Contents
- What is ovarian pain?
- Female reproductive system
- Ovarian pain causes
- Ovarian pain symptoms
- Ovarian pain diagnosis
- Ovarian pain treatment
- Ovarian cysts
- Ovarian torsion
- Ovarian cancer
- Ovarian cancer types
- Ovarian cancer causes
- Ovarian cancer risk factors
- Getting older
- Being overweight or obese
- Having children later or never having a full-term pregnancy
- Using fertility treatment
- Taking hormone therapy after menopause
- Having a family history of ovarian cancer, breast cancer, or colorectal cancer
- Having a family cancer syndrome
- Having had breast cancer
- Endometriosis or diabetes
- Smoking and alcohol use
- Asbestos
- Ovarian cancer signs and symptoms
- Can ovarian cancer be found early?
- Ovarian cancer diagnosis
- Ovarian cancer stages
- Grades of ovarian cancer
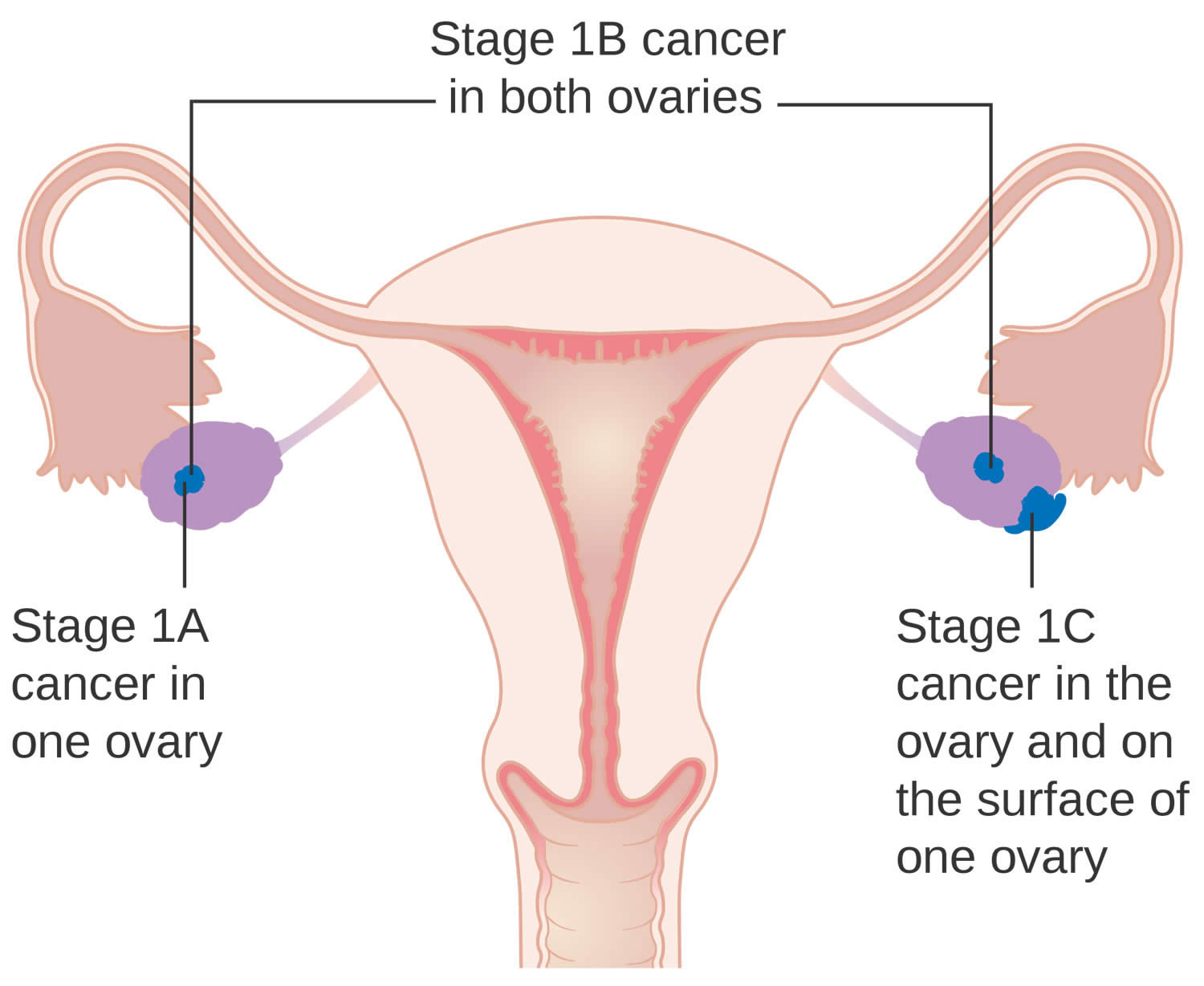
- Stage 1 ovarian cancer
- Stage 2 ovarian cancer
- Stage 3 ovarian cancer
- Stage 4 ovarian cancer
- Ovarian cancer treatment
- Ovarian cancer prognosis
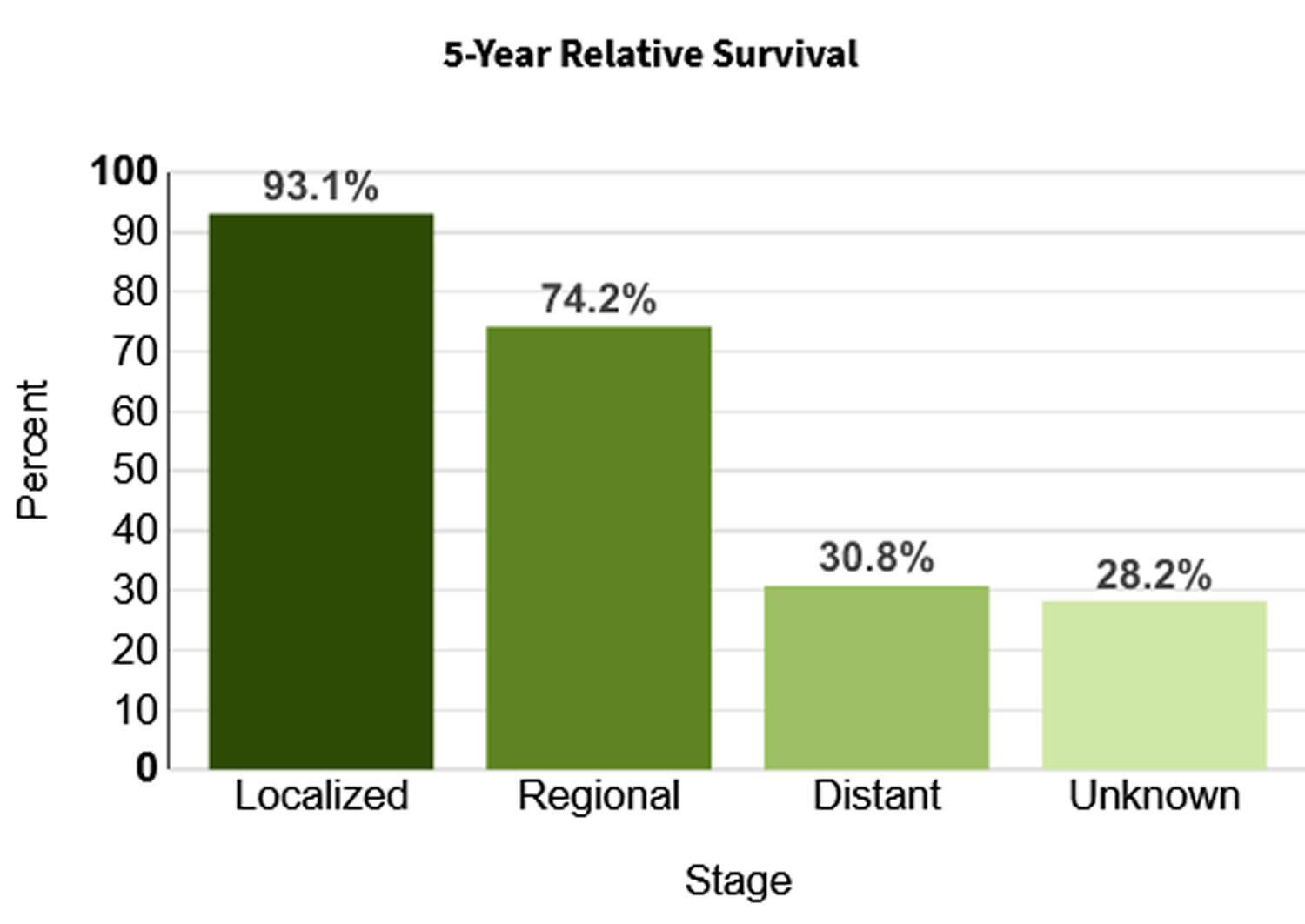
- Ovarian cancer survival rate
- Endometriosis
- Pelvic inflammatory disease
- How common is pelvic inflammatory disease in the United States?
- Can pelvic inflammatory disease be cured?
- What can happen if pelvic inflammatory disease is not treated?
- Can I get pregnant if I have had pelvic inflammatory disease?
- Who gets pelvic inflammatory disease?
- How do you get pelvic inflammatory disease?
- Can women who have sex with women get pelvic inflammatory disease?
- Pelvic inflammatory disease causes
- Risk factors for developing pelvic inflammatory disease
- Pelvic inflammatory disease prevention
- Pelvic inflammatory disease signs and symptoms
- Pelvic inflammatory disease diagnosis
- Pelvic inflammatory disease treatment
- Ectopic pregnancy
What is ovarian pain?
Ovarian pain also called pelvic pain is a general term to describe pain women feel in their lower abdomen below their belly button or in their pelvis. The pelvic region includes the lower stomach, lower back, buttocks, and genital area 1. Your pelvis contains your ovaries, uterus and fallopian tubes and also include many muscles, joints, and your bowel (intestines) and urine bladder. Ovarian pain can have many causes including ovarian cysts, ovarian cancer, endometriosis, pelvic inflammatory disease (a sexually transmitted disease [STD] or sexually transmitted infection [STI] caused by bacterial infection that are passed on through sexual contact infecting the female reproductive system that can affect your uterus, fallopian tubes, and ovaries), ovarian torsion (a medical emergency that occurs when an ovary twists on its supporting ligaments cutting off the blood supply to the ovary, which can cause tissue death if not treated promptly), ectopic pregnancy (when a fertilized egg implants and grows outside the main cavity of your uterus or womb) or other female related health issues. Your current physical factors (such as your physical health conditions, inflammation and your hormones), psychological factors (such as how pain affects your mood and sleep and how you think about your pain) and social factors (such as your relationships, your workplace and your social connections) can all contribute to you developing ovarian pain. In other words, many conditions can cause your ovarian pain or pelvic pain. Some are serious requiring emergency care, while others aren’t a cause for concern. Therefore, you should see your doctor for any ovary or pelvic pain. Moreover, not all causes of ovary pain are serious. In most cases, ovary pain isn’t cancer. Less serious conditions and diseases are more likely to be the cause of ovary pain. In any event, your doctor is the best person to evaluate your symptoms and determine an underlying cause of your ovary pain.
Be sure to get pelvic pain checked by your doctor if it’s new, it disrupts your daily life or it gets worse over time. Because your reproductive health is an important part of your overall physical, mental and emotional health and wellbeing. Having a healthy reproductive system allows you to have a safe and healthy sex life, the choice to have a child if you wish, a healthy pregnancy, and maternity care. Keeping up with your annual health and gynecological exams can be helpful because these visits help your doctor spot potential problems before they become something more serious.
How bad your pain is does not always reflect the seriousness of the condition causing your pain. Women describe pelvic pain in many ways. Ovarian pain may be constant or come and go (recurrent pain). It can be a sharp and stabbing pain felt in a specific spot, or a dull pain that is spread out. Ovarian pain can be short-lived also known as acute pelvic pain. It also may occur over weeks, months or years, also known as chronic pelvic pain or persistent pelvic pain. Ovarian pain can feel like cramping, bloating, or constipation pain in your abdomen. Some women have pain that occurs only during their menstrual periods. Some women feel pain when they need to use the bathroom, and some feel pain when lifting something heavy. Because ovarian pain is non-specific term to describe anything that can cause pelvic pain, you’ll need to see your doctor right away if you have pelvic pain so severe that you can’t move without causing more pain. Also see your doctor if you can’t sit still or find a comfortable position.
Having a healthy reproductive system requires you knowing when to ask for help from your doctor. To help prevent reproductive health problems, it is important to reach out to health services when you need them, including:
- family planning services
- health care, including preventive screening, diagnosis and treatment of reproductive issues, abortion services, and pregnancy and delivery care
- contraception
- prevention and treatment of sexually transmissible infection (STI) or sexually transmitted disease (STD)
- health care and support in cases of family, domestic and sexual violence.
To diagnose your pain, your doctor will ask you about your symptoms and do a physical examination. Your doctor may recommend having an ultrasound or other imaging scan to look at your pelvic area. Sometimes, your doctor may recommend an operation to check possible causes. A laparoscopy (keyhole surgery) uses a camera to look inside your pelvis, while a cystoscopy uses a small camera to look inside your bladder. You may need to see a gynecologist, pain specialist, physical therapist or a psychologist as part of investigating and treating your pain.
Treatment for pelvic pain is tailored to each patient, depending on the underlying causes of the pain, how bad the pain is, and how often it occurs:
- For ovarian cysts, monitoring is often the first step because many go away on their own.
- For uterine fibroids, over-the-counter medications like ibuprofen or naproxen can help with mild pain.
- Antibiotics if your doctor suspects pelvic inflammatory disease (PID) or a sexually transmitted infection (STI).
- Hormones for conditions such as endometriosis or heavy menstrual bleeding.
- Some people experience pain in the area around their ovaries just before or when they get their period. Like ovulation pain, it’s not a cause for concern. It happens because your uterus is contracting in order to shed your uterine lining. Taking over-the-counter pain relievers or using a heating pad can help.
- Treatment for ovulation pain usually involves over-the-counter (OTC) pain medication like ibuprofen. Some people find relief by taking birth control pills because they prevent ovulation from happening. Luckily, ovulation pain usually lasts just a few days and doesn’t cause any long-term complications.
- Surgery for some women with adhesions, adenomyosis or endometriosis.
- Physical therapy and biofeedback for women with myofascial (connective tissue) or muscle pain.
- Psychological therapy, medication, or both to help you cope with chronic pain. A therapist can offer support and tools to handle living with chronic pain, and can also help you and your partner cope with the relationship and sexual issues that can arise as a result of chronic pain.
- Healthy nutrition such as a diet rich in fruits, vegetables and grains is important for constipation and diverticulitis. Avoiding foods that can increase inflammation and increasing foods that decrease inflammation can be useful.
- For severe pain, seek medical advice.
Figure 1. Gastrointestinal tract (human digestive system)
Figure 2. Pelvic cavity
If you have any persistent ovary or pelvic pain, it’s best to see a doctor right away. Sudden and severe pelvic pain could be a medical emergency. You should also call your local emergency number and ask for an ambulance if you have sudden pelvic pain, you’re unable to stand up straight, nausea, severe vaginal bleeding, and are feeling faint.
See your doctor if you have the following symptoms:
- pain in your lower abdomen, upper thighs or back
- painful, heavy or irregular periods, or no periods at all
- irregular bleeding or bleeding between your periods
- periods that last more than 8 days or are more than 2 to 3 months apart
- pain during or after sex
- infertility
- there’s blood in your urine or poop
- bowel problems (such as constipation, diarrhea)
- bleeding between periods
- bleeding after intercourse
- fever
- bleeding after menopause
- you’re pregnant or have been pregnant in the last six months.
Also see your doctor if there is any change in your menstrual cycle that worries you.
Pelvic pain may be serious if your symptoms develop suddenly or if the discomfort is severe. If you have pelvic pain that lasts for more than two weeks, schedule an appointment with a doctor.
Female reproductive system
The female reproductive system includes parts of the female body that are involved in sexual activity, fertility, pregnancy and childbirth. The female reproductive system is made up of female body parts that include the following:
- Ovaries — There are 2 ovaries, which are about the size and shape of almonds, 1 ovary on each side of the uterus where female hormones (estrogen and progesterone) are produced, and eggs (ova) are stored to mature. Every month, an egg (ovum) is released. This is called ovulation. All the other female reproductive organs are there to transport, nurture and otherwise meet the needs of the egg or developing fetus.
- Fallopian tubes are 2 thin tubes that connect your ovaries to your uterus (womb), allowing the egg (ovum) to travel to your uterus (womb).
- The fallopian tubes are about 10 cm long and begin as funnel-shaped passages next to the ovary. They have a number of finger-like projections known as fimbriae on the end near the ovary. When an egg is released by the ovary it is ‘caught’ by one of the fimbriae and transported along the fallopian tube to the uterus. The egg is moved along the fallopian tube by the wafting action of cilia — hairy projections on the surfaces of cells at the entrance of the fallopian tube — and the contractions made by the tube. It takes the egg about 5 days to reach the uterus and it is on this journey down the fallopian tube that fertilisation may occur if a sperm penetrates and fuses with the egg. The egg, however, is usually viable for only 24 hours after ovulation, so fertilization usually occurs in the top one-third of the fallopian tube.
- Uterus (the womb) — Your uterus also known as the womb is a hollow muscular organ about the size of a pear (in women who have never been pregnant) that exists to house a developing fertilized egg (zygote). The main part of the uterus which sits in the pelvic cavity is called the body of the uterus, while the rounded region above the entrance of the fallopian tubes is the fundus and its narrow outlet, which protrudes into the vagina, is the cervix. The thick wall of your uterus is composed of 3 layers. The inner layer is known as the endometrium. The inner lining of your uterus (endometrium) thickens with blood and other substances every month. If an egg (ovum) has been fertilized (zygote), pregnancy occurs, the fertilized egg (zygote) will burrow into the endometrium in your uterus, where it will stay for the rest of its growth, growing into a fetus and then a baby. Your uterus (womb) will expand during a pregnancy to make room for the growing fetus. A part of the wall of the fertilized egg (zygote), which has burrowed into the endometrium, develops into the placenta. If an egg has not been fertilized, the endometrial lining is shed at the end of each menstrual cycle, this lining flows out of your body. This is known as menstruation or your period.
- The myometrium is the large middle layer of your uterus, which is made up of interlocking groups of muscle. It plays an important role during the birth of a baby, contracting rhythmically to move the baby out of the body via the birth canal (vagina).
- Cervix is the lower part of your uterus, that connects your uterus to your vagina.
- Vagina is a muscular tube connecting your cervix to the outside of your body (the vestibule of the vulva). Your vagina receives the penis and semen during sexual intercourse and also provides a passageway for menstrual blood flow to leave the body.
The female reproductive system also plays an important part in pregnancy and birth.
Figure 3. Female reproductive system (normal female reproductive system anatomy)
Figure 4. Female reproductive system
What are the ovaries?
Ovaries are female reproductive glands found only in females (women). The 2 ovaries (one ovary is on each side of your uterus or womb) produce female hormones (estrogen and progesterone) and eggs (ova) for reproduction. The eggs travel from your ovaries through the fallopian tubes into your uterus (womb) where the fertilized egg settles in and develops into a fetus (unborn baby).
Your ovaries are held in place by various ligaments which anchor them to your uterus and the pelvis. The ovary contains ovarian follicles, in which eggs develop. Once a follicle is mature, it ruptures and the developing egg is ejected from the ovary into the fallopian tubes. This is called ovulation. Ovulation occurs in the middle of the menstrual cycle and usually takes place every 28 days or so in a mature female. It takes place from either the right or left ovary at random.
Your ovaries are mainly made up of 3 kinds of cells. Each type of cell can develop into a different type of tumor:
- Epithelial tumors start from the cells that cover the outer surface of the ovary. Most ovarian tumors are epithelial cell tumors.
- Germ cell tumors start from the cells that produce the eggs (ova).
- Stromal tumors start from structural tissue cells that hold the ovary together and produce the female hormones estrogen and progesterone.
Some of these tumors are benign (non-cancerous) and never spread beyond the ovary. Malignant (cancerous) or borderline (low malignant potential) ovarian tumors can spread (metastasize) to other parts of the body and can be fatal.
Figure 5. The ovaries lie in shallow depressions in the lateral wall of the pelvic cavity
Figure 6. Ovary anatomy
Figure 7. Normal ovary
Figure 8. Ovary blood supply
What is menstruation and the menstrual cycle?
Each menstrual cycle prepares you for a possible pregnancy. The lining of your uterus thickens and once a month during ovulation, an egg releases from one of your ovaries to the endometrium (internal lining of the uterus).
During sex, the egg can be fertilized when sperm travels to the uterus. If a sperm fertilises an egg, the endometrium will thicken and grow to support the pregnancy.
If the egg isn’t fertilized, the lining which is mostly blood, breaks down from the uterus and leaves the body from the vagina as a period also known as menstruation, menses or the menstrual flow.
Menopause is when you stop having your period. This usually happens between the ages of 45 and 55 years. The average age of menopause in Western countries is 51 to 52 year of age. At menopause, your ovaries stop making hormones and eggs are no longer ripened or released.
Ovarian pain causes
Many types of diseases and health conditions that can cause pelvic pain and it may be difficult to figure out the specific cause or causes 2. Pelvic pain can start in your digestive, reproductive or urinary systems. Some pelvic pain also can come from certain muscles or ligaments within your pelvis, for example, pulling a muscle in your hip or your pelvic floor. Pelvic pain also might be caused by irritation of nerves in your pelvis. A woman’s pelvic pain may result from multiple causes occurring all at the same time 3. In many cases, pelvic pain indicates a problem with one or more of the organs in the pelvic area, such as the uterus, vagina, intestine, or bladder.
Pelvic pain might be caused by problems linked with organs in the female reproductive system. These problems include:
- Adenomyosis — when tissue that lines the inside of the uterus grows into the wall of the uterus.
- Endometriosis — when tissue that’s similar to the tissue that lines your uterus grows outside your uterus such as your fallopian tubes or ovaries. Endometriosis can cause symptoms like severe pain and cramping in your ovaries. Untreated endometriosis can make it difficult for you to get pregnant. Your doctor may perform a pelvic ultrasound, MRI or laparoscopy to get a better look at your pelvic region. There isn’t one treatment for endometriosis. Hormonal medications like birth control can help with pain and bleeding. Surgery to remove scarring from endometriosis can also help with painful symptoms.
- Ovarian tumors are solid masses that grow in your ovary. They can be cancerous or noncancerous. Ovarian germ cell tumors and granulosa cell tumors are examples of tumors that can cause painful ovaries. Some examples of noncancerous tumors include a dermoid tumor or teratoma. Doctors diagnose ovarian tumors with ultrasound and imaging tests like computed tomography (CT) or magnetic resonance imaging (MRI). Treatment for ovarian tumors usually involves surgery to remove the tumors.
- Ovarian cancer is cancer that starts in your ovaries. There are several types of ovarian cancer, and the treatment and outlook (prognosis) for each are different. Symptoms of ovarian cancer also vary. Cancer in your ovaries can cause ovary pain that’s severe or different from typical menstrual cycle pain. You may also feel bloated or full. It’s important to catch cancer early and begin treatment as soon as possible. Remember, ovary pain is rarely cancer, but you should see your doctor just in case. Your doctor may recommend a blood test called a CA-125 test that checks for proteins commonly found in people with ovarian cancer.
- Ovarian cysts are fluid-filled sacs that form in or on your ovaries and are usually noncancerous. However, ovarian cysts can cause unpleasant symptoms, like pain in your ovaries, pain during sex and irregular menstrual bleeding. Ovarian cysts can rupture (burst) and cause internal bleeding and severe abdominal pain. Your doctor can diagnose ovarian cysts with a pelvic exam and ultrasound. A lot of ovarian cysts go away on their own or with the help of hormonal birth control pills. If you need surgery, your doctor can remove an ovarian cyst with a minimally invasive procedure called laparoscopy. This involves removing the cyst through a small incision.
- Ovarian torsion is when your ovary twists around the ligaments that hold it in place. It most often occurs due to a cyst, tumor or from polycystic ovary syndrome (PCOS). You’re also at higher risk for ovarian torsion if you’re undergoing fertility treatments to get pregnant. Ovarian torsion can cause severe and sudden pain in your ovaries and pelvis. It’s a medical emergency and requires surgery to untwist your ovary.
- Ovarian remnant syndrome (ORS) occurs when ovarian tissue is left over from surgery to remove your ovaries (oophorectomy) and fallopian tubes (salpingectomy). This tissue can cause pelvic pain, pain during sex or problems when you urinate or poop.
- Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. Pelvic inflammatory disease (PID) affects the organs in your pelvis, including your ovaries. Pelvic inflammatory disease (PID) can lead to permanent damage and affect your ability to get pregnant. Symptoms of pelvic inflammatory disease (PID) are similar to other conditions involving your reproductive organs, such as pain in your abdomen, painful sex and irregular bleeding. Doctors diagnose pelvic inflammatory disease (PID) through a pelvic exam and other tests that check your vaginal fluid for infection (including sexually transmitted infections, or STIs). Antibiotics treat pelvic inflammatory disease (PID). Because it can cause long-term complications, getting prompt treatment for pelvic inflammatory disease (PID) is important.
- Uterine fibroids are noncancerous growths that develop within the muscle lining of your uterus. They can cause pain in your pelvic area, including around your ovaries. Another common symptom of fibroids is heavy or abnormal vaginal bleeding. Doctors treat uterine fibroids with medication or with a surgical procedure called a myomectomy.
- Vulvodynia — chronic pain around the opening of the vagina or the surrounding lips (vulva). The cause of vulvodynia is unknown. It’s thought that the nerves, muscles and tissues in the area are inflamed, so treatment is focused on addressing these factors. Women with vulvodynia may find it painful to insert a tampon, have sexual intercourse or even wear tight pants. Symptoms include burning, stinging, stabbing, irritation and rawness. The pain may be constant or intermittent, localized or diffuse.
Pregnancy complications might lead to pelvic pain, including:
- Ectopic pregnancy — when a fertilized egg grows outside your uterus, usually in your fallopian tubes. It causes severe pain in your ovaries and is a medical emergency. The early symptoms of an ectopic pregnancy can be very similar to typical pregnancy symptoms. Some of these include vaginal bleeding, pain in your abdomen and feeling tired or weak. Doctors usually diagnose ectopic pregnancies in the first trimester (up to 12 weeks of pregnancy) using ultrasound.
- Miscarriage — the loss of a pregnancy before 20 weeks.
- Placental abruption — when the organ that brings oxygen and nutrients to the baby called the placenta separates from the inner wall of the uterus.
- Preterm labor — when the body gets ready to give birth too early.
- Stillbirth — the loss of a pregnancy after 20 weeks.
Pelvic pain also may be caused by symptoms tied to the menstrual cycle, such as:
- Menstrual cramps also called dysmenorrhea, are throbbing or cramping pains in the lower abdomen. Many women have menstrual cramps just before and during their menstrual periods.
- Mittelschmerz is a German word for “middle pain”, which is ovulation pain that occurs midway through your menstrual cycle around the time an ovary releases an egg and about 14 days before your next menstrual period. Ovary pain during ovulation typically feels like a dull ache on just one side of your pelvis. This is because only one ovary releases an egg at a time. Other symptoms of ovulation pain may include vaginal discharge or light bleeding.
Other health conditions may cause pelvic pain. Many of these problems start in or affect your digestive system:
- Appendicitis — is inflammation of the appendix, a small tube in the lower right abdomen. It’s a medical emergency that can lead to serious complications if left untreated.
- Colon cancer — cancer that starts in the part of your large intestine called the colon.
- Constipation — which can be chronic and last for weeks or longer.
- Crohn’s disease — is a chronic inflammatory bowel disease (IBD) that affects your digestive tract. It can cause inflammation, diarrhea, weight loss, and abdominal pain.
- Diverticulitis — is an inflammation or infection of abnormal pouches in your large intestine. It can cause sudden lower abdominal pain, fever, nausea, vomiting, bloating, and changes in stool.
- Intestinal obstruction — when something blocks food or liquid from moving through the small or large intestine.
- Irritable bowel syndrome (IBS) — is a digestive condition that causes abdominal pain and changes in bowel movements. Symptoms include cramping, belly pain, bloating, gas, and diarrhea or constipation, or both. Stress and diet can aggravate the condition. IBS is an ongoing condition that needs long-term management.
- Pelvic adhesions. Adhesions are bands of scar tissue that form between internal tissues and organs binding these organs together. Adhesions can form as a result of previous pelvic or abdominal surgery or previous infections, such as appendicitis or pelvic inflammatory disease (PID) or by endometriosis 2, 4. There is disagreement about whether adhesions can cause pain. It has been proposed that pain may occur when adhesions prevent normal movement of internal organs, such as the bowel (intestine) 5. Symptoms from adhesions include generalized pelvic discomfort or localized pain. Adhesions can be difficult to diagnose, but in some cases the uterus and ovaries feel bound together on pelvic examination. A definitive diagnosis of adhesions is usually made during surgical exploration, frequently via laparoscopy. Surgery to cut bands of scar tissue can relieve pain. However, sometimes the adhesions re-form.
- Ulcerative colitis — is a chronic inflammatory bowel disease (IBD) that affects your large intestine (colon) and rectum. It can cause ulcers, inflammation, and bleeding.
Some problems in your urinary system may also cause pelvic pain:
- Interstitial cystitis also called painful bladder syndrome, is a chronic bladder condition that causes pain and discomfort in your bladder and sometimes causes pelvic pain. This pain may be a burning or sharp pain in the bladder or at the opening where urine leaves the body (urethra), and it is often relieved by emptying the bladder 6. This and other bladder symptoms, such as the need to urinate frequently or urgently, may need to be evaluated by a urologist.
- Kidney infection — which can affect one or both kidneys.
- Kidney stones also called nephrolithiasis are hard deposits of minerals and salts that form in your kidneys. Kidney stones can cause sharp pain in your side, back, lower abdomen, or groin and blood in your urine.
- Urinary tract infection (UTI) — when any part of your urinary system (the bladder, urethra, and kidneys) gets infected. Symptoms include pain or burning when urinating, frequent urination, and cloudy urine.
Pelvic pain also might be due to other health issues such as:
- Fibromyalgia — a chronic condition that causes widespread pain and tenderness throughout your body. It can also cause fatigue, sleep issues, and cognitive problems.
- Inguinal hernia also known as a groin hernia is a bulge in your groin that occurs when tissue pushes through a weak spot in the abdominal muscles.
- Musculoskeletal causes of pelvic pain are very common but are often overlooked. The muscles, joints and nerves in your pelvis can be injured just like any other part of your body. For instance, tissues can be overstretched, torn or cut in childbirth or surgery; muscles can weaken or tighten from disuse and injury; and habitual postures and movements can slowly stretch or compress structures in the pelvis, leading to pain and dysfunction. The pelvic muscles, joints and nerves may be the sole cause of pain or just a piece of the problem.
- Injury to a nerve in the pelvis that leads to ongoing pain, called pudendal neuralgia. Pudendal neuralgia occurs when the pudendal nerve is injured, irritated, or compressed. Symptoms include burning pain (often unilateral), tingling, or numbness in any of the following areas: buttocks, genitals, or perineum (area between the buttocks and genitals). Symptoms are typically present when a person is sitting but often go away when the person is standing or lying down. The pain tends to increase as the day progresses. Additional symptoms include pain during sex and needing to urinate frequently and/or urgently. Damage to the pudendal nerve can result from surgical procedures, childbirth, trauma, spasms of the pelvic floor muscles, or tumors. Pudendal Neuralgia may also result from certain infections (such as herpes simplex infections) or certain activities (such as cycling and squatting exercises). There are no imaging studies that diagnose Pudendal Neuralgia; however, MRI and CT may help to exclude other causes of the pain.
- Past physical or sexual abuse. If you have been the victim of sexual abuse, you are more likely to experience chronic pelvic pain.
- Pelvic floor muscle spasms. The muscles in your lower back and abdominal wall form the front and back borders of your pelvis, and the pelvic floor muscles around your vagina and rectum, supports the contents of your pelvis. This “sling” of muscles, along with connective tissue called fascia, lift and support the pelvic organs including the bladder, uterus and rectum. Each muscle in your body is surrounded by a strong fibrous tissue called fascia and muscles attach to bones with ligaments. These muscles, fascia, ligaments and bones share some of the same nerves as your pelvic organs. The tension, trigger points, and soft tissue restrictions can cause problems with how these muscles work which can lead to movement dysfunction, pain with movement, pain with intercourse/sex, frequent urination/peeing, problems getting urine stream started (hesitancy), constipation, bloating, and vaginal, rectal, scrotal, and low back pain. Spasms in your pelvic floor muscles — known as pelvic floor tension myalgia or levator ani syndrome — may cause pain locally. Tight bands of muscle, known as trigger points, may be tender to the touch, and they may refer pain to other areas of the pelvis, abdomen and low back. A thorough examination of your abdomen and pelvis can uncover these sources of pain, which can be treated with physical therapy and biofeedback. Some studies show physical therapy helps 60 percent of women with chronic pelvic pain and levator ani syndrome (pelvic floor tension myalgia). Physical therapy helps to align bone or muscular imbalances, decrease abnormal muscle tension and soft tissue, and strengthen your core muscles to prevent further injury. A physical therapist can also help identify other factors that may contribute to your pain, such as poor posture, positioning and habits.
- Physical factors such as your physical health conditions, inflammation and hormones.
- Psychological factors such as how pain affects your mood and sleep and how you think about your pain.
- Social factors such as your relationships, your workplace and your social connections.
Ovarian pain symptoms
Every female experiences ovarian pain differently, especially because ovarian pain can have many different causes. The area you have the pain and the type of pain you feel may not always be the same. Pelvic pain can be severe enough that it interferes with your normal activities, such as going to work, exercising, or having sex. Some women have pain in the vulva (the external genitals), which is called vulvodynia, during sex or when inserting a tampon 4, 7.
Depending on the cause of your ovarian pain or pelvic pain, you may feel:
- dull ache or aching
- sharp pain or stabbing
- burning
- cramping
- pressure or heaviness
- tingling or pins and needles.
You may feel the pain at any time, and it may be triggered at specific times such as:
- during your period
- when you sit on the toilet
- when you sit or stand for a long time
- with certain movements or activities
- during sex
- when you insert a tampon
Your pain may radiate (travel upwards) from your pelvis to your abdomen or down towards your legs.
Ovarian pain diagnosis
When diagnosing the cause of pelvic pain, your doctor will review your symptoms and medical history including your pain history, sexual history and mental health. A physical exam or other tests might also help in determining the cause of pelvic pain.
The physical exam will thoroughly assess the many possible sources of pelvic pain discussed under “causes of pelvic pain” with particular attention to the musculoskeletal system including the back, abdomen and pelvis. A Q-tip test may be performed to test the nerves outside and near the vagina.
If needed, your doctor may order other diagnostic tests such as blood work, urine tests, a pelvic ultrasound or laproscopy.
Some diagnostic tools might include:
- Blood and urine tests.
- Pregnancy tests.
- Vaginal or penile cultures to check for sexually transmitted infections like gonorrhea and chlamydia.
- Abdominal and pelvic X-rays.
- Laparoscopy (a procedure allowing a direct look at the structures in your pelvis and abdomen).
- Hysteroscopy (a procedure to examine your uterus).
- Stool sample to check for signs of blood in your poop.
- Lower endoscopy (insertion of a lighted tube to examine the inside of your rectum and colon).
- Ultrasound (a test that uses sound waves to provide images of internal organs).
- CT scan of your abdomen and pelvis (a scan that uses X-rays and computers to produce cross-sectional images of your body).
You may be referred to a urogynecologist if you have bladder symptoms, or a gastroenterologist if you have gastrointestinal symptoms. If you have a musculoskeletal component to your pelvic pain, your doctor may refer you to a physical therapist for further evaluation and treatment.
Ovarian pain treatment
The treatment of pelvic pain depends on several factors, including the underlying cause, intensity (how bad the pain is) and frequency (how often it occurs) of pain. Common pelvic pain treatments include:
- For ovarian cysts, monitoring is often the first step because many go away on their own.
- For uterine fibroids, over-the-counter medications like ibuprofen or naproxen can help with mild pain.
- Antibiotics if your doctor suspects pelvic inflammatory disease (PID) or a sexually transmitted infection (STI).
- Hormones for conditions such as endometriosis or heavy menstrual bleeding.
- Some people experience pain in the area around their ovaries just before or when they get their period. Like ovulation pain, it’s not a cause for concern. It happens because your uterus is contracting in order to shed your uterine lining. Taking over-the-counter pain relievers or using a heating pad can help.
- Treatment for ovulation pain usually involves over-the-counter (OTC) pain medication like ibuprofen. Some people find relief by taking birth control pills because they prevent ovulation from happening. Luckily, ovulation pain usually lasts just a few days and doesn’t cause any long-term complications.
- Surgery for some women with adhesions, adenomyosis or endometriosis.
- Physical therapy and biofeedback for women with myofascial (connective tissue) or muscle pain.
- Psychological therapy, medication, or both to help you cope with chronic pain. A therapist can offer support and tools to handle living with chronic pain, and can also help you and your partner cope with the relationship and sexual issues that can arise as a result of chronic pain.
- Healthy nutrition such as a diet rich in fruits, vegetables and grains is important for constipation and diverticulitis. Avoiding foods that can increase inflammation and increasing foods that decrease inflammation can be useful.
- For severe pain, seek medical advice.
Ovarian cysts
An ovarian cyst is a fluid-filled sac inside or on the surface of an ovary 8, 9, 10, 11. Most ovarian cysts occur as a normal part of the ovulation process (egg release) of your menstrual cycle, these are called functional ovarian cysts. Functional ovarian cysts usually go away within a few months without any treatment. If you develop an ovarian cyst, your doctor may want to check it again after your next menstrual cycle (period) to see if it has gotten smaller. Other types of ovarian cysts are much less common.
Ovarian cysts can occur at any age but are more common in reproductive years due to endogenous hormone production 12. An ovarian cyst can be more concerning in a female who isn’t ovulating (like a woman after menopause or a girl who hasn’t started her periods), and your doctor may want to do more tests. Your doctor may also order other tests if the ovarian cyst is large or if it does not go away in a few months. Even though most of ovarian cysts are benign (not cancer) and go away on their own without treatment, a small number of them could be cancer 11. Age is the most important independent risk factor, and post-menopausal women with any type of ovarian cyst should have proper follow-up and treatment due to a higher risk for cancer (malignancy) 13, 14. Sometimes the only way to know for sure if the ovarian cyst is cancer is to take it out with surgery. Ovarian cysts that appear to be benign (based on how they look on imaging tests) can be observed (with repeated physical exams and imaging tests), or removed with surgery.
Women have two ovaries — each about the size and shape of an almond — on each side of the uterus. Ovaries are a pair of small organs in the female reproductive system that contain and release an egg once a month in women of menstruating age. This is known as ovulation.
Many women have ovarian cysts at some time and usually form during ovulation. Ovulation happens when the ovary releases an egg each month. Many women with ovarian cysts don’t have symptoms. Most ovarian cysts present little or no discomfort and are harmless 15. The majority disappears without treatment within a few months 8.
Ovarian cysts are common in women with regular periods. In fact, most women make at least one follicle or corpus luteum cyst every month. You may not be aware that you have a cyst unless there is a problem that causes the cyst to grow or if multiple cysts form 16. Ovarian cysts — especially those that have ruptured or twisted— can cause serious symptoms 17, 18, 19. To protect your health, get regular pelvic exams and know the symptoms that can signal a potentially serious problem 19.
About 8% of premenopausal women develop large ovarian cysts that need treatment 20, 21.
Ovarian cysts are less common after menopause. Postmenopausal women with ovarian cysts are at higher risk for ovarian cancer.
At any age, see your doctor if you think you have an ovarian cyst. See your doctor also if you have symptoms such as bloating, needing to urinate more often, pelvic pressure or pain, or abnormal (unusual) vaginal bleeding. These can be signs of an ovarian cyst or other serious problem.
Most ovarian cysts occur naturally and are benign (not cancer) and go away on their own without needing any treatment 11. However, some ovarian cysts can be malignant (cancer), and large cysts greater than 5 cm can increase the risk of ovarian torsion or rupture 16, 22, 23. In these cases, surgical intervention may be indicated to avoid complications 8.
Ovarian cyst key points 24:
- Ovarian cysts are common. Most are variations of normal ovulatory function (functional ovarian cysts). Regardless of age, the likelihood of cancer is significantly less than the likelihood of a benign lesion.
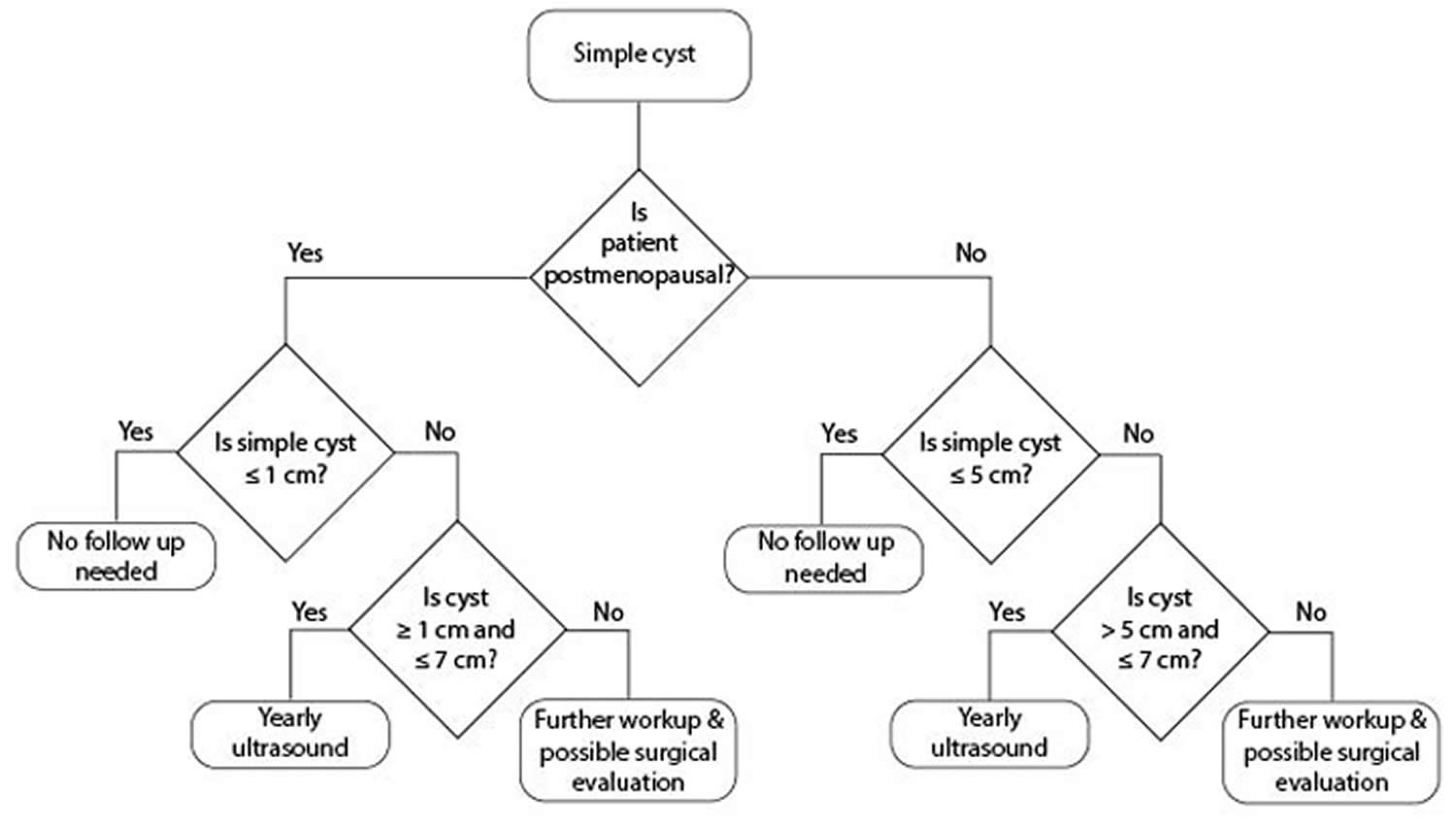
- Patients with ovarian cysts with benign characteristics (round or oval, anechoic, smooth, thin walls, no solid component, no internal flow, no or single thin septation, posterior acoustic enhancement) may be followed by your primary care doctor according to the algorithm in Figures 12 and 13 below, until resolution or stability of the ovarian cyst has been ascertained.
