Contents
- Obstructive sleep apnea
- Obstructive sleep apnea causes
- Obstructive sleep apnea prevention
- Obstructive sleep apnea symptoms
- Obstructive sleep apnea complications
- Obstructive sleep apnea diagnosis
- Obstructive sleep apnea treatment
- Obstructive sleep apnea prognosis
Obstructive sleep apnea
Obstructive sleep apnea (OSA) also known as obstructive sleep apnea-hypopnea is the most common and potentially serious sleep-related breathing disorder where the muscles of your throat (upper airway) intermittently collapse and narrow during sleep, blocking your airway during sleep and interrupting normal breathing with an associated decrease in oxygen saturation or arousal from sleep 1, 2, 3, 4. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate called the uvula, the tonsils, the side walls of the throat and the tongue. When you sleep, all of the muscles in your body become more relaxed. This includes the muscles that help keep your throat open so air can flow into your lungs. It’s normal for the muscles and soft tissues in your throat to relax and collapse to some degree while sleeping. For most people this doesn’t cause breathing problems. Obstructive sleep apnea occurs when the muscles in the back of your throat relax too much to allow normal breathing, which can lower the oxygen level in your blood (hypoxia) and cause a buildup of carbon dioxide (hypercapnia) 5, 3, 4. Your brain senses that you can’t breathe, and briefly wakes you so that you can reopen your airway. This awakening is usually so brief that you don’t remember it. You can awaken with a transient shortness of breath that corrects itself quickly, within one or two deep breaths. You may make a snorting, choking or gasping sound. This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you’ll probably feel sleepy during your waking hours. People with obstructive sleep apnea may not be aware that their sleep was interrupted. In fact, many people with obstructive sleep apnea (OSA) think they slept well all night.
Obstructive sleep apnea (OSA) causes breathing to repeatedly stop (apnea) and start during sleep. Complete closure of your upper airway can lead to apnea, while partial closure allows breathing but decrease the intake of oxygen (hypopnea). A noticeable sign of obstructive sleep apnea is snoring. Snoring is caused by air squeezing through the narrowed or blocked airway. You might also snort, choke or gasp. This pattern can repeat itself 5 to 30 times or more each hour, all night. This makes it hard to reach the deep, restful phases of sleep, which can have a big impact on quality of life and increases the risk of developing certain conditions. An estimated 58% of moderate to severe obstructive sleep apnea is caused by obesity 4. Obesity is a major risk factor for obstructive sleep apnea as 60 to 70 percent of individuals with this condition have obesity 6, 7, 8, 9, 5. It is thought that excess fatty tissue in the head and neck constricts airways and abdominal fat may prevent the chest and lungs from fully expanding and relaxing. Other risk factors for obstructive sleep apnea include alcohol use; frequent nasal congestion; and blockages of the airways, such as by enlarged tonsils.
There are two types of breathing interruption characteristic of obstructive sleep apnea:
- Apnea– where the muscles and soft tissues in yout throat relax and collapse sufficiently to cause a total blockage of the airway; it’s called an apnea when the airflow is blocked for 10 seconds or more
- Hypopnea– a partial blockage of the airway that results in an airflow reduction of greater than 50% for 10 seconds or more that results in a decrease in arterial saturation of 4% or more due to partial airway obstruction 10, 11.
People with obstructive sleep apnea may experience repeated episodes of apnea and hypopnea throughout the night. These events may occur around once every one or two minutes in severe cases.
As many people with obstructive sleep apnea experience episodes of both apnea and hypopnea, doctors sometimes refer to the condition as obstructive sleep apnea-hypopnea syndrome (OSAHS).
The term “obstructive” distinguishes obstructive sleep apnea (OSA) from rarer forms of sleep apnea, such as central sleep apnea (CSA), which is caused by the brain not sending signals to the breathing muscles during sleep. The symptoms of obstructive apnea (OSA) and central sleep apnea (CSA) overlap, sometimes making it difficult to determine which type you have. Most people with sleep apnea will have a combination of both types. The hallmark symptom of sleep apnea is excessive daytime sleepiness.
In North America, the prevalence of obstructive sleep apnea (OSA) is between 15 and 30 percent in males and 10 to 15 percent in females 12, 13. The prevalence of obstructive sleep apnea (OSA) varies by race, and in the United States is more prevalent in African Americans than in other groups, independent of body weight 14, 15.
The prevalence of obstructive sleep apnea (OSA) also appears to be increasing, which is thought to be related to a combination of increasing rates of obesity as well as increased diagnosis and detection 16. In a study by Peppard et al. 13, it was estimated that the prevalence of obstructive sleep apnea (OSA) increased from 11 to 14 percent from 1990 to 2010 among adult American males.
The most common symptoms of obstructive sleep apnea include:
- Restless sleep
- Loud snoring with periods of silence followed by gasps
- Episodes in which you stop breathing during sleep — which would be reported by another person.
- Gasping for air during sleep.
- Difficulty staying asleep, known as insomnia.
- Awakening with a dry mouth.
- Morning headache.
- Falling asleep during the day
- Excessive daytime sleepiness, known as hypersomnia.
- Trouble concentrating
- Difficulty paying attention while awake
- Irritability
- Forgetfulness
- Mood or behavior changes
- Anxiety
- Depression
Not everyone who has these symptoms will have obstructive sleep apnea (OSA), but a visit to the doctor is recommended for people experiencing even a few. Obstructive sleep apnea (OSA) is more likely to occur in males than females, and in people who are overweight or obese.
When your sleep is interrupted throughout the night, you can be drowsy during the day. Left untreated, obstructive sleep apnea (OSA) can be life threatening. People with obstructive sleep apnea (OSA) are at higher risk for car crashes, work-related accidents, and other medical problems. Obstructive sleep apnea (OSA) also appears to put individuals at risk for a major health issue associated with different forms of cardiovascular disease including high blood pressure (hypertension), coronary artery disease (coronary heart disease), heart attack, heart failure, irregular heartbeat and stroke and transient ischemic attack (TIA) also known as “mini-stroke” 17. Although there is no cure for sleep apnea, recent studies show that successful treatment can reduce the risk of heart and blood pressure problems.
Doctors diagnose sleep apnea based on medical and family histories, a physical exam, and sleep study (also called polysomnography) results. The standard test for the diagnosis of sleep apnea is polysomnography (PSG) during which patients need to sleep overnight at a sleep laboratory. However, more recently home sleep testing is increasingly being used to diagnose obstructive sleep apnea (OSA). The most commonly used type of home sleep testing device records airflow, respiratory effort, oxygen saturation, and heart rate 18. Although home sleep apnea tests are widely utilized, the accuracy of the diagnosis or severity estimation of obstructive sleep apnea (OSA) with these devices is reduced 19.
Treatments for obstructive sleep apnea are available. There are a variety of treatments for obstructive sleep apnea, depending on your medical history and the severity of your obstructive sleep apnea. Lifestyle changes, mouthpieces, surgery, and breathing devices can treat obstructive sleep apnea in many people. Lifestyle changes addressing healthy diet, regular exercise, sleep hygiene, smoking and alcohol cessation are recommended in the management of obstructive sleep apnoea (OSA). Another treatment involves using a device that keep your airway open while you sleep called continuous positive airway pressure (CPAP) in which a face mask is attached to a tube and a machine that blows pressurized air into the mask and through the airway to keep it open. Machines that offer variable positive airway pressure (VPAP) and automatic positive airway pressure (APAP) are also available. Another option is a mouthpiece to thrust your jaw forward during sleep. In more severe cases, surgery may be an option too. The U.S. Food and Drug Administration (FDA) has approved a surgically implantable device, which is placed in the upper chest to monitor a person’s respiratory signals during sleep and stimulate a nerve to stimulate and restore even breathing. Some individuals may need a combination of therapies to successfully treat their obstructive sleep apnea.
