Contents
- What is lung pain?
- Chest anatomy
- The Lungs
- Lung pain causes
- Lung pain diagnosis
- Lung pain treatment
- Air bubbles in chest
- Pneumomediastinum
- Heart failure
- What is ejection fraction?
- Who is at Risk for Heart Failure?
- Heart failure causes
- Risk factors for heart failure
- Heart failure prevention
- Heart failure symptoms
- Heart failure complications
- Heart failure diagnosis
- New York Heart Association (NYHA) classification
- American College of Cardiology/American Heart Association classification
- Heart failure treatment
- Heart failure prognosis
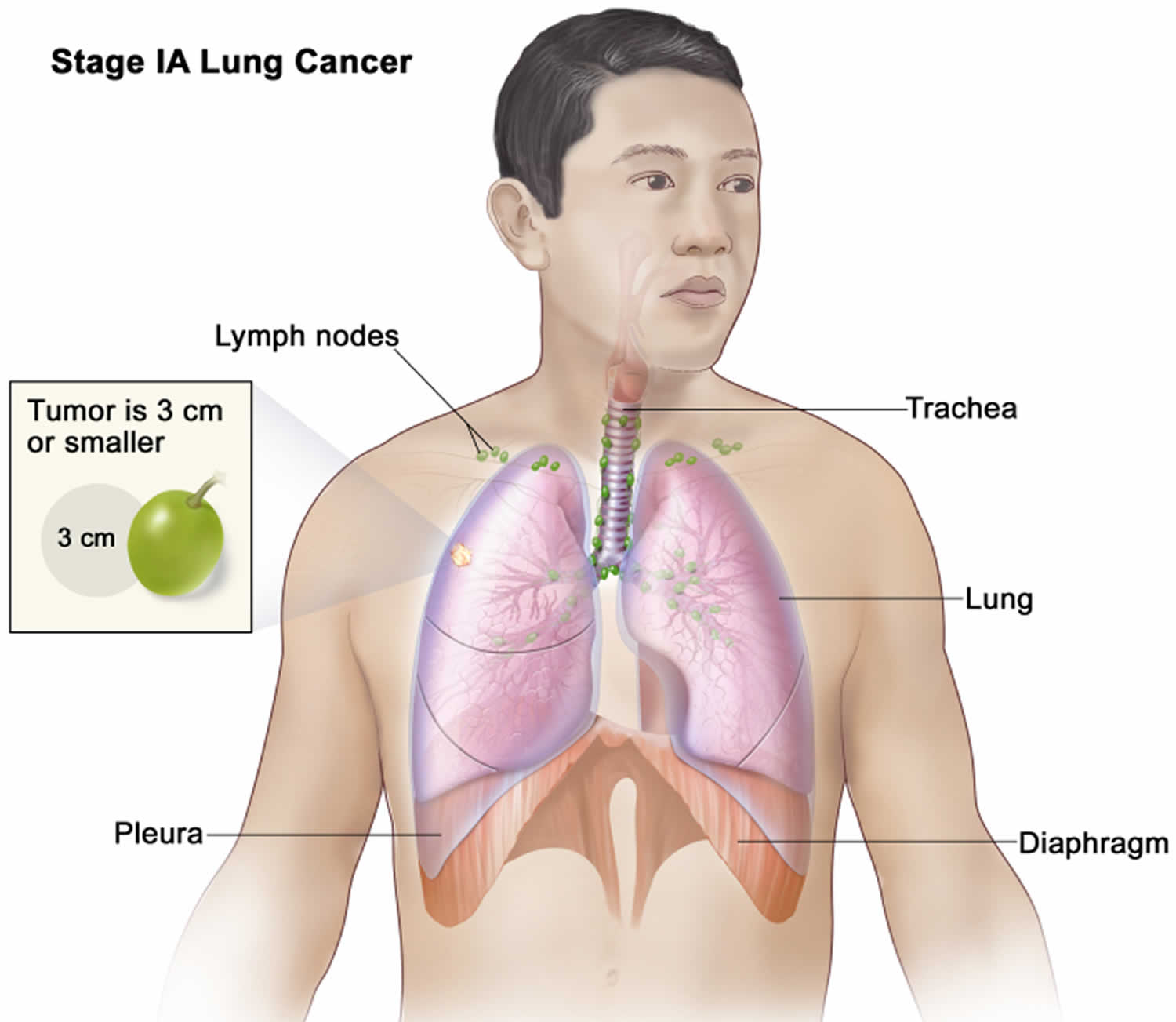
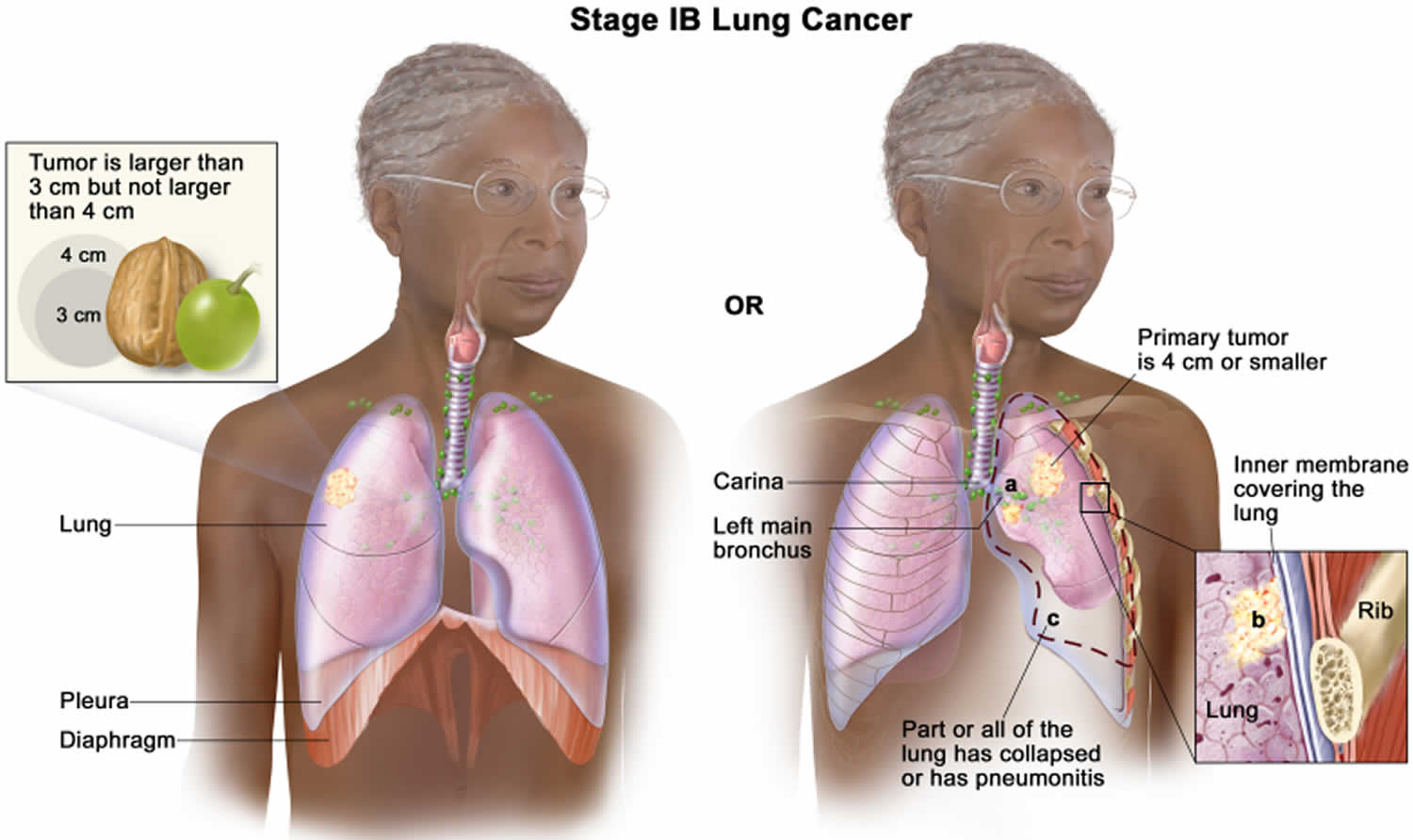
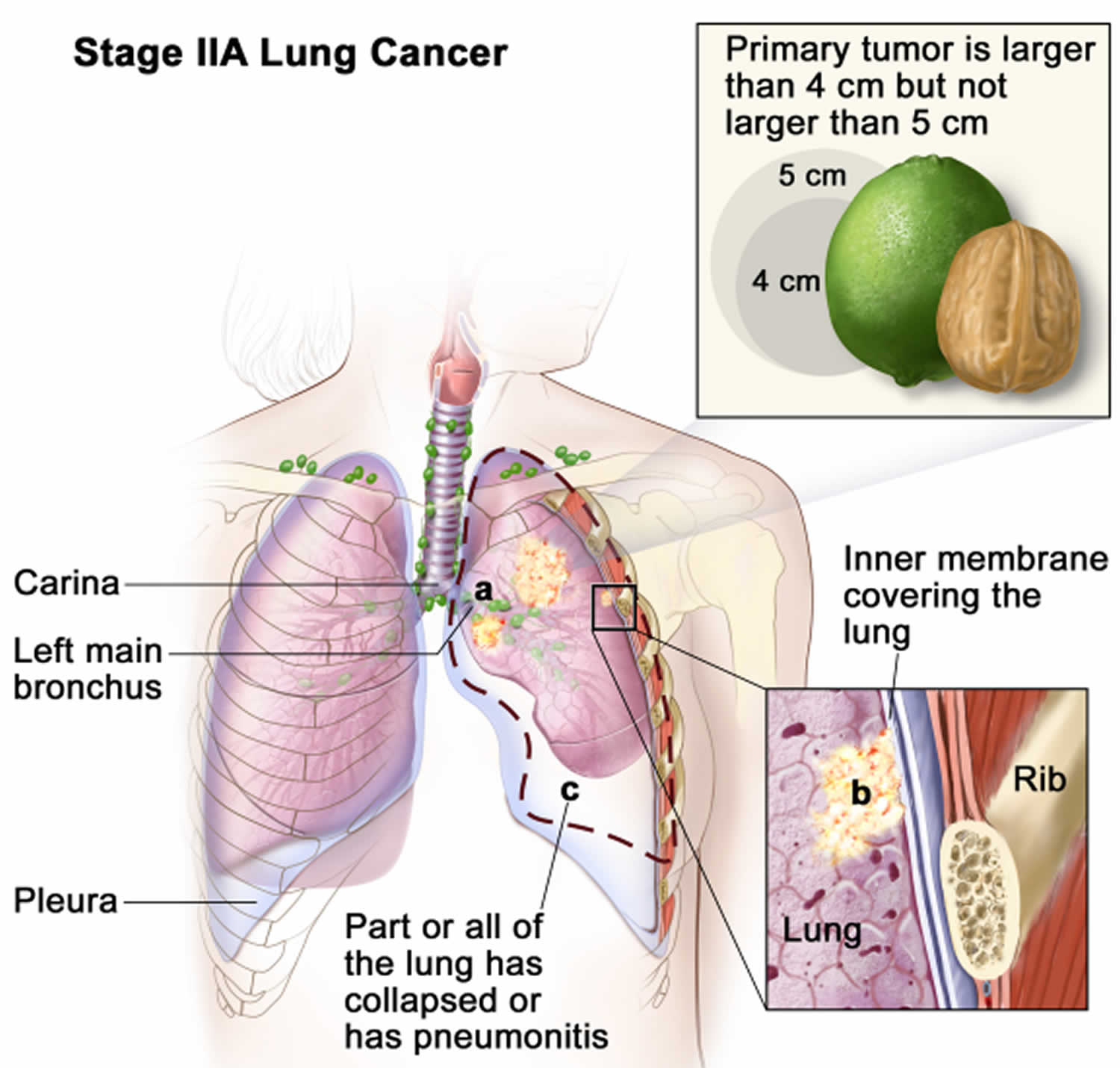
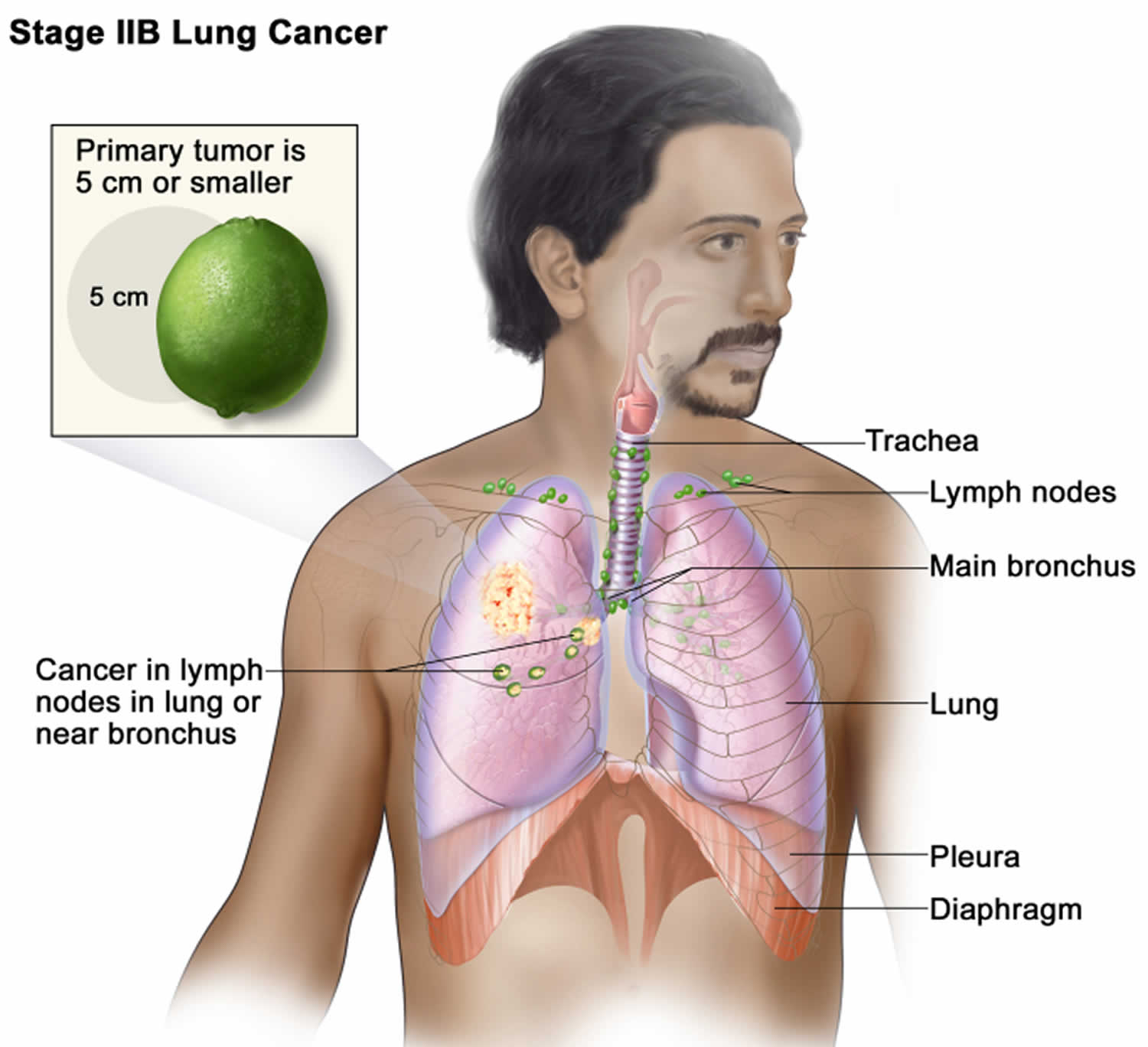
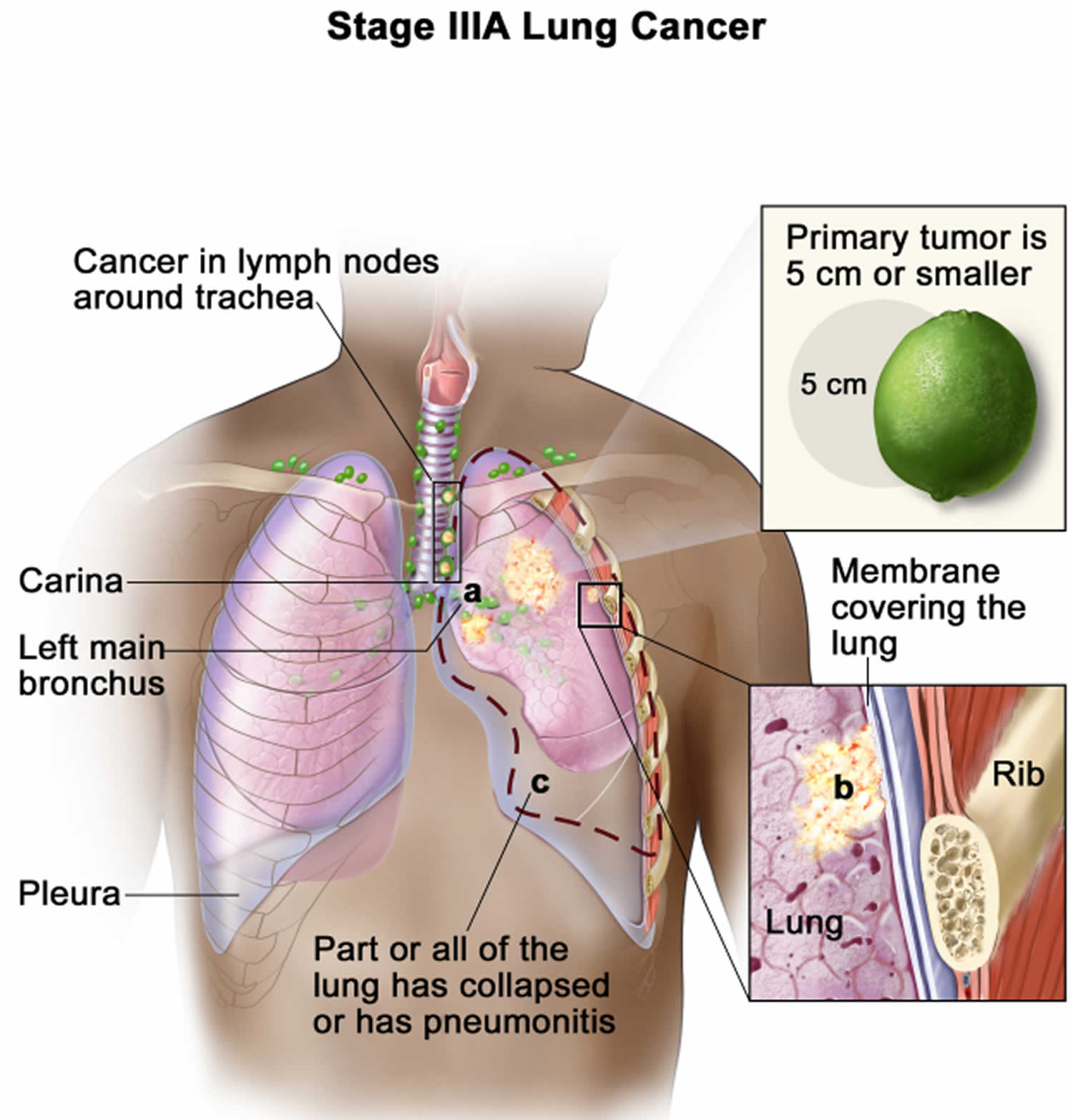
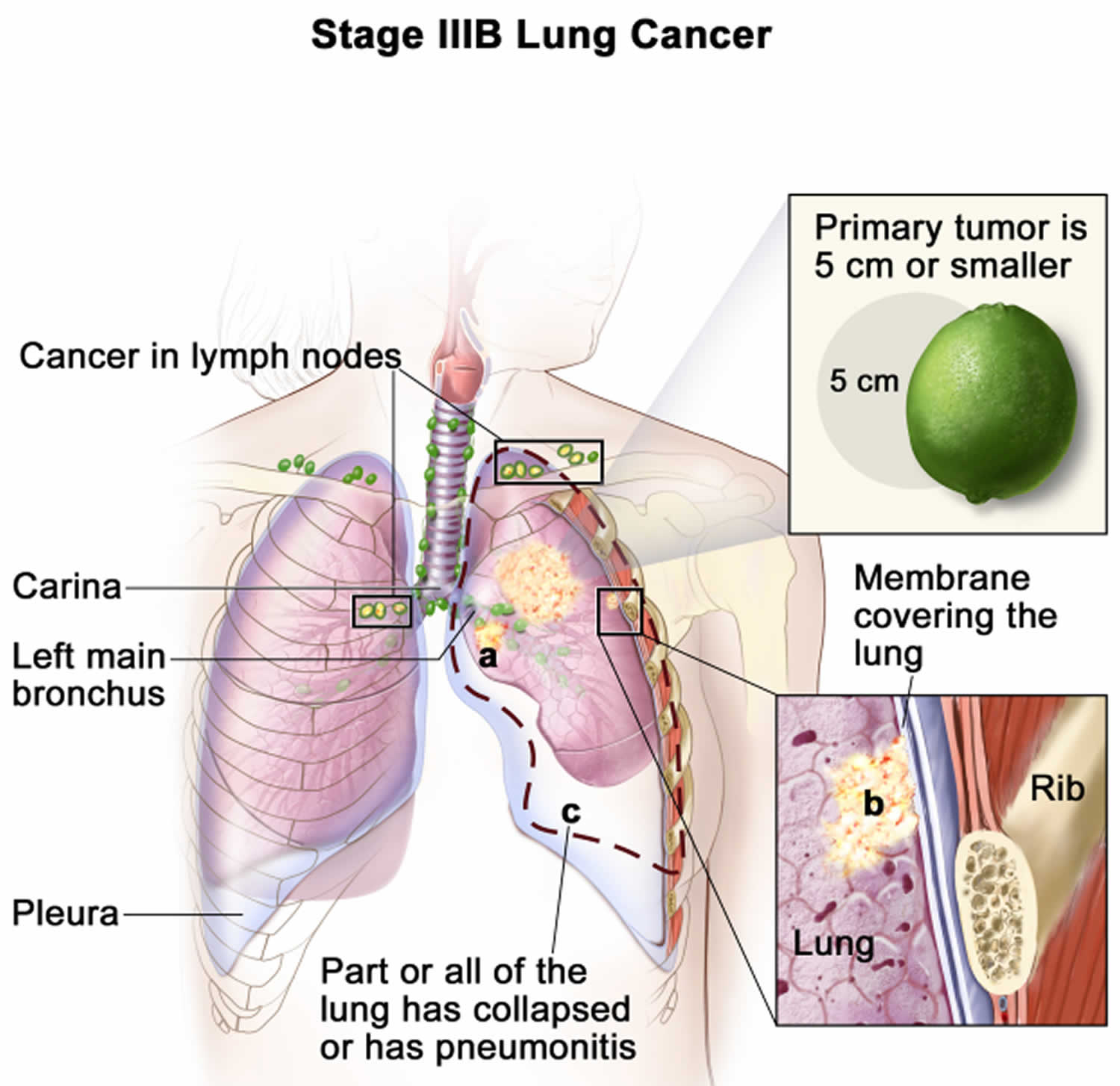
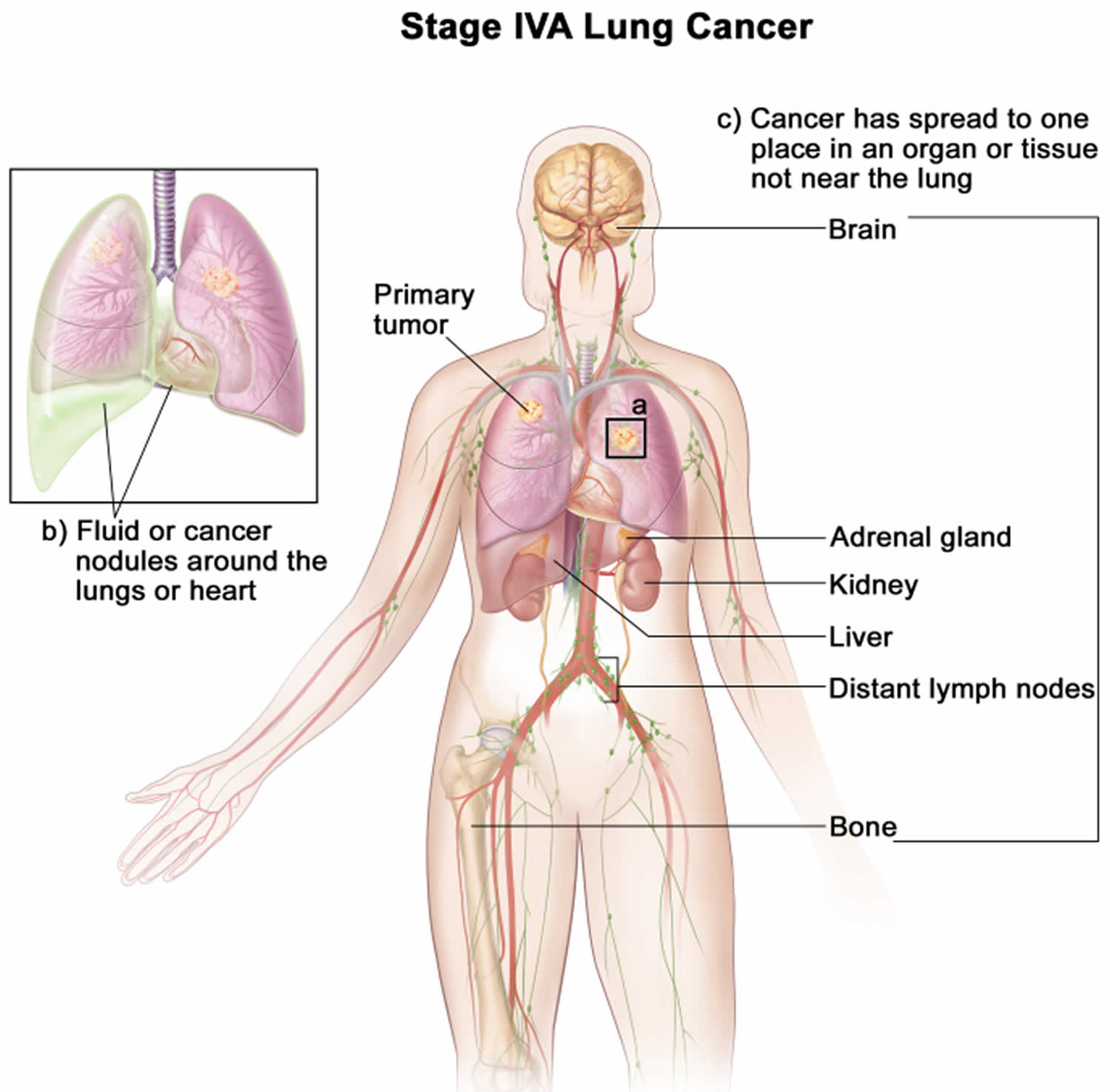
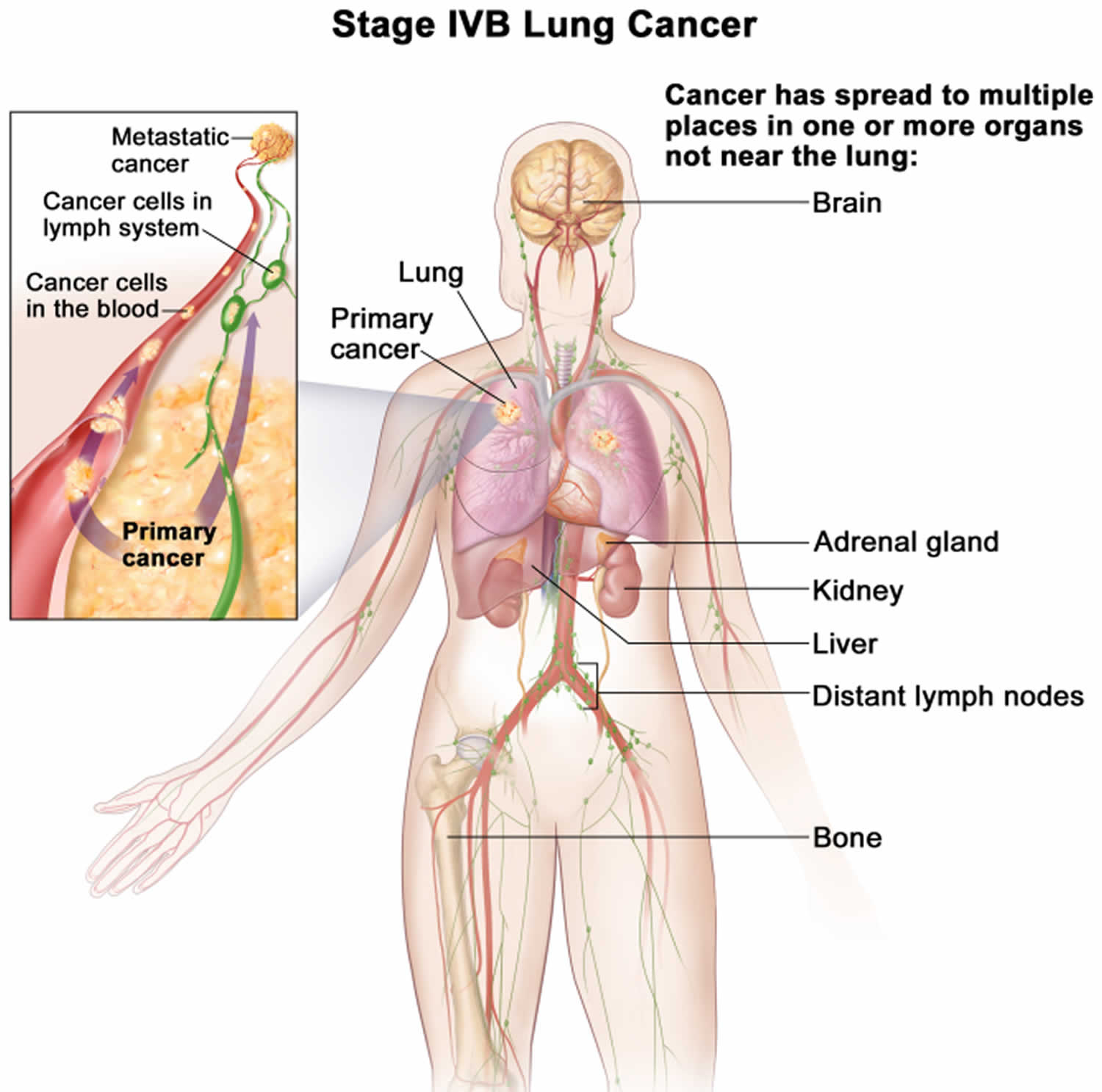
- Lung cancer
- Pleurisy
- Pneumonia
- Is pneumonia contagious?
- Pneumonia signs and symptoms
- Pneumonia types
- Pneumonia complications
- Bronchitis vs Pneumonia
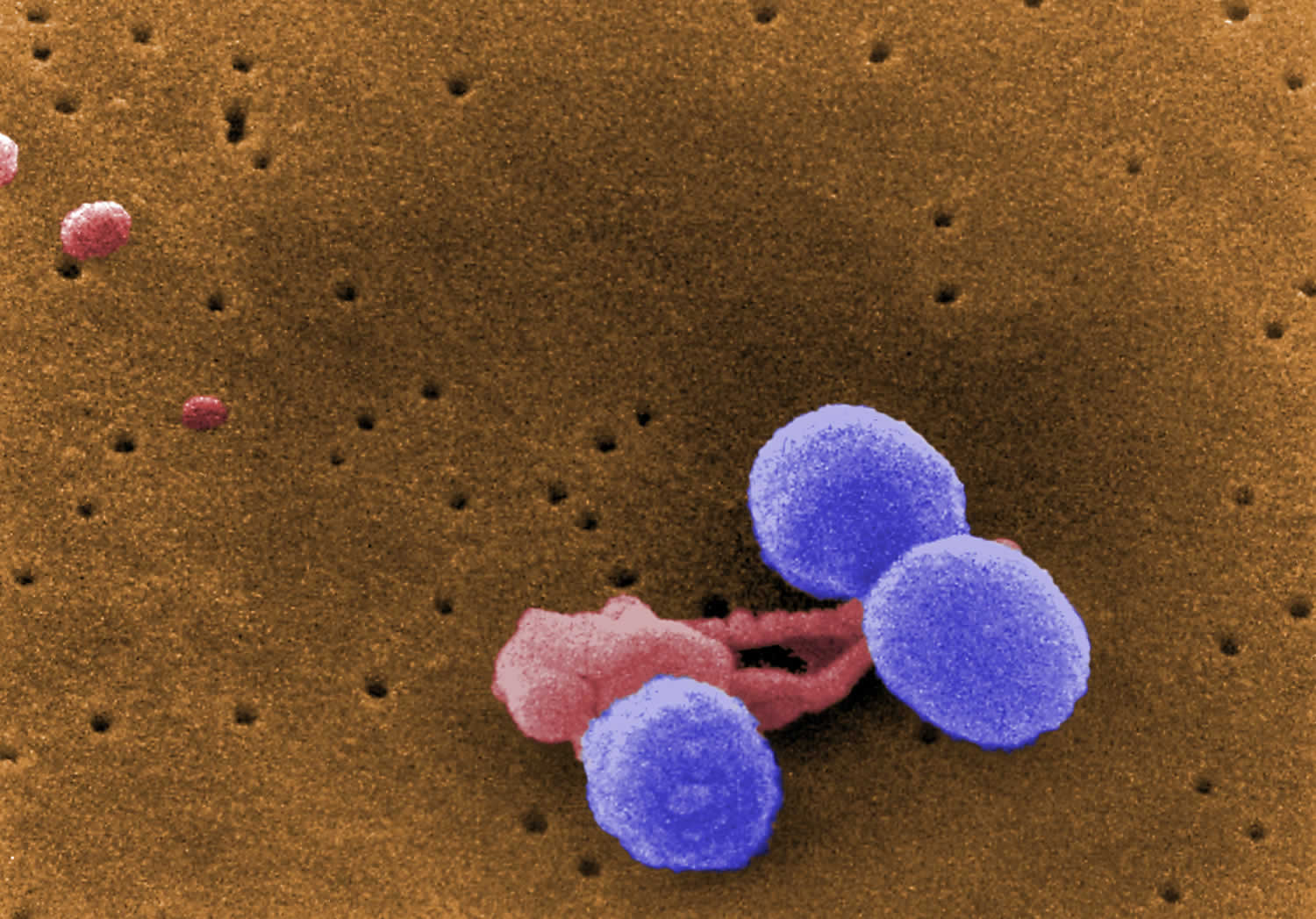
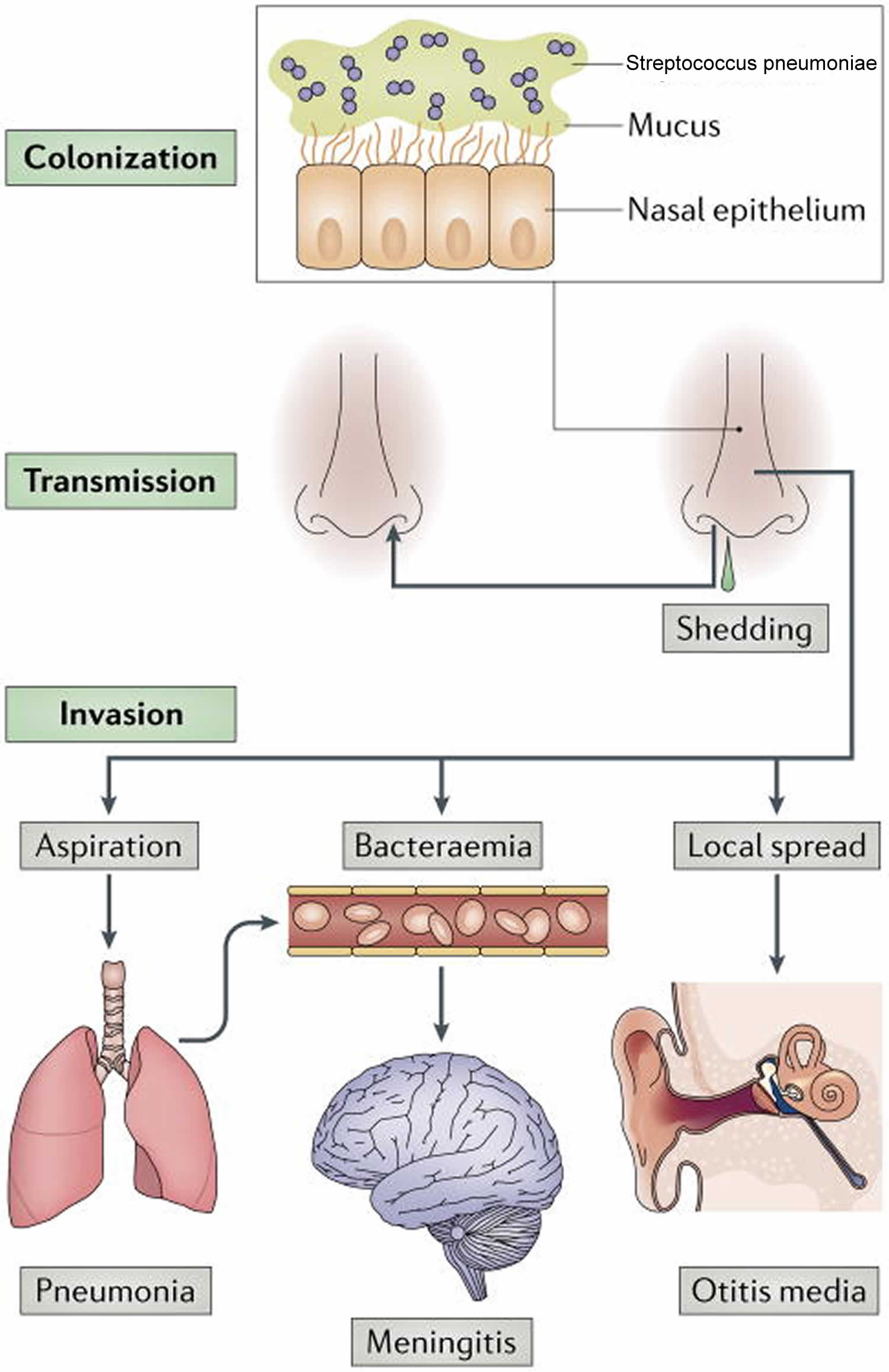
- Pneumonia causes
- Who is at risk of developing pneumonia?
- Risk factors for developing pneumonia
- Pneumonia prevention
- Pneumonia diagnosis
- Pneumonia treatment
- Pneumonia prognosis
- Collapsed lung
- How common is spontaneous collapsed lung?
- What is a small and large collapsed lung?
- How serious is a collapsed lung?
- How long does it take for a collapsed lung to heal?
- What is the recurrence rate of primary spontaneous pneumothorax?
- Is chest tube drainage superior to conservative strategy?
- Is chest tube drainage superior to needle aspiration?
- Is chest tube drainage superior to surgery?
- Is outpatient superior to inpatient management?
- Types of collapsed lung
- Progression of collapsed lung
- Collapsed lung prognosis (outlook)
- Collapsed lung complications
- Collapsed lung causes
- Risk factors for a collapsed lung
- Collapsed lung signs and symptoms
- Collapsed lung diagnosis
- Collapsed lung treatment
- Broken rib
What is lung pain?
Lung pain is a general term to describe chest pain which is non-specific sensation of discomfort or pain that you feel in your chest and can have many causes ranging from life-threatening medical emergency like a heart attack, pulmonary embolism (a sudden blockage in a lung artery due to a blood clot that breaks loose and travels through the bloodstream to the lungs) or angina (chest pain or discomfort that occurs when the heart’s blood flow is reduced) to lung issues, muscle strain, digestive problems such as acid reflux or heartburn to esophagus disorders such as esophageal spasms, esophagitis (a condition in which the lining of the esophagus becomes swollen, inflamed, or irritated), gastroesophageal reflux disease (GERD) or esophageal cancer. Heartburn, acid reflux, esophageal spasm, angina and heart attack may feel very much alike. Don’t try to diagnose the cause yourself. Even experienced doctors can’t always tell the difference from your medical history and a physical exam. That’s why you must seek urgent medical attention. So if you are not sure seek medical attention immediately. If you have persistent lung pain, unexplained shortness of breath, and you aren’t sure it’s heartburn, call your local emergency number to ask for emergency medical help and an ambulance. Treatment depends on the cause of your chest pain.
“Lung pain” can occur due to a number of possible reasons because any organ or tissue in your chest can be the source of your pain, including your heart, lungs, esophagus, muscles, ribs, tendons, or nerves. “Lung pain” may also spread to the chest from the neck, abdomen, and back and may be due to problems in any of those areas.
- Heart and vascular related causes
- Angina: Pain caused by reduced blood flow to the heart muscle.
- Heart attack also known as a myocardial infarction is a blockage of blood flow to the heart muscle. A heart attack is a medical emergency. Call your local emergency number if you think you or someone else is having a heart attack.
- Coronary artery disease: A narrowing or blockage in your heart’s arteries. Coronary artery disease (coronary heart disease) symptoms may include chest pain that may spread to your neck, jaw, arms, or back and shortness of breath. A complete blockage of blood flow to your heart can cause a heart attack (myocardial infarction). Smoking or having high blood pressure, high cholesterol, diabetes, obesity or a strong family history of heart disease makes you more likely to get coronary artery disease (coronary heart disease). If you’re at high risk of coronary artery disease, see your doctor. You may need tests to check for narrowed arteries and coronary artery disease.
- Heart failure also known as congestive heart failure, is a condition where the heart can’t pump blood properly. It can affect one or both sides of the heart.
- Pericarditis: Pericarditis is an infection or inflammation in the lining around your heart, causing a sharp pain in your chest. Symptoms include chest pain, shortness of breath, and palpitations. The pain can spread to your left shoulder and arm. The pain can be worse when you’re lying down and when taking deep breaths.
- Constrictive pericarditis: Constrictive pericarditis is a chronic condition in which your pericardium (the sac around your heart) becomes too thick or stiff. Constrictive pericarditis causes the pericardium to thicken and stiffen, making it difficult for the heart to pump blood. This can lead to heart failure. Constrictive pericarditis symptoms include fatigue, shortness of breath that worsens over time, swelling in your legs and ankles, swollen abdomen, and weakness.
- Pericardial effusion: A buildup of fluid (more than there should be) in your pericardium.
- Cardiac tamponade: A dangerous condition that happens when fluid builds up and puts pressure on your heart. This outside pressure on the heart prevents it from filling properly.
- Pericardial cysts: Pericardial cyst is a rare, benign, fluid-filled sac that develops within the pericardial sac (pericardial space) surrounding your heart, often discovered incidentally on imaging. Pericardial cyst is usually asymptomatic but can cause symptoms if they grow large or compress nearby structures. Pericardial cysts are most commonly found in the right cardiophrenic angle, but can also occur in other areas of the mediastinum (the space in the chest). In rare cases, a pericardial cyst can lead to complications like compression of the heart or lungs, or even rupture of the cyst.
- Hypertrophic cardiomyopathy (HCM). Hypertrophic cardiomyopathy (HCM) is a genetic disease that causes your heart muscle to thicken especially the ventricles or lower heart chambers, left ventricular stiffness, mitral valve changes and cellular changes. The muscle walls of your pumping ventricles or lower heart chambers become thick and stiff. This thickening can affect your heart’s ability to pump blood. With hypertrophic cardiomyopathy (HCM), you can’t get enough blood into — or out of — your heart’s chambers, and your heart has a harder time getting oxygen-rich blood.
- Aortic dissection. Aortic dissection is a tear in the aorta, the main artery that carries blood from your heart to your body. Aortic dissection is a medical emergency that can be fatal if not treated promptly. Aortic dissection can cause very strong pain in your chest, back and between your shoulder blades that happens without warning and feels like something is ripping.
- Aortic aneurysm. Aortic aneurysm is a balloon-like bulge in the aorta, your body’s main artery that carries blood from your heart to your body. Aortic aneurysm can occur in your chest (thoracic aortic aneurysm) or abdomen (abdominal aortic aneurysm). Blood that pushes against a weak part of your aorta’s wall can make it bulge out. Without treatment, this weak spot can break open and cause severe pain in your chest or abdomen. If an aortic aneurysm ruptures, it’s an emergency that requires immediate treatment.
- Mitral valve prolapse. Your mitral valve controls blood flow from your left atrium (upper left heart chamber) to your left ventricle (bottom left heart chamber). Mitral valve has two leaflets (flaps) that open to let blood flow from your left atrium to your left ventricle. When the Mitral valve closes, it prevents blood from moving backward. Sometimes, your mitral valve doesn’t work right because it’s too narrow or leaky. This can make your heart work harder to pump blood to your body. Mitral valve prolapse (MVP) is a heart condition that occurs when the mitral valve flaps bulge into the left atrium of the heart. This can cause blood to leak backward into the atrium, a condition called mitral valve regurgitation. This can make your heart work harder to pump blood to your body. Treatment for mitral valve disease depends on the severity of the condition and whether it is worsening. Sometimes, surgery is recommended to repair or replace the mitral valve.
- Lung-related causes
- Pneumonia. Pneumonia is a lung infection that can be caused by bacteria, viruses, or fungi. Pneumonia or lung infection can range from mild to severe.
- Pleurisy or pleuritis. Pleurisy or pleuritis is infection and/or inflammation of the membrane (parietal pleura and visceral pleura membranes) that surrounds your lungs and lines your chest cavity. It can cause sharp chest pain when you cough or breathe deeply. You may also have pain in your shoulder.
- Pulmonary embolism (PE). A pulmonary embolism (PE) is a blockage in your lung’s arteries caused by a blood clot. A blood clot can come from another part of your body (usually from deep vein in your leg and travels to the lungs) and get stuck in a pulmonary artery inside your lung. People with a pulmonary embolism (PE) often describe sharp chest pain that worsens when they breathe in. You may have shortness of breath especially when breathing in, coughing up blood, or a fast/racing heart rate (tachycardia). Other symptoms of pulmonary embolism (PE) include feeling like you’re having a heart attack, anxiety, dizziness, lightheadedness, or fainting, palpitations (fast, strong, or irregular heartbeat) and sweating. Pulmonary embolism (PE) is a life-threatening medical emergency that requires immediate treatment.
- Collapsed lung also known as a pneumothorax. A collapsed lung (pneumothorax) is a condition that occurs when air leaks into the pleural cavity or the space between your lung and chest wall. This causes part or all of your lung to collapse. This puts pressure on your lung, making it difficult to expand when you breathe in. With no warning, you may feel a sharp pain in your chest and possibly your neck and shoulder.
- Asthma: Asthma is a chronic lung disease that makes it hard to breathe. Asthma is caused by inflammation and muscle tightening in the airways. Asthma symptoms include coughing, wheezing, shortness of breath, chest tightness, and fatigue.
- Lung cancer: Lung cancer is cancer that starts when abnormal cells in your lungs grow and multiply out of control. People who smoke have the greatest risk of lung cancer. The risk of lung cancer increases with the length of time and number of cigarettes smoked. Lung cancer is the leading cause of cancer deaths worldwide. Lung cancer typically doesn’t cause symptoms early on. Symptoms of lung cancer usually happen when the disease is advanced. Symptoms include a chronic cough, shortness of breath, and feeling tired or weak.
- Chronic obstructive pulmonary disease (COPD). Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes it difficult to breathe. Chronic obstructive pulmonary disease (COPD) is caused by damage to your lungs air sacs and/or airway lining that narrows the airways making it difficult for you to breathe. Symptoms include coughing up phlegm, shortness of breath, chest tightness, wheezing, and tiredness. Your chest may feel tight and you may have shortness of breath and/or wheezing. COPD is not curable, but treatments can help manage your symptoms. In some people, COPD worsens over time and can lead to life-threatening problems. Treatment include inhaled medicines, oxygen, pulmonary rehabilitation programs, antibiotics, and steroid tablets.
- Pulmonary hypertension. Pulmonary hypertension is a serious condition that causes high blood pressure in the arteries of your lungs (pulmonary arteries). Pulmonary arteries are the blood vessels that take blood to your lungs to trade carbon dioxide for oxygen. It can be caused by other diseases or develop on its own. You get chest pain because it’s harder for your heart to push blood through blood vessels (pulmonary arteries) when hypertension adds resistance to blood flow. You can have shortness of breath with this condition.
- Tuberculosis (TB). Tuberculosis (TB) is a bacterial infection caused by the Mycobacterium tuberculosis bacteria. Tuberculosis (TB) most commonly affects your lungs, but can also spread to other parts of your body, such as your brain, spine, or kidneys and can cause serious illness. Tuberculosis (TB) can be cured with specific antibiotics.
- Digestive-related causes
- Esophageal spasm. Esophageal spasm are painful abnormal painful contractions of the muscles in the esophagus (the muscular tube that carries food from your mouth to your stomach). Esophageal spasms do not move food effectively to your stomach. The cause of esophageal spasm is unknown. Very hot or very cold foods may trigger an episode of esophageal spasm in some people.
- Acid reflux also called heartburn, acid indigestion, acid regurgitation or gastroesophageal reflux (GER) is a painful burning feeling in your chest or throat that occurs when stomach acid backs up into the tube called the esophagus that carries food from your mouth to your stomach 1, 2, 3. Typically, when food is swallowed, a band of muscle around the bottom of your esophagus called the lower esophageal sphincter (LES) relaxes to allow food and liquid to flow down into your stomach. Then the lower esophageal sphincter muscle tightens again. If the lower esophageal sphincter (LES) isn’t working as it should, stomach acid can flow back up into your esophagus (acid reflux) and you might feel a burning sensation in your chest, commonly called heartburn. The acid backup may be worse when you’re bent over, lying down, after eating a big meal or drinking coffee or alcohol. Pregnancy, certain foods, and some medications can bring on heartburn. Treating heartburn is important because over time as acid reflux can damage your esophagus.
- Gastroesophageal reflux disease (GERD) also called gastro-oesophageal reflux disease (GORD), is a condition that develops when there is a backward flow or reflux of stomach contents (acid from the food and liquid in your stomach) back up into your throat and esophagus causing troublesome symptoms and/or complications 4, 5, 6, 7, 8. Gastroesophageal reflux disease can present as non-erosive reflux disease or erosive esophagitis. It can occur at any age, even in babies. Many times, you or your doctor can determine the triggers for your reflux.
- Esophagitis also called erosive esophagitis or ulcerative esophagitis is present when the lining of your esophagus becomes swollen, inflamed, or irritated 9. Esophagitis can cause painful, difficult swallowing. Esophagitis can also lead to chest pain. Various things can cause esophagitis. Some common causes include stomach acids backing up into the esophagus, infection, medicines taken by mouth and allergies. Chronic acid reflux (GERD) is a common cause of esophagitis.
- Hiatal hernia. A hiatal hernia occurs the upper part of your stomach pushes up into your chest through the diaphragm (the large muscle that separates the abdomen and the chest). Normally the diaphragm has a small opening called a hiatus. The tube used for swallowing food, called the esophagus, passes through the hiatus of the diaphragm before connecting to the stomach. In a hiatal hernia, the stomach pushes up through that opening and into your chest. A small hiatal hernia usually doesn’t cause problems. You may never know you have one unless your doctor discovers it when checking for another condition. But a large hiatal hernia can allow food and acid to back up into your esophagus. This can cause heartburn, chest pain, and difficulty swallowing. Self-care measures or medicines can usually relieve these symptoms. A very large hiatal hernia might need surgery.
- Gastritis. Gastritis is when your stomach lining gets inflamed (red and swollen). Your stomach lining is strong. In most cases, acid does not hurt it. But it can get inflamed and irritated if you drink too much alcohol, have damage from pain relievers called non-steroidal anti-inflammatory drugs (NSAIDs), or smoke. Stomach lining inflammation from many causes can make your lower left chest hurt. You also might feel sick to your stomach and throw up.
- Pancreatitis. Pancreatitis is inflammation of your pancreas, an organ that produces digestive enzymes and hormones such as insulin and glucagon. Pancreatitis can be acute pancreatitis (sudden and severe) or chronic pancreatitis (ongoing). Pancreatitis symptoms may include pain in the upper abdomen that may spread to the back, nausea and vomiting, fever, rapid pulse, and weight loss.
- Esophageal cancer is cancer that occurs in the esophagus. Esophageal cancer usually begins in the cells that line the inside of the esophagus. Esophageal cancer can occur anywhere along the esophagus. More men than women get esophageal cancer.
- Gallstones also known as cholelithiasis. Gallstones are hardened deposits of bile that form in your gallbladder. Gallstones can range in size from a grain of sand to a golf ball. Some people develop just one gallstone, while others develop many gallstones at the same time. With cholesterol as their main ingredient, gallstones can block ducts where a fluid (bile) that helps digestion needs to go to reach your small intestine. Swelling in your gallbladder causes pain under your ribs on your right side. This extreme pain can last for many hours. People who experience symptoms from their gallstones usually require gallbladder removal surgery (cholecystectomy). Gallstones that don’t cause any signs and symptoms typically don’t need treatment.
- Musculoskeletal-related causes
- Costochondritis also known as chest wall pain syndrome or costosternal syndrome is inflammation of the cartilage that connects your ribs to your breastbone.
- Sprained chest muscle also known as pulled chest muscle, is a minor injury, tear or stretch in a chest muscle that usually heals on its own within a few weeks. A chest muscle sprain can cause pain, swelling, bruising, and muscle spasms.
- Broken rib. Broken rib also called rib fracture is a common injury that occurs when one of the bones in your rib cage breaks or cracks. The most common causes are hard impacts from falls, car accidents or contact sports. Broken rib hurts a lot, especially when you breathe deeply. The sharp edge of a broken bone can harm major blood vessels or lungs and other organs inside your chest. Usually, broken ribs heal on their own in about six weeks. The pain lasts for several weeks. Pain control is important for being able to breathe deeply and avoid lung issues, such as pneumonia.
- Other causes
- Shingles also known as herpes zoster, is a painful rash caused by the varicella-zoster virus (VZV), the virus that gave you chickenpox as a child can become active again later, usually in people older than 50. As shingles, the varicella-zoster virus (VZV) causes a painful rash on your upper body. It usually develops in part of your chest, and typically only on one side. Risk factors for shingles include having had chickenpox in the past, being older, and having a weakened immune system.
- Panic attack and anxiety disorders are a group of mental health conditions that cause fear, dread and other symptoms that are out of proportion to the situation. There are several types, including generalized anxiety disorder (GAD), specific phobias and social anxiety disorder. Treatment is effective and usually includes medication and psychotherapy (talk therapy).
You may not be able to tell the difference between a heart attack and non-serious chest pain. For this reason, you should always take chest pain seriously. If it’s sudden or new and lasts longer than five minutes, go to the emergency room (ER). If it goes away after a few minutes, it may not be an emergency, but you should still see your doctor as soon as possible to determine the cause. Non-serious chest pain, whatever the cause, can always occur again, and can end up affecting your quality of life.
The squeezing chest pain associated with esophageal spasms can also be caused by a heart attack. If you experience squeezing chest pain, seek immediate medical care.
If you think you’re having a heart attack, immediately call your local emergency number for an ambulance and medical care. You should call, even if you are not sure that it is a heart attack. If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only as a last option.
The average person waits 3 hours before seeking help for symptoms of a heart attack. Sadly, many people with heart attack die before they reach a hospital. The sooner the person gets to the emergency room (ER), the better the chance of survival. Prompt medical treatment reduces the amount of heart damage.
Are you having Esophageal spasm or Heart attack?
Each year almost 800,000 Americans have a heart attack. Every 40 seconds, someone in the United States has a heart attack 10. A heart attack happens when the flow of oxygen-rich blood to a section of heart muscle suddenly becomes blocked and the heart can’t get oxygen. If blood flow isn’t restored quickly, the section of heart muscle begins to die 11. But if you do get quick treatment, you may be able to prevent or limit damage to your heart muscle. That’s why it’s important to know the symptoms of a heart attack and call your local emergency services number if you or someone else is having a heart attack. You should call, even if you are not sure that it is a heart attack.
The most common warning symptoms of a heart attack for both men and women are:
- Chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest. The discomfort usually lasts for more than a few minutes or goes away and comes back. It can feel like pressure, squeezing, fullness, or pain. It also can feel like heartburn or indigestion. The feeling can be mild or severe.
- Upper body discomfort. You may feel pain or discomfort in one or both arms, the back, shoulders, neck, jaw, or upper part of the stomach (above the belly button).
- Shortness of breath. This may be your only symptom, or it may occur before or along with chest pain or discomfort. It can occur when you are resting or doing a little bit of physical activity.
Not everyone having a heart attack has typical symptoms. If you’ve already had a heart attack, your symptoms may not be the same for another one. However, some people may have a pattern of symptoms that recur.
Many people aren’t sure what’s wrong when they are having symptoms of a heart attack.
Not all heart attacks begin with the sudden, crushing chest pain that often is shown on TV or in the movies. In one study, for example, one-third of the patients who had heart attacks had no chest pain 12. These patients were more likely to be older, female, or diabetic.
The symptoms of a heart attack can vary from person to person. Some people can have few symptoms and are surprised to learn they’ve had a heart attack. If you’ve already had a heart attack, your symptoms may not be the same for another one. It is important for you to know the most common symptoms of a heart attack and also remember these facts:
- Heart attacks can start slowly and cause only mild pain or discomfort. Symptoms can be mild or more intense and sudden. Symptoms also may come and go over several hours.
- People who have high blood sugar (diabetes) may have no symptoms or very mild ones.
- The most common symptom, in both men and women, is chest pain or discomfort.
- Women are somewhat more likely to have shortness of breath, nausea and vomiting, unusual tiredness (sometimes for days), and pain in the back, shoulders, and jaw.
The more signs and symptoms you have, the more likely it is that you’re having a heart attack.
Other Common Signs and Symptoms include:
- Breaking out in a cold sweat
- Feeling unusually tired for no reason, sometimes for days (especially if you are a woman)
- Nausea (feeling sick to the stomach) and vomiting
- Light-headedness or sudden dizziness
- Any sudden, new symptom or a change in the pattern of symptoms you already have (for example, if your symptoms become stronger or last longer than usual)
The symptoms of angina can be similar to the symptoms of a heart attack. Angina is chest pain that occurs in people who have coronary heart disease, usually when they’re active. Angina pain usually lasts for only a few minutes and goes away with rest.
Chest pain or discomfort that doesn’t go away or changes from its usual pattern (for example, occurs more often or while you’re resting) can be a sign of a heart attack.
- All chest pain should be checked by a doctor.
The signs and symptoms of a heart attack can develop suddenly. However, they also can develop slowly—sometimes within hours, days, or weeks of a heart attack.
Any time you think you might be having heart attack symptoms or a heart attack, don’t ignore it or feel embarrassed to call for help. Call your local emergency number for emergency medical care, even if you are not sure whether you’re having a heart attack. Here’s why:
- Acting fast can save your life.
- An ambulance is the best and safest way to get to the hospital. Emergency medical services personnel can check how you are doing and start life-saving medicines and other treatments right away. People who arrive by ambulance often receive faster treatment at the hospital.
- The emergency phone operator or EMS technician can give you advice. You might be told to crush or chew an aspirin if you’re not allergic, unless there is a medical reason for you not to take one. Aspirin taken during a heart attack can limit the damage to your heart and save your life.
Every minute matters. Never delay calling your local emergency number in order to take aspirin or do anything else you think might help.
Heart attack treatment works best when it’s given right after symptoms occur.
- Don’t Wait–Get Help Quickly
- Quick Action Can Save Your Life
- If you think you or someone else is having a heart attack, even if you’re not sure, don’t feel embarrassed to call your local emergency number right away !
- Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. Take a nitroglycerin pill if your doctor has prescribed this type of treatment.
Other Names for a Heart Attack
- Myocardial infarction (MI)
- Acute myocardial infarction (AMI)
- Acute coronary syndrome
- Coronary thrombosis
- Coronary occlusion
Every year, about 790,000 Americans have a heart attack. Of these cases
- 580,000 are a first heart attack.
- 210,000 happen to people who have already had a first heart attack 10.
- About 15% of people who have a heart attack will die from it 10.
- Almost half of sudden cardiac deaths happen outside a hospital 13.
- One of 5 heart attacks is silent—the damage is done, but the person is not aware of it 10.
Heart attacks most often occur as a result of coronary heart disease (CHD), also called coronary artery disease. Coronary heart disease is a condition in which a waxy substance called plaque (cholesterol plaque) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart.
When plaque builds up in the arteries, the condition is called atherosclerosis. The buildup of plaque occurs over many years.
Eventually, an area of plaque can rupture (break open) inside of an artery. This causes a blood clot to form on the plaque’s surface. If the clot becomes large enough, it can mostly or completely block blood flow through a coronary artery.
If the blockage isn’t treated quickly, the portion of heart muscle fed by the artery begins to die. Healthy heart tissue is replaced with scar tissue. This heart damage may not be obvious, or it may cause severe or long-lasting problems.
Is left chest pain a symptom of a heart attack?
Yes, left-side chest pain is one of the symptoms of a heart attack. But there are others, like shortness of breath or pain in other parts of your upper body. If you think you’re having a heart attack, call your local emergency number for medical assistance and ambulance to bring you to the emergency room.
Chest anatomy
Your chest cavity also called the thoracic cavity is formed by the ribs, the muscles of the chest, the sternum (breastbone), and the thoracic portion of the vertebral column. Within your thoracic cavity are 3 smaller cavities: (a) 2 pleural cavities (fluid-filled spaces one around each lung), your left pleural cavity (holds your left lung) and your right pleural cavity (holds your right lung) and (b) a central portion of your thoracic cavity between your lungs called the mediastinum (media- = middle; -stinum = partition). The mediastinum is the central portion of your thoracic cavity between your lungs, extending from the base of your neck (from your first rib and sternum) to the diaphragm. The mediastinum contains your heart (pericardial cavity, peri- = around; -cardial = heart, a fluid-filled space that surrounds your heart), the major blood vessels connected to your heart and lungs, the trachea (windpipe) and bronchi, the esophagus (foodpipe), the thymus, and lymph nodes but not your lungs. Your right and left lungs are on either side of the mediastinum. The diaphragm is a dome-shaped muscle that separates the thoracic cavity from the abdominopelvic cavity.
Your mediastinum is divided into several parts, which researchers call compartments. The traditional or classical model divides your mediastinum into four parts:
- Superior mediastinum: The top part, located superior to (above) your heart.
- Anterior mediastinum: The part anterior to (in front of) your heart, between your heart and your sternum (breastbone).
- Middle mediastinum: The part that contains your heart.
- Posterior mediastinum: The part posterior to (behind) your heart.