- Women with symptomatic ovarian cysts, those with cysts over 6 cm in diameter, or those with an uncertain, but likely benign diagnosis, can be managed by a general gynecologist.
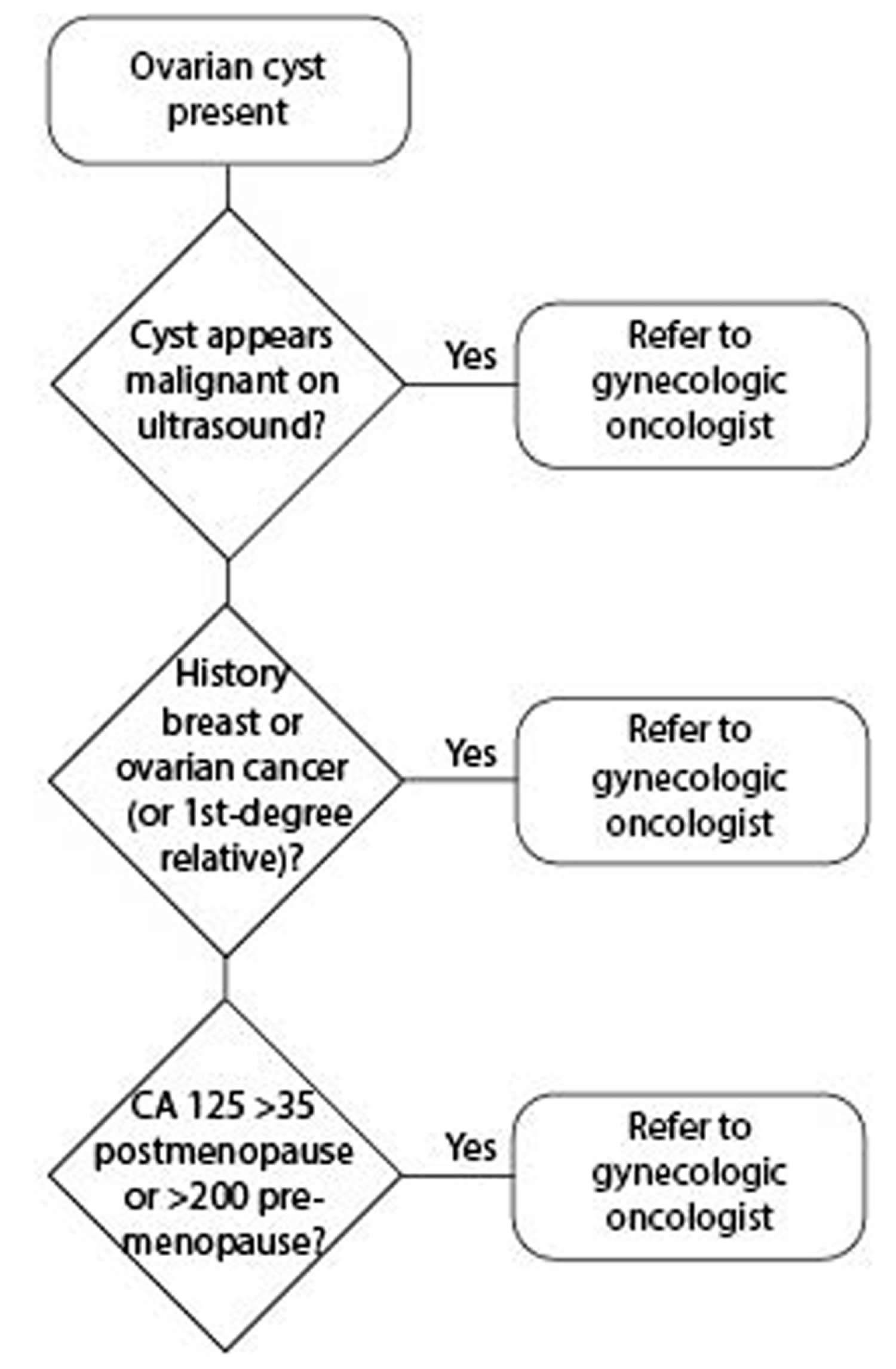
- Patients with ovarian cysts with frankly malignant characteristics (complex structure with thick >3mm septations, nodules or excrescences, especially if multiple or with internal blood flow, solid areas, or ascites) should be referred directly to a gynecologic oncologist. Referral should also be made to gynecologic oncology if the patient has an elevated CA 125 value, a personal or family history of breast or ovarian cancer in a first degree relative, or evidence of metastases.
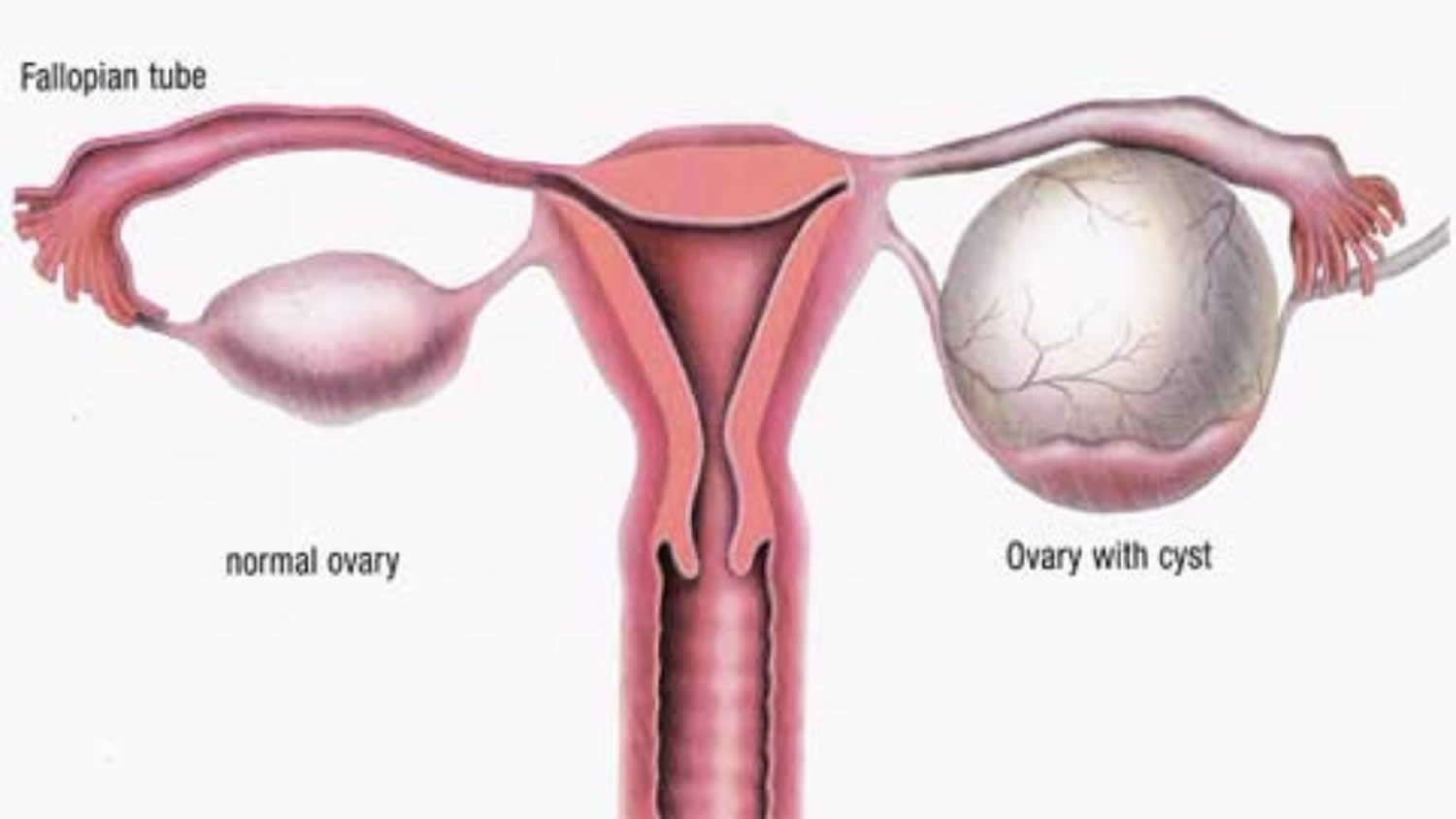
Figure 9. Ovarian cyst
Get immediate medical help if you have:
- Sudden, severe abdominal or pelvic pain.
- Pain with fever or vomiting.
- Signs of shock. These include cold, clammy skin; rapid breathing; and lightheadedness or weakness.
Are ovarian cysts ever an emergency?
Yes, sometimes 15. If your doctor told you that you have an ovarian cyst and you have any of the following symptoms, get medical help right away:
- Pain with fever and vomiting
- Sudden, severe abdominal pain
- Faintness, dizziness, or weakness
- Rapid breathing
These symptoms could mean that your cyst has broken open, or ruptured. Sometimes, large, ruptured cysts can cause heavy bleeding 15.
Can ovarian cysts lead to cancer?
Yes, some ovarian cysts can become cancerous 15. But most ovarian cysts are not cancerous 15.The risk for ovarian cancer increases as you get older. Women who are past menopause with ovarian cysts have a higher risk for ovarian cancer. Talk to your doctor about your risk for ovarian cancer. Screening for ovarian cancer is not recommended for most women 25. This is because testing can lead to “false positives.” A false positive is a test result that says a woman has ovarian cancer when she does not.
Ovarian cancer risk factors
Generally, it’s not possible to say what causes ovarian cancer in an individual woman. However, some features are more common among women who have developed ovarian cancer. These features are called risk factors. Having certain risk factors increases a woman’s chance of developing ovarian cancer.
Having one or more risk factors for ovarian cancer doesn’t mean a woman will definitely develop ovarian cancer. In fact, many women with ovarian cancer have no obvious risk factors.
Factors that increase your risk of ovarian cancers:
- Getting older. The risk of developing ovarian cancer gets higher with age. Ovarian cancer is rare in women younger than 40. Most ovarian cancers develop after menopause. Half of all ovarian cancers are found in women 63 years of age or older.
- Being overweight or obese. Obesity has been linked to a higher risk of developing many cancers. The current information available for ovarian cancer risk and obesity is not clear. Obese women (those with a body mass index [BMI] of at least 30) may have a higher risk of developing ovarian cancer, but not necessarily the most aggressive types, such as high grade serous cancers. Obesity may also affect the overall survival of a woman with ovarian cancer.
- Having children later or never having a full-term pregnancy. Women who have their first full-term pregnancy after age 35 or who never carried a pregnancy to term have a higher risk of ovarian cancer.
- Using fertility treatment. Fertility treatment with in vitro fertilization (IVF) seems to increase the risk of the type of ovarian tumors known as “borderline” or “low malignant potential” (LMP tumors). Other studies, however, have not shown an increased risk of invasive ovarian cancer with fertility drugs. If you are taking fertility drugs, you should discuss the potential risks with your doctor.
- Taking hormone therapy after menopause. Women using estrogens after menopause have an increased risk of developing ovarian cancer. The risk seems to be higher in women taking estrogen alone (without progesterone) for many years (at least 5 or 10). The increased risk is less certain for women taking both estrogen and progesterone.
- Having a family history of ovarian cancer, breast cancer, or colorectal cancer. Ovarian cancer can run in families. Your ovarian cancer risk is increased if your mother, sister, or daughter has (or has had) ovarian cancer. The risk also gets higher the more relatives you have with ovarian cancer. Increased risk for ovarian cancer can also come from your father’s side. A family history of some other types of cancer such as colorectal and breast cancer is linked to an increased risk of ovarian cancer. This is because these cancers can be caused by an inherited mutation (change) in certain genes that cause a family cancer syndrome that increases the risk of ovarian cancer.
- Having a family cancer syndrome. Up to 25% of ovarian cancers are a part of family cancer syndromes resulting from inherited changes (mutations) in certain genes.
- Hereditary breast and ovarian cancer syndrome. The hereditary breast and ovarian cancer syndrome is caused by inherited mutations in the genes BRCA1 and BRCA2, as well as possibly some other genes that have not yet been found. The hereditary breast and ovarian cancer syndrome is linked to a high risk of breast cancer as well as ovarian, fallopian tube, and primary peritoneal cancers. The risk of some other cancers, such as pancreatic cancer and prostate cancer, are also increased. Mutations in BRCA1 and BRCA2 are also responsible for most inherited ovarian cancers. Mutations in BRCA1 and BRCA2 are about 10 times more common in those who are Ashkenazi Jewish than those in the general U.S. population. The lifetime ovarian cancer risk for women with a BRCA1 mutation is estimated to be between 35% and 70%. This means that if 100 women had a BRCA1 mutation, between 35 and 70 of them would get ovarian cancer. For women with BRCA2 mutations the risk has been estimated to be between 10% and 30% by age 70. These mutations also increase the risks for primary peritoneal carcinoma and fallopian tube carcinoma. In comparison, the ovarian cancer lifetime risk for the women in the general population is less than 2%.
- PTEN tumor hamartoma syndrome. In this syndrome, also known as Cowden disease, people are primarily affected with thyroid problems, thyroid cancer, and breast cancer. Women also have an increased risk of endometrial and ovarian cancer. It is caused by inherited mutations in the PTEN gene.
- Lynch syndrome, also known as hereditary non-polyposis colorectal cancer (HNPCC). Women with this syndrome have a very high risk of colon cancer and also have an increased risk of developing cancer of the uterus (endometrial cancer) and ovarian cancer. Many different genes can cause hereditary non-polyposis colorectal cancer (HNPCC). They include MLH1, MLH3, MSH2, MSH6, TGFBR2, PMS1, and PMS2. The lifetime risk of ovarian cancer in women with hereditary nonpolyposis colon cancer (Lynch syndrome) is about 10%. Up to 1% of all ovarian epithelial cancers occur in women with hereditary nonpolyposis colon cancer (Lynch syndrome).
- Peutz-Jeghers syndrome. People with this rare genetic syndrome develop polyps in the stomach and intestine while they are teenagers. They also have a high risk of cancer, particularly cancers of the digestive tract (esophagus, stomach, small intestine, colon). Women with this syndrome have an increased risk of ovarian cancer, including both epithelial ovarian cancer and a type of stromal tumor called sex cord tumor with annular tubules (SCTAT). This syndrome is caused by mutations in the gene STK11.
- MUTYH-associated polyposis. People with this syndrome develop polyps in the colon and small intestine and have a high risk of colon cancer. They are also more likely to develop other cancers, including cancers of the ovary and bladder. This syndrome is caused by mutations in the gene MUTYH.
- Having had breast cancer. If you have had breast cancer, you might also have an increased risk of developing ovarian cancer. There are several reasons for this. Some of the reproductive risk factors for ovarian cancer may also affect breast cancer risk. The risk of ovarian cancer after breast cancer is highest in those women with a family history of breast cancer. A strong family history of breast cancer may be caused by an inherited mutation in the BRCA1 or BRCA2 genes and hereditary breast and ovarian cancer syndrome, which is linked to an increased risk of ovarian cancer.
- Smoking and alcohol use. Smoking doesn’t increase the risk of ovarian cancer overall, but it is linked to an increased risk for the mucinous type. Drinking alcohol is not linked to ovarian cancer risk.
Can ovarian cysts make it harder to get pregnant?
Typically, no 15. Most ovarian cysts do not affect your chances of getting pregnant 15. Sometimes, though, the illness causing the ovarian cyst can make it harder to get pregnant.
Two conditions that cause ovarian cysts and affect fertility are 15:
- Endometriosis, which happens when the lining of the uterus (womb) grows outside of the uterus. Cysts caused by endometriosis are called endometriomas.
- Polycystic ovary syndrome (PCOS), one of the leading causes of infertility (problems getting pregnant). Women with PCOS often have many small cysts on their ovaries.
If you need an operation to remove your cysts, your surgeon will aim to preserve your fertility whenever possible.
This may mean removing just the cyst and leaving the ovaries intact, or only removing 1 ovary.
In some cases, surgery to remove both your ovaries may be necessary, in which case you’ll no longer produce any eggs.
Make sure you talk to your surgeon about the potential effects on your fertility before your operation.
How do ovarian cysts affect pregnancy?
Ovarian cysts are common during pregnancy 15. Typically, these cysts are benign (not cancerous) and harmless 26. Ovarian cysts that continue to grow during pregnancy can rupture or twist or cause problems during childbirth. Your doctor will monitor any ovarian cyst found during pregnancy.
Can you prevent ovarian cysts?
No, you cannot prevent functional ovarian cysts if you are ovulating 15. If you get ovarian cysts often, your doctor may prescribe hormonal birth control to stop you from ovulating. This will help lower your risk of getting new cysts.
Ovarian cyst complications
Some women develop less common types of ovarian cysts that a doctor finds during a pelvic exam. Cystic ovarian masses that develop after menopause might be cancerous (malignant). That’s why it’s important to have regular pelvic exams.
Infrequent complications associated with ovarian cysts include:
- Ovarian torsion. Cysts that enlarge can cause the ovary to move, increasing the chance of painful twisting of your ovary (ovarian torsion). Symptoms can include an abrupt onset of severe pelvic pain, nausea and vomiting. Ovarian torsion can also decrease or stop blood flow to the ovaries.
- Ovarian cyst rupture. All ovarian cyst types can potentially rupture, spilling fluid into the pelvis, which is often painful. An ovarian cyst that ruptures can cause severe pain and internal bleeding. If the contents are from a dermoid or abscess, surgical lavage may be indicated. The larger the cyst, the greater the risk of rupture. Vigorous activity that affects the pelvis, such as vaginal intercourse, also increases the risk.
- Bleeding into the ovarian cyst. In the case of hemorrhagic ovarian cysts, the management of hemorrhage depends on the hemodynamic stability of the patient, but is most often expectantly managed.
The fifth most common gynecological emergency is ovarian torsion, defined as the complete or partial twisting of the ovarian vessels resulting in obstruction of blood flow to the ovary. The diagnosis is made clinically with the assistance of a history and physical examination, bloodwork, and imaging and is confirmed by diagnostic laparoscopy. The latest evidence supports a conservative approach during diagnostic laparoscopy, and detorsion of the ovary with or without cystectomy is recommended to preserve fertility.
Ovarian cysts can also rupture or hemorrhage, with most of these being physiological. Most cases are uncomplicated with mild to moderate symptoms, and those with stable vital signs can be managed expectantly. Occasionally, this can be complicated by significant blood loss resulting in hemodynamic instability requiring admission to the hospital, surgical evacuation, and blood transfusion 16.
Ruptured ovarian cyst
Ruptured ovarian cysts and hemorrhagic ovarian cysts are the most common causes of acute pelvic pain in an afebrile, premenopausal woman presenting to the emergency room 27. Rebound tenderness from the pain is possible and the bleeding from a cyst can rarely be severe enough to cause shock 28. It is a common cause of physiological pelvic intraperitoneal fluid.
Ovarian cysts may rupture during pregnancy (if a very early pregnancy, this may cause diagnostic confusion with ectopic pregnancy).
Although rupture of an ovarian follicle is a physiologic event (mittelschmerz (German for ‘middle pain’)), the rupture of an ovarian cyst (>3 cm) may cause more dramatic clinical symptoms.
The sonographic appearance depends on whether a simple or hemorrhagic ovarian cyst ruptures, and whether the cyst has completely collapsed. The most important differential consideration is a ruptured ectopic pregnancy 29.
Ruptured ovarian cyst symptoms
Ruptured ovarian cysts and hemorrhagic ovarian cysts are the most common causes of acute pelvic pain in an afebrile, premenopausal woman presenting to the emergency room 27. The pain from a ruptured ovarian cyst may come from stretching the capsule of the ovary, torquing of the ovarian pedicle, or leakage of cyst contents (serous fluid/blood) which can cause peritoneal irritation 28.
Ruptured ovarian cyst treatment
Ruptured ovarian cyst is treated conservatively in a premenopausal woman unless evidence of hypovolemic shock (tachycardia and postural drop in blood pressure) 29.
A ruptured hemorrhagic cyst in a perimenopausal woman should be viewed more suspiciously and followed up appropriately 29. A hemorrhagic cyst or ruptured cyst in a postmenopausal woman deserves surgical evaluation 29.
Ovarian torsion
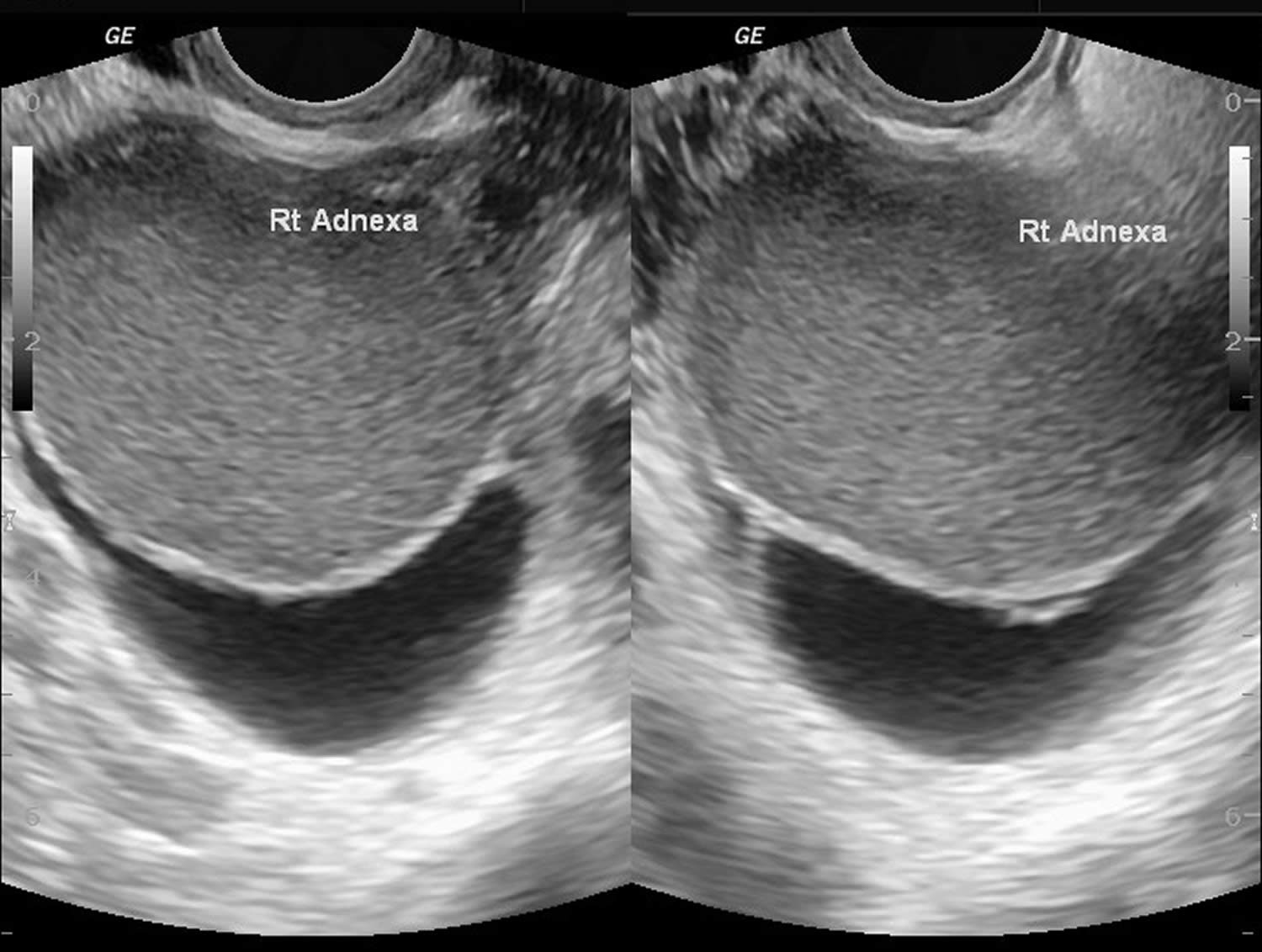
Ovarian torsion is caused by twisting of the ligaments that support the ovary, cutting off the blood flow to the ovary and represents a true surgical emergency that can lead to necrosis, loss of ovary, and infertility if not identified early 30, 31. Ovarian torsion is characterized by a twisted ovary with or without the involvement of the fallopian tube 32. When fallopian tube also twists with the ovary it is known as adnexal torsion 33. The diagnosis of ovarian torsion can only be confirmed by surgery 32. Furthermore, the female reproductive function may be negatively affected by delayed treatment because of uncertainty in the preoperative diagnosis.
The ovary has dual blood supply from the ovarian arteries and uterine arteries. The ovary is supported by multiple structures in the pelvis. One ligament it is suspended by is the infundibulopelvic ligament, also called the suspensory ligament of the ovary, which connects the ovary to the pelvic sidewall. This ligament also contains the main ovarian vessels. The ovary is also connected to the uterus by the utero-ovarian ligament 34. Twisting of these ligaments can lead to venous congestion, edema, compression of arteries, and, eventually, loss of blood supply to the ovary. This can cause a constellation of symptoms, including severe pain when blood supply is compromised.
The main risk factor for ovarian torsion is an ovarian mass that is 5 cm in diameter or larger 30. The mass increases the chance that the ovary could rotate on the axis of the two ligaments holding it in suspension. This torsion impedes venous outflow and eventually, arterial inflow.
In a study of torsions confirmed by surgery, 46% were associated with tumors, and 48% were associated with cysts. Of these masses, 89% were benign, and 80% of patients were under age 50. Therefore, reproductive-age females are at greatest risk of torsion 35. However, torsion can still occur in normal ovaries, especially in children and adolescents. Pregnancy, as well as patients undergoing fertility treatments, are high risk due to enlarged follicles on the ovary 34.
The clinical symptoms of ovarian torsion are variable and nonspecific 32. Classic clinical symptoms of ovarian torsion include the sudden onset of severe pelvic pain and a palpable adnexal mass (a lump in tissue near the uterus, usually in the ovary or fallopian tube) 36. Moreover, nausea, vomiting, and fever are present in some cases 37. Reproductive age is the peak period of incidence of ovarian torsion, and approximately 70% of cases occur during this period 38. It is estimated that 12% to 18% of patients with ovarian torsion are pregnant 39, 40, 41. However, whether pregnancy is a risk factor of ovarian torsion is still controversial 42, 43.
Physical exam in the patient is variable. The patient may have abdominal tenderness focally in the lower abdomen, pelvic area, diffusely, or not at all. Up to one-third of patients were found to have no abdominal tenderness. There could also be an abdominal mass. If the patient has guarding, rigidity, or rebound, there may already be necrosis of the ovary. Every patient should also have a pelvic exam to better evaluate for masses, discharge, and cervical motion tenderness.
Pelvic ultrasonic examination is the most frequently performed preoperative examination, but ultrasonic findings are nonspecific, despite the ultrasonic features of ovarian torsion being well-characterized 31, 44, 45.
Ovarian torsion is the fifth most common gynecological emergency requiring surgery, with an estimated prevalence of about 2.7% to 3% 46. Urgent surgery is required to prevent ovarian necrosis. Most ovaries are not salvageable, in which case a salpingo-oophorectomy is required. If not removed, the necrotic ovary can become infected and cause an abscess or peritonitis. In the case of a non-infarcted adnexa, surgical untwisting can be performed. Mortality resulting from ovarian torsion is rare. Spontaneous detorsion has also been reported.
Ovarian torsion symptoms
The clinical symptoms of ovarian torsion are variable and nonspecific 32. Most patients will present with lower abdominal pain or pelvic pain. Pain can be sharp, dull, constant, or intermittent. Pain may radiate to the abdomen, back, or flank 47. One study showed that post-menopausal women commonly presented with dull, constant pain when compared to premenopausal, who more commonly had sharp stabbing pain. Symptoms may or may not be intermittent if the ovary is torsing and detorsing.
The patient may also have associated nausea and vomiting. In one study of children and adolescents with lower abdominal pain, vomiting was found to be an independent risk factor for ovarian torsion 48. The patient may or may not already have a known ovarian mass, which predisposes them to torsion.
Fever may be present if the ovary is already necrotic. The patient could also have abnormal vaginal bleeding, or discharge if torsion involves a tubo-ovarian abscess. Infants with ovarian torsion may present with feeding intolerance or inconsolability.
Ovarian torsion treatment
Ovarian torsion requires urgent surgery to prevent ovarian necrosis 30. The treatment of ovarian torsion is surgical detorsion, preferably by a gynecologist 30.
In reproductive age females, salvage of the ovary should be attempted, and the surgeon must evaluate the ovary for viability 30. Most often, the approach to surgery should be laparoscopic and involves direct visualization of a twisted ovary. The evaluation of viability is mostly by visualization. A dark, enlarged ovary with hemorrhagic lesions may have compromised blood flow but is often salvageable 40.
After detorsion, ovaries were found to be functional in greater than 90% of patients who underwent detorsion 30. This was assessed by the appearance of the adnexa on ultrasound, including follicular development on the ovaries 49. Therefore, surgery with sparing of the ovary is the management of choice 30. Rarely, if the ovary appears necrotic and gelatinous beyond possible salvage, the surgeon may choose to perform a salpingo-oophorectomy 30. The surgeon may also perform cystectomy if a benign ovarian cyst is present. If the ovarian cyst appears to be malignant, or if the woman is post-menopausal, salpingo-oophorectomy is the preferred management 30.
Ovarian torsion prognosis
Ovarian torsion is not usually life-threatening, but it is organ threatening. In premenopausal women, surgery with sparing of the ovary is now the preferred treatment, and the majority of women had normal-appearing ovary on ultrasound after surgery 50. Ovarian salvage is increased in patients with less time from the onset of symptoms to surgical intervention. In postmenopausal women, salpingo-oophorectomy is done to prevent reoccurrence. This approach is also used in women with a mass suspicious for malignancy. The majority of ovarian masses are benign. Some case reports show less than 2% of torsions involving a malignant lesion. However, the chances of a malignant lesion involved in ovarian torsion are increased in the postmenopausal women 34.
The main complication of ovarian torsion is the inability to salvage the ovary and the need for salpingo-oophorectomy. This may affect fertility in a woman of childbearing age. Other complications of ovarian torsion include abnormal pelvic anatomy that may contribute to infertility, such as adhesions, or atrophied ovaries 51. There may be complications from the surgery itself, such as infection or venous thromboembolism. The risk of post-operative infection is increased when necrotic tissue is already present 52.
Ovarian cyst types
The most common types of ovarian cysts are called functional cysts, they form during the menstrual cycle and they happen if you have not been through the menopause (see Figure 4. Normal ovary) 53, 15. Functional ovarian cysts are usually benign (not cancerous) 15. Functional ovarian cysts are usually harmless, rarely cause pain, and often disappear on their own within two or three menstrual cycles.
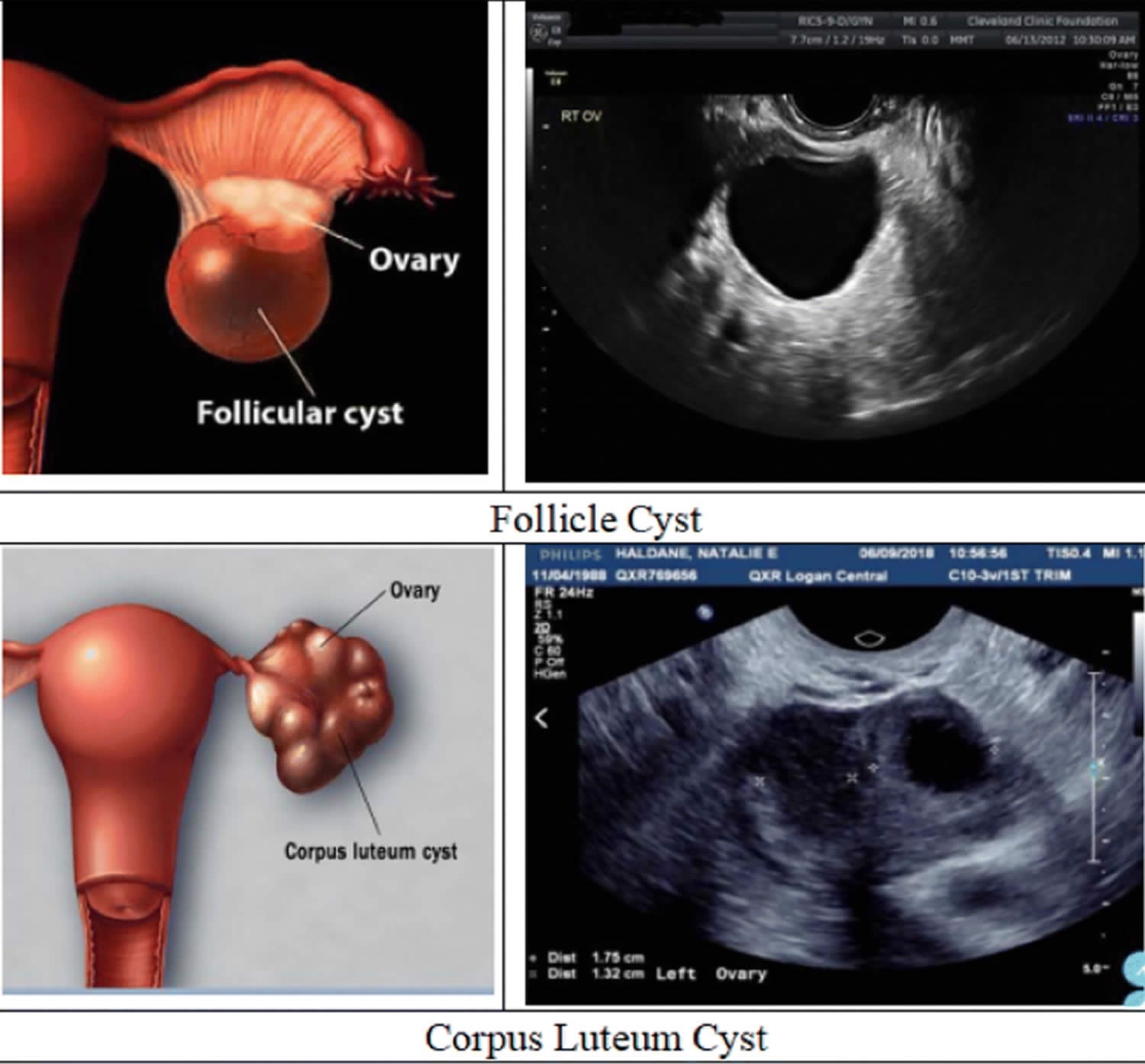
The two most common types of functional cysts are 15:
- Follicle cysts. In a normal menstrual cycle, an ovary releases an egg each month. The egg grows inside a tiny sac called a follicle. When the egg matures, the follicle breaks open to release the egg. Around the midpoint of your menstrual cycle, an egg bursts out of its follicle and travels down the fallopian tube. Follicle cysts form when the follicle doesn’t break open to release the egg. This causes the follicle to continue growing into a cyst. Follicular cysts can appear smooth, thin-walled, and unilocular. Follicle cysts may form because of a lack of physiological release of the egg due to excessive follicle-stimulating hormone (FSH) stimulation or the absence of the usual luteinizing hormone (LH) surge at mid-cycle just before ovulation. These cysts continue to grow because of hormonal stimulation. Follicular cysts are usually larger than 2.5 cm in diameter. Follicle cysts often have no symptoms and go away in one to three months.
- Corpus luteum cysts. Once the follicle breaks open and releases the egg, the empty follicle sac shrinks into a mass of cells called corpus luteum. Corpus luteum makes hormones estrogen and progesterone to prepare for the next egg for the next menstrual cycle. Without pregnancy, the life span of the corpus luteum is 14 days. Corpus luteum cysts form if the sac doesn’t shrink. Instead, the sac reseals itself after the egg is released, and then fluid builds up inside. Most corpus luteum cysts go away after a few weeks. But, they can grow to almost four inches wide. They also may bleed or twist the ovary and cause pain. Some medicines used to cause ovulation can raise the risk of getting these cysts. Corpus luteal cysts can appear complex or simple, thick-walled, or contain internal debris. Corpus luteum cysts are always present during pregnancy and usually resolve by the end of the first trimester.
Both follicular and corpus luteal cysts can turn into hemorrhagic cysts. They are generally asymptomatic and spontaneously resolve without treatment 54.
Other types of benign ovarian cysts are less common:
- Theca lutein cysts. Theca lutein cysts are luteinized follicle cysts that form as a result of overstimulation in elevated human chorionic gonadotropin (hCG) levels. Theca lutein cysts can occur in pregnant women, women with gestational trophoblastic disease, multiple gestation, and ovarian hyperstimulation.
- Endometriomas are caused by endometriosis. Endometriosis happens when the lining of the uterus (womb) grows outside of the uterus. Some of the lining of the uterus tissue can attach to your ovary and form a growth. Endometriomas (common in endometriosis) arise from ectopic growth of endometrial tissue and are often referred to as chocolate cysts because they contain dark, thick, gelatinous aged blood products. They appear as a complex mass on ultrasound and are described as having “ground glass” internal echoes. Endometriomas can be classified into two types. Type 1 endometrioma consists of small primary endometriomas that develop from surface endometrial implants. Type 2 endometrioma arises from functional cysts that have been invaded by ovarian endometriosis or type 1 endometriomas. Although the overall risk of malignant transformation is low, endometriomas increase this risk in women with endometriosis 55, 56, 57.
- Dermoids also called teratomas come from cells present from birth and do not usually cause symptoms. Dermoid cysts (teratomas) can contains different kinds of tissues that make up the body, such as hair, skin or teeth, because they form from embryonic cells. Although mostly benign, dermoid cysts (teratomas) can undergo a malignant transformation in 1 to 2% of cases 58, 59, 60.
- Cystadenomas develop on the surface of an ovary and might be filled with a watery or a mucous material. These tumors can grow very large even though they usually are benign.
- Polycystic ovary syndrome (PCOS). Polycystic ovary syndrome (PCOS) is a disorder affecting 5 to 10% of women of reproductive age and is one of the primary causes of infertility. It is associated with diabetes mellitus and cardiovascular disease. Polycystic ovary syndrome (PCOS) appears as enlarged ovaries with multiple small follicular cysts. The ovaries appear enlarged due to excess androgen hormones in the body, which cause the ovaries to form cysts and increase in size 61.
- Pregnancy ovarian cyst. Ovarian cysts in pregnancy are usually benign. Benign cystic teratomas (dermoid cysts) are the most common ovarian tumor during pregnancy, accounting for one-third of all benign ovarian tumors in pregnancy. The second most common benign ovarian cyst is a cystadenoma. In caring for pregnant women with ovarian cysts, a multidisciplinary approach and referral to a perinatologist and gynecologic oncologist is advised.
- Neonates and prepubertal children ovarian cyst. Ovarian cysts in the neonate are exceedingly rare. It is estimated that 5% of all abdominal masses in the first month of life are ovarian cysts. While there are no precise guidelines for the monitoring and management of neonatal ovarian cysts, it is generally agreed that cysts >2 cm are considered pathologic. The majority of neonatal ovarian cysts are benign and self-limiting. Ovarian malignancy becomes more common in the second decade of life than in the neonatal period. In one small study, approximately 33% of adnexal masses were malignant in children >8 years whereas 2.9% of adnexal masses were malignant in children <8 years 62.
Dermoid cysts and cystadenomas can become large, causing the ovary to move out of position. This increases the chance of painful twisting of your ovary, called ovarian torsion. Ovarian torsion may also result in decreasing or stopping blood flow to the ovary.
In some women, the ovaries make many small cysts. This is called polycystic ovary syndrome (PCOS). PCOS can cause problems with the ovaries and with getting pregnant.
Malignant (cancerous) ovarian cysts are rare 15. They are more common in older women. Cancerous cysts are ovarian cancer. For this reason, ovarian cysts should be checked by your doctor. Most ovarian cysts are not cancerous.
Ovarian cyst causes
The most common causes of ovarian cysts include 15:
- Hormonal problems. Functional cysts usually go away on their own without treatment. They may be caused by hormonal problems or by drugs used to help you ovulate.
- Endometriosis. Women with endometriosis can develop a type of ovarian cyst called an endometrioma. The endometriosis tissue may attach to the ovary and form a growth. These cysts can be painful during sex and during your period.
- Pregnancy. An ovarian cyst normally develops in early pregnancy to help support the pregnancy until the placenta forms. Sometimes, the cyst stays on the ovary until later in the pregnancy and may need to be removed.
- Severe pelvic infections. Infections can spread to the ovaries and fallopian tubes and cause cysts to form.
- A previous ovarian cyst. If you’ve had one, you’re likely to develop more.
Risk factors of developing ovarian cyst
Risk factors for ovarian cyst formation include:
- Infertility treatment. Patients treated with gonadotropins or other ovulation induction agents, for example clomiphene or letrozole (Femara), may develop ovarian cysts as part of ovarian hyperstimulation syndrome 63
- Pregnancy. Sometimes, the follicle that forms when you ovulate stays on your ovary throughout pregnancy. In pregnancy, ovarian cysts may form in the second trimester when hCG levels peak 64. It can sometimes grow larger.
- Endometriosis. Some of the tissue can attach to your ovary and form a cyst.
- Severe pelvic infection. If the infection spreads to the ovaries, it can cause cysts.
- Previous ovarian cysts. If you’ve had one ovarian cyst, you’re likely to develop more.
- Tamoxifen therapy 12. Tamoxifen is widely used as hormonal therapy in both, pre- and postmenopausal women with breast cancer and effectively reduces the risk of recurrence and mortality 65, 66.
- Underactive thyroid (hypothyroidism) 67
- Maternal gonadotropins. The transplacental effects of maternal gonadotropins may lead to the development of fetal ovarian cysts 68.
- Cigarette smoking 69.
- Tubal ligation. Functional ovarian cysts have been associated with tubal ligation sterilizations 70.
Ovarian cyst prevention
Oral contraceptives may prevent new functional cysts from forming 71, 72. However, oral contraceptives do not hasten the resolution of preexisting ovarian cysts. Some doctors will, nevertheless, prescribe oral contraceptives in an attempt to prevent new cysts from confusing the picture. Oral contraceptives are also protective against ovarian cancer 73.
In addition, getting regular pelvic exams ensure that changes in your ovaries are diagnosed as early as possible. Be alert to changes in your monthly cycle. Make a note of unusual menstrual symptoms, especially ones that go on for more than a few cycles. Talk to your doctor about changes that concern you.
Bilateral oophorectomy (surgical removal of both ovaries) protects against ovarian and breast cancer but is associated with an increase in the all-cause mortality rate 74. Current research suggests that removal of the fallopian tubes is protective against ovarian cancer 75.
Early-stage ovarian cancer rarely causes any symptoms or the symptoms can be very vague. Advanced-stage ovarian cancer may cause few and nonspecific symptoms that are often mistaken for more common benign conditions.
Signs and symptoms of ovarian cancer may include roughly 12 or more times a month of having:
- Abdominal bloating or swelling
- Pain or tenderness in your abdomen or the area between the hips (pelvis)
- No appetite or feeling full quickly after eating
- An urgent need to urinate or needing to urinate more often
These symptoms are also commonly caused by benign (non-cancerous) diseases and by cancers of other organs. When they are caused by ovarian cancer, they tend to be persistent and a change from normal − for example, they occur more often or are more severe. These symptoms are more likely to be caused by other conditions, and most of them occur just about as often in women who don’t have ovarian cancer. But if you have these symptoms more than 12 times a month, see your doctor so the problem can be found and treated if necessary.
The National Institute for Health and Care Excellence recommends that if you (especially if 50 or over) have the following symptoms on a persistent or frequent basis – particularly more than 12 times per month, your doctor should arrange tests – especially if you’re are over 50 76:
- persistent swollen tummy (abdomen) or bloating
- feeling full (early satiety) and/or loss of appetite
- pelvic or abdominal pain
- increased urinary urgency and/or frequency.
First tests:
- Measure serum cancer antigen 125 (CA125) in primary care in women with symptoms that suggest ovarian cancer
- If serum CA125 is 35 IU/ml or greater, arrange an ultrasound scan of the abdomen and pelvis.
- For any woman who has normal serum CA125 (less than 35 IU/ml), or CA125 of 35 IU/ml or greater but a normal ultrasound:
- assess her carefully for other clinical causes of her symptoms and investigate if appropriate
- if no other clinical cause is apparent, advise her to return to her doctor if her symptoms become more frequent and/or persistent.