In many cases, self-care may be the most appropriate way for you to deal with obstructive sleep apnea. Try these tips:
- Lose weight. If you’re overweight or obese, even a slight loss of excess weight may help relieve constriction of your airway. Losing weight can also improve your health and quality of life, and may reduce your sleepiness during the day.
- Exercise. Exercising, such as aerobic exercise and strength training, can help improve your condition. Aim to exercise about 150 minutes a week, and generally try to exercise most days of the week.
- Avoid alcohol and medications such as tranquilizers and sleeping pills. Alcohol can worsen obstructive sleep apnea and sleepiness and may lead to weight gain. Certain medications also can worsen your sleep.
- Sleep on your side or abdomen rather than on your back. Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat and block your airway. To prevent sleeping on your back, try sewing a tennis ball in the back of your pajama top.
- Keep your nasal passages open while you sleep. If you have congestion, use a saline nasal spray to help keep your nasal passages open. Talk to your doctor about using nasal decongestants or antihistamines, because some medications may only be recommended for short-term use.
Consult a medical professional if you experience, or if your partner observes, the following:
- Snoring loud enough to disturb your sleep or that of others
- Waking up gasping or choking
- Intermittent pauses in your breathing during sleep
- Excessive daytime drowsiness, which may cause you to fall asleep while you’re working, watching television or even driving a vehicle
Many people may not think of snoring as a sign of something potentially serious, and not everyone who snores has obstructive sleep apnea.
Be sure to talk to your doctor if you experience loud snoring, especially snoring that’s punctuated by periods of silence. With obstructive sleep apnea, snoring usually is loudest when you sleep on your back, and it quiets when you turn on your side.
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness may be due to other disorders, such as narcolepsy.
Obstructive sleep apnea causes
The causes of obstructive sleep apnea are often complex 20, 5, 3, 4. Obstructive sleep apnea (OSA) results from a combination of genetic, health, and lifestyle factors, many of which have not been identified.
The major predisposing factor for obstructive sleep apnea (OSA) is excess body weight, male sex, and advancing age (maximum prevalence in the middle age group 40 to 64 year) 21, 22. Obesity is a major risk factor for obstructive sleep apnea as 60 to 70 percent of individuals with obstructive sleep apnea (OSA) have obesity. It is thought that excess fatty tissue in the head and neck constricts airways and abdominal fat may prevent the chest and lungs from fully expanding and relaxing. Other risk factors for obstructive sleep apnea include alcohol use; frequent nasal congestion; and blockages of the airways, such as by enlarged tonsils.
Studies suggest that variations in multiple genes, each with a small effect, combine to increase the risk of developing obstructive sleep apnea 23, 7, 24, 25, 26, 27. However, it is unclear what contribution each of these genetic changes makes to obstructive sleep apnea risk 20. Most of the genetic mutations have been identified in single studies, and subsequent research has not verified them. Genes thought to be associated with the development of obstructive sleep apnea are involved in many body processes. These include communication between nerve cells, breathing regulation, control of inflammatory responses by the immune system, development of tissues in the head and face (craniofacial development), the sleep-wake cycle, and appetite control.
Obstructive sleep apnea often occurs on its own, without signs and symptoms affecting other parts of the body. However, obstructive sleep apnea can also occur as part of a syndrome, such as mucopolysaccharidosis type 1 or polycystic ovary syndrome (PCOS).
Other factors also may increase your risk of obstructive sleep apnea (OSA):
- A lower jaw that is short compared to your upper jaw
- Certain shapes of the roof of your mouth (palate) or airway that cause it to collapse more easily
- Large neck or collar size, 17 inches (43 centimeters) or more in men and 16 in (41 cm) or more in women
- Large tongue, which may fall back and block the airway
- Large tonsils and adenoids that can block the airway
- Age: Sleep apnea can occur at any age, but your risk increases as you get older. As you age, fatty tissue can build up in your neck and the tongue and raise your risk of obstructive sleep apnea (OSA). As you get older, normal changes in how your brain controls breathing during sleep may raise your risk of central sleep apnea (CSA).
- Endocrine disorders, or changes in your hormone levels: Your hormone levels can affect the size and shape of your face, tongue, and airway. People who have low levels of thyroid hormones or high levels of insulin or growth hormone have a higher risk of sleep apnea.
- Family history and genetics: Sleep apnea can be inherited. Your gene help determine the size and shape of your skull, face, and upper airway. Also, your genes can raise your risk of other health conditions that can lead to sleep apnea, such as cleft lip and cleft palate and Down syndrome.
- Heart or kidney failure: These conditions can cause fluid to build up in your neck, which can block your upper airway.
- Large tonsils and a thick neck: These features may cause sleep apnea because they narrow your upper airway. Also, having a large tongue and your tongue’s position in your mouth can make it easier for your tongue to block your airway while you sleep.
- Lifestyle habits: Drinking alcohol and smoking can raise your risk of sleep apnea. Alcohol can make the muscles of your mouth and throat relax, which may close your upper airway. Smoking can cause inflammation in your upper airway, which affects breathing.
- Obesity: This condition is a common cause of sleep apnea. People with this condition can have increased fat deposits in their necks that can block the upper airway. Maintaining a healthy weight can help prevent or treat sleep apnea caused by obesity.
- Sex: Sleep apnea is more common in men than in women. Men are more likely to have serious sleep apnea and to get sleep apnea at a younger age than women.
Risk factors for obstructive sleep apnea
Anyone can develop obstructive sleep apnea. However, certain factors put you at increased risk, including:
- Excess weight. Obesity greatly increases the risk of obstructive sleep apnea (OSA). Around half the people with obstructive sleep apnea are overweight. Fat deposits around the upper airway may obstruct breathing. However, not everyone with obstructive sleep apnea is overweight and vice versa. Thin people can develop the disorder, too.
- Narrowed airway. You may inherit naturally narrow airways. Or, your tonsils or adenoids may become enlarged, which can block your airway, particularly in children.
- Neck circumference. People with thicker necks might have narrower airways.
- Having an unusual inner neck structure – such as a narrow airway, large tonsils, adenoids or tongue, or a small lower jaw
- High blood pressure (hypertension). Obstructive sleep apnea is relatively common in people with hypertension.
- Nasal congestion. If you have trouble breathing through your nose — whether from an anatomical problem or allergies — you’re more likely to develop obstructive sleep apnea. Obstructive sleep apnea occurs twice as often in those who have consistent nasal congestion at night, regardless of the cause. Obstructive sleep apnea occurs more often in people with deviated septum, where the tissue in the nose that divides the two nostrils is bent to one side, or nasal polyps, which may be a result of the airways being narrowed.
- Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who’ve never smoked. Smoking can increase the amount of inflammation and fluid retention in the upper airway.
- Diabetes. Obstructive sleep apnea may be more common in people with diabetes.
- Being male. In general, men are 2 to 3 times as likely as women to have obstructive sleep apnea. It’s not known why obstructive sleep apnea is more common in men than in women, but it may be related to different patterns of body fat distribution. Women increase their obstructive sleep apnea risk if they’re overweight or if they’ve gone through menopause.
- A family history of obstructive sleep apnea. If you have family members with obstructive sleep apnea, you may be at increased risk. There may be genes inherited from your parents that can make you more susceptible to obstructive sleep apnea
- Asthma. Recent research has found an association between asthma and the risk of obstructive sleep apnea.
- Being 40 years of age or more – although obstructive sleep apnea can occur at any age, it’s more common in people who are over 40
- Having a large neck – men with a collar size greater than around 43cm (17 inches) have an increased risk of developing obstructive sleep apnea
- Taking medicines with a sedative effect – such as sleeping tablets or tranquillizers. These substances relax the muscles in your throat, which can worsen obstructive sleep apnea (OSA).