A membrane is a thin, pliable tissue that covers, lines, partitions, or connects internal organs (viscera). One example is a slippery, double-layered membrane associated with body cavities that does not open directly to the exterior called a serous membrane. Serous membrane covers your internal organs (viscera) within the thoracic and abdominal cavities and also lines the walls of the thorax and abdomen. The parts of a serous membrane are (1) the parietal layer (outer layer), a thin epithelium that lines the walls of the cavities, and (2) the visceral layer (inner layer), a thin epithelium that covers and adheres to the viscera within the cavities. Between the two layers is a potential space that contains a small amount of lubricating fluid (serous fluid). The fluid allows the internal organs (viscera) to slide somewhat during movements, such as when the lungs inflate and deflate during breathing.
Within the right and left sides of your thoracic cavity (chest cavity), the compartments that contain your lungs, on either side of the mediastinum, are lined with a membrane called the parietal pleura (outer serous membrane) lining the inside of your rib cage (parietal pleura lines the chest wall) and covering the superior surface of the diaphragm. A similar membrane, called the visceral pleura (inner serous membrane), clings to the surface of your lungs forming the external surface of your lung. The visceral (inner) and parietal (outer) pleural membranes are separated only by a thin film of watery fluid called serous fluid, which is secreted by the parietal and visceral pleural membranes. Although no actual space normally exists between the parietal (outer) and visceral (inner) pleural membranes, the potential space between them is called the pleural cavity. The parietal pleura (outer membrane) and visceral pleura (inner membrane) slide with little friction across the cavity walls as your lungs move, expand and collapse during respiration.
Your heart, which is located in the broadest portion of the mediastinum, is surrounded by pericardial membranes called the pericardium. Your pericardium is a protective, fluid-filled sac that surrounds your heart and helps it function properly.
Your pericardium has 2 main layers:
- Fibrous pericardium: This is the tough, outermost layer of your pericardium. It’s made of connective tissue that prevents your heart from expanding too much. It attaches to your major blood vessels at the top of your heart (i.e., aorta, main pulmonary artery, pulmonary veins, superior and inferior vena cava) and to the central tendon of your diaphragm at the bottom of your heart. At the front of your chest, ligaments connect this layer to your breastbone.
- Serous pericardium: This is the inner layer of your pericardium. It’s actually made of two layers, described below. Your serous pericardium produces pericardial fluid that lubricates your heart as it beats.
Your serous pericardium (pericardial membrane) is made of 2 layers:
- Parietal layer (outer layer) of the serous pericardium: This is the outer layer that’s firmly attached to your fibrous pericardium. There’s no space between them.
- Visceral layer (inner layer) of the serous pericardium: This is the innermost layer of your pericardium. It directly covers your heart and the roots of your great vessels. The portion that covers your heart is also known as your epicardium.
Your pericardial cavity is the space between the two layers of your serous pericardium and is filled with a small amount of lubricating serous fluid. The pericardial cavity is the potential space between these visceral pericardium and parietal pericardium membranes. The parietal (outer layer) and visceral (inner layer) serous pericardium slide with little friction across your heart as your heart pumps blood into your cardiovascular system.
Your pericardium has several important functions. These include:
- Cushioning your heart from outside forces and pressure.
- Holding your heart in place.
- Keeping your heart from expanding too much and filling with too much blood.
- Protecting your heart from infections.
- Providing lubrication to reduce friction between your heart and surrounding tissues.
Normally, your pericardium is flexible and stretchy. It can easily expand with your heart as your heart fills up with blood and then contracts to pump the blood out to your body. Pericardial conditions and disorders prevent your heart from expanding as it should. As a result, your heart can’t fill and pump blood efficiently to the rest of your body. This can lead to dangerous complications, including heart failure and cardiogenic shock.
Conditions and disorders that affect your pericardium include:
- Pericarditis: Inflammation of your pericardium. It’s usually acute but can also be chronic.
- Constrictive pericarditis: Constrictive pericarditis is a chronic condition in which your pericardium (the sac around your heart) becomes too thick or stiff. Constrictive pericarditis causes the pericardium to thicken and stiffen, making it difficult for the heart to pump blood. This can lead to heart failure. Constrictive pericarditis symptoms include fatigue, shortness of breath that worsens over time, swelling in your legs and ankles, swollen abdomen, and weakness.
- Pericardial effusion: A buildup of fluid (more than there should be) in your pericardium.
- Cardiac tamponade: A dangerous condition that happens when fluid builds up and puts pressure on your heart. This outside pressure on the heart prevents it from filling properly.
- Pericardial cysts: Growths that may cause no problems but can sometimes put pressure on your heart or lungs.
Symptoms of pericardial problems include chest pain, shortness of breath and heart palpitations.
Your respiratory system includes the trachea, the right and left lungs and their lobes, and the bronchi. Oxygen (O2) is inhaled into your lungs and passes through the alveoli (the tiny air sacs at the end of the bronchioles) and into your bloodstream, where it travels to the tissues throughout the body.
Figure 1. Chest anatomy
Figure 2. Thoracic cavity
Footnote: The black dashed lines indicate the borders of the mediastinum.
Figure 3. Thoracic cavity transverse section
Figure 4. Mediastinum
Figure 5. Pericardium
Figure 6. Respiratory system
The Lungs
The lungs are soft, spongy, cone-shaped organs in the thoracic (chest) cavity. The lungs consist largely of air tubes and spaces. The balance of the lung tissue, its stroma, is a framework of connective tissue containing many elastic fibers. As a result, the lungs are light, soft, spongy, elastic organs that each weigh only about 0.6 kg (1.25 pounds). The elasticity of healthy lungs helps to reduce the effort of breathing.
The left and right lungs are situated in the left and right pleural cavities inside the thoracic cavity. They are separated from each other by the heart and other structures of the mediastinum, which divides the thoracic cavity into two anatomically distinct chambers. As a result, if trauma causes one lung to collapse, the other may remain expanded. Below the lungs, a thin, dome-shaped muscle called the diaphragm separates the chest from the abdomen. When you breathe, the diaphragm moves up and down, forcing air in and out of the lungs. The thoracic cage encloses the rest of the lungs.
Each lung occupies most of the space on its side of the thoracic cavity. A bronchus and some large blood vessels suspend each lung in the cavity. These tubular structures enter the lung on its medial surface.
Parietal refers to a membrane attached to the wall of a cavity; visceral refers to a membrane that is deeper—toward the interior—and covers an internal organ, such as a lung. Within the thoracic (chest) cavity, the compartments that contain the lungs, on either side of the mediastinum, are lined with a membrane called the parietal pleura. A similar membrane, called the visceral pleura, covers each lung.
The parietal and visceral pleural membranes are separated only by a thin film of watery fluid (serous fluid), which they secrete. Although no actual space normally exists between these membranes, the potential space between them is called the pleural cavity.
A thin lining layer called the pleura surrounds the lungs. The pleura protects your lungs and helps them slide back and forth against the chest wall as they expand and contract during breathing. A layer of serous membrane, the visceral pleura, firmly attaches to each lung surface and folds back to become the parietal pleura. The parietal pleura, in turn, borders part of the mediastinum and lines the inner wall of the thoracic cavity and the superior surface of the diaphragm.
In certain conditions, the pleural cavities may fill with air (pneumothorax), blood (hemothorax), or pus. Air in the pleural cavities, most commonly introduced in a surgical opening of the chest or as a result of a stab or gunshot wound, may cause the lungs to collapse. This collapse of a part of a lung, or rarely an entire lung, is called atelectasis. The goal of treatment is the evacuation of air (or blood) from the pleural space, which allows the lung to reinflate. A small pneumothorax may resolve on its own, but it is oft en necessary to insert a chest tube to assist in evacuation.
The thoracic (chest) cavity is divided by a thick wall called the mediastinum. This is the region between the lungs, extending from the base of the neck to the diaphragm. It is occupied by the heart, the major blood vessels connected to it, the esophagus, the trachea and bronchi, and a gland called the thymus.
Each lung is a blunt cone with the tip, or apex, pointing superiorly. The apex on each side extends into the base of the neck, superior to the first rib. The broad concave inferior portion, or base, of each lung rests on the superior surface of the diaphragm.
On the medial (mediastinal) surface of each lung is an indentation, the hilum, through which blood vessels, bronchi, lymphatic vessels, and nerves enter and exit the lung. Collectively, these structures attach the lung to the mediastinum and are called the root of the lung. The largest components of this root are the pulmonary artery and veins and the main (primary) bronchus. Because the heart is tilted slightly to the left of the median plane of the thorax, the left and right lungs differ slightly in shape and size.
Within each root and located in the hilum are:
- a pulmonary artery,
- two pulmonary veins,
- a main bronchus,
- bronchial vessels,
- nerves, and
- lymphatics.
Generally, the pulmonary artery is superior at the hilum, the pulmonary veins are inferior, and the bronchi are somewhat posterior in position. On the right side, the lobar bronchus to the superior lobe branches from the main bronchus in the root, unlike on the left where it branches within the lung itself, and is superior to the pulmonary artery.
Several deep fissures divide the two lungs into different patterns of lobes.
- The left lung is divided into two lobes, the superior lobe and the inferior lobe, by the oblique fissure. The left lung is somewhat smaller than the right and has a cardiac notch, a deviation in its anterior border that accommodates the heart.
- The right lung is partitioned into three lobes, the superior, middle, and inferior lobes, by the oblique and horizontal fissures.
Each lung lobe is served by a lobar (secondary) bronchus and its branches. Each of the lobes, in turn, contains a number of bronchopulmonary segments separated from one another by thin partitions of dense connective tissue. Each segment receives air from an individual segmental (tertiary) bronchus. There are approximately ten bronchopulmonary segments arranged in similar, but not identical, patterns in each of the two lungs.
The bronchopulmonary segments have clinical significance in that they limit the spread of some diseases within the lung, because infections do not easily cross the connective tissue partitions between them. Furthermore, because only small veins span these partitions, surgeons can neatly remove segments without cutting any major blood vessels.
The smallest subdivision of the lung that can be seen with the naked eye is the lobule. Appearing on the lung surface as hexagons ranging from the size of a pencil eraser to the size of a penny, each lobule is served by a bronchiole and its branches. In most city dwellers and in smokers, the connective tissue that separates the individual lobules is blackened with carbon.
Each lung has a half-cone shape, with a base, apex, two surfaces, and three borders.
- The base sits on the diaphragm.
- The apex projects above rib I and into the root of the neck.
- The two surfaces-the costal surface lies immediately adjacent to the ribs and intercostal spaces of the thoracic wall. The mediastinal surface lies against the mediastinum anteriorly and the vertebral column posteriorly and contains the comma-shaped hilum of the lung, through which structures enter and leave.
- The three borders-the inferior border of the lung is sharp and separates the base from the costal surface. The anterior and posterior borders separate the costal surface from the medial surface. Unlike the anterior and inferior borders, which are sharp, the posterior border is smooth and rounded.
Figure 7. Lung anatomy
Figure 8. Lungs pleural cavity
Figure 9. Bronchial tree of the lungs

Right lung
The right lung has three lobes and two fissures. Normally, the lobes are freely movable against each other because they are separated, almost to the hilum, by invaginations of visceral pleura. These invaginations form the fissures:
- The oblique fissure separates the inferior lobe (lower lobe) from the superior lobe and the middle lobe of the right lung.
- The horizontal fissure separates the superior lobe (upper lobe) from the middle lobe.
The approximate position of the oblique fissure on a patient, in quiet respiration, can be marked by a curved line on the thoracic wall that begins roughly at the spinous process of the vertebra TIV level of the spine, crosses the fifth interspace laterally, and then follows the contour of rib VI anteriorly.
The horizontal fissure follows the fourth intercostal space from the sternum until it meets the oblique fissure as it crosses rib V.
The orientations of the oblique and horizontal fissures determine where clinicians should listen for lung sounds from each lobe. The largest surface of the superior lobe is in contact with the upper part of the anterolateral wall and the apex of this lobe proj ects into the root of the neck. The surface of the middle lobe lies mainly adjacent to the lower anterior and lateral wall. The costal surface of the inferior lobe is in contact with the posterior and inferior walls.
The medial surface of the right lung lies adjacent to a number of important structures in the mediastinum and the root of the neck. These include the:
- heart,
- inferior vena cava,
- superior vena cava,
- azygos vein, and
- esophagus.
The right subclavian artery and vein arch over and are related to the superior lobe of the right lung as they pass over the dome of the cervical pleura and into the axilla.
Left lung
The left Iung is smaller than the right lung and has two lobes separated by an oblique fissure. The oblique fissure of the left lung is slightly more oblique than the corresponding fissure of the right lung. During quiet respiration, the approximate position of the left oblique fissure can be marked by a curved line on the thoracic wall that begins between the spinous processes of thoracic vertebrae 3 (T3) and thoracic vertebrae 4 (TIV), crosses the fifth interspace laterally, and follows the contour of 6th rib anteriorly.
As with the right lung, the orientation of the oblique fissure determines where to listen for lung sounds from each lobe. The largest surface of the superior lobe is in contact with the upper part of the anterolateral wall, and the apex of this lobe proj ects into the root of the neck. The costal surface of the inferior lobe is in contact with the posterior and inferior walls.
The inferior portion o f the medial surface of the left lung, unlike the right lung, is notched because of the heart’s projection into the left pleural cavity from the middle mediastinum. From the anterior border of the lower part of the superior lobe a tongue-like extension (the lingula of the left lung) projects over the heart bulge.
The medial surface of the left lung lies adjacent to a number of important structures in the mediastinum and root of the neck. These include the:
- heart,
- aortic arch,
- thoracic aorta, and
- esophagus.
The left subclavian artery and vein arch over and are related to the superior lobe of the left lung as they pass over the dome of the cervical pleura and into the axilla.
Bronchial tree
The trachea is a flexible tube that extends from cervical spine C6 (vertebral level C VI) in the lower neck to thoracic spine T4-T5 (vertebral level T4 to T5) in the mediastinum where it bifurcates into a right and a left main bronchus. The trachea is held open by C-shaped transverse cartilage rings embedded in its wall the open part of the C facing posteriorly. The lowest tracheal ring has a hook-shaped structure, the carina, that projects backwards in the midline between the origins of the two main bronchi. The posterior wall of the trachea is composed mainly of smooth muscle. Each main bronchus enters the root of a lung and passes through the hilum into the lung itself. The right main bronchus is wider and takes a more vertical course through the root and hilum than the left main bronchus. Therefore, inhaled foreign bodies tend to lodge more frequently on the right side than on the left.
The bronchial tree consists of branched airways leading from the trachea to the microscopic air sacs in the lungs. Its branches begin with the right and left main (primary) bronchi, which arise from the trachea at the level of the fifth thoracic vertebra. Each bronchus enters its respective lung. A short distance from its origin, each main bronchus divides into lobar (secondary) bronchi. The lobar bronchi branch into segmental (tertiary) bronchi, which supply bronchopulmonary segments. Within each bronchopulmonary segment, the segmental bronchi give rise to multiple generations of divisions of increasingly finer tubes and, ultimately, to bronchioles , which further subdivide to terminal bronchioles, respiratory bronchioles, and finally to very thin tubes called alveolar ducts. These ducts lead to thin-walled outpouchings called alveolar sacs. Alveolar sacs lead to smaller, microscopic air sacs called alveoli (singular, alveolus), which lie within capillary networks (Figure 6). The alveoli are the sites of gas exchange between the inhaled air and the bloodstream.
The structure of a bronchus is similar to that of the trachea, but the tubes that branch from it have less cartilage in their walls, and the bronchioles lack cartilage. As the cartilage diminishes, a layer of smooth muscle surrounding the tube becomes more prominent. This muscular layer persists even in the smallest bronchioles, but only a few muscle cells are associated with the alveolar ducts.
The absence of cartilage in the bronchioles allows their diameters to change in response to contraction of the smooth muscle in their walls, similar to what happens with arterioles of the cardiovascular system. Part of the “fight-or-flight” response, triggered by the sympathetic nervous system, is bronchodilation, in which the smooth muscle relaxes and the airways become wider and allow more airflow. The opposite, bronchoconstriction, occurs when the smooth muscle contracts and it becomes difficult to move air in and out of the lungs. Bronchoconstriction can occur with allergies. Asthma is an extreme example of bronchoconstriction.
The mucous membranes of the bronchial tree continue to filter the incoming air, and the many branches of the tree distribute the air to alveoli throughout the lungs. The alveoli, in turn, provide a large surface area of thin simple squamous epithelial cells through which gases are easily exchanged. Oxygen diffuses from the alveoli into the blood in nearby capillaries, and carbon dioxide diffuses from the blood into the alveoli.
Lung pain causes
Lung pain is a general term to describe chest pain which is non-specific sensation of discomfort or pain that you feel in your chest and can have many causes ranging from life-threatening medical emergency like a heart attack, pulmonary embolism (a sudden blockage in a lung artery due to a blood clot that breaks loose and travels through the bloodstream to the lungs) or angina (chest pain or discomfort that occurs when the heart’s blood flow is reduced) to lung issues, muscle strain, digestive problems such as acid reflux or heartburn to esophagus disorders such as esophageal spasms, esophagitis (a condition in which the lining of the esophagus becomes swollen, inflamed, or irritated), gastroesophageal reflux disease (GERD) or esophageal cancer. Heartburn, acid reflux, esophageal spasm, angina and heart attack may feel very much alike. Don’t try to diagnose the cause yourself. Even experienced doctors can’t always tell the difference from your medical history and a physical exam. That’s why you must seek urgent medical attention. So if you are not sure seek medical attention immediately. If you have persistent lung pain, unexplained shortness of breath, and you aren’t sure it’s heartburn, call your local emergency number to ask for emergency medical help and an ambulance. Treatment depends on the cause of your chest pain.
“Lung pain” can occur due to a number of possible reasons because any organ or tissue in your chest can be the source of your pain, including your heart, lungs, esophagus, muscles, ribs, tendons, or nerves. “Lung pain” may also spread to the chest from the neck, abdomen, and back and may be due to problems in any of those areas.
- Heart and vascular related causes
- Angina: Pain caused by reduced blood flow to the heart muscle.
- Heart attack also known as a myocardial infarction is a blockage of blood flow to the heart muscle. A heart attack is a medical emergency. Call your local emergency number if you think you or someone else is having a heart attack.
- Coronary artery disease: A narrowing or blockage in your heart’s arteries. Coronary artery disease (coronary heart disease) symptoms may include chest pain that may spread to your neck, jaw, arms, or back and shortness of breath. A complete blockage of blood flow to your heart can cause a heart attack (myocardial infarction). Smoking or having high blood pressure, high cholesterol, diabetes, obesity or a strong family history of heart disease makes you more likely to get coronary artery disease (coronary heart disease). If you’re at high risk of coronary artery disease, see your doctor. You may need tests to check for narrowed arteries and coronary artery disease.
- Heart failure also known as congestive heart failure, is a condition where the heart can’t pump blood properly. It can affect one or both sides of the heart.
- Pericarditis: Pericarditis is an infection or inflammation in the lining around your heart, causing a sharp pain in your chest. Symptoms include chest pain, shortness of breath, and palpitations. The pain can spread to your left shoulder and arm. The pain can be worse when you’re lying down and when taking deep breaths.
- Constrictive pericarditis: Constrictive pericarditis is a chronic condition in which your pericardium (the sac around your heart) becomes too thick or stiff. Constrictive pericarditis causes the pericardium to thicken and stiffen, making it difficult for the heart to pump blood. This can lead to heart failure. Constrictive pericarditis symptoms include fatigue, shortness of breath that worsens over time, swelling in your legs and ankles, swollen abdomen, and weakness.
- Pericardial effusion: A buildup of fluid (more than there should be) in your pericardium.
- Cardiac tamponade: A dangerous condition that happens when fluid builds up and puts pressure on your heart. This outside pressure on the heart prevents it from filling properly.
- Pericardial cysts: Pericardial cyst is a rare, benign, fluid-filled sac that develops within the pericardial sac (pericardial space) surrounding your heart, often discovered incidentally on imaging. Pericardial cyst is usually asymptomatic but can cause symptoms if they grow large or compress nearby structures. Pericardial cysts are most commonly found in the right cardiophrenic angle, but can also occur in other areas of the mediastinum (the space in the chest). In rare cases, a pericardial cyst can lead to complications like compression of the heart or lungs, or even rupture of the cyst.
- Hypertrophic cardiomyopathy (HCM). Hypertrophic cardiomyopathy (HCM) is a genetic disease that causes your heart muscle to thicken especially the ventricles or lower heart chambers, left ventricular stiffness, mitral valve changes and cellular changes. The muscle walls of your pumping ventricles or lower heart chambers become thick and stiff. This thickening can affect your heart’s ability to pump blood. With hypertrophic cardiomyopathy (HCM), you can’t get enough blood into — or out of — your heart’s chambers, and your heart has a harder time getting oxygen-rich blood.
- Aortic dissection. Aortic dissection is a tear in the aorta, the main artery that carries blood from your heart to your body. Aortic dissection is a medical emergency that can be fatal if not treated promptly. Aortic dissection can cause very strong pain in your chest, back and between your shoulder blades that happens without warning and feels like something is ripping.
- Aortic aneurysm. Aortic aneurysm is a balloon-like bulge in the aorta, your body’s main artery that carries blood from your heart to your body. Aortic aneurysm can occur in your chest (thoracic aortic aneurysm) or abdomen (abdominal aortic aneurysm). Blood that pushes against a weak part of your aorta’s wall can make it bulge out. Without treatment, this weak spot can break open and cause severe pain in your chest or abdomen. If an aortic aneurysm ruptures, it’s an emergency that requires immediate treatment.
- Mitral valve prolapse. Your mitral valve controls blood flow from your left atrium (upper left heart chamber) to your left ventricle (bottom left heart chamber). Mitral valve has two leaflets (flaps) that open to let blood flow from your left atrium to your left ventricle. When the Mitral valve closes, it prevents blood from moving backward. Sometimes, your mitral valve doesn’t work right because it’s too narrow or leaky. This can make your heart work harder to pump blood to your body. Mitral valve prolapse (MVP) is a heart condition that occurs when the mitral valve flaps bulge into the left atrium of the heart. This can cause blood to leak backward into the atrium, a condition called mitral valve regurgitation. This can make your heart work harder to pump blood to your body. Treatment for mitral valve disease depends on the severity of the condition and whether it is worsening. Sometimes, surgery is recommended to repair or replace the mitral valve.
- Lung-related causes
- Pneumonia. Pneumonia is a lung infection that can be caused by bacteria, viruses, or fungi. Pneumonia or lung infection can range from mild to severe.
- Pleurisy or pleuritis. Pleurisy or pleuritis is infection and/or inflammation of the membrane (parietal pleura and visceral pleura membranes) that surrounds your lungs and lines your chest cavity. It can cause sharp chest pain when you cough or breathe deeply. You may also have pain in your shoulder.
- Pulmonary embolism (PE). A pulmonary embolism (PE) is a blockage in your lung’s arteries caused by a blood clot. A blood clot can come from another part of your body (usually from deep vein in your leg and travels to the lungs) and get stuck in a pulmonary artery inside your lung. People with a pulmonary embolism (PE) often describe sharp chest pain that worsens when they breathe in. You may have shortness of breath especially when breathing in, coughing up blood, or a fast/racing heart rate (tachycardia). Other symptoms of pulmonary embolism (PE) include feeling like you’re having a heart attack, anxiety, dizziness, lightheadedness, or fainting, palpitations (fast, strong, or irregular heartbeat) and sweating. Pulmonary embolism (PE) is a life-threatening medical emergency that requires immediate treatment.
- Collapsed lung also known as a pneumothorax. A collapsed lung (pneumothorax) is a condition that occurs when air leaks into the pleural cavity or the space between your lung and chest wall. This causes part or all of your lung to collapse. This puts pressure on your lung, making it difficult to expand when you breathe in. With no warning, you may feel a sharp pain in your chest and possibly your neck and shoulder.
- Asthma: Asthma is a chronic lung disease that makes it hard to breathe. Asthma is caused by inflammation and muscle tightening in the airways. Asthma symptoms include coughing, wheezing, shortness of breath, chest tightness, and fatigue.
- Lung cancer: Lung cancer is cancer that starts when abnormal cells in your lungs grow and multiply out of control. People who smoke have the greatest risk of lung cancer. The risk of lung cancer increases with the length of time and number of cigarettes smoked. Lung cancer is the leading cause of cancer deaths worldwide. Lung cancer typically doesn’t cause symptoms early on. Symptoms of lung cancer usually happen when the disease is advanced. Symptoms include a chronic cough, shortness of breath, and feeling tired or weak.
- Chronic obstructive pulmonary disease (COPD). Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes it difficult to breathe. Chronic obstructive pulmonary disease (COPD) is caused by damage to your lungs air sacs and/or airway lining that narrows the airways making it difficult for you to breathe. Symptoms include coughing up phlegm, shortness of breath, chest tightness, wheezing, and tiredness. Your chest may feel tight and you may have shortness of breath and/or wheezing. COPD is not curable, but treatments can help manage your symptoms. In some people, COPD worsens over time and can lead to life-threatening problems. Treatment include inhaled medicines, oxygen, pulmonary rehabilitation programs, antibiotics, and steroid tablets.
- Pulmonary hypertension. Pulmonary hypertension is a serious condition that causes high blood pressure in the arteries of your lungs (pulmonary arteries). Pulmonary arteries are the blood vessels that take blood to your lungs to trade carbon dioxide for oxygen. It can be caused by other diseases or develop on its own. You get chest pain because it’s harder for your heart to push blood through blood vessels (pulmonary arteries) when hypertension adds resistance to blood flow. You can have shortness of breath with this condition.
- Tuberculosis (TB). Tuberculosis (TB) is a bacterial infection caused by the Mycobacterium tuberculosis bacteria. Tuberculosis (TB) most commonly affects your lungs, but can also spread to other parts of your body, such as your brain, spine, or kidneys and can cause serious illness. Tuberculosis (TB) can be cured with specific antibiotics.
- Digestive-related causes
- Esophageal spasm. Esophageal spasm are painful abnormal painful contractions of the muscles in the esophagus (the muscular tube that carries food from your mouth to your stomach). Esophageal spasms do not move food effectively to your stomach. The cause of esophageal spasm is unknown. Very hot or very cold foods may trigger an episode of esophageal spasm in some people.
- Acid reflux also called heartburn, acid indigestion, acid regurgitation or gastroesophageal reflux (GER) is a painful burning feeling in your chest or throat that occurs when stomach acid backs up into the tube called the esophagus that carries food from your mouth to your stomach 1, 2, 3. Typically, when food is swallowed, a band of muscle around the bottom of your esophagus called the lower esophageal sphincter (LES) relaxes to allow food and liquid to flow down into your stomach. Then the lower esophageal sphincter muscle tightens again. If the lower esophageal sphincter (LES) isn’t working as it should, stomach acid can flow back up into your esophagus (acid reflux) and you might feel a burning sensation in your chest, commonly called heartburn. The acid backup may be worse when you’re bent over, lying down, after eating a big meal or drinking coffee or alcohol. Pregnancy, certain foods, and some medications can bring on heartburn. Treating heartburn is important because over time as acid reflux can damage your esophagus.
- Gastroesophageal reflux disease (GERD) also called gastro-oesophageal reflux disease (GORD), is a condition that develops when there is a backward flow or reflux of stomach contents (acid from the food and liquid in your stomach) back up into your throat and esophagus causing troublesome symptoms and/or complications 4, 5, 6, 7, 8. Gastroesophageal reflux disease can present as non-erosive reflux disease or erosive esophagitis. It can occur at any age, even in babies. Many times, you or your doctor can determine the triggers for your reflux.
- Esophagitis also called erosive esophagitis or ulcerative esophagitis is present when the lining of your esophagus becomes swollen, inflamed, or irritated 9. Esophagitis can cause painful, difficult swallowing. Esophagitis can also lead to chest pain. Various things can cause esophagitis. Some common causes include stomach acids backing up into the esophagus, infection, medicines taken by mouth and allergies. Chronic acid reflux (GERD) is a common cause of esophagitis.
- Hiatal hernia. A hiatal hernia occurs the upper part of your stomach pushes up into your chest through the diaphragm (the large muscle that separates the abdomen and the chest). Normally the diaphragm has a small opening called a hiatus. The tube used for swallowing food, called the esophagus, passes through the hiatus of the diaphragm before connecting to the stomach. In a hiatal hernia, the stomach pushes up through that opening and into your chest. A small hiatal hernia usually doesn’t cause problems. You may never know you have one unless your doctor discovers it when checking for another condition. But a large hiatal hernia can allow food and acid to back up into your esophagus. This can cause heartburn, chest pain, and difficulty swallowing. Self-care measures or medicines can usually relieve these symptoms. A very large hiatal hernia might need surgery.
- Gastritis. Gastritis is when your stomach lining gets inflamed (red and swollen). Your stomach lining is strong. In most cases, acid does not hurt it. But it can get inflamed and irritated if you drink too much alcohol, have damage from pain relievers called non-steroidal anti-inflammatory drugs (NSAIDs), or smoke. Stomach lining inflammation from many causes can make your lower left chest hurt. You also might feel sick to your stomach and throw up.
- Pancreatitis. Pancreatitis is inflammation of your pancreas, an organ that produces digestive enzymes and hormones such as insulin and glucagon. Pancreatitis can be acute pancreatitis (sudden and severe) or chronic pancreatitis (ongoing). Pancreatitis symptoms may include pain in the upper abdomen that may spread to the back, nausea and vomiting, fever, rapid pulse, and weight loss.
- Esophageal cancer is cancer that occurs in the esophagus. Esophageal cancer usually begins in the cells that line the inside of the esophagus. Esophageal cancer can occur anywhere along the esophagus. More men than women get esophageal cancer.
- Gallstones also known as cholelithiasis. Gallstones are hardened deposits of bile that form in your gallbladder. Gallstones can range in size from a grain of sand to a golf ball. Some people develop just one gallstone, while others develop many gallstones at the same time. With cholesterol as their main ingredient, gallstones can block ducts where a fluid (bile) that helps digestion needs to go to reach your small intestine. Swelling in your gallbladder causes pain under your ribs on your right side. This extreme pain can last for many hours. People who experience symptoms from their gallstones usually require gallbladder removal surgery (cholecystectomy). Gallstones that don’t cause any signs and symptoms typically don’t need treatment.
- Musculoskeletal-related causes
- Costochondritis also known as chest wall pain syndrome or costosternal syndrome is inflammation of the cartilage that connects your ribs to your breastbone.
- Sprained chest muscle also known as pulled chest muscle, is a minor injury, tear or stretch in a chest muscle that usually heals on its own within a few weeks. A chest muscle sprain can cause pain, swelling, bruising, and muscle spasms.
- Broken rib. Broken rib also called rib fracture is a common injury that occurs when one of the bones in your rib cage breaks or cracks. The most common causes are hard impacts from falls, car accidents or contact sports. Broken rib hurts a lot, especially when you breathe deeply. The sharp edge of a broken bone can harm major blood vessels or lungs and other organs inside your chest. Usually, broken ribs heal on their own in about six weeks. The pain lasts for several weeks. Pain control is important for being able to breathe deeply and avoid lung issues, such as pneumonia.
- Other causes
- Shingles also known as herpes zoster, is a painful rash caused by the varicella-zoster virus (VZV), the virus that gave you chickenpox as a child can become active again later, usually in people older than 50. As shingles, the varicella-zoster virus (VZV) causes a painful rash on your upper body. It usually develops in part of your chest, and typically only on one side. Risk factors for shingles include having had chickenpox in the past, being older, and having a weakened immune system.
- Panic attack and anxiety disorders are a group of mental health conditions that cause fear, dread and other symptoms that are out of proportion to the situation. There are several types, including generalized anxiety disorder (GAD), specific phobias and social anxiety disorder. Treatment is effective and usually includes medication and psychotherapy (talk therapy).
You may not be able to tell the difference between a heart attack and non-serious chest pain. For this reason, you should always take chest pain seriously. If it’s sudden or new and lasts longer than five minutes, go to the emergency room (ER). If it goes away after a few minutes, it may not be an emergency, but you should still see your doctor as soon as possible to determine the cause. Non-serious chest pain, whatever the cause, can always occur again, and can end up affecting your quality of life.
Right-Side Chest Pain
Right-side chest pain has multiple causes and can come from a number of issues in your lungs, muscles, bones or digestive system. Right-side chest pain can be sharp. It may hurt more when you take a deep breath. You might feel sharp pain in some cases. You may have other symptoms along with right-side chest pain, like tightness or difficulty breathing.
Right-side chest pain common causes may include:
- Pulmonary embolism (PE). A pulmonary embolism (PE) is a blockage in your lung’s arteries caused by a blood clot. A blood clot can come from another part of your body (usually from deep vein in your leg and travels to the lungs) and get stuck in a pulmonary artery inside your lung. People with a pulmonary embolism (PE) often describe sharp chest pain that worsens when they breathe in. You may have shortness of breath especially when breathing in, coughing up blood, or a fast/racing heart rate (tachycardia). Other symptoms of pulmonary embolism (PE) include feeling like you’re having a heart attack, anxiety, dizziness, lightheadedness, or fainting, palpitations (fast, strong, or irregular heartbeat) and sweating. Pulmonary embolism (PE) is a life-threatening medical emergency that requires immediate treatment.
- Chronic obstructive pulmonary disease (COPD). Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes it difficult to breathe. Chronic obstructive pulmonary disease (COPD) is caused by damage to your lungs air sacs and/or airway lining that narrows the airways making it difficult for you to breathe. Symptoms include coughing up phlegm, shortness of breath, chest tightness, wheezing, and tiredness. Your chest may feel tight and you may have shortness of breath and/or wheezing. COPD is not curable, but treatments can help manage your symptoms. In some people, COPD worsens over time and can lead to life-threatening problems. Treatment include inhaled medicines, oxygen, pulmonary rehabilitation programs, antibiotics, and steroid tablets.
- Pneumonia. Pneumonia is a lung infection that can be caused by bacteria, viruses, or fungi. Pneumonia or lung infection can range from mild to severe. Pneumonia symptoms can include:
- Coughing up mucus, which may be yellow, green, or bloody
- Fever
- Chills
- Shortness of breath
- Chest pain
- Rapid breathing or heart rate
- Sweating
- Loss of appetite
- Treatment for pneumonia depends on whether it’s caused by bacteria, viruses, or fungi including your lung function and health status. For bacterial pneumonia, antibiotics are the main treatment. For viral pneumonia, rest, fluids, and fever medicine may help. For fungal pneumonia, your doctor may prescribe antifungal medication.
- Pleurisy or pleuritis. Pleurisy or pleuritis is infection and/or inflammation of the membrane (parietal pleura and visceral pleura membranes) that surrounds your lungs and lines your chest cavity. It can cause sharp chest pain when you cough or breathe deeply. You may also have pain in your shoulder. Causes of pleurisy may include:
- Infections like pneumonia, tuberculosis, or viral infections
- A pulmonary embolus (PE)
- Cancer, such as lung cancer or mesothelioma
- Trauma to the chest wall, such as a rib fracture
- Pneumothorax (collapsed lung). A pneumothorax also known as a collapsed lung, is a condition that occurs when air leaks into the pleural cavity or the space between your lung and chest wall. This causes part or all of your lung to collapse. This puts pressure on your lung, making it difficult to expand when you breathe in. With no warning, you may feel a sharp pain in your chest and possibly your neck and shoulder.
- Pneumothorax (collapsed lung) symptoms include:
- Sudden chest pain, usually on one side
- Shortness of breath
- Bluish skin, nails, and lips
- Coughing
- Fatigue
- Fast breathing or heartbeat
- Shoulder pain
- Lightheadedness or feeling like you are about to faint
- Causes of pneumothorax (collapsed lung) can include:
- Chest trauma, such as a fractured rib or knife wound
- Excess pressure on the lungs
- Lung disease, such as chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, tuberculosis, or whooping cough
- Mechanical ventilation
- Ruptured air blisters
- Pneumothorax (collapsed lung) symptoms include:
- Pulmonary hypertension. Pulmonary hypertension is a serious condition that causes high blood pressure in the arteries of your lungs (pulmonary arteries). Pulmonary arteries are the blood vessels that take blood to your lungs to trade carbon dioxide for oxygen. It can be caused by other diseases or develop on its own. You get chest pain because it’s harder for your heart to push blood through blood vessels (pulmonary arteries) when hypertension adds resistance to blood flow. You can have shortness of breath with this condition.
- Pulmonary hypertension symptoms include:
- Shortness of breath, especially during physical activity
- Chest pain
- Lightheadedness
- Fatigue
- Racing heartbeat
- Swelling in the ankles or legs
- Coughing and wheezing
- Pain in the upper right side of the stomach
- Decreased appetite
- Pulmonary hypertension symptoms include:
- Asthma. Asthma is a chronic lung disease that makes it hard to breathe. Asthma is caused by inflammation and muscle tightening in the airways.
- Asthma triggers include:
- Inhaling allergens like pollen, dust, mold, or pet dander
- Cigarette smoke
- Exercise, especially in cold or dry air
- Workplace irritants like chemical fumes or gases
- Asthma symptoms include coughing, wheezing, shortness of breath, chest tightness, and fatigue
- Asthma triggers include:
- Lung cancer. Lung cancer is cancer that starts when abnormal cells in your lungs grow and multiply out of control. People who smoke have the greatest risk of lung cancer. The risk of lung cancer increases with the length of time and number of cigarettes smoked. Lung cancer is the leading cause of cancer deaths worldwide. Lung cancer typically doesn’t cause symptoms early on. Symptoms of lung cancer usually happen when the disease is advanced.
- Signs and symptoms of lung cancer that happen in and around the lungs may include:
- A new cough that doesn’t go away.
- Chest pain.
- Coughing up blood, even a small amount.
- Hoarseness.
- Shortness of breath.
- Wheezing.
- Signs and symptoms that happen when lung cancer spreads to other parts of the body may include:
- Bone pain.
- Headache.
- Losing weight without trying.
- Loss of appetite.
- Swelling in the face or neck.
- Signs and symptoms of lung cancer that happen in and around the lungs may include:
- Broken rib. Broken rib also called rib fracture is a common injury that occurs when one of the bones in your rib cage breaks or cracks. The most common causes are hard impacts from falls, car accidents or contact sports. Broken rib hurts a lot, especially when you breathe deeply. The sharp edge of a broken bone can harm major blood vessels or lungs and other organs inside your chest. Usually, broken ribs heal on their own in about six weeks. The pain lasts for several weeks. Pain control is important for being able to breathe deeply and avoid lung issues, such as pneumonia.
- Sprained chest muscle (pulled chest muscle). A sprained chest muscle is a minor injury, tear or stretch in a chest muscle that usually heals on its own within a few weeks. A chest muscle sprain can cause pain, swelling, bruising, and muscle spasms.
- A sprained chest muscle symptoms include:
- Pain or tenderness
- Redness or bruising
- Limited motion
- Muscle spasms
- Swelling
- Muscle weakness
- The best treatment for sprained chest muscle is rest, ice, compression, and elevation (RICE):
- Rest: Stop activities that strain the chest muscle
- Ice: Apply ice or a cold pack for 20 minutes up to three times a day
- Compression: Wrap an elastic bandage around the chest to reduce swelling
- Elevation: Keep the chest elevated, especially at night
- Medication: Take nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, to relieve pain and inflammation
- A sprained chest muscle symptoms include:
- Shingles also known as herpes zoster. Shingles is a painful rash caused by the varicella-zoster virus (VZV), the virus that gave you chickenpox as a child can become active again later, usually in people older than 50. As shingles, this virus causes a painful rash on your upper body. It usually develops in part of your chest, and typically only on one side. Risk factors for shingles include having had chickenpox in the past, being older, and having a weakened immune system.
- Shingles symptoms include:
- A painful, itchy, or tingling rash that usually appears on one side of the body
- Small red spots that turn into blisters
- Burning or shooting pain
- Skin sensitivity
- Early treatment may shorten a shingles infection and lessen the chance of complications. The most common complication is postherpetic neuralgia. This is a painful condition that causes shingles pain for a long time after your blisters have cleared.
- Shingles symptoms include:
- Gallstones also known as cholelithiasis. Gallstones are hardened deposits of bile that form in your gallbladder. Gallstones can range in size from a grain of sand to a golf ball. Some people develop just one gallstone, while others develop many gallstones at the same time. With cholesterol as their main ingredient, gallstones can block ducts where a fluid (bile) that helps digestion needs to go to reach your small intestine. Swelling in your gallbladder causes pain under your ribs on your right side. This extreme pain can last for many hours. People who experience symptoms from their gallstones usually require gallbladder removal surgery (cholecystectomy). Gallstones that don’t cause any signs and symptoms typically don’t need treatment.
- Gallstones symptoms may include:
- Sudden, severe pain in the upper right abdomen, called a gallbladder attack or biliary colic
- Pain that may spread to your side or shoulder blade
- Fever
- Yellowing of skin and whites of the eyes (jaundice).
- Gallstones symptoms may include:
- Tuberculosis (TB). Tuberculosis (TB) is a bacterial infection caused by the Mycobacterium tuberculosis bacteria. Tuberculosis (TB) most commonly affects your lungs, but can also spread to other parts of your body, such as your brain, spine, or kidneys and can cause serious illness. Tuberculosis (TB) can be cured with specific antibiotics.
Left-Side Chest Pain
Left-side chest pain has multiple causes and can come from a number of issues in your heart, blood vessels, lungs, muscles, bones or digestive system. Left-side chest pain from heart-related issues can be strong or sharp. It can feel like pressure. You can also have nausea, but that can go along with digestive issues that also cause chest pain. And there are lung issues that cause pain in your chest and difficulty breathing. You can also have chest pain due to injury or soreness of your muscles and bones.
Left-side chest pain common causes may include:
- Heart attack also known as a myocardial infarction (MI) occurs when blood flow to your heart is blocked. A heart attack is a medical emergency. Call your local emergency number if you think you or someone else is having a heart attack. Your heart muscle dies when it can’t get enough oxygen because of a blockage in the coronary artery supplying your heart muscle. A heart attack usually presents as chest pain, discomfort, tightness, burning, or squeezing or pressure over a wide area of your chest.
- Coronary artery disease also known as coronary heart disease is a heart condition that occurs when the coronary arteries that supply blood to your heart become damaged or narrowed. This can reduce blood flow and oxygen to your heart muscle. A buildup of fats, cholesterol and other substances in and on the coronary artery walls, a condition called atherosclerosis, usually causes coronary artery disease. The buildup, called plaque, makes the arteries narrow and block the coronary arteries (blood vessels that carry blood) to your heart. Symptoms may include chest pain and shortness of breath. A complete blockage of the coronary artery blood flow can cause a heart attack. It’s typically worse with exercise because you can’t get enough blood to your heart muscle and clogged coronary arteries. You can often relieve this with rest. Eating a nutritious diet, getting regular exercise and not smoking can help prevent coronary artery disease and the conditions that can cause it.
- Coronary artery dissection also called spontaneous coronary artery dissection (SCAD) is a rare but serious condition that occurs when a tear in the wall of a coronary artery blocks blood flow to your heart. Spontaneous coronary artery dissection (SCAD) can lead to a heart attack, heart rhythm problems or sudden death if it isn’t treated promptly. A coronary artery wall can rip, create a bulge and block your artery. This causes pressure or pain in your chest, and it could lead to a heart attack. Spontaneous coronary artery dissection (SCAD) most commonly affects women in their 40s and 50s, though it can occur at any age and can occur in men. People who have spontaneous coronary artery dissection (SCAD) often don’t have risk factors for heart disease, such as high blood pressure, high cholesterol or diabetes.
- Pericarditis. Pericarditis is an infection or inflammation in the lining around your heart, causing a sharp pain in your chest. Symptoms include chest pain, shortness of breath, and palpitations. The pain can spread to your left shoulder and arm. The pain can be worse when you’re lying down and when taking deep breaths.
- Constrictive pericarditis. Constrictive pericarditis is a chronic condition in which your pericardium (the sac around your heart) becomes too thick or stiff. Constrictive pericarditis causes the pericardium to thicken and stiffen, making it difficult for the heart to pump blood. This can lead to heart failure. Constrictive pericarditis symptoms include fatigue, shortness of breath that worsens over time, swelling in your legs and ankles, swollen abdomen, and weakness.
- Hypertrophic cardiomyopathy (HCM). Hypertrophic cardiomyopathy (HCM) is a genetic disease that causes your heart muscle to thicken especially the ventricles or lower heart chambers, left ventricular stiffness, mitral valve changes and cellular changes. The muscle walls of your pumping ventricles or lower heart chambers become thick and stiff. This thickening can affect your heart’s ability to pump blood. With hypertrophic cardiomyopathy (HCM), you can’t get enough blood into — or out of — your heart’s chambers, and your heart has a harder time getting oxygen-rich blood.
- Aortic dissection. Aortic dissection is a tear in the aorta, the main artery that carries blood from your heart to your body. Aortic dissection is a medical emergency that can be fatal if not treated promptly. Aortic dissection can cause very strong pain in your chest, back and between your shoulder blades that happens without warning and feels like something is ripping.
- Aortic aneurysm. Aortic aneurysm is a balloon-like bulge in the aorta, your body’s main artery that carries blood from your heart to your body. Aortic aneurysm can occur in your chest (thoracic aortic aneurysm) or abdomen (abdominal aortic aneurysm). Blood that pushes against a weak part of your aorta’s wall can make it bulge out. Without treatment, this weak spot can break open and cause severe pain in your chest or abdomen. If an aortic aneurysm ruptures, it’s an emergency that requires immediate treatment.
- Mitral valve prolapse. Your mitral valve controls blood flow from your left atrium (upper left heart chamber) to your left ventricle (bottom left heart chamber). Mitral valve has two leaflets (flaps) that open to let blood flow from your left atrium to your left ventricle. When the Mitral valve closes, it prevents blood from moving backward. Sometimes, your mitral valve doesn’t work right because it’s too narrow or leaky. This can make your heart work harder to pump blood to your body. Mitral valve prolapse (MVP) is a heart condition that occurs when the mitral valve flaps bulge into the left atrium of the heart. This can cause blood to leak backward into the atrium, a condition called mitral valve regurgitation. This can make your heart work harder to pump blood to your body. Treatment for mitral valve disease depends on the severity of the condition and whether it is worsening. Sometimes, surgery is recommended to repair or replace the mitral valve.
- Pneumonia. Pneumonia is a lung infection that can be caused by bacteria, viruses, or fungi. Pneumonia or lung infection can range from mild to severe.
- Pleurisy or pleuritis. Pleurisy or pleuritis is infection and/or inflammation of the membrane (parietal pleura and visceral pleura membranes) that surrounds your lungs and lines your chest cavity. It can cause sharp chest pain when you cough or breathe deeply. You may also have pain in your shoulder.
- Pulmonary embolism (PE). A pulmonary embolism (PE) is a blockage in your lung’s arteries caused by a blood clot. A blood clot can come from another part of your body (usually from deep vein in your leg and travels to the lungs) and get stuck in a pulmonary artery inside your lung. People with a pulmonary embolism (PE) often describe sharp chest pain that worsens when they breathe in. You may have shortness of breath especially when breathing in, coughing up blood, or a fast/racing heart rate (tachycardia). Other symptoms of pulmonary embolism (PE) include feeling like you’re having a heart attack, anxiety, dizziness, lightheadedness, or fainting, palpitations (fast, strong, or irregular heartbeat) and sweating. Pulmonary embolism (PE) is a life-threatening medical emergency that requires immediate treatment.
- Collapsed lung also known as a pneumothorax. A collapsed lung (pneumothorax) is a condition that occurs when air leaks into the pleural cavity or the space between your lung and chest wall. This causes part or all of your lung to collapse. This puts pressure on your lung, making it difficult to expand when you breathe in. With no warning, you may feel a sharp pain in your chest and possibly your neck and shoulder.
- Asthma: Asthma is a chronic lung disease that makes it hard to breathe. Asthma is caused by inflammation and muscle tightening in the airways. Asthma symptoms include coughing, wheezing, shortness of breath, chest tightness, and fatigue.
- Chronic obstructive pulmonary disease (COPD). Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that makes it difficult to breathe. Chronic obstructive pulmonary disease (COPD) is caused by damage to your lungs air sacs and/or airway lining that narrows the airways making it difficult for you to breathe. Symptoms include coughing up phlegm, shortness of breath, chest tightness, wheezing, and tiredness. Your chest may feel tight and you may have shortness of breath and/or wheezing. COPD is not curable, but treatments can help manage your symptoms. In some people, COPD worsens over time and can lead to life-threatening problems. Treatment include inhaled medicines, oxygen, pulmonary rehabilitation programs, antibiotics, and steroid tablets.
- Pulmonary hypertension. Pulmonary hypertension is a serious condition that causes high blood pressure in the arteries of your lungs (pulmonary arteries). Pulmonary arteries are the blood vessels that take blood to your lungs to trade carbon dioxide for oxygen. It can be caused by other diseases or develop on its own. You get chest pain because it’s harder for your heart to push blood through blood vessels (pulmonary arteries) when hypertension adds resistance to blood flow. You can have shortness of breath with this condition.
- Tuberculosis (TB). Tuberculosis (TB) is a bacterial infection caused by the Mycobacterium tuberculosis bacteria. Tuberculosis (TB) most commonly affects your lungs, but can also spread to other parts of your body, such as your brain, spine, or kidneys and can cause serious illness. Tuberculosis (TB) can be cured with specific antibiotics.
- Hiatal hernia. A hiatal hernia occurs the upper part of your stomach pushes up into your chest through the diaphragm (the large muscle that separates the abdomen and the chest). Normally the diaphragm has a small opening called a hiatus. The tube used for swallowing food, called the esophagus, passes through the hiatus of the diaphragm before connecting to the stomach. In a hiatal hernia, the stomach pushes up through that opening and into your chest. A small hiatal hernia usually doesn’t cause problems. You may never know you have one unless your doctor discovers it when checking for another condition. But a large hiatal hernia can allow food and acid to back up into your esophagus. This can cause heartburn, chest pain, and difficulty swallowing. Self-care measures or medicines can usually relieve these symptoms. A very large hiatal hernia might need surgery.
- Gastritis. Gastritis is when your stomach lining gets inflamed (red and swollen). Your stomach lining is strong. In most cases, acid does not hurt it. But it can get inflamed and irritated if you drink too much alcohol, have damage from pain relievers called non-steroidal anti-inflammatory drugs (NSAIDs), or smoke. Stomach lining inflammation from many causes can make your lower left chest hurt. You also might feel sick to your stomach and throw up.
- Pancreatitis. Pancreatitis is inflammation of your pancreas, an organ that produces digestive enzymes and hormones such as insulin and glucagon. Pancreatitis can be acute pancreatitis (sudden and severe) or chronic pancreatitis (ongoing). Pancreatitis symptoms may include pain in the upper abdomen that may spread to the back, nausea and vomiting, fever, rapid pulse, and weight loss.
- Gastroesophageal reflux disease (GERD) also called gastro-oesophageal reflux disease (GORD), is a condition that develops when there is a backward flow or reflux of stomach contents (acid from the food and liquid in your stomach) back up into your throat and esophagus causing troublesome symptoms and/or complications 4, 5, 6, 7, 8. Gastroesophageal reflux disease can present as non-erosive reflux disease or erosive esophagitis. It can occur at any age, even in babies. Many times, you or your doctor can determine the triggers for your reflux.
- Esophageal spasm. Esophageal spasm are painful abnormal painful contractions of the muscles in the esophagus (the muscular tube that carries food from your mouth to your stomach). Esophageal spasms do not move food effectively to your stomach. The cause of esophageal spasm is unknown. Very hot or very cold foods may trigger an episode of esophageal spasm in some people.
- Costochondritis also known as chest wall pain syndrome or costosternal syndrome is inflammation of the cartilage that connects your ribs to your breastbone.
- Sprained chest muscle also known as pulled chest muscle, is a minor injury, tear or stretch in a chest muscle that usually heals on its own within a few weeks. A chest muscle sprain can cause pain, swelling, bruising, and muscle spasms.
- Broken rib. Broken rib also called rib fracture is a common injury that occurs when one of the bones in your rib cage breaks or cracks. The most common causes are hard impacts from falls, car accidents or contact sports. Broken rib hurts a lot, especially when you breathe deeply. The sharp edge of a broken bone can harm major blood vessels or lungs and other organs inside your chest. Usually, broken ribs heal on their own in about six weeks. The pain lasts for several weeks. Pain control is important for being able to breathe deeply and avoid lung issues, such as pneumonia.
- Shingles also known as herpes zoster, is a painful rash caused by the varicella-zoster virus (VZV), the virus that gave you chickenpox as a child can become active again later, usually in people older than 50. As shingles, the varicella-zoster virus (VZV) causes a painful rash on your upper body. It usually develops in part of your chest, and typically only on one side. Risk factors for shingles include having had chickenpox in the past, being older, and having a weakened immune system.
- Lung cancer: Lung cancer is cancer that starts when abnormal cells in your lungs grow and multiply out of control. People who smoke have the greatest risk of lung cancer. The risk of lung cancer increases with the length of time and number of cigarettes smoked. Lung cancer is the leading cause of cancer deaths worldwide. Lung cancer typically doesn’t cause symptoms early on. Symptoms of lung cancer usually happen when the disease is advanced. Symptoms include a chronic cough, shortness of breath, and feeling tired or weak.
Lung pain diagnosis
If you experience lung or chest pain that resembles a heart attack chest pain, you should go to the emergency room. On arrival, you’ll receive a complete physical exam that measures all of your vital signs, including blood pressure and heart rate. Then you’ll be screened for heart attack or heart disease. Tests include an electrocardiogram (EKG or ECG) — a noninvasive test that records your heart’s electrical activity — and blood tests. Your heart releases certain proteins when a heart attack occurs that will show up in a blood test. Only when heart factors have been ruled out will you be diagnosed with non-serious chest pain.
Tests your doctor may use to find the cause of your lung pain may include:
- Chest X-ray.
- Computed tomography (CT) scan.
- CT coronary angiogram.
- Echocardiogram (Echo).
- Chest and heart MRI (magnetic resonance imaging).
- Magnetic resonance imaging (MRI) scan of your chest and heart.
- Positron emission tomography (PET) scan.
- Mediastinoscopy.
- Cardiac catheterization.
- Stress test.
- Ultrasound.
Talk with your doctor about the testing you need, why you need it and how to prepare.
Once a cardiologist or your emergency room doctor has ruled out heart causes, you’ll likely be referred to a gastroenterologist (gut specialist) next. They’ll test you for esophagus-based causes, starting with GERD. One way of testing is to send you home with a proton-pump inhibitor (PPI), a highly effective medicine for GERD. If the PPI relieves your symptoms, it can also confirm their cause. Other tests may include a PH study of the esophagus, an esophageal motility test, an upper endoscopy or ultrasound. In addition to physical tests, your healthcare provider will take a medical history and ask about your stress and emotional factors.
Lung pain treatment
Doctors tailor treatment for chest pain or lung pain to the underlying cause. Heart conditions and even some lung problems — need emergency care. Anything that keeps blood and/or oxygen from getting to your organs and tissues can be life-threatening.
You may need medicine for conditions like:
- Heart attack.
- Coronary artery disease.
- Coronary artery dissection.
- Pericarditis.
- Hypertrophic cardiomyopathy.
- Aortic dissection.
- Aortic aneurysm.
- Mitral valve prolapse.
- Hiatal hernia.
- Gallstones.
- Gastritis.
- Pancreatitis.
- Pneumonia.
- Asthma.
- COPD.
- Pulmonary embolism.
- Pulmonary hypertension.
- Pleurisy.
- Shingles.
- Broken ribs.
- Sprained chest muscle.
You may need surgeries or procedures for conditions like:
- Heart attack.
- Coronary artery disease.
- Coronary artery dissection.
- Pericarditis.
- Hypertrophic cardiomyopathy.
- Aortic dissection.
- Aortic aneurysm.
- Mitral valve prolapse.
- Hiatal hernia.
- Pancreatitis.
- Pneumothorax.
- A pulmonary embolism.
- Pleurisy.
- Gallstones.
For lung cancer, treatment could include surgery, radiation and/or chemotherapy.
Air bubbles in chest
Air trapped in your chest or the sensation of bubbling feeling in your chest can occur due to a number of medical and surgical conditions that may include pneumothorax also known as a collapsed lung, which is a condition where air leaks into the pleural space between your lung and chest wall. Pneumothorax (Collapsed Lung) can be caused by medical conditions, injuries or medical procedures. Another cause of air trapped in your chest or the sensation of bubbling feeling in your chest could be pneumomediastinum also known as air in the mediastinum, which is a condition where air leaks into the mediastinum (the space in the middle of your chest, between your lungs and around your heart). Most often, pneumomediastinum occurs when air leaks from any part of your lung or airways into the mediastinum due to injury, illness or surgery. While pneumothorax (collapsed lung) or pneumomediastinum (air in the mediastinum) itself is usually harmless, the underlying causes can be serious and it’s important you seek medical advice to determine the underlying cause. You should also be treated right away. Go to the nearest emergency room or seek medical care immediately if you have difficulty breathing, chest pain and shortness of breath or blue skin, nails or lips. These could be signs of life-threatening illnesses or conditions.
Pneumomediastinum
Spontaneous pneumomediastinum is an uncommon condition presenting in approximately one in 1,000 to one in 40,000 emergency department referrals 21, 22, 23. Young patients with spontaneous pneumomediastinum typically present with a history of asthma or recent inhalation of cocaine, methamphetamine, ecstasy, marijuana or hydrocarbons 24, 25, 26, 27, 28, 29, 30, 31. Other causes include barotrauma in asthmatics and chronic obstructive pulmonary disease (COPD) patients, rapid ascent in scuba divers, valsalva maneuvers, vomiting, infections, blast injuries and iatrogenic injuries from endoscopy or surgery 32, but can also happen with no known cause (idiopathic).
Pneumomediastinum can either be spontaneous or secondary. Spontaneous pneumomediastinum (SPM) isn’t caused by injury or illness, or the cause is unknown (idiopathic). Secondary pneumomediastinum develops because of an injury, illness or surgery. While pneumomediastinum itself is usually harmless, the underlying causes can be serious. Potential life-threatening causes include esophageal rupture (Boerhaave syndrome) and tension pneumothorax, but these are historically evident at presentation 33.
Some people with pneumomediastinum don’t have any symptoms. Pneumomediastinum usually causes chest pain behind the breastbone (nonspecific pleuritic chest pain) with shortness of breath, which may spread to the neck or arms. The pain may be worse when you take a breath or swallow.
Seek immediate medical attention or go to the nearest emergency room immediately if you’re experiencing:
- Chest pain.
- Shortness of breath.
- Severe face or neck swelling.
- Lightheadedness.
Because a subset of patients with pneumomediastinum have serious underlying condition, extensive workups are often necessary. During a physical exam, your doctor may feel small bubbles of air under the skin of your chest, arms, or neck called subcutaneous emphysema. When examined, sometimes the person can look very puffy (swollen) in the face and eyes. This can look worse than it actually is. Hearing a crunching sound in time with your heartbeat (Hamman’s sign) is a sign that you might have air in your mediastinum.
A chest x-ray or CT scan of the chest may be done. This is to confirm that air is in the mediastinum, and to help diagnose a hole in the trachea or esophagus.
A barium swallow may be indicated if Boerhaave syndrome (esophageal rupture following vomiting) is suspected from the history. If the pneumomediastinum has not resolved after 1 week, a CT of the chest is indicated to look for a source of persistent air leak.
There’s no specific treatment for pneumomediastinum. Often, no treatment is needed because your body will gradually absorb the air on its own over a period of one to two weeks without intervention and rarely recur 34. Breathing high concentrations of oxygen may speed this process. If you have an underlying health condition, like an infection or injury to an internal organ, your doctor will treat you for that condition.
Your doctor may admit you to the hospital for 24 hours or longer for observation or treatment. While there, your doctor might treat you with:
- Oxygen therapy. Breathing in additional oxygen can help the air absorb into your body faster.
- Medication. Medication like pain relievers or cough suppressants can ease your symptoms until your body absorbs the extra air.
- Needle aspiration. If you have a lot of air that’s pressing on structures inside of your body, a doctor may remove some of the air with a needle or put a drain in. This is rare.
- Your doctor may put in a chest tube if you also have a collapsed lung (pneumothorax). You may also need treatment for the cause of the pneumomediastinum. A hole in the trachea or esophagus needs to be repaired with surgery.
Your outlook (prognosis) depends on the disease or events that caused the pneumomediastinum. People with spontaneous pneumomediastinum can make a full recovery and rarely have it happen again. People with spontaneous pneumomediastinum spend an average of three days in the hospital, but are sometimes there for a week or more. People with underlying causes of pneumomediastinum can be hospitalized for several weeks. If you have secondary pneumomediastinum, recovery will depend on the severity of your underlying condition. Some conditions that cause pneumomediastinum can be fatal.
Figure 10. Pneumomediastinum
Footnotes: A 16 year old boy without asthma or smoking history presented with the sudden onset of behind the sternum chest pain for two days after performing a 4 hour push-up exercise. Chest X-ray shows gross subcutaneous emphysema over the neck and pneumomediastinum with a continuous diaphragm sign (black arrows). The gas outlining the mediastinum, aorta (red arrowheads), and heart (yellow arrowheads) extends into the neck.
[Source 19 ]Is pneumomediastinum an emergency?
Spontaneous pneumomediastinum is not an emergency. But if you have air in your mediastinum due to an injury or illness, you should be treated right away. Go to the nearest emergency room or seek medical care immediately if you have chest pain and shortness of breath. These could be signs of life-threatening illnesses or conditions.
Can pneumomediastinum be fatal?
Pneumomediastinum isn’t fatal on its own. But sometimes, serious, life-threatening health conditions can cause it. Your doctor will look for causes of the air leak and treat them if necessary.
Can pneumomediastinum be prevented?
Pneumomediastinum is rare and scientists don’t understand all the causes or risk factors. There aren’t any recommended ways to prevent it. Not smoking and not using inhaled recreational drugs might lower your risk.
What is the difference between pneumomediastinum and pneumothorax?
How do you recover from pneumomediastinum?
People with spontaneous pneumomediastinum spend an average of three days in the hospital, but are sometimes there for a week or more. People with underlying causes of pneumomediastinum can be hospitalized for several weeks.
Can pneumomediastinum be cured?
Spontaneous pneumomediastinum usually goes away on its own without treatment. If it wasn’t caused by an underlying health condition, it shouldn’t come back. The health conditions that cause it can sometimes be cured.
Pneumomediastinum causes
Pneumomediastinum is usually caused by air moving into your mediastinum from an injury or disease to an internal organ or structure. This includes your airways (trachea or bronchi), air sacs in your lungs (alveoli), tube from your throat to your stomach (esophagus) or intestines. Anything that increases pressure in your chest can cause spontaneous pneumomediastinum, though this is rare. Sometimes, doctors can’t find the cause (idiopathic).