Ovarian cyst symptoms
Most ovarian cysts are small and don’t cause symptoms. Many ovarian cysts are found during a routine pelvic exam or imaging test done for another reason. Some ovarian cysts may cause a dull or sharp ache in the abdomen and pain during certain activities. Larger ovarian cysts may cause twisting of the ovary. This twisting may cause pain on one side that comes and goes or can start suddenly. Cysts that bleed or burst also may cause sudden, severe pain.
If an ovarian cyst does cause symptoms, you may have pressure, bloating, swelling, or pain in the lower abdomen on the side of the cyst 15. This pain may be sharp or dull and may come and go 15.
If an ovarian cyst ruptures, it can cause sudden, severe pain 15.
If an ovarian cyst causes twisting of an ovary, you may have pain along with nausea and vomiting 15.
Less common symptoms include:
- Pelvic pain that may come and go. You may feel a dull ache or a sharp pain in the area below your bellybutton toward one side.
- Dull ache in the lower back and thighs
- Fullness, pressure or heaviness in your belly (abdomen)
- Feeling very full after only eating a little
- Bloating and a swollen tummy
- Problems emptying your bladder or bowel completely
- Pain during sex
- Unexplained weight gain
- Pain during your period
- Unusual (not normal) vaginal bleeding
- Heavy periods, irregular periods or lighter periods than normal
- Breast tenderness
- Needing to urinate more often
- Difficulty getting pregnant – although fertility is usually unaffected by ovarian cysts.
Ovarian cyst diagnosis
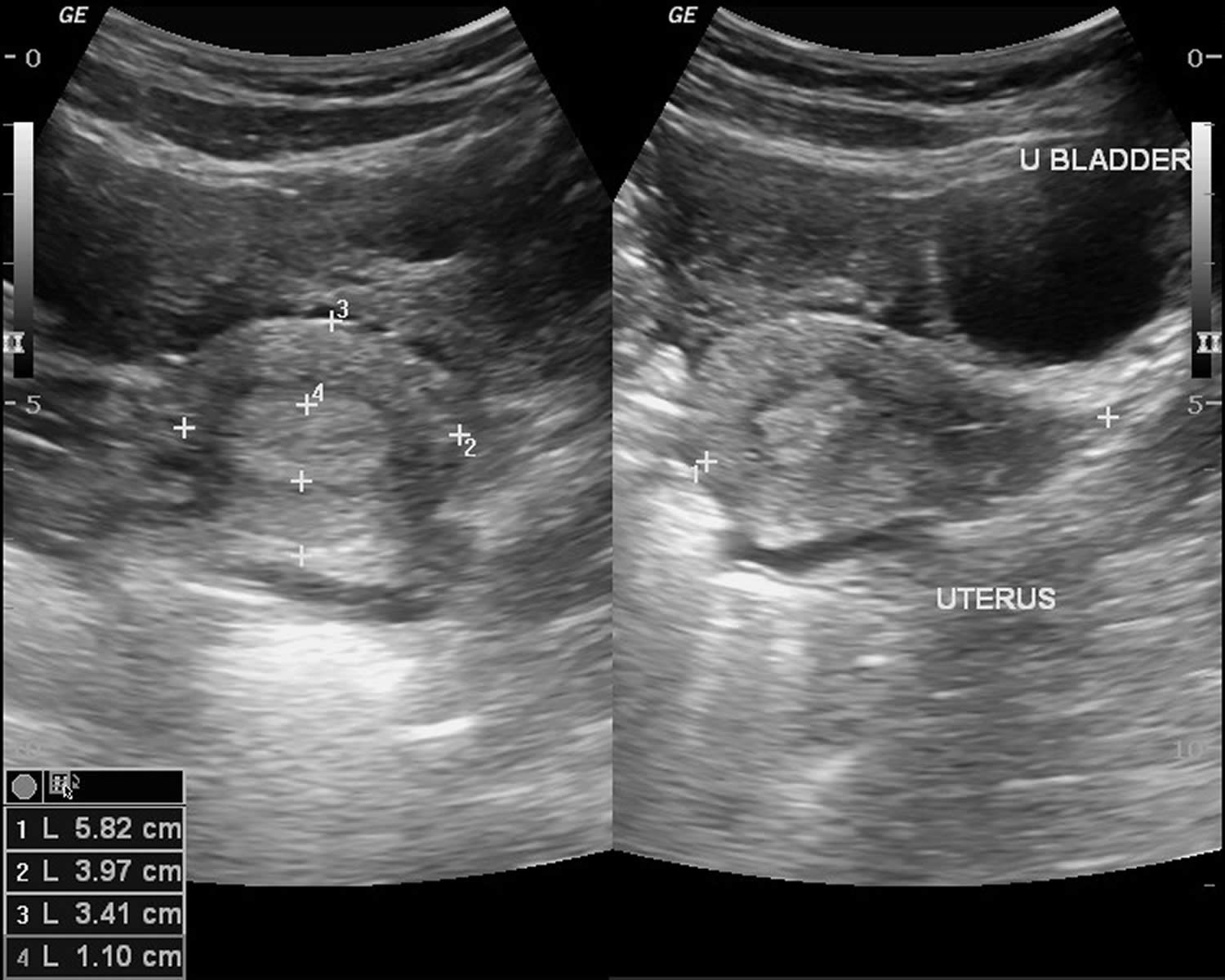
If you have symptoms of ovarian cysts, talk to your doctor. Your doctor may do a pelvic exam to feel for swelling of a cyst on your ovary.
A cyst on your ovary can also be found during a routine pelvic exam. Depending on its size and whether it’s fluid filled, solid or mixed, your doctor likely will recommend tests to determine its type and whether you need treatment.
Tests include:
- Pelvic ultrasound. This test uses sound waves to create images of the body. With ultrasound, your doctor can see the cyst’s: Shape / Size / Location / Mass (whether it is fluid-filled, solid, or mixed). If a cyst is identified during the ultrasound scan, you may need to have this monitored with a repeat ultrasound scan in a few weeks, or your doctor may refer you to a doctor who specializes in female reproductive health (obstetrician–gynecologist).
- Pregnancy test to rule out pregnancy. A positive test might suggest that you have a corpus luteum cyst.
- Hormone level tests to see if there are hormone-related problems
- Tumor marker tests. If you are past menopause, your doctor may give you a test to measure the amount of cancer-antigen 125 (CA-125) in your blood. The amount of CA-125 is higher with ovarian cancer. If your ovarian cyst is partially solid and you’re at high risk of ovarian cancer, your doctor might order this test. In premenopausal women, many other illnesses or diseases besides cancer can cause higher levels of CA-125. Elevated CA 125 levels can also occur in noncancerous conditions, such as endometriosis, uterine fibroids and pelvic inflammatory disease (PID).
- Laparoscopy. Using a laparoscope — a slim, lighted instrument inserted into your abdomen through a small incision — your doctor can see your ovaries and remove the ovarian cyst. This is a surgical procedure that requires anesthesia.
Sometimes, less common types of cysts develop that a health care provider finds during a pelvic exam. Solid ovarian cysts that develop after menopause might be cancerous (malignant). That’s why it’s important to have regular pelvic exams.
It is almost never appropriate to aspirate an ovarian cyst for diagnostic purposes. False negative results are common and leakage of cyst contents into the peritoneal cavity potentially increases the stage of any cancer found, decreasing patient survival.
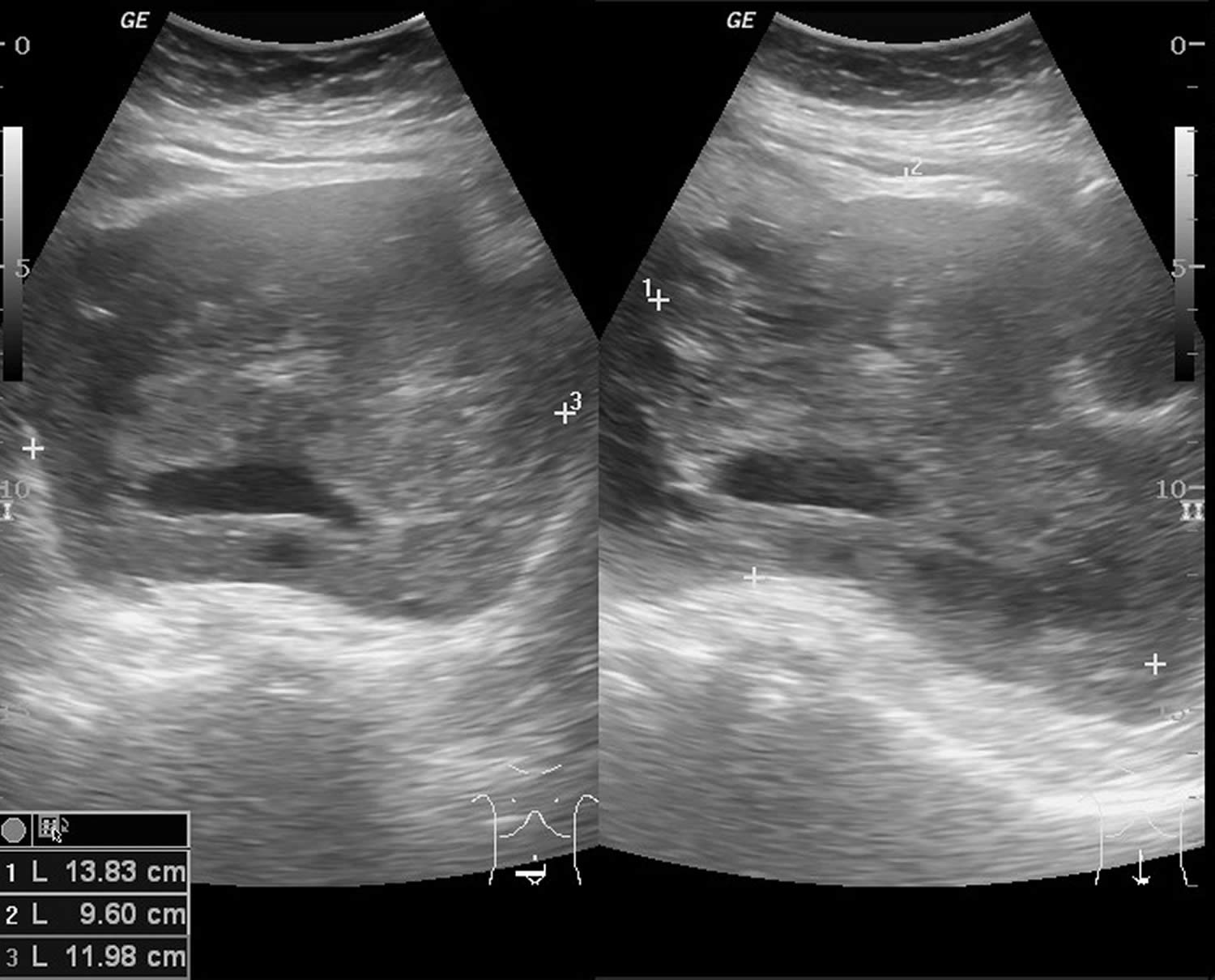
Ovarian cyst ultrasound
Ultrasound is considered the gold standard for the assessment of ovarian cysts. Transvaginal ultrasound is preferred, as the probe proximity to the ovary can result in superior images. If transvaginal ultrasound is not available or not tolerated by the patient, transabdominal ultrasound through a full bladder or transperineal ultrasound in virginal or atrophic women can still provide helpful, although limited, information. In some cases, ultrasound can specifically diagnose the type of ovarian cyst, especially if certain characteristic findings are present (Box 1). Figures 6– 11 illustrate and describe characteristic findings seen with simple ovarian cysts, hemorrhagic corpus luteum cysts, dermoid cysts, endometriomas, and malignant cysts 77.
Identifying certain ovarian cyst characteristics is especially important in differentiating benign from malignant processes. The ten “Simple Rules” are five ultrasound features indicative of benign cysts (B-features) and five ultrasound features indicative of a malignant cysts (M-features) based on the presence of tumor morphology, degree of vascularity, and ascites (Table 1) 78.
Box 1. Characteristics of Simple and Malignant ovarian cysts
| Simple ovarian cyst | Malignant ovarian cyst |
|---|---|
|
|
Table 1. “Simple Rules” differentiating Benign and Malignant Cysts
| Benign (B) features | Malignant (M) features |
|---|---|
| B1 unilocular cyst a B2 solid components present, but <7 mm B3 acoustic shadows b B4 smooth multilocular tumor, largest diameter <100 mm B5 no blood flow; color score 1 | M1 irregular solid tumor M2 ascites a M3 at least 4 papillary structures M4 irregular multilocular-solid tumor, largest diameter ≥100 mm b M5 very strong flow; color score 4 |
| If only B features are present → benign tumor If only M features are present → malignant tumor If both B and M features or neither B nor M features present → inconclusive | |
Footnote:
a Most predictive feature.
a Least predictive feature.
[Source 24, 79 ]Figure 10. Ovarian cyst ultrasound
[Source 80 ]Figure 11. Ovarian follicular cyst
Footnotes: There is a 5.5 cm anechoic lesion in the left ovary (there are a few artifactual low level echoes on some images). There are a few round structures at the border (compatible with a normal cumulus oophorus), but no wall thickening, nodularity, papillary projection or thickened septation. No flow on color Doppler imaging. This is an example of a normal ovarian follicular cyst. The ovarian follicular cyst is on the larger size (5.5 cm), but the young/premenopausal status of the patient and the lack of any aggressive features is compatible with a dominant Graafian follicle that failed to rupture. These classically resolve in 1-2 menstrual cycles and persistent cysts raise other lesions into the differential diagnosis (such as serous cystadenoma), although other options on the differential would be much less common in this age than a physiologic cyst. Some follow up a follicular cyst between 5-7 cm with ultrasound in one year, to ensure that it resolves. MRI is usually performed if there are possible aggressive features or if the cyst is >7 cm.
[Source 81 ]Figure 12. Hemorrhagic corpus luteum cysts
Footnotes: Severe pain in lower abdomen. LNMP – 20 days back. Ultrasonography was done after 3 hours of the onset of pain. Empty uterine cavity. A collapsed cyst in left ovary. Free fluid in pelvis and hepato-renal region. Findings are suggestive of ruptured hemorrhagic ovarian cyst with hemoperitoneum. Urine pregnancy test was negative. Hb level was 10.5 gm/dL. Laparoscopy was done 3 hours after ultrasonography. Findings confirmed ruptured corpus luteum cyst.
[Source 82 ]Figure 13. Ovarian dermoid cysts
Footnote: Voluminous formation containing numerous echogenic balls floating in an anechoic liquid. In the posterior region, there are echogenic structures with posterior acoustic shadow probably due to calcifications, hair strands, or foci of fat. The appearance of cysts containing multiple internal floating balls is a very rare presentation of the dermoid cyst, but is considered pathognomonic for this entity and was first described in 1991 83, 84. These internal floating balls may be single or multiple, measuring around 5 to 40 mm, composed of keratin, fibrin, hemosiderin, hair, and fat in different proportions and their mechanism of formation has not been well defined yet.
[Source 85 ]Figure 14. Endometrioma
Footnote: Large right adnexal cystic lesion with homogeneous echogenic content. Mild free fluid at the pelvis. Surgically confirmed case of right ovarian chocolate cyst.
[Source 86 ]Figure 15. Malignant ovarian cyst
Footnotes: 69 years old female with lower abdominal pain, weight loss and distension of abdomen. Ultrasound showed solid cystic mass in pelvis with vascularity on doppler. Ovaries are not seperately seen. The uterus is normal. Another solid hypoechoic hepatic nodule in segment V with ascites. CT scan performed the following day (not shown) – similar findings of ovarian tumor and hepatic solitary metastasis. Ascites fluid tapping showed malignant cells.
[Source 87 ]Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) is a valuable tool when ultrasound is inconclusive or limited. The advantages of MRI are that it is very accurate and it provides additional information on the composition of soft-tissue tumors.8 On the other hand, MRI is more expensive, is usually less available, and is more inconvenient for the patient than ultrasound. MRI for the evaluation of ovarian cysts is usually ordered with contrast, unless contraindicated.8 In one study of MRI as second-line imaging for indeterminate cysts, contrast-enhanced MRI contributed to a greater change in the probability of ovarian cancer compared with computed tomography (CT), Doppler ultrasound, or MRI without contrast.12 This may result in a reduction in unnecessary surgeries and in an increase in proper referrals in cases of suspected malignancy.
Computed Tomography (CT)
Computed tomography (CT) is usually not used in the evaluation of ovarian cysts. CT offers poor discrimination of soft tissue and exposes the patient to more radiation than does ultrasound or MRI. The utility of CT is primarily in the preoperative staging of a suspected ovarian cancer.13 Cysts discovered via CT scan should be further evaluated using ultrasonography.
Ovarian cyst differential diagnosis
The differential diagnosis of benign ovarian cysts includes:
- Simple cysts
- Hemorrhagic corpus luteum cysts
- Dermoids (mature cystic teratomas)
- Endometriomas
- Pedunculated fibroids
- Hydrosalpinges
- Paratubal and paraovarian cysts
- Peritoneal inclusion cysts (also known as pseudocysts)
- Pelvic kidneys
- Appendiceal or diverticular abscess
- Ectopic pregnancy
The diagnosis of an ovarian cyst is most often made based on imaging rather than by physical examination, laboratory testing, or diagnostic procedures.
The differential diagnosis for pain in women with ovarian cysts include tubo-ovarian abscess, ruptured ectopic, ruptured hemorrhagic cyst, and ovarian torsion 88.
Ovarian cyst treatment
Ovarian cyst treatment depends on your age, the type and size of your cyst, and your symptoms. Management of patients with simple ovarian cysts should follow the algorithm shown in Figures 12 and 13 below. Your doctor might suggest 89:
- Watchful waiting. In many cases you can wait and be re-examined to see if the cyst goes away within a few months. This is typically an option — regardless of your age — if you have no symptoms and an ultrasound shows you have a simple, small, fluid-filled cyst. Your doctor will likely recommend that you get follow-up pelvic ultrasounds at intervals to see if your cyst changes in size.
- Medication. Your doctor might recommend hormonal contraceptives, such as birth control pills, to keep ovarian cysts from recurring. However, birth control pills won’t shrink an existing cyst.
- Surgery. Your doctor might suggest removing an ovarian cyst that is large, doesn’t look like a functional cyst, is growing, continues through two or three menstrual cycles, or causes pain. The National Institutes of Health estimates that 5% to 10% of women have surgery to remove an ovarian cyst. Only 13% to 21% of these cysts are cancerous 90. An ovarian cyst that develops after menopause is sometimes cancer. In this case, you may need to see a gynecologic cancer specialist. You might need surgery to remove your uterus, cervix, fallopian tubes and ovaries. You may also need chemotherapy or radiation.
Your ovarian cyst may require surgery if you are past menopause or if your cyst:
- Does not go away after several menstrual cycles
- Gets larger
- Looks unusual on the ultrasound
- Causes pain
If your ovarian cyst does not require surgery, your doctor may:
- Talk to you about pain medicine. Your doctor may recommend over-the-counter medicine or prescribe stronger medicine for pain relief.
- Prescribe hormonal birth control if you have cysts often. Hormonal birth control, such as the pill, vaginal ring, shot, or patch, help prevent ovulation. This may lower your chances of getting more cysts.
Figure 16. Simple ovarian cyst management algorithm
[Source 24 ]Figure 17. Ovarian cyst management algorithm
[Source 24 ]Ovarian cyst with a High Likelihood of Malignancy
Women with ovarian cysts with a high likelihood of malignancy should be referred directly to a gynecologic oncologist. High likelihood of malignancy exists if malignant features are found on ultrasound, in women with a personal history or a first-degree relative with history of ovarian or breast cancer, or if cancer antigen 125 (CA 125) is >35 (postmenopausal women) or CA 125 >200 (premenopausal women) (Figure 13). Direct referral to and treatment by gynecologic oncologists has been shown to improve survival rates in women with ovarian cancer 91, 92, 93.
Ovarian cyst with an Indeterminate Likelihood of Malignancy
For women with ovarian cysts with an intermediate likelihood of malignancy, further workup is warranted. The most cost-effective test is a second ultrasound and a second opinion at a tertiary center. Obtaining the CA 125 level can be helpful in this instance (Figure 13).
Ovarian cyst with an Unclear Likelihood of Malignancy but Likely Benign
For women with ovarian cysts with an unclear likelihood of malignancy but most likely benign, repeat ultrasound in 6 to 12 weeks is warranted 88. There are no official guidelines as to when to stop serial imaging, but one or two ultrasounds to confirm size and morphologic stability has been suggested 94. Of course, once a lesion has resolved, there is no need for further imaging.
Ovarian cyst surgery
Surgery may be recommended if your ovarian cyst is very large or causing symptoms or if cancer is suspected.
If your ovarian cyst requires surgery, your doctor will either remove just the cyst or the entire ovary. Some cysts can be removed without removing the ovary (ovarian cystectomy). In some cases, the ovary with the cyst is removed (oophorectomy).
Surgery can be done in two different ways:
- Laparoscopy. With this surgery, the doctor makes a very small cut above or below your belly button to look inside your pelvic area and remove the cyst with a laparoscope and instruments inserted through small cuts in your abdomen. This is often recommended for smaller cysts that look benign (not cancerous) on the ultrasound.
- Laparotomy. Your doctor may choose this method if the cyst is large or cancer is a concern. This surgery uses a larger cut in the abdomen to remove the cyst. The cyst is then tested for cancer. If it is likely to be cancerous, it is best to see a gynecologic oncologist, who may need to remove the ovary and other tissues, like the uterus.
If a cystic mass is cancerous, your doctor will likely refer you to a gynecologic cancer specialist. You might need to have your uterus, ovaries and fallopian tubes removed (total hysterectomy) and possibly chemotherapy or radiation. Your doctor is also likely to recommend surgery when an ovarian cyst develops after menopause.
Treating conditions that cause ovarian cysts
If you have been diagnosed with a condition that can cause ovarian cysts, such as endometriosis or polycystic ovary syndrome (PCOS), your treatment may be different.
For example, endometriosis may be treated with painkillers, hormone medication, and/or surgery to remove or destroy areas of endometriosis tissue.
Ovarian cyst prognosis
Most ovarian cysts are found incidentally, are asymptomatic, and tend to be benign (not cancer) with spontaneous resolution leading to an overall favorable prognosis 53. Overall, 70% to 80% of follicular cysts resolve spontaneously 53. The potential of benign ovarian cystadenoma to become malignant has been postulated but remains unproven 53. Less aggressive tumors of low malignant potential run a benign course. The overall survival in these cases is 86.2% at five years 95. Malignant change can occur in a few cases of dermoid cysts (associated with extremely poor prognosis) and endometriosis 53. If an ovarian cyst is suspected to be malignant, the prognosis is usually poor since ovarian cancer tends to be diagnosed in the advanced stages 53.
Ovarian torsion
Ovarian torsion also sometimes termed adnexal torsion or tubo-ovarian torsion, refers to rotation of the ovary and portion of the fallopian tube on the supplying vascular pedicle leading to reduced venous return, stromal edema, internal hemorrhage, and infarction with the subsequent complications 96. The result of vascular compromise secondary to ovarian torsion is hemorrhagic infarction and necrosis, that can occur as rapidly as within hours of torsion onset. Ovarian torsion can be intermittent or sustained and results in venous, arterial and lymphatic stasis. It is a gynecological emergency and requires urgent surgical intervention to prevent ovarian necrosis. Ovarian torsion classically occurs unilaterally in a pathologically enlarged ovary. Torsion of a normal ovary is most common among young children 97.
Ovarian torsion has a bimodal age distribution occurring mainly in young women (15-30 years) and post-menopausal women. Approximately 20% of the cases occur during pregnancy 98. Studies reveal that ovarian torsion is the fifth most common gynecologic surgical emergency, accounting for 2.7% of cases of acute gynecologic complaints in 1 series. Ovarian torsion is encountered more often in women who have had ovarian stimulation, which likely accounts for a slightly increased incidence in developed countries.
The median age reported by a large review was 28 years. The percentage of patients younger than 30 years is approximately 70-75%. Two groups of women show a particular tendency to be affected by adnexal torsion (ovarian torsion): (1) women in their mid 20s and (2) women who are postmenopausal.
Approximately 20% of cases of torsion occur during pregnancy 99. Postmenopausal women with an adnexal mass may also be affected. Adolescents are also at risk; this may be because of changes in the weight of their maturing adnexa 99. Approximately 17% of cases have been found to occur in premenarchal or postmenopausal women. Although ovarian torsion in very young children is rare, a case of ovarian cyst torsion was reported in a 2-year-old 100.
What causes ovarian torsion?
Ovarian torsion occurs due to 2 main reasons 101:
- Hypermobility of the ovary: <50%
- Adnexal mass: ~50-80%
- most lesions are dermoid cysts or para ovarian cysts
- large cystic ovaries undergoing ovarian hyperstimulation are at particular risk
- masses between 5-10 cm are at most risk 102
Torsion of a normal ovary more commonly occurs in young children when developmental abnormalities predispose the ovary to torsion, such as excessively long Fallopian tubes or an absent mesosalpinx.
In adulthood, causes include both benign and malignant ovarian tumors, polycystic ovaries and adhesions. In early pregnancy, a torsion can occur secondary to a corpus luteal cyst or laxity of the adjacent tissues.
Anatomic changes affecting the weight and the size of the ovary may alter the position of the fallopian tube and allow twisting to occur.
Pregnancy is associated with, and may be responsible for, torsion in approximately 20% of adnexal torsion cases 103, probably secondary to the ovarian enlargement that occurs during ovulation in combination with laxity of the supporting tissues of the ovary.
Congenitally malformed and elongated fallopian tubes may be seen, particularly in young, prepubertal patients.
Ovarian tumors, both benign and malignant, are implicated in 50-60% of cases of torsion. Involved masses are nearly all larger than 4-6 cm, although torsion is still possible with smaller masses. Dermoid tumors are most common. Malignant tumors are much less likely to result in torsion than benign tumors are. This is because of the presence of cancerous adhesions that fix the ovary to surrounding tissues.
Conversely, patients with a history of pelvic surgery (principally tubal ligation) are at increased risk for torsion, probably because of adhesions that provide a site around which the ovarian pedicle may twist.
Ovarian torsion signs and symptoms
Most patients present with severe non-specific lower abdominal and pelvic pain, either intermittent or sustained, nausea, and vomiting. There is adnexal tenderness. A raised white cell count is common.
Classically, patients present with the sudden onset (commonly during exercise or other agitating movement) of severe, unilateral lower abdominal pain that worsens intermittently over many hours. A minority of patients, however, complain of mild pain that follows a more prolonged time course. The pain usually is localized over the involved side, often radiating to the back, pelvis, or thigh. Approximately 25% of patients experience bilateral lower quadrant pain. It may be described as sharp and stabbing or, less frequently, crampy.
Nausea and vomiting occur in approximately 70% of patients, mimicking a gastrointestinal source of pain and further obscuring the diagnosis.
A history of previous episodes may be elicited, possibly attributable to partial, spontaneously resolving torsion. Fever may occur as a late finding as the ovary becomes necrotic.
Ovarian torsion in premenarchal girls is associated with a longer interval from onset of symptoms and an increased rate of fever and pelvic mass at presentation compared with postmenarchal patients, according to one study. Median duration of symptoms before presentation was 24 hours for premenarchal patients, versus 8 hours for postmenarchal patients 104. In another study, of 32 premenarchal patients with ovarian torsion, the main presenting symptoms were abdominal pain (92.3%) and nausea and vomiting (84.6%). Abdominal tenderness was present in 64.1%.On abdominal ultrasound, an enlarged ovary was identified in 28.9% 105.
In a retrospective study of ovarian torsion in premenarchal and postmenarchal patients in Israel, there was a higher frequency of nausea and vomiting in the premenarchal patients. Ovarian cysts were more commonly demonstrated in postmenarchal patients, and a normal adnexal appearance on ultrasound was more common in premenarchal patients. Because of a normal adnexa in 69% of cases in premenarchal patients, a high index of suspicion is necessary in any premenarchal patient with acute-onset abdominal pain 106.
Ovarian torsion in the third trimester of pregnancy is likely to present as nonspecific symptoms of lower abdominal pain, nausea, and vomiting and can often be misdiagnosed as appendicitis or preterm labor. Although conservative treatment has been proposed during pregnancy, surgical intervention may be necessary if ovarian torsion is highly suspected. Ultrasonography in early pregnancy should address the cervix and the adnexa for early diagnosis and management of ovarian masses, thus avoiding later emergency situations and the possibility of preterm deliveries 107.
Signs of ovarian torsion
The whirlpool sign or whirl sign of ovarian torsion is characterized by the appearances of a twisted ovarian pedicle seen on ultrasound or even on CT scan. It appears as twisting of the thickened vascular pedicle of the enlarged ovary. It can be detected on ultrasound confirming the diagnosis along with the other suggestive imaging features and clinical presentation 108. On MRI, it is best demonstrated on axial T2 and T1 C+ fat sat sequences 109.
Figure 18. Whirl sign of ovarian torsion
Footnote: 50 year old female with acute severe right iliac fossa pain. Yellow arrow indicates torted ovarian pedicle, note the “whirl” pattern.
[Source 110 ]Ovarian torsion complications
Complications of ovarian torsion include the following:
- Infection
- Peritonitis
- Sepsis
- Adhesions
- Chronic pain
- Infertility (rare)
Ovarian torsion diagnosis
The physical examination, like the history, is typically nonspecific and is highly variable. A unilateral, tender adnexal mass has been reported in between 50 and 90% of patients. However, the absence of such a finding does not exclude the diagnosis. Tenderness to palpation is common; however, it is mild in approximately 30% and absent in another 30% of patients. Therefore, the absence of tenderness cannot be used to rule out torsion.
Peritoneal findings are infrequent and indicate advanced disease if present.
Radiographic features
The main feature of torsion is ovarian enlargement due to venous/lymphatic engorgement, edema and hemorrhage. Secondary signs include free pelvic fluid, an underlying ovarian lesion, reduced or absent vascularity and a twisted dilated tubular structure corresponding to the vascular pedicle. Adnexal torsion is commonly unilateral, with a slight (3:2) right-sided predilection (presumably due to the protective effects of the sigmoid colon on the left) 111.
Diagnostic ultrasonography should be the first examination performed; typically, the affected ovary is enlarged, with multiple immature or small follicles along its periphery.
Ultrasonography with color Doppler analysis is the method of choice for the evaluation of adnexal torsion because it can show morphologic and physiologic changes in the ovary and can help in determining whether blood flow is impaired 112. Gray-scale and spectral findings are correlated with the age of the torsion (ie, acute torsion or chronic torsion) and the degree of the twist or torsion. Normal Doppler imaging must not, however, be used as a basis for excluding the diagnosis.
Rarely, computed tomography (CT) or magnetic resonance imaging (MRI) is needed to make a definitive diagnosis. CT or MRI can serve as a secondary modality when ultrasonographic findings are nondiagnostic 113.
Culdocentesis is a nonspecific test that is unlikely to confirm or exclude torsion and therefore is not recommended in the diagnostic workup.
Ovarian torsion treatment
In a patient with a history and physical examination findings suggestive of ovarian torsion, gynecologic consultation and subsequent laparoscopy are critical, regardless of whether laboratory and radiologic studies yield normal results.
Approximately 1 in 1800 pregnancies is complicated by adnexal torsion, typically between the sixth and fourteenth weeks of gestation. This increased frequency in pregnant women is likely due to greater laxity of the tissues adjoining the ovaries and oviducts during pregnancy, as well as to enlargement of the ovary in early pregnancy secondary to the corpus luteum cyst.
Detorsion of the adnexa during pregnancy has not been found to compromise fetal well-being. However, if the corpus luteum cyst is removed during salpingo-oophorectomy, supplemental progesterone is indicated.
Outpatient care has no role in the treatment of ovarian torsion. Patients with either a suspected or confirmed diagnosis of ovarian torsion should be admitted and either operated on or observed by a gynecologist. Laparoscopy can be used for both confirmation of the diagnosis and treatment.
Ovarian torsion prognosis
With early diagnosis and appropriate treatment, the prognosis of ovarian torsion is excellent. However, most patients with ovarian torsion have a delayed diagnosis, often resulting in infarction and necrosis of the ovary. The ovarian salvage rate has been reported below 10% in adults but as high as 27% in a study among pediatric patients 114.
Although the loss of a single ovary is unlikely to result in significantly reduced fertility and no cases of death due to ovarian torsion have been reported, early diagnosis allows conservative laparoscopic treatment and reduction in complications. In a retrospective large study comparing pregnant patients with adnexal torsion to nonpregnant patients with adnexal torsion, the recurrence rate of torsion was 19.5% in pregnant women and 9.1% in nonpregnant women 115.
Ovarian cancer
Ovarian cancer is cancer that forms in tissues of the ovary (one of a pair of female reproductive glands in which the eggs or ova, are formed). The ovaries are a pair of small organs in the female reproductive system that contain and release an egg once a month in women of menstruating age. This is known as ovulation. Ovarian cancers were previously believed to begin only in the ovaries, but recent evidence suggests that many ovarian cancers may actually start in the cells in the far (distal) end of the fallopian tubes.
Most ovarian cancers are either ovarian epithelial cancers (cancer that begins in the cells on the surface of the ovary) or malignant germ cell tumors (cancer that begins in egg cells). Fallopian tube cancer and primary peritoneal cancer are similar to ovarian epithelial cancer and are staged and treated the same way.
In general, cancer begins when a cell develops errors (mutations) in its DNA. The mutations tell the cell to grow and multiply quickly, creating a mass (tumor) of abnormal cells. The abnormal cells continue living when healthy cells would die. They can invade nearby tissues and break off from an initial tumor to spread elsewhere in the body (metastasize).
There are several types of ovarian cancer. They include:
- Epithelial ovarian cancer, which affects the outer surface layers of the ovary; it is by far the most common type. About 90 percent of ovarian cancers are epithelial tumors.
- Germ cell ovarian cancer, which originate in the cells that make the eggs. These rare ovarian cancers tend to occur in younger women.
- Stromal tumors, which develop within the cells that release female hormones. Stromal tumors are usually diagnosed at an earlier stage than other ovarian cancers. About 7 percent of ovarian tumors are stromal.
It is also possible to have borderline epithelial tumors which are not as aggressive as other epithelial tumors. These are sometimes called ‘low malignant potential’ or LMP tumors.
Ovarian cancer mainly develops in older women who have experienced menopause (usually over the age of 50), but it can affect women of any age. About half of the women who are diagnosed with ovarian cancer are 63 years or older. It is more common in white women than African-American women 116.
Ovarian cancer can spread to other parts of the reproductive system and the surrounding areas, including the womb (uterus), vagina and abdomen.
The symptoms of ovarian cancer can be difficult to recognize, particularly in the early stages of the disease. They are often the same as the symptoms of other, less serious, conditions, such as irritable bowel syndrome (IBS) or premenstrual syndrome (PMS). The symptoms of ovarian cancer can be similar to other conditions making them difficult to recognize. However, there are early symptoms to look out for such as pain in the pelvis and lower stomach, persistent bloating and difficulty eating. Consult your doctor if you are experiencing any of these symptoms.
The most common symptoms of ovarian cancer are:
- Pain. You might have pain or discomfort in:
- your belly (abdomen)
- the area between your hip bones (pelvis)
- your back – although this is less common
- Swollen belly. Feeling bloated or an increase in the size of your abdomen that doesn’t go away can be a symptom of ovarian cancer.
- Loss of appetite. You might feel full quickly when you eat. Or you may not feel like eating.
- Urinary changes. You may need to pee more often, or have to go more urgently.
You may also have some other symptoms including:
- Tiredness. You might feel extremely tired for no obvious reason if you have ovarian cancer.
- Bowel changes. You might have loose poop or need to poop more often (diarrhea). Or you may go less often or have hard poop (constipation).
- Weight loss and feeling sick. You might lose weight even if you aren’t trying to. This might be due to feeling sick.
- Indigestion. Indigestion causes heartburn, bloating and sickness. It is a common problem in the general population, and for most people it isn’t a sign of cancer.
- Vaginal bleeding. You might notice bleeding in between your periods. Or you could have bleeding from your vagina after your menopause.
Ovarian cancer often goes undetected until it has spread within the pelvis and abdomen. At this late stage, ovarian cancer is more difficult to treat and is frequently fatal. Early-stage ovarian cancer, in which the disease is confined to the ovary, is more likely to be treated successfully.
Surgery and chemotherapy are generally used to treat ovarian cancer. The amount and type of surgery you have depends on how far your cancer has spread and on your general health. For women of childbearing age who have certain kinds of tumors and whose cancer is in the earliest stage, it may be possible to treat the disease without removing both ovaries and the uterus.
Some women with ovarian cancer might have:
- Targeted cancer drugs
- Hormone therapy
- Radiotherapy (radiation therapy)
The American Cancer Society estimates for ovarian cancer in the United States for 2025 are 116, 117:
- New cases: About 20,890 women will receive a new diagnosis of ovarian cancer. The rate at which women are diagnosed with ovarian cancer has been slowly falling over the past 20 years. The incidence rate declined by 1% to 2% per year from 1990 to the mid-2010s and by almost 2% per year from 2012 to 2021. This trend is likely due at least in part to increased oral contraceptive use in the latter half of the past century and decreased menopausal hormone therapy use during the 2000s, both of which can lower risk.
- Deaths: About 12,730 women will die from ovarian cancer. Ovarian cancer ranks fifth in cancer deaths among women, accounting for more deaths than any other cancer of the female reproductive system. Ovarian cancer mortality has declined from 2% annually during the 2000s and early 2010s to more than 3% annually from 2016 to 2020, reflecting both decreased incidence and improved treatment.
- 5-Year Relative Survival: 50.9%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Ovarian cancer deaths as a percentage of All Cancer Deaths: 2.1%.
- Rate of New Cases and Deaths per 100,000: The rate of new cases of ovarian cancer was 10.2 per 100,000 women per year. The death rate was 6.0 per 100,000 women per year. These rates are age-adjusted and based on 2017–2021 cases and 2018–2022 deaths.
- Lifetime Risk of Developing Ovarian Cancer: Approximately 1.1 percent of women will be diagnosed with ovarian cancer at some point during their lifetime, based on 2018–2021 data.
- In 2021, there were an estimated 238,484 women living with ovarian cancer in the United States.
A woman’s risk of getting ovarian cancer during her lifetime is about 1 in 91. Her lifetime chance of dying from ovarian cancer is about 1 in 143. These statistics don’t count low malignant potential ovarian tumors.
Known risk factors for ovarian cancer include:
- Getting older: women who are over 50 are more likely to develop ovarian cancer than younger women. The risk of ovarian cancer increases steeply from around 45 years. And is greatest in those aged between 75 and 79 years.
- Inheriting a faulty gene called a gene mutation that increases the risk of ovarian cancer. Between 5 and 15 out of 100 ovarian cancers (5 to 15%) are caused by an inherited faulty gene. Mutations in the breast cancer susceptibility genes 1 and 2 (BRCA1 and BRCA2), and those associated with Lynch syndrome, raise ovarian cancer risk.
- Having a strong family history of ovarian cancer, breast cancer, or some other cancers, including colorectal cancer and endometrial cancer
- Having had breast cancer in the past. The risk is higher in women diagnosed with breast cancer at a younger age. And those with estrogen receptor negative (ER negative) breast cancer.
Only around 5-15% of all ovarian cancers are due to inherited factors.
Research suggests that the risk of ovarian cancer is slightly higher for women who:
- have medical conditions such as endometriosis and diabetes. Studies have shown that women with endometriosis or diabetes have an increased risk of ovarian cancer. In diabetics, the increase in risk might be higher in those that use insulin.
- use long-term hormone replacement therapy (HRT). Using HRT (hormone replacement therapy) after the menopause increases the risk of ovarian cancer.
- had early puberty (menstruating before 12) or late menopause (onset after 50)
- smoke cigarettes. Smoking can increase your risk of certain types of ovarian cancer such as mucinous ovarian cancer. The longer you have smoked, the greater the risk.
- are overweight or obese. Having excess body fat is linked to an increase in risk of ovarian cancer.
Women have a lower risk of developing ovarian cancer if:
- they had a baby before the age of 26
- they used oral contraceptives (the pill) for at least 3 months
- they have had a hysterectomy (removal of the uterus) and tubal ligation (tubes tied)
Make an appointment with your doctor if you have any signs or symptoms that worry you.
If you have a family history of ovarian cancer or breast cancer, talk to your doctor about your risk of ovarian cancer. Your doctor may refer you to a genetic counselor to discuss testing for certain gene mutations that increase your risk of breast and ovarian cancers.
Ovarian cancer types
Your ovaries are made up of different types of cells. The type of ovarian cancer you have depends on the type of cell it starts in.
The main types of ovarian cancer are 118:
- Epithelial ovarian cancers which start in the surface layer which covers the ovary, fallopian tube or peritoneum.
- Germ cell ovarian cancer which begins in the cells that develop into eggs.
- Sex cord stromal cancers which begin in the tissues that support your ovaries and produce hormones.
Knowing which type of ovarian cancer you have helps your doctors decide what treatment you need.
Epithelial ovarian tumors
Epithelial ovarian tumors start in the outer surface of the ovaries. These tumors can be benign (not cancer), borderline (low malignant potential), or malignant (cancer).
Benign epithelial ovarian tumors
Epithelial ovarian tumors that are benign don’t spread and usually don’t lead to serious illness. There are several types of benign epithelial tumors including serous cystadenomas, mucinous cystadenomas, and Brenner tumors.
Borderline epithelial tumors
When looked at in the lab, some ovarian epithelial tumors don’t clearly appear to be cancerous and are known as borderline epithelial ovarian cancer. Around 15 out of 100 ovarian tumors (15%) are borderline tumors. They are sometimes called atypical proliferative tumors or tumors of low malignant potential.
Borderline epithelial ovarian tumors are different to ovarian cancer because they don’t grow into the supportive tissue of the ovary (the stroma). They usually grow slowly and in a more controlled way than cancer cells.
Borderline epithelial ovarian tumors usually affect women aged between 20 and 40. They are usually diagnosed at an early stage. This means the abnormal cells are still within the ovary.
Sometimes abnormal cells break away from the tumor and settle elsewhere in the body. This is usually in the belly (abdomen). Very rarely, these cells start to grow into the underlying tissue.
There are different types of borderline ovarian tumors. The two most common types are atypical proliferative serous carcinoma and atypical proliferative mucinous carcinoma. These tumors were previously called tumors of low malignant potential (LMP tumors). These are different from typical ovarian cancers because they don’t grow into the supporting tissue of the ovary called the ovarian stroma. If they do spread outside the ovary, for example, into the abdominal cavity (belly), they might grow on the lining of the abdomen but not into it.
These tumors grow slowly and are less life-threatening than most ovarian cancers.
Malignant epithelial ovarian tumors
Cancerous epithelial tumors are called carcinomas. About 85% to 90% of malignant ovarian cancers are epithelial ovarian carcinomas. These tumor cells have several features (when looked at in the lab) that can be used to classify epithelial ovarian carcinomas into different types. The serous type is by far the most common, and can include high grade and low grade tumors. The other main types include mucinous, endometrioid, and clear cell.
- Serous carcinomas (52%)
- High grade serous carcinoma is the most common type of epithelial ovarian cancer. It can affect the ovaries, fallopian tubes or the peritoneum. Doctors think that most high grade serous carcinomas start in the cells at the end of the fallopian tube (fimbriae). These early cancer cells then spread to the ovary and grow. So they might sometimes be called fallopian tube cancer or tubo ovarian cancer.
- Low grade serous ovarian cancers are rare. They are usually diagnosed in younger people and are slow growing. Chemotherapy doesn’t tend to work as well as it does for other types of epithelial ovarian cancer.
- Endometroid carcinoma (10%)
- Endometrioid ovarian cancer is the 2nd most common type of epithelial ovarian cancer. It can be linked to endometriosis. Most cases of endometrioid ovarian cancer are diagnosed at an early stage and are low grade. Some women have endometroid ovarian cancer at the same time as a separate womb (endometrial) cancer.
- Clear cell carcinoma (6%)
- Clear cell ovarian cancer can also be linked to endometriosis. The treatment is the same as for high grade serous ovarian cancer. But chemotherapy doesn’t tend to work as well as it does for other types of epithelial ovarian cancer.
