancer. Radiotherapy may be used where cancer is confined to the pelvic cavity. It may also be used in advanced ovarian cancer to reduce the size of the cancer and help to relieve symptoms. Radiotherapy is treatment with special X-rays that are aimed at the specific site of the cancer. The X-ray damages the DNA or genetic code in the cancer cells and this damage kills the cancer cells when they try to grow. Treatment can be external or internal and is given daily over a number of weeks.
External beam radiation therapy
This is the most common type of radiation therapy for women with ovarian cancer. External radiation therapy is much like getting an x-ray, but the radiation is stronger. A machine focuses the radiation on the area affected by the cancer. The procedure itself is painless. Each treatment lasts only a few minutes, but the setup time—getting you into place for treatment—usually takes longer. Treatments are given 5 days a week for several weeks.
Some common side effects include:
- Skin changes – the skin in the treated area may look and feel sunburned or even blister and peel
- Fatigue (tiredness)
- Nausea and vomiting
- Diarrhea
- Vaginal irritation, sometimes with a discharge (if the pelvis is being treated)
These side effects improve after treatment is stopped. Skin changes gradually fade, and the skin returns to normal in 6 to 12 months.
If you are having side effects from radiation, tell your cancer care team. There may be ways to manage them.
Brachytherapy
Brachytherapy, also known as internal radiation, is another way to deliver radiation therapy. Instead of aiming radiation beams from outside the body, a device containing radioactive seeds or pellets is placed inside the body, near the cancer. This is rarely done for ovarian cancer.
Hormone therapy
Hormone therapy uses drugs to block the effects of the hormone estrogen on ovarian cancer cells. Some ovarian cancer cells use estrogen to help them grow, so blocking estrogen may help control the cancer. Hormone therapy might be a treatment option for some types of slow-growing ovarian cancers. It may also be an option if the cancer comes back after initial treatments.
Luteinizing-hormone-releasing hormone (LHRH) agonists
Luteinizing-hormone-releasing hormone (LHRH) agonists sometimes called GnRH agonists, switch off estrogen production by the ovaries. These drugs are used to lower estrogen levels in women who are premenopausal. Examples of LHRH agonists include goserelin (Zoladex®) and leuprolide (Lupron®). These drugs are injected every 1 to 3 months. Side effects can include any of the symptoms of menopause, such as hot flashes and vaginal dryness. If they are taken for a long time (years), these drugs can weaken bones (sometimes leading to osteoporosis).
Tamoxifen
Tamoxifen is a drug that is often used to treat breast cancer. It can also be used to treat ovarian stromal tumors and is rarely used to treat advanced epithelial ovarian cancer. Tamoxifen acts as an anti-estrogen in many tissues in the body, but as a weak estrogen in others. The goal of tamoxifen therapy is to keep any estrogens circulating in the woman’s body from stimulating cancer cell growth. The anti-estrogen activity of this drug can lead to side effects like hot flashes and vaginal dryness. Because tamoxifen acts like a weak estrogen in some areas of the body, it does not cause bone loss but can increase the risk of serious blood clots in the legs.
Aromatase inhibitors
Aromatase inhibitors are drugs that block an enzyme (called aromatase) that turns other hormones into estrogen in post-menopausal women. They don’t stop the ovaries from making estrogen, so they are only helpful in lowering estrogen levels in women after menopause. These drugs are mainly used to treat breast cancer, but can also be used to treat some ovarian stromal tumors that have come back after treatment as well as low grade serous carcinomas. They include letrozole (Femara®), anastrozole (Arimidex®), and exemestane (Aromasin®). These drugs are taken as pills once a day.
Common side effects of aromatase inhibitors include hot flashes, joint and muscle pain, and bone thinning. The bone thinning can lead to osteoporosis and bones that break easily.
Immunotherapy
Immunotherapy is the use of medicines to stimulate your body’s immune system to recognize and destroy cancer cells more effectively. Your body’s disease-fighting immune system may not attack cancer cells because they produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process. Immunotherapy might be an option for treating ovarian cancer in certain situations.
Immune checkpoint inhibitors
An important part of the immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses “checkpoints” – proteins on immune cells that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system. But drugs that target these checkpoints can be used to treat some people with ovarian cancer.