- Alcohol – drinking alcohol, particularly before going to sleep, can make snoring and sleep apnea worse
- Menopause (in women) – the changes in hormone levels during the menopause may cause the throat muscles to relax more than usual.
- Medical conditions. Congestive heart failure, high blood pressure and type 2 diabetes are some of the conditions that may increase the risk of obstructive sleep apnea. Polycystic ovary syndrome (PCOS), hormonal disorders, prior stroke and chronic lung diseases such as asthma also can increase risk.
Obstructive sleep apnea prevention
It’s not always possible to prevent obstructive sleep apnea, but making certain lifestyle changes may reduce your risk of developing the condition.
These include:
- losing weight if you’re overweight or obese
- limiting how much alcohol you drink and avoiding alcohol in the evening
- stopping smoking if you smoke
- avoiding the use of sleeping tablets and tranquillizers
Obstructive sleep apnea symptoms
The symptoms of obstructive sleep apnea are often first spotted by a partner, friend or family member who notices problems while you sleep.
The most common symptoms of obstructive sleep apnea include:
- Restless sleep
- Loud snoring with periods of silence followed by gasps
- Episodes in which you stop breathing during sleep — which would be reported by another person.
- Gasping for air during sleep.
- Difficulty staying asleep, known as insomnia.
- Awakening with a dry mouth.
- Morning headache.
- Falling asleep during the day
- Excessive daytime sleepiness, known as hypersomnia.
- Trouble concentrating
- Difficulty paying attention while awake
- Irritability
- Forgetfulness
- Mood or behavior changes
- Anxiety
- Depression
Some people with obstructive sleep apnea may also experience night sweats and may wake up frequently during the night to urinate.
During an episode, the lack of oxygen triggers your brain to pull you out of deep sleep – either to a lighter sleep or to wakefulness – so your airway reopens and you can breathe normally.
These repeated sleep interruptions can make you feel very tired during the day. You’ll usually have no memory of your interrupted breathing, so you may be unaware you have a problem.
Not everyone who has these symptoms will have sleep apnea, but a visit to the doctor is recommended for people experiencing even a few. Sleep apnea is more likely to occur in males than females, and in people who are overweight or obese.
Obstructive sleep apnea complications
Obstructive sleep apnea is a serious medical condition. Obstructive sleep apnea affects many parts of your body. It can cause low oxygen levels in your body during sleep and can prevent you from getting enough good quality sleep. Also, it takes a lot of effort for you to restart breathing many times during sleep, and this can damage your organs and blood vessels. These factors may raise your risk of the following conditions 28:
- Daytime fatigue and sleepiness. The repeated awakenings associated with obstructive sleep apnea make normal, restorative sleep impossible. People with obstructive sleep apnea often experience severe daytime drowsiness, fatigue and irritability. They may have difficulty concentrating and find themselves falling asleep at work, while watching TV or even when driving. Children and young people with obstructive sleep apnea may do poorly in school and commonly have attention or behavior problems.
- Heart and blood vessel diseases. Sudden drops in blood oxygen levels that occur during obstructive sleep apnea increase blood pressure and strain the cardiovascular system.
- Many people with obstructive sleep apnea develop difficult-to-control high blood pressure (resistant hypertension), which can increase your risk of heart disease.
- The more severe the obstructive sleep apnea, the greater the risk of coronary artery disease, atrial fibrillation, atherosclerosis, heart attacks, heart failure, pulmonary hypertension, and stroke. Men with obstructive sleep apnea appear to be at risk of heart failure, while women with obstructive sleep apnea don’t.
- Obstructive sleep apnea increases the risk of abnormal heart rhythms (arrhythmias). These abnormal rhythms can lower blood oxygen levels.
- If there’s underlying heart disease, these repeated multiple episodes of low blood oxygen could lead to sudden death from a cardiac event.
- Developing type 2 diabetes – although it’s unclear if this is the result of an underlying cause, such as obesity
- Complications with medications and surgery. Obstructive sleep apnea also is a concern with certain medications and general anesthesia. These medications, such as sedatives, narcotic analgesics and general anesthetics, relax your upper airway and may worsen your obstructive sleep apnea. If you have obstructive sleep apnea, you may experience worse breathing problems after major surgery, especially after being sedated and lying on your back. People with obstructive sleep apnea may be more prone to complications after surgery. Before you have surgery, tell your doctor if you have obstructive sleep apnea or symptoms related to obstructive sleep apnea. If you have obstructive sleep apnea symptoms, your doctor may test you for obstructive sleep apnea prior to surgery.
- Eye problems. Some research has found a connection between obstructive sleep apnea and certain eye conditions, such as glaucoma, dry eye, or an eye condition called keratoconus or conical cornea, a condition in which the clear tissue on the front of the eye (cornea) bulges outward. Eye complications can usually be treated.
- Asthma
- Cancers, such as pancreatic cancer, kidney cancer and skin cancers
- Chronic kidney disease (CKD)
- Metabolic syndrome. Metabolic syndrome is the name for a group of risk factors for heart disease, diabetes, and other health problems. Metabolic syndrome includes having high blood pressure, abnormal cholesterol levels (having a high triglyceride level or a low HDL “good” cholesterol level), having a high fasting blood sugar and an increased waist circumference also called abdominal obesity or “having an apple shape”, is linked to a higher risk of heart disease, diabetes, and stroke.
- Pregnancy complications
- Complications with medicines and surgery. Obstructive sleep apnea is also a concern with certain medicines and general anesthesia. People with sleep apnea might be more likely to have complications after major surgery because they’re prone to breathing problems, especially when sedated and lying on their backs. Before you have surgery, tell your doctor about your sleep apnea and how it’s being treated.
- Liver problems. People with sleep apnea are more likely to have irregular results on liver function tests, and their livers are more likely to show signs of scarring, known as nonalcoholic fatty liver disease.
- Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. Some partners may even choose to sleep in another room. Many bed partners of people who snore are sleep deprived as well.
People with obstructive sleep apnea may also complain of memory problems, morning headaches, mood swings or feelings of depression, and a need to urinate frequently at night (nocturia).
Research has shown someone who has been deprived of sleep because of obstructive sleep apnea may be up to 12 times more likely to be involved in a car accident.
If you’re diagnosed with obstructive sleep apnea, it may mean your ability to drive is affected. It’s your legal obligation to inform the department of motor vehicles (DMV) about a medical condition that could have an impact on your driving ability.
Once a diagnosis of obstructive sleep apnea has been made, you may be advised to stop driving until your symptoms are well controlled.
Obstructive sleep apnea diagnosis
If you think you have obstructive sleep apnea, it’s important to visit your doctor in case you need to be referred to a sleep specialist for further tests and treatment. Obstructive sleep apnoea can usually be diagnosed after you’ve been observed sleeping at a sleep clinic, or by using a testing device worn overnight at home. Your doctor will ask you about your symptoms, risk factors, and whether you have a family history of sleep apnea. You’ll have a physical examination, and your doctor will examine the back of your throat, mouth and nose for extra tissue or abnormalities. Your doctor may measure your neck and waist circumference and check your blood pressure. You may need a sleep study also called polysomnography to help diagnose sleep apnea. Your doctor will ask you to see a sleep specialist or go to a center for a sleep study. The most common type of sleep studies record brain waves and monitor your heart rate, breathing, and the oxygen level in your blood during a full night of sleep (nocturnal polysomnography). Sleep studies (polysomnography) can help diagnose which type of sleep apnea you have and how serious it is. Sleep studies (polysomnography) can also help your doctor diagnose sleep-related seizure disorders, sleep-related movement disorders, and sleep disorders that cause extreme daytime tiredness such as narcolepsy. Doctors also may use sleep tests to help diagnose or rule out restless legs syndrome. Your doctor also may refer you to an ear, nose and throat (ENT) doctor to rule out any anatomic blockage in your nose or throat.