- Mucinous carcinoma (6%)
- Mucinous ovarian cancer is rare. It can be difficult to diagnose. The doctor does tests to check if the cancer started to grow in the ovary. Or if it spread there from somewhere else in your digestive system. Chemotherapy doesn’t tend to work as well for mucinous ovarian cancer. Mucinous tumors can be one of the following:
- non-cancerous (benign)
- borderline (contain abnormal cells but are not a cancer)
- cancerous (malignant)
- Mucinous ovarian cancer is rare. It can be difficult to diagnose. The doctor does tests to check if the cancer started to grow in the ovary. Or if it spread there from somewhere else in your digestive system. Chemotherapy doesn’t tend to work as well for mucinous ovarian cancer. Mucinous tumors can be one of the following:
- Undifferentiated or unclassifiable
- Some epithelial ovarian cancers are undifferentiated or unclassifiable. These cancers have cells that are very undeveloped. So it is not possible to tell which type of cell the cancer started from.
Each ovarian cancer is given a grade, based on how much the tumor cells look like normal tissue:
- Grade 1 epithelial ovarian carcinomas look more like normal tissue and tend to have a better prognosis (outlook).
- Grade 3 epithelial ovarian carcinomas look less like normal tissue and usually have a worse outlook.
Other traits are also taken into account, such as how fast the cancer cells grow and how well they respond to chemotherapy, to come up with the tumor’s type:
- Type 1 tumors tend to grow slowly and cause fewer symptoms. These tumors also seem not to respond well to chemotherapy. Low grade (grade 1) serous carcinoma, clear cell carcinoma, mucinous carcinoma and endometroid carcinoma are examples of type 1 tumors.
- Type 2 tumors grow fast and tend to spread sooner. These tumors tend to respond better to chemotherapy. High grade (grade 3) serous carcinoma is an example of a type 2 tumor.
Other cancers that are similar to epithelial ovarian cancer
Primary peritoneal carcinoma
Primary peritoneal carcinoma is a rare cancer closely related to epithelial ovarian cancer. At surgery, it looks the same as an epithelial ovarian cancer that has spread through the abdomen. In the lab, primary peritoneal carcinoma also looks just like epithelial ovarian cancer. Other names for this cancer include extra-ovarian (meaning outside the ovary) primary peritoneal carcinoma and serous surface papillary carcinoma.
Primary peritoneal carcinoma appears to start in the cells lining the inside of the fallopian tubes.
Like ovarian cancer, primary peritoneal carcinoma tends to spread along the surfaces of the pelvis and abdomen, so it is often difficult to tell exactly where the cancer first started. This type of cancer can occur in women who still have their ovaries, but it is of more concern for women who have had their ovaries removed to prevent ovarian cancer. This cancer does rarely occur in men.
Symptoms of primary peritoneal carcinoma are similar to those of ovarian cancer, including abdominal pain or bloating, nausea, vomiting, indigestion, and a change in bowel habits. Also, like ovarian cancer, primary peritoneal carcinoma may elevate the blood level of a tumor marker called CA-125.
Women with primary peritoneal carcinoma usually get the same treatment as those with widespread ovarian cancer. This could include surgery to remove as much of the cancer as possible (a process called debulking that is discussed in the section about surgery), followed by chemotherapy like that given for ovarian cancer. Its outlook is likely to be similar to widespread ovarian cancer.
Fallopian tube cancer
This is another rare cancer that is similar to epithelial ovarian cancer. It begins in the tube that carries an egg from the ovary to the uterus (the fallopian tube). Like primary peritoneal carcinoma, fallopian tube cancer and ovarian cancer have similar symptoms. The treatment for fallopian tube cancer is much like that for ovarian cancer, but the outlook (prognosis) is slightly better.
Ovarian germ cell tumors
Germ cells usually form the ova or eggs in females and the sperm in males. Germ cell ovarian tumors begin in the ovarian cells that develop into eggs (germ cells). They are rare and usually affect people up to their early 30s. Less than 2% of ovarian cancers are germ cell tumors. Most ovarian germ cell tumors are benign, but some are cancerous and may be life threatening. Overall, they have a good outlook, with more than 9 out of 10 patients surviving at least 5 years after diagnosis. You usually have surgery to remove the tumor. You might have chemotherapy if your tumor is cancerous. Treatment usually works well and most women are cured.
There are several subtypes of germ cell tumors. They can be non cancerous (benign) or cancerous (malignant).
Benign germ cell ovarian tumors
- Mature teratomas also called ovarian dermoid cysts are the most common type of ovarian germ cell tumor. They are non cancerous (benign). They are most common in women during their teens to their forties.
Malignant germ cell ovarian tumors
- These tumors contain cancer cells. There are different types including:
- immature teratomas
- dysgerminoma
- yolk sac tumor
- non gestational choriocarcinoma
- embryonal carcinoma
The most common germ cell tumors are teratomas, dysgerminomas, endodermal sinus tumors, and choriocarcinomas. Germ cell tumors can also be a mix of more than a single subtype.
Teratoma
Teratomas are germ cell tumors with areas that, when seen under the microscope, look like each of the 3 layers of a developing embryo: the endoderm (innermost layer), mesoderm (middle layer), and ectoderm (outer layer). This germ cell tumor has a benign form called mature teratoma and a cancerous form called immature teratoma.
The mature teratoma is by far the most common ovarian germ cell tumor. It is a benign tumor that usually affects women of reproductive age (teens through forties). It is often called a dermoid cyst because its lining is made up of tissue similar to skin (dermis). These tumors or cysts can contain different kinds of benign tissues including, bone, hair, and teeth. The patient is cured by surgical removal of the cyst, but sometimes a new cyst develops later in the other ovary.
Immature teratomas are a type of cancer. They occur in girls and young women, usually younger than 18. These are rare cancers that contain cells that look like those from embryonic or fetal tissues such as connective tissue, respiratory passages, and brain. Tumors that are relatively more mature (called grade 1 immature teratoma) and haven’t spread beyond the ovary are treated by surgical removal of the ovary. When they have spread beyond the ovary and/or much of the tumor has a very immature appearance (grade 2 or 3 immature teratomas), chemotherapy is recommended in addition to surgery.
Dysgerminoma
This type of cancer is rare, but it is the most common ovarian germ cell cancer. It usually affects women in their teens and twenties. Dysgerminomas are considered malignant (cancerous), but most don’t grow or spread very rapidly. When they are limited to the ovary, more than 75% of patients are cured by surgically removing the ovary, without any further treatment. Even when the tumor has spread further (or if it comes back later), surgery, radiation therapy, and/or chemotherapy are effective in controlling or curing the disease in about 90% of patients.
Endodermal sinus tumor (yolk sac tumor) and choriocarcinoma
These very rare tumors typically affect girls and young women. They tend to grow and spread rapidly but are usually very sensitive to chemotherapy. Choriocarcinoma that starts in the placenta (during pregnancy) is more common than the kind that starts in the ovary. Placental choriocarcinomas usually respond better to chemotherapy than ovarian choriocarcinomas do.
Ovarian stromal tumors
About 1% of ovarian cancers are ovarian stromal cell tumors. More than half of stromal tumors are found in women older than 50, but about 5% of stromal tumors occur in young girls.
The most common symptom of these tumors is abnormal vaginal bleeding. This happens because many of these tumors produce female hormones (estrogen). These hormones can cause vaginal bleeding (like a period) to start again after menopause. In young girls, these tumors can also cause menstrual periods and breast development to occur before puberty.
Less often, stromal tumors make male hormones (like testosterone). If male hormones are produced, the tumors can cause normal menstrual periods to stop. They can also make facial and body hair grow. If the stromal tumor starts to bleed, it can cause sudden, severe abdominal pain.
Types of malignant (cancerous) stromal tumors include granulosa cell tumors (the most common type), granulosa-theca tumors, and Sertoli-Leydig cell tumors, which are usually considered low-grade cancers. Thecomas and fibromas are benign stromal tumors. Cancerous stromal tumors are often found at an early stage and have a good outlook, with more than 75% of patients surviving long-term.
Ovarian cancer causes
Scientists don’t yet know exactly what causes most ovarian cancers. Scientists do know some risk factors that make a woman more likely to develop epithelial ovarian cancer. Much less is known about risk factors for germ cell and stromal tumors of the ovaries.
The most recent and important finding about the cause of ovarian cancer is that it starts in cells at the tail ends of the fallopian tubes and not necessarily in the ovary itself. This new information may open more research studies looking at preventing and screening for this type of cancer.
There are many theories about the causes of ovarian cancer. Some of them came from looking at the things that change the risk of ovarian cancer. For example, pregnancy and taking birth control pills both lower the risk of ovarian cancer. Since both of these things reduce the number of times the ovary releases an egg (ovulation), some researchers think that there may be some relationship between ovulation and the risk of developing ovarian cancer.
Also, experts know that tubal ligation and hysterectomy lower the risk of ovarian cancer. One theory to explain this is that some cancer-causing substances may enter the body through the vagina and pass through the uterus and fallopian tubes to reach the ovaries. This would explain how removing the uterus or blocking the fallopian tubes affects ovarian cancer risk.
Another theory is that male hormones (androgens) can cause ovarian cancer.
Researchers have made great progress in understanding how certain mutations (changes) in DNA can cause normal cells to become cancerous. DNA is the chemical that carries the instructions for nearly everything your cells do. You usually look like your parents because they are the source of your DNA. However, DNA affects more than the way you look. Some genes (parts of your DNA) contain instructions for controlling when our cells grow and divide. Mutations in these genes can lead to the development of cancer.
Inherited genetic mutations
Between 5 and 15 out of 100 ovarian cancers (5 to 15%) are caused by an inherited faulty gene. Inherited genes that increase the risk of ovarian cancer include faulty versions of BRCA1 and BRCA2 genes. Faults in BRCA1 and BRCA2 genes also increase the risk of breast cancer.
Other inherited faulty genes such as PTEN (PTEN tumor hamartoma syndrome), STK11 (Peutz-Jeghers syndrome), MUTYH (MUTYH-asociated polyposis, and the many genes that can cause hereditary nonpolyposis colon cancer (MLH1, MLH3, MSH2, MSH6, TGFBR2, PMS1, and PMS2) are related to other family cancer syndromes and linked to an increased risk of ovarian cancer.
Besides the gene mutations mentioned above, there are other genes linked to ovarian cancer. These include ATM, BRIP1, RAD51C, RAD51D, and PALB2. Some of these genes are also associated with cancers such as breast and pancreas.
Having relatives with ovarian cancer does not necessarily mean that you have a faulty inherited gene in the family. The cancers could have happened by chance. But women with a mother or sister diagnosed with ovarian cancer have around 3 times the risk of ovarian cancer. This is compared to women without a family history.
Genetic tests can detect mutations associated with these inherited syndromes. If you have a family history of cancers linked to these syndromes, such as breast and ovarian cancers, thyroid and ovarian cancer, and/or colorectal and endometrial (uterine) cancer, you might want to ask your doctor about genetic counseling and testing. The American Cancer Society recommends discussing genetic testing with a qualified cancer genetics professional before any genetic testing is done.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://findageneticcounselor.nsgc.org) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://abgc.learningbuilder.com/Search/Public/MemberRole/Verification) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (https://www.acmg.net/ACMG/Directories.aspx) has a searchable database of medical genetics clinic services in the United States.
Acquired genetic changes
Most mutations related to ovarian cancer are not inherited but instead occur during a woman’s life and are called acquired mutations. In some cancers, these types of mutations leading to the development of cancer may result from radiation or cancer-causing chemicals, but there is no evidence for this in ovarian cancer. So far, studies haven’t been able to specifically link any single chemical in the environment or in our diets to mutations that cause ovarian cancer. The cause of most acquired mutations remains unknown.
Most ovarian cancers have several acquired mutations. Research has suggested that tests to identify acquired mutations in ovarian cancers, like the TP53 tumor suppressor gene or the HER2 oncogene, can help predict a woman’s prognosis. The role of these tests is still not certain, and more research is needed.
Ovarian cancer risk factors
A risk factor is anything that increases your chance of getting a disease like cancer. Generally, it’s not possible to say what causes ovarian cancer in an individual woman. However, some features are more common among women who have developed ovarian cancer. These features are called risk factors. Having certain risk factors increases a woman’s chance of developing ovarian cancer.
Having one or more risk factors for ovarian cancer doesn’t mean a woman will definitely develop ovarian cancer. In fact, many women with ovarian cancer have no obvious risk factors.
Factors that increase your risk of ovarian cancers
Getting older
The risk of developing ovarian cancer gets higher with age. Ovarian cancer is rare in women younger than 40. The risk of ovarian cancer increases steeply from around 45 years. Most ovarian cancers develop after menopause. And is greatest in those aged between 75 and 79 years. Half of all ovarian cancers are found in women 63 years of age or older.
Being overweight or obese
Obesity has been linked to a higher risk of developing many cancers. The current information available for ovarian cancer risk and obesity is not clear. Obese women (those with a body mass index [BMI] of at least 30) may have a higher risk of developing ovarian cancer, but not necessarily the most aggressive types, such as high grade serous cancers. Obesity may also affect the overall survival of a woman with ovarian cancer.
Having children later or never having a full-term pregnancy
Women who have their first full-term pregnancy after age 35 or who never carried a pregnancy to term have a higher risk of ovarian cancer.
Using fertility treatment
Fertility treatment with in vitro fertilization (IVF) seems to increase the risk of the type of ovarian tumors known as “borderline” or “low malignant potential” (LMP tumors). Other studies, however, have not shown an increased risk of invasive ovarian cancer with fertility drugs. If you are taking fertility drugs, you should discuss the potential risks with your doctor.
Taking hormone therapy after menopause
Women using estrogens after menopause have an increased risk of developing ovarian cancer. The risk seems to be higher in women taking estrogen alone (without progesterone) for many years (at least 5 or 10). The increased risk is less certain for women taking both estrogen and progesterone.
Having a family history of ovarian cancer, breast cancer, or colorectal cancer
Ovarian cancer can run in families. Your ovarian cancer risk is increased if your mother, sister, or daughter has (or has had) ovarian cancer. The risk also gets higher the more relatives you have with ovarian cancer. Increased risk for ovarian cancer can also come from your father’s side.
A family history of some other types of cancer such as colorectal and breast cancer is linked to an increased risk of ovarian cancer. This is because these cancers can be caused by an inherited mutation (change) in certain genes that cause a family cancer syndrome that increases the risk of ovarian cancer.
Having a family cancer syndrome
About 5 to 10% of ovarian cancers are a part of family cancer syndromes resulting from inherited changes (mutations) in certain genes.
Hereditary breast and ovarian cancer syndrome
This syndrome is caused by inherited mutations in the genes BRCA1 and BRCA2, as well as possibly some other genes that have not yet been found. This syndrome is linked to a high risk of breast cancer as well as ovarian, fallopian tube, and primary peritoneal cancers. The risk of some other cancers, such as pancreatic cancer and prostate cancer, are also increased.
Mutations in BRCA1 and BRCA2 are also responsible for most inherited ovarian cancers. Mutations in BRCA1 and BRCA2 are about 10 times more common in those who are Ashkenazi Jewish than those in the general U.S. population.
The lifetime ovarian cancer risk for women with a BRCA1 mutation is estimated to be between 35% and 70%. This means that if 100 women had a BRCA1 mutation, between 35 and 70 of them would get ovarian cancer. For women with BRCA2 mutations the risk has been estimated to be between 10% and 30% by age 70. These mutations also increase the risks for primary peritoneal carcinoma and fallopian tube carcinoma.
In comparison, the ovarian cancer lifetime risk for the women in the general population is less than 2%.
PTEN tumor hamartoma syndrome
In this syndrome, also known as Cowden disease, people are primarily affected with thyroid problems, thyroid cancer, and breast cancer. Women also have an increased risk of endometrial and ovarian cancer. It is caused by inherited mutations in the PTEN gene.
Hereditary nonpolyposis colon cancer
Women with this syndrome have a very high risk of colon cancer and also have an increased risk of developing cancer of the uterus (endometrial cancer) and ovarian cancer. Many different genes can cause this syndrome. They include MLH1, MLH3, MSH2, MSH6, TGFBR2, PMS1, and PMS2. The lifetime risk of ovarian cancer in women with hereditary nonpolyposis colon cancer (Lynch syndrome) is about 10%. Up to 1% of all ovarian epithelial cancers occur in women with hereditary nonpolyposis colon cancer (Lynch syndrome).
Peutz-Jeghers syndrome
People with this rare genetic syndrome develop polyps in the stomach and intestine while they are teenagers. They also have a high risk of cancer, particularly cancers of the digestive tract (esophagus, stomach, small intestine, colon). Women with this syndrome have an increased risk of ovarian cancer, including both epithelial ovarian cancer and a type of stromal tumor called sex cord tumor with annular tubules (SCTAT). This syndrome is caused by mutations in the gene STK11.
MUTYH-associated polyposis
People with this syndrome develop polyps in the colon and small intestine and have a high risk of colon cancer. They are also more likely to develop other cancers, including cancers of the ovary and bladder. This syndrome is caused by mutations in the gene MUTYH.
Having had breast cancer
If you have had breast cancer, you might also have an increased risk of developing ovarian cancer. There are several reasons for this. Some of the reproductive risk factors for ovarian cancer may also affect breast cancer risk. The risk of ovarian cancer after breast cancer is highest in those women with a family history of breast cancer. A strong family history of breast cancer may be caused by an inherited mutation in the BRCA1 or BRCA2 genes and hereditary breast and ovarian cancer syndrome, which is linked to an increased risk of ovarian cancer.
Endometriosis or diabetes
Studies have shown that women with endometriosis or diabetes have an increased risk of ovarian cancer. In diabetics, the increase in risk might be higher in those that use insulin.
Smoking and alcohol use
Smoking doesn’t increase the risk of ovarian cancer overall, but it is linked to an increased risk for the mucinous ovarian cancer. The longer you have smoked, the greater your risk.
Drinking alcohol is not linked to ovarian cancer risk.
Asbestos
Asbestos is an insulating material that’s heat and fire resistant. The International Agency for Research on Cancer (IARC) classify asbestos as a cause of ovarian cancer. The use of asbestos was banned in the late 1990s in the US. Asbestos was widely used in:
- building industry
- shipbuilding
- manufacturing of household appliances
- motor industry
- power stations
- telephone exchanges
There are 3 main types of asbestos – blue, brown and white.
Asbestos is made up of tiny fibers. You can breathe these fibers in when you come into contact with asbestos.
Ovarian cancer signs and symptoms
Early-stage ovarian cancer rarely causes any symptoms. Advanced-stage ovarian cancer may cause few and nonspecific symptoms that are often mistaken for more common benign conditions.
Signs and symptoms of ovarian cancer may include:
- Abdominal bloating or swelling
- Quickly feeling full when eating
- Weight loss
- Discomfort in the pelvis area
- Changes in bowel habits, such as constipation
- A frequent need to urinate
These symptoms are also commonly caused by benign (non-cancerous) diseases and by cancers of other organs. When they are caused by ovarian cancer, they tend to be persistent and a change from normal − for example, they occur more often or are more severe. These symptoms are more likely to be caused by other conditions, and most of them occur just about as often in women who don’t have ovarian cancer. But if you have these symptoms more than 12 times a month, see your doctor so the problem can be found and treated if necessary.
Others symptoms of ovarian cancer can include:
- Fatigue (extreme tiredness)
- Upset stomach
- Back pain
- Pain during sex
- Constipation
- Changes in a woman’s period, such as heavier bleeding than normal or irregular bleeding
- Abdominal (belly) swelling with weight loss
Early symptoms of ovarian cancer
The symptoms of ovarian cancer can be difficult to recognize, particularly in the early stages of the disease. They are often the same as the symptoms of other, less serious, conditions, such as irritable bowel syndrome (IBS) or premenstrual syndrome (PMS). However, the most common symptoms that may indicate ovarian cancer are:
- abdominal bloating or feeling full
- abdominal or back pain
- appetite loss or feeling full quickly
- changes in toilet habits
- needing to urinate more often
- unexplained weight loss or weight gain
- indigestion or heartburn
- fatigue
- bleeding in-between periods or after menopause
- indigestion or nausea
- pain during intercourse
If any of these symptoms are unusual for you, and they persist, it’s important to see your doctor. Many of these symptoms may be the result of other conditions in the pelvic area.
If you have any of these symptoms, keep a symptom diary to see how many of these symptoms you have over a longer period. Bear in mind that ovarian cancer is rare in women under 40 years of age. If you regularly have any of these symptoms, talk to your doctor. It’s unlikely that they are being caused by a serious problem, but it’s best to be checked.
If you’ve already seen your doctor and the symptoms continue or get worse, it is important to go back and explain this, as you know your body better than anyone.
Can ovarian cancer be found early?
Only about 20% of ovarian cancers are found at an early stage. When ovarian cancer is found early, about 94% of patients live longer than 5 years after diagnosis.
The National Institute for Health and Care Excellence recommends that if you (especially if 50 or over) have the following symptoms on a persistent or frequent basis – particularly more than 12 times per month, your doctor should arrange tests – especially if you’re are over 50 76:
- persistent swollen tummy (abdomen) or bloating
- feeling full (early satiety) and/or loss of appetite
- pelvic or abdominal pain
- increased urinary urgency and/or frequency.
First tests:
- Measure serum cancer antigen 125 (CA125) in primary care in women with symptoms that suggest ovarian cancer
- If serum CA125 is 35 IU/ml or greater, arrange an ultrasound scan of the abdomen and pelvis.
- For any woman who has normal serum CA125 (less than 35 IU/ml), or CA125 of 35 IU/ml or greater but a normal ultrasound:
- assess her carefully for other clinical causes of her symptoms and investigate if appropriate
- if no other clinical cause is apparent, advise her to return to her doctor if her symptoms become more frequent and/or persistent.
Screening tests for ovarian cancer
Screening tests and exams are used to detect a disease, like cancer, in people who don’t have any symptoms. (For example, a mammogram can often detect breast cancer in its earliest stage, even before a doctor can feel the cancer.)
There has been a lot of research to develop a screening test for ovarian cancer, but there hasn’t been much success so far. The 2 tests used most often (in addition to a complete pelvic exam) to screen for ovarian cancer are transvaginal ultrasound (TVUS) and the CA-125 blood test.
- TVUS (transvaginal ultrasound) is a test that uses sound waves to look at the uterus, fallopian tubes, and ovaries by putting an ultrasound wand into the vagina. It can help find a mass (tumor) in the ovary, but it can’t actually tell if a mass is cancer or benign. When it is used for screening, most of the masses found are not cancer.
- CA-125 blood test measures the amount of a protein called CA-125 in your blood. Many women with ovarian cancer have high levels of CA-125. This test can be useful as a tumor marker to help guide treatment in women known to have ovarian cancer, because a high level often goes down if treatment is working. But checking CA-125 levels has not been found to be as useful as a screening test for ovarian cancer. The problem with using this test for ovarian cancer screening is that high levels of CA-125 is more often caused by common conditions such as endometriosis and pelvic inflammatory disease. Also, not everyone who has ovarian cancer has a high CA-125 level. When someone who is not known to have ovarian cancer has an abnormal CA-125 level, the doctor might repeat the test (to make sure the result is correct) and may consider ordering a transvaginal ultrasound test.
Better ways to screen for ovarian cancer are being researched but currently there are no reliable screening tests. Hopefully, improvements in screening tests will eventually lead to fewer deaths from ovarian cancer.
Ovarian cancer diagnosis
If your doctor finds something suspicious during a pelvic exam, or if you have symptoms that might be due to ovarian cancer, your doctor, will recommend exams and tests to find the cause.
Medical history and physical exam
Your doctor will ask about your medical history to learn about possible risk factors, including your family history. You will also be asked if you’re having any symptoms, when they started, and how long you’ve had them. Your doctor will likely do a pelvic exam to check for an enlarged ovary or signs of fluid in the abdomen (which is called ascites). During a pelvic exam, your doctor inserts gloved fingers into your vagina and simultaneously presses a hand on your abdomen in order to feel (palpate) your pelvic organs. The doctor also visually examines your external genitalia, vagina and cervix.
If there is reason to suspect you have ovarian cancer based on your symptoms and/or physical exam, your doctor will order some tests to check further.
Surgery
Sometimes your doctor can’t be certain of your diagnosis until you undergo surgery to remove an ovary and have it tested for signs of cancer.
Consultation with a specialist
If the results of your pelvic exam or other tests suggest that you have ovarian cancer, you will need a doctor or surgeon who specializes in treating women with this type of cancer. A gynecologic oncologist is an obstetrician/gynecologist who is specially trained in treating cancers of the female reproductive system. Treatment by a gynecologic oncologist helps ensure that you get the best kind of surgery for your cancer. It has also has been shown to help patients with ovarian cancer live longer. Anyone suspected of having ovarian cancer should see this type of specialist before having surgery.
Ovarian cancer tests
Imaging tests
Doctors use imaging tests to take pictures of the inside of your body. Imaging tests can show whether a pelvic mass is present, but they cannot confirm that the mass is a cancer. These tests are also useful if your doctor is looking to see if ovarian cancer has spread (metastasized) to other tissues and organs.
Ultrasound
Ultrasound (ultrasonography) uses sound waves to create an image on a video screen. Sound waves are released from a small probe placed in the woman’s vagina and a small microphone-like instrument called a transducer gives off sound waves and picks up the echoes as they bounce off organs. A computer turns these echoes into an image on the screen.
Ultrasound is often the first test done if a problem with the ovaries is suspected. It can be used to find an ovarian tumor and to check if it is a solid mass (tumor) or a fluid-filled cyst. It can also be used to get a better look at the ovary to see how big it is and how it looks inside. This helps the doctor decide which masses or cysts are more worrisome.
Computed tomography (CT) scans
The CT scan is an x-ray test that makes detailed cross-sectional images of your body. The test can help tell if ovarian cancer has spread to other organs.
CT scans do not show small ovarian tumors well, but they can see larger tumors, and may be able to see if the tumor is growing into nearby structures. A CT scan may also find enlarged lymph nodes, signs of cancer spread to liver or other organs, or signs that an ovarian tumor is affecting your kidneys or bladder.
CT scans are not usually used to biopsy an ovarian tumor (see biopsy in the section “Other tests”), but they can be used to biopsy a suspected metastasis (area of spread). For this procedure, called a CT-guided needle biopsy, the patient stays on the CT scanning table, while a radiologist moves a biopsy needle toward the mass. CT scans are repeated until the doctors are confident that the needle is in the mass. A fine needle biopsy sample (tiny fragment of tissue) or a core needle biopsy sample (a thin cylinder of tissue about ½ inch long and less than 1/8 inch in diameter) is removed and examined in the lab.
Barium enema x-ray
A barium enema is a test to see if the cancer has invaded the colon (large intestine) or rectum. This test is rarely used for women with ovarian cancer. Colonoscopy may be done instead.
Magnetic resonance imaging (MRI) scans
MRI scans also create cross-section pictures of your insides. But MRI uses strong magnets to make the images – not x-rays. A contrast material called gadolinium may be injected into a vein before the scan to see details better.
MRI scans are not used often to look for ovarian cancer, but they are particularly helpful to examine the brain and spinal cord where cancer could spread.
Chest x-ray
An x-ray might be done to determine whether ovarian cancer has spread (metastasized) to the lungs. This spread may cause one or more tumors in the lungs and more often causes fluid to collect around the lungs. This fluid, called a pleural effusion, can be seen with chest x-rays as well as other types of scans.
Positron emission tomography (PET) scan
For a PET scan, radioactive glucose (sugar) is given to look for the cancer. PET scans can help find cancer when it has spread, but are not used often to look for ovarian cancer. Body cells take in different amounts of the sugar, depending on how fast they are growing. Cancer cells, which grow quickly, are more likely to take up larger amounts of the sugar than normal cells. A special camera is used to create a picture of areas of radioactivity in the body.
The picture from a PET scan is not as detailed as a CT or MRI scan, but it provides helpful information about whether abnormal areas seen on these other tests are likely to be cancer or not.
If you have already been diagnosed with cancer, your doctor may use this test to see if the cancer has spread to lymph nodes or other parts of the body. A PET scan can also be useful if your doctor thinks the cancer may have spread but doesn’t know where.
PET/CT scan: Some machines can do both a PET and CT scan at the same time. This lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed picture of that area on the CT scan.
Other tests
Laparoscopy
This procedure uses a thin, lighted tube through which a doctor can look at the ovaries and other pelvic organs and tissues in the area. The tube is inserted through a small incision (cut) in the lower abdomen and sends the images of the pelvis or abdomen to a video monitor. Laparoscopy provides a view of organs that can help plan surgery or other treatments and can help doctors confirm the stage (how far the tumor has spread) of the cancer. Also, doctors can manipulate small instruments through the laparoscopic incision(s) to perform biopsies.
Colonoscopy
A colonoscopy is a way to examine the inside of the large intestine (colon). The doctor looks at the entire length of the colon and rectum with a colonoscope, a thin, flexible, lighted tube with a small video camera on the end. It is inserted through the anus and into the rectum and the colon. Any abnormal areas seen can by biopsied. This procedure is more commonly used to look for colorectal cancer.
Biopsy
The only way to determine for certain if a growth is cancer is to remove a piece of it and examine it in the lab. This procedure is called a biopsy. For ovarian cancer, the biopsy is most commonly done by removing the tumor during surgery.
In rare cases, a suspected ovarian cancer may be biopsied during a laparoscopy procedure or with a needle placed directly into the tumor through the skin of the abdomen. Usually the needle will be guided by either ultrasound or CT scan. This is only done if you cannot have surgery because of advanced cancer or some other serious medical condition, because there is concern that a biopsy could spread the cancer.
If you have ascites (fluid buildup inside the abdomen), samples of the fluid can also be used to diagnose the cancer. In this procedure, called paracentesis, the skin of the abdomen is numbed and a needle attached to a syringe is passed through the abdominal wall into the fluid in the abdominal cavity. Ultrasound may be used to guide the needle. The fluid is taken up into the syringe and then sent for analysis to see if it contains cancer cells.
In all these procedures, the tissue or fluid obtained is sent to the lab. There it is examined by a pathologist, a doctor who specialize in diagnosing and classifying diseases by examining cells under a microscope and using other lab tests.
Blood tests
Your doctor will order blood count tests to make sure you have enough red blood cells, white blood cells and platelets (cells that help stop bleeding). There will also be tests to measure your kidney and liver function as well as your general health. The doctor will also order a CA-125 test. Women who have a high CA-125 level are often referred to a gynecologic oncologist, but any woman with suspected ovarian cancer should see a gynecologic oncologist, as well.
Some germ cell cancers can cause elevated blood levels of the tumor markers human chorionic gonadotropin (HCG), alpha-fetoprotein (AFP), and/or lactate dehydrogenase (LDH). These may be checked if your doctor suspects that your ovarian tumor could be a germ cell tumor.
Some ovarian stromal tumors cause the blood levels of a substance called inhibin and hormones such as estrogen and testosterone to go up. These levels may be checked if your doctor suspects that you have this type of tumor.
Lab tests for gene or protein changes
In some ovarian cancers, doctors might look for specific gene or protein changes in the cancer cells that could mean certain targeted or immunotherapy drugs might help treat the cancer. These tests can be done on a piece of the cancer taken during a biopsy or surgery for ovarian cancer.
- BRCA1 and BRCA2 gene mutations: BRCA genes are normally involved in DNA repair, and mutations in these genes can cause cells to grow out of control and turn into cancer. Ovarian cancers with BRCA gene mutations are more likely to be helped by treatment with targeted drugs called PARP inhibitors.
- Folate receptor-alpha (FR-alpha) testing: In many ovarian cancers, the cells have high levels of the FR-alpha protein on their surfaces. Testing for FR-alpha levels can show if the cancer is more likely to respond to treatment with a targeted drug such as mirvetuximab soravtansine (Elahere).
- NTRK gene mutations: Some ovarian cancers might be tested for changes in one of the NTRK genes. Cells with these gene changes can lead to abnormal cell growth and cancer. Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek) are targeted drugs that stop the proteins made by the abnormal NTRK genes. The number of ovarian cancers that have this mutation is very small, but this may be an option for some women.
- MSI and MMR gene testing: Women who have clear cell, endometrioid, or mucinous ovarian cancer might have their tumor tested to see if it shows high levels of gene changes called microsatellite instability (MSI). Testing might also be done to see if the cancer cells have changes in any of the mismatch repair (MMR) genes (MLH1, MSH2, MSH6, and PMS2). Changes in MSI or in MMR genes (or both) are often seen in people with Lynch syndrome (HNPCC). Up to 10% of all ovarian epithelial cancers have changes in these genes.
There are 2 possible reasons to test ovarian cancers for MSI or for MMR gene changes:
- To identify patients who should be tested for Lynch syndrome. A diagnosis of Lynch syndrome can help determine if a person should have screenings for other types of cancer, such as endometrial or colon cancer. If a person does have Lynch syndrome, their relatives could also have it, and may want to be tested for it.
- To determine treatment options for ovarian cancer. Ovarian cancers that have certain MSI or MMR gene changes might be treated with certain immunotherapy drugs known as checkpoint inhibitors.
Ovarian cancer stages
After a woman is diagnosed with ovarian cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
Ovarian cancer stages range from stage I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV (4), means cancer has spread to distant areas of the body. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
One of the goals of surgery for ovarian cancer is to take tissue samples for diagnosis and staging. To stage the cancer, samples of tissues are taken from different parts of the pelvis and abdomen and examined in the lab.
How is ovarian cancer stage determined?
The 2 systems used for staging ovarian cancer, the FIGO (International Federation of Gynecology and Obstetrics) system and the AJCC (American Joint Committee on Cancer) TNM staging system are basically the same.
They both use 3 factors to stage (classify) ovarian cancer:
- The extent (size) of the tumor (T): Has the cancer spread outside the ovary or fallopian tube? Has the cancer reached nearby pelvic organs like the uterus or bladder?
- The spread to nearby lymph nodes (N): Has the cancer spread to the lymph nodes in the pelvis or around the aorta (the main artery that runs from the heart down along the back of the abdomen and pelvis)? Also called para-aortic lymph nodes.
- The spread (metastasis) to distant sites (M): Has the cancer spread to fluid around the lungs (malignant pleural effusion) or to distant organs such as the liver or bones?
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
The staging system in the table below uses the pathologic stage (also called the surgical stage). It is determined by examining tissue removed during an operation. This is also known as surgical staging. Sometimes, if surgery is not possible right away, the cancer will be given a clinical stage instead. This is based on the results of a physical exam, biopsy, and imaging tests done before surgery.
The system described below is the most recent American Joint Committee on Cancer (AJCC) system effective January 2018. It is the staging system for ovarian cancer, fallopian tube cancer, and primary peritoneal cancer.
Cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.
Table 2. Ovarian cancer stages
| AJCC Stage | Stage grouping | FIGO Stage | Stage description* |
|---|---|---|---|
| 1 | T1 N0 M0 | 1 | The cancer is only in the ovary (or ovaries) or fallopian tube(s) (T1). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 1A | T1a N0 M0 | 1A | The cancer is in one ovary, and the tumor is confined to the inside of the ovary; or the cancer is in in one fallopian tube, and is only inside the fallopian tube. There is no cancer on the outer surfaces of the ovary or fallopian tube. No cancer cells are found in the fluid (ascites) or washings from the abdomen and pelvis (T1a). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 1B | T1b N0 M0 | 1B | The cancer is in both ovaries or fallopian tubes but not on their outer surfaces. No cancer cells are found in the fluid (ascites) or washings from the abdomen and pelvis (T1b). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 1C | T1c N0 M0 | 1C | The cancer is in one or both ovaries or fallopian tubes and any of the following are present:
It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 2
| T2 N0 M0 | 2 | The cancer is in one or both ovaries or fallopian tubes and has spread to other organs (such as the uterus, bladder, the sigmoid colon, or the rectum) within the pelvis or there is primary peritoneal cancer (T2). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 2A | T2a N0 M0 | 2A | The cancer has spread to or has invaded (grown into) the uterus or the fallopian tubes, or the ovaries. (T2a). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 2B | T2b N0 M0 | 2B | The cancer is on the outer surface of or has grown into other nearby pelvic organs such as the bladder, the sigmoid colon, or the rectum (T2b). It has not spread to nearby lymph nodes (N0) or to distant sites (M0). |
| 3A1 | T1 or T2 N1 M0 | 3A1 | The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer (T1) and it may have spread or grown into nearby organs in the pelvis (T2). It has spread to the retroperitoneal (pelvic and/or para-aortic) lymph nodes only. It has not spread to distant sites (M0). |
| 3A2 | T3a N0 or N1 M0 | 3A2 | The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer and it has spread or grown into organs outside the pelvis. During surgery, no cancer is visible in the abdomen (outside of the pelvis) to the naked eye, but tiny deposits of cancer are found in the lining of the abdomen when it is examined in the lab (T3a). The cancer might or might not have spread to retroperitoneal lymph nodes (N0 or N1), but it has not spread to distant sites (M0). |
| 3B | T3b N0 or N1 M0 | 3B | There is cancer in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer and it has spread or grown into organs outside the pelvis. The deposits of cancer are large enough for the surgeon to see, but are no bigger than 2 cm (about 3/4 inch) across. (T3b). It may or may not have spread to the retroperitoneal lymph nodes (N0 or N1), but it has not spread to the inside of the liver or spleen or to distant sites (M0). |
| 3C | T3c N0 or N1 M0 | 3C | The cancer is in one or both ovaries or fallopian tubes, or there is primary peritoneal cancer and it has spread or grown into organs outside the pelvis. The deposits of cancer are larger than 2 cm (about 3/4 inch) across and may be on the outside (the capsule) of the liver or spleen (T3c). It may or may not have spread to the retroperitoneal lymph nodes (N0 or N1), but it has not spread to the inside of the liver or spleen or to distant sites (M0). |
| 4A | Any T Any N M1a | 4A | Cancer cells are found in the fluid around the lungs (called a malignant pleural effusion) with no other areas of cancer spread such as the liver, spleen, intestine, or lymph nodes outside the abdomen (M1a). |
| 4B | Any T Any N M1b | 4B | The cancer has spread to the inside of the spleen or liver, to lymph nodes other than the retroperitoneal lymph nodes, and/or to other organs or tissues outside the peritoneal cavity such as the lungs and bones (M1b). |
Footnotes:
* The following additional categories are not described in the table above:
- TX: Main tumor cannot be assessed due to lack of information
- T0: No evidence of a primary tumor.
- NX: Regional lymph nodes cannot be assessed due to lack of information.
Grades of ovarian cancer
The grade of a cancer tells you how much the cancer cells look like normal cells. It gives your doctor an idea of how the cancer might behave. As a normal cell grows and matures, it becomes specialized for its role and place in the body. This is called differentiation. Cancer cells can look like normal cells. They are described as well differentiated or low grade. These cancers are more likely to grow slowly. Cancer cells can also look underdeveloped and nothing like a normal cell. They are known as undifferentiated or high grade. These cancers tend to grow and spread more quickly than low grade cancers.
Doctors use different systems to grade ovarian cancer. It depends on your type of ovarian cancer.
- Doctors describe serous epithelial ovarian cancer as either high grade or low grade. This depends on how much the tumor cells look like normal tissue.
- Doctors describe other types of epithelial ovarian cancers as:
- Grade 1 or well differentiated
- Grade 2 or moderately differentiated
- Grade 3 or poorly differentiated (or undifferentiated)
Stage 1 ovarian cancer
Stage 1 ovarian cancer is only in the ovaries. Stage 1 ovarian cancer is divided into 3 groups:
- Stage 1A means the cancer is completely inside one ovary
- Stage 1B means the cancer is completely inside both ovaries
- Stage 1C is split in to 3 groups:
- Stage 1C1 means the cancer is in one or both ovaries and the ovary ruptures (bursts) during surgery
- Stage 1C2 means the cancer is in one or both ovaries and the ovary ruptures (bursts) before surgery or there is some cancer on the surface of an ovary
- Stage 1C3 means the cancer is in one or both ovaries and there are cancer cells in fluid taken from inside your abdomen during surgery
Figure 19. Stage 1 ovarian cancer
Stage 2 ovarian cancer
Stage 2 ovarian cancer means the cancer has grown outside the ovary or ovaries. And is growing within the area circled by your hip bones (the pelvis). There may also be cancer cells in the abdomen.
Stage 2 ovarian cancer is divided into 2 groups:
- Stage 2A means the cancer has grown into the fallopian tubes or the uterus
- Stage 2B means the cancer has grown into other tissues in the pelvis, for example the bladder or rectum
Figure 20. Stage 2 ovarian cancer
Stage 3 ovarian cancer
Stage 3 ovarian cancer means the cancer has spread outside the pelvis to the lining of your abdominal cavity (peritoneum). It can also spread to the lymph nodes in the back of your abdomen.
There are three groups of stage 3 ovarian cancer- 3A, 3B and 3C:
- Stage 3A has 2 groups:
- Stage 3A1 means the cancer has spread to the lymph nodes in the back of your abdomen
- Stage 3A2 means that the doctor finds cancer cells in tissue samples they take from the lining of your abdomen (peritoneum). And it might also be in your lymph nodes
- Stage 3B means there are cancer growths that are 2cm or smaller in size on the lining of your abdomen (peritoneum). And there might also be cancer in your lymph nodes.
- Stage 3C means there are cancer growths larger than 2cm on the lining of your abdomen (peritoneum). And there might also be cancer in your lymph nodes.
Figure 21. Stage 3 ovarian cancer
Stage 4 ovarian cancer
Stage 4 ovarian cancer means the cancer has spread to other body organs some distance away from the ovaries. Such as the liver or lungs.
Stage 4 ovarian cancer is divided into 2 groups:
- Stage 4A means the cancer has caused a build up of fluid in the lining of the lungs (called the pleura). This is called a pleural effusion.
- Stage 4B means the cancer has spread to:
- the inside of the liver or spleen
- lymph nodes outside the abdomen
- other organs such as the lungs
Figure 22. Stage 4 ovarian cancer
Ovarian cancer treatment
The main treatments for ovarian cancer are surgery and chemotherapy. Less often, treatment may include radiotherapy. Ovarian cancer treatment is usually managed by a gynecological oncologist as they specialize in treating cancers of the reproductive tract and have very specialized surgical skills. Ideally, they will be part of a multidisciplinary health care team – where each member of the team specializes in a different area of care and that care is co-ordinated between each member.
The type of treatment women receive depends on the type and stage of their ovarian cancer and their general health.
Almost all women with ovarian cancer will need surgery. The amount and type of surgery you have will depend on your stage and type of cancer.
For some women with very early stage ovarian cancer, surgery is the only treatment you need.
Most women with ovarian cancer are diagnosed with advanced disease and have a combination of both surgery and chemotherapy. You may have chemotherapy after surgery, or both before and after surgery.
Some women with ovarian cancer might have:
- Targeted cancer drugs
- Hormone therapy
- Radiotherapy (radiation therapy)
Surgery
Surgery to remove ovarian cancer include:
- Surgery to remove one ovary. For very early stage cancer that hasn’t spread beyond one ovary, surgery may involve removing the affected ovary and its fallopian tube. This procedure may preserve your ability to have children.
- Surgery to remove both ovaries. If cancer is present in both your ovaries, but there are no signs of additional cancer, your surgeon may remove both ovaries and both fallopian tubes. This procedure leaves your uterus intact, so you may still be able to become pregnant using your own frozen embryos or eggs or with eggs from a donor.
- Surgery to remove both ovaries and the uterus. If your cancer is more extensive or if you don’t wish to preserve your ability to have children, your surgeon will remove the ovaries, the fallopian tubes, the uterus, nearby lymph nodes and a fold of fatty abdominal tissue (omentum). This operation is called a total abdominal hysterectomy (TAH) and bilateral salpingo-oophorectomy (BSO). If the omentum is also removed (an omentectomy).
- Surgery for advanced cancer. If your cancer is advanced, your doctor may recommend chemotherapy followed by surgery to remove as much of the cancer as possible.
The first treatment for ovarian cancer is usually an operation called a ‘laparotomy’. This operation is also the main way that a diagnosis of ovarian cancer is confirmed.
During a laparotomy, a long vertical cut is made in your abdomen, which allows the surgeon to find and remove as much of the tumor as possible. In many cases, the surgeon will do a biopsy of the tumor at the beginning of the operation to confirm that it is cancer. This is called a ‘frozen section’. If the frozen section confirms that the tumor is cancer, the operation will continue.