Increased pressure in the lungs or airways may be caused by:
- Too much coughing
- Repeated bearing down to increase abdominal pressure (such as pushing during childbirth, a bowel movement or weight lifting)
- Sneezing
- Vomiting
- Idiopathic
Pneumomediastinum may also happen after:
- An infection in the neck or center of the chest (bacterial, fungal or viral infection)
- Severe injury (trauma) to your chest
- Rapid rises in altitude, or scuba diving
- Tearing of the esophagus (the tube that connects the mouth and stomach)
- Tearing of the trachea (windpipe)
- Rupture of the small sacs of your lungs (alveoli)
- Use of a breathing machine (positive pressure ventilation)
- Use of inhaled recreational drugs, such as marijuana or crack cocaine
- Surgery such as tooth extraction or digestive tract surgery
- Extensive voice exercise
- Excessive blowing
- Lung diseases such as asthma, bronchitis and pneumonia
- Valsalva maneuver (a procedure that involves forcefully exhaling against a closed airway that is used to quickly return an abnormal heart rhythm called paroxysmal supraventricular tachycardia (PSVT) to normal) 35
Pneumomediastinum also can occur with collapsed lung (pneumothorax) or other diseases.
Although it is rare, pneumomediastinum can occur spontaneously. This is considered benign and generally affects young adult males 36.
Risk factors for pneumomediastinum
You might be at higher risk for pneumomediastinum if you:
- Smoke.
- Have asthma, COPD or other lung conditions.
- Use inhaled recreational drugs.
- Recently had surgery on your abdomen, neck or chest.
- Recently gave birth.
Pneumomediastinum symptoms
Some people with pneumomediastinum don’t have any symptoms. Symptoms of pneumomediastinum include 37, 38, 39:
- Severe pain in the middle of your chest or breastbone. It may radiate to your arms or neck. The pain may be worse with breathing or swallowing.
- Shortness of breath.
- Air pockets under your skin on your face, neck or chest (subcutaneous emphysema).
- Neck or face swelling.
- High-pitched voice or other voice distortion.
- Throat pain.
- Neck pain.
- Painful swallowing (odynophagia).
- Difficulty swallowing (dysphagia).
Pneumomediastinum complications
Some rare complications of pneumomediastinum are life-threatening and need to be treated right away. They include:
- Air may build up and enter the space around your lungs (pleural space), causing your lung to collapse (pneumothorax).
- In rare cases, air may enter the area between your heart and the thin sac that surrounds the heart (pericardium). This condition is called a pneumopericardium.
- In other rare cases, so much air builds up in the middle of your chest that it pushes on your heart and the great blood vessels, so they cannot work properly.
All of these complications require urgent attention because they can be life threatening.
Pneumomediastinum diagnosis
During a physical examination, your doctor may feel small bubbles of air under the skin of your chest, arms, or neck called subcutaneous emphysema. Hearing a crunching sound in time with your heartbeat (Hamman’s sign) is a sign that you might have air in your mediastinum.
A chest X-ray or CT scan of your chest may be done. These are tests that take pictures of the inside of your chest. This is to confirm that air is in the mediastinum, and to help diagnose a hole in the trachea or esophagus.
A barium swallow may be indicated if Boerhaave syndrome (esophageal rupture following vomiting) is suspected from the history. If the pneumomediastinum has not resolved after 1 week, a CT of the chest is indicated to look for a source of persistent air leak.
Pneumomediastinum treatment
There’s no specific treatment for pneumomediastinum. Often, no treatment is needed because your body will gradually absorb the air on its own over a period of one to two weeks without intervention and rarely recur 34. Breathing high concentrations of oxygen may speed this process. If you have an underlying health condition, like an infection or injury to an internal organ, your doctor will treat you for that condition.
Your doctor may admit you to the hospital for 24 hours or longer for observation or treatment. While there, your doctor might treat you with:
- Oxygen therapy. Breathing in additional oxygen can help the air absorb into your body faster.
- Medication. Medication like pain relievers or cough suppressants can ease your symptoms until your body absorbs the extra air.
- Needle aspiration. If you have a lot of air that’s pressing on structures inside of your body, a doctor may remove some of the air with a needle or put a drain in. This is rare.
- Your doctor may put in a chest tube if you also have a collapsed lung (pneumothorax). You may also need treatment for the cause of the pneumomediastinum. A hole in the trachea or esophagus needs to be repaired with surgery.
Pneumomediastinum prognosis
Your outlook (prognosis) depends on the disease or events that caused the pneumomediastinum. People with spontaneous pneumomediastinum can make a full recovery and rarely have it happen again. If you have secondary pneumomediastinum, recovery will depend on the severity of your underlying condition. Some conditions that cause pneumomediastinum can be fatal.
The mortality rate associated with pneumomediastinum may be as high as 50-70% as seen in Boerhaave syndrome (esophageal rupture following vomiting) 40. The development of air leak, according to Weg et al 41, is not associated with an increased mortality rate in patients with sepsis-induced acute respiratory distress syndrome (ARDS). Other predisposing conditions associated with high mortality rates include trauma (blunt and penetrating, especially high velocity injury), asthma, and tracheobronchial perforation.
The most common morbidities attributable to pneumomediastinum are symptoms such as chest pain, voice change, and cough. Rarely, tension pneumomediastinum may result in decreased cardiac output. Laryngeal compression leading to stridor has been reported. Gas embolism has rarely been reported.
Heart failure
Heart failure also known as congestive heart failure (CHF) is a heart condition that develops when your heart muscle has become too weak to pump blood and oxygen effectively through your body to support the muscles and organs in your body. Heart failure can also happen if your heart becomes too stiff to fill up with blood properly, so not enough blood and oxygen is pumped around your body. As a result, your muscles and organs don’t get enough oxygen and nutrients. This may cause fluid to build up in your body, legs and make you feel breathless or tired. The term “heart failure” does not mean that your heart has stopped. However, heart failure is a serious condition that needs medical care.
Other names for Heart Failure
- Congestive heart failure.
- Left-side heart failure. This is when the heart can’t pump enough oxygen-rich blood to the body.
- Right-side heart failure. This is when the heart can’t fill with enough blood.
- Cor pulmonale. This term refers to right-side heart failure caused by high blood pressure in the pulmonary arteries and right ventricle (lower right heart chamber).
In 2024, more than 6.7 million adults 20 years old or older in the United States have heart failure, according to the American Heart Association 42.
Heart failure can develop suddenly (the acute kind) or over time as your heart gets weaker (the chronic kind). Heart failure is usually an ongoing (chronic) condition — unlike heart attacks, which occur suddenly and require immediate treatment (acute). However, both conditions can be related: a heart attack can cause ongoing muscle weakness and stiffness making your heart not able to fill up with enough blood that leads to long-term heart failure. In some cases, symptoms of heart failure can also start suddenly.
Heart failure can affect one or both sides of your heart. Left-sided and right-sided heart failure may have different causes. Most often, heart failure is caused by another medical condition that damages your heart. This includes coronary heart disease, heart inflammation, high blood pressure, cardiomyopathy, or an irregular heartbeat. Heart failure may not cause symptoms right away. But eventually, you may feel tired and short of breath and notice fluid buildup in your lower body, around your stomach, or your neck.
Your body depends on the heart’s pumping action to deliver oxygen- and nutrient-rich blood to the body’s cells. When the cells are nourished properly, the body can function normally. Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn’t pump blood as well as it should and the heart can’t pump enough blood to meet the body’s needs 43. With heart failure, the weakened heart can’t supply the cells with enough blood. This results in fatigue and shortness of breath and some people have coughing. Everyday activities such as walking, climbing stairs or carrying groceries can become very difficult. This inability may also result in fluid retention, which causes swelling, for example, in the legs, feet, or abdomen.
The term “heart failure” makes it sound like the heart is no longer working at all and there’s nothing that can be done, but that is not the case at all. Heart failure also doesn’t mean that your heart has stopped or is about to stop working.
Congestive heart failure is a type of heart failure which requires seeking timely medical attention, although sometimes heart failure and congestive heart failure, the two terms are used interchangeably.
As blood flow out of the heart slows, blood returning to the heart through the veins backs up, causing congestion in the body’s tissues. Often swelling (edema) results. Most often there’s swelling in the legs and ankles, but it can happen in other parts of the body, too.
Sometimes fluid collects in the lungs and interferes with breathing, causing shortness of breath, especially when a person is lying down. This is called pulmonary edema and if left untreated can cause respiratory distress.
Heart failure also affects the kidneys’ ability to dispose of sodium and water. This retained water also increases swelling in the body’s tissues (edema).
Congestive heart failure is a serious medical condition in which the heart cannot pump enough blood to meet the body’s needs. As blood flow out of the heart slows, blood returning to the heart through the veins backs up, causing congestion in the body’s tissues. Often swelling (edema) results. Most often there’s swelling in the legs and ankles, but it can happen in other parts of the body, too 44.
Sometimes fluid collects in the lungs and interferes with breathing, causing shortness of breath, especially when a person is lying down. This is called pulmonary edema and if left untreated can cause respiratory distress 44.
Heart failure also affects the kidneys’ ability to dispose of sodium and water. This retained water also increases swelling in the body’s tissues (edema) 44.
Congestive heart failure is often caused by hypertension, diabetes, or coronary heart disease, gradually leave your heart too weak or stiff to fill and pump efficiently.
It is estimated that 6.7 million adults in the United States have congestive heart failure 43 and at least 10 million in Europe 45. Congestive heart failure is one of the most common reasons those aged 65 and over are hospitalized 46.
- There were 1 million hospitalizations for congestive heart failure in 2000 and in 2010.
- About half of people who develop heart failure die within 5 years of diagnosis 47.
- Most congestive heart failure hospitalizations were for those aged 65 and over, but the proportion under age 65 increased significantly from 23% in 2000 to 29% in 2010.
- The overall rate of congestive heart failure hospitalization per 10,000 population did not change significantly from 2000 to 2010 (35.5 compared with 32.8), but the trends were different for those under and over age 65.
- From 2000 to 2010, the rate of congestive heart failure hospitalization for males under age 65 increased significantly while the rate for females aged 65 and over decreased significantly.
- In both 2000 and in 2010, a greater share of inpatients under age 65, compared with those aged 65 and over, were discharged to their homes.
Heart failure can damage your liver or kidneys. Other conditions it can lead to include pulmonary hypertension or other heart conditions, such as an irregular heartbeat, heart valve disease, and sudden cardiac arrest. One way to prevent heart failure is to control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
Some common symptoms of heart failure include:
- Chest pain (angina).
- Dizziness.
- Fatigue.
- Shortness of breath (dyspnea).
- Swollen hands or feet (edema).
Your doctor will diagnose heart failure based on your medical and family history, a physical exam, and results from imaging and blood tests.
Currently, heart failure is a serious condition and not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing salt in your diet, managing stress and losing weight — can improve your quality of life.
Heart failure therapies treat the underlying cause of low ejection fraction. In some cases of heart failure, the heart can’t fill with enough blood. In other cases, the heart can’t pump blood to the rest of the body with enough force. Some people have both problems. For heart failure due to an arrhythmia, you may benefit from a biventricular pacemaker. People with heart failure due to other causes, like high blood pressure, may need medications.
Heart failure treatments include:
- Biventricular pacemaker.
- Heart failure medications.
- Heart transplant.
- Heart valve repair or replacement.
- Implantable cardioverter defibrillator (ICD).
You can take additional steps to relieve strain on your heart and get the most out of treatment. Many people with mild heart failure enhance their quality of life by doing these:
- Increasing physical activity. A cardiac rehabilitation program can help you safely get started. Talk to your doctor before starting a new exercise routine if you haven’t been physically active.
- Maintaining a healthy weight.
- Limiting the amount of sodium and volume of fluids you consume.
- Quitting unhealthy habits, such as smoking, recreational drugs and alcohol. Limit caffeine.
- Track your daily fluid intake. You may need a diuretic medication to help get rid of extra fluid in your body.
- Eat a heart-healthy diet. A dietitian or nutritionist can help you build a healthy, filling meal plan.
- Manage stress, either through yoga, meditation or other stress management techniques.
- Get plenty of sleep at night.
Figure 11. Congestive Heart Failure
Figure 12. Congestive heart failure signs and symptoms
[Source 48 ]See your doctor if you think you might have symptoms of heart failure. Call your local emergency services number and get emergency medical help if you have any of the following:
- Chest pain.
- Fainting or severe weakness.
- Rapid or irregular heartbeat with shortness of breath, chest pain or fainting.
- Sudden, severe shortness of breath and coughing up white or pink, foamy mucus.
These symptoms may be due to heart failure. But there are many other possible causes. Don’t try to diagnose yourself.
At the emergency room, doctors do tests to learn if your symptoms are due to heart failure or something else.
See your doctor right away if you have heart failure and:
- Your symptoms suddenly get worse.
- You develop a new symptom.
- You gain 5 pounds (2.3 kilograms) or more within a few days.
Such changes could mean that existing heart failure is getting worse or that treatment isn’t working.
What is ejection fraction?
Ejection fraction (EF) is a measurement of your heart’s ability to pump oxygen-rich blood out to your body, expressed as a percentage (%), of how much oxygen-rich blood the left ventricle (LV) pumps out with each heart contraction 49. Ejection fraction (EF) refers to how well your heart pumps blood. Ejection fraction (EF) is the amount of blood pumped out of your heart’s lower chambers (ventricles) each time it contracts. An ejection fraction (EF) of 60 percent means that 60 percent of the total amount of blood in the left ventricle (LV) is pushed out with each heartbeat. A normal heart’s ejection fraction (normal EF) is between 50 and 70 percent 49. With each heartbeat, 50% to 70% of the blood in your left ventricle gets pumped out to your body. However, it is important to note that you can have a normal ejection fraction measurement and still have heart failure. This is called heart failure with preserved ejection fraction (HFpEF) previously known as diastolic heart failure. Heart failure with preserved ejection fraction (HFpEF) happens when your heart’s muscle has become so thick and stiff that the ventricle holds a smaller than usual volume of blood. In this case, your heart might still have an ejection fraction that falls in the normal range (EF≥50%) because your heart is pumping out a normal percentage of the blood that enters it. But in heart failure with preserved ejection fraction (HFpEF), the total amount of blood pumped isn’t enough to meet your body’s needs.
To understand ejection fraction (EF), it’s helpful to understand how blood flows through your heart:
- Blood enters your heart through the top right section (right atrium).
- Between heartbeats, there’s a short pause (diastole, the phase of the heartbeat when your heart muscle relaxes and allows heart chambers to fill with blood). This is when blood flows through a valve down to the left ventricle.
- Once the ventricle is full, the next heartbeat pumps out (ejects) a portion of the blood out to the body. Also called systole, the phase of the heartbeat when your heart muscle contracts and pumps blood from the heart chambers into the arteries.
Table 1. Ejection Fraction Percentage
| Sex | Normal | Mildly Abnormal | Moderately Abnormal | Severely Abnormal |
|---|---|---|---|---|
| Male | 52% to 72% | 41% to 51% | 30% to 40% | Below 30% |
| Female | 54% to 74% | 41% to 53% | 30% to 40% | Below 30% |
Who is at Risk for Heart Failure?
About 6.7 million adults 20 years old or older in the United States have heart failure 51. The number of people who have heart failure is growing.
Heart failure is more common in:
- People who are age 65 or older. Aging can weaken the heart muscle. Older people also may have had diseases for many years that led to heart failure. Heart failure is a leading cause of hospital stays among people on Medicare. Heart failure is rare in people younger than 50. Studies have shown that around 2% of the population younger than 54 years old have heart failure. The number increases to around 8% — about 1 in 12 — for people over 75.
- Blacks are more likely to have heart failure than people of other races. They’re also more likely to have symptoms at a younger age, have more hospital visits due to heart failure, and die from heart failure.
- People who are overweight. Excess weight puts strain on the heart. Being overweight also increases your risk of heart disease and type 2 diabetes. These diseases can lead to heart failure.
- People who have had a heart attack. Damage to the heart muscle from a heart attack and can weaken the heart muscle.
Children who have congenital heart defects also can develop heart failure. These defects occur if the heart, heart valves, or blood vessels near the heart don’t form correctly while a baby is in the womb. Congenital heart defects can make the heart work harder. This weakens the heart muscle, which can lead to heart failure. Children don’t have the same symptoms of heart failure or get the same treatments as adults.
Heart failure causes
Conditions that damage or overwork your heart muscle can cause heart failure 52. Certain lifestyle factors – smoking, being overweight, eating foods high in fat and cholesterol and physical inactivity – can contribute to heart failure because they increase your risk of developing heart conditions associated with heart failure. Your heart muscle can be damaged by certain infections, heavy alcohol use, recreational drug use and some chemotherapy medicines. Your genes also can play a role. Over time, your heart weakens. It isn’t able to fill with and/or pump blood as well as it should. As the heart weakens, certain proteins and substances might be released into the blood. These substances have a toxic effect on the heart and blood flow, and they worsen heart failure.
Any of the following conditions also can damage or weaken the heart and cause heart failure:
- Coronary heart disease. Coronary artery disease is the most common cause of heart failure. Coronary artery disease results from the buildup of fatty deposits in the arteries. The deposits narrow the arteries. This reduces blood flow and can lead to heart attack.
- Heart attack. A heart attack occurs suddenly when an artery feeding the heart becomes completely blocked. Damage to the heart muscle from a heart attack may mean that the heart can no longer pump as well as it should.
- High blood pressure. Also called hypertension, this condition forces the heart to work harder than it should to pump blood through the body. Over time, the extra work can make the heart muscle too stiff or too weak to properly pump blood.
- Heart valve disease. Heart valves keep blood flowing the right way. If a heart valve isn’t working properly, the heart must work harder to pump blood. This can weaken the heart over time. Treating some types of heart valve disease may reverse heart failure.
- Inflammation of the heart muscle (myocarditis). Myocarditis is most commonly caused by a virus and can lead to left-sided heart failure.
- Congenital heart defect. A heart condition that you’re born with is called a congenital heart defect. If the heart and its chambers or valves haven’t formed correctly, the other parts of the heart have to work harder to pump blood. This may lead to heart failure.
- Irregular heart rhythms (arrhythmias). Irregular heart rhythms may cause the heart to beat too fast, creating extra work for the heart. A slow heartbeat also may lead to heart failure. Treating an irregular heart rhythm may reverse heart failure in some people.
- Other heart conditions or diseases
- Other diseases. Some long-term diseases may contribute to chronic heart failure. Examples are diabetes, HIV infection, an overactive or underactive thyroid, or a buildup of iron or protein.
Causes of sudden heart failure also include:
- Allergic reactions.
- Any illness that affects the whole body.
- Blood clots in the lungs.
- Severe infections.
- Use of certain medicines.
- Viruses that attack the heart muscle.
Coronary Heart Disease
Coronary heart disease is a condition in which a waxy substance called plaque builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart muscle.
Plaque narrows the arteries and reduces blood flow to your heart muscle. The buildup of plaque also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow. Coronary heart disease can lead to chest pain or discomfort called angina, a heart attack, and heart damage.
Diabetes
Diabetes is a disease in which the body’s blood glucose (sugar) level is too high. The body normally breaks down food into glucose and then carries it to cells throughout the body. The cells use a hormone called insulin to turn the glucose into energy.
In diabetes, the body doesn’t make enough insulin or doesn’t use its insulin properly. Over time, high blood sugar levels can damage and weaken the heart muscle and the blood vessels around the heart, leading to heart failure.
High Blood Pressure
Blood pressure is the force of blood pushing against the walls of the arteries. If this pressure rises and stays high over time, it can weaken your heart and lead to plaque buildup.
Blood pressure is considered high if it stays at or above 140/90 mmHg over time. (The mmHg is millimeters of mercury—the units used to measure blood pressure.) If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher.
Other Heart Conditions or Diseases
Other conditions and diseases also can lead to heart failure, such as:
- Arrhythmia. Happens when a problem occurs with the rate or rhythm of the heartbeat.
- Cardiomyopathy. Happens when the heart muscle becomes enlarged, thick, or rigid.
- Congenital heart defects. Problems with the heart’s structure are present at birth.
- Heart valve disease. Occurs if one or more of your heart valves doesn’t work properly, which can be present at birth or caused by infection, other heart conditions, and age.
Other Factors
Other factors also can injure the heart muscle and lead to heart failure. Examples include:
- Alcohol abuse or cocaine and other illegal drug use
- HIV/AIDS
- Thyroid disorders (having either too much or too little thyroid hormone in the body)
- Too much vitamin E
- Treatments for cancer, such as radiation and chemotherapy.
Risk factors for heart failure
Diseases and conditions that increase your risk of heart failure include:
- Coronary artery disease. Narrowed arteries may limit the heart’s supply of oxygen-rich blood, resulting in weakened heart muscle.
- Heart attack. A heart attack is a form of coronary artery disease that occurs suddenly. Damage to the heart muscle from a heart attack may mean the heart can no longer pump as well as it should.
- Heart valve disease. Having a heart valve that doesn’t work properly raises the risk of heart failure.
- High blood pressure. The heart works harder than it has to when blood pressure is high.
- Irregular heartbeats. Irregular heartbeats, especially if they are very frequent and fast, can weaken the heart muscle and cause heart failure.
- Congenital heart disease. Some people who develop heart failure were born with changes in the structure or function of their heart.
- Diabetes. Having diabetes increases the risk of high blood pressure and coronary artery disease.
- Sleep apnea. This inability to breathe properly during sleep results in low blood-oxygen levels and an increased risk of irregular heartbeats. These things can lead to a weakened heart.
- Obesity. People who have obesity have a higher risk of developing heart failure.
- Viral infections. Some viral infections can damage to the heart muscle.
Medicines that may increase the risk of heart failure include:
- Some diabetes medicines. The diabetes medicines rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don’t stop taking these medicines without first talking to your doctor.
- Other medicines that may lead to heart failure or heart conditions include nonsteroidal anti-inflammatory drugs (NSAIDs) and some medicines used to treat high blood pressure, cancer, blood conditions, irregular heartbeats, nervous system diseases, mental health conditions, lung and urinary conditions, and infections.
Other risk factors for heart failure include:
- Aging. The heart’s ability to work decreases with age, even in healthy people.
- Alcohol use. Drinking too much alcohol may weaken the heart muscle and lead to heart failure.
- Smoking or using tobacco. If you smoke, quit. Using tobacco increases the risk of heart disease and heart failure.
Heart failure prevention
The key to preventing heart failure is to reduce your risk factors. You can control or eliminate many of the risk factors for heart disease — high blood pressure and coronary artery disease, for example — by making lifestyle changes along with the help of any needed medications.
Lifestyle changes you can make to help prevent heart failure include:
- Not smoking
- Controlling certain conditions, such as high blood pressure and diabetes
- Staying physically active
- Eating healthy foods
- Maintaining a healthy weight
- Reducing and managing stress.
Heart failure symptoms
If you have heart failure, your heart can’t supply enough blood to meet your body’s needs. Symptoms may develop slowly. Sometimes, heart failure symptoms start suddenly.
The most common signs and symptoms of heart failure are 53:
- Shortness of breath (dyspnea) or trouble breathing when you exert yourself or when you lie down
- Fatigue, tiredness and weakness
- Swelling (edema) in your legs, ankles and feet
- Rapid or irregular heartbeat
- Reduced ability to exercise
- Wheezing.
- A cough that doesn’t go away or a cough that brings up white or pink mucus with spots of blood.
- Increased need to urinate at night
- Swelling of your abdomen (ascites)
- Sudden weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty concentrating or decreased alertness
- Sudden, severe shortness of breath and coughing up pink, foamy mucus
- Chest pain if your heart failure is caused by a heart attack
- Prominent veins in the neck
All of these symptoms are the result of fluid buildup in your body. When symptoms start, you may feel tired and short of breath after routine physical effort, like climbing stairs.
As your heart grows weaker, symptoms get worse. You may begin to feel tired and short of breath after getting dressed or walking across the room. Some people have shortness of breath while lying flat.
Fluid buildup from heart failure also causes weight gain, frequent urination, and a cough that’s worse at night and when you’re lying down. This cough may be a sign of acute pulmonary edema. This is a condition in which too much fluid builds up in your lungs. The condition requires emergency treatment.
Cardiac asthma
Heart failure complications
If you have heart failure, your outlook depends on the cause and the severity, your overall health, and other factors such as your age. Complications can include:
- Kidney damage or failure. Heart failure can reduce the blood flow to your kidneys, which can eventually cause kidney failure if left untreated. Kidney damage from heart failure can require dialysis for treatment.
- Heart valve problems. The valves of your heart, which keep blood flowing in the proper direction through your heart, may not function properly if your heart is enlarged or if the pressure in your heart is very high due to heart failure.
- Heart rhythm problems. Heart rhythm problems (arrhythmias) can be a potential complication of heart failure.
- Sudden cardiac death. If the heart is weak, there is a risk of dying suddenly due to a dangerous irregular heart rhythm.
- Liver damage. Heart failure can lead to a buildup of fluid that puts too much pressure on the liver. This fluid backup can lead to scarring, which makes it more difficult for your liver to function properly.
- Malnutrition.
Some people’s symptoms and heart function will improve with proper treatment. However, heart failure can be life-threatening. People with heart failure may have severe symptoms, and some may require heart transplantation or support with a ventricular assist device.
Heart failure diagnosis
To diagnose heart failure, your doctor will take a careful medical history, review your symptoms and perform a physical examination. Your doctor will also check for the presence of risk factors, such as high blood pressure, coronary artery disease or diabetes.
Using a stethoscope, your doctor can listen to your lungs for signs of congestion. The stethoscope also picks up abnormal heart sounds that may suggest heart failure. The doctor may examine the veins in your neck and check for fluid buildup in your abdomen and legs.
After the physical exam, your doctor may also order some of these tests:
- Blood tests: Your doctor may take a sample of your blood to check your kidney, liver and thyroid function and to look for indicators of other diseases that affect the heart. A BNP blood test to check for a chemical called N-terminal pro-B-type natriuretic peptide (NT-proBNP) may help in diagnosing heart failure if the diagnosis isn’t certain when used in addition to other tests.
- Chest X-ray: Chest X-ray images help your doctor see the condition of your lungs and heart. In heart failure, your heart may appear enlarged and fluid buildup may be visible in your lungs. Your doctor can also use an X-ray to diagnose conditions other than heart failure that may explain your signs and symptoms.
- Electrocardiogram (EKG or ECG): This test records the electrical activity of your heart through electrodes attached to your skin. Impulses are recorded as waves and displayed on a monitor or printed on paper. This test helps your doctor diagnose heart rhythm problems and damage to your heart from a heart attack that may be underlying heart failure.
- Echocardiogram: An important test for diagnosing heart failure is the echocardiogram. An echocardiogram helps distinguish systolic heart failure from diastolic heart failure in which the heart is stiff and can’t fill properly. An echocardiogram uses sound waves to produce a video image of your heart. This test can help doctors see the size and shape of your heart and how well your heart is pumping. The echocardiogram also can help doctors look for valve problems or evidence of previous heart attacks, other heart abnormalities, and some unusual causes of heart failure. Your ejection fraction is measured during an echocardiogram and can also be measured by nuclear medicine tests, cardiac catheterization and cardiac MRI. This is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment.
- Doppler Ultrasound: A Doppler ultrasound uses sound waves to measure the speed and direction of blood flow. This test often is done with echo to give a more complete picture of blood flow to the heart and lungs. Doctors often use Doppler ultrasound to help diagnose right-side heart failure.
- Holter Monitor: A Holter monitor records your heart’s electrical activity for a full 24- or 48-hour period, while you go about your normal daily routine. You wear small patches called electrodes on your chest. Wires connect the patches to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
- Multigated Acquisition Scan (MUGA scan): A MUGA scan measures how your heart muscle contracts and relaxes while you rest or exercise. A MUGA scan uses an injection of a substance called technetium-99m-pertechnetate (Tc-99m) and a specialized camera. As the radionuclide (Tc-99m) travels through your blood, your doctor takes pictures of your heart. A nuclear heart scan can show where the heart muscle is healthy and where it’s damaged. A MUGA scan measures your ejection fraction (EF). EF is how much blood your heart pumps out each time it squeezes (contracts). The tracer you receive is safe for most people. Your body will get rid of it through your kidneys within about 24 hours. There is a risk of radiation exposure, bleeding and allergic reaction. If you’re pregnant or think you might be pregnant, or if you’re a nursing mother, don’t have this test. It could harm your baby.
- PET scan. A positron emission tomography (PET) scan is a type of nuclear heart scan. It shows the level of chemical activity in areas of your heart. This test can help your doctor see whether enough blood is flowing to these areas. A PET scan can show blood flow problems that other tests might not detect.
- Exercise tests or stress tests: Stress tests measure how your heart and blood vessels respond to exertion. You may walk on a treadmill or pedal a stationary bike while attached to an ECG machine. Or you may receive a drug intravenously that stimulates your heart similar to exercise. Sometimes the stress test can be done while wearing a mask that measures the ability of your heart and lungs to take in oxygen and breathe out carbon dioxide. Stress tests help doctors see if you have coronary artery disease. Stress tests also determine how well your body is responding to your heart’s decreased pumping effectiveness and can help guide long-term treatment decisions. If your doctor also wants to see images of your heart while you’re exercising, he or she may order a nuclear stress test or a stress echocardiogram. It’s similar to an exercise stress test, but it also uses imaging techniques to visualize your heart during the test.
- Cardiac computerized tomography (CT) scan. In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest.
- Cardiac magnetic resonance imaging (MRI) also called heart MRI scan. In a cardiac MRI, you lie on a table inside a long tube-like machine that produces a magnetic field. The magnetic field aligns atomic particles in some of your cells. When radio waves are broadcast toward these aligned particles, they produce signals that vary according to the type of tissue they are. The signals create images of your heart.
- Cardiac catheterization (cardiac cath or heart cath): During cardiac catheterization, a long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck and threaded to your heart. This allows your doctor to look inside your coronary (heart) arteries. During this procedure, your doctor can check the pressure and blood flow in your heart chambers, collect blood samples, and use x rays to look at your coronary arteries. Cardiac catheterization is one of the most common heart procedures performed in the U.S. Cardiac cath is usually very safe. Major complications are very rare. Some minor risks include:
- Bruises where the catheter was inserted (puncture site)
- Bleeding at the puncture site
- Reaction to the contrast dye
- Infection
- Side effects, such as nausea or vomiting, from the medications given to help you relax or sleep during the procedure
- Some other risks include:
- Abnormal heart rhythm
- Blood clots
- Damage to a blood vessel or heart from the catheter
- Heart attack
- Side effects from X-rays
- Stroke
- Coronary Angiogram: In this test, a thin, flexible tube (catheter) is inserted into a blood vessel at your groin or in your arm and guided through the aorta into your coronary arteries. A dye injected through the catheter makes the arteries supplying your heart visible on an X-ray. This test helps doctors identify narrowed arteries to your heart (coronary artery disease) that can be a cause of heart failure. The test may include a ventriculogram — a procedure to determine the strength of the heart’s main pumping chamber (left ventricle) and the health of the heart valves.
- Myocardial biopsy: In this test, your doctor inserts a small, flexible biopsy cord into a vein in your neck or groin, and small pieces of the heart muscle are taken. This test may be performed to diagnose certain types of heart muscle diseases that cause heart failure.
- Genetic Testing. A DNA test (genetic testing) is a medical test that can identify mutations in your genes, chromosomes or proteins. Genetic testing looks for changes in your genes, chromosomes and proteins. DNA tests can give you lots of information about the genes that make up who you are. They can confirm if you have or don’t have a specific disease. DNA tests can also identify your risk for developing a certain condition or passing on a genetic disorder.
Results of these tests help doctors determine the cause of your signs and symptoms and develop a program to treat your heart. Your heart doctor may tell you the stage of your heart failure.
There are 2 main ways to determine the stage of heart failure:
New York Heart Association (NYHA) classification
New York Heart Association (NYHA) classification system groups heart failure into four categories by number. You may see Roman numerals used for these category names.
- Class 1 (I) heart failure. There are no heart failure symptoms.
- Class 2 (II) heart failure. Everyday activities can be done without difficulty. But exertion causes shortness of breath or fatigue.
- Class 3 (III) heart failure. It’s difficult to complete everyday activities.
- Class 4 (IV) heart failure. Shortness of breath occurs even at rest. This category includes the most severe heart failure.
American College of Cardiology/American Heart Association classification
American College of Cardiology/American Heart Association classification system uses letters A to D 54. It includes a category for people who are at risk of developing heart failure.
Stage A: At risk for heart failure
- People who are at risk for heart failure but do not yet have symptoms or structural or functional heart disease. Risk factors for people in stage A include hypertension, coronary vascular disease, diabetes, obesity, exposure to cardiotoxic agents, genetic variants for cardiomyopathy and family history of cardiomyopathy
Stage B: Pre-heart failure
- People without current or previous symptoms of heart failure but with either structural heart disease, increased filling pressures in the heart or other risk factors
Stage C: Symptomatic heart failure
- People with current or previous symptoms of heart failure
Stage D: Advanced heart failure
- People with heart failure symptoms that interfere with daily life functions or lead to repeated hospitalizations. Advanced heart failure requires specialized treatments.
Heart failure treatment
Early diagnosis and treatment can help people who have heart failure live longer, more active lives. Treatment of heart failure depends on the cause, the type and severity of the heart failure. Treatment often includes lifestyle changes and medicines. If another health condition is causing the heart to fail, treating it may reverse heart failure.
Heart failure is a chronic disease needing lifelong management. However, with treatment, signs and symptoms of heart failure can improve, and the heart sometimes becomes stronger. Treatment may help you live longer and reduce your chance of dying suddenly.
Doctors sometimes can correct heart failure by treating the underlying cause. Some people with heart failure need surgery to open blocked arteries or to place a device to help the heart work better. For example, repairing a heart valve or controlling a fast heart rhythm may reverse heart failure. But for most people, the treatment of heart failure involves a balance of the right medications and, in some cases, use of devices that help the heart beat and contract properly.
The goals of treatment for all stages of heart failure include:
- Treating the condition’s underlying cause, such as coronary heart disease, high blood pressure, or diabetes
- Reducing symptoms
- Stopping the heart failure from getting worse
- Increasing your lifespan and improving your quality of life
Treatments usually include heart-healthy lifestyle changes, medicines, and ongoing care. If you have severe heart failure, you also may need medical procedures or surgery.
Lifestyle and home remedies
Making lifestyle changes can often help relieve signs and symptoms of heart failure and prevent the disease from worsening. These changes may be among the most important and beneficial you can make. Lifestyle changes your doctor may recommend include:
- Stop smoking. Smoking damages your blood vessels, raises blood pressure, reduces the amount of oxygen in your blood and makes your heart beat faster.
If you smoke, ask your doctor to recommend a program to help you quit. You can’t be considered for a heart transplant if you continue to smoke. Avoid secondhand smoke, too.
- Discuss weight monitoring with your doctor. Discuss with your doctor how often you should weigh yourself. Ask your doctor how much weight gain you should notify him or her about. Weight gain may mean that you’re retaining fluids and need a change in your treatment plan.
- Check your legs, ankles and feet for swelling daily. Check for any changes in swelling in your legs, ankles or feet daily. Check with your doctor if the swelling worsens.
- Eat a healthy diet. Aim to eat a diet that includes fruits and vegetables, whole grains, fat-free or low-fat dairy products, and lean proteins.
- Restrict salt in your diet. Too much sodium contributes to water retention, which makes your heart work harder and causes shortness of breath and swollen legs, ankles and feet.
Check with your doctor for the sodium restriction recommended for you. Keep in mind that salt is already added to prepared foods, and be careful when using salt substitutes.
- Maintain a healthy weight. If you’re overweight, your dietitian will help you work toward your ideal weight. Even losing a small amount of weight can help.
- Consider getting vaccinations. If you have heart failure, you may want to get influenza and pneumonia vaccinations. Ask your doctor about these vaccinations.
- Limit fats and cholesterol. In addition to avoiding high-sodium foods, limit the amount of saturated fat, trans fat and cholesterol in your diet. A diet high in fat and cholesterol is a risk factor for coronary artery disease, which often underlies or contributes to heart failure.
- Limit alcohol and fluids. Your doctor likely will recommend that you don’t drink alcohol if you have heart failure, since it can interact with your medication, weaken your heart muscle and increase your risk of abnormal heart rhythms.
- Getting medical care for other related conditions is important. If you have diabetes or high blood pressure, work with your health care team to control these conditions. Have your blood sugar level and blood pressure checked. Talk with your doctor about when you should have tests and how often to take measurements at home.
If you have severe heart failure, your doctor may also suggest you limit the amount of fluids you drink.
- Be active. Moderate aerobic activity helps keep the rest of your body healthy and conditioned, reducing the demands on your heart muscle. Before you start exercising though, talk to your doctor about an exercise program that’s right for you. Your doctor may suggest a walking program.
Check with your local hospital to see if it offers a cardiac rehabilitation program; if it does, talk to your doctor about enrolling in the program.
- Reduce stress. When you’re anxious or upset, your heart beats faster, you breathe more heavily and your blood pressure often goes up. This can make heart failure worse, since your heart is already having trouble meeting the body’s demands.
Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help keep stress at bay.
- Sleep easy. If you’re having shortness of breath, especially at night, sleep with your head propped up using a pillow or a wedge. If you snore or have had other sleep problems, make sure you get tested for sleep apnea.
To improve your sleep at night, prop up your head with pillows. Also, discuss with your doctor changing the time for taking medications, especially diuretics. Taking diuretics earlier in the day may decrease the need to urinate as often during the night.
Medications
Doctors usually treat heart failure with a combination of medications. Depending on your symptoms, you might take one or more medications, including:
- Angiotensin-converting enzyme (ACE) inhibitors. These medicines relax blood vessels to lower blood pressure, improve blood flow and decrease the strain on the heart. Examples include enalapril (Vasotec, Epaned), lisinopril (Zestril, Qbrelis) and captopril.
- Angiotensin 2 receptor blockers (ARBs). These medicines have many of the same benefits as ACE inhibitors. They may be an option for people who can’t tolerate ACE inhibitors. They include losartan (Cozaar), valsartan (Diovan) and candesartan (Atacand).
- Angiotensin receptor plus neprilysin inhibitors (ARNIs). This medicine uses two blood pressure medicines to treat heart failure. The combination medicine is sacubitril-valsartan (Entresto). It’s used to treat some people with heart failure with reduced ejection fraction. It may help prevent the need for a hospital stay in those people.
- Beta blockers. These medicines slow the heart rate and lower blood pressure. They reduce the symptoms of heart failure and help the heart work better. If you have heart failure, beta blockers may help you live longer. Examples include carvedilol (Coreg), metoprolol (Lopressor, Toprol-XL, Kapspargo Sprinkle) and bisoprolol.
- Ivabradine (Corlanor): This medication is known as an If channel blocker. This drug slows the heart rate differently from beta-blockers, without lowering blood pressure.
- Diuretics or water pills, these medicines make you urinate more frequently. This helps prevent fluid buildup in your body. Diuretics, such as furosemide (Lasix, Furoscix), also decrease fluid in the lungs, so it’s easier to breathe. Some diuretics make the body lose potassium and magnesium. Your doctor may recommend supplements to treat this. If you’re taking a diuretic, you may have regular blood tests to check your potassium and magnesium levels.
- Potassium-sparing diuretics also called aldosterone antagonists, these medicines include spironolactone (Aldactone, CaroSpir) and eplerenone (Inspra). They may help people with severe heart failure with reduced ejection fraction (HFrEF) live longer. Unlike some other diuretics, these medicines can raise the level of potassium in the blood to dangerous levels. Talk with your doctor about your diet and potassium intake.
- Sodium-glucose cotransporter-2 (SGLT2) inhibitors. These medicines help lower blood sugar. They are often prescribed with diet and exercise to treat type 2 diabetes. But they’re also one of the first treatments for heart failure. That’s because several studies showed that the medicine lowered the risk of hospital stays and death in people with certain types of heart failure — even if they didn’t have diabetes. Sodium-glucose cotransporter-2 (SGLT2) inhibitors include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance).
- Digoxin (Lanoxin) also called digitalis, helps the heart squeeze better to pump blood. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in people with heart failure with reduced ejection fraction (HFrEF). It may be more likely to be given to someone with a heart rhythm disorder, such as atrial fibrillation. The level of digoxin in the body must be checked using a blood test. If too much digoxin builds up in your blood, side effects may occur, including loss of appetite, nausea, vomiting and headaches. The heart rhythm can also become too fast or too slow. Always report any side effects of Digoxin to your doctor right away.
- Hydralazine and isosorbide dinitrate (BiDil). This combination of medicines helps relax blood vessels. It may be added to your treatment plan if you have severe heart failure symptoms and ACE inhibitors or beta blockers haven’t helped.
- Vericiguat (Verquvo). This medicine for chronic heart failure is taken once a day by mouth. This medication is known as a soluble guanylate cyclase (SGc) inhibitor. It works by increasing the amount of nitric oxide, which is a natural chemical in the body that helps to widen blood vessels. This helps reduce the workload on the heart. In studies, people with high-risk heart failure who took this medicine had fewer hospital stays for heart failure and heart disease-related deaths compared with those who got a dummy pill.
- Positive inotropes. These medicines may be given by IV to people with certain types of severe heart failure who are in the hospital. Positive inotropes can help the heart pump blood better and maintain blood pressure. Long-term use of these medicines has been linked to an increased risk of death in some people. Talk with your doctor about the benefits and risks of these medicines.
You may need to take two or more medications to treat heart failure. Your doctor may prescribe other heart medications as well — such as nitrates for chest pain, a statin to lower cholesterol or blood-thinning medications to help prevent blood clots — along with heart failure medications.
Your doctor may need to change your medicine doses frequently. This is more common when you’ve just started a new medicine or when your condition is getting worse.
You may be hospitalized if you have a flare-up of heart failure symptoms. While in the hospital, you may receive additional medications to help your heart pump better and relieve your symptoms. You may also receive supplemental oxygen through a mask or small tubes placed in your nose. If you have severe heart failure, you may need to use supplemental oxygen long term.
Your doctor may also prescribe other medications for additional health conditions that may occur with heart failure. These include:
- Potassium and magnesium supplements: Diuretics can remove potassium and magnesium from the body. Your doctor may prescribe potassium and/or magnesium supplements to ensure these levels remain normal while you are being treated.
- Anticoagulants also known as blood thinners: Anticoagulants are used in heart failure patients with atrial fibrillation, an artificial heart valve, blood clots or in people at high risk for blood clots. They help prevent blood clots from forming and blocking blood flow. Clots may form in the legs, lungs or heart. If a clot breaks off and gets stuck inside a blood vessel that supplies the brain, a stroke can result.
- Cholesterol-lowering drugs (statins): Your doctor may prescribe this class of medication if you have high cholesterol or have had a heart attack. They are not used to treat heart failure but other conditions as indicated. These medications help prevent the formation of plaque, which helps reduce the risk of heart attack and stroke.
- Oxygen therapy delivers concentrated oxygen to the lungs. This helps increase the amount of oxygen that can get into the blood. Oxygen therapy can improve shortness of breath and increase a person’s ability to be physically active.
- Some people may receive nitrates for chest pain.
Surgery and medical devices
In some cases, doctors recommend surgery to treat the underlying problem that led to heart failure. Some treatments being studied and used in certain people include:
- Coronary artery bypass graft surgery (CABG). If severely blocked coronary arteries are contributing to your heart failure, your doctor may recommend coronary artery bypass surgery. In this procedure, blood vessels from your leg, arm or chest bypass a blocked artery in your heart to allow blood to flow through your heart more freely.
- Heart valve repair or replacement. If a damaged heart valve causes your heart failure, your doctor may recommend repairing or replacing the heart valve. The surgeon can modify the original valve (valvuloplasty) to eliminate backward blood flow. Surgeons can also repair the valve by reconnecting valve leaflets or by removing excess valve tissue so that the leaflets can close tightly. Sometimes repairing the heart valve includes tightening or replacing the ring around the valve (annuloplasty). The type of heart valve surgery you need depends on the cause of your heart valve disease. Valve replacement is done when valve repair isn’t possible. In valve replacement surgery, the damaged valve is replaced by an artificial (prosthetic) valve. Certain types of heart valve repair or replacement can now be done without open heart surgery, using either minimally invasive surgery or cardiac catheterization techniques.
- Implantable cardioverter-defibrillator (ICD). An implantable cardioverter-defibrillator (ICD) is a device similar to a pacemaker. It’s implanted under the skin in your chest with wires leading through your veins and into your heart. The implantable cardioverter-defibrillator (ICD) monitors the heart rhythm. If the heart starts beating at a dangerous rhythm, or if your heart stops, the implantable cardioverter-defibrillator tries to pace your heart or shock it back into normal rhythm. An implantable cardioverter-defibrillator (ICD) can also function as a pacemaker and speed your heart up if it is going too slow.
- Cardiac resynchronization therapy (CRT) also called biventricular pacing, cardiac resynchronization therapy (CRT) is a treatment for heart failure in people whose lower heart chambers aren’t pumping in sync with each other. A biventricular pacemaker sends timed electrical impulses to both of the heart’s lower chambers (the left and right ventricles) so that they pump in a more efficient, coordinated manner. The signals tell the chambers to squeeze in a more coordinated way. This improves the pumping of blood out of the heart. Many people with heart failure have problems with their heart’s electrical system that cause their already-weak heart muscle to beat in an uncoordinated fashion. This inefficient muscle contraction may cause heart failure to worsen. Often a cardiac resynchronization therapy (CRT) or biventricular pacemaker is combined with an implantable cardioverter-defibrillator (ICD) for people with heart failure.
- Ventricular assist device (VAD) also called a mechanical circulatory support device. Ventricular assist devices are implanted into your abdomen or chest and attached to a weakened heart to help it pump blood to the rest of your body. A ventricular assist device (VAD) helps pump blood from the lower chambers of the heart to the rest of the body. Although a ventricular assist device (VAD) can be placed in one or both ventricles of the heart, it’s usually placed in the heart’s left ventricle. Your doctor may recommend a ventricular assist device (VAD) if you’re waiting for a heart transplant. Sometimes, a ventricular assist device (VAD) is used as a permanent treatment for people who have heart failure but who aren’t good candidates for a heart transplant. Doctors first used heart pumps to help keep heart transplant candidates alive while they waited for a donor heart. Ventricular assist devices are now sometimes used as an alternative to transplantation. Implanted heart pumps can significantly extend and improve the lives of some people with severe heart failure who aren’t eligible for or able to undergo heart transplantation or are waiting for a new heart. Major complications associated with left ventricular assist devices include bleeding, infection, and device malfunction. Temporary right ventricular failure immediately following an left ventricular assist device placement can occur in 30% of patients requiring inotropes or right ventricular assist device 55.
- Heart transplant. Some people have such severe heart failure that surgery or medicines don’t help. These people may need to have their hearts replaced with a healthy donor heart. A heart transplant isn’t the right treatment for everyone. A team of doctors at a transplant center helps determine whether the procedure may be safe and beneficial for you. Usually, patients <50 years of age who are brain dead are potential cardiac donors. Contraindications for heart donation include significant heart dysfunction, congenital heart disease, malignancies (except basal cell and squamous cell carcinomas of skin, primary tumors of the central nervous system with low metastatic potential), or transmissible diseases 55. Heart transplants can dramatically improve the survival and quality of life of some people with severe heart failure. However, candidates for transplantation often have to wait a long time before a suitable donor heart is found. Some transplant candidates improve during this waiting period through drug treatment or device therapy and can be removed from the transplant waiting list. Heart transplantation is the treatment of choice for patients with heart failure refractory to medical therapy. Data from the 2008 report from the registry of the International Society for Heart and Lung Transplant showed that patient survival at 1 and 3 years for patients who received cardiac transplantation was approximately 85% and 79%, respectively 56. Recent advances in medical and device therapies have also improved the survival of heart failure patients comparable to that for post-heart transplant 57. More patients need heart transplantation than there are donor hearts available. Heart transplantation is limited to patients who are most likely to benefit with a significant improvement in symptoms and life expectancy.
- Stem Cells – Experimental Approaches: Early clinical studies in patients with heart failure have shown the feasibility of transfer of distinct stem and progenitor cell populations to the heart, and have demonstrated beneficial effects on cardiac function and/or tissue viability 58. However, due to small study sizes, lack of randomised control groups, poor understanding of the mechanisms of action of transplanted cells, lack of information on procedural issues (that is, optimal cell type, cell dosage, timing of cell transfer, optimal route of application), and safety concerns with some progenitors (such as the arrhythmogenicity associated with skeletal myoblast grafts), further basic research and the initiation of large, double‐blind, placebo‐controlled, randomised clinical trials with hard end‐points (including mortality) are warranted before the role of cell‐based therapy of heart failure can be judged.
Figure 13. An intracorporeal left ventricular assist device and its components
Cardiac rehabilitation
Cardiac rehabilitation is a medically supervised program to help heart patients improve overall physical, mental and social function. The goal is to stabilize, slow or even reverse the progression of heart failure. This can help reduce the risk of heart disease, another cardiac event or death.
Cardiac rehab programs usually provide:
- A medical evaluation to determine your needs and limitations.
- A physical activity program tailored to your needs and limits.
- Counseling and education to help you understand your condition and how to manage it.
- Support and training to help you return to work or your normal activities.
- Counseling on modifying risk factors through nutrition and the use of prescribed medications.
Unfortunately, not everyone is eligible for or covered for cardiac rehab. Many people feel they can’t afford to spend the time and effort needed to complete cardiac rehab. But cardiac rehab programs save lives. There are other benefits too, both physical and emotional.
Patients repeatedly acknowledge that the benefits of cardiac rehab are worth the investment of time and energy. Even if you can’t attend rehab as often as you’d like, going when you can is beneficial.
Heart failure prognosis
Congestive heart failure is a chronic, or lifelong, condition. You’ll need to treat it for the rest of your life. Heart failure is frequently a progressive disease process, and progression is associated with decreased survival, regardless of underlying cause 54, 59. With the right care, congestive heart failure won’t stop you from doing the things you enjoy.
Your prognosis, or outlook for the future, will depend on:
- How well your heart muscle is working.
- Your symptoms.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
One study says that people with congestive heart failure have a life span 10 years shorter than those who don’t have heart failure. Another study showed that the survival rates of people with chronic heart failure were:
- 80% to 90% for one year.
- 50% to 60% for year five.
- 30% for 10 years.
A different study found that people who had heart failure had expected life spans ranging from three to 20 years after their hospital stay, depending on various factors like age and sex. It’s important to look at your specific situation when considering your prognosis.
Lung cancer
Lung cancer is a type of cancer that starts in the windpipe (trachea), the main airway (bronchus) or the lung tissue. Most lung cancer are either small cell lung cancer (SCLC) or non-small cell lung cancer (NSCLC). In general, about 13% of all lung cancers are small cell lung cancer (SCLC) and about 87% are non-small cell lung cancer (NSCLC) 60. Lung cancer is one of the most common cancers in the world. Lung cancer is the second most common cancer (not counting skin cancer) and the leading cause of cancer death in the United States 61. In men, prostate cancer is more common, while in women breast cancer is more common 62. About 14% of all new cancers are lung cancers. The most important risk factor and cause for lung cancer is smoking, which results in approximately 85% of all U.S. lung cancer cases 63. The more cigarettes you smoke per day and the earlier you started smoking, the greater your risk of lung cancer. Although the prevalence of smoking has decreased, approximately 37% of U.S. adults are current or former smokers 63. The incidence of lung cancer increases with age and occurs most commonly in persons aged 55 years or older. Increasing age and cumulative exposure to tobacco smoke are the 2 most common risk factors for lung cancer. High levels of pollution, radiation and asbestos exposure may also increase risk.
Lung cancers typically start in the cells lining the bronchi and parts of the lung such as the bronchioles or alveoli. Lung cancer has a poor prognosis, and nearly 90% of persons with lung cancer die of the disease.
There are 2 main types of lung cancer and they are treated very differently:
- Non small cell lung cancer (NSCLC). Non-small cell lung cancer is an umbrella term for several types of lung cancers. About 80% to 85% of lung cancers are non small cell lung cancer (NSCLC). The main subtypes of non small cell lung cancer are adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. These subtypes, which start from different types of lung cells are grouped together as non small cell lung cancer because their treatment and prognoses (outlook) are often similar.
- Small cell lung cancer (SCLC) also called oat cell cancer. About 10% to 15% of all lung cancers are small cell lung cancer (SCLC). Small cell lung cancer occurs almost exclusively in heavy smokers. Small cell lung cancer tends to grow and spread faster than non small cell lung cancer. About 70% of people with small cell lung cancer will have cancer that has already spread at the time they are diagnosed. Since this cancer grows quickly, it tends to respond well to chemotherapy and radiation therapy. Unfortunately, for most people, the cancer will return at some point.
- Other types of lung tumors. Along with the main types of lung cancer, other tumors can occur in the lungs.
- Lung carcinoid tumors also known as lung carcinoids: Carcinoid tumors of the lung account for fewer than 5% of lung tumors. Most of these grow slowly. Lung carcinoid tumors start in neuroendocrine cells, a special kind of cell found in the lungs. Neuroendocrine cells are also found in other areas of the body, but only cancers that form from neuroendocrine cells in the lungs are called lung carcinoid tumors.
- There are 2 types of lung carcinoid tumors 64:
- Typical carcinoids tend to grow slowly and rarely spread beyond the lungs. About 9 out of 10 lung carcinoids are typical carcinoids. They also do not seem to be linked with smoking.
- Atypical carcinoids grow a little faster and are somewhat more likely to spread to other organs. They have more cells that are dividing and look more like a fast-growing tumor. They are much less common than typical carcinoids and may be found more often in people who smoke.
- There are 2 types of lung carcinoid tumors 64:
- Other types of lung cancer such as adenoid cystic carcinomas, lymphomas, and sarcomas, as well as benign lung tumors such as hamartomas are rare.
- Cancers that spread to the lungs also known as secondary lung cancer: Cancers that start in other organs (such as the breast, pancreas, kidney, or skin) can sometimes spread (metastasize) to the lungs, but these are not lung cancers. For example, cancer that starts in the breast and spreads to the lungs is still breast cancer, not lung cancer. Treatment for metastatic cancer to the lungs is based on where it started (the primary cancer site).
- Lung carcinoid tumors also known as lung carcinoids: Carcinoid tumors of the lung account for fewer than 5% of lung tumors. Most of these grow slowly. Lung carcinoid tumors start in neuroendocrine cells, a special kind of cell found in the lungs. Neuroendocrine cells are also found in other areas of the body, but only cancers that form from neuroendocrine cells in the lungs are called lung carcinoid tumors.
Cancer that starts in the lung is called primary lung cancer. If cancer spreads to your lungs from somewhere else in your body, this is secondary lung cancer.
People who smoke have the greatest risk of lung cancer 65, though lung cancer can also occur in people who have never smoked. The risk of lung cancer increases with the length of time and number of cigarettes you’ve smoked. Smoking is estimated to account for about 90% of all lung cancer cases 66, with a relative risk of lung cancer approximately 20-fold higher in smokers than in nonsmokers 65. If you quit smoking, even after smoking for many years, you can significantly reduce your chances of developing lung cancer.
Estimated new cases and deaths from lung cancer (non–small cell lung cancer and small cell lung cancer combined) in the United States in 2025 66, 66, 60:
- New cases: About 226,650 new cases of lung cancer (110,680 in men and 115,970 in women). The number of new lung cancer cases continues to decrease, partly because people are quitting smoking.
- Deaths: About 124,730 deaths from lung cancer (64,190 in men and 60,540 in women). Death rates for lung cancer are higher among the middle-aged and older populations. Lung and bronchus cancer is the first leading cause of cancer death in the United States. The death rate was 32.4 per 100,000 men and women per year based on 2018–2022 deaths, age-adjusted.
- 5-Year Relative Survival: 26.7%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
- Percentage of All Cancer Deaths: 20.4%. Lung cancer is by far the leading cause of cancer death, making up almost 20.4% of all cancer deaths. Each year, more people die of lung cancer than of colon, breast, and prostate cancers combined.
- The percent of lung and bronchus cancer deaths is highest among people aged 65–74. With the Median Age At Death 72 years of age.
- Rate of New Lung Cancer Cases and Deaths per 100,000: The rate of new cases of lung and bronchus cancer was 49 per 100,000 men and women per year. The death rate was 32.4 per 100,000 men and women per year. These rates are age-adjusted and based on 2017–2021 cases and 2018–2022 deaths.
- Lifetime Risk of Developing Lung Cancer: Approximately 5.7 percent of men and women will be diagnosed with lung and bronchus cancer at some point during their lifetime, based on 2018–2021 data.
- Prevalence of Lung Cancer: In 2021, there were an estimated 610,816 people living with lung and bronchus cancer in the United States.
Lung cancer mainly occurs in older people. About 2 out of 3 people diagnosed with lung cancer are 65 or older, while less than 2% are younger than 45. The average age at the time of diagnosis is about 70 62.
The 5-year relative survival rate from 2014 to 2020 for patients with lung cancer was 26.7% 66. The 5-year relative survival rate for patients with local-stage (63.7%), regional-stage (35.9%), and distant-stage (8.9%) disease varies markedly, depending on the stage at diagnosis 66. However, early-stage non–small cell lung cancer (NSCLC) has a better prognosis and can be treated with surgical resection.
The type of lung cancer you have tells you the type of cell that the cancer started in. Knowing this helps your doctor decide which treatment you need.
Lung cancer typically doesn’t cause signs and symptoms in its earliest stages. Signs and symptoms of lung cancer typically occur when the disease is advanced. Common symptoms of lung cancer may include 67:
- A cough that doesn’t go away and gets worse over time
- Constant chest pain
- Coughing up blood, even a small amount
- Shortness of breath or wheezing
- Hoarseness of voice
- Repeated problems with pneumonia or bronchitis
- Frequent chest infections
- Swelling of the neck and face
- Difficulty swallowing
- Loss of appetite
- Weight loss without trying
- Fatigue
- Bone pain
- Headache
- Some people have swollen fingers and nails called finger clubbing. They may also have pain and swelling in their joints. This condition is called hypertrophic pulmonary osteoarthropathy (HPOA).
You should see your doctor right away if you have new symptoms that concern you, especially those listed above. This is particularly important if you have risk factors for lung cancer such as a history of lung disease, a family history of lung cancer or you are a smoker.
Doctors diagnose lung cancer using a physical exam, imaging, and lab tests. Treatment depends on the type, stage, and how advanced it is. Treatments include surgery, chemotherapy, radiation therapy, and targeted therapy. Targeted therapy uses substances that attack cancer cells without harming normal cells. Together, you and your medical team can create a cancer treatment plan that contains the goals of your cancer treatment and the steps that these involve.
Treatment for lung cancer usually begins with surgery to remove the cancer. If your lung cancer is very large or has spread to other parts of your body, surgery may not be possible. Treatment might start with medicine and radiation instead. Your medical team considers many factors when creating a treatment plan. These factors may include your overall health, the type and stage of your cancer, and your preferences.
Some people with lung cancer choose not to have treatment. For instance, you may feel that the side effects of treatment will outweigh the potential benefits. When that’s the case, your doctor may suggest comfort care to treat only the symptoms the cancer is causing.
The prognosis of lung cancer depends on how advanced it was at diagnosis (staging), the effectiveness of cancer treatment and your general health. Your doctor can discuss realistic expectations for your own prognosis.
Lung cancer signs and symptoms
Most lung cancers do not cause any symptoms until they have spread, but some people with early lung cancer do have symptoms. If you go to your doctor when you first notice symptoms, your cancer might be diagnosed at an earlier stage, when treatment is more likely to be effective.
Most of these symptoms are more likely to be caused by something other than lung cancer. Still, if you have any of these problems, it’s important to see your doctor right away so the cause can be found and treated, if needed.
The most common symptoms of lung cancer are:
- A cough that does not go away or gets worse
- Coughing up blood or rust-colored sputum (spit or phlegm)
- Chest pain that is often worse with deep breathing, coughing, or laughing
- Hoarseness of voice
- Loss of appetite
- Unexplained weight loss
- Shortness of breath
- Feeling tired or weak
- Infections such as bronchitis and pneumonia that don’t go away or keep coming back
- New onset of wheezing
- Some people have swollen fingers and nails called finger clubbing. They may also have pain and swelling in their joints. This condition is called hypertrophic pulmonary osteoarthropathy (HPOA).
If lung cancer spreads to other parts of the body, it may cause:
- Bone pain (like pain in the back or hips)
- Nervous system changes (such as headache, weakness or numbness of an arm or leg, dizziness, balance problems, or seizures), from cancer spread to the brain
- Yellowing of the skin and eyes (jaundice), from cancer spread to the liver
- Swelling of lymph nodes (collection of immune system cells) such as those in the neck or above the collarbone
Some lung cancers can cause syndromes, which are groups of specific symptoms.
Horner syndrome
Cancers of the upper part of the lungs are sometimes called Pancoast tumors. These tumors are more likely to be non-small cell lung cancer (NSCLC) than small cell lung cancer (SCLC).
Pancoast tumors can affect certain nerves to the eye and part of the face, causing a group of symptoms called Horner syndrome:
- Drooping or weakness of one upper eyelid (ptosis)
- A smaller pupil (dark part in the center of the eye) in the same eye (miosis)
- Little or no sweating on the same side of the face (anhidrosis)
Pancoast tumors can also sometimes cause severe shoulder pain.
Superior vena cava syndrome
The superior vena cava (SVC) is a large vein that carries blood from the head and arms down to the heart. It passes next to the upper part of the right lung and the lymph nodes inside the chest. Tumors in this area can press on the superior vena cava, which can cause the blood to back up in the veins. This can lead to swelling in the face, neck, arms, and upper chest (sometimes with a bluish-red skin color). It can also cause headaches, dizziness, and a change in consciousness if it affects the brain. While superior vena cava syndrome can develop gradually over time, in some cases it can become life-threatening, and needs to be treated right away.
Paraneoplastic syndromes
Some lung cancers make hormone-like substances that enter the bloodstream and cause problems with distant tissues and organs, even though the cancer has not spread to those places. These problems are called paraneoplastic syndromes. Sometimes paraneoplastic syndromes may be the first symptoms of lung cancer. Because the symptoms affect other organs, a disease other than lung cancer may first be suspected as causing them.
Paraneoplastic syndromes can happen with any lung cancer but are more often associated with small cell lung cancer (SCLC). Some common syndromes include:
- SIADH (syndrome of inappropriate anti-diuretic hormone): In this condition, the cancer cells make ADH (anti-diuretic hormone), a hormone that causes the kidneys to hold water. This lowers salt levels in the blood. Symptoms of syndrome of inappropriate anti-diuretic hormone (SIADH) can include fatigue, loss of appetite, muscle weakness or cramps, nausea, vomiting, restlessness, and confusion. Without treatment, severe cases may lead to seizures and coma.