Pembrolizumab (Keytruda) targets PD-1, a protein on certain immune cells (called T cells) that normally helps keep these cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth. Pembrolizumab can be used in people with certain types of advanced ovarian cancer that have high levels of MSI or changes in the MMR genes whose cancer starts growing after chemotherapy or other drug treatments.
Pembrolizumab (Keytruda) immunotherapy drug is given as an intravenous (IV) infusion every 3 weeks.
Possible side effects of immunotherapy
- Side effects of these drugs can include fatigue, cough, nausea, itching, skin rash, loss of appetite, constipation, joint pain, and diarrhea. Other, more serious side effects occur less often.
- Infusion reactions: Some people might have an infusion reaction while getting these drugs. This is like an allergic reaction, and can include fever, chills, flushing of the face, rash, itchy skin, feeling dizzy, wheezing, and trouble breathing. It’s important to tell your doctor or nurse right away if you have any of these symptoms while getting these drugs.
- Autoimmune reactions: These drugs work by basically removing one of the safeguards on the body’s immune system. Sometimes the immune system starts attacking other parts of the body, which can cause serious or even life-threatening problems in the lungs, intestines, liver, hormone-making glands, kidneys, or other organs.
It’s very important to report any new side effects to your cancer care team as soon as possible. If serious side effects do occur, treatment may need to be stopped and you may get high doses of corticosteroids to suppress your immune system.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery and chemotherapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Ovarian cancer treatment and fertility
Treatment for ovarian cancer can affect a woman’s ability to have children. If a woman who has not yet gone through menopause has both ovaries removed, she will no longer be able to have children naturally after treatment. If surgery involves removing the uterus, the woman will no longer be able to have children at all.
If ovarian cancer has not spread or if it’s found to be a borderline tumor (a type of less aggressive ovarian cancer), it may be possible to just remove only the affected ovary, leaving the other ovary and the uterus. This means that a woman may still fall pregnant after surgery.
Some women need chemotherapy following surgery. When an ovary remains after surgery, having chemotherapy can mean that a woman goes through menopause early. Women who have gone through menopause are no longer able to become pregnant.
Women who were planning to have children before their ovarian cancer diagnosis should speak to their oncologist before starting treatment for ovarian cancer. It may be possible to see a fertility specialist to discuss the available options.
Stage 1 ovarian cancer treatment
Doctors usually class stage 1 cancer as early ovarian cancer. This means the cancer is still contained within the ovaries. The main treatment for stage 1 ovarian cancer is surgery. Some women also need chemotherapy.
The specialist doctors consider several factors when deciding what type of treatment you need. These factors include;
- whether you have stage 1A, 1B or 1C ovarian cancer
- the grade of your cancer
- the type of cells the cancer started in
- your age and whether you want any more children
- other health conditions you have
Surgery
Surgery for early ovarian cancer aims to remove your cancer and find out how far it has spread. The specialist surgeon (gynecologist) usually removes your:
- ovaries
- fallopian tubes
- womb (including the cervix)
During the operation, the gynecologist examines the inside of your abdomen and your abdominal organs for signs of cancer. You might need further surgery if your cancer has spread.
Having children in the future
For some low grade stage 1A cancers, it might be possible to just remove the affected ovary and fallopian tube, leaving behind the unaffected ovary and your womb. This means you might be able to become pregnant and have a baby afterwards.
Chemotherapy
After surgery, your doctor might suggest you have chemotherapy if you have:
- stage 1C ovarian cancer
- a high grade (grade 3) cancer
This is called adjuvant chemotherapy and aims to lower the risk of your cancer coming back.
Stage 2 ovarian cancer treatment
Doctors usually class stage 2 cancer as advanced ovarian cancer. This means the cancer has spread away from the ovary. The main treatments for stage 2 ovarian cancer are surgery and chemotherapy. Treatment can cure some advanced cancers. But if treatment can’t cure you, the aim of treatment is to control the cancer for as long as possible.
The specialist doctors consider several factors when deciding whether you can have surgery. And whether you should have chemotherapy before or after the operation. These include:
- where the cancer has spread to
- whether the specialist surgeon (gynecological oncologist) thinks they can remove all the cancer
- your general health
You might have:
- Chemotherapy after surgery – this is called debulking surgery
- Chemotherapy before and after surgery – doctors sometimes call this interval debulking surgery
Chemotherapy after surgery
You have chemotherapy after surgery (debulking surgery) as your first treatment if:
- you are well enough
- the specialist surgeon thinks they can remove all the cancer.