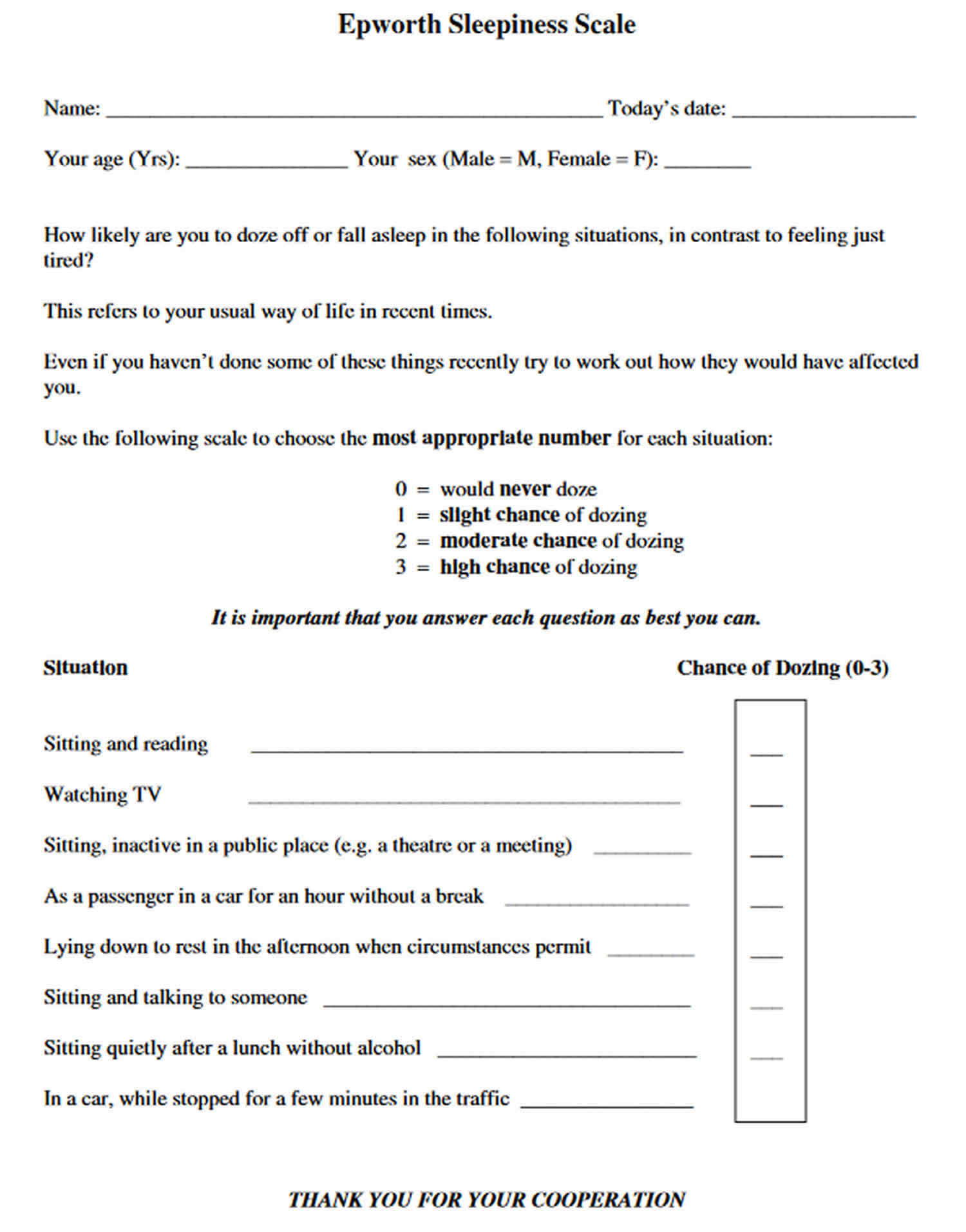
Before seeing your doctor it may be helpful to ask a partner, friend or relative to observe you while you’re asleep, if possible. If you have obstructive sleep apnea, they may be able to spot episodes of breathlessness. It may also help to fill out an Epworth Sleepiness Scale questionnaire. This asks how likely you’ll be to doze off in a number of different situations, such as watching TV or sitting in a meeting. The final score will help your doctor determine whether you may have a sleep disorder. For example, a score of 16-24 means you’re excessively sleepy and should consider seeking medical attention. A score of eight to nine is considered average during the daytime.
Figure 1. Epworth Sleepiness Scale
Sleep apnea testing
You’re likely to be referred to a sleep disorder center. There, a sleep specialist can help you determine your need for further evaluation.
An evaluation often involves overnight monitoring of your breathing and other body functions during sleep testing at a sleep center. Home sleep testing also might be an option. Tests to detect sleep apnea include:
- Nocturnal polysomnography. During this test, you’re hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep. You may have a full-night study, in which you’re monitored all night, or a split-night sleep study. In a split-night sleep study, you’ll be monitored during the first half of the night. If you’re diagnosed with obstructive sleep apnea, staff may wake you and give you continuous positive airway pressure for the second half of the night. This test can help your doctor diagnose obstructive sleep apnea and adjust positive airway pressure therapy, if appropriate. This sleep study can also help rule out other sleep disorders, such as periodic limb movements of sleep or narcolepsy, which also can cause excessive daytime sleepiness, but require different treatment.
- Home sleep tests. Under certain circumstances, your sleep specialist may provide you with an at-home version of polysomnography to diagnose obstructive sleep apnea. These tests usually measure your heart rate, blood oxygen level, airflow and breathing patterns. Your sleep specialist is more likely to recommend polysomnography in a sleep testing facility, rather than a home sleep test, if central sleep apnea (CSA) is suspected.
If your results abnormal, your sleep specialist might be able to prescribe a therapy without further testing. Portable monitoring devices sometimes miss sleep apnea. So your sleep specialist might still recommend polysomnography even if your first results are within the standard range.
If you have obstructive sleep apnea (OSA), your sleep specialist might refer you to an ear, nose and throat (ENT) specialist to rule out a blockage in your nose or throat. An evaluation by a heart specialist, known as a cardiologist, or a doctor who specializes in the nervous system, called a neurologist, might be necessary to look for causes of central sleep apnea (CSA).
Determining the severity of obstructive sleep apnea
The severity of obstructive sleep apnea is determined by how often your breathing is affected over the course of an hour. These episodes are measured using the apnea-hypopnea index (AHI).
Severity is measured using the following criteria:
- Mild obstructive sleep apnea – an apnea-hypopnea index reading of 5 to 14 episodes an hour
- Moderate obstructive sleep apnea – an apnea-hypopnea index reading of 15 to 30 episodes an hour
- Severe obstructive sleep apnea – an apnea-hypopnea index reading of more than 30 episodes an hour
Current evidence suggests treatment is most likely to be beneficial in people with moderate or severe obstructive sleep apnea. However, some research has suggested treatment may also help some people with mild obstructive sleep apnea.
Ruling out other medical conditions
Your sleep specialist may order other tests to help rule out other medical conditions that can cause sleep apnea.
- Blood tests check the levels of certain hormones to check for endocrine disorders that could contribute to sleep apnea. Thyroid hormones tests can rule out hypothyroidism. Growth hormone tests can rule out acromegaly. Total testosterone and dehydroepiandrosterone sulphate (DHEAS) tests can help rule out polycystic ovary syndrome (PCOS).