- Cushing syndrome: In this condition, the cancer cells make ACTH, a hormone that causes the adrenal glands to make cortisol. This can lead to symptoms such as weight gain, easy bruising, weakness, drowsiness, and fluid retention. Cushing syndrome can also cause high blood pressure, high blood sugar levels, or even diabetes.
- Nervous system problems: Small cell lung cancer (SCLC) can sometimes cause the body’s immune system to attack parts of the nervous system, which can lead to problems. One example is a muscle disorder called Lambert-Eaton syndrome. In this syndrome, muscles around the hips become weak. One of the first signs may be trouble getting up from a sitting position. Later, muscles around the shoulder may become weak. A less common problem is paraneoplastic cerebellar degeneration, which can cause loss of balance and unsteadiness in arm and leg movement, as well as trouble speaking or swallowing. Small cell lung cancer can also cause other nervous system problems, such as muscle weakness, sensation changes, vision problems, or even changes in behavior.
- High levels of calcium in the blood (hypercalcemia), which can cause frequent urination, thirst, constipation, nausea, vomiting, belly pain, weakness, fatigue, dizziness, and confusion
- Blood clots
Again, many of these symptoms are more likely to be caused by something other than lung cancer. Still, if you have any of these problems, it’s important to see your doctor right away so the cause can be found and treated, if needed.
Lung cancer complications
Some people with lung cancer will develop symptoms, such as shortness of breath, a cough and/or chest pain, because of how the cancer affects the lung’s function. As it advances, lung cancer may cause other complications. These can include fluid build-up in the space around your lung (pleural effusion). Lung cancer can also affect your appetite and you may lose weight. You may feel very fatigued and/or have difficulty sleeping.
You may also experience these symptoms and others as side effects of lung-cancer treatments.
Your medical team has a lot of experience in treating symptoms and complications of lung cancer and can give you advice and support to manage them.
Even if you are receiving cancer treatment, there is still a chance that your cancer can spread to another part of your body (metastasis). If this happens, you and your medical team may adjust your cancer treatment plan.
Lung cancer can cause complications, such as:
- Shortness of breath. People with lung cancer can experience shortness of breath if cancer grows to block the major airways. Lung cancer can also cause fluid to accumulate around the lungs, making it harder for the affected lung to expand fully when you inhale.
- Coughing up blood. Lung cancer can cause bleeding in the airway, which can cause you to cough up blood (hemoptysis). Sometimes bleeding can become severe. Treatments are available to control bleeding.
- Pain. Advanced lung cancer that spreads to the lining of a lung or to another area of the body, such as a bone, can cause pain. Tell your doctor if you experience pain, as many treatments are available to control pain.
- Fluid in the chest (pleural effusion). Lung cancer can cause fluid to accumulate in the space that surrounds the affected lung in the chest cavity (pleural space). Fluid accumulating in the chest can cause shortness of breath. Treatments are available to drain the fluid from your chest and reduce the risk that pleural effusion will occur again.
- Cancer that spreads to other parts of the body (metastasis). Lung cancer often spreads (metastasizes) to other parts of the body, such as the brain and the bones. Cancer that spreads can cause pain, nausea, headaches, or other signs and symptoms depending on what organ is affected. Once lung cancer has spread beyond the lungs, it’s generally not curable. Treatments are available to decrease signs and symptoms and to help you live longer.
Lung cancer causes
Smoking causes the majority of lung cancers — both in smokers and in people exposed to secondhand smoke. About 80% of lung cancer deaths are caused by smoking, and many others are caused by exposure to secondhand smoke. But lung cancer also occurs in people who never smoked and in those who never had prolonged exposure to secondhand smoke. In these cases, there may be no clear cause of lung cancer. People who smoke and are exposed to other known risk factors such as radon and asbestos are at an even higher risk.
Doctors believe smoking causes lung cancer by damaging the cells that line the lungs. When you inhale cigarette smoke, which is full of cancer-causing substances (carcinogens), changes in the lung tissue begin almost immediately. At first your body may be able to repair this damage. But with each repeated exposure, normal cells that line your lungs are increasingly damaged. Over time, the damage causes cells to act abnormally and eventually cancer may develop.
Workplace exposures to asbestos, diesel exhaust or certain other chemicals can also cause lung cancers in some people who don’t smoke.
A small portion of lung cancers develop in people with no known risk factors for the disease. Some of these might just be random events that don’t have an outside cause, but others might be due to factors that scientists don’t yet know about.
Lung cancers in people who don’t smoke are often different from those that occur in people who do. They tend to develop in younger people and often have certain gene changes that are different from those in tumors found in people who smoke. In some cases, these gene changes can be used to guide treatment.
Inherited gene changes
Some people inherit DNA mutations (changes) from their parents that greatly increase their risk for developing certain cancers. But inherited mutations alone are not thought to cause very many lung cancers. Still, genes do seem to play a role in some families with a history of lung cancer. For example, people who inherit certain DNA changes in a particular chromosome (chromosome 6) are more likely to develop lung cancer, even if they don’t smoke or only smoke a little.
Some people seem to inherit a reduced ability to break down or get rid of certain types of cancer-causing chemicals in the body, such as those found in tobacco smoke. This could put them at higher risk for lung cancer.
Other people inherit faulty DNA repair mechanisms that make it more likely they will end up with DNA changes. People with DNA repair enzymes that don’t work normally might be especially vulnerable to cancer-causing chemicals and radiation.
Some non-small cell lung cancers (NSCLCs) make too much EGFR protein (which comes from an abnormal EGFR gene). This specific gene change is seen more often with adenocarcinoma of the lung in young, non-smoking, Asian women, but the excess EGFR protein has also been seen in more than 60% of metastatic non-small cell lung cancers.
Researchers are developing tests that may help identify such people, but these tests are not yet used routinely. For now, doctors recommend that all people avoid tobacco smoke and other exposures that might increase their cancer risk.
Acquired gene changes
Gene changes related to lung cancer are usually acquired during a person’s lifetime rather than inherited. Acquired mutations in lung cells often result from exposure to factors in the environment, such as cancer-causing chemicals in tobacco smoke. But some gene changes may just be random events that sometimes happen inside a cell, without having an outside cause.
Acquired changes in certain genes, such as the RB1 tumor suppressor gene, are thought to be important in the development of small cell lung cancer (SCLC). Acquired changes in genes such as the p16 tumor suppressor gene and the K-RAS oncogene, are thought to be important in the development of non-small cell lung cancer. Changes in the TP53 tumor suppression gene and to chromosome 3 can be seen in both non-small cell lung cancer and small cell lung cancer. Not all lung cancers share the same gene changes, so there are undoubtedly changes in other genes that have not yet been found.
Risk factors for lung cancer
A number of factors may increase your risk of lung cancer. Some risk factors can be controlled, for instance, by quitting smoking. And other factors can’t be controlled, such as your family history.
Risk factors for lung cancer include:
- Smoking. Your risk of lung cancer increases with the number of cigarettes you smoke each day and the number of years you have smoked. Cigar smoking and pipe smoking are almost as likely to cause lung cancer as cigarette smoking. Smoking low-tar or “light” cigarettes increases lung cancer risk as much as regular cigarettes. Smoking menthol cigarettes might increase the risk even more since the menthol may allow people to inhale more deeply. Quitting at any age can significantly lower your risk of developing lung cancer.
- Exposure to secondhand smoke. Even if you don’t smoke, your risk of lung cancer increases if you’re exposed to secondhand smoke. Secondhand smoke is thought to cause more than 7,000 deaths from lung cancer each year.
- Previous radiation therapy. If you’ve undergone radiation therapy to the chest for another type of cancer, you may have an increased risk of developing lung cancer.
- Exposure to radon gas. Radon is produced by the natural breakdown of uranium in soil, rock and water that eventually becomes part of the air you breathe. Unsafe levels of radon can accumulate in any building, including homes. Homes and other buildings in nearly any part of the United States can have high indoor radon levels (especially in basements). According to the US Environmental Protection Agency (EPA), radon is the second leading cause of lung cancer in this country, and is the leading cause among people who don’t smoke.
- Exposure to asbestos and other carcinogens. Workplace exposure to asbestos and other substances known to cause cancer — such as uranium, beryllium, cadmium, silica, vinyl chloride, nickel compounds, chromium compounds, coal products, mustard gas, chloromethyl ethers and diesel exhaust— can increase your risk of developing lung cancer, especially if you’re a smoker. Government and industry have taken steps in recent years to help protect workers from many of these exposures. But the dangers are still there, so if you work around these agents, be careful to limit your exposure whenever possible.
- Taking certain dietary supplements. Studies looking at the possible role of vitamin supplements in reducing lung cancer risk have had disappointing results. In fact, 2 large studies found that people who smoked who took beta carotene supplements actually had an increased risk of lung cancer. The results of these studies suggest that people who smoke should avoid taking beta carotene supplements.
- Arsenic in drinking water. Studies of people in parts of Southeast Asia and South America with high levels of arsenic in their drinking water have found a higher risk of lung cancer. In most of these studies, the levels of arsenic in the water were many times higher than those typically seen in the United States, even areas where arsenic levels are above normal. For most Americans who are on public water systems, drinking water is not a major source of arsenic.
- Air pollution. In cities, air pollution (especially near heavily trafficked roads) appears to raise the risk of lung cancer slightly. This risk is far less than the risk caused by smoking, but some researchers estimate that worldwide about 5% of all deaths from lung cancer may be due to outdoor air pollution.
- Family history of lung cancer. Brothers, sisters, and children of people who have had lung cancer may have a slightly higher risk of lung cancer themselves, especially if the relative was diagnosed at a younger age. It’s not clear how much of this risk might be due to shared genes among family members and how much might be from shared household exposures (such as tobacco smoke or radon). Researchers have found that genetics seems to play a role in some families with a strong history of lung cancer.
Lifetime chance of getting lung cancer
Overall, the chance that a man will develop lung cancer in his lifetime is about 1 in 17; for a woman, the risk is about 1 in 18 62. These numbers include both smokers and non-smokers. For smokers the risk is much higher, while for non-smokers the risk is lower.
Black men are about 12% more likely to develop lung cancer than White men 62. The rate is about 16% lower in Black women than in White women 62. Both black and white women have lower rates than men, but the gap is closing. The lung cancer rate has been dropping among men over the past few decades, but only for about the last decade in women 62.
Statistics on survival in people with lung cancer vary depending on the type of lung cancer, the stage (extent) of the cancer when it is diagnosed, and other factors.. For survival statistics based on the stage of the cancer, see Non-Small Cell Lung Cancer Survival Rates By Stage.
Despite the very serious prognosis (outlook) of lung cancer, some people with earlier stage cancers are cured. More than 430,000 people alive today have been diagnosed with lung cancer at some point 62.
Lung cancer prevention
You can reduce your risk of lung cancer if you:
- Don’t smoke. If you’ve never smoked, don’t start. Talk to your children about not smoking so that they can understand how to avoid this major risk factor for lung cancer. Begin conversations about the dangers of smoking with your children early so that they know how to react to peer pressure.
- Stop smoking. Stop smoking now. Quitting reduces your risk of lung cancer, even if you’ve smoked for years. Talk to your healthcare team about strategies and aids that can help you quit. Options include nicotine replacement products, medicines and support groups.
- Avoid secondhand smoke. If you live or work with a person who smokes, urge them to quit. At the very least, ask them to smoke outside. Avoid areas where people smoke, such as bars. Seek out smoke-free options.
- Avoid carcinogens at work. Take precautions to protect yourself from exposure to toxic chemicals at work. Follow your employer’s precautions. For instance, if you’re given a face mask for protection, always wear it. Ask your healthcare professional what more you can do to protect yourself at work. Your risk of lung damage from workplace carcinogens increases if you smoke.
- Eat a diet full of fruits and vegetables. Choose a healthy diet with a variety of fruits and vegetables. Food sources of vitamins and nutrients are best. Avoid taking large doses of vitamins in pill form, as they may be harmful. For instance, researchers hoping to reduce the risk of lung cancer in people who smoked heavily gave them beta carotene supplements. Results showed the supplements increased the risk of cancer in people who smoke.
- Exercise most days of the week. If you don’t exercise regularly, start out slowly. Try to exercise most days of the week.
Tobacco smoke
Prevention offers the greatest opportunity to fight lung cancer. Although decades have passed since the link between smoking and lung cancers became clear, smoking is still responsible for most lung cancer deaths.
Quitting reduces your risk of lung cancer, even if you’ve smoked for years. Talk to your doctor about strategies and stop-smoking aids that can help you quit. Options include nicotine replacement products, medications and support groups.
Avoid secondhand smoke. If you live or work with a smoker, urge him or her to quit. At the very least, ask him or her to smoke outside. Avoid areas where people smoke, such as bars and restaurants, and seek out smoke-free options.
Environmental causes
Researchers also continue to look into some of the other causes of lung cancer, such as exposure to radon and diesel exhaust. Finding new ways to limit these exposures could potentially save many more lives.
Test your home for radon. Have the radon levels in your home checked, especially if you live in an area where radon is known to be a problem. High radon levels can be remedied to make your home safer. For information on radon testing, contact your local department of public health or a local chapter of the American Lung Association.
Avoid carcinogens at work. Take precautions to protect yourself from exposure to toxic chemicals at work. Follow your employer’s precautions. For instance, if you’re given a face mask for protection, always wear it. Ask your doctor what more you can do to protect yourself at work. Your risk of lung damage from workplace carcinogens increases if you smoke.
Healthy Diet, Nutrition, and Lifestyle
Researchers are looking for ways to use vitamins or medicines to prevent lung cancer in people at high risk, but so far none have been shown to clearly reduce risk.
Some studies have suggested that a diet high in fruits and vegetables may offer some protection, but more research is needed to confirm this. While any protective effect of fruits and vegetables on lung cancer risk is likely to be much smaller than the increased risk from smoking, following the American Cancer Society dietary recommendations (such as staying at a healthy weight and eating a diet high in fruits, vegetables, and whole grains) may still be helpful.
Avoid taking large doses of vitamins in pill form, as they may be harmful. For instance, researchers hoping to reduce the risk of lung cancer in heavy smokers gave them beta carotene supplements. Results showed beta-carotene supplements actually increased the risk of lung cancer in smokers. The Carotene and Retinol Efficacy Trial 68 included 18,314 male and female current and former smokers (with at least a 20 pack-year history [equivalent to smoking 1 pack per day for 20 years or 2 packs per day for 10 years, for example] of cigarette smoking), as well as some men occupationally exposed to asbestos (who also have a higher risk of lung cancer), all aged 45–74 years. The study randomized participants to take supplements containing 30 mg beta-carotene plus 25,000 IU (7,500 mcg RAE) retinyl palmitate or a placebo daily for about 6 years to evaluate the potential effects on lung cancer risk 68. The trial was ended prematurely after a mean of 4 years, partly because the supplements were unexpectedly found to have increased lung cancer risk by 28% and death from lung cancer by 46%; the supplements also increased the risk of all-cause mortality by 17%. A subsequent study followed the Carotene and Retinol Efficacy Trial participants for an additional 6 years after they stopped taking the study supplements 69. During this time, the differences in lung cancer risk between the intervention and placebo groups were no longer statistically significant, with one exception: women in the intervention group had a 33% higher risk of lung cancer 69.
Exercise most days of the week. A meta-analysis of leisure-time physical activity and lung cancer risk revealed that higher levels of physical activity protect against lung cancer 70. The overall evidence for physical activity has been mixed, but several studies have reported that individuals who are more physically active have a lower risk of lung cancer than those who are more sedentary, even after adjustment for cigarette smoking 71, 72. The American Institute for Cancer Research evidence review rated the inverse association between physical activity and lung cancer as limited suggestive evidence 73.
Early detection
As mentioned in lung cancer screening, screening with low dose spiral CT (LDCT) scans in people at high risk of lung cancer (due to smoking history) lowers the risk of death from lung cancer, when compared to chest x-rays 74. Lung cancer screening is generally offered to older adults who have smoked heavily for many years or who have quit in the past 15 years.
Another approach now being studied uses newer, sensitive tests to look for cancer cells in sputum samples 75. Researchers have found several changes often seen in the DNA of lung cancer cells. Studies are looking at tests that can spot these DNA changes to see if they can find lung cancers at an earlier stage.
Lung cancer screening
Screening is meant to find cancer in people who do not have symptoms of the disease. The U.S. Preventive Services Task Force (USPSTF) makes recommendations about the effectiveness of specific preventive care services for patients without related signs or symptoms 76.
It U.S. Preventive Services Task Force bases its recommendations on the evidence of both the benefits and harms of the service and an assessment of the balance. The U.S. Preventive Services Task Force does not consider the costs of providing a service in this assessment.
In 2021, the USPSTF recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years 77. Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery 77.
For low-dose computed tomography (LDCT), you lie on a thin, flat table that slides back and forth inside the hole in the middle of the CT scanner, which is a large, doughnut-shaped machine. As the table moves into the opening, an x-ray tube rotates within the scanner, sending out many tiny x-ray beams at precise angles. These beams quickly pass through your body and are detected on the other side of the scanner. A computer then converts these results into detailed images of the lungs.
The main benefit of screening is finding the cancer earlier and thus, lowering the chance of dying from lung cancer.
As with any type of screening, it’s important to be aware that, not everyone who gets screened will benefit. Screening with LDCT will not find all lung cancers. Not all of the cancers that are found will be found at an early stage. Some people with lung cancer that is found by screening will still die from that cancer.
Low-dose computed tomography (LDCT) scans can also find things that turn out not to be cancer, but that still have to be checked out with more tests to know what they are. You might need more CT scans, or less often, invasive tests such as a lung biopsy, in which a piece of lung tissue is removed with a needle or during surgery. These tests may lead to serious complications, but they rarely do.
Low-dose computed tomography (LDCT) scans also expose people to a small amount of radiation with each test. It is less than the dose from a standard CT, but it is more than the dose from a chest x-ray. Some people who are screened may end up needing further CT scans, which means more radiation exposure.
American Cancer Society’s guidelines for lung cancer screening
The American Cancer Society has thoroughly reviewed the subject of lung cancer screening and issued guidelines that are aimed at doctors and other health care providers 78:
The American Cancer Society recommends yearly screening for lung cancer with a low-dose CT (LDCT) scan for people ages 50 to 80 years who 79:
- Smoke or used to smoke
- AND
- Have at least a 20 pack-year history of smoking
A pack-year is equal to smoking 1 pack (or about 20 cigarettes) per day for a year. For example, a person could have a 20 pack-year history by smoking 1 pack a day for 20 years, or by smoking 2 packs a day for 10 years.
Before deciding to be screened, people should have a discussion with a health care professional about the purpose of screening and how it is done, as well as the benefits, limits, and possible harms of screening.
People who still smoke should be counseled about quitting and offered interventions and resources to help them.
People should not be screened if they have serious health problems that will likely limit how long they will live, or if they won’t be able to or won’t want to get treatment if lung cancer is found.
To get the most benefit from screening, patients need to be in good health. For example, they need to be able to have surgery and other treatments to try to cure lung cancer if it is found. Patients who need home oxygen therapy probably couldn’t withstand having part of a lung removed, and so are not candidates for screening. Patients with other serious medical problems that would shorten their lives or keep them from having surgery might not benefit enough from screening for it to be worth the risks, and so should also not be screened.
Metal implants in the chest (like pacemakers) or back (like rods in the spine) can interfere with x-rays and lead to poor quality CT images of the lungs. People with these types of implants were also kept out of the National Lung Screening Trial, and so should not be screened with CT scans for lung cancer according to the American Cancer Society guidelines.
Doctors should talk to these patients about the benefits, limitations, and potential harms of lung cancer screening. Screening should only be done at facilities that have the right type of CT scanner and that have a lot of experience using low-dose CT scans for lung cancer screening. The facility should also have a team of specialists that can provide the appropriate care and follow-up of patients with abnormal results on the scans.
If you and your doctor decide that you should be screened, you should get a low-dose CT scan every year until you reach the age of 74, as long as you are still in good health.
Lung cancer diagnosis
If there’s reason to think that you may have lung cancer, your doctor can order a number of tests to look for cancerous cells and to rule out other conditions.
Tests may include:
- Imaging tests. An X-ray image of your lungs may reveal an abnormal mass or nodule. A CT scan can reveal small lesions in your lungs that might not be detected on an X-ray. MRI scans are most often used to look for possible spread of lung cancer to the brain or spinal cord. Positron emission tomography (PET) scan a slightly radioactive form of sugar (known as FDG) is injected into the blood and collects mainly in cancer cells.
- Sputum cytology. If you have a cough and are producing sputum, looking at the sputum under the microscope can sometimes reveal the presence of lung cancer cells. The best way to do this is to get early morning samples 3 days in a row. This test is more likely to help find cancers that start in the major airways of the lung, such as squamous cell lung cancers. It might not be as helpful for finding other types of lung cancer. If your doctor suspects lung cancer, further testing will be done even if no cancer cells are found in the sputum.
- Tissue sample (biopsy). A sample of abnormal cells may be removed in a procedure called a biopsy. Your doctor can perform a biopsy in a number of ways, including bronchoscopy, in which your doctor examines abnormal areas of your lungs using a lighted tube that’s passed down your throat and into your lungs. Mediastinoscopy, in which an incision is made at the base of your neck and surgical tools are inserted behind your breastbone to take tissue samples from lymph nodes is also an option. Another option is needle biopsy, in which your doctor uses X-ray or CT images to guide a needle through your chest wall and into the lung tissue to collect suspicious cells. A biopsy sample may also be taken from lymph nodes or other areas where cancer has spread, such as your liver.
Careful analysis of your cancer cells in a lab will reveal what type of lung cancer you have. Results of sophisticated testing can tell your doctor the specific characteristics of your cells that can help determine your prognosis and guide your treatment.
Molecular tests for gene changes
In some cases, especially for non-small cell lung cancer (NSCLC), doctors may test for specific gene changes in the cancer cells that could mean certain targeted drugs might help treat the cancer. For example:
- About 20% to 25% of non-small cell lung cancer (NSCLC) have changes in the KRAS gene that cause them to make an abnormal KRAS protein, which helps the cancer cells grow and spread. Non-small cell lung cancer (NSCLC) with this mutation are often adenocarcinomas, resistant to other drugs such as EGFR inhibitors, and are most often found in people with a smoking history.
- EGFR (epidermal growth factor receptor) is a protein that appears in high amounts on the surface of 10% to 20% of NSCLC cells and helps them grow. Some drugs that target EGFR can be used to treat NSCLC with changes in the EGFR gene, which are more common in certain groups, such as those who don’t smoke, women, and Asians. But these drugs don’t seem to be as helpful in patients whose cancer cells have changes in the KRAS gene.
- About 5% of non-small cell lung cancer (NSCLC) have a change in the ALK gene. This change is most often seen in people who don’t smoke (or who smoke lightly) and have the adenocarcinoma subtype of non-small cell lung cancer (NSCLC). Doctors may test cancers for changes in the ALK gene to see if drugs that target this change may help them.
- About 1% to 2% of non-small cell lung cancer (NSCLC) have a rearrangement in the ROS1 gene, which might make the tumor respond to certain targeted drugs.
- A small percentage of non-small cell lung cancer (NSCLC) have changes in the RET gene. Certain drugs that target cells with RET gene changes might be options for treating these tumors.
- About 5% of non-small cell lung cancer (NSCLC) have changes in the BRAF gene. Certain drugs that target cells with BRAF gene changes might be an option for treating these tumors.
- A small percentage of non-small cell lung cancer (NSCLC) have certain changes in the MET gene that make them more likely to respond to some targeted drugs.
- In a small percentage of non-small cell lung cancer (NSCLC), the cancer cells have certain changes in the HER2 gene that make them more likely to respond to a targeted drug.
- A small number of non-small cell lung cancer (NSCLC) have changes in one of the NTRK genes that make them more likely to respond to some targeted drugs.
These genetic tests can be done on tissue taken during a biopsy or surgery for lung cancer. If the biopsy sample is too small and all the studies cannot be done, the testing may also be done on blood that is taken from a vein just like a regular blood draw. This blood contains the DNA from dead tumor cells found in the bloodstream of people with advanced lung cancer. Obtaining the tumor DNA through a blood draw is called a “liquid biopsy”. Liquid biopsies are done in cases where a tissue biopsy is not possible or if a tissue biopsy is felt to be too dangerous for the patient.
Tests for certain proteins on tumor cells
Lab tests might also be done to look for certain proteins on the cancer cells. For example, non-small cell lung cancer (NSCLC) cells might be tested for the PD-L1 (program death ligand 1) protein, which can show if the cancer is more likely to respond to treatment with certain immunotherapy drugs.
Lung cancer grades
Grading is a way of dividing cancer cells into groups based on how the cells look under a microscope. This gives your doctors an idea of how quickly or slowly the cancer might grow and whether it is likely to spread.
For most lung cancers, there isn’t a specific grading system doctors use. But generally:
- Grade 1: The cells look very like normal cells. They tend to be slow growing and are less likely to spread than higher grade cancer cells. They are called low grade.
- Grade 2: The cells look more abnormal and are more likely to spread. This grade is also called moderately well differentiated or moderate grade.
- Grades 3 and 4: The cells look very abnormal and not like normal cells. They tend to grow quickly and are more likely to spread. They are called poorly differentiated or high grade.
Lung cancer staging
Once your lung cancer has been diagnosed, your doctor will work to determine the stage (extent) of your cancer. The stage of a cancer tells you how big it is and whether it has spread. Your cancer’s stage helps you and your doctor decide what treatment is most appropriate. For example, the best treatment for an early-stage cancer may be surgery or radiation, while a more advanced-stage cancer may need treatments that reach all parts of the body, such as chemotherapy, targeted drug therapy, or immunotherapy.
Staging tests may include imaging procedures that allow your doctor to look for evidence that cancer has spread beyond your lungs. These tests include CT, MRI, positron emission tomography (PET) and bone scans. Sometimes it’s not possible to be certain about the stage of a cancer until after surgery. Not every test is appropriate for every person, so talk with your doctor about which procedures are right for you.
When a cancer is staged again after the initial staging, it is sometimes referred to as restaging. Often the same tests that were done when the cancer was first diagnosed (such as physical exams, imaging tests, endoscopy exams, biopsies, and maybe surgery) are done again.
With any type of restaging, the new stage classification is added to the original stage, but it doesn’t replace it. The stage assigned at diagnosis is still the one that is most important when discussing statistics like survival rates.
A more formal system to describe the growth and spread of lung cancer is the American Joint Committee on Cancer (AJCC) TNM staging system, which is based on 3 key pieces of information:
- The size and extent of the main tumor (T): How large is the tumor? Has it grown into nearby structures or organs?
- The spread to nearby (regional) lymph nodes (N): Has the cancer spread to nearby lymph nodes?
- The spread (metastasis) (M) to other organs of the body: Has the cancer spread to distant organs such as the brain, bones, adrenal glands, liver, or the other lung?
Numbers or letters appear after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced. Once the T, N, and M categories have been determined, this information is combined in a process called stage grouping, to assign an overall stage.
The following explains what the letters and numbers mean:
Primary tumor (T)
- TX: Main tumor cannot be measured.
- T0: Main tumor cannot be found.
- T1, T2, T3, T4: Refers to the size and/or extent of the main tumor. The higher the number after the T, the larger the tumor or the more it has grown into nearby tissues. T’s may be further divided to provide more detail, such as T3a and T3b.
Regional lymph nodes (N)
- NX: Cancer in nearby lymph nodes cannot be measured.
- N0: There is no cancer in nearby lymph nodes.
- N1, N2, N3: Refers to the number and location of lymph nodes that contain cancer. The higher the number after the N, the more lymph nodes that contain cancer.
Distant metastasis (M)
- MX: Metastasis cannot be measured.
- M0: Cancer has not spread to other parts of the body.
- M1: Cancer has spread to other parts of the body.
Other ways to describe lung cancer stage
The TNM system helps describe cancer in great detail and the TNM combinations are often grouped into five less-detailed stages. When talking about your cancer, your doctor may describe it as one of these stages:
- Stage 0: The earliest stage (pre-cancer) where abnormal cells are present but have not spread to nearby tissue. Also called carcinoma in situ (CIS) or in-situ carcinoma. Carcinoma in situ (CIS) is not cancer, but it may become cancer. In carcinoma in situ (CIS) the carcinoma cells are only in the top layer of cells of the bronchi, bronchioles, or alveoli, without growing into the deeper layers below.
- Stage 1, Stage 2 and Stage 3: Cancer is present. The higher the number, the larger the cancer tumor and the more it has spread into nearby tissues.
- Stage 4: The cancer has spread (metastasize) outside the lung to lymph nodes and other parts of your body.
As a rule, the lower the stage number, the less the cancer has spread. A higher number, such as stage IV (4), means the cancer is considered advanced and has spread to other areas of the body. And within a stage, an earlier letter (or number) means a lower stage.
The same TNM staging system is used for both small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC), although it’s generally not as important for small cell lung cancer (SCLC).
Another staging system that is used for all types of cancer groups the cancer into one of five main categories. This staging system is more often used by cancer registries than by doctors. But, you may still hear your doctor describe your cancer in one of the following ways:
- In situ:Abnormal cells are present but have not spread to nearby tissue.
- Localized: Cancer is limited to the place where it started, with no sign that it has spread.
- Regional: Cancer has spread to nearby lymph nodes, tissues, or organs.
- Distant: Cancer has spread to distant parts of the body.
- Unknown: There is not enough information to figure out the stage.
Stage 1 lung cancer
Stage 1 is part of the number staging system and means your cancer is small. It hasn’t spread to your lymph nodes or other distant organs.
Stage 1 can be divided into 1A and 1B.
Here is a simplified description:
- Stage 1A means the cancer is 3 cm or smaller.
- Stage 1B means the cancer is between 3 cm and 4 cm.
It might also be growing into structures such as:
- the main airway of the lung (main bronchus)
- the membrane covering the lung (visceral pleura)
- Or the cancer is making the lung partly or completely collapse by blocking the airway.
In the TNM staging system, stage 1A is the same as T1a-c, N0, M0.
Stage 1B is the same as T2a, N0, M0
Stage 1A lung cancer
Footnote: Stage 1A lung cancer. The tumor is in the lung only and is 3 centimeters or smaller. Cancer has not spread to the lymph nodes.
[Source 80 ]Stage 1B lung cancer
Footnote: Stage 1B lung cancer. The tumor is larger than 3 centimeters but not larger than 4 centimeters. Cancer has not spread to the lymph nodes; OR the tumor is 4 centimeters or smaller. Cancer has not spread to the lymph nodes and one or more of the following is found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).
[Source 81 ]Stage 2 lung cancer
Stage 2 is part of the number staging system. It can be divided into stage 2A and 2B. Part of the affected lung might have collapsed.
Stage 2 non small cell lung cancer is sometimes called early stage non small cell lung cancer.
- Stage 2A means that the cancer is between 4 cm and 5 cm in size but there are no cancer cells in any lymph nodes.
- Stage 2B means that the cancer is up to 5 cm in size and there are cancer cells in the lymph nodes close to the affected lung.
- Or the cancer is between 5 cm and 7 cm but there are no cancer cells in any lymph nodes.
- Or the cancer is not in any lymph nodes but has spread into one or more of the following areas:
- the chest wall (ribs, muscle or skin)
- the nerve close to the lung (the phrenic nerve)
- the layers that cover the heart (mediastinal pleura and parietal pericardium)
- Or the cancer is less than 7 cm but there is more than one tumor in the same lobe of the lung.
In the TNM staging system stage 2A is the same as T2b, N0, M0
Stage 2B is the same as one of the following:
- T1a-c, N1, M0
- T2a-b, N1, M0
- T3, N0, M0
Stage 2A lung cancer
Footnote: Stage 2A lung cancer. The tumor is larger than 4 centimeters but not larger than 5 centimeters. Cancer has not spread to the lymph nodes and one or more of the following may be found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).
[Source 82 ]Stage 2B lung cancer
Footnote: Stage 2B lung cancer. The primary tumor is 5 centimeters or smaller and cancer has spread to the lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus.
[Source 83 ]Stage 3 lung cancer
Stage 3 is part of the number staging system. Stage 3 non small cell lung cancer is sometimes called locally advanced cancer.
Stage 3 can be divided into 3A, 3B and 3C.
- Stage 3A can mean different things.
- Your cancer is up to 5 cm in size and has spread to the lymph nodes in the center of the chest on the same side as the tumor.
- Or the cancer is between 5 cm and 7 cm and there is more than one tumor in the same lobe of the lung.
- Or the cancer has spread into one or more of the following areas just outside the lung:
- the chest wall (ribs, muscle or skin)
- the nerve close to the lung (the phrenic nerve)
- the layers that cover the heart (mediastinal pleura and parietal pericardium)
- lymph nodes in the lung or close to the lung
- Or your cancer is larger than 7 cm. It hasn’t spread into lymph nodes but has spread into one or more of the following areas:
- the muscle under the lung (diaphragm)
- the center area of the chest (mediastinum)
- the heart
- a main blood vessel
- the wind pipe (trachea)
- the nerve that goes to the voice box (larynx)
- the food pipe (oesophagus)
- a spinal bone
- the area where the wind pipe divides (the carina)
- Or your cancer is in more than one lobe of the same lung and there might also be cancer cells in lymph nodes close to the affected lung.
- Stage 3B can also mean different things.
- Your cancer is less than 5cm and has spread into lymph nodes in one of these places:
- the opposite side of the chest from the affected lung
- the neck
- above the collarbone
- Or your cancer is between 5cm to 7 cm and has spread into lymph nodes in the center of the chest.
- Or the cancer is any size, has spread into lymph nodes in the center of the chest, and has spread into one or more of the following areas:
- the chest wall
- the muscle under the lung (diaphragm)
- the layers that cover the heart (mediastinal pleura and parietal pericardium)
- Or stage 3B means that your cancer has spread into the lymph nodes in the center of the chest. The lung tumor is more than 7 cm or it has spread into a major structure in your chest such as:
- the heart
- the wind pipe (trachea)
- the food pipe (oesophagus)
- a main blood vessel
- Your cancer is less than 5cm and has spread into lymph nodes in one of these places:
- Stage 3C can also mean different things.
- Your cancer is between 5 cm and 7 cm in size or has spread into one or more of the following:
- the nerve close to the lung (phrenic nerve)
- the covering of the heart (parietal pericardium)
- and it has spread into lymph nodes:
- in the center of the chest on the opposite side from the affected lung or
- at the top of the lung on the same side or opposite side or
- above the collar bone
- Or there is more than one tumour in a different lobe of the same lung.
- Or stage 3C can mean the cancer is bigger than 7 cm or it has spread into one of the following:
- the muscle under the lung (the diaphragm)
- the center of the chest (mediastinum)
- the heart
- a major blood vessel
- the wind pipe (trachea)
- the nerve going to the voice box (the recurrent laryngeal nerve)
- the food pipe (esophagus)
- a spinal bone
- the area where the windpipe divides (the carina)
- and it has spread into lymph nodes:
- in the center of the chest on the opposite side from the affected lung or
- at the top of the lung on the same side or opposite side or
- above the collar bone
- Or there are tumors in more than one lobe of the lung.
- Your cancer is between 5 cm and 7 cm in size or has spread into one or more of the following:
In the TNM staging system stage 3A is the same as one of the following:
- T1a-c, N2, M0
- T2a-b, N2, M0
- T3, N1, M0
- T4, N0, M0
- T4, N1, M0
Stage 3B is the same as one of the following:
- T1a-c, N3, M0
- T2a-b, N3, M0
- T3, N2, M0
- T4, N2, M0
Stage 3C is the same as:
- T3, N3, M0
- T4, N3, M0
Stage 3A lung cancer
Footnote: Stage 3A lung cancer. The tumor is 5 centimeters or smaller and cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are around the trachea or aorta (not shown), or where the trachea divides into the bronchi. Also, one or more of the following may be found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).
[Source 84 ]Stage 3B lung cancer
Footnote: Stage 3B lung cancer. The primary tumor is 5 centimeters or smaller and cancer has spread to lymph nodes above the collarbone on the same side of the chest as the primary tumor or to any lymph nodes on the opposite side of the chest as the primary tumor. Also, one or more of the following may be found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).
[Source 85 ]Stage 4 lung cancer
Stage 4 lung cancer also called advanced lung cancer, which means the cancer has spread. Stage 4 is divided into stage 4A and 4B.
- Stage 4A can mean any of the following:
- there is cancer in both lungs
- the cancer is in the covering of the lung (the pleura) or the covering of the heart (pericardium)
- or there is fluid around the lungs or the heart that contains cancer cells
- Or it can mean that there is a single area of cancer that has spread outside the chest to a lymph node or to an organ such as the liver or bone.
- Stage 4B means that the cancer has spread to several areas in one or more organs.
In the TNM staging system, stage 4 is the same as one of the following:
- Any T, Any N, M1a
- Any T, Any N, M1b
- Any T, Any N, M1c
Stage 4A lung cancer
Footnote: Stage 4A lung cancer. The tumor may be any size and cancer may have spread to the lymph nodes. One or more of the following is found: (a) there are one or more tumors in the lung that does not have the primary tumor; and/or (b) cancer is found in fluid around the lungs or heart or there are cancer nodules in the lining around the lungs or the sac around the heart; and/or (c) cancer has spread to one place in an organ or tissue not near the lung, such as the brain, adrenal gland, kidney, liver, or bone, or to a lymph node that is not near the lung.
[Source 86 ]Stage 4B lung cancer
Footnote: Stage 4B lung cancer. The cancer has spread to multiple places in one or more organs that are not near the lung, such as the brain, adrenal gland, kidney, liver, distant lymph nodes, or bone.
[Source 87 ]Lung cancer treatment
You and your doctor choose a cancer treatment plan based on a number of factors, such as your overall health, the type and stage of your cancer, the goal of treatment and your preferences. The most suitable treatment will also depend on whether the cancer started in your lung (primary) or spread from another part of your body (metastasis). In the case of a metastasis to the lung, the treatment is usually chosen based on the location of the primary cancer.
Types of lung cancer treatments can include:
- Surgery, to cut out the cancer — this includes a lobectomy where one lobe of a lung is removed, a pneumonectomy, where one whole lung is removed, or a wedge resection where only part of a lung is removed
- Radiotherapy, which damages cancer cells and stops them dividing or spreading
- Chemotherapy, which uses strong medicines to kill cancer cells
- Targeted therapy, which uses medicine that attacks specific features of a cancer — for example, certain genetic mutations
- Immunotherapy, which helps your immune system see cancer cells and kill them
Your medical team may recommend one or a combination of these treatments, depending on your situation.
Cancer treatment may be given with the aim of removing all signs of cancer (curative). In other cases, the goal may be to relieve symptoms and maximise quality of life (palliative care) without necessarily curing the cancer completely.
In some cases, you may choose not to undergo treatment. For instance, you may feel that the side effects of treatment will outweigh the potential benefits. When that’s the case, your doctor may suggest comfort care to treat only the symptoms the cancer is causing, such as pain or shortness of breath.
Surgery
During surgery, your surgeon works to remove the lung cancer and a margin of healthy tissue. Procedures to remove lung cancer include:
- Wedge resection to remove a small section of lung that contains the tumor along with a margin of healthy tissue
- Segmental resection to remove a larger portion of lung, but not an entire lobe
- Lobectomy to remove the entire lobe of one lung
- Pneumonectomy to remove an entire lung
If you undergo surgery, your surgeon may also remove lymph nodes from your chest in order to check them for signs of cancer.
Surgery may be an option if your cancer is confined to the lungs. If you have a larger lung cancer, your doctor may recommend chemotherapy or radiation therapy before surgery in order to shrink the cancer. If there’s a risk that cancer cells were left behind after surgery or that your cancer may recur, your doctor may recommend chemotherapy or radiation therapy after surgery.
Radiation therapy
Radiation therapy uses high-powered energy beams from sources such as X-rays and protons to kill cancer cells. During radiation therapy, you lie on a table while a machine moves around you, directing radiation to precise points on your body.
For people with locally advanced lung cancer, radiation may be used before surgery or after surgery. It’s often combined with chemotherapy treatments. If surgery isn’t an option, combined chemotherapy and radiation therapy may be your primary treatment.
For advanced lung cancers and those that have spread to other areas of the body, radiation therapy may help relieve symptoms, such as pain.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. One or more chemotherapy drugs may be given through a vein in your arm (intravenously) or taken orally. A combination of drugs usually is given in a series of treatments over a period of weeks or months, with breaks in between so that you can recover.
Chemotherapy is often used after surgery to kill any cancer cells that may remain. It can be used alone or combined with radiation therapy. Chemotherapy may also be used before surgery to shrink cancers and make them easier to remove.
In people with advanced lung cancer, chemotherapy can be used to relieve pain and other symptoms.
Stereotactic body radiotherapy
Stereotactic body radiotherapy, also known as radiosurgery, is an intense radiation treatment that aims many beams of radiation from many angles at the cancer. Stereotactic body radiotherapy treatment is typically completed in one or a few treatments.
Stereotactic body radiotherapy may be an option for people with small lung cancers who can’t undergo surgery. It may also be used to treat lung cancer that spreads to other parts of the body, including the brain.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Many targeted therapy drugs are used to treat lung cancer, though most are reserved for people with advanced or recurrent cancer.
Some targeted therapies only work in people whose cancer cells have certain genetic mutations. Your cancer cells may be tested in a laboratory to see if these drugs might help you.
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body’s disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy treatments are generally reserved for people with locally advanced lung cancers and cancers that have spread to other parts of the body.
Alternative medicine
Complementary and alternative lung cancer treatments can’t cure your cancer. But complementary and alternative treatments can often be combined with your doctor’s care to help relieve signs and symptoms.
The American College of Chest Physicians suggests people with lung cancer may find comfort in:
- Acupuncture. During an acupuncture session, a trained practitioner inserts small needles into precise points on your body. Acupuncture may relieve pain and ease cancer treatment side effects, such as nausea and vomiting, but there’s no evidence that acupuncture has any effect on your cancer.
- Hypnosis. Hypnosis is typically done by a therapist who leads you through relaxation exercises and asks you to think pleasing and positive thoughts. Hypnosis may reduce anxiety, nausea and pain in people with cancer.
- Massage. During a massage, a massage therapist uses his or her hands to apply pressure to your skin and muscles. Massage can help relieve anxiety and pain in people with cancer. Some massage therapists are specially trained to work with people who have cancer.
- Meditation. Meditation is a time of quiet reflection in which you focus on something, such as an idea, image or sound. Meditation may reduce stress and improve quality of life in people with cancer.
- Yoga. Yoga combines gentle stretching movements with deep breathing and meditation. Yoga may help people with cancer sleep better.
Palliative care
People with lung cancer often experience signs and symptoms of the cancer, as well as side effects of treatment. Supportive care, also known as palliative care, is a specialty area of medicine that involves working with a doctor to minimize your signs and symptoms. The palliative care team’s goal is to improve quality of life for you and your family.
Your doctor may recommend that you meet with a palliative care team soon after your diagnosis to ensure that you’re comfortable during and after your cancer treatment.
Palliative care specialists work with you, your family and your care team. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time you’re getting strong cancer treatments, such as surgery, chemotherapy or radiation therapy.
In one study, people with advanced non-small cell lung cancer who began receiving supportive care soon after their diagnosis lived longer than those who continued with treatments, such as chemotherapy and radiation. Those receiving supportive care reported improved mood and quality of life. They survived, on average, almost three months longer than did those receiving standard care.
Pleurisy
Pleurisy also called pleuritis is an inflammation of the pleura, a large, thin sheet of tissue that wraps around the outside of your lungs and lines the inside of your chest cavity (Figures 1 and 2) 88, 89. These two large, thin layers of tissue called the pleura separate your lungs from your chest wall. One layer wraps around the outside of the lungs (visceral pleura). The other layer lines the inner chest wall (parietal pleura). The visceral pleura does not contain pain receptors, whereas the parietal pleura is innervated by somatic nerves that sense pain due to trauma or inflammation. Between these two layers is a very thin space called the pleural space, that’s usually filled with a very small amount of fluid that helps the two layers of the pleura glide smoothly past each other as your lungs breathe air in and out. The layers act like two pieces of smooth satin gliding past each other, allowing your lungs to expand and contract when you breathe without any resistance from the lining of the chest wall. Pleurisy occurs when the two layers of the pleura become irritated and inflamed, rubbing against each other like two pieces of sandpaper, producing sharp chest pain when you inhale and exhale. Pleuritic pain is usually worse when you breathe or cough and lessens or stops when you hold your breath. Pleurisy is usually caused by a chest infection – either a viral infection such as influenza or a bacterial infection such as pneumonia. Other causes of pleurisy include autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus (SLE), heart and lung diseases, with 30% to 40% of cases classified as idiopathic or unknown cause 90.
Studies of pleuritic chest pain have shown that pulmonary embolism is the most common life-threatening cause and the source of the pain 5% to 21% of the time 91, 92. A recent prospective trial of 7,940 patients evaluated for pulmonary embolism revealed that pleuritic-type chest pain was significantly associated with confirmed pulmonary embolism 93. The most commonly occurring symptoms of pulmonary embolism were shortness of breath (dyspnea) and pleuritic chest pain in 73% and 66% of patients, respectively 91.
Pleuritic pain occurs in nearly 90% of patients with pneumothorax and 50% of those with community-acquired pneumonia 94. A recent study revealed that when surgical pleural biopsy is used to investigate the cause of pleurisy, 56% of cases are attributed to neoplastic diseases, including mesothelioma (23%), lung cancer (16%), and lymphoma (2.5%) 95. Infectious diseases account for 24%, with tuberculosis leading at 16.2%, followed by parapneumonic pleural effusion (3.6%), empyema (3.5%), nontuberculous mycobacteriosis (0.5%), and paragonimiasis or lung fluke disease, a parasitic infection caused by eating raw or undercooked crabs or crayfish containing lung fluke (trematode) larvae, most commonly Paragonimus westermani (0.1%). Autoimmune diseases account for 2.8% of pleural biopsy findings, with rheumatoid arthritis (1.3%) and systemic lupus erythematosus (SLE) (0.3%) being the most common 95. Pleurisy is the initial symptom in 10% of systemic lupus erythematosus (SLE) patients and occurs at some stage in 40% to 60% systemic lupus erythematosus (SLE) patients. Symptomatic pleurisy is also relatively common in rheumatoid arthritis; while 70% of patients show pleural effusion in autopsy studies, only 3% to 5% experience symptoms 96, 97, 98. Recent studies indicate that the lymph nodes and pleura are the most commonly involved extrapulmonary sites in tuberculosis 94, 99, 100.
The main symptom of pleurisy is a sharp or stabbing knife-like pain in your chest that gets worse when you breathe in deeply, cough, sneeze or laugh. The pain may stay in one place or it may spread to your shoulder or back. Sometimes it becomes a fairly constant dull ache. Depending on what’s causing the pleurisy, you may have other symptoms, such as:
- Shortness of breath
- A cough
- Fever and chills
- Rapid, shallow breathing
- Unexplained weight loss
- A sore throat followed by pain and swelling in your joints
Some people also get a pleural effusion, which is when the inflammation causes a large build-up of fluid between the linings of the lung and chest wall.
This can help relieve the symptoms of pleurisy because the linings no longer rub against each other. However, it can also cause compression of the lungs, leading to breathing problems.
Treatment of pleurisy involves pain control and treating the underlying cause. For example, if bacterial pneumonia is the cause, an antibiotic can be prescribed to manage the infection. If the cause is a viral infection, pleurisy may go away on its own.
The pain and inflammation associated with pleurisy is usually treated with nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others). Occasionally, your doctor may prescribe corticosteroid medication. Corticosteroids should be reserved for patients who are intolerant of nonsteroidal anti-inflammatory drugs (NSAIDs). Corticosteroids are also used in the treatment of tuberculous pleurisy and have been shown to result in some reduction in effusions and symptoms, but they have not demonstrated improvements in mortality 101.
The outcome of pleurisy treatment depends on the seriousness of the underlying cause. Early diagnosis and treatment of the condition that caused pleurisy can help you feel better. Depending on the cause and the condition, you may make a full recovery.
Figure 14. Pleuritic chest pain diagnostic algorithm
Abbreviations: CTA = computed tomography angiography; CXR = chest radiography; ECG = electrocardiography; MI = myocardial infarction; NSAID = nonsteroidal anti-inflammatory drug; V-Q = ventilation-perfusion.
[Source 89 ]Figure 15. Pleuritic chest pain life-threatening causes and red flags
[Source 89 ]How do you get pleurisy?
You can get pleurisy when inflammation from your lungs — caused by a virus, bacteria or other illness — moves into your pleural space (the potential space between the two layers of the pleura, visceral and parietal pleura that surrounds the lungs), causing them to swell up and rub against each other. This can also happen if there’s a blockage like a tumor or damage to your lung.
Is pleurisy contagious?
Depends on the cause of your pleurisy. Pleurisy caused by the flu or bacterial infection is contagious.
Who does pleurisy affect?
Anyone can get pleurisy, but you’re at a higher risk if you:
- Are over 65.
- Have a condition that causes inflammation in your body like an autoimmune disease (a disease in which your immune system mistakenly attacks your own healthy cells, tissues, and organs, leading to inflammation and damage in your body).
- Take medications that cause inflammation in your body.
- Have tumors or scarring in your lungs.
How serious is pleurisy?
Pleurisy can be mild or very serious. It depends on what’s causing it and whether you have additional complications.
Can pleurisy go away on its own?
If pleurisy is caused by a virus, it can go away on its own as you get over being sick. More serious underlying causes such as cancer or other illnesses need to be treated before pleurisy will get better.
How long does pleurisy last?
Recovery and how long does pleurisy last depends on the cause of the pleurisy. In most cases of pleuritic chest pain from viral infection, pain and symptoms will resolve within two to four weeks.
Health problems that may develop from pleurisy include:
- Breathing difficulty
- Fluid buildup between chest wall and lung (pleural effusion)
- Complications from the original illness.
Can you get pleurisy more than once?
Yes. If you have an illness that puts you at risk for pleural inflammation, you might get pleurisy more than once.
Pleurisy causes
Most cases of pleurisy are caused by a virus, such as the flu (influenza) virus 88, 89.
Less common causes of pleurisy include:
- Bacterial infections, such as pneumonia and tuberculosis, and infections from parasites
- Common bacterial infections that can lead to pleurisy 89, 102, 103:
- Empyema
- Tuberculosis
- Legionellae
- Bacterial pneumonia
- Spontaneous bacterial pleuritis
- Mediterranean spotted fever also known as boutonneuse fever, is a tick-borne rickettsial disease caused by Rickettsia conorii and transmitted by the brown dog tick (Rhipicephalus sanguineus), primarily found in the Mediterranean Basin, Southern Europe, Africa, and the Middle East
- Parasitic causes, such as amebiasis and paragonimiasis caused by consuming undercooked crab or crayfish infected with Paragonimus westermani, are potential contributors to pleurisy 104.
- Common bacterial infections that can lead to pleurisy 89, 102, 103:
- Viral causes of pleurisy 89:
- Fungal infection
- A blood clot that travels through the blood vessels to the lungs (pulmonary embolism)
- Chest injury – if the ribs are bruised or fractured, the pleura can become inflamed
- Cancer, such as lung cancer, lymphoma, and mesothelioma
- Autoimmune conditions, such as rheumatoid arthritis and lupus. Additional autoimmune or inflammatory conditions causing pleurisy include 105:
- Ankylosing spondylitis
- Collagen vascular disease
- Reactive eosinophilic pleuritis
- Sjögren syndrome
- Chest and heart surgery, especially coronary artery bypass grafting (CABG)
- Certain medications
- Rib fracture
- Lung diseases, such as chronic obstructive pulmonary disease (COPD), pneumothorax, hemothorax, pulmonary embolism, pleural effusion, pulmonary adhesions, lymphangioleiomyomatosis or asbestosis
- Inflammatory bowel disease (IBD) e.g., Crohn’s disease 106
- Certain inherited diseases, such as sickle cell disease or Familial Mediterranean fever, an inherited condition that often causes fever and swelling in the abdomen or lungs.
- Kidney conditions
- Chronic kidney disease (CKD)
- Renal capsule hematoma 107
Other causes of pleurisy include chest injuries, pancreatitis (an inflamed pancreas), and reactions to certain medicines and recreational drugs such as cocaine, heroin, and methadone 108. Reactions to certain medicines can cause a condition similar to lupus. These medicines include isoniazid, hydralazine, nitrofurantoin, and cyclophosphamide.
Sometimes doctors can’t find the cause of pleurisy (idiopathic).
Pleurisy symptoms
The signs and symptoms of pleurisy might include:
- Sharp or stabbing knife-like pain chest pain that worsens when you breathe, cough or sneeze
- Shortness of breath — because you are trying to minimize breathing in and out
- A cough — only in some cases
- A fever — only in some cases
Pain caused by pleurisy also might affect your shoulders or back.
You may have other conditions along with pleurisy, including:
- Partial lung collapse (atelectasis).
- Excess fluid around your lungs (pleural effusion).
- Pus collecting around your lungs (empyema).
In some cases of pleurisy, fluid builds up in the small space between the two layers of tissue (pleural space). This is called pleural effusion. When there is a fair amount of fluid, pleuritic pain lessens or disappears because the two layers of pleura are no longer in contact. A large amount of fluid in the pleural space can create pressure, compressing your lung to the point that it partially or completely collapses. This makes breathing difficult and might cause you to cough. The extra fluid can also become infected. This is called an empyema – a collection of pus in the space between the lung and the inner surface of the chest wall (pleural space). An empyema is often accompanied by fever.
Pleurisy complications
The potential complications of pleurisy vary widely and are closely tied to its underlying cause.
Cardiovascular disease complications:
- Papillary muscle rupture
- Left ventricular free wall rupture
- Interventricular septum rupture
- Acute and chronic heart failure
- Death
- Arrhythmias and conduction abnormalities
- Post-cardiac injury syndrome
- Cardiac tamponade
Lung disease complications:
- Shock
- Recurrence
- Pneumonia
- Stroke
- Pulmonary hypertension
- Respiratory failure
- Empyema
- Atelectasis
- Tension pneumothorax
- Hemopneumothorax is when blood and air enter your pleural space and put pressure around your lungs
Autoimmune conditions complications:
- Cholesterol effusions
- Lung entrapment
Infectious disease complications:
- Sepsis
- Empyema
- Pneumothorax
- Cancer associated with tuberculosis
- Bronchiectasis
- Broncholithiasis a condition characterized by the presence of calcified or ossified material, often originating from calcified lymph nodes, within the tracheobronchial tree, potentially causing airway obstruction and inflammation
- Acute respiratory distress syndrome (ARDS)
- Venous thromboembolism
- Chronic pulmonary aspergillosis 109
- Pleural lymphoma associated with longstanding chronic pleural infection 110, 111
- Bronchopleural fistula
- Pleural fibrosis is the scarring, thickening and stiffening of the pleura (the membrane surrounding the lungs) due to inflammation or exposure to irritants like asbestos, leading to scar tissue accumulation and potentially restricting lung function
Kidney disease complications:
- Constrictive pleural thickening
- Pulmonary embolism
- Empyema
- Pulmonary edema
Drug-Induced Pleural Disease complications:
- Hypoxia
- Pulmonary embolism
- Pleural fibrosis is the scarring, thickening and stiffening of the pleura (the membrane surrounding the lungs) due to inflammation or exposure to irritants like asbestos, leading to scar tissue accumulation and potentially restricting lung function
Pleurisy diagnosis
Your doctor will find out if you have pleurisy or another pleural disorder by taking a detailed medical history and doing a physical exam with a stethoscope and several diagnostic tests, including:
- Blood tests. A blood test might tell your doctor if you have an infection. Other blood tests also might detect an autoimmune disorder, such as rheumatoid arthritis or lupus. In these conditions, pleurisy can be the first sign.
- Arterial blood gas tests, which show how well your lungs are taking in oxygen. For this test, a blood sample is taken from an artery, usually in your wrist. The blood’s oxygen and carbon dioxide levels are checked. This test shows how well your lungs are taking in oxygen.
- Chest X-ray. A chest X-ray can show if your lungs are fully inflating or if there is air or fluid between the lungs and ribs. Your doctor might recommend a special type of chest X-ray in which you lie on your side (decubitus chest X-ray).
- Computerized tomography (CT) scan. In a CT scan, a computer translates information from X-rays into images of thin sections (slices) of your chest, producing more-detailed images. A chest CT scan can show if there is a blood clot in the lung or find other causes of pleuritic pain.
- Ultrasound. This imaging method uses high-frequency sound waves to produce precise images of structures within your body. Your doctor might use ultrasound to determine whether you have a pleural effusion.
- Electrocardiogram (ECG or EKG). Your doctor might recommend this heart-monitoring test to rule out certain heart problems as a cause for your chest pain.
Medical history
The time course of the onset of symptoms is the most useful historical information for narrowing the differential diagnosis. Most potentially deadly causes of pleuritic chest pain (i.e., pulmonary embolism, heart attack, aortic dissection, and pneumothorax) typically have an acute onset over minutes 89. In contrast, less immediately life-threatening causes of pleuritic chest pain (e.g., infection, cancer, inflammatory processes) progress over hours to days or weeks 112. Pain that worsens when you’re supine (lying on your back with your face upwards) and lessens when you’re upright and leaning forward should prompt consideration for pericarditis 113, 114, 112. True shortness of breath (dyspnea) should also increase suspicion for a pulmonary embolus, pneumothorax, or pneumonia 115, 116, 117. It is clinically useful to distinguish true shortness of breath (dyspnea) from patient-perceived dyspnea caused by a desire to suppress respirations to avoid pain 118, 119.
Cardiac symptoms such as diaphoresis, nausea, and palpitations should be elucidated. Pain that is described as sharp and stabbing is typical of noncardiac chest pain 118. Radiation of pain to the shoulders or arms has a positive likelihood ratio of 4.07 for acute myocardial infarction 118. In contrast, pain that radiates to the back and is maximal in intensity at onset is more commonly associated with aortic dissection than cardiac ischemia 118.
Cough, fever, and sputum production should prompt evaluation for community-acquired pneumonia. Symptoms such as weight loss, malaise, night sweats, or arthralgias indicate chronic inflammatory causes of pleuritic chest pain, such as tuberculosis infection, rheumatoid arthritis, or malignancy. A family history of similar symptoms increases the likelihood of rare diagnoses such as familial Mediterranean fever. A medication history that includes the use of drugs with a high risk of adverse pulmonary effects should raise concerns for a pharmacologic reaction. A sickle cell crisis must be considered in any patient with known sickle cell disease.
Physical examination
Tachycardia or tachypnea may be present with any of the serious causes of pleuritic chest pain but should raise suspicion for pulmonary embolism, pneumothorax, or myocardial infarction 89. Patients may demonstrate shallower breaths as they attempt to avoid deep breathing that triggers pain 119. Likewise, hypotension and a markedly widened pulse pressure should raise concerns for aortic dissection or severe myocardial infarction. Fever increases the likelihood of infection.
Pleural inflammation, or pleurisy, causes roughening of the smooth surfaces of the parietal and visceral pleurae. As these surfaces rub against each other with normal inspiration and expiration, a scratching sound or friction rub may be heard. This may also occur in 4% of patients with pneumonia or pulmonary embolism 120. Pneumonia with lung consolidation may also lead to decreased breath sounds, rales, and egophony. In contrast, pneumothorax could lead to hyperresonance on lung examination.
In new-onset heart failure due to large myocardial infarction, cardiac examination may show an extra heart sound (third S3 or fourth S4 heart sound). A friction rub may be heard over the heart in severe cases of pericarditis. Patients may present with an initial normal examination even when serious conditions are present. The absence of a clear diagnosis warrants additional diagnostic testing.
Diagnostic tests
Most patients presenting with pleuritic chest pain will require imaging with chest X-ray to fully define their diagnosis 117. If pleural fluid is seen on a chest X-ray, the fluid can be aspirated and examined for additional clues about the source of the pleuritic chest pain 121, 122 Lung ultrasonography can guide thoracentesis, as well as localize a small pneumothorax and identify other pulmonary conditions 123, 124.
When a cardiac or vascular source is considered, electrocardiography (ECG), cardiac enzyme studies, and echocardiography are useful tests. Widespread ST segment elevation is a typical electrocardiographic finding in pericarditis 125, 126. In the case of infection, a complete blood count, serology, and cultures of blood, sputum, or pleural fluid may be indicated. A validated clinical decision rule for pulmonary embolism should be employed to guide the use of additional tests such as d-dimer assays, ventilation-perfusion scans, or computed tomography angiography 127, 128, 129, 130. Figure 2 above integrates red flag symptoms of serious causes of pleuritic chest pain, physical examination, and diagnostic findings to aid in the evaluation of pleuritic chest pain.
Diagnostic tests might include:
- Thoracentesis. To remove fluid for laboratory analysis, your doctor might suggest thoracentesis. In this procedure, your doctor injects a local anesthetic between your ribs to the area where fluid was seen on your imaging studies. Next your doctor inserts a needle through your chest wall between your ribs to remove fluid for laboratory analysis. Your doctor might insert the needle with the help of ultrasound guidance.
- Thoracoscopy or pleuroscopy. If tuberculosis or cancer is a suspected cause of your condition, your doctor might perform a procedure that allows for direct visualization inside your chest to look for any abnormalities or to obtain a tissue sample (biopsy) if needed.
- Biopsy. Your doctor may suspect that tuberculosis or cancer has caused fluid to build up in your pleural space. If so, he or she may want to look at a small piece of the pleura under a microscope. To take a tissue sample, your doctor may do one of the following procedures:
- Insert a needle into your chest to remove a small sample of the pleura’s outer layer.
- Insert a tube with a light on the end (endoscope) into tiny cuts in your chest wall so that he or she can see the pleura. Your doctor can then snip out small pieces of tissue. This procedure must be done in a hospital. You’ll be given medicine to make you sleep during the procedure.
- Snip out a sample of the pleura through a small cut in your chest wall. This is called an open pleural biopsy. It’s usually done if the sample from the needle biopsy is too small for an accurate diagnosis. This procedure must be done in a hospital. You’ll be given medicine to make you sleep during the procedure.
Your doctor will look at the fluid under a microscope to determine what’s causing the fluid buildup. If the fluid is infected, treatment involves antibiotics and draining the fluid. If the infection is tuberculosis or from a fungus, treatment involves long-term use of antibiotics or antifungal medicines. If the fluid is caused by tumors of the pleura, it may build up again quickly after it’s drained. Sometimes antitumor medicines will prevent further fluid buildup. If they don’t, the doctor may seal the pleural space.
Pleurisy treatment
Treatments used in pleurisy and pleural effusion focus primarily on the underlying cause.