To know where the ovarian cancer is in your body to remove it, the surgeon typically uses the imaging tests done before surgery as well as a bright light and feeling for the tumors during the operation. Still, some tumors that are not easily seen or felt by hand might be missed. To help find these tumors, intraoperative imaging might be used. This approach uses a special imaging system in the operating room during the surgery. A fluorescent drug called pafolacianine (Cytalux) will be injected into your blood a few hours before surgery. The drug travels through the body and attaches to a specific protein found on ovarian cancer cells. During surgery, the imaging system gives off near-infrared fluorescent light that will cause the drug to light up so the surgeon can see which areas need to be removed. The most common side effects from pafolacianine (Cytalux) are belly pain, heartburn, itching, chest pain, nausea, vomiting, and flushing. Your doctor will probably ask you to avoid taking any supplements that have folic acid in them for a few days before the procedure so they don’t disturb the test.
For most women, the operation will involve removal of the ovaries, fallopian tubes, the uterus, the omentum (the fat pad around the organs in your abdomen), the appendix and some of the lymph glands in the area. Sometimes it may be necessary to remove some of the bowel.
After your operation, samples of the tissue removed are sent to a laboratory for further examination. The results of these biopsies will provide more information about the type and extent of your cancer and enables the gynecological oncologist to make decisions about further treatment.
If you were still having menstrual periods before you were diagnosed with ovarian cancer and you have both your ovaries removed, this surgery will result in menopause and can affect your ability to have children. As well as learning that you have ovarian cancer, this surgically-induced menopause and infertility creates all kinds of extra challenges to live with. It’s important for women who have not yet completed their family to speak to a doctor about these issues before surgery.
Staging epithelial ovarian cancer
The first goal of ovarian cancer surgery is to stage your ovarian cancer − to see how far the cancer has spread from the ovary. Usually this means removing the uterus (this operation is called a hysterectomy), along with both ovaries and fallopian tubes (this is called a bilateral salpingo-oophorectomy or BSO). In addition, the omentum is also removed (an omentectomy). The omentum is a layer of fatty tissue that covers the abdominal contents like an apron, and ovarian cancer sometimes spreads to this area. Some lymph nodes in the pelvis and abdomen might also be biopsied (taken out to see if the cancer has spread from the ovary).
If there is fluid in the pelvis or abdominal cavity, it will be removed for testing. The surgeon may “wash” the abdominal cavity with salt water (saline) and send that fluid to the lab for testing. Biopsies may also be taken from different areas inside the abdomen and pelvis. All the tissue and fluid samples taken during the operation are sent to a lab to look for cancer cells. Staging is very important because ovarian cancers at different stages are treated differently. If the staging isn’t done correctly, the doctor may not be able to decide on the best treatment.
Intraoperative imaging
To know where the ovarian cancer is in your body to remove it, the surgeon typically uses the imaging tests done before surgery as well as a bright light and feeling for the tumors during the operation. Still, some tumors that are not easily seen or felt by hand might be missed. To help find these tumors, intraoperative imaging might be used.
This approach uses a special imaging system in the operating room during the surgery. A fluorescent drug called pafolacianine (Cytalux) will be injected into your blood a few hours before surgery. The drug travels through the body and attaches to a specific protein found on ovarian cancer cells. During surgery, the imaging system gives off near-infrared fluorescent light that will cause the drug to light up so the surgeon can see which areas need to be removed.
The most common side effects from pafolacianine (Cytalux) are belly pain, heartburn, itching, chest pain, nausea, vomiting, and flushing.
Your doctor will probably ask you to avoid taking any supplements that have folic acid in them for a few days before the procedure so they don’t disturb the test.
Debulking epithelial ovarian cancer
The other important goal of ovarian cancer surgery is to remove as much of the tumor as possible − this is called debulking. Debulking is very important when ovarian cancer has already spread throughout the abdomen (belly) at the time of surgery. The aim of debulking surgery is to leave behind no visible cancer or no tumors larger than 1 cm (less than 1/2 an inch). This is called optimally debulked. Patients whose tumors have been optimally debulked, have a better outlook (prognosis) than those left with larger tumors after surgery (called sub-optimally debulked).
In some cases, other organs might be affected by debulking:
- Sometimes the surgeon will need to remove a piece of colon to debulk the cancer properly. In some cases, a piece of colon is removed and then the 2 ends that remain are sewn back together. In other cases, though, the ends can’t be sewn back together right away. Instead, the top end of the colon is attached to an opening (stoma) in the skin of the abdomen to allow body wastes to get out. This is known as a colostomy. Most often, this is only temporary, and the ends of the colon can be reattached later in another operation.
- Sometimes, a part of the small intestine may need to be removed. Just like with the colon, the small intestine can either be reconnected (which is most common) or an ileostomy might be made. This is usually temporary, but will need special care, so ask your doctor if this is a possibility before having surgery.
- Debulking surgery might also mean removing a piece of the bladder. If this happens, a catheter (to empty the bladder) will be placed during surgery. This will be left in place until the bladder recovers enough to be able to empty on its own. Then, the catheter can be removed.
- Debulking might also require removing the spleen and/or the gallbladder, as well as part of the stomach, liver, and/or pancreas.
If both ovaries and/or the uterus are removed, you will not be able to become pregnant. It also means that you will go into menopause if you haven’t done so already. Most women will stay in the hospital for 3 to 7 days after the operation and can resume their usual activities within 4 to 6 weeks.
Surgery for ovarian germ cell tumors and ovarian stromal tumors
For germ cell tumors and stromal tumors, the main goal of surgery is to remove the cancer. Most ovarian germ cell tumors are treated with a hysterectomy and bilateral salpingo-oophorectomy (BSO). If the cancer is in only one ovary and you still want to be able to have children, only the ovary containing the cancer and the fallopian tube on the same side are removed (leaving behind the other ovary and fallopian tube and the uterus).
Ovarian stromal tumors are often confined to just one ovary, so surgery may just remove that ovary. If the cancer has spread, more tissue may need to be removed. This could mean a hysterectomy and bilateral salpingo-oophorectomy and even debulking surgery.
Sometimes, after child bearing is finished, surgery to remove the other ovary, the other fallopian tube, and the uterus may be recommended, for both germ cell and stromal ovarian tumors.
Chemotherapy
Chemotherapy also called chemo is a drug treatment that uses chemicals to kill fast-growing cells in the body, including cancer cells. Chemotherapy drugs can be injected into a vein or taken by mouth. Sometimes the drugs are injected directly into the abdomen (intraperitoneal chemotherapy).
Chemotherapy is often used after surgery to kill any cancer cells that might remain. It can also be used before surgery.
In certain situations, chemotherapy drugs may be heated and infused into the abdomen during surgery (hyperthermic intraperitoneal chemotherapy). The drugs are left in place for a certain amount of time before they’re drained. Then the operation is completed.
Chemo drugs can cause side effects. These depend on the type and dose of drugs given, and the length of treatment. Some of the most common possible side effects include:
- Nausea and vomiting
- Loss of appetite
- Loss of hair
- Hand and foot rashes
- Mouth sores
Chemotherapy can also affect the blood-forming cells of the bone marrow, which can lead to:
- Increased chance of infections (from low white blood cell counts, also called leukopenia)
- Easy bruising or bleeding (from low blood platelet counts. also called thrombocytopenia)
- Fatigue (from low red blood cell counts and other reasons, also called anemia)
These side effects usually go away after treatment is finished. While you are in treatment, tell your cancer care team about any side effects you are having. There are often ways to lessen these side effects. For example, drugs can be given to help prevent or reduce nausea and vomiting.
Some chemo drugs may have long-term or even permanent side effects:
- Cisplatin can cause kidney damage. To help prevent this, doctors give lots of IV fluid before and after this drug is given.
- Both cisplatin and the taxanes can cause nerve damage (called neuropathy). This can lead to problems with numbness, tingling, or even pain in the hands and feet.
- Cisplatin can also damage the nerves to the ear, which can lead to hearing loss (called ototoxicity).
- Chemo can also cause early menopause and infertility (being unable to become pregnant), which may be permanent. This is rarely an issue in the treatment of epithelial ovarian cancer, since most women have both ovaries removed as a part of treatment.
- Rarely, some chemo drugs can permanently damage bone marrow. This can later cause a bone marrow cancer such as myelodysplastic syndrome or even acute myeloid leukemia. This is called a second cancer. Your health care team knows which drugs can cause this problem and will discuss this possibility with you. Their positive effects against ovarian cancer offset the small chance that any of these drugs will cause another cancer.
- Ifosfamide can cause irritation and bleeding of the bladder lining (hemorrhagic cystitis). This can usually be prevented by giving the drug mesna with the ifosfamide.
Other drugs can have other side effects, so ask your doctor what side effects to expect from the drugs that you will receive. Most side effects improve once treatment is stopped, but some can last a long time and may never go away completely.
Chemotherapy for epithelial ovarian cancer
Chemo for ovarian cancer usually involves getting two different types of drugs together. Getting a combination of drugs instead of just one drug alone seems to work better as a first treatment for ovarian cancer. Usually, the combination includes a type of chemo drug called a platinum compound (usually cisplatin or carboplatin), and another type of chemo drug called a taxane, such as paclitaxel (Taxol®) or docetaxel (Taxotere®). These drugs are usually given as an IV (put into a vein) every 3 to 4 weeks.
The typical course of chemo for epithelial ovarian cancer involves 3 to 6 cycles of treatment, depending on the stage and type of ovarian cancer. A cycle is a schedule of regular doses of a drug, followed by a rest period. Different drugs have varying cycles; your doctor will let you know what schedule is planned for your chemo.
Epithelial ovarian cancer often shrinks or even seems to go away with chemo, but the cancer cells may eventually begin to grow again. If the first chemo seemed to work well and the cancer stayed away for at least 6 to 12 months, it can be treated with the same chemotherapy used the first time. In some cases, different drugs may be used.
Some of the other chemo drugs that are helpful in treating ovarian cancer include:
- Albumin bound paclitaxel (nab-paclitaxel, Abraxane®)
- Altretamine (Hexalen®)
- Capecitabine (Xeloda®)
- Cyclophosphamide (Cytoxan®)
- Etoposide (VP-16)
- Gemcitabine (Gemzar®)
- Ifosfamide (Ifex®)
- Irinotecan (CPT-11, Camptosar®)
- Liposomal doxorubicin (Doxil®)
- Melphalan
- Pemetrexed (Alimta®)
- Topotecan
- Vinorelbine (Navelbine®)
Intraperitoneal chemotherapy
For women who have stage 3 ovarian cancer (cancer that has not spread outside the abdomen) and whose cancers were optimally debulked (no tumors larger than 1 cm after surgery), intraperitoneal (IP) chemotherapy might be given in addition to systemic chemo (paclitaxel given in a vein).
In intraperitoneal (IP) chemotherapy, the drugs cisplatin and paclitaxel are injected into the abdominal cavity through a catheter (thin tube). The tube can be placed during the staging/debulking surgery, but sometimes it is placed later. If it is done later, it can be placed by a surgeon using laparoscopy, or by an interventional radiologist under x-ray guidance. The catheter is usually connected to a port, a half dollar-sized disk topped with a pliable diaphragm. The port is placed under the skin against a bony structure of the abdominal wall, such as a rib or pelvic bone. A needle can be placed through the skin and into the port to give chemo and other drugs. Over time, problems may occur with the catheter (for example, it might become plugged or infected), but this is rare.
Giving chemo this way gives the most concentrated dose of the drugs directly to the cancer cells in the abdominal cavity. This chemo also gets absorbed into the bloodstream and so can reach cancer cells outside the abdominal cavity. Intraperitoneal (IP) chemotherapy seems to help some women live longer than intravenous (IV) chemo alone, but the side effects are often more severe. Women getting intraperitoneal (IP) chemotherapy might have more abdominal pain, nausea, vomiting, and other side effects, which might make some women stop their treatment early. The risk of side effects also means a woman must have normal kidney function and be in good overall heath before starting intraperitoneal (IP) chemotherapy. Women also cannot have a lot of adhesions or scar tissue inside their abdomen (belly) because this can keep the chemo from reaching all the exposed cancer cells.
Chemotherapy for germ cell tumors
If you have a germ cell tumor, you will likely be treated with combination chemo (several different drugs at once). The combination used most often is called BEP, and includes the chemotherapy drugs bleomycin, etoposide and cisplatin (Platinol). If the cancer is a dysgerminoma, these are usually very sensitive to chemotherapy, and can sometimes be treated with the less toxic combination of carboplatin and etoposide. Other drug combinations may be used if the cancer isn’t responding to treatment or to treat cancer that has recurred (come back). These include:
- High dose chemotherapy (the exact drugs used can vary depending on what cancer center is giving the treatment)
- TIP (paclitaxel/Taxol, ifosfamide, and cisplatin/Platinol)
- VeIP (vinblastine, ifosfamide, and cisplatin/Platinol)
- VIP (etoposide/VP-16, ifosfamide, and cisplatin/Platinol)
- VAC (vincristine, dactinomycin, and cyclophosphamide)
Chemotherapy for stromal tumors
Ovarian stromal tumors are not often treated with chemotherapy, but when they are, the combination of carboplatin plus paclitaxel or PEB (cisplatin/Platinol, etoposide, and bleomycin) is used most often.
Targeted Drug Therapy for Ovarian Cancer
Targeted therapy is a type of cancer treatment that uses drugs that target the specific weaknesses present within your cancer cells. By attacking these weaknesses, targeted drug treatments can cause cancer cells to die. Each type of targeted therapy works differently, but they all change the way a cancer cell grows, divides, repairs itself, or interacts with other cells.
Targeted therapy drugs are usually reserved for treating ovarian cancer that returns after initial treatment or cancer that resists other treatments. Your doctor may test your cancer cells to determine which targeted therapy is most likely to have an effect on your cancer.
Targeted therapy is an active area of cancer research. Many clinical trials are testing new targeted therapies.
Bevacizumab
Bevacizumab (Avastin, other names) belongs to a class of drugs called angiogenesis inhibitors. For cancers to grow and spread, they need to make new blood vessels to nourish themselves (called angiogenesis). This drug attaches to a protein called VEGF (that signals new blood vessels to form) and slows or stops cancer growth. Bevacizumab is given as an infusion into the vein (IV) every 2 to 3 weeks.
Bevacizumab has been shown to shrink or slow the growth of advanced epithelial ovarian cancers. Bevacizumab appears to work even better when given along with chemotherapy having shown good results in terms of shrinking (or stopping the growth of) tumors. But it doesn’t seem to help women live longer.
Bevacizumab can also be given with olaparib as maintenance treatment in women whose cancers have a BRCA gene mutation or genomic instability (see below) and have shrunk quite a bit with chemotherapy containing carboplatin or cisplatin.
Side effects of bevacizumab
- Common side effects can include high blood pressure, tiredness, bleeding, low white blood cell counts, headaches, mouth sores, loss of appetite, and diarrhea.
- Rare but possibly serious side effects can include blood clots, severe bleeding, slow wound healing, holes forming in the colon (called perforations), and the formation of abnormal connections between the bowel and the skin or bladder (fistulas). If a perforation or fistula occurs it can lead to severe infection and may require surgery to correct.
PARP inhibitors
Olaparib (Lynparza), rucaparib (Rubraca), and niraparib (Zejula) are drugs known as a PARP (poly(ADP)-ribose polymerase) inhibitors. PARP enzymes normally help repair damaged DNA inside cells. The proteins made by the BRCA genes (BRCA1 and BRCA2) also normally help repair DNA, but in a different way. Mutations in BRCA genes can make it hard for a cell to repair its DNA. PARP inhibitors can make it even harder for tumor cells with an abnormal BRCA gene to repair damaged DNA, which often leads to the death of these cells. All of these drugs are taken daily by mouth, as pills or capsules.
If you are not known to have a BRCA mutation, your doctor might test your blood or saliva and your tumor to be sure you have one before starting treatment with one of these drugs.
PARP inhibitors have been shown to help shrink or slow the growth of some advanced ovarian cancers for a time. So far, though, it’s not clear if they can help women live longer.
Olaparib (Lynparza) is used to treat advanced ovarian cancer, typically after chemotherapy has been tried. This drug can be used in patients with or without mutations in one of the BRCA genes.
- In women with a BRCA mutation:
- Olaparib can be used as maintenance treatment for advanced ovarian cancer that has gotten smaller in response to first treatment with chemotherapy containing cisplatin or carboplatin.
- Olaparib can be used with bevacizumab (see above) as maintenance treatment in women whose cancers have shrunk quite a bit with chemotherapy containing carboplatin or cisplatin.
- In women without a BRCA mutation:
- If the tumor has a high genomic instability score (a test measuring the amount of abnormal genes in cancer cells), olaparib can be used with bevacizumab as maintenance treatment in women whose cancers have shrunk quite a bit with chemotherapy containing carboplatin or cisplatin.
- In women with or without a BRCA mutation:
- Olaparib can be used as maintenance treatment for advanced ovarian cancer that has come back after treatment, and then has shrunk in response to chemotherapy containing cisplatin or carboplatin.
Niraparib (Zejula) may be used in some situations to treat ovarian cancer.
- In women with or without a BRCA gene mutation:
- Niraparib might be used as maintenance treatment for advanced ovarian cancer, where the cancer has shrunk with first-line chemotherapy containing cisplatin or carboplatin.
- In women with a BRCA gene mutation:
- Niraparib might be used as maintenance treatment for advanced ovarian cancer that has come back after treatment, where the cancer has then shrunk with chemotherapy containing cisplatin or carboplatin.
Rucaparib (Rubraca) can be used in women with or without a BRCA mutation, as maintenance treatment for advanced ovarian cancer that has come back after treatment, and then has shrunk in response to chemotherapy containing cisplatin or carboplatin.
Side effects of PARP inhibitors
- Side effects of these drugs can include nausea, vomiting, diarrhea, fatigue, loss of appetite, taste changes, low red blood cell counts (anemia), belly pain, and muscle and joint pain.
- Rarely, some patients treated with these drugs have developed a blood cancer, such as myelodysplastic syndrome or acute myeloid leukemia.
Drugs that target folate receptor-alpha
In many ovarian cancers, the cells have high levels of the folate receptor-alpha (FR-alpha) protein on their surfaces. Drugs that target this protein might be an option to treat these cancers.
Mirvetuximab soravtansine (Elahere) is an antibody-drug conjugate (ADC), which is a lab-made antibody linked to a chemotherapy drug. Once it’s in the body, the antibody acts like a homing device by attaching to the folate receptor-alpha protein on cancer cells, which brings the chemo directly to them. Mirvetuximab soravtansine (Elahere) can be used to treat epithelial ovarian cancer that tests positive for folate receptor-alpha and that is no longer responding to platinum chemotherapy drugs such as cisplatin or carboplatin.
Mirvetuximab soravtansine is infused into a vein (through an IV line or central venous catheter), typically once every 3 weeks. Before each treatment, you’ll get medicines to help prevent infusion reactions, nausea, and vomiting.
Side effects of mirvetuximab soravtansine:
- Common side effects of this drug can include nausea and vomiting, diarrhea or constipation, feeling tired, belly pain, low blood cell counts, and changes in mineral levels in the blood.
- Mirvetuximab soravtansine can cause eye problems, which can sometimes be serious. Problems can include blurred vision, dry eyes, light sensitivity, eye pain, or vision changes. You’ll need an eye exam before being treated with this drug, and your doctor will prescribe eye drops for you to use before and during your treatment. Tell your doctor or nurse right away if you develop any eye problems.
- Mirvetuximab soravtansine can cause serious lung disease in some people, which might even be life threatening. It’s very important to let your doctor or nurse know right away if you’re having symptoms such as coughing, trouble breathing, or chest pain.
- Mirvetuximab soravtansine can also cause nerve damage (peripheral neuropathy), which can lead to numbness, tingling, or weakness in the hands or feet.
Drugs that target cells with NTRK gene changes
A very small number of ovarian cancers have changes in one of the NTRK genes. Cells with these gene changes can lead to abnormal cell growth and cancer. Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek) are targeted drugs that stop the proteins made by the abnormal NTRK genes. These drugs can be used in people with advanced ovarian cancer whose tumor has an NTRK gene change and is still growing despite other treatments. Larotrectinib (Vitrakvi) and entrectinib (Rozlytrek) are taken as pills, once or twice a day.
Side effects of drugs that target NTRK gene changes:
- Common side effects can include dizziness, fatigue, nausea, vomiting, constipation, weight gain, and diarrhea.
- Less common but serious side effects can include abnormal liver tests, heart problems, and confusion.
Radiotherapy
Radiotherapy is occasionally used as a treatment option for ovarian cancer. Radiotherapy may be used where cancer is confined to the pelvic cavity. It may also be used in advanced ovarian cancer to reduce the size of the cancer and help to relieve symptoms. Radiotherapy is treatment with special X-rays that are aimed at the specific site of the cancer. The X-ray damages the DNA or genetic code in the cancer cells and this damage kills the cancer cells when they try to grow. Treatment can be external or internal and is given daily over a number of weeks.
External beam radiation therapy
This is the most common type of radiation therapy for women with ovarian cancer. External radiation therapy is much like getting an x-ray, but the radiation is stronger. A machine focuses the radiation on the area affected by the cancer. The procedure itself is painless. Each treatment lasts only a few minutes, but the setup time—getting you into place for treatment—usually takes longer. Treatments are given 5 days a week for several weeks.
Some common side effects include:
- Skin changes – the skin in the treated area may look and feel sunburned or even blister and peel
- Fatigue (tiredness)
- Nausea and vomiting
- Diarrhea
- Vaginal irritation, sometimes with a discharge (if the pelvis is being treated)
These side effects improve after treatment is stopped. Skin changes gradually fade, and the skin returns to normal in 6 to 12 months.
If you are having side effects from radiation, tell your cancer care team. There may be ways to manage them.
Brachytherapy
Brachytherapy, also known as internal radiation, is another way to deliver radiation therapy. Instead of aiming radiation beams from outside the body, a device containing radioactive seeds or pellets is placed inside the body, near the cancer. This is rarely done for ovarian cancer.
Hormone therapy
Hormone therapy uses drugs to block the effects of the hormone estrogen on ovarian cancer cells. Some ovarian cancer cells use estrogen to help them grow, so blocking estrogen may help control the cancer. Hormone therapy might be a treatment option for some types of slow-growing ovarian cancers. It may also be an option if the cancer comes back after initial treatments.
Luteinizing-hormone-releasing hormone (LHRH) agonists
Luteinizing-hormone-releasing hormone (LHRH) agonists sometimes called GnRH agonists, switch off estrogen production by the ovaries. These drugs are used to lower estrogen levels in women who are premenopausal. Examples of LHRH agonists include goserelin (Zoladex®) and leuprolide (Lupron®). These drugs are injected every 1 to 3 months. Side effects can include any of the symptoms of menopause, such as hot flashes and vaginal dryness. If they are taken for a long time (years), these drugs can weaken bones (sometimes leading to osteoporosis).
Tamoxifen
Tamoxifen is a drug that is often used to treat breast cancer. It can also be used to treat ovarian stromal tumors and is rarely used to treat advanced epithelial ovarian cancer. Tamoxifen acts as an anti-estrogen in many tissues in the body, but as a weak estrogen in others. The goal of tamoxifen therapy is to keep any estrogens circulating in the woman’s body from stimulating cancer cell growth. The anti-estrogen activity of this drug can lead to side effects like hot flashes and vaginal dryness. Because tamoxifen acts like a weak estrogen in some areas of the body, it does not cause bone loss but can increase the risk of serious blood clots in the legs.
Aromatase inhibitors
Aromatase inhibitors are drugs that block an enzyme (called aromatase) that turns other hormones into estrogen in post-menopausal women. They don’t stop the ovaries from making estrogen, so they are only helpful in lowering estrogen levels in women after menopause. These drugs are mainly used to treat breast cancer, but can also be used to treat some ovarian stromal tumors that have come back after treatment as well as low grade serous carcinomas. They include letrozole (Femara®), anastrozole (Arimidex®), and exemestane (Aromasin®). These drugs are taken as pills once a day.
Common side effects of aromatase inhibitors include hot flashes, joint and muscle pain, and bone thinning. The bone thinning can lead to osteoporosis and bones that break easily.
Immunotherapy
Immunotherapy is the use of medicines to stimulate your body’s immune system to recognize and destroy cancer cells more effectively. Your body’s disease-fighting immune system may not attack cancer cells because they produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process. Immunotherapy might be an option for treating ovarian cancer in certain situations.
Immune checkpoint inhibitors
An important part of the immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses “checkpoints” – proteins on immune cells that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system. But drugs that target these checkpoints can be used to treat some people with ovarian cancer.
Pembrolizumab (Keytruda) targets PD-1, a protein on certain immune cells (called T cells) that normally helps keep these cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth. Pembrolizumab can be used in people with certain types of advanced ovarian cancer that have high levels of MSI or changes in the MMR genes whose cancer starts growing after chemotherapy or other drug treatments.
Pembrolizumab (Keytruda) immunotherapy drug is given as an intravenous (IV) infusion every 3 weeks.
Possible side effects of immunotherapy
- Side effects of these drugs can include fatigue, cough, nausea, itching, skin rash, loss of appetite, constipation, joint pain, and diarrhea. Other, more serious side effects occur less often.
- Infusion reactions: Some people might have an infusion reaction while getting these drugs. This is like an allergic reaction, and can include fever, chills, flushing of the face, rash, itchy skin, feeling dizzy, wheezing, and trouble breathing. It’s important to tell your doctor or nurse right away if you have any of these symptoms while getting these drugs.
- Autoimmune reactions: These drugs work by basically removing one of the safeguards on the body’s immune system. Sometimes the immune system starts attacking other parts of the body, which can cause serious or even life-threatening problems in the lungs, intestines, liver, hormone-making glands, kidneys, or other organs.
It’s very important to report any new side effects to your cancer care team as soon as possible. If serious side effects do occur, treatment may need to be stopped and you may get high doses of corticosteroids to suppress your immune system.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery and chemotherapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Ovarian cancer treatment and fertility
Treatment for ovarian cancer can affect a woman’s ability to have children. If a woman who has not yet gone through menopause has both ovaries removed, she will no longer be able to have children naturally after treatment. If surgery involves removing the uterus, the woman will no longer be able to have children at all.
If ovarian cancer has not spread or if it’s found to be a borderline tumor (a type of less aggressive ovarian cancer), it may be possible to just remove only the affected ovary, leaving the other ovary and the uterus. This means that a woman may still fall pregnant after surgery.
Some women need chemotherapy following surgery. When an ovary remains after surgery, having chemotherapy can mean that a woman goes through menopause early. Women who have gone through menopause are no longer able to become pregnant.
Women who were planning to have children before their ovarian cancer diagnosis should speak to their oncologist before starting treatment for ovarian cancer. It may be possible to see a fertility specialist to discuss the available options.
Ovarian cancer prognosis
The prognosis of ovarian cancer is directly dependent on the disease stage at the time of diagnosis 120. It is also significantly associated with baseline performance status, FIGO (International Federation of Gynecology and Obstetrics) system and the AJCC (American Joint Committee on Cancer) TNM stage, and volume of residual disease post-primary cytoreductive surgery. Ovarian cancer 5 year relative survival is 49.7% 117. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
In women with a disease that spread to adjacent tissues, 5-year survival rates drop down to 80% and 25% for the ones with metastatic disease 121. Patients with recurrent disease can be treated. However, they are usually incurable. Recurrent platinum-sensitive ovarian cancer median survival is approximately 3 years; however, it is about just 1 year for platinum-resistant patients 122, 123.
Most of these patients with ovarian cancer develop malignant bowel obstruction in the late-stage, which is quite difficult to manage. Palliative symptom management is the mainstay in such patients. Debulking surgery is the strongest predictor of prognosis, where the volume of residual disease post-surgery is directly correlated to overall survival and progression-free survival 124.
Figure 23. Ovarian cancer 5 year relative survival
[Source SEER 17 2012–2018 117 ]Ovarian cancer survival rate
Survival rates tell you what percentage of people with the same type and stage of cancer are still alive a certain length of time (usually 5 years) after they were diagnosed. These numbers can’t tell you how long you will live, but they may help give you a better understanding about how likely it is that your treatment will be successful.
Remember, survival rates are estimates – your outlook can vary based on a number of factors specific to you.
Survival rates are often based on previous outcomes of large numbers of people who had the disease, but they can’t predict what will happen in any particular person’s case. There are a number of limitations to remember:
- The numbers below are among the most current available. But to get 5-year survival rates, doctors look at people who were treated at least 5 years ago. As treatments are improving over time, people who are now being diagnosed with ovarian cancer may have a better outlook than these statistics show.
- These statistics are based on the stage of the cancer when it was first diagnosed. They do not apply to cancers that come back later or spread, for example.
- Besides the cancer stage, many other factors can affect a person’s outlook, such as age and overall health, and how well the cancer responds to treatment.
Your doctor can tell you how these numbers may apply to you, as he or she is familiar with the aspects of your particular situation.
The Surveillance, Epidemiology, and End Results (SEER) from the National Cancer Institute database tracks 5-year relative survival rates for ovarian cancer in the United States, based on how far the cancer has spread. The SEER database, however, does not group cancers by AJCC or FIGO stages (stage 1, stage 2, stage 3, etc.). Instead, it groups cancers into localized, regional, and distant stages:
- Localized: There is no sign that the cancer has spread outside of the ovaries.
- Regional: The cancer has spread outside the ovaries to nearby structures or lymph nodes.
- Distant: The cancer has spread to distant parts of the body, such as the liver or lungs.
For all types of ovarian cancer, the 5-year relative survival is 49.7% 117. The 5-year relative survival for localized ovarian cancer is 93.1% 117.
The survival rates given below are for the different types of ovarian cancer. They come from the National Cancer Institute, SEER Database and are based on patients diagnosed with cancers of the ovary (or fallopian tube) between 2011 to 2017. These survival rates differ based on the type of ovarian cancer (invasive epithelial, stromal, or germ cell tumor).
- These numbers apply only to the stage of the cancer when it is first diagnosed. They do not apply later on if the cancer grows, spreads, or comes back after treatment.
- These numbers don’t take everything into account. Survival rates are grouped based on how far the cancer has spread. But other factors, such as your age and overall health, and how well the cancer responds to treatment, can also affect your outlook.
- People now being diagnosed with ovarian (or fallopian tube) cancer may have a better outlook than these numbers show. Treatments improve over time, and these numbers are based on people who were diagnosed and treated at least five years earlier.
Table 3. Invasive epithelial ovarian cancer survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 93% |
| Regional | 75% |
| Distant | 31% |
| All SEER stages combined | 49% |
Table 4. Ovarian stromal tumors survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 97% |
| Regional | 90% |
| Distant | 70% |
| All SEER stages combined | 90% |
Table 5. Germ cell tumors of the ovary survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 98% |
| Regional | 94% |
| Distant | 74% |
| All SEER stages combined | 93% |
Table 6. Fallopian tube carcinoma survival rate
| SEER stage | 5-year relative survival rate |
|---|---|
| Localized | 95% |
| Regional | 54% |
| Distant | 44% |
| All SEER stages combined | 56% |
Endometriosis
Endometriosis is a condition in which the tissue that is similar to the lining of your uterus called the endometrium (the inner lining of your uterus) that normally grows inside your uterus (womb) grows outside your uterus 125, 126, 127, 128, 129, 130, 131, 132. Your uterus or womb is the place where your baby grows during pregnancy. Endometriosis happens when tissue similar to the lining of your uterus (the endometrium) grows outside of your uterus and on other areas in your body where it doesn’t belong. Endometriosis can grow or implants in the cul-de-sac (the space behind the uterus), outer surfaces of the uterus, on the ovaries, fallopian (uterine) tubes, intestines and rectum, ureters or bladder. Rarely, endometriosis appears in other parts of your body, such as your lungs, brain, and skin 133. With endometriosis, the displaced endometrial tissue continues to act as it normally would — it thickens, breaks down and bleeds with each menstrual cycle. Because the displaced endometrium (the inner lining of your uterus) has no way to exit your body, it becomes trapped. When endometriosis involves the ovaries, cysts called endometriomas may form. Surrounding tissue can become irritated, eventually developing scar tissue and adhesions — abnormal bands of fibrous tissue that can cause pelvic tissues and organs to stick to each other and may make it harder for you to get pregnant. Endometriosis can cause pelvic pain — sometimes severe — especially during your period.
Endometriosis may affect more than 11% of American women between 15 and 44 134. Endometriosis is especially common among women in their 30s and 40s and can cause infertility.
Pelvic pain is the most common symptom of endometriosis. Women with endometriosis may have many different kinds of pain:
- Very painful menstrual cramps. The pain may get worse over time.
- Chronic (long-term) pain in the lower back and pelvis
- Pain during or after sex. This is usually described as a “deep” pain and is different from pain felt at the entrance to the vagina when penetration begins.
- Intestinal pain
- Painful bowel movements or pain when urinating during menstrual periods. In rare cases, you may also find blood in your stool or urine.
Endometriosis implants respond to changes in estrogen, a female hormone. The implants may grow and bleed like the uterine lining does during the menstrual cycle. Surrounding tissue can become irritated, inflamed, and swollen. The breakdown and bleeding of this tissue each month also can cause scar tissue, called adhesions, to form. Sometimes adhesions can cause organs to stick together. The bleeding, inflammation, and scarring can cause pain, especially before and during menstruation.
To diagnose endometriosis and other conditions that can cause pelvic pain, your doctor will ask you to describe your symptoms, including the location of your pain and when it occurs.
Tests to check for clues of endometriosis include:
- Pelvic exam. During a pelvic exam, your doctor manually feels (palpates) areas in your pelvis for abnormalities, such as cysts on your reproductive organs or scars behind your uterus. Often it’s not possible to feel small areas of endometriosis, unless they’ve caused a cyst to form.
- Ultrasound. This test uses high-frequency sound waves to create images of the inside of your body. To capture the images, a device called a transducer is either pressed against your abdomen or inserted into your vagina called transvaginal ultrasound. Both types of ultrasound may be done to get the best view of your reproductive organs. Ultrasound imaging won’t definitively tell your doctor whether you have endometriosis, but it can identify cysts associated with endometriosis (endometriomas).
- Magnetic resonance imaging (MRI). This exam uses a magnetic field and radio waves to make images of the organs and tissues within the body. For some, an MRI helps with surgical planning. It gives your surgeon detailed information about the location and size of endometriosis growths.
- Laparoscopy. Medical management is usually tried first. But to be certain you have endometriosis, your doctor may refer you to a surgeon to look inside your abdomen for signs of endometriosis using a surgical procedure called laparoscopy. A laparoscopy can provide information about the location, extent and size of the endometriosis growths to help determine the best treatment options. While you’re under general anesthesia, your surgeon makes a tiny incision near your navel (belly button) and inserts a slender viewing instrument called a laparoscope, looking for endometrial tissue outside your uterus. Your surgeon may take a tissue sample called biopsy for more testing. With proper planning, a surgeon can often treat endometriosis during the laparoscopy so that you need only one surgery.
Definitive diagnosis requires visualization of lesions during surgery, resulting in a delay in diagnosis that globally averages 7 years from symptom onset 135.
Fortunately, effective treatments are available that can help you manage your symptoms and improve your chances of getting pregnant.
Treatment for endometriosis often involves medicine or surgery. The approach you and your doctor choose will depend on how serious your symptoms are and whether you hope to become pregnant. Typically, medicine is recommended first. If it doesn’t help enough, surgery becomes an option.
How common is endometriosis?
Endometriosis is a common health problem for women. Researchers think that at least 11% of women, or more than 6.5 million women in the United States, have endometriosis 136. According to the findings of systematic reviews, the prevalence of endometriosis is around 3 to 5% in the general female population of reproductive age, but around 30% in women with infertility, 50% in women with pelvic pain 137, 138, 139, and as high as 65 to 75% in symptomatic adolescents who do not respond to medical treatment 140, 141.
Who gets endometriosis?
Endometriosis can happen in any girl or woman who has menstrual periods, but it is more common in women in their 30s and 40s.
You might be more likely to get endometriosis if you have:
- Never had children
- Menstrual periods that last more than seven days
- Short menstrual cycles (27 days or fewer)
- A family member (mother, aunt, sister) with endometriosis
- A medical condition that blocks the normal flow of menstrual blood from your body during your menstrual period.
How can I prevent endometriosis?
You can’t prevent endometriosis. But you can reduce your chances of developing it by lowering the levels of the hormone estrogen in your body. Estrogen helps to thicken the lining of your uterus during your menstrual cycle.
To keep lower estrogen levels in your body, you can:
- Talk to your doctor about hormonal birth control methods, such as pills, patches or rings with lower doses of estrogen.
- Exercise regularly (more than 4 hours a week). This will also help you keep a low percentage of body fat 142. Regular exercise and a lower amount of body fat help decrease the amount of estrogen circulating through the body.
- Avoid large amounts of alcohol. Alcohol raises estrogen levels 143. No more than one drink per day is recommended for women who choose to drink alcohol.
- Avoid large amount of drinks with caffeine. Studies show that drinking more than one caffeinated drink a day, especially sodas and green tea, can raise estrogen levels 144.
Can I get pregnant if I have endometriosis?
Yes. Many women with endometriosis get pregnant. But, you may find it harder to get pregnant. Researchers think endometriosis may affect as many as one in every two women with infertility 145.
No one knows exactly how endometriosis might cause infertility. Some possible reasons include 146:
- Patches of endometriosis block off or change the shape of the pelvis and reproductive organs. This can make it harder for the sperm to find the egg.
- The immune system, which normally helps defend the body against disease, attacks the embryo.
- The endometrium (the layer of the uterine lining where implantation happens) does not develop as it should.
If you have endometriosis and are having trouble getting pregnant, talk to your doctor. He or she can recommend treatments, such as surgery to remove the endometrial growths 146.
What other health conditions are linked to endometriosis?
Research shows a link between endometriosis and other health problems in women and their families. Some of these include:
- Allergies, asthma, and chemical sensitivities 147
- Autoimmune diseases, in which your body’s immune system that fights illness attacks itself instead. These can include multiple sclerosis, lupus, and some types of hypothyroidism 148
- Chronic fatigue syndrome and fibromyalgia 148
- Certain cancers, such as ovarian cancer 149 and breast cancer 150.
Does endometriosis go away on its own?
For some women diagnosed with endometriosis, endometriosis patches go away on their own 151.
Also, after menopause, symptoms of endometriosis typically lessen because there is a drop in the natural hormones and the growths gradually shrink. However, this is not true for all women. If a woman takes hormones for menopausal symptoms, both her pain symptoms and the growths may return.
Women with endometriosis who are experiencing symptoms, especially after menopause, should talk with their healthcare providers about treatment options.
Does endometriosis go away after menopause?
For some women, the painful symptoms of endometriosis improve after menopause. As the body stops making the hormone estrogen, the growths shrink slowly. However, some women who take menopausal hormone therapy may still have symptoms of endometriosis.
If you are having symptoms of endometriosis after menopause, talk to your doctor about your treatment options.
Figure 24. Endometriosis

Endometriosis causes
Although the exact cause of endometriosis is not certain, possible explanations include:
- Retrograde menstruation. In retrograde menstruation, menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity instead of out of your body. These displaced endometrial cells stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle.
- Transformation of peritoneal cells. In what’s known as the “induction theory”, experts propose that hormones or immune factors promote transformation of peritoneal cells — cells that line the inner side of your abdomen — into endometrial cells.
- Embryonic cell transformation. Hormones such as estrogen may transform embryonic cells — cells in the earliest stages of development — into endometrial-like cell implants during puberty.
- Surgical scar implantation. After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
- Endometrial cells transport. The blood vessels or tissue fluid (lymphatic) system may transport endometrial cells to other parts of your body.
- Immune system disorder. It’s possible that a problem with your immune system may make the body unable to recognize and destroy endometrial tissue that’s growing outside your uterus.
The retrograde menstruation, based on the implantation of endometrial cells reaching the pelvis via transtubal retrograde flow during menstruation, is supported by the largest body of evidence 152, 153, 154, 155, 131, 156, 157, 158.
Risk factors for developing endometriosis
Several factors place you at greater risk of developing endometriosis, such as:
- Never giving birth
- Mother, sister, or daughter had endometriosis (raises the risk about six times)
- Starting your period at an early age (before age 11)
- Going through menopause at an older age
- Short menstrual cycles — for instance, less than 27 days
- Heavy menstrual periods that last longer than seven days.
- Having higher levels of estrogen in your body or a greater lifetime exposure to estrogen your body produces
- Low body mass index
- Alcohol consumption
- One or more relatives (mother, aunt or sister) with endometriosis 159, 160
- Any medical condition that prevents the blood from flowing out of your body during menstrual periods
- Uterine abnormalities
Endometriosis usually develops several years after the onset of menstruation (menarche). Signs and symptoms of endometriosis end temporarily with pregnancy and end permanently with menopause, unless you’re taking estrogen therapy.
Endometriosis symptoms
The most common symptom of endometriosis is chronic (long-term) pelvic pain, especially just before and during the menstrual period. Although many women experience cramping during their menstrual period, women with endometriosis typically describe menstrual pain that’s far worse than usual. They also tend to report that the pain increases over time.
Pelvic pain also may occur during sex. If endometriosis is present on the bowel, pain during bowel movements can occur. If it affects the bladder, pain may be felt during urination. Heavy menstrual bleeding is another symptom of endometriosis. Many women with endometriosis have no symptoms at all. Having trouble getting pregnant may be the first sign.
Common signs and symptoms of endometriosis may include:
- Painful periods (dysmenorrhea). Pelvic pain and cramping may begin before your period and extend several days into your period. You may also have lower back and abdominal pain.
- Pain with intercourse. Pain during or after sex is common with endometriosis.
- Pain with bowel movements or urination. You’re most likely to experience these symptoms during your menstrual period.
- Excessive bleeding. You may experience occasional heavy periods (menorrhagia) or bleeding between periods (menometrorrhagia).
- Infertility or not being able to get pregnant. Endometriosis is first diagnosed in some women who are seeking treatment for infertility.
- Other symptoms. You may also experience fatigue, diarrhea, constipation, bloating or nausea, especially before or during your menstrual periods.
The severity of your pain isn’t necessarily a reliable indicator of the number or extent of endometriosis growths in your body. Some women with mild endometriosis have intense pain, while others with lots of endometriosis tissue may have little pain or even no pain at all. Still, some women with endometriosis have no symptoms. Often, they find out they have endometriosis when they can’t get pregnant or after they get surgery for another reason.
Endometriosis is sometimes mistaken for other conditions that can cause pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts. It may be confused with irritable bowel syndrome (IBS), a condition that causes bouts of diarrhea, constipation and abdominal cramping. Irritable bowel syndrome (IBS) can happen along with endometriosis, which can complicate the diagnosis.
Endometriosis pain
Pelvic pain is the most common symptom of endometriosis. Women with endometriosis may have many different kinds of pain:
- Very painful menstrual cramps. The pain may get worse over time.
- Chronic (long-term) pain in the lower back and pelvis
- Pain during or after sex. This is usually described as a “deep” pain and is different from pain felt at the entrance to the vagina when penetration begins.
- Intestinal pain
- Painful bowel movements or pain when urinating during menstrual periods. In rare cases, you may also find blood in your stool or urine.
Endometriosis implants respond to changes in estrogen, a female hormone. The implants may grow and bleed like the uterine lining does during the menstrual cycle. Surrounding tissue can become irritated, inflamed, and swollen. The breakdown and bleeding of this tissue each month also can cause scar tissue, called adhesions, to form. Sometimes adhesions can cause organs to stick together. The bleeding, inflammation, and scarring can cause pain, especially before and during menstruation.
When to see a doctor
See your doctor if you have signs and symptoms that may indicate endometriosis.
Endometriosis can be a challenging condition to manage. An early diagnosis, a multidisciplinary medical team and an understanding of your diagnosis may result in better management of your symptoms.
Endometriosis complications
The main complication of endometriosis is trouble getting pregnant or infertility and chronic pain. Approximately one-third to one-half of women with endometriosis have difficulty getting pregnant. Furthermore, is a chronic condition with a large impact on the woman’s quality of life causing a decrease in the quality of life of patients, complications of surgical procedures, anatomical abnormalities due to possible adhesions, bowel or/and bladder dysfunction, and in the case of ovarian endometriomas could even lead to the development of ovarian, breast and thyroid cancers 161. Additionally, women with endometriosis have higher stress levels, report worse quality of sleep, and lower physical activity compared to healthy women 162. Bowel dysfunction like constipation or other digestive problems can appear in females who have endometriosis as a result of the inflammatory process of irritation of the gastrointestinal system rather than due to the involvement of endometriotic nodules affecting the rectum since patients undergoing surgical treatment for rectal endometriosis might continue experiencing those symptoms 163. Although primarily endometriosis was considered a benign condition, later research findings showed a higher risk for ovarian cancer in patients with endometriosis 164.