- Pelvic ultrasounds examine the ovaries and help detect cysts. This can rule out polycystic ovary syndrome (PCOS).
Your doctor will also want to know whether you are using medicines, such as opioids, that could affect your sleep or cause breathing symptoms of sleep apnea. Your doctor may want to know whether you have traveled recently to altitudes greater than 6,000 feet, because these low-oxygen environments can cause symptoms of sleep apnea for a few weeks after traveling.
Obstructive sleep apnea treatment
Obstructive sleep apnea is a treatable condition, and there are a variety of treatments for sleep apnea, depending on your medical history, condition and the severity of your sleep apnea. Lifestyle changes, mouthpieces, surgery, and breathing devices can treat sleep apnea in many people.
Treatment options for obstructive sleep apnea include:
- Lifestyle changes – such as losing excess weight, cutting down on alcohol and sleeping on your side
- Using a continuous positive airway pressure (CPAP) device – these devices prevent your airway closing while you sleep by delivering a continuous supply of compressed air through a mask
- Wearing a mandibular advancement device (MAD) – this gum shield-like device fits around your teeth, holding your jaw and tongue forward to increase the space at the back of your throat while you sleep
Surgery may also be an option if obstructive sleep apnea is thought to be the result of a physical problem that can be corrected surgically, such as an unusual inner neck structure.
However, for most people surgery isn’t appropriate and may only be considered as a last resort if other treatments haven’t helped.
The treatments mentioned above can often help control the symptoms of obstructive sleep apnea, although treatment will need to be lifelong in most cases.
If obstructive sleep apnea is left untreated, it can have a significant impact on your quality of life, causing problems such as poor performance at work and school, and placing a strain on your relationships with others.
Healthy lifestyle changes
Most obstructive sleep apnea (OSA) treatment regimens begin with lifestyle changes, such as:
- Lose weight if you’re overweight.
- Exercise regularly.
- Drink alcohol moderately, if at all, and don’t drink several hours before bedtime.
- Avoiding medications that relax the central nervous system (e.g., sedatives and muscle relaxants)
- Quit smoking.
- Use a nasal decongestant or allergy medications. If you have nasal allergies, your doctor may recommend treatment for your allergies.
- Don’t sleep on your back. Some people find relief when using special pillows or devices that keep them from sleeping on their backs, or oral appliances to keep the airway open during sleep.
If these conservative measures don’t improve your sleep or if your obstructive sleep apnea is moderate to severe, then your doctor may recommend other treatments such as continuous positive airway pressure (CPAP), in which a face mask is attached to a tube and a machine that blows pressurized air into the mask and through the airway to keep it open. Machines that offer variable positive airway pressure (VPAP) and automatic positive airway pressure (APAP) are also available. Certain devices can help open up a blocked airway. In other cases, surgery may be necessary.
Therapies
Continuous positive airway pressure (CPAP)
If you have obstructive sleep apnea, you may benefit from positive airway pressure. In this treatment, a machine delivers air pressure through a piece that fits into your nose or is placed over your nose and mouth while you sleep.
Positive airway pressure reduces the number of respiratory events that occur as you sleep, reduces daytime sleepiness and improves your quality of life.
The most common type is called continuous positive airway pressure (CPAP). With this treatment, the pressure of the air breathed is continuous, constant and somewhat greater than that of the surrounding air, which is just enough to keep your upper airway passages open. This air pressure prevents obstructive sleep apnea and snoring.
Side effects of continuous positive airway pressure (CPAP) treatment may include:
- Congestion
- Dry eyes
- Dry mouth
- Nosebleeds
- Runny nose
If you experience stomach discomfort or bloating, you should stop using your CPAP machine and contact your doctor. Depending on the type of sleep apnea you have, you may need another type of breathing device, such as an auto-adjusting positive airway pressure (APAP) machine or a bilevel positive airway pressure (BPAP or BiPAP) machine. It’s recommended that you discuss the most appropriate breathing device for you with your sleep specialist.
Although continuous positive airway pressure (CPAP) is the most common and reliable method of treating sleep apnea, some people find the mask cumbersome, uncomfortable or loud. Some people give up on the CPAP machine. But with practice, most people learn to adjust the tension of the straps on the mask to obtain a comfortable and secure fit. You may need to try different types to find a suitable mask that’s comfortable. Several options are available, such as nasal masks, nasal pillows or face masks. Moreover, newer machines are smaller and less noisy than older machines.
Don’t stop using the CPAP machine if you have problems. Check with your doctor to see what changes can be made to increase your comfort. Additionally, contact your doctor if you’re still snoring or begin snoring again despite treatment. If your weight changes, the pressure settings of the CPAP machine might need to be adjusted.
If you’re having particular difficulties tolerating pressure, some machines have special adaptive pressure functions to improve comfort. You also may benefit from using a humidifier along with your CPAP system.
If using a continuous (fixed) pressure CPAP machine continues to be a problem for you, you might be able to use a different type of airway pressure device that automatically adjusts the pressure while you’re sleeping (autotitrating-CPAP). In fixed CPAP, the pressure stays constant. In autotitrating CPAP, the levels of pressure are adjusted if the device senses increased airway resistance.
Units that supply bilevel positive airway pressure (BPAP or BiPAP) also are available. These provide more pressure when you inhale and less when you exhale.
Sleep apnea masks
Continuous positive airway pressure (CPAP) masks and headgear come in many styles and sizes to comfortably treat your sleep apnea. Everyone has different needs, preferences and face shapes, and sometimes you will need to try different mask styles before you find the one that works the best for you.
Sizes may vary across different CPAP mask styles and brands. You may need to try on several styles and sizes to find the best combination of comfort and efficiency.
For example, if you take a small in one type it does not necessarily mean you will need a small in a different brand. Proper sizing is very important to comfort and performance of CPAP masks.
Work with your doctor and CPAP mask supplier to make sure you have a mask that suits your needs and fits you properly.