How to treat pleurisy
To relieve symptoms, your doctor may recommend:
- Acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, to control pain
- Codeine-based cough syrups to control a cough
- Lying on the painful side to make you more comfortable. It seems strange, but lying on the side of your chest that hurts may also help reduce the pain.
- Breathing deeply and coughing to clear mucus as the pain eases
- Getting plenty of rest.
The outcome of pleurisy treatment depends on the seriousness of the underlying disease. If the condition that caused pleurisy is diagnosed and treated early, a full recovery is typical.
Treating the underlying cause of pleurisy
If your pleurisy is caused by a viral infection, it’ll usually get better on its own after a few days.
If it’s caused by a bacterial infection, you’ll need antibiotics. Depending on the severity of your symptoms, this may be either tablets or injections.
If your symptoms are particularly severe or you’re already in poor health, you may need to be admitted to hospital.
Treating pleural effusion
In some cases, pleurisy causes a build-up of excess fluid around the lungs called pleural effusion.
Pleural effusion can lead to shortness of breath that gets progressively worse. This is more likely if pleurisy is caused by pulmonary embolism or a bacterial infection.
If pleural effusion doesn’t clear up as your pleurisy is treated or you’re very short of breath, the fluid may need to be drained by inserting a needle or tube through the chest wall.
A procedure called thoracentesis is used to remove fluid from the pleural space. The doctor inserts a needle or a thin, hollow, plastic tube through the ribs in the back of your chest into your chest wall. A syringe is attached to draw fluid out of your chest.
- If your doctor needs to remove a lot of fluid, he or she may use a chest tube. Your doctor will inject a painkiller into the area of your chest wall where the fluid is. He or she will then insert a plastic tube into your chest between two ribs. The tube will be connected to a box that suctions out the fluid. Your doctor will use a chest x ray to check the tube’s position.
- Your doctor also can use a chest tube to drain blood and air from the pleural space. This process can take several days. The tube will be left in place, and you’ll likely stay in the hospital during this time.
This can be done under general anesthetic or local anesthetic. You may need to stay in hospital for a few days if a lot of fluid has to be drained away.
The fluid sample that was removed during thoracentesis will be checked under a microscope. This can tell your doctor what’s causing the fluid buildup, and he or she can decide the best way to treat it.
If the fluid is infected, treatment will involve antibiotics and drainage. If you have tuberculosis or a fungal infection, treatment will involve long-term use of antibiotics or antifungal medicines.
If tumors in the pleura are causing fluid buildup, the fluid may quickly build up again after it’s drained. Sometimes antitumor medicines will prevent further fluid buildup. If they don’t, your doctor may seal the pleural space. Sealing the pleural space is called pleurodesis.
For this procedure, your doctor will drain all of the fluid out of your chest through a chest tube. Then he or she will push a substance through the chest tube into the pleural space. The substance will irritate the surface of the pleura. This will cause the two layers of the pleura to stick together, preventing more fluid from building up.
Chemotherapy or radiation treatment also may be used to reduce the size of the tumors.
If heart failure is causing fluid buildup, treatment usually includes diuretics (medicines that help reduce fluid buildup) and other medicines.
Pleurisy treatment at home
The following steps might help relieve symptoms related to pleurisy:
- Take medication. Take medication such as ibuprofen (Advil, Motrin IB, others) as needed to relieve pain and inflammation.
- Get plenty of rest. Find the position that causes you the least discomfort and try to stay in it. Even when you start to feel better, be careful not to overdo it.
- Don’t smoke. Smoking can cause more irritation to your lungs. If you smoke and can’t quit on your own, ask your healthcare provider for help.
Pleurisy prognosis
Your prognosis (outlook) for pleurisy depends on what’s causing it and the effectiveness of your treatment. If your pleurisy is caused by infection, it should go away as you get better. If it’s caused by an ongoing illness like cancer or an autoimmune disease, you may always have some risk of pleurisy coming back. Very rarely, pleurisy has life-threatening complications.
Infectious causes
Viral pleuritis is generally self-limited, with symptoms typically resolving within a few days or weeks 88. People with bacterial pleural infections usually improve with appropriate antibiotic treatment. The reported 30-day mortality rate for bacterial infections is 10.5%, with 1-year mortality nearing 19% 131. Recent studies indicate that affected patients face an increased risk of thromboembolic events (a condition where a blood clot or thrombus breaks off and travels through the bloodstream to obstruct a blood vessel) due to significant inflammation, prolonged hospitalizations, frequent comorbidities, and the need for operative interventions 132.
Autoimmune conditions
The prognosis of lupus pleuritis is generally good 88. However, the prognosis of pleuritis associated with rheumatoid arthritis varies 88. While many patients experience spontaneous resolution within 3 months, some may develop persistent effusion and pleural thickening. Anti-inflammatory therapy does not appear to be effective in resolving rheumatoid pleuritis 88.
Cancer
Cancer causing pleural disease is associated with a poor prognosis. A study in patients with malignant mesothelioma showed a median survival of just 13 months following diagnosis 133.
Lung conditions
The presence of a pleural effusion is linked to increased mortality, with 15% of patients dying within 30 days and 32% within 1 year of hospital admission 134. However, with early treatment, the mortality rate for pulmonary embolism decreases from 30% to 8%.
Heart and blood vessel conditions
Acute heart attack has a mortality rate of 30%, with nearly 50% of deaths occurring before patients reach the hospital 88. Early reperfusion through fibrinolysis or percutaneous coronary intervention within 90 minutes of arrival, along with preserved left ventricular function and short- and long-term treatment with beta-blockers, aspirin, and angiotensin-converting enzyme inhibitors, all contribute to improved survival 88. The strongest predictor of a poor outcome is poorly preserved left ventricular function 135.
Additional factors that worsen mortality include:
- Older age
- Diabetes
- Delayed reperfusion
- Elevated B-type natriuretic (BNP) peptide and high-sensitivity C-reactive protein (CRP)
- Depression
- Involvement of lead aVR on ECG 136.
- Presence of heart failure or pulmonary edema
- History of cerebrovascular disease or peripheral vascular disease
- Elevated thrombolysis in myocardial infarction risk score for unstable angina/non–ST-elevation acute coronary syndrome
The thrombolysis in myocardial infarction (heart attack) risk score includes 7 factors, including age 65 or older, 3 or more risk factors for cardiac disease, previous coronary disease, ST-segment deviation of 0.5 mm or more, 2 or more episodes of angina in the last 24 hours, aspirin use within the prior week, and elevated cardiac enzyme levels 137.
The overall prognosis for Dressler syndrome also known as postmyocardial infarction syndrome, is a form of secondary pericarditis (inflammation of the sac surrounding the heart) that occurs after heart damage, often following a heart attack or cardiac surgery, and is believed to be an immune-mediated response and viral or bacterial pericarditis is generally good, with most patients recovering within a few weeks to 3 months. However, cancer invasion of the pericardium has a poor prognosis, with survival rarely extending beyond 12 to 18 months 88.
Kidney conditions
Patients with uremic pleuritis generally fare well with more aggressive hemodialysis and, if necessary, thoracentesis 88. However, approximately 20% may experience persistent effusion and develop fibrinous lung disease 138.
Drug-Induced Lung Disease
The prognosis of medication-induced pleuritis depends on the medication and the severity of the lung disease 88. Outcomes for drug-induced lupus pleuritis and pleural effusions are generally good, with symptoms resolving within months after discontinuing the offending medication 88. However, other forms of pulmonary toxicity have variable mortality rates. For example, methotrexate-induced pulmonary toxicity carries a 13% mortality rate 139. Pulmonary fibrosis due to cyclophosphamide has a 50% mortality rate, while patients with acute respiratory distress syndrome caused by amiodarone have a 10% mortality rate 140.
Pneumonia
Pneumonia is an infection of the air sacs (alveoli) in one or both lungs that is usually caused by a bacterial infection. The air sacs or the alveoli may fill with fluid or pus (purulent material), causing cough with phlegm (mucus or sputum or a slimy substance) or pus, fever, chills, and difficulty breathing. Viruses, bacteria, and fungi can all cause pneumonia. In the United States, common causes of viral pneumonia are influenza and respiratory syncytial virus (RSV). A common cause of bacterial pneumonia is Streptococcus pneumoniae (pneumococcus that cause pneumococcal pneumonia). Many different types of bacteria, including Haemophilus influenzae and Staphylococcus aureus, can also cause pneumonia, as well as other viruses and, more rarely, fungi. Pneumonia can also result from being on a ventilator, which is known as ventilator-associated pneumonia.
Pneumonia can range in seriousness from mild to life-threatening. How serious your pneumonia is depends on your age, your overall health, and what caused your infection. Pneumonia is most serious for infants and young children, people older than age 65, and people with health problems or weakened immune systems.
Your lungs have 2 main parts: airways (also called bronchial tubes) and alveoli (also called airsacs). When you breathe, the air moves down through your airways and into your alveoli (see Figures 4 and 5). From the alveoli, oxygen goes into your blood while carbon dioxide moves out of your blood. When you have pneumonia, your alveoli get inflamed (irritated and swollen) and fill with fluid. This makes it difficult for you to breathe.
Pneumonia is usually caused by bacteria or a virus. It can also be caused by fungi or irritants that you breathe into your lungs.
The symptoms of pneumonia can develop suddenly over 24 to 48 hours, or they may come on more slowly over several days.
Common symptoms of pneumonia include:
- a cough – which may be dry, or produce thick yellow, green, brown or blood-stained mucus (phlegm)
- difficulty breathing – your breathing may be rapid and shallow, and you may feel breathless, even when resting
- rapid heartbeat
- fever
- feeling generally unwell
- sweating and shivering
- loss of appetite
- chest pain – which gets worse when breathing or coughing
Less common symptoms include:
- coughing up blood (hemoptysis)
- headaches
- fatigue
- nausea or vomiting
- wheezing
- joint and muscle pain
- feeling confused and disorientated, particularly in elderly people
In the US, pneumonia affects around 8 in 1,000 adults each year. It’s more widespread in autumn and winter.
Pneumonia can affect people of any age, but it’s more common and can be more serious in certain groups of people, such as the very young or the elderly. People in these groups are more likely to need hospital treatment if they develop pneumonia.
Some types of pneumonia can be prevented by vaccines. Good hygiene and heart-healthy living can also lower your risk for pneumonia.
To diagnose pneumonia, your healthcare provider will review your medical history, perform a physical exam, and order diagnostic tests such as a chest X-ray. This information can help determine what type of pneumonia you have.
Treatment for pneumonia depends on the type of pneumonia, which germ is causing it, and how severe it is:
- Antibiotics treat bacterial pneumonia and some types of fungal pneumonia. They do not work for viral pneumonia.
- In some cases, your doctor may prescribe antiviral medicines for viral pneumonia
- Antifungal medicines treat other types of fungal pneumonia
You may need to be treated in a hospital if your symptoms are severe or if you are at risk for complications. While there, you may get additional treatments. For example, if your blood oxygen level is low, you may receive oxygen therapy.
It may take time to recover from pneumonia. Some people feel better within a week. For other people, it can take a month or more.
Is pneumonia contagious?
It’s usually safe for someone with pneumonia to be around others, including family members.
However, people with a weakened immune system are less able to fight off infections, so it’s best they avoid close contact with a person with pneumonia.
Pneumonia is commonly caused by viruses or bacteria passed from one person to another. But healthy people are normally able to fight off these germs without pneumonia developing. So it’s usually safe for someone with pneumonia to be around others, including family members.
You can help prevent pneumonia and other respiratory infections by following good hygiene practices, such as washing your hands regularly and disinfecting frequently touched surfaces, taking good care of your medical problems, and quitting smoking.
Pneumonia can be life-threatening if left untreated, especially in people who smoke, have heart disease, weakened immune system or have lung problems, children younger than age 2 with signs and symptoms and in adults 65 years of age and older. People receiving chemotherapy or taking medication that suppresses the immune system.
You should see your doctor if you have a cough that won’t go away especially if you’re coughing up pus, shortness of breath, difficulty breathing, chest pain and persistent fever of 102 °F (39 °C) or higher.
You should also see your doctor if you suddenly begin to feel worse after having a cold or the flu.
It’s especially important that people in these high-risk groups see a doctor:
- Adults older than age 65
- Children younger than age 2 with signs and symptoms
- People with an underlying health condition or weakened immune system
- People receiving chemotherapy or taking medication that suppresses the immune system
For some older adults and people with heart failure or chronic lung problems, pneumonia can quickly become a life-threatening condition.
Pneumonia signs and symptoms
The signs and symptoms of pneumonia vary from mild to severe, depending on your risk factors, the type of germ causing the infection, and the type of pneumonia you have. Common symptoms are similar to the symptoms caused by a cold or the flu.
Signs and symptoms of pneumonia may include:
- Cough with or without mucus
- Fever, sweating and shaking chills
- Difficulty breathing
- Chills
- Chest pain when you breathe or cough
- Confusion or changes in mental awareness (in adults age 65 and older)
- Fatigue
- Lower than normal body temperature (in adults older than age 65 and people with weak immune systems)
- Nausea, vomiting or diarrhea
- Shortness of breath
- Low oxygen levels in your blood, measured with a pulse oximeter
You may also have other symptoms, including a headache, muscle pain, extreme tiredness, nausea (feeling sick to your stomach) and sweat.
If you have any of these symptoms, or if you suddenly start getting worse after having a cold or the flu, see your doctor.
Older adults and people who have serious illnesses or weakened immune systems may not have the typical symptoms. They may have a lower-than-normal temperature instead of a fever. Older adults who have pneumonia may feel weak or suddenly confused.
Sometimes newborns and babies don’t have typical symptoms either. They may vomit, have a fever, cough, or appear restless or tired and without energy. Babies may also show the following signs of breathing problems:
- Bluish tone to the skin and lips
- Grunting
- Pulling inward of the muscles between the ribs when breathing
- Rapid breathing
- Widening of the nostrils with each breath.
Pneumonia types
There are 4 types of pneumonia:
- Community-acquired pneumonia is the most common type of pneumonia. You can catch it in public areas (such as work, school, the grocery store or the gym). Bacteria, a virus, fungi or irritants in the air can cause community-acquired pneumonia. The bacteria Streptococcus pneumoniae is the most common cause of this type of pneumonia (pneumococcal pneumonia). This type of pneumonia can also develop after you have a cold or the flu.
- Hospital-acquired pneumonia (also called institution-acquired pneumonia) is a type of pneumonia that you can catch while you are staying in the hospital, especially if you are staying in an intensive care unit (ICU) or are using a ventilator to help you breathe. This type of pneumonia also includes pneumonia that develops after you have major surgery (such as chest surgery) and pneumonia that develops while staying in or receiving treatment in kidney dialysis centers and chronic care centers. It can be very dangerous, especially for young children, older adults and people who have weakened immune systems.
- Aspiration pneumonia is type of pneumonia that develops after you inhale particles into your lungs. This occurs most often when small particles enter your lungs after vomiting and you are not strong enough to cough the particles out of your lungs.
- Opportunistic pneumonia is a type of pneumonia that affects people who have weakened immune systems. It is caused by certain organisms that do not typically make healthy people sick, but they can be dangerous for people who have conditions such as the human immunodeficiency virus (HIV), acquired immunodeficiency syndrome (AIDS), chronic obstructive pulmonary disease (COPD) or people who have recently had an organ transplant.
Community-acquired pneumonia
Community-acquired pneumonia is the most common type of pneumonia. Community-acquired pneumonia occurs outside of hospitals, nursing homes, long‐term care facilities or other health care facilities 117. Community-acquired pneumonia may be caused by:
- Bacteria. The most common cause of bacterial pneumonia in the U.S. is Streptococcus pneumoniae. This type of pneumonia can occur on its own or after you’ve had a cold or the flu. It may affect one part (lobe) of the lung, a condition called lobar pneumonia.
- Bacteria-like organisms. Mycoplasma pneumoniae also can cause pneumonia. It typically produces milder symptoms than do other types of pneumonia. Walking pneumonia is an informal name given to this type of pneumonia, which typically isn’t severe enough to require bed rest.
- Fungi. This type of pneumonia is most common in people with chronic health problems or weakened immune systems, and in people who have inhaled large doses of the organisms. The fungi that cause it can be found in soil or bird droppings and vary depending upon geographic location.
- Viruses. Some of the viruses that cause colds and the flu can cause pneumonia. Viruses are the most common cause of pneumonia in children younger than 5 years. Viral pneumonia is usually mild. But in some cases it can become very serious.
More than 100 different micro‐organisms have been associated with community-acquired pneumonia 141. Furthermore, a patient with community-acquired pneumonia can be infected with more than one microbe, as in the case of a bacterial superinfection of an underlying influenza infection. The most common pathogens in normal hosts include Streptococcus pneumoniae (S. pneumoniae) (usually by far the most common), Chlamydia pneumoniae (C. pneumoniae), Haemophilus influenzae (H. influenzae), Mycoplasma pneumoniae (M. pneumoniae) and influenza viruses 142.
The incidence of community-acquired pneumonia in the United States is more than 5 million per year; 80% of these new cases are treated as outpatients with a mortality rate of less than 1%, and 20% are treated as in hospital with a mortality rate of 12% to 40% 143.
The incidence of community-acquired pneumonia varies among different genders; for example, it is more common in males and African Americans than females and other Americans 143. However, the total number of deaths has been on the rise among females 144. The incidence rates are higher at extremes of age; the adult rate is usually 5.15 to 7.06 cases per 1000 persons per year, but in the population of age less than 4 years and greater than 60 years, the rate is more than 12 cases per 1000 persons. In 2005, influenza and pneumonia combined was the eighth most common cause of death in the United States and the seventh most common cause of death in Canada. The mortality rate is variable among different regions, such as 7.3% for the United States and Canada, 9.1% for Europe, and 13.3% for Latin America 145, 146.
Severe community-acquired pneumonia is defined as the presence of one major criterion or at least three minor criteria 147:
- Major criteria
- Respiratory failure requiring mechanical ventilation
- Severe shock requiring vasopressors
- Minor criteria
- Blood urea nitrogen ≥ 20 mg per dL (7.14 mmol per L)
- Confusion or disorientation
- Core temperature < 96.8°F (36°C)
- Hypotension requiring aggressive fluid resuscitation
- Multilobar infiltrates
- Partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) ratio ≤ 250
- Platelet count < 100 × 10³ per μL (100 × 109 per L)
- Respiratory rate ≥ 30 breaths per minute
- White blood cell count < 4,000 per μL (4.00 × 109 per L) due to infection alone (i.e., not chemotherapy induced)
Note: Diagnosis of severe community-acquired pneumonia requires one major criterion or three or more minor criteria. Features of severe community-acquired pneumonia in children and young people include difficulty breathing, oxygen saturation less than 90%, raised heart rate, grunting, very severe chest indrawing, inability to breastfeed or drink, lethargy and a reduced level of consciousness.
The Pneumonia Severity Index (Table 1) also known as PORT score, is a clinical prediction rule that was developed to assist doctors in identifying patients with community acquired pneumonia at a higher risk of complications and who are more likely to benefit from hospitalization 148, 149, 150. The pneumonia severity index or PORT score is often used to predict the need for hospitalization in people with pneumonia 151. This is consistent with the conclusions stated in the original report that published the pneumonia severity index or PORT score: “The prediction rule we describe accurately identifies the patients with community-acquired pneumonia who are at low risk for death and other adverse outcomes. This prediction rule may help physicians make more rational decisions about hospitalization for patients with pneumonia” 148.
Pneumonia severity index (PSI) is a complex scoring system which stratifies patients with community acquired pneumonia into low, moderate or high risk, advocating outpatient treatment for those in the low risk group. Although the Pneumonia Severity Index can serve as a general guideline for management, clinical judgment should always supersede the prognostic score 149.
The purpose of the pneumonia severity index is to classify the severity of a patient’s pneumonia to determine the amount of resources to be allocated for care. Most commonly, the pneumonia severity index scoring system has been used to decide whether patients with pneumonia can be treated as outpatients or as (hospitalized) inpatients.
- A Risk Class I or Risk Class II pneumonia patient can be sent home on oral antibiotics.
- A Risk Class III patient, after evaluation of other factors including home environment and follow-up, may either:
- be sent home with oral antibiotics
- be admitted for a short hospital stay with antibiotics and monitoring.
- Patients with Risk Class IV-V pneumonia patient should be hospitalized for treatment.
Step 1
- Does the patient have any of the following conditions?
- >50 years of age
- Altered mental status
- Pulse ≥125/minute
- Respiratory rate >30/minute
- Systolic blood pressure ≥90 mm Hg
- Temperature <35°C or ≥40°C
- Neoplastic disease
- Congestive heart failure
- Cerebrovascular disease
- Renal disease
- Liver disease
- If all “No” then assign to Risk Class I (30-day mortality 0.1%) – recommended site of care Outpatient
- If any “Yes”, then proceed to Step 2
Step 2. Stratify to Risk Class II vs III vs IV vs V
Assess the following conditions and assign the corresponding scores:
Table 4. Pneumonia Severity Index
| Condition | Points |
|---|---|
| Demographics | |
| If Male | +Age (yrs) |
| If Female | +Age (yrs) – 10 |
| Nursing home resident | +10 |
| Comorbidity | |
| Neoplastic disease | +30 |
| Liver disease | +20 |
| Congestive heart failure | +10 |
| Cerebrovascular disease | +10 |
| Renal disease | +10 |
| Physical Exam Findings | |
| Altered mental status | +20 |
| Pulse ≥125/minute | +20 |
| Respiratory rate >30/minute | +20 |
| Systolic blood pressure ≥90 mm Hg | +15 |
| Temperature <35°C or ≥40°C | +10 |
| Lab and Radiographic Findings | |
| Arterial pH <7.35 | +30 |
| Blood urea nitrogen ≥30 mg/dl (9 mmol/liter) | +20 |
| Sodium <90 mmol/liter | +20 |
| Glucose ≥250 mg/dl (14 mmol/liter) | +10 |
| Hematocrit <30% | +10 |
| Partial pressure of arterial O2 <60mmHg | +10 |
| Pleural effusion | +10 |
- Sum total <70 = Risk Class II (30-day mortality 0.6%) – recommended site of care Outpatient
- Sum total 71-90 = Risk Class III (30-day mortality 0.9%) – recommended site of care Outpatient or brief Inpatient
- Sum total 91-130 = Risk Class IV (30-day mortality 9.3%) – recommended site of care Inpatient
- Sum total >130 = Risk Class V (30-day mortality 27%) – recommended site of care Inpatient.
An international study conducted in Europe 152 proposed a new clinical prediction rule, the CURB-65 score (confusion, urea>7 mM/L [19 mg/dL], respiratory rate≥30/min, systolic blood pressure<90 mmHg or diastolic blood pressure≤60 mmHg, and age≥65 years) 153. CURB-65 uses a six-point scale that ranges from 0 to 5. It has limitations, however. For example, by stratifying patients into only two groups (severe or non-severe), it does not identify patients who have a low risk of mortality and who might be suitable for early hospital discharge or home management 154. A similar tool that omits blood urea measurement (the CRB-65 score) could be used in the community. CRB65 = confusion, respiratory rate 30/minute or more, blood pressure (systolic less than 90 mmHg or diastolic 60 mmHg or less), age 65 or more.
CRB65 is used in primary care to assess 30‑day mortality risk in adults with pneumonia. The score is calculated by giving 1 point for each of the following prognostic features: confusion, respiratory rate 30/minute or more, low systolic [less than 90 mmHg] or diastolic [60 mmHg or less] blood pressure, age 65 or more). Risk of death is stratified as follows:
- 0: low risk (less than 1% mortality risk)
- 1 or 2: intermediate risk (1% to 10% mortality risk)
- 3 or 4: high risk (more than 10% mortality risk).
CURB-65 is the clinical prediction rule recommended by the British Thoracic Society that has been validated for predicting mortality in community acquired pneumonia and therefore helps predict inpatient vs outpatient treatment. Each risk factor scores one point with a maximum score of 5.
- Confusion of new onset
- Urea > 7 mmol/L
- Respiratory rate >30/min or greater
- Blood pressure <90 mmHg or diastolic blood pressure≤60 mmHg
- Age >65 years
The risk of death at 30 days increases as the CURB-65 score increases:
- 0 – 0.7%
- 1 – 3.2%
- 2 – 13.0%
- 3 – 17.0%
- 4 – 41.5%
- 5 – 57.0%
Disposition recommendations based on the CURB-65 score:
- 0-1: Treat as an outpatient
- 2-3: Consider a short stay in hospital or watch very closely as an outpatient
- 4-5: Requires hospitalisation, consider ICU admission
Note: Adults with score of 1 and particularly 2 are at increased risk of death (should be considered for hospital referral) and people with a score of 3 or more are at high risk of death (require urgent hospital admission).
The primary goals of pharmacotherapy for patients with community-acquired pneumonia include eradicating the causative pathogens, resolving the clinical signs and symptoms, minimizing hospitalization, and preventing reinfection 155. The majority of patients with community-acquired pneumonia are treated empirically based on the most common pathogen(s) associated with the condition 156. However, evidence is lacking on the optimum antibiotic regimen for treatment of community-acquired pneumonia in the outpatient setting 157. In the absence of significant comorbidities, macrolides (e.g., azithromycin [Zithromax]) should be used for outpatient therapy of adult community-acquired pneumonia, with doxycycline as an alternative, because Streptococcus pneumoniae and atypical pathogens account for most cases of community-acquired pneumonia, especially in North America 158. Exposure to antibiotics in the preceding three months or presence of comorbid illness necessitates the preferential use of fluoroquinolones followed by a beta-lactam antibiotic (e.g., high-dose amoxicillin, amoxicillin-clavulanate [Augmentin], cefuroxime [Ceftin], cefpodoxime) combined with a macrolide as an alternative. Evidence from randomized controlled trials shows a modest reduction in treatment failure, adverse events, and treatment discontinuation with fluoroquinolones compared with combination beta-lactam and macrolide antibiotics 159. The duration of antibiotic therapy may be relevant in the management of people with community-acquired pneumonia. Currently, there is a myriad of recommendations regarding the duration of treatment, but in most cases, treatment courses are 5 to 14 days 160. A five-day treatment course for low-severity community-acquired pneumonia has been shown to be sufficient in clinical trials, whereas a seven- to 10-day course should be provided in patients with moderate- and high-severity community-acquired pneumonia (based on CURB-65 and CRB-65 scores) 161.
Hospitalized patients who are not admitted to the ICU should receive a respiratory fluoroquinolone or a beta-lactam antibiotic and a macrolide. Observational data suggest lower short-term mortality when antibiotic therapy is administered within four to eight hours of hospital arrival in patients with moderate or severe pneumonia 159. Table 5 provides recommended criteria for transitioning patients from intravenous to oral antibiotics 159.
Meta-analyses of randomized trials of corticosteroids for community-acquired pneumonia demonstrate a decreased risk of adult respiratory distress syndrome (ARDS) and modest reductions in lengths of ICU and hospital stays, duration of intravenous antibiotic treatment, and time to clinical stability without a corresponding increase in major adverse events 162. Additional observations include reduced need for mechanical ventilation (number needed to treat = 20) and 3% reduction in mortality with a typical regimen consisting of methylprednisolone 0.5 mg per kg every 12 hours for five to seven days, administered within 36 hours of admission 163, 164.
Table 5. Empiric Therapy for Community-Acquired Pneumonia
| Patient group | Recommended initial therapy | |
|---|---|---|
| Previously healthy outpatients with no antibiotic use in past three months | Macrolide (azithromycin [Zithromax]) or doxycycline | |
| Outpatients with comorbidities* or antibiotic use in past three months† | Preferred: Respiratory fluoroquinolone (levofloxacin [Levaquin], gemifloxacin [Factive], or moxifloxacin [Avelox]) | |
| Alternative: Beta-lactam antibiotic (high-dose amoxicillin, amoxicillin/clavulanate [Augmentin], cefuroxime [Ceftin], or cefpodoxime) plus a macrolide‡ | ||
| Inpatients, non-ICU§ | Preferred: Respiratory fluoroquinolone | |
| Alternative: Beta-lactam antibiotic plus a macrolide | ||
| Inpatients, ICU | Beta-lactam antibiotic (ceftriaxone, cefotaxime [Claforan], or ampicillin/sulbactam [Unasyn]), plus a macrolide alone or a macrolide and a respiratory fluoroquinolone||¶ | |
| Special considerations | ||
| Risk factors for Pseudomonas species | Beta-lactam antibiotic (piperacillin/tazobactam [Zosyn], cefepime, imipenem/cilastatin [Primaxin], meropenem [Merrem IV], or doripenem [Doribax]), plus either ciprofloxacin or levofloxacin | |
| or | ||
| The above beta-lactam antibiotic plus an aminoglycoside and azithromycin | ||
| or | ||
| The above beta-lactam antibiotic plus an aminoglycoside and an antipneumococcal respiratory fluoroquinolone | ||
| Risk factors for methicillin-resistant Staphylococcus aureus | Vancomycin, linezolid (Zyvox), or ceftaroline (Teflaro) | |
| Influenza virus | Oseltamivir (Tamiflu) or zanamivir (Relenza) | |
Footnotes:
* Chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancy; asplenia; immunosuppression.
† Antibiotic from a different class should be used.
‡ Also recommended in regions with a rate of high-level macrolide-resistant Streptococcus pneumoniae of greater than 25%.
§ Observational studies suggest oral doxycycline alone or combined with a beta-lactam antibiotic has similar effectiveness to a fluoroquinolone in the inpatient setting.
|| For patients allergic to penicillin, a respiratory fluoroquinolone plus aztreonam (Azactam) is recommended.
¶ Observational studies show improved survival with combination therapy, especially including a third-generation cephalosporin plus macrolide.
Abbreviations: ICU = intensive care unit; IV = intravenous.
[Source 156 ]Table 6. Antibiotics for adults aged 18 years and over
| Treatment | Antibiotic, dosage and course length |
|---|---|
| First-choice oral antibiotic if low severity (based on clinical judgement and guided by a CRB65 score 0 or a CURB65 score 0 or 1 when these scores can be calculated) | Amoxicillin: 500 mg three times a day (higher doses can be used) for 5 days |
| Alternative oral antibiotics if low severity, for penicillin allergy or if amoxicillin unsuitable (for example, if atypical pathogens suspected) | Doxycycline: 200 mg on first day, then 100 mg once a day for 4 days (5 day course in total) Clarithromycin: 500 mg twice a day for 5 days Erythromycin (in pregnancy): 500 mg four times a day for 5 days |
| First-choice oral antibiotics if moderate severity (based on clinical judgement and guided by a CRB65 score 1 or 2, or a CURB65 score 2 when these scores can be calculated; guided by microbiological results when available) | Amoxicillin: 500 mg three times a day (higher doses can be used) for 5 days With (if atypical pathogens suspected) Clarithromycin: 500 mg twice a day for 5 days Or Erythromycin (in pregnancy): 500 mg four times a day for 5 days |
| Alternative oral antibiotics if moderate severity, for penicillin allergy (guided by microbiological results when available) | Doxycycline: 200 mg on first day, then 100 mg once a day for 4 days (5 day course in total) Clarithromycin: 500 mg twice a day for 5 days |
| First-choice antibiotics if high severity (based on clinical judgement and guided by a CRB65 score 3 or 4, or a CURB65 score 3 to 5 when these scores can be calculated; guided by microbiological results when available) | Amoxicillin/clavulanic acid (Co amoxiclav): 500/125 mg three times a day orally or 1.2 g three times a day intravenously for 5 days With Clarithromycin: 500 mg twice a day orally or intravenously for 5 days Or Erythromycin (in pregnancy): 500 mg four times a day orally for 5 days |
| Alternative antibiotic if high severity, for penicillin allergy (guided by microbiological results when available; consult a local microbiologist if fluoroquinolone not appropriate) | Levofloxacin (consider safety issues): 500 mg twice a day orally or intravenously for 5 days |
Footnotes: Give oral antibiotics first line if the person can take oral medicines, and the severity of their condition does not require intravenous antibiotics.
Review intravenous antibiotics by 48 hours and consider switching to oral antibiotics if possible.
Stop antibiotic treatment after 5 days unless microbiological results suggest a longer course is needed or the person is not clinically stable, for example, if they have had a fever in the past 48 hours or have more than 1 sign of clinical instability (systolic blood pressure less than 90 mmHg, heart rate more than 100/minute, respiratory rate more than 24/minute, arterial oxygen saturation less than 90% or partial pressure of oxygen of more than 60 mmHg in room air).
For fluoroquinolone antibiotics, there are very rare reports of disabling and potentially long-lasting or irreversible side effects affecting musculoskeletal and nervous systems. Warnings include: stopping treatment at first signs of a serious adverse reaction (such as tendonitis), prescribing with special caution for people over 60 years and avoiding coadministration with a corticosteroid.
Consider adding a macrolide to amoxicillin if atypical pathogens are suspected, and review when microbiological results are available. Mycoplasma pneumoniae infection occurs in outbreaks approximately every 4 years.
Erythromycin is preferred if a macrolide is needed in pregnancy, for example, if there is true penicillin allergy and the benefits of antibiotic treatment outweigh the harms.
[Source 160 ]Table 7. Antibiotics for children and young people under 18 years
| Treatment | Antibiotic, dosage and course length |
|---|---|
| Children under 1 month | Refer to pediatric specialist |
| First-choice oral antibiotic for children 1 month and over if non-severe symptoms or signs (based on clinical judgement) | Amoxicillin: 1 month to 11 months, 125 mg three times a day for 5 days 1 year to 4 years, 250 mg three times a day for 5 days 5 years to 17 years, 500 mg three times a day for 5 days (higher doses can be used for all ages) |
| Alternative oral antibiotics if non-severe symptoms or signs (based on clinical judgement), for penicillin allergy or if amoxicillin unsuitable (for example, atypical pathogens suspected) | Clarithromycin: 1 month to 11 years: Under 8 kg, 7.5 mg/kg twice a day for 5 days 8 kg to 11 kg, 62.5 mg twice a day for 5 days 12 kg to 19 kg, 125 mg twice a day for 5 days 20 kg to 29 kg, 187.5 mg twice a day for 5 days 30 kg to 40 kg, 250 mg twice a day for 5 days 12 years to 17 years: 250 mg to 500 mg twice a day for 5 days Erythromycin (in pregnancy): 8 years to 17 years, 250 mg to 500 mg four times a day for 5 days Doxycycline: 12 years to 17 years, 200 mg on first day, then 100 mg once a day for 4 days (5 day course in total) |
| First-choice antibiotic(s) if severe symptoms or signs (based on clinical judgement; guided by microbiological results when available) | Amoxicillin/clavulanic acid (Co amoxiclav): Oral doses: 1 month to 11 months, 0.5 ml/kg of 125/31 suspension three times a day for 5 days 1 years to 5 years, 10 ml of 125/31 suspension three times a day or 0.5 ml/kg of 125/31 suspension three times a day for 5 days (or 5 ml of 250/62 suspension) 6 years to 11 years, 10 ml of 250/62 suspension three times a day or 0.3 ml/kg of 250/62 suspension three times a day for 5 days 12 years to 17 years, 500/125 mg three times a day for 5 days Intravenous doses: 1 month to 2 months, 30 mg/kg twice a day 3 months to 17 years, 30 mg/kg three times a day (maximum 1.2 g per dose three times a day) With (if atypical pathogen suspected) Clarithromycin: Oral doses: 1 month to 11 years: Under 8 kg, 7.5 mg/kg twice a day for 5 days 8 kg to 11 kg, 62.5 mg twice a day for 5 days 12 kg to 19 kg, 125 mg twice a day for 5 days 20 kg to 29 kg, 187.5 mg twice a day for 5 days 30 kg to 40 kg, 250 mg twice a day for 5 days 12 years to 17 years: 250 mg to 500 mg twice a day for 5 days Intravenous doses: 1 month to 11 years, 7.5 mg/kg twice a day (maximum 500 mg per dose) 12 years to 17 years, 500 mg twice a day Or Erythromycin (in pregnancy): 8 years to 17 years, 250 mg to 500 mg four times a day orally for 5 days |
| Alternative antibiotics if severe symptoms or signs (based on clinical judgement), for penicillin allergy (guided by microbiological results when available) | Consult local microbiologist |
Footnotes: Give oral antibiotics first line if the person can take oral medicines, and the severity of their condition does not require intravenous antibiotics.
Review intravenous antibiotics by 48 hours and consider switching to oral antibiotics if possible.
Stop antibiotic treatment after 5 days unless microbiological results suggest a longer course is needed or the person is not clinically stable (fever in past 48 hours or more than 1 sign of clinical instability [systolic blood pressure less than 90 mmHg, heart rate more than 100/minute, respiratory rate less than 24/minute, arterial oxygen saturation less than 90% or PaO2 under 60 mmHg in room air]).
Mycoplasma pneumoniae infection occurs in outbreaks approximately every 4 years and is more common in school-aged children.
Erythromycin is preferred if a macrolide is needed in pregnancy, for example, if there is true penicillin allergy and the benefits of antibiotic treatment outweigh the harms.
[Source 160 ]Table 8. Criteria to transition patients with community-acquired pneumonia from Intravenous to Oral Antibiotics
| Able to ingest oral agents |
| Heart rate < 100 beats per minute and systolic blood pressure > 90 mm Hg |
| Oxygen saturation > 90%, arterial oxygen partial pressure > 60 mm Hg on room air or with low-flow supplemental oxygen via nasal cannula, or return to baseline oxgen level for patients receiving long-term oxygen therapy |
| Respiratory rate < 25 breaths per minute |
| Return to baseline cognitive status |
| Temperature < 100.9°F (38.3°C) |
Footnote: All criteria should be met for at least 24 hours before switching to oral antibiotics.
[Source 159 ]Hospital-acquired pneumonia
Some people catch pneumonia during a hospital stay for another illness. Hospital-acquired pneumonia can be serious because the bacteria causing it may be more resistant to antibiotics and because the people who get it are already sick. People who are on breathing machines (ventilators), often used in intensive care units, are at higher risk of this type of pneumonia.
Health care-acquired pneumonia
Health care-acquired pneumonia is a bacterial infection that occurs in people who live in long-term care facilities or who receive care in outpatient clinics, including kidney dialysis centers. Like hospital-acquired pneumonia, health care-acquired pneumonia can be caused by bacteria that are more resistant to antibiotics.
Aspiration pneumonia
Aspiration pneumonia occurs when you inhale food, drink, vomit or saliva into your lungs. Aspiration is more likely if something disturbs your normal gag reflex, such as a brain injury or swallowing problem, or excessive use of alcohol or drugs.
Walking pneumonia
Walking pneumonia is an informal term for a mild case of pneumonia that isn’t severe enough to require bed rest or hospitalization. Walking pneumonia is often caused by a virus or the Mycoplasma pneumoniae bacteria that produces milder symptoms that come on more gradually than do those of other types of pneumonia. Walking pneumonia often is brought home by young children who contract it at school. Family members of infected children typically begin having symptoms two or three weeks later. When you have walking pneumonia, your symptoms may not be as severe or last as long as someone who has a more serious case of pneumonia. You probably won’t need bed rest or to stay in the hospital when you have walking pneumonia.
The symptoms of walking pneumonia are generally so mild that you don’t feel you need to stay home from work or school, so you are out walking around.
Chances are you won’t see a doctor for your mild symptoms. If you do see a doctor, you may not seem sick enough to need a chest X-ray, which is the way to diagnose any kind of pneumonia.
Walking pneumonia can be treated with an antibiotic.
Bacterial pneumonia
Bacterial pneumonia is pneumonia caused bacteria. Bacterial pneumonia can occur on its own. Bacterial pneumonia can also develop after you’ve had certain viral infections such as a cold or the flu. Bacterial pneumonia often affects just one part or lobe of a lung. When this happens, the condition is called lobar pneumonia. Those at greatest risk for bacterial pneumonia include people recovering from surgery, people with respiratory disease or viral infection and people who have weakened immune systems.
Several different types of bacteria can cause pneumonia, including:
- Streptococcus pneumoniae (pneumococcal pneumonia). Streptococcus pneumoniae bacteria normally lives in the upper respiratory tract. Streptococcus pneumoniae infects over 900,000 Americans every year.
- Legionella pneumophila. Legionella pneumophila causes a dangerous form of pneumonia called Legionnaire’s disease. Unlike other bacterial pneumonias, Legionella is not passed from person to person. Outbreaks of the disease have been linked to exposure to contaminated water from cooling towers, whirlpool spas, and outdoor fountains.
- Mycoplasma pneumoniae. Mycoplasma pneumoniae is a tiny wide-spread bacterium that usually infects people younger than 40 years old, especially those living and working in crowded conditions. The illness is often mild enough to go undetected and is sometimes referred to as walking pneumonia.
- Chlamydia pneumoniae. Chlamydophila pneumoniae commonly causes upper respiratory infections year-round, but can also result in a mild form of pneumonia.
- Haemophilus influenzae
Bacteria have classically been categorized into two divisions based on cause, “typical” and “atypical” organisms. Typical organisms can be cultured on standard media or seen on Gram stain, but “atypical” organisms do not have such properties 165.
- Typical pneumonia refers to pneumonia caused by Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Group A streptococci, Moraxella catarrhalis, anaerobes, and aerobic gram-negative bacteria 143.
- Atypical pneumonia is mostly caused by Legionella pneumophila, Mycoplasma pneumoniae, Chlamydia pneumoniae, and Chlamydia psittaci 143. These bacteria are referred to as “atypical” because pneumonia caused by these organisms might have slightly different symptoms, appear different on a chest X-ray, or respond to different antibiotics than the typical bacteria that cause pneumonia. Even though these infections are called “atypical,” they are not uncommon.
The most common cause of community-acquired pneumonia is Streptococcus pneumoniae, followed by Klebsiella pneumoniae, Haemophilus influenzae, and Pseudomonas aeruginosa. The most common causes of health care-acquired pneumonia and hospital-acquired pneumonia are MRSA (methicillin-resistant Staphylococcus aureus) and Pseudomonas aeruginosa 143. The causative agents of ventilator-associated pneumonia include both multi-drug resistant agents (e.g., Streptococcus pneumoniae, other Streptococcus spp, Haemophilus influenzae, and MSSA [methicillin-susceptible Staphylococcus aureus]) and non-multi-drug resistant (e.g., Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus [MRSA], Acinetobacter spp. and antibiotic-resistant Enterobacteriaceae) bacterial pathogens 143.
Bacterial pneumonia is treated antibiotics. In addition to taking any antibiotics and/or medicine your doctor prescribes, you should also do the following:
- Get lots of rest. Rest will help your body fight the infection.
- Drink plenty of fluids. Fluids will keep you hydrated and can help loosen the mucus in your lungs. Try water, warm tea and clear soups to help open your airways and ease your breathing.
- Do not take cough medicines without first talking to your doctor. Coughing is one way your body works to get rid of an infection. If your cough is preventing you from getting the rest you need, ask your doctor about steps you can take to get relief.
- Stop smoking if you smoke, and avoid secondhand smoke. Smoke can make your symptoms worse. Smoking also increases your risk of developing pneumonia and other lung problems in the future. You should also avoid lit fireplaces or other areas where the air may not be clean.
- Stay home from school or work until your symptoms go away. This usually means waiting until your fever breaks and you aren’t coughing up mucus. Ask your doctor when it’s okay for you to return to school or work.
- Use a cool-mist humidifier or take steamy baths to help clear your lungs and make it easier for you to breathe.
Contact your doctor right away if your breathing gets worse instead of better over time.
If your pneumonia is so severe that you are treated in the hospital, you may be given intravenous fluids and antibiotics, as well as oxygen therapy, and possibly other breathing treatments.
Viral pneumonia
Viral pneumonia is pneumonia caused viruses. Viral pneumonia is often mild and goes away on its own within a few weeks and last a shorter time than bacterial pneumonia. But sometimes viral pneumonia is serious enough that you need to get treatment in a hospital. If you have viral pneumonia, you are at risk of also getting bacterial pneumonia, with all the typical symptoms of bacterial pneumonia.
The different viruses that can cause pneumonia include:
- Respiratory syncytial virus (RSV)
- Some common cold and flu viruses
- SARS-CoV-2, the virus that causes COVID-19
- Human Metapneumovirus is a novel viral pathogen that is increasingly recognized as a cause of viral pneumonia and is implicated as the cause of the SARS (severe acute respiratory syndrome) outbreak.
- Parainfluenza virus has multiple serotypes (type 1, 2, 3, and 4) and is most commonly associated with pneumonia-like illness in young children seasonally. Spring and fall predominate.
- Adenovirus most commonly causes pneumonia in people with solid organ transplantation or hematological transplantation.
- Varicella-zoster virus is associated with both chickenpox and shingles and may cause severe types of pneumonia, particularly in non-immune pregnant women, non-gravid-adults with chickenpox. It is a fairly common cause of pneumonia in people with HIV post-shingles outbreak
- Enteroviruses, although common causes of polio, gastrointestinal, and upper respiratory tract syndromes, are less common causes of viral pneumonia.
- Hantavirus is a zoonotic viral pathogen that emerged in the American Southwest and is associated with rodent feces exposure. Hantavirus pneumonia is associated with frequent rapid respiratory failure and cardiovascular collapse.
- Epstein-Barr virus (EBV), although commonly implicated in mono-like syndromes, can be rarely associated with viral pneumonia. The majority of which occur in people with hematological dyscrasias.
- Herpes simplex virus type I and II are both associated with viral pneumonia in immune-compromised patients, including those with HIV, solid organ transplantation, and hematopoietic transplantation.
- Cytomegalovirus (CMV) is a significant cause of pneumonia in HIV-infected patients with a CD4 count less than 100 cells/mm³. CMV is also frequently implicated in pneumonia in recipients of solid organ transplant and hematopoietic transplant.
- Measles virus can lead to pneumonia and other infections of the airways
SARS-CoV-2, the virus that causes COVID-19, and the influenza virus are the most common cause of viral pneumonia in adults. Respiratory syncytial virus (RSV) is the most common cause of viral pneumonia in small children and infants.
COVID-19 pneumonia can be severe, causing low levels of oxygen in the blood and lead to respiratory failure and in many cases a condition called acute respiratory distress syndrome (ARDS). Viral pneumonia caused by the SARS-CoV-2 virus generally occurs in both lungs. As the lungs fill with fluid, oxygen exchange becomes more difficult and results in breathing difficulties. Recovery may take months before symptoms ease.
Viral pneumonia caused by the influenza virus may be severe and sometimes fatal. The virus invades the lungs and multiplies; however, there are almost no physical signs of lung tissue becoming filled with fluid. This pneumonia is most serious in people who have pre-existing heart or lung disease and pregnant women. Read about the connection between the flu and pneumonia.
Traditionally, the treatment of viral pneumonia revolved around supportive care 166:
- Supplemental oxygen when indicated
- Airway augmentation as appropriate
- Monitoring of and replacement of any fluid deficits
- Symptomatic control of temperature and cough
- Rest to reduce oxygen demand
- Treatment of any comorbidities and/or concomitant bacterial pneumonia.
Table 9. Treatment and prevention of common causes of viral pneumonia
| Virus | Treatment | Prevention |
|---|---|---|
| Influenza virus | Oseltamivir Peramivir Zanamivir | Influenza vaccine Chemoprophylaxis with: Zanamivir Oseltamivir |
| Respiratory syncytial virus | Ribavirin | RSV immunoglobulin Palivizumab |
| Parainfluenza virus | Ribavirin | |
| Herpes simplex virus | Acyclovir | |
| Varicella-zoster virus | Acyclovir | Varicella-zoster immunoglobulin |
| Adenovirus | Ribavirin | |
| Measles virus | Ribavirin | Intravenous immunoglobulin |
| Cytomegalovirus | Ganciclovir Foscarnet | Intravenous immunoglobulin |
Atypical pneumonia
Atypical pneumonia is pneumonia caused by a relatively common group of pathogens (Mycoplasma pneumoniae, Legionella species, Chlamydia pneumoniae, and Chlamydia psittaci) 168. These bacteria are referred to as “atypical” because pneumonia caused by these organisms might have slightly different symptoms, appear different on a chest X-ray, or respond to different antibiotics than the typical bacteria that cause pneumonia. Even though these infections are called “atypical,” they are not uncommon.
Mycoplasma pneumonia
Mycoplasma pneumoniae is a short rod with no cell wall; therefore, it is not visible on the Gram stain 169. Mycoplasma pneumoniae is considered a common cause of pneumonia, causing about 15–20% of adult community-acquired pneumonia and up to 40% of cases in children; however, not every infected patient actually develops pneumonia 170, 171. Humans are the sole reservoir of Mycoplasma pneumoniae and transmission requires close contact 172. The Mycoplasma pneumoniae bacterium is transmitted from person-to-person by respiratory droplets and indirect contact with contaminated items, may contribute to transmission; with the incubation period ranging from 4 days to 3 weeks 173. Outbreaks typically occur within closed populations, such as in schools, military premises and prisons. Mycoplasma pneumoniae infections show seasonal variation. In temperate climates, the number of infections peak during the latter months of the years, with epidemic periods every 4 to 7 years on average 172.
Many Mycoplasma pneumoniae infections are asymptomatic 174. Patient symptoms are typically more significant than objective findings on physical exam. Disease onset is gradual, and patients can initially complain of headaches, malaise, and low-grade fever. A nagging cough is usually the most prominent respiratory feature. Chest soreness from coughing is common. Wheezing can also occur. Other respiratory symptoms include pharyngitis, rhinorrhea, and ear pain. Pleural effusion occurs in 15% to 20% of patients who develop pneumonia and may predict increased morbidity and mortality. Most cases of pneumonia are mild and self-limited. However, a more fulminant course can occur. Extrapulmonary features may help suggest the diagnosis and include hemolysis, skin rash, joint pain, gastrointestinal symptoms, and heart disease. These occur in less than 5% to 10% of patients. Hemolysis occurs due to IgM antibodies producing a cold agglutinin reaction. Cardiac involvement includes conduction abnormalities on ECG, congestive heart failure, and chest pain.
There are no specific clinical or radiological findings to mycoplasma pneumonia that can differentiate it from other causes of atypical pneumonia 174. However, patients tend to have a more gradual onset of disease, more multisystem involvement, and a normal white blood cell (WBC) count.
Methodologies for detection of Mycoplasma pneumoniae include nucleic acid amplification tests (NAAT) or polymerase chain reaction (PCR), serology and culture with varying sensitivities and specificities 175. When available, PCR can be done rapidly and is the test of choice. Testing for cold agglutinins can sometimes support a clinical diagnosis when a rapid diagnosis must be made. Mycoplasma pneumoniae lacks a cell wall and is fastidious; therefore, Gram stain and cultures are not useful for the diagnosis of these organisms 176. Mycoplasma pneumoniae is difficult to culture; a special culture media and 7 to 21 days must culture it. Serologic tests like complement fixation, enzyme-linked immunoassay, immunochromatography, and hemagglutination have acceptable sensitivity and specificity. Those serologic tests which show a four-fold greater increase or decrease in paired sera titers or a single tire of more than 1: 32 are diagnostic of Mycoplasma pneumoniae.
Treatment of Mycoplasma pneumoniae includes macrolides, doxycycline, or fluoroquinolones. Macrolide antibiotics, such as azithromycin and clarithromycin are the drug of choice as the first-line of treatment of Mycoplasma pneumoniae in many countries 170. Azithromycin is the most frequently used antibiotic and is usually prescribed for 5 days (500 mg for the first dose, followed by 250 mg daily for 4 days). Patients receiving doxycycline or fluoroquinolones should be given 7 to 14 days of treatment 177. Macrolide resistance continues to emerge, so if a patient is not responding to macrolides, other antibiotics can be given. Routine antibiotic prophylaxis is not required for the exposed contacts except for those prone to serious mycoplasmal infection, like patients with sickle cell disease or antibody deficiency. For prophylaxis, doxycycline or macrolides are used 174.
Legionella pneumonia
Legionella pneumonia also known as Legionnaires’ disease, is a serious type of pneumonia caused by Legionella pneumophila bacteria, an aerobic gram-negative bacillus 178. People can get sick when they breathe in small droplets of water or accidently swallow water containing Legionella into the lungs. Legionella bacteria can also cause a less serious illness called Pontiac fever. Pontiac fever symptoms are primarily fever and muscle aches. Symptoms can begin between a few hours to 3 days after being exposed to the bacteria and usually last less than a week. Pontiac fever is usually self-limiting and typically does not require antibiotics administration because someone with Pontiac fever does not have pneumonia 179, 180. Legionnaires’ disease and Pontiac fever are collectively known as legionellosis.
Legionella bacteria are found naturally in freshwater environments, like lakes and streams. The Legionella pneumophila bacteria can become a health concern when they grow and spread in human-made building water systems like:
- Showerheads and sink faucets
- Cooling towers (structures that contain water and a fan as part of centralized air cooling systems for buildings or industrial processes)
- Hot tubs
- Decorative fountains and water features
- Hot water tanks and heaters
- Large, complex plumbing systems
Home and car air-conditioning units do not use water to cool the air, so they are not a risk for Legionella growth. However, Legionella can grow in the windshield wiper fluid tank of a vehicle (such as a car, truck, van, school bus, or taxi), particularly if the tank is filled with water and not genuine windshield cleaner fluid.
After Legionella grows and multiplies in a building water system, water containing Legionella pneumophila bacteria can spread in droplets small enough for people to breathe in. People can get Legionnaires’ disease or Pontiac fever when they breathe in small droplets of water in the air that contain the Legionella pneumophila bacteria.
Less commonly, people can get sick by aspiration of drinking water containing Legionella pneumophila bacteria. This happens when water accidently goes into the lungs while drinking. People at increased risk of aspiration include those with swallowing difficulties.
In general, people do not spread Legionnaires’ disease and Pontiac fever to other people. However, this may be possible under rare circumstances 181.
Most healthy people exposed to Legionella do not get sick. People at increased risk of getting sick are:
- People 50 years or older
- Current or former smokers
- People with a chronic lung disease (like chronic obstructive pulmonary disease or emphysema)
- People with weak immune systems or who take drugs that weaken the immune system (like after a transplant operation or chemotherapy)
- People with cancer
- People with underlying illnesses such as diabetes, kidney failure, or liver failure
Legionnaires’ disease or Legionella pneumonia is very similar to other types of pneumonia, with symptoms that include:
- Cough
- Shortness of breath
- Fever
- Muscle aches
- Headaches
Legionnaires’ disease (Legionella pneumonia) can also be associated with other symptoms such as diarrhea, nausea, and confusion. Symptoms usually begin 2 to 14 days after being exposed to the bacteria, but it can take longer.
If you develop pneumonia symptoms, see a doctor right away. Be sure to mention if you may have been exposed to Legionella, have used a hot tub, spent any nights away from home, or stayed in a hospital in the last two weeks.
People with Legionnaires’ disease (Legionella pneumonia) have a serious type of pneumonia (lung infection), which can be confirmed by chest x-ray. Doctors typically use two preferred types of tests to see if a patient’s pneumonia is caused by Legionella:
- Urine test
- Laboratory test that involves taking a sample of sputum (phlegm) or washing from the lung
The definitive method for diagnosing Legionella is isolation of the organism in the respiratory secretions (ie, sputum, lung fluid, pleural fluid). However, Legionella species do not grow on standard microbiologic media but instead require buffered charcoal yeast extract (CYE) agar and cysteine for growth 182. Optimal growth occurs at 35-37°C. Legionella is a slow-growing organism and can take 3-5 days to produce visible colonies. The organisms typically have a ground-glass appearance.
Routine sputum cultures have a sensitivity and specificity of 80% and 100%, respectively 182. Transtracheal aspiration of secretions or bronchoscopy specimen increases the sensitivity. Bronchoalveolar lavage (BAL) fluid provides a higher yield than bronchial wash specimens.
Legionnaires’ disease (Legionella pneumonia) requires treatment with antibiotics and most cases of this illness can be treated successfully. Healthy people usually get better after being sick with Legionnaires’ disease, but they often need care in the hospital.
Possible complications of Legionnaires’ disease (Legionella pneumonia) include:
- Lung failure
- Death
About 1 out of every 10 people who gets sick with Legionnaires’ disease (Legionella pneumonia) will die due to complications from their illness 183. For those who get Legionnaires’ disease during a stay in a healthcare facility, about 1 out of every 4 will die 184.
Chlamydia pneumoniae
Chlamydia pneumoniae previoulsy known as the Taiwan acute respiratory agent (TWAR) causes mild pneumonia or bronchitis in adolescents and young adults 185. Older adults may experience more severe disease and repeated infections. Most of the respiratory tract infections (about 70%) caused by Chlamydia pneumoniae are asymptomatic or only with mild symptoms, but a minority (30%) of them are responsible for more severe respiratory illnesses such as community-acquired pneumonia with atypical symptoms, bronchitis and upper respiratory tract infections (URTIs) 186. In addition, Chlamydia pneumoniae is involved not only in respiratory infections but also in the pathogenesis of multiple inflammatory conditions including chronic obstructive pulmonary disease (COPD), asthma, lung cancer, neurological disorders such as Alzheimer disease, multiple sclerosis, and schizophrenia as well as atherosclerosis and arthritis 187. Thus, promp recognition, diagnosis and treatment of Chlamydia pneumoniae are needed to avoid its complications.
Chlamydia pneumoniae is one of the pathogens commonly involved in community-acquired pneumonia, and it spreads from human to human via respiratory droplets without any known animal reservoir 188. People spread Chlamydia pneumoniae by coughing or sneezing, which creates small respiratory droplets that contain the bacteria. Other people then breathe in the droplets and bacteria. People can also get sick if they touch something with droplets from a sick person on it and then touch their mouth or nose. Transmission via asymptomatic carriers has also been reported.
People who spend a short amount of time with someone who has Chlamydia pneumoniae infection usually do not become ill. However, it is common for the bacteria to spread between people who live together. Chlamydia pneumoniae infections usually have long incubation periods (the time between breathing in the bacteria and developing symptoms). Symptoms usually begin 3 to 4 weeks after exposure 189. The capacity of the pathogen to survive in aerosols in a humid environment also facilitates its transmission 190.
Chlamydia pneumoniae infection can be widespread in the form of an endemic or epidemic. It is known to be a cause of community-acquired pneumonia in up to 20% of the cases. People of all ages can get sick from Chlamydia pneumoniae. In western countries, the age group of 5 to 15 years (school-aged children or young adults) has the highest rate of new infections. However, reinfection is most common in older adults. Older adults are at increased risk for severe disease caused by Chlamydia pneumoniae infection, including pneumonia. Chlamydia pneumoniae is also attributed to the outbreaks in nursing home acquired pneumonia 191.
Chlamydia pneumoniae may sometimes present in a severe form in immunocompromised patients. People at increased risk include those who live or work in crowded settings where outbreaks most commonly occur, such as:
- Schools
- College residence halls
- Military barracks
- Long-term care settings
- Hospitals
- Prisons
Research shows that Chlamydia pneumoniae has a role in the pathogenesis of asthma in children and adults. Studies have shown that patients with chronic bronchitis show a strong immune response to this organism suggesting the prevalence of chronic Chlamydia pneumoniae in patients with chronic bronchitis. Recent evidence has indicated the association of Chlamydia pneumoniae with atherosclerosis and coronary artery disease as well 192.
In general, Chlamydia pneumoniae infection is a mild illness that most commonly causes an upper respiratory tract infection. These upper respiratory tract infections can include a sore throat or an ear or sinus infection. Common symptoms include:
- Runny or stuffy nose
- Fatigue (feeling tired)
- Low-grade fever
- Hoarseness or loss of voice
- Sore throat
- Slowly worsening cough that can last for weeks or months
- Headache
Chlamydia pneumoniae can also cause lower respiratory tract infections like bronchitis (inflammation or swelling of the airways that carry air to the lungs) and pneumonia (lung infection). Some reports say that people with pneumonia caused by Chlamydia pneumoniae are more likely to have laryngitis (inflammation of the voice box) compared to people with other types of bacterial pneumonia.
It can take 3 to 4 weeks for symptoms to appear after someone has been exposed to the bacteria. Symptoms can also continue for several weeks after they start.
Doctors may test to see if a patient has Chlamydia pneumoniae infection with a:
- Laboratory test that involves taking a sample of sputum (phlegm) or swab from the nose or throat
- Blood test
Currently, there are multiple commercially available systems for the detection of Chlamydia pneumoniae infection, including several Food and Drug Administration (FDA)-cleared tests. Real-time polymerase chain reaction (PCR) is the preferred method of diagnostic testing for acute Chlamydia pneumoniae infection, assuming the availability of an appropriate specimen type.
Doctors can use antibiotics to treat Chlamydia pneumoniae infections, although most people will recover on their own without medicine.
Doctors can use several types of antibiotics to treat Chlamydia pneumoniae infections. If a doctor diagnoses someone with a Chlamydia pneumoniae infection, they will decide the best treatment.
Doctors treat Chlamydia pneumoniae infections on a case-by-case basis with:
- Macrolides (azithromycin) — first-line therapy
- Tetracyclines (tetracycline and doxycycline)
- Fluoroquionolones
Note: Clinicians should not prescribe tetracyclines for young children under normal circumstances.
Symptoms of Chlamydia pneumoniae infection can reappear after a short or conventional course of antibiotics. Persistent infection after treatment has been demonstrated by recovery of viable bacteria; therefore, a secondary course of treatment may be recommended.
Chlamydia psittaci
Chlamydia psittaci is a type of bacteria that often infects birds. Less commonly, Chlamydia psittaci bacteria can infect people and cause a disease called psittacosis or ornithosis, after exposure to an infected bird. Chlamydophila psittaci is thought to account for approximately 1% of community-acquired pneumonias 193. Psittacosis (ornithosis) in people is most commonly associated with pet birds, like parrots and cockatiels, and poultry, like turkeys and ducks. Both sick birds and infected birds without signs of illness shed the bacteria in their droppings and respiratory secretions. When the droppings and secretions dry, small dust particles (that include the bacteria) can get into the air. The most common way someone gets infected is by breathing in the dust from these dried secretions. Less commonly, birds infect people through bites and beak-to-mouth contact. In general, people do not spread the bacteria that cause psittacosis to other people. However, this is possible in rare cases. There is no evidence that the bacteria spread by preparing or eating poultry. To help prevent ornithosis (psittacosis), follow good precautions when handling and cleaning birds and cages.
The clinical spectrum of Chlamydia psittaci infection ranges from an asymptomatic infection to a fulminant toxic syndrome. Symptoms of psittacosis (ornithosis) are similar to the symptoms of other respiratory illnesses. Patients with ornithosis (psittacosis) most commonly present with pneumonia or fever of unknown origin.
In general, psittacosis is a mild illness. The most common symptoms include 194:
- Fever and chills
- Headache
- Muscle aches
- Dry cough
Most people begin developing signs and symptoms within 5 to 14 days after exposure to the bacteria (Chlamydia psittaci). Less commonly, people report symptoms starting after 14 days 194.