Infertility
The main complication of endometriosis is impaired fertility. Approximately one-third to one-half of women with endometriosis have difficulty getting pregnant.
For pregnancy to occur, an egg must be released from an ovary, travel through the neighboring fallopian tube, become fertilized by a sperm cell and attach itself to the uterine wall to begin development. Endometriosis may block the fallopian tube and keep the egg and sperm from uniting. But endometriosis also seems to affect fertility in less-direct ways, such as damage to the sperm or egg.
Even so, many women with mild to moderate endometriosis can still conceive and carry a pregnancy to term. Doctors sometimes advise women with endometriosis not to delay having children because the condition may become worse with time.
What is the link between infertility and endometriosis?
This is one of the most perplexing aspects of endometriosis, confronting researchers and patients alike. Almost 40% of women with infertility have endometriosis. Not only do some of these women have difficulty conceiving and carrying a live birth to term, they are less likely to conceive following assisted reproduction, such as fertility medication, artificial insemination, and in vitro fertilization. Studies to address the link between endometriosis and infertility have just begun. These studies suggest that women with endometriosis may have implantation defects (abnormalities of the environment that make it difficult for the embryo to attach and survive) and/or low quality eggs. These conditions, in turn, could be related to an abnormal immune environment that some suspect exist in women with endometriosis. Furthermore, inflammation from endometriosis may damage the sperm or egg or interfere with their movement through the fallopian tubes and uterus. In severe cases of endometriosis, the fallopian tubes may be blocked by adhesions or scar tissue.
Ovarian cancer
Chronic pelvic pain
Chronic pelvic pain is closely associated with endometriosis since endometriosis has been the cause in 71% to 87% of women suffering from chronic pelvic pain 165. Chronic pelvic pain can negatively affect the health-related quality of life and hinder social, emotional, and sexual well-being as well as other domains like daily routines, family planning, or productivity of patients in the work environment 162.
Endometriosis diagnosis
To diagnose endometriosis and other conditions that can cause pelvic pain, your doctor will ask you to describe your symptoms, including the location of your pain and when it occurs.
Tests to check for clues of endometriosis include:
- Pelvic exam. During a pelvic exam, your doctor manually feels (palpates) areas in your pelvis for abnormalities, such as cysts on your reproductive organs or scars behind your uterus. Often it’s not possible to feel small areas of endometriosis, unless they’ve caused a cyst to form.
- Ultrasound. This test uses high-frequency sound waves to create images of the inside of your body. To capture the images, a device called a transducer is either pressed against your abdomen or inserted into your vagina called transvaginal ultrasound. Both types of ultrasound may be done to get the best view of your reproductive organs. Ultrasound imaging won’t definitively tell your doctor whether you have endometriosis, but it can identify cysts associated with endometriosis (endometriomas).
- Magnetic resonance imaging (MRI). This exam uses a magnetic field and radio waves to make images of the organs and tissues within the body. For some, an MRI helps with surgical planning. It gives your surgeon detailed information about the location and size of endometriosis growths.
- Laparoscopy. Medical management is usually tried first. But to be certain you have endometriosis, your doctor may refer you to a surgeon to look inside your abdomen for signs of endometriosis using a surgical procedure called laparoscopy. A laparoscopy can provide information about the location, extent and size of the endometriosis growths to help determine the best treatment options. While you’re under general anesthesia, your surgeon makes a tiny incision near your navel (belly button) and inserts a slender viewing instrument called a laparoscope, looking for endometrial tissue outside your uterus. Your surgeon may take a tissue sample called biopsy for more testing. With proper planning, a surgeon can often treat endometriosis during the laparoscopy so that you need only one surgery.
Endometriosis treatment
Treatment for endometriosis is usually with medications or surgery. The approach you and your doctor choose will depend on the severity of your signs and symptoms and whether you hope to become pregnant.
Generally, doctors recommend trying conservative treatment approaches first, opting for surgery as a last resort.
Finding a doctor with whom you feel comfortable is crucial in managing and treating endometriosis. You may also want to get a second opinion before starting any treatment to be sure you know all of your options and the possible outcomes.
Pain medications
Your doctor may recommend that you take an over-the-counter pain reliever, such as the nonsteroidal anti-inflammatory drugs (NSAIDs) ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve, others), to help ease painful menstrual cramps.
If you find that taking the maximum dose of these medications doesn’t provide full relief, you may need to try another approach to manage your signs and symptoms.
Home remedies for endometriosis
If your pain persists or if finding a treatment that works takes some time, you can try measures at home to relieve your discomfort.
- Apply a hot water bottle or heating pad to your lower stomach. This can get blood flowing and relax your muscles. Warm baths also may help relieve pain.
- Lie down and rest. Place a pillow under your knees when lying on your back. If you prefer to lie on your side, pull your knees up toward your chest. These positions help take the pressure off your back.
- Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve, others), can help ease painful menstrual cramps. If the pain is worse during your periods, try starting these medicines 1 to 2 days before your period begins.
- Regular exercise may help improve symptoms. Exercise helps improve blood flow. It also triggers your body’s natural painkillers, called endorphins.
- Eat a balanced, healthy diet. Maintaining a healthy weight will help improve your overall health. Eating plenty of fiber can help keep you regular so you don’t have to strain during bowel movements.
Techniques that also offer ways to relax and may help relieve pain include:
- Muscle relaxation
- Deep breathing
- Visualization
- Biofeedback
- Yoga
Some women find that acupuncture helps ease painful periods. Some studies show it also helps with chronic pain.
Hormone therapy
Sometimes, hormone medicine help ease or get rid of your endometriosis pain. The rise and fall of hormones during your menstrual cycle causes endometriosis tissue to thicken, break down and bleed. Hormone medication may slow the growth of this tissue and prevent new endometrial tissue from forming.
However, hormone therapy isn’t a permanent fix for endometriosis. You could experience a return of your symptoms after stopping treatment.
Hormone medications used to treat endometriosis include:
- Hormonal contraceptives. Birth control pills, patches and vaginal rings help control the hormones responsible for the buildup of endometrial tissue each month. Most women have lighter and shorter menstrual flow when they’re using a hormonal contraceptive. Using hormonal contraceptives — especially continuous cycle regimens — may reduce or eliminate the pain of mild to moderate endometriosis. The chances of relief seem to go up if you use birth control pills for a year or more with no breaks.
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists. These drugs block the production of ovarian-stimulating hormones, lowering estrogen levels and preventing menstruation. This causes endometrial tissue to shrink. Because these drugs create an artificial menopause, taking a low dose of estrogen or progestin along with Gn-RH agonists and antagonists may decrease menopausal side effects, such as hot flashes, vaginal dryness and bone loss. Your menstrual periods and the ability to get pregnant return when you stop taking the medication.
- Progestin therapy. A progestin-only contraceptive (lab-made version of the progesterone hormone), such as an intrauterine device (Mirena, Skyla, others), a contraceptive rod placed under the skin of the arm (Nexplanon) or contraceptive injection (Depo-Provera) or a progestin-only birth control pill (Camila, Slynd), can stop menstrual periods and the growth of endometrial implants, which may relieve endometriosis signs and symptoms.
- Danazol. This drug suppresses the growth of the endometrium by blocking the production of ovarian-stimulating hormones, preventing menstruation and the symptoms of endometriosis. However, danazol may not be the first choice because it can cause serious side effects and can be harmful to the baby if you become pregnant while taking this medication.
- Aromatase inhibitors. Aromatase inhibitors are a class of medicines that lower the amount of estrogen in your body. Your doctor may recommend an aromatase inhibitor along with a progestin or combination birth control pills to treat your endometriosis.
- Researchers are exploring the use of other hormones for treating endometriosis and the pain related to it. One example is gestrinone, which has been used in Europe but is not available in the United States.
If you are TRYING to get pregnant, your doctor may prescribe a gonadotropin-releasing hormone (GnRH) agonist. This medicine stops your body from making the hormones responsible for ovulation, the menstrual cycle, and the growth of endometriosis. This treatment causes a temporary menopause, but it also helps control the growth of endometriosis. Once you stop taking the medicine, your menstrual cycle returns, but you may have a better chance of getting pregnant.
If you are NOT trying to get pregnant, hormonal birth control is generally the first step in treatment. This may include 133:
- Extended-cycle (you have only a few periods a year) or continuous cycle (you have no periods) birth control. These types of hormonal birth control are available in the pill or the shot and help stop bleeding and reduce or eliminate pain.
- Intrauterine device (IUD) to help reduce pain and bleeding. The hormonal IUD protects against pregnancy for up to 7 years. But the hormonal IUD may not help your pain and bleeding due to endometriosis for that long.
Oral contraceptives or birth control pills
These help make your period lighter, more regular, and shorter. Women prescribed contraceptives also report relief from pain 166.
- In general, the therapy contains two hormones-estrogen and progestin (a man-made progesterone-like hormone). Women who can’t take estrogen because of cardiovascular disease or a high risk of blood clots can use progestin-only pills to reduce menstrual flow.
- Typically, a woman takes the pill for 21 days and then takes sugar pills for 7 days to mimic the natural menstrual cycle. Some women take birth control pills continuously, without using the sugar pills that signal the body to go through menstruation. Taken without the sugar pills, birth control pills may stop the menstrual period altogether, which can reduce or eliminate the pain. There are also birth control pills available that provide only a couple days of sugar pills every 3 months; these also help reduce or eliminate pain.
- Pain relief usually lasts only while taking the pills, while the endometriosis is suppressed. When treatment stops, the symptoms of endometriosis may return (along with the ability to get pregnant). Many women continue treatment indefinitely. Occasionally, some women have no pain for several years after stopping treatment.
- There are some mild side effects from these hormones, such as weight gain, bloating, and bleeding between periods (especially when women first start to take the pills continuously).
Progesterone and progestin
Progesterone and progestin, taken as a pill, by injection, or through an intrauterine device (IUD), improve symptoms by reducing a woman’s period or stopping it completely. This also prevents pregnancy.
- As a pill taken daily, these hormones reduce menstrual flow without causing the uterus lining to grow. As soon as a woman stops taking the progestin pill, symptoms may return and pregnancy is possible.
- An IUD containing progestin, such as Mirena®, may be effective in reducing endometriosis-associated pain. It reduces the size of lesions and reduces menstrual flow (one third of women no longer get their period after a year of use) 167.
- As an Depo-Provera injection taken every 3 months, these hormones usually stop menstrual flow. However, one-third of women bleed several times in the first year of injection use. During these times of bleeding, pain may occur. Additionally, it may take a few months for a period to return after stopping the injections. When menstruation starts again, the ability to get pregnant returns.
- Women taking these hormones may gain weight, feel depressed, or have irregular vaginal bleeding.
Gonadotropin-releasing hormone (GnRH) agonists
Gonadotropin-releasing hormone (GnRH) agonists stop the production of certain hormones to prevent ovulation, menstruation, and the growth of endometriosis. This treatment sends the body into a “menopausal” state.
- GnRH agonists come in a nose spray taken daily, as an injection given once a month, or as an injection given every 3 months.
- The low-dose elagolix (Orilissa) pill should not be taken for more than 24 months and the high‑dose pill should not be taken for more than 6 months because it may cause bone loss 168
- Most health care providers recommend staying on GnRH agonists for only about 6 months at a time, with several months between treatments if they are repeated. The risk for heart complications and bone loss can rise when taking them longer 142. After stopping the GnRH agonist, the body comes out of the menopausal state, menstruation begins, and pregnancy is possible 169.
- As with all hormonal treatments, endometriosis symptoms return after women stop taking GnRH agonists.
- These medications also have side effects, including hot flashes, tiredness, problems sleeping, headache, depression, joint and muscle stiffness, bone loss, and vaginal dryness 168.
Danazol
Danazol also called Danocrine treatment stops the release of hormones that are involved in the menstrual cycle. While taking this drug, women will have a period only now and then or sometimes not at all.
- Common side effects include oily skin, pimples or acne, weight gain, muscle cramps, tiredness, smaller breasts, and sore breasts. Headaches, dizziness, weakness, hot flashes, or a deepening of the voice may also occur while on this treatment. Danazol’s side effects are more severe than those from other hormone treatment options 170.
- Danazol can harm a developing fetus. Therefore, it is important to prevent pregnancy while on this medication. Hormonal birth control methods are not recommended while on danazol. Instead, health care providers recommend using barrier methods of birth control, such as condoms or a diaphragm.
Surgery
Conservative surgery is usually chosen for severe symptoms, when hormones are not providing relief or if you are having fertility problems. If you have endometriosis and are trying to become pregnant, surgery to remove as much endometriosis as possible while preserving your uterus and ovaries (conservative surgery) may increase your chances of success. If you have severe pain from endometriosis, you may also benefit from surgery. After surgery, most women have relief from pain. However, about 40 to 80% of women have pain again within 2 years after surgery. The more severe the disease, the more likely it is to return. Taking birth control pills or other medications after having surgery may help extend the pain-free period.
In some cases, hormone therapy is used before or after surgery to reduce pain and/or continue treatment. Current evidence supports the use of an intrauterine device (IUD) containing progestin after surgery to reduce pain. Currently, the only such device approved by the FDA is Mirena®.
Your doctor may do this procedure laparoscopically or through traditional abdominal surgery in more extensive cases. In laparoscopic surgery, your surgeon inserts a slender viewing instrument (laparoscope) through a small incision near your navel and inserts instruments to remove endometrial tissue through another small incision.
After surgery, your doctor may recommend taking hormone medicine to help improve pain.
Laparoscopy
The surgeon uses an instrument to inflate the abdomen slightly with a harmless gas and then inserts a small viewing instrument with a light, called a laparoscope, into the abdomen through a small cut to see the growths.
To remove the endometriosis, the surgeon makes at least two more small cuts in the abdomen and inserts lasers or other surgical instruments to:
- Remove the lesions, which is a process called excising.
- Destroy the lesions with intense heat and seal the blood vessels without stitches, a process called cauterizing or vaporizing.
- Some surgeons also will remove scar tissue at this time because it may be contributing to endometriosis-associated pain.
- The goal is to treat the endometriosis without harming the healthy tissue around it.
- Although most women have relief from pain with surgery in the short term, pain often returns 170. The excision of deep lesions seems to be associated with long-term pain relief.
- Some evidence shows that surgical treatment for endometriosis-related pain is actually more effective in women who have moderate endometriosis rather than minimal endometriosis. The reason is that women with minimal endometriosis may have changes in their pain perception that persist after the lesions are removed 167, 171.
Laparotomy
In this major abdominal surgery procedure, the surgeon may remove the endometriosis patches. Sometimes, the endometriosis lesions are too small to see in a laparotomy.
- During this procedure, the surgeon may also remove the uterus. Removing the uterus is called hysterectomy.
- If the ovaries have endometriosis on them or if damage is severe, the surgeon may remove the ovaries and fallopian tubes along with the uterus. This process is called total hysterectomy and bilateral (meaning “on both sides”) salpingo-oophorectomy.
- When possible, health care providers will try to leave the ovaries in place because of the important role ovaries play in overall health.
- Doctors recommend major surgery as a last resort for endometriosis treatment.
- Having a hysterectomy or salpingo-oophorectomy does not guarantee that the lesions will not return or that the pain will go away. Endometriosis symptoms and lesions may come back in as many as 15% of women who have a total hysterectomy with bilateral salpingo-oophorectomy 142.
Hysterectomy
In severe cases of endometriosis, surgery to remove the uterus and cervix (total hysterectomy) as well as both ovaries (oophorectomy) may be the best treatment but causes early menopause. Early menopause also carries a risk of heart and blood vessel diseases, certain metabolic conditions and early death. You can’t get pregnant after a hysterectomy. The lack of hormones made by the ovaries may improve endometriosis pain for some. But for others, endometriosis that remains after surgery continues to cause symptoms.
A hysterectomy alone is not effective — the estrogen your ovaries produce can stimulate any remaining endometriosis and cause pain to persist. There is a small chance that pain will come back even if your uterus and ovaries are removed. This may be due to endometriosis that was not visible or could not be removed at the time of surgery.
Taking out your uterus and ovaries was once thought to be the most effective treatment for endometriosis. Today, some experts consider it to be a last resort to ease pain when other treatments haven’t worked. Other experts instead recommend surgery that focuses on the careful and thorough removal of all endometriosis tissue.
Treatments for Infertility Related to Endometriosis
Endometriosis can lead to trouble getting pregnant. In most cases, doctor will recommend laparoscopy to remove or vaporize the growths as a way to also improve fertility in women who have mild or minimal endometriosis 167. Although studies show improved pregnancy rates following this type of surgery, the success rate is not clear.
If pregnancy does not occur after laparoscopic treatment, in vitro fertilization (IVF) may be the best option to improve fertility. Taking any other hormonal therapy usually used for endometriosis-associated pain will only suppress ovulation and delay pregnancy. Performing another laparoscopy is not the preferred approach to improving fertility unless symptoms of pain prevent undergoing IVF. Multiple surgeries, especially those that remove cysts from the ovaries, may reduce ovarian function and hamper the success of IVF 167.
IVF makes it possible to combine sperm and eggs in a laboratory to make an embryo. Then the resulting embryos are placed into the woman’s uterus. IVF is one type of assisted reproductive technology (ART) that may be an option for women and families affected by infertility related to endometriosis.
In general, the process of IVF involves the following steps. First, a woman takes hormones to cause “superovulation”, which triggers her body to produce many eggs at one time. Once mature, the eggs are collected from the woman, using a probe inserted into the vagina and guided by ultrasound. The collected eggs are placed in a dish for fertilization with a man’s sperm. The fertilized cells are then placed in an incubator, a machine that keeps them warm and allows them to develop into embryos. After 3 to 5 days, the embryos are transferred to the woman’s uterus. It takes about 2 weeks to know if the process is successful.
Even though the use of hormones in IVF is successful in treating infertility related to endometriosis, other forms of hormone therapy are not as successful. For instance, the American College of Obstetricians and Gynecologists does not recommend using oral contraceptive pills or GnRH agonists to treat endometriosis-related infertility. The use of these hormonal agents prevents ovulation and delays pregnancy 142, 130.
In addition, the hormones used during IVF do not cure the endometriosis lesions, which means that pain may recur after pregnancy and that not all women with endometriosis are able to become pregnant with IVF. Researchers are still looking for hormone treatments for infertility due to endometriosis.
Alternative medicine
Alternative medicine involves treatments that aren’t part of standard medical care. Some people with endometriosis say they get pain relief from alternative therapies such as:
- Acupuncture, in which a trained practitioner places fine needles into your skin. Acupuncture has shown some promise at easing endometriosis pain.
- Chiropractic care, in which a licensed professional adjusts the spine or other body parts.
- Herbs such as cinnamon trig or licorice root.
- Supplements including vitamin B1 (thiamine), magnesium or omega-3 fatty acids.
Overall, there’s little research on much relief women with endometriosis might get from alternative medicine. Always check with your doctor before you try a new alternative therapy to find out if it’s safe for you. For example, supplements and herbs can affect standard treatments such as medicines. If you’re interested in trying acupuncture or chiropractic care, ask your doctor to recommend reputable professionals.
Endometriosis prognosis
Women with endometriosis have fewer chances for childbearing and a higher risk for miscarriages and ectopic pregnancies than those without endometriosis 172. Additionally, endometriotic lesions can spontaneously regress in approximately one-third of affected women who are not receiving any treatment 173. According to different estimates, endometriosis recurrence rates after surgery vary between 6 and 67% 174. Potential risk factors predicting a possible recurrence have not been completely clarified, but the recurrent endometriotic lesions may arise from de novo cells or residual endometriotic tissue 174. Medical treatment can be proven effective, but in 5% to 59% of patients, the pain continues to exist at the end of the therapy 175. Even in cases of treatment cessation, pain recurrence has been reported in 17% to 34% of cases 175.
Pelvic inflammatory disease
Pelvic inflammatory disease (PID) is an infection of a woman’s reproductive organs. The reproductive organs include the uterus (womb), fallopian tubes (uterine tubes), ovaries, and cervix. In 2013, about 88,000 women ages 15–44 in the United States were diagnosed with Pelvic inflammatory disease 176. Pelvic inflammatory disease is often caused by a sexually transmitted infection (STI). If left untreated, pelvic inflammatory disease can cause problems getting pregnant, problems during pregnancy, and long-term pelvic pain. 1 in 8 women with a history of pelvic inflammatory disease experience difficulties getting pregnant 177.
Pelvic inflammatory disease can be caused by many different types of bacteria. Usually pelvic inflammatory disease is caused by bacteria from sexually transmitted infections (STIs) also called sexually transmitted diseases (STDs). Sometimes pelvic inflammatory disease is caused by normal bacteria found in the vagina.
Any woman can get pelvic inflammatory disease, but you’re more likely to get it if you:
- have more than 1 sexual partner
- have a new sexual partner
- have a history of sexually transmitted infections (STIs)
- have had pelvic inflammatory disease in the past
- are under 25
- started having sex at a young age
Pelvic inflammatory disease (PID) comprises a spectrum of inflammatory disorders of the upper female genital tract, including any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis 178. Sexually transmitted organisms, especially Neisseria gonorrhoeae and Chlamydia trachomatis, are implicated in many cases. Recent studies suggest that the proportion of pelvic inflammatory disease cases attributable to Neisseria gonorrhoeae or Chlamydia trachomatis is declining; of women who received a diagnosis of acute pelvic inflammatory disease, <50% test positive for either of these organisms 179. Microorganisms that comprise the vaginal flora (e.g., anaerobes, Gardnerella vaginalis, Haemophilus influenzae, enteric Gram-negative rods, and Streptococcus agalactiae) have been associated with pelvic inflammatory disease 180. In addition, cytomegalovirus (CMV), Mycoplasma hominis, Ureaplasma urealyticum, and Mycoplasma genitalium might be associated with some pelvic inflammatory disease cases 181. Newer data suggest that Mycoplasma genitalium might play a role in the pathogenesis of pelvic inflammatory disease 179 and might be associated with milder symptoms 182, although one study failed to demonstrate a significant increase in pelvic inflammatory disease following detection of Mycoplasma genitalium in the lower genital tract 183. All women who receive a diagnosis of acute pelvic inflammatory disease should be tested for HIV, as well as gonorrhea and chlamydia, using nucleic acid amplification test (NAAT). The value of testing women with pelvic inflammatory disease for Mycoplasma genitalium is unknown, and there is no commercially available diagnostic test that has been cleared by FDA for use in the United States 184.
Screening and treating sexually active women for chlamydia reduces their risk for pelvic inflammatory disease 185. Although bacterial vaginosis is associated with pelvic inflammatory disease, whether the incidence of pelvic inflammatory disease can be reduced by identifying and treating women with bacterial vaginosis is unclear 180.
Many episodes of pelvic inflammatory disease (PID) go unrecognized. Although some cases are asymptomatic, others are not diagnosed because the patient or the health-care provider fails to recognize the implications of mild or nonspecific symptoms or signs (e.g., abnormal bleeding, painful sex, and vaginal discharge). Even women with mild or asymptomatic pelvic inflammatory disease might be at risk for infertility 186. Because of the difficulty of diagnosis and the potential for damage to the reproductive health of women, health-care providers usually maintain a low threshold for the diagnosis of pelvic inflammatory disease 187. The following recommendations for diagnosing pelvic inflammatory disease are intended to help health-care providers recognize when pelvic inflammatory disease should be suspected and when additional information should be obtained to increase diagnostic certainty. Diagnosis and management of other common causes of lower abdominal pain (e.g., ectopic pregnancy, acute appendicitis, ovarian cyst, and functional pain) are unlikely to be impaired by initiating antimicrobial therapy for pelvic inflammatory disease.
Presumptive treatment for pelvic inflammatory disease should be initiated in sexually active young women and other women at risk for sexually transmitted infections (STIs) if they are experiencing pelvic or lower abdominal pain, if no cause for the illness other than pelvic inflammatory disease can be identified, and if one or more of the following minimum clinical criteria are present on pelvic examination:
- cervical motion tenderness
OR - uterine tenderness
OR - adnexal tenderness.
The requirement that all three minimum criteria be present before the initiation of empiric treatment could result in insufficient sensitivity for the diagnosis of pelvic inflammatory disease. After deciding whether to initiate empiric treatment, clinicians should also consider the risk profile for sexually transmitted diseases (STDs).
Several types of antibiotics can cure pelvic inflammatory disease. Antibiotic treatment does not, however, reverse any scarring caused by the infection. For this reason, it is critical that a woman receive care immediately if she has pelvic pain or other symptoms of pelvic inflammatory disease. Prompt antibiotic treatment can prevent severe damage to the reproductive organs. The longer a woman delays treatment for pelvic inflammatory disease, the more likely she is to become infertile or to have a future ectopic pregnancy because of damage to the fallopian tubes.
Pelvic inflammatory disease is treated with a combination of antibiotics for at least 14 days. Most of the time, at least two antibiotics are used that work against many different types of bacteria. You must take all of your antibiotics, even if your symptoms go away. This helps to make sure the infection is fully cured. See your doctor or nurse again two to three days after starting the antibiotics to make sure they are working. During treatment you are advised not to have sex. If you or your partner are diagnosed with an sexually transmitted disease (STD) you may also need to contact previous sexual partners to inform them they should get checked. Your doctor or nurse can assist you with how to contact trace your sexual partners.
When pelvic inflammatory disease is treated early, it greatly reduces the risk of complications like lower fertility, chronic abdominal pain, ectopic pregnancy (foetus development in the fallopian tubes), miscarriage, premature birth and stillbirth.
Condoms are the best method of protection against both sexually transmitted infections and pelvic inflammatory disease. It is also important to have regular tests for sexually transmitted infections if you are sexually active and to have an sexually transmitted disease (STD) check before any gynecological procedure, such as intrauterine device (IUD) insertion or abortion.
Your doctor or nurse may suggest going into the hospital to treat your pelvic inflammatory disease if:
- You are very sick
- You are pregnant
- Your symptoms do not go away after taking the antibiotics or if you cannot swallow pills. If this is the case, you will need IV antibiotics.
- You have an abscess in a fallopian tube or ovary
If you still have symptoms or if the abscess does not go away after treatment, you may need surgery. Problems caused by pelvic inflammatory disease, such as chronic pelvic pain and scarring, are often hard to treat. But sometimes they get better after surgery.
How common is pelvic inflammatory disease in the United States?
Despite declining trends, pelvic inflammatory disease is a frequent and important infection that occurs among women of reproductive age. Based on data from the National Health and Nutrition Examination Survey (NHANES) 2013-2014 cycle, the estimated prevalence of self-reported lifetime pelvic inflammatory disease was 4.4% in sexually experienced women of reproductive age (18–44 years) 188. This equates to an estimated 2.5 million women in the United States with a reported lifetime history of pelvic inflammatory disease diagnosis . The prevalence was highest in women at increased risk, such as those with previous sexually transmitted infections (STIs) 188.
The significant burden of disease attributed to pelvic inflammatory disease comes predominantly from the long-term reproductive complications of tubal infection: tubal factor infertility, ectopic pregnancy, and pelvic adhesions, which can lead to chronic pelvic pain. The Centers for Disease Control and Prevention (CDC) knowledge of the longitudinal outcomes for affected women who experience pelvic inflammatory disease is primarily derived from data published using a Scandinavian cohort of inpatients diagnosed with pelvic inflammatory disease 189. Data from this study indicated that those women with pelvic inflammatory disease were more likely to have ectopic pregnancy (6 times increased rate), tubal factor infertility (ranging 8% after first episode to as high as 40% after three episodes) and chronic pelvic pain (18% following 1 episode).
Can pelvic inflammatory disease be cured?
Yes, if pelvic inflammatory disease is diagnosed early, it can be treated. However, treatment won’t undo any damage that has already happened to your reproductive system. The longer you wait to get treated, the more likely it is that you will have complications from pelvic inflammatory disease. While taking antibiotics, your symptoms may go away before the infection is cured. Even if symptoms go away, you should finish taking all of your medicine. Be sure to tell your recent sex partner(s), so they can get tested and treated for sexually transmitted infections (STIs), too. It is also very important that you and your partner both finish your treatment before having any kind of sex so that you don’t re-infect each other.
You can get pelvic inflammatory disease again if you get infected with an sexually transmitted infection (STI) again. Also, if you have had pelvic inflammatory disease before, you have a higher chance of getting it again.
What can happen if pelvic inflammatory disease is not treated?
Without treatment, pelvic inflammatory disease can lead to serious problems like infertility, ectopic pregnancy, and chronic pelvic pain (pain that does not go away). If you think you may have pelvic inflammatory disease, see a doctor or nurse as soon as possible.
Antibiotics will treat pelvic inflammatory disease, but they will not fix any permanent damage done to your internal organs.
Pelvic inflammatory disease (PID) can sometimes lead to serious and long-term problems, particularly if the condition isn’t treated with antibiotics quickly.
But most women with pelvic inflammatory disease who complete their course of antibiotics have no long-term problems.
Repeated episodes of pelvic inflammatory disease
Some women experience repeated episodes of pelvic inflammatory disease. This is known as recurrent pelvic inflammatory disease. The condition can return if the initial infection isn’t entirely cleared. This is often because the course of antibiotics wasn’t completed or because a sexual partner wasn’t tested and treated.
If an episode of pelvic inflammatory disease damages the womb or fallopian tubes, it can become easier for bacteria to infect these areas in the future, making it more likely that you’ll develop the condition again.
Repeated episodes of pelvic inflammatory disease are associated with an increased risk of infertility.
Abscesses
Pelvic inflammatory disease can sometimes cause collections of infected fluid called abscesses to develop, most commonly in the fallopian tubes and ovaries (tubo-ovarian abscess). Abscesses may be treated with broad-spectrum antibiotics, but sometimes laparoscopic surgery (keyhole surgery) may be needed to drain the fluid away. The fluid can also sometimes be drained using a needle that’s guided into place using an ultrasound scan.
Women infected with HIV may be at higher risk for tubo-ovarian abscess. Mortality from pelvic inflammatory disease is less than 1% and is usually secondary to rupture of a tubo-ovarian abscess or to ectopic pregnancy.
Long-term pelvic pain
Some women with pelvic inflammatory disease develop long-term (chronic) pain around their pelvis and lower abdomen, which can be difficult to live with and lead to further problems, such as depression and difficulty sleeping (insomnia). If you develop chronic pelvic pain, you may be given painkillers to help control your symptoms.
Tests to determine the cause may be carried out. If painkillers don’t control your pain, you may be referred to a pain management team or a specialist pelvic pain clinic.
Ectopic pregnancy
An ectopic pregnancy is when a fertilized egg implants itself outside of the womb, usually in one of the fallopian tubes. If pelvic inflammatory disease infects the fallopian tubes, it can scar the lining of the tubes, making it more difficult for eggs to pass through.
If a fertilized egg gets stuck and begins to grow inside the tube, it can cause the tube to burst, which can sometimes lead to severe and life-threatening internal bleeding.
If you’re diagnosed with an ectopic pregnancy, you may be given medication to stop the egg growing or have surgery to remove it.
Infertility
As well as increasing your risk of having an ectopic pregnancy, scarring or abscesses in the fallopian tubes can make it difficult for you to get pregnant if eggs can’t pass easily into the womb.
It’s estimated about 1 in 10 women with pelvic inflammatory disease become infertile as a result of the condition, with the highest risk for women who delayed treatment or had repeated episodes of pelvic inflammatory disease.
But a long-term study in the US showed that women who’d been successfully treated for pelvic inflammatory disease had the same pregnancy rates as the rest of the population.
Blocked or damaged fallopian tubes can sometimes be treated with surgery. If this isn’t possible and you want to have children, you may want to consider an assisted conception technique, such as in-vitro fertilization (IVF).
In-vitro fertilization (IVF) involves surgically removing eggs from a woman’s ovaries and fertilizing them with sperm in a laboratory, before planting the fertilized eggs into the woman’s womb.
This technique can help you get pregnant if you can’t have children naturally. But the success rate is often low, depending on your age and other factors.
Can I get pregnant if I have had pelvic inflammatory disease?
Maybe. Your chances of getting pregnant are lower if you have had pelvic inflammatory disease more than once. When you have pelvic inflammatory disease, bacteria can get into the fallopian tubes or cause inflammation of the fallopian tubes. This can cause scarring in the tissue that makes up your fallopian tubes.
Scar tissue can block an egg from your ovary from entering or traveling down the fallopian tube to your uterus (womb). The egg needs to be fertilized by a man’s sperm and then attach to your uterus for pregnancy to happen. Even having just a little scar tissue can keep you from getting pregnant without fertility treatment.
Scar tissue from pelvic inflammatory disease can also cause a dangerous ectopic pregnancy (a pregnancy outside of the uterus) instead of a normal pregnancy. Ectopic pregnancies are more than six times more common in women who have had pelvic inflammatory disease compared with women who have not had pelvic inflammatory disease 190. Most of these pregnancies end in miscarriage.
Who gets pelvic inflammatory disease?
Pelvic inflammatory disease affects about 5% of women in the United States 191. Your risk for Pelvic inflammatory disease is higher if you 177:
- Have had an sexually transmitted disease (STD)
- Have had pelvic inflammatory disease before
- Are younger than 25 and have sex. Pelvic inflammatory disease is most common in women 15 to 24 years old.
- Have more than one sex partner or have a partner who has multiple sexual partners
- Douche. Douching can push bacteria into the reproductive organs and cause Pelvic inflammatory disease. Douching can also hide the signs of Pelvic inflammatory disease.
- Recently had an intrauterine device (IUD) inserted 192. The risk of Pelvic inflammatory disease is higher for the first few weeks only after insertion of an IUD (intrauterine device), but Pelvic inflammatory disease is rare after that. Getting tested for sexually transmitted infections (STIs) before the intrauterine device (IUD) is inserted lowers your risk for pelvic inflammatory disease.
How do you get pelvic inflammatory disease?
A woman can get pelvic inflammatory disease if bacteria move up from her vagina or cervix and into her reproductive organs. Many different types of bacteria can cause pelvic inflammatory disease. Most often, pelvic inflammatory disease is caused by infection from two common sexually transmitted infections (STIs): gonorrhea and chlamydia. The number of women with pelvic inflammatory disease has dropped in recent years. This may be because more women are getting tested regularly for chlamydia and gonorrhea 193.
You can also get pelvic inflammatory disease without having an sexually transmitted infection. Normal bacteria in the vagina can travel into a woman’s reproductive organs and can sometimes cause pelvic inflammatory disease. Sometimes the bacteria travel up to a woman’s reproductive organs because of douching. Do not douche. No doctor or nurse recommends douching.
You are more likely to get pelvic inflammatory disease if you:
- Have an sexually transmitted infection (STI) and do not get treated;
- Have more than one sex partner;
- Have a sex partner who has sex partners other than you;
- Have had pelvic inflammatory disease before;
- Are sexually active and are age 25 or younger;
- Douche;
- Use an intrauterine device (IUD) for birth control. However, the small increased risk is mostly limited to the first three weeks after the IUD is placed inside the uterus by a doctor.
Can women who have sex with women get pelvic inflammatory disease?
Yes. It is possible to get pelvic inflammatory disease, or an sexually transmitted infection (STI), if you are a woman who has sex only with women.
Talk to your partner about her sexual history before having sex, and ask your doctor about getting tested if you have signs or symptoms of pelvic inflammatory disease.
Pelvic inflammatory disease causes
Most cases of pelvic inflammatory disease are caused by a bacterial infection that’s spread from the vagina or the cervix (entrance to the womb) into the reproductive organs higher up – the womb, fallopian tubes and ovaries.
If an infection spreads upwards from the vagina and cervix, it can cause inflammation of the:
- Womb lining (endometrium)
- Fallopian tubes
- Tissue around the womb
- Ovaries
- Lining of the inside of the abdomen (peritoneum)
- Pockets of infected fluid called abscesses can also develop in the ovaries and fallopian tubes (tubo-ovarian abscess).
Many different types of bacteria can cause pelvic inflammatory disease and it can sometimes be difficult for doctors to pinpoint which are responsible. The sexually transmitted pathogens Chlamydia trachomatis and Neisseria gonorrhoeae have been implicated in a third to half of pelvic inflammatory disease cases 194. However, in many other cases, pelvic inflammatory disease is caused by bacteria that normally live in the vagina, including gram positive and negative anaerobic organisms and aerobic/facultative gram positive and negative rods and cocci, found at high levels in women with bacterial vaginosis, also have been implicated in the pathogenesis of pelvic inflammatory disease 195. Newer data suggest that Mycoplasma genitalium may also play a role in pelvic inflammatory disease and may be associated with milder symptoms 196 although one study failed to demonstrate a significant increase in pelvic inflammatory disease following detection of M. genitalium in the lower genital tract 183. Because of the polymicrobial nature of pelvic inflammatory disease, a combination of antibiotics will be prescribed so a variety of bacteria can be treated.
Sexually transmitted infections (STIs)
In about a third to half of pelvic inflammatory disease cases, pelvic inflammatory disease is caused by a sexually transmitted infection (STI) such as chlamydia, gonorrhoea or mycoplasma genitalium.
These bacteria usually only infect the cervix, where they can be easily treated with a single dose of an antibiotic.
But if they’re not treated there’s a risk the bacteria could travel into the upper genital tract.
It’s estimated 1 in 10 women with untreated chlamydia may develop pelvic inflammatory disease within a year.
Other causes
In many cases, the cause of the infection that leads to pelvic inflammatory disease is unknown. Sometimes normally harmless bacteria found in the vagina can get past the cervix and into the reproductive organs. Although harmless in the vagina, these types of bacteria can cause infection in other parts of the body.
This is most likely to happen if:
- you have had pelvic inflammatory disease before
- there’s been damage to the cervix following childbirth or a miscarriage
- you have a procedure that involves opening the cervix (such as an abortion, inspection of the womb, or insertion of an intrauterine (IUD) contraceptive device)
Risk factors for developing pelvic inflammatory disease
Risk factors for pelvic inflammatory disease include factors associated with sexually transmitted infection (STI) acquisition, such as younger age, having a new or multiple sex partners, having a sex partner who has other concurrent sex partners, and inconsistent use of condoms during sex. Other factors that have been associated with pelvic inflammatory disease include a history of sexually transmitted infections (STIs) or prior pelvic inflammatory disease, and vaginal douching 188. A small increased risk of pelvic inflammatory disease associated with intrauterine device (IUD) use is primarily confined to the first three weeks after IUD insertion 197.
Intrauterine Contraceptive Devices
IUDs (intrauterine contraceptive devices) are one of the most effective contraceptive methods. Copper-containing and levonorgestrel-releasing IUDs are available in the United States. The risk for pelvic inflammatory disease associated with IUD use is primarily confined to the first 3 weeks after insertion 198. If an IUD user receives a diagnosis of pelvic inflammatory disease, the IUD does not need to be removed 199. However, the woman should receive treatment according to these recommendations and should have close clinical follow-up. If no clinical improvement occurs within 48–72 hours of initiating treatment, providers should consider removing the IUD. A systematic review of evidence found that treatment outcomes did not generally differ between women with pelvic inflammatory disease who retained the IUD and those who had the IUD removed 200. These studies primarily included women using copper or other nonhormonal IUDs. No studies are available regarding treatment outcomes in women using levonorgestrel-releasing IUDs.
Pelvic inflammatory disease prevention
You may not be able to prevent pelvic inflammatory disease. It is not always caused by an sexually transmitted infection (STI). Sometimes, normal bacteria in your vagina can travel up to your reproductive organs and cause pelvic inflammatory disease.
But, you can lower your risk of pelvic inflammatory disease by not douching. You can also prevent sexually transmitted infections (STIs) by not having vaginal, oral, or anal sex.
If you do have sex, lower your risk of getting an sexually transmitted infection (STI) with the following steps:
- Use condoms. Condoms are the best way to prevent sexually transmitted infections (STIs) when you have sex. Because a man does not need to ejaculate (come) to give or get sexually transmitted infections (STIs), make sure to put the condom on before the penis touches the vagina, mouth, or anus. Other methods of birth control, like birth control pills, shots, implants, or diaphragms, will not protect you from sexually transmitted infections (STIs).
- Get tested. Be sure you and your partner are tested for sexually transmitted infections (STIs). Talk to each other about the test results before you have sex.
- Be monogamous. Having sex with just one partner can lower your risk for sexually transmitted infections (STIs). After being tested for sexually transmitted infections (STIs), be faithful to each other. That means that you have sex only with each other and no one else.
- Limit your number of sex partners. Your risk of getting sexually transmitted infections (STIs) goes up with the number of partners you have.
- Do not douche. Douching removes some of the normal bacteria in the vagina that protect you from infection. Douching may also raise your risk for pelvic inflammatory disease by helping bacteria travel to other areas, like your uterus, ovaries, and fallopian tubes.
- Do not abuse alcohol or drugs. Drinking too much alcohol or using drugs increases risky behavior and may put you at risk of sexual assault and possible exposure to sexually transmitted infections (STIs).
The steps work best when used together. No single step can protect you from every single type of sexually transmitted infection (STI).
Pelvic inflammatory disease signs and symptoms
Many women do not know they have pelvic inflammatory disease because they do not have any signs or symptoms. When symptoms do happen, they can be mild or more serious.
Pelvic inflammatory disease signs and symptoms include:
- Pain in the lower abdomen (this is the most common symptom) or back pain
- Fever 100.4° F (38 °C) or higher, chills, nausea or vomiting.
- Vaginal discharge that may smell foul
- Painful sex, including bleeding after sex
- Pain when urinating
- Irregular menstrual periods or increased pain during periods
- Pain in the upper right abdomen (this is rare)
Most women have mild symptoms that may include 1 or more of the above symptoms. Pelvic inflammatory disease can come on fast, with extreme pain and fever, especially if it is caused by gonorrhea.
A few women become very ill with:
- severe lower abdominal pain
- a high temperature (fever)
- nausea and vomiting
If you have any of these symptoms, please see your doctor.
It’s important to visit your doctor or a sexual health clinic if you experience any of the above symptoms.
If you have severe pain, you should seek urgent medical attention from your doctor or local emergency department.
Delaying treatment for pelvic inflammatory disease or having repeated episodes of pelvic inflammatory disease can increase your risk of serious and long-term complications.
There’s no simple test to diagnose pelvic inflammatory disease. Diagnosis is based on your symptoms and the finding of tenderness on a vaginal (internal) examination.
Swabs will be taken from your vagina and cervix (neck of the womb), but negative swabs don’t rule out pelvic inflammatory disease.
Pelvic inflammatory disease diagnosis
It can be difficult for a woman to tell if they have pelvic inflammatory disease. Many women with pelvic inflammatory disease have subtle or nonspecific symptoms or are asymptomatic. Some women may not have any symptoms, particularly when pelvic inflammatory disease is caused by a chlamydia infection.
However, there’s no single test for diagnosing pelvic inflammatory disease (PID). Pelvic inflammatory disease is diagnosed based on your symptoms and a gynecological examination. Your doctor will first ask about your medical and sexual history.
The next step is to carry out a pelvic examination to check for any tenderness and abnormal vaginal discharge.
Pelvic inflammatory disease can be diagnosed by taking vaginal and cervical swabs, but may also require a pelvic examination or other tests, particularly if there are no symptoms.
You may experience some discomfort during this examination, particularly if you do have pelvic inflammatory disease.
Swabs are usually taken from the inside of your vagina and cervix. These are sent to a laboratory to look for signs of a bacterial infection and identify the bacteria responsible.
A positive test for chlamydia, gonorrhoea or mycoplasma genitalium supports the diagnosis of pelvic inflammatory disease.
But most women have negative swabs and this doesn’t rule out the diagnosis.
As pelvic inflammatory disease can be difficult to diagnose, other tests may also be required to look for signs of infection or inflammation, or rule out other possible causes of your symptoms.
These tests may include:
- a urine or blood test
- a pregnancy test
- an ultrasound scan, which is usually carried out using a probe passed through the vagina (transvaginal ultrasound)
Most women with pelvic inflammatory disease have either mucopurulent cervical discharge or evidence of white blood cells on a microscopic evaluation of a saline preparation of vaginal fluid (i.e., wet prep). If the cervical discharge appears normal and no white blood cells are observed on the wet prep of vaginal fluid, the diagnosis of pelvic inflammatory disease is unlikely, and alternative causes of pain should be considered. A wet prep of vaginal fluid also can detect the presence of concomitant infections (e.g., bacterial vaginosis and trichomoniasis).