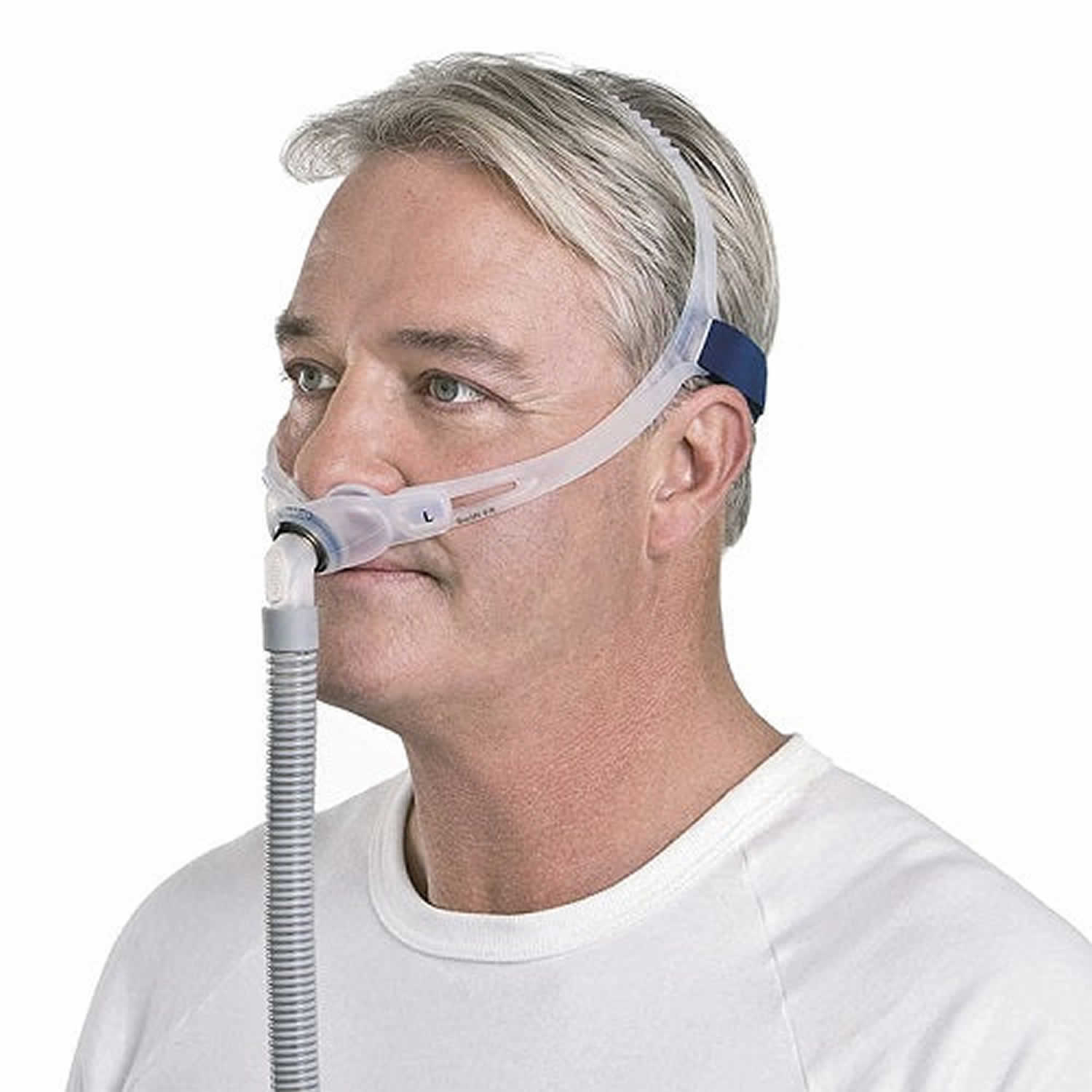
Nasal pillow CPAP mask
Nasal pillow CPAP mask fits at the nostrils to supply air pressure. Nasal pillow CPAP masks might be good if:
- You feel claustrophobic in masks that cover more of your face.
- You want a full field of vision for reading or watching TV.
- You want to wear your glasses.
- You have facial hair that interferes with other masks.
Figure 2. Nasal pillow CPAP mask
Nasal CPAP masks
Nasal CPAP masks cover your nose to supply air pressure. Nasal CPAP masks might be good if:
- Your doctor has prescribed a high air pressure setting.
- You move around a lot in your sleep.
Figure 3. Nasal CPAP masks
Full-face CPAP masks
Full-face CPAP masks also called oronasal CPAP masks cover your nose and mouth to supply air pressure. Full-face CPAP masks might be a good choice if:
- You have nasal blockage or congestion that makes it hard to breathe through your nose.
- You breathe through your mouth at night despite a month of trying a nasal mask or nasal pillow. A nasal mask or nasal pillow are typically combined with a heated humidity feature, a chin strap or both to keep your mouth closed.
Figure 4. Full-face CPAP masks
Oral CPAP masks
Oral CPAP masks also known as a hybrid CPAP masks deliver air pressure through your mouth. Oral CPAP masks might be right for you if:
- You breathe through your mouth.
- You wear eyeglasses.
Figure 5. Oral CPAP mask
Bilevel positive airway pressure (BiPAP)
Bilevel positive airway pressure (BiPAP), another type of positive airway pressure, delivers a preset amount of pressure when you breathe in and a different amount of pressure when you breathe out.
CPAP is more commonly used because it’s been well-studied for obstructive sleep apnea and has been shown to effectively treat obstructive sleep apnea. However, for people who have difficulty tolerating fixed CPAP, BiPAP or autotitrating CPAP may be worth a try.
Don’t stop using your positive airway pressure machine if you have problems. Check with your doctor to see what adjustments you can make to improve its comfort. In addition, contact your doctor if you still snore despite treatment, if you begin snoring again or if your weight changes.
Mouthpiece (oral device)
If you have sleep apnea, your doctor may prescribe an oral device also called oral appliance to keep your throat open if you do not want to use or cannot tolerate continuous positive airway pressure (CPAP). You may be referred to a dentist who custom-fits a device to your mouth so that it is comfortable and teaches you how to use it for best results. These devices may reduce your sleepiness and improve your quality of life.
Some oral devices are designed to open your throat by bringing your jaw forward, which can sometimes relieve snoring and mild obstructive sleep apnea.
A number of oral devices are available from your dentist. You might need to try different oral devices before finding one that works for you. Once you find the right fit, you’ll need to follow up with your dentist repeatedly during the first year and then regularly after that to ensure that the fit is still good and to reassess your symptoms.
Two types of oral devices work differently to open the upper airway while you sleep:
- Mandibular repositioning mouthpieces also called mandibular advancement device (MAD) are devices that cover the upper and lower teeth and hold the lower jaw in a position that prevents it from sliding backward and blocking the upper airway, which can sometimes relieve snoring and mild obstructive sleep apnea. Other devices hold your tongue in a different position. An mandibular advancement device is worn over your teeth when you’re asleep. It’s designed to hold your jaw and tongue forward to increase the space at the back of your throat and reduce the narrowing of your airway that causes snoring. Mandibular advancement devices not generally recommended for more severe obstructive sleep apnea, although they may be an option if you’re unable to tolerate using a CPAP device. Off-the-shelf mandibular advancement devices are available from specialist websites, but most experts don’t recommend them, as poor-fitting mandibular advancement devices can make symptoms worse. It’s recommended you have an mandibular advancement device made for you by a dentist or orthodontist with training and experience in treating sleep apnea.
- An mandibular advancement device may not be suitable treatment for you if you don’t have many – or any – teeth. If you have dental caps, crowns or bridgework, consult your dentist to ensure they won’t be stressed or damaged by an mandibular advancement device.
- If you and your doctor decide to explore this option, you’ll need to see a dentist experienced in dental sleep medicine appliances for the fitting and follow-up therapy. A number of devices are available. Close follow-up is needed to ensure successful treatment.
- Tongue-retaining devices are mouthpieces that hold the tongue in a forward position to prevent it from blocking the upper airway.
There are other devices that combine these features and/or use electrical stimulation to keep your upper airways open during sleep.
- Neuromuscular electrical stimulation (NMES) devices are removable devices that stimulate and tone the tongue and upper airway muscles to prevent them from collapsing and blocking the airway during sleep.
The U.S. Food and Drug Administration (FDA) has approved an neuromuscular electrical stimulation (NMES) oral device for use while awake 29. The neuromuscular electrical stimulation (NMES) device delivers electrical muscle stimulation through a removable mouthpiece that sits around the tongue. You wear the mouthpiece once a day for 20 minutes at a time, for six weeks. This device is approved for people with mild obstructive sleep apnea.
You’ll likely read, hear or see TV ads about different treatments for sleep apnea. Talk with your doctor about any treatment before you try it.
Surgery or other procedures
Surgery to treat obstructive sleep apnea isn’t routinely recommended because evidence shows it’s not as effective as CPAP at controlling the symptoms of the condition. Surgery also carries the risk of more serious complications.
Surgery is usually only considered as a last resort when all other treatment options have failed, and also if the condition is severely affecting your quality of life.
A range of surgical treatments have been used to treat obstructive sleep apnea. These include:
- Tonsillectomy – where the tonsils are removed if they’re enlarged and blocking your airway when you sleep
- Adenoidectomy – where the adenoids, small lumps of tissue at the back of the throat above the tonsils, are removed if they’re enlarged and are blocking the airway during sleep.