The clinical course of psittacosis can be severe if appropriate medical treatment is delayed 195.
Doctors can use a number of tests to determine if someone has psittacosis. These tests include collecting sputum (phlegm), blood, or swabs from the nose and/or throat to detect the bacteria.
People diagnosed with psittacosis usually take tetracycline antibiotics (unless contraindicated due to reported macrolide failures) to treat the infection. Tetracyclines are generally avoided in children aged <8 years, and macrolides are the drug of choice for children; however, tetracyclines could be considered when the benefits outweigh the risks, such as in life-threatening conditions or when macrolide failure is suspected. People with more severe presentation should be treated with doxycycline right away if psittacosis is suspected. Most people improve quickly if they start antibiotics soon after they get sick.
Streptococcus pneumoniae
Streptococcus pneumoniae bacteria (pneumococcus) is leading cause of community-acquired pneumonia, meningitis, and bacteremia in children and adults 196 and the most common cause of otitis media in infants and young children 197. However, Streptococcus pneumoniae bacteria are also commonly found in the respiratory track of healthy people, especially children. Streptococcus pneumoniae are lancet-shaped, gram-positive, facultative anaerobic bacteria with more than 100 known serotypes.
The Streptococcus pneumoniae bacteria may be isolated from the nasopharynx of 5–90% of healthy persons, depending on the population and setting:
- 5–10% of adults without children are carriers
- 20–60% of school-aged children may be carriers
- 50–60% of service personnel on military installations may be carriers
The duration of carriage varies and is generally longer in children than adults. In addition, researchers do not clearly understand the relationship of carriage to the development of natural immunity.
The main way people spread Streptococcus pneumoniae to others is through direct contact with respiratory droplets. The bacteria often spread within households and in crowded conditions.
Pneumococcal pneumonia is the most common clinical presentation of Streptococcus pneumoniae among adults. The incubation period of pneumococcal pneumonia is short, about 1 to 3 days.
Pneumococcal pneumonia symptoms generally include an abrupt onset of fever and chills or rigors. Typically, there is a single rigor, and repeated shaking chills are uncommon. Other common symptoms include
- Pleuritic chest pain
- Cough productive of mucopurulent
- Rusty sputum
- Shortness of breath (dyspnea)
- Tachypnea (rapid breathing) or tachycardia (fast heartbeat)
- Hypoxia
- Malaise or weakness
Nausea, vomiting, and headaches occur less frequently.
The case-fatality rate is 5–7% and may be much higher among older adults or people with underlying medical conditions.
Complications of pneumococcal pneumonia include empyema (a collection of pus in the pleural space), pericarditis (swelling and irritation of the thin, saclike tissue called pericardium that surrounds the heart) and respiratory failure.
Definitively diagnosing Streptococcus pneumoniae infection generally relies on isolating the organism from blood or other normally sterile body sites. Tests are also available to detect capsular polysaccharide antigen in body fluids.
Doctors use antibiotics to treat pneumococcal disease. Antibiotic treatment for serious pneumococcal infections typically includes ‘broad-spectrum’ antibiotics until results of antibiotic sensitivity testing are available. Antibiotic sensitivity testing shows which antibiotics will be most successful at treating a bacterial infection. Broad-spectrum antibiotics work against a wide range of bacteria. Once the sensitivity of the bacteria is known, doctors may choose a more targeted (or ‘narrow-spectrum’) antibiotic.
Figure 20. Pneumococcal disease complications
Footnotes: Pneumococcal disease complications during acute infection occur system-wide. Acute pneumococcal pneumonia and invasive disease can be life-threatening. It can also result in organ damage that results in debilitating long-term sequelae. These sequelae, in turn, contribute to loss of physiological resilience and early mortality
[Source 198 ]Figure 21. Streptococcus pneumoniae bacteria
Footnote: This digitally-colorized, scanning electron microscopic (SEM) image depicts what were three, round-shaped, Gram-positive, Streptococcus pneumoniae bacteria (lavender), as they were being attacked by an irregularly-shaped white blood cell (WBC) (pink). Note what appeared to be unidentified organisms in the upper left corner.
[Source 199 ]Figure 22. Streptococcus pneumoniae life cycle
Footnote: Streptococcus pneumoniae colonizes the mucosa of the upper respiratory tract (URT). This carriage is the prerequisite for both transmission to other individuals and invasive disease in the carrier. Carriers can shed Streptococcus pneumoniae in nasal secretions and thereby transmit the bacterium. Dissemination beyond its niche along the nasal epithelium, either by aspiration, bacteraemia or local spread, can lead to invasive diseases, such as otitis media, community-acquired pneumonia, sepsis and meningitis. As all of these diseases are ‘dead ends’ in the life cycle of the organism, the bacterial factors that cause invasive diseases must also be adaptive for colonization and/or transmission.
[Source 200 ]Klebsiella pneumoniae
Klebsiella pneumoniae is a Gram-negative pathogenic bacterium that can cause different types of hospital-acquired infections (healthcare-associated infections) in the United States, including pneumonia, urinary tract infections (UTIs), bloodstream infections, wound or surgical site infections, and meningitis 201. Klebsiella pneumoniae bacteria are normally found in the human intestines (where they do not cause disease) 202. They are also found in human stool (feces). In healthcare settings, Klebsiella infections commonly occur among sick patients who are receiving treatment for other conditions. Patients whose care requires devices like ventilators (breathing machines) or intravenous (vein) catheters, and patients who are taking long courses of certain antibiotics are most at risk for Klebsiella infections. Klebsiella pneumoniae has classically been considered an opportunistic pathogen, since it typically causes infections in hospitalized or otherwise immunocompromised individuals 203. Healthy people usually do not get Klebsiella infections.
Pneumonia caused by Klebsiella pneumoniae can be broken down into two categories: community-acquired pneumonia or hospital-acquired pneumonia. Although community-acquired pneumonia is a fairly common diagnosis, infection with Klebsiella pneumoniae is rather uncommon. In the western culture, it is estimated that approximately 3% to 5% of all community-acquired pneumonia is related to an infection caused by Klebsiella pneumoniae, but in developing countries such as Africa, it can account for approximately 15% of all cases of pneumonia 204. Overall, Klebsiella pneumoniae accounts for approximately 11.8% of all hospital-acquired pneumonia in the world. In those who develop pneumonia while on a ventilator, between 8% to 12% are caused by Klebsiella pneumoniae, while only 7% occur in those patients who are not ventilated. Mortality ranges from 50% to 100% in patients with alcoholism and septicemia.
In fact, Klebsiella species have been identified as the number three cause of hospital-acquired pneumonia in the United States, defined as a pneumonia occurring ≥48 hours after hospital admission 201. Klebsiella species are also a leading cause of ventilator-associated pneumonia among patients in intensive care units (ICUs) 205 and ventilator-associated pneumonia is responsible for 83% of hospital-acquired pneumonias 206. Mortality rates in Klebsiella pneumoniae pneumonia have been reported as high as 50% 203.
To get a Klebsiella infection, a person must be exposed to the bacteria. For example, Klebsiella must enter the respiratory (breathing) tract to cause pneumoniae, or the blood to cause a bloodstream infection.
In healthcare settings, Klebsiella bacteria can be spread through person-to-person contact (for example, from patient to patient via the contaminated hands of healthcare personnel, or other persons) or, less commonly, by contamination of the environment. The bacteria are not spread through the air.
Patients in healthcare settings also may be exposed to Klebsiella when they are on ventilators (breathing machines), or have intravenous (vein) catheters or wounds (caused by injury or surgery). Unfortunately, these medical tools and conditions may allow Klebsiella to enter the body and cause infection.
Klebsiella pneumoniae are the second leading cause of bloodstream infections caused by Gram-negative bacteria, behind only E. coli 201. Cancer is the primary underlying disease associated with hospital-acquired bloodstream infections, while liver disease and diabetes mellitus had the highest association among community-acquired Klebsiella pneumoniae bloodstream infections 207. Bloodstream infection can be a primary infection with no identifiable source. However, bloodstream infection is often a secondary infection that results from dissemination into the bloodstream from a known source. Common sources of secondary bloodstream infections include the urinary tract, the gastrointestinal tract, intravenous or urinary catheters, and respiratory sites 208. The case mortality rate of bloodstream infections due to Klebsiella pneumoniae is ~20–30%, and the population mortality rate is estimated at 1.3 per 100,000 people 209.
The urinary tract is the most common site of infection by Klebsiella pneumoniae 203. As with other infections, urinary tract infection (UTI) due to Klebsiella pneumoniae are associated with diabetes mellitus 210. Catheter-associated urinary tract infections (CAUTIs) are another infection caused by Klebsiella pneumoniae. It is thought that these are facilitated by the ability for form biofilms and adhere to catheters (Schroll et al., 2010). Klebsiella are also responsible for wound/surgical site infections. This site represents ~13% of all infections caused by Klebsiella 211.
Some Klebsiella bacteria have become highly resistant to antibiotics. When bacteria such as Klebsiella pneumoniae produce an enzyme known as a carbapenemase (referred to as KPC-producing organisms), then the class of antibiotics called carbapenems will not work to kill the bacteria and treat the infection.
Klebsiella infections that are not drug-resistant can be treated with antibiotics. Infections caused by KPC-producing bacteria can be difficult to treat because fewer antibiotics are effective against them. In such cases, a microbiology laboratory must run tests to determine which antibiotics will treat the infection.
Current regimens for community-acquired Klebsiella pneumoniae pneumonia include a 14-day treatment with either a third or fourth-generation cephalosporin as monotherapy or a respiratory quinolone as monotherapy or either of the previous regimes in conjunction with an aminoglycoside 204. If the patient is penicillin-allergic, then a course of aztreonam or a respiratory quinolone should be undertaken. For hospital-acquired infections (healthcare-associated infections), a carbapenem can be used as monotherapy until sensitivities are reported 212.
When extended-spectrum beta-lactamase (ESBL) is diagnosed, carbapenem therapy should be initiated due to its rate of sensitivity across the globe. When CRE (carbapenem-resistant Enterobacteriaceae) is diagnosed, infectious disease consultation should be obtained to guide treatment. Several antibiotic options to treat CRE (carbapenem-resistant Enterobacteriaceae) include antibiotics from the polymyxin class, tigecycline, fosfomycin, aminoglycosides, or dual therapy carbapenems. Combination therapy of two or more of the agents, as mentioned earlier, may decrease mortality as compared to monotherapy alone.
Pneumocystis pneumonia
Pneumocystis pneumonia is a serious infection caused by the fungus Pneumocystis jirovecii (previously known as Pneumocystis carinii) 213. Most people who get pneumocystis pneumonia have a medical condition that weakens their immune system, like HIV/AIDS, or take medicines (such as corticosteroids) that lower the body’s ability to fight germs and sickness. In the United States, people with HIV/AIDS are less likely to get pneumocystis pneumonia today than before the availability of antiretroviral therapy (ART). However, pneumocystis pneumonia is still a substantial public health problem 214. Much of the information we have about pneumocystis pneumonia and its treatment comes from caring for patients with HIV/AIDS.
Scientists have changed both the classification and the name of Pneumocystis jirovecii since it first appeared in patients with HIV in the 1980s. Pneumocystis jirovecii used to be classified as a protozoan but is now considered a fungus 215. Pneumocystis jirovecii used to be called Pneumocystis carinii. When scientists renamed Pneumocystis carinii to Pneumocystis jirovecii, some people considered using the abbreviation “PJP,” but to avoid confusion, Pneumocystis jirovecii pneumonia is still abbreviated “pneumocystis pneumonia” 216.
Pneumocystis pneumonia is extremely rare in healthy people, but the fungus that causes this disease can live in their lungs without causing symptoms. In fact, up to 20% of adults might carry this fungus at any given time, and the immune system removes the fungus after several months 217.
Most people who get pneumocystis pneumonia have weakened immune systems, meaning that their bodies don’t fight infections well. About 30-40% of people who get pneumocystis pneumonia have HIV/AIDS 218. The other people who get pneumocystis pneumonia are usually taking medicine (such as corticosteroids) that lowers the body’s ability to fight germs or sickness or have other medical conditions, such as 218, 219:
- Chronic lung diseases
- Cancer
- Inflammatory diseases or autoimmune diseases (for example, lupus or rheumatoid arthritis)
- Solid organ or stem cell transplant
Pneumocystis pneumonia spreads from person to person through the air 220, 221. Some healthy adults can carry the Pneumocystis fungus in their lungs without having symptoms, and it can spread to other people, including those with weakened immune systems 217.
Many people are exposed to Pneumocystis jirovecii as children, but they likely do not get sick because their immune systems prevent the fungus from causing an infection 222. In the past, scientists believed that people who had been exposed to Pneumocystis jirovecii as children could later develop pneumocystis pneumonia from that childhood infection if their immune systems became weakened 223. However, it is more likely that people get pneumocystis pneumonia after being exposed to someone else who has pneumocystis pneumonia or who is carrying the fungus in their lungs without having symptoms.
The symptoms of pneumocystis pneumonia can develop over several days or weeks and include 214, 224, 217:
- Fever
- Cough
- Difficulty breathing
- Chest pain
- Chills
- Fatigue (tiredness)
Contact your healthcare provider if you have symptoms that you think are related to pneumocystis pneumonia.
Pneumocystis pneumonia is diagnosed using a sample from a patient’s lungs. The sample is usually mucus that is either coughed up by the patient called sputum or collected by a procedure called bronchoalveolar lavage (BAL). Sometimes, a small sample of lung tissue (a biopsy) is used to diagnose pneumocystis pneumonia. The patient’s sample is sent to a laboratory, usually to be examined under a microscope. Polymerase chain reaction (PCR) can also be used to detect Pneumocystis DNA in different types of samples. A blood test to detect beta-D-glucan (a part of the cell wall of many different types of fungi) can also help diagnose pneumocystis pneumonia 225.
Pneumocystis pneumonia must be treated with prescription medicine. Without treatment, pneumocystis pneumonia can cause death. The most common form of treatment is trimethoprim/sulfamethoxazole (TMP/SMX), which is also known as co-trimoxazole and by several different brand names, including Bactrim, Septra, and Cotrim. This medicine is given by mouth or through a vein for 3 weeks. Trimethoprim/sulfamethoxazole can cause side effects such as rash and fever. Other medicines are available for patients who cannot take trimethoprim/sulfamethoxazole.
For mild to moderate treatment, trimethoprim 15 to 20 mg/kg/day and sulfamethoxazole 75 to 100 mg/kg/day, given orally in 3 divided doses or trimethoprim-sulfamethoxazole double strength, 2 tablets 3 times per day 226. For moderate to severe cases, trimethoprim 15 to 20 mg/kg/day and sulfamethoxazole 75-100 mg/kg/day given intravenously (IV) every 6 to 8 hours with a switch to oral when the patient shows clinical improvement. In patients with a mild allergy to trimethoprim/sulfamethoxazole (TMP/SMX), desensitization should be attempted as this is the most effective drug of choice. In patients with severe allergies to trimethoprim/sulfamethoxazole (TMP/SMX), desensitization is no longer recommended, and it is more appropriate to choose a different drug regimen.
Alternative drug regimens for the treatment of pneumocystis pneumonia in those with sulfa allergies and mild to moderate disease include Atavaquone 750 mg, by mouth twice per day, Trimethoprim 15 mg/kg/day by mouth twice per day plus Dapsone 100 mg by mouth every day, or Primaquine 30 mg by mouth every day plus Clindamycin by mouth 450 mg every 6 hours or 600 mg every 8 hours 226. Alternative treatment for moderate to severe cases includes Pentamidine 4 mg/kg IV once daily over 60 minutes or Primaquine 30 mg by mouth every day plus Clindamycin IV 600 mg every 6 hours or 900 mg every 8 hours 226. Primaquine can only be orally administered, and patients who cannot tolerate oral medications should be given IV Pentamidine, but caution should be used due to its increased toxicity and side effects when compared to Primaquine. Caution must be used in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency if Dapsone or Primaquine are used as they can cause an increased risk of hemolytic anemia.
In HIV-infected patients with a moderate or severe disease, current recommendations suggest the addition of glucocorticoids to the treatment regimen as their use has been shown to improve clinical outcome and mortality 226. HIV-infected patients with a room air arterial blood gas partial pressure of oxygen that is less than or equal to 70 mm Hg, an alveolar-arterial (A-a) gradient greater than or equal to 35 mm Hg, or hypoxia on pulse oximetry should receive steroids 226. Corticosteroids also may be recommended in HIV-uninfected patients with pneumocystis pneumonia due to the potential for high mortality and fulminant course of illness, but data is limited on whether there are benefits or a decrease in in-hospital mortality. Dosing for prednisone should be started as soon as possible or within 72 hours of starting treatment for pneumocystis pneumonia and is as follows: 40 mg by mouth twice per day on days 1 through 5, 40 mg by mouth daily days 6 through 10, and 20 mg orally daily on days 11 through 21 226. IV methylprednisone can be given at 75% of the prednisone dose if oral therapy cannot be tolerated. HIV-infected patients who are not already on them should have antiretroviral therapy (ART) initiated within two weeks of Pneumocystis treatment or as soon as they are stable enough to begin treatment. Patients will usually show slightly worsening clinical signs around days 3 to 4 due to the host’s inflammatory response to dying organisms and then improvement afterward.
Prophylaxis treatment guidelines have been established for certain patient populations. Patients who are immunocompromised such as those with malignancy and who are taking glucocorticoid doses greater than 20 mg daily for one month or longer, patients who have received bone marrow suppressive therapies or antineoplastic therapies, and those who have undergone hematopoietic cell or solid organ transplantation should receive primary prophylaxis for Pneumocystis. First-line prophylaxis treatment is trimethoprim-sulfamethoxazole 1 double-strength tablet by mouth daily or 1 single-strength tablet by mouth daily 226. For those with sulfa allergies, recommended prophylaxis includes Dapsone 100 mg by mouth daily or 50 mg by mouth twice each day, Dapsone 50 mg by mouth daily plus pyrimethamine 50 mg plus leucovorin 25 mg by mouth weekly, Dapsone 200 mg plus pyrimethamine 75 mg plus leucovorin 25 mg by mouth weekly, Atovaquone 1500 mg by mouth daily, Atovaquone 1500 mg plus pyrimethamine 25 mg plus leucovorin 10 mg by mouth daily, or Aerosolized pentamidine 300 mg monthly via Respigard II nebulizer. HIV-infected individuals should receive prophylaxis with the same medications recommended above when CD4+ count is below 200 cells/microL or CD4+ less than 14 percent, presence of oropharyngeal candidiasis, and a CD4+ of 200-250 cells/microL when ART cannot be started or if monitoring of CD4+ count every 3 months is not possible.
Currently, at least 10-20% of patients with pneumocystis pneumonia will die. Pneumocystis pneumonia carries an even worse prognosis in patients without HIV infection, with mortality rates over 50%. In general, the mortality rates are much higher when there is an underlying lung disorder and in patients who require mechanical ventilation 227.
Fungal pneumonia
Fungal pneumonia is a pneumonia caused by one or more endemic or opportunistic fungi. Fungal infection occurs following the inhalation of spores, after the inhalation of conidia, or by the reactivation of a latent infection. Blood dissemination frequently occurs, especially in an immunocompromised host.
Endemic fungal pathogens (eg, Histoplasma capsulatum, Coccidioides immitis, Blastomyces dermatitidis, Paracoccidioides brasiliensis, Sporothrix schenckii, Cryptococcus neoformans) cause infection in healthy hosts and in immunocompromised persons, in defined geographic locations of the Americas and around the world 228.
Opportunistic fungal organisms (eg, Candida species, Aspergillus species, Mucor species) tend to cause pneumonia in patients with congenital or acquired defects in the host immune defenses 229. Hyalohyphomycosis is a broad term that describes infections due to a number of rare and emerging heterogeneous fungi that when isolated from infected lung tissue, appear as hyaline (lightly colored), filamentous fungi difficult to distinguish from Aspergillus. These genera include Scedosporium, Fusarium, Paecilomyces, Acremonium, and Trichoderma 228.
The diagnosis of fungal pneumonias is difficult to prove and is often made on a presumptive basis 228. It relies on a combination of clinical, radiologic, and microbiological factors 230. Candida organisms and some ubiquitous filamentous fungi (Aspergillus and Scedosporium) can be isolated from oropharyngeal and respiratory tracts as colonizers without evidence of invasion or symptoms until a breakdown of tissue barriers or of the host’s immune system occurs. Nonmolecular fungal markers in serum or other biological samples represent a noninvasive diagnostic tool, which can help in therapeutic decisions 229.
Conditions that predispose people to any of the opportunistic fungal pathogens are as follows:
- Acute leukemia or lymphoma during myeloablative chemotherapy
- Bone marrow or peripheral blood stem cell transplantation
- Solid organ transplantation on immunosuppressive treatment
- Prolonged corticosteroid therapy
- Acquired immunodeficiency syndrome (AIDS)
- Prolonged neutropenia from various causes
- Congenital immune deficiency syndromes
- Postsplenectomy state
- Genetic predisposition
Workers or farmers with heavy exposure to bird, bat, or rodent droppings or other animal excreta in endemic areas are predisposed to any of the endemic fungal pneumonias, such as histoplasmosis, in which the environmental exposure to avian or bat feces encourages the growth of the organism. In addition, farmers, nursery workers, landscapers, and gardeners are at higher risk of acquiring sporotrichosis because of their chance of cuts or puncture wounds while working with soil. The Pseudoallescheria boydii/Scedosporium apiospermum complex has been implicated as an important pathogen in delayed disseminated infections among victims of near-drowning in polluted waters 231 or recent natural disasters 232.
Complications of fungal pneumonia include:
- disease dissemination to other sites (ie, brain, meninges, skin, liver, spleen, kidneys, adrenals, heart, eyes) and sepsis syndrome and
- blood vessel invasion, which can lead to hemoptysis, pulmonary infarction, myocardial infarction, cerebral septic emboli, cerebral infarction, or blindness.
Other complications may include the following:
- Bronchopleural or tracheoesophageal fistulas
- Chronic pulmonary symptoms
- Mediastinal fibromatosis (histoplasmosis)
- Broncholithiasis (histoplasmosis)
- Pericarditis and other rheumatologic symptoms
Signs and symptoms of fungal pneumonia may include the following 233:
- Fever
- Cough, usually nonproductive
- Pleuritic chest pain or dull discomfort
- Progressive dyspnea leading to respiratory failure
- Airway obstructive symptoms from enlarged mediastinal adenopathy in the endemic mycoses
- Hemoptysis (in invasive aspergillosis or mucormycosis)
- History of travel to or exposure in areas containing endemic mycoses
- Symptoms from involvement of extrapulmonary systems (may suggest disease)
- Rheumatologic syndromes (common among endemic mycoses) – Arthritis and arthralgia, erythema nodosum, erythema multiforme, and pericarditis
- Endemic mycoses with associated dissemination
- Hypersensitivity or allergic reactions
- Extrapulmonary sites in individuals who are immunocompromised
- Meningoencephalitis in patients with AIDS and cryptococcosis
In individuals who are neutropenic or immunocompromised, persistent fever (even before pulmonary findings) may be an early sign of infection, especially if the fever is unresponsive to broad-spectrum antibiotics.
Hypersensitivity or allergic reactions include allergic bronchial asthma (Aspergillus species, Candida species), allergic bronchopulmonary mycoses (Aspergillus species, Candida species), bronchocentric granulomatosis (necrotizing granulomatous replacement and eosinophilic infiltration of bronchial mucosa in infection with Aspergillus species), and extrinsic allergic alveolitis (malt worker’s lung, farmer’s lung).
Nonculture-based diagnostic tools, such as galactomannan and beta-D-glucan, are part of the diagnostic workup of invasive fungal pneumonia with other clinical, radiologic, and microbiologic criteria. Galactomannan enzyme immunoassay (GM-EIA) for detection of invasive aspergillosis, are now in clinical use. Polymerase chain reaction (PCR)–based assays are also available for detecting various pathogens, including Aspergillus, Histoplasma, and Candida species 234, 235.
Therapy for fungal pneumonias must include antifungal agents. The type of antifungal drug employed must be selected based on the particular pathogen that is isolated or that is clinically suspected. Many classes of antifungal agents are now available, including the classic antibiotics; first-, second-, and third-generation triazoles; and the echinocandins. In patients with invasive aspergillosis, including pulmonary aspergillosis, voriconazole is the new standard of care, based on its superiority over amphotericin B as primary therapy 236. Vary the dose and treatment duration depending on the underlying pathogen causing the pneumonia. Care should be taken regarding patients on long-term voriconazole treatment. Bone pain with radiologic evidence of periostitis and 10-fold increased fluoride levels have been reported in allogeneic stem cell transplant patients taking the drug for at least 3 months. Symptoms and findings were reversed with discontinuation of voriconazole 237. There is a possible association between the use of voriconazole in markedly immunosuppressed patients as prophylactic agent and the development of mucormycosis, but this matter is still controversial 236.
Amphotericin B is less frequently used and, when used, is often given as a liposomal formulation to decrease toxicity 236.
Pneumonia complications
Complications of pneumonia are more common in young children, the elderly and those with pre-existing health conditions, such as diabetes.
People who have heart or lung problems, people who smoke, and people who are 65 years of age and older are more likely to experience complications from pneumonia.
Possible complications of pneumonia include:
- Difficulty breathing. If your pneumonia is severe or you have chronic underlying lung diseases, you may have trouble breathing in enough oxygen. You may need to be hospitalized and use a breathing machine (ventilator) while your lung heals.
- Pleurisy – where the thin linings between your lungs and ribcage (pleura) become inflamed, which can lead to respiratory failure
- Pleural effusion is when fluid builds up in the layers of tissue between your lungs and the wall of your chest cavity (pleura) and becomes infected. Pleural effusion can make breathing very difficult. To drain the fluid, a tube may need to be placed between your lungs and your chest wall, or you may need surgery.
- Lung abscess – a rare complication that’s mostly seen in people with a serious pre-existing illness or a history of severe alcohol misuse. An abscess occurs if pus forms in a cavity in the lung. An abscess is usually treated with antibiotics. Sometimes, surgery or drainage with a long needle or tube placed into the abscess is needed to remove the pus.
- Kidney failure (renal failure) is a term used to describe a situation in which the kidneys are no longer able to function effectively. If your kidneys fail, you need treatment to replace the work they normally do. The treatment options are dialysis or a kidney transplant.
- Respiratory failure. Respiratory failure is a condition in which your blood doesn’t have enough oxygen (O2) or has too much carbon dioxide (CO2). Sometimes you can have both problems. A low oxygen level in the blood can cause shortness of breath and air hunger (the feeling that you can’t breathe in enough air). Your skin, lips, and fingernails may also have a bluish color. A high carbon dioxide level can cause rapid breathing and confusion. Some people who have respiratory failure may become very sleepy or lose consciousness. They also may have arrhythmia (irregular heartbeat). You may have these symptoms if your brain and heart are not getting enough oxygen.
- Bacteria in the bloodstream (bacteremia). Bacteria that enter the bloodstream from your lungs can spread the infection to other organs, potentially causing organ failure.
- Blood poisoning (septicemia) – also a rare but serious complication
You’ll be admitted to hospital for treatment if you develop one of these complications.
Your doctor may give you oxygen to help you breathe or antibiotics through an IV.
Bacteria in the bloodstream occur when the pneumonia infection in your lungs spreads to your blood. This increases the risk that the infection will spread to other organs in your body. Bacteria in the bloodstream are treated with antibiotics.
Bronchitis vs Pneumonia
Bronchitis is the inflammation of the larger airways in your lungs, causing an ongoing cough.
Bronchitis can be caused by viruses, bacteria, or breathing in smoke or dust.
- Acute bronchitis is usually caused by a viral infection, such as cold viruses or influenza virus and can last for weeks, whereas chronic bronchitis lasts for months and may come back each year.
- Chronic bronchitis is usually related to smoking. Chronic bronchitis is defined as a productive cough that lasts at least three months, with recurring bouts occurring for at least two consecutive years.
Most people with acute bronchitis will feel better with time and rest, with a number of treatments available to help ease the cough and other symptoms.
If you think you have bronchitis, your doctor can assess you and discuss treatment.
Is bronchitis contagious?
Mostly, bronchitis is caused by contagious viruses. These can be spread by air when someone coughs, or by touch after the virus is left on a surface.
Hand washing, covering your mouth when coughing and staying home while unwell can reduce the spread.
People at risk of developing bronchitis include:
- the elderly
- people breathing in irritating chemicals
- smokers
- those with a lung condition, such as asthma
- people with poor immunity
You can reduce your risk by hand washing, and if you smoke, cutting down or quitting. The annual flu vaccine is recommended for people with chronic bronchitis.
Bronchitis causes
Acute bronchitis is usually caused by viruses, typically the same viruses that cause colds and flu (influenza). Antibiotics don’t kill viruses, so this type of medication isn’t useful in most cases of bronchitis.
The most common cause of chronic bronchitis is cigarette smoking. Air pollution and dust or toxic gases in the environment or workplace also can contribute to the condition.
Bronchitis symptoms
Someone with bronchitis may have:
- cough (either dry or bringing up phlegm). Mucus (phlegm or sputum), which can be clear, white, yellowish-gray or green in color — rarely, it may be streaked with blood
- wheezing
- aches and pains
- fever
- feeling short of breath
- chest tightness
Risk factors for bronchitis
Factors that increase your risk of bronchitis include:
- Cigarette smoke. People who smoke or who live with a smoker are at higher risk of both acute bronchitis and chronic bronchitis.
- Low resistance. This may result from another acute illness, such as a cold, or from a chronic condition that compromises your immune system. Older adults, infants and young children have greater vulnerability to infection.
- Exposure to irritants on the job. Your risk of developing bronchitis is greater if you work around certain lung irritants, such as grains or textiles, or are exposed to chemical fumes.
- Gastric reflux. Repeated bouts of severe heartburn can irritate your throat and make you more prone to developing bronchitis.
Bronchitis complications
Although a single episode of bronchitis usually isn’t cause for concern, it can lead to pneumonia in some people. Repeated bouts of bronchitis, however, may mean that you have chronic obstructive pulmonary disease (COPD).
Do you need a chest X-ray for bronchitis?
An X-ray is usually not necessary for simple cases of bronchitis.
Bronchitis treatment
Because most cases of bronchitis are caused by viral infections, antibiotics aren’t effective. Most people with acute bronchitis will feel better with time and rest, usually within a couple of weeks.
You can help ease the cough and other symptoms by:
- inhaling steam or having a warm bath
- avoiding cigarette smoke and other irritants
- drinking plenty of fluids
- simple pain relief medication, such as paracetamol (follow the directions on the label)
- a teaspoon of honey at night, either by itself or in warm water
- consider a face mask outside. If cold air aggravates your cough and causes shortness of breath, put on a cold-air face mask before you go outside.
Cough medicines are available, but they might or might not help.
If you are very unwell or not getting better, or if you get worse, see your doctor.
Pneumonia causes
Many germs can cause pneumonia. The most common are bacteria and viruses in the air we breathe. Your body usually prevents these germs from infecting your lungs. But sometimes these germs can overpower your immune system, even if your health is generally good.
Pneumonia is usually the result of a pneumococcal infection, caused by bacteria called Streptococcus pneumoniae.
Many different types of bacteria, including Haemophilus influenzae and Staphylococcus aureus, can also cause pneumonia, as well as viruses and, more rarely, fungi.
As well as bacterial pneumonia, other types include:
- Viral pneumonia – most commonly caused by the respiratory syncytial virus (RSV) and sometimes influenza type A or B; viruses are a common cause of pneumonia in young children
- Aspiration pneumonia – caused by breathing in vomit, a foreign object, such as a peanut, or a harmful substance, such as smoke or a chemical
- Fungal pneumonia – rare in the US and more likely to affect people with a weakened immune system
- Hospital-acquired pneumonia – pneumonia that develops in hospital while being treated for another condition or having an operation; people in intensive care on breathing machines are particularly at risk of developing ventilator-associated pneumonia
Higher Risk groups
The following groups have an increased risk of developing pneumonia:
- babies and very young children
- elderly people
- people who smoke
- people with other health conditions, such as asthma, cystic fibrosis, or a heart, kidney or liver condition
- people with a weakened immune system – for example, as a result of a recent illness, such as flu, having HIV or AIDS, having chemotherapy, or taking medication following an organ transplant.
Who is at risk of developing pneumonia?
You are more at risk of developing pneumonia if:
- Chronic obstructive pulmonary disease (COPD), especially if you have taken inhaled corticosteroids for 24 weeks or longer
- Human immunodeficiency virus (HIV)
- Acquired immunodeficiency syndrome (AIDS)
- Heart disease
- Emphysema
- Diabetes
You are older than 65 years of age. As you get older, your immune system becomes less able to fight off infections like pneumonia. Babies and young children are also at increased risk because their immune systems are not yet fully developed.
You have a disease or condition that weakens your immune system. When your immune system is weakened, it’s easier for you to get pneumonia because your body can’t fight off the infection. People who have weakened immune systems are also more likely to develop pneumonia from bacteria, viruses and germs that don’t cause pneumonia in healthy people.
People who have any of the following are at increased risk:
- People who have recently had an organ transplant and people who are receiving chemotherapy are also at increased risk.
- You work in construction or agriculture. Working in environments where you breathe in dust, chemicals, air pollution or toxic fumes can damage your lungs and make them more vulnerable to infections like pneumonia.
- You smoke or abuse alcohol. Smoking damages the tiny hairs in the lungs that help remove germs and bacteria. Alcohol abuse can put you at increased risk of aspiration pneumonia,a type of pneumonia that develops after you inhale particles into your lungs.This occurs most often when you vomit and small particles enter your lungs because you are not strong enough to cough the particles out. Alcohol abuse also interferes with the way your white blood cells (which are responsible for fighting infection) work.
- You are hospitalized, especially in an intensive care unit (ICU). Pneumonia that you catch in a hospital (called hospital-acquired pneumonia) can be more serious than other types of pneumonia. Your risk increases if you are using a ventilator to help you breathe. Ventilators make it hard for you to cough and can trap germs that cause infection in your lungs.
- You have recently had major surgery or a serious injury. Recovering from major surgery or a serious injury often makes you weak. It can also make it difficult for you to cough, which is the body’s quickest defense for getting particles out of the lungs. Recovery also typically requires a lot of bed rest. Lying down on your back for an extended period of time can allow fluid or mucus to gather in your lungs, giving bacteria a place to grow.
- You are of Native Alaskan or Native American descent. For reasons unknown to doctors, people of these ethnic groups are at increased risk for pneumonia.
Risk factors for developing pneumonia
Pneumonia can affect anyone. But the two age groups at highest risk for pneumonia are:
- Children who are 2 years old or younger
- People who are age 65 or older
Other risk factors include:
- Being hospitalized. You’re at greater risk of pneumonia if you’re in a hospital intensive care unit, especially if you’re on a machine that helps you breathe (a ventilator).
- Chronic disease. You’re more likely to get pneumonia if you have asthma, chronic obstructive pulmonary disease (COPD) or heart disease.
- Smoking. Smoking damages your body’s natural defenses against the bacteria and viruses that cause pneumonia.
- Weakened or suppressed immune system. People who have HIV/AIDS, who’ve had an organ transplant, or who receive chemotherapy or long-term steroids are at risk.
Pneumonia prevention
Although most cases of pneumonia are bacterial and aren’t passed on from one person to another, ensuring good standards of hygiene will help prevent germs spreading.
You can help prevent pneumonia by doing the following:
- Get the flu vaccine each year. People often develop bacterial pneumonia after a case of the flu. You can reduce this risk by getting the yearly flu shot. The flu shot doesn’t protect against all strains of the flu, just the 3 to 4 strains that doctors feel will be most dangerous or wide spread in the coming year. The seasonal flu vaccine protects against the influenza viruses that research indicates will be most common during the upcoming season. Traditional flu vaccines (called “trivalent” vaccines) are made to protect against three flu viruses; an influenza A (H1N1) virus, an influenza A (H3N2) virus, and an influenza B virus. There are also flu vaccines made to protect against four flu viruses (called “quadrivalent” vaccines). These vaccines protect against the same viruses as the trivalent vaccine and an additional B virus. The flu vaccine is usually given in September through October, before flu season starts.
- Get the pneumococcal vaccine. Pneumococcus vaccines are especially important for people at high risk of pneumonia, including:
- Adults age 65 or older
- Children age 2 or younger
- People who have chronic (ongoing) diseases, serious long-term health problems, or weak immune systems. This may include people who have cancer, HIV, asthma, sickle cell disease, or damaged or removed spleens.
- People who smoke
- Haemophilus influenzae type b (Hib) vaccine. Haemophilus influenzae type b (Hib) is a type of bacteria that can cause pneumonia and meningitis. The Haemophilus influenzae type b (Hib) vaccine is recommended for all children under 5 years old in the United States. The Hib vaccine often is given to infants starting when they are 2 months old.
- Keep your immune system strong. Get enough sleep, exercise regularly and eat a healthy diet.
- Practice good hygiene. Your hands come in contact with many germs throughout the day. You pick them up from surfaces such as doorknobs, other people’s hands and your computer keyboard. Take time to wash your hands often, especially after using the restroom and before eating. Use lukewarm water and soap for at least 20 seconds. If soap and water are not available,using an alcohol-based hand sanitizer is the next best thing.
- cover your mouth and nose with a handkerchief or tissue when you cough or sneeze
- throw away used tissues immediately – germs can live for several hours after they leave your nose or mouth
- Don’t smoke. Smoking damages your lungs and makes it harder for your body to defend itself from germs and disease. If you smoke, talk to your doctor about quitting as soon as possible.
- Practice a healthy lifestyle. Eat a balanced diet full of fruits and vegetables. Exercise regularly. Get plenty of sleep. These things help your immune system stay strong.
- Excessive and prolonged alcohol misuse also weakens your lungs’ natural defences against infections, making you more vulnerable to pneumonia.
- Avoid sick people. Being around people who are sick increases your risk of catching what they have.
- If you have problems swallowing, eat smaller meals of thickened food and sleep with the head of your bed raised up. These steps can help you avoid getting food, drink, or saliva into your lungs.
- If you have a planned surgery, your doctor may recommend that you don’t eat for 8 hours or drink liquids for 2 hours before your surgery. This can help prevent food or drink from getting into your airway while you are sedated.
- If your immune system is impaired or weakened, your doctor may recommend you take antibiotics to prevent bacteria from growing in your lungs.
Pneumonia shot
Pneumococcal disease is common in young children, but older adults are at greatest risk of serious illness and death. There are two kinds of vaccines that help prevent pneumococcal disease.
There are 2 types of pneumococcal vaccines used in the United States 238, 239:
- Pneumococcal conjugate vaccines (PCVs). A conjugate vaccine is a type of vaccine that joins a protein to an antigen (in the case of pneumococcal vaccines, the protein is connected to unique polysaccharides [long chains of sugar molecules] from the surface of each of the pneumococcal serotypes). The conjugate vaccines have the polysaccharides for different serotypes attached (or conjugated) to a carrier protein. The protein helps improve the quality of the immune system response to the vaccine compared to the response to an unconjugated polysaccharide (PPV). Immune response to pneumococcal conjugate vaccine (PCV) is a T-cell dependent response that produces memory B-cells and reduces carriage of the bacteria in the respiratory track. Pneumococcal conjugate vaccines (PCVs) are given to children younger than 5 years old and to older children who need it. Vaccine providers also give pneumococcal conjugate vaccines (PCVs) to adults 65 years or older and other adults who need it.
- Pneumococcal polysaccharide vaccine (PPV). A polysaccharide vaccine is a type of vaccine that is composed of long chains of sugar molecules called polysaccharides, that resemble the surface of certain serotypes of pneumococcal bacteria in order to help the immune system mount a response. The immune response to the Pneumovax23 (PPSV23) vaccine is a T-cell independent immune response but does not reduce bacterial carriage. Vaccine providers may give Pneumovax23 (PPSV23) to children 2 through 18 years old with certain medical conditions. Vaccine providers give it to adults who receive PCV15 (Vaxneuvance). They also may give it to adults who have received an earlier vaccine called PCV13 (Prevnar 13). PCV13 (Prevnar 13) is FDA-licensed and may still be available in some clinics. PCV13 (Prevnar 13) is no longer routinely recommended; however, CDC guidance allows for its use as previously recommended in situations where PCV15, PCV20, or PCV21 is indicated but unavailable and the alternative is that the patient would not be vaccinated 243.
- PPSV23 (Pneumovax23) helps protect against 23 types of Streptococcus pneumoniae bacteria 244. Following the 2022 changes to the pneumococcal vaccination schedule for adults, PPSV23 (Pneumovax23) is no longer recommended alone, however PPSV23 (Pneumovax23) is recommended for adults following PCV13 (Prevnar 13) or PCV15 (Vaxneuvance) vaccination. PPSV23 (Pneumovax23) is not recommended for people who have previously received a PCV20 (Prevnar 20) or PCV21 (Capvaxive) vaccination.
Each of these vaccines helps protect against specific serotypes, or strains of Streptococcus pneumoniae bacteria. The number at the end of the vaccine name tells how many serotypes the pneumococcal vaccine includes.
The Centers for Disease Control and Prevention (CDC) recommends pneumococcal vaccination for 245:
- Children
- All children younger than 5 years old
- Children 5 through 18 years old with certain risk conditions
- Adults
- All adults 65 years or older
- 19 through 64 years old with certain risk conditions
The Centers for Disease Control and Prevention (CDC) recommends pneumococcal conjugate (PCV) vaccination for:
- All babies and children younger than 2 years old
- All adults 65 years or older
- People 2 through 64 years old with certain medical conditions
CDC recommends pneumococcal polysaccharide (PPSV) vaccination for:
- All adults 65 years or older
- People 2 through 64 years old with certain medical conditions
- Adults 19 through 64 years old who smoke cigarettes
The pneumococcal vaccine is recommended if you:
- Are 65 years of age or older
- Smoke
- Abuse alcohol
- Have certain chronic conditions, such as asthma, diabetes, heart disease or lung disease
- Have cirrhosis
- Have a condition that weakens your immune system, such as the human immunodeficiency virus (HIV), acquired immunodeficiency syndrome (AIDS), kidney failure or a damaged spleen
- Have had your spleen removed for any reason
- Have sickle cell disease
- Have cochlear implants (an electronic device that helps you hear)
- Are taking medicine for a recent organ transplant (these medicines suppress your immune system)
- Are receiving chemotherapy
Pneumococcal vaccines that help protect against pneumococcal disease work well, but cannot prevent all cases. But they can make it less likely that people who are at risk will experience the severe, and possibly life-threatening, complications of pneumonia.
Studies* show that at least 1 dose of pneumococcal conjugate vaccine (PCV) protects:
- At least 8 in 10 babies from serious infections called invasive pneumococcal disease
- 75 in 100 adults 65 years or older against invasive pneumococcal disease
- 45 in 100 adults 65 years or older against pneumococcal pneumonia
Studies* show that 1 dose of pneumococcal polysaccharide vaccine (PPSV) protects:
- Between 50 to 85 in 100 healthy adults against invasive pneumococcal disease.
Who Should NOT Get These Vaccines?
You shouldn’t get PCV15 (Vaxneuvance), PCV20 (Prevnar 20) or PCV21 (Capvaxive) if you’ve:
- Had a life-threatening allergic reaction after any type of pneumococcal conjugate vaccination (PCV)
- Had a life-threatening allergic reaction to any vaccine containing diphtheria toxoid (DTaP)
- Have a severe allergy to any part of these vaccines
You shouldn’t get Pneumovax23 (PPSV23) if you:
- Are younger than 2 years old
- Had a life-threatening allergic reaction after getting Pneumovax23 (PPSV23)
- Have a severe allergy to any part of Pneumovax23 (PPSV23)
Pneumococcal Conjugate Vaccine (PCV)
Tell the person who is giving you or your child a pneumococcal conjugate vaccine if:
You or your child have had a life-threatening allergic reaction or have a severe allergy.
- Anyone who has had a life-threatening allergic reaction to any of the following should not get PCV13:
- A dose of this vaccine
- An earlier pneumococcal conjugate vaccine called PCV7 (or Prevnar®)
- Any vaccine containing diphtheria toxoid (for example, DTaP)
- Anyone with a severe allergy to any component of PCV13 should not get the vaccine. Your or your child’s healthcare professional can tell you about the vaccine’s components.
You or your child are not feeling well.
People who have a mild illness, such as a cold, can probably get the vaccine. People who have a more serious illness should probably wait until they recover. Your or your child’s healthcare professional can advise you.
Pneumococcal Polysaccharide Vaccine (PPSV)
Children younger than 2 years old should not get this vaccine. In addition, tell the person who is giving you or your child a pneumococcal polysaccharide vaccine if:
You or your child have had a life-threatening allergic reaction or have a severe allergy.
- Anyone who has had a life-threatening allergic reaction to PPSV23 should not get another dose.
- Anyone who has a severe allergy to any component of PPSV23 should not get it. Your or your child’s healthcare professional can tell you about the vaccine’s components.
You or your child are not feeling well.
- People who have a mild illness, such as a cold, can probably get the vaccine. People who have a more serious illness should probably wait until they recover. Your or your child’s healthcare professional can advise you.
You are pregnant.
- There is no evidence that PPSV23 is harmful either to a pregnant woman or to her baby. However, as a precaution, women who need the vaccine should get it before becoming pregnant, if possible.
What Are the Possible Side Effects of pneumococcal vaccination?
Most people who get a pneumococcal vaccine do not have any serious problems with it. With any medicine, including vaccines, there is a chance of side effects. These are usually mild and go away on their own within a few days, but serious reactions are possible.
Mild Problems
Pneumococcal Conjugate Vaccine (PCV)
Mild problems following pneumococcal conjugate vaccination can include:
- Reactions where the shot was given
- Redness
- Swelling
- Pain or tenderness
- Fever
- Loss of appetite
- Fussiness (irritability)
- Feeling tired
- Headache
- Chills
Young children who get pneumococcal conjugate vaccine at the same time as inactivated flu vaccine may be at increased risk for seizures caused by fever. Ask your doctor for more information.
Pneumococcal Polysaccharide Vaccine (PPSV)
Mild problems following pneumococcal polysaccharide vaccination can include:
- Reactions where the shot was given
- Redness
- Pain
- Fever
- Muscle aches
If these problems occur, they usually go away within about two days.
Problems that Could Happen After Getting Any Injected Vaccine
- People sometimes faint after a medical procedure, including vaccination. Sitting or lying down for about 15 minutes can help prevent fainting and injuries caused by a fall. Tell your healthcare professional if you or your child:
- Feels dizzy
- Has vision changes
- Has ringing in the ears
- Some people get severe pain in the shoulder and have difficulty moving the arm where the doctor gave the shot. This happens very rarely.
- Any medicine can cause a severe allergic reaction. Such reactions from a vaccine are very rare, estimated at about 1 in a million doses. These types of reactions would happen within a few minutes to a few hours after the vaccination.
- As with any medicine, there is a very remote chance of a vaccine causing a serious injury or death.
Pneumonia diagnosis
Your doctor will diagnose pneumonia based on your medical history and the results from a physical exam.
Pneumonia can be difficult to diagnose because it shares many symptoms with other conditions, such as the common cold, bronchitis and asthma.
To help make a diagnosis, your doctor may ask you:
- whether you feel breathless or you’re breathing faster than usual
- how long you’ve had your cough, and whether you’re coughing up mucus and what color it is
- if the pain in your chest is worse when you breathe in or out
Your doctor may also take your temperature and listen to your chest and back with a stethoscope to check for any crackling or rattling sounds.
They may also listen to your chest by tapping it. Lungs filled with fluid produce a different sound from normal healthy lungs.
If you have mild pneumonia, you probably won’t need to have a chest X-ray or any other tests.
If pneumonia is suspected, your doctor may recommend the following tests:
- Blood tests. Blood tests are used to confirm an infection and to try to identify the type of organism causing the infection. However, precise identification isn’t always possible.
- Chest X-ray. A chest X-ray looks for inflammation in your lungs. This helps your doctor diagnose pneumonia and determine the extent and location of the infection. However, it can’t tell your doctor what kind of germ is causing the pneumonia.
- Pulse oximetry. Pulse oximetry measures how much oxygen is in your blood. Pneumonia can prevent your lungs from moving enough oxygen into your bloodstream. To measure the levels, a small sensor called a pulse oximeter is attached to your finger or ear.
- Sputum test. A sample of fluid from your lungs (sputum) is taken after a deep cough and analyzed to help pinpoint the cause of the infection and to find out what germ is causing your pneumonia.
Your doctor might order additional tests if you’re older than age 65, are in the hospital, or have serious symptoms or health conditions. These may include:
- CT scan. If your pneumonia isn’t clearing as quickly as expected, your doctor may recommend a chest CT scan to obtain a more detailed image of your lungs. Chest CT scan can also show whether you have complications such as lung abscesses or pleural disorders. A CT scan shows more detail than a chest X-ray.
- Arterial blood gas test. A blood gas test may be done if you are very sick. For this test, your doctor measures your blood oxygen levels using a blood sample from an artery, usually in your wrist.
- Blood culture. A blood culture is a test that checks samples of your blood for the presence of disease-causing germs like bacteria and fungi. During blood culture test, a blood sample is placed in a special container in a laboratory and watched to see if germs grow. Blood culture testing is frequently used to identify the germ causing your pneumonia and determine if germs have entered the bloodstream. A blood culture test identifies the specific germ causing an infection and enables further testing to determine what type of treatment may be most effective.
- Polymerase chain reaction (PCR) test quickly checks your blood or sputum sample to find the DNA of germs that cause pneumonia.
- Bronchoscopy looks inside your airways. If your treatment is not working well, this procedure may be needed. At the same time, your doctor may also collect samples of your lung tissue and fluid from your lungs to help find the cause of your pneumonia.
- Pleural fluid culture. A fluid sample from the pleural space between your lungs and chest wall is taken by putting a needle between your ribs from the pleural area (thoracentesis) and analyzed to help determine the type of infection.
Pneumonia treatment
Treatment for pneumonia depends on the type of pneumonia you have, which germ is causing it, how severe your symptoms are, how healthy you are overall and your age.
The goals of treatment are to cure the infection and prevent complications. It is important to follow your treatment plan carefully until you are fully recovered.
Treatment for pneumonia may include:
- Antibiotics treat bacterial pneumonia and some types of fungal pneumonia. They do not work for viral pneumonia.
- In some cases, your doctor may prescribe antiviral medicines for viral pneumonia
- Antifungal medicines treat other types of fungal pneumonia
You may need to be treated in a hospital if your symptoms are severe or if you are at risk for complications. While there, you may antibiotics given through an intravenous (IV) line and oxygen therapy. For example, if your blood oxygen level is low, you may receive oxygen therapy.
It may take several weeks to recover from pneumonia. Some people feel better within a week. For other people, it can take a month or more.
Mild pneumonia can usually be treated at home by:
- getting plenty of rest
- taking antibiotics
- drinking plenty of fluids
If you don’t have any other health problems, you should respond well to treatment and soon recover, although your cough may last for some time.
It’s usually safe for someone with pneumonia to be around others, including family members.
However, people with a weakened immune system are less able to fight off infections, so it’s best they avoid close contact with a person with pneumonia.
For at-risk groups, pneumonia can be severe and may need to be treated in hospital. This is because it can lead to serious complications, which in some cases can be fatal, depending on a person’s health and age.
For bacterial pneumonia, your doctor will probably prescribe antibiotics. Most of your symptoms should improve within a few days, although a cough can last for several weeks. Be sure to follow your doctor’s directions carefully. Take all the antibiotic medicine that your doctor prescribes. If you don’t, some bacteria may stay in your body. This can cause your pneumonia to come back. It can also increase your risk of antibiotic resistance.
- Unless a healthcare professional tells you otherwise, you should always finish taking a prescribed course of antibiotics, even if you feel better.
- If you stop taking an antibiotic part way through a course, the bacteria can become resistant to the antibiotic.
After starting treatment, your symptoms should steadily improve.
However, how quickly they improve will depend on how severe your pneumonia is.
As a general guide, after:
- one week – fever should have gone
- four weeks – chest pain and mucus production should have substantially reduced
- six weeks – cough and breathlessness should have substantially reduced
- three months – most symptoms should have resolved, but you may still feel very tired (fatigue)
- six months – most people will feel back to normal
Visit your doctor if your symptoms don’t improve within three days of starting antibiotics.
Symptoms may not improve if:
- the bacteria causing the infection is resistant to antibiotics – your doctor may prescribe a different antibiotic, or they may prescribe a second antibiotic for you to take with the first one
- a virus is causing the infection, rather than bacteria – antibiotics have no effect on viruses, and your body’s immune system will have to fight the viral infection by creating antibodies
Painkillers, such as acetaminophen (paracetamol) or ibuprofen, may help relieve pain and reduce fever. DO NOT give aspirin to children.
However, you shouldn’t take ibuprofen if you:
- are allergic to aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs)
- have asthma, kidney disease, a history of stomach ulcers or indigestion
Cough medicines aren’t recommended as there’s also little evidence they are effective. A warm honey and lemon drink can help relieve discomfort caused by coughing.
Your cough may persist for two to three weeks after you finish your course of antibiotics, and you may feel tired for even longer as your body continues to recover.
Drink plenty of fluids to avoid dehydration, and get plenty of rest to help your body recover.
If you smoke, it’s more important than ever to stop, as smoking damages your lungs.
See your doctor if, after following the above self-help measures, your condition is deteriorating or isn’t improving as expected.
Pneumonia is commonly caused by viruses or bacteria passed from one person to another. But healthy people are normally able to fight off these germs without pneumonia developing. So it’s usually safe for someone with pneumonia to be around others, including family members.
However, people with a weakened immune system are less able to fight off infections, so it’s best they avoid close contact with a person with pneumonia.
Antibiotics don’t work to treat viral infections. If you have viral pneumonia, your doctor will likely talk to you about ways to treat your symptoms and your doctor may prescribe an antiviral medication to treat it. Sometimes, though, symptom management and rest are all that is needed. Over-the-counter (OTC) medicines are available to lower fever,relieve pain and ease your cough. However, some coughing is okay because it can help clear your lungs. Be sure to talk to your doctor before you take a cough suppressant.
If a fungus is causing your pneumonia, your doctor may prescribe an antifungal medicine.
If your case of pneumonia is severe, you may need to be hospitalized. If you are experiencing shortness of breath, you may be given oxygen to help your breathing. You might also receive antibiotics intravenously(through an IV). People who have weakened immune systems, heart disease or lung conditions, and people who were already very sick before developing pneumonia are most likely to be hospitalized. Babies, young children and adults who are 65 years of age and older are also at increased risk.
Home remedies
In addition to taking any antibiotics and/or medicine your doctor prescribes, you should also do the following:
- Get lots of rest. Rest will help your body fight the infection.
- Drink plenty of fluids. Fluids will keep you hydrated and can help loosen the mucus in your lungs. Try water, warm tea and clear soups to help open your airways and ease your breathing.
- Do not take cough medicines without first talking to your doctor. Coughing is one way your body works to get rid of an infection. If your cough is preventing you from getting the rest you need, ask your doctor about steps you can take to get relief.
- Stop smoking if you smoke, and avoid secondhand smoke. Smoke can make your symptoms worse. Smoking also increases your risk of developing pneumonia and other lung problems in the future. You should also avoid lit fireplaces or other areas where the air may not be clean.
- Stay home from school or work until your symptoms go away. This usually means waiting until your fever breaks and you aren’t coughing up mucus. Ask your doctor when it’s okay for you to return to school or work.
- Use a cool-mist humidifier or take steamy baths to help clear your lungs and make it easier for you to breathe.
Contact your doctor right away if your breathing gets worse instead of better over time.
If your pneumonia is so severe that you are treated in the hospital, you may be given intravenous fluids and antibiotics, as well as oxygen therapy, and possibly other breathing treatments.
Follow up with your doctor
Your doctor may schedule a follow-up appointment after he or she diagnoses you with pneumonia. At this visit, your doctor might take another chest X-ray to make sure the pneumonia infection is clearing up. Keep in mind that chest X-rays can take months to return to normal. However, if your symptoms are not improving, your doctor may decide to try another form of treatment.
Although you may be feeling better, it’s important to keep your follow-up appointment, especially if you smoke. The infection can still be in your lungs even if you’re no longer experiencing symptoms.
Your doctor will probably arrange another follow-up appointment for you about six weeks after you start your course of antibiotics.
In some cases, they may arrange follow-up tests, such as a chest X-ray, if:
- your symptoms haven’t improved
- your symptoms have come back
- you smoke
- you’re over the age of 50
Some people may be advised to have a flu vaccination or pneumococcal vaccination after recovering from pneumonia.
Aspiration pneumonia
If you’ve breathed in an object that’s causing pneumonia, it may need to be removed.
To do this, an instrument called a bronchoscope may be used to look into your airways and lungs so that the object can be located and removed. This procedure is known as a bronchoscopy.
Treatment in hospital
You may need treatment in hospital if your symptoms are severe. You’ll be given antibiotics and fluids intravenously through a drip, and you may need oxygen to help breathing.
In very serious cases of pneumonia, breathing assistance through a ventilator in an intensive care unit (ICU) may be required.
You may need to be hospitalized if:
- You are older than age 65
- You are confused about time, people or places
- Your kidney function has declined
- Your systolic blood pressure is below 90 millimeters of mercury (mm Hg) or your diastolic blood pressure is 60 mm Hg or below
- Your breathing is rapid (30 breaths or more a minute)
- You need breathing assistance
- Your temperature is below normal
- Your heart rate is below 50 or above 100
You may be admitted to the intensive care unit if you need to be placed on a breathing machine (ventilator) or if your symptoms are severe.
Children may be hospitalized if:
- They are younger than age 2 months
- They are lethargic or excessively sleepy
- They have trouble breathing
- They have low blood oxygen levels
- They appear dehydrated.
Pneumonia prognosis
Pneumonia prognosis depends on many factors, including age, comorbidities, and hospital setting (inpatient or outpatient). Generally, pneumonia prognosis is promising in otherwise healthy patients. Patients older than 60 years or younger than 4 years of age have a relatively poorer prognosis than young adults. If pneumonia is left untreated, the overall mortality may become 30%. Antibiotic resistance is very concerning due to the excessive and unjustified use of antibiotics. The Pneumonia Severity Index (PSI) may be utilized as a tool to establish a patient’s risk of mortality.
In a study conducted on causes of community-acquired pneumonia, Streptococcus pneumoniae (pneumococcus) was found to be the cause of mortality in most patients; however, Pseudomonas, Staphylococcus aureus, and mixed causes had the highest mortality rates in those affected 246.
Recovering from pneumonia
It may take time to recover from pneumonia. Some people feel better and are able to return to their normal routines within a week. For other people, it can take a month or more. Most people continue to feel tired for about a month. Adequate rest is important to maintain progress toward full recovery and to avoid relapse. Don’t rush your recovery! Talk with your doctor about when you can go back to your normal routine.
While you are recovering, try to limit your contact with family and friends, to help keep your germs from spreading to other people. Cover your mouth and nose when you cough, promptly dispose of tissues in a closed waste container and wash your hands often.
If you have taken antibiotics, your doctor will want to make sure your chest X-ray is normal again after you finish the whole prescription. It may take many weeks for your X-ray to clear up.
Possible pneumonia complications
People who may be more likely to have complications from pneumonia include:
- Older adults or very young children.
- People whose immune system does not work well.
- People with other, serious medical problems such as diabetes or cirrhosis of the liver.
Possible complications include:
- Respiratory failure, which requires a breathing machine or ventilator.
- Sepsis, a condition in which there is uncontrolled inflammation in the body, which may lead to widespread organ failure.
- Acute respiratory distress syndrome (ARDS), a severe form of respiratory failure.
- Lung abscesses, which are infrequent, but serious complications of pneumonia. They occur when pockets of pus form inside or around the lung. These may sometimes need to be drained with surgery.
Collapsed lung
Collapsed lung is also known as pneumothorax which is the presence of air or gas in the pleural cavity (the space between your lung and chest wall). A collapsed lung or pneumothorax occurs when air leaks into the space between your lung and chest wall. This air in the pleural space can build up and pushes on the outside of your lung and makes it partially or fully collapse. A collapsed lung or pneumothorax can be a complete lung collapse or a collapse of only a portion of the lung. In most cases, only some of the lung collapses. A pneumothorax is reasonably common and has many different causes. A collapsed lung or pneumothorax can be caused by a blunt or penetrating chest injury, certain medical procedures, or damage from underlying lung disease. Or it may occur for no obvious reason called spontaneous pneumothorax.
Signs and symptoms of a collapsed lung or pneumothorax include:
- Chest pain on one side, especially when taking breaths.
- Cough.
- Fast breathing.
- Fast heart rate.
- Fatigue.
- Shortness of breath (dyspnea).
- Bluish skin, lips or nails (cyanosis).
If you have symptoms of a collapsed lung, go to the nearest emergency room. You may need immediate care.
Collapsed lung symptoms usually include sudden chest pain, shortness of breath with blue skin, nails or lips. On some occasions, a collapsed lung can be a life-threatening event.
The clinical results are dependent on the degree of collapse of the lung on the affected side. If the collapsed lung or pneumothorax is significant, it can cause a shift of the mediastinum and compromise hemodynamic stability.
- If you have a collapsed lung or pneumothorax and you feel it is getting harder to breathe, call your local emergency number for an ambulance.
There are no direct figures on the incidence of collapsed lung or pneumothorax. However, it is a common problem, frequently as a complication of trauma (often undiagnosed), and it also commonly occurs as a spontaneous occurrence and in people with previous lung disease.
The goal in treating a collapsed lung or pneumothorax is to relieve the pressure on your lung, allowing it to re-expand. Treatment options for a collapsed lung or pneumothorax may include observation, needle aspiration, chest tube insertion, nonsurgical repair or surgery. You may receive supplemental oxygen therapy to speed air reabsorption and lung expansion. Depending on the cause of the pneumothorax, a second goal may be to prevent recurrences. The methods for achieving these goals depend on the severity of the lung collapse and sometimes on your overall health.
Treatment for a pneumothorax usually involves inserting a flexible tube or needle between the ribs to remove the excess air. However, a small pneumothorax may heal on its own.
Figure 23. Collapsed and normal lung
Figure 24. A large, right-sided pneumothorax has occurred from a rupture of a subpleural bleb (chest X-ray).
Figure 25. Large spontaneous pneumothorax
Footnotes: 35 year old male with symptoms of breathlessness on exertion and fatigue. On exam noted to have diminished air entry in the left lower lung base. Oxygen levels 97% at rest. Odd episodes of cough, lateral flow test negative. Chest X-ray showed large left sided pneumothorax with total collapse of the left lung. Minor mediastinal shift. Heart size normal. Right lung clear.