The surgeon removes as much of the cancer as possible. After you recover from surgery, you have chemotherapy. This is adjuvant chemotherapy.
Adjuvant chemotherapy aims to reduce the risk of the cancer coming back. If the surgeon couldn’t remove all the cancer, then chemotherapy aims to shrink the cancer that is left behind. Some women may then have further surgery.
Chemotherapy before and after surgery
You might have chemotherapy as your first treatment if:
- your surgeon looks at your scans and decides it isn’t possible to remove all your cancer
- you aren’t well enough for surgery straight away
This is neoadjuvant chemotherapy or primary chemotherapy. The chemotherapy aims to shrink the cancer and make it easier to remove.
You have a scan halfway through the chemotherapy course. You then have surgery if the scan shows your cancer is shrinking. You may hear your specialist call this interval debulking surgery. After the surgery, you have the rest of the course of chemotherapy.
Stage 3 ovarian cancer treatment
Doctors usually class stage 3 ovarian cancer as advanced ovarian cancer. This means the cancer has spread away from the ovary. The main treatments for stage 3 ovarian cancer are surgery and chemotherapy. Treatment can cure some advanced cancers. But if treatment can’t cure you, the aim of treatment is to control the cancer for as long as possible.
The specialist doctors consider several factors when deciding whether you can have surgery. And whether you should have chemotherapy before or after the operation. These include:
- where the cancer has spread to
- whether the specialist surgeon (gynecological oncologist) thinks they can remove all the cancer
- your general health
You might have:
- Chemotherapy after surgery (debulking surgery)
- Chemotherapy before and after surgery – doctors sometimes call this interval debulking surgery
Chemotherapy after surgery
You have chemotherapy after surgery (debulking surgery) as your first treatment if:
- you are well enough
- the specialist surgeon thinks they can remove all the cancer.
The surgeon removes as much of the cancer as possible. After you recover from surgery, you have chemotherapy. This is adjuvant chemotherapy.
Adjuvant chemotherapy aims to reduce the risk of the cancer coming back. If the surgeon couldn’t remove all the cancer, then chemotherapy aims to shrink the cancer that is left behind. Some women may then have further surgery.
Chemotherapy before and after surgery
You might have chemotherapy as your first treatment if:
- your surgeon looks at your scans and decides it isn’t possible to remove all your cancer
- you aren’t well enough for surgery straight away
This is neoadjuvant chemotherapy or primary chemotherapy. The chemotherapy aims to shrink the cancer and make it easier to remove.
You have a scan halfway through the chemotherapy course. You then have surgery if the scan shows your cancer is shrinking. You may hear your specialist call this interval debulking surgery. After the surgery, you have the rest of the course of chemotherapy.
Targeted cancer drug treatment
For some stage 3 cancers, you might have a type of targeted drug treatment called bevacizumab with chemotherapy.
If surgery isn’t possible
It might not be possible to have surgery if your cancer has spread widely or you are not well enough. You can have chemotherapy on its own to shrink the cancer as much as possible and to slow it down. You might have radiotherapy to relieve your symptoms. This depends on where in the body the cancer has spread.
You might have other types of treatment to help relieve your symptoms. For example, treatment for fluid in the abdomen (ascites) or for a blocked bowel.
Stage 4 ovarian cancer treatment
Stage 4 ovarian cancer is classed as advanced (metastatic) cancer. This means the cancer has spread away from the ovary to other body organs, such as the liver or lungs. The aim of treatment is to control the cancer for as long as possible. And to help you feel better and live longer. The main treatments for stage 4 ovarian cancer are surgery and chemotherapy. Some women have targeted cancer drug treatment or radiotherapy.
The specialist doctors consider several factors when deciding whether you can have surgery. And when you should have the operation. These factors include:
- where the cancer has spread to
- your general health
You might have:
- Chemotherapy before and after surgery – doctors sometimes call this interval debulking surgery
- Chemotherapy after surgery (debulking surgery)
- Chemotherapy without surgery
Chemotherapy before surgery
You might have chemotherapy as your first treatment. This is neoadjuvant chemotherapy or primary chemotherapy. The chemotherapy aims to shrink the cancer and make it easier to remove.