The most specific criteria for diagnosing pelvic inflammatory disease include:
- endometrial biopsy with histopathologic evidence of endometritis;
- transvaginal ultrasound or magnetic resonance imaging (MRI) techniques showing thickened, fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex, or Doppler studies suggesting pelvic infection (e.g., tubal hyperemia); or
- laparoscopic findings consistent with pelvic inflammatory disease.
A diagnostic evaluation that includes some of these more extensive procedures might be warranted in some cases. Endometrial biopsy is warranted in women undergoing laparoscopy who do not have visual evidence of salpingitis, because endometritis is the only sign of pelvic inflammatory disease for some women.
In some cases, laparoscopy (keyhole surgery) may be used to diagnose pelvic inflammatory disease.
A laparoscopy is a minor operation where 2 small cuts are made in the abdomen.
A thin camera is inserted so the doctor can look at your internal organs and, if necessary, take tissue samples.
This is usually only done in more severe cases where there may be other possible causes of the symptoms, such as appendicitis.
Admission to hospital
You may be urgently admitted to hospital if:
- you’re pregnant (especially if there’s a chance you may have an ectopic pregnancy)
- your symptoms are severe (such as nausea, vomiting and a high fever)
- you have signs of pelvic peritonitis
- an abscess is suspected
- you’re unable to take oral antibiotics and need to be given them through a drip (intravenously)
- you may need emergency surgery, such as for appendicitis
To diagnose pelvic inflammatory disease, doctors usually do a physical exam to check for signs of pelvic inflammatory disease and test for sexually transmitted infections (STIs). If you think that you may have pelvic inflammatory disease, see a doctor or nurse as soon as possible.
If you have pain in your lower abdomen, your doctor or nurse will check for:
- Unusual discharge from your vagina or cervix
- An abscess (collection of pus) near your ovaries or fallopian tubes
- Tenderness or pain in your reproductive organs
Your doctor may do tests to find out whether you have pelvic inflammatory disease or a different problem that looks like pelvic inflammatory disease. These can include 192:
- Tests for sexually transmitted infections (STIs), especially gonorrhea and chlamydia. These infections can cause pelvic inflammatory disease.
- A test for a urinary tract infection or other conditions that can cause pelvic pain
- Ultrasound or another imaging test so your doctor can look at your internal organs for signs of pelvic inflammatory disease
A Pap test is not used to detect pelvic inflammatory disease.
Pelvic inflammatory disease treatment
If it’s diagnosed at an early stage, pelvic inflammatory disease (PID) can be treated easily and effectively with antibiotics.
These can be prescribed by your doctor or a doctor at a sexual health clinic. But left untreated, pelvic inflammatory disease (PID) can lead to more serious long-term complications.
Antibiotics
Treatment with antibiotics needs to be started quickly, before the results of the swabs are available.
Pelvic inflammatory disease is usually caused by a variety of different bacteria, even in cases where chlamydia, gonorrhoea or mycoplasma genitalium is identified.
This means you’ll be given a mixture of antibiotics to cover the most likely infections.
Antibiotics commonly prescribed to treat pelvic inflammatory disease include:
- Cefotetan
- Doxycycline
- Clindamycin
- Gentamicin
- Ceftriaxone
- Cefoxitin
- Azithromycin
- Metronidazole
Tell your doctor if you think you may be pregnant before starting antibiotic treatment, as some antibiotics should be avoided during pregnancy.
You’ll usually have to take the antibiotic tablets for 14 days, sometimes beginning with a single antibiotic injection.
It’s very important to complete the entire course of antibiotics, even if you’re feeling better, to help ensure the infection is properly cleared.
In particularly severe cases of pelvic inflammatory disease, you may have to be admitted to hospital to receive antibiotics through a drip in your arm (intravenously).
If you have pain around your pelvis or tummy, you can take painkillers such as paracetamol or ibuprofen while you’re being treated with antibiotics.
Parenteral Treatment
Several randomized trials have demonstrated the efficacy of parenteral regimens 201. Clinical experience should guide decisions regarding transition to oral therapy, which usually can be initiated within 24–48 hours of clinical improvement. In women with tubo-ovarian abscesses, at least 24 hours of inpatient observation is recommended.
Recommended Parenteral Regimens 192:
- Cefotetan 2 g IV every 12 hours PLUS Doxycycline 100 mg orally or IV every 12 hours
- OR
- Cefoxitin 2 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours
- OR
- Clindamycin 900 mg IV every 8 hours PLUS Gentamicin loading dose IV or IM (2 mg/kg), followed by a maintenance dose (1.5 mg/kg) every 8 hours. Single daily dosing (3–5 mg/kg) can be substituted.
Because of the pain associated with intravenous infusion, doxycycline should be administered orally when possible. Oral and IV administration of doxycycline provide similar bioavailability. Although use of a single daily dose of gentamicin has not been evaluated for the treatment of pelvic inflammatory disease, it is efficacious in analogous situations.
When using the parenteral cefotetan or cefoxitin regimens, oral therapy with doxycycline 100 mg twice daily can be used 24–48 hours after clinical improvement to complete the 14 days of therapy. For the clindamycin/gentamicin regimen, oral therapy with clindamycin (450 mg orally four times daily) or doxycycline (100 mg twice daily) can be used to complete the 14 days of therapy. However, when tubo-ovarian abscess is present, clindamycin (450 mg orally four times daily) or metronidazole (500 mg twice daily) should be used to complete at least 14 days of therapy with doxycycline to provide more effective anaerobic coverage than doxycycline alone.
Limited data are available to support use of other parenteral second- or third-generation cephalosporins (e.g., ceftizoxime, cefotaxime, and ceftriaxone). In addition, these cephalosporins are less active than cefotetan or cefoxitin against anaerobic bacteria.
Alternative Parenteral Regimens
Ampicillin/sulbactam plus doxycycline has been investigated in at least one clinical trial and has broad-spectrum coverage 202. Ampicillin/sulbactam plus doxycycline is effective against Chlamydia trachomatis, Neisseria gonorrhoeae, and anaerobes in women with tubo-ovarian abscess. Another trial demonstrated high short-term clinical cure rates with azithromycin, either as monotherapy for 1 week (500 mg IV daily for 1 or 2 doses followed by 250 mg orally for 5–6 days) or combined with a 12-day course of metronidazole 203. Limited data are available to support the use of other parenteral regimens.
Alternative Parenteral Regimen
- Ampicillin/Sulbactam 3 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours
Intramuscular/Oral Treatment
Intramuscular/oral therapy can be considered for women with mild-to-moderately severe acute pelvic inflammatory disease, because the clinical outcomes among women treated with these regimens are similar to those treated with intravenous therapy 187. Women who do not respond to IM/oral therapy within 72 hours should be reevaluated to confirm the diagnosis and should be administered intravenous therapy.
Recommended Intramuscular/Oral Regimens
- Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH* or WITHOUT Metronidazole 500 mg orally twice a day for 14 days
- OR
- Cefoxitin 2 g IM in a single dose and Probenecid, 1 g orally administered concurrently in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH or WITHOUT Metronidazole 500 mg orally twice a day for 14 days
- OR
- Other parenteral third-generation cephalosporin (e.g., ceftizoxime or cefotaxime) PLUS Doxycycline 100 mg orally twice a day for 14 days WITH* or WITHOUT Metronidazole 500 mg orally twice a day for 14 days
*The recommended third-generation cephalsporins are limited in the coverage of anaerobes. Therefore, until it is known that extended anaerobic coverage is not important for treatment of acute pelvic inflammatory disease, the addition of metronidazole to treatment regimens with third-generation cephalosporins should be considered 204.
These regimens provide coverage against frequent etiologic agents of pelvic inflammatory disease, but the optimal choice of a cephalosporin is unclear. Cefoxitin, a second-generation cephalosporin, has better anaerobic coverage than ceftriaxone, and in combination with probenecid and doxycycline has been effective in short-term clinical response in women with pelvic inflammatory disease. Ceftriaxone has better coverage against Neisseria gonorrhoeae. The addition of metronidazole will also effectively treat bacterial vaginosis, which is frequently associated with pelvic inflammatory disease.
Alternative IM/Oral Regimens
Although information regarding other IM and oral regimens is limited, a few have undergone at least one clinical trial and have demonstrated broad-spectrum coverage. Azithromycin has demonstrated short-term clinical effectiveness in one randomized trial when used as monotherapy (500 mg IV daily for 1–2 doses, followed by 250 mg orally daily for 12–14 days) or in combination with metronidazole 203, and in another study, it was effective when used 1 g orally once a week for 2 weeks in combination with ceftriaxone 250 mg IM single dose 205. When considering these alternative regimens, the addition of metronidazole should be considered to provide anaerobic coverage. No data have been published regarding the use of oral cephalosporins for the treatment of pelvic inflammatory disease. As a result of the emergence of quinolone-resistant Neisseria gonorrhoeae, regimens that include a quinolone agent are no longer routinely recommended for the treatment of pelvic inflammatory disease. If allergy precludes the use of cephalosporin therapy, if the community prevalence and individual risk for gonorrhea are low, and if follow-up is likely, use of fluoroquinolones for 14 days (levofloxacin 500 mg orally once daily, ofloxacin 400 mg twice daily, or moxifloxacin 400 mg orally once daily) with metronidazole for 14 days (500 mg orally twice daily) can be considered 206. Diagnostic tests for gonorrhea must be obtained before instituting therapy, and persons should be managed as follows.
- If the culture for gonorrhea is positive, treatment should be based on results of antimicrobial susceptibility testing.
- If the isolate is determined to be quinolone-resistant Neisseria gonorrhoeae or if antimicrobial susceptibility cannot be assessed (e.g., if only nucleic acid amplification test (NAAT) testing is available), consultation with an infectious-disease specialist is recommended.
Other Management Considerations
To minimize disease transmission, women should be instructed to abstain from sexual intercourse until therapy is completed, symptoms have resolved, and sex partners have been adequately treated. All women who received a diagnosis of acute pelvic inflammatory disease should be tested for HIV, as well as gonorrhea and chlamydia, using nucleic acid amplification test (NAAT).
Follow-up
In some cases, you may be advised to have a follow-up appointment 3 days after starting treatment so your doctor can check if the antibiotics are working. Women should demonstrate clinical improvement (e.g., defervescence; reduction in direct or rebound abdominal tenderness; and reduction in uterine, adnexal, and cervical motion tenderness) within 3 days after initiation of therapy.
If the antibiotics seem to be working, you may have another follow-up appointment at the end of the course to check if treatment has been successful.
If no clinical improvement has occurred within 72 hours after outpatient IM/oral therapy, hospitalization, assessment of the antimicrobial regimen, and additional diagnostics (including consideration of diagnostic laparoscopy for alternative diagnoses) are recommended. All women who have received a diagnosis of chlamydial or gonococcal pelvic inflammatory disease should be retested 3 months after treatment, regardless of whether their sex partners were treated (480). If retesting at 3 months is not possible, these women should be retested whenever they next present for medical care in the 12 months following treatment.
If you have an intrauterine device (IUD) fitted, you may be advised to have it removed if your symptoms haven’t improved within a few days, as it may be the cause of the infection.
Treating sexual partners
Any sexual partners you have been with in the 6 months before your symptoms started should be tested and treated to stop the infection recurring or being spread to others, even if no specific cause is identified. Men who have had sexual contact with a woman with pelvic inflammatory disease during the 60 days preceding her onset of symptoms should be evaluated, tested, and presumptively treated for chlamydia and gonorrhea, regardless of the etiology of pelvic inflammatory disease or pathogens isolated from the woman. If a woman’s last sexual intercourse was >60 days before onset of symptoms or diagnosis, the most recent sex partner should be treated.
Pelvic inflammatory disease can occur in long-term relationships where neither partner has had sex with anyone else.
It’s more likely to return if both partners aren’t treated at the same time.
Male partners of women who have pelvic inflammatory disease caused by Chlamydia trachomatis and/or Neisseria gonorrhoeae frequently are asymptomatic. Arrangements should be made to link male partners to care. If linkage is delayed or unlikely, Expedited Partner Therapy (EPT) and enhanced referral are alternative approaches to treating male partners of women who have chlamydia or gonococcal infections 207.
You and your partner should avoid having sex until you, your partner and their sex partners have completed the course of treatment (i.e., until therapy is completed and symptoms have resolved, if originally present).
If you haven’t had a sexual partner in the previous 6 months, your most recent partner should be tested and treated.
Your doctor or sexual health clinic can help you contact your previous partners.
Pregnancy
Pregnant women suspected to have pelvic inflammatory disease are at high risk for maternal morbidity and preterm delivery. These women should be hospitalized and treated with intravenous antibiotics.
HIV Infection
Differences in the clinical manifestations of pelvic inflammatory disease between women with HIV infection and women without HIV infection have not been well delineated. In early observational studies, women with HIV infection and pelvic inflammatory disease were more likely to require surgical intervention. More comprehensive observational and controlled studies have demonstrated that women with HIV infection and pelvic inflammatory disease have similar symptoms when compared with HIV-negative women with pelvic inflammatory disease 208, except they are more likely to have a tubo-ovarian abscess; women with HIV infection responded equally well to recommended parenteral and IM/oral antibiotic regimens as women without HIV infection. The microbiologic findings for women with HIV infection and women without HIV infection were similar, except women with HIV infection had higher rates of concomitant Mycoplasma hominis and streptococcal infections. These data are insufficient for determining whether women with HIV infection and pelvic inflammatory disease require more aggressive management (e.g., hospitalization or intravenous antimicrobial regimens).
Ectopic pregnancy
An ectopic pregnancy is when a fertilized egg (an embryo) implants itself outside of the womb (uterus), usually in one of the Fallopian tubes (uterine tubes) or less commonly it attaches to an ovary, the cervix or your abdomen (belly). These areas don’t have enough space or the right tissue for a baby to grow. Left untreated, ectopic pregnancy is a life threatening condition. It is the leading cause of death in the first trimester of pregnancy and the fourth leading cause of all maternal deaths in the United Kingdom. Ectopic pregnancy is also a leading cause of early pregnancy death in United States.
Ectopic pregnancy locations
In the vast majority of cases, the ectopic implantation site is within a Fallopian tube (uterine tubes).
- Fallopian tubal ectopic pregnancy: 93-97%
- Ampullary ectopic pregnancy: most common ~70% of tubal ectopics and ~65% of all ectopics
- Isthmal ectopic: ~12% of tubal ectopics and ~11% of all ectopics
- Fimbrial ectopic: ~11% of tubal ectopics and ~10% of all ectopics
- Interstitial ectopic/cornual ectopic pregnancy: 3-4%; also essentially a type of tubal ectopic
- Ovarian ectopic pregnancy: ovarian pregnancy; 0.5-1%
- Cervical ectopic pregnancy: cervical pregnancy; rare <1%
- Scar ectopic pregnancy: site of previous Caesarian section scar; rare
- Abdominal ectopic pregnancy: rare ~1.4%
Figure 25. Ectopic pregnancy
The fallopian tubes are the tubes connecting the ovaries to the womb. If an egg gets stuck in them, it won’t develop into a baby and your health may be at risk if the pregnancy continues. Without treatment, an ectopic pregnancy can cause the place where it’s attached to bleed heavily or burst. This can lead to serious bleeding and even death in the pregnant woman.
- Unfortunately, it’s not possible to save the pregnancy. An ectopic pregnancy always ends in pregnancy loss. Ectopic pregnancy usually has to be removed using medicine or an operation before it grows too large.
The main treatment options are:
- expectant management – your condition is carefully monitored to see whether treatment is necessary
- medication – a medicine called methotrexate is used to stop the pregnancy growing
- surgery – surgery is used to remove the pregnancy, usually along with the affected fallopian tube
These options each have advantages and disadvantages that your doctor will discuss with you.
In the US, the overall incidence has increased over the last few decades and is currently thought to affect 1-2% (around 1 in every 50) of pregnancies. The risk is as high as 18% for first trimester pregnancies with bleeding 209.
Increasing incidence of ectopic pregnancy is in part due to improvements in the way ectopic pregnancy is diagnosed (e.g. ultrasound, which is the usual way to diagnose ectopic pregnancy today, was much less accessible several decades ago). Other factors thought to play a role in the changing incidence of ectopic pregnancy include changes in smoking patterns in women and increased incidence of pelvic inflammatory disease (PID) and chlamydia trachomatis, a sexually transmitted infection (STI). There is also an increased incidence associated with in-vitro fertilisation (IVF) pregnancies.
An ectopic pregnancy may start out with usual signs and symptoms of pregnancy, like missing your period or having nausea (feeling sick to your stomach or morning sickness) and tender breasts. Or you may not have any signs or symptoms and not even know you’re pregnant.
- Light vaginal bleeding with abdominal or pelvic pain is often the first warning sign of an ectopic pregnancy.
- The most common symptoms of ectopic pregnancy are lower abdominal pain (reported by over 90% of women with ectopic pregnancy) and abnormal menstrual bleeding (reported by over 80% of women). If left untreated, the consequences of ectopic pregnancy include damage to the reproductive organs, reduced fertility and in the most severe cases, death.
Early treatment of an ectopic pregnancy can help preserve the chance for future healthy pregnancies.
Seek emergency medical help if you experience any signs or symptoms of an ectopic pregnancy, including:
- Severe abdominal or pelvic pain accompanied by vaginal bleeding
- Bleeding from the vagina
- Feeling faint, lightheadedness or dizzy. This can be caused by blood loss which can cause low blood pressure. Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body.
- Pain in your lower back or even your shoulder
- Pain in your pelvic area (the part of your body between the stomach and legs). The pain may be mainly on one side. It can come and go, start out mild and then become sharp and stabbing.
Who is at risk for having an ectopic pregnancy?
Any woman can have an ectopic pregnancy. But the risk is higher if you:
- Are older than 35. The risk of ectopic pregnancy increases with age. Women who are more than 40 years of age are 2.9 times more likely to develop an ectopic pregnancy if they become pregnant, than women who are 25-29 years.
- Smoking. A French study reported that cigarette smoking accounted for 35% of the risk associated with ectopic pregnancy. The more a woman smokes, the more likely she is to develop an ectopic pregnancy. Women who smoke more than 20 cigarettes per day are almost four times more likely to experience an ectopic pregnancy than those who have never smoked. Women who smoke less than 10 cigarettes per day are less than 2 times more likely to develop ectopic pregnancy than those who never smoked;
- Have more than one sex partner. This can put you at risk for getting a sexually transmitted infection (also called STI). An STI is an infection you can get from having sex with someone who is infected. Sexually transmitted infections can lead to pelvic inflammatory disease (also called PID), an infection that can damage the fallopian tubes, uterus and other organs.
- History of pelvic inflammatory disease. Pelvic inflammatory disease (PID) often leads to scarring and deformation of the pelvic cavity, which is thought to increase risk for ectopic pregnancy. A French study reported the risk of ectopic in women with a history of pelvic inflammatory disease to be 3.4 times higher than in women who had never experienced pelvic inflammatory disease.
- History of sexually transmitted infection (particularly chlamydia and gonorrhoea): Women with a history of sexually transmitted infection are more likely to develop an ectopic pregnancy and a history of multiple sexually transmitted infections may increase the risk even further. Sexually transmitted infections are associated with pelvic infection, post inflammatory scarring and distortion of normal reproductive anatomy which appear to cause the increased risk of ectopic pregnancy.
Medical conditions that increase your risk for having an ectopic pregnancy include:
- You’ve had a previous ectopic pregnancy.
- You’ve had surgery on a fallopian tube, or you have problems, like a birth defect in a fallopian tube. A birth defect is a health condition that is present at birth. It can change the shape or function of one or more parts of the body. It can cause problems in overall health, in how the body develops, or in how the body works.
- History of tubal surgery: Women who have undergone surgery involving the fallopian tubes are 4 times more likely to have an ectopic pregnancy than those who have not had tubal surgery;
- Sterilization: Pregnancy in general is uncommon following sterilization, however when it does occur, pregnancy is usually ectopic. Women sterilized using the bipolar coagulation technique had the highest rate of ectopic pregnancy following sterilization (17.3 events per 1000 sterilisations), while women sterilized by postpartum partial salpingectomy, had the lowest rate of ectopic pregnancy (1.5 per 1000). Women under 30 years of age at the time of sterilization had a higher risk of ectopic pregnancy than those who were aged 30 or more when sterilized.
- You have scars inside the pelvic area from a (ruptured) burst appendix or from past surgeries. Your appendix is part of your digestive tract that helps you process the food you eat.
- You’ve had endometriosis. This is when tissue from the uterus grows somewhere outside the uterus.
- You’ve had a history of infertility: Women who have been infertile in the past are more likely to develop an ectopic pregnancy than those who have not been infertile. The risk of developing an ectopic pregnancy increases with the number of years of infertility. Women who have been infertile for two or more years are 2.7 times more likely, women who have been infertile for 1-2 years are 2.6 times more likely, and those who have been infertile for less than one year 2.1 times more likely to develop an ectopic pregnancy than women who have never been infertile.
- You’ve had fertility treatment to help you get pregnant. Ectopic pregnancies account for some 4% of all pregnancies in women who have used assisted reproductive techniques, compared to estimated 2% of pregnancies in total.
- You got pregnant while using an intreauterine device (also called IUD) or after tubal ligation (also called having your tubes tied). An IUD is a form of birth control that your provider places inside your uterus. Tubal ligation is surgery to close the fallopian tubes to prevent you from getting pregnant. Women who have previously used an intrauterine device are 1.3 times more likely to develop an ectopic pregnancy than those who have not. When a woman who is using an intrauterine device becomes pregnant (a rare event), there is a high chance the pregnancy is ectopic.
- Previous miscarriage: The risk of ectopic pregnancy increases with the number of miscarriages a woman has previously experienced. Women who have experienced 1-2 miscarriages in the past are 1.2 times more likely to develop an ectopic pregnancy than women who have never miscarried. Three or more miscarriages in the past increases the risk of developing an ectopic pregnancy to three times that of women who have never had a miscarriage.
- Previous medically induced abortion: Women who have medically terminated a pregnancy are 2.8 times more likely to experience ectopic pregnancy than those who had never induced abortion. There is no increased risk associated with a history of induced surgical abortion.
If I’ve had an ectopic pregnancy before, can I go on to have a healthy pregnancy?
Yes. About 1 in 3 women (33 percent) who have had one ectopic pregnancy go on to have a healthy pregnancy later. Women who have had one ectopic pregnancy in the past are about seven times more likely to develop an ectopic pregnancy in the future than women who have never had an ectopic pregnancy. Women who have had two or more ectopic pregnancies in the past are over 70 times more likely to develop an ectopic pregnancy in the future.
Ectopic pregnancy causes
A tubal ectopic pregnancy — the most common type of ectopic pregnancy — happens when a fertilized egg gets stuck on its way to the uterus, often because the fallopian tube is damaged by inflammation or is misshapen. Hormonal imbalances or abnormal development of the fertilized egg also might play a role.
Risk factors for ectopic pregnancy
Various factors are associated with ectopic pregnancy, including:
- Are older than 35. The risk of ectopic pregnancy increases with age. Women who are more than 40 years of age are 2.9 times more likely to develop an ectopic pregnancy if they become pregnant, than women who are 25-29 years.
- In vitro fertilisation (IVF)
- Fertility issues. Some research suggests an association between difficulties with fertility — as well as use of fertility drugs — and ectopic pregnancy.
- Prior ectopic pregnancy. If you’ve had one ectopic pregnancy, you’re more likely to have another.
- Tubal injury or surgery / tubal ligation
- Pelvic inflammatory disease (sexually transmitted infections). Often, these infections are caused by gonorrhea or chlamydia. Pelvic inflammatory disease (PID) often leads to scarring and deformation of the pelvic cavity, which is thought to increase risk for ectopic pregnancy. A French study reported the risk of ectopic in women with a history of pelvic inflammatory disease to be 3.4 times higher than in women who had never experienced pelvic inflammatory disease.
- Salpingitis isthmica nodosa. Inflammation of the fallopian tube (salpingitis) or an infection of the uterus, fallopian tubes or ovaries (pelvic inflammatory disease) increases the risk of ectopic pregnancy.
- Endometrial injury or congenital anomalies. An ectopic pregnancy is more likely if you have an unusually shaped fallopian tube or the fallopian tube was damaged, possibly during surgery. Even surgery to reconstruct the fallopian tube can increase the risk of ectopic pregnancy.
- Use of intrauterine contraceptive devices. Pregnancy when using an intrauterine device (IUD) is rare. If pregnancy occurs, however, it’s more likely to be ectopic. The same goes for pregnancy after tubal ligation — a permanent method of birth control commonly known as “having your tubes tied.” Although pregnancy after tubal ligation is rare, if it happens, it’s more likely to be ectopic. Women who have previously used an intrauterine device are 1.3 times more likely to develop an ectopic pregnancy than those who have not. When a woman who is using an intrauterine device becomes pregnant (a rare event), there is a high chance the pregnancy is ectopic.
- Smoking. Cigarette smoking just before you get pregnant can increase the risk of an ectopic pregnancy. And the more you smoke, the greater the risk.
- Previous miscarriage: The risk of ectopic pregnancy increases with the number of miscarriages a woman has previously experienced. Women who have experienced 1-2 miscarriages in the past are 1.2 times more likely to develop an ectopic pregnancy than women who have never miscarried. Three or more miscarriages in the past increases the risk of developing an ectopic pregnancy to three times that of women who have never had a miscarriage.
- Previous medically induced abortion: Women who have medically terminated a pregnancy are 2.8 times more likely to experience ectopic pregnancy than those who had never induced abortion. There is no increased risk associated with a history of induced surgical abortion.
- History of tubal surgery: Women who have undergone surgery involving the fallopian tubes are 4 times more likely to have an ectopic pregnancy than those who have not had tubal surgery;
- Sterilization: Pregnancy in general is uncommon following sterilization, however when it does occur, pregnancy is usually ectopic. Women sterilized using the bipolar coagulation technique had the highest rate of ectopic pregnancy following sterilization (17.3 events per 1000 sterilisations), while women sterilized by postpartum partial salpingectomy, had the lowest rate of ectopic pregnancy (1.5 per 1000). Women under 30 years of age at the time of sterilization had a higher risk of ectopic pregnancy than those who were aged 30 or more when sterilized.
- History of sexually transmitted infection (particularly chlamydia and gonorrhoea): Women with a history of sexually transmitted infection are more likely to develop an ectopic pregnancy and a history of multiple sexually transmitted infections may increase the risk even further. Sexually transmitted infections are associated with pelvic infection, post inflammatory scarring and distortion of normal reproductive anatomy which appear to cause the increased risk of ectopic pregnancy.
- Many lifetime sexual partners.
- History of infertility: Women who have been infertile in the past are more likely to develop an ectopic pregnancy than those who have not been infertile. The risk of developing an ectopic pregnancy increases with the number of years of infertility. Women who have been infertile for two or more years are 2.7 times more likely, women who have been infertile for 1-2 years are 2.6 times more likely, and those who have been infertile for less than one year 2.1 times more likely to develop an ectopic pregnancy than women who have never been infertile.
- You’ve had fertility treatment to help you get pregnant. Ectopic pregnancies account for some 4% of all pregnancies in women who have used assisted reproductive techniques, compared to estimated 2% of pregnancies in total.
Ectopic pregnancy prevention
You can’t prevent an ectopic pregnancy, but you can decrease certain risk factors. For example, limit your number of sexual partners and use a condom when you have sex to help prevent sexually transmitted infections and reduce the risk of pelvic inflammatory disease. Quitting smoking before you attempt to get pregnant may also reduce your risk.
Ectopic pregnancy signs and symptoms
At first, an ectopic pregnancy might not cause any signs or symptoms and may only be detected during a routine pregnancy scan. Symptoms of an ectopic pregnancy usually develop between the 4th and 12th weeks of pregnancy.
In other cases, early signs and symptoms of an ectopic pregnancy might be the same as those of any pregnancy — a missed period, breast tenderness and nausea.
- You may have an ectopic pregnancy if you miss a period, have a positive pregnancy test, and have other signs of pregnancy, in addition to any of the symptoms listed below.
If you take a pregnancy test, the result will be positive. Still, an ectopic pregnancy can’t continue as normal.
Early signs of ectopic pregnancy
Light vaginal bleeding with abdominal or pelvic pain is often the first warning sign of an ectopic pregnancy. If blood leaks from the fallopian tube, it’s also possible to feel shoulder pain or an urge to have a bowel movement — depending on where the blood pools or which nerves are irritated. If the fallopian tube ruptures, heavy bleeding inside the abdomen is likely — followed by lightheadedness, fainting and shock.
Signs of ectopic pregnancy
If you do have symptoms, they tend to develop between the 4th and 12th week of pregnancy.
Symptoms can include a combination of:
- a missed period and other signs of pregnancy
- tummy pain low down on one side
- vaginal bleeding or a brown watery discharge
- pain in the tip of your shoulder
- discomfort when peeing or pooing
But these symptoms aren’t necessarily a sign of a serious problem. They can sometimes be caused by other problems, such as a stomach bug.
Vaginal bleeding
Vaginal bleeding tends to be a bit different to your regular period. It often starts and stops, and may be watery and dark brown in color.
Some women mistake this bleeding for a regular period and don’t realize they’re pregnant.
Vaginal bleeding during pregnancy is relatively common and isn’t necessarily a sign of a serious problem, but you should seek medical advice if you experience it.
Tummy pain
You may experience tummy pain, typically low down on one side. It can develop suddenly or gradually, and may be persistent or come and go.
Tummy pain can have lots of causes, including stomach bugs and trapped wind, so it doesn’t necessarily mean you have an ectopic pregnancy.
But you should get medical advice if you have it and think you might be pregnant.
Shoulder tip pain
Shoulder tip pain is an unusual pain felt where your shoulder ends and your arm begins.
It’s not known exactly why it occurs, but it can be a sign of an ectopic pregnancy causing some internal bleeding, so you should get medical advice right away if you experience it.
Discomfort when going to the toilet
You may experience pain when going for a pee or poo. You may also have diarrhea.
Some changes to your normal bladder and bowel patterns are normal during pregnancy, and these symptoms can be caused by urinary tract infections and stomach bugs.
But it’s still a good idea to seek medical advice if you experience these symptoms and think you might be pregnant.
Ruptured ectopic pregnancy
In a few cases, an ectopic pregnancy can grow large enough to split open the fallopian tube. This is known as a ruptured ectopic pregnancy.
Ruptures are very serious, and surgery to repair the fallopian tube needs to be carried out as soon as possible.
Signs of a ruptured ectopic pregnancy include a combination of:
- a sharp, sudden and intense pain in your tummy
- feeling very dizzy or fainting
- feeling sick
- looking very pale
Call your local emergency number for an ambulance or go to your nearest hospital accident and emergency (ER) department immediately if you experience these symptoms.
Ectopic pregnancy complications
When you have an ectopic pregnancy, the stakes are high. Without treatment, the embryo can grow too large to be accommodated by the surrounding organs. In this case the embryo can cause a rupture and considerably damage the reproductive organs. In very serious cases, ectopic pregnancy also poses a threat to the pregnant woman’s life because a ruptured fallopian tube could lead to life-threatening bleeding.
Ectopic pregnancy diagnosis
It can be difficult to diagnose an ectopic pregnancy from the symptoms alone, as they can be similar to other conditions.
If your doctor suspects an ectopic pregnancy, he or she might do a pelvic exam to check for pain, tenderness, or a mass in the fallopian tube or ovary. A physical exam alone usually isn’t enough to diagnose an ectopic pregnancy, however. The diagnosis is typically confirmed with blood tests and imaging studies, such as an ultrasound.
Ectopic pregnancy test
Your provider may do these tests to look for an ectopic pregnancy:
- A pelvic exam
- Blood tests to measure the levels of a pregnancy hormone called human chorionic gonadotropin (hCG). In an ectopic pregnancy the level of hCG tends to be lower and can cause hCG levels to rise more slowly than a healthy pregnancy. The results of the test can also be useful in determining the best treatment for an ectopic pregnancy.
- Ultrasound. This test uses sound waves and a computer screen to show a picture of your baby inside the womb. During an ultrasound, your health care provider uses a wand-like tool called a transducer on your belly (also called a transabdominal ultrasound) or inside the vagina (also called a transvaginal ultrasound). Providers often use transvaginal ultrasound to find an ectopic pregnancy because it can show a pregnancy earlier than a transabdominal ultrasound.
Sometimes it’s too soon to detect a pregnancy through ultrasound. If the diagnosis is in question, your doctor might monitor your condition with blood tests until the ectopic pregnancy can be confirmed or ruled out through ultrasound — usually by four to five weeks after conception. It’s hard to see a pregnancy less than 5 weeks after your last period. In an emergency situation — if you’re bleeding heavily, your provider may need to do surgery to diagnose and treat an ectopic pregnancy.
Ectopic pregnancy ultrasound
It is useful to know a quantitative beta HCG prior to scanning as this will guide what the sonographer expect to see. At levels <2000 IU, a normal early pregnancy may not be visible.
The most reliable sign of ectopic pregnancy is visualisation of an extra-uterine gestation, but this is not seen in 15-35% of ectopic pregnancies 210.
The ultrasound exam should be performed both transabdominally and transvaginally. The transabdominal component provides a wider overview of the abdomen, whereas a transvaginal scan is important for diagnostic sensitivity.
Positive sonographic findings include:
uterus
- empty uterine cavity or no evidence of intrauterine pregnancy
- pseudogestational sac or decidual cyst: may be seen in 10-20% of ectopic pregnancies
- current evidence suggests that one should not initiate treatment for an ectopic pregnancy in a hemodynamically stable woman on the basis of a single hCG value 211
- decidual cast
- thick echogenic endometrium
tube and ovary
- simple adnexal cyst: 10% chance of an ectopic pregnancy
- complex extra-adnexal cyst/mass: 95% chance of a tubal ectopic pregnancy (if no intra-uterine pregnancy)
- an intra-adnexal cyst/mass is more likely to be a corpus luteum
- solid hyperechoic mass is possible, but non-specific
- tubal ring sign
- 95% chance of a tubal ectopic pregnancy if seen
- described in 49% of ectopics and in 68% of unruptured ectopics
- ring of fire sign: can be seen on colour Doppler in a tubal ectopic pregnancy, but can also be seen in a corpus luteum
- absence of color Doppler flow does not exclude an ectopic pregnancy
- live extrauterine pregnancy (i.e. extra-uterine fetal cardiac activity): 100% specific, but only seen in a minority of cases
peritoneal cavity
- free pelvic fluid or hemoperitoneum in the pouch of Douglas
- the presence of free intraperitoneal fluid in the context of a positive beta HCG and empty uterus is
- ~70% specific for an ectopic pregnancy 4
- ~63% sensitive for ectopic pregnancy 4
- not specific for ruptured ectopic (seen in 37% of intact tubal ectopics)
- the presence of free intraperitoneal fluid in the context of a positive beta HCG and empty uterus is
- live pregnancy: 100% specific, but only seen in a minority of cases
In patients receiving in vitro fertilisation (IVF), it is important not to be completely reassured by the presence of a live intrauterine pregnancy 8, as there is a possibility of a coexisting ectopic pregnancy in ~1:500 (i.e. heterotopic pregnancy). In patients not receiving IVF, the risk of heterotopic pregnancy is minuscule (1:30,000).
Figure 26. Ectopic pregnancy ultrasound
Ectopic pregnancy treatment
A fertilized egg can’t develop normally outside the uterus. To prevent life-threatening complications, the ectopic tissue needs to be removed.
Expectant management
If you have no symptoms or mild symptoms and the pregnancy is very small or can’t be found, you may only need to be closely monitored, as there’s a good chance the pregnancy will dissolve by itself.
This is known as expectant management.
The following is likely to happen:
- You’ll have regular blood tests to check that the level of hCG in your blood is going down – these will be needed until the hormone is no longer found.
- You may need further treatment if your hormone level doesn’t go down or it increases.
- You’ll usually have some vaginal bleeding – use sanitary pads or towels, rather than tampons, until this clears up.
- You may experience some tummy pain – take paracetamol to relieve this.
- You’ll be told what to do if you develop more severe symptoms.
The main advantage of monitoring is that you won’t experience any side effects of treatment.
A disadvantage is that there’s still a small risk of your fallopian tubes splitting open (rupturing) and you may eventually need treatment.
There are two treatments for ectopic pregnancy:
- Medicine. Your doctor gives you an injection of medicine called methotrexate to stop the embryo from growing. This treatment works best if the embryo is small and in the fallopian tube. Methotrexate (a folate antagonist) either administered systemically or by direct ultrasound guided injection or potassium chloride (direct injection only obviously).
- Relative contraindications to methotrexate include 212:
- rupture
- mass >3.5 cm
- fetal cardiac activity
- bHCG >6000-15,000 mIU/mL
- Relative contraindications to methotrexate include 212:
- Surgery. Your doctor removes the embryo with surgical instruments placed through very small cuts in the belly. This type of surgery is called laparoscopic surgery.
These options each have advantages and disadvantages that your doctor will discuss with you.
They’ll recommend what they think is the most suitable option for you, depending on factors such as your symptoms, the size of the pregnancy, and the level of pregnancy hormone (human chorionic gonadotropin, or hCG) in your blood.
If the ectopic pregnancy is detected early, an injection of the drug methotrexate is sometimes used to stop cell growth and dissolve existing cells. It’s imperative that the diagnosis of ectopic pregnancy is certain before this treatment is undertaken. After the injection, your healthcare provider regularly checks your hCG levels until they return to zero. This can take a few weeks. If your levels stay high, it may mean that you still have ectopic tissue in your body. If so, you may need more treatment with methotrexate or surgery to remove the tissue.
If using the drug methotrexate, you’ll need to use reliable contraception for at least 3 months after treatment.
This is because methotrexate can be harmful for a baby if you become pregnant during this time.
It’s also important to avoid alcohol until you’re told it’s safe, as drinking soon after receiving a dose of methotrexate can damage your liver.
Other side effects of methotrexate include:
- tummy pain – this is usually mild and should pass within a day or two
- dizziness
- feeling and being sick
- diarrhea
There’s also a chance of your fallopian tubes rupturing after treatment. You’ll be told what to look out for and what to do if you think this has happened.
Ectopic pregnancy surgery
In most cases, ectopic pregnancy is usually treated with laparoscopic (keyhole) surgery. In this procedure, you’re given general anesthetic, so you’re asleep while it’s carried out and a small incision is made in the abdomen, near or in the navel. Then your doctor uses a thin tube equipped with a camera lens and light (laparoscope) to view the area.
Other instruments can be inserted into the tube or through other small incisions to remove the ectopic tissue and repair the fallopian tube. If the fallopian tube is significantly damaged, it might need to be removed.
Removing the affected fallopian tube is the most effective treatment and isn’t thought to reduce your chances of becoming pregnant again.
Your doctor will discuss this with you beforehand, and you’ll be asked whether you consent to having the Fallopian tube removed.
Most women can leave hospital a few days after surgery, although it can take 4 to 6 weeks to fully recover.
If the ectopic pregnancy is causing heavy bleeding or your fallopian tube has already ruptured, you’ll need emergency surgery.
The surgeon will make a larger incision in your tummy (laparotomy) to stop the bleeding and repair your fallopian tube, if that’s possible.
After either type of surgery, a treatment called anti-D rhesus prophylaxis will be given if your blood type is RhD negative. This involves an injection of a medicine that helps to prevent rhesus disease in future pregnancies.
Your doctor will monitor your HCG levels after surgery to be sure all of the ectopic tissue was removed. If HCG levels don’t come down quickly, an injection of methotrexate may be needed.
Coping and support
Losing a pregnancy is devastating, even if you’ve only known about it for a short time. Recognize the loss, and give yourself time to grieve. Talk about your feelings and allow yourself to experience them fully.
Rely on your partner, loved ones and friends for support. You might also seek the help of a support group, grief counselor or other mental health provider.
Most women who have ectopic pregnancies go on to have other, healthy pregnancies. If one fallopian tube was injured or removed, an egg can be fertilized in the other tube before entering the uterus.
If both fallopian tubes were injured or removed, in vitro fertilization might be an option. With this procedure, mature eggs are fertilized in a lab and then implanted into the uterus.
If you choose to conceive again, seek your doctor’s advice. Early blood tests and ultrasound imaging can offer prompt detection of another ectopic pregnancy — or reassurance that the pregnancy is developing normally.
Ectopic pregnancy prognosis
Ectopic pregnancy is potentially life threatening if left untreated, however a proportion of cases will resolve naturally and can be managed using expectant techniques (i.e. a “wait and see” approach, in which the woman is monitored for signs that the pregnancy has resolved). However in most cases ectopic pregnancies require either medical or surgical intervention. Both techniques are effective in removing the abnormal embryo and the majority of women are able to fall pregnant again after either medical or surgical treatments.