[Source 247 ]Figure 26. Bilateral pneumothoraces
Footnotes: 40 year old male with acute severe shortness of breath. No history of trauma. Chest X-ray large bilateral pneumothoraces. Although the costophrenic angles are excluded from the image, the deep sulcus sign is evident bilaterally.
[Source 248 ]Figure 27. Spontaneous pneumothorax due to ruptured apical bullae
Footnotes: 55 year old male with sudden severe breathlessness and right-sided pleuritic chest pain. Chest CT showed loculated pneumothorax due to pleural adhesions. Apical lung bullae or blebs that predispose to spontaneous pneumothorax. These blebs are not on the background of bullous emphysema.
[Source 249 ]How common is spontaneous collapsed lung?
Spontaneous collapsed lung or pneumothorax occurs more frequently in adults than children and more frequently in males than females 250. Spontaneous pneumothorax is a common clinical presentation, with 14.1 admissions per 100 000 people per year aged ≥15 years 251. In the United States, the adult incidence of primary spontaneous pneumothorax is estimated to be 7.4 per 100,000 to 18 per 100,000 people per year in males and 1.2 per 100,000 to 6.0 per 100,000 people per year in females, with similar rates of secondary spontaneous pneumothorax in males and females, 6.3 and 2.0 per 100,000 people per year, respectively 250. In children, the combined incidence of spontaneous pneumothorax is estimated to be 4.0 per 100,000 children per year in males and 1.1 per 100,000 children per year in females. Other risk factors include a history of smoking, and a tall, thin body habitus 252, 253.
What is a small and large collapsed lung?
Estimating the size of collapsed lung or pneumothorax is somewhat controversial with no international consensus. Chest CT scan is considered more accurate than plain chest X-ray.
British Thoracic Society (BTS) guidelines (2010) measured from chest wall to lung edge at the level of the hilum 254:
- <2 cm: Small
- ≥2 cm: Large
American College of Chest Physicians guidelines (ACCP) measured from thoracic cupola to lung apex 255:
- <3 cm: Small
- ≥3 cm: Large
Expert group considers a pneumothorax as large when there is a visible rim along the entire axillary line, ≥ 2 cm between the lung margin and the chest wall at the hilum level 256.
Figure 28. Large collapsed lung size
Footnotes: Estimation of size of a pneumothorax based on routine chest X-ray. (a) The American College of Chest Physicians (ACCP) generally use the intrapleural distance from the apex to the cupola of the lung, whereas the British Thoracic Society (BTS) uses the intrapleural distance at the hilum (b).
[Source 257 ]How serious is a collapsed lung?
The seriousness of a collapsed lung or pneumothorax depends on the cause and how much of your lung is collapsed. Some cases aren’t serious, and some are medical emergencies. Pneumothorax can be caused by a variety of health problems, and some can be life-threatening, so seek medical attention. If your chest pain is severe or breathing becomes increasingly difficult, get immediate emergency care.
Your doctor can tell you how much of your lung is collapsed and what your treatment options are. The goal in treating a pneumothorax is to relieve the pressure on your lung, allowing it to re-expand. Treatment options may include observation, needle aspiration, chest tube insertion, nonsurgical repair or surgery. You may receive supplemental oxygen therapy to speed air reabsorption and lung expansion.
How long does it take for a collapsed lung to heal?
If the collapsed lung or pneumothorax is small, the leak usually heals itself and the trapped air is gradually absorbed by your body. This normally takes 1 to 2 weeks. You can use over-the-counter painkillers to manage your pain and you might also be given oxygen.
What is the recurrence rate of primary spontaneous pneumothorax?
Primary spontaneous pneumothorax recurrence rates vary widely in the published literature, with limited data describing the factors that influence recurrence. This systematic review showed a 32% recurrence rate in primary spontaneous pneumothorax, with greatest risk in the first year 258. There are no established factors that predict pneumothorax recurrence and consequently no method for risk-stratifying patients. Female sex, low body weight (lower BMI), smoking and height in males have all been postulated as risk factors for higher risk of pneumothorax recurrence 259, 260, 261, 262. Certain radiographic features have also been suggested to confer additional risk, including bullae on computed tomography (CT) and pleural thickening on chest radiography 263, 264, 265. Importantly, there is no consensus on which treatment offers the greatest reduction in risk of pneumothorax recurrence 266, 267, 268, 269.
Is chest tube drainage superior to conservative strategy?
A single study has assessed the conservative strategy in patients with a first episode of a large unilateral primary spontaneous pneumothorax 270. This multicenter, open-label, randomized controlled trial included 316 patients aged 14 to 50 years: 154 in the chest tube drainage and hospitalization (“standard”) arm and 162 in the conservative strategy arm.
The conservative management was non-inferior to the “standard” management on the primary endpoint (eight weeks radiographic resolution) 270. The risk of ipsilateral recurrence at one year was lower in the conservative arm (8.8% vs 16.8%) 270, 266. However, these data should be considered with caution as 1-year recurrence rate was lower than usual in both arms, 29% in the meta-analysis by Walker et al 271. The conservative strategy allowed reducing the number of procedures (percutaneous pleural procedures, need for surgery, imaging), the hospital length of stay, the rate of adverse events and the number of days out of work 270. The failure rate of the conservative strategy (defined as the need for chest tube drainage) ranged between 15 and 21% 270, 272.
However, some biases limit its conclusions, rending questionable and hardly generalizable these results:
- In sensitivity analyzes, if all lost to follow-up patients are considered as “failures”, the difference in success at eight weeks exceeds the non-inferiority limit and the study is negative, with conservative management less effective than chest tube drainage;
- There might be an inclusion bias, as only 316 patients out of the 2637 screened were included;
- The type of included patients seems unusual: the duration of primary spontaneous pneumothorax evolution was about of 40 hours, the patients being barely asymptomatic (median dyspnea and pain visual analog scale scores respectively of 1 and 2 on 10-points scales).
Further studies are needed to assess the safety and better define the profile of patients who could benefit from a conservative strategy.
Is chest tube drainage superior to needle aspiration?
Needle aspiration requires a transient pleural approach, performed until bubbling stops 273, 274, until aspiration is no longer possible 275, 276, until a fixed volume is aspirated 277, 276, 278 or for a maximal time 273, 274, 275. If needle aspiration is not sufficient, studies suggest either switching to chest tube drainage 279, 274, 280, 281, 282 or to attempt a second (or a third) needle aspiration 273, 274, 275, 283, although not recommended 284, 285. Needle aspiration failure is defined as an attempted needle aspiration followed by a chest tube drainage 273, 280, 281, 282, 283.
Chest tube drainage shows a higher “immediate success” rate compared to needle aspiration 273, 286, 276, 287, 288. A later success rate (at day 7 or later), appears similar between chest tube drainage and needle aspiration 275, 289, 286, 278, 290. The overall immediate success rate is 51% for needle aspiration (after 1 − 3 procedures) and about 68% for chest tube drainage 273, 275, 277, 289, 278, 283, 291.
Needle aspiration reduces the hospital length of stay compared chest tube drainage (i.e. with hospitalization) 273, 275, 277, 289, 278, 283, 291, 292, 288.
Needle aspiration allowed decreasing drainage duration compared to chest tube drainage in an randomized controlled trial 278.
The risk of complications is rarely reported and lower during needle aspiration than chest tube drainage 275, 276, 290. One study found similar complication rates between needle aspiration and chest tube drainage 283.
Conflicting data exist in pain. Although some report less pain with needle aspiration 275, 290 and higher analgesic use in chest tube drainage 275, older studies did not report any difference between techniques 273, 283.
Treatment satisfaction did not differ between needle aspiration and chest tube drainage 283.
Surgery rate did not differ between needle aspiration and chest tube drainage 283, 278. A single old study, of low level of evidence, reported a more frequent need for pleurectomy in chest tube drainage as compared to needle aspiration 277.
Costs had not been analyzed in these studies. The 2017 Cochrane Database considered that no conclusion was possible 293. However, as needle aspiration reduces the hospital length of stay as compared to chest tube drainage, the cost of such management would be lower. Dedicated medico-economic studies are needed.
One-year (and sometimes 3 months) recurrence rates did not differ between needle aspiration and chest tube drainage 273, 275, 277, 289, 286, 287, 290, 291.
Based on these findings, needle aspiration might appear superior to chest tube drainage. Given the possibility of an outpatient management with a chest tube drainage, these two approaches were kept as first-line management of large primary spontaneous pneumothorax.
Is chest tube drainage superior to surgery?
Seventy percent of patients with a first primary spontaneous pneumothorax will never relapse. Therefore, performing surgery at first episode of primary spontaneous pneumothorax seems too invasive 271. However, several studies compared surgical treatment (pleurodesis and bleb removal) following chest tube drainage or needle aspiration to a conventional chest tube drainage strategy without surgery during a first episode of large primary spontaneous pneumothorax. These studies reported a reduced one-year risk of recurrence, a shorter length of stay, a lower cost and no difference in analgesic for surgically treated patients compared to conventional chest tube drainage 294, 295, 296, 297, 298, 299. These studies had several biases drawing the conclusion was not easy.
Is outpatient superior to inpatient management?
No high-quality study has directly compared the outpatient management with needle aspiration versus mini-chest tube drainage with one-way valve. At least one such study is ongoing (PNEUM-AMBU, NCT03691480) 300.
Exclusive outpatient management is feasible in 4 out of 5 patients treated with needle aspiration or chest tube drainage with a one-way valve 301, 302, 303.
Compared with inpatient care, outpatient management reduces the hospital length of stay, as reported in a study comparing a drainage system with an integrated one-way valve versus a standard management with needle aspiration in most cases (68% of patients in the control arm) 303. In most other publications, outpatient needle aspiration has been compared to drainage with hospital-based monitoring. Series reporting outpatient management have also suggested a reduced hospital length of stay but without control arm 304, 302, 301, 305.
Use of surgery was not assessed specifically in study reporting outpatient strategy.
Outpatient management could increase the complications rates as compared to inpatient management 303. However, the design of this prospective study explains most of the severe complications, as adverse events were defined as the need for hospitalization, which could only concern patients of the outpatient arm.
On the other hand, in observational studies, no serious adverse events were reported, but mainly bent or displaced catheters (ranging from 1.5% to 22.6%) 304, 302, 301, 305.
Outpatient management was associated with a similar 1-year recurrence rate as inpatient management, ranging from 12% to 33.1% 304, 302, 301, 305, 301.
Indirect evidence suggest a lower overall health care costs of outpatient management 304, 302.
Expert group recommends outpatient management in patients with large primary spontaneous pneumothorax without signs of immediate severity 256.
The expert group recommends an outpatient management based on needle aspiration or on mini-chest tube with one-way valve, if the following criteria are met 256:
- the patient is stable after intrapleural air removal,
- and a dedicated outpatient care system is previously organized
- and a consultation with chest ultrasound or chest X-ray is scheduled at 24−72 hour to assess the evolution.
The expert group proposes outpatient management of primary spontaneous pneumothorax only if all of the following conditions are met 256:
- A patient information leaflet providing guidance on the way to behave in case of problem and phone numbers available 24/7, is given to the patient before hospital discharge,
- Patient’s comprehension of discharge instructions has been checked
- The patient should not stay alone for the first 24 − 48 hour after being discharged home,
- The patient should be able to access a medical facility within 1 hour, regardless of the means of transportation, in the event of deterioration,
- The time of discharge does not matter if all of the above criteria are met (nighttime discharge is possible).
Types of collapsed lung
There are different types of collapsed lung or pneumothorax:
Spontaneous pneumothorax
Spontaneous pneumothorax is a collapsed lung that happens without an injury. Spontaneous pneumothorax types include:
Primary spontaneous pneumothorax
Primary spontaneous pneumothorax is the most common type of pneumothorax, has no known cause and develops in otherwise healthy people. Primary spontaneous pneumothorax is thought to be caused by a tiny tear of an outer part of the lung. This can happen if abnormal air pockets in your lung (blebs) break apart and release air. Primary spontaneous pneumothorax is more common in tall people and mainly affects healthy young adults without lung disease.
Secondary spontaneous pneumothorax
Secondary spontaneous pneumothorax develops as a complication of existing lung disease, such as chronic obstructive pulmonary disease (COPD), pneumonia, tuberculosis, sarcoidosis or cystic fibrosis. The lung disease weakens the edge of the lung in some way, making the lung more likely to tear and cause air to escape.
Catamenial pneumothorax
Catamenial pneumothorax is a pneumothorax occurring during the perimenstrual period that affect women with endometriosis 306. “Perimenstrual period” encompasses the period of 72 – 96 hours before and after menstrual bleeding. Endometrial tissue growing outside of your uterus can form cysts that can bleed into the pleural space, causing your lung to collapse.
The broadest definitions of catamenial pneumothorax describe it as pneumothorax occurring from 7 days before the start of monthly bleeding to 7 days after its completion 307. The additional criteria include: characteristic pleural lesions, right-sided location of the pneumothorax, and concomitant endometriosis 308, 309. Concomitance of catamenial pneumothorax and endometriosis was described in a woman in the 8th week of pregnancy 310. Thoracic endometriosis is defined as the presence of ectopic endometrium within the chest, the symptoms of which appear during ovulation 311. Symptoms of pelvic endometriosis, secondary or primary infertility, and previous gynecological procedures 308 may suggest the diagnosis of catamenial pneumothorax in the course of endometriosis. A review of the treatment results of 110 patients with thoracic endometriosis revealed that pneumothorax occurred in 72% of the women, hemoptysis in 14%, pleural hematomas in 12%, and lung nodules in 2% 311. Pelvic endometriosis may precede the development of thoracic endometriosis by 5 years 312. Despite the fact that the most common manifestation of thoracic endometriosis is pneumothorax 311, in some cases of catamenial pneumothorax, endometrial character of the disease cannot be confirmed histologically 307. Abnormal fenestrations in the tendinous part of the diaphragm can be observed during surgical procedures performed on patients suffering from catamenial pneumothorax concomitant with endometriosis. Furthermore, the patients’ pleurae feature spots and nodules which are endometrial implants. The lesions are most often located on the diaphragmatic pleura.
3% to 6% of spontaneous pneumothorax cases meet the definition of catamenial pneumothorax, constituting an indication for surgical treatment in 1/3 of the affected women. The mean age of onset is 32-35 years 313. The condition may develop as late as at 39 years of age 314. Catamenial pneumothorax is most often (85-95%) unilateral, occurring on the right side of the chest, but it may also occur on the left side or bilaterally 314.
The cause and subsequent development of catamenial pneumothorax is explained by the following theories: physiological, migrational, microembolic-metastatic, and the diaphragmatic theory of air “passage” (Table 1).
Catamenial pneumothorax is associated with the following findings: single or multiple fenestrations in the tendinous part of the diaphragm; red/brown spots or nodules located on the diaphragmatic or visceral pleura. Histopathological analysis of these nodules (spots) reveals glandular cells, endometrial stroma, and macrophages filled with hemosiderin, whereas immunohistochemical testing may demonstrate the presence of estrogen and progesterone receptors 315. These findings are observed if pneumothorax is accompanied by endometriosis, especially within the pelvis, as occurs in 30-51% of cases.
Table 10. Theories for the development of thoracic foci of endometriosis in the development of catamenial pneumothorax
| Physiological | High concentration of prostaglandin F2 during menses may cause blood vessels and bronchioles to contract, which leads to alveolar rupture and development of pneumothorax. |
| Migrational | Endometrial cells may migrate from the uterus, through the fallopian tubes, into the lesser pelvis and further, into the area of the diaphragm. The cyclical proliferation and necrosis of endometrial cells may injure the diaphragm, enabling the cells to migrate further into the chest and the visceral pleura, which may lead to pulmonary alveolar injury and pneumothorax. |
| Microembolic-metastatic | Metastatic spread or pulmonary microembolization from endometrial cells through blood or lymph vessels. Necrosis of subpleural interstitial endometriotic foci leads to pneumothorax; foci located more centrally cause hemoptysis. |
| Diaphragmatic theory of air “passage” | Air passes through the uterus and fallopian tubes into the peritoneal cavity and, through diaphragmatic fenestrations, into the pleural cavity. |
Traumatic pneumothorax
Traumatic pneumothorax is a type of pneumothorax is caused by an incident such as a car accident, broken ribs or a stab wound.
Iatrogenic pneumothorax
Iatrogenic pneumothorax is a pneumothorax that occurs as a result of mechanical ventilation, which causes an imbalance in the air pressure around the lungs. Iatrogenic pneumothorax is also caused by a medical procedure when your lung is punctured during a lung biopsy or a central venous line insertion.
Tension pneumothorax
Progression of collapsed lung
Excluding that caused by chest trauma, collapsed lung or pneumothorax arises due to rupture of alveoli, followed by rupture of the pleural lining of the lung. Provided this communication then seals itself off, air in the pleural space is gradually resorbed. If the communication between the pleural space and the airways remains open, a ‘bronchopleural fistula’ is created.
Rarely, the communication remains open, but the defect acts as a flap valve, allowing air into the pleural space on inspiration, but preventing it from escaping during expiration. Thus, air accumulates in the pleural space with each breath, compressing adjacent lung, and eventually compressing other structures in the chest, including the heart. This is called ‘tension pneumothorax’. Tension pneumothorax rarely occurs spontaneously.
Collapsed lung prognosis (outlook)
Tension pneumothorax is a potentially life-threatening condition, due to restriction of venous return, and respiratroy and cardiac shock. Otherwise, pneumothorax tends to slowly resolve, such that a pneumothorax causing 50% collapse of the lung will take 40 days to heal.
Collapsed lung complications
Many people who have had one collapsed lung or pneumothorax can have another, usually within one to two years of the first. Air may sometimes continue to leak if the opening in the lung won’t close. Surgery may eventually be needed to close the air leak.
Although most collapsed lungs heal without issues, some people have serious complications. These can include:
- Re-expansion pulmonary edema.
- Damage or infection caused by the treatment.
- Respiratory failure.
- Heart failure.
Collapsed lung causes
A collapsed lung or pneumothorax can be caused by:
- Chest injury. Any blunt or penetrating injury to your chest can cause lung collapse. Some injuries may happen during physical assaults (gunshot wound, stab wound) or car crashes, while others may inadvertently occur during medical procedures that involve the insertion of a needle into your chest for a nerve block, lung biopsy or central venous line placement.
- Lung disease. Damaged lung tissue is more likely to collapse. Lung damage can be caused by many types of underlying diseases, including chronic obstructive pulmonary disease (COPD), cystic fibrosis, asthma, pneumonia, tuberculosis, idiopathic pulmonary fibrosis, emphysema, lung cancer, acute respiratory distress syndrome (ARDS), lymphangioleiomyomatosis or collagen vascular disease (a group of autoimmune disorders that cause the body’s immune system to attack its own tissues).
- Ruptured air blisters. Small air blisters (blebs) can develop on the top of your lung. These blebs sometimes burst — allowing air to leak into the space that surrounds the lungs.
- Mechanical ventilation. A severe type of pneumothorax can occur in people who need mechanical assistance to breathe. The ventilator can create an imbalance of air pressure within the chest. The lung may collapse completely.
- Lifestyle factors such as drug use, especially inhaled drugs, smoking, flying that involves drastic changes in air pressure or scuba or deep-sea diving.
Risk factors for a collapsed lung
Pneumothorax in those over 40 years of age is commonly seen in the background of emphysema or chronic bronchitis. Occasionally, asthma, and other lung disease can cause a pneumothorax.
In younger patients, pneumothorax may occur spontaneously or due to chest trauma. Spontaneous pneumothorax commonly occurs in tall, thin young men (sex ratio: 6:1), due to rupture of small subpleural ‘blebs’. Trauma such as a rib fracture, or penetrating chest wall injury, may also cause pneumothorax.
Risk factors for a pneumothorax include:
- Your sex. In general, men are far more likely to have a pneumothorax than are women.
- Smoking. The risk increases with the length of time and the number of cigarettes smoked, even without emphysema.
- Age. The type of pneumothorax caused by ruptured air blisters is most likely to occur in people between 20 and 40 years old, especially if the person is a very tall and underweight.
- Genetics. Certain types of pneumothorax appear to run in families.
- Lung disease. Having an underlying lung disease — especially chronic obstructive pulmonary disease (COPD) — makes a collapsed lung more likely.
- Mechanical ventilation. People who need mechanical ventilation to assist their breathing are at higher risk of pneumothorax.
- Previous pneumothorax. Anyone who has had one pneumothorax is at increased risk of another, usually within one to two years of the first.
- Pregnancy
- Have a tall, thin body type, especially if you are a man.
- Marfan syndrome.
- Endometriosis.
Collapsed lung signs and symptoms
The presentation of patients with pneumothorax varies depending on the types of pneumothorax and ranges from completely asymptomatic to life-threatening respiratory distress:
- Spontaneous pneumothorax: No clinical signs or symptoms in primary spontaneous pneumothorax until a bleb ruptures and causes pneumothorax; typically, the result is acute onset of chest pain and shortness of breath, particularly with secondary spontaneous pneumothoraces
- Iatrogenic pneumothorax: Symptoms similar to those of spontaneous pneumothorax, depending on patient’s age, presence of underlying lung disease, and extent of pneumothorax
- Tension pneumothorax: Hypotension, hypoxia, chest pain, dyspnea
- Catamenial pneumothorax: Women aged 30-40 years with onset of symptoms within 48 hours of menstruation, right-sided pneumothorax, and recurrence
- Pneumomediastinum: Must be differentiated from spontaneous pneumothorax; patients may or may not have symptoms of chest pain, persistent cough, sore throat, dysphagia, shortness of breath, or nausea/vomiting.
The main symptoms of a collapsed lung or pneumothorax are sudden chest pain and shortness of breath. But these symptoms can be caused by a variety of health problems, and some can be life-threatening. If your chest pain is severe or breathing becomes increasingly difficult, get immediate emergency care.
Tension pneumothorax
Signs and symptoms of tension pneumothorax are usually more impressive than those seen with a simple pneumothorax, and clinical interpretation of these is crucial for diagnosing and treating the condition. Tension pneumothorax is classically characterized by hypotension (low blood pressure) and hypoxia (low blood oxygen). On examination, breath sounds are absent on the affected hemothorax and the trachea deviates away from the affected side. The thorax may also be hyperresonant; jugular venous distention and tachycardia may be present. If on mechanical ventilation, the airway pressure alarms are triggered.
Because of subtle presentations that do not always present with the classically described clinical findings of this condition or the complexity of the patient with critical illness or injury to describe a tension pneumothorax, actual case reports include descriptions of the diagnosis of the condition being missed or delayed. Nevertheless, tension pneumothorax should always be a consideration when acute compromise occurs.
Symptoms of tension pneumothorax may include chest pain (90%), dyspnea (80%), anxiety, fatigue, or acute epigastric pain (a rare finding).
Catamenial pneumothorax
The symptoms of catamenial pneumothorax are typical of spontaneous pneumothorax, but the condition may also be asymptomatic.
Women aged 30-40 years who present with onset of symptoms within 48 hours of menstruation, right-sided pneumothorax, and recurrence raise suspicion for catamenial pneumothorax.
Pneumomediastinum
Pneumomediastinum must be differentiated from spontaneous pneumothorax. Patients may or may not have symptoms, as this is typically a well-tolerated disease, although mortality in cases of esophageal rupture is very high.
This condition usually occurs when intrathoracic pressures become elevated, such as with an exacerbation of asthma, coughing, vomiting, childbirth, seizures, and a Valsalva maneuver. In many patients who present with pneumomediastinum, it occurs as a result of endoscopy and small esophageal perforation.
In a retrospective review of cases presenting to an academic medical center, 67% of identified patients had chest pain; 42% had persistent cough; 25% had sore throat; and 8% had dysphagia, shortness of breath, or nausea/vomiting.
Other symptoms may include substernal chest pain, usually radiating to the neck, back, or shoulders and exacerbated by deep inspiration, coughing, or supine positioning; dyspnea; neck or jaw pain; dysphagia, dysphonia, and/or abdominal pain (unusual symptoms).
Traumatic mediastinum, although present in up to 6% of patients, does not portend serious injury 316.
Collapsed lung diagnosis
If you have a sudden onset of shortness of breath or sharp chest pain that is worsened by breathing, go to the Emergency Room to be evaluated or call your local emergency number. In order to make an accurate diagnosis, the medical team will evaluate your symptoms and perform a physical exam, including the following:
- History: Your physician will obtain your full medical history, in addition to assessing the symptoms you’re currently experiencing. You may be asked questions about when the symptoms started, the severity of the pain or shortness of breath, and length of time you waited prior to arriving to the Emergency Room.
- Physical exam: Using a stethoscope, your doctor will listen for decreased or no breath sounds on the affected side.
- Chest X-ray: This radiologic test will show a pneumothorax if it is present. Perform frontal chest X-ray in inspiration, without expiratory films, in case of suspected spontaneous pneumothorax to diagnose it and assess its size.
- In some cases, a chest computerized tomography (CT) scan (low-dose chest CT-scan) may be needed to provide more-detailed images. The chest CT-scan is superior to the chest X-ray for assessing the size of a pneumothorax and to determine secondary pneumothorax causes 317. However, the cost, time and radiation exposure do not support its use as a first-line examination.
- Chest ultrasound imaging also may be used to identify a pneumothorax. The added value of chest ultrasound is currently for chest trauma patients or the diagnosis of iatrogenic pneumothorax, with a high pretest probability 318, 319.
Physical Examination
The presentation of a patient with pneumothorax may range from completely asymptomatic to life-threatening respiratory distress. Symptoms may include diaphoresis, splinting chest wall to relieve pleuritic pain, and cyanosis (in the case of tension pneumothorax). Findings on lung auscultation also vary depending on the extent of the pneumothorax. Affected patients may also reveal altered mental status changes, including decreased alertness and/or consciousness (a rare finding).
Respiratory findings may include the following:
- Respiratory distress (considered a universal finding) or respiratory arrest
- Tachypnea (or bradypnea as a preterminal event)
- Asymmetric lung expansion – A mediastinal and tracheal shift to the contralateral side can occur with a large tension pneumothorax
- Distant or absent breath sounds – Unilaterally decreased or absent lung sounds is a common finding, but decreased air entry may be absent even in an advanced state of the disease
- Lung sounds transmitted from the unaffected hemithorax are minimal with auscultation at the midaxillary line
- Hyperresonance on percussion – This is a rare finding and may be absent even in an advanced state of the disease
- Decreased tactile fremitus
- Adventitious lung sounds (crackles, wheeze; an ipsilateral finding)
Cardiovascular findings may include the following:
- Tachycardia – This is the most common finding. If the heart rate is faster than 135 beats/min, tension pneumothorax is likely
- Pulsus paradoxus
- Hypotension – This should be considered as an inconsistently present finding; although hypotension is typically considered a key sign of a tension pneumothorax, studies suggest that hypotension can be delayed until its appearance immediately precedes cardiovascular collapse
- Jugular venous distention – This is generally seen in tension pneumothorax, although it may be absent if hypotension is severe
- Cardiac apical displacement – This is a rare finding
Spontaneous and iatrogenic pneumothorax
Signs of spontaneous and iatrogenic pneumothorax are similar and depend on the underlying lung disease and extent of the pneumothorax. Tachycardia is the most common finding, and tachypnea and hypoxia may be present.
Tension pneumothorax
Although tension pneumothorax may be a difficult diagnosis to make and may present with considerable variability in signs, respiratory distress and chest pain are generally accepted as being universally present, and tachycardia and ipsilateral air entry on auscultation are also common findings. Sometimes, reliance on history alone may be warranted.
Findings may be affected by the volume status of the patient. In hypovolemic trauma patients with ongoing hemorrhage, the physical findings may lag behind the presentation of shock and cardiopulmonary collapse. Increased pulmonary artery pressures and decreased cardiac output or cardiac index are evidence of tension pneumothorax in patients with Swan-Ganz catheters.
When examining a patient for suspected tension pneumothorax, any clue may be helpful, as subtle thoracic size and thoracic mobility differences may be elicited by performing careful visual inspection along the line of the thorax. In a supine patient, the examiner should lower themselves to be on a level with the patient.
Tracheal deviation is an inconsistent finding. Although historic emphasis has been placed on tracheal deviation in the setting of tension pneumothorax, tracheal deviation is a relatively late finding caused by midline shift.
Abdominal distention may occur from increased pressure in the thoracic cavity producing caudal deviation of the diaphragm and from secondary pneumoperitoneum produced as air dissects across the diaphragm through the pores of Kohn.
If patients who are mechanically ventilated are difficult to ventilate during resuscitation, high peak airway pressures are clues to pneumothorax. A tension pneumothorax causes progressive difficulty with ventilation as the normal lung is compressed. On volume-control ventilation, this is indicated by marked increase in both peak and plateau pressures, with relatively preserved peak and plateau pressure difference. On pressure control ventilation, tension pneumothorax causes sudden drop in tidal volume. However, these observations are neither sensitive nor specific for making the diagnosis of pneumothorax or ruling out the possibility of pneumothorax.
The development of tension pneumothorax in patients who are ventilated will generally be of faster onset with immediate, progressive arterial and mixed venous oxyhemoglobin saturation decline and immediate decline in cardiac output. Cardiac arrest associated with asystole or pulseless electrical activity (PEA) may ultimately result. Occasionally, the tension pneumothorax may be tolerated and its diagnosis delayed for hours to days after the initial insult. The diagnosis may become evident only if the patient is receiving positive-pressure ventilation. Tension pneumothorax has been reported during surgery with both single- and double-lumen tubes.
Pneumomediastinum
As with pneumothorax, physical findings of pneumomediastinum may be variable, including absent signs in some patients. However, subcutaneous emphysema is the most consistent sign. Another sign, the Hamman sign—a precordial crunching noise synchronous with the heartbeat and often accentuated during expiration—has a variable rate of occurrence, with one series reporting 10%.
Catamenial pneumothorax
Bagan et al. point to the increase in the serum titer of the CA125 antigen as a helpful marker of catamenial pneumothorax associated with endometriosis 320. In accordance with the presented data, the value of CA125 that indicates high probability of endometriosis is 76 U/ml. In a study published by Haga in 2013, an increase of the Ca125 antigen to 36.7 ±42.3 U/ml was considered significant 314. However, the marker is not specific, which limits its routine use.
Collapsed lung treatment
The goal in treating a collapsed lung or pneumothorax is to relieve the pressure on your lung, allowing it to re-expand. Depending on the cause of the pneumothorax, a second goal may be to prevent recurrences. The methods for achieving these goals depend on the severity of the lung collapse and sometimes on your overall health.
Selection among various management options in pneumothorax requires an understanding of the natural history of pneumothorax, the risk of recurrent pneumothorax, and the benefits and limitations of treatment options. Observation without oxygen, administering supplemental oxygen, simple aspiration, chest tube placement, video-assisted thoracoscopic surgery (VATS), open thoracotomy, and pleurodesis are among these options.
- Small pneumothorax may not require treatment. If only a small portion of your lung is collapsed, your doctor may simply monitor your condition at 2-weekly intervals with a series of chest X-rays until the excess air is completely absorbed and your lung has re-expanded. Normally this takes a week or two. Supplemental oxygen may speed the absorption process.
- Larger, and tension, pneumothorax requires aspiration of air (needle passed between the ribs, into the pleural space), with insertion of an intercostal drainage tube soon after. This drainage tube ends with an underwater seal; thus, escaping air is seen as bubbles in the water, but air from the atmosphere can not go back in.
- Occasionally, the pneumothorax keeps bubbling after several days; this indicates the presence of bronchopleural fistula, and surgery may be needed. This involves either removal of the pleura, or adhesion of the two pleural layers to each other, by placing talc in the pleural space (talc pleurodesis).
- A tension pneumothorax should be treated with immediate decompression with a needle in the 2nd intercostal space (between the second and third rib at the front). This is then followed by a formal intercostal tube insertion as above.
- Treatment for catamenial pneumothorax involves hormonal therapy and surgical treatment (wedge lung resection, pleurectomy, chemical or mechanical pleurodesis, and diaphragm reconstruction – direct or using synthetic meshes) 306. Video-assisted thoracoscopic surgery (VATS) is the access of choice in the treatment of pneumothorax. Thoracotomy is indicated almost exclusively in cases of recurrence after a previous procedure. The use of video-assisted mini-thoracotomy has been suggested if the procedure involves extensive lesions within the diaphragm 308. Most authors are in agreement in their recommendations to perform bullectomy, pleurectomy, or pleurodesis.
Observation
If only a small portion of your lung is collapsed, your doctor may simply monitor your condition with a series of chest X-rays until the excess air is completely absorbed and your lung has re-expanded. This may take several weeks.
Needle aspiration or chest tube insertion
If a larger area of your lung has collapsed, it’s likely that a needle or chest tube will be used to remove the excess air.
- Needle aspiration. A hollow needle with a small flexible tube (catheter) is inserted between the ribs into the air-filled space that’s pressing on the collapsed lung. Then the doctor removes the needle, attaches a syringe to the catheter and pulls out the excess air. The catheter may be left in for a few hours to ensure the lung is re-expanded and the pneumothorax does not recur.
- Chest tube insertion. A flexible chest tube is inserted into the air-filled space and may be attached to a one-way valve device that continuously removes air from the chest cavity until your lung is re-expanded and healed.
Nonsurgical repair
If a chest tube doesn’t re-expand your lung, nonsurgical options to close the air leak may include:
- Chemical pleurodesis: Using a substance (such as doxycycline or talcum powder to irritate the tissues around your lung so that they’ll stick together and seal any leaks. This can be done through the chest tube, but it may be done during surgery.
- Drawing blood from your arm and placing it into the chest tube. The blood creates a fibrinous patch on the lung (autologous blood patch), sealing the air leak.
- Passing a thin tube (bronchoscope) down your throat and into your lungs to look at your lungs and air passages and placing a one-way valve. The valve allows the lung to re-expand and the air leak to heal.
Surgery
Sometimes surgery may be necessary to close the air leak. In most cases, the surgery can be performed through small incisions, using a tiny fiber-optic camera and narrow, long-handled surgical tools. The surgeon will look for the leaking area or ruptured air blister and close it off.
Rarely, the surgeon will have to make a larger incision between the ribs to get better access to multiple or larger air leaks.
Ongoing care
You may need to avoid certain activities that put extra pressure on your lungs for a time after your pneumothorax heals. Examples include flying, scuba diving or playing a wind instrument. Talk to your doctor about the type and length of your activity restrictions. Keep follow-up appointments with your doctor to monitor your healing.
Broken rib
A broken rib also called a rib fracture is a common injury that occurs when one of the bones in your rib cage breaks or cracks. The most common cause is strong blunt force trauma to your chest, such as from a fall, motor vehicle accident, a hit with a baseball bat or impact during contact sports. However, sometimes in older people who have osteoporosis, only a slight force as occurs in a minor fall is required.
Many broken ribs are merely cracked. While still painful, cracked ribs aren’t as potentially dangerous as ribs that have been broken into separate pieces. A jagged edge of broken bone can damage major blood vessels or internal organs, such as your lung.
The fracture itself is rarely serious, although the force that caused the fracture occasionally causes other problems, such as a bruised lung (pulmonary contusion) or a collapsed lung (pneumothorax). An injury that fractures your lower ribs sometimes also damages your liver or spleen. The more ribs that are broken, the more likely your lungs or other organs are to be damaged.
Flail chest can result if several adjacent ribs are broken in more than one place. In flail chest, a segment of your chest wall separates from the rest and moves in the opposite direction from the rest of your chest wall when you breathe. Breathing becomes more difficult and tiring. Usually, a blow strong enough to cause flail chest also bruises your lung beneath the injured area.
In most cases, broken ribs usually heal on their own in one or two months (most broken ribs heal on their own within 6 weeks). Adequate pain control is important so that you can continue to breathe deeply and avoid lung complications, such as pneumonia.
See your doctor if you have a very tender spot in your rib area that occurs after trauma or if you have difficulty breathing or pain with deep breathing.
Seek medical attention immediately if you feel pressure, fullness or a squeezing pain in the center of your chest that lasts for more than a few minutes or pain that extends beyond your chest to your shoulder or arm. These symptoms can indicate a heart attack.
Ribs anatomy
You have twelve pairs of ribs, numbered 1 to 12 from superior (top) to inferior (bottom). Your ribs give structural support to the sides of your thoracic cavity (chest cavity). The ribs increase in length from the first through seventh (ribs #1 to ribs #7) and then decrease in length to rib 12. Each rib articulates posteriorly with its corresponding thoracic vertebra.
Ribs #1 to ribs #7 have a direct anterior attachment to the sternum by a strip of hyaline cartilage called costal cartilage. The costal cartilages contribute to the elasticity of the thoracic cage and prevent various blows to the chest from fracturing the sternum and/or ribs. The ribs that have costal cartilages and attach directly to the sternum are called true (vertebrosternal) ribs. The articulations formed between the true ribs and the sternum are called sternocostal joints. The remaining five pairs of ribs (ribs #8 to ribs #12) are termed false ribs because their costal cartilages either attach indirectly to the sternum or do not attach to the sternum at all (see ribs #11 to ribs #12). The cartilages of the eighth, ninth, and tenth pairs of ribs attach to one another and then to the cartilages of the seventh pair of ribs. These false ribs are called vertebrochondral ribs. The eleventh and twelfth pairs of ribs are false ribs designated as floating (vertebral) ribs because the costal cartilages at their anterior ends do not attach to the sternum at all. These ribs attach only posteriorly to the thoracic vertebrae. Inflammation of one or more costal cartilages, called costochondritis, is characterized by local tenderness and pain in the anterior chest wall that may radiate. The symptoms mimic the chest pain (angina pectoris) associated with a heart attack.
The ribcage is supported by ligaments and muscles, including the muscles between the ribs (intercostal muscles). These muscles allow the ribcage to expand when you breathe in and to drop when you breathe out.
The curved design of the ribs makes them resistant to fractures. Their ability to flex helps the bone to absorb the force of a blow. However, any bone will break if the force exerted against it is stronger than it can structurally withstand. A rib is most likely to fracture at its outer curve, which is its weakest point.
Older people are more prone to rib fractures because bones thin with age. Children are less likely to break ribs because their bones are relatively flexible.
Figure 29. Ribs
Figure 31. Rib articulation with the thoracic vertebra
Broken rib complications
A broken rib can injure blood vessels and internal organs. The risk increases with the number of broken ribs. Complications vary depending on which ribs break.
The ribs enclose vital organs such as the heart and lungs, so chest trauma can cause life-threatening injuries.
Possible complications include:
- Cardiac and torn or punctured aorta – for example, a sharp end of a break in one of the first three ribs at the top of your rib cage could rupture your aorta or another major blood vessel servicing the heart (coronary artery)
- Pneumothorax – collapsed lung due to changes in pressure within the chest. This could be caused by a broken rib tearing the lung or a puncture in the chest wall. Symptoms can include breathing difficulties, chest pain and coughing up blood.
- Lacerated spleen, liver or kidneys. The bottom two ribs rarely fracture because they have more flexibility than do the upper and middle ribs, which are anchored to the breastbone. But if you break a lower rib, the broken ends can cause serious damage to your spleen, liver or a kidney. Splenic rupture – the spleen is located on the left side of the abdomen. Its roles include filtering the blood to remove abnormal cells and the manufacture of some immune system cells including antibodies and lymphocytes. Splenic rupture means the outer capsule has split and the spleen bleeds into the abdominal cavity.
Flail chest
Flail chest is the most common serious injury to the ribs. Flail chest occurs when three or more ribs are broken in at least two places, front and back. This will only happen if there has been a great deal of blunt force. The key sign of flail chest is ‘paradoxical movement’, which means the natural movement of the ribcage during breathing is in reverse. For example, the injured area of ribcage sinks in when the person inhales, instead of lifting outwards. This reversal is caused by changes to air pressure in the ribcage as a result of injury. However, it is the accompanying injury to your lungs that usually causes complications, not the broken ribcage. Intubating the person (putting oxygen into the lungs via a tube placed down the trachea, or windpipe) will create a ‘normal’ pressure in the lungs.
If you have:
- An injury caused by a serious accident – such as a car accident
- Shortness of breath that is getting worse
- Chest pain that is getting worse
- Pain in your tummy or shoulder
- Coughing up blood
- Coughing up yellow or green mucus
- Avery high temperature or you feel hot and shivery
It could mean you have a chest infection or that a broken rib has damaged something else like your lung, liver or spleen.
Broken rib causes
Broken ribs are most commonly caused by direct impacts — such as those from motor vehicle accidents, falls, child abuse or contact sports. Ribs also can be fractured by repetitive trauma from sports like golf and rowing or from severe and prolonged coughing.
Blunt force is the common cause of injury
Rib injuries typically occur when the chest is directly hit. Situations that could cause blunt injuries to the ribcage include:
- Motor vehicle accidents – for example, slamming the chest against the steering wheel
- Crush injuries – for example, a heavy object landing directly on the chest
- Sports-related injuries – for example, a heavy tackle
- Falling from a reasonable height – for example, off a roof or ladder
- Assault – for example, getting hit by a baseball bat.
Risk factors for broken ribs
The following factors can increase your risk of breaking a rib:
- Osteoporosis. Having this disease in which your bones lose their density makes you more susceptible to a bone fracture.
- Sports participation. Playing contact sports, such as hockey or football, increases your risk of trauma to your chest.
- Cancerous lesion in a rib. A cancerous lesion can weaken the bone, making it more susceptible to breaks.
Broken rib prevention
The following measures may help you prevent a broken rib:
- Protect yourself from athletic injuries. Wear protective equipment when playing contact sports.
- Reduce your risk of household falls. Remove clutter from your floors and clean spills promptly, use a rubber mat in the shower, keep your home well-lit, and put skidproof backing on carpets and area rugs.
- Strengthen your bones. Getting enough calcium and vitamin D in your diet is important for maintaining strong bones. Aim for about 1,200 milligrams of calcium and 600 International Units of vitamin D daily from food and supplements.
Broken rib signs and symptoms
Broken rib can cause severe pain, particularly when people breathe deeply. The pain lasts for weeks.
Because of the pain, people may breathe less deeply, increasing the risk of complications, such as collapse of parts of the lung (atelectasis) and pneumonia.
Complications are more likely to occur in:
- Older people
- People with several rib fractures
Because older people are more likely to develop these complications, they also have a higher risk of death due to a rib fracture than do younger people.
Broken rib symptoms include:
- Strong pain in your chest area, particularly when you breathe in
- Pain when the ribcage flexes – with movement, with a deep breath or when you cough, sneeze or laugh
- Swelling or tenderness around the affected ribs
- Muscle spasms of the ribcage
- Crunching or grinding sounds (crepitus) when the injury site is touched or moved
- Muscle spasms of the ribcage
- Sometimes bruising on the skin
- Feeling or hearing a crack if it’s a broken rib
- Muscle spasms of the ribcage
Ribs can’t be easily splinted or supported like other bones, so they’re usually left to heal naturally. There’s often no need for an X-ray.
Soft tissue injuries
Soft tissue of the ribcage includes the intercostal muscles and the costal cartilage. Common injuries include:
- Bruising – the blood vessels rupture and leak blood into the surrounding tissues. Bruising of the chest wall is a common rib trauma.
- Intercostal strains – intercostal muscles allow the ribcage to move up and down. These muscles can be strained by any activity that involves extreme or forceful twisting of the body or swinging of the arms. Sports that commonly cause this type of injury include golf and tennis.
- Costochondral separation – the rib is torn loose from the costal cartilage and is detached from the sternum.
Broken rib diagnosis
During the physical exam, your doctor will press gently on your ribs. He or she might also listen to your lungs and watch your rib cage move as you breathe.
Your doctor likely will order one or more of the following imaging tests:
- X-ray. Using low levels of radiation, X-rays make bones visible. But X-rays often have problems revealing fresh rib fractures, especially if the bone is merely cracked. X-rays are also useful in diagnosing a collapsed lung.
- CT scan. This often can uncover rib fractures that X-rays might miss. Injuries to soft tissues and blood vessels are also easier to see on CT scans. This technology takes X-rays from a variety of angles and combines them to depict cross-sectional slices of your body’s internal structures.
- MRI. This can be used to look at the soft tissues and organs around the ribs to determine if there’s damage. It can also help in the detection of more subtle rib fractures. An MRI uses a powerful magnet and radio waves to produce cross-sectional images.
- Bone scan. This technique is good for viewing stress fractures, where a bone is cracked after repetitive trauma — such as long bouts of coughing. During a bone scan, a small amount of radioactive material is injected into your bloodstream. It collects in the bones, particularly in places where a bone is healing, and is detected by a scanner.
Broken rib treatment
Unlike bones of the arms and legs, broken ribs can’t be set in a cast. Most broken ribs heal on their own within six weeks. Treatment aims to relieve pain while the injury heals, which can take up to six weeks (in the case of fracture), and 12 weeks or more if the rib has been torn from the cartilage. Treatment for bruised ribs is the same as for fractured ribs, but with a shorter recovery time.
Restricting activities and icing the area regularly can help with healing and pain relief.
How to treat broken ribs yourself
Options include:
- Rest
- Prescription strength pain-killing drugs
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Avoiding activities that aggravate the injury, such as sport
- Icepacks – may help to reduce inflammation in the early stages
- Mechanical ventilation (help with breathing) – may be needed in cases of severe flail chest.
Medications
It’s important to obtain adequate pain relief — if it hurts to breathe deeply, you may develop pneumonia. If oral medications don’t help enough, your doctor might suggest injections of long-lasting anesthesia around the nerves that supply the ribs.
How to heal broken ribs faster
DO
- take painkillers such as paracetamol or ibuprofen – avoid taking ibuprofen for 48 hours after your injury as it may slow down healing
- hold an ice pack (or bag of frozen peas in a tea towel) to the affected ribs regularly in the first few days to bring down swelling
- rest and take time off work if you need to
- breathe normally and cough when you need to – this helps clear mucus from your lungs to prevent chest infections
- if you need to cough, hold a pillow against your chest
- walk around and sometimes move your shoulders to help you breathe and clear mucus from your lungs
- take 10 slow, deep breaths every hour to help clear your lungs
- try to sleep more upright for the first few nights
DON’T
- wrap a bandage tightly around your chest to stop your lungs expanding properly
- lie down or stay still for a long time
- strain yourself or lift heavy objects
- play any sports or do any exercise that makes your pain worse
- smoke – stopping smoking may also help your recovery
Therapy
Once your pain is under control, your doctor might prescribe breathing exercises to help you breathe more deeply because shallow breathing can put you at risk of developing pneumonia.
- In the past, doctors would use compression wraps — elastic bandages that you can wrap around your chest — to help splint and immobilize the area. Compression wraps aren’t recommended for broken ribs anymore because they can keep you from breathing deeply, which can increase the risk of pneumonia.