You have a scan halfway through the chemotherapy course. You then have surgery if the scan shows your cancer is shrinking. You may hear your surgeon call this interval debulking surgery. After the surgery, you have the rest of the course of chemotherapy.
Chemotherapy after surgery
You might have chemotherapy after surgery (debulking surgery) as your first treatment if you are well enough. The surgeon removes as much of the cancer as possible. After you recover from surgery, you have chemotherapy. This is adjuvant chemotherapy. Adjuvant chemotherapy aims to shrink the cancer that has been left behind. Some women may then have further surgery.
If you can’t have surgery
It might not be possible to have surgery if you have very advanced cancer. Or you are not well enough.
You can have chemotherapy on its own to shrink the cancer as much as possible and to slow it down. You might have radiotherapy to relieve symptoms. This depends on where in the body the cancer has spread.
Instead of cancer treatments, you might have other treatments to help relieve your symptoms. For example, treatment for fluid in the abdomen (ascites) or for a blocked bowel.
Targeted cancer drugs
For some advanced cancers, you may have a type of targeted drug called bevacizumab with chemotherapy.
You might have a targeted cancer drug called olaparib or niraparib if your cancer comes back after treatment.
Coping and support
A diagnosis of ovarian cancer can be overwhelming and scary. In time you’ll find ways to cope with your feelings, but in the meantime you might find it helpful to:
- Find someone to talk with. You may feel comfortable discussing your feelings with a friend or family member, or you might prefer meeting with a formal support group. Support groups for the families of cancer survivors also are available.
- Let people help. Cancer treatments can be exhausting. Let people know what would be most useful for you.
- Set reasonable goals. Having goals helps you feel in control and can give you a sense of purpose. But choose goals that you can reach.
- Take time for yourself. Eating well, relaxing and getting enough rest can help combat the stress and fatigue of cancer.
Complementary therapies
Many women with ovarian cancer are interested in trying complementary therapies – natural therapies that may be used to help manage symptoms and side effects, reduce pain, relieve stress and encourage a feeling of wellbeing. Let your doctor know if you are considering natural therapies to ensure they are compatible with the treatment you are receiving. Your cancer care team can also help you learn what is known (or not known) about the method you are thinking about using, which can help you make an informed decision.
Ovarian cancer prognosis
The prognosis of ovarian cancer is directly dependent on the disease stage at the time of diagnosis 6. It is also significantly associated with baseline performance status, FIGO (International Federation of Gynecology and Obstetrics) system and the AJCC (American Joint Committee on Cancer) TNM stage, and volume of residual disease post-primary cytoreductive surgery. Ovarian cancer 5 year relative survival is 49.7% 2. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
In women with a disease that spread to adjacent tissues, 5-year survival rates drop down to 80% and 25% for the ones with metastatic disease 7. Patients with recurrent disease can be treated. However, they are usually incurable. Recurrent platinum-sensitive ovarian cancer median survival is approximately 3 years; however, it is about just 1 year for platinum-resistant patients 8, 9.
Most of these patients with ovarian cancer develop malignant bowel obstruction in the late-stage, which is quite difficult to manage. Palliative symptom management is the mainstay in such patients. Debulking surgery is the strongest predictor of prognosis, where the volume of residual disease post-surgery is directly correlated to overall survival and progression-free survival 10.
Figure 10. Ovarian cancer 5 year relative survival
[Source SEER 17 2012–2018 2 ]Ovarian cancer survival rate
Survival rates tell you what percentage of people with the same type and stage of cancer are still alive a certain length of time (usually 5 years) after they were diagnosed. These numbers can’t tell you how long you will live, but they may help give you a better understanding about how likely it is that your treatment will be successful.
Remember, survival rates are estimates – your outlook can vary based on a number of factors specific to you.
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they can’t predict what will happen in any particular person’s case. There are a number of limitations to remember:
- The numbers below are among the most current available. But to get 5-year survival rates, doctors look at people who were treated at least 5 years ago. As treatments are improving over time, people who are now being diagnosed with ovarian cancer may have a better outlook than these statistics show.