- American College of Obstetricians and Gynecologists. (2004). ACOG practice bulletin no. 51. Chronic pelvic pain. Obstetrics & Gynecology, 103, 589–605.[↩]
- ACOG Committee on Practice Bulletins–Gynecology. ACOG Practice Bulletin No. 51. Chronic pelvic pain. Obstet Gynecol. 2004 Mar;103(3):589-605.[↩][↩]
- What causes pelvic pain? https://www.nichd.nih.gov/health/topics/pelvicpain/conditioninfo/causes[↩]
- Pelvic Pain. https://www.ucsfhealth.org/conditions/pelvic-pain[↩][↩]
- Abdominal Adhesions. https://www.niddk.nih.gov/health-information/digestive-diseases/abdominal-adhesions[↩]
- Interstitial Cystitis (Bladder Pain Syndrome). https://www.niddk.nih.gov/health-information/urologic-diseases/interstitial-cystitis-bladder-pain-syndrome[↩]
- INTERDISCIPLINARY APPROACH TO PELVIC PAIN. https://www.pelvicpain.org/images/pdf/Patient%20Info%20Handouts%202023/INTERDISCIPLINARY%20APPROACH%20TO%20PELVIC%20PAIN%202023.pdf[↩]
- Farghaly SA. Current diagnosis and management of ovarian cysts. Clinical and Experimental Obstetrics & Gynecology. 2014 ;41(6):609-612.[↩][↩][↩]
- Kristjansdottir B, Levan K, Partheen K, Carlsohn E, Sundfeldt K. Potential tumor biomarkers identified in ovarian cyst fluid by quantitative proteomic analysis, iTRAQ. Clin Proteomics. 2013 Apr 4;10(1):4. doi: 10.1186/1559-0275-10-4[↩]
- Ovarian cysts. https://www.mayoclinic.org/diseases-conditions/ovarian-cysts/symptoms-causes/syc-20353405[↩]
- Ovarian Cysts. https://www.acog.org/womens-health/faqs/ovarian-cysts[↩][↩][↩]
- Lee S, Kim YH, Kim SC, Joo JK, Seo DS, Kim KH, Lee KS. The effect of tamoxifen therapy on the endometrium and ovarian cyst formation in patients with breast cancer. Obstet Gynecol Sci. 2018 Sep;61(5):615-620. doi: 10.5468/ogs.2018.61.5.615[↩][↩]
- Kelleher CM, Goldstein AM. Adnexal masses in children and adolescents. Clin Obstet Gynecol. 2015 Mar;58(1):76-92. doi: 10.1097/GRF.0000000000000084[↩]
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology. Practice Bulletin No. 174: Evaluation and Management of Adnexal Masses. Obstet Gynecol. 2016 Nov;128(5):e210-e226. doi: 10.1097/AOG.0000000000001768[↩]
- The Office on Women’s Health, U.S. Department of Health and Human Services. Ovarian cysts. https://www.womenshealth.gov/a-z-topics/ovarian-cysts[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Bottomley C, Bourne T. Diagnosis and management of ovarian cyst accidents. Best Pract Res Clin Obstet Gynaecol. 2009 Oct;23(5):711-24. doi: 10.1016/j.bpobgyn.2009.02.001[↩][↩][↩]
- Idris S, Daud S, Ahmad Sani N, Tee Mei Li S. A Case of Twisted Ovarian Cyst in a Young Patient and Review of the Literature. Am J Case Rep. 2021 Nov 17;22:e933438. doi: 10.12659/AJCR.933438[↩]
- Kolluru V, Gurumurthy R, Vellanki V, Gururaj D. Torsion of ovarian cyst during pregnancy: a case report. Cases J. 2009 Dec 31;2:9405. doi: 10.1186/1757-1626-2-9405[↩]
- Mayo Foundation for Medical Education and Research. Ovarian cysts. http://www.mayoclinic.org/diseases-conditions/ovarian-cysts/home/ovc-20341904[↩][↩]
- Ross, E.K. (2013). Incidental Ovarian Cysts: When to Reassure, When to Reassess, When to Refer. Cleveland Clinic Journal of Medicine; 80(8): 503–514. https://www.ncbi.nlm.nih.gov/pubmed/23908107[↩]
- Kiemtoré S, Zamané H, Sawadogo YA, Sib RS, Komboigo E, Ouédraogo A, Bonané B. Diagnosis and management of a giant ovarian cyst in the gravid-puerperium period: a case report. BMC Pregnancy Childbirth. 2019 Dec 26;19(1):523. doi: 10.1186/s12884-019-2678-8[↩]
- De Lima SHM, dos Santos VM, Daros AC, Campos VP, Modesto FRD. A 57-year-old Brazilian woman with a giant mucinous cystadenocarcinoma of the ovary: a case report. J Med Case Rep. 2014;4:82. doi: 10.1186/1752-1947-8-82[↩]
- Bhasin S k, Kumar V, Kumar R. Giant ovarian cyst: a case report. JK Sci. 2014;16:3.[↩]
- Ovarian Cysts. https://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/womens-health/ovarian-cysts[↩][↩][↩][↩][↩]
- U.S. Preventive Services Task Force (2016). Screening for Ovarian Cancer. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/ovarian-cancer-screening[↩]
- Horowitz, N.S. (2011). Management of adnexal masses in pregnancy. Clinical Obstetrics & Gynecology; 54: 519–527. https://www.ncbi.nlm.nih.gov/pubmed/22031242[↩]
- Cicchiello LA, Hamper UM, Scoutt LM. Ultrasound evaluation of gynecologic causes of pelvic pain. Obstet Gynecol Clin North Am. 2011 Mar;38(1):85-114, viii. doi: 10.1016/j.ogc.2011.02.005[↩][↩]
- Amirbekian S, Hooley RJ. Ultrasound evaluation of pelvic pain. Radiol Clin North Am. 2014 Nov;52(6):1215-35. doi: 10.1016/j.rcl.2014.07.008[↩][↩]
- Morgan M, Molinari A, Jones J, et al. Ruptured ovarian cyst. https://radiopaedia.org/articles/33379[↩][↩][↩][↩]
- Guile SL, Mathai JK. Ovarian Torsion. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560675[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Chang HC, Bhatt S, Dogra VS. Pearls and pitfalls in diagnosis of ovarian torsion. Radiographics 2008;28:1355-68. 10.1148/rg.285075130[↩][↩]
- Feng JL, Zheng J, Lei T, Xu YJ, Pang H, Xie HN. Comparison of ovarian torsion between pregnant and non-pregnant women at reproductive ages: sonographic and pathological findings. Quant Imaging Med Surg. 2020 Jan;10(1):137-147. doi: 10.21037/qims.2019.11.06[↩][↩][↩][↩]
- Growdon Whitfield B, Laufer Marc R. Ovarian and fallopian tube torsion. Uptodate. 2013;4:1–18.[↩]
- Mahonski S, Hu KM. Female Nonobstetric Genitourinary Emergencies. Emerg Med Clin North Am. 2019 Nov;37(4):771-784. doi: 10.1016/j.emc.2019.07.012[↩][↩][↩]
- Varras M, Tsikini A, Polyzos D, Samara Ch, Hadjopoulos G, Akrivis Ch. Uterine adnexal torsion: pathologic and gray-scale ultrasonographic findings. Clin Exp Obstet Gynecol. 2004;31(1):34-8.[↩]
- Nair S, Joy S, Nayar J. Five year retrospective case series of adnexal torsion. J Clin Diagn Res. 2014 Dec;8(12):OC09-13. doi: 10.7860/JCDR/2014/9464.5251[↩]
- Huchon C, Fauconnier A. Adnexal torsion: a literature review. Eur J Obstet Gynecol Reprod Biol 2010;150:8-12. 10.1016/j.ejogrb.2010.02.006[↩]
- Erdemoğlu M, Kuyumcuoglu U, Guzel AI. Clinical experience of adnexal torsion: evaluation of 143 cases. J Exp Ther Oncol. 2011;9(3):171-4.[↩]
- Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann Emerg Med 2001;38:156-9. 10.1067/mem.2001.114303[↩]
- Bider D, Mashiach S, Dulitzky M, Kokia E, Lipitz S, Ben-Rafael Z. Clinical, surgical and pathologic findings of adnexal torsion in pregnant and nonpregnant women. Surg Gynecol Obstet. 1991 Nov;173(5):363-6.[↩][↩]
- Feng JL, Lei T, Xie HN, Li LJ, Du L. Spectrums and Outcomes of Adnexal Torsion at Different Ages. J Ultrasound Med 2017;36:1859-66. 10.1002/jum.14225[↩]
- Oelsner G, Shashar D. Adnexal torsion. Clin Obstet Gynecol 2006;49:459-63. 10.1097/00003081-200609000-00006[↩]
- Yuk JS, Shin JY, Park WI, Kim DW, Shin JW, Lee JH. Association between pregnancy and adnexal torsion: A population-based, matched case-control study. Medicine 2016;95:e3861. 10.1097/MD.0000000000003861[↩]
- Valsky DV, Esh-Broder E, Cohen SM, Lipschuetz M, Yagel S. Added value of the gray-scale whirlpool sign in the diagnosis of adnexal torsion. Ultrasound Obstet Gynecol 2010;36:630-4. 10.1002/uog.7732[↩]
- Gerscovich EO, Corwin MT, Sekhon S, Runner GJ, Gandour-Edwards RF. Sonographic appearance of adnexal torsion, correlation with other imaging modalities, and clinical history. Ultrasound Q 2014;30:49-55. 10.1097/RUQ.0000000000000049[↩]
- Mashiach R, Melamed N, Gilad N, Ben-Shitrit G, Meizner I. Sonographic diagnosis of ovarian torsion accuracy and predictive factors. J Ultrasound Med 2011;30:1205-10. 10.7863/jum.2011.30.9.1205[↩]
- Cohen A, Solomon N, Almog B, Cohen Y, Tsafrir Z, Rimon E, Levin I. Adnexal Torsion in Postmenopausal Women: Clinical Presentation and Risk of Ovarian Malignancy. J Minim Invasive Gynecol. 2017 Jan 1;24(1):94-97. doi: 10.1016/j.jmig.2016.09.019[↩]
- Schwartz BI, Huppert JS, Chen C, Huang B, Reed JL. Creation of a Composite Score to Predict Adnexal Torsion in Children and Adolescents. J Pediatr Adolesc Gynecol. 2018 Apr;31(2):132-137. doi: 10.1016/j.jpag.2017.08.007[↩]
- Gabriel Oelsner, Shlomo B. Cohen, David Soriano, Dahlia Admon, Shlomo Mashiach, Howard Carp, Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function, Human Reproduction, Volume 18, Issue 12, 1 December 2003, Pages 2599–2602, https://doi.org/10.1093/humrep/deg498[↩]
- Oelsner G, Bider D, Goldenberg M, Admon D, Mashiach S. Long-term follow-up of the twisted ischemic adnexa managed by detorsion. Fertil Steril. 1993 Dec;60(6):976-9. doi: 10.1016/s0015-0282(16)56395-x[↩]
- Wang JH, Wu DH, Jin H, Wu YZ. Predominant etiology of adnexal torsion and ovarian outcome after detorsion in premenarchal girls. Eur J Pediatr Surg. 2010 Sep;20(5):298-301. doi: 10.1055/s-0030-1254110[↩]
- Pryor RA, Wiczyk HP, O’Shea DL. Adnexal infarction after conservative surgical management of torsion of a hyperstimulated ovary. Fertil Steril. 1995 Jun;63(6):1344-6. doi: 10.1016/s0015-0282(16)57624-9[↩]
- Mobeen S, Apostol R. Ovarian Cyst. [Updated 2022 Jun 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560541[↩][↩][↩][↩][↩][↩]
- Jain, K.A. (2002), Sonographic Spectrum of Hemorrhagic Ovarian Cysts. Journal of Ultrasound in Medicine, 21: 879-886. https://doi.org/10.7863/jum.2002.21.8.879[↩]
- Khati NJ, Kim T, Riess J. Imaging of Benign Adnexal Disease. Radiol Clin North Am. 2020 Mar;58(2):257-273. doi: 10.1016/j.rcl.2019.10.009[↩]
- Nezhat F, Apostol R, Mahmoud M, el Daouk M. Malignant transformation of endometriosis and its clinical significance. Fertil Steril. 2014 Aug;102(2):342-4. doi: 10.1016/j.fertnstert.2014.04.050[↩]
- Nezhat FR, Apostol R, Nezhat C, Pejovic T. New insights in the pathophysiology of ovarian cancer and implications for screening and prevention. Am J Obstet Gynecol. 2015 Sep;213(3):262-7. doi: 10.1016/j.ajog.2015.03.044[↩]
- Killackey MA, Neuwirth RS. Evaluation and management of the pelvic mass: a review of 540 cases. Obstet Gynecol. 1988 Mar;71(3 Pt 1):319-22.[↩]
- Pradhan P, Thapa M. Dermoid Cyst and its bizarre presentation. JNMA J Nepal Med Assoc. 2014 Apr-Jun;52(194):837-44.[↩]
- Mayo Foundation for Medical Education and Research. Symptoms and causes of Ovarian cysts. http://www.mayoclinic.org/diseases-conditions/ovarian-cysts/symptoms-causes/dxc-20341906[↩]
- Manique MES, Ferreira AMAP. Polycystic Ovary Syndrome in Adolescence: Challenges in Diagnosis and Management. Rev Bras Ginecol Obstet. 2022 Apr;44(4):425-433. English. doi: 10.1055/s-0042-1742292[↩]
- Jones HW, Rock JA, eds. Te Linde’s Operative Gynecology, 11th ed. Philadelphia, PA: Wolters Kluwer; 2015.[↩]
- Pakhomov SP, Orlova VS, Verzilina IN, Sukhih NV, Nagorniy AV, Matrosova AV. Risk Factors and Methods for Predicting Ovarian Hyperstimulation Syndrome (OHSS) in the in vitro Fertilization. Arch Razi Inst. 2021 Nov 30;76(5):1461-1468. doi: 10.22092/ari.2021.355581.1700[↩]
- Stany MP, Hamilton CA. Benign disorders of the ovary. Obstet Gynecol Clin North Am. 2008 Jun;35(2):271-84, ix. doi: 10.1016/j.ogc.2008.03.004[↩]
- Figg WD 2nd, Cook K, Clarke R. Aromatase inhibitor plus ovarian suppression as adjuvant therapy in premenopausal women with breast cancer. Cancer Biol Ther. 2014;15(12):1586-7. doi: 10.4161/15384047.2014.972783[↩]
- LE Donne M, Alibrandi A, Ciancimino L, Azzerboni A, Chiofalo B, Triolo O. Endometrial pathology in breast cancer patients: Effect of different treatments on ultrasonographic, hysteroscopic and histological findings. Oncol Lett. 2013 Apr;5(4):1305-1310. doi: 10.3892/ol.2013.1156[↩]
- Tresa A, Rema P, Suchetha S, Dinesh D, Sivaranjith J, Nath AG. Hypothyroidism Presenting as Ovarian Cysts-a Case Series. Indian J Surg Oncol. 2021 Dec;12(Suppl 2):343-347. doi: 10.1007/s13193-020-01263-8[↩]
- Heling, K.-.-S., Chaoui, R., Kirchmair, F., Stadie, S. and Bollmann, R. (2002), Fetal ovarian cysts: prenatal diagnosis, management and postnatal outcome. Ultrasound Obstet Gynecol, 20: 47-50. https://doi.org/10.1046/j.1469-0705.2002.00725.x[↩]
- Victoria L. Holt, Kara L. Cushing-Haugen, Janet R. Daling, Risk of Functional Ovarian Cyst: Effects of Smoking and Marijuana Use according to Body Mass Index, American Journal of Epidemiology, Volume 161, Issue 6, 15 March 2005, Pages 520–525, https://doi.org/10.1093/aje/kwi080[↩]
- Holt VL, Cushing-Haugen KL, Daling JR. Oral contraceptives, tubal sterilization, and functional ovarian cyst risk. Obstet Gynecol. 2003 Aug;102(2):252-8. doi: 10.1016/s0029-7844(03)00572-6[↩]
- Grimes DA, Jones LB, Lopez LM, Schulz KF. Oral contraceptives for functional ovarian cysts. Cochrane Database Syst Rev. 2014 Apr 29;(4):CD006134. doi: 10.1002/14651858.CD006134.pub5[↩]
- Young RL, Snabes MC, Frank ML, Reilly M. A randomized, double-blind, placebo-controlled comparison of the impact of low-dose and triphasic oral contraceptives on follicular development. Am J Obstet Gynecol. 1992 Sep;167(3):678-82. doi: 10.1016/s0002-9378(11)91570-1[↩]
- Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development. The reduction in risk of ovarian cancer associated with oral-contraceptive use. N Engl J Med. 1987 Mar 12;316(11):650-5. doi: 10.1056/NEJM198703123161102[↩]
- Parker WH, Broder MS, Chang E, Feskanich D, Farquhar C, Liu Z, Shoupe D, Berek JS, Hankinson S, Manson JE. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses’ health study. Obstet Gynecol. 2009 May;113(5):1027-1037. doi: 10.1097/AOG.0b013e3181a11c64[↩]
- Kurman RJ, Shih IeM. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010 Mar;34(3):433-43. doi: 10.1097/PAS.0b013e3181cf3d79[↩]
- Ovarian cancer: recognition and initial management. https://www.nice.org.uk/guidance/cg122[↩][↩]
- Ross EK, Kebria M. Incidental ovarian cysts: when to reassure, when to reassess, when to refer. Cleve Clin J Med 2013; 80:503–514.[↩]
- Kinkel K, Lu Y, Mehdizade A, Pelte MF, Hricak H. Indeterminate ovarian mass at US: incremental value of second imaging test for characterization–meta-analysis and Bayesian analysis. Radiology. 2005 Jul;236(1):85-94. https://doi.org/10.1148/radiol.2361041618[↩]
- Timmerman D, Van Calster B, Testa A, Savelli L, Fischerova D, Froyman W, Wynants L, Van Holsbeke C, Epstein E, Franchi D, Kaijser J, Czekierdowski A, Guerriero S, Fruscio R, Leone FPG, Rossi A, Landolfo C, Vergote I, Bourne T, Valentin L. Predicting the risk of malignancy in adnexal masses based on the Simple Rules from the International Ovarian Tumor Analysis group. Am J Obstet Gynecol. 2016 Apr;214(4):424-437. doi: 10.1016/j.ajog.2016.01.007[↩]
- Srivastava, S., Kumar, P., Chaudhry, V. et al. Detection of Ovarian Cyst in Ultrasound Images Using Fine-Tuned VGG-16 Deep Learning Network. SN COMPUT. SCI. 1, 81 (2020). https://doi.org/10.1007/s42979-020-0109-6[↩]
- Ovarian follicular cyst. https://radiopaedia.org/cases/ovarian-follicular-cyst-1[↩]
- Ruptured hemorrhagic corpus luteal cyst. https://radiopaedia.org/cases/ruptured-haemorrhagic-corpus-luteal-cyst[↩]
- Yazici B, Erdoğmuş B. Floating ball appearance in ovarian cystic teratoma. Diagn Interv Radiol. 2006 Sep;12(3):136-8.[↩]
- Muramatsu Y, Moriyama N, Takayasu K, Nawano S, Yamada T. CT and MR imaging of cystic ovarian teratoma with intracystic fat balls. J Comput Assist Tomogr. 1991 May-Jun;15(3):528-9.[↩]
- Mature cystic ovarian teratoma – floating ball appearance. https://radiopaedia.org/cases/mature-cystic-ovarian-teratoma-floating-ball-appearance[↩]
- Endometrioma. https://radiopaedia.org/cases/endometrioma[↩]
- Ovarian malignancy. https://radiopaedia.org/cases/ovarian-malignancy?lang=us[↩]
- Ross EK, Kebria M. Incidental ovarian cysts: When to reassure, when to reassess, when to refer. Cleve Clin J Med. 2013 Aug;80(8):503-14. doi: 10.3949/ccjm.80a.12155[↩][↩]
- Mayo Foundation for Medical Education and Research. Treatment of Ovarian cysts. http://www.mayoclinic.org/diseases-conditions/ovarian-cysts/diagnosis-treatment/treatment/txc-20341929[↩]
- NIH consensus conference (1995). Ovarian cancer: screening, treatment, and follow-up. NIH Consensus Development Panel on Ovarian Cancer. JAMA; 273: 491–497. https://www.ncbi.nlm.nih.gov/pubmed/7837369[↩]
- Engelen, M.J.A., Kos, H.E., Willemse, P.H.B., Aalders, J.G., de Vries, E.G.E., Schaapveld, M., Otter, R. and van der Zee, A.G.J. (2006), Surgery by consultant gynecologic oncologists improves survival in patients with ovarian carcinoma. Cancer, 106: 589-598. https://doi.org/10.1002/cncr.21616[↩]
- Giede KC, Kieser K, Dodge J, Rosen B. Who should operate on patients with ovarian cancer? An evidence-based review. Gynecol Oncol. 2005 Nov;99(2):447-61. doi: 10.1016/j.ygyno.2005.07.008[↩]
- Vernooij F, Heintz P, Witteveen E, van der Graaf Y. The outcomes of ovarian cancer treatment are better when provided by gynecologic oncologists and in specialized hospitals: a systematic review. Gynecol Oncol. 2007 Jun;105(3):801-12. doi: 10.1016/j.ygyno.2007.02.030[↩]
- Liu JH, Zanotti KM. Management of the adnexal mass. Obstet Gynecol. 2011 Jun;117(6):1413-1428. doi: 10.1097/AOG.0b013e31821c62b6[↩]
- Glanc P, Salem S, Farine D. Adnexal masses in the pregnant patient: a diagnostic and management challenge. Ultrasound Q. 2008 Dec;24(4):225-40. doi: 10.1097/RUQ.0b013e31819032f[↩]
- Ovarian Torsion. https://emedicine.medscape.com/article/2026938-overview[↩]
- Naffaa L, Deshmukh T, Tumu S, Johnson C, Boyd KP, Meyers AB. Imaging of Acute Pelvic Pain in Girls: Ovarian Torsion and Beyond☆. Curr Probl Diagn Radiol. 2017 Jul – Aug. 46 (4):317-329.[↩]
- Bider D, Mashiach S, Dulitzky M et-al. Clinical, surgical and pathologic findings of adnexal torsion in pregnant and nonpregnant women. Surg Gynecol Obstet. 1991;173 (5): 363-6[↩]
- Griffin D, Shiver SA. Unusual presentation of acute ovarian torsion in an adolescent. Am J Emerg Med. 2008 May. 26(4):520.e1-3.[↩][↩]
- Huang TY, Lau BH, Lin LW, Wang TL, Chong CF, Chen CC. Ovarian cyst torsion in a toddler. Am J Emerg Med. 2009 Jun. 27(5):632.e1-3.[↩]
- Dähnert W. Radiology Review Manual. Hubsta Ltd. (2007) ISBN:0781766206[↩]
- Amirbekian S, Hooley RJ. Ultrasound Evaluation of Pelvic Pain. Radiol. Clin. North Am. 2014;52 (6): 1215-1235. doi:10.1016/j.rcl.2014.07.008[↩]
- Asfour V, Varma R, Menon P. Clinical risk factors for ovarian torsion. J Obstet Gynaecol. 2015. 35 (7):721-5[↩]
- Ashwal E, Hiersch L, Krissi H, Eitan R, Less S, Wiznitzer A, et al. Characteristics and Management of Ovarian Torsion in Premenarchal Compared With Postmenarchal Patients. Obstet Gynecol. 2015 Sep. 126 (3):514-20[↩]
- Ashwal E, Krissi H, Hiersch L, Less S, Eitan R, Peled Y. Presentation, Diagnosis, and Treatment of Ovarian Torsion in Premenarchal Girls. J Pediatr Adolesc Gynecol. 2015 Mar 28.[↩]
- Ganer Herman H, Shalev A, Ginat S, Kerner R, Keidar R, Bar J, et al. Clinical characteristics of adnexal torsion in premenarchal patients. Arch Gynecol Obstet. 2016 Mar. 293 (3):603-8.[↩]
- Koumoutsea EV, Gupta M, Hollingworth A, Gorry A. Ovarian Torsion in the Third Trimester of Pregnancy Leading to Iatrogenic Preterm Delivery. Case Rep Obstet Gynecol. 2016. 2016:8426270.[↩]
- Sonographic whirlpool sign in ovarian torsion. J Ultrasound Med. 2004 Dec;23(12):1643-9; quiz 1650-1. https://doi.org/10.7863/jum.2004.23.12.1643[↩]
- Duigenan S, Oliva E, Lee SI. Ovarian torsion: diagnostic features on CT and MRI with pathologic correlation. AJR Am J Roentgenol. 2012;198 (2): W122-31. doi:10.2214/AJR.10.7293[↩]
- Ovarian torsion. https://radiopaedia.org/cases/ovarian-torsion-6 [↩]
- Chiou SY, Lev-toaff AS, Masuda E et-al. Adnexal torsion: new clinical and imaging observations by sonography, computed tomography, and magnetic resonance imaging. J Ultrasound Med. 2007;26 (10): 1289-301.[↩]
- Mashiach R, Melamed N, Gilad N, Ben-Shitrit G, Meizner I. Sonographic diagnosis of ovarian torsion: accuracy and predictive factors. J Ultrasound Med. 2011 Sep. 30(9):1205-10.[↩]
- Van Kerkhove F, Cannie M, Op de Beeck K, Timmerman D, Pienaar A, Smet MH, et al. Ovarian torsion in a premenarcheal girl: MRI findings. Abdom Imaging. 2007 May-Jun. 32(3):424-7[↩]
- Anders JF, Powell EC. Urgency of evaluation and outcome of acute ovarian torsion in pediatric patients. Arch Pediatr Adolesc Med. 2005 Jun. 159(6):532-5.[↩]
- Hasson J, Tsafrir Z, Azem F, Bar-On S, Almog B, Mashiach R, et al. Comparison of adnexal torsion between pregnant and nonpregnant women. Am J Obstet Gynecol. 2010 Jun. 202(6):536.e1-6.[↩]
- Key Statistics for Ovarian Cancer. https://www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html[↩][↩]
- Ovarian Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/ovary.html[↩][↩][↩][↩][↩]
- What is ovarian cancer? https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/what-is-ovarian-cancer[↩]
- Ovarian Cancer Stages. https://www.cancer.org/cancer/ovarian-cancer/detection-diagnosis-staging/staging.html[↩]
- Arora T, Mullangi S, Lekkala MR. Ovarian Cancer. [Updated 2022 Aug 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567760[↩]
- Stewart C, Ralyea C, Lockwood S. Ovarian Cancer: An Integrated Review. Semin Oncol Nurs. 2019 Apr;35(2):151-156. doi: 10.1016/j.soncn.2019.02.001[↩]
- Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. Lancet. 2014 Oct 11;384(9951):1376-88. doi: 10.1016/S0140-6736(13)62146-7[↩]
- Griffiths RW, Zee YK, Evans S, Mitchell CL, Kumaran GC, Welch RS, Jayson GC, Clamp AR, Hasan J. Outcomes after multiple lines of chemotherapy for platinum-resistant epithelial cancers of the ovary, peritoneum, and fallopian tube. Int J Gynecol Cancer. 2011 Jan;21(1):58-65. doi: 10.1097/IGC.0b013e3182049273[↩]
- Chang SJ, Hodeib M, Chang J, Bristow RE. Survival impact of complete cytoreduction to no gross residual disease for advanced-stage ovarian cancer: a meta-analysis. Gynecol Oncol. 2013 Sep;130(3):493-8. doi: 10.1016/j.ygyno.2013.05.040[↩]
- Carpinello OJ, Sundheimer LW, Alford CE, et al. Endometriosis. [Updated 2017 Oct 22]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278996[↩]
- Tsamantioti ES, Mahdy H. Endometriosis. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567777[↩]
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Overview: Endometriosis. [Updated 2021 Mar 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279501[↩]
- Becker CM, Bokor A, Heikinheimo O, Horne A, Jansen F, Kiesel L, King K, Kvaskoff M, Nap A, Petersen K, Saridogan E, Tomassetti C, van Hanegem N, Vulliemoz N, Vermeulen N; ESHRE Endometriosis Guideline Group. ESHRE guideline: endometriosis. Hum Reprod Open. 2022 Feb 26;2022(2):hoac009. doi: 10.1093/hropen/hoac009[↩]
- Giudice LC, Oskotsky TT, Falako S, Opoku-Anane J, Sirota M. Endometriosis in the era of precision medicine and impact on sexual and reproductive health across the lifespan and in diverse populations. FASEB J. 2023 Sep;37(9):e23130. doi: 10.1096/fj.202300907[↩]
- Brown J, Farquhar C. Endometriosis: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2014 Mar 10;2014(3):CD009590. doi: 10.1002/14651858.CD009590.pub2[↩][↩]
- Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020 Mar 26;382(13):1244-1256. doi: 10.1056/NEJMra1810764[↩][↩]
- Endometriosis. Medline Plus. https://medlineplus.gov/endometriosis.html[↩]
- Endometriosis. https://womenshealth.gov/a-z-topics/endometriosis[↩][↩]
- Buck, L.G.M., Hediger, M.L., Peterson, C.M., Croughan, M., Sundaram, R., Stanford, J., Chen, Z., et al. (2011). Incidence of endometriosis by study population and diagnostic method: the ENDO study. Fertility and Sterility; 96(2): 360-5. https://pmc.ncbi.nlm.nih.gov/articles/PMC3143230[↩]
- Nnoaham KE, Hummelshoj L, Webster P, d’Hooghe T, de Cicco Nardone F, de Cicco Nardone C, Jenkinson C, Kennedy SH, Zondervan KT; World Endometriosis Research Foundation Global Study of Women’s Health consortium. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2011 Aug;96(2):366-373.e8. doi: 10.1016/j.fertnstert.2011.05.090[↩]
- Buck Louis GM, Hediger ML, Peterson CM, Croughan M, Sundaram R, Stanford J, Chen Z, Fujimoto VY, Varner MW, Trumble A, Giudice LC; ENDO Study Working Group. Incidence of endometriosis by study population and diagnostic method: the ENDO study. Fertil Steril. 2011 Aug;96(2):360-5. https://pmc.ncbi.nlm.nih.gov/articles/PMC3143230[↩]
- Ghiasi M, Kulkarni MT, Missmer SA. Is Endometriosis More Common and More Severe Than It Was 30 Years Ago? J Minim Invasive Gynecol. 2020 Feb;27(2):452-461. doi: 10.1016/j.jmig.2019.11.018[↩]
- Parazzini F, Roncella E, Cipriani S, Trojano G, Barbera V, Herranz B, Colli E.. The frequency of endometriosis in the general and selected populations: a systematic review. J Endometriosis Pelvic Pain Disorders 2020;12:176–189.[↩]
- Sarria-Santamera A, Orazumbekova B, Terzic M, Issanov A, Chaowen C, Asúnsolo-Del-Barco A. Systematic Review and Meta-Analysis of Incidence and Prevalence of Endometriosis. Healthcare (Basel). 2020 Dec 30;9(1):29. doi: 10.3390/healthcare9010029[↩]
- Janssen EB, Rijkers AC, Hoppenbrouwers K, Meuleman C, D’Hooghe TM. Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: a systematic review. Hum Reprod Update. 2013 Sep-Oct;19(5):570-82. doi: 10.1093/humupd/dmt016[↩]
- Hirsch M, Dhillon-Smith R, Cutner AS, Yap M, Creighton SM. The Prevalence of Endometriosis in Adolescents with Pelvic Pain: A Systematic Review. J Pediatr Adolesc Gynecol. 2020 Dec;33(6):623-630. doi: 10.1016/j.jpag.2020.07.011[↩]
- Practice bulletin no. 114: management of endometriosis. Obstet Gynecol. 2010 Jul;116(1):223-236. doi: 10.1097/AOG.0b013e3181e8b073[↩][↩][↩][↩]
- Emanuele MA, Wezeman F, Emanuele NV. Alcohol’s effects on female reproductive function. Alcohol Res Health. 2002;26(4):274-81. https://pmc.ncbi.nlm.nih.gov/articles/PMC6676690[↩]
- Schliep KC, Schisterman EF, Mumford SL, Pollack AZ, Zhang C, Ye A, Stanford JB, Hammoud AO, Porucznik CA, Wactawski-Wende J. Caffeinated beverage intake and reproductive hormones among premenopausal women in the BioCycle Study. Am J Clin Nutr. 2012 Feb;95(2):488-97. doi: 10.3945/ajcn.111.021287[↩]
- Macer ML, Taylor HS. Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstet Gynecol Clin North Am. 2012 Dec;39(4):535-49. doi: 10.1016/j.ogc.2012.10.002[↩]
- Endometriosis. https://www.nichd.nih.gov/health/topics/endometriosis[↩][↩]
- Matalliotakis I, Cakmak H, Matalliotakis M, Kappou D, Arici A. High rate of allergies among women with endometriosis. J Obstet Gynaecol. 2012 Apr;32(3):291-3. doi: 10.3109/01443615.2011.644358[↩]
- Sinaii N, Cleary SD, Ballweg ML, Nieman LK, Stratton P. High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: a survey analysis. Hum Reprod. 2002 Oct;17(10):2715-24. doi: 10.1093/humrep/17.10.2715[↩][↩]
- Sayasneh A, Tsivos D, Crawford R. Endometriosis and ovarian cancer: a systematic review. ISRN Obstet Gynecol. 2011;2011:140310. doi: 10.5402/2011/140310[↩][↩]
- Munksgaard PS, Blaakaer J. The association between endometriosis and gynecological cancers and breast cancer: a review of epidemiological data. Gynecol Oncol. 2011 Oct;123(1):157-63. doi: 10.1016/j.ygyno.2011.06.017[↩]
- Giudice LC. Clinical practice. Endometriosis. N Engl J Med. 2010 Jun 24;362(25):2389-98. doi: 10.1056/NEJMcp1000274[↩]
- Vercellini P, Aimi G, De Giorgi O, Maddalena S, Carinelli S, Crosignani PG. Is cystic ovarian endometriosis an asymmetric disease? Br J Obstet Gynaecol. 1998 Sep;105(9):1018-21. doi: 10.1111/j.1471-0528.1998.tb10267.x[↩]
- Vercellini P, Abbiati A, Viganò P, Somigliana ED, Daguati R, Meroni F, Crosignani PG. Asymmetry in distribution of diaphragmatic endometriotic lesions: evidence in favour of the menstrual reflux theory. Hum Reprod. 2007 Sep;22(9):2359-67. doi: 10.1093/humrep/dem224[↩]
- Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014 May;10(5):261-75. doi: 10.1038/nrendo.2013.255[↩]
- Zondervan KT, Becker CM, Koga K, Missmer SA, Taylor RN, Viganò P. Endometriosis. Nat Rev Dis Primers. 2018 Jul 19;4(1):9. doi: 10.1038/s41572-018-0008-5[↩]
- Bulun SE, Yilmaz BD, Sison C, Miyazaki K, Bernardi L, Liu S, Kohlmeier A, Yin P, Milad M, Wei J. Endometriosis. Endocr Rev. 2019 Aug 1;40(4):1048-1079. doi: 10.1210/er.2018-00242[↩]
- Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. Lancet. 2021 Feb 27;397(10276):839-852. doi: 10.1016/S0140-6736(21)00389-5[↩]
- Horne AW, Missmer SA. Pathophysiology, diagnosis, and management of endometriosis. BMJ. 2022 Nov 14;379:e070750. doi: 10.1136/bmj-2022-070750[↩]
- Saha R, Pettersson HJ, Svedberg P, Olovsson M, Bergqvist A, Marions L, Tornvall P, Kuja-Halkola R. Heritability of endometriosis. Fertil Steril. 2015 Oct;104(4):947-952. doi: 10.1016/j.fertnstert.2015.06.035[↩]
- Treloar SA, O’Connor DT, O’Connor VM, Martin NG. Genetic influences on endometriosis in an Australian twin sample. [email protected]. Fertil Steril. 1999 Apr;71(4):701-10. doi: 10.1016/s0015-0282(98)00540-8[↩]
- Kvaskoff M, Mahamat-Saleh Y, Farland LV, Shigesi N, Terry KL, Harris HR, Roman H, Becker CM, As-Sanie S, Zondervan KT, Horne AW, Missmer SA. Endometriosis and cancer: a systematic review and meta-analysis. Hum Reprod Update. 2021 Feb 19;27(2):393-420. doi: 10.1093/humupd/dmaa045[↩]
- Marinho MCP, Magalhaes TF, Fernandes LFC, Augusto KL, Brilhante AVM, Bezerra LRPS. Quality of Life in Women with Endometriosis: An Integrative Review. J Womens Health (Larchmt). 2018 Mar;27(3):399-408. doi: 10.1089/jwh.2017.6397[↩][↩]
- Roman H, Bridoux V, Tuech JJ, Marpeau L, da Costa C, Savoye G, Puscasiu L. Bowel dysfunction before and after surgery for endometriosis. Am J Obstet Gynecol. 2013 Dec;209(6):524-30. doi: 10.1016/j.ajog.2013.04.015[↩]
- Králíčková M, Laganà AS, Ghezzi F, Vetvicka V. Endometriosis and risk of ovarian cancer: what do we know? Arch Gynecol Obstet. 2020 Jan;301(1):1-10. doi: 10.1007/s00404-019-05358-8[↩]
- Bloski T, Pierson R. Endometriosis and Chronic Pelvic Pain: Unraveling the Mystery Behind this Complex Condition. Nurs Womens Health. 2008 Oct;12(5):382-95. doi: 10.1111/j.1751-486X.2008.00362.x[↩]
- Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis: a committee opinion. Fertil Steril. 2014 Apr;101(4):927-35. doi: 10.1016/j.fertnstert.2014.02.012. Epub 2014 Mar 13. Erratum in: Fertil Steril. 2015 Aug;104(2):498.[↩]
- Yeung PP Jr, Shwayder J, Pasic RP. Laparoscopic management of endometriosis: comprehensive review of best evidence. J Minim Invasive Gynecol. 2009 May-Jun;16(3):269-81. doi: 10.1016/j.jmig.2009.02.007[↩][↩][↩][↩]
- Drug Trials Snapshots: ORILISSA. https://www.fda.gov/drugs/drug-approvals-and-databases/drug-trials-snapshots-orilissa[↩][↩]
- Limonta, P., Marelli, M. M., Moretti, R., Marzagalli, M., Fontana, F., & Maggi, R. (2018). Chapter two – GnRH in the human female reproductive axis. In G. Litwack (Ed.), Vitamins and hormones Vol. 107, pp. 27–66. Cambridge, MA: Academic Press. https://doi.org/10.1016/bs.vh.2018.01.003[↩]
- American College of Obstetricians and Gynecologists. (2010). Management of endometriosis (Practice Bulletin No. 114). Obstetrics & Gynecology, 116(1), 223-236.[↩][↩]
- Stratton P, Berkley KJ. Chronic pelvic pain and endometriosis: translational evidence of the relationship and implications. Hum Reprod Update. 2011 May-Jun;17(3):327-46. doi: 10.1093/humupd/dmq050[↩]
- Hjordt Hansen MV, Dalsgaard T, Hartwell D, Skovlund CW, Lidegaard O. Reproductive prognosis in endometriosis. A national cohort study. Acta Obstet Gynecol Scand. 2014 May;93(5):483-9. doi: 10.1111/aogs.12373[↩]
- Harrison RF, Barry-Kinsella C. Efficacy of medroxyprogesterone treatment in infertile women with endometriosis: a prospective, randomized, placebo-controlled study. Fertil Steril. 2000 Jul;74(1):24-30. doi: 10.1016/s0015-0282(00)00577-x[↩]
- Selçuk I, Bozdağ G. Recurrence of endometriosis; risk factors, mechanisms and biomarkers; review of the literature. J Turk Ger Gynecol Assoc. 2013 Jun 1;14(2):98-103. doi: 10.5152/jtgga.2013.52385[↩][↩]
- Becker CM, Gattrell WT, Gude K, Singh SS. Reevaluating response and failure of medical treatment of endometriosis: a systematic review. Fertil Steril. 2017 Jul;108(1):125-136. doi: 10.1016/j.fertnstert.2017.05.004[↩][↩]
- 2013 Sexually Transmitted Diseases Surveillance. https://www.cdc.gov/std/stats13/tables/45.htm[↩]
- Pelvic Inflammatory Disease (PID) – CDC Fact Sheet. https://www.cdc.gov/std/pid/stdfact-pid.htm[↩][↩]
- Wiesenfeld HC, Sweet RL, Ness RB, et al. Comparison of acute and subclinical pelvic inflammatory disease. Sex Transm Dis 2005;32:400–5.[↩]
- Wiesenfeld HC, Hillier SL, Meyn L, et al. Mycoplasma genitalium – is it a pathogen in acute pelvic inflammatory disease (PID)? STI & AIDS World Congress 2013 (Joint Meeting of the 20th ISSTDR and 14th IUSTI Meeting); July 14-27, 2013; Vienna, Austria.[↩][↩]
- Ness RB, Kip KE, Hillier SL, et al. A cluster analysis of bacterial vaginosis-associated microflora and pelvic inflammatory disease. Am J Epidemiol 2005;162:585–90.[↩][↩]
- Haggerty CL, Totten PA, Astete SG, et al. Mycoplasma genitalium among women with nongonococcal, nonchlamydial pelvic inflammatory disease. Infect Dis Obstet Gynecol 2006:30184.[↩]
- Short VL, Totten PA, Ness RB, et al. Clinical presentation of Mycoplasma genitalium infection versus Neisseria gonorrhoeae infection among women with pelvic inflammatory disease. Clin Infect Dis 2009;48:41–7.[↩]
- Oakeshott P, Aghaizu A, Hay P, et al. Is Mycoplasma genitalium in women the “New Chlamydia?” A community-based prospective cohort study. Clin Infect Dis 2010;51:1160–6.[↩][↩]
- 2015 Sexually Transmitted Diseases Treatment Guidelines. https://www.cdc.gov/std/tg2015/pid.htm[↩]
- Jares EJ, Sanchez-Borges M, Cardona-Villa R, et al. Multinational experience with hypersensitivity drug reactions in Latin America. Ann Allergy Asthma Immunol 2014;113:282–9.[↩]
- Wiesenfeld HC, Hillier SL, Meyn LA, et al. Subclinical pelvic inflammatory disease and infertility. Obstet Gynecol 2012;120:37–43.[↩]
- Ness RB, Soper DE, Holley RL, et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) randomized trial. Am J Obstet Gynecol 2002;186:929–37.[↩][↩]
- Kreisel K, Torrone E, Bernstein K, Hong J, Gorwitz R. Prevalence of Pelvic Inflammatory Disease in Sexually Experienced Women of Reproductive Age — United States, 2013–2014. MMWR Morb Mortal Wkly Rep 2017;66:80–83.[↩][↩][↩]
- Rein, D B. Kassler, W J. Irwin, et al. Direct medical cost of pelvic inflammatory disease and its sequelae: decreasing, but still substantial. Obstet & Gynecol. 2000;95:397-402.[↩]
- Weström, L., Joesoef, R., Reynolds, G., Hagdu, A., Thompson, S.E. (1992). Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sexually Transmitted Diseases; 19(4): 185–192.[↩]
- Leichliter, J., Chandra, A., Aral, S.O. (2013). Correlates of Self-Reported Pelvic Inflammatory Disease Treatment in Sexually Experienced Reproductive-Aged Women in the United States, 1995 and 2006–2010. Sex Transm Dis; 40(5):413–418.[↩]
- Pelvic Inflammatory Disease (PID). 2015 Sexually Transmitted Diseases Treatment Guidelines. https://www.cdc.gov/std/tg2015/pid.htm[↩][↩][↩]
- Centers for Disease Control and Prevention. (2014). STDs in Women and Infants. https://www.cdc.gov/std/stats13/womenandinf.htm#pid[↩]
- Haggerty CL, Ness RB. Epidemiology, pathogenesis and treatment of pelvic inflammatory disease. Expert Rev Anti Infect Ther. 2006;4:235-47.[↩]
- Hillier SL, Kiviat NB, Hawes SE, et al. Role of bacterial vaginosis-associated microorganisms in endometritis. Am J Obstet Gynecolo 1996;175;435-41.[↩]
- Cohen CR, Mugo NR, Astete SG, et al. Detection of Mycoplasma genitalium in women with laparoscopically diagnosed acute salpingitis. Sex Transm Infect. 2005;81:463-466.[↩]
- Grimes DA. Intrauterine device and upper-genital-tract infection. Lancet 2000;356:1013–9; Viberga I, Odlind V, Lazdane G, et al. Microbiology profile in women with pelvic inflammatory disease in relation to IUD use. Infect Dis Obstet Gynecol 2005;13:183–90.[↩]
- Viberga I, Odlind V, Lazdane G, et al. Microbiology profile in women with pelvic inflammatory disease in relation to IUD use. Infect Dis Obstet Gynecol 2005;13:183–90.[↩]
- CDC. U.S. Selected practice recommendations for contraceptive use, 2013: Adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd ed. MMWR Recomm Rep 2013;62(No. RR-05).[↩]
- Tepper NK, Steenland MW, Gaffield ME, et al. Retention of intrauterine devices in women who acquire pelvic inflammatory disease: a systematic review. Contraception 2013;87:655–60.[↩]
- Ness RB, Hillier SL, Kip KE, et al. Bacterial vaginosis and risk of pelvic inflammatory disease. Obstet Gynecol 2004;104:761–9.[↩]
- McGregor JA, Crombleholme WR, Newton E, et al. Randomized comparison of ampicillin-sulbactam to cefoxitin and doxycycline or clindamycin and gentamicin in the treatment of pelvic inflammatory disease or endometritis. Obstet Gynecol 1994;83:998–1004.[↩]
- Bevan CD, Ridgway GL, Rothermel CD. Efficacy and safety of azithromycin as monotherapy or combined with metronidazole compared with two standard multidrug regimens for the treatment of acute pelvic inflammatory disease. J Int Med Res 2003;31:45–54.[↩][↩]
- Walker CK, Wiesenfeld HC. Antibiotic therapy for acute pelvic inflammatory disease: the 2006 CDC Sexually Transmitted Diseases Treatment Guidelines. Clin Infect Dis 2007;28[Supp 1]:S29–36[↩]
- Savaris RF, Teixeira LM, Torres TG, et al. Comparing ceftriaxone plus azithromycin or doxycycline for pelvic inflammatory disease: a randomized controlled trial. Obstet Gynecol 2007;110:53–60.[↩]
- Judlin P, Liao Q, Liu Z, et al. Efficacy and safety of moxifloxacin in uncomplicated pelvic inflammatory disease: the MONALISA study. Br J Obstet Gynaecol 2010;117:1475–84.[↩]
- Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med 2005;352:676–85.[↩]
- Irwin KL, Moorman AC, O’Sullivan MJ, et al. Influence of human immunodeficiency virus infection on pelvic inflammatory disease. Obstet Gynecol 2000;95:525–34.[↩]
- Histed SN, Deshmukh M, Masamed R, Jude CM, Mohammad S, Patel MK. Ectopic Pregnancy: A Trainee’s Guide to Making the Right Call: Women’s Imaging. Radiographics : a review publication of the Radiological Society of North America, Inc. 36 (7): 2236-2237. doi:10.1148/rg.2016160080 https://pubs.rsna.org/doi/10.1148/rg.2016160080[↩]
- Levine D. Ectopic pregnancy. Radiology. 2007;245 (2): 385-97. doi:10.1148/radiol.2452061031 https://www.ncbi.nlm.nih.gov/pubmed/17940301[↩]
- Lipscomb GH, Stovall TG, and Ling FW. Nonsurgical Treatment of Ectopic Pregnancy. N Engl J Med 2000; 343:1325-1329[↩]
- Bachman EA, Barnhart K. Medical management of ectopic pregnancy: a comparison of regimens. Clin Obstet Gynecol. 2012;55 (2): 440-7. doi:10.1097/GRF.0b013e3182510a73 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3329644/[↩]