- Provenza D, Gillette C, Peacock B, Rejeski J. Managing heartburn and reflux in primary care. JAAPA. 2024 Mar 1;37(3):24-29. doi: 10.1097/01.JAA.0001005620.54669.f4[↩][↩]
- Peery AF, Crockett SD, Murphy CC, Jensen ET, Kim HP, Egberg MD, Lund JL, Moon AM, Pate V, Barnes EL, Schlusser CL, Baron TH, Shaheen NJ, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022 Feb;162(2):621-644. doi: 10.1053/j.gastro.2021.10.017[↩][↩]
- Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022 Jan 1;117(1):27-56. doi: 10.14309/ajg.0000000000001538[↩][↩]
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x[↩][↩][↩]
- Hungin APS, Molloy-Bland M, Scarpignato C. Revisiting Montreal: new insights into symptoms and their causes, and implications for the future of GERD. Am J Gastroenterol. 2019;114:414–421. doi: 10.1038/s41395-018-0287-1[↩][↩][↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589[↩][↩][↩]
- Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018 Mar;67(3):430-440. doi: 10.1136/gutjnl-2016-313589[↩][↩][↩]
- Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441938[↩][↩][↩]
- Esophagitis. Medline Plus. https://medlineplus.gov/ency/article/001153.htm[↩][↩]
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. 2017; 135:e1–e458. DOI: 10.1161/CIR.0000000000000485.[↩][↩][↩][↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Attack. https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Are the Symptoms of a Heart Attack ? https://www.nhlbi.nih.gov/health/health-topics/topics/heartattack/signs[↩]
- Zheng ZJ, Croft JB, Giles WH, Ayala CI, Greenlund KJ, Keenan NL, Neff L, Wattigney WA, Mensah GA. State Specific Mortality from Sudden Cardiac Death: United States, 1999. MMWR 2002;51(6):123–126. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5106a3.htm[↩]
- Iteen AJ, Bianchi W, Sharman T. Pneumomediastinum. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557440[↩]
- Choo MJ, Shin SO, Kim JS. A case of spontaneous cervical and mediastinal emphysema. J Korean Med Sci. 1998 Apr;13(2):223-6. https://pmc.ncbi.nlm.nih.gov/articles/instance/3054475/pdf/9610628.pdf[↩]
- Nożewski JB, Dura ML, Kłopocka M, Kwiatkowska MM, Konieczny JP, Nicpoń-Nożewska KK. A 39-Year-Old Woman with Cervicofacial and Mediastinal Emphysema 10 Hours After an Elective Lower Molar Dental Extraction. Am J Case Rep. 2021 Nov 5;22:e931793. doi: 10.12659/AJCR.931793[↩]
- Spille J, Wagner J, Spille DC, Naujokat H, Gülses A, Wiltfang J, Kübel P. Pronounced mediastinal emphysema after restorative treatment of the lower left molar-a case report and a systematic review of the literature. Oral Maxillofac Surg. 2023 Sep;27(3):533-541. doi: 10.1007/s10006-022-01088-5[↩]
- Abolnik I, Lossos IS, Breuer R. Spontaneous pneumomediastinum. A report of 25 cases. Chest. 1991 Jul;100(1):93-5. doi: 10.1378/chest.100.1.93[↩]
- Tsay CY, Chen YL, Chen CS, Lin PC, Wu MY. Pediatric Spontaneous Pneumomediastinum after a Push-Up Exercise: An Uncommon Complication of a Common Exercise. Children (Basel). 2020 Dec 11;7(12):287. doi: 10.3390/children7120287[↩][↩]
- Chiang KH, Chou AS. Images in clinical medicine. Pneumomediastinum. N Engl J Med. 2006 Mar 16;354(11):1177. doi: 10.1056/NEJMicm050132[↩]
- Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: a benign curiosity or a significant problem? Chest. 2005 Nov;128(5):3298-302. doi: 10.1378/chest.128.5.3298[↩]
- McMahon DJ. Spontaneous pneumomediastinum. Am J Surg. 1976;131:550–551. doi: 10.1016/0002-9610(76)90008-8[↩]
- Bodey GP. Medical Mediastinal Emphysema. Ann Intern Med. 1961;54:46–56.[↩]
- Badaoui R, El Kettani C, Fikri M, Ouendo M, Canova-Bartoli P, Ossart M. Spontaneous cervical and mediastinal air emphysema after ecstasy abuse. Anesth Analg. 2002 Oct;95(4):1123. doi: 10.1097/00000539-200210000-00071[↩]
- Pittman JA, Pounsford JC. Spontaneous pneumomediastinum and Ecstasy abuse. J Accid Emerg Med. 1997 Sep;14(5):335-6. https://pmc.ncbi.nlm.nih.gov/articles/instance/1343105/pdf/jaccidem00020-0063.pdf[↩]
- Quin GI, McCarthy GM, Harries DK. Spontaneous pneumomediastinum and ecstasy abuse. J Accid Emerg Med. 1999 Sep;16(5):382. https://pmc.ncbi.nlm.nih.gov/articles/instance/1347073/pdf/jaccidem00032-0064a.pdf[↩]
- Naidoo M, Govind M. On your toes: Detecting mediastinal air on the chest radiograph in ecstasy abusers. S Afr Med J. 2016 Mar 30;106(5):46-7. doi: 10.7196/SAMJ.2016.v106i5.9867[↩]
- Ezoubi S, Kahal H, Waring WS. Pneumomediastinum as a complication of MDMA (3,4-methylenedioxymetamfetamine, Ecstasy) ingestion. Acute Med. 2016;15(3):152-156.[↩]
- Malas M, Fatani N, Aljuhani Z. A Young Healthy Male with Spontaneous Subcutaneous Emphysema Occurring in Neck, Retropharyngeal and Mediastinal Spaces. Case Rep Otolaryngol. 2020 Feb 7;2020:6963796. doi: 10.1155/2020/6963796[↩]
- Obiechina NE, Jayakumar A, Khan Y, Bass J. Bilateral pneumothorax, surgical emphysema and pneumomediastinum in a young male patient following MDMA intake. BMJ Case Rep. 2018 Apr 7;2018:bcr2017223103. doi: 10.1136/bcr-2017-223103[↩]
- Johnson JN, Jones R, Wills BK. Spontaneous pneumomediastinum. West J Emerg Med. 2008 Nov;9(4):217-8. https://pmc.ncbi.nlm.nih.gov/articles/PMC2672281[↩]
- Bartelmaos T, Blanc R, Claviere GD, Benhamou D. Delayed pneumomediastinum and pneumothorax complicating laparoscopic extraperitoneal inguinal hernia repair. J Clin Anesth. 2005;17:209–212. doi: 10.1016/j.jclinane.2004.05.009[↩]
- Henderson JA, Péloquin AJ. Boerhaave revisited: spontaneous esophageal perforation as a diagnostic masquerader. Am J Med. 1989 May;86(5):559-67. doi: 10.1016/0002-9343(89)90385-9[↩]
- Lee CC, Chen TJ, Wu YH, Tsai KC, Yuan A. Spontaneous retropharyngeal emphysema and pneumomediastinum presented with signs of acute upper airway obstruction. Am J Emerg Med. 2005 May;23(3):402-4. doi: 10.1016/j.ajem.2005.02.011[↩][↩]
- Rodrigues AC, Picard MH, Carbone A, Arruda AL, Flores T, Klohn J, Furtado M, Lira-Filho EB, Cerri GG, Andrade JL. Importance of adequately performed Valsalva maneuver to detect patent foramen ovale during transesophageal echocardiography. J Am Soc Echocardiogr. 2013 Nov;26(11):1337-43. doi: 10.1016/j.echo.2013.07.016[↩]
- Jougon JB, Ballester M, Delcambre F, Mac Bride T, Dromer CE, Velly JF. Assessment of spontaneous pneumomediastinum: experience with 12 patients. Ann Thorac Surg. 2003 Jun;75(6):1711-4. doi: 10.1016/s0003-4975(03)00027-4[↩]
- Dionísio P., Martins L., Moreira S., Manique A., Macedo R., Caeiro F., Boal L., Bárbara C. Spontaneous pneumomediastinum: Experience in 18 patients during the last 12 years. J. Bras. Pneumol. Publicacao Soc. Bras. Pneumol. E Tisilogia. 2017;43:101–105. doi: 10.1590/s1806-37562016000000052[↩]
- Dajer-Fadel W.L., Argüero-Sánchez R., Ibarra-Pérez C., Navarro-Reynoso F.P. Systematic review of spontaneous pneumomediastinum: A survey of 22 years’ data. Asian Cardiovasc. Thorac. Ann. 2014;22:997–1002. doi: 10.1177/0218492313504091[↩]
- Takada K., Matsumoto S., Hiramatsu T., Kojima E., Watanabe H., Sizu M., Okachi S., Ninomiya K. Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir. Med. 2008;102:1329–1334. doi: 10.1016/j.rmed.2008.03.023[↩]
- Pneumomediastinum Prognosis. https://emedicine.medscape.com/article/1003409-overview#a2[↩]
- Weg JG, Anzueto A, Balk RA, Wiedemann HP, Pattishall EN, Schork MA, Wagner LA. The relation of pneumothorax and other air leaks to mortality in the acute respiratory distress syndrome. N Engl J Med. 1998 Feb 5;338(6):341-6. doi: 10.1056/NEJM199802053380601[↩]
- Martin SS, Aday AW, Almarzooq ZI, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2024 Feb 20;149(8):e347-e913. https://www.ahajournals.org/doi/10.1161/CIR.0000000000001209 Erratum in: Circulation. 2024 May 7;149(19):e1164. doi: 10.1161/CIR.0000000000001247[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Heart Failure. https://www.nhlbi.nih.gov/health/health-topics/topics/hf[↩][↩]
- American Heart Association. Types of Heart Failure. http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Types-of-Heart-Failure_UCM_306323_Article.jsp[↩][↩][↩]
- Guidelines for therapy of chronic heart failure. Hoppe UC, Böhm M, Dietz R, Hanrath P, Kroemer HK, Osterspey A, Schmaltz AA, Erdmann E, Vorstand der Deutschen Gesellschaft fur Kardiologie–Herz- und Kreislaufforschung e.V. Z Kardiol. 2005 Aug; 94(8):488-509. https://www.ncbi.nlm.nih.gov/pubmed/16049651/[↩]
- Hall MJ, DeFrances CJ, Williams SN, et al. National Hospital Discharge Survey: 2007 summary. National health statistics reports; no 29. Hyattsville, MD: National Center for Health Statistics. 2010. https://www.cdc.gov/nchs/data/nhsr/nhsr029.pdf[↩]
- Mozzafarian D, Benjamin EJ, Go AS, et al. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38-e360.[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Are the Signs and Symptoms of Heart Failure ? https://www.nhlbi.nih.gov/health/health-topics/topics/hf/signs[↩]
- Ejection Fraction Heart Failure Measurement. https://www.heart.org/en/health-topics/heart-failure/diagnosing-heart-failure/ejection-fraction-heart-failure-measurement[↩][↩]
- Kosaraju A, Goyal A, Grigorova Y, et al. Left Ventricular Ejection Fraction. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459131[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. Who Is at Risk for Heart Failure ? https://www.nhlbi.nih.gov/health/health-topics/topics/hf/atrisk[↩]
- National Institutes of Health. National Heart, Lung and Blood Institute. What Causes Heart Failure ? https://www.nhlbi.nih.gov/health/health-topics/topics/hf/causes[↩]
- Mayo Foundation for Medical Education and Research. Heart Failure Symptoms. http://www.mayoclinic.org/diseases-conditions/heart-failure/basics/symptoms/con-20029801[↩]
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022 May 3;79(17):e263-e421. doi: 10.1016/j.jacc.2021.12.012. Erratum in: J Am Coll Cardiol. 2023 Apr 18;81(15):1551. doi: 10.1016/j.jacc.2023.03.002[↩][↩]
- Gaddam KK, Yelamanchili P, Sedghi Y, Ventura HO. Advanced Heart Failure and Management Strategies. The Ochsner Journal. 2009;9(4):227-233. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096284/[↩][↩][↩]
- Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult heart transplant report–2008. Taylor DO, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, Rahmel AO, Kucheryavaya AY, Hertz MI. J Heart Lung Transplant. 2008 Sep; 27(9):943-56. https://www.ncbi.nlm.nih.gov/pubmed/18765186/[↩]
- Selection of patients for heart transplantation in the current era of heart failure therapy. Butler J, Khadim G, Paul KM, Davis SF, Kronenberg MW, Chomsky DB, Pierson RN 3rd, Wilson JR. J Am Coll Cardiol. 2004 Mar 3; 43(5):787-93. https://www.ncbi.nlm.nih.gov/pubmed/14998618/[↩]
- Cell-based therapy for heart failure. Wollert KC, Drexler H. Curr Opin Cardiol. 2006 May; 21(3):234-9. https://www.ncbi.nlm.nih.gov/pubmed/16601463/[↩]
- Ammar KA, Jacobsen SJ, Mahoney DW, Kors JA, Redfield MM, Burnett JC Jr, Rodeheffer RJ. Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation. 2007 Mar 27;115(12):1563-70. doi: 10.1161/CIRCULATIONAHA.106.666818[↩]
- Key Statistics for Lung Cancer. https://www.cancer.org/cancer/types/lung-cancer/about/key-statistics.html[↩][↩]
- American Cancer Society: Cancer Facts and Figures 2017. Atlanta, Ga: American Cancer Society, 2017. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf[↩]
- Key Statistics for Lung Cancer. American Cancer Society. https://www.cancer.org/cancer/non-small-cell-lung-cancer/about/key-statistics.html[↩][↩][↩][↩][↩][↩][↩]
- Humphrey L, Deffebach M, Pappas M, Baumann C, Artis K, Priest Mitchell JP, et al. Screening for Lung Cancer: Systematic Review to Update the U.S. Preventive Services Task Force Recommendation Statement. Evidence Synthesis No. 105. AHRQ Publication No. 13-05196-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; 2013.[↩][↩]
- What Are Lung Carcinoid Tumors? https://www.cancer.org/cancer/lung-carcinoid-tumor/about/what-is-lung-carcinoid-tumor.html[↩]
- Alberg AJ, Brock MV, Ford JG, et al. Epidemiology of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 suppl):e1S-e29S.[↩][↩]
- Lung and Bronchus Cancer — Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/lungb.html[↩][↩][↩][↩][↩]
- Lung Cancer. Medline Plus. https://medlineplus.gov/lungcancer.html[↩]
- Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, Keogh JP, Meyskens FL, Valanis B, Williams JH, Barnhart S, Hammar S. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med. 1996 May 2;334(18):1150-5. doi: 10.1056/NEJM199605023341802[↩][↩]
- Goodman GE, Thornquist MD, Balmes J, Cullen MR, Meyskens FL Jr, Omenn GS, Valanis B, Williams JH Jr. The Beta-Carotene and Retinol Efficacy Trial: incidence of lung cancer and cardiovascular disease mortality during 6-year follow-up after stopping beta-carotene and retinol supplements. J Natl Cancer Inst. 2004 Dec 1;96(23):1743-50. doi: 10.1093/jnci/djh320[↩][↩]
- Tardon, A., Lee, W. J., Delgado-Rodriguez, M., Dosemeci, M., Albanes, D., Hoover, R., & Blair, A. (2005). Leisure-time physical activity and lung cancer: a meta-analysis. Cancer causes & control : CCC, 16(4), 389–397. https://doi.org/10.1007/s10552-004-5026-9[↩]
- Lee IM, Sesso HD, Paffenbarger RS Jr. Physical activity and risk of lung cancer. Int J Epidemiol. 1999 Aug;28(4):620-5. doi: 10.1093/ije/28.4.620[↩]
- Mao Y, Pan S, Wen SW, Johnson KC; Canadian Cancer Registries Epidemiology Research Group. Physical activity and the risk of lung cancer in Canada. Am J Epidemiol. 2003 Sep 15;158(6):564-75. doi: 10.1093/aje/kwg186[↩]
- Wiseman M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc. 2008 Aug;67(3):253-6. doi: 10.1017/S002966510800712X[↩]
- Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, Libby DM, Pasmantier MW, Koizumi J, Altorki NK, Smith JP. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet. 1999 Jul 10;354(9173):99-105. doi: 10.1016/S0140-6736(99)06093-6[↩]
- What’s New in Non-Small Cell Lung Cancer Research ? American Cancer Society. https://www.cancer.org/cancer/non-small-cell-lung-cancer/about/new-research.html[↩]
- The U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/[↩]
- Lung Cancer: Screening. Final Recommendation Statement March 09, 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening[↩][↩]
- Can Non-Small Cell Lung Cancer Be Found Early ? American Cancer Society. https://www.cancer.org/cancer/non-small-cell-lung-cancer/detection-diagnosis-staging/detection.html[↩]
- Can Lung Cancer Be Found Early? https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/detection.html[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IA lung cancer. The…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__534[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IB lung cancer. The…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__535[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIA lung cancer. The…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__536[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIB lung cancer (1)…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__537[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIIA lung cancer (1)…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__539[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IIIB lung cancer (1)…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__542[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IVA lung cancer. The…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__545[↩]
- PDQ Adult Treatment Editorial Board. Non-Small Cell Lung Cancer Treatment (PDQ®): Patient Version. 2021 Aug 27. In: PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-. [Figure, Stage IVB lung cancer. The…] Available from: https://www.ncbi.nlm.nih.gov/books/NBK65917/figure/CDR0000062956__546[↩]
- Hunter MP, Goldin J, Regunath H. Pleurisy. [Updated 2024 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558958[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Reamy BV, Williams PM, Odom MR. Pleuritic Chest Pain: Sorting Through the Differential Diagnosis. Am Fam Physician. 2017 Sep 1;96(5):306-312. https://www.aafp.org/pubs/afp/issues/2017/0901/p306.html[↩][↩][↩][↩][↩][↩][↩][↩]
- Castaniere I, Tonelli R, Fantini R, Marchioni A, Garofalo M, Clini EM, Cerri S. The encaged lung: rapidly progressive idiopathic pleurisy. Oxf Med Case Reports. 2018 Aug 9;2018(8):omy041. doi: 10.1093/omcr/omy041[↩]
- Hogg K, Dawson D, Mackway-Jones K. Outpatient diagnosis of pulmonary embolism: the MIOPED (Manchester Investigation Of Pulmonary Embolism Diagnosis) study. Emerg Med J. 2006 Feb;23(2):123-7. doi: 10.1136/emj.2005.027110[↩][↩]
- Hull RD, Raskob GE, Carter CJ, et al. Pulmonary Embolism in Outpatients With Pleuritic Chest Pain. Arch Intern Med. 1988;148(4):838–844. doi:10.1001/archinte.1988.00380040078014[↩]
- Courtney DM, Kline JA, Kabrhel C, Moore CL, Smithline HA, Nordenholz KE, Richman PB, Plewa MC. Clinical features from the history and physical examination that predict the presence or absence of pulmonary embolism in symptomatic emergency department patients: results of a prospective, multicenter study. Ann Emerg Med. 2010 Apr;55(4):307-315.e1. doi: 10.1016/j.annemergmed.2009.11.010[↩]
- Brims FJ, Davies HE, Lee YC. Respiratory chest pain: diagnosis and treatment. Med Clin North Am. 2010 Mar;94(2):217-32. doi: 10.1016/j.mcna.2010.01.003[↩][↩]
- Hara K, Yamasaki K, Tahara M, Ikegami H, Nishida C, Muramutsu K, Fujino Y, Matsuda S, Fushimi K, Mukae H, Yatera K. Epidemiologic evaluation of pleurisy diagnosed by surgical pleural biopsy using data from a nationwide administrative database. Thorac Cancer. 2022 Apr;13(8):1136-1142. doi: 10.1111/1759-7714.14368[↩][↩]
- Dinwiddie R, Sonnappa S. Systemic diseases and the lung. Paediatr Respir Rev. 2005 Sep;6(3):181-9. doi: 10.1016/j.prrv.2005.06.007[↩]
- Shaw M, Collins BF, Ho LA, Raghu G. Rheumatoid arthritis-associated lung disease. Eur Respir Rev. 2015 Mar;24(135):1-16. doi: 10.1183/09059180.00008014[↩]
- Light RW. Pleural effusion due to pulmonary emboli. Curr Opin Pulm Med. 2001 Jul;7(4):198-201. doi: 10.1097/00063198-200107000-00006[↩]
- Ozbay B, Uzun K. Extrapulmonary tuberculosis in high prevalence of tuberculosis and low prevalence of HIV. Clin Chest Med. 2002 Jun;23(2):351-4. doi: 10.1016/s0272-5231(02)00002-3[↩]
- Rolo M, González-Blanco B, Reyes CA, Rosillo N, López-Roa P. Epidemiology and factors associated with Extra-pulmonary tuberculosis in a Low-prevalence area. J Clin Tuberc Other Mycobact Dis. 2023 May 12;32:100377. doi: 10.1016/j.jctube.2023.100377[↩]
- Engel ME, Matchaba PT, Volmink J. Corticosteroids for tuberculous pleurisy. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD001876. doi: 10.1002/14651858.CD001876.pub2. Update in: Cochrane Database Syst Rev. 2017 Mar 14;3:CD001876. doi: 10.1002/14651858.CD001876.pub3[↩]
- Yu S, Gao Y, Lu J, Zhang G, Chen X, Zhang R, Kong W, Shang L. Clinical profiles and related factors in tuberculosis patients with positive sputum smear mycobacterium tuberculosis tests. Sci Rep. 2024 Sep 2;14(1):20376. doi: 10.1038/s41598-024-71403-5[↩]
- Kamus L, Roquebert B, Allyn J, Allou N, Valance D, Simon C, Jaffar-Bandjee MC, Descours G, Jarraud S, Miltgen G. Severe bilateral pleuropneumonia caused by Legionella sainthelensi: a case report. BMC Infect Dis. 2021 Sep 17;21(1):966. doi: 10.1186/s12879-021-06651-1[↩]
- Mbaye PS, Koffi N, Camara P, Burgel PR, Hovette P, Klotz F. Manifestations pleuropulmonaires de l’amibiase [Pleuropulmonary manifestations of amebiasis]. Rev Pneumol Clin. 1998 Dec;54(6):346-52. French[↩]
- Bouros D, Pneumatikos I, Tzouvelekis A. Pleural involvement in systemic autoimmune disorders. Respiration. 2008;75(4):361-71. doi: 10.1159/000119051[↩]
- Ahmed HK, Hiwa DS, Tahir SH, Ali RM, Gharib DT, Asaad HR, Hamahussein KF, Mohammed AA, Najar KA, Kakamad FH. Crohn’s disease presenting with pleural effusion: a case report. Oxf Med Case Reports. 2024 Oct 10;2024(10):omae113. doi: 10.1093/omcr/omae113[↩]
- Wang L, Qiu Z, Zhan S, Shi G, He W, Cen Z, Xu F, Tian W, Li D. Case report: Page kidney with multiple serosal effusions caused by bilateral spontaneous renal subcapsular hemorrhage. Front Med (Lausanne). 2024 Jan 24;11:1290470. doi: 10.3389/fmed.2024.1290470[↩]
- Bontempo LJ, Magidson PD, Hayes BD, Martinez JP. Acute Pulmonary Injury after Inhalation of Free-Base Cocaine: A Case Report. J Acute Med. 2017 Jun 1;7(2):82-86. doi: 10.6705/j.jacme.2017.0702.007[↩]
- Ocansey BK, Otoo B, Adjei A, Gbadamosi H, Kotey FCN, Kosmidis C, Afriyie-Mensah JS, Denning DW, Opintan JA. Chronic pulmonary aspergillosis is common among patients with presumed tuberculosis relapse in Ghana. Med Mycol. 2022 Sep 9;60(9):myac063. doi: 10.1093/mmy/myac063[↩]
- Iuchi K, Aozasa K, Yamamoto S, Mori T, Tajima K, Minato K, Mukai K, Komatsu H, Tagaki T, Kobashi Y, et al. Non-Hodgkin’s lymphoma of the pleural cavity developing from long-standing pyothorax. Summary of clinical and pathological findings in thirty-seven cases. Jpn J Clin Oncol. 1989 Sep;19(3):249-57.[↩]
- Narimatsu H, Ota Y, Kami M, Takeuchi K, Suzuki R, Matsuo K, Matsumura T, Yuji K, Kishi Y, Hamaki T, Sawada U, Miyata S, Sasaki T, Tobinai K, Kawabata M, Atsuta Y, Tanaka Y, Ueda R, Nakamura S. Clinicopathological features of pyothorax-associated lymphoma; a retrospective survey involving 98 patients. Ann Oncol. 2007 Jan;18(1):122-128. doi: 10.1093/annonc/mdl349[↩]
- Nadal JA, Murray JF, Mason RJ. Textbook of Respiratory Medicine. 4th ed. Philadelphia, Pa.: Saunders-Elsevier; 2005.[↩][↩]
- Peterson TA, Turner SP, Dolezal KA. Acute Pericarditis: Rapid Evidence Review. Am Fam Physician. 2024 May;109(5):441-446. https://www.aafp.org/pubs/afp/issues/2024/0500/acute-pericarditis.html[↩]
- Marinella MA. Electrocardiographic manifestations and differential diagnosis of acute pericarditis. Am Fam Physician. 1998 Feb 15;57(4):699-704. https://www.aafp.org/pubs/afp/issues/1998/0215/p699.html[↩]
- Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med. 2000 Mar 23;342(12):868-74. doi: 10.1056/NEJM200003233421207[↩]
- Perrier A, Roy PM, Aujesky D, Chagnon I, Howarth N, Gourdier AL, Leftheriotis G, Barghouth G, Cornuz J, Hayoz D, Bounameaux H. Diagnosing pulmonary embolism in outpatients with clinical assessment, D-dimer measurement, venous ultrasound, and helical computed tomography: a multicenter management study. Am J Med. 2004 Mar 1;116(5):291-9. doi: 10.1016/j.amjmed.2003.09.041[↩]
- Metlay JP, Kapoor WN, Fine MJ. Does This Patient Have Community-Acquired Pneumonia? Diagnosing Pneumonia by History and Physical Examination. JAMA. 1997;278(17):1440–1445. doi:10.1001/jama.1997.03550170070035[↩][↩][↩]
- Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005 Nov 23;294(20):2623-9. doi: 10.1001/jama.294.20.2623. Erratum in: JAMA. 2006 May 17;295(19):2250.[↩][↩][↩][↩]
- Lanham DA, Taylor AN, Chessell SJ, Lanham JG. Non-cardiac chest pain: a clinical assessment tool. Br J Hosp Med (Lond). 2015 May;76(5):296-300. doi: 10.12968/hmed.2015.76.5.296[↩][↩]
- Miniati M, Prediletto R, Formichi B, Marini C, Di Ricco G, Tonelli L, Allescia G, Pistolesi M. Accuracy of clinical assessment in the diagnosis of pulmonary embolism. Am J Respir Crit Care Med. 1999 Mar;159(3):864-71. doi: 10.1164/ajrccm.159.3.9806130[↩]
- Shen-Wagner J, Gamble C, MacGilvray P. Pleural Effusion: Diagnostic Approach in Adults. Am Fam Physician. 2023 Nov;108(5):464-475. https://www.aafp.org/pubs/afp/issues/2023/1100/pleural-effusion.html[↩]
- Light RW. Clinical practice. Pleural effusion. N Engl J Med. 2002 Jun 20;346(25):1971-7. doi: 10.1056/NEJMcp010731[↩]
- Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011 Oct;140(4):859-866. doi: 10.1378/chest.10-294[↩]
- Volpicelli G, Cardinale L, Berchialla P, Mussa A, Bar F, Frascisco MF. A comparison of different diagnostic tests in the bedside evaluation of pleuritic pain in the ED. Am J Emerg Med. 2012 Feb;30(2):317-24. doi: 10.1016/j.ajem.2010.11.035[↩]
- Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004 Nov 18;351(21):2195-202. doi: 10.1056/NEJMcp041997. Erratum in: N Engl J Med. 2005 Mar 17;352(11):1163.[↩]
- Hiratzka LF, Bakris GL, Beckman JA, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology,American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons,and Society for Vascular Medicine. J Am Coll Cardiol. 2010 Apr 6;55(14):e27-e129. doi: 10.1016/j.jacc.2010.02.015. Erratum in: J Am Coll Cardiol. 2013 Sep 10;62(11):1039-40.[↩]
- Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, Forgie M, Kovacs G, Ward J, Kovacs MJ. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001 Jul 17;135(2):98-107. doi: 10.7326/0003-4819-135-2-200107170-00010[↩]
- Kline JA, Courtney DM, Kabrhel C, Moore CL, Smithline HA, Plewa MC, Richman PB, O’Neil BJ, Nordenholz K. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008 May;6(5):772-80. doi: 10.1111/j.1538-7836.2008.02944.x[↩]
- Lucassen WA, Douma RA, Toll DB, Büller HR, van Weert HC. Excluding pulmonary embolism in primary care using the Wells-rule in combination with a point-of care D-dimer test: a scenario analysis. BMC Fam Pract. 2010 Sep 13;11:64. doi: 10.1186/1471-2296-11-64[↩]
- Le Gal G, Righini M, Roy PM, Sanchez O, Aujesky D, Bounameaux H, Perrier A. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med. 2006 Feb 7;144(3):165-71. doi: 10.7326/0003-4819-144-3-200602070-00004[↩]
- Addala DN, Bedawi EO, Rahman NM. Parapneumonic Effusion and Empyema. Clin Chest Med. 2021 Dec;42(4):637-647. doi: 10.1016/j.ccm.2021.08.001[↩]
- Ala-Seppälä HM, Ukkonen MT, Lehtomäki AI, Pohja ES, Nieminen JJ, Laurikka JO, Khan JA. High Occurrence of Thrombo-Embolic Complications During Long-Term Follow-up After Pleural Infections-A Single-Center Experience with 536 Consecutive Patients Over 17 Years. Lung. 2020 Aug;198(4):671-678. doi: 10.1007/s00408-020-00374-x[↩]
- Saunders J, Ashton M, Hall C, Laird B, MacLeod N. Pain management in patients with malignant mesothelioma: challenges and solutions. Lung Cancer (Auckl). 2019 Apr 2;10:37-46. doi: 10.2147/LCTT.S192558[↩]
- Kookoolis AS, Puchalski JT, Murphy TE, Araujo KL, Pisani MA. Mortality of Hospitalized Patients with Pleural Effusions. J Pulm Respir Med. 2014 Jun;4(3):184. doi: 10.4172/2161-105X.1000184[↩]
- Kim H, Lee KY, Choo EH, Hwang BH, Kim JJ, Kim CJ, Chang K, Hong YJ, Kim JH, Ahn Y, Choi Y; KAMIR‐NIH Investigators. Long-Term Risk of Cardiovascular Death in Patients With Mildly Reduced Ejection Fraction After Acute Myocardial Infarction: A Multicenter, Prospective Registry Study. J Am Heart Assoc. 2024 Sep 17;13(18):e034870. doi: 10.1161/JAHA.124.034870[↩]
- Alherbish A, Westerhout CM, Fu Y, White HD, Granger CB, Wagner G, Armstrong PW. The forgotten lead: does aVR ST-deviation add insight into the outcomes of ST-elevation myocardial infarction patients? Am Heart J. 2013 Aug;166(2):333-9. doi: 10.1016/j.ahj.2013.05.018[↩]
- Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-e228. doi: 10.1016/j.jacc.2014.09.017. Epub 2014 Sep 23. Erratum in: J Am Coll Cardiol. 2014 Dec 23;64(24):2713-4. Dosage error in article text.[↩]
- McGraw MD, Galambos C, Stillwell PC. Uremic pleuritis: A case report and review of recurrent exudative pleural effusions in children. Pediatr Pulmonol. 2017 Sep;52(9):E52-E54. doi: 10.1002/ppul.23708[↩]
- Jakubovic BD, Donovan A, Webster PM, Shear NH. Methotrexate-induced pulmonary toxicity. Can Respir J. 2013 May-Jun;20(3):153-5. doi: 10.1155/2013/527912[↩]
- Teerakanok J, Tantrachoti P, Chariyawong P, Nugent K. Acute Amiodarone Pulmonary Toxicity After Surgical Procedures. Am J Med Sci. 2016 Dec;352(6):646-651. doi: 10.1016/j.amjms.2016.08.013[↩]
- Loeb M. Community‐acquired pneumonia. Clinical Evidence. Vol. 8, London: BMJ Publishing Group, 2002.[↩]
- Welte T, Torres A, Nathwani D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax. 2012 Jan;67(1):71-9. doi: 10.1136/thx.2009.129502[↩]
- Sattar SBA, Sharma S. Bacterial Pneumonia. [Updated 2021 Dec 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513321[↩][↩][↩][↩][↩][↩]
- Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep. 2008 Apr 24;56(10):1-120. https://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf[↩]
- Lat I, Daley MJ, Shewale A, Pangrazzi MH, Hammond D, Olsen KM; DEFINE study group and the Discovery Research Network. A Multicenter, Prospective, Observational Study to Determine Predictive Factors for Multidrug-Resistant Pneumonia in Critically Ill Adults: The DEFINE Study. Pharmacotherapy. 2019 Mar;39(3):253-260. doi: 10.1002/phar.2171[↩]
- Shin, E. J., Kim, Y., Jeong, J. Y., Jung, Y. M., Lee, M. H., & Chung, E. H. (2018). The changes of prevalence and etiology of pediatric pneumonia from National Emergency Department Information System in Korea, between 2007 and 2014. Korean journal of pediatrics, 61(9), 291–300. https://doi.org/10.3345/kjp.2017.06100[↩]
- Metlay, J. P., Waterer, G. W., Long, A. C., et al. (2019). Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American journal of respiratory and critical care medicine, 200(7), e45–e67. https://doi.org/10.1164/rccm.201908-1581ST[↩]
- Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997 Jan 23;336(4):243–250. DOI: 10.1056/NEJM199701233360402[↩][↩][↩]
- Mandell, L. A., Bartlett, J. G., Dowell, S. F., File, T. M., Jr, Musher, D. M., Whitney, C., & Infectious Diseases Society of America (2003). Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 37(11), 1405–1433. https://doi.org/10.1086/380488[↩][↩]
- Fine MJ, Hough LJ, Medsger AR, Li YH, Ricci EM, Singer DE, Marrie TJ, Coley CM, Walsh MB, Karpf M, Lahive KC, Kapoor WN. The hospital admission decision for patients with community-acquired pneumonia. Results from the pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med. 1997 Jan 13;157(1):36-44.[↩]
- Mark Williams; Scott A. Flanders; Winthrop F. Whitcomb (28 September 2007). Comprehensive hospital medicine: an evidence based approach. Elsevier Health Sciences. pp. 273–. ISBN 978-1-4160-0223-9[↩]
- Capelastegui A, España PP, Quintana JM, Areitio I, Gorordo I, Egurrola M, Bilbao A. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006;27:151–157.[↩]
- Chalmers JD, Singanayagam A, Akram AR, et al. (October 2010). “Severity assessment tools for predicting mortality in hospitalised patients with community-acquired pneumonia. Systematic review and meta-analysis”. Thorax. 65 (10): 878–83. doi:10.1136/thx.2009.133280[↩]
- Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, Lewis SA, Macfarlane JT. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–382.[↩]
- Mandell LA, Marrie TJ, Grossman RF, Chow AW, Hyland RH. Canadian guidelines for the initial management of community-acquired pneumonia: an evidence-based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Canadian Community-Acquired Pneumonia Working Group. Clin Infect Dis. 2000 Aug;31(2):383-421. doi: 10.1086/313959[↩]
- Mandell, L. A., Wunderink, R. G., Anzueto, A., Bartlett, J. G., Campbell, G. D., Dean, N. C., Dowell, S. F., File, T. M., Jr, Musher, D. M., Niederman, M. S., Torres, A., Whitney, C. G., Infectious Diseases Society of America, & American Thoracic Society (2007). Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 44 Suppl 2(Suppl 2), S27–S72. https://doi.org/10.1086/511159[↩][↩]
- Pakhale, S., Mulpuru, S., Verheij, T. J., Kochen, M. M., Rohde, G. G., & Bjerre, L. M. (2014). Antibiotics for community-acquired pneumonia in adult outpatients. The Cochrane database of systematic reviews, 2014(10), CD002109. https://doi.org/10.1002/14651858.CD002109.pub4[↩]
- Common Questions About Pneumonia in Nursing Home Residents. Am Fam Physician. 2015 Oct 1;92(7):612-620. https://www.aafp.org/afp/2015/1001/p612.html[↩]
- Lee JS, Giesler DL, Gellad WF, Fine MJ. Antibiotic Therapy for Adults Hospitalized With Community-Acquired Pneumonia: A Systematic Review. JAMA. 2016 Feb 9;315(6):593-602. doi: 10.1001/jama.2016.0115[↩][↩][↩][↩]
- Pneumonia (community-acquired): antimicrobial prescribing. https://www.nice.org.uk/guidance/ng138/chapter/Recommendations[↩][↩][↩]
- Lim, W. S., Smith, D. L., Wise, M. P., & Welham, S. A. (2015). British Thoracic Society community acquired pneumonia guideline and the NICE pneumonia guideline: how they fit together. BMJ open respiratory research, 2(1), e000091. https://doi.org/10.1136/bmjresp-2015-000091[↩]
- Wan YD, Sun TW, Liu ZQ, Zhang SG, Wang LX, Kan QC. Efficacy and Safety of Corticosteroids for Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis. Chest. 2016 Jan;149(1):209-19. doi: 10.1378/chest.15-1733[↩]
- Siemieniuk RA, Meade MO, Alonso-Coello P, Briel M, Evaniew N, Prasad M, Alexander PE, Fei Y, Vandvik PO, Loeb M, Guyatt GH. Corticosteroid Therapy for Patients Hospitalized With Community-Acquired Pneumonia: A Systematic Review and Meta-analysis. Ann Intern Med. 2015 Oct 6;163(7):519-28. doi: 10.7326/M15-0715[↩]
- Torres A, Sibila O, Ferrer M, Polverino E, Menendez R, Mensa J, Gabarrús A, Sellarés J, Restrepo MI, Anzueto A, Niederman MS, Agustí C. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA. 2015 Feb 17;313(7):677-86. doi: 10.1001/jama.2015.88[↩]
- Calik, S., Ari, A., Bilgir, O., Cetintepe, T., Yis, R., Sonmez, U., & Tosun, S. (2018). The relationship between mortality and microbiological parameters in febrile neutropenic patients with hematological malignancies. Saudi medical journal, 39(9), 878–885. https://doi.org/10.15537/smj.2018.9.22824[↩]
- Freeman AM, Leigh, Jr TR. Viral Pneumonia. [Updated 2021 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513286[↩]
- Viral Pneumonia Treatment & Management. https://emedicine.medscape.com/article/300455-treatment[↩]
- Murdoch, D. R., & Chambers, S. T. (2009). Atypical pneumonia–time to breathe new life into a useful term?. The Lancet. Infectious diseases, 9(8), 512–519. https://doi.org/10.1016/S1473-3099(09)70148-3[↩]
- Rhim, J. W., Kang, H. M., Yang, E. A., & Lee, K. Y. (2019). Epidemiological relationship between Mycoplasma pneumoniae pneumonia and recurrent wheezing episode in children: an observational study at a single hospital in Korea. BMJ open, 9(4), e026461. https://doi.org/10.1136/bmjopen-2018-026461[↩]
- Beeton, Michael L et al. “Mycoplasma pneumoniae infections, 11 countries in Europe and Israel, 2011 to 2016.” Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin vol. 25,2 (2020): 1900112. https://doi.org/10.2807/1560-7917.ES.2020.25.2.1900112[↩][↩]
- Dumke R, Strubel A, Cyncynatus C, Nuyttens H, Herrmann R, Lück C, Jacobs E. Optimized serodiagnosis of Mycoplasma pneumoniae infections. Diagn Microbiol Infect Dis. 2012 Jun;73(2):200-3. doi: 10.1016/j.diagmicrobio.2012.02.014[↩]
- Zhang, X. S., Zhao, H., Vynnycky, E., & Chalker, V. (2019). Positively interacting strains that co-circulate within a network structured population induce cycling epidemics of Mycoplasma pneumoniae. Scientific reports, 9(1), 541. https://doi.org/10.1038/s41598-018-36325-z[↩][↩]
- Sánchez-Vargas FM, Gómez-Duarte OG. Mycoplasma pneumoniae-an emerging extra-pulmonary pathogen. Clin Microbiol Infect. 2008 Feb;14(2):105-17. doi: 10.1111/j.1469-0691.2007.01834.x[↩]
- Abdulhadi B, Kiel J. Mycoplasma Pneumonia. [Updated 2022 Jan 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430780[↩][↩][↩]
- Liu, J., & Li, Y. (2021). Thrombosis associated with mycoplasma pneumoniae infection (Review). Experimental and therapeutic medicine, 22(3), 967. https://doi.org/10.3892/etm.2021.10399[↩]
- Bajantri, B., Venkatram, S., & Diaz-Fuentes, G. (2018). Mycoplasma pneumoniae: A Potentially Severe Infection. Journal of clinical medicine research, 10(7), 535–544. https://doi.org/10.14740/jocmr3421w[↩]
- Wen, Z., Wei, J., Xue, H., Chen, Y., Melnick, D., Gonzalez, J., Hackett, J., Li, X., & Cao, Z. (2018). Epidemiology, microbiology, and treatment patterns of pediatric patients hospitalized with pneumonia at two hospitals in China: a patient chart review study. Therapeutics and clinical risk management, 14, 501–510. https://doi.org/10.2147/TCRM.S143266[↩]
- Brady MF, Sundareshan V. Legionnaires’ Disease. [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430807[↩]
- Legionnaires Disease. https://emedicine.medscape.com/article/220163-overview[↩]
- Legionella (Legionnaires’ Disease and Pontiac Fever). https://www.cdc.gov/legionella/about/signs-symptoms.html[↩]
- Correia AM, GonCalves J, Gomes, JP, et al. Probable Person-to-Person Transmission of Legionnaires’ Disease. N Engl J Med. 2016;374:497–8. DOI: 10.1056/NEJMc1505356[↩]
- Legionnaires Disease Workup. https://emedicine.medscape.com/article/220163-workup#c5[↩][↩]
- Active Bacterial Core Surveillance for Legionellosis — United States, 2011–2013. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6442a2.htm[↩]
- Soda EA, Barskey AE, Shah PP, et al. Vital Signs: Health Care–Associated Legionnaires’ Disease Surveillance Data from 20 States and a Large Metropolitan Area — United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66:584–589. DOI: http://dx.doi.org/10.15585/mmwr.mm6622e1[↩]
- Kuo, C. C., Jackson, L. A., Campbell, L. A., & Grayston, J. T. (1995). Chlamydia pneumoniae (TWAR). Clinical microbiology reviews, 8(4), 451–461. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172870/pdf/080451.pdf[↩]
- Hahn DL, Azenabor AA, Beatty WL, Byrne GI. Chlamydia pneumoniae as a respiratory pathogen. Front Biosci. 2002 Mar 1;7:e66-76. doi: 10.2741/hahn[↩]
- Porritt, R. A., & Crother, T. R. (2016). Chlamydia pneumoniae Infection and Inflammatory Diseases. Forum on immunopathological diseases and therapeutics, 7(3-4), 237–254. https://doi.org/10.1615/ForumImmunDisTher.2017020161[↩]
- Gautam J, Krawiec C. Chlamydia Pneumonia. [Updated 2021 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560874[↩]
- Kuo, C. C., Jackson, L. A., Campbell, L. A., & Grayston, J. T. (1995). Chlamydia pneumoniae (TWAR). Clinical microbiology reviews, 8(4), 451–461. https://doi.org/10.1128/CMR.8.4.451[↩]
- Theunissen, H. J., Lemmens-den Toom, N. A., Burggraaf, A., Stolz, E., & Michel, M. F. (1993). Influence of temperature and relative humidity on the survival of Chlamydia pneumoniae in aerosols. Applied and environmental microbiology, 59(8), 2589–2593. https://doi.org/10.1128/aem.59.8.2589-2593.1993[↩]
- Cunha B. A. (2006). The atypical pneumonias: clinical diagnosis and importance. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases, 12 Suppl 3, 12–24. https://doi.org/10.1111/j.1469-0691.2006.01393.x[↩]
- Blasi F, Tarsia P, Arosio C, Fagetti L, Allegra L. Epidemiology of Chlamydia pneumoniae. Clin Microbiol Infect. 1998 Jan;4 Suppl 4:S1-S6.[↩]
- Hogerwerf L, DE Gier B, Baan B, VAN DER Hoek W. Chlamydia psittaci (psittacosis) as a cause of community-acquired pneumonia: a systematic review and meta-analysis. Epidemiol Infect. 2017 Nov;145(15):3096-3105. doi: 10.1017/S0950268817002060[↩]
- Psittacosis Signs and Symptoms. https://www.cdc.gov/pneumonia/atypical/psittacosis/about/signs-symptoms.html[↩][↩]
- Soni R., Seale J.P., Young I.H. Fulminant psittacosis requiring mechanical ventilation and demonstrating serological cross-reactivity between Legionella longbeachae and Chlamydia psittaci. Respirology. 1999;4(2):203–205. doi: 10.1046/j.1440-1843.1999.00176.x[↩]
- Lynch JP 3rd, Zhanel GG. Streptococcus pneumoniae: epidemiology, risk factors, and strategies for prevention. Semin Respir Crit Care Med. 2009 Apr;30(2):189-209. doi: 10.1055/s-0029-1202938[↩]
- Kim, L., McGee, L., Tomczyk, S., & Beall, B. (2016). Biological and Epidemiological Features of Antibiotic-Resistant Streptococcus pneumoniae in Pre- and Post-Conjugate Vaccine Eras: a United States Perspective. Clinical microbiology reviews, 29(3), 525–552. https://doi.org/10.1128/CMR.00058-15[↩]
- Kruckow KL, Zhao K, Bowdish DME, Orihuela CJ. Acute organ injury and long-term sequelae of severe pneumococcal infections. Pneumonia (Nathan). 2023 Mar 5;15(1):5. doi: 10.1186/s41479-023-00110-y[↩]
- https://phil.cdc.gov/Details.aspx?pid=9996[↩]
- Weiser, J. N., Ferreira, D. M., & Paton, J. C. (2018). Streptococcus pneumoniae: transmission, colonization and invasion. Nature reviews. Microbiology, 16(6), 355–367. https://doi.org/10.1038/s41579-018-0001-8[↩]
- Magill, S. S., Edwards, J. R., Bamberg, W., Beldavs, Z. G., Dumyati, G., Kainer, M. A., Lynfield, R., Maloney, M., McAllister-Hollod, L., Nadle, J., Ray, S. M., Thompson, D. L., Wilson, L. E., Fridkin, S. K., & Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team (2014). Multistate point-prevalence survey of health care-associated infections. The New England journal of medicine, 370(13), 1198–1208. https://doi.org/10.1056/NEJMoa1306801[↩][↩][↩]
- Klebsiella pneumoniae in Healthcare Settings. https://www.cdc.gov/hai/organisms/klebsiella/klebsiella.html[↩]
- Podschun, R., & Ullmann, U. (1998). Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clinical microbiology reviews, 11(4), 589–603. https://doi.org/10.1128/CMR.11.4.589[↩][↩][↩]
- Ashurst JV, Dawson A. Klebsiella Pneumonia. [Updated 2022 Feb 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519004[↩][↩]
- Kalanuria, A. A., Ziai, W., & Mirski, M. (2014). Ventilator-associated pneumonia in the ICU. Critical care (London, England), 18(2), 208. https://doi.org/10.1186/cc13775[↩]
- Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000 Aug;21(8):510-5. doi: 10.1086/501795[↩]
- Kang, C. I., Kim, S. H., Bang, J. W., Kim, H. B., Kim, N. J., Kim, E. C., Oh, M. D., & Choe, K. W. (2006). Community-acquired versus nosocomial Klebsiella pneumoniae bacteremia: clinical features, treatment outcomes, and clinical implication of antimicrobial resistance. Journal of Korean medical science, 21(5), 816–822. https://doi.org/10.3346/jkms.2006.21.5.816[↩]
- Montgomerie JZ, Ota JK. Klebsiella bacteremia. Arch Intern Med. 1980 Apr;140(4):525-7.[↩]
- Meatherall BL, Gregson D, Ross T, Pitout JD, Laupland KB. Incidence, risk factors, and outcomes of Klebsiella pneumoniae bacteremia. Am J Med. 2009 Sep;122(9):866-73. doi: 10.1016/j.amjmed.2009.03.034[↩]
- Lye WC, Chan RK, Lee EJ, Kumarasinghe G. Urinary tract infections in patients with diabetes mellitus. J Infect. 1992 Mar;24(2):169-74. doi: 10.1016/0163-4453(92)92876-k[↩]
- Schroll, C., Barken, K. B., Krogfelt, K. A., & Struve, C. (2010). Role of type 1 and type 3 fimbriae in Klebsiella pneumoniae biofilm formation. BMC microbiology, 10, 179. https://doi.org/10.1186/1471-2180-10-179[↩]
- Liu, C., & Guo, J. (2018). Characteristics of ventilator-associated pneumonia due to hypervirulent Klebsiella pneumoniae genotype in genetic background for the elderly in two tertiary hospitals in China. Antimicrobial resistance and infection control, 7, 95. https://doi.org/10.1186/s13756-018-0371-8[↩]
- Pneumocystis pneumonia. https://www.cdc.gov/fungal/diseases/pneumocystis-pneumonia[↩]
- Harris, J.R., Balajee, S.A. & Park, B.J. Pneumocystis Jirovecii Pneumonia: Current Knowledge and Outstanding Public Health Issues. Curr Fungal Infect Rep 4, 229–237 (2010). https://doi.org/10.1007/s12281-010-0029-3[↩][↩]
- Edman JC, Kovacs JA, Masur H, Santi DV, Elwood HJ, Sogin ML. Ribosomal RNA sequence shows Pneumocystis carinii to be a member of the fungi. Nature. 1988 Aug 11;334(6182):519-22. doi: 10.1038/334519a0[↩]
- Stringer, J. R., Beard, C. B., Miller, R. F., & Wakefield, A. E. (2002). A new name (Pneumocystis jiroveci) for Pneumocystis from humans. Emerging infectious diseases, 8(9), 891–896. https://doi.org/10.3201/eid0809.020096[↩]
- Medrano, F. J., Montes-Cano, M., Conde, M., de la Horra, C., Respaldiza, N., Gasch, A., Perez-Lozano, M. J., Varela, J. M., & Calderon, E. J. (2005). Pneumocystis jirovecii in general population. Emerging infectious diseases, 11(2), 245–250. https://doi.org/10.3201/eid1102.040487[↩][↩][↩]
- Jeremy A W Gold, Brendan R Jackson, Kaitlin Benedict, Possible Diagnostic Delays and Missed Prevention Opportunities in Pneumocystis Pneumonia Patients Without HIV: Analysis of Commercial Insurance Claims Data—United States, 2011–2015, Open Forum Infectious Diseases, Volume 7, Issue 7, July 2020, ofaa255, https://doi.org/10.1093/ofid/ofaa255[↩][↩]
- Roux, A., Canet, E., Valade, S., Gangneux-Robert, F., Hamane, S., Lafabrie, A., Maubon, D., Debourgogne, A., Le Gal, S., Dalle, F., Leterrier, M., Toubas, D., Pomares, C., Bellanger, A. P., Bonhomme, J., Berry, A., Durand-Joly, I., Magne, D., Pons, D., Hennequin, C., … Azoulay, É. (2014). Pneumocystis jirovecii pneumonia in patients with or without AIDS, France. Emerging infectious diseases, 20(9), 1490–1497. https://doi.org/10.3201/eid2009.131668[↩]
- Gianella S, Haeberli L, Joos B, Ledergerber B, Wüthrich RP, Weber R, Kuster H, Hauser PM, Fehr T, Mueller NJ. Molecular evidence of interhuman transmission in an outbreak of Pneumocystis jirovecii pneumonia among renal transplant recipients. Transpl Infect Dis. 2010 Feb;12(1):1-10. doi: 10.1111/j.1399-3062.2009.00447.x[↩]
- A Cluster of Pneumocystis jirovecii Infection Among Outpatients with Rheumatoid Arthritis. The Journal of Rheumatology Jul 2010, 37 (7) 1547-1548; DOI: 10.3899/jrheum.091294[↩]
- Pifer LL, Hughes WT, Stagno S, Woods D. Pneumocystis carinii infection: evidence for high prevalence in normal and immunosuppressed children. Pediatrics. 1978 Jan;61(1):35-41.[↩]
- Wakefield AE, Lindley AR, Ambrose HE, Denis CM, Miller RF. Limited asymptomatic carriage of Pneumocystis jiroveci in human immunodeficiency virus-infected patients. J Infect Dis. 2003 Mar 15;187(6):901-8. doi: 10.1086/368165[↩]
- Kovacs JA, Hiemenz JW, Macher AM, Stover D, Murray HW, Shelhamer J, Lane HC, Urmacher C, Honig C, Longo DL, et al. Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med. 1984 May;100(5):663-71. doi: 10.7326/0003-4819-100-5-663[↩]
- Accuracy of β-D-glucan for the diagnosis of Pneumocystis jirovecii pneumonia: a meta-analysis. Karageorgopoulos, D.E. et al. Clinical Microbiology and Infection, Volume 19, Issue 1, 39 – 49. https://doi.org/10.1111/j.1469-0691.2011.03760.x[↩]
- Truong J, Ashurst JV. Pneumocystis Jirovecii Pneumonia. [Updated 2022 Feb 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482370[↩][↩][↩][↩][↩][↩][↩]
- Newberry L, O’Hare B, Kennedy N, Selman A, Omar S, Dawson P, Stevenson K, Nishihara Y, Lissauer S, Molyneux E. Early use of corticosteroids in infants with a clinical diagnosis of Pneumocystis jiroveci pneumonia in Malawi: a double-blind, randomised clinical trial. Paediatr Int Child Health. 2017 May;37(2):121-128. doi: 10.1080/20469047.2016.1260891[↩]
- Fungal Pneumonia. https://emedicine.medscape.com/article/300341-overview[↩][↩][↩]
- Lamoth F, Alexander BD. Nonmolecular methods for the diagnosis of respiratory fungal infections. Clin Lab Med. 2014 Jun;34(2):315-36. doi: 10.1016/j.cll.2014.02.006[↩][↩]
- Limper AH. The changing spectrum of fungal infections in pulmonary and critical care practice: clinical approach to diagnosis. Proc Am Thorac Soc. 2010 May;7(3):163-8. doi: 10.1513/pats.200906-049AL[↩]
- Chen TC, Ho MW, Chien WC, Lin HH. Disseminated Scedosporium apiospermum infection in a near-drowning patient. J Formos Med Assoc. 2016 Mar;115(3):213-4. doi: 10.1016/j.jfma.2015.02.007[↩]
- Garzoni, C., Emonet, S., Legout, L., Benedict, R., Hoffmeyer, P., Bernard, L., & Garbino, J. (2005). Atypical infections in tsunami survivors. Emerging infectious diseases, 11(10), 1591–1593. https://doi.org/10.3201/eid1110.050715[↩]
- Fungal Pneumonia. https://emedicine.medscape.com/article/300341-overview#a5[↩]
- White, P. L., Archer, A. E., & Barnes, R. A. (2005). Comparison of non-culture-based methods for detection of systemic fungal infections, with an emphasis on invasive Candida infections. Journal of clinical microbiology, 43(5), 2181–2187. https://doi.org/10.1128/JCM.43.5.2181-2187.2005[↩]
- Lass-Flörl C, Gunsilius E, Gastl G, Freund M, Dierich MP, Petzer A. Clinical evaluation of Aspergillus-PCR for detection of invasive aspergillosis in immunosuppressed patients. Mycoses. 2005;48 Suppl 1:12-7. doi: 10.1111/j.1439-0507.2005.01104.x[↩]
- Smith JA, Kauffman CA. Pulmonary fungal infections. Respirology. 2012 Aug;17(6):913-26. doi: 10.1111/j.1440-1843.2012.02150.x[↩][↩][↩]
- Gerber B, Guggenberger R, Fasler D, Nair G, Manz MG, Stussi G, Schanz U. Reversible skeletal disease and high fluoride serum levels in hematologic patients receiving voriconazole. Blood. 2012 Sep 20;120(12):2390-4. doi: 10.1182/blood-2012-01-403030[↩]
- About Pneumococcal Vaccines. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/about-vaccine.html[↩]
- Types of Pneumococcal Vaccines. https://www.cdc.gov/pneumococcal/vaccines/types.html[↩]
- VAXNEUVANCE. https://www.fda.gov/vaccines-blood-biologics/vaccines/vaxneuvance[↩]
- PREVNAR 20. https://www.fda.gov/vaccines-blood-biologics/vaccines/prevnar-20[↩]
- CAPVAXIVE. https://www.fda.gov/vaccines-blood-biologics/capvaxive[↩]
- Centers for Disease Control and Prevention (CDC). Licensure of 13-valent pneumococcal conjugate vaccine for adults aged 50 years and older. MMWR Morb Mortal Wkly Rep. 2012 Jun 1;61(21):394-5. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6121a3.htm[↩]
- PNEUMOVAX 23 – Pneumococcal Vaccine, Polyvalent. https://www.fda.gov/vaccines-blood-biologics/vaccines/pneumovax-23-pneumococcal-vaccine-polyvalent[↩]
- Pneumococcal Vaccination. https://www.cdc.gov/pneumococcal/vaccines/index.html[↩]
- Cillóniz C, Ewig S, Polverino E, Marcos MA, Esquinas C, Gabarrús A, Mensa J, Torres A. Microbial aetiology of community-acquired pneumonia and its relation to severity. Thorax. 2011 Apr;66(4):340-6. doi: 10.1136/thx.2010.143982[↩]
- Large spontaneous pneumothorax. https://radiopaedia.org/cases/large-spontaneous-pneumothorax#image-54418964[↩]
- Bilateral pneumothoraces with deep sulcus sign. https://radiopaedia.org/cases/bilateral-pneumothoraces-with-deep-sulcus-sign#image-51875702[↩]
- Spontaneous pneumothorax due to ruptured apical bullae. https://radiopaedia.org/cases/spontaneous-pneumothorax-due-to-ruptured-apical-bullae-1#image-2441527 [↩]
- Costumbrado J, Ghassemzadeh S. Spontaneous Pneumothorax. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459302[↩][↩]
- Hallifax RJ, Goldacre R, Landray MJ, et al. Trends in the incidence and recurrence of inpatient-treated spontaneous pneumothorax, 1968–2016. JAMA 2018; 320: 1471–1480. doi: 10.1001/jama.2018.14299[↩]
- Hallifax RJ, Goldacre R, Landray MJ, Rahman NM, Goldacre MJ. Trends in the Incidence and Recurrence of Inpatient-Treated Spontaneous Pneumothorax, 1968-2016. JAMA. 2018 Oct 9;320(14):1471-1480. doi: 10.1001/jama.2018.14299[↩]
- Savitsky E, Oh SS, Lee JM. The Evolving Epidemiology and Management of Spontaneous Pneumothorax. JAMA. 2018 Oct 9;320(14):1441-1443. doi: 10.1001/jama.2018.12878[↩]
- MacDuff A, Arnold A, Harvey J; BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010 Aug;65 Suppl 2:ii18-31. doi: 10.1136/thx.2010.136986[↩]
- Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA; AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001 Feb;119(2):590-602. doi: 10.1378/chest.119.2.590[↩]
- Jouneau S, Ricard JD, Seguin-Givelet A, Bigé N, Contou D, Desmettre T, Hugenschmitt D, Kepka S, Le Gloan K, Maitre B, Mangiapan G, Marchand-Adam S, Mariolo A, Marx T, Messika J, Noël-Savina E, Oberlin M, Palmier L, Perruez M, Pichereau C, Roche N, Garnier M, Martinez M. SPLF/SMFU/SRLF/SFAR/SFCTCV Guidelines for the management of patients with primary spontaneous pneumothorax. Ann Intensive Care. 2023 Sep 19;13(1):88. doi: 10.1186/s13613-023-01181-2[↩][↩][↩][↩]
- Louw EH, Shaw JA, Koegelenberg CFN. New insights into spontaneous pneumothorax: A review. Afr J Thorac Crit Care Med. 2021 Mar 9;27(1):10.7196/AJTCCM.2021.v27i1.054. doi: 10.7196/AJTCCM.2021.v27i1.054[↩]
- Walker SP, Bibby AC, Halford P, Stadon L, White P, Maskell NA. Recurrence rates in primary spontaneous pneumothorax: a systematic review and meta-analysis. Eur Respir J. 2018 Sep 6;52(3):1800864. doi: 10.1183/13993003.00864-2018[↩]
- Tan J, Yang Y, Zhong J, Zuo C, Tang H, Zhao H, Zeng G, Zhang J, Guo J, Yang N. Association Between BMI and Recurrence of Primary Spontaneous Pneumothorax. World J Surg. 2017 May;41(5):1274-1280. doi: 10.1007/s00268-016-3848-8[↩]
- Sadikot RT, Greene T, Meadows K, Arnold AG. Recurrence of primary spontaneous pneumothorax. Thorax. 1997 Sep;52(9):805-9. doi: 10.1136/thx.52.9.805[↩]
- Olesen WH, Lindahl-Jacobsen R, Katballe N, Sindby JE, Titlestad IL, Andersen PE, Licht PB. Recurrent Primary Spontaneous Pneumothorax is Common Following Chest Tube and Conservative Treatment. World J Surg. 2016 Sep;40(9):2163-70. doi: 10.1007/s00268-016-3508-z[↩]
- Guo Y, Xie C, Rodriguez RM, Light RW. Factors related to recurrence of spontaneous pneumothorax. Respirology. 2005 Jun;10(3):378-84. doi: 10.1111/j.1440-1843.2005.00715.x[↩]
- Primavesi F, Jäger T, Meissnitzer T, Buchner S, Reich-Weinberger S, Öfner D, Hutter J, Aspalter M. First Episode of Spontaneous Pneumothorax: CT-based Scoring to Select Patients for Early Surgery. World J Surg. 2016 May;40(5):1112-20. doi: 10.1007/s00268-015-3371-3[↩]
- Ganesalingam R, O’Neil RA, Shadbolt B, Tharion J. Radiological predictors of recurrent primary spontaneous pneumothorax following non-surgical management. Heart Lung Circ. 2010 Oct;19(10):606-10. doi: 10.1016/j.hlc.2010.06.663[↩]
- Casali C, Stefani A, Ligabue G, Natali P, Aramini B, Torricelli P, Morandi U. Role of blebs and bullae detected by high-resolution computed tomography and recurrent spontaneous pneumothorax. Ann Thorac Surg. 2013 Jan;95(1):249-55. doi: 10.1016/j.athoracsur.2012.05.073[↩]
- Brown SG, Ball EL, Macdonald SP, Wright C, McD Taylor D. Spontaneous pneumothorax; a multicentre retrospective analysis of emergency treatment, complications and outcomes. Intern Med J. 2014 May;44(5):450-7. doi: 10.1111/imj.12398[↩][↩]
- Chan SS, Rainer TH. Primary spontaneous pneumothorax: 1-year recurrence rate after simple aspiration. Eur J Emerg Med. 2006 Apr;13(2):88-91. doi: 10.1097/01.mej.0000192047.97105.59[↩]
- Ouanes-Besbes L, Golli M, Knani J, Dachraoui F, Nciri N, El Atrous S, Gannouni A, Abroug F. Prediction of recurrent spontaneous pneumothorax: CT scan findings versus management features. Respir Med. 2007 Feb;101(2):230-6. doi: 10.1016/j.rmed.2006.05.016[↩]
- Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraeten A. Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter, prospective, randomized pilot study. Am J Respir Crit Care Med. 2002 May 1;165(9):1240-4. doi: 10.1164/rccm.200111-078OC[↩]
- Brown SGA, Ball EL, Perrin K, Asha SE, Braithwaite I, Egerton-Warburton D, et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020;382(5):405–415. doi: 10.1056/NEJMoa1910775[↩][↩][↩][↩][↩]
- Walker SP, Bibby AC, Halford P, Stadon L, White P, Maskell NA. Recurrence rates in primary spontaneous pneumothorax: a systematic review and meta-analysis. Eur Respir J. 2018;52(3):1800864. doi: 10.1183/13993003.00864-2018[↩][↩]
- Kelly AM, Kerr D, Clooney M. Outcomes of emergency department patients treated for primary spontaneous pneumothorax. Chest. 2008;134(5):1033–1036. doi: 10.1378/chest.08-0910[↩]
- Andrivet P, Djedaini K, Teboul JL, Brochard L, Dreyfuss D. Spontaneous pneumothorax. Comparison of thoracic drainage vs immediate or delayed needle aspiration. Chest. 1995;108(2):335–339. doi: 10.1378/chest.108.2.335[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Vuillard C, Dib F, Achamlal J, Gaudry S, Roux D, Chemouny M, et al. Longer symptom onset to aspiration time predicts success of needle aspiration in primary spontaneous pneumothorax. Thorax. 2019;74(8):780–786. doi: 10.1136/thoraxjnl-2019-213168[↩][↩][↩][↩]
- Ayed AK, Chandrasekaran C, Sukumar M. Aspiration versus tube drainage in primary spontaneous pneumothorax: a randomised study. Eur Respir J. 2006;27(3):477–482. doi: 10.1183/09031936.06.00091505[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Thelle A, Gjerdevik M, SueChu M, Hagen OM, Bakke P. Randomised comparison of needle aspiration and chest tube drainage in spontaneous pneumothorax. Eur Respir J. 2017;49(4):1601296. doi: 10.1183/13993003.01296-2016[↩][↩][↩][↩]
- Harvey J, Prescott RJ. Simple aspiration versus intercostal tube drainage for spontaneous pneumothorax in patients with normal lungs. British thoracic society research committee. BMJ. 1994;309(6965):1338–1339. doi: 10.1136/bmj.309.6965.1338[↩][↩][↩][↩][↩]
- Korczynski P, Gorska K, Nasilowski J, Chazan R, Krenke R. Comparison of small bore catheter aspiration and chest tube drainage in the management of spontaneous pneumothorax. Adv Exp Med Biol. 2015;866:15–23. doi: 10.1007/5584_2015_146[↩][↩][↩][↩][↩][↩]
- Camuset J, Laganier J, Brugiere O, Dauriat G, Jebrak G, Thabut G, et al. Needle aspiration as first-line management of primary spontaneous pneumothorax. Presse Med. 2006;35(5 Pt 1):765–768. doi: 10.1016/s0755-4982(06)74687-5[↩]
- Chen JS, Tsai KT, Hsu HH, Yuan A, Chen WJ, Lee YC. Intrapleural minocycline following simple aspiration for initial treatment of primary spontaneous pneumothorax. Respir Med. 2008;102(7):1004–1010. doi: 10.1016/j.rmed.2008.02.006[↩][↩]
- Nishiuma T, Ohnishi H, Katsurada N, Yamamoto S, Yoshimura S, Kinami S. Evaluation of simple aspiration therapy in the initial treatment for primary spontaneous pneumothorax. Intern Med. 2012;51(11):1329–1333. doi: 10.2169/internalmedicine.51.6919[↩][↩]
- Chan SS, Lam PK. Simple aspiration as initial treatment for primary spontaneous pneumothorax: results of 91 consecutive cases. J Emerg Med. 2005;28(2):133–138. doi: 10.1016/j.jemermed.2004.11.001[↩][↩]
- Ho KK, Ong ME, Koh MS, Wong E, Raghuram J. A randomized controlled trial comparing minichest tube and needle aspiration in outpatient management of primary spontaneous pneumothorax. Am J Emerg Med. 2011;29(9):1152–1157. doi: 10.1016/j.ajem.2010.05.017[↩][↩][↩][↩][↩][↩][↩][↩]
- MacDuff A, Arnold A, Harvey J, Group BTSPDG Management of spontaneous pneumothorax: British thoracic society pleural disease guideline 2010. Thorax. 2010;65(Suppl 2):18–31. doi: 10.1136/thx.2010.136986[↩]
- Tschopp JM, Bintcliffe O, Astoul P, Canalis E, Driesen P, Janssen J, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J. 2015;46(2):321–335. doi: 10.1183/09031936.00219214[↩]
- Parlak M, Uil SM, van den Berg JW. A prospective, randomised trial of pneumothorax therapy: manual aspiration versus conventional chest tube drainage. Respir Med. 2012;106(11):1600–1605. doi: 10.1016/j.rmed.2012.08.005[↩][↩][↩]
- Ganaie MB, Maqsood U, Lea S, Bankart MJ, Bikmalla S, Afridi MA, et al. How should complete lung collapse secondary to primary spontaneous pneumothorax be managed? Clin Med (Lond) 2019;19(2):163–168. doi: 10.7861/clinmedicine.19-2-163[↩][↩]
- Chan JW, Ko FW, Ng CK, Yeung AW, Yee WK, So LK, Lam B, Wong MM, Choo KL, Ho AS, Tse PY, Fung SL, Lo CK, Yu WC. Management of patients admitted with pneumothorax: a multi-centre study of the practice and outcomes in Hong Kong. Hong Kong Med J. 2009 Dec;15(6):427-33. https://www.hkmj.org/system/files/hkm0912p427.pdf[↩][↩]
- Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraeten A. Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter, prospective, randomized pilot study. Am J Respir Crit Care Med. 2002;165(9):1240–1244. doi: 10.1164/rccm.200111-078OC[↩][↩][↩][↩]
- Ramouz A, Lashkari MH, Fakour S, Rasihashemi SZ. Randomized controlled trial on the comparison of chest tube drainage and needle aspiration in the treatment of primary spontaneous pneumothorax. Pak J Med Sci. 2018;34(6):1369–1374. doi: 10.12669/pjms.346.16126[↩][↩][↩][↩]
- Kim IH, Kang DK, Min HK, Hwang YH. A prospective randomized trial comparing manual needle aspiration to closed thoracostomy as an initial treatment for the first episode of primary spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg. 2019;52(2):85–90. doi: 10.5090/kjtcs.2019.52.2.85[↩][↩][↩]
- Contou D, Razazi K, Katsahian S, Maitre B, Mekontso-Dessap A, Brun-Buisson C, et al. Small-bore catheter versus chest tube drainage for pneumothorax. Am J Emerg Med. 2012;30(8):1407–1413. doi: 10.1016/j.ajem.2011.10.014[↩]
- Carson-Chahhoud KV, Wakai A, van Agteren JE, Smith BJ, McCabe G, Brinn MP, et al. Simple aspiration versus intercostal tube drainage for primary spontaneous pneumothorax in adults. Cochrane Database Syst Rev. 2017;9:CD004479. doi: 10.1002/14651858.CD004479.pub3[↩]
- Olesen WH, Katballe N, Sindby JE, Titlestad IL, Andersen PE, Lindahl-Jacobsen R, et al. Surgical treatment versus conventional chest tube drainage in primary spontaneous pneumothorax: a randomized controlled trial. Eur J Cardiothorac Surg. 2018;54(1):113–121. doi: 10.1093/ejcts/ezy003[↩]
- Hofmann HS, Suttner T, Neu R, Potzger T, Szoke T, Grosser C, et al. Burden between undersupply and overtreatment in the care of primary spontaneous pneumothorax. Thorac Cardiovasc Surg. 2018;66(7):575–582. doi: 10.1055/s-0037-1609011[↩]
- Divisi D, Di Leonardo G, Crisci R. Video-assisted thoracic surgery versus pleural drainage in the management of the first episode of primary spontaneous pneumothorax. Am J Surg. 2015;210(1):68–73. doi: 10.1016/j.amjsurg.2014.10.025[↩]
- Torresini G, Vaccarili M, Divisi D, Crisci R. Is video-assisted thoracic surgery justified at first spontaneous pneumothorax? Eur J Cardiothorac Surg. 2001;20(1):42–45. doi: 10.1016/s1010-7940(01)00679-0[↩]
- Chen JS, Hsu HH, Tsai KT, Yuan A, Chen WJ, Lee YC. Salvage for unsuccessful aspiration of primary pneumothorax: thoracoscopic surgery or chest tube drainage? Ann Thorac Surg. 2008;85(6):1908–1913. doi: 10.1016/j.athoracsur.2008.02.038[↩]
- Al-Mourgi M, Alshehri F. Video-Assisted Thoracoscopic Surgery for the Treatment of First-Time Spontaneous Pneumothorax versus Conservative Treatment. Int J Health Sci (Qassim). 2015 Oct;9(4):428-32. https://pmc.ncbi.nlm.nih.gov/articles/PMC4682597[↩]
- Outpatient Management of Primary Spontaneous Pneumothorax: Pigtail Catheter With Unidirectional Valve vs. Exsufflation, Randomized Prospective Study (PNEUM-AMBU). https://clinicaltrials.gov/study/NCT03691480[↩]
- Sale A, Sohier L, Campion M, Le Ho R, Bazin Y, Gangloff C, et al. Exclusive ambulatory management of spontaneous pneumothorax with pigtail catheters, a prospective multicentric study. Respir Med. 2020;166:105931. doi: 10.1016/j.rmed.2020.105931[↩][↩][↩][↩][↩]
- Voisin F, Sohier L, Rochas Y, Kerjouan M, Ricordel C, Belleguic C, et al. Ambulatory management of large spontaneous pneumothorax with pigtail catheters. Ann Emerg Med. 2014;64(3):222–228. doi: 10.1016/j.annemergmed.2013.12.017[↩][↩][↩][↩][↩]
- Hallifax RJ, McKeown E, Sivakumar P, Fairbairn I, Peter C, Leitch A, et al. Ambulatory management of primary spontaneous pneumothorax: an open-label, randomised controlled trial. Lancet. 2020;396(10243):39–49. doi: 10.1016/S0140-6736(20)31043-6[↩][↩][↩]
- Massongo M, Leroy S, Scherpereel A, Vaniet F, Dhalluin X, Chahine B, et al. Outpatient management of primary spontaneous pneumothorax: a prospective study. Eur Respir J. 2014;43(2):582–590. doi: 10.1183/09031936.00179112[↩][↩][↩][↩]
- Hassani B, Foote J, Borgundvaag B. Outpatient management of primary spontaneous pneumothorax in the emergency department of a community hospital using a small-bore catheter and a Heimlich valve. Acad Emerg Med. 2009;16(6):513–518. doi: 10.1111/j.1553-2712.2009.00402.x[↩][↩][↩]
- Marjański T, Sowa K, Czapla A, Rzyman W. Catamenial pneumothorax – a review of the literature. Kardiochirurgia i Torakochirurgia Polska = Polish Journal of Cardio-Thoracic Surgery. 2016;13(2):117-121. doi:10.5114/kitp.2016.61044. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4971265/[↩][↩][↩]
- Rousset-Jablonski C, Alifano M, Plu-Bureau G, Camilleri-Broet S, Rousset P, Regnard JF, Gompel A. Catamenial pneumothorax endometriosis-related pneumothorax: clinical features and risk factors. Hum Repord. 2011;26:2322–2329. https://www.ncbi.nlm.nih.gov/pubmed/21685141[↩][↩]
- Alifano M, Legras A, Rousset-Jablonski C, Bobbio A, Magdeleinat P, Damotte D, Roche N, Regnard JF. Pneumothorax recurrence after surgery in women: clinicopathologic characteristic and management. Ann Thorac Surg. 2011;92:322–326. https://www.ncbi.nlm.nih.gov/pubmed/21718864[↩][↩][↩]
- Majak P, Langebrekke A, Hagen OM, Qviqstad E. Catamenial pneumothorax, clinical manifestations – a multidisciplinary challenge. Pneumonol Alergol Pol. 2011;79:347–350. https://www.ncbi.nlm.nih.gov/pubmed/21861259[↩]
- Yoshioka H, Fukui T, Mori S, Usami N, Nagasaka T, Yokoi K. Catamenial pneumothorax in a pregnant patient. Jpn J Thorac Cardiovasc Surg. 2005;53:280–282. https://www.ncbi.nlm.nih.gov/pubmed/15952324[↩]
- Channabasavaiah AD, Joseph JV. Thoracic endometriosis: revisiting the association between clinical presentation and thoracic pathology based on thoracoscopic findings in 110 patients. Medicine (Baltimore) 2010;89:183–188. https://www.ncbi.nlm.nih.gov/pubmed/20453605[↩][↩][↩]
- Joseph J, Sahn SA. Thoracic endometriosis syndrome: new observation from an analysis of 110 cases. Am J Med. 1996;100:164–170. https://www.ncbi.nlm.nih.gov/pubmed/8629650[↩]
- Attaran S, Bille A, Karenovics W, Lang-Lazdunski L. Videothoracoscopic repair of diaphragm and pleurectomy/abrasion in patients with catamenial pneumothorax: a 9-year experience. Chest. 2013;143:1066–1069. https://www.ncbi.nlm.nih.gov/pubmed/23117231[↩]
- Haga T, Kurihara M, Kataoka H, Ebana H. Clinical-pathological findings of catamenial pneumothorax: comparison between recurrent cases and non-recurrent cases. Ann Thorac Cardiovasc Surg. 2014;20:202–206. https://www.jstage.jst.go.jp/article/atcs/20/3/20_oa.12.02227/_pdf/-char/en[↩][↩][↩]
- Visouli AN, Darwiche K, Mpakas A, Zarogoulidis P, Papagiannis A, Tsakiridis K, Machairiotis N, Stylianaki A, Katsikogiannis N, Courcoutsakis N, Zarogoulidis K. Catamenial pneumothorax: a rare entity? Report of 5 cases and review of the literature. J Thorac Dis. 2012;4(Suppl 1):17–31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3537379/[↩]
- Rezende-Neto JB, Hoffmann J, Al Mahroos M, et al. Occult pneumomediastinum in blunt chest trauma: clinical significance. Injury. 2010 Jan. 41(1):40-3.[↩]
- Hilliard NJ, Marciniak SJ, Babar JL, Balan A. Evaluation of secondary spontaneous pneumothorax with multidetector CT. Clin Radiol. 2013;68(5):521–528. doi: 10.1016/j.crad.2012.10.008[↩]
- Frankel HL, Kirkpatrick AW, Elbarbary M, Blaivas M, Desai H, Evans D, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically Ill patients-Part I: general ultrasonography. Crit Care Med. 2015;43(11):2479–2502. doi: 10.1097/CCM.0000000000001216[↩]
- Tasci O, Hatipoglu ON, Cagli B, Ermis V. Sonography of the chest using linear-array versus sector transducers: correlation with auscultation, chest radiography, and computed tomography. J Clin Ultrasound. 2016;44(6):383–389. doi: 10.1002/jcu.22331[↩]
- Bagan P, Berna P, Assouad J, Hupertan V, Le Pimpec Barthes F, Riquet M. Value of cancer antigen 125 for diagnosis of pleural endometriosis in females with recurrent pneumothorax. Eur Respir J. 2008;31:140–142. http://erj.ersjournals.com/content/31/1/140.long[↩]