- These statistics are based on the stage of the cancer when it was first diagnosed. They do not apply to cancers that come back later or spread, for example.
- Besides the cancer stage, many other factors can affect a person’s outlook, such as age and overall health, and how well the cancer responds to treatment.
Your doctor can tell you how these numbers may apply to you, as he or she is familiar with the aspects of your particular situation.
The Surveillance, Epidemiology, and End Results (SEER) from the National Cancer Institute database tracks 5-year relative survival rates for ovarian cancer in the United States, based on how far the cancer has spread. The SEER database, however, does not group cancers by AJCC or FIGO stages (stage 1, stage 2, stage 3, etc.). Instead, it groups cancers into localized, regional, and distant stages:
- Localized: There is no sign that the cancer has spread outside of the ovaries.
- Regional: The cancer has spread outside the ovaries to nearby structures or lymph nodes.
- Distant: The cancer has spread to distant parts of the body, such as the liver or lungs.
For all types of ovarian cancer, the 5-year relative survival is 49.7% 2. The 5-year relative survival for localized ovarian cancer is 93.1% 2.
The survival rates given below are for the different types of ovarian cancer. They come from the National Cancer Institute, SEER Database and are based on patients diagnosed with cancers of the ovary (or fallopian tube) between 2011 to 2017. These survival rates differ based on the type of ovarian cancer (invasive epithelial, stromal, or germ cell tumor).
- These numbers apply only to the stage of the cancer when it is first diagnosed. They do not apply later on if the cancer grows, spreads, or comes back after treatment.
- These numbers don’t take everything into account. Survival rates are grouped based on how far the cancer has spread. But other factors, such as your age and overall health, and how well the cancer responds to treatment, can also affect your outlook.
- People now being diagnosed with ovarian (or fallopian tube) cancer may have a better outlook than these numbers show. Treatments improve over time, and these numbers are based on people who were diagnosed and treated at least five years earlier.
Table 2. Invasive epithelial ovarian cancer survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 93% |
| Regional | 75% |
| Distant | 31% |
| All SEER stages combined | 49% |
Table 3. Ovarian stromal tumors survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 97% |
| Regional | 90% |
| Distant | 70% |
| All SEER stages combined | 90% |
Table 4. Germ cell tumors of the ovary survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 98% |
| Regional | 94% |
| Distant | 74% |
| All SEER stages combined | 93% |
Table 5. Fallopian tube carcinoma survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 95% |
| Regional | 54% |
| Distant | 44% |
| All SEER stages combined | 56% |
- Key Statistics for Ovarian Cancer. https://www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html[↩][↩]
- Ovarian Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/ovary.html[↩][↩][↩][↩][↩]
- What is ovarian cancer? https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/what-is-ovarian-cancer[↩]
- Ovarian cancer: recognition and initial management. https://www.nice.org.uk/guidance/cg122[↩]
- Ovarian Cancer Stages. https://www.cancer.org/cancer/ovarian-cancer/detection-diagnosis-staging/staging.html[↩]
- Arora T, Mullangi S, Lekkala MR. Ovarian Cancer. [Updated 2022 Aug 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567760[↩]
- Stewart C, Ralyea C, Lockwood S. Ovarian Cancer: An Integrated Review. Semin Oncol Nurs. 2019 Apr;35(2):151-156. doi: 10.1016/j.soncn.2019.02.001[↩]
- Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. Lancet. 2014 Oct 11;384(9951):1376-88. doi: 10.1016/S0140-6736(13)62146-7[↩]
- Griffiths RW, Zee YK, Evans S, Mitchell CL, Kumaran GC, Welch RS, Jayson GC, Clamp AR, Hasan J. Outcomes after multiple lines of chemotherapy for platinum-resistant epithelial cancers of the ovary, peritoneum, and fallopian tube. Int J Gynecol Cancer. 2011 Jan;21(1):58-65. doi: 10.1097/IGC.0b013e3182049273[↩]
- Chang SJ, Hodeib M, Chang J, Bristow RE. Survival impact of complete cytoreduction to no gross residual disease for advanced-stage ovarian cancer: a meta-analysis. Gynecol Oncol. 2013 Sep;130(3):493-8. doi: 10.1016/j.ygyno.2013.05.040[↩]