- Uvulopalatopharyngoplasty is a procedure in which your doctor removes tissue from the back of your mouth and top of your throat. Your tonsils and adenoids may be removed as well. Uvulopalatopharyngoplasty usually is performed in a hospital and requires a general anesthetic. Doctors sometimes remove tissue from the back of the throat with a laser (laser-assisted uvulopalatoplasty) or with radiofrequency energy (radiofrequency ablation) to treat snoring. These procedures don’t treat obstructive sleep apnea, but they may reduce snoring. Uvulopalatopharyngoplasty used to be a common surgical treatment for obstructive sleep apnea, but it’s performed less often nowadays. This is because more effective treatments are available, such as CPAP. This type of surgery can mean you’re unable to use a CPAP device properly in the future if you need to.
- Upper airway stimulation. This new device is approved for use in people with moderate to severe obstructive sleep apnea who can’t tolerate CPAP or BiPAP. A small, thin impulse generator is implanted under the skin in the upper chest. The device detects your breathing patterns and when necessary, stimulates the nerve that controls movement of the tongue. A study on the device found that it led to significant improvement in obstructive sleep apnea symptoms and improvements in quality of life.
- Jaw surgery. In this procedure, called maxillomandibular advancement, the upper and lower parts of your jaw are moved forward from the rest of your facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
- Tracheostomy. Surgical opening in the neck. You may need this form of surgery if other treatments have failed and you have severe, life-threatening obstructive sleep apnea. In this procedure, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. Air passes in and out of your lungs, bypassing the blocked air passage in your throat.
- Weight loss (bariatric) surgery – where the size of the stomach is reduced if you’re severely obese and this is making your sleep apnoea worse
- Soft palate implants. This minimally invasive treatment involves placement of three tiny polyester rods in the soft palate. These inserts stiffen and support the tissue of the soft palate and reduce upper airway collapse and snoring. This treatment is recommended only for people with mild obstructive sleep apnea. The National Institute for Health and Care Excellence (NICE) has said soft palate implants are safe, but they’re not currently recommended for treating obstructive sleep apnea as there’s a lack of evidence about their effectiveness. However, this form of treatment is recommended for treating snoring associated with obstructive sleep apnea in exceptional cases.
Other types of surgery may help reduce snoring and sleep apnea by clearing or enlarging air passages, including:
- Nasal surgery to remove polyps or straighten a crooked partition between your nostrils (deviated septum)
Surgery for obstructive sleep apnea (OSA)
Surgery may be an option for people with obstructive sleep apnea (OSA), but usually only after other treatments have failed. Generally, at least a three-month trial of other treatment options is suggested before considering surgery. However, for a small number of people with certain jaw structure problems, surgery is a good first option.
Surgical options might include:
- Tissue removal. During this procedure (uvulopalatopharyngoplasty), a surgeon removes tissue from the rear of your mouth and top of the throat. Your tonsils and adenoids usually are removed as well. This type of surgery might be successful in stopping throat structures from vibrating and causing snoring. It’s less effective than CPAP and isn’t considered a reliable treatment for obstructive sleep apnea. Removing tissues in the back of the throat with radiofrequency energy (radiofrequency ablation) might be an option for those who can’t tolerate CPAP or oral appliances.
- Tissue shrinkage. Another option is to shrink the tissue at the rear of the mouth and the back of the throat using radiofrequency ablation. This procedure might be used for mild to moderate sleep apnea. One study found this to have effects similar to that of tissue removal, but with fewer surgical risks.
- Jaw repositioning also known as maxillomandibular advancement. In this procedure, the jaw is moved forward from the remainder of the face bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
- Implants. Soft rods, usually made of polyester or plastic, are surgically implanted into the soft palate after numbing with a local anesthetic. More research is needed to determine how well implants work.
- Nerve stimulation. This requires surgery to insert a stimulator for the nerve that controls tongue movement (hypoglossal nerve). The increased stimulation helps keep the tongue in a position that keeps the airway open. More research is needed.
- Creating a new air passageway also known as tracheostomy. You may need this form of surgery if other treatments have failed and you have severe, life-threatening sleep apnea. In this procedure, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. You keep the opening covered during the day. But at night you uncover it to allow air to pass in and out of your lungs, bypassing the blocked air passage in your throat.
Other types of surgery may help reduce snoring and contribute to the treatment of sleep apnea by clearing or enlarging air passages:
- Surgery to remove enlarged tonsils and adenoids (adenotonsillectomy).
- Weight-loss surgery, also known as bariatric surgery.
Therapy for your mouth and facial muscles
Exercises for your mouth and facial muscles, called orofacial therapy, may also be an effective treatment for obstructive sleep apnea (OSA) in children and adults. This therapy helps to strengthen and reposition the tongue and muscles that control your lips, tongue, upper airway, and face.
Sleep apnea monitoring
If you have been diagnosed with sleep apnea, you will need to schedule regular check-ups to make sure that your treatment is working and whether you have any complications. You may need to repeat your sleep study to monitor your symptoms while using your treatment, especially if you gain or lose a lot of weight. You may also need treatment for other health conditions that caused your sleep apnea or can make it worse.
Obstructive sleep apnea prognosis
Undiagnosed or untreated sleep apnea prevents you from getting enough rest, which can cause problems concentrating, remembering things, making decisions, or controlling your behavior, as well as dementia in older adults. In children, sleep apnea can lead to problems with learning and memory, known as learning disabilities. The daytime sleepiness and fatigue that results from sleep apnea can also impact your child’s behavior and their desire to be physically active.
The short-term prognosis of obstructive sleep apnea (OSA) with treatment is good, but the long-term prognosis is guarded 3. The biggest problem is the lack of adherence to CPAP, as nearly 50% of patients stop using CPAP within the first month despite education 30. Many patients have two or more other medical conditions on top of sleep apnea or are at risk for adverse heart events and stroke. Therefore, those who do not use CPAP are at increased risk of heart and brain adverse events in addition to higher annual healthcare-related expenses 31, 32.
Furthermore, obstructive sleep apnea (OSA) is also associated with pulmonary hypertension, hypercapnia, hypoxemia, and daytime sedation, and these individuals have a high risk of motor vehicle accidents 3. The overall life expectancy of patients with obstructive sleep apnea (OSA) is lower than the general population 3. Obstructive sleep apnea (OSA) is known to affect heart function, particularly in obese individuals 33, 34. CPAP treatment was recently found to improve left and right ventricular mechanics in patients with obstructive sleep apnea (OSA) 35.
- Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014 Feb 22;383(9918):736-47. doi: 10.1016/S0140-6736(13)60734-5[↩]
- Heatley E.M., Harris M., Battersby M., McEvoy R.D., Chai-Coetzer C.L., Antic N.A. Obstructive sleep apnoea in adults: A common chronic condition in need of a comprehensive chronic condition management approach. Sleep Med. Rev. 2013;17:349–355. doi: 10.1016/j.smrv.2012.09.004[↩]
- Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea. [Updated 2024 Mar 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459252[↩][↩][↩][↩][↩][↩]
- Memon J, Manganaro SN. Obstructive Sleep-Disordered Breathing. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441909[↩][↩][↩][↩]
- Sankri-Tarbichi AG. Obstructive sleep apnea-hypopnea syndrome: Etiology and diagnosis. Avicenna J Med. 2012 Jan;2(1):3-8. doi: 10.4103/2231-0770.94803[↩][↩][↩]
- Carneiro-Barrera A, Díaz-Román A, Guillén-Riquelme A, Buela-Casal G. Weight loss and lifestyle interventions for obstructive sleep apnoea in adults: Systematic review and meta-analysis. Obes Rev. 2019 May;20(5):750-762. doi: 10.1111/obr.12824[↩]
- Feliciano A, Torres VM, Vaz F, Carvalho AS, Matthiesen R, Pinto P, Malhotra A, Barbara C, Penque D. Overview of proteomics studies in obstructive sleep apnea. Sleep Med. 2015 Apr;16(4):437-45. doi: 10.1016/j.sleep.2014.11.014[↩][↩]
- Mehrtash M, Bakker JP, Ayas N. Predictors of Continuous Positive Airway Pressure Adherence in Patients with Obstructive Sleep Apnea. Lung. 2019 Apr;197(2):115-121. doi: 10.1007/s00408-018-00193-1[↩]
- Esteller E, Carrasco M, Díaz-Herrera MÁ, Vila J, Sampol G, Juvanteny J, Sieira R, Farré A, Vilaseca I. Clinical Practice Guideline recommendations on examination of the upper airway for adults with suspected obstructive sleep apnoea-hypopnoea syndrome. Acta Otorrinolaringol Esp (Engl Ed). 2019 Nov-Dec;70(6):364-372. English, Spanish. doi: 10.1016/j.otorri.2018.06.008[↩]
- Sleep apnoea: What Is Sleep Apnoea? NHLBI: Health information for the public. U S Department of Health and Human services. 2009 May; Assessed from internet on 20th November, 2010[↩]
- US Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, García FA, Herzstein J, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Phillips WR, Phipps MG, Pignone MP, Silverstein M, Tseng CW. Screening for Obstructive Sleep Apnea in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2017 Jan 24;317(4):407-414. doi: 10.1001/jama.2016.20325[↩]
- Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ. 2009 Aug;108(5):246-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2858234[↩]
- Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013 May 1;177(9):1006-14. doi: 10.1093/aje/kws342[↩][↩]
- Redline S, Tishler PV, Hans MG, Tosteson TD, Strohl KP, Spry K. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997 Jan;155(1):186-92. doi: 10.1164/ajrccm.155.1.9001310. Erratum in: Am J Respir Crit Care Med 1997 May;155(5):1820.[↩]
- Ancoli-Israel S, Klauber MR, Stepnowsky C, Estline E, Chinn A, Fell R. Sleep-disordered breathing in African-American elderly. Am J Respir Crit Care Med. 1995 Dec;152(6 Pt 1):1946-9. doi: 10.1164/ajrccm.152.6.8520760[↩]
- Cumpston E, Chen P. Sleep Apnea Syndrome. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564431[↩]
- Tietjens JR, Claman D, Kezirian EJ, De Marco T, Mirzayan A, Sadroonri B, Goldberg AN, Long C, Gerstenfeld EP, Yeghiazarians Y. Obstructive Sleep Apnea in Cardiovascular Disease: A Review of the Literature and Proposed Multidisciplinary Clinical Management Strategy. J Am Heart Assoc. 2019 Jan 8;8(1):e010440. doi: 10.1161/JAHA.118.010440[↩]
- Bazoukis G, Bollepalli SC, Chung CT, Li X, Tse G, Bartley BL, Batool-Anwar S, Quan SF, Armoundas AA. Application of artificial intelligence in the diagnosis of sleep apnea. J Clin Sleep Med. 2023 Jul 1;19(7):1337-1363. doi: 10.5664/jcsm.10532[↩]
- Kapoor M, Greenough G. Home Sleep Tests for Obstructive Sleep Apnea (OSA). J Am Board Fam Med. 2015 Jul-Aug;28(4):504-9. doi: 10.3122/jabfm.2015.04.140266[↩]
- Obstructive sleep apnea. https://medlineplus.gov/genetics/condition/obstructive-sleep-apnea[↩][↩]
- Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010 May;11(5):441-6. doi: 10.1016/j.sleep.2009.10.005[↩]
- Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998 Jan;157(1):144-8. doi: 10.1164/ajrccm.157.1.9706079[↩]
- de Lima FF, Mazzotti DR, Tufik S, Bittencourt L. The role inflammatory response genes in obstructive sleep apnea syndrome: a review. Sleep Breath. 2016 Mar;20(1):331-8. doi: 10.1007/s11325-015-1226-7[↩]
- Larkin EK, Patel SR, Goodloe RJ, Li Y, Zhu X, Gray-McGuire C, Adams MD, Redline S. A candidate gene study of obstructive sleep apnea in European Americans and African Americans. Am J Respir Crit Care Med. 2010 Oct 1;182(7):947-53. doi: 10.1164/rccm.201002-0192OC[↩]
- Parish JM. Genetic and immunologic aspects of sleep and sleep disorders. Chest. 2013 May;143(5):1489-1499. doi: 10.1378/chest.12-1219. Erratum In: Chest. 2013 Aug;144(2):721.[↩]
- Patel SR, Goodloe R, De G, Kowgier M, Weng J, Buxbaum SG, Cade B, Fulop T, Gharib SA, Gottlieb DJ, Hillman D, Larkin EK, Lauderdale DS, Li L, Mukherjee S, Palmer L, Zee P, Zhu X, Redline S. Association of genetic loci with sleep apnea in European Americans and African-Americans: the Candidate Gene Association Resource (CARe). PLoS One. 2012;7(11):e48836. doi: 10.1371/journal.pone.0048836[↩]
- Xu H, Guan J, Yi H, Yin S. A systematic review and meta-analysis of the association between serotonergic gene polymorphisms and obstructive sleep apnea syndrome. PLoS One. 2014 Jan 27;9(1):e86460. doi: 10.1371/journal.pone.0086460[↩]
- Living With Sleep Apnea. https://www.nhlbi.nih.gov/health/sleep-apnea/living-with[↩]
- FDA Authorizes Marketing of Novel Device to Reduce Snoring and Mild Obstructive Sleep Apnea in Patients 18 Years and Older. https://www.fda.gov/news-events/press-announcements/fda-authorizes-marketing-novel-device-reduce-snoring-and-mild-obstructive-sleep-apnea-patients-18[↩]
- Guralnick AS, Balachandran JS, Szutenbach S, Adley K, Emami L, Mohammadi M, Farnan JM, Arora VM, Mokhlesi B. Educational video to improve CPAP use in patients with obstructive sleep apnoea at risk for poor adherence: a randomised controlled trial. Thorax. 2017 Dec;72(12):1132-1139. doi: 10.1136/thoraxjnl-2017-210106[↩]
- Marshall NS, Wong KK, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study cohort. J Clin Sleep Med. 2014 Apr 15;10(4):355-62. doi: 10.5664/jcsm.3600[↩]
- Bock JM, Needham KA, Gregory DA, Ekono MM, Wickwire EM, Somers VK, Lerman A. Continuous Positive Airway Pressure Adherence and Treatment Cost in Patients With Obstructive Sleep Apnea and Cardiovascular Disease. Mayo Clin Proc Innov Qual Outcomes. 2022 Apr 4;6(2):166-175. doi: 10.1016/j.mayocpiqo.2022.01.002[↩]
- Alkatib S, Sankri-Tarbichi AG, Badr MS. The impact of obesity on cardiac dysfunction in patients with sleep-disordered breathing. Sleep Breath. 2014 Mar;18(1):137-42. doi: 10.1007/s11325-013-0861-0[↩]
- Saeed S, Romarheim A, Solheim E, Bjorvatn B, Lehmann S. Cardiovascular remodeling in obstructive sleep apnea: focus on arterial stiffness, left ventricular geometry and atrial fibrillation. Expert Rev Cardiovasc Ther. 2022 Jun;20(6):455-464. doi: 10.1080/14779072.2022.2081547[↩]
- Tadic M, Gherbesi E, Faggiano A, Sala C, Carugo S, Cuspidi C. The impact of continuous positive airway pressure on cardiac mechanics: Findings from a meta-analysis of echocardiographic studies. J Clin Hypertens (Greenwich). 2022 Jul;24(7):795-803. doi: 10.1111/jch.14488[↩]